USLME medecine interne
A family brings their 82-year-old grandmother to the emergency room stating that they cannot care for her anymore. They tell you, “She has just been getting sicker and sicker.” Now she stays in bed and won’t eat because of stomach pain. She has diarrhea most of the time and can barely make it to the bathroom because of her weakness. Her symptoms have been worsening over the past year, but she has refused to see a doctor. The patient denies symptoms of depression. Blood pressure is 90/54 mmHg with the patient supine; it drops to 76/40 mmHg when she stands. Heart and lungs are normal. Skin examination reveals a bronze coloring to the elbows and palmar creases. What laboratory abnormality would you expect to find in this patient?
Low serum Ca+
Low serum K+
Low serum Na+
Normal serum K+
Microcytic anemia
A 58-year-old woman presents to her physician because of neck discomfort and difficulty swallowing. She first began to have difficulty with swallowing solids 2 years ago, but the problem is getting progressively worse. She denies hemoptysis, hematemesis, abdominal pain, or change in bowel habits. She is a nonsmoker and past medical history is significant only for mild hypertension. Her temperature is 36.9°C (98.4°F), heart rate is 72/min, and blood pressure is 132/78 mmHg. She has an asymmetrically enlarged thyroid gland that is particularly firm on the right, with poorly palpable borders. Laboratory evaluation reveals a free thyroxine level of 4.1 ng/dL and thyroid-stimulating hormone of 5μU/mL. Based on the results of a radioisotope scan and a fine needle aspiration biopsy, the physician decides to perform surgery. For which of the following is the patient at increased risk postoperatively?
Bone metastases
Hypercalcemia
Hypocalcemia
Hypophosphatemia
Pheochromocytoma
A 53-year-old woman presents to the clinic with complaints of headache and blurred vision for the past several months. She also says her family has commented that her face looks different, and her nose is bigger than it used to be. In addition, she says her shoes feel tighter. On physical examination she has coarse facial features with a prominent mandible and widely spaced incisors. MRI of the brain reveals a mass in the pituitary. This patient may be at increased risk of developing which of the following malignancies?
Colon cancer
Hepatocellular carcinoma
Lung cancer
Malignant brain tumor
Pancreatic adenocarcinoma
A 35-year-old white female comes to her primary care physician for the evaluation of palpitations, weight loss, increased appetite and diarrhea for the past 2 months. She denies smoking cigarettes or drinking alcohol. Her temperature is 37.1°C (98°F), blood pressure is 135/80 mmHg, respirations are 14/min, and pulse is 90/min. Physical examination shows exophthalmos, lid lag, lid retraction, and a diffusely enlarged, non-tender thyroid gland. Lab studies show very low levels of serum TSH, and increased levels of serum free T4 and T3. The diagnosis of Graves' disease is established. Various treatment options are discussed with the patient, and she opts for long-term treatment with propylthiouracil. Which of the following conditions is this patient at risk for developing?
Agranulocytosis
Hypocalcemia
Permanent hypothyroidism
Recurrent laryngeal nerve palsy
Thyroid cancer
A 35-year-old white female presents with complaints of weight gain, lethargy and constipation for the last 2 months. She also complains of cold intolerance and oligomenorrhea. She is not taking any medication. She is a non-smoker, and does not drink alcohol. Her pulse is 67/min, and blood pressure is 130/90 mmHg. She is afebrile. Her hands are dry and cold. There is a non-tender, diffuse rubbery enlargement of the thyroid gland without any discrete nodularity. She does not have exophthalmos, lid lag or lid retraction. Labs show decreased serum T4 levels, elevated serum TSH levels and positive anti-thyroperoxidase (TPO) antibodies. Which of the following complications may develop in this patient?
Lymphoma of the thyroid
Papillary carcinoma of the thyroid
Follicular carcinoma of the thyroid
Anaplastic carcinoma of the thyroid
Medullary carcinoma of the thyroid
A 36-year-old female presents with weight loss, palpitations, mild shortness of breath, heat intolerance, tremors, and increased sweating. She does not have any past medical problems. Her family history is unremarkable. Her blood pressure is 140/70 mmHg, heart rate is 104/min and regular, temperature is 99.0°F (37.2°C) and respiratory rate is 22/min. Physical examination reveals a 2 x 2 cm nodule in her left thyroid lobe. The rest of her thyroid gland feels normal. There are no palpable lymph nodes in her neck. Eye examination reveals minimal lid lag, but no signs of proptosis or chemosis. She has tremors in both of her upper extremities. Her hands are moist and warm. Thyroid function testing reveals: Serum TSH < 0.03 micro IU/ml, Total T3 330 ng/dl, Total T4 14 mcg/dl. Radioactive iodine scan shows uptake only in her left-sided nodule. Which of the following disorders is this patient at risk of developing if she is left untreated?
Bone loss
Airway compression
Thyroid cancer
Coronary artery disease
Proptosis
A 55-year-old male presents with complaints of an ulcer over the sole of his right great toe for one week. His medical problems include a ten year history of hypertension, diabetes and hypercholesterolemia. His current medications are ramipril, aspirin, metformin, glibenclamide and pravastatin. He has a 20-pack year history of smoking and occasionally drinks alcohol. He denies illegal drug use or multiple sexual partners. Which of the following is most likely contributing to the development of his foot ulcer?
History of smoking
Diabetic neuropathy
Poor glycemic control
Peripheral vascular disease
Bony abnormality of the foot
A 49-year-old woman presents to the emergency department (ED) with profuse, foul-smelling, watery diarrhea and abdominal pain. Five days ago, she was hospitalized for urosepsis and treated with amoxicillin and sulbactam. She recovered well, and was discharged three days ago with a prescription for oral amoxicillin plus clavulanic acid. Her current temperature is 38.8°C (101.9°F), blood pressure is 110/70 mmHg, pulse is 102/min, and respirations are 15/min. Abdominal examination shows tenderness in the left lower quadrant. CBC shows a WBC count of 25,000/microl. She is started on intravenous normal saline in the ED. Which of the following is the most appropriate next step in management?
Continue rehydration
Start oral metronidazole
Discontinue antibiotics
Discontinue antibiotics and start oral metronidazole
Discontinue antibiotics and start oral vancomycin
A 64-year-old man is brought to the ER after an episode of coffee ground emesis followed by lightheadedness. He has been having black, tarry stools for the past few days. He has a history of coronary artery disease and he underwent coronary artery bypass surgery three years ago. He is currently taking aspirin, metoprolol, lisinopril, and pravastatin. He drinks 2-3 beers over the weekend but he quit smoking after the bypass surgery. His temperature is 36.7°C (98°F), pulse is 110/min, respirations are 16/min, and blood pressure is 90/60 mmHg. Examination shows coffee ground-like material in the oropharynx. His lungs are clear. Abdomen is slightly tender in the epigastrium. Laboratory studies show: Complete blood count: Leukocyte count 9,500/mm3, Hemoglobin 8.1 g/L, Platelets 130,000/mm3. Chemistry panel: Serum sodium 140 mEq/L, Serum potassium 3.5 mEq/L, Bicarbonate 27 mEq/L, Blood urea nitrogen (BUN) 54 mg/dL, Serum creatinine 1.2 mg/dL Which of the following is the most appropriate next step in management of this patient?
Whole blood transfusion
Packed red blood cell transfusion
Fresh frozen plasma infusion
Hemodialysis
Platelet transfusion
A 50-year-old female presents with heartburn and gnawing abdominal pain. She was diagnosed with peptic ulcer disease 3 years ago, but she has been non-adherent to her medications. She asks you if her nonadherence puts her at increased risk of any complications. Which of the following is the most common complication of peptic ulcer disease?
Perforation
Penetration
Gastric outlet obstruction
Hemorrhage
Atrophic gastritis
A 37 -year-old male is brought to the emergency department due to an episode of hematemesis. He has a history of peptic ulcer disease. A nasogastric tube lavage yields coffee-ground-like material. Physical examination reveals pallor and delayed capillary refill, without cyanosis. His temperature is 36.7°C (98°F), blood pressure is 85/40 mmHg, pulse is 125/min, and respirations are 18/min. Which of the following is the most appropriate first step in management?
Intravenous octreotide
Upper GI endoscopy
Surgical intervention
Intravenous pantoprazole
Fluid resuscitation
A 54-year-old man is brought to the ER because of an episode of coffee ground emesis and lightheadedness. He has a history of intravenous drug use, hepatitis C infection, and alcohol use. He says he has not had an alcoholic drink for about three days. He has been noncompliant with medications and follow-ups. He takes no medications. His temperature is 36.7°C (98°F), pulse is 110/min, respirations are 16/min, and blood pressure is 90/60 mmHg. Scleral icterus is present. Examination shows coffee ground material in the oropharynx. His lungs are clear. His abdomen is distended and a fluid wave is present. He is slightly tender to palpation in the epigastrium. Laboratory studies show: Complete blood count:Leukocyte count 9,500/mm3, Hemoglobin 10.0 g/L, Platelets 120,000/mm3. Chemistry panel:Serum sodium 140 mEq/L, Serum potassium 3.5 mEq/L, Bicarbonate 27 mEq/L, Blood urea nitrogen (BUN) 34 mg/dL, Serum creatinine 0.8 mg/dL. Coagulation studies :Prothrombin time 27 sec, Partial thromboplastin time 42 sec. Which of the following is the most appropriate next step in the management of this patient?
Whole blood transfusion
Fresh frozen plasma infusion
Hemodialysis
Pooled platelet transfusion
Plasmapheresis
An undomiciled 41-year-old man walks into the ED complaining of abdominal pain, nausea, and vomiting. He tells you that he has been drinking beer continuously over the previous 18 hours. On examination, his vitals are BP 150/75 mm Hg, HR 104 beats per minute, RR 16 breaths per minute, oxygen saturation 97% on room air, temperature of 99.1°F rectally, and finger stick glucose 81 mg/dL. The patient is alert and oriented, his pupils anicteric. You notice gynecomastia and spider angiomata. His abdomen is soft but tender in the RUQ. Laboratory tests reveal an AST of 212 U/L, ALT 170 U/L, alkaline phosphatase of 98 U/L, total bilirubin of 1.9 mg/dL, international normalized ratio (INR) of 1.3, WBC 12,000/μL. Urinalysis shows 1+ protein. Chest x-ray is unremarkable. Which of the following is the most appropriate next step in management?
