USMLE PART3.2(PNEUMO)
A 67-year-old male presents with a one-month history of dyspnea on exertion and chest pain. He denies hemoptysis, cough, fever, night sweats or weight loss. His past medical history is significant for hypertension and chronic obstructive pulmonary disease. He has a 48 pack-year smoking history but quit six years ago. He works as a salesman. On physical examination, the patient has a temperature of 38.2C (100.8.F), blood pressure of 128/72 mm Hg, pulse of 92/minute, and respirations of 20 breaths/minute. His complete blood count, chemistry panel, and hepatic function tests are all within normal limits. A chest x-ray and computed tomography scan of the chest reveal a right-sided pleural effusion and calcified nodules in both upper lobes. The patient undergoes thoracentesis. Characteristics of the pleural fluid are given below: Total protein 5.2 g/dl Glucose 83 mg/dl Adenosine deaminase 98.5 U/L Cytologic examination reveals 600 white blood cells/mm3, 1% macrophages and 99% leukocytes. Of the leukocytes, 45% are neutrophils, 50% are lymphocytes, and 5% are monocytes, with no basophils or eosinophils. No neoplastic cells are found. Which of the following is the most likely mechanism underlying development of this pleural effusion?
Elevation of hydrostatic pressure
Decreased plasma osmotic pressure
Increased capillary permeability
Passage of fluid through openings in the diaphragm
Reduction of pleural space pressures
Other
Please Specify:
A 33-year-old white female complains of repeated episodes of fever, malaise, chills, breathlessness and dry cough over the past 6 months. She says that each episode starts suddenly and lasts for several days. She otherwise has no significant past medical history and does not take any medications. There is no family history of lung disorders. She does not smoke cigarettes or drink alcohol. She has never been abroad, and has had no sick contacts. She breeds budgerigars (a small Australian parrot) as a hobby. Chest x-ray shows diffuse generalized haziness in both lower lung fields. Pulmonary function tests reveal reduced lung volumes and an FEV1/FVC ratio of 87%. PPD test is negative. Serology shows antibodies to budgerigar antigens. What is the best treatment for this disease?
Inhaled beclomethasone
Oral prednisolone
Inhaled cromolyn
Avoid exposure to birds
Reassurance

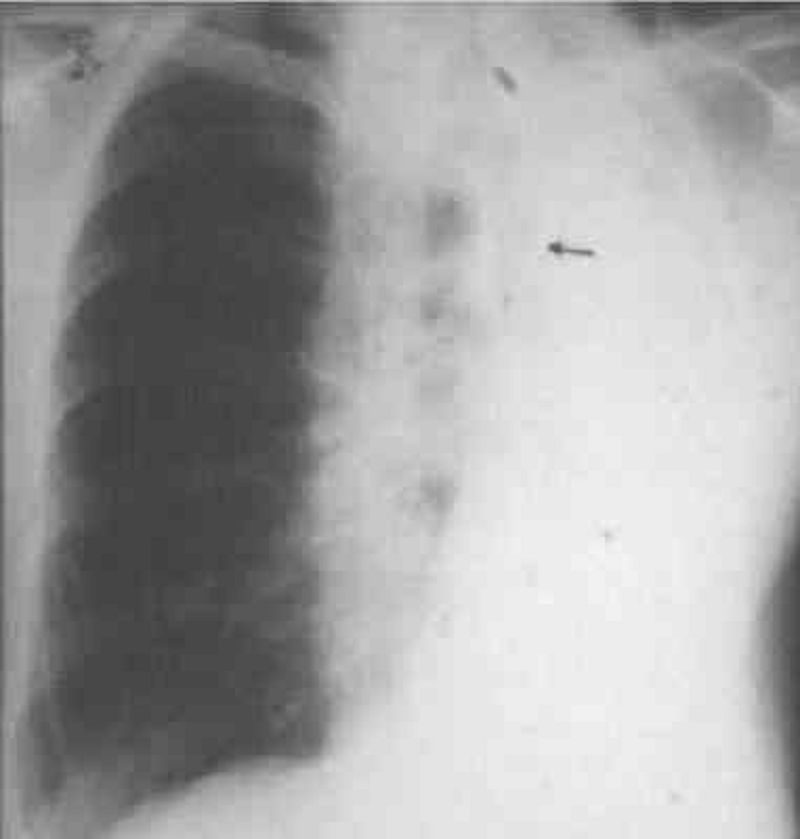
A 43-year-old man presents to your office complaint of nagging left-side chest pain that increases on deep inspiration, plus two weeks of non-productive cough. He denies chills, fever or weight loss. His medical history is significant for Hodgkin's disease treated 20 years ago with chemotherapy and radiation therapy. On physical examination today, his blood pressure is 140/90 mmHg and his heart rate is 90/min. His chest x-ray is shown below. Which of the following is the most likely cause of his chest pain?
Radiation-induced fibrosis
Recurrence of Hodgkin's disease
Fungal pneumonia
Pulmonary tuberculosis
Secondary malignancy
A 44-year-old male is involved in a serious motor vehicle accident. He is admitted to the intensive care unit with multiple fractures and internal bleeding, and is placed on mechanical ventilation. Over the next two days, his oxygen saturation repeatedly drops below 90%, requiring gradual increases in the FiO2. On day three of his admission, the patient's chest x-ray, which was initially clear, shows bilateral fluffy infiltrates. He has no prior medical problems and does not take any medications. Skin examination reveals no rashes. Lab studies show: Hemoglobin 10.1 g/L Platelets 160,000/mm3 Leukocyte count 13,500/mm3 Sputum cultures are negative. The ventilator settings are: Fi02 90% Tidal volume 400 ml (body weight 60 kg) Respiratory rate 12/min PEEP 5cmH2O The patient's oxygenation continues to drop below 90%. Which of the following interventions would be best for improving the patient's oxygenation?
Increase the respiratory rate
Increase the tidal volume
Increase the PEEP
Increase the intravenous fluids
Administer packed red blood cells
A 65-year-old white man comes to the Emergency Room complaining of headache, insomnia, palpitations, and vomiting. His past medical history is significant for chronic obstructive pulmonary disease (COPD) treated with theophylline, ipratropium, and occasional albuterol. He had a puncture wound of the foot one week ago, and it is being treated effectively with amoxicillin-clavulanate and ciprofloxacin. For the past three days, his shortness of breath is worsening, and his primary care physician gave oral prednisone. His blood pressure is 150/80 mmHg and heart rate is 105/min with frequent ectopic beats. You suspect that drug toxicity may be responsible for this patient's complaints. Which of the following drugs is most likely responsible for his condition?
Theophylline
Lpratropium
Albuterol
Ciprofloxacin
Steroids
A 67-year-old woman with a past medical history significant for hypertension, hypercholesterolemia, and type 2 diabetes calls 911 for severe shortness of breath. Her symptoms started 2 hours ago with chest pain and progressed rapidly to orthopnea and shortness of breath. Her blood pressure is 170/100 mmHg and heart rate is 120/min and regular. A third heart sound is present. Bilateral crackles are heard on chest auscultation. Her oxygen saturation is 78% with 40% inspired oxygen. She is intubated in the field by paramedics for progressive respiratory failure and is treated with nitrates and diuretics. After the initial resuscitation, breath sounds on the left side are markedly decreased. Which of the following is most likely to restore breath sounds to this hemithorax?
Left-sided chest tube
Left-sided needle thoracostomy
Pericardiocentesis
Endotracheal tube withdrawal
Tidal volume increase
A 65-year-old man presents to your office complaining of progressive breathing difficulty. His past medical history is significant for hypertension, diabetes mellitus, type 2, and myocardial infarction experienced two years ago. His current medications are hydrochlorothiazide, atenolol, glipizide, and aspirin. He does not smoke or consume alcohol. His vital signs are BP 156/96 mmHg, PR 65/min, RR 18/min, T 36.7C (98F). Physical examination shows mild symmetric edema of the lower extremities. Hepatojugular reflex is positive. Point of maximal impulse is displaced downward and to the left. Soft blowing systolic murmur is heard on the apex. Breath sounds are diminished on the right side. Serum protein level is 6.5 g/dl and serum LDH is 200 mg/ml. After taking a chest radiograph, you suspect pleural effusion on the right and decide to perform diagnostic thoracocentesis. Which of the following findings, on pleural fluid analysis, is most consistent with this patient's condition?
LDH level of 180 mg/ml
Protein level of 5.0 g/dl
Glucose 60 mg/dl
PH of 7.35
High amylase level
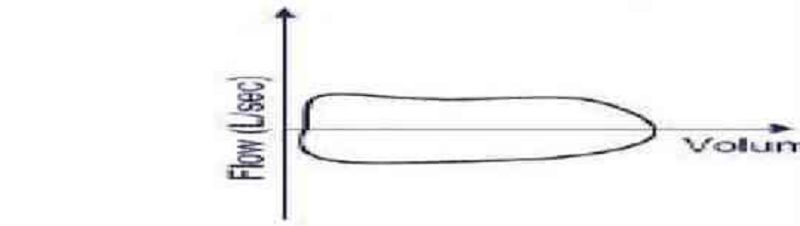
A 56-year-old woman is brought to the hospital from a local restaurant after suddenly becoming short of breath. Her flow-volume loop is shown below. Which of the following is the most likely cause of her symptoms?
Asthma attack
Pneumothorax
Pulmonary edema
Laryngeal edema
Panic attack
A 54-year-old black male from the southeast USA presents to you with complaints of generalized malaise, fever, and a cough. He claims that he has had intermittent hemoptysis for the past six months. He denies smoking and has never had tuberculosis. Examination is unremarkable and his chest x-ray is shown below. On changing position, you notice that the part of the lesion seen on x-ray also moves. The most likely diagnosis is?
Lung abscess
Pulmonary embolism
Aspergilloma
Histoplasmosi
Bronchiectasis
A 66-year-old male presents to the emergency department with acute onset of severe chest pain and dyspnea. He localizes the pain to the right upper chest, and says that it is aggravated by deep breathing and coughing. On physical examination, his pulse is 116/min and regular, blood pressure is 110/70 mmHg, and respirations are 22/min. His lungs are clear to auscultation. Chest x-ray is unremarkable. EKG shows sinus tachycardia. CT angiogram of the chest shows a thrombus in the right pulmonary artery. Which of the following is the most likely source of his pulmonary thrombus?
Clot in the right heart
Upper extremity deep vein clot
Renal vein clot
Calf vein clot
Iliofemoral vein clot
A 55-year-old chronic smoker comes to you because of worsening shortness of breath. He says that he has had lung problems due to smoking for the past five years. He has hypertension controlled with hydrochlorothiazide, and type 2 diabetes mellitus, controlled with diet. He has smoked two packs of cigarettes daily for 25 years. Physical examination shows bilateral decrease in breath sounds with prolonged expiration and wheezing in both the lung fields. He is hypoxic on room air. An x-ray film of the chest shows hyperinflation of both lung fields. His pulmonary function tests showed moderate obstructive disease, with very little bronchodilator response. The patient is started on bronchodilators. He is being considered for home oxygen therapy. Which of the following is a criterion for initiating home oxygen in such patients?
Worsening of shortness of breath
Patients with SaO2 less than 88% on room air
Patients with PaO2 1ess than 65 mmHg on room air
Patients with SaO2 less than 92% on room air
Development of pulmonary osteoarthropathy
A 35-year-old male presents to the emergency room complaining of increasing shortness of breath, fever and malaise for several days. His past medical history is significant for two years of recurrent sinusitis. He is a former smoker and has an occasional glass of wine. His temperature today is 38.4°C (101.1F), blood pressure is 110/65 mm Hg, pulse is 110/min, and respirations are 22/min. Examination reveals an illappearing male in mild respiratory distress. Patchy rales are appreciated on lung auscultation. Chest x-ray reveals multiple nodular densities bilaterally. His serum creatinine is 2.7 mg/dl and urinalysis shows red blood cell casts. Which of the following would be most helpful in diagnosing his condition?
Serum alpha fetoprotein
CT scan of the chest
Serum antineutrophilic cytoplasmic antibody
Sputum acid fast stain
Erythrocyte sedimentation rate
A 64-year-old male presents to the ER with a one-week history of progressive exertional dyspnea. Each of the past two nights he has awakened with a choking sensation and has had to sit up to catch his breath. His past medical history is significant for hypertension and a myocardial infarction two years ago. He takes a baby aspirin and lisinopril daily. His blood pressure is 140/90 mmHg, and his heart rate is 110/min, irregularly irregular. His temperature is 98F (36.7C) and his respiratory rate is 24/min. His oxygen saturation is 91% on room air. There is moderate jugular venous distention. Markedly reduced breath sounds are heard over the right lung base. Which of the following most likely underlies this patient's physical findings?
Lung tissue consolidation
Atelectasis
Bronchoconstriction
Pleural effusion
Emphysema

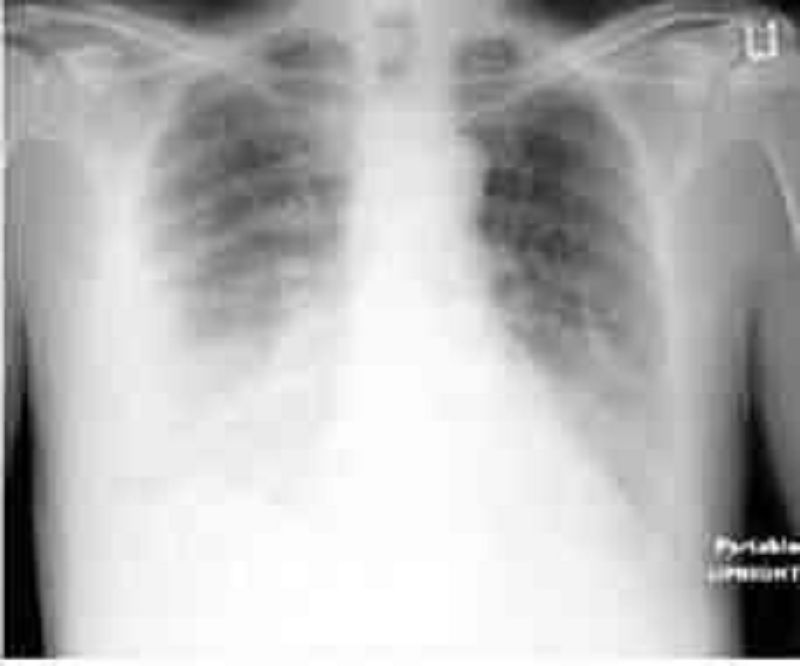
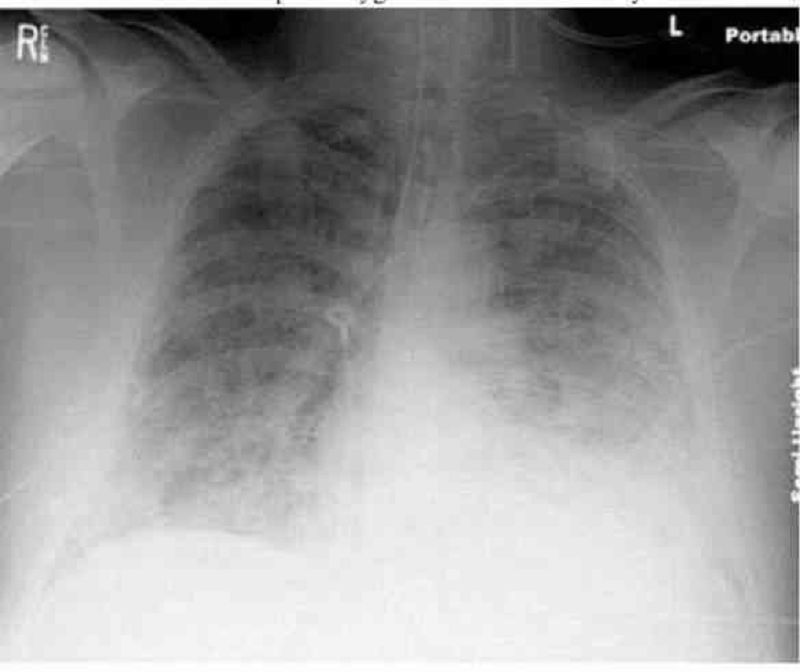
A 65-year-old white male who has a history of chronic obstructive pulmonary disease, congestive heart failure, and coronary artery disease presented with a three-day history of worsening shortness of breath, cough with yellowish expectoration, and fever. He is not on steroids and does not use oxygen at home. He takes ipratropium, albuterol, aspirin, digoxin, furosemide, metoprolol, and lisinopril. He lives at home with his wife. His temperature is 39.4C (103F), blood pressure is 110/70 mmHg, pulse is 110/min, and respirations are 24/min. He is saturating 88% on room air. He was started on 3-liters of oxygen to keep the saturations above 92%. The chest x-ray of the patient is shown below. What is the most appropriate next step in the management of this patient?
Admit the patient and give ampicillin
Outpatient trimethoprim-sulfamethoxazole
Admit the patient and start levofloxacin
Admit the patient and start ciprofloxacin
Admit the patient and start vancomycin
A 62-year-old male is brought to the ER after passing out at work. He reports having had difficulty walking over the past couple of days due to an infected wound on his right foot. His past medical history is significant for diabetes mellitus. On physical examination, his blood pressure is 80/40 mm Hg and his heart rate is 120/min, regular. His skin is cold and clammy. Right heart catheterization is performed, and the following readings are obtained: Right atrial pressure 18 mmHg Pulmonary artery pressure 40/20 mmHg Pulmonary capillary wedge pressure 9 mmHg Which of the following is the most likely diagnosis?
Aortic dissection
Myocardial infarction
Pulmonary embolism
Hypovolemic shock
Septic shock
You are asked to evaluate four different patients, all who have presented with cough and progressive dyspnea. Each has a chest x-ray showing diffuse pulmonary infiltrates. In which of the following patients would bronchoscopy with bronchoalveolar lavage be most likely to yield a diagnosis?
35-year-old female with suspected sarcoidosis
37-year-old female with positive rheumatoid factor
35-year-old HIV patient with CD4 count of 150
56-year -old female with suspected interstitial pulmonary fibrosis
50-year-old female with cardiopathy congestive
A 68-year-old female is admitted with a broken hip after a fall. She undergoes a left hip replacement, which was uneventful. After spending two days in bed, she undergoes partial non-weight bearing physiotherapy. Five days later, she has developed shortness of breath and a swollen leg. A deep vein thrombosis is discovered. An arterial blood gas evaluation is done for suspected pulmonary embolism. What is the most consistent finding of pulmonary embolism?
Elevated PaCO2
Decreased A-a gradient
Right axis deviation on ECG
Decreased PO2
Pulmonary infarction
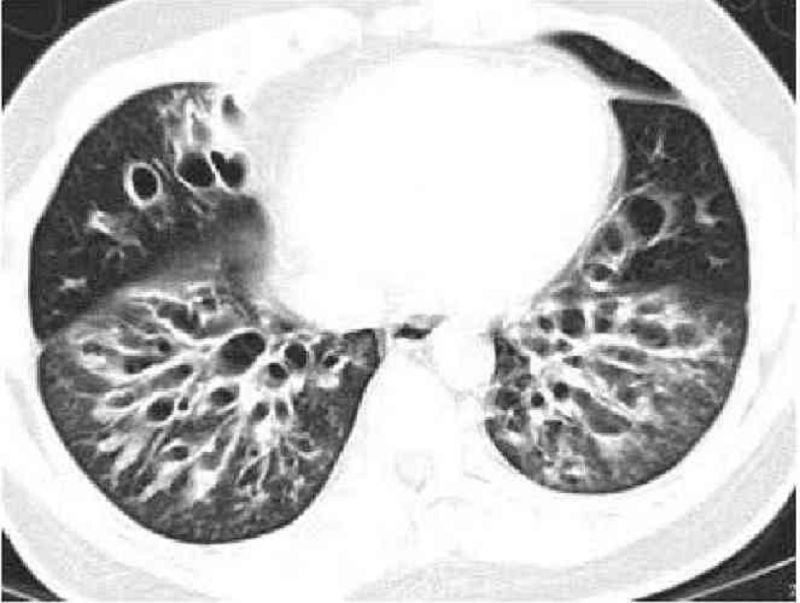
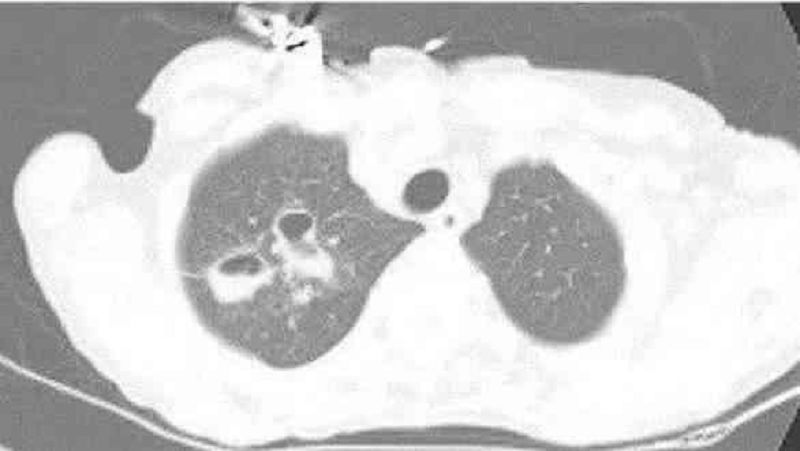
A 48-year-old male presents to the doctor with a history of persistent cough, tenacious mucopurulent sputum, and intermittent chills. He has been treated with several courses of antibiotics without resolution of his symptoms. On examination, he has an emaciated appearance and there is decreased air entry in the right lung base. His sputum has a foul smell. High resolution CT scan of the chest is shown below:Which of the following is the most feared complication of this patient's condition?
