Pediatric_USMLE 251-375
251. A 12-year-old, previously healthy girl presents to her physician with a chief complaint of early morning headaches. She states that these headaches wake her up from sleep 2-3 days a week. She also complains of some vomiting associated with the headaches. The headaches have been getting progressively worse for the past 2 months. She denies any photophobia, dizziness, or blurred vision. There is no history of a recent respiratory infection, runny nose, or cough. There is no history of recent trauma. In the office, her vital signs are within normal limits. Her examination shows pupils that are equal, round, and reactive, with no maxillary or frontal sinus tenderness. Her tympanic membranes are clear and intact. Her neck is supple with full range of motion. Neurologic examination shows a positive Romberg sign. Which of the following tests would most likely confirm the diagnosis?
CT of the brain
MRI of the brain
Plain film of the skull
Sinus x-ray film
Spinal tap
252. A 10-month-old boy develops an upper respiratory tract infection 2 days before presentation. On the day of presentation, he has a generalized tonic-clonic seizure lasting 30 seconds. His temperature is 40.0 C (104 F), blood pressure is 90/60 mm Hg, and respirations are 22/min. He is alert and smiling. He has rhinorrhea, and his neck is supple. He has bruises below his knees. Which of the following is the most likely diagnosis?
Child abuse
Idiopathic epilepsy
Infantile spasms
Meningitis
Simple febrile seizure
253. A 4-month-old child presents with a 2-day history of vomiting and intermittent irritability. On examination, “currant jelly” stool is noted in the diaper, and a sausage-shaped mass is palpated in the right upper quadrant of the abdomen. Which of the following conditions is most likely to cause this?
Appendicitis
Diaphragmatic hernia
Giardiasis
Intussusception
Rotavirus gastroenteritis
254. During a routine yearly checkup, a 10-year-old boy is found to have 2+ proteinuria on urinalysis. Which of the following would be the most appropriate diagnostic test?
Electrolytes, BUN, and serum creatinine
Antistreptococcal antibodies
IVP
Renal ultrasound
A repeat urinalysis
255. An 18-month-old boy has received 5 days of amoxicillin for otitis media. He continues to have fever, and on physical examination, the right tympanic membrane is bulging with purulent fluid behind it. Which of the following is the best antibiotic to use?
Amoxicillin-clavulanic acid
Dicloxacillin
Cephalexin
Erythromycin
Penicillin
256. A newborn is noted to be quite jaundiced at 3 days of life. Laboratory data demonstrate his total bilirubin to be 17.8 mg/dL (direct bilirubin is 0.3 mg/dL). Which of the following factors is associated with an increased risk of neurologic damage in a jaundiced newborn?
Metabolic alkalosis
Increased attachment of bilirubin to binding sites caused by drugs such as sulfisoxazole
Hyperalbuminemia
Neonatal sepsis
Maternal ingestion of phenobarbital during pregnancy
257. A 2-hour-old full-term newborn infant is noted by the nursing staff to be having episodes of cyanosis and apnea. Per nursery protocol they place an oxygen saturation monitor on him. When they attempted to feed him, his oxygen levels drop into the 60s. When he is stimulated and cries, his oxygen levels increase into the 90s. Which of the following is the most important next step to quickly establish the diagnosis?
Echocardiogram
Ventilation perfusion scan
Passage of catheter into nose
Hemoglobin electrophoresis
Bronchoscopic evaluation of palate and larynx
258. A 2-year-old boy is brought to the pediatrician for a routine well-child visit. He has been growing and developing normally. He is starting to put words together into 2-word phrases. The boy eats a variety of foods including meats, vegetables, and fruits, and drinks 24-28 ounces (700ml) of whole milk each day. Past medical history is unremarkable. His mother has no concerns at today's visit. His physical examination is within normal limits. Laboratory results are as follows: Complete blood count Hemoglobin 9.4 g/dl Hematocrit 28% Mean corpuscular volume 64 fl Red cell distribution width 14% (normal 11.5%-16.0%) Reticulocytes 3.0% Platelets 240,000/µL Leukocytes 7,500/µL Blood, plasma, and serum Ferritin 100 ng/ml (7-140 ng/ml) Iron-binding capacity 300 µg/dl (240-450 µg/dl) Which of the following is the most likely cause for this child's anemia?
Abnormal utilization of iron
Cobalamin deficiency
Iron deficiency
Red blood cell membrane instability
Reduced production of globin chains
259. A 2-year-old boy with cough and difficulty breathing is brought to the emergency department by his mother. She says that he was well and playing with his toys until 2 hours prior to presentation. He is healthy, but his 6-year old brother has a peanut allergy. The patient's temperature is 36.7 C (98 F), blood pressure is 92/48 mmHg, pulse is 114/min, and respirations are 48/min. The patient's pulse oximetry shows 91 % on room air. Physical examination shows nasal flaring and grunting with both subcostal and intercostal retractions. Wheezing is heard in the right lung field; the left field is clear to auscultation. No rales or rhonchi are noted. The remainder of the physical examination is within normal limits. Supplementary oxygen is applied. Chest x-ray reveals mild hyperinflation of the right lung. Which of the following is the most appropriate next step in management of this child?
Bronchoscopy
Chest computed tomography scan
Chest physiotherapy
Chest tube placement
Intramuscular epinephrine
260. An 8-year-old boy is brought to the emergency department by his mother. Two weeks ago, he developed a low-grade fever followed by a persistent cough. He occasionally has severe paroxysms of cough that are precipitated by eating and do not resolve with antitussive medications. On physical examination, extensive subcutaneous emphysema over the anterior chest is noted. What is the most appropriate next step in the management of this patient?
Chest x-ray
Throat culture
Ear examination
CT scan of head
Blood cultures
261. The police bring a 14-year-old boy to the clinic after he was found setting fire to the neighbor's house. He has been previously arrested and warned by the cops twice. The first time was 15 months ago for stealing his neighbor's motorcycle. The second occasion was 6 months ago for a fight with his peers on the roadside. His parents arrive and tell you that he has been behaving this way for the past 3 years, and often argues at home. He steals money from them and tries to hurt the pets. Although they have not seen him using any drugs, they suspect that his behavior could be due to drugs. What is the most likely diagnosis?
Conduct disorder
Antisocial personality disorder
Oppositional defiant disorder
Attention deficit hyperactivity disorder
Substance abuse
262. A 9-year-old boy is brought to the emergency department due to an episode of seizures during class. His teacher says that the seizure started suddenly, and he fell to the ground with sustained flexion of the arms and extension of the legs, followed by clonic movements of the whole body. He has also been irritable lately, and his school performance has declined. His parents arrive shortly and say that they recently noticed he was lethargic and frequently complained of headaches, especially in the morning. His medical history is unremarkable. Physical examination reveals decreased muscle strength of the left side of the body, with brisk deep tendon reflexes in the left arm and leg. MRI of the head reveals a space-occupying lesion in the right parietal lobe. What tumor is most likely responsible for this patient's symptoms?
Benign astrocytoma
Medulloblastoma
Glioblastoma multiforme
Pinealoma
Craniopharyngioma
263. A 2-year-old child was recently adopted from India. She appears to be healthy, and there are no abnormal symptoms. Her weight and height are at 25th percentile for age. Her examination is normal. On screening, you find a positive TB skin test using purified protein derivative (PPD) with 20 mm induration. She has a history of receiving a BCG vaccination at birth. Your management plan is to do which of the following?
Obtain a chest x-ray and treat only if this is abnormal.
Obtain a chest x-ray and initiate prophylactic treatment with isoniazid (INH).
Repeat the test in 3-6 months.
Attribute the positive PPD to the BCG vaccination and do serial yearly x-rays.
Obtain sputum cultures.
264. A baby is born to a mother who is positive for hepatitis B surface antigen (HBsAg). Your plan is to do which of the following?
Give the infant a hepatitis B immunization.
Give the infant hepatitis B immune globulin (HBIG).
Give the infant a hepatitis B immunization and HBIG
Obtain liver function tests and hepatitis serology of the infant.
Give the HBIG only if the child is positive for HBsAg.
265. In an adolescent presenting with pityriasis rosea, which of the following would be an appropriate blood test to order?
Venereal Disease Research Laboratory (VDRL)
Complete blood count (CBC)
Hepatitis A immunoglobulin M (IgM)
Fluorescent antinuclear antibody (FANA)
Glucose
266. A 14-year-old girl presents to the emergency room for severe lower mid-abdominal pain that has been increasing over the past 12 hours. She describes it as crampy and sharp . Her last menstrual period was about 2 weeks ago. It was regular with no pain and lasted 4 to 5 days. She has had menstrual periods for nearly 2 years, and over the past 6 months she has noticed some cramping pain the first day or two of her menses. She denies sexual activity and has not had any vaginal discharge. Her bowel movements have been normal and she reports no urinary frequency, urgency, or burning with urination. Which of the following is the most likely diagnosis?
Dysmenorrhea
Ectopic pregnancy
Ovarian cyst
Pelvic inflammatory disease
Mittelschmertz
267. A 9-month-old boy is taken to the emergency room because of high fever. Breath sounds are diminished in the lungs, and a chest x-ray film shows lobar pneumonia. Probable streptococcal pneumonia is demonstrated in Gram's stain of sputum and then later confirmed by culture. The child responds to antibiotic therapy. A detailed history is taken during the admission, which reveals that this is the third episode of pneumonia in this young child; the two previous episodes occurred at 6 and 71/2 months of age. One of the mother's brothers had died of infection at age 9. Immunoglobulin studies demonstrate the following: IgG 80 mg/dL [normal 723-1685 mg/dL] IgA 60 mg/dL [normal 81-463 mg/dL] IgM 20 mg/dL [normal 48-271 mg/dL] Studies of the lymphocyte population demonstrate normal numbers of T cells and markedly decreased B cells. Which of the following is the most likely diagnosis?
