Cardiovascular
A 74-year-old man presents to your office for a routine He has no present complaint His medical history is significant for right knee osteoarthritis He takes naproxen occasionally, to relieve knee pain. He does not smoke or consume alcohol His BP is 165/75 mm Hg and PR is 70/min. The physical examination showed a mild systolic ejection type murmur at the base of the heat to the right. An E-KG revealed left ventricular hypertrophy and secondary ST segment and T wave change Moderate left ventricular hypertrophy, without any flow abnormalities, was demonstrated on echocardiography. The ejection fraction was 60%. What is the most probable cause of hypertension in this patient?
Rigidity of the arterial wall
Elevated plasma renin activity
Aortic insufficiency
Increased cardiac output
Increased intravascular volume
A 32-year-old Caucasian female comes to the physician because of a one-week history of fatigue, progressive worsening of shortness of breath and swelling of feet. She denies any chest pain She has no other medical problems except a recent cold two weeks ago. She is not taking any medication Her temperature is 36 7 C (98 F), blood pressure is 110/65 mmHg, pulse is g0/min, and respirations are 20/min Bilateral basal crackles, elevated jugular venous pressure, and 2+ bilateral pitting edema of the ankles are noted Complete blood count is unremarkable. Transthoracic echocardiogram of her heat will most likely show?
Concentric hypertrophy of the heart
Eccentric hypertrophy of the heart
Mitral stenosis
Hypokinesia of the inferior wall
Dilated ventricles with diffuse hypokinesia
A 47-year-old woman loses consciousness for 2 minutes while shopping in a supermarket. In the emergency room, she recounts feeling nausea and warmth spreading over her body immediately before passing out She has never had a similar episode before. She has not seen a doctor for several years and does not take any medications, nor does she use tobacco, alcohol or drug. Her family history is unremarkable. Which of the following most likely caused this episode?
Cardiac arrythmia
Seizure
Neurocardiogenic syncope
Heat valve disease
Orthostatic hypotension
A 25-year-old woman experiences sudden-onset palpitations and generalized weakness. During this episode, her blood pressure is 100/60 mmHg and her heat rate is 160/min and regular. She has no significant past medical history and does not take any medications She reports having a few similar episodes in the past which she has self-treated by immersing her face in cold water Generally, she says, cold water immersion relieves her symptoms within several minutes. This cold water therapy works by affecting which of the following?
Vascular tone
Sinoatrial node automatism
Atrioventricular node conductivity
Purkinje fiber conduction
Ventricular myocardium contractility
A 67-year-old man is evaluated for hypertension He complains of occasional morning headaches. His past medical history is also significant for type 2 diabetes mellitus, coronary artery disease, and a stroke with residual left-sided weakness. He underwent coronary artery bypass surgery seven years ago and carotid endarterectomy five years ago. His current medication list includes lisinopril hydrochlorothiazide, amlodipine, metoprolol, aspirin, metformin and glyburide His blood pressure is 190/120 mmHg on the right arm and 170/110 mmHg on the left arm. His heat rate is 65/min Physical examination reveals a periumbilical systolic-diastolic bruit. The latter finding is best explained by which of the following?
Abdominal aortic aneurysm
Aortic dissection
Aortic coarctation
Renal artery stenosis
Aorto-enteric fistula
A 67-year-old male is brought to the emergency department after a syncopal episode. He lost consciousness while shopping in the mall. He denies any nausea, diaphoresis, chest pain, or shortness of breath. He has had two episodes of lightheadedness over the last month but has not seen a doctor. His past medical history is significant for long-standing hypertension, which is being treated with enalapril. His blood pressure is 135/90 mmHg while supine, and 130/85 mmHg while standing His heat rate is 64/min ECG shows a sinus rhythm with high voltage, prolonged PR interval, prolonged QRS interval, normal QT interval and occasional premature ventricular contractions (PVC) E-chocardiography reveals left ventricular hypertrophy and an ejection fraction (EF) of 55% Which of the following is the most likely cause of this patient's syncope?
Bradyarrhythmia
Decreased myocardial contractility
Torsades de pointes
Autonomic dysfunction
Ventricular premature beats
A 60-year-old male is 2 days status post primary percutaneous coronary intervention (PCI) with stent placement. He had previously suffered from an antero-lateral myocardial infarction. His cardiac enzymes have been trending down since admission He has recovered well and is ready for discharge He is currently asymptomatic. His temperature is 37.5 C (99.5 F), blood pressure is 130/70 mm Hg, pulse is 66/min, and respirations are 14/min He is discharged with instructions to take the following medications aspirin simvastatin, lisinopril metoprolol and sublingual nitroglycerine. In addition to the medications listed above, which of the following medications should this patient also be taking after discharge?
Isosorbide mononitrate
Low molecular weight heparin
Waffarin
Clopidogrel
Amlodipine
A 47-year-old male presents to your office with a two-month history of lethargy and decreased libido His medical records reveal that he has been treated for joint pain and swelling over the last six months and was diagnosed with diabetes mellitus one year ago Physical examination reveals hepatomegaly and testicular atrophy Which of the following cardiac abnormalities is most likely to also be present in this patient?
Atrial septal defect
Aortic stenosis
Hypertrophic cardiomyopathy
Cardiac conduction block
Endocardial fibroelastosis
A 35-year-old Caucasian male is being evaluated for poor exercise tolerance and muscle weakness He has no past medical history His blood pressure ranges from 175-185 mmHg systolic and 105-1 15 mmHg diastolic on repeat measurement His heat rate is 78-g5/min His serum chemistry is significant for blood glucose of 95 mg/dL serum creatinine of 0.7mg/dL serum Na of 146 mEq/L and serum K of 2.4 mEq/l_ CT scan of the abdomen reveals a 3 cm mass in the left adrenal gland. Which of the following additional findings would you expect in this patient? Plasma renin activity, Serum aldosterone, Serum bicarbonate A High
High High Low
High High High
Low High High
Low High Low
High Low High
A 67-year-old homeless male presents 24 hours after the onset of substernal chest pain and is diagnosed with an anterior wall myocardial infarction. There is no history of previous chest pain, dyspnea, palpitations, syncope or leg swelling. He has no hypertension or diabetes mellitus. He does acknowledge a 40 pack-year smoking history. Upon discharge, echocardiography shows normal left ventricular size, left ventricular anterior wall hypokinesis and an ejection fraction of 50%. Two years later, the patient is found dead in the street. Autopsy reveals a dilated left ventricle with a globular shape and thinned walls along with a scar on the anterior wall. Which of the following would have most likely prevented this patient's pathologic findings?
Aspirin
Enalapril
Amlodipine
Isosorbide dinitrate
Digoxin
A 50-year-old woman presents to your office complaining of lower extremity edema that stated several weeks ago, and slowly progressed thereafter. Her past medical history is significant for hypertension, treated with metoprolol for 2 years. Amlodipine was added recently because of inadequate control of BP with metoprolol alone. She does not smoke or consume alcohol. She has no known drug allergies. Her blood pressure is 130/80mm Hg and her heart rate is 64/min. The physical examination reveals bilateral symmetric 3+ pitting edema of both lower extremities, without any skin changes or varicosities Her neck vein pulsation is normal. Other physical findings are within normal limits. Her laboratory studies reveal the following: Serum albumin 4.5 g/dL Total serum bilirubin 0.8 mg/dL Serum sodium 140 mEq/L Serum potassium 4.0 mEq/L Serum creatinine 0.8 mg/dL Urinalysis is within normal limite. What is the most likely cause of the edema in this patient?
Heart failure
Liver disease
Renal disease
Venous insufficiency
Side effect of her medications
A 64-year-old male who has not seen a doctor for the past 20 years presents to the emergency room with excruciating chest pain that stated suddenly about three hours ago. He describes the pain as tearing in quality and says that it radiates to his back. On physical examination, you hear an early diastolic decrescendo murmur at the sternal border. Chest x ray shows widening of the superior mediastinum. EKG is normal. Which of the following medical conditions most likely accounts for this patients presentation?
Systemic hypertension
Marfan's syndrome
Ehlers-Darlos syndrome
Bicuspid aortic valve
Giant cell arteritis
A 40-year-old female presents to the emergency room with palpitations and lightheadedness of acute onset. Also, she has experienced insomnia, fatigability, and weight loss lately. She does not smoke or consume alcohol. She is not taking any medication. Her blood pressure is 110/80 mmHg and heat rate is 120/min, irregular. Physical examination reveals lid lag and fine tremor of the outstretched hands. ECG shows atrial fibrillation with rapid ventricular response. What is the next best step in the management of this patient?
Digoxin
Propranolol
Lidocaine
Quinidine
Immediate cardioversion
A 43-year-old Caucasian man with a two-year history of diabetes mellitus presents to your office for a routine. He has no complaint His medications are metformin and aspirin. He works as a computer programmer and has a sedentary lifestyle. He drinks one to two cans of beer on weekends and smokes one pack of cigarettes per day. On physical examination, his blood pressure is 153/94 mm Hg and his heat rate is 82/min His BMI is 32.5 kg/m2. The remainder of the physical examination is unremarkable Laboratory studies reveal an HbA1c of 7.6%. At his check-up one month ago, his blood pressure was 149/92 mmHg. Which of the following interventions would be most effective for controlling his blood pressure?