Place a nasogastric tube in the patient’s stomach to remove any remaining ethanol
Order a HIDA scan to evaluate for acute cholecystitis
Administer hepatitis B immune globulin
Send viral hepatitis titers
Provide supportive care by correcting any fluid and electrolyte imbalances
An 84-year-old woman with coronary artery disease, congestive heart failure, peripheral vascular disease, and atrial fibrillation presents to the emergency department with dizziness, weakness, and sudden-onset crampy periumbilical pain. The pain is associated with one episode of diarrhea and one episode of emesis. The patient notes she has been having similar pain after meals for “several months” but never this severe. Her temperature is 37.2°C (98.9°F), heart rate is 135/min, blood pressure is 96/60 mm Hg, and respiratory rate is 16/min. Physical examination is notable for a slightly distended abdomen that is extremely tender to palpation with diminished bowel sounds. There is no rigidity or rebound tenderness noted on the abdominal examination. In addition, the patient has heme positive stool. Her WBC count is 19,500/mm³, hemoglobin is 10.9 g/dL, and platelet count is 159,000/mm³. Liver function testing results are normal. After stabilizing the patient, what is the best next step in management?
Barium enema
Colonoscopy
Laparotomy
Obstruction series
Warfarin therapy
A 51-year-old man is brought to the emergency department (ED) by emergency medical services (EMS) with a blood pressure (BP) of 90/60 mm Hg, heart rate (HR) of 110 beats per minute, respiratory rate (RR) of 18 breaths per minute, and oxygen saturation of 97% on room air. The patient tells you that he has a history of bleeding ulcers. On examination, his abdomen is tender in the epigastric area. He is guaiac positive, with black stool. He has a bout of hematemesis and you notice that his BP is now 80/50 mm Hg, HR is 114 beats per minute, as he is slowly starting to drift off. Which of the following is the most appropriate next step in therapy?
Assess airway, establish two large-bore intravenous (IV) lines, cross-match for two units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Assess airway, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor
Place two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor
19-year-old woman presents to the ED with 1 hour of acute-onset progressively worsening pain in her RLQ. She developed nausea shortly after the pain and vomited twice over the last hour. She had similar but less severe pain 2 weeks ago that resolved spontaneously. Her BP is 123/78 mm Hg, HR is 99 beats per minute, temperature is 99.1°F, and her RR is 16 breaths per minute. On physical examination, the patient appears uncomfortable, not moving on the gurney. Her abdomen is nondistended, diffusely tender, worst in the RLQ. Pelvic examination reveals a normal-sized uterus and moderate right-sided adnexal tenderness. Laboratory results reveal WBC 10,000/μL, hematocrit 38%, and a negative urinalysis and β-hCG. Pelvic ultrasound reveals an enlarged right ovary with decreased flow. Which of the following is the most appropriate management for this patient?
Admit to the gynecology service for observation
Administer IV antibiotics and operate once inflammation resolves
Attempt manual detorsion
Order an abdominal CT
Go for immediate laparoscopic surgery
A 22-year-old woman is brought to the ED by ambulance complaining of sudden onset of severe abdominal pain for 1 hour. The pain is in the RLQ and is not associated with nausea, vomiting, fever, or diarrhea. On the pelvic examination you palpate a tender right adnexal mass. The patient’s last menstrual period was 6 weeks ago. Her BP is 95/65 mm Hg, HR is 124 beats per minute, temperature is 99.8°F, and RR is 20 breaths per minute. Which of the following are the most appropriate next steps in management?
Provide her oxygen via face mask and administer morphine sulfate
Administer morphine sulfate, order an abdominal CT with contrast, and call an emergent surgery consult
Send the patient’s urine for analysis and order an abdominal CT
Bolus 2 L NS, order a type and crossmatch and β-hCG, and call gynecology for possible surgery
Provide oxygen via face mask, give morphine sulfate, and order a transvaginal ultrasound
A 67-year-old man is brought to the ED by emergency medical service (EMS). His wife states that the patient was doing his usual chores around the house when all of a sudden he started complaining of severe abdominal pain. He has a past medical history of coronary artery disease and hypertension. His BP is 85/70 mm Hg, HR is 105 beats per minute, temperature is 98.9°F, and his RR is 18 breaths per minute. On physical examination, he is diaphoretic and in obvious pain. Upon palpating his abdomen, you feel a large pulsatile mass. An electrocardiogram (ECG) reveals sinus tachycardia. You place the patient on a monitor, administer oxygen, insert two largebore IVs, and send his blood to the laboratory. His BP does not improve after a 1-L fluid bolus. Which of the following is the most appropriate next step in management?
Order a CT scan to evaluate his aorta
Call the angiography suite and have them prepare the room for the patient
Order a portable abdominal radiograph
Call surgery and have them prepare the operating room (OR) for an exploratory laparotomy
Call the cardiac catheterization laboratory to prepare for stent insertion
A 32-year-old man with Crohn’s disease presents to the emergency department with acute-onset diffuse abdominal pain and emesis. The patient states these symptoms are different than his usual Crohn’s disease flare-ups. The pain is severe (10/10) and is cramping in nature. He says his abdomen feels larger than usual. His Crohn’s disease has been well managed on 6-mercaptopurine for the past 6 months. The patient denies any recent sick contacts or eating underprepared foods. He states he had a bowel movement and flatus since the abdominal pain began. In addition to Crohn’s disease, the patient had appendicitis for which he underwent an appendectomy 12 years ago. His temperature is 37.1°C (98.7°F), blood pressure is 135/86 mm Hg, pulse is 84/min, and respiratory rate is 14/ min. On physical examination the abdomen is distended and diffusely tender with high-pitched bowel sounds. There is rebound tenderness throughout the abdomen along with guarding. The remainder of the physical examination is noncontributory. An x-ray of the abdomen shows dilated small loops of bowel along with absence of gas in the colon. What is the best next step in management?
Bowel rest only
Intravenous fluids and antibiotics only
Laparotomy
MRI of the abdomen
Ultrasound
A 24-year-old man with a history of depression is brought to the emergency room because of a drug overdose. He is experiencing some nausea and vomiting, but no other symptoms. Physical examination and vital signs are normal. Six hours prior to presentation, he intentionally took 40 tablets of acetaminophen (500mg/tablet). Which of the following is the most appropriate next step in management?
Give ethanol to compete with the parent drug for metabolism, therefore preventing formation of toxic metabolites
Give Narcan to block its actions directly
Give intravenous prostacyclins to maintain cellular integrity
Give N-acetylcysteine to allow binding of the toxic metabolite
Give glucocorticoids to block the immune cascade
A 59-year-old woman with renal cell carcinoma presents to the emergency department with severe right upper quadrant (RUQ) pain. She is afebrile, acutely tender in the RUQ, and has shifting dullness and a palpable liver edge. Murphy’s sign is negative. Laboratory studies show: Na+: 138 mEq/L, K+: 3.6 mEq/L, Glucose: 80 mg/dL. Aspartate aminotransferase: 50 U/L Alanine aminotransferase: 43 U/L Alkaline phosphatase: 138 U/L Total protein: 6.4 g/dL, Albumin: 3.8 g/dL, Total bilirubin: 1.1 mg/dL. Imaging demonstrates a spider web of collateral veins in the liver. Although extensive measures are taken, the patient dies 6 hours after arriving. Which of the following was the most likely initial treatment?
β-Blocker followed by lactulose
Cholecystectomy
Endoscopic retrograde cholangiopancreatography with dilation of the common bile duct
Exploratory laparotomy
Tissue plasminogen activator followed by anticoagulation
A 67-year-old woman with a history of hypertension and congestive heart failure presents with “burning” epigastric pain that began 2 hours after eating a meal. She states that she has had similar pain over the past several weeks, and has been taking antacids and a medication that her primary care physician had prescribed with moderate relief. The pain has occurred with increasing frequency and now awakens her from sleep. She states she came to the ED today because the pain was not relieved with her usual medications. She denies nausea, vomiting, diarrhea, or fever. She also denies hematemesis, black stool, or bright red blood per rectum. On physical examination, she is tender at the epigastrium, with an otherwise normal abdominal, pulmonary, and heart examination. Stool guaiac tests positive for occult blood. Which of the following is the most common serious complication of peptic ulcer disease?
GI haemorrhage
GI perforation
GI penetration
Gastric outlet obstruction
Pernicious anemia
A 70-year-old man with a history of constipation has been experiencing intermittent left-sided abdominal pain and fevers for 2 days. He came to the emergency department immediately after he noticed blood in his toilet this morning. His heart rate is 110/min, blood pressure is 90/50 mm Hg, respiratory rate is 18/ min, and oxygen saturation is 95% on room air. On physical examination the physician notes copious amounts of bright red blood per rectum. The physician immediately places two large bore intravenous lines, administers fluid, and sends blood for type and screen. Which of the following is the best next step in management?
Arteriography
Colonoscopy
Endoscopy
Nasogastric tube aspiration
Surgical consultation
A 75-year-old woman with a history of diabetes and coronary heart failure presents to the emergency department because of increasing abdominal girth. In recent months she has been feeling increasingly fatigued, and although she has had decreased appetite, she has gained weight. Her heart rate is 100/min and blood pressure is 112/70 mm Hg. She has scleral icterus; the skin over her face, neck, and lower legs is slightly bronze in color; she has palmar erythema; and she has numerous ecchymoses over her body. Her abdominal examination is significant for ascites. Laboratory tests show: Aspartate transaminase: 102 U/L, Alanine transaminase: 97 U/L, Alkaline phosphatase: 300 U/L, Total bilirubin: 1.9 mg/dL, Albumin: 2.9 g/dL, Prothrombin time: 22 sec, Partial thromboplastin time: 42 sec. An ultrasound of her abdomen shows a shrunken and nodular liver. A liver biopsy using Perls Prussian blue stain is shown in the image. Which of the following is the most likely complication of her disease?
Acute pancreatitis
Amyloidosis
Bone marrow failure
Hepatocellular carcinoma
Splenomegaly
A 62-year-old woman with a history of diabetes mellitus presents to the emergency department complaining of severe abdominal pain for the past 12 hours, first beginning as dull pain near the umbilicus but now localized to the right lower quadrant. She initially thought she was suffering from heartburn, but decided to come to the hospital because of the unrelenting pain. The patient reports that just prior to examination by the physician, she experienced a sudden decrease in intensity of pain, but she remains feeling very uncomfortable and must remain on the stretcher. On examination the patient appears in distress secondary to pain, tachycardic, slightly hypotensive, and febrile at 39°C (102°F). She has a diffusely tender abdomen with point tenderness over her right lower quadrant, accompanied by guarding and rebound. Laboratory values showed a leukocytosis of 20,000/mm³ with 95% polymorphonuclear lymphocytes. After confirming the diagnosis with imaging, which of the following is the most appropriate management?
Emergent appendectomy and postoperative antibiotics
Give nothing by mouth with intravenous hydration
Percutaneous drainage and interval appendectomy
Serial abdominal examinations
Urgent ECG and cardiac enzymes
A 57-year-old woman presents to the ED with a basin in her hand and actively vomiting. You insert an IV catheter, start IV fluids, and administer an antiemetic agent. The patient feels much better but also complains of severe crampy abdominal pain that comes in waves. You examine her abdomen and note that it is distended and that there is a small midline scar in the lower abdomen. Upon auscultation, you hear high-pitched noises that sound like “tinkles.” Palpation elicits pain in all four quadrants but no rebound tenderness. She is guaiac negative. Which of the following is the most common cause of this patient’s presentation?
