DES C_Emergency (2) Prepared : CHILLY
A 27-year-old primigravid woman at 39 weeks' gestation comes to the labor and delivery ward with a gush of fluid and regular contractions. Examination shows that she is grossly ruptured, contracting every 2 minutes, and that her cervix is dilated to 4 cm. The fetal heart rate tracing is in the 140s and reactive. She is admitted to labor and delivery, and over the following 4 hours she progresses to 9 cm dilation. Over the past hour, the fetal heart rate has increased from a baseline of 140 to a baseline of 160. Furthermore, moderate to severe variable decelerations are seen with each contraction. The fetal heart rate does not respond to scalp stimulation. The decision is made to proceed with cesarean delivery. Which of the following is the reason for the cesarean delivery and the preoperative diagnosis?
Fetal acidemia
Low neonatal APGAR scores
Fetal hypoxic encephalopathy
Fetal distress
Non-reassuring fetal heart rate tracing
A 27-year-old woman presents to the ED 6 hours after the onset of body aches, abdominal cramping, and diarrhea. She is currently visiting relatives and normally lives in another state. She regularly takes six to eight tablets daily of hydrocodone for chronic low-back pain, sumatriptan for migraines, and amitriptyline and paroxetine for bulimia nervosa. Her BP is 130/80 mmHg, HR is 100 beats per minute, temperature is 98.6°F, RR is 16 breaths per minute, and oxygen saturation is 99% on room air. Examination shows diaphoresis, dilated pupils, and piloerection. Neurologically she is moving all four extremities and you do not note tremors. She is alert and cooperative but seems restless. She denies hallucinations or suicidal ideations. She becomes very angry when you ask her for the phone numbers of her regular physicians. Which of the following is the most likely explanation of her symptoms?
Anticholinergic overdose
TCA intoxication
Ethanol withdrawal
Serotonin syndrome
Opiate withdrawal
A 27-year-old woman presents to the ED complaining of an intensely pruritic rash all-over her body, abdominal cramping, and chest tightness. She states that 1 hour ago she was at dinner and accidentally ate some shrimp. She has a known anaphylactic allergy to shrimp. Her BP is 115/75 mmHg, HR is 95 beats per minute, temperature is 98.9°F, RR is 20 breaths per minute, and oxygen saturation is 97% on room air. She appears anxious, and her skin is flushed with urticarial lesions. Auscultation of her lungs reveals scattered wheezes with decreased air entry. Which of the following is the most appropriate next step in management?
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and administer methylprednisolone intravenously
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and administer methylprednisolone and diphenhydramine intravenously
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, administer methylprednisolone and diphenhydramine intravenously, and give intramuscular epinephrine
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and start aerosolized albuterol
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and start aerosolized epinephrine
A 27-year-old man sustains a single gunshot wound to the left thigh. In the ER, he is noted to have a large hematoma of his medial thigh. He complains of paresthesias in his left foot. On examination, there are weak pulses palpable distal to the injury and the patient is unable to move his foot. Which of the following is the most appropriate initial management of this patient?
Angiography
Immediate exploration and repair in the operating room
Observation for resolution of spasm
Local wound exploration at the bedside
Fasciotomy of the anterior compartment of the calf
A 28-year-old male is brought to the emergency department after being an unrestrained passenger in a motor vehicle collision. In the ambulance on his way to the hospital, he receives 2 liters of normal saline intravenously and 5 Umin of oxygen by nasal cannula. On physical examination, his blood pressure is 100/70 mmHg, heart rate is 120/min, and respiratory rate is 40/min. He is agitated and moves all four extremities spontaneously. His pupils are symmetric and reactive to light. His neck veins are distended, and his trachea is deviated to the right. Which of the following is the best initial management for this patient?
Immediate chest x-ray to confirm pneumothorax
Immediate ultrasound exam to confirm pleural fluid accumulation
X-ray series to exclude cervical spine injury
Immediate endotracheal intubation to establish an adequate airway
Needle insertion into the second intercostal space in the left mid-clavicular line
A 28-year-old man is brought to the emergency department 4 hours after being involved in a motor vehicle collision. His blood pressure is 90/50 mm Hg, pulse is 120/min and respirations are 30/min. Examination shows a stuporous man with bruises over his extremities and upper abdomen. His trachea is midline and his neck veins are flat. His abdomen is moderately distended but non-tender. Immediately after being intubated and placed on mechanical ventilation he goes into cardiac arrest. Which of the following could have prevented cardiac arrest in this patient?
High initial tidal volume
Chest tube placement
Positive end-expiratory pressure
Volume resuscitation
Pain management
A 28-year-old man presents to ER with fever, chills, and generalized weakness for the past one week. He has no history of pre-existing heart disease, but he was admitted to the hospital six months ago for cellulitis of the right arm. His temperature is 40.0°C (104°F), pulse is 110/min, respirations are 22/min, and blood pressure is 110/65 mmHg. Oropharynx is clear. Lungs are clear to auscultation. A holosystolic murmur is heard at the lower sternum which increases in intensity with inspiration. His blood is drawn and sent for culture. What is the most appropriate initial antibiotic therapy for this patient?
Ampicillin-sulbactam
Clindamycin
Oxacillin
Penicillin G and gentamycin
Vancomycin
A 28-year-old primigravid woman at 34 weeks gestation is brought to the emergency department following a motor vehicle accident. She had intense abdominal pain and became agitated and restless in the ambulance. She has mild vaginal bleeding and diffuse abdominal pain. She is on continuous fetal heart monitoring. Her prenatal course, prenatal tests and fetal growth have been normal. Prenatal ultrasound at the 16th week showed no abnormalities and an intrauterine gestation consistent with dates. Her blood pressure is 90/60mmHg, pulse is 120/min and respirations are 32/min. Physical examination shows hyperventilation, cold extremities and a distended abdomen with irregular contours. Fetal heart monitoring shows repetitive late decelerations and a long-term variability of 2 cycles/min. Which of the following is the most likely diagnosis?
Abruptio placenta
Placenta previa
Vasa previa
Uterine rupture
Rupture of ectopic pregnancy
A 28-year-old woman at 30 weeks gestation comes to the physician because of 2 days of a near absence of fetal movements. This is only her second prenatal visit because she has skipped many appointments. She has a medical history significant for chronic hepatitis C infection and a MRSA skin abscess that was drained. She smokes cigarettes and uses heroin, cocaine and alcohol. She says that she is trying hard to be sober. Her temperature is 37.0C (98.7F), blood pressure is 138/85 mm Hg and pulse is 80/min. Physical examination shows a fundal height of 26cm (10.2in). Fetal heart tones are heard by Doppler. Nonstress test (NST) shows no accelerations. After vibroacoustic stimulation, NST is still not reactive so a biophysical profile is ordered and shows a score of 2. Her lab work showed the following: Complete blood count: Hemoglobin: 8.0 g/L, MCV: 105fl, Platelets: 120,000/mm3, Leukocyte count: 3,500/mm3. Which of the following is the most appropriate next step in management?
Repeat non-stress test, twice weekly
Perform contraction stress test
Administer corticosteroids and repeat biophysical profile in 24 hours
Deliver the baby immediately
Assess for fetal lung maturity and deliver if it is achieved
A 28-year-old woman, gravida 3, para 2, at 35 weeks gestation is rushed to the emergency department because of vaginal bleeding. She was sleeping when she first noticed the bleeding. She has had no uterine contractions. Her prenatal course, prenatal tests and fetal growth have been normal. Prenatal ultrasound at the 14th week of gestation showed an intrauterine gestation consistent with dates and showed no abnormalities. Her previous pregnancies were uncomplicated. Her temperature is 37.0C (98.7F), blood pressure is 90/60 mmHg, pulse is 11 6/min and respirations are 16/min. Physical examination shows cold extremities and bright red vaginal bleeding. Which of the following is the most appropriate next step in management?
Obtain blood for PT/INR and PTI
Immediate vaginal examination
Emergency transvaginal ultrasonogram
Immediate cesarean section
Obtain venous access with two large bore needles
A 29-year-old G3P1011 with an IUP at 37 weeks' gestation presents to the emergency department because ofagush offluid from her vagina. The patient denies any other complaints. States that she was watching TV when shefelt the gush. The fluid appeared clear. Vital sign: BP, 110/80 mm Hg; P, 88 beats/min; R, 12 breaths/min; T, 98.6°F. Fetal movement: Present. Contractions: Absent. Vaginal bleeding: Absent. Leakage of fluid: Present. Physical Examination: CVS: Normal, Lungs: Normal, Abdomen: gravid, nontender, nondistended, +Bowel Sound; Extrimities: No edema bilaterally. What is the next step in the management of this patient?
Administer betamethasone
Digital cervical examination
Fetal fibronectin
Sterile speculum examination
Nothing to do
A 29-year-old male is brought to the emergency room because of sudden onset confusion and fever. He was recently admitted to the hospital for hallucinations and was discharged instable condition. His temperature is 38.6°C (101.6°F), blood pressure is 150/100 mmHg, pulse is 112/min, and respirations are 24/min. Mucus membranes are dry. Profuse diaphoresis is present. Lungs are clear to auscultation. Abdominal muscles are rigid. Muscle tone is increased; "lead pipe rigidity" is noted in all four extremities. Deep tendon reflexes are 2+. Tremor is noted. Which of the following is the most likely diagnosis?
Tetanus
Drug induced idiosyncratic reaction
Meningitis
Cocaine intoxication
Lithium intoxication
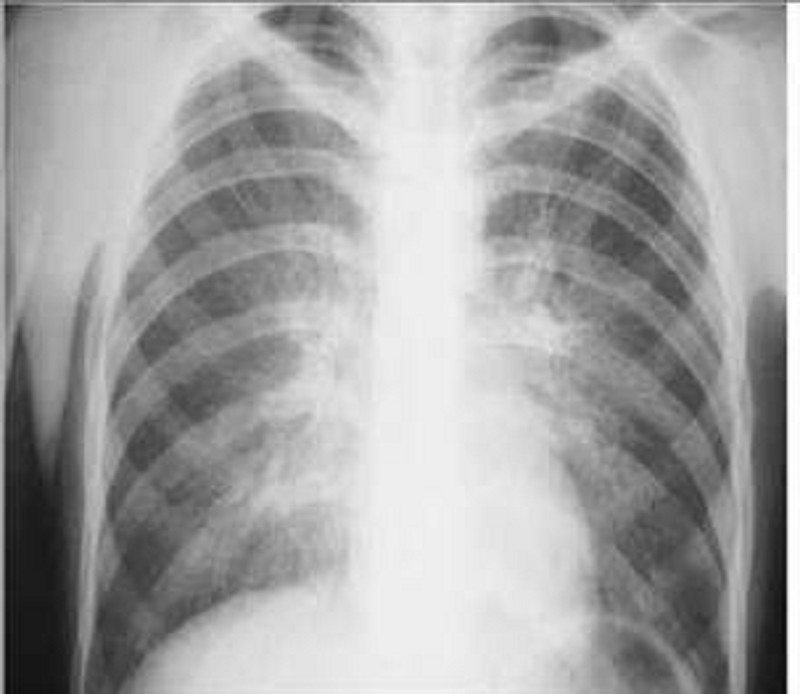
A 29-year-old male, known intravenous drug user presents to the emergency department with a chief complaint of dyspnea. Over the last few days, he has become short of breath and he has very little exercise tolerance. His other symptoms are a persistent dry cough, low-grade fever for the past two days, watery diarrhea, abdominal cramps, and general malaise. He self-treated his fever with acetaminophen. He has a history of anaphylaxis with sulfonamides. Physical examination reveals an emaciated man with numerous needle marks on his hands. Arterial blood gas analysis reveals a PCO2 of 32 mm Hg and PO2 of 64 mm Hg on room air. The chest x-ray is shown below. Which of the following is the most appropriate initial treatment regimen for this patient?