Bruton agammaglobulinemia
Common variable immunodeficiency
DiGeorge syndrome
Transient hypogammaglobulinemia of infancy
Wiskott-Aldrich syndrome
268. A 2-year-old girl is brought to the clinic due to fever, irritability and lethargy for the past two weeks. Over the past two months, she has complained of intermittent abdominal discomfort and has lost weight. Abdominal palpation reveals a firm nodular mass in the right flank. No bruits are heard. Abdominal x-ray reveals multiple calcifications in the renal area. Urine examination reveals increased levels of homovanillic acid and vanillylmandelic acid. Which embryonic structure has this mass most likely arisen from?
Metanephros
Mesonephron
Paramesonephron
Neural crest cells
Lymphoid stem cells
269. A newborn baby is noted to have abnormal facies with low-set ears; a small receding jaw; and widely separated eyes. At 30 hours of age, the baby develops multiple muscle spasms. Serum studies are notable for calcium of 4.5 mg/dL. Which of the following is the most likely diagnosis?
Bruton's agammaglobulinemia
Common variable immunodeficiency
DiGeorge syndrome
Selective IgA deficiency
Transient hypogammaglobulinemia of infancy
270. An otherwise healthy 5-year-old boy is brought to the emergency department of a small hospital because of a simple 3-cm laceration in his forehead. The patient is crying and frightened. The practitioner decides to perform conscious sedation before suturing the laceration. Support personnel and equipment are available for monitoring the patient's vital status and carrying out resuscitation measures if needed. Which of the following is the most appropriate pharmacologic agent to achieve a safe level of conscious sedation in this situation?
Oral or rectal midazolam or diazepam
Concomitant opioid and benzodiazepine administration
Intravenous propofol
Intravenous ketamine
Concomitant analgesic-sedative agents and muscle relaxants
271. A 2-year-old boy has been doing well despite his diagnosis of tetralogy of Fallot. He presented to an outside ER a few days ago with a complaint of an acute febrile illness for which he was started on a “pink antibiotic.” His mother reports that for the past 12 hours or so he has had a headache and is more lethargic than normal. On your examination he seems to have a severe headache, nystagmus, and ataxia. Which of the following would be the most appropriate first test to order?
Urine drug screen
Blood culture
Lumbar puncture
CT or MRI of the brain
Stat echocardiogram
272. A 5-year-old girl is being evaluated for generalized swelling. Her blood pressure is 98/60 mm Hg. Her laboratory results show: Creatinine 0.7 mg/dl Albumin 1.6 g/dL Cholesterol 360 mg/dL Triglycerides 400 mg/dL C3 complement 120 mg/dL (normal, >80 mg/dL) Antinuclear antibody Negative Urinalysis 1 RBC/hpf, protein 400 mg/dL Which of the following is the most likely diagnosis?
Membranoproliferative glomerulonephritis
Membranous glomerulopathy
Minimal change disease
Postinfectious acute glomerulonephritis
Systemic lupus erythematosus
273. A 13-year-old girl presents with a 1-week history of a sore throat and a nonproductive cough. She has been previously healthy and has not been exposed to any other sick person. She has not been taking any medications. On examination, she has normal oxygen saturation and a low-grade fever. The remainder of the examination is unremarkable. Which of the following is the most appropriate pharmacotherapy?
Amoxicillin
Cefazolin
Erythromycin
Metronidazole
Trimethoprim-sulfamethoxazole
274. A 10-year-old girl is evaluated by a pediatrician. She is already 5'8" tall and is taller than other members of her family were at this age. Her arms are disproportionately long compared with her trunk, and her sternum is outwardly displaced. Her joints are hyperextensible, particularly at the knees. Ocular examination demonstrates dislocation of one lens. Which of the following is the most likely diagnosis?
Achondroplasia
Cutis laxa
Ehlers-Danlos syndrome
Marfan syndrome
Osteogenesis imperfect
275. A 6-year-old child is hospitalized for observation because of a short period of unconsciousness after a fall from a playground swing. He has developed unilateral pupillary dilatation, focal seizures, recurrence of depressed consciousness, and hemiplegia. Which of the following is the most appropriate management at this time?
Spinal tap
CT scan
Rapid fluid hydration
Naloxone
Gastric decontamination with charcoal
276. A 6-year-old boy is seen in the office for evaluation of polyuria. Further questioning reveals several months of headache with occasional emesis. Your physical examination reveals a child who is less than 5% for weight. He has mild papilledema. His glucose is normal, and his first urine void specific gravity after a night without liquids is 1.005 g/mL. Which of the following might also be expected to be seen in this patient?
Sixth nerve palsy
Unilateral cerebellar ataxia
Unilateral pupillary dilatation
Unilateral anosmia
Bitemporalhemianopsia
277. An 8-year-old boy is brought to the clinic by his mother, who states that he has been complaining of pain in both knees. The mother also states that he had a rash on his leg 3 weeks ago. She said it was there for almost 2 weeks and then went away. She describes the rash as reddish and circular, with a small clear area in the center. She said the rash was not itchy or painful. The child has also complained of headaches and muscle aches over the past several weeks. On questioning, the mother states that they were vacationing in Wisconsin about 1 month ago and the boy was hiking in the woods when he was bitten by a tick. Which of the following is the most likely diagnosis?
Babesiosis
Colorado tick fever
Lyme disease
Rocky Mountain spotted fever
Tularemia
278. A male child born to a 25-year-old Caucasian mother by normal vaginal delivery at 36 weeks of gestation is found to have a small face, a small jaw, and a prominence on the back of his head. There are no skin creases on the palmar aspect of his digits. There is overlapping of his fingers bilaterally, along with rocker bottom feet and limited hip abduction. Heart murmur is present. Which of the following cardiovascular abnormality is most likely seen in this patient?
Atrial septal defect
Ventricular septal defect
Supravalvular aortic stenosis
Conotruncal abnormality
Congenital heart block

279. The newborn nursery calls to notify you that a 1-day-old baby boy has developed abdominal distension and bilious emesis. Prenatal history was significant for areas of echogenic bowel seen on ultrasound. You order an abdominal radiograph; based on the results you order a contrast enema. Both are shown here. This infant is most likely to have which of the following?
Duodenal atresia
Cystic fibrosis
Gastroenteritis
Malrotation with volvulus
Hirschsprung disease
280. A 15-year-old girl is admitted to the hospital with a 6-kg weight loss, bloody diarrhea, and fever that have occurred intermittently over the previous 6 months. She reports cramping abdominal pain with bowel movements. She also reports secondary amenorrhea during this time. Stool cultures in her physician’s office have shown only normal intestinal flora. A urine pregnancy test was negative, while an erythrocyte sedimentation rate (ESR) was elevated. Her examination is significant for the lack of oral mucosal ulcerations and a normal perianal examination. Anti-Saccharomyces cerevisiae antibodies (ASCA) are negative, while anti-neutrophil cytoplasm antibodies (p-ANCA) are positive. You confirm your presumptive diagnosis with a rectal biopsy. In counseling her about her disease, which of the following statements would be true?
Inheritance is autosomal dominant.
Her risk of colon cancer is minimally elevated over the general population.
Intestinal strictures are common.
The most serious complication of her disease is toxic megacolon.
The intestinal involvement is separated by areas of normal bowel.
281. A 2-month-old female infant born at term is brought to the office for a well-baby visit. Her antenatal and birth histories are unremarkable. Her developmental milestones are all normal for her age. Ophthalmoscopic examination reveals a white reflex in the right eye. The rest of the examination is normal. What is the most appropriate next step in the management of this patient?
Covering the affected eye
Covering the normal eye
Referral to an ophthalmologist
Reassurance
Watchful waiting
282. A 6-year-old boy is brought to the physician by his mother with complaints of "inattentivity." His school teacher frequently complains about him, saying that he, "cannot sit still and just does not listen." He rarely completes his classroom assignments in time. When asked to run errands at home, he appears not to listen and continues to do whatever he is engaged in. He makes poor eye contact and has limited language skills compared to his peers. He usually prefers to play by himself. Which of these is the most likely diagnosis in this case?