Aerobic exercise
Weight loss
Smoking cessation
Better diabetes control
Quitting alcohol
A 38-year-old woman presents to the emergency room complaining of chest pain for the past several hours She describes it as sharp, centrally located and non-radiation. The pain worsens somewhat with inspiration and movement. The patient denies having fevers, chills, dyspnea, swelling, or difficulty breathing at night. She says she first noticed the pain while exercising three weeks ago, but has experienced it at rest as well. She says that she has been exercising heavily in an attempt to lose weight. Her BMI is currently 34kg/m2. Her father had a myocardial infarction at age 60. Her medical history is significant for two normal vaginal deliveries. She smokes a half-pack of cigarettes daily. On physical examination, her blood pressure is 112/69 mm Hg and her heat rate is 72/min. Cardiac exam reveals a regular Sl and S2 without extra sounds or murmurs There is tenderness to palpation over the sternum. What is the most likely cause of her chest pain?
Gastroesophageal reflux disease
Pulmonary embolism
Unstable angina
Ericarditis
Costochondritis
A 63-year-old man presents to the ER with substernal chest pain and diaphoresis. The pain stated one hour ago and did not remit with antacids. He has a past medical history of asthma for which he uses inhaled fluticasone and peptic ulcer disease for which he takes omeprazole. His family history is significant for prostate cancer in his father and breast cancer in his mother. Physical examination reveals a blood pressure of 160/100 mmHg and a heat rate of 90/min. A bruit is heard over the right carotid artery and a mild systolic murmur is present at the cardiac apex Sublingual nitroglycerin and aspirin are administered in the. Within minutes, the patient reports decreased pain. Which of the following most likely accounts for this improvement in his symptoms?
Increased left ventricular compliance
Decreased left ventricular volume
Decreased left ventricular contractility
Increased systemic afterload
Increased cardiac preload
A 38-year-old female comes to your office complaining of occasional palpitations She describes feeling a fast and irregular heartbeat Over the past two months, she has had three such episodes, each lasting about two hours She denies any associated chest pain, shortness of breath cough or ankle swelling. She drinks alcohol on social occasions and does not smoke cigarettes She has no other medical problems and is not taking any medications On physical examination, her temperature is 37.1 C (98.9F), pulse is 80/min, blood pressure is 130/70mmHg, and respirations are 14/min. On auscultation of her heat the apical impulse is displaced and there is an S3. You also hear a pansystolic murmur, which is loudest at the apex and radiates to the axilla. Which of the following is the most likely cause of her symptoms?
Mitral valve prolapse
Myocardial ischemia
Rheumatic heat disease
Mitral annular calcification
Infective endocarditis
A 42-year-old woman is evaluated for depression, mood swings and poor. She also complains of mild headaches and muscle weakness. She has had two ER Visits for kidney stones over the past year. She denies any illicit drug use. Her blood pressure is 160/105 mmHg and her heat rate is 85/min. Her laboratory findings are shown below: Sodium 140mEq/L Potassium 3.6 mEq/L Chloride 101 mEq/L Bicarbonate 24 mEq/L BUN 13 mEq/L Creatinine 0.9 mEq/L Glucose 98 mEq/L Calcium 11.7 mg/dL Which of the following is the most likely cause of this patient's hypertension?
Renal parenchymal disease
Renal vascular stenosis
Aortic dissection
Hypothyroidism
Hypothyroidism E. Parathyroid gland disease
A 14-year-old African American male is referred to your office after his older brother experienced sudden cardiac arrest during hiking trip. He has no current complaints. He denies any illicit drug use His blood pressure is 110/60 mmHg and his heat rate is 75/min. Neck is supple, no jugular venous distention is appreciated. Carotid pulse seems to have dual upstroke. Lungs are clear. There is strong apical impulse and a systolic ejection type murmur along the left sternal border. Which of the following is most likely to increase the murmur intensity in this patient?
Squatting
Valsalva maneuver
Sustained handgrip
Recumbency
Leg raising
A 60-year-old male is brought to ER by his son because he had an episode of syncope. He was watching TV in an arm-chair when suddenly lost his consciousness without any warning sign. He had several clonic jerks while unconscious He never had such an episode before. His past medical history is significant for acute myocardial infarction six months ago and well-controlled hypertension. His current medications include captopril metoprolol hydrochlorothiazide, clopidogrel and aspirin. His blood pressure is 130/85 mmHg and heat rate is 80/min with frequent ectopic beat. Physical examination revealed mild holosystolic apical murmur radiating to the axilla. Which of the following is the most probable pathophysiologic mechanism for his syncopal episode?
Vasovagal reaction
Arrhythmia
Autonomic dysfunction
Seizure
Postural hypotension
A 45-year-old recently immigrated Mexican farmer comes to your office complaining of dyspnea, fatigue and abdominal distention for the past two months. On physical exam, his temperature is 37 C (98F), blood pressure is 126/80 mmHg, pulse is 80/min, and respirations are16/min. You note pedal edema, elevated jugular venous pressure with positive Kussmaul's sign, and increased abdominal girth with free fluid. Chest auscultation reveals decreased heart sound intensity at the apex and an early heart sound following S2 The jugular venous pressure tracing shows prominent 'x and 'y' descents. Which of the following is the most likely cause of this patient's symptoms?
Cor pulmonale
Tuberculosis
Trypanosoma cruzi infection
Psittacosis
Pneumoconiosis
A 25-year-old G2, PI at 28 weeks gestation is brought to the emergency department by her boyfriend, who found her lying on her bed in a pool of blood She is very drowsy, but denies any pain or uterine contractione Her temperature is 38 C (100.4 F) and respirations are 18/min Physical examination is suggestive of a transverse lie Inspection of the perineum reveals gross blood and active bleeding per vagina. Which of the following set of parameters would most likely be seen in this patient? CO PCWP SVR BP HR Set A Decreased Increased Increased Decreased Increased set B Decreased Decreased Increased Decreased Decreased Set C Decreased Decreased Increased Decreased Increased set D Decreased Decreased Decreased Decreased Increased set E Increased Decreased Increased Decreased Increased
Set A
Set B
Set C
Set D
Set E
A 54 year-old male comes to the physician because of abdominal distention He thinks his big belly is making it hard for him to breathe He received radiation therapy for Hodgkin lymphoma several years ago and was told that he is cured He drinks alcohol on a regular basis His temperature is 36.7C (98F), blood pressure is 120/76 mm Hg, pulse is 80/min and respirations are 20/min Examination shows a jugular venous pressure7 cm above the sternal angle Dullness to percussion and decreased breath sounds are noted in the right lung base The abdomen is quite distended with an obvious fluid wave Mild hepatomegaly is present Extremities have 2+ lower extremity edema. Initial laboratory studies are shown below: Serum creatinine 08 mg/dL Alburnin 4.0 mg/dL Total bihrubin 1.0 mg/dl Prothrombin time 11 sec Urinalysis is within normal limits. Which of the following is the most likely cause of his condition?
Urinary protein loss
Portal vein thrombosis
Portal vein compression
Inelastic pericardium
Thoracic duct obstruction
A 32-year-old woman presents with progressively worsening dyspnea on exertion one month after returning from a vacation in Texas. She says that her symptoms have progressed to the point that she now wakes during the night with a choking sensation that improves only with sitting up. Recently her shortness of breath has required her to significantly limit her physical activity. She denies having associated chest pain, skin rash or joint pain She has no significant past medical history. Family history is significant for thyroid cancer in her aunt and lung cancer in her father, a heavy smoker. On physical examination, her temperature is 37.20C (99 F), pulse is g6/min, blood pressure is 110/70 mmHg, and respirations are 14/min. Bilateral pitting ankle edema is present. Her liver is enlarged 2 cm below the right costal marginal. Lung auscultation reveals decreased breath sounds at the bilateral bases. Cardiac exam reveals the presence of a third heat sound. Chest x ray shows an enlarged cardiac silhouette and small bilateral pleural effusion. EKG is unremarkable. Which of the following is the most likely cause of her symptoms?
Atherosclerosis
Viral infection
Lyme disease
Coccidioidomycosis
Autoimmune disease
A 45-year-old mildly overweight male recovering from an anterior wall myocardial infarction develops sudden onset of sharp pain in the left side of his chest He presented five days earlier with substernal chest pain and diaphoresis. He has had no dyspnea, extremity swelling or palpitations since admission. His past medical history is significant for diabetes mellitus type 2. He seems mildly restless, especially in the supine position. The pain improves when sitting up and leaning forward. His breathing is fast and shallow due to the pain. His lungs are clear on auscultation. His blood pressure is 120/78 mmHg and his heart rate is 60/min There is no change in blood pressure upon deep inspiration. ECG shows sinus rhythm with new diffuse ST segment elevation. Which of the following is the most likely diagnosis?
Interventricular wall rupture
Ventricular free wall rupture
Pulmonary infarction
Recurrent ischemia
Acute pericarditis
An 88-year-old female nursing home resident is brought to the hospital with a one-week history of moaning, decreased oral intake and decreased ambulation. Physical examination reveals a very thin female who is moaning and appears to be in pain. She opens her eyes spontaneously but does not respond to questions. Her blood pressure is 75/43 mmHg, pulse is 105/min, temperature is 35.5°C (96°F), and respirations are 22/min. Oxygen saturation (pulse oximetry) is 97% on room air. Her skin and oral mucosa are dry and her neck veins are flat. There is no lymphadenopathy. On chest auscultation, there are crackles in the right upper lung lobe. Abdomen is soft and non-distended. There is 2+ pitting presacral and lower extremity edema, and a deep pressure ulcer in the sacral area. Laboratory analysis reveals the following: Sodium 155mEq/L Potassium 5.3 mEq/L Glucose 88mg/dL Bicarbonate 14mEq/L BUN 151mg/dL Creatinine 3.1mg/dl Which of the following is the most likely cause of her lower extremity edema?