Travel to Mexico
Ethanol abuse
Hysterectomy
Hernia
Constipation
A 48-year-old woman comes to the office because her regular screening mammogram revealed irregular densities. Radiographic-guided needle biopsy shows evidence of invasive lobular carcinoma. The tumor is hormone receptor positive (HR +). Further investigation reveals involvement of the axillary lymph nodes; the other breast seems to be spared. No distant metastasis is detected. She undergoes modified radical mastectomy, along with radiotherapy. She is then prescribed adjuvant chemotherapy and tamoxifen for 5 years. This patient's use of tamoxifen increases her risk for developing which of the following cancers:
Ovarian cancer
Endometrial cancer
Lung cancer
Pancreatic cancer
Cervical cancer
A 54-year-old Caucasian woman presents to your office with fatigue. She also reports dizziness and palpitations after moderate physical activity. Additionally, her feet feel "numb" and are less sensitive to cold than they used to be. She has no significant past medical history. Physical examination reveals pale conjunctivae and a shiny tongue. Ankle reflex is decreased bilaterally. Laboratory findings include: Hemoglobin 7.6 mg/dL, MCV 110 fL, MCHC 36 g/dL, WBC count 3,900/mm3, Platelet count 150,000/mm3. This patient should be monitored for which of the following long-term complications?
Acute myelogenous leukemia
Hodgkin's disease
Celiac sprue
Gastric cancer
Liver cirrhosis
A 34-year-old male is brought to the emergency room after being involved in a motor vehicle accident. He suffers blunt abdominal trauma and bilateral femur fractures. He has no significant past medical history. On physical examination, his blood pressure is 80/40 mmHg and his heart rate is 110/min. He receives several units of packed red blood cells. Once stabilized, the patient begins complaining of a tingling sensation in his toes and fingers. His serum calcium level is noted to be 7.2 mg/dL. Which of the following is the most likely cause of this patient's current symptoms?
Increased renal tubular secretion of calcium
Calcium chelation by a substance in the transfused blood
Electrolyte leakage from red blood cells during pre-transfusion storage
Antibody-mediated red blood cell membrane damage
Parathyroid gland suppression due to fluid overload
An 81-year-old man is brought to the hospital due to complaints of very severe pain in his back and thighs. Seven months ago, he was diagnosed with stage IV prostate cancer which reached the spine. He has had palliative radiotherapy of his spine, and is now taking leuprolide. He is restless and very irritable, even after the nursing home staff gave him ibuprofen. He has never received any narcotics. What is the best next step in this patient's pain management?
Give high dose NSAIDs
T ransdermal fentanyl patch
Start with short-acting morphine
Long-acting opiates
Repeat radiotherapy
A 45-year-old previously healthy male is brought to the emergency room because of headaches and confusion for 2 days. He denies any focal weakness or sensory symptoms. He has no significant past medical history and does not use any medications. He does not use tobacco, alcohol or drugs. On physical exam, the patient has a temperature of 37.9°C (100.2°F), a blood pressure of 140/86 mm Hg, a pulse of 96/min, and respirations of 16/min. Mild icterus is present. The patient's oropharynx is clear and his neck is supple and without rigidity. Examination of the patient's chest and abdomen is unremarkable. Neurologic examination reveals no focal deficits. Laboratory studies show: Complete blood count: Hemoglobin 84 g/L, Platelet count 80,000/mm3, Leukocyte count 5,500/mm3. Chemistry panel:Blood urea nitrogen (BUN) 30 mg/dL, Serum creatinine 2.2 mg/dL, Serum calcium 10.0 mg/dL, Blood glucose 98 mg/dL. A peripheral blood smear shows many fragmented red blood cells. The prothrombin time is normal. Which of the following is the most appropriate next step in the management of this patient?
Hemodialysis
MRI of the brain
Electroencephalogram
Plasma exchange
Platelet transfusion
A 54-year-old male comes to the emergency department with complaints of cough and bloody sputum. He used to smoke 2 packs of cigarettes daily for 22 years, but states that he quit last month. He also complains of weight loss, anorexia, constipation, increased thirst, and easy fatigability, which he attributes to depression. He lost his wife 4 months ago and "life never felt the same after that." He is sure that he cannot have cancer because he does not smoke anymore. His vital signs are stable. He appears slim, pale, slightly irritable, and short of breath. The laboratory studies and chest x-ray results are as follows: Sodium 144 mEq/dL, Potassium 4.3 mEq/dL, Chloride 98 mEq/dL, Bicarbonate 21 mEq/dL, Calcium 14.5 mg/dl, BUN 48 mg/dl, Creatinine 2.0 mg/dl, Chest x-ray hilar mass in the left lung. While in the ED, he becomes more somnolent and vomits twice. What is the best next step in the management of this patient?
V furosemide
CT scan of the head
IV normal saline
Emergency hemodialysis
IV pamidronate
A 75-year-old Caucasian male who was diagnosed with carcinoma of the prostate presents to ER with worsening back pain for the past 2-3 days. He never had this pain before. He denies any weakness of the legs. On examination, his muscle power in the lower extremities is 4.5/5 and has brisk reflexes. Rectal sphincter tone is weak. He has point tenderness over the L5 and S1 region. His vital signs are, BP: 122/80 mm Hg, PR 80/min, RR 16/min and Temperature 37°C (98°F). What is the most appropriate next step in management of this patient?
Radiotherapy.
Intravenous dexamethasone.
Immediate MRI of spine
Decompression surgery of spine.
CT myelogram.
A 22-year-old African American male suffering from sickle cell anemia presents in the emergency department with a sustained painful penile erection for the last 4 hours. Previously, he had one episode of acute chest syndrome that was treated with oxygenation, hydration and blood transfusion. His pulse is 76/min, respirations are 16/min, blood pressure is 115/76 mm Hg, and temperature is 37°C (98.6°F). Examination of all his systems is unrevealing. What is the best next step in the management of this patient?
Observation
Hyperbaric oxygen therapy
Exchange transfusion
Surgical intervention
Hydroxyurea
A 65-year-old man presents to the emergency department with a two-day history of fever, headache, altered mental status, and vomiting. His past medical history is significant for renal transplantation secondary to polycystic kidney disease, hypertension, and diabetes. He takes aspirin, insulin, nifedipine, cyclosporine, and prednisone. He has no known drug allergies. His temperature is 39.2°C (102.5°F), pulse is 102/min, respirations are 18/min, and blood pressure is 120/75 mm Hg. He is alert but confused. Fundoscopy does not show any abnormalities. His neck is stiff. Lungs are clear to auscultation. He has a normal S1 and S2 with a II/IV systolic ejection murmur heard best in the right infraclavicular area. Complete blood count shows a WBC count of 17,000/cm3 with neutrophilic leukocytosis. His blood is drawn and sent for culture. Lumbar puncture is performed and the results are pending. Which of the following is the most appropriate empiric antibiotic therapy for this patient?
Ceftriaxone
Ceftriaxone and vancomycin
Cefotaxime and ampicillin
Ceftriaxone, vancomycin, and ampicillin
Ceftazidime and vancomycin
A 7-year-old Caucasian boy with a history of cystic fibrosis presents to the emergency department with a two-day history of high-grade fever and cough productive of purulent, green-colored sputum. He also complains of chest pain, which is worsened by breathing. His temperature is 39.6°C (103.2°F), pulse is 112/min, respirations are 26/min, and blood pressure is 90/60 mm Hg. Chest examination shows dullness on percussion and increased tactile fremitus in the right lung base. Chest x-ray shows a right lower lobe infiltrate. Which of the following is the most appropriate pharmacotherapy for this patient?
Ceftriaxone and gentamicin
Azithromycin
Piperacillin and tobramycin
Piperacillin and ciprofloxacin
Dicloxacillin
A 28-year-old man presents to ER with fever, chills, and generalized weakness for the past one week. He has no history of pre-existing heart disease, but he was admitted to the hospital six months ago for cellulitis of the right arm. His temperature is 40.0°C (104°F), pulse is 110/min, respirations are 22/min, and blood pressure is 110/65 mmHg. Oropharynx is clear. Lungs are clear to auscultation. A holosystolic murmur is heard at the lower sternum which increases in intensity with inspiration. His blood is drawn and sent for culture. What is the most appropriate initial antibiotic therapy for this patient?
Ampicillin-sulbactam
Clindamycin
Oxacillin
Penicillin G and gentamycin
Vancomycin
A 45-year-old female presents to emergency room complaining of urinary frequency, burning during urination, and weakness. Her last menstrual period was one year ago, and she is not sexually active. She is not taking any medications. Her temperature is 37.8°C (100°F), blood pressure is 120/76 mmHg, pulse is 80/min, and respirations are 14/min. Very mild costovertebral angle tenderness is present. IV ceftriaxone is started. Two days later, the patient feels much better. Antibiotic susceptibility testing returned with an uropathogen (E.coli) highly sensitive to ceftriaxone, gentamicin, ciprofloxacin and trimethoprim/sulfamethoxazole (TMP/SMX). Which of the following is the most reasonable next step in the management of this patient?
Add ciprofloxacin to the regimen
Switch to TMP/SMX
Switch to gentamicin
Continue ceftriaxone
Discontinue antibiotic therapy
A 54-year-old diabetic woman comes to the emergency department because of increasing neck and facial pain, fever, and chills. A few weeks ago, she developed an infection on the side of her neck. She thought it would go away with over-the-counter medication, but the infection has now started to drain. For the past twenty years, she has had diabetes, which is well-controlled with an oral hypoglycemic. She denies trauma, travel, and smoking. Physical examination reveals an area of erythema and induration at the base of the neck. Serosanguineous fluid is draining from a small defect in the skin near the center of the lesion. There is no crepitus. Histological analysis of the discharge reveals the presence of gram positive, branching bacteria. The treatment for this patient is?
Surgical debridement
Start triple combination TB therapy
Start amphotericin
Hyperbaric oxygenation
Intravenous penicillin
A 72-year-old man presents to the ED during the month of January complaining of non-productive cough, fever, malaise, runny nose, and severe body aches. The symptoms came on suddenly last night. He has no other medical problems. Physical examination reveals a temperature of 38.9°C (102.0°F) and oxygen saturation of 88% on room air. His lung exam reveals diffuse crackles with occasional wheezes. Laboratory values are: Hematocrit 44%, Platelets 219,000/mm3, Leukocyte count 4,100/mm3, Neutrophils 65%, Lymphocytes 32%. His chest x-ray reveals diffuse interstitial infiltrates bilaterally. What is the most appropriate initial therapy for this patient?
