Madigan General Surgery MSIII Quiz
A 22 year old previously healthy male presents with a 1 day history of right lower quadrant abdominal pain, fever, nausea, and anorexia. The differential diagnosis for this patient includes: (select one)
A. Appendicitis
B. Meckel’s Diverticulitis
C. Mesenteric Lymphadenitis
D. All of the above
E. A & C only
Explanation:
Appendicitis should be high on your differential diagnosis for this young healthy male. However, other disease processes should be considered in the differential diagnosis. Both Meckel's Diverticulitis and Mesenteric Lymphadenitis can cause acute right lower quadrant abdominal pain. Other diagnoses to consider are nephrolithiasis, terminal ileitis (infectious or inflammatory), torsion of the epiploic appendix, omental torsion, urinary tract infection, right sided diverticulitis, inflammatory bowel disease, cholecystitis, and many more. In females, the differential diagnosis includes conditions of the reproductive tract such as ovarian torsion, ovarian cysts, pelvic inflammatory disease, and endometriosis.
Explanation:
Appendicitis should be high on your differential diagnosis for this young healthy male. However, other disease processes should be considered in the differential diagnosis. Both Meckel's Diverticulitis and Mesenteric Lymphadenitis can cause acute right lower quadrant abdominal pain. Other diagnoses to consider are nephrolithiasis, terminal ileitis (infectious or inflammatory), torsion of the epiploic appendix, omental torsion, urinary tract infection, right sided diverticulitis, inflammatory bowel disease, cholecystitis, and many more. In females, the differential diagnosis includes conditions of the reproductive tract such as ovarian torsion, ovarian cysts, pelvic inflammatory disease, and endometriosis.
For patient’s with clinical and radiographic evidence of a small bowel obstruction, possible treatment options include which of the following: (select one)
A. Nasogastric tube placement, NPO, bowel rest, IV fluids
B. Exploratory laparotomy, lysis of adhesions
C. Magnesium citrate by mouth, Mineral oil enema, rectal tube placement
D. All of the above
E. A & B only
Explanation:
Depending on the clinical scenario, it may be acceptable to manage a patient with a small bowel obstruction operatively or nonoperatively. Operative management usually involves and exploratory laparotomy or laparoscopy with lysis of adhesions (division of adhesion causing the obstruction). Nonoperative management of a small bowel obstruction typically involves decompressing the GI tract with an NG tube, maintaining the patient NPO, and maintaining hydration with IV fluids until the patient displays some return of bowel function. Magnesium citrate and enemas may be used in patients with constipation. However, constipation has a very different pathophysiology than a small bowel obstruction and the treatment for the two disease processes are not the same.
Explanation:
Depending on the clinical scenario, it may be acceptable to manage a patient with a small bowel obstruction operatively or nonoperatively. Operative management usually involves and exploratory laparotomy or laparoscopy with lysis of adhesions (division of adhesion causing the obstruction). Nonoperative management of a small bowel obstruction typically involves decompressing the GI tract with an NG tube, maintaining the patient NPO, and maintaining hydration with IV fluids until the patient displays some return of bowel function. Magnesium citrate and enemas may be used in patients with constipation. However, constipation has a very different pathophysiology than a small bowel obstruction and the treatment for the two disease processes are not the same.
Which of the following surgical procedures are options for the surgical management of morbid obesity? (select one)
A. Distal gastrectomy with Billroth II reconstruction
B. R-En-Y Gastric bypass
C. Sleeve gastrectomy
D. All of the above
E. B & C only
Explanation:
R-En-Y gastric bypass and sleeve gastrectomy are both options for patients who meet clinical criteria and desire surgical treatment of their morbid obesity. Distal gastrectomy with Billroth II reconstruction may be employed in conjunction with a vagotomy for the treatment of recalcitrant peptic ulcer disease. These procedures are rarely performed today due to the efficacy of modern antacid medications (PPI's and H2 blockers).
Explanation:
R-En-Y gastric bypass and sleeve gastrectomy are both options for patients who meet clinical criteria and desire surgical treatment of their morbid obesity. Distal gastrectomy with Billroth II reconstruction may be employed in conjunction with a vagotomy for the treatment of recalcitrant peptic ulcer disease. These procedures are rarely performed today due to the efficacy of modern antacid medications (PPI's and H2 blockers).