Selective mutism
Attention deficit hyperactivity disorder
Undetected hearing impairment
Autism
Oppositional defiant disorder
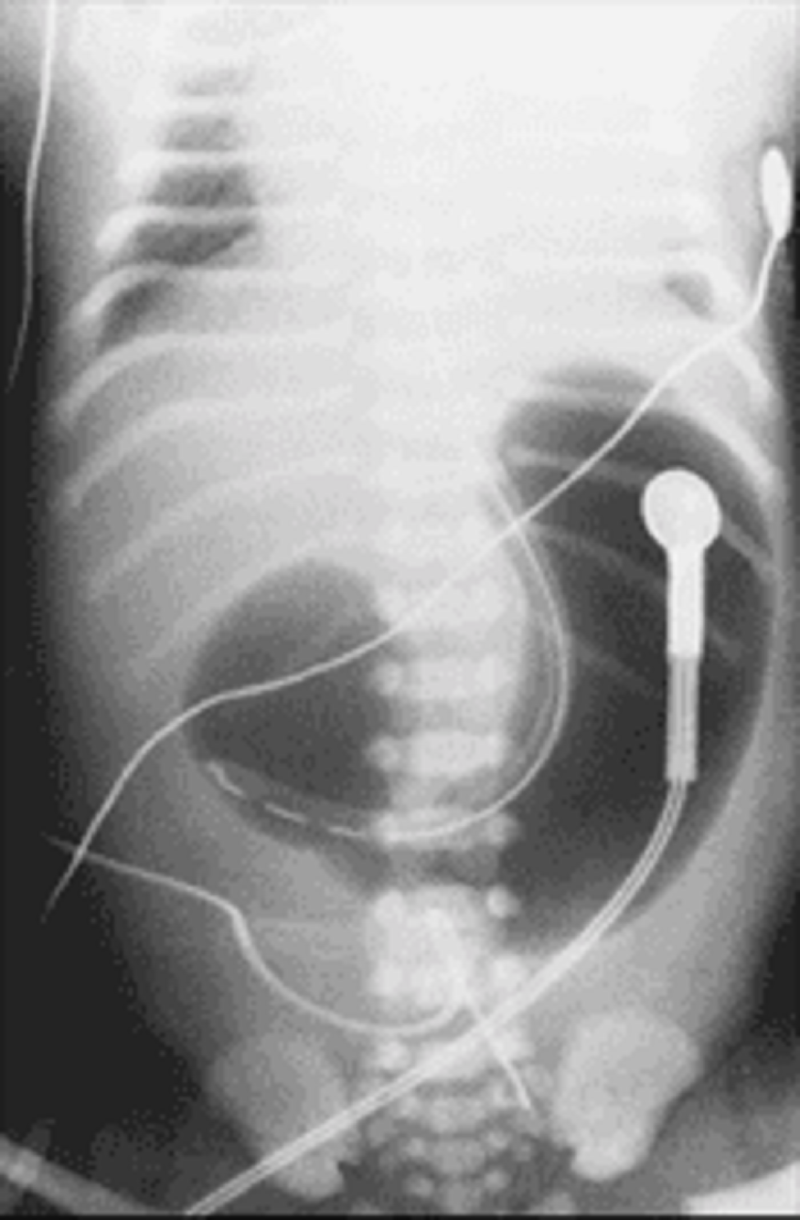
283. At the time of delivery, a woman is noted to have a large volume of amniotic fluid. At 6 hours of age, her baby begins regurgitating small amounts of mucus and bile-stained fluid. Physical examination of the infant is normal, and an abdominal x-ray is obtained (see below). Which of the following is the most likely diagnosis of this infant’s disorder?
Gastric duplication
Pyloric stenosis
Esophageal atresia
Duodenal atresia
Midgut volvulus
284. A 15-month-old Asian girl is brought to the physician's office because of persistent non-productive cough and skin rash. Other accompanying symptoms are a runny nose, sneezing and intermittent nasal obstruction. She has had these symptoms for the past four days. Her parents report that she seems to have lost interest in her usual activities and is irritable all the time. Her pulse is 130/min, temperature is 38.8C (102F), and respirations are 24/min. Her eyes are red and have a watery discharge; there is congestion that is more marked over the canthi; the inner conjunctiva has bluish white lesions on an erythematous background. Throat examination reveals erythema of the posterior pharyngeal wall and tonsillar pillars, and yellowish exudates on the tonsils. The buccal mucous membranes are red with bluish-white lesions. The face has blanching, erythematous "brick-red" maculopapular rash. No rash is present over the extremities. Cervical lymphadenopathy is noted. The lab results are as follows: Hct 46% WBC count 3,000/mm3 Platelet 160,000/mm3 Urine Dipstick ++ for proteins What is the most likely diagnosis?
Atypical measles
Human herpes virus 8
Kawasaki disease
Rubeola
Scarlet fever
285. A 17-year-old teenage girl presents to your office after having problems during sex with her boyfriend. She also states that she has been developing facial hair, which she has constantly been removing. She started her menstruations at the age of 13 and her cycles have always been regular. On examination she is obese but appears a little masculine and has an enlarged clitoris. Initial lab values are as follows: Serum LH 20 IU/L Serum FSH 10 IU/L 17 -hydroxyprogesterone 600ng/ml (Normal is 15ng/ml) Serum testosterone Normal Serum DHEA 4.0ng/ml (Normal is 4.2ng/ml) What is the most likely diagnosis?
Polycystic ovarian disease
Cushing's syndrome
Cushing's disease
Adrenal carcinoma
Congenital adrenal hyperplasia
286. A 2-week-old male infant is brought to the office by his 28-year-old primiparous mother for the evaluation of jaundice that was noted two days ago. The infant's stool has a lighter color. He is exclusively breastfed. The pregnancy was uncomplicated, and prenatal screening tests for TORCH organisms were all negative. The infant was delivered vaginally with no complications. His temperature is 37.2 C (99F), pulse is 140/min, respirations are 50/min, and capillary refill is < 2 sec. Examination reveals jaundiced skin and mucous membranes. Abdominal palpation reveals hepatomegaly. The initial investigations show the following: Hb 18.0 g/dl Hct 52% Bilirubin, Total 5 mg/dl Bilirubin, Direct 4 mg/dl Blood type 0 + (The mother's blood type is B-) Coombs' test Negative What is the most likely diagnosis?
Breast milk jaundice
Biliary atresia
Physiologic jaundice
Gilbert syndrome
Crigler-Najjar syndrome
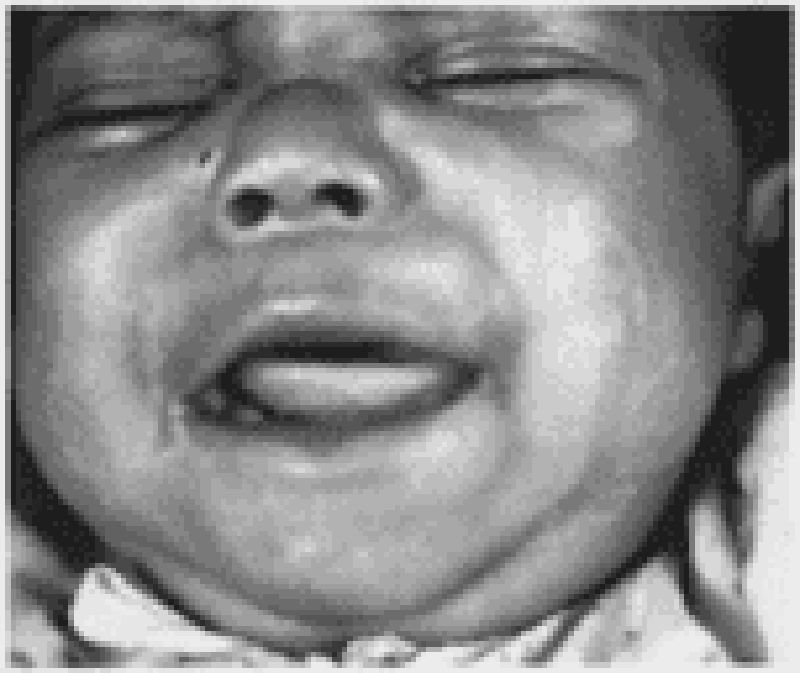
287. The infant in the following picture presents with hepatosplenomegaly, anemia, persistent rhinitis, and a maculopapular rash. Which of the following is the most likely diagnosis for this child?
Toxoplasmosis
Glycogen storage disease
Congenital hypothyroidism
Congenital syphilis
Cytomegalovirus disease
288. A premature infant develops respiratory distress several hours after birth. The infant is placed in an incubator with supplemental oxygen. The physician instructs the nurse to cover the infant's eyes to minimize the chance of damage by the high oxygen tension. Which of the following is characteristic of eye damage produced by exposure to high oxygen tensions in premature infants with respiratory distress?
Blood vessels in the vitreous
Cotton wool exudates in the retina
Microaneurysms of the retinal arterioles
Papilledema of the optic nerve head
Ulcers on the cornea
289. A 7-year-old boy is brought to the clinic by his mother, who states that he has been complaining of abdominal pain for 2-3 days. He has been afebrile, with no vomiting or diarrhea. His mother states she brought him to the office today because she noticed a rash on his legs that is getting worse, and he is now complaining of knee pain. On examination, there are palpable purpuric lesions on both legs and buttocks. He has pain around his ankle and knee joints with minimal swelling, and no warmth or erythema. Which of the following is the most likely diagnosis?
Dermatomyositis
Gastroenteritis
Henoch-Schonlein purpura
Juvenile rheumatoid arthritis
Kawasaki disease
290. A 5-year-old boy presents to the emergency department with 2-day history of fever, anorexia, loose stools, and yellow skin color. He attends a large daycare center. On physical examination, his temperature is 38.1 C (100.7 F), blood pressure is 88/56 mm Hg, pulse is 74/min, and respirations are 15/min. Initial laboratory evaluation reveals a total bilirubin of 1.8 mg/dL and alanine aminotransferase of 764 U/L. Which of the following is the most appropriate diagnostic test?
Hepatitis B surface antigen in serum
IgG for hepatitis A in serum
IgG for hepatitis B surface antigen in serum
IgM for hepatitis A in serum
Stool culture for hepatitis A
291. A new born infant is in respiratory distress and requires several attempts at resuscitation in the delivery room because of difficulty breathing and frequent cyanosis. The neonatologist notes that during crying, her breathing improves and breath and heart sounds are normal. Direct laryngoscopy is unremarkable as well. Deep inspirations by the neonate are ineffective. Which of the following is the most effective intervention?