Penicillin and acyclovir
Acyclovir and azithromycin
Ganciclovir and azithromycin
Pentamidine and azithromycin
Tetracycline and azithromycin
A 29-year-old man is brought to the ED by EMS after being stabbed in the left side of his back. His BP is 120/80 mmHg, HR is 105 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 98% on room air. On the secondary survey, you note motor weakness of his left lower extremity and the loss of pain sensation in the right lower extremity. Which of the following is the most likely diagnosis?
Spinal shock
Anterior cord syndrome
Central cord syndrome
Brown-Sequard syndrome
Cauda equina syndrome
A 29-year-old man presents to the ED after being stabbed in his neck. The patient is speaking in full sentences. His breath sounds are equal bilaterally. His BP is 130/75 mmHg, HR is 95 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 99% on room air. The stab wound is located between the angle of the mandible and the cricoid cartilage and violates the platysma. There is blood oozing from the site although there is no expanding hematoma. Which of the following is the most appropriate next step in management?
Explore the wound and blind clamp any bleeding site
Probe the wound looking for injured vessels
Apply direct pressure and bring the patient immediately to the OR to explore the zone I injury
Apply direct pressure and bring the patient immediately to the OR to explore the zone II injury
Apply direct pressure and bring the patient immediately to the OR to explore the zone III injury
A 29-year-old woman presents to the ED for hyperventilation. Her initial vitals include an RR of 28 breaths per minute with an oxygen saturation of 100% on room air. She is able to speak in full sentences and tells you that she cannot breathe and that her hands and feet are cramping up. She denies any trauma, past medical history, or illicit drug use. Chest auscultation reveals clear breath sounds bilaterally. A subsequent chest radiograph is normal. Upon reevaluation, the patient reports that she is breathing better. Her vitals include an RR of 12 breaths per minute with an oxygen saturation of 100% on room air. Which of the following conditions is most likely the etiology of this patient’s symptoms?
Pneumothorax
Hemopneumothorax
Pleural effusion
Anxiety attack
Asthma exacerbation
A 29-year-old woman, gravida 2, para 1, comes to the labor and delivery ward because of contractions. Her prenatal course was significant for a positive Group B Streptococcus (GBS) perineal culture at 35 weeks’ gestation. She has no medical problems. She had a cholecystectomy at the age of 17. She takes no medications and has no known drug allergies. She is found to be 5 cm dilated with contractions every 2 minutes. She is admitted to the labor and delivery unit in active labor and penicillin is started for GBS prophylaxis. Shortly after admission to labor and delivery the patient complains of warmth and tingling of her face. She notes feeling like her lips and tongue are swollen. Physical examination demonstrates normal vital signs but with generalized urticaria and angioedema. Her abdomen is gravid and there is scant bloody mucous around her genital area. Which of the following is the most likely diagnosis?
Eclampsia
Penicillin allergy
Placental abruption
Preeclampsia
Thyroid storm
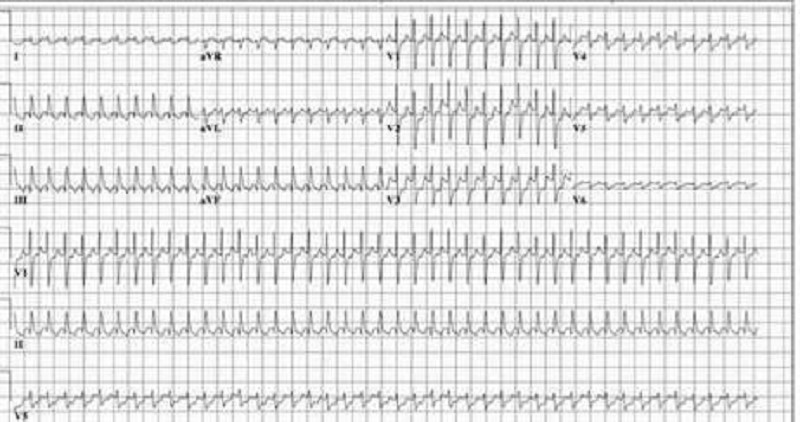
A 3-month-old infant is brought to your office for pallor and listless- ness. Your physical examination reveals tachycardia that is constant and does not vary with crying. He has no hepatomegaly and the lungs are clear. His ECG is shown. Which of the following is the most appropriate initial management of this patient?
Rapid verapamil infusion
Transthoracic pacing of the heart
Carotid massage
DC cardioversion
Precordial thump
A 3-month-old, previously well male infant presents to the emergency department in January with a 2-day history of clear rhinorrhea, low-grade fever, and poor appetite, but no cough. On physical examination, there are mild subcostal retractions, coarse breath sounds heard throughout the lung fields, and scattered expiratory wheezes. The child receives an intravenous fluid bolus in the emergency department and is admitted for observation. Which of the following is the most severe, life-threatening complication of this child's illness?
Apnea
Congestive heart failure
Dehydration
Hypoxemia
Wheezing
A 3-year-old boy is brought to the emergency room after spilling bleach onto his lower extremities. He is diagnosed with a chemical burn and all involved clothing are removed. In addition to resuscitation, which of the following is the most appropriate initial management of this patient?
Treatment of the burn wound with antimicrobial agents
Neutralize the burn wound with weak acids
Treatment of the burn wound with calcium gluconate gel
Wound debridement in the operating room
Lavage of the burn wound with large volumes of water
A 3-year-old girl is brought to the emergency department because of fever, chills, vomiting, and abdominal pain. Her temperature is 39.5°C (103.1°F), blood pressure is 70/40 mm Hg, pulse is 110/min, and respirations are 20/min. She is restless and diaphoretic. The abdominal examination shows right costovertebral tenderness. Laboratory studies show: Hemoglobin 15.0 g/L, Platelets 260,000/mm3, Leukocyte count 16,500/mm3, BUN 20 mg/dL, Serum creatinine 1.1 mg/dL. Urinalysis: Blood Negative, Glucose Negative, Ketones Negative, Leukocyte esterase Positive, Nitrites Positive, WBC 40-50/hpf, RBC 5-9/hpf. Blood and urine cultures are taken. Which of the following is the most appropriate next step in management?
Empiric therapy with oral antibiotics
Renal ultrasound
Empiric therapy with intravenous antibiotics
Voiding cystoureterogram
Plain abdominal x-ray
A 3-year-old girl is brought to the emergency department because she became partially unconscious, lethargic and febrile. Her mother claims that "she suddenly took a turn for the worse" 24 hours ago after an upper respiratory tract infection. She has no allergies, and was not taking oral antibiotics. Her blood pressure is 60/45mm Hg and pulse is 120/min. On examination, she appears emaciated and lethargic. Despite numerous attempts, it is impossible to start a peripheral intravenous line, and the child's condition continues to deteriorate. What is the best next step to obtain IV access in this patient?
Subclavian central line
Intraosseous
Jugular cut down
Femoral vein
Fluids down endotracheal tube
A 30-year-old man is brought to the ED by police officers. The patient is agitated, vomiting, and complaining of body aches. He states that he is withdrawing from his medication. His vital signs are BP 160/85 mmHg, RR 20 breaths per minute, HR 107 beats per minute, and temperature 99.7°F. On examination he is diaphoretic, has rhinorrhea, piloerection, and hyperactive bowel sounds. Which of the following substances is this patient most likely withdrawing from?
Ethanol
Cocaine
Nicotine
Methadone
Clonidine
A 30-year-old man with type 1 diabetes presents to the emergency department (ED). His blood pressure (BP) is 100/70 mmHg and heart rate (HR) is 140 beats per minute. His blood glucose is 750 mg/dL, potassium level is 5.9 mEq/L, bicarbonate is 5 mEq/L, and arterial pH 7.1. His urine is positive for ketones. Which of the following is the best initial therapy for this patient?
Give normal saline as a 2-L bolus; then administer 20 units of regular insulin subcutaneously
Bolus 2 ampules of bicarbonate and administer 10 units of insulin intravenously
Give him 5 mg of metoprolol to slow down his heart, start intravenous (IV) hydration, and then give 10 units of regular insulin intravenously
Give normal saline in 2 L bolus and then administer 10 units of insulin intravenously followed by an insulin drip and continued hydration
Give normal saline in 2 L bolus with 20 mEq/L potassium chloride (KCl) in each bag
A 30-year-old obese woman with no significant past medical history presents to the ED complaining of shortness of breath and coughing up blood-streaked sputum. The patient states that she traveled to Moscow a month ago. Upon returning to the United States, the patient developed a persistent cough associated with dyspnea. She was seen by a pulmonologist, who diagnosed her with bronchitis and prescribed an inhaler. However, over the following weeks, the patient’s symptoms worsened, and she developed pleuritic chest pain. In the ED, she lets you know that she smokes half a pack per day. Her vitals include a temperature of 99°F, BP of 105/65 mmHg, HR of 124 beats per minute, RR of 22 breaths per minute, and an oxygen saturation of 94% on room air. Physical examination is noncontributory, except for rales at the left-mid lung. Her ECG reveals sinus tachycardia with large R waves in V1 to V3 and inverted T waves. Given this patient’s history and presentation, what is the most likely etiology of her symptoms?
