(EXAM) Part 4 (765-865) (765-1019) NR 4

Emergency Medicine Knowledge Assessment
Test your knowledge of emergency medicine with this comprehensive quiz designed for medical professionals and students alike. With 30 challenging questions focused on real-world clinical scenarios, you'll be able to assess your understanding and application of critical medical concepts.
Topics covered include:
- Diagnostic procedures
- Management of acute conditions
- Infectious diseases
- Trauma care
- Pharmacology
A 43-year-old man, who currently uses drugs intravenously (IV), presents to the emergency department (ED) with 2 weeks of fever, back pain, and progressive weakness in his legs bilaterally. He denies any history of trauma or prior surgery. His blood pressure (BP) is 130/75 mmHg, heart rate (HR) is 106 beats per minute, temperature is 103°F, and respiratory rate (RR) is 16 breaths per minute. On physical examination, he has tenderness to palpation in the mid-lumbar spine, increased patellar reflexes, and decreased strength in the lower extremities bilaterally, with normal range of motion. Laboratory results reveal a white blood cell (WBC) count of 15,500/μL, hematocrit 40%, and platelets 225/μL. Urinalysis and spinal x-rays are unremarkable. Which of the following is the most likely diagnosis?
Spinal epidural abscess
Fibromyalgia
Ankylosing spondylitis
Vertebral compression fracture
Spinal metastatic lesion
An 81-year-old woman is brought to the ED by her children who state that the patient is acting more tired than usual, has had fever for the last 2 days, and is more confused. Ordinarily, the patient is high functioning: she is ambulatory, cooks for herself, and walks on a treadmill 30 minutes a day. Her vital signs are BP 85/60 mmHg, HR 125, RR 20, temperature 101.3°F, and pulse oxygenation 97% on room air. On examination, the patient has dry mucous membranes but is otherwise unremarkable. She is oriented to person and place but states that the year is 1925. Her laboratory results show a WBC 14,300/μL, hematocrit 31%, and platelets 350/μL. Her electrolytes are within normal limits. Blood glucose is 92 mg/dL. A chest radiograph does not show any infiltrates. Urinalysis reveals 2+ protein, trace ketones, WBC > 100/hpf, red blood cell (RBC) 5 to 10/hpf, nitrite positive, and leukocyte esterase positive. After administering a 500-cc normal saline fluid bolus and broad-spectrum antibiotics through her peripheral IV line, the patient’s BP is 82/60 mmHg. You suspect that the patient is in septic shock due to an acute urinary tract infection. Which of the following is the next most appropriate course of action to manage this patient with earlygoal-directed therapy (EGDT)?
Place a central venous line into the right internal jugular vein to measure central venous pressure (CVP)
Immediately start a norepinephrine infusion to increase the blood pressure given the low systolic blood pressure
Prepare to transfuse uncrossed matched packed RBC to increase oxygen-carrying capacity given the low hematocrit
Transport the patient to radiology for a stat CT scan of her head given the acute change in mental status
Place a central venous line into the right internal jugular vein to measure mixed venous oxygen saturation (SVO2)
A 23-year-old man presents to the ED with left lower abdominal pain and left testicular pain that started 1 to 2 weeks ago and has gradually worsened. He has some nausea and vomiting. His HR is 98 beats per minute, BP is 125/65 mmHg, temperature is 100.9°F, and RR is 18 breaths per minute. Physical examination reveals a tender left testicle with a firm nodularity on the posterolateral aspect of the testicle. Pain is relieved slightly with elevation of the testicle and the cremasteric reflex in normal. You make the presumptive diagnosis of epididymitis. Which of the following is the next best step?
Give ceftriaxone 250 mg intramuscularly (IM), plus a 10-day course of oral doxycycline
Prescribe pain medications and penicillin for coverage of syphilis, the most likely causative organism
Recommend bed rest, ice, and scrotal elevation with prompt urology follow-up
Give ceftriaxone 125 mg intramuscularly (IM), plus a one-time dose of azithromycin 1g orally
Confirm the diagnosis with transillumination of the testicle, and then consult urology for surgical drainage
A 40-year-old man with insulin-dependent diabetes presents to the ED with complaints of 2 days of increasingly severe perineal pain and subjective fevers. His HR is 118 beats per minute, BP is 95/55 mmHg, temperature is 103.4°F, and RR is 22 breaths per minute. The bedside sugar reading is “high.” Physical examination demonstrates crepitus over the medial thigh and widespread erythema and purple discoloration with sharp demarcation over the scrotum. The scrotum is markedly tender, warm, and edematous. Which of the following is the most likely diagnosis?
Fournier syndrome
Cutaneous candidiasis
Phimosis
Paraphimosis
Testicular torsion
A 55-year-old man with a history of diabetes presents with complaints of developed left knee pain several days following a fall from standing height. The patient was brought to the ED by ambulance after being found on a park bench stating he was unable to walk because of the pain. On physical examination, there are no rashes or external signs of trauma. His left knee is warm, diffusely tender, and swollen with a large effusion. He has pain on passive range of motion and is refusing to walk. His BP is 150/85 mmHg, HR is 105 beats per minute, temperature is 102.7°F, RR is 16 breaths per minute, and fingerstick glucose is 89 mg/dL. Which of the following is the most appropriate diagnostic test?
Arthrocentesis
Knee radiographs
Magnetic resonance imaging (MRI)
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
Bone scan
A 35-year-old woman with systemic lupus erythematosus (SLE) is brought to the ED by her brother after he found her febrile and confused. Physical examination reveals fever, tachycardia, a waxing and waning mental status, petechiae over her oral mucosa, pallor, and mildly heme-positive stool. Her urinalysis is positive for blood, red cell casts, and proteinuria. Laboratory results reveal blood urea nitrogen (BUN) of 40 mg/dL and creatinine of 2 mg/dL. Her bilirubin is elevated (unconjugated > conjugated) and her international normalized ratio (INR) is 0.98. Her complete blood count reveals WBC 12,000/μL, hematocrit 29%, and platelet count 17,000/μL with schistocytes on the peripheral smear. Which of the following is the most appropriate next step in management?
