Pediatric USMLE 101 - 200

Pediatric USMLE 101 - 200 Quiz
Test your knowledge on pediatric medicine with our comprehensive 100-question quiz tailored for aspiring medical professionals preparing for the USMLE. This engaging quiz covers a wide range of topics, ensuring that you understand the nuances of pediatric care.
Key Features:
- 100 carefully crafted questions
- Multiple choice format
- Focus on clinical scenarios and pediatric principles
101. A child is brought to the physician for a routine visit. On examination, the child can name multiple items in the examination room, and can also combine 2 words into a short sentence. His mother estimates that he knows about 200 words. When his mother tries to help him onto the examination table, he says "me do it." Although his mother seems to understand most of what he says, you can only understand about half of his speech. Which of the following is the most likely age of this child?
A 12 months
B. 15 months
C. 18 months
D. 24 months
E. 36 months
102. A one-month-old child is brought to the office due to persistent vomiting for the last six days. His mother complains of increasing episodes of projectile vomiting. These episodes occur every time she attempts to feed him, and have persisted despite changing formulas. On physical examination, peristaltic waves are seen over the upper abdomen, and an olive-sized mass is palpated. Laboratory studies reveal a potassium level of 3 mEq/mL. What is the most appropriate management for this patient?
A. Immediate surgery
B. Medical treatment with metoclopramide
C. Surgery before school age
D. Intravenous hydration and potassium replacement
E. Avoid milk products
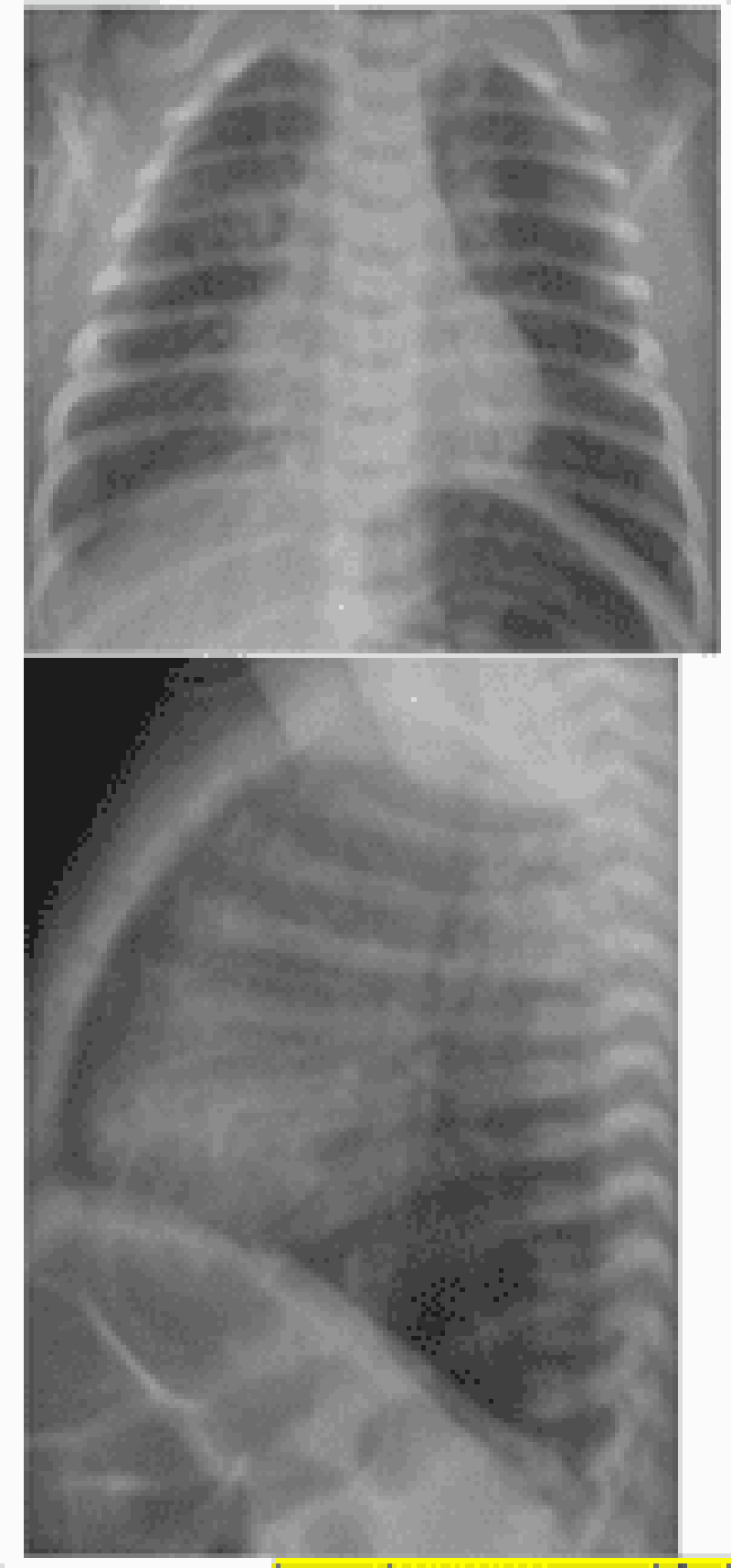
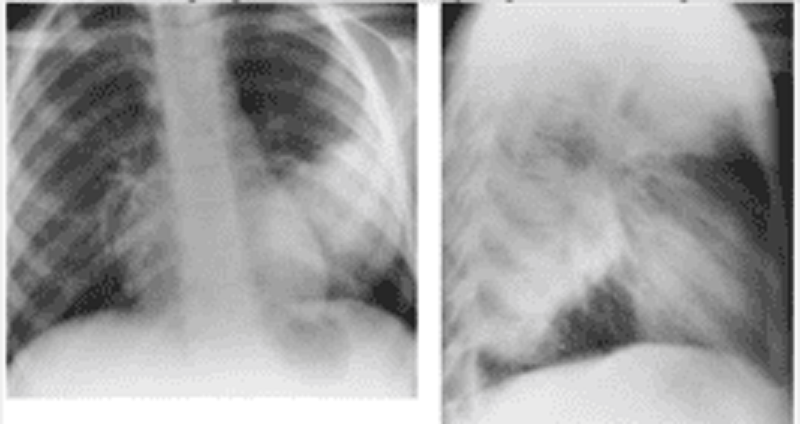
103. Coughing for 2 days. Two other members of the family had similar symptoms. Four hours ago, his cough became much worse. On physical examination, he is in moderate respiratory distress with nasal flaring, hyper- expansion of the chest, and easily audible wheezing without rales. His chest radiographs are shown. Which of the following is the appropriate next course of action?
A. Monitoring oxygenation and fluid status alone
B. Inhaled epinephrine and a single dose of steroids
C. Acute-acting bronchodilators and a short course of oral steroids
D. Emergent intubation and antibiotics
E. Chest tube placement

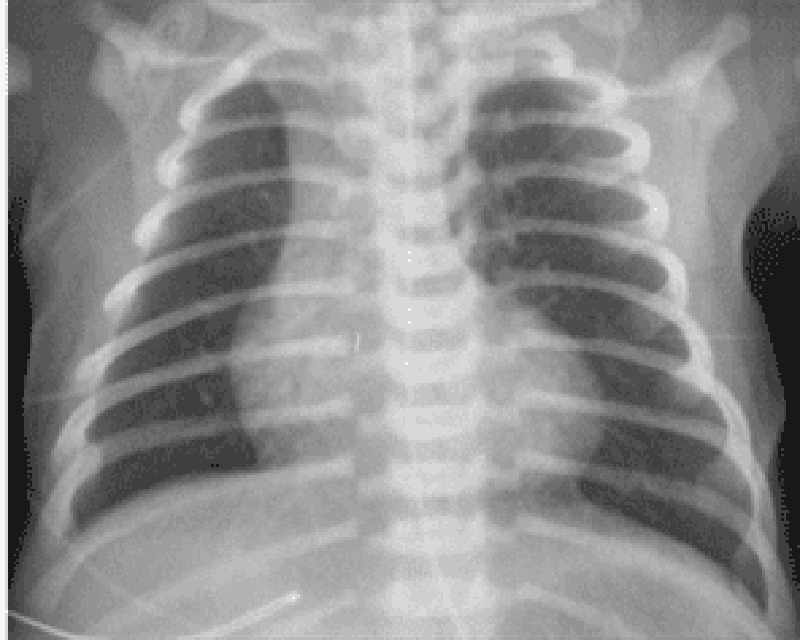
104. A 6-year-old girl presents with a 2-day history of cough and fever. At your office she has a temperature of 39.4°C (103°F), a respiratory rate of 45 breaths per minute, and decreased breath sounds on the left side. Her chest x-ray is shown below. Which of the following is the most appropriate initial treatment?
A. N-acetylcysteine chest physiotherapy
B. Vancomycin
C. Partial lobectomy
D. Postural drainage
E. Placement of tuberculosis skin test
105. A 2-year-old girl is playing in the garage with her Chihuahua, only par- tially supervised by her father, who is weed-whacking around the garden gnomes in the front yard. He finds her in the garage, gagging and vomiting. She smells of gasoline. In a few minutes she stops vomiting, but later that day she develops cough, tachypnea, and subcostal retractions. She is brought to your emergency center. Which of the following is the most appropriate first step in management?