Mycoplasma pneumoniae (“walking” pneumonia)
Pneumocystis jiroveci pneumonia (PCP)
Q fever pneumonia
PE
Acute respiratory distress syndrome (ARDS)
A 30-year-old woman presents to the ED with fever, headache, a “sunburn-like” rash, and confusion. A friend states that the patient has complained of nausea, vomiting, diarrhea, and a sore throat over the past few days. Her last menstrual period began 4 days ago. Vital signs are HR 110 beats per minute, BP 80/45 mmHg, RR of 18 breaths per minute, and temperature of 103°F. On physical examination, you note an ill-appearing woman with a diffuse blanching erythroderma. Her neck is supple without signs of meningeal irritation. On pelvic examination, you remove a tampon. You note a fine desquamation of her skin, especially over the hands and feet, and hyperemia of her oropharyngeal, conjunctival, and vaginal mucous membranes. Laboratory results reveal a creatine phosphokinase (CPK) of 5000, WBC 15,000/μL, platelets of 90,000/μL, BUN 40 mg/dL, creatinine 2 mg/dL, and elevated liver enzymes. You suspect thediagnosis of toxic shock syndrome and initiate IV fluids. You target antibiotics at which of the following causative organism?
Staphylococcus aureus
Streptococcus pyogenes
Rickettsia rickettsii
Neisseria meningitidis
Neisseria gonorrhoeae
A 31 -year-old G2P1001 with an IUP at 39 weeks' gestation present to the labor and delivery unitfor contractions. The patient states that her last pregnancy was delivered via C-section, but she wants to deliver this one vaginally. She states that she knows the risks and is willing to accept them. Vital sign: BP, 115/75 mm Hg; P, 82 beats/min; R, 12 breaths/min; T, 98.6°F. Contractions: Present, Fetal movement: Present, Vaginal bleeding: Absent, Leakage of fluid: Present. Physical examination: Gen: Awake, alert-oriented x3, mild pain distress, CVS: Normal, Lungs: Clear, Abd: Gravid, contraction present, Ext: 1+ edema bilaterally. Cervical examination: 7 cm, 100% effaced, -1 station. Fetal Heart Monitoring: Reassuring, good variability, + accelerations, no decelerations. Which of the following is a complication of vaginal birth after C-section (VBAC)?
Infection
Pelvic floor damage
Hemorrhage
Uterine rupture
Sudden death
A 31-year-old man is brought to the ED by EMS who state that the man was found lying on the floor of his garage. He is rousable in the ED, speaks with slurred speech, and vomits. His BP is 140/85 mmHg, HR is 94 beats per minute, temperature is 98.8°F, RR is 17 breaths per minute, and oxygen saturation is 99% on room air. You place an IV line, draw blood, and start a liter of normal saline running through the line. Laboratory results reveal serum sodium 139 mEq/L, potassium 3.5 mEq/L, chloride 101 mEq/L, bicarbonate 14 mEq/L, BUN 15 mg/dL, creatinine 1 mg/dL, glucose 105 mg/dL, arterial blood pH 7.27, COHb 4%, and lactate 2.8 mEq/L. Urinalysis shows 1+ protein, trace ketones, WBC 4/hpf (high-power field), red blood cell (RBC) 2 to 3/hpf, and multiple envelope-shaped and needle shaped crystals. Which of the following conditions would best explain his metabolic acidosis?
Ibuprofen toxicity
Diabetic ketoacidosis (DKA)
Ethylene glycol poisoning
Lactic acidosis
Isopropyl alcohol poisoning
A 31-year-old woman with a known psychiatric history presents to the ED after ingesting an unknown quantity of pills from her medication vial. In the ED, she complains of nausea, abdominal cramping, and feels unsteady on her feet. On physical examination, you observe that she is tachycardic and ataxic. Which of the following substances will best be treated by activated charcoal that could present like this?
Phenobarbital
Carbamazepine
Lye (sodium hydroxide)
Lithium
Acetaminophen
A 32-year-old diabetic man presents to the ED with a fever and 1 week of increasing right foot pain. He states he stepped on a nail while running barefoot 2 weeks ago but didn’t think much of it at that time. On physical examination, his heel is mildly erythematous and diffusely tender to palpation, with overlying warmth and edema. There is a small amount of purulent drainage through the puncture hole in his heel. A plain radiograph of his foot demonstrates a slight lucency of the calcaneus. He has decreased range of motion, but you are able to passively dorsiflex and plantarflex his ankle without difficulty. His vital signs include a temperature of 101.4°F, HR of 98 beats per minute, BP of 130/75 mmHg, and RR of 16 breaths per minute. Which of the following is the most common causative organism of this condition?
Salmonella sp
Staphylococcus aureus
Pseudomonas aeruginosa
Group B streptococci
Pasteurella multocida
A 32-year-old firefighter presents to the ED in acute respiratory distress. He was taken to the ED shortly after extinguishing a large fire in a warehouse. His initial vitals include an HR of 90 beats per minute, a BP of 120/55 mmHg, and an RR of 18 breaths per minute with an oxygen saturation of 98% on 2-L nasal cannula. An ECG shows a first-degree heart block. Upon physical examination, there are diffuse rhonchi bilaterally. The patient is covered in soot and the hairs in his nares are singed. Given this clinical presentation, which of the following maybe responsible for this patient’s respiratory distress?
Reactive airway disease
Foreign body aspiration
Decompression sickness
Thermal burns
Pneumothorax
A 32-year-old G3P2 at 39 weeks gestation presented to the hospital with ruptured membranes and 4 cm dilated. She has a history of two prior vaginal deliveries, with her largest child weighing 3800 g at birth. Over the next 2 hours she progresses to 7 cm dilated. Two hours later, she remains 7 cm dilated. The estimated fetal weight by ultrasound is 3200 g. Which of the following labor abnormalities best describes this patient?
Prolonged latent phase
Hypertonic dysfunction
Protracted active-phase dilation
Secondary arrest of dilation
Primary dysfunction
A 32-year-old male comes to the hospital complaining of pain, swelling and redness of his right arm. His past medical history is significant for substance abuse. His temperature is 38.9°C (102.0°F), blood pressure is 110/60 mmHg, pulse is 110/min and respirations are 14/min. He is started on intravenous clindamycin. The next day the swelling and pain improve, but he develops nausea, vomiting, abdominal cramps and diarrhea. He is restless and asks for pain medication to treat his aching muscles and joints. His temperature now is 37.3°C (99.1°F), blood pressure is 120/70 mmHg, pulse is 80/min and respirations are 16/min. His laboratory studies at the time of admission and the following day show: Hemoglobin 13.0 g/L (12.8 g/L), Leukocyte count 17,500/mm3 (8,500/mm3), NeutrophiIs 86% (64%), Lymphocytes 14% (26%). Which of the following is the most appropriate next step in management?
Stool for Clostridium difficile toxin
Start chlordiazepoxide
Discontinue clindamycin
Start methadone
Start intravenous morphine
A 32-year-old male is admitted to the hospital because of confusion. He was recently diagnosed with schizophrenia His temperature is 38.6°C (101.6°F), blood pressure is 160/100 mmHg, pulse is 116/min, and respirations are 22/min. He is not oriented to time, place or person. Mucus membranes are dry. Profuse diaphoresis is present. Lungs are clear to auscultation. Abdominal, neck and extremity muscles are rigid. Muscle tone is increased. Deep tendon reflexes are 2+. Laboratory studies show a serum CK of 50,000 IU/L. CSF fluid analysis shows a total white blood cell count of 5/microL. Which of the following is the most appropriate next step in management?
Risperidone
Dantrolene
L-Dopa
Prednisone
Antibiotics
A 32-year-old man is brought into the ED by EMS with fever, shortness of breath, and stridor. The patient was treated yesterday in the ED for a viral syndrome. His BP is 90/50 mmHg, HR is 110 beats per minute, temperature is 101.2°F, and his RR is 28 breaths per minute. A chest radiograph reveals a widened mediastinum. The patient is endotracheally intubated, given a 2-L bolus of normal saline, and started on antibiotics. His BP improves to 110/70 mmHg and he is transferred to the intensive care unit (ICU). You see a friend that accompanied the patient to the hospital and ask him some questions. You find out that the patient is a drum maker and works with animal hides. What is the most likely organism that is responsible for the patient’s presentation?
Streptococcus pneumoniae
Coxiella burnetii
Corynebacterium diphtheriae
Haemophilus influenzae
Bacillus anthracis
A 32-year-old man is brought to the ED by EMS for confusion. EMS reports that the patient was at a local pharmacy filing his prescriptions when the pharmacist noticed the patient sweating and having difficulty answering questions. In the ED, the patient’s BP is 130/68 mmHg, HR is 120 beats per minute, temperature is 98.9°F, and RR is 12 breaths per minute. The patient is unable to explain what happened. His fingerstick glucose is 410 mg/dL and his urine is positive for ketones. An electrolyte panel reveals Na + 131 mEq/L, K + 4 mEq/L, Cl − 91 mEq/L, and Ca 2+ 11 mEq/L. Which of the following electrolytes are most important to supplement during the management of his medical condition?
Sodium, potassium, and calcium
Sodium
Potassium
Calcium
Sodium and calcium
A 32-year-old man is brought to the ED by paramedics after a diving accident. The lifeguard on duty accompanies the patient and states that he dove head first into the shallow end of the pool and did not resurface. On examination, the patient is speaking but cannot move his arms or legs and cannot feel pain below his clavicle. He is able to feel light touch and position of his four extremities. A cervical spine radiograph does not reveal a fracture. Which of the following is the most likely diagnosis?
Spinal cord injury without radiographic abnormality (SCIWORA)
Central cord syndrome
Anterior cord syndrome
Cauda equina syndrome
Brown-Sequard syndrome
A 32-year-old man is stabbed in the left chest and presents to the emergency department in distress. His pulse is 130/min, blood pressure is 70/50 mmHg, and respiratory rate is 39/min. The stab wound is in the left fifth intercostal space in the midaxillary line. On examination his trachea is deviated to the right, jugular veins are distended bilaterally, and he has absent breath sounds and hyperresonance to percussion on the left side. Subcutaneous emphysema is palpated on the left thoracic wall. What is the best next step in management?
Chest tube thoracotomy
Needle thoracostomy
Diagnostic peritoneal lavage
Pericardiocentesis
Surgical exploration
A 32-year-old man presented to the emergency department five hours ago with an acute asthma exacerbation. He has been receiving continuous albuterol nebulizer treatments since that time. He has a 20-year history of asthma but notes that recently the frequency of his attacks has increased. Presently, his blood pressure is 110/70 mmHg and heart rate is 120 and regular. On physical exam, the patient appears drowsy. Breath sounds are diminished bilaterally but there are no wheezes. The most recent ABG reveals: pH 7.32, pO2 65mmHg, pCO2 50mmHg. Which of the following is the best next step in managing this patient?
Inhaled corticosteroids
Intravenous theophylline
Ipratropium inhalation
Oral prednisone
Endotracheal intubation
A 32-year-old man undergoes a distal pancreatectomy, splenectomy, and partial colectomy for a gunshot wound to the left upper quadrant of the abdomen. One week later he develops a shaking chill in conjunction with a temperature spike of 39.4°C (103°F). His blood pressure is 70/40 mm Hg, pulse is 140 beats per minute and respiratory rate is 45 breaths per minute. He is transferred to the intensive care unit (ICU), where he is intubated and a Swan-Ganz catheter is placed. Which of the following is consistent with the expected initial Swan-Ganz catheter readings?