Admit to the intensive care unit (ICU) for plasmapheresis and close monitoring for acute bleeds
Admit to the ICU for platelet transfusion and monitoring for acute bleeds
Admit to the ICU for corticosteroid infusion, transfusion of platelets, and prompt surgical consultation for emergent splenectomy
Admit to the ICU for dialysis and close monitoring for acute bleeds
Perform a noncontrast head computed tomography (CT) to screen for intracranial bleeding and mass effect followed by a lumbar puncture (LP) for analysis of cerebrospinal fluid (CSF). If negative, admit to telemetry for hemodynamic monitoring
A 30-year-old woman presents to the ED with fever, headache, a “sunburn-like” rash, and confusion. A friend states that the patient has complained of nausea, vomiting, diarrhea, and a sore throat over the past few days. Her last menstrual period began 4 days ago. Vital signs are HR 110 beats per minute, BP 80/45 mmHg, RR of 18 breaths per minute, and temperature of 103°F. On physical examination, you note an ill-appearing woman with a diffuse blanching erythroderma. Her neck is supple without signs of meningeal irritation. On pelvic examination, you remove a tampon. You note a fine desquamation of her skin, especially over the hands and feet, and hyperemia of her oropharyngeal, conjunctival, and vaginal mucous membranes. Laboratory results reveal a creatine phosphokinase (CPK) of 5000, WBC 15,000/μL, platelets of 90,000/μL, BUN 40 mg/dL, creatinine 2 mg/dL, and elevated liver enzymes. You suspect thediagnosis of toxic shock syndrome and initiate IV fluids. You target antibiotics at which of the following causative organism?
Staphylococcus aureus
Rickettsia rickettsii
Streptococcus pyogenes
Neisseria meningitidis
Neisseria gonorrhoeae
A 32-year-old diabetic man presents to the ED with a fever and 1 week of increasing right foot pain. He states he stepped on a nail while running barefoot 2 weeks ago but didn’t think much of it at that time. On physical examination, his heel is mildly erythematous and diffusely tender to palpation, with overlying warmth and edema. There is a small amount of purulent drainage through the puncture hole in his heel. A plain radiograph of his foot demonstrates a slight lucency of the calcaneus. He has decreased range of motion, but you are able to passively dorsiflex and plantarflex his ankle without difficulty. His vital signs include a temperature of 101.4°F, HR of 98 beats per minute, BP of 130/75 mmHg, and RR of 16 breaths per minute. Which of the following is the most common causative organism of this condition?
Staphylococcus aureus
Salmonella sp
Pseudomonas aeruginosa
Group B streptococci
Pasteurella multocida
A 75-year-old woman is transferred to your ED from the local nursing home for fever, cough, and increasing lethargy. Over the past 3 days, the nursing home staff noticed increasing yellow sputum and decreasing urine output from the patient. Her BP is 118/75 mmHg, RR is 20 breaths per minute, HR is 105 beats per minute, temperature is 100.9°F, and pulse oxygenation is 94% on room air. On examination, auscultation of the lungs reveals bibasilar crackles. Laboratory results reveal WBC 14,500/μL, hematocrit 39%, platelets 250/μL, sodium 132 mEq/L, potassium 3.5 mEq/L, chloride 100 mEq/L, bicarbonate 18 mEq/L, BUN 27 mg/dL, creatinine 1.5 mg/dL, and glucose 85 mg/dL. Serum lactate is 4.7 mmol/dL. Chest radiography reveals bilateral lower lobe infiltrates. Based on this patient’s presentation, which of the following is the most likely diagnosis?
Health care–associated pneumonia (HCAP)
Hospital-acquired pneumonia (HAP)
Community-acquired pneumonia (CAP)
Ventilator-associated pneumonia (VAP)
Atypical pneumonia
A 55-year-old man presents to the ED with fever, drooling, trismus, and a swollen neck. He reports a foul taste in his mouth caused by a tooth extraction 2 days ago. On physical examination, the patient appears anxious. He has bilateral submandibular swelling and elevation and protrusion of the tongue. He appears “bull-necked” with tense and markedly tender edema and brawny induration of the upper neck, and he is tender over the lower second and third molars. There is no cervical lymphadenopathy. These lungs are clear to auscultation with good air movement. His vital signs are HR 105 beats per minute, BP 140/85 mmHg, RR 26 breaths per minute, and temperature 102°F. Which of the following is the most appropriate next step in management?
Secure his airway, administer a dose of IV antibiotics, and obtain an emergent ENT (ear, nose, and throat) consult
Obtain a sample for culture, administer a dose of IV antibiotics, and obtain a soft tissue radiograph of the neck
Obtain a sample for culture, perform a broad incision and drainage at bedside, and administer a dose of IV antibiotics
Administer a dose of IV antibiotics and obtain a CT scan of the soft tissues of the neck
Administer a dose of IV antibiotics, obtain a CT scan of the soft tissues of the neck, and obtain an emergent ENT consult
A 67-year-old woman with a history of steroid-dependent COPD, non–insulin-dependent diabetes, and hypertension presents to the ED with complaints of a painful, red, swollen left lower leg. She states she noted a “bug bite” in that area 1 week ago and since then has had gradually increasing symptoms. On examination, you note a 12 cm × 10 cm sharply demarcated area of blanching erythema, warmth, and tenderness on the medial thigh with ascending erythema to the groin. You also note tender adenopathy in the left inguinal region. Her BP is 90/55 mmHg, RR is 24 breaths per minute, HR is 105 beats per minute, temperature is 102.4°F, and pulse oxygenation is 98% on room air. Laboratory results reveal WBC 19,500/μL, hematocrit 39%, platelets 175/μL, sodium 132 mEq/L, potassium 3.5 mEq/L, chloride 100 mEq/L, bicarbonate 14 mEq/L, BUN 32 mg/dL, creatinine 1.7 mg/dL, and glucose 455 mg/dL. Serum lactate is 4.7 mmol/dL. Which of the following best describes her clinical state?