A. Administer charcoal
B. Begin nasogastric lavage
C. Administer ipecac
D. Perform pulse oximetry and arterial blood gas
E. Administer gasoline-binding agent intravenously
106. A 3-day-old girl has trouble feeding and pulmonary congestion. The mother says that the infant is so busy breathing, that she literally has no time to suckle. The girl was bom at home, with the delivery attended by a midwife. Physical examination confirms that she is in respiratory distress and shows bounding peripheral pulses with a loud continuous precordial machinerylike murmur. X-ray films show increased pulmonary vascular markings. Shortly thereafter, the infant goes into overt heart failure. Which of the following would most likely be required to correct this problem?
(A) Indomethacin
(B) Digitalis and diuretics
(C) Emergency surgical closure of atrial septal defect
(D) Emergency surgical closure of ventricular septal defect
(E) Emergency surgical division of patent ductus arteriosus
107. A 12-year-old girl presents with a 2-month history of vaginal discharge. She describes it as clear and states that it stains her underwear. She says that she hates boys, and that "no way" has she ever had sex or even kissed a boy. She reports having had developing breasts for 2 years and thinks that her growth spurt was about a year ago. Genital findings include a pubic hair stage of Tanner III with no evidence of redness or irritation of the vulvovaginal area. A slight amount of odorless, clear mucus is seen. Microscopic examination of the mucus reveals epithelial cells and a few bacteria, but no white cells. The pH is between 3.5 and 4. Which of the following is the most appropriate next step in management?
(A) No treatment, but the girl should he reassessed in a few months
(B) Advise the girl to discontinue all bubble baths and wipe herself front to back after voiding
(C) Pelvic examination to obtain cultures for gonorrhea and Chlamydia
(D) Clotrimazole cream to be applied once a day for 10 days
(E) Sitz baths one or two times a day and 1% hydrocortisone cream applications once a day for a week
108. A 10-year-old girl is involved in a motor vehicle accident, sustaining multiple injuries to her head, arms, and abdomen. Her blood pressure is 90/60 mm Hg, and her pulse is 120/min. Her forearm is disfigured, and bone can be seen through the wound. She is breathing periodically and has cyanotic lips. Her abdomen is rigid, and there is flank discoloration. Which of the following is the most appropriate next step in management?
(A) Splint the arm and cover wound with sterile gauze
(B) Administer crystalloid solution
(C) Administer vasopressors immediately
(D) Administer packed red blood cells
(E) Perform exploratory laparotomy
109. An 18-year-old male undergoes elective hernia repair. During the operation, he suffers considerable blood loss, and receives a blood transfusion. He then experiences an anaphylactic transfusion reaction. He is resuscitated and further hospital course is uncomplicated. His past medical history is significant for recurrent sinopulmonary infections and intermittent episodes of diarrhea since childhood. Which of the following is the most likely cause of his symptoms?
A. lgA deficiency
B. DiGeorge Syndrome
C. X linked agammaglobulinemia
D. Wiskott-Aldrich syndrome
E. Cystic fibrosis
110. A 12-year-old boy is brought to the emergency department because of severe pain near his left knee. He has sickle cell disease and has been hospitalized previously for sickle cell crisis. Vital signs are notable for persistent fever. Examination of the left lower extremity reveals a normal knee joint with marked tenderness and swelling over the proximal tibia. Laboratory studies show leukocytosis and elevated ESR. Imaging studies confirm the diagnosis of osteomyelitis. Which of the following organisms is the most likely cause of his condition?
A. Escherichia coli
B. Pseudomonasspecies
C. Salmonella species
D. Streptococcus pneumoniae
E. Group B streptococcus
111. A 2-hour-old male neonate has developed worsening cyanosis over the past few minutes. The infant was vaginally delivered (assisted with forceps) at full term and weighed 4.1 kg (9 lb). The Apgar scores were 7 and 8 at 1 and 5 minutes, respectively. Oxygen is administered by mask but does not relieve the cyanosis. Further examination reveals tachypnea, subcostal retractions, a normal first heart sound, a single and loud second heart sound (S2), and no murmur. Which of the following is the most likely cause of the infant's cyanosis?
A. Transposition of the great vessels
B. Atrial septaI defect
C. Coarctation of the aorta
D. Ventricular septal defect
E. Patent ductus arteriosus
112. A 4-week-old infant is brought to the office due to several episodes of vomiting over the past week. The episodes have progressively become more frequent and forceful, but the vomitus never contains any blood or bile. The infant has been breastfed since birth. His vital signs are stable, and he is afebrile. An olive-shaped mass is palpated just to the right of the umbilicus, and peristaltic waves are seen in the upper abdomen. Lab studies reveal a sodium level of 135 mEq/L, potassium level of 3.3 mEq/L, chloride level of 92 mEq/L and bicarbonate level of 30 mEq/L. Which of the following is the most appropriate diagnostic test for this patient?
A. Abdominal ultrasound
B. Plain abdominal x-rays
C. Contrast radiography
D. Gastroduodenoscopy
E. CT scan of the abdomen
113. A one-year-old girl is brought to the office for the evaluation of sickle cell anemia. Both her parents have sickle cell trait, and her elder sister has sickle cell anemia. Her vital signs are stable. Her height and weight are appropriate for age. On examination, she appears healthy and normal. Her birth and past medical histories are insignificant. Hemoglobin electrophoresis reveals 40% hemoglobin S. What is the most common presentation of this condition?
A. Acute painful episodes
B. Painless hematuria
Splenic infarction
Dactylitis
Frequent UTI
114. A boy is brought to the office by his parents for a routine visit. During the physical examination, he can obey two-step commands, use two- to three-word phrases, and can build a tower of six blocks. According to his mother, he can walk up and down the stairs without help. What is the most likely age of this child?
A. 15 months
18 months
2 years
3 years
4 years
115. A 5 year old girl presents to the emergency department with acute onset of muscle weakness. The mother carried the girl to the examination room and states that the muscle weakness started in her daughter's legs yesterday. The weakness became worse today and progressed to the trunk and both arms. She was also complaining difficulty of breathing earlier today. She has been otherwise healthy but had a common cold about 10 days ago. On examination, her respirations are 26/min and shallow. She has profound muscle weakness in her lower extremities, and moderate weakness in her upper extremities. Her deep tendon reflexes are absent. A lumbar puncture is performed, which shows increased protein concentration but no pleocytosis. Which of the following is the most likely diagnosis?
A. Botulism
B. Dermatomyositis
C. Guillain-Barre̝ syndrome
D. Myasthenia gravis
E. Toxic neuropathy
116. A full-term infant is brought to the office on her 6th day of life because her mother noted that she looked "yellow". The mother states that the infant is strictly breast-fed and has been eating every 2-3 hours. On examination, she is noted to be jaundiced over her trunk and face. There is no scleral icterus. She is otherwise healthy. Both the mother and baby are Rh positive. Which of the following is the most likely cause of this infant's jaundice?
A. Breast-feeding jaundice
B. Glucose-6-phosphate dehydrogenase (G6PD) deficiency
C. Hypothyroidism
D. Physiologic jaundice
E. Rh incompatibility
117. A 4-year-old girl was diagnosed of left-side otitis media about 10 days ago and was prescribed oral amoxicillin, 40 mg/kg/day for 7 days. She has since developed bloody diarrhea with mucus, crampy abdominal pain, and fever. On physical examination, her temperature is 39.4 C (102.9 F), pulse is 88/min, and respirations are 16/min. She has normal bowel sounds and is diffusely tender to palpation. Which of the following is the most appropriate initial step in diagnosis?
A. Barium enema
B. Evaluation of stool for Clostridium difficile toxins
C. Evaluation of stool for rotavirus
D. Stool examination for ova and parasites
E. Stool Hemoccult test
118. A 5-year-old pedestrian is hit by a car in a mall parking lot and he is brought to the emergency department. There was loss of consciousness for less than 1 minute. On evaluation, the child has no neurologic deficits and a CT scan of the head reveals no intracranial abnormalities and no obvious skull fractures. The parents want to know what possible long-term problems there might be. You remember that problems after head trauma may include the development of seizures and that the risk of developing posttraumatic epilepsy is increased by which of the following?
(A) a brief loss of consciousness
(B) an acute intracranial hemorrhage
(C) retrograde amnesia
(D) posttraumatic vomiting
(E) a small linear skull fracture
119. A 4-year-old previously healthy but unimmunized boy presents with sudden onset of high fever, inspiratory stridor, and refusal to drink. Of the following causes of inspiratory stridor, which best fits this clinical scenario?
(A) epiglottitis
(B) vascular ring
(C) croup
(D) foreign body aspiration
(E) laryngeal tumor
120. A week-old infant presents blood in his stools. He was born at home, with the father assisting in the delivery; no physician or midwife was present. He has been breast-fed and has been nursing well. On examination, you also note some blood in his nose. He is not jaundiced; a rectal examination and guaic test of the stool confirms that blood is present. His examination is otherwise normal. He is on no medications. Which of the following is the most likely diagnosis?
(A) child abuse
(B) vitamin K deficiency
(C) breast milk allergy
(D) sepsis
(E) liver disease
121. A 16-year-old boy with a history of ulcerative colitis presents to the physician complaining of diarrhea and a rash. He states that his appetite has been decreased recently, and also complains of nausea and abdominal pain in addition to watery diarrhea. He has an erythematous rash on his distal arms and legs that "burns". His mother reports that he has had poor concentration and has been irritable lately. Vital signs are stable. Examination reveals a beefy red tongue that appears swollen. Abdominal examination is normal. The rash resembles a sunburn and is located on his distal arms and legs. It is symmetrical and tender to palpation. Neurological examination is normal. This patient's symptoms are most likely due to a deficiency of which of the following vitamins?