Ganciclovir
Tenofovir
Oseltamivir
Valacyclovir
Nevirapine
23-year-old man is brought to the emergency room because of confusion and hallucinations. While in ER, he has an episode of generalized tonic-clonic seizures. His past medical history is significant for illicit drug use. His temperature is 40.0°C (104.0°F), pulse is 95/min, and blood pressure is 120/80 mm Hg. He is confused and disoriented. Fundoscopy is with in normal limits. There is no neck stiffness. The neurological examination shows upgoing plantar reflexes bilaterally. Lumbar puncture is performed and CSF analysis shows the following: Glucose 35mg/dl, Protein 80mg/dl, WBC count 150/cm3, Neutrophils 10%, Lymphocytes 90%, Gram stain Negative. CT scan of the brain without contrast is normal. Which of the following is the most appropriate next step in the management of this patient?
Intravenous acyclovir
MRI of the brain
Intravenous ceftriaxone and vancomycin
CSF culture for herpes simplex virus
Urine toxicology screen
A 65-year-old female who lives in nursing home and is bed ridden due to severe right hemiparesis is brought to the ER because of altered mental status and decreased oral intake. Her past medical history includes hypertension, diabetes, hyperlipidemia, and myocardial infarction. She has a chronic indwelling Foley catheter to avoid contamination of a sacral decubitus ulcer. She is febrile in the ER. Examination shows dry mucus membranes and clear lungs. She is disoriented. The decubitus ulcer has good granulation tissue and does not appear infected. Labs show: Hemoglobin 12.0 g/L, Leukocyte count 12 500/mm3, Blood urea nitrogen (BUN) 28 mg/dL, Serum creatinine 0.8 mg/dL, Serum bicarbonate 24 mg/dL. Urinalysis: Specific gravity 1.036, Protein 1+, pH 8.5, Blood negative, Glucose 1+, Ketones negative, Leukocyte esterase positive, WBC 50-100/hpf, Bacteria few. Which of the following is the most likely cause of her altered mental status?
Urinary tract infection from Escherichia coli
Urinary tract infection from Klebsiella species
Urinary tract infection from Proteus species
Urinary tract infection from Pseudomonas aeruginosa
Urinary tract infection from Candida species
A 21-year-old man presents with symptoms of headache, fever, chills, and discomfort in both sides of his jaw. He has also noticed discomfort in his testes, but no dysuria or urethral discharge. Physical examination reveals bilateral enlargement of the parotid glands, as well as bilateral testicular enlargement and tenderness on palpation. His temperature is 38.5°C pulse rate of 92/min, and the remaining examination is normal. Laboratory data show hemoglobin 15 g/dL; hematocrit 40%; WBC 12000/mL, with 30% segmented neutrophils, 8% monocytes, and 62% lymphocytes. Which of the following statements concerning this dis- ease is true?
The disease is caused by a herpesvirus
The incubation period is 3–5 days
The most common complication of this disease in post pubertal boys and men is orchitis
Recurrent infections may occur
An increased serum amylase is proof of the existence of pancreatitis as a complication
An 8-year-old boy from an impoverished inner- city area has never been vaccinated appropriately. He develops fever, cough, and coryza. The next day, blue white spots develop on the buccal mucosa. On the third day, an erythematous, nonpruritic maculopapular rash develops on the face and spreads over the entire body. Which of the following is the most likely complication?
Pneumonia
Encephalitis
Otitis media
Bronchitis
Mastoiditis
A 6-year-old boy develops symptoms of cough, fever, and malaise followed by a generalized maculopapular rash that has spread from the head downwards. A clinical diagnosis of measles is made. A few days after the onset of the rash he is drowsy, lethargic, and complaining of headache. A lumbar puncture, electroencephalogram (EEG), and computerized tomography (CT) of the brain exclude other etiologies and confirm the diagnosis of encephalitis. Which of the following is the most likely delayed neurologic complication of measles virus encephalitis?
Meningitis
Pure motor paralysis
Autonomic neuropathy
Mental retardation or epilepsy
Stocking-glove peripheral neuropathy
A 24-year-old man complains of fatigue, malaise, fever, and a sore throat. He was previously well, but now feels tired all the time and has to rest multiple times a day. Physical examination shows enlarged tonsils and palpable anterior and posterior cervical, axillary, and inguinal lymph nodes. There is also tenderness in the right upper quadrant with a liver span of 10 cm. Laboratory data is significant for a heterophil antibody (sheep cell agglutination) test that is positive. Which of the following rare complications can be associated with this condition?
Retinitis
Esophagitis
Splenic rupture
Kaposi sarcoma
Hemorrhage
A 65-year-old male presents to the emergency department complaining of fever, chills, and a productive cough for the past 3 days. He also complains of right-sided chest pain and shortness of breath. He says that his chest pain worsens with deep breathing. The patient's past medical history is significant for diabetes and hyperlipidemia. He takes aspirin, simvastatin, metformin, glipizide and rosiglitazone. He does not use tobacco, alcohol or drugs. On physical exam, he has a temperature of 39.2°C (102.5°F), a blood pressure of 110/70 mm Hg, a pulse of 112/min, and respirations of 24/min. His mucus membranes are dry. Chest x-ray reveals a right lower lobe pneumonia. Laboratory studies show: Hemoglobin 17.0 g/L, Platelets 250,000/mm3, Leukocyte count 16,500/mm3, Serum sodium 140 mEq/L, Serum potassium 4.5 mEq/L, Blood urea nitrogen (BUN) 48 mg/dL, Serum creatinine 2.0 mg/dL, Serum calcium 10.3 mg/dL, Blood glucose 128 mg/dL. Blood cultures are obtained and antibiotics are administered. What is the appropriate next step in the management of this patient?
Add lisinopril
Discontinue rosiglitazone
Discontinue metformin
Discontinue glipizide
Begin bisphosphonate therapy
A 70-year-old woman is brought to the emergency department by her daughter because of altered mental status. She lives alone and is able to perform all daily activities. She experienced a minor febrile illness with decreased appetite several days ago, but has otherwise been in good health. She takes no medications. Her temperature is 37.2°C (99°F), blood pressure is 92/50 mm Hg, pulse is 100/min, and respirations are 18/min. Physical examination shows dry oral mucosa. Laboratory studies show: Hematocrit 45%, Serum sodium 147 mEq/L, Serum potassium 5.2 mEq/L, BUN 70 mg/dl, Serum creatinine 1.8 mg/dl. Which of the following is the most appropriate next step in management?
Intravenous colloids
Intravenous crystalloids
Order packed red blood cells
Intravenous antibiotics
Diuretics
A 45-year-old woman presents to the emergency department (ED) with vomiting and severe right flank pain that radiates to her groin. She has been to the ED twice in the past due to similar episodes of renal colic, and was subsequently discharged on both occasions. She admits to not seeking further medical care because she has no insurance. KUB shows a renal stone. 24-hour urine collection shows a urinary calcium excretion of 350 mg (normal is less than 250 mg in women). Laboratory studies show a serum calcium concentration of 8.9 mg/dL; serum PTH is normal. An x-ray film of the chest shows no abnormalities. Further investigations fail to reveal the cause of her hypercalciuria. Apart from advising her to increase her fluid intake, which of the following interventions will benefit this patient?
Restriction of calcium in her diet
Thiazide diuretics
Low dose furosemide
High sodium intake
Potassium citrate
A 65-year-old man is brought to the emergency department due to the sudden onset of weakness. He was lying on the floor for several hours before he was brought in. His other medical problems include hypertension, diabetes mellitus, coronary artery disease, transient ischemic attacks and osteoarthritis. CT scan of the head shows evidence of a right middle cerebral artery territory stroke. Laboratory studies show: Serum Na 137 mEq/L, Serum K 64 mEq/L, Chloride 104 mEq/L, Bicarbonate 18 mEq/L, BUN 36 mg/dl, Serum creatinine 3.0 mg/dl, Calcium 8.3 mg/dl, Blood glucose 178 mg/dl. His serum creatinine level one month ago was 1.4 mg/dl. EKG shows tall 'T' waves. CK level is pending. Which of the following is the most appropriate next step in management?
Insulin with dextrose
Kayexalate
Sodium bicarbonate
Calcium gluconate
Regular insulin
A 3-year-old girl is brought to the emergency department because of fever, chills, vomiting, and abdominal pain. Her temperature is 39.5°C (103.1°F), blood pressure is 70/40 mm Hg, pulse is 110/min, and respirations are 20/min. She is restless and diaphoretic. The abdominal examination shows right costovertebral tenderness. Laboratory studies show: Hemoglobin 15.0 g/L, Platelets 260,000/mm3, Leukocyte count 16,500/mm3, BUN 20 mg/dL, Serum creatinine 1.1 mg/dL. Urinalysis: Blood Negative, Glucose Negative, Ketones Negative, Leukocyte esterase Positive, Nitrites Positive, WBC 40-50/hpf, RBC 5-9/hpf. Blood and urine cultures are taken. Which of the following is the most appropriate next step in management?
Empiric therapy with oral antibiotics
Empiric therapy with intravenous antibiotics
Renal ultrasound
Voiding cystoureterogram
Plain abdominal x-ray
A 45-year-old man comes to the emergency department (ED) with severe right flank pain. He is tossing in bed due to the pain. KUB done in the ED shows no abnormalities; however, abdominal ultrasound shows a 5 mm stone in the right ureter. Urinalysis shows: Urine pH 4.5 (normal is 5-6), WBC Absent, RBC 2-3/HPF, Bacteria Absent, Nitrites Negative, Esterase Negative. Which of the following is the most beneficial next step in management?
Oral sodium bicarbonate
Hydrochlorothiazide
Furosemide
High-protein diet
Calcium-restricted diet
A 35-year-old man comes to the physician due to a one-month history of weight gain and facial edema. The facial edema resolves at the end of the day, but ankle edema develops. His temperature is 37.2°C (99°F), blood pressure is 142/80 mm Hg, pulse is 80/min, and respirations are 16/min. Examination shows 2+ ankle edema. Laboratory studies show: Hb 11.0 g/dl, WBC 8,000/cmm, Platelets 200,000/cmm, Serum Na 135 mEq/L, Serum albumin 2.2 g/dl, BUN 16 mg/dl, Serum creatinine 1.0 mg/dl. Urinalysis: Glucose Absent, Protein 4+, WBC 1-2/HPF, RBC Absent, Casts Fatty casts. This patient is most likely at risk for developing which of the following?
Rupture of brain aneurysm
Abdominal aortic aneurysm
Hypercoagulability
Pulmonary hemorrhage
Gall stone pancreatitis
A 73-year-old man presents to the emergency department complaining of lower abdominal pain and nausea. He denies any vomiting or diarrhea, and his last bowel movement was two days ago. The patient also notes that several days ago he began taking amitriptyline for chronic neck pain. He does not smoke or consume alcohol. On physical examination, his blood pressure is 160/70 mmHg and his heart rate is 100/min. His lung fields are clear to auscultation. Palpation of the abdomen reveals fullness and tenderness along the midline below the umbilicus. Which of the following is the best initial management for this patient?