Hemoptysis
Pneumonia
Respiratory failure
Pneumothorax
Pulmonary embolism

A 64-year-old African American male presents to you with complaints of a dry cough, weight loss and pain in his right arm. The symptoms started approximately 2 months ago. His past medical history is significant for type 2 diabetes mellitus and hypertension. He smokes 1 pack per day and drinks alcohol occasionally. He denies any drug allergies. Physical examination is unremarkable. ECG reveals normal sinus rhythm. An MRI of his chest is shown below.Which of the following is most likely responsible for this patient's symptoms?
Aspergilloma
Bronchial carcinoid
Superior sulcus tumor
Cryptogenic organizing pneumonia
Lung abscess
A 45-year-old man presents with two days of bilateral hand pain that is most severe in his wrists. Physical examination reveals bilateral wrist tenderness, thickening of the distal fingers, and convex nail beds. There is nicotine staining of the right index and middle fingers. He states that he has been smoking 2 packs of cigarettes a day for the past 25 years. Chest examination reveals decreased breath sounds and a prolonged expiratory phase. The patient relates the pain's onset to a data entry job he recently started. He notes that his boss believes he is fabricating his pain to get off work. His job records reveal numerous sick leaves. Which of the following is the most appropriate course of action?
Reassure the patient and prescribe analgesics
Obtain chest x-ray
Obtain rheumatoid factor levels
Recommend psychiatry evaluation
Order serum calcium and uric acid levels
A 45-year-old man presents to the emergency department with a two-day history of fever, chills and productive cough. He reports having had two episodes of pneumonia over the past six months, both of which resolved completely with levofloxacin therapy. He smoked cigarettes for twenty years, but quit recently with the second bout of pneumonia. Today, his temperature is 38.9°C (102.F), pulse is 98/minute, blood pressure is 110/80 mm Hg, and respirations are 18/min. On physical examination, there are crackles and bronchial breath sounds over the right lower lobe of the lung. Chest x-ray shows right lower lobe consolidation; previous x-rays also show consolidation in this area. What is the most appropriate next step in the management of this patient?
Administer vancomycin
Administer ciprofloxacin
Schedule bronchoscopy
Obtain CT scan of the chest
Obtain pulmonary function tests
A 76-year-old male nursing home resident is hospitalized with confusion, fever and decreased oral intake. His past medical history is significant for type 2 diabetes mellitus, hypertension, osteoarthritis and gout. Blood cultures are positive for E coli. Despite antibiotic therapy, he slips into respiratory failure. He is intubated and placed on mechanical ventilation with an FiO2 of 70%, tidal volume of 500 ml and respiratory rate of 14/min. His current arterial blood gases are: pH 7.45 pO2 59 mmHg pCO2 30 mmHg HCO3 21 mEq/L Which of the following is the best next step in managing this patient?
Increase tidal volume
Increase respiratory rate
Increase the fraction of inspired oxygen
Add positive end-expiratory pressure
Decrease the fraction of inspired oxygen

A 61-year-old man is being evaluated for progressive exertional dyspnea and decreased exercise tolerance. He has also noticed some ankle swelling. The patient has a 40 pack-year smoking history but denies illicit drug use or occupational exposures. His chest x-ray is shown below. The abnormal diaphragmatic contour seen here most likely results in which of the following?
Higher inspiratory flow
Reduced expiratory effort
Increased work of breathing
Increased thoracic wall recoil
Decreased lung compliance
A 65-year-old man complains of two years of persistent cough. He says that he coughs up whitish sputum almost every morning on waking, and then continues coughing throughout the day. He also complains of exertional shortness of breath that becomes disabling if he gets an upper respiratory infection. He has smoked one pack of cigarettes daily for the past 40 years. Pulmonary function testing reveals a vital capacity that is 65% of his predicted. Which of the following best explains this finding?
Alveolar-capillary membrane thickening
Decreased functional residual capacity
Air trapping during expiration
Decreased lung distensibility
Respiratory muscle fatigue
A 65-year-old male comes to the emergency department with severe shortness of breath. The symptoms started one week ago with fever and a non-productive cough. His past medical history is significant for coronary artery disease with bypass surgery two years ago, hypertension and diabetes mellitus. His temperature is 38.9C (102 F), blood pressure is 160/70 mm Hg, pulse is 110/min, and respirations are 26/min. Physical examination reveals decreased breath sounds over the right lower lung base. His chest X-ray is shown on the slide below: Which of the following is the most likely cause of this patient's current complaints?
Bronchopleural fistula
Lung abscess
Empyema
Pneumothorax
Pulmonary infarction
A 45-year-old female with a past medical history of rheumatoid arthritis presents to the emergency department with right calf pain and swelling of sudden onset. She denies fever, chills, dyspnea, chest pain, or history of trauma to the leg. She has smoked a half pack of cigarettes daily for 20 years. Her only medicine is methotrexate for her rheumatoid arthritis. On physical examination, her temperature is 37.0°C (98.6.F), pulse is 70/min, blood pressure is 140/80 mmHg, and respirations are 14/min. Her BMI is 30 kg/m2. Examination of the right calf reveals mild redness, warmth and tenderness. Which of the following is the most appropriate next step in the management of this patient?
Initiate warfarin therapy
Initiate heparin therapy
Perform compression ultrasonography
Perform contrast venography
Obtain blood cultures and start antibiotics
A 54-year-old man is being evaluated for shortness of breath. Examination shows dullness to percussion and increased breath sounds, particularly during expiration, in the right lower lobe. Cardiac examination reveals regular rate and rhythm with normal S1 and S2. There is no murmur. Moderate peripheral edema is present. Which of the following is the most likely cause of his shortness of breath?
Pleural effusion
Pneumothorax
Emphysema
Interstitial lung disease
Consolidation of the lung
A 15-year-old male comes to your office with a one-week history of fever, non-productive cough, sore throat and headaches. Today he noticed a skin rash. His temperature is 38.5°C (101.3.F), pulse is 90/min, blood pressure is 115/78 mm Hg and respirations are 16/min. His throat is hyperemic, but there is no cervical lymphadenopathy. Chest auscultation and percussion reveal no abnormalities. You note dusky red, target shaped skin lesions over all four extremities. Chest x-ray reveals interstitial infiltrates in the left lower lobe. Sputum gram stain reveals polymorphonuclear cells but no organisms. Which of the following organisms is most likely responsible for this presentation?
Streptococcus pneumoniae
Hemophilus influenzae
Legionel/a pneumophila
Influenza virus
Mycoplasma pneumonia
A 53-year-old man presents with two episodes of hemoptysis over the last week. He describes a preceding two-year history of morning cough productive of approximately one tablespoon of yellowish sputum. During the last week his morning cough was accompanied by a small amount of blood on two occasions. He denies any dyspnea, fever, chest pain, or weight loss. He has been smoking for 30 years but has tried to cut down recently. He works in construction. His only medication is ranitidine for occasional heartburn. Which of the following is the most likely cause of his hemoptysis?
Thrombocytopenia
Pulmonary thromboembolism
Bronchiectasis
Chronic bronchitis
Tuberculosis
A 60-year-old Caucasian man comes to the physician because of a productive cough and dyspnea on exertion. He denies hemoptysis, chest pain, and leg swelling. He has smoked one-and-a-half packs of cigarettes daily for 40 years and drinks 2-ounces of alcohol daily. He has worked in a shipyard for 10 years. His temperature is 37.2 C (99 F), blood pressure is 140/80 mmHg, pulse is 80/min, and respirations are 20/min. His chest x-ray shows prominent bronchovascular markings and mild diaphragmatic flattening. His pulmonary function testing shows decreased FEV1/FVC ratio and normal DLCO. Which of the following is the most likely diagnosis?
Emphysema
Chronic bronchitis
Sarcoidosis
Silicosis
Asbestosis
A 47-year-old smoker presents to the emergency room with a three-day history of shortness of breath and cough. His past medical history is significant for tuberculosis ten years ago, treated with six months of a multidrug regimen. On exam today, his blood pressure is 140/90 mmHg and his heart rate is 110/min. Breath sounds are decreased over the right lung base. Over the same area there is dullness to percussion and increased fremitus. The patient also has trace ankle edema. Which of the following most likely accounts for these findings?
Pneumothorax
Pleural effusion
Emphysema
Consolidation
Asthma
A 51-year-old man develops acute respiratory distress syndrome (ARDS) while hospitalized for acute pancreatitis. On his third day in the intensive care unit, he is sedated, intubated, and ventilated with a PEEP (positive end-expiratory pressure) of 15 cm water and Fi0 2 of 0.6 (60%). Suddenly his pulse increases from 100 to 140/min, systolic blood pressure drops from 120 to 90 mm Hg, and central venous pressure increases from 10 to 15 cm water. On chest auscultation, breath sounds are absent on the left side. Which of the following is the most likely explanation for this sudden deterioration?
Endotracheal tube shift into the right main bronchus
Pulmonary thromboembolism
Myocardial infarction
Tension pneumothorax
Mucous plugging and atelectasis
A 53-year-old white male comes to your office with long history of cough, periodic shortness of breath, and wheezing. His family history is significant for asthma in his mother and hypertension and diabetes in his father. He is not taking any medications. He smokes two packs a day ever since he was 16 years of age and consumes alcohol occasionally. Physical examination reveals bilateral scattered expiratory wheezes. Which of the following tests can help you most in differentiating asthma from emphysema in this patient?
Chest x-ray
Bronchoscopy with bronchial washings
FEV1 measurement with and without a bronchodilator
Serum lgE measurement
Sputum analysis
A 71-year-old man is brought to the ER after a witnessed tonic-clonic seizure. He is somnolent and intermittently combative on exam. No past medical history is available. His arterial blood gas (ABG) at room air is given below. pH 7.23 pCO2 69 mmHg pO2 57 mmHg HCO3 28 mmHg Which of the following best explains the acid-base disturbances in this patient?
Lactic acid accumulation
Hypoventilation
Pulmonary embolism
Renal failure
Protracted vomiting
A 60-year-old white male presents to the Emergency Room with sudden onset of dyspnea. He is a truck driver and just returned from a long trip. His past medical history is insignificant. He is not taking any medications. His blood pressure is 110/70 mmHg and heart rate is 110/min. Physical examination reveals a moderately overweight man with tachypnea. Lungs are clear on auscultation. ECG shows right axis deviation. You order ventilation/perfusion scanning. Which of the following findings will help you the most to confirm the diagnosis?
An area of perfusion defect without ventilation
An area of ventilation defect without perfusion defect
An area of perfusion defect without ventilation defect
Several small perfusion and ventilation defects
Absence of ventilation and perfusion abnormalities
A 65-year-old female undergoes total right hip replacement after fracturing the neck of her femur. There are no surgical complications, and afterwards she is started on enoxaparin (low molecular weight heparin) for deep venous thrombosis prophylaxis. On the third postoperative day, she suddenly becomes anxious and complains of right sided chest pain and shortness of breath. She has a history of hypertension, diabetes and hyperlipidemia. She has a 20 pack-year smoking history, but quit 10 years ago. On exam, her temperature is 37.2°C (98.9. F), blood pressure is 126/76 mm Hg, pulse is 110/min and respirations are 30/min. Her oxygen saturation is 88% on room air. She is diaphoretic but her chest is clear to auscultation. A portable chest x-ray shows no abnormalities. EKG reveals sinus tachycardia and non-specific ST/T-wave changes. Which of the following studies would most likely reveal the diagnosis?
Serial cardiac enzymes
Helical CT pulmonary angiography
Echocardiogram
Arterial blood gas analysis
8-type natriuretic peptide levels
A 29-year-old woman presents with chest pain and exertional dyspnea of 10days duration. Her medical history is significant for a normal spontaneous vaginal delivery three months ago, after which she has had frequent episodes of dark bloody vaginal discharge. The most recent bleeding episode was 6 days ago. The patient denies fever, chills, hemoptysis, orthopnea, or leg pain. She does not smoke cigarettes, drink alcohol, or use illicit drugs. Her temperature is 37.7C (98.9.F), pulse is 80/min, blood pressure is 110/68 mmHg and respirations are 16/min. Examination shows clear lungs. Pelvic examination shows an enlarged uterus. Complete blood count and serum electrolytes are within normal limits. Chest radiographs reveal multiple bilateral infiltrates of various shapes. Which of the following investigations will be most helpful in establishing the diagnosis?
Ventilation perfusion scan
Chocardiogram
Quantitative beta HCG
Pulmonary function tests
CT scan of the chest
A 45-year-old male with mild persistent asthma comes to you for a routine checkup. He is taking a low-dose beclomethasone inhaler daily and inhaled albuterol, as needed, for the last year. His past medical history is otherwise not significant. His family history is significant for diabetes mellitus type 2, hypertension and obesity. His blood pressure is 136/90 mmHg and his heart rate is 80/min. His BMI is 26 kg/m2. Which of the following is the most likely complication of chronic beclomethasone use in this patient?
Cushing's syndrome
Thrush
Osteoporosis
Adrenal suppression
Purpura
A 56-year-old morbidly obese man twisted his ankle five days ago and has been bed-ridden since. Today he presents to the emergency department with acute-onset shortness of breath and chest tightness. His past medical history is significant for diabetes mellitus, hypertension, right knee osteoarthritis, and a deep venous thrombosis. His current medications are lisinopril, metoprolol, and metformin. His blood pressure is 110/60 mmHg and his heart rate is 110/min. A CT scan of the chest with contrast is consistent with pulmonary thromboembolism. Which of the following is the best treatment for this patient?
Start heparin now, and in 5-6 days stop heparin and start warfarin
Start both heparin and warfarin now, and stop heparin in 1-2 days
Start heparin and warfarin now, and stop heparin in 5-6 days
Start heparin now and continue for 3-4 weeks
Start warfarin now and continue for at least 6 months
A 35-year old male presents to your office complaining of nocturnal wheezing and chest tightness for the past three months. He has also noticed new hoarseness, particularly in the morning. He has no history of bronchial asthma, hypertension or diabetes. He is a non-smoker but occasionally drinks alcohol. On examination, he is an obese male in no acute distress. His pulse is 84/min, blood pressure is 130/80 mmHg, and respirations are 16/min. His chest is clear to auscultation and percussion. Laryngoscopy reveals a red and inflamed posterior pharynx and larynx. Which of the following pharmacotherapies would be most helpful for this patient?
Bedtime fluticasone inhaler
Bedtime albuterol inhaler
Oral theophylline
Oral omeprazole
Oral prednisone
A 38-year-old female comes to your office with a recent episode of hemoptysis. The symptoms started one week ago with malaise, throat pain and dry cough. The cough progressed becoming productive of yellowish sputum. She started noticing speckles of red blood in her sputum as of yesterday. Her past medical history is significant for peptic ulcer disease. She has a 5 pack-year smoking history, but she quit 10 years ago. Her temperature is 98F (36.7C), blood pressure is 130/80 mmHg and heart rate is 87/min. Physical examination reveals scattered bilateral wheezes. Chest X-ray shows clear lung fields. Which of the following is the most appropriate next step in management?
CT scan of the chest
Pulmonary function tests
Sputum Gram stain and culture
Observation
Sputum cytology
A 27-year-old male presents to you with complaints of cough, chest discomfort and dyspnea on exertion. He says that he has lost 10 pounds over the past 2 months. He has been smoking 1 pack per day for the past 10 years. He drinks 2 beers every weekend. He denies illegal drug use and has not had multiple sexual partners. Physical examination is unremarkable. Chest-x ray reveals a large anterior mediastinal mass. Blood work reveals that he has elevated levels of HCG and alpha-fetoprotein (AFP). What is the most likely diagnosis?
Benign teratoma
Seminoma
Nonseminomatous germ cell tumors
Pericardial cysts
Thymoma
A 74-year-old nursing home resident is brought to the ER with a low-grade fever, cough and shortness of breath for the last two days. The cough is productive of small amounts of greenish sputum. His past medical history is significant for hypertension, diabetes mellitus type 2, COPD, hypercholesterolemia and mild dementia. His blood pressure is 152/78 mmHg and his heart rate is 89/min, regular. Physical examination reveals decreased breath sounds, coarse rhonchi, and increased fremitus over the lower left lung field. His oxygen saturation is 92% on room air when lying on his right side but drops to 84% when he lies on his left. Which of the following best explains this finding?
Increased dead space ventilation
Decreased cardiac output
Decreased oxygen diffusion capacity
Increased arterio-venous shunting
Effort-dependent hypoventilation
A 55-year-old male presents with face and arm swelling that he says is worst when he wakes in the morning. He also notes a 10-pound unintentional weight loss over the past three months, plus new-onset exertional dyspnea. His past medical history is significant for hypertension, for which he takes hydrochlorothiazide. He has smoked cigarettes for the past 40 years and drinks alcohol occasionally. On physical examination, he is afebrile and his vital signs are within normal limits. His face is plethoric and darkappearing. The veins on the anterior chest wall appear engorged. His abdomen is soft, non-tender, and nondistended, and there is no organomegaly. The lower extremities are non-edematous. What is the most appropriate next step in the management of this patient?
Echocardiogram
Doppler ultrasound of the upper extremities
Chest x-ray
Urine for 24-hour protein excretion
Serum albumin level
A 34-year-old male presents to his physician's office for a routine health maintenance examination. He has a five-year history of bronchial asthma for which he uses an albuterol inhaler. He says that he uses the inhaler an average of two times per week during the day. In addition, he states that his asthma symptoms wake him from sleep approximately 3-4 times per month. He does not use tobacco, alcohol or illicit drugs. His family history is significant for asthma in his grandfather. Physical examination is unremarkable. Which of the following is the most appropriate next step in his management?
Add long-acting beta-2 agonist inhaler
Add inhaled corticosteroids
Add oral theophylline
Add oral prednisone
Continue current medical regimen
A 34-year-old male is recovering from head trauma sustained in a motor vehicle accident. He is currently in the intensive care unit on mechanical ventilation. His most recent arterial blood gas analysis shows: pH 7.54 PaO2 124 mmHg PaCO2 20 mmHg Bicarbonate 17 mEq/L Which of the following additional findings do you most expect in this patient?
Low urine bicarbonate excretion
High urine pH
High serum aldosterone level
High serum anion gap
High serum albumin level
A 35-year-old man who recently emigrated from Mexico complains of persistent cough. He says that he coughs up yellowish sputum that is occasionally streaked with blood. He also notes occasional fevers and frequent nighttime awakenings with cough and choking. He has a 20 pack-year smoking history but does not use alcohol or drugs. CT of his chest is shown below. What is the most likely diagnosis?
Bronchiectasis
Pulmonary tuberculosis
Lung cancer
Bronchopulmonary aspergillosis
Sarcoidosis
A 33-year-old male was involved in a motor vehicle accident with numerous rib fractures. His course in the hospital was complicated by difficulty with deep breathing and later developed pneumonia. The chest x-ray later confirmed that the patient had developed a parapneumonic effusion. Which one of the following laboratory tests on the pleural fluid is currently thought to be most helpful in determining the need for chest tube placement in parapneumonic effusion?
Lactate dehydrogenase
WBC count
Pleural fluid pH
Total protein
Color of the pleural fluid
A 4 2-year-old man presents to his primary care physician complaining of daytime sleepiness. He says that he often falls asleep during meetings, watching TV, and even while driving his car. He does not feel refreshed after his daytime naps, and has not experienced vivid hallucinations when falling asleep or upon awakening. He has occasional morning headaches and his wife complains that he sometimes keeps her up at night. Physical exam reveals a body mass index (BMI) of 31.3 kg/m2. An arterial blood gas is normal What is this patient's most likely diagnosis?
Narcolepsy
Obesity hypoventilation syndrome
Obstructive sleep apnea
Central sleep apnea
Primary insomnia
A 24-year-old Caucasian man is brought to the emergency room with acute asthma exacerbation. His current medications include inhaled fluticasone and salmeterol. The attack started 10 hours ago and did not respond to numerous albuterol inhalations and systemic steroids. His blood pressure is 120/70 mmHg and heart rate is 110/min. The patient is tachypneic and speaks with difficulty. Lung auscultation reveals decreased breath sounds, prolonged expiration, and bilateral wheezing. Pulse oximetry showed 86% at room air. ABG at room air are: pH 7.43, Po2 68 mmHg, PCO2 40mmHg. The chest x-ray demonstrates hyperinflated lungs. Which of the following findings indicates that the patient is getting worse?
Lung hyperinflation
Tachypnea
Tachycardia
Hypoxia
Normal PCO2
A 19-year woman presents to her physician's office for a routine health maintenance examination. She notes experiencing occasional wheezing and breathlessness following aerobic exercise, but has no symptoms at other times of the day or night. Her medical history is otherwise significant for allergic rhinitis and acne, for which she uses topical benzoyl peroxide and erythromycin cream. She does not use tobacco, alcohol or illicit drugs. On physical examination, her vital signs are within normal limits and chest auscultation is unremarkable. Which of the following is the most appropriate next step in her management?
A. Beta-adrenergic agonists before exercise
Daily oral steroids
Daily steroid inhalers
Daily oral theophylline
Lpratropium inhalers before exercise
A 34-year-old male is rushed to the emergency room with severe respiratory distress. He is agitated and gasping for breath. He has been seen in the ER several times before for difficulty breathing, food intolerances and skin allergies. Physical examination is notable for excessive accessory respiratory muscle use, retraction of the subclavicular fossae during inspiration, and scattered urticaria over the upper body. What is the most likely diagnosis?