A. Thiamine
B. Riboflavin
C. Niacin
D. Pyridoxine
E. Cyanocobalamin
122. A 9-month-old child comes in for a routine visit. She has had several episodes of otitis media in the past, but no major illnesses or hospitalizations. Her mother is concerned because the child was previously happy and social around other people, but now cries if her mother is not in the room. The child constantly wants to be held by her mother and becomes upset if her mother walks into the next room. Her grandmother keeps her during the day, and she now cries when her mother leaves her in the morning. Developmentally, she is crawling and waves bye-bye. She does not yet respond to her name or say words. She previously babbled but stopped several months ago. When you hide a toy with your hand, she lifts your hand to look for the toy. Which of the following is the best next step in the management of this child?
A. Psychological evaluation
B. Audiology evaluation
C. Physical therapy evaluation
D. Social services referral
E. Reassure the mother that the child's development is normal.
123. A 12-year-old American boy comes to you with the complaints of abdominal pain and dark urine. On examination he has normal vitals, icteric sclerae, and abdominal tenderness with a mass palpable in right upper quadrant. His laboratory report shows bilirubin: 6.5 mg/di, negative viral serologies and mild elevations of amylase and lipase. Ultrasonography shows a cystic extra hepatic mass and a gall bladder separated from the mass. What is the most likely diagnosis in this patient?
A. Caroli's syndrome.
B. Choledochal cyst
C. Biliary abscess.
D. Biliary atresia.
E. Pseudo pancreatic cyst
124. A 10-year-old boy has been having “bellyaches” for about 2 years. They occur at night as well as during the day. Occasionally, he vomits after the onset of pain. Occult blood has been found in his stool. His father also gets frequent, nonspecific stomachaches. Which of the following is the most likely diagnosis?
A. Peptic ulcer
B. Appendicitis
C. Meckel diverticulum
D. Functional abdominal pain
E. Pinworm infestation
125. An 8-year-old boy presents to your office for a second opinion. He has a 2-year history of intermittent vomiting, dysphagia, and epigastric pain. His father reports he occasionally gets food “stuck” in his throat. He has been on a proton pump inhibitor for 18 months without symptom relief. His past history is significant only for eczema and a peanut allergy. Endoscopy was performed 6 months ago; no erosive lesions were noted and a biopsy was not performed. You arrange for a repeat endoscopy with biopsy. Microscopy on the biopsy sample reveals many eosinophils. Treatment of this condition should include which of the following?
A. Corticosteroids
B. Prolonged acid blockade
C. Treatment for Candida sp.
D. Treatmentfor Aspergillus sp.
E. Observation
126. A 4-year-old girl presents to the emergency department with fever and a petechial rash. A sepsis workup is performed, and IV antibiotics are administered. Gram-negative diplococci are identified in the CSF. Which of the following is true of this condition?
(A) Antibiotic prophylaxis of fellow daycare attendees is not necessary.
(B) The most common neurologic residual is seizures.
(C) The presence of meningitis decreases the survival rate.
(D) Shock is the usual cause of death.
(E) Vancomycin administered intravenously is the treatment of choice.
127. A 3-year-old boy suddenly begins choking and coughing while eating peanuts. On physical examination he is coughing frequently. He has inspiratory stridor and mild intercostal and suprasternal retractions. Initial management should include which of the following?
(A) back blows
(B) abdominal thrusts
(C) blind finger-sweeps of the hypopharynx
(D) permitting him to clear the foreign body by coughing
(E) emergency tracheostomy
128. During a well-child visit, the grandmother of an 18-month-old patient is concerned because the child’s feet turn inward. She first noticed this when her grandson began to walk. It does not seem to bother the child. On examining his gait, his knees point forward and his feet turn inward. Which of the following is the most likely cause of this condition?
(A) adducted great toe
(B) femoral anteversion
(C) Legg-Calve̝-Perthes disease
(D) medial tibial torsion
(E) metatarsus adductus
129. Two weeks after a viral syndrome, a 9-year-old boy presents to your clinic with a complaint of several days of weakness of his mouth. In addition to the drooping of the left side of his mouth, you note that he is unable to completely shut his left eye. His smile is asymmetric, but his examination is otherwise normal. Which of the following is the most likely diagnosis?
A. Guillain-Barre̝ syndrome
B. Botulism
C. Cerebral vascular accident
D. Brainstem tumor
E. Bell palsy
130. An infant can regard his parent’s face, follow to the midline, lift his head from the examining table, smile spontaneously, and respond to a bell. He does not yet regard his own hand, follow past the midline, nor lift his head to a 45° angle off the examining table. Which of the following is the most likely age of the infant?
A. 1 month
B. 3 months
C. 6 months
D. 9 months
E. 12 months
131. A child is brought to your clinic for a routine examination. She can put on a T-shirt but requires a bit of help dressing otherwise. She can copy a circle well but has difficulty in copying a square. Her speech is understandable and she knows four colors. She balances proudly on each foot for 2 seconds but is unable to hold the stance for 5 seconds. Which of the following is the most likely age of this child?
A. 1 year
B. 2 years
C. 3 years
D. 4 years
E. 5 years
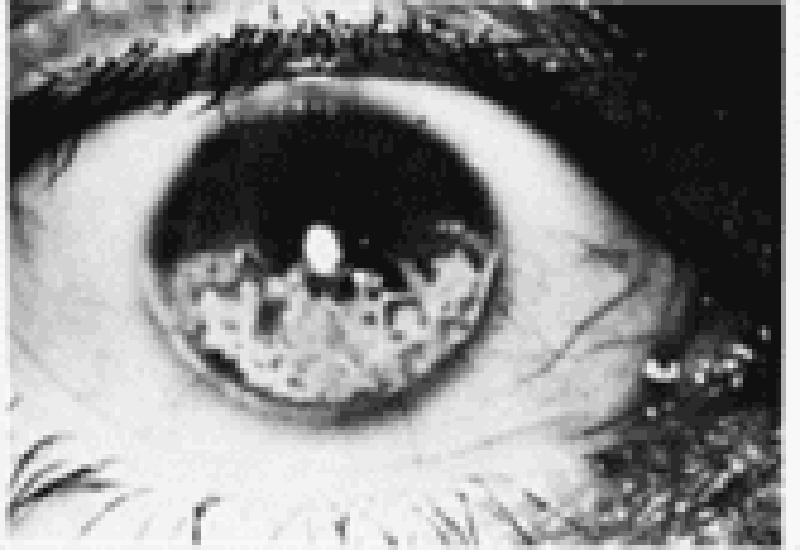
132. A 4-year-old girl is noticed by her grandmother to have a limp and a some-what swollen left knee. The parents report that the patient occasionally com- plains of pain in that knee. An ophthalmologic examination reveals findings as depicted in the photograph. Which of the following conditions is most likely to be associated with these findings?
Juvenile rheumatoid arthritis
Slipped capital femoral epiphysis
Henoch-Schönlein purpura
Legg-Calve̝-Perthes disease
Osgood-Schlatter disease
133. A 1-month old boy is brought to the emergency department by his mother, who states that he has been having what she describes as "projectile vomiting" for the past several days. She states that he vomits every time she feeds him, and the situation seems to be getting worse, although he does not seem to be in pain. She describes the vomitus as non-bilious, and he has had normal stools with no blood in them. On examination, the infant appears to be mildly dehydrated, his abdomen is soft, and there is a palpable, olive-sized, firm moveable mass in the right upper quadrant. Which of the following is the most likely diagnosis?
A. Duodenal atresia
B. Intussusception
C. Hirschsprung disease
D. Midgut volvulus
E. Pyloric stenosis
134. A 3-month old infant is brought to a pediatrician's office because of increased lethargy and irritability. The parents state that the child rolled off the couch and fell on the floor one day prior to presentation. His parents report that the child has been previously healthy and is up to date on his vaccinations. He has been meeting his development milestones. His fontanelles are full. While in office the patient develops a tonic-clonic seizure. Which of the following is the next appropriate step?
A. Obtain a head computerized tomography scan
B. Perform a retinoscopic examination
C. Check serum levels of ammonia
D. Administer intravenous benzodiazepines
E. Perform a lumbar puncture
135. A toddler is brought to the emergency department with burns on both of his buttocks. The areas are moist, have blisters, and are exquisitely painful to touch. The parents explain that the child accidentally pulled a pot of boiling water over himself. Which of the following is the most important step in management?
A. Application of mafenide acetate to the burned areas B. Early excision and grafting of the burned areas
C. Education of the parents on accident prevention
D. Prompt administration of fluid resuscitation
E. Referral to the proper authorities for suspected child abuse
136. A pediatrician examines a 2-month-old infant who had been born at term. The pediatrician hears a continuous murmur at the upper left sternal border. The peripheral pulses in all extremities are full and show widened pulse pressure. Which of the following is the most likely diagnosis?
A. Coarctation of the aorta
B. Patent ductus arteriosus
C. Peripheral pulmonic stenosis
D. Persistent truncus arteriosus
E. Ventricular septal defect
137. A 3-week-old infant is being evaluated for hema- : tochezia. His mother states that the infant passed stools j that contain both blood and mucus. There were no complications during her pregnancy, and the infant has been otherwise healthy. On physical examination, his temperature is 37.1 C (98.9 F), pulse is 110/min, and respirations are 18/min. He appears well, and his fontanelle is flat and level. Abdominal examination reveals normal active bowel sounds; his abdomen is nontender to palpation and there is no mass. His diaper contains stool that has bright red blood on it with mucus. Which of the following is the most likely explanation of his hematochezia?