Increased plasma hydrostatic pressure
Decreased plasma oncotic pressure
Renal water and sodium retention
Increased interstitial oncotic pressure
Decreased lymphatic drainage
A 64-year-old man complains of palpitations and progressive shortness of breath over the past several hours. He says that he also develops a choking sensation every time he tries to lie down. His medical history is significant for hypertension for the past 20 years and medication non-compliance. He also has a 35-year smoking history. He reports that his father died of a heart attack at age 70 and his mother suffered from asthma. On physical examination, his blood pressure is 170/100 mmHg and his heat rate is 130/min and irregularly irregular. Lung exam reveals bibasilar crackles. There is 2+ pitting edema of the lower extremities. Bedside echocardiography shows a left ventricular ejection fraction of 55%. Which of the following is most likely responsible for his symptoms?
Cardiogenic shock
Diastolic dysfunction
High-output heat failure
Small airway bronchoconstriction
Increased lung compliance
A 22-year-old Caucasian male is evaluated for an episode of syncope that occurred while playing soccer It lasted only 2 minutes without any post-syncopal confusion, sleepiness or weakness. He had prior episodes of dizziness while playing active sports as well as vague chest discomfort. His uncle died suddenly at a young age. Auscultation of his precordium reveals a III/IV systolic murmur along the left sternal border. The patient is most likely to benefit from which of the following medications?
Nitrates
Beta-blockers
Disopyramide
Amlodipine
Digitalis
A 55-year-old Caucasian male presents to your office with muscle pain of recent onset. His past medical history is significant for hypertension and an acute myocardial infarction experienced 2 months ago. His current medications include metoprolol captopril, aspirin and simvastatin. His blood pressure is 130/80 mmHg and heat rate is 60/min Liver function tests are slightly abnormal. Serum creatine kinase level is elevated. You suspect a drug-induced reaction. Which of the following is the most possible mechanism of drug-induced reaction in this patient?
Immune-mediated reaction
Cell surface receptor blockage
Extracellular enzyme blockage
Synthetic reaction inhibition
Damage of membrane-bound lipids
A 40-year-old male presents with six months of worsening dyspnea. His symptoms have progressed to the point that walking even one block causes him to become shot of breath. He has a history of cigarette smoking, but quit 10 years ago. He drinks approximately one alcoholic drink daily. His medical history is significant for peptic ulcer disease for which he takes antacids. On physical examination, he is afebrile. His pulse is 86/min, blood pressure is 140/56 mmHg, and respiratory rate is 14/min While examining his heat you note a high-pitched blowing, early diastolic, decrescendo murmur, which is heard best in the left third intercostal space and is intensified by handgrip. There is prominent cardiomegaly on chest x-ray. Which of the following medications would improve both this patient’s symptoms and cardiomegaly?
Quinidine
Metoprolol
Nifedipine
Ephedrine
Amiodarone
A 70-year-old man is brought to the Emergency Room because he lost his consciousness while working in the garden. He says that he had several episodes of near-syncope on exertion recently. His past medical history is insignificant He is not taking any medications. His blood pressure is 110/85 mmHg and heat rate is 80/min. Point of maximal impulse is increased in intensity. Cardiac auscultation reveals ejection type systolic murmur at the base of the heat with radiation to the carotid arteries. ECG demonstrates left ventricular hypertrophy, and secondary ST segment and T wave change. What is the most probable cause of this patient's condition?
Rheumatic endocarditis
Bacterial endocarditis
Hypertension
Congenital anomaly
Age-related sclerocalcific changes
A 20-year-old female presents to your office for a routine. She has no complaints and her past medical history is insignificant. She is not taking any medications and denies drug abuse. Her blood pressure is 125/65 mmHg and heat rate is 80/min. Cardiac auscultation reveals early diastolic murmur at the left sternal border. What is the next best step in the management of this patient?
Electrocardiogram
Chest x ray
Coronary angiography
Echocardiography
No further work-up
A 23-year-old woman who is 26 weeks pregnant presents to the emergency department with sudden onset severe shortness of breath and inability to lie flat. She recently emigrated from Eastern Europa. Her medical history is significant for recurrent sore throats requiring tonsillectomy as a child. Presently, her blood pressure is 110/60 mmHg and her heart rate is 120/min. An EKG rhythm strip suggests atrial fibrillation. Which of the following is the most likely diagnosis?
Hypertrophic cardiomyopathy
Constrictive pericarditis
Mitral stenosis
Myocardial infarction
Aortic insufficiency
A 68-year-old man is brought to the emergency room after he passed out for one minute during an early morning jog. He was not confused after the episode and did not have bowel or bladder incontinence. He has been having exertional chest pain and shortness of breath for the past few months. He has never had any resting chest pain. He has been healthy except for hypertension, for which he takes hydrochlorothiazide. He has a 20 pack year smoking history and occasionally drinks a glass of wine. His blood pressure is 142/90 mm Hg, pulse is 80/min, and respirations are 16/min. Carotid pulse is delayed S2 is weak and an S4 is present. A grade 3/6 systolic ejection murmur is in the right 2nd intercostal space, radiating to the carotids. Neurological examination reveals no focal findings, and there are no signs of head trauma. An EKG shows left ventricular hypertrophy. The first set of cardiac enzymes is negative. Which of the following is the most appropriate next step in management?
CT scan of the head
Electroencephalogram (EEG)
Exercise stress test
Echocardiogram
CT angiogram of the chest
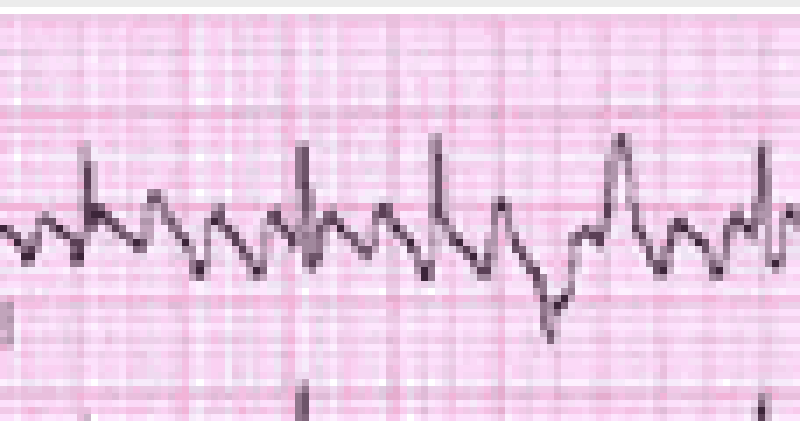
A 72-year-old female is admitted to the ICU with severe chest pain. The initial set of cardiac enzymes is positive and her EKG reveals an anterior wall myocardial infarction. She receives treatment with aspirin clopidogrel, metoprolol nitroglycerine drip, and morphine. Two hours later, her telemetry monitor displays the following rhythm Which of the following is the best next step in managing this patient?
Lidocaine
Defibrillation
Digoxin
Amiodarone
Immediate echocardiogram
A 63-year-old Caucasian female presents to the emergency room with a recent onset of left-sided Weakness. She has been experiencing increased fatigability, low-grade fevers and occasional palpitations over the past two months. She has lost seven pounds during the same period. Her temperature is 37C (98.6 F), pulse is 80/min (regular), blood pressure is 120/76mmHg and respirations are 14/min. Her lungs are clear. Cardiac auscultation reveals normal first and second heat sounds and a mid-diastolic rumble at the apex. Echocardiography shows a mass in the left atrium. Which of the following is the most likely diagnosis?
Congenital heart defect
Infective endocarditis
Intracardiac tumor
Myxomatous valve degeneration
Rheumatic fever and atrial thrombus
A 67-year-old male presents to the ER with chest pain. His medical history is significant for stable angina for which he takes aspirin and isosorbide dinitrate, as well as hypertension and bronchial asthma. Occasionally, he uses an albuterol inhaler. He is admitted to the hospital and five hours later, he begins to feel lightheaded and weak. His blood pressure is 100/60 mmHg. An EKG is obtained and is shown below Which of the following is the best next step in managing this patient?
Cardiac catheterization
Pacemaker insertion
Adenosine
Digoxin
Metoprolol
A 56-year-old male presents with progressively worsening dyspnea and ankle edema. He denies chest pain syncope or palpitations. He does not smoke or drink alcohol. He denies diabetes mellitus, hypertension, or hyperlipidemia. His temperature is 37.1C (98.7F), pulse is 70/min, blood pressure is 136/70mmHg, and respirations are 15/min. Examination shows elevated jugular venous pressure, bilateral ankle edema, and tender hepatomegaly. Chest auscultation shows bibasilar rales. His heat sounds are distant and there is no murmur. Chest x ray shows mild cardiomegaly and a right-sided pleural effusion. ECG shows low voltage QRS complexes and nonspecific ST-T wave changes. Echocardiography shows normal left ventricular volume with symmetrical thickening of the left ventricular walls and slightly reduced systolic function. Which of the following would represent a potentially reversible cause of this patient’s heat disease?