True or False – Patients with symptomatic cholelithiasis require emergent cholecystectomy (surgery within 1 hour)
True
False
Explanation:
Gallbladder/biliary tract pathology includes the following diagnoses: biliary dyskinesia, symptomatic cholelithiasis (AKA biliary colic), acute cholecystitis, chronic cholecystitis, choledocholithiasis, cholangitis, ascending cholangitis. Of these diagnoses, ascending cholangitis is considered the condition that requires the most expeditious intervention (drainage of the bile duct). Emergent cholecystectomy is not required for any of the diagnoses listed above. Patients with acute cholecystitis are typically admitted to the hospital, started on antibiotics, and taken for cholecystectomy within the first 24 to 72 hours.
Explanation:
Gallbladder/biliary tract pathology includes the following diagnoses: biliary dyskinesia, symptomatic cholelithiasis (AKA biliary colic), acute cholecystitis, chronic cholecystitis, choledocholithiasis, cholangitis, ascending cholangitis. Of these diagnoses, ascending cholangitis is considered the condition that requires the most expeditious intervention (drainage of the bile duct). Emergent cholecystectomy is not required for any of the diagnoses listed above. Patients with acute cholecystitis are typically admitted to the hospital, started on antibiotics, and taken for cholecystectomy within the first 24 to 72 hours.
A 50 year-old otherwise healthy woman with no prior personal or family history of breast cancer presents with a grape-sized palpable right breast mass. Mammogram and ultrasound reveal a highly suspicious corresponding lesion and no other imaging concerns. Physical exam is negative except for the non-fixed UOQ mass. The most appropriate next step in management is: (select one)
Fine needle aspiration
Ultrasound-directed core biopsy
Incisional biopsy
Excisional biopsy
Oncologic lumpectomy
Explanation:
Patients with a palpable breast mass that, based on physical exam and radiographic studies, is concerning for malignancy should undergo tissue sampling prior to open biopsy or excision of any type. Tissue sampling is performed efficiently using ultrasound guidance and a core biopsy needle. Fine needle aspiration is not routinely used in the diagnosis of breast cancer as the diagnostic yield is typically poor. Once a diagnosis of cancer is made, a surgical plan to include treatment of the primary tumor (lumpectomy vs mastectomy) and axillary lymph node sampling (axillary lymph node biopsy vs axillary dissection) can be discussed with the patient.
Explanation:
Patients with a palpable breast mass that, based on physical exam and radiographic studies, is concerning for malignancy should undergo tissue sampling prior to open biopsy or excision of any type. Tissue sampling is performed efficiently using ultrasound guidance and a core biopsy needle. Fine needle aspiration is not routinely used in the diagnosis of breast cancer as the diagnostic yield is typically poor. Once a diagnosis of cancer is made, a surgical plan to include treatment of the primary tumor (lumpectomy vs mastectomy) and axillary lymph node sampling (axillary lymph node biopsy vs axillary dissection) can be discussed with the patient.
A 50 year-old otherwise healthy woman with no prior personal or family history of breast cancer presents with a grape-sized palpable right breast mass. Mammogram and ultrasound reveal a highly suspicious corresponding lesion and no other imaging concerns. Physical exam is negative except for the non-fixed UOQ mass. Part 2 of previous question: Biopsy confirms invasive ductal carcinoma. After appropriate counseling for alternatives, the treatment most likely to be recommended to this patient is: (select one)
Lumpectomy
Lumpectomy and sentinel node staging
Lumpectomy and sentinel node staging, postop breast radiation
Simple mastectomy and sentinel node staging
Modified radical mastectomy
Explanation:
Most women with early stage breast cancer elect for breast conservation therapy (BCT). The treatment of the primary tumor includes lumpectomy and radiation therapy (XRT). Lumpectomy is not typically offered to patients with breast cancer who refuse or are not eligible to receive XRT. Patients who do not receive XRT usually undergo mastectomy. All patients with invasive breast cancer undergo some form of axillary lymph node sampling. Currently the most common and least invasive method is via sentinel node biopsy. Axillary lymph node sampling is essential in order to assign the patient the correct pathologic stage. Pathologic staging is essential in order to decide the need for additional medical, surgical, or XRT therapies.
Explanation:
Most women with early stage breast cancer elect for breast conservation therapy (BCT). The treatment of the primary tumor includes lumpectomy and radiation therapy (XRT). Lumpectomy is not typically offered to patients with breast cancer who refuse or are not eligible to receive XRT. Patients who do not receive XRT usually undergo mastectomy. All patients with invasive breast cancer undergo some form of axillary lymph node sampling. Currently the most common and least invasive method is via sentinel node biopsy. Axillary lymph node sampling is essential in order to assign the patient the correct pathologic stage. Pathologic staging is essential in order to decide the need for additional medical, surgical, or XRT therapies.