Abdominal CT scan
Upright abdominal x-ray
Barium enema
Broad spectrum antibiotics
Urinary catheterization
A 34-year-old woman comes to the physician's office because of occasional headaches and palpitations. She has no other medical problems. She takes no medications. She smokes one and a half packs of cigarettes daily. Her blood pressure is 170/100 mm Hg in both arms, and heart rate is 80/min. Physical examination shows bilateral flank masses. Laboratory studies show: Serum sodium 140 mEq/L, Serum potassium 4.4 mEq/L, BUN 26 mg/dL, Serum creatinine 1.3 mg/dL. Urinalysis shows 10-12 red blood cells/hpf, but otherwise shows no abnormalities. The most likely complication that can occur in this patient is which of the following?
Liver necrosis
Intracranial aneurysms
Restrictive cardiomyopathy
Pancreatic cancer
Aortic dissection
A 47-year-old HIV-positive man is brought to the emergency room because of weakness. The patient has HIV nephropathy and adrenal insufficiency. He takes trimethoprim-sulfamethoxazole for PCP prophylaxis and is on triple-agent antiretroviral treatment. He was recently started on spironolactone for ascites due to alcoholic liver disease. Physical examination reveals normal vital signs, but his muscles are diffusely weak. Frequent extrasystoles are noted. He has mild ascites and 1+ peripheral edema. Laboratory studies show a serum creatinine of 2.5 with a potassium value of 7.3 mEq/L. An EKG shows peaking of the T waves and QRS duration of 0.14. What is the most important immediate treatment?
Sodium polystyrene sulfonate (Kayexalate)
Acute hemodialysis
IV normal saline
IV calcium gluconate
IV furosemide 80 mg stat
A 69-year-old man is brought to the ER by his family for increasing confusion. At baseline the patient is interactive and pleasant, but he has become withdrawn and confused over the last several months. He has also complained of abdominal pain, nausea, vomiting and back pain over the same period of time. His medical history is significant for diabetes controlled with metformin and hypertension treated with hydrochlorothiazide. Exam reveals normal vital signs and a disheveled, confused man. His neurologic exam is otherwise normal. Examination of the heart and lungs is unremarkable and no neck masses or nodes are appreciated. Laboratory results are given below: Sodium 139 mEq/L, Potassium 4.2 mEq/L, Chloride 111 mEq/L, Bicarbonate 26 mEq/L, Creatinine 1.4 mg/dl, Glucose 142 mgldl, Calcium 12.8 mEq/L, WBC 3,200/mm3, Hematocrit 32%, Platelets 47,000/mm3. What is the most appropriate next step for this patient?
Hemodialysis
0.9% saline infusion
Pamidronate
Calcitonin
Furosemide
A 38-year-old woman presents to the emergency department and complains of persistent vomiting that has increased in severity over the last week. Her other complaints are muscular weakness, twitching and cramps. Her urine output has decreased over the last 20 hours. Her past medical history is significant for a previously diagnosed prepyloric peptic ulcer. Her pulse is 100/min, blood pressure is 100/60 mmHg, respirations are 12/min, and temperature is 37.2°C (99°F). Physical examination reveals dry oral mucosa and decreased skin turgor. Abdominal examination reveals hypoactive bowel sounds and mild tenderness on palpation of the epigastrium. Nasogastric suction is started, and intravenous normal saline is given. Laboratory studies show: Serum sodium 135 mEq/L, Serum potassium 2.8 mEq/L, Chloride 81 mEq/L, Bicarbonate 40 mEq/L, Blood urea nitrogen (BUN) 42 mg/dl, Serum creatinine 1.3 mg/dl, Calcium 8.6 mg/dl, Ionized calcium 0.7 mmoi/L (1.1-1.3 mmoi/L), Serum pH 7.54. Which of the listed agents should be added to the patient's current therapy?
Ammonium chloride
Potasium chloride
Calcium chloride
Furosemide
Sodium bicarbonate
A 22-year-old man presents to the emergency department complaining of fever, nausea, vomiting, and right lower quadrant pain. He has no significant medical history and does not take any medications. He is a senior in college and denies cigarette smoking or drug use. He drinks alcohol occasionally. Physical examination reveals a temperature of 38.6°C, with all other vital signs within normal limits. ACT scan of his abdomen confirms acute appendicitis. Laboratory analyses reveal a leukocytosis but no electrolyte abnormalities. He is taken to the operating room and undergoes a successful laparoscopic appendectomy. Following the procedure, he is given intravenous fluids containing 5% dextrose in a 0.45% (½normal) saline solution at a rate of 150 ml/hr. The next morning the patient feels well but he then becomes progressively confused throughout the afternoon. You are called to his bedside after he has two grand mal seizures lasting 30 seconds apiece. Serum chemistries drawn at that time reveal a sodium concentration of 115mEq/L. What is the most appropriate therapy for this patient?
Fosphenytoin
3% saline
Normal saline
Phenobarbital
Lorazepam
A 71-year-old man with inclusion body myositis is brought to the emergency department from his nursing home after becoming less interactive. His temperature is 37.1°C, blood pressure is 90/60, heart rate is 98/min, and respiratory rate is 16/min. He has orthostatic vital signs. Physical examination reveals a frail man with dry oral mucosa and decreased axillary perspiration. Laboratory studies reveal the following: Sodium 164 mEq/L, Potassium 4.9 mEq/L, Bicarbonate 29 mEq/L, Chloride 122 mEq/L. What is the most appropriate next step in the management of this patient?
Oral free water
IV 0.9% saline
IV 5% dextrose in water
IV 5% dextrose in 04 5% saline
IV free water
A 55-year-old male is brought to the emergency department with a gunshot wound to his abdomen. He went to the operating room for repair of his injuries. On postoperative day 4, he develops a waxing and waning fever, tachypnea and shortness of breath. His temperature is 40°C (104°F), blood pressure is 90/60 mm Hg, pulse is 110/min and respirations are 22/min. Physical examination reveals an altered sensorium, crackles at the right lung base and a well healing abdominal wound. His urine output over the last 12 hours is 100ml. His laboratory profile shows: Blood pH 7.23, PaO2 60 mm Hg, PaCO2 32 mmHg, HCO3- 16 mEq/L. Broad-spectrum antibiotics are started. Which of the following additional treatments is most appropriate in this patient?
Intravenous sodium bicarbonate
Intravenous Dextrose in water (D5W)
Intravenous 3% saline
Intravenous 0.9% saline
Intravenous dopamine
A 34-year-old Mexican male comes to the emergency department and complains of severe episodic headache, especially at night, for the past month. He also complains of unilateral, sharp, stabbing pain in the eye, which wakes him from sleep. The pain often starts suddenly just behind the right eye, and spreads to his face and temple region. It is not associated with nausea or visual disturbances, but is associated with watering of the eyes and nose, and with red eye. He had a similar episode one year ago, and it lasted for 2 months. Which of the following is the best treatment regimen for aborting the patient's pain during an acute attack?
Oral NSAIDs
Verapamil
Nasal sumatriptan
100 % oxygen
Ergotamine
A 63-year-old man presents to the emergency department with a 6-hour history of slurred speech and right hand weakness. His past medical history is significant for chronic hypertension and a myocardial infarction 2 years ago. His current medications include enalapril and aspirin. He smokes 2 packs of cigarettes daily and consumes alcohol occasionally. His blood pressure is 165/95 mmHg, pulse is 80/min, and respirations are 14/min. Physical examination reveals right hand weakness and mild motor aphasia without sensory abnormalities Which of the following is the most probable cause of this patient's condition?
Large artery atherosclerosis
Cardiac embolus
Berry aneurysm
Hypertension
Arterial dissection
A 37-year-old white female with myasthenia gravis presents to the office with a fever and cough productive of yellow-green sputum. She has been on pyridostigmine for the past few months. She refuses to have a thymectomy. Her pulse is 90/min, blood pressure is 120/76 mm Hg, respirations are 18/min, and temperature is 38.9°C (102°F). Her respiratory effort is weak. Pulse oximetry reveals 86% oxygen saturation on room air. There is a consistent decline on serial measurement of vital capacity. Which of the following is the most appropriate next step in management?
Increase the dose of pyridostigmine
Treatment with edrophonium
Treatment with atropine
Treatment with prednisolone
Endotracheal intubation
A 36-year-old white female is brought to the emergency department due to paraplegia and bladder incontinence. She immediately tells you that she has, "multiple sclerosis in remission." She has a history of optic neuritis and internuclear ophthalmoplegia, and both resolved with treatment. At that time, MRI showed plaques in the periventricular region. She is currently not taking any medications. Which of the following is the most appropriate next step in the management of this patient?
Corticosteroids
Plasmapheresis
Interferon
Cyclophosphamide
Intravenous Immunoglobulins
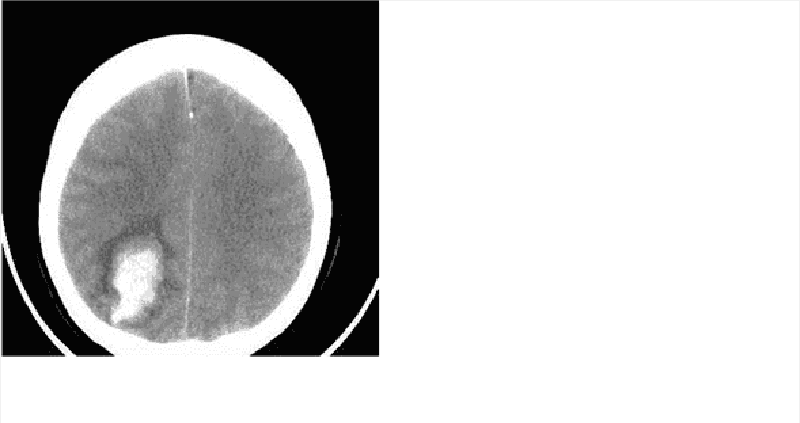
A 64-year-old Caucasian female is rushed to the emergency department (ED) due to a sudden onset of severe headache and altered mental status. By the time she arrived at the ED, she had deteriorated to a stuporous state. She developed a fever and severe dry cough yesterday, but did not take any medicine nor consult her physician. Her medical problems include hypertension, coronary artery disease, atrial fibrillation, mitral valve regurgitation, and psoriasis. Her medications include aspirin, metoprolol, warfarin, amiodarone, and multivitamin tablets. Her blood pressure is 162/80 mm Hg, pulse is 80/min, respirations are 16/min and temperature is 37°C (98°F). Her lab results are: Hb 13 g/dl, WBC 11,000/cmm, Platelets 180,000/cmm, Blood Glucose 118 mg/dl, Serum Na 138 mEq/L, Serum K 4.5 mEq/L, BUN 16 mg/dl, Serum Creatinine 1.0 mg/dl, PT 25.0sec, INR 4.0. Which of the following is the most appropriate next step in management?