Amyloidosis
Sarcoidosis
Hemochromatosis
Scleroderma
LED
A 43-year-old white male is found to have premature atrial complexes (PACs) on routine EKG. He denies chest pain, shortness of breath or lightheadedness. He has smoked 1-2 packs of cigarettes daily for the past 20 years. He also has a 20-year history of alcoholism, though recently he has limited his use to 1-2 beers/day The patient's family history is significant for a myocardial infarction in his mother at age 65 and a stroke in his father at age 72. He has no personal history of hypertension or diabetes. Physical examination including Vital signs, is entirely within normal limits. What is the best next step in the management of this patient?
Reassurance
24-hour Halter monitoring
Echocardiogram
Start beta-blocker therapy
Advise him to stop alcohol and tobacco
A 60-year-old man is brought to the emergency department due to syncope. He has had similar episodes a few times during the past few weeks. These episodes usually occur after he exerts himself. He does not feel confused or tired after these episodes. He denies any chest pain or palpitation. His wife reports that when he collapses, he seems to lose consciousness for a few seconds, but then is back to being alert right away. She denies any jerking movement. His past medical history is significant diverticulosis, for which he takes fiber supplements. He is not on any other medication. His temperature is 37.1 C (98.8 F), blood pressure is 110/98 mm Hg, pulse is 88/min, and respirations are 14/min. On examination, he has a fourth heart sound and harsh 3/6 systolic murmur, best heard over the right sternal border. The murmur is accentuated on expiration. The lung fields are clear to auscultation. After performing an echocardiograph to confirm the diagnosis, which of the following management options is most appropriate?
Aortic valvotomy
Aortic valve replacement
Close outpatient follow-up with serial echocardiograms
Exercise test looking for arrhythmias
Observe until the patient develops breathlessness
A 12-year-old white male wants to participate in sports at school. He has been growing normally since birth. His immunizations are up-to-date and he is not suffering from any known medical conditions. Which of the following measures should be taken to screen him for underlying heart disease that could cause sudden cardiac death?
No screening is required
History and physical exam
12 lead ECG
Echocardiography
Exercise stress testing
A 55-year-old male presents to the emergency room with right-sided weakness that has persisted for the past several hours. He also complains of severe central chest pain that is "ripping" in quality and radiates to his back. He has had hypertension for the past seven years and has not been taking any anti-hypertensive medication. He has been smoking one pack of cigarettes per day for the past 25 years. His father died of coronary artery disease at age 44 years. His temperature is 37.1C (98.6F), pulse is 78/min, blood pressure is 180/120 mm Hg in the right arm and 110/70 mm Hg in the left arm, and respirations are 16/min. He is diaphoretic and confuse. His neurological examination is significant for decreased power and tone in the right upper and right lower extremities. The rest of his physical examination is unremarkable ECG shows left axis-deviation and a chest x ray is normal. Based on these findings, what is the most likely diagnosis?
Subarachnoid hemorrhage
Hemorrhagic stroke
Paradoxical pulmonary embolism
Myocardial infarction with thromboembolism
Aortic dissection
A 54-year-old man is brought to the ER three hours after the onset of severe, 10/10, tearing, substernal chest pain radiating to his back. He still complains of pain and dizziness at the time of arrival. Physical examination demonstrates a pale thin male who is anxious and diaphoretic. His blood pressure is 90/60 mmHg in the right arm and 70/40 mmHg in the left arm. There is an 18 mmHg difference in systolic blood pressure between inspiration and expiration. His jugular veins are distended while sitting. Bedside echocardiogram demonstrates a moderate amount of pericardial fluid. Which of the following is the most likely diagnosis?
Acute myocardial infarction
Acute pericarditis
Aortic dissection
Pulmonary embolism
Tension pneumothorax
A 46-year-old man collapsed while getting out of his bed. He has been feeling weak over the last several days and has complained of vague chest discomfort. He ascribed the symptoms to a recent respiratory infection and did not visit a doctor. His mother died of a stroke and his father suffered from recurrent myocardial infarctions. He eats a balanced diet and takes a multivitamin daily. His most recent blood cholesterol level was 200 mg/dl. An ECG strip taken by EMS is shown below. Which of the following is the best initial management of this patient?
Procainamide
Synchronized DC cardioversion
Thrombolytic therapy
Beta-blockers and aspirin
Pericardiocentesis
A 59-year-old male suffers a myocardial infarction. He is treated medically and is discharged home ten dayslater on aspirin, atorvastatin, metoprolol, lisinopril, and sublingual nitroglycerin. One month later, he presentsto your office for a follow-up visit. He denies chest pain, dyspnea or lightheadedness. His blood pressure is120/75 mmHg. His EKG is pictured below. Echocardiogram reveals an ejection fraction of 45%. What is the best next step in his management?
Observation
Amiodarone
Digoxin
DC cardioversion
Verapamil
A 55-year-old white male presents to the Emergency Room with a four-hour history of chest pain. The pain is substernal and radiates to the left arm. He has a history of hypertension, diabetes, and hypercholesterolemia. His temperature is 36.7 C (98 F), blood pressure is 110/65 mmHg, pulse is 110/min, and respirations are 18/min. ECG is recorded and reveals ST segment elevation in the anterior leads and several ventricular premature beats (VPBs). What would the administration of lidocaine to such a patient most likely result in?
Increase in the risk of ventricular fibrillation
Improvement in overall prognosis
No change in frequency of VPBs
Increase in the risk of asystole
Increase in the risk of congestive heart failure
A 22-year-old male presents to you with feelings of general malaise. He is always tired and has noticed that he has frequent headaches. Exam reveals an elevated arm blood pressure with a radial to femoral delay. ECG shows left ventricular hypertrophy and the chest-x ray is shown below. Close examination of the x-ray reveals a "3" sign. What is the most likely diagnosis in this patient?
Tetralogy of F allot
Patent ductus arteriosus
Coarctation of aorta
Atrial septal defect
Aortic aneurysm
A 67-year-old Caucasian male is hospitalized in the intensive care unit (ICU) with an episode of prolonged hypotension and shortness of breath. His skin is cold and clammy. Intra-arterial blood pressure monitoring is established, and pulmonary artery catheterization is performed to control basic hemodynamic parameters. His blood pressure is 70/40 mmHg, and heart rate is 100/min. Cardiac output (CO) measured by thermodilution method is 2.3 Umin. Pulmonary capillary wedge pressure (PCWP) is estimated to be 22 mmHg. Systemic vascular resistance (SVR) calculated using data on mean arterial pressure, right atrial pressure and cardiac output is 2000 dynes*s/cm5 (N= 700 - 1200 dynes*s/cm5). Which of the following is the most likely underlying problem in this patient?
Cardiogenic shock
Volume depletion
Septic shock
Volume overload
Right ventricular infarction
A 32-year-old male complains of progressive weakness and exertional dyspnea. His past medical history is significant for a knife injury to the right thigh two months ago. He has been arrested several times for robbery. He consumes alcohol regularly, and smokes crack occasionally. His younger brother died of cystic fibrosis. His blood pressure is 160/60 mmHg, and heart rate is 100/min. His extremities are warm and flushed. Carotid upstroke is brisk. The point of maximal impulse is displaced to the left, and a soft, holosystolic murmur is heard over the cardiac apex. The murmur does not change with the Valsalva maneuver. Which of the following is the most likely cause of this patient's symptoms?
Decreased cardiac output
Hypertrophic cardiomyopathy
Increased cardiac preload
Papillary muscle dysfunction
Pulmonary hypertension
A 21-year-old woman presents to the ED complaining of lightheadedness. Her symptoms appeared 45 minutes ago. She has no other symptoms and is not on any medications. She has a medical history of mitral valve prolapse. Her HR is 170 beats per minute and BP is 105/55 mm Hg. Physical examination is unremarkable. After administering the appropriate medication, her HR slows down and her symptoms resolve. You repeat a 12-lead ECG that shows a rate of 89 beats per minute with a regular rhythm. The PR interval measures 100 milliseconds and there is a slurred upstroke of the QRS complex. Based on this information, which of the following is the most likely diagnosis?
Ventricular tachycardia
Atrial flutter with 3:1 block
Atrial fibrillation
Lown-Ganong-Levine (LGL) syndrome
Wolff-Parkinson-White (WPW) syndrome
A 61-year-old woman with a history of diabetes and hypertension is brought to the ED by her daughter. The patient states that she started feeling short of breath approximately 12 hours ago and then noticed a tingling sensation in the middle of her chest and became diaphoretic. An ECG reveals ST depression in leads II, III, and aVF. You believe that the patient had a non–ST-elevation MI (NSTEMI). Which of the following cardiac markers begins to rise within 3 to 6 hours of chest pain onset, peaks at 12 to 24 hours, and returns to baseline in 7 to 10 days?
Myoglobin
Creatinine kinase (CK)
Creatinine kinase-MB (CK-MB)
Troponin I
Lactic dehydrogenase
A 71-year-old man is playing cards with some friends when he starts to feel a pain in the left side of his chest. His fingers in the left hand become numb and he feels short of breath. His wife calls the ambulance and he is brought to the hospital. In the ED, an ECG is performed. Which of the following best describes the order of ECG changes seen in an MI?
Hyperacute T wave, ST-segment elevation, Q wave
Q wave, ST-segment elevation, hyperacute T wave
Hyperacute T wave, Q wave, ST-segment elevation
ST-segment elevation, Q wave, hyperacute T wave
ST-segment elevation, hyperacute T wave, Q wave
While playing a match of tennis, a 56-year-old man with a medical history significant only for acid reflux disease starts to feel substernal chest pain that radiates into his left arm and shortness of breath. His pain feels better after drinking antacid, but since it is not completely resolved, his partner calls 911. Upon arrival, EMS administers aspirin and sublingual nitroglycerin. After 20 minutes, the man’s symptoms resolve. He is brought to the ED for further evaluation where his ECG shows sinus rhythm without any ischemic abnormalities. You order a chest radiograph and send his blood work to the laboratory for analysis. Which of the following statements regarding the diagnosis of acute MI is most accurate?