Obtaining a chest x-ray film
Obtaining an electrocardiogram
Obtaining an arterial blood gas
Administering atropine
Inserting an oropharyngeal tube
292. A 7-year-old boy who has had pain in his right leg for 4 months is being evaluated. The pain is worse at night and is unrelenting, but it can usually be relieved with ibuprofen. On physical examination, there is localized tenderness over the anterior aspect of the right thigh. There is also mild atrophy of the affected limb. A radiograph of the femur reveals a radiolucent nidus with surrounding reactive sclerotic bone. Which of the following is the most likely diagnosis?
Brodie's abscess
Ewing sarcoma
Osteosarcoma
Osteoid osteoma
Stress fracture
293. A previously healthy 12-year-old boy is brought to the physician the day after a nocturnal crisis of difficulty breathing, chest tightness, and cough. He has a history of atopic dermatitis that resolved around 6 years of age. He now has no apparent respiratory distress. His breathing is regular, and his respirations are 12/min. Blood pressure, pulse, and temperature are normal. Chest examination reveals only a few crackles that quickly clear after coughing and mild end-expiratory wheezes. Which of the following is the most appropriate next step in diagnosis?
Arterial blood gas analysis
Bronchial provocation test with histamine or methacholine
Complete blood count
Chest x-ray examination
Spirometry before and after administration of a bronchodilator
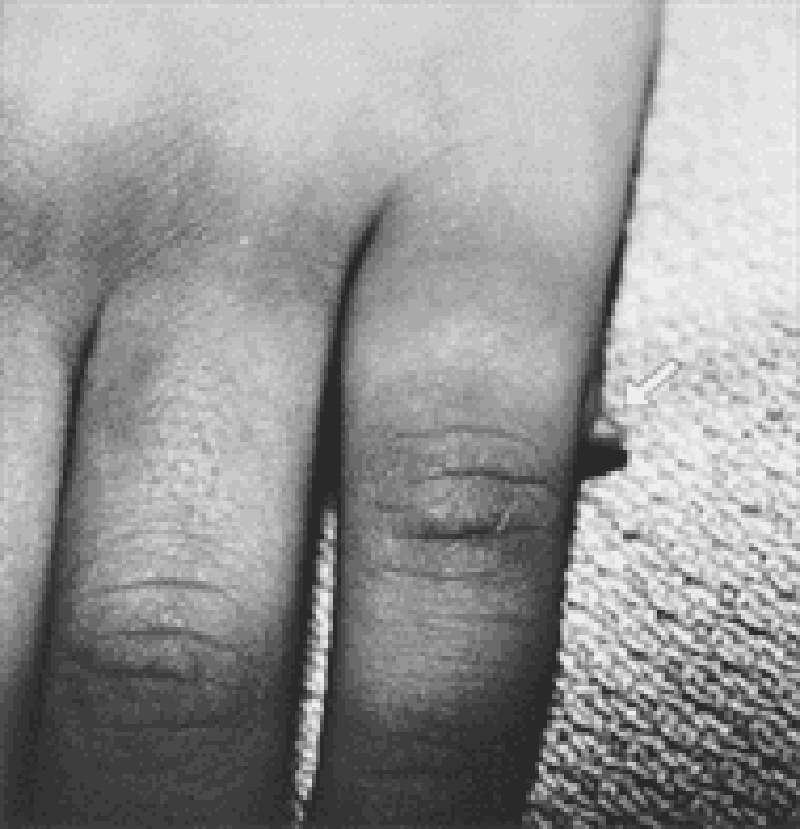
294. A well-appearing, 3200-g (7-lb, 1-oz) black infant is noted to have fifth finger (postaxial) polydactyly. The extra digit has no skeletal duplications and is attached to the rest of the hand by a threadlike soft tissue pedicle (see photograph). Appropriate treatment for this condition includes which of the following?
Chromosomal analysis
Excision of extra digit
Skeletal survey for other skeletal abnormalities
Echocardiogram
Renal ultrasound
295. A 2-year-old boy is brought to the office by his parents due to severe diarrhea since yesterday. He has had approximately 20 episodes of non-bloody, non-mucoid stool passage in the last twenty hours, and one episode of bilious vomiting. He is also feeding less than usual. He is febrile, tachycardic and moderately dehydrated. What is the most likely cause of his presentation?
Norwalk virus
E.coli
Campylobacter jejuni
Shigella
Rotavirus
296. Routine examination of an otherwise healthy kindergarten child with a history of asthma reveals a BP of 140/90 mmHg. Which of the following is the most likely cause of the hypertension?
Theophylline toxicity
Chronic lung disease
Renal disease
Coarctation of the aorta
Obesity
297. A 13-year-old girl presents with lethargy, fever, severe headache, and a stiff neck. On examination, a unilateral fixed, dilated pupil and papilledema are noted. Which of the following is the most appropriate initial step in managing this patient?
Administration of IV cefotaxime
Administration of IV mannitol
CT of the head
Intubation and hyperventilation
Performance of a lumbar puncture
298. A newborn infant requires repeated resuscitation in the delivery room because of failure to breathe and cyanosis. During spells of crying, which appear to alleviate the cyanosis, his breath and heart sounds are normal, as is direct laryngoscopy. Vigorous respiratory movements appear ineffectual. Immediate management of this infant consists of which of the following?
Obtaining a chest x-ray
Obtaining an electrocardiogram (ECG)
Arterial blood gas determinations
Inserting an oropharyngeal airway
Administration of naloxone
299. A 2-year-old boy is brought to the office by his mother because he has not started to walk yet. His birth history is significant for prolonged labor, and his APGAR scores at 1 and 5 minutes were 3 and 5, respectively. His older brother is 4 years old, and has a normal developmental history. On examination, the child has hypotonia, learning disabilities and hyperactive deep tendon reflexes. What is the most likely cause for the child's delayed milestones?
Cerebral anoxia
Congenital infection
Congenital muscular dystrophy
Friedreich's ataxia
Infantile spinal muscular atrophy
300. A 2-year-old boy is brought to the emergency department due to a cough and a "whistling" sound with breathing. Two days ago, he developed rhinorrhea, fever, a hoarse cry and a progressively worsening, harsh, "barky" cough. His immunizations are up-to-date. His 6-year-old brother also has cold symptoms. His temperature is 37.5C (99.5F), pulse is 140/min, and respirations are 36/min. On examination, he is alert, in mild respiratory distress, has a dry barking cough, hoarse cry, and some clear mucoid rhinorrhea. His pharynx is slightly injected, but without enlargement or asymmetry. The lungs are clear on auscultation. Lateral neck x-rays reveal a mildly narrowed subglottic region. What is the most likely diagnosis?
Epiglottitis
Croup
Laryngotracheobronchopneumonitis
Foreign body aspiration
Laryngeal diphtheria
301. You admitted to the hospital the previous evening a 1-year-old boy who presented with cough, fever, and mild hypoxia. At the time of his admission, he had evidence of a right upper lobe consolidation on his chest radiograph. A blood culture has become positive in less than 24 hours for Staphylococcus aureus. Approximately 20 hours into his hospitalization, the nurse calls you because the child has acutely worsened over the previous few minutes, with markedly increased work in breathing, increasing oxy- gen requirement, and hypotension. As you move swiftly to the child’s hospital room, you tell the nurse to order which of the following?
A second chest radiograph to evaluate for pneumatocele formation
A large-bore needle and chest tube kit for aspiration of a probable tension
pneumothorax
A change in antibiotics to include gentamicin
A sedative to treat the child’s attack of severe anxiety
A thoracentesis kit to drain his probable pleural effusion
302. A 15-year-old boy has been immobilized in a double hip spica cast for 6 weeks after having fractured his femur in a skiing accident. He has become depressed and listless during the past few days and has complained of nausea and constipation. He is found to have microscopic hematuria and a blood pressure of 150/100 mm Hg. Which of the following is the most appropriate course of action?
Request a psychiatric evaluation
Check blood pressure every 2 hours for 2 days
Collect urine for measurement of the calcium to creatinine ratio
Order a renal sonogram and intravenous pyelogram (IVP)
Measure 24-hour urinary protein
303. An adolescent with type 1 diabetes returns for a follow-up visit after his annual checkup last week. You note that his serum glucose is elevated and his glycosylated hemoglobin (hemoglobin A1C) is 16.7%. This finding suggests poor control of his diabetes over at least which of the following time periods?
8 hours
1 week
1 month
2 months
6 months
304. A 6-year-old male presents to the physician with eyelid swelling. His mother noted an insect bite on his left cheek yesterday, and states that this morning his left eyelid was completely swollen shut and painful. He has not had a fever, fatigue, headache, or rhinorrhea. On examination, he is afebrile. The left eyelid is erythematous, tender to palpation, and swollen shut. When trying to clinically distinguish between preseptal and orbital cellulitis, which of the following findings is most likely to be seen with preseptal cellulitis?
Decreased eye movements
Decreased visual acuity
Proptosis
Eyelid discoloration
Fever
305. A 41-year-old woman who is 32-weeks pregnant presents to the emergency department in labor. Her pregnancy has been complicated by gestational hypertension. Her medical history is otherwise unremarkable. She does not abuse alcohol, tobacco, or illicit drugs. Despite medical interventions, her preterm labor cannot be arrested, and she delivers a 2 kg (41b, 5oz) female infant. Both she and the child do well after delivery. Which of the following is true regarding immunizations for this infant?
Immunizations should be given according to the chronologic age
Immunizations should be given according to the gestational age.
Toxoid and polysaccharide vaccines should be given according to chronologic age, but live attenuated vaccines should be given according to the gestational age.
Immunizations should be started after she reaches 3 kg.