Give fresh frozen plasma
IV infusion of vitamin K
Order t-PA
Stop warfarin and start heparin
Obtain liver function panel
A 24-year-old male is brought to the emergency room after he fainted while practicing football on a bright sunny day. He complained of dizziness and headache before he collapsed. He was in his usual state of health until today and has no medical problems. He takes no medication. On arrival to the emergency room, his temperature is 41°C (105.8°F), blood pressure is 90/60 mm Hg, pulse is 140/min, and respirations are 22/min. He is not oriented. Skin is dry and hot. Neck is supple. Auscultation of the chest is unremarkable. Abdomen is soft and non-tender. Muscle tone and reflexes are within normal limits. Intravenous hydration is started. Which of the following is the most appropriate next step in management?
Evaporation cooling of the patient
Empirical antibiotic therapy
Gastric lavage with cold water
Immersion of the patient in cold water
High dose acetaminophen therapy
A 23-year-old male with a history of drug abuse is brought to the emergency department (ED) by an ambulance while having a tonic-clonic seizure. His mother soon arrives at the ED and says that she found him on the floor, where "he must have fallen." She says his seizure has lasted for more than 30 minutes now, and that he never regained consciousness since she found him. In the ED, he is unresponsive and cyanotic. He is biting his tongue and is incontinent. Despite resuscitation and administration of intravenous lorazepam, phenytoin, and glucose, the seizures continue. What is the best next step in the management of this patient?
Obtain CBC and electrolytes as soon as possible
Stat electroencephalogram (EEG)
Anesthesia with midazolam and intubation
Obtain CT scan of the head
Do a drug screen and attempt detoxification
A 27 -year-old white female comes to the office and complains of a headache for the last two weeks. She characterizes the headache as intermittent, "feels like a dull ache", 5/10 in severity, and associated with nausea and vomiting. She is afebrile and never had such a headache before. She has no visual complaints. She is a non-smoker and drinks alcohol only on weekends. Her only drugs are oral contraceptive pills (OCPs). Her menses are regular, and she has never conceived. She has no family history of similar problem. Her pulse is 80/min, temperature is 37.1°C, blood pressure is 120/75mmHg and respirations are 15/min. She is 5 feet 10 inches tall, and her weight is 210 lbs. The neurological examination is non-focal, and there are no signs of meningeal irritation. Funduscopy reveals papilledema. MRI of the brain is normal. Which of the following complications is likely to develop if this patient is left untreated?
Seizures
Blindness
Intracranial bleed
Paralysis
Urinary incontinence
A 64-year-old male is brought to the emergency department (ED) due to a sudden onset of lower extremity weakness. He was swimming in the pool, when he suddenly felt his legs become weak. He then felt that his legs had no more strength, and he was not able to move them. He struggled out of the pool, called EMS, and was rushed to the ED. He denies any trauma, loss of consciousness, visual or speech problems. He cannot pass urine. He has a long history of back problems. The physical examination reveals significant motor weakness in both legs, and numbness from the buttocks to the soles of the feet. He has no sensation in the perineal area. The rectal tone is absent. A Foley catheter is placed, and 800 cc of urine is collected. What is the best treatment for this patient?
CT head without contrast
Complete bed rest for 24 hours
Physiotherapy and NSAIDs
Emergency surgery
Nerve conduction studies
A 78-year-old woman is brought to the emergency department with agitation and insomnia. She screams out loudly and tries to run away while being examined. She is a nursing home resident and has a recent medical history that includes severe memory loss, gait disturbance and urinary incontinence. Her chronic medical issues include hypertension, diabetes mellitus, atrial fibrillation, peptic ulcer disease and chronic pyelonephritis. Her blood pressure is 160/100 mmHg and heart rate is 95/min and irregular. ECG reveals atrial fibrillation but no acute ischemic changes. Laboratory investigations reveal the following: Hematocrit 41%, WBC count 9,000/mm3, Platelets 160,000/mm3, Sodium 137 meq/L, Potassium 5.5 meq/L, Chloride 95 meq/L, Creatinine 1.4 mg/dl, BUN 25 mg/dl. Urinalysis shows trace protein, numerous leukocytes and occasional erythrocytes. Which of the following is the best initial treatment for this patient?
Heparin
Aspirin
Haloperidol
Lorazepam
Amitriptyline
A 79-year-old woman is brought to the emergency department due to a suspected cerebrovascular accident on her right side. She complains of diffuse paresthesias and tingling in her right hand. She did not lose consciousness. The physical examination reveals normal speech, symmetric deep tendon reflexes (2/4 on both upper extremities, 2/4 both patellar reflexes, and 0/4 both Achilles reflexes), a cold right hand, and undetectable arterial radial pulse. Tinel and Phalen's signs are negative. The rest of the examination is normal. What is the most appropriate next step in the management of this patient?
CT scan of the brain without contrast
MRI scan of the brain with diffusion images
Doppler of the carotid arteries
Schedule for EMG, and nerve conduction studies
Immediate vascular surgery consultation for intervention
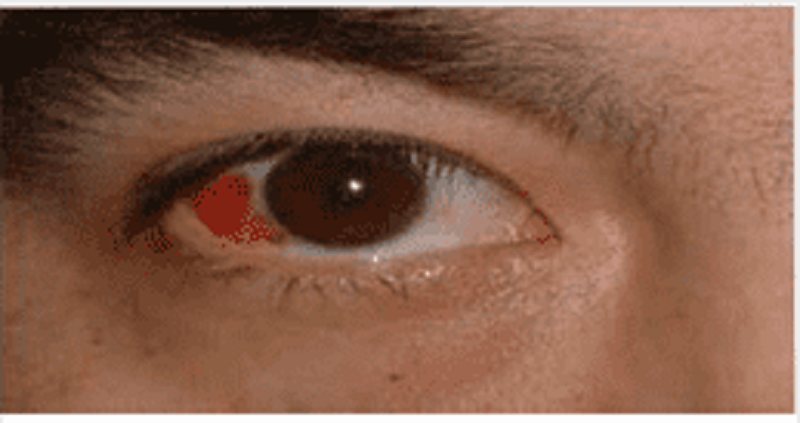
A 34-year-old male presents to the emergency department with a red eye. He says, "I just woke up this morning and saw that my right eye was red." He denies any itching, pain or discharge. He has no known drug or environmental allergies. He takes no medication. His vital signs are stable. The photo of his eye is shown below. What is the best next step in his management?
Check intraocular pressure
Refer to ophthalmologist
Check coagulation parameters
Observation
Antibiotics
A 24-year-old woman presents to the emergency department (ED) complaining of right eye pain and blurry vision since waking up this morning. She states that the pain began after taking out contact lenses that were in her eyes for over 1 week. Her blood pressure (BP) is 120/75 mm Hg, heart rate (HR) is 75 beats per minute, temperature is 99.1°F, and respiratory rate (RR) is 16 breaths per minute. Her right and left eye visual acuity is 20/60 and 20/20, respectively. Her conjunctivae are injected. The slitlamp examination reveals a large area of fluorescein uptake over the visual axis. Which of the following is the most appropriate therapy?
Call the ophthalmology consult for an emergent corneal transplant
Prescribe a systemic analgesic for pain control and advise the patient to not wear her contact lenses for the next week
Prescribe ciprofloxacin eye drops, oral analgesia, update tetanus prophylaxis, and arrange for ophthalmology follow-up
Prescribe oral amoxicillin, a topical anesthetic, such as tetracaine, and have patient follow-up with an ophthalmologist
Prescribe ciprofloxacin eye drops and have patient strictly wear an eye patch until her pain resolves
A 60-year-old woman presents to the ED complaining of pain in her right eye and burning sensation over half of her forehead and scalp. On physical examination, you notice a patch of grouped vesicles on an erythematous base located in a dermatomal distribution on her scalp and forehead. There are also a few vesicles located at the tip of the patient’s nose. Her visual acuity is 20/20 bilaterally, heart is without murmurs, lungs are clear, abdomen is soft, and there are no gross findings on neurologic examination. Which of the following is the most concerning complication of this patient’s clinical presentation?
Central nervous system (CNS) involvement leading to meningitis
Ophthalmic involvement leading to anterior uveitis or corneal scarring
Cardiac involvement leading to endocarditis
Permanent scarring of her face
Nasopalatine involvement leading to epistaxis
A 24-year-old woman presents to the ED at 4 AM with severe left eye pain that woke her up from sleep. She wears soft contact lenses and does not routinely take them out to sleep. She is in severe pain and wearing sunglasses in the examination room. You give her a drop of proparacaine to treat her pain prior to your examination. On examination, her vision is at baseline and she has no afferent pupillary defect. There is some perilimbic conjunctival erythema. On fluorescein examination, a linear area on the left side of the cornea is highlighted when cobalt blue light is applied. No underlying white infiltrate is visualized. No white cells or flare are visualized in the anterior chamber. What is the most appropriate treatment for this condition?
Immediate ophthalmology consult
Tobramycin ophthalmic ointment
Erythromycin ophthalmic ointment
Eye patch
Proparacaine ophthalmic drops
A 45-year-old man lacerated his right forehead after an altercation in a local bar. Instead of seeking medical attention, the patient applied super glue to his wound. He successfully stopped the bleeding, but some of the glue got into his right eye and now he comes to the ED with difficulty opening his right eye. What is the most appropriate treatment of this patient?
Call ophthalmology immediately
Wash eye with acetone
Wash eye with normal saline
Use forceps to remove all the glue from the eye
Apply erythromycin ointment
A 12-year-old girl presents to the ED for left eye pain and swelling for 2 days. The patient has had cough, congestion, and rhinorrhea for the last week that is improving. On examination, her temperature is 100.8°F, HR 115 beats per minute, RR 12 breaths per minute, and BP 110/70 mm Hg. On eye examination, there is purple-red swelling of both upper and lower eyelids with injection of the conjunctiva. Pupils are equal and reactive to light. There is restricted lateral gaze. Visual acuity is 20/70 in the left eye and 20/25 in the right eye. The rest of the physical examination is normal. What is the most appropriate next step in management?