Upper airway obstruction
Asthma exacerbation
Pneumothorax
Eosinophilic pneumonia
Leukocytoclastic vasculitis
A 57-year-old male was involved in a motor vehicle accident and was immediately brought to the Emergency Room. He suffered minor head and neck injury, but was found to have a broken tibia. He underwent repair of the tibial fracture the following day. Five days later, he suddenly develops tachycardia and is tachypneic. He complains of increasing chest discomfort and has a syncopal episode. His blood pressure is 80/55 mmHg, pulse is 130/min, and respirations are 24/min. Pulse oximetry showed 82% on room air. Stat echocardiogram reveals obstruction in the main pulmonary artery. Which of the following choices is the most appropriate course of action?
Heparin infusion
Fibrinolytic therapy
Embolectomy
Inferior vena cava filter
A CT scan of the lung
A 60-year-old man comes to the office with worsening shortness of breath over the last 5 months. He has had two episodes of bronchitis over the last 12 months. He now has a mild nonproductive cough. He denies any fever, chills, hemoptysis, chest pain, or difficulty breathing while lying on his back. His medications include an ipratropium inhaler, aspirin, and amlodipine. He was hospitalized twice in the last 3 years due to an exacerbation of his chronic obstructive pulmonary disease. He has been smoking 1 pack of cigarettes per day for the last 40 years. His temperature is 99 F (37.2 C), blood pressure is 130/86 mm Hg, pulse is 98/min, and respirations are 18/min. Examination shows a thin man in mild respiratory distress with increased anteroposterior chest diameter, diffuse expiratory wheeze and loud S2. Chest X-ray shows hyperinflation of bilateral lung fields with diaphragm flattening and small heart size. Which of the following is the most effective measure to decrease mortality in this patient?
Adding a short acting beta-agonist inhaler
Adding an inhaled corticosteroid
Adding a long-acting beta agonist
Adding systemic corticosteroids
Smoking cessation
A 68-year-old female comes to the Emergency Room with increased shortness of breath and cough for 12 hours. She has a history of chronic obstructive pulmonary disease for the past 14 years and has been oxygen dependent for two years. Twelve hours ago, she felt unable to get her breath. She took two extra nebulizer treatments and used her as-needed inhaler with no relief of symptoms. She denies any fever, chills, sweating, nausea or vomiting, and hemoptysis. She rarely uses alcohol, but had smoked two packs/day for 45 years. She quit smoking about six years ago. Her medications include ipratropium, albuterol, multivitamins, and oxygen 2 liters/min by nasal cannula. She is a thin, frail female in moderate distress. Her temperature is 36.7C (98F), blood pressure is 110/65 mmHg, pulse is 110/min, and respirations are 28/min. Pulse oximetry shows 84% on 2 liters oxygen by nasal cannula. The patient is given oxygen, methyl prednisolone, aerosolized ipratropium, and albuterol; however, the patient remains dyspneic and bedridden. ABGs are ordered and the results show: pH 7.32, PCO2 60 mmHg, and PO2 52 mmHg on 4-liters O2. What is the next best step in the management of this patient?
Increase oxygen by nasal cannula
Decrease oxygen
Intubate and mechanically ventilate the patient
Noninvasive positive pressure ventilation
Aminophylline
A 67-year-old white male with a long history of bronchial asthma and chronic obstructive pulmonary disease (COPD) presents to the emergency room complaining of acute onset of shortness of breath for the last 30 minutes. He says that for the past 2 or 3 days he has been having some difficulty breathing and a productive cough with thick phlegm, but nothing as bad as the current episode. He also has a history of congestive heart failure after suffering a myocardial infarction for which he is taking furosemide and lisinopril. While talking to you in halting sentences, you note that he appears cyanotic, confused and are sweating profusely. He normally takes albuterol, ipratropium and budesonide inhalers for his breathing difficulties, but they have not relieved his current symptoms. On examination, he is found to be markedly dyspneic and his PaO2 is 55 mm Hg. A chest x-ray done in the ER is shown below. Which of the following is the most appropriate next step in the management of this patient?
Start intravenous theophylline
Urgent thoracocentesis
Urgent bronchoscopy
Place central venous line
Increase furosemide and start digoxin
A healthy 36-year-old Caucasian woman comes to the physician because of dyspnea on exertion. She has no other medical problems. She does not use tobacco, alcohol, or drugs. Her father has prostate cancer and her mother had a stroke. She takes no medication and has no known drug allergies. Her temperature is 36.7C (98 F), blood pressure is 140/90 mmHg, pulse is 84/min, and respirations are 22/min. Examination shows clear lung fields. Her chest x-ray shows prominent pulmonary arteries and an enlarged right heart border. EKG shows right axis deviation. Which of the following is the most likely diagnosis?
Mitral stenosis
Mitral valve prolapse
Left ventricular failure
Emphysema
Pulmonary hypertension
A 65-year-old male comes to the physician because of fever, chills, and productive cough. The symptoms started four days ago. He also complains of chest pain, which increases with inspiration. He has smoked one pack of cigarettes daily for 45 years. He drinks 3-4 ounces of alcohol daily. His chest x-ray showed an infiltrate in the right upper lobe. The sputum examination of the patient reveals capsulated gram-negative bacilli. Sputum culture is growing mucoid colonies. Which of the following is the most likely causative organism in this patient?
Escherichia coli
Streptococcus pneumoniae
Klebsiella pneumoniae
Legionella species
Mycoplasma pneumonia
A 26-year-old Caucasian male comes to the physician because of severe productive cough for the past two months. He also complains of occasional blood in sputum, and dyspnea for the last three weeks. His past medical history is significant for otitis media, two episodes of pneumonia, and sinusitis. He and his wife were recently worked up for infertility. Physical examination shows crackles in the left upper lobe. Chest x-ray shows dilated and thickened airways and irregular peripheral opacities in the left upper lobe. Which of the following is the most appropriate test to make the diagnosis of his condition?
Sweat chloride test
DNA studies
Pulmonary function tests
Semen analysis
Bronchoscopy
A 68-year-old male is hospitalized following an intracerebral hemorrhage. On hospital day 3, he develops redness, swelling, and tenderness of the left calf. There is no fever. Compression ultrasonography reveals a thrombus in the popliteal vein. Which of the following is the most appropriate next step in the management of this patient?
Anticoagulation with heparin
Thrombolytic therapy
Compression stockings
No treatment for his deep vein thrombosis
Placement of an inferior vena cava filter

A 69-year -old Caucasian man presents with a two-day history of increasing shortness of breath and lower extremity edema. He is currently short of breath at rest and has an occasional cough. There is no past history of hypertension or ischemic heart disease. He reports drinking half a bottle of vodka daily and has smoked 1 pack of cigarettes per day for 45 years. His blood pressure is 160/90 mm Hg, pulse is 90/min, and oxygen saturation is 90% on room air. JVP is elevated and auscultation of his heart reveals faint heart sounds. The liver span is 18 cm and ascites is also present. No rales are heard in the lungs. There is 3+ lower extremity pitting edema up to the knees. The chest radiograph is shown below. Which of the following is the most likely diagnosis?
Alcoholic cirrhosis
Coronary artery disease
Cardiac tamponade
Metastatic carcinoma of the liver
Cor pulmonale
A 59-year-old male is brought to the emergency department with severe dyspnea and left-sided chest discomfort. He says that he was driving to work when he began to feel suddenly weak and short of breath. He has a long history of chronic obstructive pulmonary disease, esophageal reflux and chronic pyelonephritis. He smokes one pack of cigarettes per day. His current medications include ranitidine and inhaled ipratropium and albuterol as needed. Physical examination reveals trace ankle edema, decreased breath sounds over the left chest and scattered wheezes over the right chest. ECG shows sinus tachycardia. Arterial blood gas analysis is given below: pH 7.42 pO2 59 mmHg pCO2 41 mmHg Which of the following most likely underlies this patient's current condition?
Diffuse bronchial obstruction
Inflammatory pulmonary infiltrates
Interstitial pulmonary edema
Dilated apical airspaces
Pleural fluid transudation
A 31-year-old woman presents to the emergency department complaining of shortness of breath. She denies associated chest pain or palpitations. She tells you that she recently returned from a trip to Thailand. She smokes one pack of cigarettes per day and drinks alcohol occasionally. She is married and uses oral contraceptives. She has no significant past medical history. On physical examination, her blood pressure is 110/70 mmHg and her heart rate is 120/min. A negative result on which of the following tests would best exclude pulmonary venous thromboembolism in this patient?
Echocardiography
Chest x-ray
Plasma D-dimer
Venous ultrasound
Lectrocardiogram
A 32-year-old man with a known history of recreational drug abuse is found by a friend on the floor of his apartment. There is a pool of urine around him. He is confused, not oriented to time or place, and does not recall recent events. His blood pressure is 110/70 mmHg and his heart rate is 120/min. He talks and moves all his extremities. His laboratory findings are the following: Hemoglobin 15.2 mg/dl WBC 12,500/mm3 Platelets 160,000/mm3 Sodium 136 mEq/L Potassium 5.1 mEq/L Creatinine 1.1 mg/dl AST 35 units/L AL T 40 units/L Alkaline phosphatase 70 units/L CPK 26,000 units/L His urine toxicology screen is positive for cocaine and cannabinoids. The patient is at the greatest risk of which of the following?
Aseptic meningitis
Acute renal failure
Reye syndrome
Dermatomyositis
Splenic rupture
A 66-year-old man complains of exertional dyspnea that has progressed over the last two years. As a result, he has had to limit his physical activities to avoid becoming short of breath. He denies any significant chest pain, but does note having a recurrent cough productive of whitish sputum. His past medical history is significant for hypertension controlled with hydrochlorothiazide. He has a 40 pack-year smoking history. His family history is significant for a stroke in his mother. His blood pressure is 160/90 mmHg and his heart rate is 80/min. Physical examination reveals a mildly overweight patient in no acute distress. His anteroposterior chest diameter is markedly increased. Breath sounds are decreased bilaterally with scattered expiratory wheezes. Which of the following agents is most likely to reduce this patient's symptoms?
Alpha-adrenergic blocker
Beta-adrenergic blocker
Muscarinic antagonist
Dopamine agonist
Alpha 2-adrenergic agonist
A 52-year-old nursing home worker presents with a four-week history of non-productive cough and night-time sweating. She also reports having unintentionally lost five pounds over the last month. Her medical history is significant for a mastectomy for left-sided breast cancer five years ago and hepatitis C for which she does not take treatment. She says she was last tested for HIV 6 months ago and the test was negative. She takes no medications currently. She emigrated from Mexico two years ago. She smokes one pack of cigarettes daily and consumes two bottles of beer every weekend. Chest x-ray shows a right upper lobe cavity with surrounding infiltration. Which of the following is the most important epidemiologic clue to the etiology of this patient's disease?
Nursing home worker
Foreign born individual
Smoking history
Previous breast cancer
Hepatitis C
A 44-year-old obese Asian immigrant presents to the ER complaining of a persistent cough for about 3 months. He denies any fever, chills, runny nose or sputum production. He does complain of dyspnea on exertion, which also has been of a short duration. He says that over the last year, he has become progressively short of breath and is unable to sleep lying down. He denies any chest pain or diaphoresis, but has had palpitations in the past. He does not smoke or drink alcohol. On examination, he is alert and in mild distress. He has a BP of 110/70 mmHg, pulse 100/min and is afebrile. Auscultation is difficult. The chest-x ray reveals an enlarged cardiac silhouette. It appears that the left main stem bronchus is elevated. There is no other lung pathology visible. The ECG shows irregularly irregular rhythm. The pathophysiology of this condition is related to which of the following?
Acute pericarditis
Rheumatic fever
Interstitial lung disease
Malignancy
Sarcoidosis
A 72-year-old white male with a past medical history of hypertension, hypothyroidism, and coronary artery disease presented to the physician's office because of fever, malaise, nonproductive cough, and shortness of breath. His temperature was 38.3C (101 F). His chest x-ray showed a patchy right lower lobe infiltrate. He was sent home on oral amoxicillin. Four days later, the patient was brought to the emergency room because he was having continuous fevers, headache, pleuritic chest pain, and abdominal pain. He appears confused. His blood pressure is 120/70 mmHg, pulse rate is 100 per minute, respiratory rate is 24 per minute, and temperature is 38.9C (102 F). His chest x-ray showed consolidation of the right lower lobe. Which of the following is the most likely cause of this patient's pneumonia?
Streptococcus pneumoniae
Mycoplasma pneumoniae
Mycobacterium tuberculosis
Haemophilus influenzae
Legionella pneumonia
A 64-year-old man presents to the emergency department with progressive exertional dyspnea that worsened after he contracted an upper respiratory infection. He also complains of bilateral ankle swelling. He has a 40 pack-year history of smoking. Physical examination reveals a mildly overweight patient in mild respiratory distress. Lung auscultation reveals bilateral wheezes and a prolonged expiratory phase. His white blood cell count is 14,500/mm3 and his hemoglobin level is 16 mg/dl. Arterial blood gas analysis reveals the following: pH 7.37 pO2 65mmHg pCO2 60mmHg Absence of marked acidosis in this patient is best explained by which of the following?
Increased minute ventilation
Increased dead space ventilation
Pulmonary vasoconstriction
Renal tubular compensation
Erythrocyte chloride shift
A 43-year-old woman with congestive heart failure, rheumatoid arthritis and chronic hepatitis C complains of abdominal discomfort and difficulty breathing. Physical examination shows dullness to percussion at the right lung base. Chest x-ray reveals a large right-sided pleural effusion. Thoracentesis yields pleural fluid with a glucose content of 30 mg/dl and an LDH of 192units/L. Which of the following explains the pleural fluid glucose concentration?
Increased pleural membrane permeability
Increased capillary hydrostatic pressure
Increased permeability of the right hemidiaphragm
High white blood cell content of the pleural fluid
High amylase content of the pleural fluid
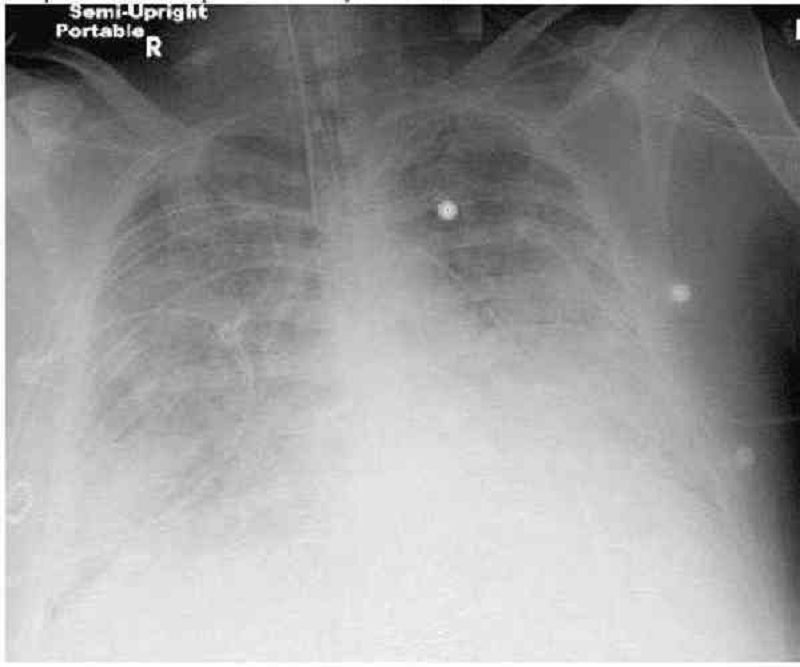
A 64-year-old male is admitted to the hospital with abdominal pain, abdominal distention, and confusion. Upon arrival his blood pressure is 90/60 mmHg and pulse is 120/min. On physical examination, his abdomen is tender, distended, and rigid with positive rebound tenderness. His past medical history is significant for rheumatic fever as a child, hypertension, coronary artery disease and atrial fibrillation. He receives a total of 6 liters of normal saline and undergoes emergent laparotomy. Postoperatively he complains of shortness of breath. His respiratory rate is 34/min. He is emergently intubated because of poor oxygenation. His chest x-ray is shown below: This film is compared to a chest x-ray performed one week earlier, which was within normal limits. Currently, the pulmonary capillary wedge pressure is 8 mmHg. Which of the following is the most likely cause of his current condition?
Idiopathic pulmonary fibrosis
Mitral stenosis
Acute respiratory distress syndrome
Left ventricular systolic dysfunction
Iatrogenic fluid overload

A 45-year-old black female presents to you because of a dry cough and has not been feeling well for the past month. She did have some pain in her shins a few weeks ago. She denies any allergies, smoking, or other medical problems. Her ECG shows normal sinus rhythm. The chest x-ray is shown below. What is the most likely pathophysiology in this patient?
A. Pulmonary venous congestion
Lupus pneumonitis
Inflammatory granulomas
Malignancy of the lung
Interstitial lung disease
A 4 2-year-old morbidly obese man is being evaluated for poor sleep. He complains of frequent awakenings due to a choking sensation and says that the resulting tiredness severely limits his physical activity. He also complains of chronic leg swelling. He denies cigarette, alcohol, or drug use. On physical examination, his blood pressure is 160/100 mmHg and his heart rate is 110/min. Which of the following additional findings is most likely to be present in this patient?
Anemia due to low erythropoietin
Decreased chloride due to bicarbonate retention
Decreased sodium due to increased ADH secretion
Decreased C02 due to persistent hypoxia
Increased BUN due to volume constriction
A 32-year-old Caucasian female presents to your office with persistent cough and shortness of breath. She has had three episodes of pneumonia over the last year. She had severe sinusitis one year ago, and an episode of bloody diarrhea that required hospitalization and IV antibiotic therapy six months ago. She does not smoke or consume alcohol. She denies any illicit drug use. She is currently not taking any medications. All her immunizations are up-to-date. Her blood pressure is 130/80 mmHg and heart rate is 90/min. Physical examination reveals fine crackles over the right lower lung lobe. No lower extremity edema is present. Neck palpation does not reveal any lymph node enlargement. The chest x-ray shows right lower lobe infiltrates and left upper lobe fibrosis. The ECG reveals non-specific ST segment and T wave changes. What is the best next step in the management of this patient?
Measurement of serum alpha- 1-antitrypsin level
Methacholine challenge test
Quantitative measurement of serum lg levels
Sweat chloride test
Ventilation/perfusion lung scan
A 32-year-old man presented to the emergency department five hours ago with an acute asthma exacerbation. He has been receiving continuous albuterol nebulizer treatments since that time. He has a 20-year history of asthma but notes that recently the frequency of his attacks has increased. Presently, his blood pressure is 110/70 mmHg and heart rate is 120 and regular. On physical exam, the patient appears drowsy. Breath sounds are diminished bilaterally but there are no wheezes. The most recent ABG reveals: pH 7.32 pO2 65mmHg pCO2 50mmHg Which of the following is the best next step in managing this patient?
Inhaled corticosteroids
Lpratropium inhalation
Intravenous theophylline
Oral prednisone
Endotracheal intubation
A 25-year-old male presents with progressive shortness of breath over the past 6 months. His past medical history is significant only for neonatal hepatitis that resolved spontaneously when he was 6 months of age. The man has never smoked. On lung auscultation today, there are decreased breath sounds over both lower lobes. Chest x-ray demonstrates emphysematous changes in the bilateral lower lobes. Routine blood work is normal. Which of the following analyses would be most helpful in establishing this patient's diagnosis?
Open lung biopsy
Serum alpha-1 antitrypsin level
Video-assisted lung biopsy
High resolution CT scan of chest
Pulmonary function testing
A 38-year -old male is brought to the emergency room with high-grade fever, shaking chills, productive cough and shortness of breath that started two days ago. His medical history is significant for two hospital admissions for alcohol withdrawal seizures. He continues to drink alcohol every day. He has no other medical problems and does not take any medications. On admission, his temperature is 39.7°C (103.5.F), pulse is 110/min, blood pressure is 100/70 mmHg, and respirations are 20/min. His skin and mucous membranes are dry. Physical examination reveals crackles and bronchial breath sounds in the right lower lobe. Chest x-ray demonstrates right lower lobe consolidation. He is started on ceftriaxone, azithromycin and intravenous normal saline at 200 ml/hr. Six hours later the nurse calls you because he is breathing at 38/min and requiring 100% oxygen. Emergent intubation is performed. A repeat chest x-ray is shown below.Which of the following is now most likely to be present in this patient?
Normal pulmonary capillary wedge pressure
Increased lung compliance
Increased left ventricular end diastolic pressure
Normal pulmonary arterial pressure
Normal alveolar-arterial oxygen gradient
A 64-year-old male presents to the physician's office with increasing shortness of breath. He denies orthopnoea, paroxysmal nocturnal dyspnea, or chest pain. He was hospitalized for pneumonia four years ago but has otherwise been healthy. He has smoked one pack of cigarettes daily for the past 30 years. He does not take any medications. His temperature is 37.2°C (98.9.F), blood pressure is 124/76 mm Hg, pulse is 82/min and respirations are 16/min. Pulse oximetry reveals an oxygen saturation of 88%. On chest auscultation, breath sounds are diminished throughout, and the expiratory phase is prolonged. Heart sounds are regular and there are no murmurs or gallops. There is no peripheral edema or jugular venous distention. Laboratory studies show a hematocrit of 56% and WBC count of 6,700/mm3. Which of the following interventions will have the maximum impact on this patient's survival?