Immunizations should be given when allergen testing confirms an immune response
306. As you are about to step out of a newly delivered mother’s room, she mentions that she wants to breast-feed her healthy infant, but that her obstetrician was concerned about one of the medicines she was taking. Which of the woman’s medicines, listed below, is clearly contraindicated in breast-feeding?
Ibuprofen as needed for pain or fever
Labetalol for her chronic hypertension
Amphetamines for her attention deficit disorder
Carbamazepine for her seizure disorder
Acyclovir for her HSV outbreak
307. A recovering premature infant who weighs 950 g (2 lb, 1 oz) is fed breast milk to provide 120 cal/kg/d. Over the ensuing weeks, the baby is most apt to develop which of the following?
Hypernatremia
Hypocalcemia
Blood in the stool
Hyperphosphatemia
Vitamin D toxicity
308. A 15-year-old female presents to your office with secondary amenorrhea. As part of your evaluation, you find that she is pregnant. After informing her of the pregnancy, you continue to explain that young mothers have a higher risk of several pregnancy-related complications, including which of the following?
Twin gestation
Low-birth weight infants
Hypotension
Excessive weight gain
Infants with genetic defects
309. A 16-year-old boy who is the backup quarterback for the local high school team is in your office complaining of worsening acne. For the last few months he has noted more acne and more oily hair. On his examination, you note gynecomastia and small testicular volume. He is SMR 5. Which of the following drugs of abuse is the likely explanation for all of his findings?
Cocaine
Oxandrolone
Marijuana
Toluene
Methylenedioxymethamphetamine
310. A 4-year-old Caucasian boy is brought to his physician's office for a health maintenance exam. He will be starting preschool soon, and his parents want to make sure that he is in optimal health. The child has no complaints, and is generally happy. His medical history is significant for pneumonia as a newborn, and three episodes of otitis media since birth. He does not take any medications on a regular basis. His newborn screening test results are normal. His developmental milestones are at par with his age. He lives with his parents in a middle-class, suburban house built in 1981. Which of the following is the most appropriate next step for this child's primary care?
Screen him for inguinal hernias
Serum lead level
Meningococcal vaccine
Vision exam
Rotavirus vaccine
311. A term infant is born to a known HIV-positive mother. She has been taking antiretroviral medications for the weeks prior to the delivery of her infant. Routine management of the healthy infant should include which of the following?
Admission to the neonatal intensive care unit for close cardiovascular monitoring
HIV ELISA on the infant to determine if congenital infection has occurred
A course of zidovudine for the infant
Chest radiographs to evaluate for congenital Pneumocystis carinii
Administration of IVIG to the baby to decrease the risk of perinatal HIV infection
312. Initial examination of a full-term infant weighing less than 2500 g (5 lb, 8 oz) shows edema over the dorsum of her hands and feet. Which of the following findings would support a diagnosis of Turner syndrome?
A liver palpable to 2 cm below the costal margin
Tremulous movements and ankle clonus
Redundant skin folds at the nape of the neck
A transient, longitudinal division of the body into a red half and a pale half
Softness of the parietal bones at the vertex
313. A 3-year-old boy is brought to the office by his Caucasian mother because his speech is difficult to understand. He is a very slow learner, is unusually calm, stays to himself, doesn't hug his parents, prefers to play by himself, speaks in mumbles, and repetitively tries to make towers with cubes. He becomes very aggressive if he is stopped from his activities. He was born at term from an uncomplicated pregnancy and delivery, and his physical growth has been normal. His brother used to be aggressive as a child, and was diagnosed with attention deficit hyperactivity disorder. In the office, the patient is sitting quietly and trying to make towers with cubes. He seems to be oblivious of his environment. On calling his name thrice, he turns towards you once and then resumes playing with the cubes. What do you tell his mother?
He has attention deficit hyperactivity disorder and would benefit from methylphenidate
This could be autism and would benefit from antipsychotics
He has hearing problems and he needs ear, nose and throat evaluation
He has autism and will need special behavioral and educational programs
His diagnosis is Asperger syndrome
314. A father brings his 3-year-old daughter to the emergency center after noting her to be pale and tired and with a subjective fever for several days. Her past history is significant for an upper respiratory infection 4 weeks prior, but she had been otherwise healthy. The father denies emesis or diarrhea, but does report his daughter has had leg pain over the previous week, waking her from sleep. He also reports that she has been bleeding from her gums after brushing her teeth. Examination reveals a listless pale child. She has diffuse lymphadenopathy with splenomegaly but no hepatomegaly. She has a few petechiae scattered across her face and abdomen and is mildly tender over her shins, but does not have associated erythema or joint swelling. A CBC reveals a leukocyte count of 8,000/L with a hemoglobin of 4 g/dL and a platelet count of 7,000/L. The automated differential reports an elevated number of atypical lymphocytes. Which of the following diagnostic studies is the most appropriate next step in the management of this child?
Epstein-Barr virus titers
Serum haptoglobin
Antiplatelet antibody assay
Reticulocyte count
Bone marrow biopsy
315. While bathing her newly-received 2-year-old son, a foster mother feels a mass in his abdomen. A thorough medical evaluation of the child reveals aniridia, hypospadias, horseshoe kidney, and hemihypertrophy. Which of the following is the most likely diagnosis for this child?
Neuroblastoma
Wilms tumor
Hepatoblastoma
Rhabdomyosarcoma
Testicular cancer
316. A 7 -year-old Caucasian male with a history of peanut allergy develops sudden shortness of breath after lunch at school. On physical examination, his blood pressure is 70/50 mmHg and his heart rate is 130/min. Inspirations and expirations are labored and noisy. Which of the following is the best initial treatment?
Albuterol nebulizer
Subcutaneous epinephrine injection
Intravenous steroids
Intravenous diphenhydramine
Endotracheal intubation
317. A 1-year-old boy is brought to the pediatrician for a routine visit. While talking to his mother, she reports that they moved into an old house several months ago and are in the process of renovating. The child eats table food and drinks whole milk. His height, weight, and head circumference are all at the 50th percentile for his age. Physical examination is normal. The results of a fingerstick blood test are shown below: Hemoglobin 1 0.5 g/dL Hematocrit 30.0% Lead level 12 μg/dL (Normal < 10 μg/dL) Which of the following is the most appropriate next step in management?
Remove the child from the house
Check a serum lead level
Initiate chelation therapy with dimercaprol
Initiate chelation therapy with dimercaptosuccinic acid (DMSA, succimer)
Recheck lead level in one month
318. A 7-day-old boy is admitted to a hospital for evaluation of vomiting and dehydration. Physical examination is otherwise normal except for minimal hyperpigmentation of the nipples. Serum sodium and potassium concentrations are 120 mEq/L and 9 mEq/L (without hemolysis), respectively; serum glucose is 40 mg/dL. Which of the following is the most likely diagnosis?
Pyloric stenosis
Congenital adrenal hyperplasia
Secondary hypothyroidism
Panhypopituitarism
Hyperaldosteronism
319. A 14-year-old boy presents with the complaint of “breast swelling.” The boy reports that he has been in good health and without other problems, but has noticed over the past month or so that his left breast has been “achy” and that he has now noticed some mild swelling under the nipple. He has never seen discharge; the other breast has not been swelling; and he denies trauma. Your examination demonstrates a quarter-sized area of breast tissue under the left nipple that is not tender and has no discharge. The right breast has no such tissue. He has a normal genitourinary examination, and is Tanner stage 3. Which of the following is the best next course of action?
CT scan of the pituitary
Measurement of serum luteinizing hormone (LH) and follicle-stimulating hormone (FSH)
Measurement of serum testosterone
Reassurance of the normalcy of the condition
Chromosomes
320. A 12-week-old female infant is brought to the office by her mother due to a three- week history of weakness, poor appetite, and choking spells during feeding. Other accompanying symptoms include excessive sleeping, constipation and apathy. Her prenatal history is unremarkable. She was delivered vaginally at 38 weeks of gestation. Her weight and length at birth were within normal range. She is exclusively breastfed. Her mother's family history is unremarkable. The identity and family history of her father are unknown. The pertinent physical findings include apathy, weakness, hypotonia, large tongue, sluggish movement, abdominal bloating, and an umbilical hernia. Based on the given information, what is the most likely diagnosis?
Infant botulism
Werdnig-Hoffmann syndrome
Myotonic congenital myopathy
Congenital hypothyroidism
Myasthenia gravis
321. While making rounds in the newborn nursery, the nurses ask you to examine a 2-day- old infant who is not feeding well. The nurse reports that the infant is irritable, is not sleeping well, and has had several episodes of vomiting and loose stools today. A review of the maternal history reveals that she had poor prenatal care and the pregnancy was complicated by intrauterine growth restriction. On examination, the infant is diaphoretic and has a high- pitched cry. The infant is also noted to have occasional sneezing and is mildly tachypneic. No dysmorphic features are noted and the remainder of the examination is unremarkable. This infant's symptoms are most likely caused by prenatal exposure to which of the following?
Valproic acid
Phenytoin
Alcohol
Cocaine
Heroin
322. A 2-year-old boy is being followed for congenital cytomegalovirus (CMV) infection. He is deaf and developmentally delayed. The child’s mother informs you that she has just become pregnant and is concerned that the new baby will be infected and may develop serious consequences. Which of the following is true?
The mother has antibodies to CMV that are passed to the fetus.
The mother’s infection cannot become reactivated.
The likelihood that the new baby will become clinically ill is approximately 80%.
Termination of pregnancy is advised.
The new infant should be isolated from the older child.
323. A full-term infant is born after a normal pregnancy; delivery, however, is complicated by marginal placental separation. At 12 hours of age, the child, although appearing to be in good health, passes a bloody meconium stool. For determining the cause of the bleeding, which of the following diagnostic procedures should be performed first?