(A) Food allergy-induced colitis
(B) Meckel diverticulum
(C) Necrotizing enterocolitis
(D) Rectal fissure
(E) Ulcerative colitis j
138. A 7-year-old boy is brought to the physician because of a persistent mucopurulent nasal discharge for 2 weeks following a common cold. The mother also reports that the child has had frequent cough during the day and occasional temperatures up to 38.0 C (100.5 F). The child does not appear critically ill, but he complains of mild pain in the maxillary region and nasal obstruction. Rhinoscopic examination reveals a rivulet of purulent fluid coming from the inferior meatus. The rest of the physical examination is normal. Which of the following is the most likely diagnosis?
(A) Acute bacterial sinusitis
(B) Acute otitis media
(C) Acute viral rhinitis
(D) Allergic rhinosinusitis
(E) Asthma
139. A9-year-old boy presents with a several-day history of progressive arm and leg weakness. He has been well except for an upper respiratory infection 2 weeks ago. The patient is alert and oriented. On repeated examination, the heart rate varies between 60 and 140 beats/min, and the blood pressure (BP) varies between 90/60 and 140/90 mmHg. Respirations are shallow, with a rate of 50/min. There is symmetric weakness of the face and all four extremities. Deep tendon reflexes are absent. Sensation is intact. Which of the following is the most likely diagnosis?
(A) polymyositis
(B) myasthenia gravis
(C) transverse myelitis
(D) Guillain-Barre̝ syndrome
(E) viral encephalitis
140. An 18-month-old boy is brought to the clinic for a checkup. As part of his routine care, a serum lead level is obtained. It is 25 g/mL. Which of the following is the most appropriate next step in his management?
(A) chelation with CaEDTA
(B) chelation with succimer
(C) investigation of his home for lead hazards
(D) reassurance that this level is not a problem
(E) repeating the level in 6 months
141. An infant is due for her first dose of polio vaccine. Her parents have heard that there are two different types of vaccine for polio. They want to know why their daughter needs to get another shot rather than just taking the oral form of the vaccine. You tell the parents the major advantage of the injectable vaccine is which of the following?
(A) lower cost
(B) increased mucosal immunity
(C) better efficacy
(D) avoidance of vaccine-associated paralytic poliomyelitis
(E) boosting her immunity through secondary transmission
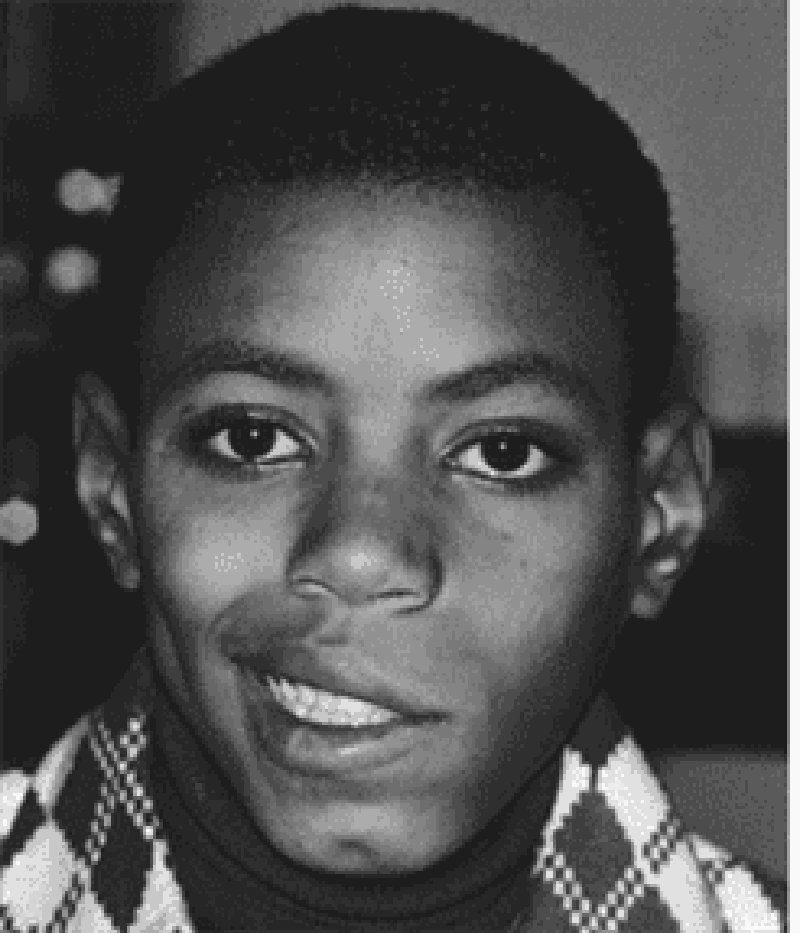
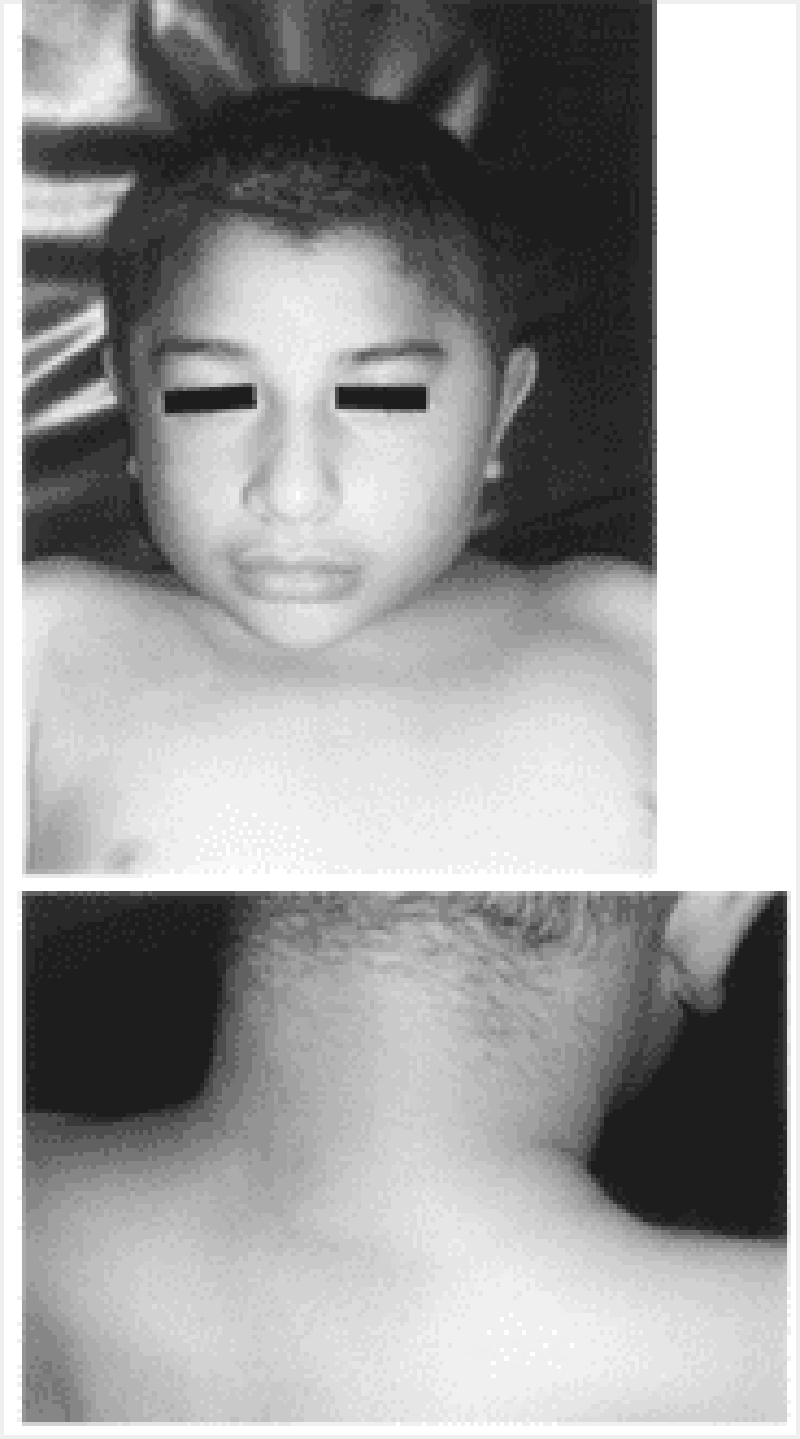
142. A previously healthy 4-year-old child pictured below presents to the emergency room (ER) with a 2-day history of a brightly erythematous rash and temperature of 40°C (104°F). The exquisitely tender, generalized rash is worse in the flexural and perioral areas. The child is admitted and over the next day develops crusting and fissuring around the eyes, mouth, and nose. The desquamation of skin shown in the photograph occurs with gentle traction. Which of the following is the most likely diagnosis?
A. Epidermolysis bullosa
B. Staphylococcal scalded skin syndrome
C. Erythema multiforme
D. Drug eruption
E. Scarlet fever
143. A patient comes to your office for a hospital follow-up. You had sent him to the hospital 3 weeks earlier for persistent fevers but no other symptoms; he was diagnosed with endocarditis and is currently being treated appropriately. Advice to this family should now include which of the following?
A. Restrict the child from all strenuous activities.
B. Give the child a no-salt-added diet.
C. Provide the child with antibiotic prophylaxis for dental procedures
D. Test all family members in the home with repeated blood cultures.
E. Avoid allowing the child to get upset or agitated.
144. A mother calls you on the telephone and says that your 4-year-old son bit the hand of her 2-year-old son 48 hours previously. The area around the injury has become red, indurated, and swollen, and he has a temperature of 39.4°C (103°F). Which of the following is the most appropriate response?