An increase in pulmonary artery pressure
An increase in PCWP
An increase in cardiac output
An increase in peripheral vascular resistance
An increase in central venous pressure
A 32-year-old man with Crohn’s disease presents to the emergency department with acute-onset diffuse abdominal pain and emesis. The patient states these symptoms are different than his usual Crohn’s disease flare-ups. The pain is severe (10/10) and is cramping in nature. He says his abdomen feels larger than usual. His Crohn’s disease has been well managed on 6-mercaptopurine for the past 6 months. The patient denies any recent sick contacts or eating underprepared foods. He states he had a bowel movement and flatus since the abdominal pain began. In addition to Crohn’s disease, the patient had appendicitis for which he underwent an appendectomy 12 years ago. His temperature is 37.1°C (98.7°F), blood pressure is 135/86 mm Hg, pulse is 84/min, and respiratory rate is 14/ min. On physical examination the abdomen is distended and diffusely tender with high-pitched bowel sounds. There is rebound tenderness throughout the abdomen along with guarding. The remainder of the physical examination is noncontributory. An x-ray of the abdomen shows dilated small loops of bowel along with absence of gas in the colon. What is the best next step in management?
Bowel rest only
Intravenous fluids and antibiotics only
Laparotomy
MRI of the abdomen
Ultrasound
A 32-year-old woman is brought to the emergency department by her husband because of slurred speech and difficulty walking. She has also been very drowsy for the past several hours, a non-typical behavior for a very active woman. She has a history of bipolar disorder, insomnia, migraine headaches, seizures and hypothyroidism. Her temperature is 37°C (98.6°F), blood pressure is 110/70 mmHg, pulse is 76/min, and respirations are 16/min. She is lethargic and falls asleep during the interview and physical examination. Pupils are 5 mm in size and reactive to light. Neck is supple. Oropharynx is clear. Chest auscultation is unremarkable. Abdomen is soft and non-tender; bowel sounds are normal. Limited neurologic examination shows 1+ deep tendon reflexes in all four extremities; there is no Babinski sign; strength is 5/5 throughout. There is no nystagmus or hand tremor. Blood sugar is 130 mg/dL. Which of the following is the most likely cause of her symptoms?
Cerebrovascular accident
Phenytoin toxicity
Benzodiazepine overdose
Ethanol intoxication
Lithium toxicity
A 32-year-old woman presents to the ED with 7 days of vaginal discharge and pelvic pain. She is sexually active and admits to several recent “one night stands.” She denies trauma/injury and does not have any urinary or other abdominal complaints. Her HR is 85 beats per minute, BP is 135/90 mmHg, RR is 18 breaths per minute, and temperature is 101.4°F. On bimanual examination, you note a copious, thin, white discharge with mild diffuse adnexal tenderness with significant cervical motion tenderness. There are no rashes, skin lesions, or adenopathy. Laboratory results are notable for a WBC of 18,000/μL. A urinalysis shows WBCs but is otherwise within normal limits. Which of the following is the most appropriate next step in management?
Prescribe her a 14-day course of levofloxacin (500 mg PO once per day) and urgent gynecology follow-up within 1 week
Give her a dose of metronidazole (2 g PO) and prescribe her a 14-day course of cephalexin (500 mg) with urgent gynecology follow-up within 1 week
Give her a one-time dose of oral metronidazole (2 g PO), azithromycin (1 g PO), and ceftriaxone (250 mg IM) with gynecology follow-up if she is not feeling better
Give her a one-time dose azithromycin (1 g PO), and ceftriaxone (250 mg IM) with urgent gynecology follow-up within 1 week
Give her a dose of ceftriaxone (250 mg IM), and prescribe her a 10-day course of doxycycline (100 mg PO BID) with urgent gynecology follow-up within 1 week
A 32-year-old woman presents to the ED with a 1-month history of general malaise, mild cough, and subjective fevers. She states that she is human immunodeficiency virus (HIV) positive and her last CD4 count, 6 months ago, was 220. She is not on antiretroviral therapy or any other medications. Initial vitals include an HR of 88 beats per minute, a BP of 130/60 mmHg, and an RR of 12 breaths per minute with an oxygen saturation of 91% on room air. Her chest radiograph shows bilateral diffuse interstitial infiltrates. Subsequent laboratory tests are unremarkable except for an elevated lactate dehydrogenase level. Given this patient’s history and physical examination, which of the following is the most likely organism responsible for her clinical presentation?
Coccidioides immitis
Pneumocystis jiroveci
Mycobacterium tuberculosis
Mycoplasma pneumoniae
Haemophilus influenzae
A 33-year-old man, who was drinking heavily at a bar, presents to the ED after getting into a fight. A bystander tells paramedics that the patient was punched and kicked multiple times and sustained multiple blows to his head with a stool. In the ED, his BP is 150/75 mmHg, HR is 90 beats per minute, RR is 13 breaths per minute, and oxygen saturation is 100% on non-rebreather. On examination, he opens his eyes to pain and his pupils are equal and reactive. There is a laceration on the right side of his head. He withdraws his arm to pain but otherwise does not move. You ask him questions, but he just moans. Which of the following is the most appropriate next step in management?
Prepare for intubation
Administer mannitol
Suture repair of head laceration
Bilateral burr holes
Neurosurgical intervention
A 33-year-old woman comes to your office for a blood pressure check. She has had chronic hypertension for the past 4 years, for which she takes hydrochlorothiazide. Her blood pressure has been reasonably well controlled with this medication. She also uses the combined oral contraceptive pill (i.e., the pill containing an estrogen and a progestin). She has no other medical problems and has never had surgery. She is allergic to penicillin. Her physical examination is normal. This patient should be counseled that patients with chronic hypertension who are also using the combined oral contraceptive pill might be at increased risk of which of the following?
Endometrial cancer and ovarian cancer
Myocardial infarction and ovarian cancer
Elevated blood pressure and smoking
Myocardial infarction and stroke
Endometrial cancer and stroke
A 33-year-old woman is brought to the emergency room from the scene of a severe motor vehicle accident. She is combative, confused, uncooperative, and appear dusky and dyspneic. Which of the following is the most appropriate management of her airway?
Awake endotracheal intubation is indicated in patients with penetrating ocular injury
Steroids have been shown to be of value in the treatment of aspiration of acidic gastric secretions
The stomach may be assumed to be empty only if a history is obtained indicating no ingestion of food or liquid during the prior 8 hours
Intubation should be performed as soon as possible (in the emergency room) if the patient is unstable
Cricothyroidotomy is contraindicated in the presence of maxillofacial injuries
A 33-year-old woman is seen in the ER with severe rectal bleeding. She has a history of ulcerative colitis. Her blood pressure is 78/56 mm Hg, her pulse is 144, and she is pale and clammy. Which of the following responses is likely to occur after administration of Ringer lactate solution?
Increase in serum lactate concentration
Impairment of liver function
Improvement in hemodynamics by alleviating the deficit in the interstitial fluid compartment
Increase in metabolic acidosis
Increase in the need for blood transfusion
A 33-year-old woman presents to the ED with a painful sprained ankle. She has a past medical history of depression for which she is taking phenelzine, a monoamine oxidase inhibitor. After you place an elastic wrap on her ankle, she asks you to prescribe her some pain medication. Which of the following medications is contraindicated in patients taking a monoamine oxidase inhibitor?
Ibuprofen
Acetaminophen
Meperidine
Oxycodone
Hydrocodone
A 34-year-old Caucasian female comes to the emergency department and complains that her heart is "racing out of control." She began to feel this way only this morning. She denies any chest pain or shortness of breath. Over the past few months, she has unintentionally lost 10 pounds. Her past medical history is significant for panic attacks, but she claims she has not had an attack for over 10 years. She is very concerned because her father died of a heart attack at the age of 40. The EKG reveals sinus tachycardia at a rate of 120/min. The initial labs show: CBC: Hb 12.9g/dL, Ht 39%, MCV 88 fl, Platelet count 200,000/cmm, Leukocyte count 8,500/cmm, Neutrophils 67%, Eosinophils 1%, Lymphocytes 24%, Monocytes 8%. Serum: Serum Na 139 mEq/L, Serum K 4.2 mEq/L, Chloride 100 mEq/L, Bicarbonate 25 mEq/L, BUN 10 mg/dL, Serum Creatinine 1.0 mg/dL, Calcium 9.1 mg/dL, Blood Glucose 102 mg/dL, TSH < 0.1 microU/mL, Free T4 4.6 ng/dL (N0.9-24). Which of the following is the best immediate step to control this patient's symptoms?
Propylthiouracil
Subtotal thyroidectomy
Alprazolam
Radioactive Iodine
Propanolol
A 34-year-old construction worker is brought to the ED by EMS after falling 30 ft from a scaffold. His vital signs are HR 124 beats per minute, BP 80/40 mmHg, and oxygen saturation 93% on 100% oxygen. He has obvious head trauma with a scalp laceration overlying a skull fracture on his occiput. He does not speak when asked his name, his respirations are poor, and you hear gurgling with each attempted breath. Auscultation of the chest reveals diminished breath sounds on the right. There is no JVD or anterior chest wall crepitus. His pelvis is unstable with movement laterally to medially and you note blood at the urethral meatus. His right leg is grossly deformed at the knee and there is an obvious fracture of his left arm. Which of the following is the most appropriate next step in management?
Insert a 32F chest tube into the right thoracic cavity
Perform a DPL to rule out intra-abdominal hemorrhage
Create two Burr holes into the cranial vault to treat a potential epidural hematoma
Immediately reduce the extremity injuries and place in a splint until the patient is stabilized
Plan for endotracheal intubation of the airway with in-line stabilization of the cervical spine
A 34-year-old farmer is brought to the hospital after attempting suicide. His body and clothes are soiled with vomitus. He is short of breath and appears agitated. His family reports no previous medical history or regular use of prescription medications. His temperature is 36.6°C (98°F), blood pressure is 110/60 mmHg, pulse is 50/min, and respirations are 22/min. His oxygen saturation is 86% on room air. Examination shows watering of the eyes and 1 mm pupils, bilaterally. Lung examination shows widespread rhonchi with prolonged expiration. Abdominal examination shows increased bowel sounds. Neurologic examination shows muscle fasciculations. What would be the most appropriate next step in management of this patient?