A barium enema
An Apt test
Gastric lavage with normal saline
An upper gastrointestinal series
A platelet count, prothrombin time, and partial thromboplastin time
324. A 1 0-year-old boy is brought to the emergency department due to abdominal pain and bloody diarrhea. The mother says that he was "fine" a few days ago, and then suddenly became ill. Physical examination shows a pale and jaundiced child. There is diffuse abdominal tenderness and 2+ pedal edema. Laboratory studies show anemia, thrombocytopenia and renal insufficiency. What is the most likely cause of the patient's symptoms?
Vibrio cholera
Escherichia coli
Crohn's disease
Lactose intolerance
Salmonella poisoning
325. A 2-year-old boy presents to the emergency department (ED) with severe wheezing. His symptoms have not improved even after three treatments with nebulizers. This is his third trip to the ED in the past two weeks. In the ED, he is given a dose of intravenous steroids, but continues to wheeze. On auscultation, there is no air entry bilaterally. His chest x-ray result is normal. His oxygen saturation is 91% on 6 liters of oxygen. What is the next best step in the management of this patient?
Start theophylline
Tracheostomy
Mechanical ventilation
Racemic epinephrine
Intravenous antibiotics
326. A 16-year-old girl is brought to the office due to abdominal pain and bloody diarrhea for the past two days. Her immunizations are up to date. Her past medical history is unremarkable. On examination, she appears lethargic and weak. Her skin turgor is poor, face and extremities are swollen, and skin appears yellow. Abdominal examination shows moderate non-localized, abdominal pain. Laboratory studies show: Hb 64 g/dl Hct 26.9% Platelets 45,000/mm3 Creatinine 2.3 mg/dl Total bilirubin 5.0 mg/dl What is the most common complication of the patient's condition?
Renal damage
Liver damage
Bone marrow failure
Pneumonia
Bowel obstruction
327. A fully immunized 2-year-old presents to the emergency room with several days of low-grade fever, barking cough, and noisy breathing. Over the past few hours he has developed a fever of 40°C (104°F) and looks toxic. He has inspiratory and expiratory stridor. The family has not noticed drooling, and he seems to be drinking without pain. Direct laryngoscopy reveals a normal epiglottis. The management of this disease process includes which of the following?
Intubation and intravenous antibiotics
Inhaled epinephrine and oral steroids
Inhaled steroids
Observation in a cool mist tent
Oral antibiotics and outpatient follow-up
328. An obese Caucasian father brings his 1 0-year-old obese son to your office. The father states that he was recently diagnosed with high cholesterol levels and coronary artery disease. Even though his son is asymptomatic, he is worried about the obesity. Which of the following best explains the next best step in management?
Get a fasting lipid profile
Get a screening test for total cholesterol level
Advise parents to start him on a low cholesterol diet
Evaluate him for coronary artery disease
Advise parents to start him on a regular physical exercise schedule

329. A 24-year-old woman arrives in the emergency center in active labor. She is at term, but received no prenatal care after 16 weeks of gestation when she lost her insurance coverage. The mother has an uncomplicated vaginal delivery. You are paged shortly after birth when the baby is noted to have respiratory distress. The infant has diminished breath sounds on the left, and the PMI is shifted toward the right. A chest radiograph is shown. The NG tube you placed earlier reveals the stomach to be below the diaphragm. Which of the following is the most likely diagnosis at this point?
Congenital cystic adenomatoid malformation
Congenital diaphragmatic hernia
Bronchogenic cysts
Congenital lobar emphysema
Congenital pneumonia
330. A 4-year-old boy, whose past medical history is positive for three urinary tract infections, presents with a blood pressure of 135/90 mm Hg. He is likely to exhibit which of the following symptoms or signs?
Multiple cranial nerve palsy
Headache
Hyporeflexia
Increased urine output
Right ventricular hypertrophy
331. The 1-year-old boy in the photograph below, who recently had a circumcision, requires an additional operation on his genitalia that will probably eliminate his risk of which of the following?
Testicular malignancy
Decreased sperm count
Torsion of testes
Urinary tract infection
Epididymitis
332. A previously healthy 3-year-old boy brought in by his parents for help with potty training. The boy refuses to use the toilet. If his parents try to place him on the toilet, he becomes upset and cries. He has regular urination in his diaper. He has 1-2 soft bowel movements a day. In the office, you note that the child speaks in short sentences that are mostly understandable. He runs well and can climb up on the examination table without help. His physical examination is unremarkable. Which of the following is the next best step in the management of this patient?
Increase fiber in his diet
Put him on the toilet at regularly scheduled times
Use a positive reward system
Stop potty training attempts for several months
Perform a urinalysis
333. A 6-year-old boy is brought to the ER with a two-day history of difficulty walking. He is dragging his right leg and seems to have weakness in his right arm. He also complains of headaches. The family just emigrated from Eastern Europe. According to his parents, the child suffers from delayed growth compared to his peers and does not like to engage in active play. His lips and fingers turn blue when he cries. His vital signs today are a blood pressure of 100/70 mmHg, pulse of 90/min, temperature of 38.3 0C (102.0 0F), and respiratory rate of 22/min. Which of the following is most likely responsible for his current complaints?
Glycogen storage disorder
Demyelinating disorder
Malignancy
Brain abscess
Malformation of the central nervous system
334. A 15-year-old is participating in high school football practice in August in Texas. He had complained of headache and nausea earlier in practice, but kept playing after a cup of water. He is now confused and combative. He is dizzy and sweating profusely. His temperature is 41°C (105.8°F). Therapy should consist of which of the following?
Provide oral rehydration solutions
Administer acetaminophen rectally
Order to rest on the bench until symptoms resolve
Initiate whole body cold water immersion
Tell him to go take a shower and rest until the next day’s practice

335. The term infant pictured below weighs 2200 g (4 lb, 14 oz). He is found to have a ventricular septal defect on cardiac evaluation. This infant appears to have features consistent with which of the following?
Perinatal phenytoin exposure
Trisomy 21
Alport syndrome
Fetal alcohol syndrome
Infant of diabetic mother
336. A previously healthy 4-year-old child is brought to the physician for a school physical for kindergarten. His mother has brought in his immunization record and reports that received all his immunizations prior to age 2. He has received only a yearly influenza vaccine since age 2. His physical examination is unremarkable. Which of the following immunizations should he be given during this visit?
Haemophilus influenza type B #4
Pneumococcal #3
Inactivated polio #4
Measles-mumps-rubella #1
Hepatitis B #3
337. A 6-week-old child is being evaluated for a fever of unknown etiology. As part of the laboratory evaluation, a urine specimen was obtained that grew E coli with a colony count of 2000/L. These findings would be definite evidence of a urinary tract infection if which of the following is true about the sampled urine?
It has a specific gravity of 1.008.
It is from a bag attached to the perineum of an uncircumcised boy.
It is from an ileal-loop bag.
It is from a suprapubic tap.
It is the first morning sample.
338. A previously healthy 16-year-old girl presents to the emergency center with the complaint of “falling out.” She was with her friends at a local fast food restaurant when she felt faint and, according to her friends, lost consciousness for about a minute. There was no seizure activity noted, but the friends did notice her arms twitching irregularly. She is now acting normally. She denies chest pain or palpitations, and her electrocardiogram (ECG) is normal. Further management of this patient should include which of the following?
Obtain an EEG
Refer to a child psychiatrist
Begin -blocker therapy
Encourage adequate fluid and salt intake
Obtain serum and urine drug screens
339. A female infant is born by vaginal delivery at 39 weeks' gestational age without any significant complications. There is no history of any genetic diseases in the family. She is noted to have a port-wine stain on the right side of her face that is 4 cm in length and 3 cm in width. Which of the following treatment modalities offers the best palliation for cosmetic purposes?
Cryosurgery
Pulsed dye laser
Radiation therapy with gamma particles
Skin grafting
Topical corticosteroid therapy
340. A 4-year-old, apparently healthy child is examined by a pediatrician. The pediatrician hears a loud systolic ejection murmur with a prominent systolic ejection click. He also hears a soft, early diastolic murmur. Both murmurs are heard best at the upper right sternal border. ECG shows left ventricular hypertrophy. Which of the following is the most likely diagnosis?
Aortic valve stenosis
Atrial septal defect
Tetralogy of Fallot
Transposition of great arteries
Ventricular septal defect
341. A 19-year-old primiparous woman develops toxemia in her last trimester of pregnancy and during the course of her labor is treated with magnesium sulfate. At 38 weeks’ gestation, she delivers a 2100-g (4-lb, 10-oz) infant with Apgar scores of 1 at 1 minute and 5 at 5 minutes. Laboratory studies at 18 hours of age reveal a hematocrit of 79%, platelet count of 100,000/μL, glucose 41 mg/dL, magnesium 2.5 mEq/L, and calcium 8.7 mg/dL. Soon after, the infant has a generalized convulsion. Which of the following is the most likely cause of the infant’s seizure?
Polycythemia
Hypoglycemia
Hypocalcemia
Hypermagnesemia
Thrombocytopenia
342. An infant who appears to be of normal size is noted to be lethargic and somewhat limp after birth. The mother is 28 years old, and this is her fourth delivery. The pregnancy was uncomplicated, with normal fetal monitoring prior to delivery. Labor was rapid, with local anesthesia and intravenous meperidine (Demerol) administered for maternal pain control. Which of the following therapeutic maneuvers is likely to improve this infant’s condition most rapidly?