A normal ECG rules out the diagnosis of acute MI.
One set of negative cardiac enzymes is sufficient to exclude the diagnosis of MI in this patient.
Troponin may not reach peak levels for at least 12 hours
Relief of symptoms by antacids essentially rules out a cardiac cause of his chest pain
Epigastric discomfort and indigestion is a rare presentation of ACS
A 22-year-old college student went to the health clinic complaining of a fever over the last 5 days, fatigue, myalgias, and a bout of vomiting and diarrhea. The clinic doctor diagnosed him with acute gastroenteritis and told him to drink more fluids. Three days later, the student presents to the ED complaining of substernal chest pain that is constant. He also feels short of breath. His temperature is 100.9°F, HR is 119 beats per minute, BP is 120/75 mm Hg, and RR is 18 breaths per minute. An ECG is performed revealing sinus tachycardia. A chest radiograph is unremarkable. Laboratory tests are normal except for slightly elevated WBCs. Which of the following is the most common cause of this patient’s diagnosis?
Streptococcus viridans
Influenza A
Coxsackie B virus
Atherosclerotic disease
Cocaine abuse
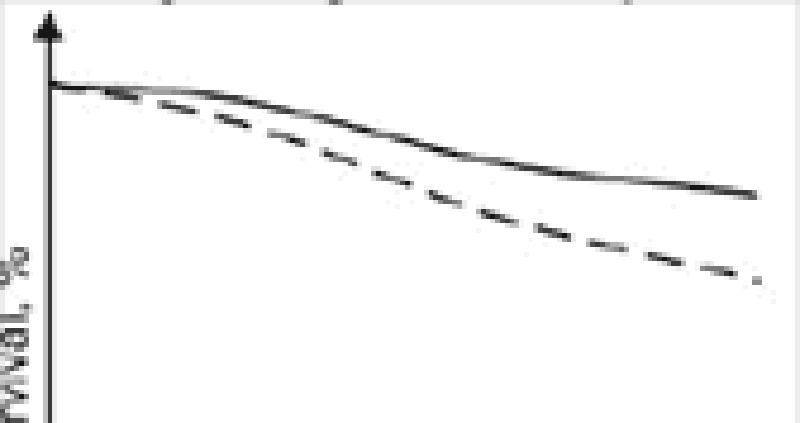
Diuretics, vasodilators and oxygen are standard inpatient therapy for patients hospitalized with left-sided heart failure. When patients are discharged, a different outpatient regimen is instituted. A team of researchers compares long-term cardiovascular mortality between patients treated with two different outpatient regimens. The study results are depicted below: In comparison to the patients depicted by the dashed curve, those depicted by the solid line most likely
ACE inhibitor
Calcium channel blocker
Loop diuretic
Digoxin
Dobutamine
A 60-year-old man is brought to the ER by his wife because he lost consciousness in the bathroom at night. He says that he woke up, went to the bathroom to urinate, and fainted there. He rapidly recovered his consciousness without any indication of disorientation. He has never had such an episode before. He admits' problems with urination,' including difficulty with initiating urination and frequent awakening to void at night. He does not take any medication. His past medical history is insignificant. He smokes 2 packs of cigarettes per day and does not consume alcohol. His blood pressure is 130/80 mm Hg while supine, and 132/80 while standing. His heart rate is 70/min. His physical examination is within normal limits. The ECG is normal. What is the most probable cause of the syncopal episode in this patient?
Arrhythmia
Postural hypotension
Situational syncope
Seizure
Transient ischemic attack
A 76-year-old man was operated on for a strangulated inguinal hernia and had approximately 40 cm of small bowel resected. On the morning of his third post-operative day, he falls while getting out of bed. Immediately after the fall, he is responsive but his speech is slurred and he cannot explain what happened. His pulse is 122/min, blood pressure is 96/50 mm Hg, and respirations are 23/min. Lungs are clear to auscultation and his heart has a regular rate and rhythm. His neck veins are distended. An ECG is remarkable for a new onset right bundle branch block (RBBB). Immediate resuscitation is started with wide open intravenous fluids, but he becomes unresponsive. Shortly thereafter, his pupils start to dilate and his heart rate drops to 45/min. He eventually dies despite resuscitative efforts. What is the most likely cause of his death?
Hypovolemia accompanied by syncope
Acute ischemic stroke
Myocardial infarction
Post-operative sepsis
Massive pulmonary thromboembolism
A 57-year-old female with a past medical history of bronchial asthma presents to the physician's office for evaluation of high blood pressure. On her previous two visits, her blood pressure has been 154/88 and 150/90. Her blood pressure during this visit is 150/90 mmHg. She denies headaches and has no complaints. She uses fluticasone and albuterol inhalers for her chronic persistent asthma. She denies smoking or alcohol intake, and has no known drug allergies. Her family history is significant for myocardial infarction in both her mother and father. Exercise and a low salt diet have not improved her hypertension. Which of the following is the most appropriate next step in managing this patient's hypertension?
Discontinue asthma medications
Prescribe propranolol
Prescribe enalapril
Prescribe hydrochlorothiazide
Obtain an echocardiogram
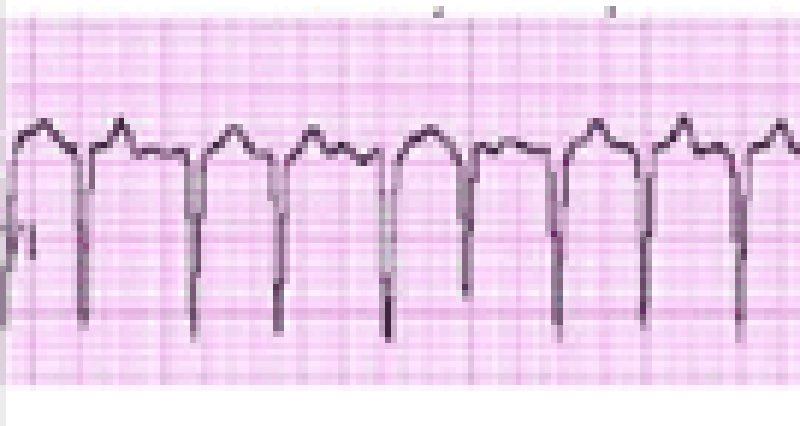
A 63-year-old female presents to your clinic complaining of palpitations. For the past 3 weeks, she has noticed pounding of her heart that comes and goes. Her symptoms are more frequent at night. Her only medicine is insulin for diabetes mellitus. On physical examination, she is alert and oriented, and in no distress. Her EKG is shown below. Which of the following best accounts for this patient's symptoms?
Sinus arrhythmia
Irregularly irregular atrial activation
Variable AV node conduction
Atrial ectopy
Ventricular ectopy
A 53-year-old Caucasian female is admitted to the ER with hypotension. Her condition is considered very serious, and invasive hemodynamic monitoring is established. Blood pressure measured by intra-arterial method is 72/46 mmHg. Her heart rate is 120/min, regular. Pulmonary capillary wedge pressure (PCWP) estimated using Swan-Ganz catheter is 6 mmHg. Mixed venous oxygen concentration (MVo2) is 16 vol% (Normal = 15.5 vol%). Which of the following is the most likely cause of this patient's condition?
Cardiogenic shock
Volume depletion
Septic shock
Hemorrhagic shock
Neurogenic shock
A 27-year-old female presents to your office for a follow-up. The previous two visits revealed an elevated blood pressure in the range of 150-155/90-95 mm Hg. She has no present complaints. Her past medical history is insignificant. She smokes 1/2 pack of cigarettes per day and does not consume alcohol. Her current medications include a combination oral contraceptive for the last 2 years, and an occasional acetaminophen for tension headache relief. There is no family history of hypertension or heart attacks. This visit, her blood pressure is 155/95 and her heart rate is 80/min. The physical examination is unremarkable. The ECG is normal. Her total cholesterol level, measured 6 months ago, was 170 mg/dL. Which of the following is the most appropriate next step in the management of this patient?
Lifestyle modification
Discontinuation of the oral contraceptive
Low-dose thiazide diuretic
Intravenous pyelography
No intervention at this point
A 60-year-old female comes to your office for progressive exertional dyspnea and new-onset ankle swelling. She has been recently worked up for proteinuria and easy bruisability. Otherwise her past medical history is insignificant. She has a ten pack-year history of smoking and she drinks two to three glasses of wine every day. Her temperature is 37.1 C (98.8F), blood pressure is 130/70 mm Hg, pulse is 80/min and respirations are 14/min. There is mild jugular venous distention on physical examination. Chest auscultation shows scattered bibasilar crackles. Echocardiography reveals symmetrical thickening of the ventricular walls, normal ventricular dimensions and a slightly reduced systolic function. Which of the following is the most likely diagnosis?