Patients with colon cancer will ALWAYS receive which of the following therapeutic options as part of their treatment for curative intent: (select one)
A. Immunotherapy
B. Radiation therapy
C. Oncologic colon resection
D. Wedge resection of colonic mass with diverting colostomy
E. B & C only
Explanation:
A surgical procedure is always required in patients who desire a cure for their colon cancer. Colon cancers are surgically excised by removing a segment of colon proximal and distal to the lesion and a generous portion of the adjoining colonic mesentery. Wedge resections of colonic masses are not oncologically sound surgical procedures. This procedure would lead to a high recurrence rate and does not obtain a sample of the colonic mesentery which provides addition staging information.
Explanation:
A surgical procedure is always required in patients who desire a cure for their colon cancer. Colon cancers are surgically excised by removing a segment of colon proximal and distal to the lesion and a generous portion of the adjoining colonic mesentery. Wedge resections of colonic masses are not oncologically sound surgical procedures. This procedure would lead to a high recurrence rate and does not obtain a sample of the colonic mesentery which provides addition staging information.
True or False – First-line treatment for patients with internal hemorrhoids is 3 column hemorrhoidectomy
True
False
Explanation:
First line treatment for most hemorrhoids (internal or external) usually involves stool softeners, fiber, increased oral hydration, and possibly Sitz baths. Surgery is reserved for failure of medical therapy. The one exception to this rule is the acutely thrombosed hemorrhoid (presenting within 24 hours). This condition is treated by surgically evacuating of the clot.
Explanation:
First line treatment for most hemorrhoids (internal or external) usually involves stool softeners, fiber, increased oral hydration, and possibly Sitz baths. Surgery is reserved for failure of medical therapy. The one exception to this rule is the acutely thrombosed hemorrhoid (presenting within 24 hours). This condition is treated by surgically evacuating of the clot.
True of False – First-line treatment for patients with a fluctuant perirectal abscess is a well chosen antibiotic
True
False
Explanation:
A fluctuant perirectal abscess should be treated with incision and drainage. Depending on the size, pain level, comorbidities, associated findings, the procedure could be performed in the clinic or in the operating room. Patients should always be counseled that a fistula in ano may develop after the procedure and appropriate follow up should be advised. Oral or IV antibiotics without surgical drainage is insufficient treatment for an obvious perirectal abscess.
Explanation:
A fluctuant perirectal abscess should be treated with incision and drainage. Depending on the size, pain level, comorbidities, associated findings, the procedure could be performed in the clinic or in the operating room. Patients should always be counseled that a fistula in ano may develop after the procedure and appropriate follow up should be advised. Oral or IV antibiotics without surgical drainage is insufficient treatment for an obvious perirectal abscess.
All of the following structures serve as anatomical borders of the inguinal triangle (Hesselbach's triangle) EXCEPT: (choose one)
The inguinal ligament
The lateral margin of the rectus sheath
The conjoint tendon
The inferior epigastric vessels
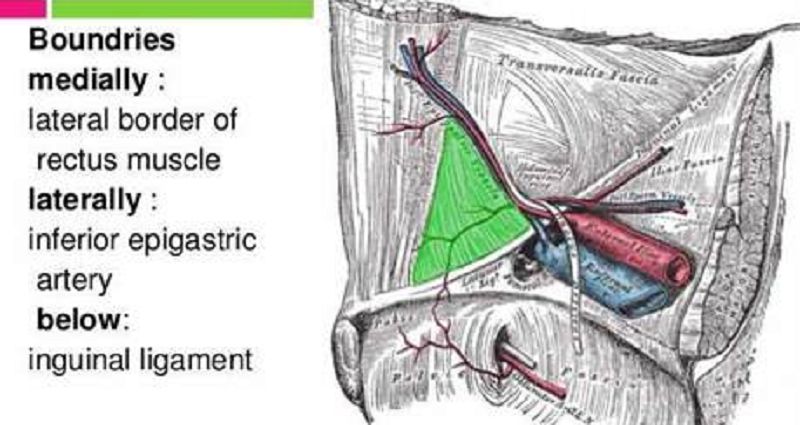
See above laparoscopic (inside) view
Hasselbach's triangle is the space defined by the anatomic relationships described above. A direct hernia comes through this anatomic space.
See above laparoscopic (inside) view
Hasselbach's triangle is the space defined by the anatomic relationships described above. A direct hernia comes through this anatomic space.