She has sepsis
She has systemic inflammatory response syndrome (SIRS)
She has severe sepsis
She is in septic shock
She has multiple organ dysfunction syndrome (MODS)
An 84-year-old man presents to the ED with his family due to concerns that his condition is worsening despite being placed on levofloxacin for a urinary tract infection 5 days ago by his primary care physician. His is obtunded and unable to give any additional history. Physical examination does not reveal the source of infection. His BP is 84/45 mmHg, HR is 135 beats per minute, temperature is 102.8°F, and his RR is 28 breaths per minute. Laboratory results reveal WBC 24,500/μL, hematocrit 19%, platelets 90/μL, sodium 132 mEq/L, potassium 7.5 mEq/L, chloride 100 mEq/L, bicarbonate 12 mEq/L, BUN 37 mg/dL, creatinine 6.5 mg/dL, and glucose 255 mg/dL. Serum lactate is 11.3 mmol/dL. Cardiac enzymes and troponin are mildly elevated, and he has hyperacute T-waves on electrocardiogram (ECG). His chest radiograph shows cardiomegaly with bilateral patchy opacities and pulmonary vascular congestion. Rapid urinalysis reveals 3+ WBCs and blood and nitrates. You secure his airway with intubation, initiate broad-spectrum antibiotics, IV fluids, and other supportive therapies, and emergently consult nephrology, cardiology, and pulmonology. Which of the following best describes his clinical state?
He has MODS
He has SIRS
He has sepsis
He has severe sepsis
He is in septic shock
A 37-year-old man presents to the ED with complaints of 2 days of a sore throat and subjective fever at home. He denies cough or vomiting. His BP is 130/75 mmHg, HR is 85 beats per minute, temperature is 101°F, and his RR is 14 breaths per minute. He has diffuse tonsillar swelling and bilateral exudates with bilaterally enlarged and tender lymph nodes of the neck. Which of the following is the next best step in management?
Administer penicillin and discharge the patient without further testing
Perform a rapid antigen test. If it is negative, confirm with a throat culture, and administer penicillin if the results are positive
Perform a rapid antigen test. If it is negative, administer penicillin and discharge the patient
Perform a rapid antigen test. If it is positive, administer penicillin and discharge the patient
Discharge the patient without treatment or further testing
A 37-year-old man who just finished a full course of penicillin for pharyngitis presents to the ED requesting to be checked out again. He states he took the antibiotics exactly as prescribed and initially felt somewhat improved, but over the last 2 to 3 days has had increased pain and progressive difficulty swallowing. His BP is 130/65 mmHg, HR is 95 beats per minute, temperature is 100.1°F, RR is 16 breaths per minute, and oxygen saturation is 99%. On examination, the patient is in no acute distress but has a fluctuant mass on the right side of his neck. You visualize a normal soft palate with swelling of the right tonsillar arch and deviation of the uvula to the left, but additional examination is limited because he is unable to open his mouth fully. Review of his records reveals a throat culture that was positive for Streptococcus. Which of the following is the most appropriate next step in management?
Attempt needle aspiration, treat him with a new course of antibiotics (either penicillin or clindamycin), and have him return in 24 hours
Give him morphine for pain control, give him a dose of IV antibiotics, and observe him in the ED for 6 hours
Admit him for incision and drainage in the OR under general anesthesia
Switch his antibiotic to clindamycin and have him return in 24 hours
Order a CT scan to visualize his neck, continue the penicillin, and have him return in 24 hours
A 50-year-old man presents to the ED complaining of fever, headache, and neck pain for 24 hours. He states that 1 week ago he had rhinorrhea, nasal congestion, a sore throat, and occasional dry cough. He noted generalized weakness, myalgias, and malaise yesterday afternoon, and woke up today “feeling terrible.” His BP is 145/75 mmHg, HR is 102 beats per minute, temperature is 101.2°F, and his RR is 16 breaths per minute. On examination, he is awake, alert, and nontoxic appearing although he has discomfort in his neck with flexion. He has a nonfocal neurologic examination without increased deep tendon reflexes or opthalmoplegia. There are no rashes. Which of the following CSF results is most consistent with your clinical diagnosis of viral meningitis?
A mildly elevated total protein level with a WBC count of fewer than 500 cells/mm 3
Identification of viral particles on Gram stain with an elevated CSF-to-serum glucose level
A mildly elevated total protein level with a decreased glucose level
Increased turbidity with marked xanthochromia
A markedly elevated lymphocyte count, often exceeding 100,000 cells/mm 3 with a mildly elevated total protein level
A 32-year-old woman presents to the ED with 7 days of vaginal discharge and pelvic pain. She is sexually active and admits to several recent “one night stands.” She denies trauma/injury and does not have any urinary or other abdominal complaints. Her HR is 85 beats per minute, BP is 135/90 mmHg, RR is 18 breaths per minute, and temperature is 101.4°F. On bimanual examination, you note a copious, thin, white discharge with mild diffuse adnexal tenderness with significant cervical motion tenderness. There are no rashes, skin lesions, or adenopathy. Laboratory results are notable for a WBC of 18,000/μL. A urinalysis shows WBCs but is otherwise within normal limits. Which of the following is the most appropriate next step in management?
Give her a dose of ceftriaxone (250 mg IM), and prescribe her a 10-day course of doxycycline (100 mg PO BID) with urgent gynecology follow-up within 1 week
Prescribe her a 14-day course of levofloxacin (500 mg PO once per day) and urgent gynecology follow-up within 1 week
Give her a dose of metronidazole (2 g PO) and prescribe her a 14-day course of cephalexin (500 mg) with urgent gynecology follow-up within 1 week
Give her a one-time dose of oral metronidazole (2 g PO), azithromycin (1 g PO), and ceftriaxone (250 mg IM) with gynecology follow-up if she is not feeling better
Give her a one-time dose azithromycin (1 g PO), and ceftriaxone (250 mg IM) with urgent gynecology follow-up within 1 week
A 45-year-old woman presents to the ED complaining of 3 days of fever and worsening throat pain and painful odynophagia without cough or coryza. She sits on a chair, leaning forward with her mouth slightly open. She is refusing to swallow and has a cup of saliva and a box of facial tissues at her side. Vitals are HR of 120 beats per minute, BP of 110/70 mmHg, RR of 22 breaths per minute, oxygen saturation of 99% on room air, and temperature of 102.8°F. You note a slight wheezing noise coming from her anterior neck. Her voice is hoarse and she is able to open her mouth fully, making her examination quite difficult. From what you can visualize, her posterior oropharynx is moderately hyperemic, without exudates or tonsillar enlargement. A soft tissue lateral cervical radiograph shows marked edema of the prevertebral soft tissues and absence of the vallecular space. Which of the following is the most likely diagnosis?