Maintenance oral steroids
Prophylactic antibiotics to reduce exacerbations
Influenza and pneumococcal vaccinations
Long-term supplemental oxygen therapy
Long-term beta-blocker therapy
A 47-year-old male who has just returned from a cruise to the Bahamas presents to the hospital with a high-grade fever, productive cough and shortness of breath for the past two days. He also complains of frequent vomiting and diarrhea. He has no prior medical problems, does not take any medications, and denies using tobacco, alcohol or drugs. His temperature is 40°C (104 °F), blood pressure is 110/65 mm Hg, pulse is 80/min, and respirations are 18/min. Lung examination reveals right lower lobe crackles. The abdomen is soft and non-tender. Chest x-ray demonstrates right lower lobe consolidation. Sputum Gram stain contains many neutrophils with no organisms. Which of the following antibiotics must be given to this patient?
Vancomycin
Clindamycin
Fluconazole
Amoxicillin
Azithromycin
A 56-year-old woman is brought to the emergency room with shortness of breath, which she says began suddenly two hours ago while she was enjoying her favorite television show. She also reports the simultaneous onset of sharp, left-sided chest pain. Her previous medical history includes diabetes mellitus for the past 10 years and hypertension for the past 6 years. Her family history is significant for heart disease in her father, who died at age 40. Her medications include enteric-coated aspirin, captopril and glipizide. She has a 30 pack-year smoking history, but does not smoke currently. On physical examination, she is in acute distress and is sweating profusely. Her temperature is 38.0°C (100.5.F), pulse is 140/min and irregular, respiratory rate is 30/min, and blood pressure is 110/60 mm Hg. Her oxygen saturation is 84% on room air by pulse oximetry. Jugular venous pressure is within normal limits and her lungs are clear to auscultation. Serum analysis reveals the following: Hematocrit 40% WBC count 11,600/mm3 Platelet count 190,000/mm3 Chest x-ray is unremarkable. ECG reveals irregular RR intervals, with no definite P waves and narrow QRS complexes. Which of the following is the most likely cause of her current symptoms?
Myocardial infarction
Mitral stenosis
Cardiac tamponade
Tension pneumothorax
Pulmonary embolism
A 36-year-old female presented to the emergency room with fever and a productive cough. The physician on call suspected community acquired pneumonia and prescribed azithromycin for 5 days. After 5 days of treatment, she comes to your office with no improvement of her symptoms and complains of worsening foul smelling sputum. Further inquiry reveals that she had undergone an upper GI endoscopy 8 days ago for a long history of heartburn and suspected peptic ulcer disease. She also reports a history of manic-type bipolar disorder. In your office she has a blood pressure of 130/80 mm Hg, her pulse is 108/min, temperature is 38.7C (101.6F) and respirations are 26/min. Chest x-ray showed a right upper lobe infiltrate. Which of the following additional therapies would be most helpful for this patient's condition?
Doxycycline
Ciprofloxacin
Trimethoprim-sulfamethoxazole
Clindamycin
Gentamicin+ ampicillin
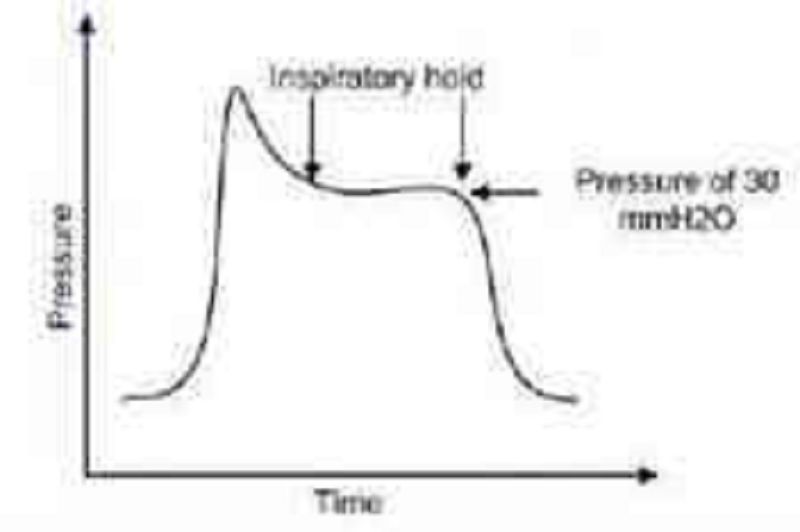
A 32-year-old man is intubated and mechanically ventilated after an opioid drug overdose. The ventilator triggers 12 breaths per minute, each delivering 500 ml of tidal volume at a flow rate of 60 L/min. You perform an inspiratory hold for 2 seconds following delivery of the tidal volume, and the airway pressure is measured to be 30 cm H2O: The measured pressure reflects which of the following?
Upper airway resistance
Total airway resistance
Pulmonary compliance
Expiratory muscle strength
End-expiratory pressure
A 55-year-old man presents to your office with a six-month history of non-productive cough, especially at night. He denies postnasal drip, chest pain, difficulty breathing, or wheezing. His only other complaint is water brash. His past medical history is insignificant, and he is not taking any medications. He does not smoke or consume alcohol. Physical examination is insignificant. Chest x-ray and pulmonary function testing are normal. Esophagoscopy is also normal. What is the next best step in the management of this patient?
Esophageal mucosal biopsy
24-hour pH recording
Barium swallow
Bernstein test
Esophageal manometry
A 53-year-old homosexual man comes to the ER with shortness of breath and dry cough over the past week. You note that he was hospitalized for Candida esophagitis one month ago, but left against medical advice. On physical examination, his blood pressure is 120/70 mmHg, heart rate is 120/min and regular, oxygen saturation is 89% on 2Umin of oxygen by nasal cannula, and temperature is 38.3° (101°F). There are extensive white plaques over the oral mucosa and there is a soft 2/6 systolic murmur over the cardiac apex. Lung auscultation is remarkable for faint bilateral crackles. Which of the following is most likely responsible?
Increased pulmonary capillary wedge pressure
Alveolar hypoventilation
Increased alveolar-arterial oxygen gradient
Increased lung compliance
Pulmonary hypertension
A 65-year-old Caucasian male comes to the physician because of shortness of breath, fever, and a productive cough for the last four days. He is a chronic smoker and alcoholic. He quit smoking two years ago. His medical problems include hypertension, chronic obstructive pulmonary disease, paroxysmal atrial fibrillation, and coronary artery disease. He is taking daily-inhaled ipratropium bromide, albuterol, metformin, metoprolol, warfarin, and diltiazem. His temperature is 38.9 C (102 F), blood pressure is 140/88 mmHg, pulse is 110/min, and respirations are 28/min. Pulse oximetry showed 88% on room air. Examination shows decreased breath sounds and crackles over the right lower lobe of the lung. Which of the following is the most appropriate next step in his management?
Bronchoscopy
Sputum gram stain
Chest x-ray
Mycoplasma serology
Sputum culture
A 42-year-old white male presents to your office complaining of periodic breathing difficulty and wheezing. He visited an otolaryngologist for persistent nasal blockage recently. His past medical history is significant for unstable angina experienced five months ago. His current treatment includes aspirin, diltiazem, and pravastatin. He does not use tobacco, alcohol, or drugs. His vital signs are within limits. What is the most probable cause of this patient's respiratory complaints?
IgE-mediated reaction
Immune complex disease
Cytotoxic antibodies
Cell-mediated hypersensitivity
Pseudo-allergic reaction
A 45-year-old male comes to the emergency room complaining of shortness of breath that began 3 hours ago. He also has a nonproductive cough, a low-grade fever and right-sided chest pain that worsen with inspiration. He denies coughing up blood, wheezing, palpitations, leg pain or swelling of his lower extremities. He recently returned home from a trip to Singapore. He has a history of hypertension and diabetes mellitus. His takes fosinopril, metformin and glyburide. He doesn't use tobacco, alcohol or illicit drugs. His temperature is 98.0 F (36.6C), blood pressure is 115/70 mmHg, pulse is 128/min, respirations are 32/min, and O2 saturation is 84% on room air. Physical examination shows a slightly obese man in acute respiratory distress. He is alert and cooperative without any cyanosis or jaundice. He has a slightly displaced apical impulse with a S4. Chest-x ray shows mild cardiomegaly with no infiltrates. EKG shows sinus tachycardia and left ventricular hypertrophy without ST-T wave changes. His arterial blood gas analysis shows pH 7.52, pCO2 30, pO2 55, HC03 22. What is the next best step in the management of this patient?
Pulmonary angiogram
Lower extremity venous ultrasound
Spiral CT scans of the chest
Initiate heparin weight-based protocol
Broad spectrum antibiotics

A 35-year-old male from Arizona presents to the physician's office with a low-grade fever and cough of two months duration. He also reports malaise and a weight loss of 71bs over this same period. He has a history of HIV infection diagnosed two years ago. He received a pneumococcal vaccine at the time his HIV was diagnosed. He also receives an annual influenza vaccine. He is not on any antiretroviral therapy. His temperature is 37.7C (99.8F), pulse is 75/min, blood pressure is 130/80 mm Hg and respirations are 14/min. Examination shows clear lungs to auscultation. His current CD4 count is 450cells/microl. His chest radiograph is shown below:Which of the following is the most likely cause of his cough?
Bronchial asthma
Gastroesophageal reflux disease
Postnasal drip
Mycobacterial infection
Coccidioidomycosis
A 56-year-old male presents with progressively worsening dyspnea over a 4-month period. He denies fever, chest pain, cough or ankle swelling and does not use tobacco, alcohol or drugs. He works for a home insulation and plumbing company. He has never been abroad and does not own any pets. His only medications are hydrochlorothiazide and metoprolol for blood pressure control. On physical examination, his temperature is 36.8°C (98.2.F), pulse is 76/min, blood pressure is 130/78 mmHg, and respirations are 15/min. Examination shows digital clubbing and fine bibasilar end-inspiratory crackles. Jugular venous pressure is 7 cm and there is no peripheral edema. Which of the following additional findings is most likely in this patient?
Increased pulmonary capillary wedge pressure
Decreased diffusion lung capacity (DLCO)
Decreased pulmonary arterial pressure
Increased residual lung volume
Reduced FEV1/FVC ratio
A 43-year-old moderately overweight woman presents to the emergency department complaining of two days of shortness of breath. Today, while climbing stairs, she had an episode of severe lightheadedness and near syncope. Her medical history is significant for a right calf deep venous thrombosis one year ago. She takes no medications currently. On physical examination, her blood pressure is 90/50 mmHg and her heart rate is 120/min and regular Imaging studies are most likely to reveal which of the following?
Mitral stenosis
Pericardial effusion
Right ventricular dilation
Bilateral pulmonary nodules
Asymmetric hypertrophy of the intraventricular septum
A healthy 33-year-old man comes for a pre-employment examination. He has no complaints and has no medical problems. He does not use tobacco, alcohol, or drugs and takes no medications. He has no occupational exposures and has lived his entire life in suburban Mississippi. His temperature is 36.7 C (98.0F), blood pressure is 120/80 mmHg, pulse is 78/min, and respirations are 16/min. Examination shows no abnormalities. His chest x-ray shows a 1.5 cm nodule in his right mid-lung field. Other labs are unremarkable. Which of the following is the most likely diagnosis?
Coccidioidomycosis
Histoplasmosis
Tuberculosis
HIV infection
Pneumocystis jiroveci infection
A 30-year-old African American female presents with a two-month history of shortness of breath and nonproductive cough. She has never had symptoms like these before. Her past medical history is significant for an episode of uveitis six months ago. She does not take any medications. She works as a secretary in a local office building. She does not use tobacco and drinks alcohol only on special occasions. She has no pets and has been monogamous with a single partner for the last three years. On physical examination, her temperature is 37.2°C (98.9.F), blood pressure is 126/76 mm Hg, pulse is 76/min and respirations are 16/min. Lung auscultation reveals patchy rales. The remainder of her examination is unremarkable. Chest x-ray shows diffuse interstitial infiltrates. Which of the following is the most likely cause of her shortness of breath?
Pneumocystis pneumonia
Congestive heart failure
Sarcoidosis
Idiopathic pulmonary fibrosis
Ankylosing spondylitis
A 63-year-old male complains of cough and nocturnal wheezing. The cough is mostly non-productive but can sometimes relieve chest tightness if a small amount of yellow sputum is produced. His past medical history is significant for a hospitalization for a 'chest infection' two years ago. His appetite is good but he lost 5 pounds over the last several months. He has smoked one pack of cigarettes per day for the past 40 years. He drinks 2-3 cans of beer per day on the weekends. His mother suffered from diabetes mellitus and his father died of a stroke. On physical examination, his blood pressure is 140/80 mmHg and his heart rate is 80/min. There is chest hyperinflation and scattered expiratory wheezes on auscultation. The patient expires through pursed lips. His fingers demonstrate prominent clubbing. This patient's clubbing is most likely related to:
Lung hyperinflation
Airflow obstruction
Pulmonary hypertension
Hypoxemia
Occult malignancy
A 65-year-old male with oxygen-dependent chronic obstructive pulmonary disease, chronic atrial fibrillation, and depression comes into the Emergency Room, with symptoms of increased dyspnea and worsening cough pattern. His recent history had been significant for a gradual worsening of his baseline lung disease over the past month, which had been treated by his outpatient doctor with increased frequency of inhaled beta-agonist and azithromycin. This morning he had a severe shortness of breath that was unresponsive to "stacked" home nebulizer treatments. The ER physician notes that the patient is in moderate severe respiratory distress. His temperature is 37.2C (99F), blood pressure is 150/90 mmHg, pulse is 110/min, and respirations are 28/min. Accessory muscle use was noted. Lung exam shows diffuse rhonchi and wheezing. A pulse oximetry revealed an oxygen saturation of 80% on room air. His chest x-ray showed no new infiltrates. His WBC count is 7,000/cmm with normal differential. The ER physician had given nebulization, and the patient is on 5-liters of oxygen. Which of the following should also be considered in this patient?
Gatifloxacin
Methylprednisolone
N-acetylcysteine
Clarithromycin
Aminophyllin
An 80-year-old Caucasian female is brought to the emergency room by her son with a three-day history of fever and a foul-smelling, productive cough. Her past medical history is significant for advanced dementia, diabetes, and hypertension. She takes aspirin, metformin, insulin, and atenolol. She was admitted two times with pneumonia during the past two months. Her temperature is 38.3 C (101 F), blood pressure is 100/70mmHg, pulse is 105/min, and respirations are 20/min. The patient is not oriented in time and place. Physical examination reveals dry mucus membranes and decreased skin turgor. Breath sounds are decreased to the right. A chest x-ray revealed right, lower lobe infiltrate. Which of the following is the most important predisposing factor for this condition in this patient?
Decreased lung elasticity
Gastro-esophageal reflux
Impaired epiglottic reflex
Decreased thyroid function
Depressed cell-mediated immunity
A 40-year-old Caucasian man comes to the emergency department because of fever, dry cough, and shortness of breath. Symptoms started 24 hours ago. He denies hemoptysis. He was recently discharged from the hospital after a second cycle of chemotherapy for acute myeloid leukemia. He does not use tobacco, alcohol, or drugs. His temperature is 38.9 C (102.0 F), blood pressure is 120/70 mmHg, pulse is 112/min and respirations are 28/min. The patient's pulse oximetry showed 86% at room air. Examination shows diffuse crackles all over the lung fields. His chest x-ray shows diffuse interstitial infiltrates. Which of the following is the most likely cause of his condition?
Tuberculosis
Coccidioidomycosis
HIV infection
Histoplasmosis
Pneumocystis jiroveci

A 65-year-old female presents with 6 months of worsening dyspnea and dry cough. Whereas she had previously enjoyed an active lifestyle, she now becomes breathless after walking just a few steps. The patient denies fever or chest pain and does not use tobacco, alcohol or illicit drugs. Her only medicine is hydrochlorothiazide for hypertension. She is retired and lives with her husband. She has never travelled abroad and denies any history of exposure to pets. On physical examination, her temperature is 37.2°C (98.9.F), blood pressure is 140/86 mm Hg, pulse is 84/min and respirations are 18/min. Examination shows dry, late inspiratory crackles and finger clubbing. Her chest x-ray is shown below:WHich of the following abnormalities is most likely to be present in this patient?
Increased diffusing capacity of carbon monoxide
Decreased FEV1/FVC ratio
Increased residual volume
Creased PaCO2
Increased A-a gradient
45-year-old woman comes to your office with a three-month history of fatigue, exertional dyspnea, and non-productive cough. She has also been having difficulty swallowing. Her only other medical problems are Raynaud's phenomenon, heartburn, and high blood pressure. On examination, diffuse thickening of the skin with telangiectasia is noted. Her current medications include amlodipine, enalapril, and ranitidine. What is the most probable pathologic mechanism of her pulmonary complaints?
Pulmonary fibrosis
Pulmonary vascular lesions
Aspiration pneumonia
Bronchogenic carcinoma
Restriction of chest movement
A 65-year-old man with chronic obstructive pulmonary disease, chronic atrial fibrillation, hypertension, and diabetes mellitus presents with a three-day history of shortness of breath. His condition began with runny nose, itchy eyes, and sore throat, but his symptoms progressed to productive cough, wheeze, and dyspnea. Physical examination reveals a mildly overweight man in moderate respiratory distress. His blood pressure is 150/90 mmHg and his heart rate is 110/min and irregular. On chest auscultation, expirations are prolonged and there are bilateral wheezes. You administer bronchodilators, facial mask oxygen, and lorazepam for agitation. Thirty minutes later, he is lethargic and confused. While you discuss the case with your attending, the patient experiences a generalized tonic-clonic seizure. Which of the following most likely underlies his neurologic symptoms?
New-onset thromboembolic stroke
Cerebral vasoconstriction
Subarachnoid hemorrhage
Carbon dioxide retention
Metabolic acidosis
A 32-year-old man presents to the emergency department with pain and swelling in the right leg. He was recently hospitalized for a right lower extremity deep venous thrombosis and discharged on warfarin. Today his INR is 1.12. Ultrasound reveals a right popliteal vein thrombosis extending into the deep femoral vein. What is the best initial management step for this patient?
Increase warfarin dose for goal INR > 2.0
Start intravenous unfractionated heparin
Initiate thrombolytic therapy
Place inferior vena cava filter
Discontinue warfarin and reassure
A 56-year-old Caucasian male complains of chronic exertional dyspnea for the past several years that has progressively worsened. He cannot remember the last time that he saw a doctor, and does not take any medications regularly. It is difficult for him to climb two flights of stairs without having to rest. His dyspnea has gotten so bad that it has severely limited his activity level, and he now spends most of his time on the couch. He also describes recurrent episodes of nocturnal dyspnea, during which he wakes up at around 2:00 AM with difficulty breathing, coughing, and wheezing that improve when he sits up. He usually coughs up some yellowish sputum before being able to go back to sleep. He has had no fever, chills, or chest pain. Which of the following is the most likely cause of this patient's complaints?
Left ventricular failure
Bronchial asthma
Chronic bronchitis
Pulmonary thromboembolism
Pulmonary fibrosis
A 62-year-old man presents to his primary care physician's office with progressive exertional dyspnea. His past medical history is significant for hypertension treated with hydrochlorothiazide and diabetes mellitus treated with metformin. He was an industrial worker for 30 years and retired one year ago. He smokes one pack of cigarettes per day and consumes alcohol occasionally. His blood pressure is 150/100 mmHg and his heart rate is 80/min. His BMI is 31 kg/m2. Chest x-ray reveals pleural calcifications. Pulmonary function studies show the following: FEV1 70% of predicted FVC 65% of predicted Residual volume 70% of predicted DLCO decreased Which of the following is the most likely cause of this patient's symptoms?
Impaired lung expansion due to pleural calcifications
Emphysema from smoking
Interstitial lung disease from occupational exposure
Impaired lung expansion due to obesity
Increased pulmonary capillary wedge pressure
A 32-year-old woman comes to the emergency department complaining of sudden onset shortness of breath accompanied by a non-productive cough and left-sided chest discomfort that increases on inspiration. She denies subjective fever, coughing up blood, wheezing, palpitations, leg pain, and swelling of the lower extremities or any recent travel. Past medical history is significant for an appendectomy at age 15. Her medications include birth control pills and over- the-counter vitamins. She is a known carrier of sickle cell trait. Her father, age 65, has had diabetes for 20 years; mother, age 58, has coronary artery disease. She has never been pregnant, drinks alcohol socially and does not smoke. Her temperature is 99 F (38C), blood pressure is 110/70 mmHg, pulse 130/min and respirations are 33/min. Pulse oximetry shows an oxygen saturation of 85% on 6 liters of oxygen. Her BMI is 30 kg/m2. She is alert and cooperative without cyanosis or jaundice. Her lungs are clear to auscultation. Her abdomen is soft, nondistended and non-tender. Which of the following is the best test to confirm this patient's diagnosis?
EKG and cardiac enzymes
Echocardiogram
Doppler ultrasound of lower extremities
Spiral CT-Scan of the chest
Chest-x ray and sputum cultures
A 53-year-old male presents with progressively worsening dyspnea over a 4-month period. He also complains of decreased appetite, weight loss, and nagging epigastric discomfort. His past medical history is significant for a chronic duodenal ulcer for which he takes ranitidine on and off. He does not use tobacco, alcohol or illicit drugs. He has worked as a plumber for the past 30 years. On physical examination, his temperature is 36.9°C (98.4.F), blood pressure is 140/86 mm Hg, pulse is 80/min, and respirations are 15/min. Physical exam reveals fingernail clubbing and bibasilar end-inspiratory crackles on lung auscultation. Chest x-ray demonstrates ground glass opacities of the lower lung fields, multiple pleural plaques, and one 3x3 cm mass in the right lung periphery. CT guided biopsy of the mass is planned. Biopsy is most likely to show which of the following?