A. Arrange for a plastic surgery consultation at the next available appointment.
B. Admit the child to the hospital immediately for surgical debridement and antibiotic treatment.
C. Prescribe penicillin over the telephone and have the mother apply warm soaks for 15 minutes four times a day.
D. Suggest purchase of bacitracin ointment to apply to the lesion three times a day.
E. See the patient in the ER to suture the laceration.
145. A 6-year-old boy is brought to the emergency department (ED) by the paramedics due to nausea, vomiting, diarrhea and abdominal pain over the past hour. His mother found an open multivitamin supplement bottle and some pills scattered on the kitchen floor. After his admission to the ED, he starts hyperventilating and experiences hematemesis. His blood pressure is 90/60 mmHg, pulse is 130/min, respirations are 50/min and temperature is 37.2 C (99F). Abdominal plain x-ray reveals several small opacities in the stomach and duodenum. Lab results are: Hb 13.5 g/dL Ht 42% WBC 10,000/cmm Platelets 300,000/cmm Blood Glucose 118 mg/dL Serum Na 135 mEq/L Serum K 34 mEq/L Chloride 102 mEq/L Bicarbonate 16 mEq/L BUN 16 mg/dL Serum Creatinine 1.0 mg/dL pH 7.30 P02 90 mm Hg PC02 29 mm Hg What is the most likely diagnosis?
A Riboflavin poisoning
B. Vitamin A poisoning
C. Vitamin D poisoning
D. Vitamin K poisoning
E. Iron poisoning
146. A 3-year-old boy is brought to the office by his mother because he has been having painless passage of black stools for the past few days. Otherwise, his bowel habits are normal. He has no other medical problems. He takes no medication. His vital signs are within normal limits. The physical examination is unremarkable. What is the most likely diagnosis of this patient?
A. Peptic ulcer disease
B. Anal fissure
C. Intussusception
D. Inflammatory bowel disease
E. Meckel's diverticulum
147. And photophobia. He has some difficulty in adapting to darkness. He is a very poor eater, and his diet consists mainly of canned foods, and very rarely, fresh vegetables or milk. Examination reveals dry, scaly skin, follicular hyperkeratosis in the extensor surfaces of the A 3-year-old boy is brought to the office by his parents for the evaluation of dry eyes extremities, and dry, silver-gray plaques on the bulbar conjunctiva. What is the most likely diagnosis of this patient?
A Vitamin A deficiency
B. Thiamine deficiency
C. Ariboflavinosis
D. Scurvy
E. Hypervitaminosis A
148. A 2-week-old Caucasian male presents with constipation since birth. He was born full term via a normal vaginal delivery. He did not pass meconium till his 3rd day of life, after he was given a glycerin suppository. He has since stooled every 3–4 days, only with the help of a suppository. The stools are pellet like. He has had increasing abdominal distention. On rectal examination, tone appears normal and the ampulla contains no stool. Which of the following is the most likely cause?
(A) cystic fibrosis
(B) Hirschprung disease
(C) anal stenosis
(D) functional constipation
(E) hypothyroidism
149. Which of the following is the most appropriate evaluative procedure for an otherwise normal 7-day-old boy with perineal hypospadias?
(A) renal ultrasonography
(B) serum creatinine determination
(C) cystography
(D) circumcision
(E) intravenous pyelography (IVP)
150. A 44 year old woman delivers a 3120 g (6 lb 14 oz) newborn male. Her pregnancy was normal except that she noted decreased fetal movement compared to her previous pregnancies. She declined an amniocentesis offered by her obstetrician. Physical examination of the newborn reveals an infant with facial features suggestive of Down Syndrome. The infant then has bilious vomiting. An x-ray film showing the kidneys, ureters, and bladder (KUB) is performed, which shows a "double bubble" sign. Which of the following is the most likely cause of the abdominal signs and symptoms?
A. Duodenal atresia
B. Hirschsprung Disease
C. Malrotation
D. Meconium ileus
E. Pyloric stenosis
151. The parents of a 10-year-old girl with newly diagnosed, generalized tonic-clonic epilepsy come to the physician seeking advice regarding what they should do when the child has a seizure. Which of the following suggestions is appropriate?
A. Call an ambulance immediately as soon as seizure begins
B. Put something in the child's mouth at the onset of seizure
C. Try to place the child on her side during the seizure
D. Try to restrain the child during the seizure
E. Do not allow the child to return to her activities after recovery
152. A 10-year-old boy has a long history of recurrent infections. These have included pneumonia, suppurative lymphadenitis, persistent rhinitis, dermatitis, diarrhea, and perianal abscesses. Involved organisms have included Staphylococcus aureus, Serratia, Escherichia coli, and Pseudomonas. Biopsy of skin and lymph nodes have demonstrated granulomatous lesions, even though the only species isolated were those noted above. Immunoglobulin levels are higher than normal. Which of the following findings would be most helpful in establishing the diagnosis?
A. Absent B cells and normal numbers of T cells
B. Deficient nitroblue tetrazolium dye reduction in neutrophils
C. High serum IgM and very low serum IgG
D. Very low CD11 on the surface of white blood cells
E. Very low serum calcium levels
153. A 9-year-old Caucasian male complains of fever, sore throat and difficulty swallowing. Small tender lymph nodes are palpated in the cervical region. The symptoms subside quickly on penicillin therapy. Ten days later, the patient presents again with fever, skin rash and fleeting joint pain in the lower extremities. Physical examination reveals scattered urticaria and palpable lymph nodes in the cervical, axillary and inguinal regions. Which of the following is the most likely cause of this patient's current complaints?
A. Rheumatic fever
B. Drug-induced reaction
C. Lymphoproliferative disorder
D. Henoch-Schonlein purpura
E. Infective endocarditis
154. A 4-week-old male infant is brought to the office due to several episodes of projectile vomiting for the last few days. The vomitus contains milk and doesn't contain bile or blood. The child's appetite has increased for the last few days. He has been fed with goat's milk since birth, but doesn't seem to tolerate it anymore for the last few days. He vomits a few minutes after feedings. He appears dehydrated, and abdominal examination reveals no mass. Blood tests reveal macrocytosis. What is the most appropriate next step in the management of this patient?
A. Barium swallowing
B. Ultrasound of the abdomen
C. Substitute goat's milk with another form of milk
D. Divide his feedings
E. Add folic acid to relieve his vomiting
155. A 10-year-old boy presents with a 1-day history of fever, cough, and chest pain. He has not been eating and has been listless. He does not have any previous history of health problems. On physical examination, his temperature is 40°C, and he is tachypneic. He looks ill. He has rales on his left posterior lower lung fields. You order a chest x-ray. Which of the following organisms is most likely responsible for his pneumonia?
(A) Haemophilus influenzae
(B) Mycoplasma pneumoniae
(C) Pneumocystis carinii
(D) Staphylococcus aureus
(E) Streptococcus pneumoniae
156. A 10-year-old patient with sickle cell disease comes to the physician for a routine visit. The patient has a history of multiple pain crises and pneumonias. He was started on hydroxyurea one year ago and has not had any further pain crises since then. He has had no recent illnesses or hospitalizations. His physical examination is unremarkable. The patient's laboratory results are shown below. Complete blood count Hemoglobin 9.0 g/L Erythrocyte count 2.2 mln/mm3 MCHC 32% MCV 105 fl Reticulocytes 2.0% Platelets 212,000/mm3 Leukocyte count 9500/mm3 Neutrophils 56% Eosinophils 3% Lymphocytes 36% Monocytes 5% Which of the following best describes the role of hydroxyurea in the treatment of patients with sickle cell disease?
A. Removes sickled red blood cells from the circulation
B. Lyses microthrombi in the circulation
C. Protects against encapsulated bacterial infections
D. Increases fetal hemoglobin
E. Chelates iron to prevent iron toxicity
157. A 2-year-old child is brought to the physician for a routine visit. He is growing and developing appropriately. He eats a variety of foods including meat, vegetables, and fruits, and drinks 3-4 glasses of whole milk each day. He is starting to put words together into short sentences. His mother has no concerns. Physical examination is unremarkable. Routine laboratory studies show the following: Hemoglobin 9.5 g/dl RDW 14% MCV 65 fl Reticulocyte count 3.0% Platelet count 212,000/mm3 Leukocyte count 6,500/mm3 TIBC 300 mcg/dl (240-450 mcg/dl) Ferritin 1 00 ng/ml (7 -140 ng/ml) What is the most likely cause for this child's anemia?
A. Iron deficiency
B. Anemia of chronic disease
C. Thalassemia trait
D. Cyanocobalamin deficiency
E. Spherocytosis
158. A previously healthy 5-year-old girl is brought to the physician for evaluation of night awakenings. She has woken up screaming in each of the past three nights about one hour after going to sleep. When her parents go to her room, she is crying, sweating, and looks frightened. She does not respond to her parents and does not seem fully awake. When her parents hold her, she calms down and goes back to sleep. The next morning, she does not recall the incident. She started kindergarten this week and has just begun going all day without taking a nap. On examination, she is afebrile and her vital signs are within normal limits. A complete physical examination is unremarkable. What is the most likely diagnosis?
A Nightmare
B. Somnambulism
C. Epilepsy
D. Night terrors
E. Benign paroxysmal vertigo
159. A 3-year-old boy is brought to the ER with a two-day history of decreased appetite, neck swelling, and irritability. He keeps his head rotated slightly to the right side. He resists passive flexion of the neck and rotation to the left side. Which of the following is the best next step in managing this patient?