Alcohol-related heart disease
Hemochromatosis
Sarcoidosis
Amyloidosis
Constrictive pericarditis
A 65-year-old male presents to the emergency department with substernal chest pain, severe shortness of breath, and diaphoresis that began suddenly 40 minutes ago. Since the pain started, the patient has vomited twice. The pain radiates to his left arm and does not remit with sublingual nitroglycerine. EKG shows 2 mm ST elevations in the anterior leads. On physical examination, the patient's temperature is 36.9°c (98.4.F), blood pressure is 110/70 mm Hg, pulse is 60/min, respirations are 32/min, and oxygen saturation is 90% on 4L oxygen by nasal canula. Cardiac exam reveals a muffled S1 and S2 and the presence of an S3. Lung exam reveals basilar crackles that extend halfway up the lung fields bilaterally. Which of the following is the best next step in managing this patient?
Metoprolol
Digoxin
Furosemide
Spironolactone
IV fluids
During a routine office visit, a 62-year-old male is found to have a pulsatile non-tender mass above his umbilicus. His medical history is significant for hypertension, chronic renal insufficiency, myocardial infarction, and peripheral vascular disease. He quit smoking 10 years ago. On physical examination, his blood pressure is 160/90 mm Hg and pulse is 76/min. Laboratory analyses reveal a serum creatinine of 2.0 mg/dl. Which of the following is the most appropriate next step in evaluating this patient's abdominal mass?
Plain abdominal x-ray
CT scan with contrast
Abdominal ultrasound
Abdominal MRI
No testing required
A 20-year-old white female presents with chest pain for the past few weeks. She describes the pain as sharp, located to the left of the sternum, and lasting 5-10 seconds at a time. There is no associated fever, cough, breathlessness, palpitations, or syncope. She does not smoke or drink alcohol. On cardiac examination, there is a short systolic murmur at the apex that disappears with squatting. Which of the following is the most likely diagnosis?
Mitral valve prolapse
Ventricular septal defect
Rheumatic heart disease
Bicuspid aortic valve
Infective endocarditis
A 42-year-old man presents to the emergency department complaining of two weeks of weakness, low-grade fevers, and exertional shortness of breath. He also notes fingertip pain and urine that has been dark and cloudy recently. On physical examination, several of his proximal interphalangeal joints are swollen. Which of the following diagnoses is most consistent with his presentation?
Rheumatoid arthritis
Post-streptococcal glomerulonephritis
Adult Still's disease
Infective endocarditis
Adrenal insufficiency
A 59-year-old man comes to visit his friend in the hospital and collapses in the parking lot. He had been feeling unwell all day due to vague chest discomfort. A bystander witnesses his collapse, finds no pulse, and immediately calls for help. Which of the following is the most important factor for survival in this patient?
Time to chest compressions
Time to defibrillation
Time to endotracheal intubation
Time to epinephrine injection
Time to cardiac catheterization lab
A 73-year-old man presents to the ED after a syncopal episode. He had been resting in bed for approximately one week after injuring his right knee. This morning, his knee felt better and he attempted to get up from bed. However, upon attempting to stand, he sustained a brief loss of consciousness. He had no symptoms or medical history prior to the knee injury. Medications include acetaminophen and ibuprofen for knee pain. On exam, his pulse is 73/min, respirations are 14/min, and blood pressure is 136/83 mmHg. Which of the following is the most likely cause of this patient's syncope?
Cardiac arrhythmia
Valvular obstruction
Orthostatic hypotension
Vagal nerve hyperactivity
Hyperventilation

A 47-year-old female, who is a chronic alcoholic, is admitted to the hospital with epigastric pain, nausea, and vomiting. Her serum amylase and lipase levels are significantly elevated and the diagnosis of acute pancreatitis is made. She is maintained nothing by mouth (NPO), and receives intravenous hydration and narcotic analgesics. On the second day of hospitalization she develops progressive shortness of breath. Her temperature is 37.2 C (98.9 F), blood pressure is 110/66 mm Hg, pulse is 110/min, and respirations are 24/min. Her oxygenation is measured at 84% on 100% non-rebreather mask and the decision is made to intubate. Since the time of admission, she has received 5 liters of normal saline and has produced 3 liters of urine output. On examination, there is no evidence of jugular venous distention. Chest auscultation reveals diffuse bilateral crackles. Auscultation of the heart reveals normal heart sounds with no murmurs. A chest x-ray from the time of admission and one from the time of intubation are shown below:Based on these findings, what is the most likely diagnosis in this patient?
Acute respiratory distress syndrome
Hospital acquired pneumonia
Iatrogenic volume overload
Congestive heart failure from myocardial infarction
Alcoholic cardiomyopathy
A 59-year-old male presents to the ER with sudden onset severe chest pain associated with vomiting and diaphoresis. The pain radiates to the left shoulder and is not relieved by sublingual nitroglycerine. His past medical history is significant for diabetes mellitus for seven years and hypercholesterolemia for six years. His medications include metformin, glipizide and simvastatin. On physical examination, his blood pressure is 150/98 mmHg and pulse is 86/min. An EKG obtained in the ER shows ST segment elevations in leads aVL and I. Cardiac troponin and CK-MB are elevated. Which of the following medications should be avoided in this patient at this time?
Heparin
Captopril
Nifedipine
Metoprolol
Aspirin
A 46-year-old woman is hospitalized for agitation, restlessness and poor sleep. She has been complaining of headaches recently and has gained 14 pounds over the past three months. She denies any illicit drug use. Her blood pressure is 160/110 mmHg and her heart rate is 90/min. Her laboratory findings are shown below: Sodium 142 mEq/L Potassium 3.2 mEq/L Chloride 98 mEq/L Bicarbonate 26 mEq/L BUN 12 mg/dl Creatinine 0.9 mg/dl Glucose 205 mg/dl Calcium 94 mg/dl Which of the following is the most likely cause of this patient's hypertension?
Renal parenchymal disease
Adrenal medullary disease
Adrenal cortical disease
Hypothyroidism
Parathyroid gland disease
A 55-year-old male with a history of rheumatoid arthritis and rheumatoid lung disease is admitted to the hospital with palpitations. His restrictive lung disease is of moderate severity, requiring use of 2 liters of oxygen by nasal cannula at all times. He has no known history of coronary artery disease, hypertension or diabetes. On physical examination, his blood pressure is 110/70 mmHg and heart rate is 120 and irregular. EKG shows atrial fibrillation with a rapid ventricular rate. Which of the following medications should be avoided in this patient?
Verapamil
Quinidine
Amiodarone
Digoxin
Metoprolol
A 37-year-old Cambodian woman presents to the emergency room with acute onset of left-sided weakness. She has been experiencing progressive exertional dyspnea, nocturnal cough and occasional hemoptysis over the past six months. She also describes frequent episodes of palpitations and irregular heartbeats. Which of the following is the most likely diagnosis?
Mitral stenosis
Hypertrophic cardiomyopathy
Aortic insufficiency
Wolf-Parkinson-White syndrome
Primary pulmonary hypertension
A 32-year-old anxious-appearing male is wheeled into the emergency room with the sudden onset of excruciating left-sided chest pain. His temperature is 37.2C (99F), blood pressure is 160/88 mmHg, pulse is 125/min, regular and respirations are 20/min. Physical examination is normal, except for multiple venous track marks on his extremities and atrophic nasal mucosa. An EKG is done which shows ST depression and T wave inversion in leads V1-V6. Cardiac enzymes including CK-MB and Troponin Tare not elevated. Which of the following is the most appropriate next step in the management of this patient?
Cardiac catheterization
Administer metoprolol
Administer thrombolytics
Close observation
Intravenous diazepam
A 67-year-old man presents to the emergency department after losing consciousness while shoveling snow near his house. He reports having had a similar episode one month ago while carrying heavy bags from the grocery store. The patient has reduced his physical activity level over the last several months because of progressive exertional dyspnea and fatigue. His past medical history is significant for diabetes mellitus and hypercholesterolemia. Metformin and simvastatin are his only medications. Which of the following physical examination findings is most likely in this patient?
Pulsus paradoxus
Capillary pulsations
Late diastolic murmur
Systolic ejection murmur
Pleural friction rub
A 66-year-old white male presents for evaluation of progressively worsening dyspnea that affects him at rest and wakes him from sleep. He also notes bilateral ankle swelling. His medical history is significant for coronary artery disease for which he has undergone angioplasty and coronary artery bypass grafting. On examination today, his pulse is 86/min, blood pressure is 110/70 mmHg, and respirations are 19/min. His neck veins are distended and there is bilaterally symmetric pitting ankle edema. On chest auscultation, you hear crackles at the bilateral lung bases and a third heart sound. Chest x-ray shows an enlarged cardiacsilhouette and bilateral alveolar and interstitial pulmonary edema. Of the medications listed below, which has not been shown to improve survival in patients with the above presentation?
Captopril
Losartan
Metoprolol
Digoxin
Aspirin
A 69-year-old male undergoes coronary artery bypass and aortic valve replacement surgery. The procedure goes well, and he is extubated and discharged to the step-down unit on postoperative day 2. That night, he complains of weakness, chest tightness and shortness of breath. His blood pressure is 70/30 mmHg, respiratory rate is 26/min, and heart rate is 148 beats per minute. Lung auscultation reveals bibasilar crackles. An EKG rhythm strip is obtained: Which of the following is the best next step in the management of this patient?
Amiodarone
Transcutaneous pacing
DC cardioversion
Lidocaine
Digoxin
A 53-year-old man presents to the emergency room with squeezing chest pain that started two hours ago. He also complains of shortness of breath that is worse when lying down. He has never had pain like this before. He has no significant past medical history and he takes no medications. A routine health maintenance visit two weeks ago was normal. On physical examination in the ER, his blood pressure is 140/90 mmHg and his heart rate is 100/min. Chest auscultation reveals a grade IINI blowing systolic murmur at the cardiac apex and bibasilar crackles in the lungs. ECG shows ST segment elevations in leads I, aVL, and v1-v3. Which of the following is most likely increased in this patient?