Metastatic stomach cancer
Metastatic colon cancer
Metastatic pancreatic cancer
Bronchogenic carcinoma
Peritoneal mesothelioma
A 50-year-old female comes into your office complaining of four-month history of dry cough. She denies dyspnea or hemoptysis. Past medical history is significant for hypertension, diabetes, and gout. Her current medications include enalapril, metformin, hydrochlorothiazide, and allopurinol. She does not smoke or consume alcohol. Her vital signs are BP 130/80 mmHg, HR 80/min, T 36.7C (98F) and RR 16/min. Physical examination is within normal limits. The best next step in the management of this patient is:
Chest radiograph
Reevaluation of drug therapy
Pulmonary function testing
Barium esophagography
Bronchoscopy
106. A 47-year-old African American woman presents with two days of shortness of breath and left-sided chest pain. Her past medical history is significant for a mastectomy six months ago for breast cancer, for which she also received adjuvant chemotherapy. Her mobility has been limited recently due to progressive back pain. Her current medications include tamoxifen. On chest x-ray, there is an infiltrate obscuring the right heart border as well as a right-sided pleural effusion. Pleural fluid analysis reveals the following: pH 5.75 Nucleated cells 10,050/mm3 RBC 1,500/mm3 Protein 3.9 g/dl LDH 620 units/L Glucose 38 mg/dl Her serum chemistries are notable for an LDH of 310 units/L and protein of 6.1 g/dl. Which of the following is the most likely cause of her effusion?
Heart failure
Pneumonia
Drug-induced lupus
Pulmonary embolism
Hypoalbuminemia
A 45-year-old white man presents to your office complaining of daytime somnolence, increased fatigability, and morning headaches. He says that his wife complains that he snores loudly. He is not taking any medications and does not smoke or consume alcohol. His blood pressure is 145/90 mmHg and heart rate is 90/min. Physical examination reveals a well-nourished man with BMI = 31 kg/m2. What is the next best step in the management of this patient?
A benzodiazepine to improve sleep
Advise to sleep in supine position
Weight reduction
A thiazide diuretic for hypertension
Tracheostomy
A 64-year-old male presents to the ER with shortness of breath. The symptoms started one week ago with a dry cough and mild fever. His past medical history includes hypertension and exertional angina. He was hospitalized six months ago for pneumonia. He has a 35 pack-year smoking history. His blood pressure is 140/90 mmHg and heart rate is 90 and regular. On examination, the patient is in mild respiratory distress. He uses some accessory respiratory muscles for breathing, but he can speak in full sentences. Chest auscultation reveals bilateral wheezes and crackles at the left lung base. His ABG shows: pH 7.36 pO2 72mmHg pCO2 51mmHg Which of the following is the most likely cause of this patient's current symptoms?
Congestive heart failure (CHF)
COPD exacerbation
Pulmonary embolism
Pneumothorax
Adult respiratory distress syndrome
A 37-year-old female with a long history of multiple sclerosis presents to her primary care physician complaining of dyspnea. She denies cough and fever but admits to right-sided chest pain. Her medical history is significant for an episode of atrial fibrillation diagnosed in the emergency department two weeks ago, which resolved spontaneously without intervention. She is wheelchair-bound due to spastic paraparesis and has saccadic speech. Her only allergy is to penicillin. On physical examination, her blood pressure is 120/70 mmHg and her heart rate is 110/min and regular. Chest x-ray demonstrates a right-sided pleural effusion. Therapeutic thoracocentesis is performed, and pleural fluid analysis reveals the following: Protein 3.1 g/L RBC count 230/mm3 WBC count 150/mm3 LDH 220 IU/L Glucose 100 mg/dl Which of the following is the most likely cause of this patient's pleural effusion?
Congestive heart failure
Hypoalbuminemia
Pulmonary embolism
Aspiration pneumonia
Malignancy
A 43-year-old previously healthy male is hospitalized for acute pancreatitis. On day 3 of his admission, he develops respiratory distress. He is transferred to the intensive care unit and intubated. His initial ventilator settings are: FiO2 0.8 (80%) Respiratory rate 10/min Tidal volume 500 ml PEEP 5 mm H20 Ten minutes after being intubated, the man's blood pressure is 110/70 mmHg and his heart rate is 90/min. His arterial blood gases are: pH 7.42 pO2 105 mmHg pCO2 37 mmHg Which of the following is the best next step in the management of this patient?
Decrease the positive end expiratory pressure (PEEP)
Decrease the tidal volume
Decrease the FiO2
Decrease the respiratory rate
Increase the respiratory rate
A 35-year-old male from Wisconsin presents to his physician complaining of fever, night sweats, productive cough, and an unintentional 17-lb weight loss over the past 3 months. Several days ago, he also began to notice multiple skin lesions. He has no known medical problems and does not take any medications, nor does he use tobacco, alcohol or illicit drugs. He works outdoors in wood cutting and construction. Physical examination reveals a man of medium build in no apparent distress. His temperature is 38.4°C (101.1°F), blood pressure is 120/68 mm Hg, pulse is 86/min, and respirations are 14/min. Skin examination reveals multiple, well-circumscribed, verrucous, crusted lesions. Chest x-ray shows left upper lobe consolidation and two lytic lesions in the anterior ribs. Which of the following is the most likely cause of his current symptoms?
Disseminated tuberculosis
Sarcoidosis
Metastatic osteosarcoma
Blastomycosis
Coccidioidomycosi
A 35-year-old male was involved in a motor vehicle injury and suffered serious chest trauma. A chest tube was placed for a hemothorax. 800 cc of blood was evacuated from the chest, and, after ten days, the patient was discharged home. He returns again with a low-grade fever and dyspnea. CT scan reveals a complex loculated effusion with a thick surrounding peel. A chest tube is placed; however, after 24 hours, there is little drainage, and the patient continues to have a low-grade fever. What is the next step in his management?
Surgery
Streptokinase into the chest tube
Increase the dose of IV antibiotics
Place a second chest tube
Pulmonary consult for bronchoscopy
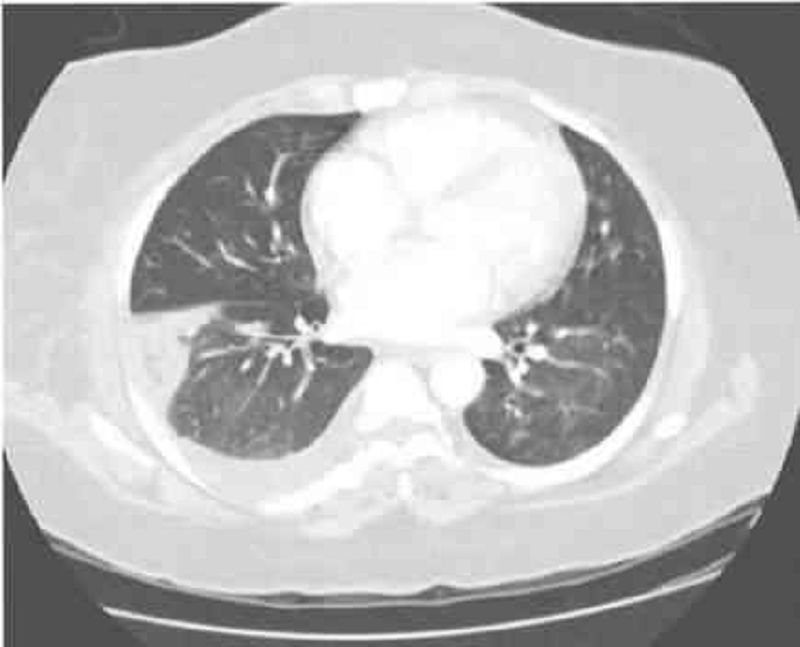
A 34-year-old woman presents with one week of low-grade fever, diarrhea, and lethargy plus two days of hemoptysis and severe pleuritic-type chest pain. In the past she abused heroin but is currently in a methadone program. She has a 20 pack-year cigarette smoking history. Her medical history is significant for HIV and hepatitis C infections. Her last CD4 count was 350/μl two months ago. PPD testing revealed 2 mm of induration at the same time. On physical examination today, her blood pressure is 130/80 mmHg, heart rate is 100/min, and temperature 38.1°C (100.6.F). Breath sounds are diminished at the base of the right lung. Chest CT is shown below. Which of the following is the most likely diagnosis?
Pulmonary tuberculosis
Pulmonary thromboembolism
Pneumocystis pneumonia
Bacterial pneumonia
Lung cancer
40-year-old white male develops a proximal deep vein thrombosis in the left lower extremity. Detailed history, examination and lab testing fail to reveal any obvious cause or risk factor for his deep venous thrombosis. Idiopathic deep vein thrombosis is diagnosed and the patient starts a 6-month course of warfarin anticoagulation. What is the goal INR therapeutic range in this patient
1.0 to 1.5
.1.5to2.0
2.0 to 3.0
2.5 to 3.5
Greater than 4
A 25-year-old man presents to the emergency room with shortness of breath and cough productive of blood tinged sputum for the past few days. He denies associated fever, arthralgias or weight loss. He has never had these symptoms before, and is extremely concerned. He has no history of recent travel or sick contacts. He smokes half a pack of cigarettes daily, and has had two sexual partners in the past six months. On physical examination, his temperature is 37.2°C (98.9.F), blood pressure is 120/70 mm Hg, pulse is 102/min, and respirations are 22/min. Lung auscultation reveals patchy bilateral rales. Chest x-ray demonstrates bilateral pulmonary infiltrates. His serum creatinine is 2.6 mg/dl and urinalysis shows dysmorphic red cells. Which of the following is the most likely cause of his current condition?
Basement membrane antibodies
Pneumocystis pneumonia
Infection with acid fast bacilli
Pulmonary thromboembolism
Cardiac valve infection
A 32-year-old female complains of a 'nagging' dry cough over the last 4 weeks. She says that the cough is present during the day and also wakes her from sleep at night. There is no associated shortness of breath, chest pain or wheezing. Her past medical history is significant for chronic rhinorrhea and an occasional itching skin rash. She takes no medications. Chest x-ray shows no abnormalities. One week of treatment with chlorpheniramine significantly improves her symptoms. Decrease in which of the following is most likely responsible her symptom relief
Airway hyperreactivity
Bronchial inflammation
C. Acid aspiration
Nasal secretions
Bradykinin production
A 50-year-old male presents to his physician complaining of daytime somnolence. He reports that yesterday, he fell asleep while stopped at a red light. His wife adds that he is a habitual snorer, and sometimes seems to stop breathing for seconds at a time while sleeping. His past medical history is significant for hypertension, a 25 pack-year smoking history, and a two beer per day drinking habit. Physical examination reveals an obese, middle-aged man in no apparent distress. His pulse is 88/min, blood pressure is 160/100 mm Hg, and respirations are 14/min. The remainder of the physical examination, including chest auscultation, is within normal limits. Which of the following is the most appropriate next step in the management of this patient?
Prescribe methylphenidate
Pulmonary function testing
MRI of the upper airways
Nocturnal polysomnography
Dexamethasone suppression test
37-year-old male is being evaluated after a motor vehicle accident. He complains of right sided chest pain. Physical examination reveals mild bruising over the right chest wall, and is otherwise unremarkable. Chest x-ray shows no rib fractures but a solitary round lesion is seen in the right upper lobe of the lung. Upon further questioning the patient denies recent weight loss or appetite change. He has never smoked cigarettes. Which of the following is the most appropriate next step in the management of his lung lesion?
CT-guided biopsy
CT scan of the chest
Bronchoscopy
Obtain previous x-rays to compare
Obtain whole body CT scan
An obese 56-year-old female presents to her physician concerned that her asthma is worsening. She describes night-time cough and wheezing that have been increasing over recent months. She also reports feeling tired each morning because she works late hours and has no time to relax after dinner. On review of systems, the patient denies dyspnea on exertion, but acknowledges that her throat has been sore lately. Her past medical history is significant for bronchial asthma, type2 diabetes and hypertension. Her medications include an albuterol inhaler which she uses occasionally, lisinopril and aspirin. Her vital signs are within normal limits, and there are no abnormalities on physical exam. Which of the following is the most appropriate next step in the management of this patient?
Discontinue lisinopril
Discontinue aspirin
Add inhaled fluticasone
Add pantoprazole
Add salmeterol
A 66-year-old male presents to the emergency room with shortness of breath. The symptoms started one week ago with a dry cough and exertional dyspnea. His past medical history includes hypertension and recent stenting for double-vessel coronary artery disease. He was hospitalized six months ago for pneumonia. He has a 35 pack-year smoking history. His temperature is 37.2 C (98.9F), blood pressure is 160/90 mmHg, and heart rate is 90 and regular. On examination, the patient is in mild respiratory distress, but he can speak in full sentences. Chest auscultation reveals decreased breath sounds at the lung bases, bilateral crackles and occasional wheezes. His ABG shows: pH 7.46 pO2 73mmHg pCO2 31mmHg Which of the following is the most likely explanation for this patient's symptoms?
Congestive heart failure
COPD exacerbation
Pulmonary embolism
D. Pneumothorax
Adult respiratory distress syndrome
A 55-year-old Caucasian man comes to the emergency department because of fever and productive cough, with foul-smelling sputum. He also complains of shortness of breath. His other medical problems include hypertension and hypercholesterolemia. In the past three months, he was admitted in the hospital two times for pneumonia. He has smoked one pack of cigarettes daily for 28 years and drinks 5-6 beers daily. Family history is not significant. His medications include hydrochlorothiazide and simvastatin. His temperature is 38.9 C (102 F), blood pressure is 120/70 mmHg, pulse is 112/min, and respirations are 24/min. The patient's pulse oximetry showed 89% at room air. Examination shows crackles at the right lung base. His chest x-ray shows right, lower lobe infiltrate. A CT scan of the chest shows no mass or obstruction. Which of the following is most likely responsible for this patient's symptoms?
Excessive smoking
Excessive alcohol intake
Depressed humoral immunity
Depressed cell-mediated immunity
Underlying malignancy
A 45-year-old female presents to the emergency department because of increasing somnolence and shortness of breath. Her past medical history is significant for hyperlipidemia, hypertension and type2 diabetes. She has never smoked and does not use drugs or alcohol. Her temperature is 36.7°C (98.F), blood pressure is 160/80 mm Hg, pulse is 80/min, and respirations are 16/min. Her BMI is 55 kg/m2. On physical examination, she is drowsy but able to respond to commands. Jugular venous distention is difficult to visualize due to a thick neck. Lungs are clear to auscultation. Heart sounds are distant. Abdomen is obese and non-tender. Lower extremities have edema bilaterally. There are no obvious focal deficits on neurologic examination. Chest x-ray is poor in quality but no obvious abnormalities are noted. EKG shows low voltage QRS complexes but no significant ST-segment or T-wave abnormalities. Laboratory studies show: Complete blood count: Hemoglobin 16.0 g/L Hematocrit 48% Mean corpuscular volume 85 fl Platelet count 224,000/mm3 Leukocyte count 6,600/mm3 Arterial blood gas: pH 7.30 pO2 60mmHg pCO2 69mm Hg Which of the following is the most likely cause of her condition?
Venous thromboembolism
Aspiration pneumonia
Pneumocystis pneumonia
Impaired chest wall compliance
Pulmonary edema
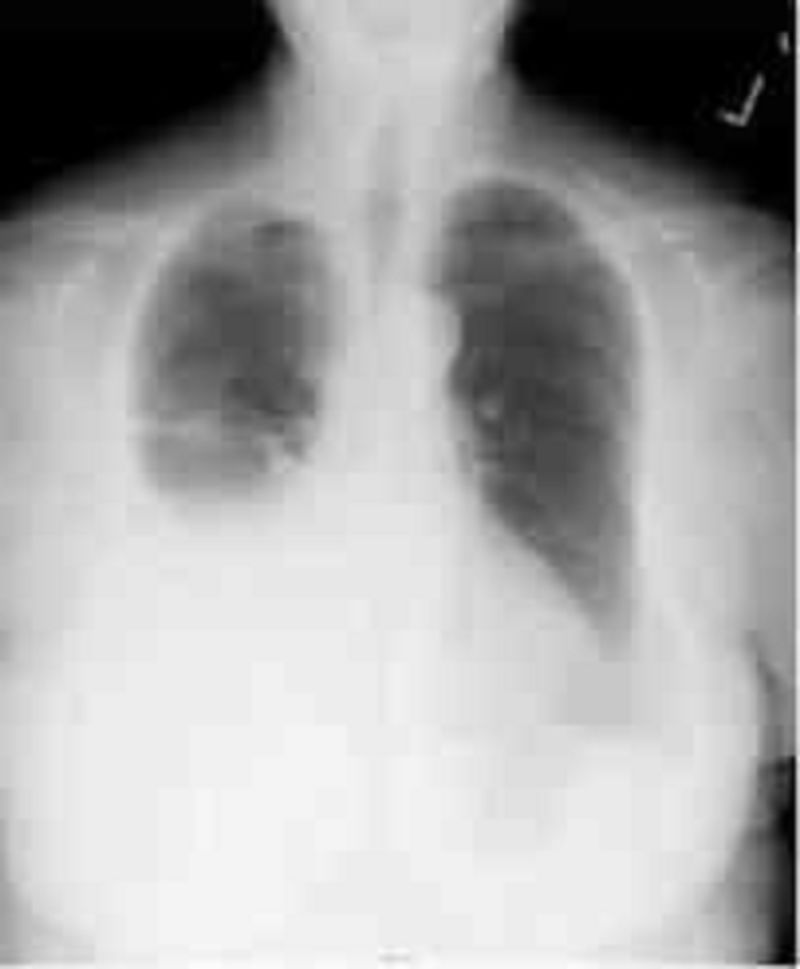
A 60-year-old Caucasian female comes to the physician because of progressive shortness of breath for the past month. She has had a 13.6 kg (30 lb) weight loss during this period. She has a history of hypertension and hypothyroidism and takes metoprolol and levothyroxine. She has smoked two packs of cigarettes daily for 35 years. Her temperature is 36.7 C (98 F), blood pressure is 130/70 mmHg, pulse is 80/min, and respirations are 20/min. On examination, decreased breath sounds and dullness to percussion are noted on the right, middle and lower lobes of the lung. Her chest x-ray is shown below.Which of the following is the most appropriate next step in the management?
Bronchoscopy
Mediastinoscopy
Thoracentesis
Video-assisted thoracoscopy
Open pleural biopsy
A 60-year-old male with a history of hypertension, diabetes, coronary artery disease, asthma, and cigarette smoking undergoes emergent laparotomy for a perforated peptic ulcer. He receives 4 liters of intravenous normal saline intraoperatively. Following the procedure, he is extubated without complication, but subsequently develops respiratory distress. Immediate arterial blood gas analysis on room air shows: PaO2 60mmHg pH 7.46 PaCO2 37mmHg HCO3 22mmHg His temperature is 37.2°C (98.9.F) and blood pressure is 126/76 mm Hg. Lung auscultation reveals bilateral rales. His arterial blood gas fails to improve with administration of 100% oxygen. What is the most likely cause of his respiratory distress?
Excessive anesthesia
Pulmonary edema
Pulmonary embolism
Aspiration pneumonia
Exacerbation of bronchial asthma
A 40-year-old man presents to the emergency room with shortness of breath, cough and hemoptysis for the past two days. He says he has never had symptoms like these before. His medical history is significant for a non-healing leg ulcer and chronic purulent nasal discharge. He has smoked a pack of cigarettes daily for the past 20 years. On physical examination, his temperature is 37.6°C (99.7°F), blood pressure is 130/90 mm Hg, pulse is 94/min and respiratory rate is 18/min. Lung auscultation reveals patchy rales bilaterally. Heart sounds are regular. A 2x3cm ulcer with rolled, undermined borders is noted on the right lower leg. Which of the following is the most likely explanation for his hemoptysis?
Pulmonary tuberculosis
Bronchogenic carcinoma
Wegener's granulomatosis
Mitral stenosis
Pulmonary embolism
A 62-year-old Caucasian male presents to your office because of a non-productive cough that is 'quite disturbing.' The cough has been present for several weeks. He visited your office two times before for poorly controlled hypertension, and was started on lisinopril. He usually takes aspirin, amlodipine, and metoprolol. He does not smoke or consume alcohol. His blood pressure is 130/90 mmHg and heart rate is 60/min. Physical examination reveals a bruit over the right carotid artery, but is otherwise normal. Which of the following is the most likely cause of this patient's complaint?
Inhibition of beta-adrenoreceptors
Inhibition of prostaglandin synthesis
Increased serum renin level
Low level of circulating catecholamines
High kinin level
A 46-year-old male is hospitalized with severe acute pancreatitis. Because of progressive respiratory difficulty, he is intubated and placed on mechanical ventilation. His weight is 70 kg (152 lb), blood pressure is 110/70 mmHg, and heart rate is 90/min. Chest x-ray shows patchy opacities bilaterally, consistent with pulmonary edema. His current ventilator settings are: assist control mode, respiratory rate of 12/min, tidal volume of 450 ml, FiO2 of 40%, and positive end-expiratory pressure (PEEP) of 5 cm H20. His blood gas readings are: pH 7.51 pCO2 22mmHg pO2 121mmHg Which of the following is the best next step in managing this patient?