True or False – Females can NOT develop an indirect inguinal hernia because they do not have a spermatic cord
True
False
Explanation:
Females CAN develop both indirect and direct inguinal hernias. While females do not have a spermatic cord and thus do not have a persistent processus vaginalis, their equivalent embryologic structure is known as the Canal of Nuck. Women with a patent Canal of Nuck can develop an indirect hernia. Direct hernias in women and men occur through the same anatomic structures and boundaries (Hasselbach's triangle).
Explanation:
Females CAN develop both indirect and direct inguinal hernias. While females do not have a spermatic cord and thus do not have a persistent processus vaginalis, their equivalent embryologic structure is known as the Canal of Nuck. Women with a patent Canal of Nuck can develop an indirect hernia. Direct hernias in women and men occur through the same anatomic structures and boundaries (Hasselbach's triangle).
Which of the following children can be safely observed for months to years due to the fact that their hernia may spontaneously resolve?
A. 12 month old with a reducible umbilical hernia
B. 6 month old with reducible inguinal hernia
C. 12 month old with an incarcerated umbilical hernia
D. 6 month old with an incarcerated inguinal hernia
E. A & B only
Explanation:
All children (regardless of age) who present with an incarcerated umbilical or inguinal hernia should be taken urgently to the operating room for surgical reduction and repair of the hernia. Young children, typically less than 5 years old, with reducible umbilical hernias can be safely observed as many of these umbilical hernias will resolve spontaneously. All children of any age with a reducible inguinal hernia should undergo elective hernia repair. Inguinal hernias do not resolve spontaneously and always require repair. Younger infants and children are at increased risk of incarceration of inguinal hernias.
Explanation:
All children (regardless of age) who present with an incarcerated umbilical or inguinal hernia should be taken urgently to the operating room for surgical reduction and repair of the hernia. Young children, typically less than 5 years old, with reducible umbilical hernias can be safely observed as many of these umbilical hernias will resolve spontaneously. All children of any age with a reducible inguinal hernia should undergo elective hernia repair. Inguinal hernias do not resolve spontaneously and always require repair. Younger infants and children are at increased risk of incarceration of inguinal hernias.
All of the following are common causes of postoperative fever EXCEPT: (choose one)
Walking (DVT/PE)
Wind (Atelectasis)
Wound (surgical site infection)
Watery Diarrhea (Rotovirus)
Wonder Drugs (Drug fever)
Explanation:
The five 5 W's is a common mnemonic to remember the causes of post-op fever.
1. Walking (DVT/PE)
2. Wind (atelectasis)
3. Wound (surgical site infection)
4. Water (Urinary tract infection)
5. Wonder drugs (drug fever)
Watery Diarrhea is not a common cause of post-operative fever. Antibiotic associated colitis (c-diff colitis, not rotovirus) can cause a fever, but is a less common cause of post-op fever than the 5 W's.
Explanation:
The five 5 W's is a common mnemonic to remember the causes of post-op fever.
1. Walking (DVT/PE)
2. Wind (atelectasis)
3. Wound (surgical site infection)
4. Water (Urinary tract infection)
5. Wonder drugs (drug fever)
Watery Diarrhea is not a common cause of post-operative fever. Antibiotic associated colitis (c-diff colitis, not rotovirus) can cause a fever, but is a less common cause of post-op fever than the 5 W's.
Trauma patients with multiple injuries and significant blood loss are susceptible to the development of: (choose one)
Hyperthermia, coagulopathy, acidosis
Hypotension, coagulopathy, alkalosis
Hypothermia, hyperglycemia, alkalosis
Hypothermia, coagulopathy, acidosis
Explanation:
Hypothermia, coagulopathy, and acidosis is known is known by many names (bloody viscous cycle, trauma triad of death, etc). The triad is multifactorial and self sustaining. It typically occurs in patients sustaining multiple serious traumatic injuries and massive blood loss. The cycle is best treated by employing preventative strategies (control of hemorrhage, patient warming, blood product replacement). For patients who develop this often lethal triad, the surgical principles involve control of surgical bleeding, packing to control non-surgical bleeding, contamination control, temporary abdominal closure, rapid return to ICU for continued resuscitation, and planned return to the OR in 12-24 hours. Definitive repair of nonlethal injuries is delayed until the patient is stabilized. This surgical approach is known as "damage control surgery".
Explanation:
Hypothermia, coagulopathy, and acidosis is known is known by many names (bloody viscous cycle, trauma triad of death, etc). The triad is multifactorial and self sustaining. It typically occurs in patients sustaining multiple serious traumatic injuries and massive blood loss. The cycle is best treated by employing preventative strategies (control of hemorrhage, patient warming, blood product replacement). For patients who develop this often lethal triad, the surgical principles involve control of surgical bleeding, packing to control non-surgical bleeding, contamination control, temporary abdominal closure, rapid return to ICU for continued resuscitation, and planned return to the OR in 12-24 hours. Definitive repair of nonlethal injuries is delayed until the patient is stabilized. This surgical approach is known as "damage control surgery".