Intravenous infusion of 10% dextrose in water
Administration of naloxone (Narcan)
Administration of vitamin K
Measurement of electrolytes and magnesium levels
Neurologic consultation
343. At 43 weeks’ gestation, a long, thin infant is delivered. The infant is apneic, limp, pale, and covered with ―pea soup‖ amniotic fluid. Which of the following is the best first step in the resuscitation of this infant at delivery?
Intubation and suction of the trachea; provision of oxygen
Artificial ventilation with bag and mask
Chest compressions
Administration of 100% oxygen by mask
Catheterization of the umbilical vein
344. A 4-year-old child presents with an enlarged submandibular node that is 4 cm in diameter, nontender, and not fluctuant. The node has been enlarged for about 4 weeks, and there is no history of fever or contact with any person who was ill. A CBC is normal, and a Mantoux test with 5 tuberculin units of PPD shows 6 mm of induration. Which of the following is the most likely diagnosis?
Cat-scratch fever
Acute pyogenic lymphadenitis
Acute lymphoblastic leukemia
Tuberculous lymphadenitis
Atypical mycobacteria lymphadenitis
345. A 4-year-old child with grade III vesicoureteral reflux has recurrent UTIs despite adequate antibiotic prophylaxis. Which of the following is the most appropriate next step in the treatment of this patient?
IV antibiotic treatment for 2 weeks
Repeat renal scan
Renal arteriogram
Antireflux surgery
Addition of vitamin C (ascorbic acid) to the treatment regimen
346. A 2-week-old infant presents with hepatosplenomegaly and a thick, purulent, bloody nasal discharge. Coppery, oval, maculopapular skin lesions are present in an acral distribution. The neurologic examination is normal, including head circumference. Which of the following is the most likely cause of this congenital infection?
Cytomegalovirus (CMV)
HSV
GBS
T. gondii
T. pallidum
347. A 7-month-old patient presents with a history of 3 days of fever to 104°F, which resolved the same day that an exanthem erupted. The exanthem is prominent on the neck and trunk. It is macular, with discrete lesions 3-5 mm in diameter. Which of the following is the most likely diagnosis?
Erythema infectiosum
Measles
Roseola infantum
Rubella
Scarlet fever
348. A newborn infant has respiratory distress and trouble feeding in the nursery. The mother has no significant medical history, but the pregnancy was complicated by decreased fetal movement. On physical examination, you note that aside from shallow respirations and some twitching of the fingers and toes, the infant is not moving, and is very hypotonic. In the mouth there is pooled saliva and you note tongue fasciculations. Deep tendon reflexes are absent. Spinal fluid is normal. Appropriate statements about this condition include which of the following statements?
The condition is caused by the absence of the muscle cytoskeletal protein dystrophin.
The condition is caused by the degeneration of anterior horn cells in the spinal cord.
The condition is caused by the antibodies that bind the acetylcholine receptor at the postsynaptic muscle membrane.
The condition is caused by progressive autoimmune demyelination.
The condition is caused by birth trauma.
349. A 3-year-old boy’s parents complain that their child has difficulty walking. The child rolled, sat, and first stood at essentially normal ages and first walked at 13 months of age. Over the past several months, however, the family has noticed an increased inward curvature of the lower spine as he walks and that his gait has become more “waddling” in nature. On examination, you confirm these findings and also notice that he has enlargement of his calves. Which of the following is the most likely diagnosis?
Occult spina bifida
Muscular dystrophy
Brain tumor
Guillain-Barrésyndrome
Botulism
350. Your 6-year-old son awakens at 1:00 AM screaming. You note that he is hyperventilating, is tachycardic, and has dilated pupils. He cannot be consoled, does not respond, and is unaware of his environment. After a few minutes, he returns to normal sleep. He recalls nothing the following morning. Which of the following is the most likely diagnosis?
Seizure disorder
Night terrors
Drug ingestion
Psychiatric disorder
Migraine headache
351. A 5-year-old febrile child presents with swelling of the right eyelid. Proptosis and limitation of ocular movements is noted. Which of the following is the most likely diagnosis?
Retinoblastoma
Orbital cellulitis
Periorbital cellulitis
Neuroblastoma
Hyphema
352. A 6-month-old infant is diagnosed with her first episode of otitis media. She does not have any allergies to medications. Which of the following medications would be the recommended initial therapy for this infant?
Amoxicillin
Amoxicillin-clavulanic acid
Cephalexin
Ceftriaxone
Erythromycin
353. A 10-year-old boy is brought in with a chief complaint of multiple colds. On further questioning, you elicit a history of chronic, clear nasal discharge with no seasonal variation. Other symptoms include sneezing, itching of the nose and eyes, as well as tearing and occasional eye redness. Some relief is obtained with an over-the-counter cold medicine containing antihistamine and a decongestant. His history suggests which of the following?
Nasal foreign body
Immunologic deficiency
Rhinitis medicamentosa
Chronic sinusitis
Allergic rhinitis

354. A 15-year-old boy comes to the physician with left shoulder joint pain and swelling. He has had these symptoms for the past 3 months and they are getting progressively worse. He has no fever, weight loss, or night sweats. The patient lifts weights and plays baseball 5 days a week. He has taken acetaminophen and ibuprofen with little relief. Examination shows a tender mass at the left proximal humerus. Range of motion is normal. Laboratory evaluation shows elevated alkaline phosphatase, erythrocyte sedimentation rate, and lactate dehydrogenase. X-ray of the shoulder is shown in the photograph below. Which of the following is the most likely diagnosis?
Ewing sarcoma
Osteoid osteoma
Osteomyelitis
Osteosarcoma
Stress fracture
355. A 7-year-old boy is brought to your office with a sore throat, decreased appetite, and nausea. His past medical history is insignificant. All of his vaccinations are up-to-date. He has no known allergies. His temperature is 39.0°C (102.5°F), blood pressure is 110/70 mmHg, pulse is 104/min, and respirations are 16/min. On examination, the pharynx and tonsils are red, sv1ollen, and have white exudates on their surface. There is also bilateral tender cervical lymphadenopathy. The rapid diagnostic test for streptococcal antigen is positive. What is the most appropriate next step in management?
Throat culture
Monospot test
Antistreptolysin O antibodies
Oral penicillin V
Oral azithromycin
356. A 4-day-old infant presents with yellow discoloration of the skin and sclera. The baby was born at term by a normal vaginal delivery. Pregnancy was uncomplicated; there were no risk factors for sepsis and no history of maternal alcohol or drug use. The baby is breast-fed and has been nursing every 2 hours, about 10 minutes at each breast. The bilirubin level is 15 mg/dL (all unconjugated), the hematocrit is 45%, and the Coombs test is negative. Which of the following is the most likely diagnosis?
Congenital biliary atresia
Soimmune hemolytic disease
Crigler-Najjar syndrome
Breast milk jaundice
Breast-feeding jaundice
357. A previously healthy, active, 18-month-old African American child presents with unilateral nasal obstruction and foul-smelling discharge. The child’s examination is otherwise unremarkable. Which of the following is the most likely diagnosis?
Foreign body
Nasal polyps
Frontal sinusitis
Deviated septum
Choanal atresia
358. A 7-year-old child is brought by his mother for a school physical. His growth parameters show his height to be 50th percentile and his weight to be significantly higher than 95th percentile. His mother complains that he always seems sleepy during the day and that he has started complaining of headaches. His second-grade teacher has commented that he has difficulty staying awake in class. His mother complains that he wakes up the whole house with his snoring at night. Which of the following is the most appropriate next step in evaluating and managing this condition?
Try steroids to decrease tonsillar and adenoid hypertrophy.
Refer to an otolaryngologist for tonsillectomy and adenoidectomy.
Arrange for continuous positive airway pressure (CPAP) at home.
Arrange for home oxygen therapy for use at night.
Arrange for polysomnography.
359. A 3-year-old boy is brought to the emergency department three hours after having a seizure. He has been having severe diarrhea for the last three days. His mother recently read about the importance of maintaining adequate hydration during diarrhea, so she had been giving him a lot of milk mixed with water. On examination, his vital signs are stable and mucus membranes are moist. Initial lab results are: Hb 13 g/dl WBC 6,000/mm3 Platelets 300,000/mm3 Blood Glucose 98 mg/dl Serum Na 120 mEq/L Serum K 34 mEq/L Chloride 92 mEq/L BUN 22 mg/dl Creatinine 1.2 mg/dl What is the most likely cause of this patient's seizure?
SIADH
Water intoxication
Severe dehydration
Acute renal failure
Sepsis
360. The state laboratory calls your office telling you that a newborn infant, now 8 days old, has an elevated thyroid stimulating hormone (TSH), and low thyroxin (T4) on his newborn screen. If this condition is left untreated, the infant is likely to demonstrate which of the following in the first few months of life?
Hyperreflexia
Hyperirritability
Diarrhea
Prolonged jaundice
Hyperphagia
361. A 1-year-old boy presents with the complaint from his parents of “not developing normally.” He was the product of an uneventful term pregnancy and delivery, and reportedly was normal at birth. His previous health-care provider noted his developmental delay, and also noted that the child seemed to have an enlarged spleen and liver. On your examination, you confirm the developmental delay and the hepatosplenomegaly, and also notice that the child has short stature, macrocephaly, hirsutism, a coarse facies, and decreased joint mobility. Which of the following is the most likely etiology of his condition?