Bronchodilator therapy
Decrease Fi02
Decrease respiratory rate
Increase tidal volume
Incentive spirometry
A 69-year-old male presents to the ER with severe shortness of breath for the past 12 hours. He reports that he has used his albuterol inhaler many times without relief. On review of systems he notes having had a mild fever yesterday that resolved with acetaminophen. The patient quit smoking 2 years ago but has a 100 pack year smoking history. On physical examination, his blood pressure is 150/90 mmHg and heart rate is 110/min. The patient is using accessory muscles of respiration. Expirations are prolonged, and there are wheezes bilaterally. Arterial blood gas (ABG) analysis reveals the following: pH 7.36 pO2 64 mmHg pCO2 57 mmHg HCO3 32 mEq/L The patient is treated with ipratropium and albuterol nebulizers and moxifloxacin. Which of the following additional therapies is most likely to benefit this patient?
Corticosteroids
Loop diuretic
Mucolytic agents
Aminophylline
Diltiazem
A 28-year-old male presents to the physician's office for a routine health maintenance examination. He has a two-year history of bronchial asthma for which he uses an albuterol inhaler. He states that he experiences asthma symptoms an average of 2 times per week, for which his albuterol inhaler provides relief. He has not had nighttime awakenings over the past month. He does not use tobacco, alcohol or illicit drugs. His family history is significant for asthma in his grandfather. Physical examination is unremarkable. Which of the following is the most appropriate next step in his management?
Add long-acting beta-2 agonist inhaler
Add inhaled corticosteroids
Add oral theophylline
Add oral prednisone
Continue current medical regimen
A 25-year-old female presents to the emergency department with sudden-onset severe shortness of breath and wheezing. She has a history of asthma. On examination, she is unable to speak in full sentences and is using accessory muscles of respiration. She is intubated, mechanically ventilated and treated with continuous albuterol nebulization and intravenous methylprednisolone. Within six hours, her condition is improved. She is extubated and treated with hourly nebulizer treatments. The next morning, she complains of muscle weakness. On physical examination, she has difficulty lifting her arms over her head and mild hand tremors. Her vital signs are stable What should be the immediate next step in her management?
Check peak expiratory flow rate
Check chest x-ray, PA view
Check serum TSH level
Check serum electrolyte panel
Obtain electromyography (EMG)
A 26-year-old white female comes to the Emergency Room with severe shortness of breath. She has a long history of asthma with periodic exacerbations. She is taking an inhaled albuterol, inhaled steroid, salmeterol and cromolyn. Her temperature is 37.2C (99F), blood pressure is 150/90 mmHg, pulse is 110/min, and respirations are 24/min. On examination, she has moderate respiratory distress, prolonged expiratory phase, and significant wheezing all over the lung fields. Patient is admitted and is given nebulized albuterol, intravenous methyl prednisone, and oxygen. The next day her respiratory status improved. Her vital signs did not change much, except normalization of respiratory rate. Still scattered bilateral wheezes are heard on lung auscultation. The next day her laboratory values are: Hemoglobin 14 g/dL MCV 95 fL Leukocyte count 19,000/cmm Segmented Neutrophils 80% Bands 5% Lymphocytes 13% Eosinophils 0% Basophils 0% Monocytes 2% Chest x-ray obtained at the time of admission is normal, except for hyperinflated lung fields. What is the most probable cause of the abnormal lab findings in this patient?
Pneumonia
Hypersensitivity reaction
Myeloproliferative state
Metabolic disorder
Drug reaction
A 40-year-old black male presents with dyspnea and tachypnea of sudden onset. He says that he was diagnosed with deep venous thrombosis (DVT) of the lower extremities three times before. Ventilation/perfusion scan reveals mismatched perfusion defect. Venous ultrasonography is positive for DVT. You suspect that inherited predisposition to hypercoagulation may be present. Which of the following is the most common form of such a predisposition?
Protein C deficiency
Protein S deficiency
Antithrombin Ill deficiency
Factor V Leiden
Plasminogen disorders
A 45-year-old male immigrant from Haiti complains of cough and tenacious mucopurulent sputum for several months. He denies fever or chest pain, but notes shortness of breath and occasional blood-tinged sputum. He has received antibiotic treatment for similar symptoms twice in the past year. He has smoked 1 pack of cigarettes daily for the past 20 years. On physical examination, his temperature is 37.2°C (98.9.F), blood pressure is 120/68 mm Hg, pulse is 80/min, and respirations are 14/min. On lung auscultation there are coarse crepitations at the bilateral bases. Chest x-ray reveals prominent bronchioles in the lower lobes but is otherwise unremarkable. What is the most appropriate next step in the management of this patient?
High resolution CT scan of the chest
Bronchoscopy and alveolar lavage
Bronchography using non-iodinated contrast medium
Check sputum for acid fast bacillus (AFB)
Echocardiography
A 32-year-old male presents to your office complaining of daytime sleepiness and frequent night-time awakenings. He says that his sleep gets disrupted by a choking sensation, sometimes accompanied by cough and dyspnea. After such episodes he typically has trouble falling back to sleep. The patient notes that his symptoms are somewhat improved when he sleeps with multiple pillows. Physical examination is unremarkable except for a BMI of 29 Kg/m2. What is the most likely diagnosis?
Restless leg syndrome
Asthma
Left ventricular failure
Obstructive sleep apnea
Gastroesophageal reflux disease
A 78-year-old man is seen in the doctor’s office for a nonproductive cough, 9-kg (20-lb) unintentional weight loss, and bilateral breast enlargement, all occurring within the past 6 months. He has smoked two packs per day for the past 40 years. His past medical history is otherwise unremarkable, and he takes no medications. His temperature is 36.7°C (98.1°F), blood pressure is 125/85 mm Hg, pulse is 68/ min and regular, respiratory rate is 15/min, and oxygen saturation is 99% on room air. There are crackles at the left lower lung field and a ridge of symmetric glandular tissue (1 cm in diameter) around the nipple-areolar complexes of both breasts. Complete blood cell count shows a WBC count of 6000/mm³ hemoglobin of 14.7 g/dL, and platelet count of 210,000/ mm³. All other laboratory results are normal. X-ray of the chest shows a focal 5-cm mass lesion in the left lower lung corroborated by CT scan. Which of the following is most likely histologic type of lung cancer present in this patient?
Adenocarcinoma
Bronchoalveolar cell carcinoma
Large cell carcinoma
Small cell carcinoma
Squamous cell carcinoma
A 30-year-old patient with a history of mild persistent asthma (baseline peak expiratory flow rate of 85%) presents to the emergency department with shortness of breath and wheezing that has not relieved by her albuterol inhaler for the past 12 hours. She was able to tolerate pulmonary function tests and a set was performed. Which of the following is the most likely test result?
Decreased FEV1, normal/increased FVC, decreased FEV1: FVC ratio, with post- bronchodilator FEV1 increased by 13%
Decreased residual volume and total lung capacity
Increased FEV1, increased FVC, normal FEV1: FVC ratio
Increased residual volume, increased total lung capacity, increased FEV1
Normal FEV1, decreased FVC, increased FEV1: FVC ratio

A 3-year-old boy presents to the emergency department with a fever and difficulty breathing. He is the product of a normal pregnancy and has been healthy since birth. His immunizations are up to date. This morning he appeared to be in his usual state of health and was dropped off at day care by his father. Later on, his teacher noticed that he had suddenly become fussy and flushed and could not be consoled with toys, rocking, or hearing a story. He also felt warm to the touch and was drooling more than usual. When she took his temperature, it was 39°C (102.2°F). His parents were contacted immediately, and the patient was brought to the emergency department. He appears toxic and anxious, and has loud labored breathing. He is sitting upright, bracing himself on his arms, with his neck hyperextended and mouth open. His temperature is 40°C (104°F), respiratory rate is 50/min, pulse is 140/min, blood pressure is 102/62 mm Hg, and oxygen saturation is 100% on room air. Lateral x-ray of the neck is shown in the image. Laryngoscopy reveals a large cherryred epiglottitis. What is the most appropriate next step in management?
Antibiotic therapy
Corticosteroids
Nasotracheal intubation
Observation
Tracheostomy
A 27-year-old woman is 7 months pregnant with her first child. Her pregnancy has been uncomplicated to date. She presents to the emergency department complaining of sudden-onset, right-sided chest pain that is exacerbated with deep breathing and shortness of breath, which began 1 hour ago. She denies leg pain and notes that her legs began swelling during the sixth month of her pregnancy but the swelling has not worsened. Her temperature is 37.9°C (100.3°F), blood pressure is 130/87 mm Hg, pulse is 107/min and regular, respiratory rate is 24/min, and oxygen saturation is 90% on room air, increasing to 98% with 4 L oxygen via nasal cannula. Physical examination is significant for crackles at the lower right lung field and a negative Homans’ sign bilaterally. X-ray of the chest appears nor- mal. The D-dimer level is elevated. ECG shows sinus tachycardia, right-axis deviation, S wave in lead I, Q wave in lead III, and an inverted T wave in lead III. Which of the following is the most appropriate next step in diagnosis?
Arterial blood gas analysis
Doppler ultrasound of the lower extremity
MRI of the lower extremity
Pulmonary angiography
Ventilation/perfusion scans
A 20-year-old African American woman presents with mild dyspnea on exertion and joint discomfort in her knees, wrists, and ankles. She also has a fever and red tender rash on her shins. Physical examination reveals hepatosplenomegaly, generalized lymphadenopathy, corneal opacities, and tender erythematous nodules on her legs. CXR shows bilateral symmetric hilar adenopathy. Transbronchial biopsy reveals noncaseating granulomas. Which of the following is the most likely cause for the eye lesion?
Uveitis
Diabetic complications
Steroids
Congenital origin
Infectious infiltration
A 74-year-old man with a history of smoking notices blood in his chronic daily sputum production. He has no fever or chills, but has lost 10 lb in the past 6 months. On examination, he has bilateral expiratory wheezes, and his fingers are clubbed. There are no lymph nodes and the remaining examination is normal. CXR reveals a left hilar mass. Which of the following suggests that the tumor is a small cell lung cancer?
Syndrome of inappropriate antidiuretic hormone (SIADH) secretion
Acanthosis nigricans
Cushing’s syndrome
Leukemoid reaction
Stevens-Johnson syndrome
A 44-year-old woman presents with increased shortness of breath, cough, and sputum production. She has had asthma since childhood and uses her medications as directed. Recently, she noticed that her peak flow readings were decreasing after the symptoms started. On examination, she is in moderate respiratory distress, respirations 25/min, there are bilateral wheezes and oxygen saturation is 90% on room air. On her blood gas, the PCO2 is 50 mm Hg. Which of the following is the most likely mechanism for her carbon dioxide retention?
Impaired diffusion syndromes
Right-to-left shunt
Hyperventilation
Ventilation-perfusion ratio inequality
Mechanical ventilation at fixed volume
A 35-year-old HIV-positive man (CD4+ cell count 150/mm³) is seen in the emergency department with right-sided chest pain. The patient has become progressively dyspneic over the past few days. Suddenly, 30 minutes ago he noticed a sharp pain in his chest associated with shortness of breath. His temperature is 37.7° (99.9°F), blood pressure is 128/84 mm Hg, pulse is 102/min and regular, respiratory rate is 25/min, and oxygen saturation is 90% on room air. Physical examination reveals diminished right-sided breath sounds and hyperresonance. Jugular venous distention is 5 cm and there is no tracheal deviation. ECG shows sinus tachycardia. X-ray of the chest shows a right-sided pneumothorax occupying approximately 10% of the right thoracic cavity. Which of the following most likely caused this patient’s presentation?
Intravenous drug use
Kaposi’s sarcoma
Mycobacterium tuberculosis
Pneumocystis jiroveci pneumonia
Toxoplasmosis
A 55-year-old man presents to his physician’s office with increasing dyspnea on exertion. He denies chest pain, diaphoresis, nausea, or vomiting. He has been involved in eight motor vehicle accidents in the past 3 years. Past medical history is significant for hypertension, for which he takes a diuretic. His temperature is 37.2°C (99.0°F), blood pressure is 121/82 mm Hg, pulse is 85/min, respiratory rate is 14/min, and oxygen saturation is 99% on room air. Physical examination is significant for a body mass index of 35 kg/m², a diffuse and laterally displaced point of maximal intensity, and an S3 gallop. Which of the following is the most appropriate next step in diagnosing his most likely underlying condition?
Cardiac catheterization
Echocardiogram
Exercise tolerance test
Polysomnography
X-ray of the chest
A 74-year-old man presents to his primary care physician complaining of dyspnea and cough with blood-tinged sputum for the past several weeks. He has diabetes and elevated cholesterol. Medications include a sulfonylurea and a statin. The patient has a 50-pack-year smoking history and a family history of hypertension. His vital signs are within normal limits. Physical examination reveals abdominal striae and moon facies, along with a truncal fat distribution. X-ray of the chest reveals a single central nodule, and follow-up CT again demonstrates the nodule and multiple solid hepatic masses. Which of the following is the most likely diagnosis?
Adenocarcinoma of the lung
Carcinoma metastatic to the lung
Large cell carcinoma of the lung
Small cell carcinoma of the lung
Squamous cell carcinoma of the lung
A 35-year-old homeless man presents to the emergency department with chief complaints of a cough and fever. He is intoxicated. He admits to drinking about a fifth of vodka every day and confirms a history of delirium tremens and blackouts. X-ray of the chest is significant for an air-fluid level in the superior segment of the right lower lobe. Which of the following is the most appropriate first-line agent for treating this patient’s condition?
Azithromycin
Clindamycin
Isoniazid
Moxifloxacin
Piperacillin-tazobactam
A 5-month-old infant has failed to gain weight despite a good appetite. The child’s mother reports that the baby has up to eight bulky, foul-smelling, oily stools per day. A sweat chloride test reveals a chloride level of 78 mEq/L (normal: <60 mEq/L). Which of the following sequelae is most likely to occur as a result of this patient’s disease?
Cirrhosis and subsequent hepatic failure
Dehydration, electrolyte abnormalities, and acute hypotension
Esophageal ulceration or strictures and upper gastrointestinal bleeding
Purple lines on the gums, red-brown discoloration of the urine, and renal tubular acidosis
Recurrent airway disease with eventual respiratory insufficiency associated with bronchiectasis
A 33-year-old farmer complains of recurrent episodes of wheezing after working in a barn where hay is stored. On auscultation, there are bibasilar crackles and heart sounds are normal. His laboratory work is normal with no increase in eosinophils and the chest x-ray (CXR) reveals patchy lower lobe infiltrates. Which of the following is the most likely diagnosis?
Asthma
Chronic obstructive lung disease
Hypersensitivity pneumonitis
Bronchiectasis
Sarcoidosis
A 57-year-old man with a 40-pack-per-year his- tory of smoking experiences symptoms of shortness of breath on exertion. He has bilateral wheezes on expiration and increased resonance to percussion of the chest. Pulmonary function tests confirm the diagnosis of chronic obstructive lung disease (COPD). Which of the following is the best definition of this condition?
It is caused by bronchial asthma
It is preceded by chronic bronchitis
It is airflow limitation that is not fully reversible
It is due to destruction and dilatation of lung alveoli
Is due to small airways disease only
An agitated and nervous 24-year-old woman has had severe wheezing and shortness of breath for 2 days. After receiving oxygen, steroids, and salbutamol (Ventolin) in the emergency room, her breathing improves. She is still wheezing and now feels tremulous and anxious with a pulse of 110/min and respirations 30/min. Arterial blood gases on oxygen reveal a pH of 7.40, PO2 340 mm Hg, PCO2 40 mm Hg, and bicarbonate of 24 mEq/L. She is hospitalized for further treatment. Which of the following treatments or medications should be avoided in her?
Theophylline
Sedatives
Corticosteroids
Sympathomimetic amines
Intravenous (IV) fluids
A 29-year-old woman has a long history of mild asthma. She now has a flare and experiences recurrent episodes of bronchial obstruction, fever, malaise, and expectoration of brownish mucous plug. On examination, there is bilateral wheezing. Infection is suspected and a CXR reveals upper lobe pulmonary infiltrates. The eosinophil count is 2000/mL, and serum precipitating antibodies to Aspergillus are positive. Which of the following is the most appropriate next step in management?
Antihelminthic therapy
A short course of systemic glucocorticoid therapy
Desensitization treatment
High-dose glucocorticoids by puffer
Long-term systemic glucocorticoid therapy
A 31-year-old African American man presents with dyspnea on exertion. He also has fever and red tender rash on his shins. Physical examination reveals fine inspiratory crackles in both lower lung lobes and tender erythematous nodules on his legs. CXR shows bilateral hilar adenopathy and reticulonodular changes in both lungs. Transbronchial biopsy reveals noncaseating granulomas. Which of the following is the most appropriate next step in management?
Aspirin
Isoniazid (INH) and streptomycin
Steroids
Nitrogen mustard
No therapy
A 53-year-old man with a long respiratory his- tory is admitted to the hospital because of increasing shortness of breath and sputum production. He is started on antibiotics and inhaled bronchodilators and anticholinergic agents. The next day he is found in his room confused and sleepy. A PCO2 determination reveals severe hypercarbia (PCO2 70 mmHg). Which of the following explanations regarding his elevated PCO2 is correct?
Occurs only with CO2 inhalation
Does not occur in obstructive lung disease
Does not occur in restrictive lung disease
May worsen with oxygen administration
Occurs with chronic hypocapnia
A 30-year-old man presents to the resuscitation bay with gunshot wounds in the anterior and posterior left chest. Although in distress and dyspneic, the patient is cooperative. He has a patent airway and is moving all extremities. His pulse is 120/min, blood pressure is 120/90 mm Hg, and respiratory rate is 30/min. He has bounding distal pulses, and no other injuries are identified on secondary examination. X-ray of the chest reveals fluid in the pleural space, and a left chest tube thoracostomy yields 600 mL of bright red fluid. Over the next hour 750 mL of blood is collected. What is the most ap- propriate next step in management?
Autotransfuse with the collected blood and continue to observe closely
Insert another chest tube
Left thoracotomy
Remove the chest tube and suture the inci- sion closed
Thoracentesis
A 38-year-old man is being seen in his physician’s office after being involved in a car accident. He has a vague pain along his right sternal border, where he crashed into the steering wheel. His temperature is 36.6°C (97.8°F), pulse is 80/min, blood pressure is 123/75 mm Hg, respiratory rate is 14/min, and oxygen saturation is 99% on room air. Physical examination is significant for point tenderness over the right sternal border. X-ray of the chest shows no broken ribs but a single, well-circumscribed pulmonary nodule, 1.5 cm in diameter, located in the left lower lung field. A search through the patient’s electronic medical file reveals that he had an x-ray of the chest taken 2 years ago. The radiology report from that time reveals that the nodule was only 0.75 cm in diameter. To characterize the lesion, CT of the chest is performed and shows dense, flocculated calcification within the lesion. Which of the following risk factors most increases the chances of malignancy in this patient?
Increased doubling time of tumor
Increased patient age
Nodule diameter of 1.5 cm or higher
Presence of discrete border
Presence of flocculated calcification

A 21-year-old nonsmoking college student comes to the local emergency department because pf cough, weight loss, and low-grade fever. Occasionally his sputum is tinged with blood. X-ray of the chest is shown in the image. He reports traveling to Haiti on a “medical mission” trip several years ago. Which of the following is the most likely diagnosis?
Aspergillosis
Klebsiella infection
Lung cancer
Sarcoidosis
Tuberculosis
A 63-year-old woman is seen in the emergency room with acute shortness of breath. There is no history of heart or lung problems in the past. She was recently diagnosed with breast cancer and is undergoing active treatment. On examination, her blood pressure is 120/80 mm Hg, pulse 100/min, and heart and lungs are normal. There are no clinical signs of deep venous thrombosis (DVT). Which of the following investigations is most likely to rule out a pulmonary embolism (PE)?
Normal CXR
Normal electrocardiogram (ECG)
Normal ventilation-perfusion lung scan
Normal ventilation scan
Normal magnetic resonance image (MRI)
A 53-year-old man presents to the clinic with complaints of increasing shortness of breath, a nagging cough, and weight loss over several months. He reports no history of cigarette smoking but has worked underground in the New York City subway system for the past 20 years. Spirometry demonstrates an FEV1: FVC ratio of 0.7 and an FEV1 value that is 60% of expected. The FEV1 improves to 70% of expected with bronchodilator treatment. Which of the following is the most likely diagnosis?
Asthma
Chronic aspiration
Chronic obstructive pulmonary disease
Histoplasmosis
Tuberculosis
A 22-year-old woman with mild persistent asthma comes to the primary care clinic after an emergency department visit 2 days ago for an acute asthma exacerbation. She notes an increase in frequency of wheezing and shortness of breath for the past 4 months, with daily symptoms, and has been symptomatic for at least 2 nights per week. She has also had three emergency department visits during the same period. Her current asthma medications include montelukast (leukotriene inhibitor) daily and an albuterol inhaler as needed. The patient’s peak flow is 75% of predicted. Which of the following is the most appropriate next step in management?
Add a long-acting inhaled β-adrenergic agonist and low-dose inhaled steroid to the regimen
Add systemic steroids to the regimen
Admit to the hospital for further pulmonary work-up
Discontinue the leukotriene inhibitor and change the regimen to daily low-dose in- haled steroids
Start cromolyn sodium
A 78-year-old woman is seen in the emergency department for difficulty breathing and cough over the past 4 hours. She has a history of congestive heart failure for which she takes hydrochlorothiazide, metoprolol, and enalapril. Her oxygen saturation is 92% on room air. On examination there is a high-pitched systolic crescendodecrescendo murmur best heard at the right upper sternal border with radiation to the carotids, and rales are present in both lung fields on inspiration. There is 2+ symmetrical pitting edema bilaterally in the lower extremities. X-ray of the chest shows an enlarged heart and prominent pulmonary vasculature. Which of the following is the most likely cause of the patient’s pulmonary edema?