Administer diphenhydramine
Administer amoxicillin/clavulanate
Administer vancomycin IV
Perform computed tomographic (CT) scan of orbits and sinuses
Administer artificial tears
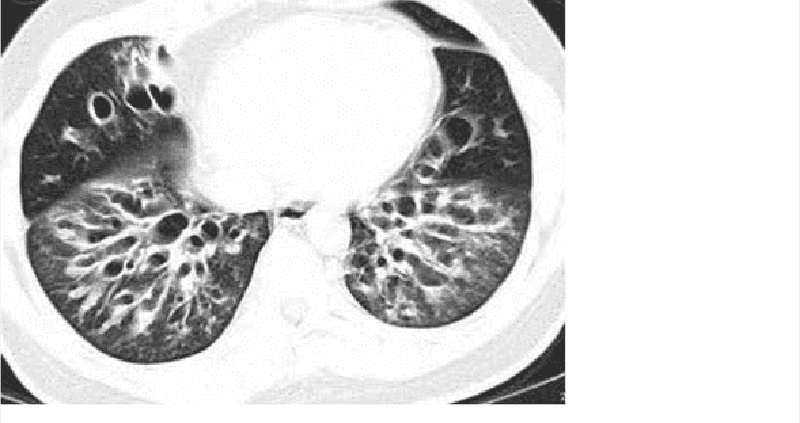
A 48-year-old male presents to the doctor with a history of persistent cough, tenacious mucopurulent sputum, and intermittent chills. He has been treated with several courses of antibiotics without resolution of his symptoms. On examination, he has an emaciated appearance and there is decreased air entry in the right lung base. His sputum has a foul smell. High resolution CT scan of the chest is shown below. Which of the following is the most feared complication of this patient's condition?
Pneumonia
Hemoptysis
Respiratory failure
Pneumothorax
Pulmonary embolism
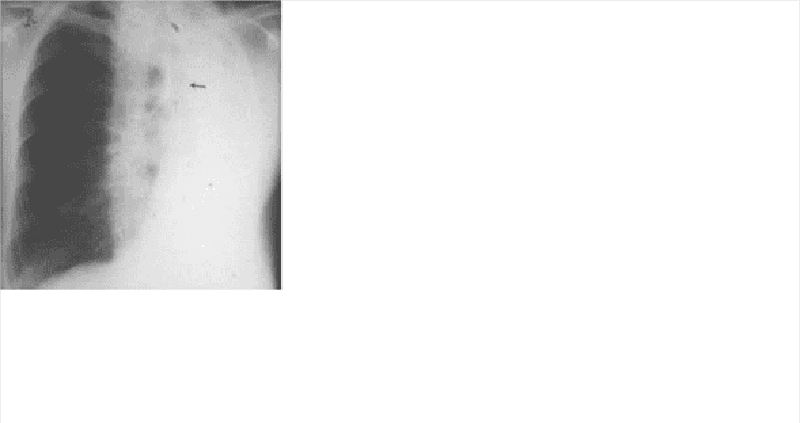
A 67-year-old white male with a long history of bronchial asthma and chronic obstructive pulmonary disease (COPD) presents to the emergency room complaining of acute onset of shortness of breath for the last 30 minutes. He says that for the past 2 or 3 days he has been having some difficulty breathing and a productive cough with thick phlegm, but nothing as bad as the current episode. He also has a history of congestive heart failure after suffering a myocardial infarction for which he is taking furosemide and lisinopril. While talking to you in halting sentences, you note that he appears cyanotic, confused and are sweating profusely. He normally takes albuterol, ipratropium and budesonide inhalers for his breathing difficulties, but they have not relieved his current symptoms. On examination, he is found to be markedly dyspneic and his PaO2 is 55 mm Hg. A chest x-ray done in the ER is shown below. Which of the following is the most appropriate next step in the management of this patient?
Start intravenous theophylline
Urgent thoracocentesis
Urgent bronchoscopy
Place central venous line
Increase furosemide and start digoxin
A 32-year-old man presented to the emergency department five hours ago with an acute asthma exacerbation. He has been receiving continuous albuterol nebulizer treatments since that time. He has a 20-year history of asthma but notes that recently the frequency of his attacks has increased. Presently, his blood pressure is 110/70 mmHg and heart rate is 120 and regular. On physical exam, the patient appears drowsy. Breath sounds are diminished bilaterally but there are no wheezes. The most recent ABG reveals: pH 7.32, pO2 65mmHg, pCO2 50mmHg. Which of the following is the best next step in managing this patient?
Inhaled corticosteroids
Ipratropium inhalation
Intravenous theophylline
Oral prednisone
Endotracheal intubation
A 75-year-old man develops increased ventilatory requirements several days after requiring intubation for respiratory failure. X-ray of the chest shows bilateral infiltrates, and based on his ventilatory settings, the ratio of the partial arterial pressure of oxygen to the fraction of inspired oxygen (PaO2:FiO2) is 190. Which of the following is the most common underlying etiology of acute respiratory distress syndrome?
Aspiration of gastric contents
Drug overdose
Lung or bone marrow transplantation
Massive blood transfusion
Sepsis
A 25-year-old Caucasian woman presents as a new patient after having recently moved to the neighborhood. She says that she was diagnosed with anorexia nervosa two years ago, and that her disorder resolved after intensive psychotherapy. Although her eating pattern is normal now, she is still underweight. Her menstrual cycles have been regular for the past year. She recently married and is now interested in starting a family with her husband. She asks whether her history of anorexia nervosa will affect her ability to conceive or carry a healthy child to term. Given this clinical presentation, which of the following complications is most likely?
Congenital anomalies
Macrosomia
Small for gestational age baby
Infertility
Postpartum psychosis
A 22-year-old woman is seen in the emergency room after a suicide attempt. She swallowed 10 aspirin in the presence of her mother, with whom she had just had an argument. The patient has a long history of cutting herself superficially with razor blades, which her psychiatrist of the last 5 years confirms by telephone. The patient currently lives in a stable environment (a halfway house) where she has been for 3 years. Which of the following option is the best course of action for the physician in the emergency room?
Admit the patient involuntarily
Admit the patient voluntarily
Admit the patient to a medical floor
Discharge the patient to outpatient therapy after meeting with the patient’s mother
Discharge the patient back to outpatient therapy and the halfway house
A 62-year-old Caucasian female complains of frequent headaches, fatigue and recent weight loss. Her shoulder muscles feel stiff in the morning. Her ESR is 85 mm/hr. Which of the following will be the most likely complication of this patient's condition?
Chronic lymphocytic leukemia
Hypothyroidism
Aortic aneurysm
Ulcerative colitis
Membranous glomerulonephritis
A 40-year-old female presents to the emergency room with palpitations and lightheadedness of acute onset. Also, she has experienced insomnia, fatigability, and weight loss lately. She does not smoke or consume alcohol. She is not taking any medication. Her blood pressure is 110/80 mmHg and heat rate is 120/min, irregular. Physical examination reveals lid lag and fine tremor of the outstretched hands. ECG shows atrial fibrillation with rapid ventricular response. What is the next best step in the management of this patient?
Digoxin
Propranolol
Lidocaine
Quinidine
Immediate cardioversion
A 43-year-old Caucasian man with a two-year history of diabetes mellitus presents to your office for a routine. He has no complaint His medications are metformin and aspirin. He works as a computer programmer and has a sedentary lifestyle. He drinks one to two cans of beer on weekends and smokes one pack of cigarettes per day. On physical examination, his blood pressure is 153/94 mmHg and his heat rate is 82/min. His BMI is 32.5 kg/m2. The remainder of the physical examination is unremarkable. Laboratory studies reveal an HbA1c of 7.6%. At his check-up one month ago, his blood pressure was 149/92 mmHg. Which of the following interventions would be most effective for controlling his blood pressure?
Aerobic exercise
Weight loss
Smoking cessation
Better diabetes control
Quitting alcohol
A 60-year-old male is 2 days status post primary percutaneous coronary intervention (PCI) with stent placement. He had previously suffered from an antero-lateral myocardial infarction. His cardiac enzymes have been trending down since admission. He has recovered well and is ready for discharge. He is currently asymptomatic. His temperature is 37.5°C (99.5°F), blood pressure is 130/70 mmHg, pulse is 66/min, and respirations are 14/min He is discharged with instructions to take the following medications aspirin simvastatin, lisinopril metoprolol and sublingual nitroglycerine. In addition to the medications listed above, which of the following medications should this patient also be taking after discharge?
Isosorbide mononitrate
Low molecular weight heparin
Waffarin
Clopidogrel
Amlodipine
A 22-year-old Caucasian male is evaluated for an episode of syncope that occurred while playing soccer. It lasted only 2 minutes without any post-syncopal confusion, sleepiness or weakness. He had prior episodes of dizziness while playing active sports as well as vague chest discomfort. His uncle died suddenly at a young age. Auscultation of his precordium reveals a III/IV systolic murmur along the left sternal border. The patient is most likely to benefit from which of the following medications?
Nitrates
Beta-blockers
Disopyramide
Amlodipine
Digitalis
A 40-year-old male presents with six months of worsening dyspnea. His symptoms have progressed to the point that walking even one block causes him to become shot of breath. He has a history of cigarette smoking, but quit 10 years ago. He drinks approximately one alcoholic drink daily. His medical history is significant for peptic ulcer disease for which he takes antacids. On physical examination, he is afebrile. His pulse is 86/min, blood pressure is 140/56 mmHg, and respiratory rate is 14/min. While examining his heat you note a high-pitched blowing, early diastolic, decrescendo murmur, which is heard best in the left third intercostal space and is intensified by handgrip. There is prominent cardiomegaly on chest x-ray. Which of the following medications would improve both this patient’s symptoms and cardiomegaly?
Quinidine
Metoprolol
Nifedipine
Ephedrine
Amiodarone
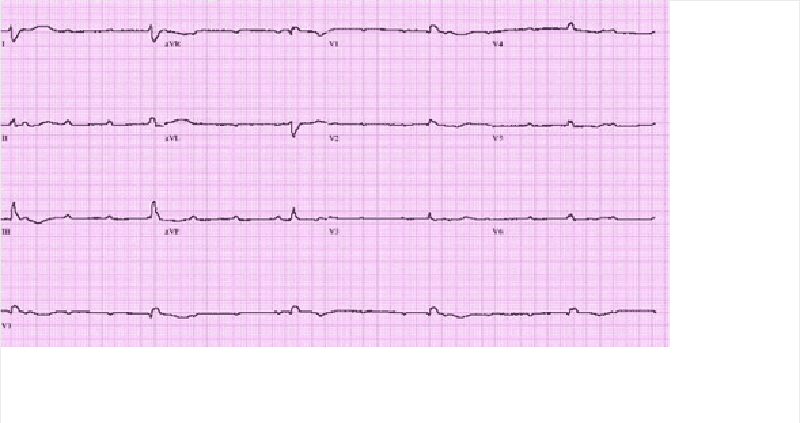
A 67-year-old male presents to the ER with chest pain. His medical history is significant for stable angina for which he takes aspirin and isosorbide dinitrate, as well as hypertension and bronchial asthma. Occasionally, he uses an albuterol inhaler. He is admitted to the hospital and five hours later, he begins to feel lightheaded and weak. His blood pressure is 100/60 mmHg. An EKG is obtained and is shown below. Which of the following is the best next step in managing this patient?
Cardiac catheterization
Pacemaker insertion
Adenosine
Digoxin
Metoprolol
A 43-year-old white male is found to have premature atrial complexes (PACs) on routine EKG. He denies chest pain, shortness of breath or lightheadedness. He has smoked 1-2 packs of cigarettes daily for the past 20 years. He also has a 20-year history of alcoholism, though recently he has limited his use to 1-2 beers/day. The patient's family history is significant for a myocardial infarction in his mother at age 65 and a stroke in his father at age 72. He has no personal history of hypertension or diabetes. Physical examination including vital signs, is entirely within normal limits. What is the best next step in the management of this patient?