Beckwith-Wiedemann syndrome
Crouzon syndrome
Trisomy 18 (Edwards syndrome)
Jeune syndrome
Hurler syndrome
362. A 22-year-old Caucasian female who has received no prenatal care experiences a stillbirth. This is her first pregnancy. The baby has multiple fractures, blue sclerae and short, bent extremities. Her past medical history is significant for a seizure disorder. She has been taking phenytoin regularly and had no seizure episodes during the pregnancy. She admits to eating poorly and occasionally drinking alcohol during the first trimester. She lives with her boyfriend who abuses her physically. She recalls several episodes of abuse during the pregnancy. Which of the following is most likely responsible for fetal abnormalities?
Folic acid deficiency
Collagen synthesis defect
Prenatal abuse
Phenytoin use
Alcohol abuse
363. You are awakened in the night by your 2-year-old son, who has developed noisy breathing on inspiration, marked retractions of the chest wall, flaring of the nostrils, and a barking cough. He has had a mild upper respiratory infection (URI) for 2 days. Which of the following therapies is indicated?
Short-acting bronchodilators and a 5-day course of steroids
Intubation and antibiotics
Observation for hypoxia and dehydration alone
Inhaled epinephrine and a dose of steroids
Rigid bronchoscopy
364. You receive a telephone call from the mother of a 4-year-old child with sickle-cell anemia. She tells you that the child is breathing fast, coughing, and has a temperature of 40°C (104°F). Which of the following is the most conservative, prudent course of action?
Prescribe aspirin and ask her to call back if the fever does not respond.
Make an office appointment for the next available opening.
Make an office appointment for the next day.
Refer the child to the laboratory for an immediate hematocrit, white blood cell count, and differential.
Admit the child to the hospital
365. A 7-month-old baby presents with a history of constipation for 1 month. He has one hard stool every week. He has been well otherwise. His physical examination is normal. Which of the following is the most likely cause of his problem?
Hypothyroidism
Lead poisoning
Functional constipation
Hirschsprung disease
Hypocalcemia
366. A specific pattern of abnormalities has been identified among infants born to mothers who consume moderate-to-large amounts of alcohol during their pregnancies. Which of the following abnormalities is characteristic of these infants?
Cataracts
Developmental dysplasia of the hip
Gonadal dysgenesis
Neural tube defects
Mental retardation

367. A 1-week-old black infant presents to you for the first time with a large, fairly well- defined, purple lesion over the buttocks bilaterally, as shown in the photograph. The lesion is not palpable, and it is not warm nor tender. The mother denies trauma and reports that the lesion has been present since birth. This otherwise well-appearing infant is growing and developing normally and appears normal upon physical examination. Which of the following is the most appropriate course of action in this infant?
Report the family to child protective services
Reassurance of the normalcy of the condition
Soft tissues films of the buttocks to identify calcifications
Administration of vitamin K
Measurement of bleeding time as well as factor VII and XI levels

368. A newborn infant develops respiratory distress immediately after birth. His abdomen is scaphoid. No breath sounds are heard on the left side of his chest, but they are audible on the right. Immediate intubation is successful with little or no improvement in clinical status. Emergency chest x-ray is shown (A) along with an x-ray 2 hours later (B). Which of the following is the most likely explanation for this infant’s condition?
Pneumonia
Cystic adenomatoid malformation
Diaphragmatic hernia
Choanal atresia
Pneumothorax
369. A 9-month-old infant is brought to the pediatrician's office because his weight is persistently below the 10th percentile. His mother states that the infant seems to be hungry all the time and usually consumes 8-12 oz of formula every 2-3 hours in addition to some table food. He also has frequent, bulky, and malodorous stools. A malabsorption syndrome is suspected. The results of which of the following tests will most likely be abnormal?
Abdominal radiography
Fecal fat quantification
Serum albumin
Stool culture for Clostridium difficile toxins
Stool smear for leukocytes and eosinophils
370. The parents of a previously healthy 2-year-old child note her to be pale and bring her to your clinic for evaluation. She currently has no fever, nausea, emesis, bone pain, or other complaints. Her examination is significant for pallor, tachycardia, and a systolic ejection murmur, but she has no organomegaly. Her complete blood count (CBC) reveals a hemoglobin of 4 g/dL, normal indices for age, a WBC count of 6.5/L, and a platelet count of 750,000/L. Her reticulocyte count is 0%. Coombs test is negative. Her peripheral blood smear shows no blast forms and no fragments. Red blood cell (RBC) adenosine deaminase levels are normal. A bone marrow reveals markedly decreased erythroid precursors. Which of the following is this child’s likely diagnosis?
Diamond-Blackfan anemia
Sickle-cell anemia
Pearson marrow-pancreas syndrome
Iron deficiency anemia
Transient erythroblastopenia of childhood
371. On a routine-screening CBC, a 1-year-old is noted to have a microcytic anemia. A follow-up hemoglobin electrophoresis demonstrates an increased concentration of hemoglobin A2. The child is most likely to have which of the following?
Iron deficiency
ρ�-Thalassemia trait
Sickle-cell anemia
Chronic systemic illness
Lead poisoning
372. A 2-year-old child is brought to the office by his parents for the evaluation of failure to thrive and chronic diarrhea. His diarrhea is "almost continuous", and he also has recurrent episodes of fever. He was initially quite well and was on the 60th percentile for weight; however, for the past seven months, he didn't seem to grow and failed to gain weight. Over the past three months, he fell to the 3rd percentile for weight. His parents deny any use of drugs, but they drink occasionally. His mother mentions that her former boyfriend was a heroin addict. Physical examination reveals oral thrush, generalized lymphadenopathy and eczema. What is the most likely diagnosis in this patient?
Congenital Toxoplasmosis
Non-Hodgkin lymphoma infiltrating small intestine
HIV infection
Miliary tuberculosis
Malabsorptive disease
373. A 3-year-old girl is brought to the emergency department because she became partially unconscious, lethargic and febrile. Her mother claims that "she suddenly took a turn for the worse" 24 hours ago after an upper respiratory tract infection. She has no allergies, and was not taking oral antibiotics. Her blood pressure is 60/45mm Hg and pulse is 120/min. On examination, she appears emaciated and lethargic. Despite numerous attempts, it is impossible to start a peripheral intravenous line, and the child's condition continues to deteriorate. What is the best next step to obtain IV access in this patient?
Subclavian central line
Lntraosseous
Jugular cut down
Femoral vein
Fluids down endotracheal tube
374. After being delivered following a benign gestation, a newborn infant is noted to have a platelet count of 35,000/L, decreased fibrinogen, and elevated fibrin spilt products. On examination you note a large cutaneous hemangioma on the abdomen that is purple and firm. Which of the following anomalies might also be expected in this infant?
Kaposiform hemangioendothelioma
Nevus simplex
Nevus flammeus
PHACE(S) syndrome
Infantile fibrosarcoma
375. A 4-year-old previously well African American boy is brought to the office by his aunt. She reports that he developed pallor, dark urine, and jaundice over the past few days. He stays with her, has not traveled, and has not been exposed to a jaundiced person, but he is taking trimethoprim sulfamethoxazole for otitis media. The CBC in the office shows a low hemoglobin and hematocrit, while his “stat” serum electrolytes, blood urea nitrogen (BUN), and chemistries are remarkable only for an elevation of his bilirubin levels. His aunt seems to recall his 8-year-old brother having had an “allergic reaction” to aspirin, which also caused a short-lived period of anemia and jaundice. Which of the following is the most likely cause of this patient’s symptoms?
Hepatitis B
Hepatitis A
Hemolytic-uremic syndrome
Gilbert syndrome
Glucose-6-phosphate dehydrogenase deficiency
{"name":"Pediatric_USMLE 251-375", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"251. A 12-year-old, previously healthy girl presents to her physician with a chief complaint of early morning headaches. She states that these headaches wake her up from sleep 2-3 days a week. She also complains of some vomiting associated with the headaches. The headaches have been getting progressively worse for the past 2 months. She denies any photophobia, dizziness, or blurred vision. There is no history of a recent respiratory infection, runny nose, or cough. There is no history of recent trauma. In the office, her vital signs are within normal limits. Her examination shows pupils that are equal, round, and reactive, with no maxillary or frontal sinus tenderness. Her tympanic membranes are clear and intact. Her neck is supple with full range of motion. Neurologic examination shows a positive Romberg sign. Which of the following tests would most likely confirm the diagnosis?, 252. A 10-month-old boy develops an upper respiratory tract infection 2 days before presentation. On the day of presentation, he has a generalized tonic-clonic seizure lasting 30 seconds. His temperature is 40.0 C (104 F), blood pressure is 90\/60 mm Hg, and respirations are 22\/min. He is alert and smiling. He has rhinorrhea, and his neck is supple. He has bruises below his knees. Which of the following is the most likely diagnosis?, 253. A 4-month-old child presents with a 2-day history of vomiting and intermittent irritability. On examination, “currant jelly” stool is noted in the diaper, and a sausage-shaped mass is palpated in the right upper quadrant of the abdomen. Which of the following conditions is most likely to cause this?","img":"https://cdn.poll-maker.com/18-733774/untitled1.png?sz=1200"}
More Quizzes
Star Wars Expanded Universe Quiz
10536
Loss prevention
9412
1- សំនួរប្រលងចេញ ADN by Kim Tathavan
100500
Mature Quiz
10514
Camping Trivia - Test Your Outdoor Knowledge
201023164
Which Alice in Wonderland Character Are You? Free
201017033
Wicca - Free Trivia on Beliefs, Rituals & History
201018328
Should I Go to Law School - Free Self‑Assessment
201017284
Which Incredibles Character Are You? Study Habits
201017961
Am I Cold-Hearted? - Free Personality Test
201017890
Watsons Go to Birmingham Chapter 1 Questions - Free
201017157
What Tablet Should I Buy? - Free Instant Results
201016617