Decreased capillary fluid oncotic pressure
Decreased interstitial fluid hydrostatic pressure
Increased capillary fluid hydrostatic pressure
Increased capillary permeability
Increased interstitial fluid oncotic pressure
A 40-year-old woman has been complaining of a 3-year history of increasing dyspnea and fatigue. She has no other medical illness. Physical examination reveals increased jugular venous pressure (JVP) with prominent c-v wave, and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests show a slight restrictive pattern. Primary pulmonary hypertension is suspected. Which of the following is the most appropriate test to confirm the diagnosis?
Open lung biopsy
Pulmonary angiography
Cardiac catheterization
Noninvasive exercise testing
Electrophysiologic testing
A 56-year-old man is evaluated for chronic cough. It is present most of the time and is progressively getting worse over the past 3 years. With the cough he usually has white to yellow sputum that he has to expectorate. There is no history of wheezing, asthma, congestive heart failure (CHF), or acid reflux disease. He currently smokes one pack a day for the past 25 years. On examination, his chest is clear. CXR is normal and his forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) on spirometry are normal. Which of the following is the most likely diagnosis?
Chronic obstructive pulmonary disease (COPD)
Early cor pulmonale
Chronic bronchitis
Asthma
Emphysema
A 58-year-old man is recently diagnosed with bowel cancer. He now complains of vague chest discomfort and shortness of breath. On examination, he is unwell, blood pressure 90/50 mm Hg, pulse 110/min, respirations 26/min, and oxygen saturation 88%. His lungs are normal on auscultation, the JVP is 8 cm, and P2 is loud. There is no edema or leg tenderness on palpation. A quantitative (ELISA) D-dimer assay is positive, ECG reveals sinus tachycardia, and cardiac enzymes are negative. The lung scan is read as high probability for PE. Which of the following tests is most likely to help in guiding emergent therapy?
Echocardiogram
CT scan
Venous ultrasound of the legs
Contrast phlebography
Pulmonary function tests
A 35-year-old man is evaluated for symptoms of shortness of breath. He reports no other lung or heart disease. He smokes half pack a day for the past 10 years. On examination, his JVP is 2 cm, heart sounds normal, and lungs are clear. A CXR shows hyperinflation and increased lucency of the lung fields. A chest CT reveals bullae and emphysematous changes, while pulmonary function tests show an FEV1/FVC ratio of <70%. Evaluation of his family reveals other affected individuals. Which of the following is the most likely diagnosis?
Alpha1-antitrypsin deficiency
Beta-glycosidase deficiency
Glucose-6-phosphatase deficiency
Glucocerebrosides deficiency
Growth hormone deficiency
A 23-year-old man notices a gradual but progressive increase in breathing difficulty. He has a long history of back pain with prolonged morning stiffness. He has also had an episode of iritis in the past. On examination, there is reduced range of motion in the lumbar spine with forward flexion and pain on palpation of the sacroiliac joint and surrounding soft tissue. X-rays of the pelvis show erosions and sclerosis of the sacroiliac joint. Which of the following is the most likely pulmonary complication of this condition?
Fibrocavitary disease
Airflow obstruction
Bilateral lower lobe involvement
Pleural effusions
Hilar adenopathy
A 45-year-old Haitian immigrant presents to the emergency department with a chief complaint of productive, blood-tinged cough for 2 months. He has been in the United States for 1 month. His temperature is 40.1°C (104.2°F) and heart rate is 105/min. On physical examination he appears cachectic, and pulmonary rales are heard throughout his lung fields. X-ray of the chest reveals multiple bilateral upper lobe cavitary lesions with associated intrathoracic adenopathy. Results of sputum culture are pending. Which of the following tuberculosis medications can potentially cause optic neuritis?
Ethambutol
Isoniazid
Levofloxacin
Pyrazinamide
Rifampin
A 30-year-old man has episodes of wheezing and shortness of breath two to three times per week. Approximately every 2 weeks he awakens at night due to cough and difficulties breathing. He reports having similar symptoms since he was a child, but believes that they are worsening somewhat now. His symptoms are worsened by cold air and exercise and are improved by rest. Which of the following is the most appropriate treatment?
Daily high-dose inhaled corticosteroid and β-agonist when needed
Daily high-dose inhaled corticosteroid with oral steroids for exacerbations and short-acting β-agonist when needed
Daily low-dose inhaled corticosteroid and short-acting β-agonist when needed
Daily oral steroids and long-acting β-agonist
Short-acting β-agonist when needed
A 44-year-old woman has been complaining of a 4-year history of increasing dyspnea and fatigue. Physical examination reveals increased JVP and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests show a slight restrictive pattern. A diagnosis of primary pulmonary hypertension is made. Which of the following is the most likely cause of death in this condition?
Intractable left ventricular failure
Intractable respiratory failure
Massive PE
Intractable right ventricular failure or sudden death
Myocardial infarction
A 63-year-old woman presents with dyspnea and coughing up foul smelling purulent sputum. She has had many similar episodes in the past. There are no other constitutional symptoms and she denies excessive alcohol intake. On physical examination, she appears chronically ill with clubbing of the fingers. Heart sounds are normal, JVP is measured at 4 cm, and there are inspiratory crackles heard at the lung bases posteriorly. There is no hepatosplenomegaly or any palpable lymph nodes. CXR shows scaring in the left lower lobe, which on chest CT scan is identified as cystic changes with airway dilatation and bronchial wall thickening. Which of the following is the most appropriate initial next step in management?
Antibiotics and postural drainage
Steroids
Radiotherapy
Aerosols
INH
A 65-year-old smoker previously diagnosed with chronic obstructive pulmonary disease presents to the emergency department complaining of worsening cough and sputum production. She reports feeling breathless when climbing the stairs to her first floor walk-up apartment, and has moderate difficulty in providing her history in complete sentences. X-ray of the chest shows hyper inflated lungs with flattened diaphragms, attenuated vascular markings, and a narrow mediastinum. What agent(s) will provide the greatest relief of symptoms in the emergency department?
Albuterol and ipratropium bromide
Antibiotics
Magnesium sulfate
N-acetylcysteine
Theophylline
A 75-year-old man develops increased ventilatory requirements several days after requiring intubation for respiratory failure. X-ray of the chest shows bilateral infiltrates, and based on his ventilatory settings, the ratio of the partial arterial pressure of oxygen to the fraction of inspired oxygen (PaO2:FiO2) is 190. Which of the following is the most common underlying etiology of acute respiratory distress syndrome?
Aspiration of gastric content
Drug overdose
Lung or bone marrow transplantation
Massive blood transfusion
Sepsis
After an uncomplicated pregnancy and cesarean section for breech presentation, twins are born at 32 weeks’ gestation to a 24-year-old primigravida mother. Twin A weighs 1610 g (3.5 lb) and has Apgar scores of 8 and 9 at 1 and 5 minutes, respectively. Twin B weighs 1600 g (3.5 lb) and has Apgar scores of 7 and 8 at 1 and 5 minutes, respectively. Within minutes of birth, twin B becomes mildly cyanotic and tachypneic with subcostal retractions, expiratory grunting, and nasal flaring. Twin B’s blood pressure is 58/39 mm Hg, heart rate is 130/min, respiratory rate is 100/min, and temperature is 37.0°C (98.6°F). Twin B is intubated and given 70% fraction of inspired oxygen. Compared to twin A, what is twin B at greater risk of developing?
Apnea of prematurity
Gastroesophageal reflux disease
Hyperbilirubinemia
No difference because they are both pre- mature
Retinopathy of prematurity
A 32-year-old white man with HIV and a re- cent CD4+ cell count of 400/mm³ presents to the emergency department with a 3-day history of fever, anorexia, cough, and night sweats. He recently returned from a camping vacation in Arizona, approximately 1 month prior to presentation. He also describes diffuse joint pains. His temperature is 38.9°C (102°F), oxygen saturation is 99% on room air, and there is a rash on his arms and hands. There is dullness to percussion at the right lung base. X-ray of the chest reveals a small right-sided infiltrate and hilar lymphadenopathy. Sputum analysis does not reveal any organisms. He reportedly had a negative purified protein derivative test 2 months ago. Which of the following is the most likely diagnosis?
Coccidioidomycosis
Histoplasmosis
Lung carcinoma
Pneumocystis jiroveci pneumonia
Sarcoidosis
A 55-year-old man was admitted to the hospital 2 weeks ago for rapid onset of cough, fatigue, and pleuritic chest pain. He has worked as a sandblaster for the past year. When first seen in the hospital, he denied hemoptysis and smoking. Currently, the patient is intubated and on assist-control ventilation. His temperature is 36.7°C (98°F), pulse is 96/min, blood pressure is 138/85 mm Hg, and respiratory rate is 18/ min. A recent arterial blood gas study showed a pH 7.42, arterial carbon dioxide pressure of 36 mm Hg, and arterial oxygen pressure of 110 mm Hg while on 100% oxygen. Physical examination is significant for diffuse crackles throughout both lung fields, a loud pulmonic component of the second heart sound, and jugular venous distention of 9 cm with a prominent A wave, a left parasternal heave, and symmetric 3+ lower extremity pitting edema. Which of the following is the most likely diagnosis?
Asbestosis
Berylliosis
Byssinosis
Coal worker’s pneumoconiosis
Silicosis
A 32-year-old man develops symptoms of wheezing, cough, and shortness of breath. He has bilateral expiratory wheezes, and the rest of the examination is normal. Further evaluation with pulmonary function tests reveals a reduced FEV1/FVC ratio that corrects with bronchodilators. Which of the following statements about a diagnosis of idiosyncratic asthma (also called nonatopic) is correct?
Known antigenic stimulus
Adult onset
History of atopy
Positive skin tests
High immunoglobulin E (IgE) levels
A 28-year-old man presents with coughing up blood and sputum. He gives a history of recur- rent pneumonias and a chronic cough productive of foul-smelling purulent sputum. He has no other past medical history and is a lifetime nonsmoker. On physical examination, there are no oral lesions, heart sounds are normal, and wet inspiratory crackles are heard at the lung bases posteriorly. He also has clubbing of his fingers, but there is no hepatosplenomegaly or any palpable lymph nodes. CXR show fibrosis and pulmonary infiltrates in the right lower lung. Which of the following is the most appropriate initial diagnostic test?
Chest CT scan
Bronchoscopy
Bronchography
Open thoracotomy
Bronchoalveolar lavage

A 25-year-old man is recovering in the hospital from an open repair of his broken femur, which he suffered during an automobile accident. On postoperative day 3 he develops sudden onset shortness of breath and vague chest discomfort. His temperature is 37.6°C (99.6°F), heart rate is 108/min, blood pressure is 95/62 mm Hg, respiratory rate is 42/min, and oxygen saturation is 89% on room air. Physical examination is significant for jugular venous distention to 9 cm and an accentuated pulmonic component of S2. A pulmonary angiogram is shown in the image. Which of the following is most likely to be decreased?
Airway resistance
Alveolar dead space
Alveolar ventilation
Pulmonary compliance
Pulmonary vascular resistance
A 51-year-old man presenting to the clinic for routine examination mentions that he has not been able to get over the flu. Further questioning clarifies that he has had a nonproductive cough for the past 3–4 months and is unable to sustain his normal walking pace for prolonged periods. He reports feeling more fatigued than he recalls feeling last year. His medical history is significant for hypertension, alcoholism, and obesity. His blood pressure is well controlled on losartan and hydrochlorothiazide. He has no known drug allergies. His mother died of complications of type 2 diabetes mellitus. His father had a fatal myocardial infarction at age 56 years. The patient smokes half a pack of cigarettes per day and has done so for the past 7 years. He has worked all his adult life as an accountant and has no known exposures to asbestos or organic dusts. His blood pressure is 134/96 mm Hg, heart rate is 78/min, respiratory rate is 16/min, temperature is 37°C (98.6°F), and oxygen saturation is 94% on room air. Lung examination reveals bilateral inspiratory crackles in the lung bases. High-resolution CT shows patchy areas of ground glass, reticular abnormalities, and traction bronchiectasis. Laboratory findings are normal except for an elevated erythrocyte sedimentation rate of 54 mm/hr. What is the recommended treatment for this patient’s cough?
Change the antihypertensive agent
Prescribe amantadine
Prescribe bronchodilators and long-term domiciliary oxygen therapy
Prescribe glucocorticoids
Resect diseased lung fields
A 30-year-old woman presents to her physician’s office because of 3 months of nonproductive cough, exertional dyspnea, fatigue, malaise, and blurred vision. She denies weight loss, fever, chills, sweats, recent travel, or sick contacts. She works on the assembly line of an electronics plant. Vital signs are unremarkable. Physical examination reveals she has tender red papules over her shins. The patient said she first noticed the bumps when she changed oral contraceptive pills (her only medication), but assumed they would disappear. X-ray of the chest shows bilateral hilar lymphadenopathy with pulmonary infiltrates. Laboratory findings are: WBC count: 5600/mm3 Hemoglobin: 14.3 g/dL Platelet count: 300,000/mm3 Na+: 140 mEq/L K+: 4.2 mEq/L Cl−: 108 mEq/L Ca2+: 16 mg/dL CO2: 24 mmol/L Blood urea nitrogen: 10 mg/dL Creatinine: 1.0 mg/dL Culture of bronchoalveolar lavage fluid is neg- ative. Which of the following is the most likely diagnosis?
Berylliosis
Fungal infection
Lymphoma
Sarcoidosis
Tuberculosis
A 38-year-old woman has been complaining of a 2-year history of increasing dyspnea and fatigue. Physical examination reveals increased JVP and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests show a slight restrictive pattern. Primary pulmonary hypertension is diagnosed. Which of the following treatments is helpful in this condition?
Corticosteroids
Nitrates
Alpha-adrenergic blockers
Calcium channel blockers
Angiotensin-converting enzyme (ACE) inhibitors
A 5-year old girl is brought to the emergency department in December by her mother, who complains that her daughter seems confused. The mother reports that her daughter has complained of intermittent headaches since the two of them moved into the first floor of an older apartment building 6 months ago. The mother has been at home with the daughter for the past 24 hours and the girl appears lethargic and is complaining of joint aches, nausea, and a headache. Her pulse is 120/min, blood pressure is 130/85 mm Hg, respiratory rate is 25/min, and oxygen saturation is 100% on room air. The girl’s mother also notes having a slight headache that started yesterday. Which of the following diagnostic tests should be most rapidly pursued?
Arterial blood gas
CT scan of the head
Direct laryngoscopy
ECG
Toxicology screen
A 1-year-old child with cerebral palsy secondary to perinatal asphyxia presents to her general pediatrician for a well-child visit. She was delivered at 37 weeks’ gestation by emergency cesarean section for a tight nuchal chord. The patient has severe spastic quadriparesis that is limiting her movements. She also has mental retardation and is unable to speak. She has received physical and occupational therapy since early infancy; however, her parents are concerned by her lack of improvement. Which of the following is the best choice for treatment of spasticity in this child?
Baclofen
Botulinum toxin
Carbamazepine
Discontinue physical therapy
Hyperbaric oxygen
A 58-year-old man presents to the emergency department complaining of fever and chills. The fever started last night and has not sub- sided, even though he took acetaminophen. He had a successful appendectomy 3 days ago and was discharged from the hospital 2 days ago. His only medication is ibuprofen, which is adequately controlling his pain. He is a 30-pack-year smoker with a chronic cough productive of white sputum. He has noticed increased sputum production, which has become yellowish-green. He denies dysuria, urgency, or frequency. His temperature is 38.4°C (101.1°F), heart rate is 88/min, respiratory rate is 16/min, and blood pressure is 126/74 mm Hg. On examination he appears to be tired but not in acute distress. Pulmonary examination is limited be- cause deep inhalation causes coughing and slight abdominal pain. There is no tactile fremitus or dullness to percussion. He has a slightly erythematous, appropriately tender healing incision in the right lower quadrant without exudates and normal active bowel sounds. Extremities are warm and well perfused without erythema or edema. Pulses are intact. Which of the following most likely could have prevented this condition?
Aggressive incentive spirometry
Early removal of the Foley catheter
Early removal of the intravenous catheter
Pre- and postoperative antibiotic prophylaxis
Use of compression stockings and subcutaneous heparin
A 64-year-old woman is admitted to the hospital with right lobar pneumonia and sepsis syndrome. She becomes progressively more short of breath and hypoxemic requiring intubation and mechanical ventilation. Her repeat CXR in the intensive care unit now shows diffuse pulmonary infiltrates and a diagnosis of acute respiratory distress syndrome (ARDS) is made. Which of the following mechanisms is the most likely cause for the early exudative phase of ARDS?
Increased lung compliance
Increased interstitial fibrosis
Increased vascular permeability to fluid and proteins
Decreased pulmonary perfusion
Decreased ventilatory dead space

A 24-year-old African American woman presents with mild dyspnea on exertion, fever, and a rash on her legs. Her symptoms have come on gradually and she reports no pleuritic chest pain, hemoptysis or sputum production. She has no significant past medical history, smokes 10 cigarettes/day and is not taking any medications. Physical examination reveals generalized lymphadenopathy and tender erythematous nodules on her legs. CXR shows bilateral symmetric hilar adenopathy and reticulonodular changes in both lungs. She has a restrictive lung disease pattern on pulmonary function testing. Which of the following is the most likely diagnosis?
Hodgkin’s disease
Tuberculosis
Rheumatic fever
Sarcoidosis
Rheumatoid arthritis (RA)
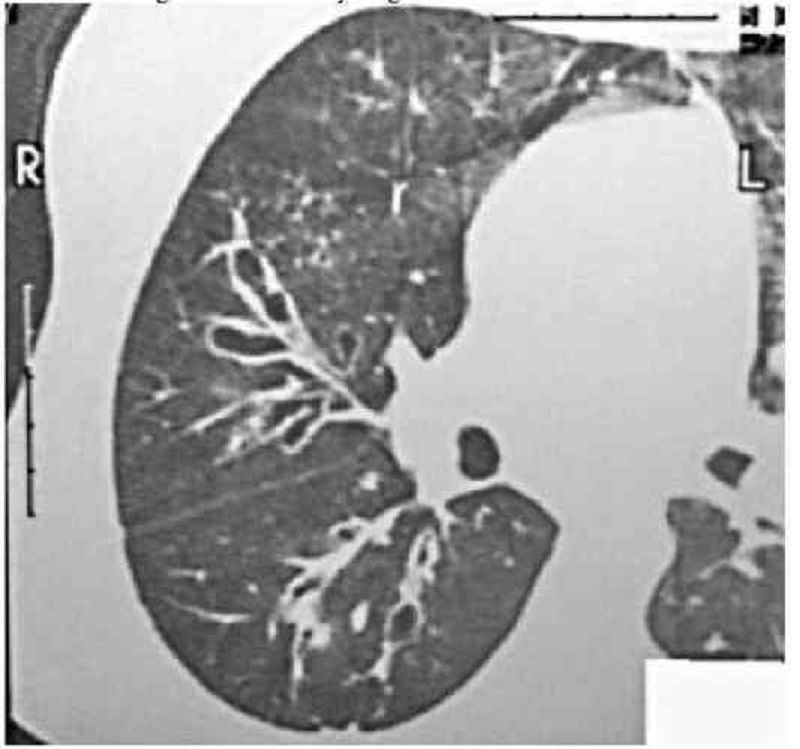
A 30-year-old man presents with coughing up blood and sputum. There is no associated dyspnea, fever, or pleuritic chest pain. His past medical history is significant for recurrent pneumonias and a chronic cough productive of foul-smelling purulent sputum. The sputum production is usually worse when lying down and in the morning. He quit smoking 5 years ago and started when he was 18 years old. On physical examination, he appears chronically ill with clubbing of the fingers. Wet inspiratory crackles are heard at the lung bases posteriorly. CXR shows scaring in the right lower lobe, which on chest CT scan is identified as airway dilatation, bronchial wall thickening, and grapelike cysts. Which of the following is the most likely diagnosis? (A)
Bronchiectasis
Chronic bronchitis
Disseminated pulmonary tuberculosis
Pulmonary neoplasm
Chronic obstructive emphysema
A 23-year-old man is experiencing a flare of his asthma. He is using his salbutamol inhaler more frequently than usual and despite increasing his inhaled steroids he is still short of breath. Previously his asthma was considered mild with no severe exacerbations requiring oral steroids or hospitalization. With his flare, he has recurrent episodes of bronchial obstruction, fever, malaise, and expectoration of brownish mucous plugs. On examination, there is bilateral wheezing. The heart, abdomen, neurologic, and skin exams are normal. CXR reveals upper lobe pulmonary infiltrates; the eosinophil count is 3000/mL, and serum precipitating antibodies to Aspergillus are positive. Which of the following is the most likely diagnosis?
Ascaris infestation
Allergic bronchopulmonary aspergillosis
Churg-Strauss allergic granulomatosis
Löeffler’s syndrome
Hypereosinophilic syndrome
A 34-year-old African American man presents with mild dyspnea on exertion and joint discomfort in his knees, wrists, and ankles. He also has a fever and red tender rash on his shins. Physical examination reveals hepatosplenomegaly, generalized lymphadenopathy, and tender erythematous nodules on his legs. CXR shows bilateral symmetric hilar adenopathy. Which of the following laboratory findings is not characteristic of this condition?
Hyperglobulinemia
Elevated ACE level
Elevated sedimentation rate (ESR)
Elevated serum calcium
Normal gallium scan
A 66-year-old man has progressive shortness of breath due to COPD. He is currently able to do his activities of daily living, but has trouble walking more than one block. His physical examination reveals hyperinflation, increased resonance to percussion, and bilateral expiratory wheezes. He is on appropriate medical therapy for his stage of COPD. Which of the following is also indicated in the management of this condition?