Epiglottitis
Retropharyngeal abscess
Peritonsillar abscess
Pharyngitis
Laryngotracheitis
A 19-year-old woman presents with 4 days of bilateral lower abdominal pain right greater than left. She also complains of a fever, nausea, vomiting, and general malaise. Her last menstrual period was 5 days ago. Vitals are HR 98 beats per minute, BP 110/65 mmHg, RR 18 breaths per minute, and temperature of 102.7°F. Pelvic examination demonstrates exquisite cervical motion tenderness and right adnexal tenderness. Laboratory reports are notable for a WBC 15,000/μL, an ESR of 95 mm/h, and a negative urine β-human chorionic gonadotropin (β-hCG). Transvaginal ultrasound demonstrates a right complex mass with cystic and solid components. Which of the following is the most appropriate next step in management?
Given her a one-time dose with emergent gynecology consultation for possible laparoscopic drainage
Prescribe her a 14-day course of levofloxacin (500 mg PO once per day) and urgent gynecology follow-up within 1 week
Give her a dose of metronidazole (2 g PO) and prescribe her a 14-day course of cephalexin (500 mg) with urgent gynecology follow-up within 1 week
Give her a one-time dose of oral metronidazole (2 g PO), azithromycin (1 g PO), and ceftriaxone (250 mg IM) with gynecology follow-up if she is not feeling better
Give her a dose of ceftriaxone (250 mg IM), and prescribe her a 10-day course of doxycycline (100 mg PO BID) with urgent gynecology follow-up within 1 week
A 42-year-old IV drug user presents to the ED with fever, chills, pleuritic chest pain, myalgias, and general malaise. The patient’s vitals include an HR of 110 beats per minute, BP of 110/65 mmHg, RR of 18 breaths per minute, and temperature of 103.4°F. Physical examination is notable for retinal hemorrhages, petechiae on the conjunctivae and mucous membranes, a faint systolic ejection murmur, and splenomegaly. Which of the following is the most likely diagnosis?
Endocarditis
Disseminated gonorrhea
Myocarditis
Pericarditis
Infectious mononucleosis
A 51-year-old diabetic man complains of intense right-ear pain and discharge. On physical examination, his BP is 145/65 mmHg, HR 91 beats per minute, and temperature 101°F. He withdraws when you retract the pinna of his ear. The external auditory canal is erythematous, edematous, and contains what looks like friable granulation tissue in the external auditory canal. The tympanic membrane is partially obstructed but appears to be erythematous, as well. You make the presumptive diagnosis of necrotizing (malignant) otitis externa. Which of the following statements regarding this condition is true?
Pseudomonas aeruginosa is the most common causative organism
It is an uncommon complication of otitis media in otherwise healthy patients
The mainstay of treatment is outpatient with oral antibiotics
Cranial nerve IX palsy is the most common complication
Hearing loss is the most common complication
A 26-year-old woman presents to the ED with fever, malaise, and an evolving rash in the right axilla that she initially thought was from an insect bite that she received while hiking 1 week earlier. She complains of generalized fatigue, nausea, headache, and joint pain over the past several days. Her vitals are BP of 120/75 mmHg, HR of 75 beats per minute, RR of 16 breaths per minute, and temperature of 101°F. On physical examination, she is awake and alert, with a nonfocal neurologic examination. Her neck is supple, but she is diffusely tender over the shoulder, knee, and hip joints bilaterally without any distinct effusions. Her abdomen is soft and nontender. She has a 9-cm erythematous annular plaque with partial central clearing and a bright red outer border and a target center under her right axilla. Which of the following is the next best step?
Treat empirically for Lyme disease with doxycycline for 21 days and arrange follow-up with her primary-care doctor
Treat empirically with broad-spectrum antibiotics and consult dermatology emergently for a biopsy of the rash
Treat empirically for a cellulitis with cephalexin for 10 days and arrange follow-up with her primary care doctor
Treat empirically for an allergic dermatitis with prednisone, diphenhydramine, and famotidine for 3 days, and arrange follow-up with her primary care doctor
Perform serologic testing for Borrelia burgdorferi to confirm the diagnosis of Lyme disease and arrange follow-up with her primary care doctor
A 22-year-old man without medical complaints presents to the ED with a 3-day history of fever, malaise, and myalgias. He denies chest pain, shortness of breath, nausea or vomiting, abdominal pain, cough, sore throat, genitourinary symptoms, or respiratory tract complaints. On examination, the patient’s BP is 100/60 mmHg, HR is 110 beats per minute, RR is 20 breaths per minute, and temperature is 102°F. He appears awake, alert, and comfortable. His physical examination is normal. Which of the following is the most appropriate next step in management?
Discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination
Order a CBC, urinalysis, and chest x-ray. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination
Order a CBC, urinalysis, chest x-ray, and two sets of blood cultures. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination
Order a CBC, urinalysis, chest x-ray, two sets of blood cultures, and perform an LP. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination
Order a CBC, urinalysis, chest x-ray, two sets of blood cultures, and perform an LP. Start empiric IV antibiotics and admit him for observation
A 54-year-old man with a history of hepatitis C, alcohol abuse, and cirrhotic ascites presents with increasing abdominal girth and abdominal pain. He complains of increasing difficulty breathing, especially when lying down, caused by worsening ascites. On physical examination, the patient is cachectic and appears older than his stated age. He has a diffusely tender abdomen and tense ascites. The liver is palpable 4 cm below the costal margin. Vitals include a BP of 110/65 mmHg, HR of 110 beats per minute, RR of 22 breaths per minute, and temperature of 102°F. Which of the following is the most common organism seen in spontaneous bacterial peritonitis?