Left atrial pressure
Left atrial size
Left ventricular compliance
Left ventricular ejection fraction
Right ventricular preload
A 35-year-old woman who has recently emigrated from Asia presents to the emergency room with acute onset of dyspnea. She denies any cough, chest pain, or fever. She has a history of rheumatic heart disease as a teen. On examination, she has an irregular pulse of 97/min, blood pressure of 125/75 mm of Hg and temperature of 37.2C (98.9F). The first heart sound is loud and a mid-diastolic rumble is heard at the apex. Crackles are present in both lung fields. ECG shows an irregularly, irregular heart rhythm and the absence of 'P' waves. Which of the following is the most likely cause of this patient's abnormal heart rhythm?
Left atrial dilatation
Right atrial dilatation
Left ventricular dilatation
Left ventricular hypertrophy
Pulmonary hypertension
A 17-year-old girl is brought to the ER 30 minutes after an episode where she lost consciousness. She is accompanied by her father who witnessed the event. He says that the patient recently broke up with her boyfriend and has been under a lot of stress. Her sleep has been poor. She has had three similar episodes over the last month. On exam, her heart rate is 90/min, respirations are 13/min, and blood pressure is 120/70 mmHg. She seems sleepy but can be aroused easily. She gives her correct name but is disoriented to time and place. Pupils are symmetric and reactive to light. Blood glucose level is 100 mg/dl. Which of the following findings would you most expect in this patient?
Systolic murmur that increases with standing
Pulsus paradoxus
Orthostatic hypotension
Positive stool guaiac test
Bitten tongue
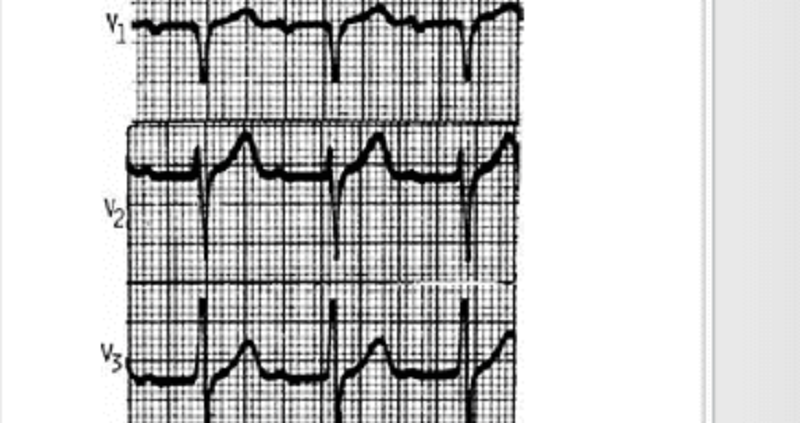
An 18-year-old male complains of fever and transient pain in both knees and elbows. The right knee was red and swollen for 1 day during the week prior to presentation. On physical examination, the patient has a low-grade fever. He has a III/VI, high pitched, apical systolic murmur with radiation to the axilla, as well as a soft, mid-diastolic murmur heard at the base. A tender nodule is palpated over an extensor tendon of the hand. There are pink erythematous lesions over the abdomen, some with central clearing. The following laboratory values are obtained: Hct: 42 WBC: 12,000/μL with 80% polymorphonuclear leukocytes, 20% lymphocytes ESR: 60 mm/h The patient’s ECG is shown below. Which of the following tests is most critical to diagnosis?
Blood cultures
Antistreptolysin O antibody
Echocardiogram
Antinuclear antibodies
Creatine kinase
A 50-year-old construction worker continues to have elevated blood pressure of 160/95 even after a third agent is added to his antihypertensive regimen. Physical examination is normal, electrolytes are normal, and the patient is taking no over-the-counter medications. Which of the following is the best next step for this patient?
Check pill count.
Evaluate for Cushing syndrome.
Check chest x-ray for coarctation of the aorta.
Obtain a renal angiogram.
Obtain an adrenal CT scan.
A 35-year-old male complains of substernal chest pain aggravated by inspiration and relieved by sitting up. Lung fields are clear to auscultation, and heart sounds are somewhat distant. Chest x-ray shows an enlarged cardiac silhouette. Which of the following is the best next step in evaluation?
Right lateral decubitus chest x-ray
Cardiac catheterization
Echocardiogram
Serial ECGs
Thallium stress test
A 32-year-old male presents to your office with concern about progressive fatigue and lower extremity edema. He has experienced decreased exercise tolerance over the past few months, and occasionally awakens coughing at night. Past medical history is significant for sickle cell anemia and diabetes mellitus. He has had multiple admissions to the hospital secondary to vasoocclusive crises since the age of three. Physical examination reveals a displaced PMI, but is otherwise unremarkable. ECG shows a first degree AV block and low voltage. Chest x-ray shows an enlarged cardiac silhouette with clear lung fields. Which of the following would be the best initial diagnostic approach?
Order serum iron, iron-binding capacity, and ferritin level.
Order brain-natriuretic peptide (BNP)
Order CT scan of the chest.
Arrange for placement of a 24-hour ambulatory cardiac monitor.
Arrange for cardiac catheterization.
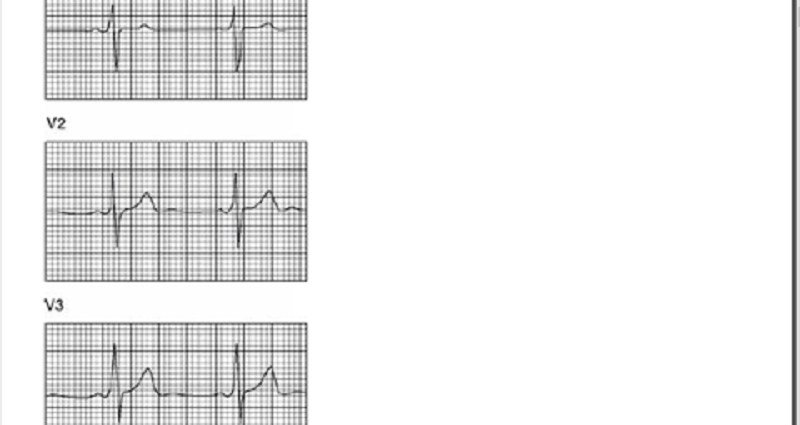
You are performing medical screening of new military recruits when an 18-year-old male reports several episodes of palpitation and syncope over the past several years. Physical examination is unremarkable. An ECG is obtained with excerpts shown below. What is the most likely diagnosis?
Prior myocardial infarction secondary to coronary artery disease
Congenital prolonged QT syndrome
Hypertrophic obstructive cardiomyopathy
Preexcitation syndrome (Wolff-Parkinson-White)
Rheumatic mitral stenosis
A 26-year-old primigravida at 20th week gestation presents to the emergency room with a sudden onset of tearing chest pain radiating to her back and left arm. The patient is pale and diaphoretic. Her PR: 116/min; BP: 192/ 104 in left arm, and 123/65 in right arm; RR: 36/min. Her cardiac examination reveals a diastolic murmur along the left sternal border. Her previous prenatal care is not known. She is a smoker with a 10 pack/year history and drinks alcohol. Her ECG reveals mild left axis deviation and ST segment depression in lead II, Ill, and AVF. What is the most appropriate next step in the management of this patient?
Obtain CK-MB and T roponin levels
T ransesophageal echocardiogram (TEE)
Transthoracic echocardiogram (TTE)
Antihypertensive treatment
CT scan of chest
A 45-year-old mildly overweight male recovering from an anterior wall myocardial infarction develops sudden onset of left-sided chest pain. He appears agitated and restless. Two minutes later, he is unresponsive. His pulse is not palpable and ECG monitor shows sinus tachycardia at the rate of 130/min. He presented five days earlier with substernal chest pain and diaphoresis. He has had no dyspnea, extremity swelling or palpitations since admission. His past medical history is significant for diabetes mellitus type 2. Which of the following is the most likely diagnosis?
Interventricular wall rupture
Ventricular free wall rupture
Pulmonary infarction
Recurrent ischemia
Right ventricular infarction
A 53-year-old woman presents to the physician's office with a 3-week history of burning, substernal chest pain that usually comes on with exertion and is relieved with rest. The pain does not radiate to the arms or jaw. Her past medical history is significant for bronchial asthma, type 2 diabetes, hypercholesterolemia, and hypertension. A diagnosis of stable angina is suspected, and the patient is scheduled for an exercise EKG stress test. Which of her medications should be withheld 24 hours before the test?
Admit him to the hospital to control his blood pressure
Start an ACE inhibitor
Increase the dose of thiazide diuretic
Reduction in alcohol intake
Reassurance and repeat measurement in 2 weeks
A 34-year-old Caucasian woman presents to your office with dyspnea and severe chest pain after returning from a trip to Central Asia. The pain is localized on the left side and increases with inspiration. She also had one episode of hemoptysis. She does not smoke or consume alcohol. She is sexually active with one partner and uses oral contraceptives. Her father died of a myocardial infarction at 52 years of age. Her temperature is 36.7C (98.F), pulse is 100/min, respirations are 28/min, and blood pressure is 110/66 mmHg. Which of the following most likely accounts for this patient's chest pain?