Reassurance
24-hour Halter monitoring
Echocardiogram
Start beta-blocker therapy
Advise him to stop alcohol and tobacco
A 60-year-old man is brought to the emergency department due to syncope. He has had similar episodes a few times during the past few weeks. These episodes usually occur after he exerts himself. He does not feel confused or tired after these episodes. He denies any chest pain or palpitation. His wife reports that when he collapses, he seems to lose consciousness for a few seconds, but then is back to being alert right away. She denies any jerking movement. His past medical history is significant diverticulosis, for which he takes fiber supplements. He is not on any other medication. His temperature is 37.1°C (98.8°F), blood pressure is 110/98 mm Hg, pulse is 88/min, and respirations are 14/min. On examination, he has a fourth heart sound and harsh 3/6 systolic murmur, best heard over the right sternal border. The murmur is accentuated on expiration. The lung fields are clear to auscultation. After performing an echocardiograph to confirm the diagnosis, which of the following management options is most appropriate?
Aortic valvotomy
Aortic valve replacement
Close outpatient follow-up with serial echocardiograms
Exercise test looking for arrhythmias
Observe until the patient develops breathlessness
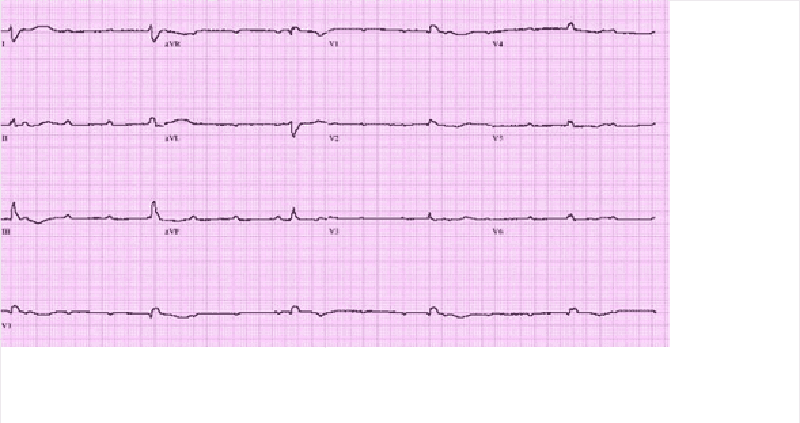
A 59-year-old male suffers a myocardial infarction. He is treated medically and is discharged home ten days later on aspirin, atorvastatin, metoprolol, lisinopril, and sublingual nitroglycerin. One month later, he presents to your office for a follow-up visit. He denies chest pain, dyspnea or lightheadedness. His blood pressure is 120/75 mmHg. His EKG is pictured below. Echocardiogram reveals an ejection fraction of 45%. What is the best next step in his management?
Observation
Amiodarone
Digoxin
DC cardioversion
Verapamil
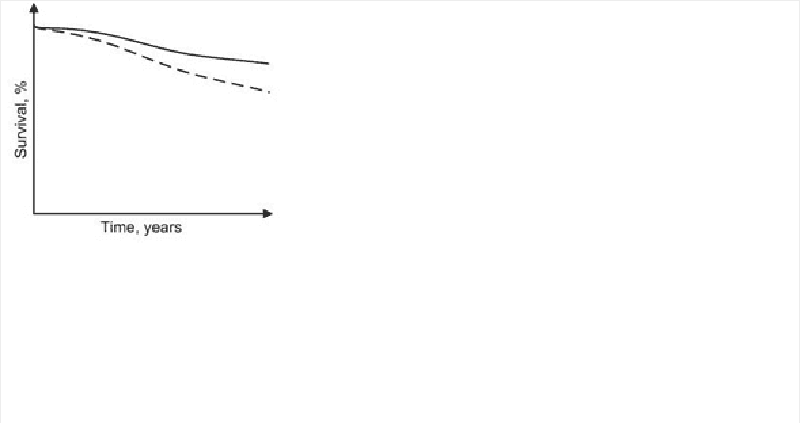
Diuretics, vasodilators and oxygen are standard inpatient therapy for patients hospitalized with left-sided heart failure. When patients are discharged, a different outpatient regimen is instituted. A team of researchers compares long-term cardiovascular mortality between patients treated with two different outpatient regimens. The study results are depicted below. In comparison to the patients depicted by the dashed curve, those depicted by the solid line most likely received treatment with which of the following?
ACE inhibitor
Calcium channel blocker
Loop diuretic
Digoxin
Dobutamine
A 57-year-old female with a past medical history of bronchial asthma presents to the physician's office for evaluation of high blood pressure. On her previous two visits, her blood pressure has been 154/88 mmHg and 150/90 mmHg. Her blood pressure during this visit is 150/90 mmHg. She denies headaches and has no complaints. She uses fluticasone and albuterol inhalers for her chronic persistent asthma. She denies smoking or alcohol intake, and has no known drug allergies. Her family history is significant for myocardial infarction in both her mother and father. Exercise and a low salt diet have not improved her hypertension. Which of the following is the most appropriate next step in managing this patient's hypertension?
Discontinue asthma medications
Prescribe propranolol
Prescribe enalapril
Prescribe hydrochlorothiazide
Obtain an echocardiogram
A 27-year-old female presents to your office for a follow-up. The previous two visits revealed an elevated blood pressure in the range of 150- 155/90-95 mmHg. She has no present complaints. Her past medical history is insignificant. She smokes 1/2 pack of cigarettes per day and does not consume alcohol. Her current medications include a combination oral contraceptive for the last 2 years, and an occasional acetaminophen for tension headache relief. There is no family history of hypertension or heart attacks. This visit, her blood pressure is 155/95 and her heart rate is 80/min. The physical examination is unremarkable. The ECG is normal. Her total cholesterol level, measured 6 months ago, was 170 mg/dL. Which of the following is the most appropriate next step in the management of this patient?
Lifestyle modification
Discontinuation of the oral contraceptive
Low-dose thiazide diuretic
Intravenous pyelography
No intervention at this point
A 65-year-old male presents to the emergency department with substernal chest pain, severe shortness of breath, and diaphoresis that began suddenly 40 minutes ago. Since the pain started, the patient has vomited twice. The pain radiates to his left arm and does not remit with sublingual nitroglycerine. EKG shows 2 mm ST elevations in the anterior leads. On physical examination, the patient's temperature is 36.9°C (98.4°F), blood pressure is 110/70 mmHg, pulse is 60/min, respirations are 32/min, and oxygen saturation is 90% on 4L oxygen by nasal canula. Cardiac exam reveals a muffled S1 and S2 and the presence of an S3. Lung exam reveals basilar crackles that extend halfway up the lung fields bilaterally. Which of the following is the best next step in managing this patient?
Metoprolol
Digoxin
Furosemide
Spironolactone
IV fluids
A 55-year-old male with a history of rheumatoid arthritis and rheumatoid lung disease is admitted to the hospital with palpitations. His restrictive lung disease is of moderate severity, requiring use of 2 liters of oxygen by nasal cannula at all times. He has no known history of coronary artery disease, hypertension or diabetes. On physical examination, his blood pressure is 110/70 mmHg and heart rate is 120 and irregular. EKG shows atrial fibrillation with a rapid ventricular rate. Which of the following medications should be avoided in this patient?
Verapamil
Digoxin
Quinidine
Amiodarone
Metoprolol
A 32-year-old anxious-appearing male is wheeled into the emergency room with the sudden onset of excruciating left-sided chest pain. His temperature is 37.2°C (99°F), blood pressure is 160/88 mmHg, pulse is 125/min, regular and respirations are 20/min. Physical examination is normal, except for multiple venous track marks on his extremities and atrophic nasal mucosa. An EKG is done which shows ST depression and T wave inversion in leads V1-V6. Cardiac enzymes including CK-MB and Troponin Tare not elevated. Which of the following is the most appropriate next step in the management of this patient?
Cardiac catheterization
Administer metoprolol
Administer thrombolytics
Close observation
Intravenous diazepam
{"name":"USLME medecine interne", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A family brings their 82-year-old grandmother to the emergency room stating that they cannot care for her anymore. They tell you, “She has just been getting sicker and sicker.” Now she stays in bed and won’t eat because of stomach pain. She has diarrhea most of the time and can barely make it to the bathroom because of her weakness. Her symptoms have been worsening over the past year, but she has refused to see a doctor. The patient denies symptoms of depression. Blood pressure is 90\/54 mmHg with the patient supine; it drops to 76\/40 mmHg when she stands. Heart and lungs are normal. Skin examination reveals a bronze coloring to the elbows and palmar creases. What laboratory abnormality would you expect to find in this patient?, A 58-year-old woman presents to her physician because of neck discomfort and difficulty swallowing. She first began to have difficulty with swallowing solids 2 years ago, but the problem is getting progressively worse. She denies hemoptysis, hematemesis, abdominal pain, or change in bowel habits. She is a nonsmoker and past medical history is significant only for mild hypertension. Her temperature is 36.9°C (98.4°F), heart rate is 72\/min, and blood pressure is 132\/78 mmHg. She has an asymmetrically enlarged thyroid gland that is particularly firm on the right, with poorly palpable borders. Laboratory evaluation reveals a free thyroxine level of 4.1 ng\/dL and thyroid-stimulating hormone of 5μU\/mL. Based on the results of a radioisotope scan and a fine needle aspiration biopsy, the physician decides to perform surgery. For which of the following is the patient at increased risk postoperatively?, A 53-year-old woman presents to the clinic with complaints of headache and blurred vision for the past several months. She also says her family has commented that her face looks different, and her nose is bigger than it used to be. In addition, she says her shoes feel tighter. On physical examination she has coarse facial features with a prominent mandible and widely spaced incisors. MRI of the brain reveals a mass in the pituitary. This patient may be at increased risk of developing which of the following malignancies?","img":"https://cdn.poll-maker.com/11-518025/2.png?sz=1200-00000000001000005300"}
More Quizzes
L’USUFRUIT ET LA NUE-PROPRIÉTÉ
420
Circulatory System
6320
How Sustainable Are You?
1050
Zemnoalkalni metali
9432
Male or Female Brain Test - Find Out Your Brain Type
201017618
Direct Materials Requisition - Job Order Costing
201017966
Conditional Sentence - Test Your If-Clauses
201016678
Which Medical Specialty Should I Choose? Free
201017551
Watsons Go to Birmingham Chapter 1 Questions - Free
201017162
Lab Equipment Test - Identify Common Chemistry Apparatus
201015970
Miley Cyrus Real Name - Can You Guess It?
201016621
Punishment for Parents - Find the Right Discipline
201017037