Enterobacteriaceae
Pseudomonas aeruginosa
Enterococcus
Streptococcus pneumoniae
Streptococcus viridans
A 30-year-old man with type 1 diabetes presents to the emergency department (ED). His blood pressure (BP) is 100/70 mmHg and heart rate (HR) is 140 beats per minute. His blood glucose is 750 mg/dL, potassium level is 5.9 mEq/L, bicarbonate is 5 mEq/L, and arterial pH 7.1. His urine is positive for ketones. Which of the following is the best initial therapy for this patient?
Give normal saline in 2 L bolus and then administer 10 units of insulin intravenously followed by an insulin drip and continued hydration
Give normal saline as a 2-L bolus; then administer 20 units of regular insulin subcutaneously
Bolus 2 ampules of bicarbonate and administer 10 units of insulin intravenously
Give him 5 mg of metoprolol to slow down his heart, start intravenous (IV) hydration, and then give 10 units of regular insulin intravenously
Give normal saline in 2 L bolus with 20 mEq/L potassium chloride (KCl) in each bag
A 39-year-old woman, brought into the ED by her family, states that she has had 4 days of diarrhea and has now started acting “crazy” with mood swings and confusion. The family states that she usually takes a medication for a problem with her neck. Her BP is 130/45 mmHg, HR is 140 beats per minute, temperature is 101.5°F, and her respiratory rate (RR) is 22 breaths per minute. An electrocardiogram (ECG) reveals atrial fibrillation with a normal QRS complex. After you address the airway, breathing, and circulation (ABCs), which of the following is the most appropriate next step in management?
Administer propranolol and propylthiouracil (PTU); then wait an hour to give Lugol iodine solution
Administer 2 ampules of bicarbonate to treat for tricyclic antidepressant overdose
Administer chlordiazepoxide, thiamine, and folate
Administer ceftriaxone and prepare for a lumbar puncture
Administer ciprofloxacin and give a 2-L bolus of normal saline for treatment of dehydration secondary to infectious diarrhea
A 65-year-old woman brought into the ED by her family, states that she has been weak, lethargic, and saying “crazy things” over the last 2 days. Her family also states that her medical history is significant only for a disease of her thyroid. Her BP is 120/90 mmHg, HR is 51 beats per minute, temperature is 94°F rectally, and RR is 12 breaths per minute. On examination, the patient is overweight, her skin is dry, and you notice periorbital nonpitting edema. On neurologic examination, the patient does not respond to stimulation. Which of the following is the most likely diagnosis?
Myxedema coma
Apathetic thyrotoxicosis
Graves disease
Acute stroke
Schizophrenia
A 74-year-old woman who is a known diabetic is brought to the ED by emergency medical service (EMS) with altered mental status. The home health aide states that the patient ran out of her medications 4 days ago. Her BP is 130/85 mmHg, HR is 110 beats per minute, temperature is 99.8°F, and RR is 18 breaths per minute. On examination, she cannot follow commands but responds to stimuli. Laboratory results reveal white blood cell (WBC) count of 14,000/L, hematocrit 49%, platelets 325/L, sodium 128 mEq/L, potassium 3.0 mEq/L, chloride 95 mEq/L, bicarbonate 22 mEq/L, blood urea nitrogen (BUN) 40 mg/dL, creatinine 1.8 mg/dL, and glucose 850 mg/dL. Urinalysis shows 3+ glucose, 1+ protein, and no blood or ketones. After addressing the ABCs, which of the following is the most appropriate next step in management?
Begin fluid resuscitation with a 2- to 3-L bolus of normal saline; then administer 10 units of regular insulin intravenously
Begin fluid resuscitation with a 2- to 3-L bolus of normal saline; then administer 10 units of regular insulin intravenously and begin phenytoin for seizure prophylaxis
Administer 10 units of regular insulin intravenously; then begin fluid resuscitation with a 2- to 3-L bolus of normal saline
Order a computed tomographic (CT) scan of the brain; if negative for acute stroke, begin fluid resuscitation with a 2- to 3-L bolus of normal saline
Arrange for urgent hemodialysis
A 21-year-old man presents to the ED. He has a known history of type 1 diabetes. He is hypotensive with BP of 95/65 mmHg, tachycardic at 120 beats per minute, and tachypneic at 30 breaths per minute. Laboratory results reveal a WBC 20,000/μL, hematocrit 45%, platelets 225/μL, sodium 131 mEq/L, potassium 5.3 mEq/L, chloride 95 mEq/L, bicarbonate 5 mEq/L, BUN 20 mg/dL, creatinine 0.9 mg/dL, and glucose 425 mg/dL. Arterial blood gas reveals a pH of 7.2. Urinalysis reveals glucosuria and ketosis. There is a fruity odor to his breath. Which of the following provides the strongest evidence for the diagnosis?
Glucose of 425 mg/dL, ketosis, pH 7.2, and bicarbonate of 5 mEq/L
Hypotension, tachycardia, and tachypnea
Glucose of 425 mg/dL, ketosis, and leukocytosis
Glucose of 425 mg/dL, hypotension, and fruity odor to breath
Glucosuria, hypotension, and leukocytosis
A 32-year-old man is brought to the ED by EMS for confusion. EMS reports that the patient was at a local pharmacy filing his prescriptions when the pharmacist noticed the patient sweating and having difficulty answering questions. In the ED, the patient’s BP is 130/68 mmHg, HR is 120 beats per minute, temperature is 98.9°F, and RR is 12 breaths per minute. The patient is unable to explain what happened. His fingerstick glucose is 410 mg/dL and his urine is positive for ketones. An electrolyte panel reveals Na + 131 mEq/L, K + 4 mEq/L, Cl − 91 mEq/L, and Ca 2+ 11 mEq/L. Which of the following electrolytes are most important to supplement during the management of his medical condition?
Potassium
Sodium, potassium, and calcium
Sodium
Calcium
Sodium and calcium
A 36-year-old immigrant woman is brought to the ED from her workplace. She was found to be agitated and behaving bizarrely. The patient’s past medical history and medications are unknown. Her BP is 162/92 mmHg, HR is 140 beats per minute, temperature is 101.8°F, and RR is 18 breaths per minute. On examination, the patient is delirious, tremulous, and has a large goiter. Which of the following is the most appropriate management of this patient?