Obtain EKG for QRS duration
Obtain a chest x-ray
Remove all the clothing and wash the body
Obtain a head CT scan
Give physostigmine
A 34-year-old homeless male is brought to the ER in a confused state. He complains of flank pain. His past medical history is unknown. His temperature is 36.8°C (98.2F), blood pressure is 110/60 mmHg, pulse is 110/min and respirations are 22/min. His appearance is disheveled. Pupils are equal, 4 mm in size and reactive to light. Funduscopic examination is within normal limits. Lungs have crackles at both bases. Mild costovertebral angle tenderness is present. Foley catheter is placed and urine appears red. Laboratory studies show: Serum sodium 136 mEq/L, Serum potassium 3.5 mEq/L, Chloride 93 mEq/L, Bicarbonate 6 mEq/L, Blood urea nitrogen (BUN) 34 mg/dl, Serum creatinine 2.8 mg/dl, Blood glucose 80 mg/dl, Calcium 6.5 mg/dl, Serum ketones negative, Plasma lactate 2.4 mEq/L. Which of the following is the most appropriate next step in management?
Broad spectrum antibiotics
Fomepizole
N-acetylcysteine
Regular insulin
Glucagon
A 34-year-old homeless man is brought to the emergency room in a confused state. He complains of epigastric pain, vomiting and blurred vision. His temperature is 36.8°C (98.2°F), blood pressure is 110/60 mmHg, pulse is 110/min and respirations are 22/min. Physical examination shows poor oral hygiene and dry mucous membranes. Lungs are clear to auscultation. Abdominal exam shows mild epigastric discomfort. Funduscopic examination reveals optic disc hyperemia. Laboratory studies show: Serum sodium 136 mEq/L, Serum potassium 3.0 mEq/L, Chloride 93 mEq/L, Bicarbonate 6 mEq/L, Blood urea nitrogen (BUN) 30 mg/dL, Serum creatinine 0.8 mg/dL, Blood glucose 80 mg/dL, Serum ketones negative, Plasma lactate 2.2 mEq/L. Which of the following is the most likely cause of his symptoms?
Ethylene glycol poisoning
Mesenteric ischemia
Septic shock
Diabetic ketoacidosis
Methanol poisoning
A 34-year-old male is brought to the emergency department by his neighbor. The neighbor found the man lying on the floor beside an empty bottle of unknown substance. At the hospital, the patient is conscious and alert, but in severe pain. His temperature is 36.8°C (98.2°F), blood pressure is 130/70 mmHg, pulse is 90/min and respirations are 20/min. Abdomen is benign, with normal bowel sounds. Pupils are 5 mm, bilaterally. His tongue is white, heavy drooling of saliva is noted and he is unable to swallow. Which of the following is the most likely explanation for this patient's symptoms?
Anticholinergic poisoning
Tricyclic antidepressant poisoning
Caustic poisoning
Cyanide poisoning
Alcohol intoxication
A 34-year-old male is brought to the emergency room after being involved in a motor vehicle accident. He suffers blunt abdominal trauma and bilateral femur fractures. He has no significant past medical history. On physical examination, his blood pressure is 80/40 mmHg and his heart rate is 110/min. He receives several units of packed red blood cells. Once stabilized, the patient begins complaining of a tingling sensation in his toes and fingers. His serum calcium level is noted to be 7.2 mg/dL. Which of the following is the most likely cause of this patient's current symptoms?
Increased renal tubular secretion of calcium
Calcium chelation by a substance in the transfused blood
Parathyroid gland suppression due to fluid overload
Antibody-mediated red blood cell membrane damage
Electrolyte leakage from red blood cells during pre-transfusion storage
A 34-year-old man is brought to the emergency department after being rescued from a burning building. His temperature is 36.90C (98.60 F), blood pressure is 90/60 mm Hg, pulse is 100/min and respirations are 28/min. Examination shows second and third degree burns over 15% of his body. His oropharynx shows erythema and scattered blisters. His lungs are clear to auscultation and his abdomen is soft and nondistended. His blood carboxyhemoglobin concentration is 20%. Which of the following is the best management for this patient?
High-dose corticosteroids
Broad-spectrum antibiotics
Endotracheal intubation
Fluid restriction
Acetylcysteine inhalation
A 34-year-old Mexican male comes to the emergency department and complains of severe episodic headache, especially at night, for the past month. He also complains of unilateral, sharp, stabbing pain in the eye, which wakes him from sleep. The pain often starts suddenly just behind the right eye, and spreads to his face and temple region. It is not associated with nausea or visual disturbances, but is associated with watering of the eyes and nose, and with red eye. He had a similar episode one year ago, and it lasted for 2 months. Which of the following is the best treatment regimen for aborting the patient's pain during an acute attack?
Oral NSAIDs
Verapamil
Nasal sumatriptan
100 % oxygen
Ergotamine
A 34-year-old woman comes to the physician's office because of occasional headaches and palpitations. She has no other medical problems. She takes no medications. She smokes one and a half packs of cigarettes daily. Her blood pressure is 170/100 mm Hg in both arms, and heart rate is 80/min. Physical examination shows bilateral flank masses. Laboratory studies show: Serum sodium 140 mEq/L, Serum potassium 4.4 mEq/L, BUN 26 mg/dL, Serum creatinine 1.3 mg/dL. Urinalysis shows 10-12 red blood cells/hpf, but otherwise shows no abnormalities. The most likely complication that can occur in this patient is which of the following?
Liver necrosis
Intracranial aneurysms
Restrictive cardiomyopathy
Pancreatic cancer
Aortic dissection
A 34-year-old woman presents to the ED after ingesting an unknown quantity of her antidepressant pills. EMS workers found an empty bottle of amitriptyline on her apartment floor. She is awake but appears delirious. Her BP is 130/65 mmHg, HR is 101 beats per minute, temperature is 99.1°F, RR is 16 breaths per minute, and oxygen saturation is 100% on room air. On examination, her pupils are 7 mm and reactive. Her face is flushed and mucous membranes are dry. Her lungs are clear and heart is without murmurs. The abdomen is soft, nontender, and with decreased bowel sounds. She is moving all four extremities. ECG reveals sinus rhythm at a rate of 99 and QRS just under 100 milliseconds. In a TCA overdose, which of the following is responsible for her mydriasis, dry mucous membranes, and delirium?
Muscarinic receptor blockade
Histamine receptor blockade
Sodium channel blockade
α-Receptor blockade
Inhibition of serotonin and norepinephrine reuptake
A 34-year-old woman, gravida 4, para 3 at 38 weeks' gestation, comes to the labor and delivery ward because of contractions. Her prenatal course was significant for low maternal weight gain. She had a normal 18-week ultrasound survey of the fetus and normal 36-week ultrasound to check fetal presentation. Her blood type is O positive, and she is rubella immune. Three years ago, she had a multiple myomectomy. She takes prenatal vitamins and has no known drug allergies. She smokes one pack of cigarettes per day. Which of the following complications is most likely to occur?
Amniotic fluid embolism
Anencephaly
Macrosomia
Rh isoimmunization
Uterine rupture
A 34-year-old woman, gravida 4, para 3, at 32 weeks gestation is brought to the emergency department because of vaginal bleeding. She has had no uterine contractions or abdominal pain. Her prenatal course, prenatal tests and fetal growth have been normal. Prenatal ultrasound at the 12th week showed an intrauterine gestation consistent with dates. Her temperature is 37.0 C (98.7F), blood pressure is 90/70 mm of Hg, pulse is 98/min and respirations are 18/min. Physical examination shows continuous bright red vaginal bleeding. Ultrasonogram in the emergency department shows complete placenta previa. Fetal heart tracing shows repetitive late decelerations. The patient's vital signs are stabilized, but the bleeding continues. Which of the following is the most appropriate next step in management?
Immediate induction of labor
Emergency cesarean section
Administer corticosteroids and perform elective surgery
Forceps delivery
Continue expectant management until the bleeding stops
A 35-year-old agitated man presents to the ED in police custody. He denies any past medical history and takes no medication. He admits to using some drugs today. His BP is 195/90 mmHg, HR is 121 beats per minute, temperature is 100.1°F, RR is 18 breaths per minute, and oxygen saturation is 99% on room air. On examination, he is diaphoretic, and has pupils that are 8 mm in diameter, along with 3+ patella reflexes bilaterally. Electrocardiogram (ECG) reveals sinus tachycardia with a rate of 123. Which of the following toxic syndromes is this patient exhibiting?
Anticholinergic
Cholinergic
Sympathomimetic
Opioid
Sedative hypnotic
A 35-year-old man comes to the physician due to a one-month history of weight gain and facial edema. The facial edema resolves at the end of the day, but ankle edema develops. His temperature is 37.2°C (99°F), blood pressure is 142/80 mm Hg, pulse is 80/min, and respirations are 16/min. Examination shows 2+ ankle edema. Laboratory studies show: Hb 11.0 g/dl, WBC 8,000/cmm, Platelets 200,000/cmm, Serum Na 135 mEq/L, Serum albumin 2.2 g/dl, BUN 16 mg/dl, Serum creatinine 1.0 mg/dl. Urinalysis: Glucose Absent, Protein 4+, WBC 1-2/HPF, RBC Absent, Casts Fatty casts. This patient is most likely at risk for developing which of the following?
Rupture of brain aneurysm
Hypercoagulability
Abdominal aortic aneurysm
Pulmonary hemorrhage
Gall stone pancreatitis

A 34-year-old male presents to the emergency department with a red eye. He says, "I just woke up this morning and saw that my right eye was red." He denies any itching, pain or discharge. He has no known drug or environmental allergies. He takes no medication. His vital signs are stable. The photo of his eye is shown below. What is the best next step in his management?
Check intraocular pressure
Check coagulation parameters
Observation
Antibiotics
Refer to ophthalmologist
A 35-year-old man who is employed as a forklift operator was found sitting outside a warehouse. He came stumbling out complaining of dizziness and headaches. Co-workers in an adjoining warehouse also complained of headache and nausea. After collapsing outside, he regained consciousness immediately but appeared confused. In the ED, his BP is 100/54 mmHg, HR is 103 beats per minute, temperature is 100°F, pulse ox is 91% on room air, and RR is 23 breaths per minute. Physical examination is unremarkable. Laboratory results reveal WBC 10,500/μL, hematocrit 45%, platelets 110/μL, sodium 137 mEq/L, potassium 4 mEq/L, chloride 103 mEq/L, bicarbonate 21 mEq/L, BUN 8 mg/dL, creatinine 0.5 mg/dL, and glucose 89 mg/dL. Arterial blood gas results are pH 7.32, PCO2 32 mm Hg, and PO2 124 mm Hg. Which of the following is the most likely diagnosis?