A Direct laryngoscopy
B. Soft neck collar
C. X-ray of the neck
D. Lumbar puncture
E. Botulinum toxin injection
160. A previously healthy 15-month-old girl is brought to the emergency department after she had several episodes in which she lost consciousness after crying. Her parents state that the episodes always occur when the child gets frustrated or upset. She has no cyanosis or incontinence. The episodes last about 45 seconds each. After the episode, she is alert and appropriate. Physical examination is unremarkable. What is the next best step in the management of this patient?
A. Reassure the parents
B. Obtain an electroencephalogram
C. Obtain an electrocardiogram
D. Computed tomography of the head
E. Magnetic resonance imaging of the brain
161. Apathient has the sudden onset of fretfulness and pain. He curls up with his legs drawn in to his abdomen. Over the next few hours he continued to have episodes of pain and cries with tears, but between these times he acts normally. The patient's mother fears something is terribly wrong and brings him to the hospital. His past medical history was unremarkable. The previous week he had had a cold with a runny nose. His stools had been normal that day. On examination he is quiet and his abdomen is surprisingly soft and normal. In the emergency room there is a semi-soft stool with some blood mixed with mucus. This classic presentation of intussusception is most likely to occur in which of the following age groups?
A. Birth to 4 weeks of age
B. 6 to 12 months of age
C. 3 to 5 years of age
D. Early adolescence
E. Late adolescence
162. A 12-year-old boy is brought to the clinic because of a several-month history of strange behavior. According to his parents, the boy occasionally will start staring and not respond. He will also have tears in his eyes. These episodes last several seconds and he then returns to his baseline. He has not sustained any head trauma and is on no medications. Which of the following drugs is the most appropriate treatment?
A. Diazepam
B. Diphenhydramine
C. Ethosuximide
D. Phenobarbital
E. Phenytoin
163. A 9-month-old is brought to the emergency center by ambulance. The child had been having emesis and diarrhea with decreased urine output for several days, and the parents noted that she was hard to wake up this morning. Her weight is 9 kg, down from 11 kg the week prior at her 9-month checkup. You note her heart rate and blood pressure to be normal. She is lethargic, and her skin is noted to be “doughy.” After confirming that her respiratory status is stable, you send electrolytes, which you expect to be abnormal. You start an IV. Which of the following is the best solution for an initial IV bolus?
A. One-fourth normal saline (38.5 mEq sodium/L)
B. D10 water (100 g glucose/L)
C. Normal saline (154 mEq sodium/L)
D. 3% saline (513 mEq sodium/L)
E. Fresh-frozen plasma
164. You are admitting to the hospital a 3-month-old infant who has been having poor feeding, emesis, and diarrhea for 3 days. In the emergency center, her electrolytes were found to be: sodium 157 mEq/L, potassium 2.6 mEq/L, chloride120 mEq/L, bicarbonate 14 mEq/L,creatinine1.8 mEq/L, blood urea nitrogen(BUN) 68 mEq/L, and glucose195 mEq/L. She was given a fluid bolus in the emergency center and has subsequently produced urine. Which of the following is the most appropriate next step in her management?
A. Slow rehydration over 48 hours
B. Continued rapid volume expansion with 1/4 normal saline
C. Packed red blood cells (RBCs)
D. Rehydration with free water
E. Urinary electrolytes
165. At exploratory laparotomy for blunt abdominal trauma, a 14-year-old boy is found to have a ruptured spleen. The spleen is shattered into multiple fragments, and there are other serious intraabdominal injuries that will require significant operative time. For the above reasons, it is decided that a quick splenectomy is indicated, and it is done. In the postoperative period, this young man should receive which of the following treatments?
(A) Anticoagulation
(B) Long-term prophylactic antibiotics
(C) Platelet transfusions
(D) Prolonged parenteral nutrition
(E) Vaccinations for encapsulated organisms
166. A 10-year-old girl has bullous target lesions and mucosal erythema, which developed after her third dose of trimethoprim-sulfamethoxazole for a urinary tract infection. Which of the following is a likely associated clinical finding?
(A) Diarrhea
(B) Fever
(C) Lymphadenopathy
(D) Vomiting
(E) Nausea
167. A 16-year-old boy is brought into the emergency department by his friends. He is semicomatose, with a pulse of 60/min and respirations of 6-8/min. His pupils are constricted. Which of the following will most likely be revealed on a urine toxicology screen?
A. Amphetamine intoxication
B. Cocaine intoxication
C. Ethanol intoxication
D. Opiate intoxication
E. Tricyclic antidepressant intoxication
168. A 6-month-old previously health child is brought to the doctor's office because of sudden onset of lethargy, constipation, generalized weakness and poor feeding. He has been meeting all development milestones and his immunization schedule is up to date. On further questioning, his parents mention that his diet was recently advanced to a homemade formula of evaporated milk and honey. On physical examination, he has stable vital signs, clear lungs, normal skin turgor and full fontanelles. Which of the following is the most likely explanation for the patient's presentation?
A. Botulism
B. Hirschsprung disease
C. Hypernatremia
D. Hyponatremia
E. Hypothyroidism
169. A 12-year-old girl was hit in the face by a baseball 15 minutes earlier and has had her mandibular incisors knocked out. Which of the following represents the best plan of action?
A. The teeth should be rinsed in hot water then carefully dried.
B. Foreign matter adhering to the teeth should be immediately scrubbed off.
C. The teeth may be transported in tea, juice, or cola.
D. Avulsed teeth can be transported in the mouth of the parent or a cooperative patient.
E. A dental appointment should be made within 48 to 72 hours.

170. A 55-day-old infant born prematurely at 27 weeks of gestation is shown below. The swelling is not tender, firm, hot, or red, and it does not transil luminate. It seems to resolve with pressure, but returns when the infant cries or strains. Which of the following is the most appropriate course of action at this point?
A. Obtain a surgical consultation
B. Perform a needle aspiration
C. Order a barium enema
D. Order a KUB (plain radiographs of kidney, ureter, and bladder) e. Observe the patient and reassure the patient and family
171. A 17-year-old boy comes to medical attention because of recurrent sinusitis and pneumonia, and persistent watery diarrhea due to Giardia lamblia. His parents and a sister are in excellent health. Physical examination reveals enlarged lymph nodes in cervical, axillary and inguinal regions. A lymph node biopsy shows hyperplastic follicles with an absence of plasma cells. Laboratory investigations show: Hematocrit.......................44% Leukocyte count...............9,800/mm3 Neutrophils.....................55% Lymphocytes..................30% Monocytes.....................5% CD4 T-cell count............1000 cells/mm3 Proteins, serum...............6.2 g/dL Albumin........................5.0 g/dL Globulin........................1.2 g/dL Additional studies demonstrate severely depressed levels of serum IgG, with slightly below- normal levels of IgM and IgA. Which of the following is the most likely diagnosis?
A. Acquired immunodeficiency syndrome (AIDS)
B. Common variable immunodeficiency
C. Hodgkin disease
D. Isolated IgA deficiency
E. X-linked agammaglobulinemia of Bruton
172. An 8-year-old boy presents with a 2-day history of rash. The rash started on the head and spread downward to his trunk and extremities. He also complains of a fever, cough, and a runny nose for the past 5 days. On physical examination, his temperature is 38.2 C (100.7 F), blood pressure is 88/56 mm Hg, pulse is 76/min, and respirations are 16/min. There is a small, irregular red spot with a central gray color on his buccal mucosa. The rash on his body is erythematous and maculopapular in quality. Which of the following is the most likely diagnosis?
A. Erythema infectiosum
B. Hand-foot-mouth disease
C. Measles
D. Roseola infantum
E. Rubella
173. A 4-week-old male infant has been spitting up his formula feedings for the past few days. He does not vomit bilious material or blood. The spitting up is gradually becoming more frequent, and forceful vomiting ensues. The vomitus seems to shoot straight out and nearly hit the wall. On examination, the baby seems hungry and is chewing his fist. His mucous membranes appear dry. A small, round mass, about the size of an adult thumbnail, is palpated in the upper abdomen. Laboratory data reveal Na+ of 133 mEq/L, K+ of 3.5 mEq/L, CI of 93 mEq/L, and HC0 3 - of 29 mEq/L. Which of the following is the most appropriate next step in management?
(A) Change the feedings to clear liquids or Pedialyte
(B) Obtain a surgical consult immediately
(C) Obtain flat plate and upright x-ray films of the abdomen
(D) Insert a nasogastric tube
(E) Begin parenteral antibiotics
174. A 3-year-old child presents in clinic with marked erythema of the cheeks, with no prior symptoms. The rash soon involves the arms and has a reticular erythematous maculopapular appearance. The patient has been previously healthy and is not on any medications. He has not been exposed to any other ill individual. Which of the following is the most likely diagnosis?
(A) Fifth disease (erythema infectiosum)
(B) Measles
(C) Roseola
(D) Rubella
(E) Varicella
175. The mother of a 6-month-old infant is concerned that her baby may be teething. You explain to her that the first teeth to erupt in most children are which of the following?
A. Mandibular central incisors
B. Maxillary lateral incisors
C. Maxillary first molars
D. Mandibular cuspids (canines)
E. First premolars (bicuspids)
176. A male infant born at term is found to have bilateral colobomas, choanal atresia, ear anomalies, and cryptorchidism. There is no history maternal drug or alcohol abuse during pregnancy. There is no family history of similar congenital defects. Which of the following is the most appropriate initial test to exclude any associated abnormalities?