Protect airway; administer acetaminophen, propranolol, and PTU
Administer dantrolene
Administer acetaminophen and broad-coverage antibiotics
Protect airway; administer iodine
Administer diazepam
A 75-year-old woman is brought to the ED by EMS after she had a witnessed seizure on the street. A bystander reports that the patient fell to the ground, had tonic-clonic activity, and was drooling. Her BP is 162/85mmHg, HR is 95 beats per minute, temperature is 99.4°F, and RR is 16 breaths per minute. On examination, the patient is unresponsive and has a bleeding superficial scalp laceration. Which of the following electrolyte disturbances is least likely to cause a seizure?
Hypokalemia
Hypoglycemia
Hyperglycemia
Hyponatremia
Hypernatremia
A 53-year-old woman is brought to the ED by her husband. He states that his wife is feeling very weak over the last 2 days, is nauseated, and vomiting at least three times. The husband states that she was taking a high-dose medication for her joint pain but ran out of her pills last week. Her vital signs are BP of 90/50 mmHg, HR 87 beats per minute, RR 16 breaths per minute, and temperature 98.1°F. You place her on the monitor, begin IV fluids, and send her blood to the laboratory. Thirty minutes later the metabolic panel results are back and reveal the following: Na+ 126 mEq/L, K+ 5 mEq/L, Cl− 99 mEq/L, HCO3 21 mEq/L, BUN 24 mg/dL, Creatinine 1.6 mg/dL, Glucose 69 mg/dL, Ca+ 11 mEq/L. What is the most likely diagnosis?
Adrenal insufficiency
Myxedema coma
Thyroid storm
Hyperaldosteronism
Diabetic ketoacidosis (DKA)
A 44-year-old agitated woman is brought to the ED by her husband. He states that she has had fevers to 101°F and a productive cough at home for the last 3 days. Today she became labile, agitated, and complained of abdominal pain. She was recently diagnosed with Graves disease and started on PTU. Her BP is 156/87 mmHg, HR is 145 beats per minute, temperature is 102.4°F, and RR is 20 breaths per minute. On examination, the patient is agitated, confused, and has rales on auscultation bilaterally. Which of the following is the most likely diagnosis?
Thyroid storm
Pheochromocytoma
Cocaine ingestion
Heat stroke
Neuroleptic malignant syndrome
An 81-year-old diabetic woman with a history of atrial fibrillation is transferred to your emergency department (ED) from the local nursing home. The note from the facility states that the patient is complaining of abdominal pain, having already vomited once. Her vital signs in the ED are temperature 100.1°F, blood pressure (BP) 105/75 mmHg, heart rate (HR) 95 beats per minute, and respiratory rate (RR) 18 breaths per minute. You examine the patient and focus on her abdomen. Considering that the patient has not stopped moaning in pain since arriving to the ED, you are surprised to find that her abdomen is soft on palpation. You decide to order an abdominal radiographic series. Which of the findings on plain abdominal film is strongly suggestive of mesenteric infarction?
Pneumatosis intestinalis
Sentinel loop of bowel
No gas in the rectum
Presence of an ileus
Air fluid levels
A husband and wife present to the ED with 1 day of subjective fever, vomiting, watery diarrhea, and abdominal cramps. They were at a restaurant a day before for dinner and both ate the seafood special, which consisted of raw shellfish. In the ED, they are both tachycardic with temperatures of 99.8°F and 99.6°F for him and her, respectively. Which of the following is responsible for the majority of acute episodes of diarrhea?
Viruses
Parasites
Enterotoxin-producing bacteria
Anaerobic bacteria
Invasive bacteria
A 49-year-old man presents to the ED with nausea, vomiting, and abdominal pain that began approximately 2 days ago. The patient states that he usually drinks a six pack of beer daily, but increased his drinking to 2 six packs daily over the last week because of pressures at work. He notes decreased appetite over the last 3 days and states he has not had anything to eat in 2 days. His BP is 125/75 mmHg, HR is 105 beats per minute, and RR is 20 breaths per minute. You note generalized abdominal tenderness on examination. Laboratory results reveal the following: White blood cells (WBC) 9000/μL, Hematocrit 48%, Platelets 210/μL, Aspartate transaminase (AST) 85 U/L, Alanine transaminase (ALT) 60 U/L, Alkaline phosphatase 75 U/L, Total bilirubin 0.5 mg/dL, Lipase 40 IU, Sodium 131 mEq/L, Potassium 3.5 mEq/L, Chloride 101 mEq/L, Bicarbonate 10 mEq/L, Blood urea nitrogen (BUN) 9 mg/dL, Creatinine 0.5 mg/dL, Glucose 190 mg/dL, Nitroprusside test weakly positive for ketones. Which of the following is the mainstay of therapy for patients with this condition?
Solution containing both saline and glucose (D5/NS or D5 1/2 NS)
Normal saline (NS) solution
Half normal saline (1/2 NS
Glucose solution (D5W)
The type of solution is irrelevant
As you palpate the right upper quadrant (RUQ) of a 38-year-old woman’s abdomen, you notice that she stops her inspiration for a brief moment. During the history, the patient states that over the last 2 days she gets pain in her RUQ that radiates to her back shortly after eating. Her vitals include a temperature of 100.4°F, HR of 95 beats per minute, BP of 130/75 mmHg, and RR of 16 breaths per minute. What is the initial diagnostic modality of choice for this disorder?
Ultrasonography
Plain film radiograph
Computed tomography (CT) scan
Magnetic resonance imaging (MRI)
Radioisotope cholescintigraphy (HIDA scan)
A 31-year-old man from Florida presents to the ED complaining of severe pain that starts in his left flank and radiates to his testicle. The pain lasts for about 1 hour and then improves. He had similar pain last week that resolved spontaneously. He noted some blood in his urine this morning. His BP is 145/75 mmHg, HR is 90 beats per minute, temperature is 98.9°F, and his RR is 24 breaths per minute. His abdomen is soft and nontender. As you examine the patient, he vomits and has trouble lying still in his stretcher. Which of the following is the most appropriate next step in management?