Methemoglobinemia
Hypoglycemic syncope
Hydrocarbon poisoning
Opioid overdose
CO poisoning
A 35-year-old previously healthy male comes to the emergency department because of a 4-hour history of severe abdominal pain. The pain had initially started in the periumbilical area but has now shifted to the right lower quadrant. He also felt nauseated and vomited twice. He has had no previous surgeries. His temperature is 38.9C (102F), blood pressure is 125/80 mm Hg, pulse is 100/min and respirations are 20/min. Examination shows tenderness in the right lower quadrant. Palpation of the left lower quadrant produces pain in the right lower quadrant. Urinalysis is negative. Which of the following is the most appropriate next step in management?
Ultrasound of the abdomen
Conservative management
CT scan of the abdomen
Immediate surgery
Colonoscopy
A 35-year-old white female comes to her primary care physician for the evaluation of palpitations, weight loss, increased appetite and diarrhea for the past 2 months. She denies smoking cigarettes or drinking alcohol. Her temperature is 37.1°C (98°F), blood pressure is 135/80 mmHg, respirations are 14/min, and pulse is 90/min. Physical examination shows exophthalmos, lid lag, lid retraction, and a diffusely enlarged, non-tender thyroid gland. Lab studies show very low levels of serum TSH, and increased levels of serum free T4 and T3. The diagnosis of Graves' disease is established. Various treatment options are discussed with the patient, and she opts for long-term treatment with propylthiouracil. Which of the following conditions is this patient at risk for developing?
Agranulocytosis
Permanent hypothyroidism
Hypocalcemia
Recurrent laryngeal nerve palsy
Thyroid cancer
A 35-year-old white female presents with complaints of weight gain, lethargy and constipation for the last 2 months. She also complains of cold intolerance and oligomenorrhea. She is not taking any medication. She is a non-smoker, and does not drink alcohol. Her pulse is 67/min, and blood pressure is 130/90 mmHg. She is afebrile. Her hands are dry and cold. There is a non-tender, diffuse rubbery enlargement of the thyroid gland without any discrete nodularity. She does not have exophthalmos, lid lag or lid retraction. Labs show decreased serum T4 levels, elevated serum TSH levels and positive anti-thyroperoxidase (TPO) antibodies. Which of the following complications may develop in this patient?
Papillary carcinoma of the thyroid
Anaplastic carcinoma of the thyroid
Lymphoma of the thyroid
Medullary carcinoma of the thyroid
Follicular carcinoma of the thyroid
A 35-year-old woman calls her family physician after her 7-year old son accidentally splashed an unknown liquid containing acid on his face. Some liquid likely entered his eye, as the child is complaining of severe pain in his right eye. She knows a doctor living in her immediate neighborhood but is hesitant about what to do next. Which of the following is the most appropriate initial course of action that the mother should take?
Call 911 immediately
Go to local emergency room immediately
Do not try to wash the eye as it can enhance the damage
Wash the eye with copious amount of water
Go to the doctor in the neighborhood immediately
A 35-year-old woman is brought to the emergency room after an apparent suicide attempt. Her current prescription of imipramine was found at her bedside along with a suicide note. En route to the hospital, she suffered a seizure. She has been treated with many different anti-depressants over the past several years without improvement. Her temperature is 38.3°C (101°F), blood pressure is 90/50 mmHg, pulse is 120/min and respirations are 24/min. EKG shows QRS widening (0.18sec). She is given sodium bicarbonate along with supportive treatment. Which of the following is the most likely mechanism that explains the beneficial effects of sodium bicarbonate?
Alkalinization of urine will promote diuresis of the antidepressants
Acidification of urine will promote diuresis of the antidepressants
Sodium load of sodium bicarbonate will alleviate depressant action on sodium channels
Sodium load of sodium bicarbonate will alleviate depressant action on potassium channels
Sodium load of sodium bicarbonate will alleviate depressant action on calcium channels
A 35-year-old woman with systemic lupus erythematosus (SLE) is brought to the ED by her brother after he found her febrile and confused. Physical examination reveals fever, tachycardia, a waxing and waning mental status, petechiae over her oral mucosa, pallor, and mildly heme-positive stool. Her urinalysis is positive for blood, red cell casts, and proteinuria. Laboratory results reveal blood urea nitrogen (BUN) of 40 mg/dL and creatinine of 2 mg/dL. Her bilirubin is elevated (unconjugated > conjugated) and her international normalized ratio (INR) is 0.98. Her complete blood count reveals WBC 12,000/μL, hematocrit 29%, and platelet count 17,000/μL with schistocytes on the peripheral smear. Which of the following is the most appropriate next step in management?
Admit to the intensive care unit (ICU) for plasmapheresis and close monitoring for acute bleeds
Admit to the ICU for platelet transfusion and monitoring for acute bleeds
Admit to the ICU for corticosteroid infusion, transfusion of platelets, and prompt surgical consultation for emergent splenectomy
Admit to the ICU for dialysis and close monitoring for acute bleeds
Perform a noncontrast head computed tomography (CT) to screen for intracranial bleeding and mass effect followed by a lumbar puncture (LP) for analysis of cerebrospinal fluid (CSF). If negative, admit to telemetry for hemodynamic monitoring
A 36-year-old female presents to the emergency room complaining of chest pain that started suddenly while she was shopping at the mall. She also reports shortness of breath, palpitations and diaphoresis. The pain is retrosternal and radiates to the left arm. There are no aggravating or relieving factors. On review of systems, the patient reports having had a runny nose, sore throat and dry cough for the past 3 days. Her past medical history is significant for panic attacks, for which she takes paroxetine, and dysfunctional uterine bleeding, for which she takes estrogen. Her family history is significant for the sudden death of her father at age 44 from a heart attack. Social history reveals that she has smoked one pack of cigarettes per day for the past 15 years. Which of the following is the most appropriate initial therapy for this patient?
Lorazepam
Heparin
Aspirin
Ibuprofen
Acetaminophen
A 36-year-old female presents with weight loss, palpitations, mild shortness of breath, heat intolerance, tremors, and increased sweating. She does not have any past medical problems. Her family history is unremarkable. Her blood pressure is 140/70 mmHg, heart rate is 104/min and regular, temperature is 99.0°F (37.2°C) and respiratory rate is 22/min. Physical examination reveals a 2 x 2 cm nodule in her left thyroid lobe. The rest of her thyroid gland feels normal. There are no palpable lymph nodes in her neck. Eye examination reveals minimal lid lag, but no signs of proptosis or chemosis. She has tremors in both of her upper extremities. Her hands are moist and warm. Thyroid function testing reveals: Serum TSH < 0.03 micro IU/ml, Total T3 330 ng/dl, Total T4 14 mcg/dl. Radioactive iodine scan shows uptake only in her left-sided nodule. Which of the following disorders is this patient at risk of developing if she is left untreated?
Bone loss
Airway compression
Thyroid cancer
Coronary artery disease
Proptosis
A 36-year-old immigrant woman is brought to the ED from her workplace. She was found to be agitated and behaving bizarrely. The patient’s past medical history and medications are unknown. Her BP is 162/92 mmHg, HR is 140 beats per minute, temperature is 101.8°F, and RR is 18 breaths per minute. On examination, the patient is delirious, tremulous, and has a large goiter. Which of the following is the most appropriate management of this patient?
Administer dantrolene
Protect airway; administer iodine
Administer acetaminophen and broad-coverage antibiotics
Administer diazepam
Protect airway; administer acetaminophen, propranolol, and PTU
A 36-year-old male presents with the sensation of a racing heart. His blood pressure is 110/70 mmHg, respiratory rate 14/minute, and O2 saturation 98%. His ECG shows a narrow QRS complex tachycardia with rate 180, which you correctly diagnose as paroxysmal atrial tachycardia. Carotid massage and Valsalva maneuver do not improve the heart rate. Which of the following is the initial therapy of choice?
Adenosine 6-mg rapid IV bolus
Diltiazem 0.25-mg/kg IV over 2 min
Verapamil 2.5 to 5 mg IV over 1 to 2 min
Digoxin 0.5 mg IV slowly
Electrical cardioversion at 50 J
A 36-year-old white female is brought to the emergency department due to paraplegia and bladder incontinence. She immediately tells you that she has, "multiple sclerosis in remission." She has a history of optic neuritis and internuclear ophthalmoplegia, and both resolved with treatment. At that time, MRI showed plaques in the periventricular region. She is currently not taking any medications. Which of the following is the most appropriate next step in the management of this patient?
Corticosteroids
Plasmapheresis
Interferon
Cyclophosphamide
Intravenous Immunoglobulins
A 36-year-old woman, gravida 2, para 1, at 16 weeks' gestation undergoes amniocentesis for evaluation of Down syndrome. She has no past medical history. Immediately after the procedure she becomes breathless, cyanotic and loses consciousness. Minutes later, she experiences a generalized tonic-clonic seizure. A generalized purpuric rash is noted. Her blood pressure is 90/50 mm Hg, pulse is 110/min, and respirations are 26/min. Oxygen saturation is 75% on 100% facemask. Which of the following is the most appropriate next step in management?
Low molecular w eight heparin
Intravenous fluids
Immediate induction of labor
Intubation and mechanical ventilation
Administer intravenous diazepam
A 37 -year-old male is brought to the emergency department due to an episode of hematemesis. He has a history of peptic ulcer disease. A nasogastric tube lavage yields coffee-ground-like material. Physical examination reveals pallor and delayed capillary refill, without cyanosis. His temperature is 36.7°C (98°F), blood pressure is 85/40 mmHg, pulse is 125/min, and respirations are 18/min. Which of the following is the most appropriate first step in management?
Intravenous octreotide
Surgical intervention
Upper GI endoscopy
Intravenous pantoprazole
Fluid resuscitation
A 37-year-old G4 P3 woman delivered a 4,100gram (9.02lbs) infant by spontaneous vaginal delivery one hour ago. This pregnancy has been complicated by gestational diabetes for which she is being treated with insulin. The patient is currently on magnesium sulfate for elevated blood pressures and proteinuria. You are called to evaluate her because she began to have very heavy vaginal bleeding and is feeling lightheaded. Her blood pressure is 90/60 mmHg and pulse is 98/min. On physical examination you see heavy vaginal bleeding and numerous blood clots. Her cervix is closed and the uterus can be palpated 3cm above the umbilicus. The uterus feels boggy. The next best step in management is?
Dilatation and curettage
Cesarean hysterectomy
Oxytocin infusion
Packing of the uterine cavity
Immediate uterine artery embolization
A 37-year-old man presents to the ED with complaints of 2 days of a sore throat and subjective fever at home. He denies cough or vomiting. His BP is 130/75 mmHg, HR is 85 beats per minute, temperature is 101°F, and his RR is 14 breaths per minute. He has diffuse tonsillar swelling and bilateral exudates with bilaterally enlarged and tender lymph nodes of the neck. Which of the following is the next best step in management?