A. Barium swallow
B. Echocardiography
C. Fiberoptic bronchoscopy
D. Renal ultrasonography
E. Skeletal survey
177. A 15-year-old girl presents to the emergency department with the sudden onset of watery diarrhea tinged with blood. The girl was previously healthy. Her only medications are topical benzoyl peroxide and oral clindamycin for acne vulgaris. Physical examination reveals a slightly distended abdomen that is diffusely tender. Her temperature is 38.1 C (100.5 F). She has not been exposed to any uncooked meat and has not eaten any unusual foods. Which of the following is the most likely diagnosis?
A. Gastroenteritis
B. Irritable bowel syndrome
C. Pseudomembranous enterocolitis
D. Salmonella infection
E. Ulcerative colitis
178. A 22-year-old woman has just delivered a male infant at 41 weeks of gestation. Her medical history is normal and her pregnancy was uncomplicated. She is an assistant in a veterinary clinic. Examination of the infant reveals jaundice, hepatosplenomegaly, and generalized lymphadenopathy. During the examination, he suddenly begins to have tonic- clonic seizures. The CT scan reveals active inflammatory lesions, hydrocephalus and intracranial calcifications. What is the most likely diagnosis of this patient?
A. Congenital syphilis
B. Congenital rubella
C. Congenital toxoplasmosis
D. Congenital herpes simplex
E. Congenital hepatitis B
179. A 5-year-old girl is brought to the physician's office for a follow-up visit after recovering from an episode of acute bacterial meningitis. Five weeks ago, she developed pneumococcal meningitis, and was admitted to the hospital, where she underwent lumbar puncture, CT scan of the head, and ceftriaxone therapy. She was discharged in a stable condition. According to the mother, the child has not been performing well in school since her illness. She also noticed that the child has forgotten how to copy figures such as triangles and squares, and is unable to identify colors accurately. What is the most likely cause for the regression of milestones in this patient?
A. Drug reaction
B. Lumbar puncture
C. Meningitis
D. Alexia
E. Amnesia
180. You are seeing a 2-year-old boy for the first time. His father denies any past medical or surgical history, but does note that the child’s day care recently sent a note home asking about several episodes, usually after the child does not get what he wants, when he “breathes funny” and sits in a corner with his knees under his chin for a few minutes. The day-care staffers think this “self-imposed time-out” is a good thing, but they worry about the breathing. One teacher even though he once looked blue, but decided that it was probably because of the finger paints he had been using. On examination, you identify a right ventricular impulse, a systolic thrill along the left sternal border, and a harsh systolic murmur (loudest at the left sternal border but radiating through the lung fields). His chest radio- graph and ECG are shown. Which of the following congenital cardiac lesions would you expect to find in this child?
A. Patent ductus arteriosus
B. Right ventricular outflow obstruction
C. Atrial septal defect (ASD)
D. Transposition of the great vessels with a patent foramen ovale
E. Hypoplastic left heart
181. The parents of a 2-month-old baby boy are concerned about his risk of coronary artery disease because of the recent death of his 40-year-old maternal uncle from a myocardial infarction. Which of the following is the most appropriate management in this situation?
A. Screen the parents for total cholesterol.
B. Counsel the parents regarding appropriate dietary practices for a 2-month-old infant and test him for total cholesterol at 6 months of age.
C. Reduce the infant’s dietary fat to less than 30% of his calories by giving him skim milk.
D. Initiate lipid-lowering agents.
E. Recommend yearly ECGs for the patient.
182. An 8-month-old female infant is brought to the clinic for a well-baby examination. She was born prematurely at 35 weeks gestation. She weighs 2.3kg (5 Ib). She cannot sit unsupported. Physical examination reveals mild facial hypoplasia, epicanthal folds, micrognathia, long nasal philtrum, thin upper lip and short palpebral fissures. Auscultation of the heart reveals an III/ IV harsh holosystolic murmur over the precordium. Her karyotype is normal. What is the most likely cause of these findings?
A. Maternal age
B. Moderate or excessive intake of alcohol during pregnancy
C. Treatment with lithium for manic disorder
D. Maternal hyperglycemia
E. Infection with rubella during pregnancy
183. A 12-year-old boy is brought to the clinic by his parents because "he cannot walk anymore." Yesterday, he became irritable, uneasy, and complained of tingling and weakness in both his legs. This morning, he couldn't stand up or move his legs, and complained of pain in his leg and thigh muscles. He denies any headaches, nausea or vomiting. He had an episode of febrile diarrhea 10 days ago. His family history is unremarkable. Physical examination reveals symmetric flaccid paralysis of both legs, absent deep tendon reflexes, and decreased superficial touch and vibratory sense. There is no nuchal rigidity. What structure is most likely affected in this patient's condition?
A. Cerebral cortex
B. Medial lemniscus
C. Corticospinal tract
D. Gracile fasciculus
E. Peripheral nerves
184. A 5-month-old infant is brought to the physician for a routine visit. The child was born full term without complications. The infant has been seen several times for poor weight gain. The infant takes 5 ounces of formula every 4 hours, and has been tried on increased calorie formula without success. Family history is significant only for nephrolithiasis. On examination, the infant's weight is <5%, height is at the 20% and head circumference is at the 20%. The infant appears thin, but the remainder of the physical examination is unremarkable. Screening labs are shown below. Chemistry panel Serum sodium 140 mEq/L Serum potassium 3.0 mEq/L Chloride 113 mEq/L Bicarbonate 15 mEq/L Blood urea nitrogen (BUN) 10 mg/dl Serum creatinine 0.5 mg/dl Calcium 9.0 mg/dl Blood glucose 98 mg/dl The urine pH is 7.9 and urinary sodium and potassium are within normal limits. What is the most likely cause for this patient's failure to thrive?
A. Insufficient calories
B. Lactic acidosis
C. Cystic fibrosis
D. Renal tubular acidosis
E. Gastroesophageal reflux
185. A 6-year-old boy has had a fever for 8 days. He just finished a 5-day course of amoxicillin for otitis media. On examination, his temperature is 38.6 C (101.4 F). He has meningismus and palsy of the left sixth cranial nerve. Cerebrospinal fluid (CSF) analysis reveals 200 white cells per mL with 80% lymphocytes and 20% polymorphonuclear leukocytes, glucose of 18 mg/dL, protein of 260 mg/dL, and a negative Gram stain. There is basilar enhancement without focal lesions on CT. Which of the following CSF tests will most likely identify the cause of meningitis?
(A) Antigen test for Cryptococcus
(B) Bacterial culture
(C) Culture for mycobacteria
(D) Latex agglutination test for pneumococcus
(E) Test for Treponema pallidum
186. A previously healthy 5-month-old boy has been irritable and has had a decreased oral intake for 2 days. His rectal temperature is 37.4 C (99.3 F), pulse is 220/min, and respirations are 50/min. The radial and posterior tibial pulses are diminished with good brachial and femoral pulses. ECG shows tachycardia; QRS complexes are narrow without preceding P waves. Which of the following is the most appropriate initial step in management?
(A) Administer adenosine intravenously
(B) Administer verapamil intravenously
(C) Apply an ice-filled plastic bag to the entire face for 5-10 seconds
(D) Cardiac pacing
(E) Perform synchronized direct current cardioversion
187. A 5-year-old boy suffers from a condition characterized by recurrent fungal and viral infections, thymic hypoplasia, tetany, and abnormal facies. Serum levels of immunoglobulins are mildly depressed, and lymph node biopsy shows lymphocyte depletion of T-dependent areas. Which of the following is the underlying pathogenetic mechanism?
A. Developmental defect of the third/fourth pharyngeal pouches
B. In utero infection by human immunodeficiency virus (HIV)
C. Mutations of an autosomal gene encoding adenosine deaminase
D. Mutations of an X-linked gene coding for a cytokine receptor subunit
E. Mutations of an X-linked gene coding for a tyrosine kinase
188. A 5-year-old boy is brought to the physician because of a malodorous discharge coming from his right nostril. His parents report that the child developed frequent sneezing and mucus discharge for one week. They thought it was a common cold. The child is afebrile and in apparent good health. There is no history of allergic diseases or recurrent infections. Examination reveals obstruction of the right nasal fossa with associated purulent discharge from the right nostril. Which of the following is the most likely diagnosis?
A. Allergic rhinitis
B. Juvenile angiofibroma
C. Nasal foreign body
D. Nasal polyp
E. Rhinitis medicamentosa
189. A 4-year-old girl is brought to your office by her mother for recent onset of fever and rash. For the past 4 days, she has had headaches, fever, and sore throat. She was apparently normal4 days ago, and upon presentation of the symptoms, her mother thought that she was having a simple viral fever which would go away with time; however, she then developed a pale pink maculo-papular rash, first on the face and neck, and then it rapidly spread onto the trunk and limbs. On examination, the child is afebrile and doesn't appear ill, but there are few palpable suboccipital and posterior auricular lymph nodes. What is the most likely cause of this patient's condition?
A. Group A beta- hemolytic streptococci
B. Measles virus
C. Rubella virus
D. Varicella virus
E. Human parvovirus
190. While working in the newborn nursery, you have the chance to counsel a first time mother. She had a healthy pregnancy and good prenatal care. The infant was delivered via normal spontaneous vaginal delivery and is doing well. You are counseling the mother on the benefits of breastfeeding, and she asks you what the differences are between human milk and formula. Which of the following is a true statement?