Start intravenous (IV) fluids and administer an IV nonsteroidal anti-inflammatory drug (NSAID) and antiemetic
Call surgery consult to evaluate the patient for appendicitis
Order an abdominal CT
Perform an ultrasound to evaluate for an abdominal aortic aneurysm (AAA)
Perform an ultrasound to evaluate for testicular torsion
A 48-year-old man with a past medical history of hepatitis C and cirrhosis presents to the ED complaining of acute-onset abdominal pain and chills. His BP is 118/75 mmHg, HR is 105 beats per minute, RR is 16 breaths per minute, temperature is 101.2°F rectally, and oxygen saturation is 97% on room air. His abdomen is distended, and diffusely tender. You decide to perform a paracentesis and retrieve 1 L of cloudy fluid. Laboratory analysis of the fluid shows a neutrophil count of 550 cells/mm 3. Which of the following is the most appropriate choice of treatment?
Cefotaxime
Metronidazole
Vancomycin
Sulfamethoxazole/trimethoprim (SMX/TMP)
Neomycin and lactulose
A 24-year-old man woke up from sleep 1 hour ago with severe pain in his right testicle. He states that he is sexually active with multiple partners. On examination, the right scrotum is swollen, tender, and firm. You cannot elicit a cremasteric reflex. His BP is 145/75 mmHg, HR is 103 beats per minute, RR is 14 breaths per minute, temperature is 98.9°F, and oxygen saturation is 99% on room air. Which of the following is the most appropriate next step in management?
Treat the patient for epididymitis and have him return if symptoms persist
Administer one dose of ceftriaxone and doxycycline for 10 days and have him follow-up with a urologist
Swab his urethra, send a culture for gonorrhea and Chlamydia, and treat if positive
Send a urinalysis and treat for a urinary tract infection (UTI) if positive
Order a statim (STAT) color Doppler ultrasound and urologic consultation
A 55-year-old woman with a past medical history of diabetes walks into the emergency department (ED) stating that her tongue and lips feel like they are swollen. During the history, she tells you that her doctor just started her on a new blood pressure (BP) medication. Her only other medication is a baby aspirin. Her vitals at triage are: BP 130/70 mmHg, heart rate (HR) 85 beats per minute, respiratory rate (RR) 16 breaths per minute, oxygen saturation 99% on room air, and temperature 98.7°F. On physical examination, you detect mild lip and tongue swelling. Over the next hour, you notice that not only are her tongue and lips getting more swollen, but her face is starting to swell, too. What is the most likely inciting agent?
Lisinopril
Metoprolol
Furosemide
Aspirin
Diltiazem
A 45-year-old woman presents to the ED immediately after landing at the airport from a transatlantic flight. She states that a few moments after landing she felt short of breath and felt pain in her chest when she took a deep breath. Her only medications are oral contraceptive pills and levothyroxine. She is a social drinker and smokes cigarettes occasionally. Her BP is 130/75 mmHg, HR is 98 beats per minute, temperature is 98.9°F, RR is 20 breaths per minute, and oxygen saturation is 97% on room air. You send her for a duplex ultrasound of her legs, which is positive for deep vein thrombosis. What is the most appropriate management for this patient?
Place patient on a monitor, provide supplemental oxygen, and administer unfractionated heparin
Place patient on a monitor, order a chest computed tomography (CT) scan to confirm a pulmonary embolism (PE), and then administer unfractionated heparin
Place patient on a monitor and administer aspirin
Instruct the patient to walk around the ED so that she remains mobile and does not exacerbate thrombus formation
Place the patient on a monitor, provide supplemental oxygen, and administer warfarin
A tall, thin 18-year-old man presents to the ED with acute onset of dyspnea while at rest. The patient reports sitting at his desk when he felt a sharp pain on the right side of his chest that worsened with inspiration. His past medical history is significant for peptic ulcer disease. He reports taking a 2-hour plane trip a month ago. His initial vitals include an HR of 100 beats per minute, a BP of 120/60 mmHg, an RR of 16 breaths per minute, and an oxygen saturation of 97% on room air. On physical examination, you note decreased breath sounds on the right side. Which of the following tests should be performed next?
Chest radiograph
Electrocardiogram (ECG)
D-dimer
Ventilation perfusion scan (V/Q scan)
Upright abdominal radiograph
A 30-year-old obese woman with no significant past medical history presents to the ED complaining of shortness of breath and coughing up blood-streaked sputum. The patient states that she traveled to Moscow a month ago. Upon returning to the United States, the patient developed a persistent cough associated with dyspnea. She was seen by a pulmonologist, who diagnosed her with bronchitis and prescribed an inhaler. However, over the following weeks, the patient’s symptoms worsened, and she developed pleuritic chest pain. In the ED, she lets you know that she smokes half a pack per day. Her vitals include a temperature of 99°F, BP of 105/65 mmHg, HR of 124 beats per minute, RR of 22 breaths per minute, and an oxygen saturation of 94% on room air. Physical examination is noncontributory, except for rales at the left-mid lung. Her ECG reveals sinus tachycardia with large R waves in V1 to V3 and inverted T waves. Given this patient’s history and presentation, what is the most likely etiology of her symptoms?
Acute respiratory distress syndrome (ARDS)
Mycoplasma pneumoniae (“walking” pneumonia)
Q fever pneumonia
Pneumocystis jiroveci pneumonia (PCP)
PE
A 24-year-old woman is brought to the ED after being found on a nearby street hunched over and in mild respiratory distress. Upon arrival, she is tachypneic at 24 breaths per minute with an oxygen saturation of 97% on face mask oxygen administration. Upon physical examination, the patient appears to be in mild distress with supraclavicular retractions. Scattered wheezing is heard throughout bilateral lung fields. Which of the following medications should be administered first?