Administer penicillin and discharge the patient without further testing
Perform a rapid antigen test. If it is negative, confirm with a throat culture, and administer penicillin if the results are positive
Perform a rapid antigen test. If it is negative, administer penicillin and discharge the patient
Perform a rapid antigen test. If it is positive, administer penicillin and discharge the patient
Discharge the patient without treatment or further testing
A 37-year-old man who just finished a full course of penicillin for pharyngitis presents to the ED requesting to be checked out again. He states he took the antibiotics exactly as prescribed and initially felt somewhat improved, but over the last 2 to 3 days has had increased pain and progressive difficulty swallowing. His BP is 130/65 mmHg, HR is 95 beats per minute, temperature is 100.1°F, RR is 16 breaths per minute, and oxygen saturation is 99%. On examination, the patient is in no acute distress but has a fluctuant mass on the right side of his neck. You visualize a normal soft palate with swelling of the right tonsillar arch and deviation of the uvula to the left, but additional examination is limited because he is unable to open his mouth fully. Review of his records reveals a throat culture that was positive for Streptococcus. Which of the following is the most appropriate next step in management?
Attempt needle aspiration, treat him with a new course of antibiotics (either penicillin or clindamycin), and have him return in 24 hours
Give him morphine for pain control, give him a dose of IV antibiotics, and observe him in the ED for 6 hours
Switch his antibiotic to clindamycin and have him return in 24 hours
Admit him for incision and drainage in the OR under general anesthesia
Order a CT scan to visualize his neck, continue the penicillin, and have him return in 24 hours
A 37-year-old white female with myasthenia gravis presents to the office with a fever and cough productive of yellow-green sputum. She has been on pyridostigmine for the past few months. She refuses to have a thymectomy. Her pulse is 90/min, blood pressure is 120/76 mm Hg, respirations are 18/min, and temperature is 38.9°C (102°F). Her respiratory effort is weak. Pulse oximetry reveals 86% oxygen saturation on room air. There is a consistent decline on serial measurement of vital capacity. Which of the following is the most appropriate next step in management?
Increase the dose of pyridostigmine
Treatment with atropine
Treatment with edrophonium
Treatment with prednisolone
Endotracheal intubation
A 37-year-old woman is brought into the ED by her friend who states that the patient swallowed approximately 50 capsules of 325-mg acetaminophen (APAP) 6 hours ago in an attempted suicide. The patient states she feels nauseated and vomits while you take her history. Her BP is 100/75 mmHg, HR is 97 beats per minute, temperature is 98.9°F, RR is 18 breaths per minute, and oxygen saturation is 99% on room air. Examination is unremarkable except for mild epigastric tenderness. Which of the following is the correct antidote for APAP overdose?
NAC
Physostigmine
Flumazenil
Naloxone
Digibind
A 37-year-old woman is brought to the surgical floor after undergoing a routine vaginal hysterectomy that morning. She had been fasting since midnight the night prior to her surgery. She has no past medical history except for uterine fibroids and takes only oral contraceptive pills regularly. During the procedure, she was reported to lose approximately 300 mL of blood. On the floor, she appears well but complains of some fatigue. Her blood pressure is 110/60 mm Hg, and her pulse is 100/min. She is not taking food or water yet because of persistent nausea and vomiting postoperatively. Which of the following is the most appropriate next step in management?
Administer IV 25% albumin (colloid)
Re-explore the patient under anesthesia for possible bleeding
No further intervention
Administer IV crystalloid
Transfuse packed red blood cells
A 38-year-old G6P4 is brought to the hospital by ambulance for vaginal bleeding at 34 weeks. She undergoes an emergency cesarean delivery for fetal bradycardia under general anesthesia. In the recovery room 4 hours after her surgery, the patient develops respiratory distress and tachycardia. Lung examination reveals rhonchi and rales in the right lower lobe. Oxygen therapy is initiated and chest x-ray is ordered. Which of the following is most likely to have contributed to her condition?
Fasting during labor
Antacid medications prior to anesthesia
Endotracheal intubation
Extubation with the patient in the lateral recumbent position with her head lowered
Extubation with the patient in the semierect position (semi-Fowler position)
A 38-year-old homeless man is brought to the emergency room. He is obtunded and unable to speak. No previous medical history is known. His temperature is 34.0°C (93.2°F), blood pressure is 90/60 mmHg, pulse is 60/min and respirations are 6/min. Oxygen saturation is 86% on room air. Pupils are 5 mm in size, bilaterally. Oropharynx is dry. Lungs are clear to auscultation. Abdomen is soft; bowel sounds are decreased; there is no organomegaly. Extremities reveal several needle marks. Babinski sign is negative. Deep tendon reflexes are 2+ throughout. Which of the following is the most appropriate next step in management?
CT scan of the head
Glucagon
Methadone
Naloxone
Flumazenil
A 38-year-old man is brought to the emergency room by EMS after an apparent suicide attempt. En route to the hospital, he appeared confused and suffered a seizure. He has a history of hypertension and major depression. His temperature is 37.7°C (100°F), blood pressure is 70/40 mmHg, pulse is 40/min, and respirations are 12/min. Examination shows normal heart sounds and diffuse wheezing. Extremities are cold and clammy. EKG shows AV block. The patient is given intravenous fluids and atropine; however, his bradycardia and hypotension do not improve. Which of the following is the most appropriate next step in management?
Epinephrine
Aminophylline
Digoxin specific antibody
Glucagon
Pacemaker
A 38-year-old woman presents to the emergency department and complains of persistent vomiting that has increased in severity over the last week. Her other complaints are muscular weakness, twitching and cramps. Her urine output has decreased over the last 20 hours. Her past medical history is significant for a previously diagnosed prepyloric peptic ulcer. Her pulse is 100/min, blood pressure is 100/60 mmHg, respirations are 12/min, and temperature is 37.2°C (99°F). Physical examination reveals dry oral mucosa and decreased skin turgor. Abdominal examination reveals hypoactive bowel sounds and mild tenderness on palpation of the epigastrium. Nasogastric suction is started, and intravenous normal saline is given. Laboratory studies show: Serum sodium 135 mEq/L, Serum potassium 2.8 mEq/L, Chloride 81 mEq/L, Bicarbonate 40 mEq/L, Blood urea nitrogen (BUN) 42 mg/dl, Serum creatinine 1.3 mg/dl, Calcium 8.6 mg/dl, Ionized calcium 0.7 mmol/L (1.1-1.3 mmoi/L), Serum pH 7.54. Which of the listed agents should be added to the patient's current therapy?
Ammonium chloride
Potasium chloride
Calcium chloride
Furosemide
Sodium bicarbonate
A 38-year-old woman, gravida 3, para 2, at 32 weeks' gestation comes to the physician because of bleeding from the vagina. She states that this morning she passed 2 quarter-sized clots of blood from her vagina. Otherwise, she states that she is feeling well. The baby has been moving normally and she has had no contractions or gush of fluid from the vagina. Her obstetrical history is significant for 2 low-transverse cesarean deliveries for non-reassuring fetal heart rate tracings. An ultrasound is performed that demonstrates a complete placenta previa. For which of the following conditions is this patient at highest risk?
Dystocia
Intrauterine fetal demise (IUFD)
Placenta accreta
Preeclampsia
Uterine rupture
A 39-year-old white man with essential hypertension presents for a routine health maintenance visit. He has no complaints and reports compliance with his hydrochlorothiazide. His pulse is 70/min, blood pressure is 145/92 mmHg, and respiratory rate is 16/min. His body mass index is 24 kg/m2. His physical examination is within normal limits. For which condition is the patient at increased risk?
End-stage renal disease
Hypercholesterolemia
Hypertrophic cardiomyopathy
Second-degree Mobitz I atrioventricular block
Type 2 diabetes mellitus
A 39-year-old woman, brought into the ED by her family, states that she has had 4 days of diarrhea and has now started acting “crazy” with mood swings and confusion. The family states that she usually takes a medication for a problem with her neck. Her BP is 130/45 mmHg, HR is 140 beats per minute, temperature is 101.5°F, and her respiratory rate (RR) is 22 breaths per minute. An electrocardiogram (ECG) reveals atrial fibrillation with a normal QRS complex. After you address the airway, breathing, and circulation (ABCs), which of the following is the most appropriate next step in management?
Administer chlordiazepoxide, thiamine, and folate
Administer ceftriaxone and prepare for a lumbar puncture
Administer 2 ampules of bicarbonate to treat for tricyclic antidepressant overdose
Administer propranolol and propylthiouracil (PTU); then wait an hour to give Lugol iodine solution
Administer ciprofloxacin and give a 2-L bolus of normal saline for treatment of dehydration secondary to infectious diarrhea
A 4-week-old male infant presents with projectile, nonbilious emesis. Ultrasound of the abdomen reveals a pyloric muscle thickness of 8 mm (normal 3-4 mm). Which of the following is the best initial management of this patient?
Urgent pyloromyotomy
Urgent pyloroplasty
Urgent gastroduodenostomy
Fluid hydration and correction of electrolyte abnormalities prior to operative management
Administration of sodium bicarbonate to correct aciduria prior to operative management
A 40-year-old man is brought to the emergency room after his wife found him alone in a confused state. He admits to overdosing in a suicide attempt, but does not specify the drug taken. En route to the hospital, he is drowsy and ataxic with blurred vision. His past medical history is significant for asthma, insomnia, depression, and substance abuse. His temperature is 38.3°C (100°F), blood pressure is 130/80mmHg, pulse is 100/min, and respirations are 22/min. Examination shows dry mucus membranes and skin; pupils are 8mm bilaterally. There is no neck stiffness. Lungs are clear to auscultation. Heart sounds are within normal limits. Abdominal examination shows reduced bowel sounds with no tenderness. A Foley catheter is placed in the ER and 600 ml of urine is collected over one hour. Which of the following is the most likely diagnosis?
Salicylate intoxication
Cocaine intoxication
Serotonin syndrome
Diphenhydramine poisoning
Phencyclidine poisoning
A 40-year-old man is brought to the emergency room for retrosternal and epigastric pain after ingesting an unknown amount of "lye" (drain cleaner) 45 minutes ago. His past medical history is significant for major depression and suicide attempt. He is unable to swallow his saliva and is drooling. His temperature is 36.8°C (98.2°F), blood pressure is 120/70 mmHg, pulse is 110/min, and respirations are 20/min. Examination shows oropharyngeal erythema and edema. Lungs are clear to auscultation. Abdominal examination reveals tenderness at the epigastrium without rebound or guarding. Chest x-ray shows no abnormalities. Intravenous hydration is started. Which of the following is the most appropriate next step in treatment?