Pulmonary artery distention
Myocardial ischemia
Pericardial inflammation
Pleural infection
Pulmonary infarction
An 82-year-old male presents for evaluation of chronic back pain. On physical examination, he is found to have a blood pressure of 160/85 mmHg while supine and 135/70 mmHg while standing. He is otherwise healthy; his only medicine is occasional ibuprofen for back pain. Which of the following age-related changes best explains the observed finding?
Increased left ventricular wall stiffness
Decreased left ventricular contractility
Decreased baroreceptor responsiveness
Decreased stress-mediated catecholamine release
Decreased glomerular filtration rate
A 64-year-old diabetic with a long history of uncontrolled hypertension is admitted for chest pain. ECG reveals elevated ST segments in the anterior wall leads. Cardiac enzymes are elevated and the patient is admitted to the ICU for supportive care. He receives low molecular weight heparin and is placed on a nitroglycerin drip. He continues to have chest pain and requires intravenous morphine. Three days later, the patient is transferred to the floor and he remains on bed rest. During the night the nurse on call informs you that the patient has a cold leg. On examination, the left leg is cold and there are no distal pulses. There is minimal swelling and the leg appears mottled. Emergency vascular surgery consult was placed and the appropriate treatment was given Which of the following should also be considered in this patient?
Venous duplex study
Chest x-ray
Echocardiogram
V/Q scan
D-dimer level

A 66-year-old male is rushed to the emergency department because he feels dizzy and light-headed. He denies chest pain or palpitations. He has a history of hypertension and diabetes. His blood pressure is 116/62 mm Hg and his pulse is 35-40/min. He is alert, awake, and fully oriented. He is breathing comfortably and does not appear to be in any distress. His extremities are slightly cold and capillary refill is 3 seconds. His EKG is shown below. Which of the following is the most appropriate next step in management? A. Intravenous
Intravenous adenosine push
Intravenous atropine
Intravenous epinephrine
Intravenous amiodarone
Transcutaneous pacing
A 34-year-old woman is referred by an OB-GYN colleague for the onset of fatigue and dyspnea on exertion 1 month after her second vaginal delivery. Physical examination reveals a laterally displaced PMI, elevated jugular venous pressure and 2+pitting lower extremity edema. Echocardiogram shows systolic dysfunction with an ejection fraction of 30%. Which statement most accurately describes her condition?
This disease may occur unexpectedly years after pregnancy and delivery.
About half of similar patients will recover completely.
The condition is idiosyncratic; the risk of recurrence with a future pregnancy is no greater than averag
This condition will require a different therapeutic approach than the typical dilated cardiomyopathy.
This condition will require endomyocardial biopsy for diagnosis.
A 72-year-old Caucasian male presents with shortness of breath that awakens him at night. At baseline he is able to walk less than a block before stopping to catch his breath. Physical examination findings include bilateral basilar rales and neck vein distention. The patient has a known history of congestive heart failure, and his last echocardiogram revealed an ejection fraction of 25%. The patient is compliant with a medication regimen including an ACE inhibitor, beta-blocker, and loop diuretic. Blood pressure is well controlled. What additional treatment should you begin next?
Spironolactone
Aspirin
Amlodipine
Warfarin
Hydralazine and isosorbide dinitrate
A 68-year-old male was intubated in the emergency room because of pulmonary edema. Stat echocardiogram reveals an ejection fraction of 45% and severe mitral regurgitation. In spite of aggressive diuresis with furosemide, the patient continues to require mechanical ventilation secondary to pulmonary edema. What is the best next step in treating this patient?
Arrange for mitral valve replacement surgery.
Place an intra-aortic balloon pump.
Begin metoprolol.
Begin a second loop diuretic
Begin intravenous enalapril.
A 30-year-old female presents with a chief complaint of palpitations. A 24-hour Holter monitor shows occasional unifocal premature ventricular contractions and premature atrial contractions. Which of the following is the best management for this patient?
Anxiolytic therapy
Beta-blocker therapy
Digoxin
Quinidine
Reassurance, no medication
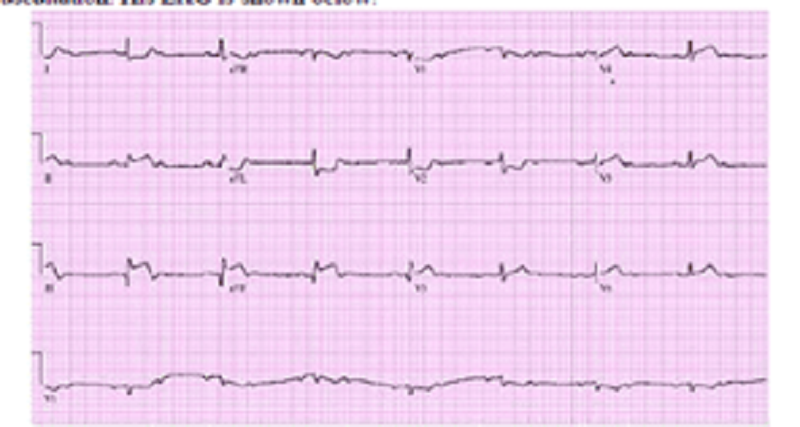
A 70-year-old Caucasian man comes to the emergency department because of the sudden onset of nausea, vomiting, diaphoresis, and chest pain. His other medical problems include hypertension, diabetes mellitus-type 2, and aortic stenosis. He has smoked one-and-a-half packs of cigarettes daily for 30 years and drinks 4 ounces of alcohol daily. His temperature is 37.2 C (99 F), blood pressure is 100/60 mmHg, pulse is 60/min, and respirations are 18/min. The patient's pulse oximetry showed 98% at room air. Examination shows normal first and second he sounds. Lungs are clear to auscultation. His EKG is shown below. Which of the following is the most likely mechanism of this patient's condition?
Occlusion of the right coronary artery
Occlusion of the left circumflex artery
Occlusion of the left anterior descending artery
Inflammation of the pericardium
Vasospasm of the left circumflex artery
A 36-year-old man presents to your office for a routine pre-employment physical. He has no complaints except for occasional morning headaches. His father died suddenly at the age of 54. The patient's blood pressure is 175/103 mmHg in the right arm and 180/105 in the left arm. His heart rate is 82/min. His lungs are clear bilaterally and his heart sounds are normal. Bilateral, non-tender, upper abdominal masses are palpated on exam. His hemoglobin level is 15.2 g/dl and creatinine concentration is 0.8 mg/dl. Which of the following is most likely to diagnose this patient's condition?
Urine metanephrines
Abdominal ultrasound
Captopril-enhanced radionuclide renal scan
Aldosterone: renin ratio
24-hour urine cortisol
A 52-year-old man complains of frequent chest pain. The pain typically occurs at night and is described as retrosternal and burning in quality. He leads a sedentary lifestyle but does not smoke or drink alcohol. His past medical history includes a chronic cough and occasional hoarseness. He does not take any medications. His BMI is 28.5 kg/m2 ECG stress testing reveals 1 mm ST segment depression in the inferior leads at 90% of predicted maximal heart rate. He did not experience chest pain during the stress test. Which of the following is most likely to relieve this patient's chest pain?
Ibuprofen
Nitroglycerin
Propranolol
Alprazolam
Omeprazole
{"name":"Cardiovascular", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 74-year-old man presents to your office for a routine He has no present complaint His medical history is significant for right knee osteoarthritis He takes naproxen occasionally, to relieve knee pain. He does not smoke or consume alcohol His BP is 165\/75 mm Hg and PR is 70\/min. The physical examination showed a mild systolic ejection type murmur at the base of the heat to the right. An E-KG revealed left ventricular hypertrophy and secondary ST segment and T wave change Moderate left ventricular hypertrophy, without any flow abnormalities, was demonstrated on echocardiography. The ejection fraction was 60%. What is the most probable cause of hypertension in this patient?, A 32-year-old Caucasian female comes to the physician because of a one-week history of fatigue, progressive worsening of shortness of breath and swelling of feet. She denies any chest pain She has no other medical problems except a recent cold two weeks ago. She is not taking any medication Her temperature is 36 7 C (98 F), blood pressure is 110\/65 mmHg, pulse is g0\/min, and respirations are 20\/min Bilateral basal crackles, elevated jugular venous pressure, and 2+ bilateral pitting edema of the ankles are noted Complete blood count is unremarkable. Transthoracic echocardiogram of her heat will most likely show?, A 47-year-old woman loses consciousness for 2 minutes while shopping in a supermarket. In the emergency room, she recounts feeling nausea and warmth spreading over her body immediately before passing out She has never had a similar episode before. She has not seen a doctor for several years and does not take any medications, nor does she use tobacco, alcohol or drug. Her family history is unremarkable. Which of the following most likely caused this episode?","img":"https://cdn.poll-maker.com/11-487801/55.png?sz=1200-000000100053"}
More Quizzes
Get to Know Me Quiz
5217
The Fun They Had
7454
WHICH DISNEY CHARACTER ARE YOU ?
8436
Are you black quiz!?!??!? (Gone Sexual, In The Hood)
100
Which Until Dawn Character Are You? - Free
201018188
Basic Physics Test - Free Practice Questions
201017228
Stuart Little 3rd Grade - Free Literature Practice
201022773
Free Biological Age Test - Find Your True Body Age
201016623
Are Lithium-Ion Batteries Wet-Cell? True or False
201019761
Media: Introduction to the Media - Free Online
15817292
Is It Cheating If Questions? Take Our Partner Cheating
201016623
What Is My Favorite Restaurant? Free Personality
201017690