A. Human milk has more calcium and phosphorus than formula
B. Human milk provides adequate amounts of vitamin D
C. Human milk contains only trace amounts of immunoglobulin A
D. Human milk protein absorbs better and improves gastric emptying
E. The main advantage of formula is it decreases colic
191. An 18-month-old male infant is brought to the office by his parents for a follow-up visit. He has a congenital condition that started at the age of 6 months with repeated vomiting and hypotonia, and progressively evolved into choreoathetosis, spasticity and dystonia. Over the past month, he has started biting his hands and arms, pinching himself and banging his limbs against the wall. His family history is unremarkable. On examination, he has several scars, cuts and bruises over his arms and hands. His uric acid levels are elevated. What is the most likely deficient enzyme in this patient?
A. Glutamine-phosphorylase pyrophosphate aminotransferase
B. Xanthine oxidase
C. Hypoxanthine-guanine phosphoribosyl transferase
D. Adenyl succinate synthase
E. Purine nucleoside phosphorylase
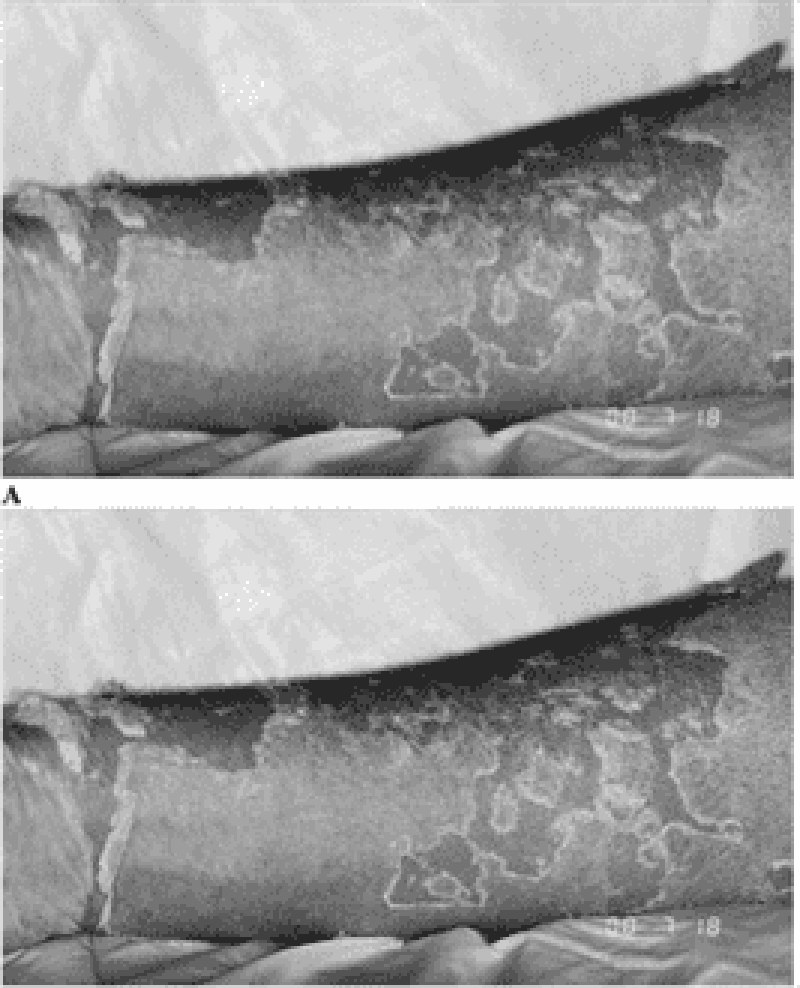
192. For the past year, a 12-year-old boy has had recurrent episodes of swelling of his hands and feet, which has been getting worse recently. These episodes occur following exercise and emotional stress, last for 2 to 3 days, and resolve spontaneously. The last episode was accompanied by abdominal pain, vomiting, and diarrhea. The results of routine laboratory workup are normal. An older sister and a maternal uncle have had similar episodes, but they were not given a diagnosis. He presents today with another episode as shown in the photographs on the next page. Which of the following is the most likely diagnosis?
A. Systemic lupus erythematosus
B. Focal glomerulosclerosis
C. Congenital nephrotic syndrome
D. Hereditary angioedema
E. Henoch-Schönlein purpura
193. A newborn is diagnosed with congenital heart disease. You counsel the family that the incidence of heart disease in future children is which of the following?
A. 1%
B. 2% to 6%
C. 8% to 10%
D. 15% to 20%
E. 25% to 30%
194. A 5-year-old girl is brought to medical attention by her parents 12 hours after the onset of generalized tonicoclonic seizures. She never had similar episodes in the past. The girl is otherwise healthy. Her temperature is 37 C (98.6 F). Physical examination is unremarkable. There is no evidence that the girl had a fever at the onset of the convulsive episode. The parents fear that seizures may damage the child's brain and may eventually recur. Which of the following is the most appropriate next step in management?
(A) Provide reassurance to child and family
(B) Admit patient to the hospital for further evaluation
(C) Perform electroencephalographic studies
(D) Perform CT/MW studies of the brain
E) Start antiepileptic medication
195. An otherwise healthy 13-year-old boy has seasonal allergic rhinitis. He complains of excessive rhinorrhea, frequent sneezing, and nasal congestion. He has a nasal voice and breathes with his mouth. He derives some relief from keeping windows closed at home and spending as litde time as possible outdoors in periods of high pollen concentration. However, he is excessively bothered by nasal congestion. Which of the following drugs would be most effective in relieving nasal congestion?
(A) Alpha-adrenergic agents such as phenylephrine
(B) Antihistamines such as chlorpheniramine
(C) Antihistamines such as loratadine
(D) Cromoglycate or similar mast cell stabilizers
(E) Ipratropium bromide
196. During a regular checkup of an 8-year-old child, you note a loud first heart sound with a fixed and widely split second heart sound at the upper left sternal border that does not change with respirations. The patient is otherwise active and healthy. Which of the following heart lesions most likely explains these findings?
A. Atrial septal defect (ASD)
B. V entricular septal defect (VSD)
C. Isolated tricuspid regurgitation
D. Tetralogy of Fallot
E. Mitral valve prolapse
97. A 2-year-old child with minimal cyanosis has an S3 and S4 (a quadruple rhythm), a systolic murmur in the pulmonic area, and a middiastolic murmur along the lower left sternal border. An ECG shows right atrial hypertrophy and a ventricular block pattern in the right chest leads. Which of the following is the most likely diagnosis?
A. Tricuspid regurgitation and pulmonic stenosis
B. Pulmonic stenosis and a VSD (tetralogy of Fallot)
C. Atrioventricular canal
D. Ebstein anomaly
E. Wolff-Parkinson-White syndrome
198. A woman brings her 3-year-old son to the emergency room after witnessing him swallow a disk-shaped battery. She adds that he vomited once on the way to the hospital. The vomitus was non-bloody and did not contain the battery. Physical examination of the child's chest is unremarkable. Plain radiographs reveal that the battery is located in the esophagus. What is the most appropriate next step in the management of this patient?
A. Induce emesis to expel the battery
B. Observation for next 24-48 hours for spontaneous expulsion
C. Immediate endoscopic removal
D. Advance the battery into the stomach with a nasogastric tube
E. Increase gastrointestinal motility with metoclopramide
199. A 7 -year-old Caucasian boy is brought to the emergency room with a severe headache, vomiting, and altered mental status of acute onset. His temperature is 36.7 C (98 F), blood pressure is 130/70 mm Hg, pulse is 60/min, and respirations are 18/min. Neurologic examination reveals nuchal rigidity, but no focal neurologic signs. A CT scan shows blood in the subarachnoid space. Which of the following is the most probable additional finding in this patient?
A. History of seizures
B. Mental retardation
C. Congenital heart disease
D. Coagulation abnormalities
E. Trauma
200. A 28-month-old female has been living with her mother in a shelter for homeless women and children. She is brought to the Emergency Department in status epilepticus, which is stopped with intravenous lorazepam. She is placed on a cardiac monitor and a wide complex tachycardia is noted. The ventricular tachycardia reverts to sinus tachycardia after defibrillation is performed. Her temperature is 38.5 C (101.3 F), blood pressure is 120/80 mm Hg, pulse is 195, and respirations are 26. Physical examination reveals a lethargic, pale toddler with dilated and reactive pupils, dry mucous membranes, shallow respirations, diaphoresis and brisk deep tendon reflexes. A urine toxicology screen is most likely to detect which of the following substances?
A. Barbiturates
B. Cocaine
C. Heroin
D. Marijuana
E. PCP
{"name":"Pediatric USMLE 101 - 200", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge on pediatric medicine with our comprehensive 100-question quiz tailored for aspiring medical professionals preparing for the USMLE. This engaging quiz covers a wide range of topics, ensuring that you understand the nuances of pediatric care.Key Features:100 carefully crafted questionsMultiple choice formatFocus on clinical scenarios and pediatric principles","img":"https:/images/course8.png"}
More Quizzes
USMLE_Emergency II
150750
2020 pediatri
45220
Yokoo
210
MythBusters COVID-19
1050
Which JoJo Are You? - Free Joestar Bloodline
201016616
JROTC: 20 Practice Questions - Free Online
201015966
Escherichia and Salmonella: Cocci or Bacilli?
201022230
Are You Cool in School? Free Personality
201018177
Reliability in Psychology - Research Methods
201022230
What Skyrim Race Am I? Free to Find Your Match
201017412
Which of the Following Is a Complex Sentence?
201017545
Fall Prevention for Nurses - Risk Assessment Skills
201016616