Administer activated charcoal in water
Upper gastrointestinal contrast studies and endoscopy
Gastric decontamination with ipecac
Neutralization and dilution of the alkali
Administer high dose systemic steroids
A 40-year-old man with a known history of ethanol abuse states that 2 hours ago he ingested two bottles of extra strength Tylenol. The patient has no medical complaints except for some nausea. At 4 hours post ingestion, you send blood to the laboratory to measure the serum acetaminophen concentration. The level returns and falls above the treatment line when you plot it on the APAP nomogram. You administer activated charcoal and decide to start IV NAC. Which of the following is a known adverse effect of IV NAC administration?
Hepatic failure
Anaphylactoid reaction
Hypertensive crisis
Confusion
Change in urine color

A 4-year-old boy is brought into the emergency room by his parents for difficulty in breathing and swallowing. On physical examination the child is febrile, tachycardic, and tachypneic. He is anxious, drooling, and becomes increasingly exhausted while struggling to breathe. A lateral cervical spine radiograph is shown here. Which of the following is the most appropriate management of this patient?
Examine the larynx at bedside
Immediate tracheostomy in the operating room
Immediate endotracheal intubation in the operating room
Immediate endotracheal intubation in the emergency room
IV antibiotics and admission to the floor
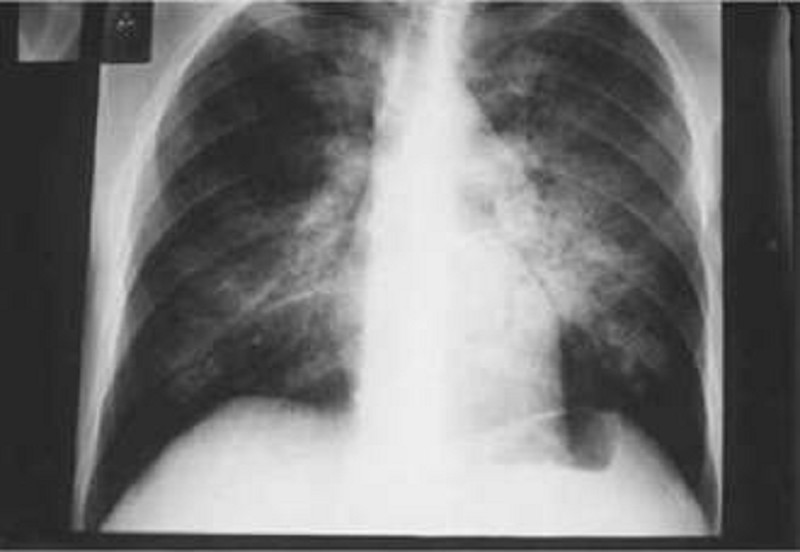
A 40-year-old man with a history of untreated HIV for 8 years comes into the ED complaining of cough, fever, and malaise for 3 days. He is tachypneic and diaphoretic. Chest radiograph reveals bilateral infiltrates. Arterial blood gas (ABG) analysis is significant for a PaO2 of 62 on room air. His chest radiograph is seen below. Which of the following is the most appropriate initial management?
Treat with corticosteroid prior to antibiotic therapy
Treat with nebulizer
Treat with racemic epinephrine
Treat immediately with IV trimethoprim/sulfamethoxazole (TMP/SMX)
Administer antibiotics after a rapid sputum Gram stain is obtained
A 40-year-old man with insulin-dependent diabetes presents to the ED with complaints of 2 days of increasingly severe perineal pain and subjective fevers. His HR is 118 beats per minute, BP is 95/55 mmHg, temperature is 103.4°F, and RR is 22 breaths per minute. The bedside sugar reading is “high.” Physical examination demonstrates crepitus over the medial thigh and widespread erythema and purple discoloration with sharp demarcation over the scrotum. The scrotum is markedly tender, warm, and edematous. Which of the following is the most likely diagnosis?
Cutaneous candidiasis
Fournier syndrome
Phimosis
Paraphimosis
Testicular torsion
A 40-year-old woman complains of mild, intermittent pain and paresthesias in her right wrist. She reports the pain is worse at night and with driving. On physical examination hyperflexion of the right wrist reproduces the paresthesia. With regard to her diagnosis, which of the following is the most appropriate initial treatment?
Ice pack to the affected wrist at nighttime
Heat pad to the affected wrist at nighttime
Wrist splint worn at nighttime
Surgical treatment with division of the flexor retinaculum
Surgical treatment with division of the extensor retinaculum
A 41-year-old man, the restrained driver in a high-speed motor vehicle collision, is brought to the ED by EMS. The patient is breathing without difficulty with bilateral and equal breaths sounds. He has strong pulses peripherally indicating a BP of at least 90 mmHg. The HR is 121 beats per minute. His Glasgow coma scale (GCS) is 14. A secondary survey reveals chest wall bruising. You suspect a cardiac injury. Which of the following locations most commonly involve cardiac contusions?
Right atrium
Right ventricle
Left atrium
Left ventricle
Septum
A 42-year-old IV drug user presents to the ED with fever, chills, pleuritic chest pain, myalgias, and general malaise. The patient’s vitals include an HR of 110 beats per minute, BP of 110/65 mmHg, RR of 18 breaths per minute, and temperature of 103.4°F. Physical examination is notable for retinal hemorrhages, petechiae on the conjunctivae and mucous membranes, a faint systolic ejection murmur, and splenomegaly. Which of the following is the most likely diagnosis?
Disseminated gonorrhea
Myocarditis
Pericarditis
Infectious mononucleosis
Endocarditis
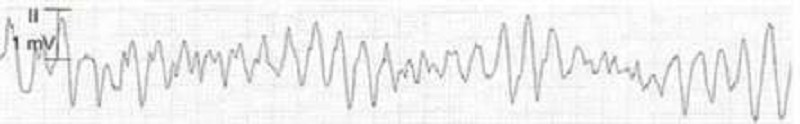
A 42-year-old male is admitted to the hospital with fever and shortness of breath. He has HIV infection, hepatitis C infection, and alcohol induced cardiomyopathy. His temperature is 38.6°C (101.5°F). Thrush is noted in the oropharynx. Chest x-ray reveals right lower lobe consolidation. He is started on fluconazole and moxifloxacin. His pneumonia and thrush improve over the next 2 days. However, on the third day, he develops palpitations. His EKG strip is shown below. Which of the following is the most appropriate next step in management?
Calcium gluconate
Magnesium sulphate
Sotalol
Amiodarone
Adenosine
A 42-year-old man is found unconscious at the scene of a motor vehicle collision. He is rushed to the emergency department, where his blood pressure is found to be 70/40 mm Hg and his respirations are 32/min. On physical examination, his trachea is deviated to the left and his breath sounds are decreased on the right side. His neck veins are distended bilaterally. The abdomen is soft and non-distended. There is significant swelling of the right thigh. Which of the following is the most appropriate next step in the management of this patient?
CT scan of the chest with contrast
Needle thoracostomy
Bedside echocardiography
Two large bore IV lines and fluid resuscitation
Intubation and mechanical ventilation
A 42-year-old man presents to the ED via ambulance after activating EMS for dyspnea. He is currently on an oxygen face mask and was administered one nebulized treatment of a β2-agonist by the paramedics. His initial vitals include an RR of 16 breaths per minute with an oxygen saturation of 96% on room air. The patient appears to be in mild distress with some intercostal retractions. Upon chest auscultation, there are minimal wheezes localized over bilateral lower lung fields. The patient’s symptoms completely resolve after two more nebulizer treatments. Which of the following medications, in addition to a rescue β2-agonist inhaler, should be prescribed for outpatient use?
Magnesium sulfate
Epinephrine injection (EpiPen)
Corticosteroids
Cromolyn sodium
Ipratropium
A 42-year-old man who is actively seizing is brought to the ED by EMS after a massive ingestion of an unknown substance. The man is known to have a history of acquired immunodeficiency syndrome (AIDS). An intravenous (IV) line is established and anticonvulsant therapy is administered. After high doses of diazepam, phenobarbital, and phenytoin, it is determined that the seizures are refractory to standard anticonvulsant therapy. Which of the following substances did this patient most likely ingest?
Cocaine
Diphenhydramine
Tricyclic antidepressant (TCA)
Haloperidol
Isoniazid (INH)
A 42-year-old man who was in a house fire is transferred to your burn unit. He has singed nose hairs and facial burns. Direct laryngoscopy in the emergency room demonstrates pharyngeal edema and mucosal sloughing. He has 60% total body surface area burns. Which of the following is the next step in the management of this patient?
Hyperbaric oxygen
Intravenous steroids
Inhaled steroids
Bronchoscopy
Intubation
A 43-year-old man, who currently uses drugs intravenously (IV), presents to the emergency department (ED) with 2 weeks of fever, back pain, and progressive weakness in his legs bilaterally. He denies any history of trauma or prior surgery. His blood pressure (BP) is 130/75 mmHg, heart rate (HR) is 106 beats per minute, temperature is 103°F, and respiratory rate (RR) is 16 breaths per minute. On physical examination, he has tenderness to palpation in the mid-lumbar spine, increased patellar reflexes, and decreased strength in the lower extremities bilaterally, with normal range of motion. Laboratory results reveal a white blood cell (WBC) count of 15,500/μL, hematocrit 40%, and platelets 225/μL. Urinalysis and spinal x-rays are unremarkable. Which of the following is the most likely diagnosis?
Fibromyalgia
Spinal epidural abscess
Ankylosing spondylitis
Vertebral compression fracture
Spinal metastatic lesion
{"name":"DES C_Emergency (2) Prepared : CHILLY", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 27-year-old primigravid woman at 39 weeks' gestation comes to the labor and delivery ward with a gush of fluid and regular contractions. Examination shows that she is grossly ruptured, contracting every 2 minutes, and that her cervix is dilated to 4 cm. The fetal heart rate tracing is in the 140s and reactive. She is admitted to labor and delivery, and over the following 4 hours she progresses to 9 cm dilation. Over the past hour, the fetal heart rate has increased from a baseline of 140 to a baseline of 160. Furthermore, moderate to severe variable decelerations are seen with each contraction. The fetal heart rate does not respond to scalp stimulation. The decision is made to proceed with cesarean delivery. Which of the following is the reason for the cesarean delivery and the preoperative diagnosis?","img":"https://cdn.poll-maker.com/18-721889/image.jpeg?sz=1200"}
More Quizzes
Dating
10512
The Perfect Boot for Your Personality
63224
Matlab Plotting Quiz
4222
How strong is your faith in God
10519
APUSH Unit 3 Practice Test - Free Period 3 Review
201017234
Chamber Music History - Free Online Practice
201016467
Arabic Alphabet - Free Letter Recognition
201018040
Do I Have Pneumonia or Bronchitis? Free Symptom
201016467
Why Am I Single - Find Out What's Holding You Back
201016467
Am I Charismatic? Free with Instant Results
201018408
LSU Trivia: Alma Mater Lyrics & Tiger Traditions
201016522
Stroop Test Online - Free Reaction Time Challenge
201018878