Stable trauma patients that suffer an isolated moderate grade (grade II or III) blunt abdominal solid organ injury are usually managed successfully with: (choose one)
Emergent exploratory laparotomy and removal of injured solid organ
Emergent exploratory laparotomy, abdominal packing, temporary abdominal closure
Interventional radiology consult for angioembolization of bleeding organ
Admission to a monitored bed for close observation, bed rest, serial hematocrit levels, serial abdominal exams
Explanation:
Blunt abdominal solid organ injury is a common injury encountered by trauma and general surgeons. Commonly injured solid organs within the abdomen include the liver, spleen, kidneys, and pancreas. Surgeons can typically manage moderate grade blunt abdominal solid organ injury successfully by utilizing a nonoperative approach. Patients who are hemodynamically unstable or exhibit persistent bleeding may need more aggressive therapy to include interventional radiology procedures or laparotomy.
Explanation:
Blunt abdominal solid organ injury is a common injury encountered by trauma and general surgeons. Commonly injured solid organs within the abdomen include the liver, spleen, kidneys, and pancreas. Surgeons can typically manage moderate grade blunt abdominal solid organ injury successfully by utilizing a nonoperative approach. Patients who are hemodynamically unstable or exhibit persistent bleeding may need more aggressive therapy to include interventional radiology procedures or laparotomy.
An ankle-brachial index (ABI) of 0.6 is indicative of: (select one)
Significant peripheral vascular disease
Noncompressible/calcified vessels in a patient with longstanding diabetes
Abdominal aortic aneurysm > 5 cm diameter
Popliteal artery aneurysm > 2 cm diameter
The ankle brachial index (ABI) is a noninvasive test that is calculated by dividing the systolic blood pressure just proximal to the ankle with the systolic blood pressure measured at the upper arm. Normal ABI is 1. ABI < 0.9 is abnormal and and ABI of < 0.6 is usually indicative of significant peripheral vascular disease (often associated with rest pain or critical limb ischemia). ABI of >1.2 is indicative of calcified vessels often seen in patients with long standing diabetes.
The ankle brachial index (ABI) is a noninvasive test that is calculated by dividing the systolic blood pressure just proximal to the ankle with the systolic blood pressure measured at the upper arm. Normal ABI is 1. ABI < 0.9 is abnormal and and ABI of < 0.6 is usually indicative of significant peripheral vascular disease (often associated with rest pain or critical limb ischemia). ABI of >1.2 is indicative of calcified vessels often seen in patients with long standing diabetes.
{"name":"Madigan General Surgery MSIII Quiz", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 22 year old previously healthy male presents with a 1 day history of right lower quadrant abdominal pain, fever, nausea, and anorexia. The differential diagnosis for this patient includes: (select one), Explanation:Appendicitis should be high on your differential diagnosis for this young healthy male. However, other disease processes should be considered in the differential diagnosis. Both Meckel's Diverticulitis and Mesenteric Lymphadenitis can cause acute right lower quadrant abdominal pain. Other diagnoses to consider are nephrolithiasis, terminal ileitis (infectious or inflammatory), torsion of the epiploic appendix, omental torsion, urinary tract infection, right sided diverticulitis, inflammatory bowel disease, cholecystitis, and many more. In females, the differential diagnosis includes conditions of the reproductive tract such as ovarian torsion, ovarian cysts, pelvic inflammatory disease, and endometriosis., For patient’s with clinical and radiographic evidence of a small bowel obstruction, possible treatment options include which of the following: (select one)","img":"https://cdn.poll-maker.com/8-402670/hernia-11-638.jpg?sz=1200-000019100053"}
More Quizzes
Study Guide part 2
104520
Where the Food Comes From
10515
Quien eres de pitukis?
52629
Chimie thrapeutic ung channy (101-179)
80400
Free Counting Money Practice Test
201022444
Amplification Lab
15824699
Think You Understand Heat? Free Thermal Energy Inside
201032358
Discover Your Hidden Power With This Fun Magic
201027076
Engineering Ambassadors Leadership Training
15826813
Quiz Volcanoes: Test Your Earthquake & Volcano IQ
201030105
Free Economics Final Exam Review
201024913
The Giver Book Chapter 13-15: Test Your Knowledge
201026813