Meningococcal vaccination
Yearly influenza vaccination
Weight reduction if obese
Haemophilus influenzae B vaccination
Pneumococcal vaccination
A 55-year-old woman presents with coughing up blood and sputum. She gives a history of recurrent pneumonias and a chronic cough productive of foul-smelling purulent sputum. The sputum production is worse on lying down and in the morning. On physical examination, she appears chronically ill with clubbing of the fingers. Wet inspiratory crackles are heard at the lung bases posteriorly. There are no hepatosplenomegaly or any palpable lymph nodes. CXR shows scaring in the right lower lobe, which on chest CT scan is identified as airway dilatation, bronchial wall thickening, and grapelike cysts. Which of the following is a recognized precursor to this patient’s condition?
Bronchial asthma
Cigarette smoking
Lung infection and impairment of drainage
Lung cancer
Silicosis
A 50-year-old man presents with excessive day- time sleepiness and a history of snoring. One week ago, he fell asleep while driving his car and got into a minor accident. On examination, he is obese (body mass index [BMI] >30) and his blood pressure is 160/90 mm Hg. His lungs are clear and heart sounds are distant. Which of the following is the most likely explanation for the symptoms associated with this condition?
Related to cardiac dysfunction
Neuropsychiatric and behavi
Pulmonary
Gastrointestinal (GI)
Musculoskeletal
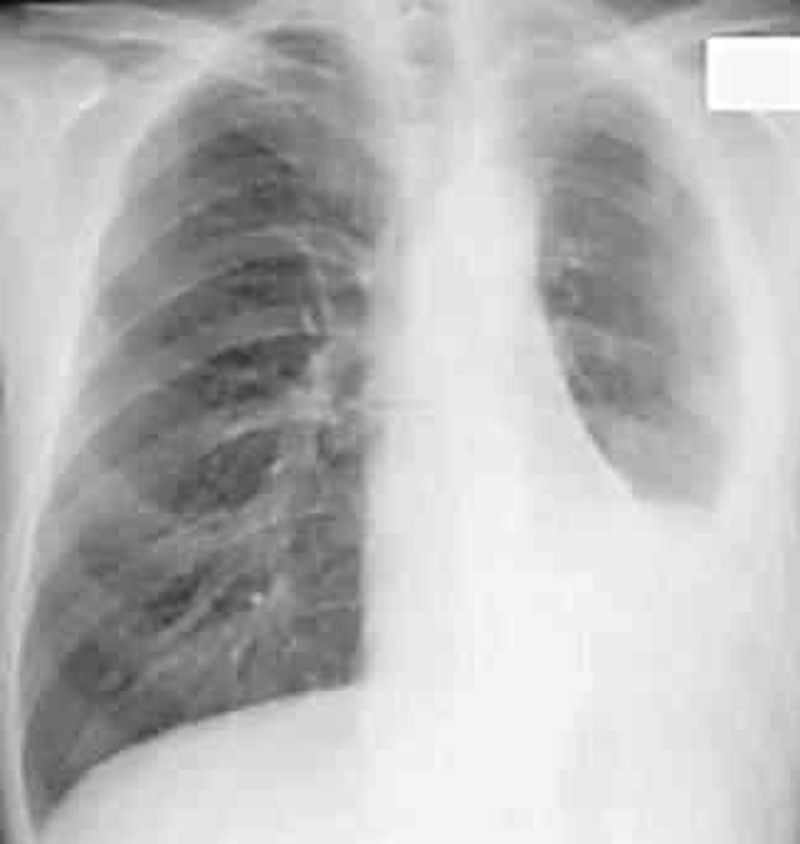
A 58-year-old steam pipe worker presents with a vague ache in the left chest and mild dyspnea of several months’ duration. There is dullness on percussion of the left chest associated with diminished breath sounds. His CXR is shown in Fig. Which of the following is the most likely diagnosis?
Pleural metastases
Paget’s disease
Mesothelioma and asbestosis
Pleural effusion
Multiple myeloma
A 23-year-old man presents with coughing up blood and sputum. He gives a history of recurrent pneumonias and a chronic cough productive of foul-smelling purulent sputum. The sputum production is worse when lying down and in the morning. On physical examination, he appears chronically ill with clubbing of the fingers. Wet inspiratory crackles are heard at the lung bases posteriorly. There are no hepatosplenomegaly or any palpable lymph nodes. CXR shows scaring in the right lower lobe, which on chest CT scan is identified as airway dilatation, bronchial wall thickening, and grapelike cysts. Which of the following is sometimes seen in this condition?
Lung cancer
Dextrocardia
Fungal infection
Carcinoid syndrome
Hodgkin’s disease
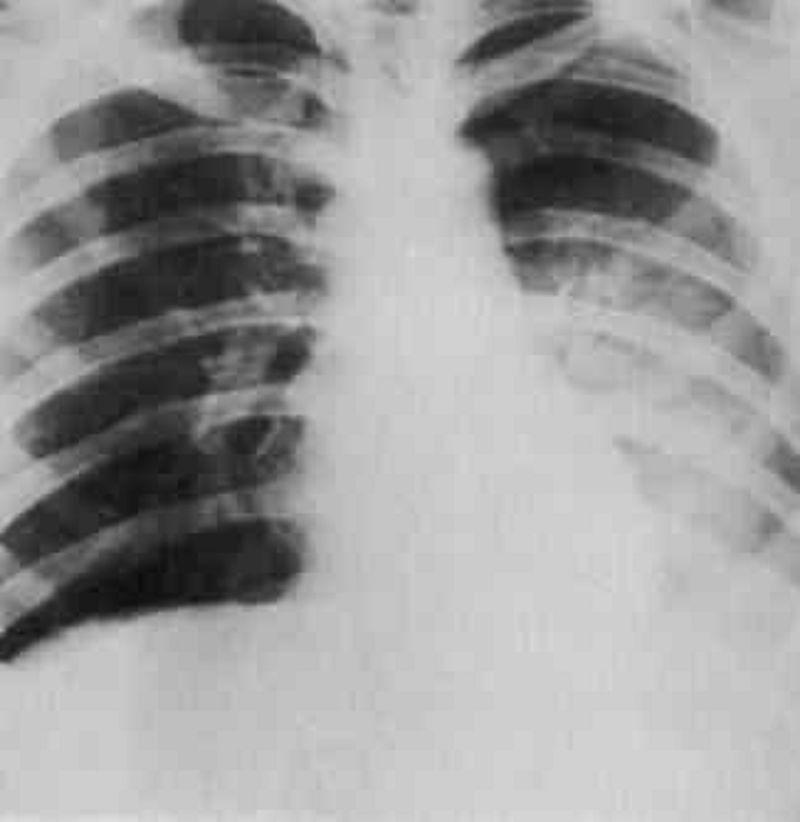
A 27-year-old man presents with chest pain and feeling unwell. He describes cough with blood-tinged sputum, chills, and fever of 2 days’ duration. Physical findings reveal dullness and moist rales in the left lower chest. His CXR is shown in Fig. Which of the following is the most likely diagnosis?
Pneumonia, left lower lobe
Atelectasis, left lower lobe
PE
Tuberculosis
Sarcoidosis

A 40-year-old man is seen for an insurance assessment. He has no past medical history and feels well. His compete physical examination is normal. His biochemistry, complete blood count (CBC), ECG, and urinalysis are also normal. His CXR is abnormal and presented in Fig. Which of the following is the most likely diagnosis?
Hamartoma of the lung
Tuberculous granuloma of the left apex
Osteochondroma of the left 4th rib
Bronchogenic carcinoma
Pulmonary metastases
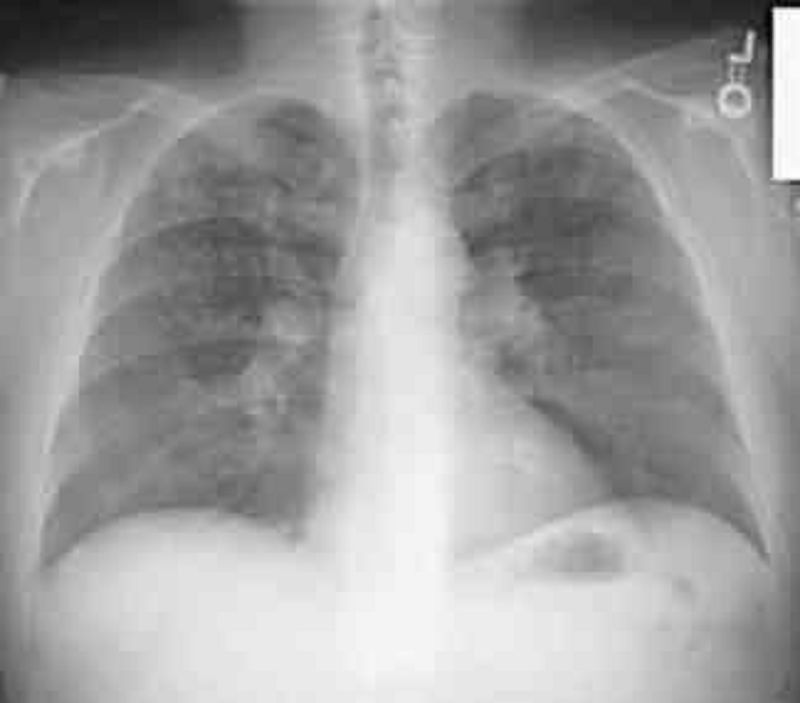
A 21-year-old man has a nonproductive cough, shortness of breath, and chest pain, which changes with breathing. He also has pain in the left arm. On examination, there is tenderness over the left shoulder, heart sounds are normal, and the lungs are clear. CXR reveals a lytic lesion in the left humerus and reticulonodular opacities in the upper and middles lobes. The eosinophil count is normal. Which of the following is the most appropriate initial diagnostic test?
Lung biopsy
Humerus bone biopsy
CT scan of chest
Bronchoscopy
Pulmonary function tests
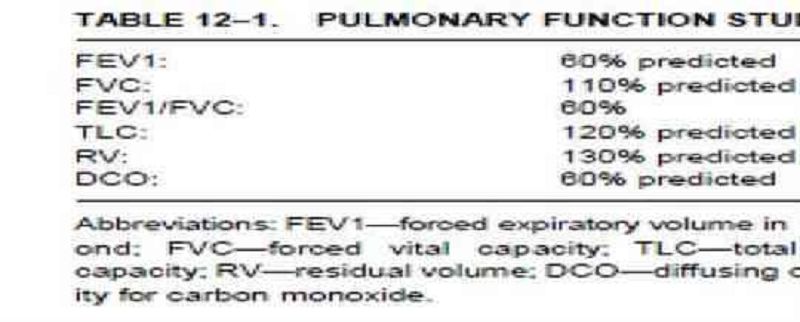
The pulmonary function studies shown in Table 12–1 are of a 65-year-old man with severe dyspnea and cough. Which of the following is the most likely diagnosis?
Emphysema
Lobar pneumonia
Chronic bronchitis
Acute bronchitis
CHF
A 33-year-old woman, otherwise perfectly well, presents with recurrent episodes of hemopty- sis. She has no fever, weight loss, cough, or sputum production. Her physical examination is entirely normal. Her CXR, biochemisty, CBC, and coagulation profile are also normal. Which of the following is the most appropriate initial diagnostic test?
Echocardiogram
Gallium scan
CT scan of chest
Bronchoscopy
Pulmonary function tests
A 34-year-old woman is complaining of progressive and worsening shortness of breath. Her symptoms first started 3 years ago, and she now gets dyspneic and fatigued while doing her activities of daily living. Her past medical history is not significant and she not taking any medications. Physical examination reveals increased JVP and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests are normal. Which of the following is the most likely diagnosis?
Asthma (without wheezing)
Primary pulmonary hypertension
Pulmonary veno-occlusive disease
Pulmonary leiomyomatosis
Silent tricuspid valve disease
A 45-year-old woman has severe symptoms of epigastric and abdominal pain after eating. A trial of acid suppression therapy with proton pump inhibitors (PPI) only partially improved her symptoms. She undergoes elective outpatient upper endoscopy, which is positive for a small duodenal ulcer. Two hours later, she is short of breath and complaining of severe anterior chest pain, which is made worse with deep inspiration. On examination, she looks unwell, blood pressure is 150/90 mm Hg, pulse 110/min, and lungs are clear. Heart sounds are normal but an “extra crunching” type sound is intermittently heard. CXR demonstrates air surrounding the heart. Which of the following is the most likely diagnosis?
Acute pericarditis
Acute cardiac ischemia
Acute mediastinitis
Aortic dissection
Pneumothorax
A 55-year-old woman is in the intensive care unit on a ventilator for hypoxemia following “flash” pulmonary edema. Her PO2 on the blood gas prior to intubation was 44 mm Hg, and now while breathing 100% oxygen on the ventilator her repeat blood gas reveals a PO2 of 80 mm Hg. Hypoxemia while receiving 100% oxygen indicates which of the following problems?
Ventilation-perfusion ratio inequality
Right-to-left shunt
Hypoventilation
Impaired diffusion
Interstitial lung disease
A 31-year-old man with severe kyphoscoliosis due to cerebral palsy is experiencing worsening shortness of breath with exertion. On examination, he has a severe scoliosis to the left and decreased air entry to that side. His right lung is clear, JVP is 3 cm, and heart sounds are normal. Pulmonary function tests are performed. Which of the following is the most likely abnormality to be seen on the pulmonary function tests?
Increased total lung capacity (TLC)
Increased functional residual capacity (FRC)
Decreased TLC
Increased compliance
Increased vital capacity (VC)
A 52-year-old man develops sudden-onset shortness of breath on postoperative day 4 after a hemicolectomy for colon cancer. His surgery went well with no operative complications. He reports no cough, sputum, or pleuritic chest pain. His blood pressure is 155/90 mm Hg, pulse 100/min, temperature 37.8°C, lungs are clear, and heart sounds normal. He has bilateral pedal edema, but no discomfort in his legs. His CXR and ECG are normal. A chest CT with contrast reveals a thrombus in his right upper lobe artery. Which of the following statements concerning the management of this condition is most likely correct?
Continuous IV heparin or subcutaneous low-molecular-weight heparin (LMWH) therapy is indicated
Urgent thrombolytic therapy is indicated
Urgent inferior vena cava (IVC)
Filter insertion is indicated
Confirmation of the diagnosis with bilateral ultrasound leg Dopplers
An 83-year-old man with Parkinson’s disease presents with low-grade fever and cough for several weeks. Lately, he has been experiencing more rigidity and difficulty with his walking. He is on a levodopa/carbidopa combination for treatment for the past 5 years. On examination, his gait is shuffling and slow. He has a tremor in his left hand at rest, and there is cogwheel rigidity of the forearm. There are crackles in the left lower lung field. CXR reveals a lung abscess in the left lower lobe. Which of the following is the most likely bacteriologic diagnosis for the lung abscess?
Tuberculosis
Oropharyngeal flora
Pseudomonas aeruginosa
Staphylococcus aureus
Candida albicans
A 31-year-old G4P3 woman gave birth via re- peat cesarean section to a full-term, 3700-gm (8.2-lb) baby girl. There were no complications during the pregnancy or delivery. Two hours after the birth the resident is called to evaluate the baby girl. She is afebrile but is breathing rapidly with mild subcostal retractions. Breath sounds are equal and clear bilaterally. S1 and S2 are normal and the point of maximal intensity is not displaced. X-ray of the chest reveals flattened diaphragms, prominent vascular markings, and fluid lines in the fissures. Which of the following is the most likely diagnosis?
Diaphragmatic hernia
Neonatal respiratory distress syndrome
Pulmonary hemorrhage
Pulmonary interstitial emphysema
Transient tachypnea of the newborn
A 67-year-old man presents to his primary care physician with complaints of dyspnea on exertion over the past 6 months that has progressively worsened to dyspnea at rest. He denies cough and wheezing and has had no fevers, night sweats, or unintentional weight loss. The man has never smoked and worked as a ship-builder for >30 years. Which of the following findings on x-ray of the chest would confirm the most likely diagnosis?
Bilateral diffuse infiltrates
Bilateral hilar adenopathy
Consolidation of lung tissue
Focal mass with air bronchograms
Multiple pleural plaques with patchy parenchymal opacities
A 23-year-old man is seen in the emergency department for sudden onset, right-sided pleuritic chest pain that developed 30 minutes ago while he was watching television. The patient also complains of difficulty breathing. He has no prior medical history, denies smoking and intravenous drug use, and does not take any medications. His temperature is 37.3°C (99.1°F), blood pressure is 130/82 mm Hg, pulse is 92/ min and regular, respiratory rate is 20/min and shallow, and oxygen saturation is 98% on room air. His body mass index is 18 kg/m². Diminished breath sounds, hyperresonance, and decreased tactile fremitus are prominent in the right lung field. The trachea is midline. X-ray of the chest shows a 10% pneumothorax on the right. Which of the following is the most appropriate initial management?
Needle decompression
Observation with supplemental oxygen
Open thoracotomy with oversewing of the pleural blebs and scarification of the pleura
Thoracoscopy with stapling of blebs
Tube thoracostomy with doxycycline pleurodesis
A 28-year-old African American woman presents with mild dyspnea on exertion. She reports no coughing, sputum production, or wheezing symptoms, but has noticed a red tender rash on her shins. Physical examination reveals hepatosplenomegaly, generalized lymphadenopathy, and tender erythematous nodules on her legs. CXR shows bilateral symmetric hilar adenopathy. Her pulmonary function tests reveal a mild restrictive pattern. Which of the following tests will most likely make a definitive diagnosis?
Tuberculin skin test
Bronchoscopy with transbronchial biopsy
Elevated ACE level
Serum hypercalcemia
Increased uptake on gallium scan
69-year-old woman has recently returned on an overnight flight from Europe. She now complains of vague chest discomfort and shortness of breath. On examination, she is comfortable, blood pressure 130/80 mm Hg, pulse 90/min, respirations 18/min, and oxygen saturation 97%. Her heart and lungs are normal on auscultation, and there is no edema or leg tenderness on palpation. A quantitative (ELISA) D-dimer assay is positive. Which of the following statements regarding the D-dimer assay is correct?
It is sensitive but not specific
It is specific but not sensitive
It is neither specific nor sensitive
A negative result suggests myocardial ischem
It is both sensitive and specific
{"name":"USMLE PART3.2(PNEUMO)", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 67-year-old male presents with a one-month history of dyspnea on exertion and chest pain. He denies hemoptysis, cough, fever, night sweats or weight loss. His past medical history is significant for hypertension and chronic obstructive pulmonary disease. He has a 48 pack-year smoking history but quit six years ago. He works as a salesman. On physical examination, the patient has a temperature of 38.2C (100.8.F), blood pressure of 128\/72 mm Hg, pulse of 92\/minute, and respirations of 20 breaths\/minute. His complete blood count, chemistry panel, and hepatic function tests are all within normal limits. A chest x-ray and computed tomography scan of the chest reveal a right-sided pleural effusion and calcified nodules in both upper lobes. The patient undergoes thoracentesis. Characteristics of the pleural fluid are given below: Total protein 5.2 g\/dl Glucose 83 mg\/dl Adenosine deaminase 98.5 U\/L Cytologic examination reveals 600 white blood cells\/mm3, 1% macrophages and 99% leukocytes. Of the leukocytes, 45% are neutrophils, 50% are lymphocytes, and 5% are monocytes, with no basophils or eosinophils. No neoplastic cells are found. Which of the following is the most likely mechanism underlying development of this pleural effusion?, A 33-year-old white female complains of repeated episodes of fever, malaise, chills, breathlessness and dry cough over the past 6 months. She says that each episode starts suddenly and lasts for several days. She otherwise has no significant past medical history and does not take any medications. There is no family history of lung disorders. She does not smoke cigarettes or drink alcohol. She has never been abroad, and has had no sick contacts. She breeds budgerigars (a small Australian parrot) as a hobby. Chest x-ray shows diffuse generalized haziness in both lower lung fields. Pulmonary function tests reveal reduced lung volumes and an FEV1\/FVC ratio of 87%. PPD test is negative. Serology shows antibodies to budgerigar antigens. What is the best treatment for this disease?, A 43-year-old man presents to your office complaint of nagging left-side chest pain that increases on deep inspiration, plus two weeks of non-productive cough. He denies chills, fever or weight loss. His medical history is significant for Hodgkin's disease treated 20 years ago with chemotherapy and radiation therapy. On physical examination today, his blood pressure is 140\/90 mmHg and his heart rate is 90\/min. His chest x-ray is shown below. Which of the following is the most likely cause of his chest pain?","img":"https://cdn.poll-maker.com/10-459608/11.bmp?sz=1200"}
More Quizzes
SAB KHELO SAB JITO
320
Maths Quiz 1
4220
World Cup Quiz
210
UNDIAN PERCALONAN JAWATANKUASA BADAN KELUARGA SEKOLAH RENDAH ISLAM INDERA MAHKOTA (BAKA)
5234
Queen - Test Your Rock Royalty Knowledge
201026928
CHP School Bus Practice Test - Free Questions
201021000
Which Massage Movement Uses Light, Gliding Strokes?
201027869
Adverb - Free English Grammar Practice
201018472
Emo or Preppy - Discover Your Style Type (Free)
201020311
Alien Movie Trivia - How Well Do You Know Aliens?
201018911
George & Cecilius Calvert APUSH - Maryland Colony
201018821
SparkNotes Persepolis - Free Comprehension Check
201024518