β2-Agonist nebulizer treatment
Corticosteroids
Magnesium sulfate
Epinephrine
Anticholinergic nebulizer treatment
An 81-year-old woman presents to the ED with acute onset of shortness of breath just before arrival. She refuses to answer questions for the interview, but repeatedly states that she is feeling short of breath. Her initial vitals include an HR of 89 beats per minute, a BP of 168/76 mmHg, and an RR of 18 breaths per minute with an oxygen saturation of 89% on room air. A portable chest x-ray appears normal. Her physical examination is unremarkable, except for a systolic ejection murmur. Intravenous (IV) access is successfully obtained. After placing the patient on oxygen and a monitor, which of the following should be performed first?
ECG
Evaluation of troponin level
Evaluation of D-dimer level
Rectal temperature
Repeat chest x-ray
As you evaluate a patient with shortness of breath, you appreciate decreased breath sounds at the left-lung base. You suspect the patient has a small pleural effusion. In which of the following views of the chest is this small pleural effusion most likely to be detected?
Lateral decubitus left-side down
Supine
Lateral decubitus right-side down
Lateral
Posterior-anterior (PA)
A 32-year-old firefighter presents to the ED in acute respiratory distress. He was taken to the ED shortly after extinguishing a large fire in a warehouse. His initial vitals include an HR of 90 beats per minute, a BP of 120/55 mmHg, and an RR of 18 breaths per minute with an oxygen saturation of 98% on 2-L nasal cannula. An ECG shows a first-degree heart block. Upon physical examination, there are diffuse rhonchi bilaterally. The patient is covered in soot and the hairs in his nares are singed. Given this clinical presentation, which of the following maybe responsible for this patient’s respiratory distress?
Thermal burns
Morphine sulfate only
Nitroglycerin only
Aspirin
Antibiotics
A 67-year-old man is brought to the ED in respiratory distress. His initial vitals include an HR of 112 beats per minute, a BP of 145/88 mmHg, and an RR of 18 breaths per minute with an oxygen saturation of 92% on room air. He is also febrile at 102°F. After obtaining IV access, placing the patient on a monitor, and administering oxygen via nasal cannula, a chest radiograph is performed and shows patchy alveolar infiltrates with consolidation in the lower lobes. On review of systems, the patient tells you that he had five to six watery bowel movements a day for the last 2 days with a few bouts of emesis. Which of the following infectious etiologies is most likely responsible for the patient’s presentation?
Legionella pneumophila
Streptococcus pneumoniae
Haemophilus influenzae
Mycoplasma pneumoniae
Chlamydophila pneumoniae
A 32-year-old woman presents to the ED with a 1-month history of general malaise, mild cough, and subjective fevers. She states that she is human immunodeficiency virus (HIV) positive and her last CD4 count, 6 months ago, was 220. She is not on antiretroviral therapy or any other medications. Initial vitals include an HR of 88 beats per minute, a BP of 130/60 mmHg, and an RR of 12 breaths per minute with an oxygen saturation of 91% on room air. Her chest radiograph shows bilateral diffuse interstitial infiltrates. Subsequent laboratory tests are unremarkable except for an elevated lactate dehydrogenase level. Given this patient’s history and physical examination, which of the following is the most likely organism responsible for her clinical presentation?
Pneumocystis jiroveci
Coccidioides immitis
Mycobacterium tuberculosis
Mycoplasma pneumoniae
Haemophilus influenzae
A 27-year-old woman presents to the ED complaining of an intensely pruritic rash all-over her body, abdominal cramping, and chest tightness. She states that 1 hour ago she was at dinner and accidentally ate some shrimp. She has a known anaphylactic allergy to shrimp. Her BP is 115/75 mmHg, HR is 95 beats per minute, temperature is 98.9°F, RR is 20 breaths per minute, and oxygen saturation is 97% on room air. She appears anxious, and her skin is flushed with urticarial lesions. Auscultation of her lungs reveals scattered wheezes with decreased air entry. Which of the following is the most appropriate next step in management?
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, administer methylprednisolone and diphenhydramine intravenously, and give intramuscular epinephrine
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and administer methylprednisolone intravenously
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and administer methylprednisolone and diphenhydramine intravenously
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and start aerosolized albuterol
Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and start aerosolized epinephrine
A 72-year-old man presents to the ED with worsening dyspnea. His initial vitals include an HR of 93 beats per minute, BP of 110/50 mmHg, and RR of 20 breaths per minute with an oxygen saturation of 88% on room air. The patient appears thin and anxious. He is using accessory muscles to breathe. Despite distant breath sounds, you hear end-expiratory rhonchi and a prolonged expiratory phase. An ECG shows peaked P waves in leads II, III, and aVF. Given this patient’s history and physical examination, which of the following conditions does this patient most likely have?
Emphysema
Chronic bronchitis
Asthma
Congestive heart failure (CHF)
Pneumothorax
A 71-year-old woman presents to the ED after a reported mechanical fall 2 days ago. Her initial vitals include an HR of 55 beats per minute, a BP of 110/60 mmHg, an RR of 14 breaths per minute, and an oxygen saturation of 96% on room air. The patient does not appear to be taking deep breaths. Her physical examination is significant for decreased breath sounds bilaterally and tenderness to palpation along the right side of her chest. After initial stabilization, which of the following is the diagnostic test of choice for this patient’s condition?
Rib radiographs
Chest x-ray
Chest CT scan
ECG
Thoracentesis
A 29-year-old woman presents to the ED for hyperventilation. Her initial vitals include an RR of 28 breaths per minute with an oxygen saturation of 100% on room air. She is able to speak in full sentences and tells you that she cannot breathe and that her hands and feet are cramping up. She denies any trauma, past medical history, or illicit drug use. Chest auscultation reveals clear breath sounds bilaterally. A subsequent chest radiograph is normal. Upon reevaluation, the patient reports that she is breathing better. Her vitals include an RR of 12 breaths per minute with an oxygen saturation of 100% on room air. Which of the following conditions is most likely the etiology of this patient’s symptoms?
Anxiety attack
Pneumothorax
Hemopneumothorax
Pleural effusion
Asthma exacerbation
A 42-year-old man presents to the ED via ambulance after activating EMS for dyspnea. He is currently on an oxygen face mask and was administered one nebulized treatment of a β2-agonist by the paramedics. His initial vitals include an RR of 16 breaths per minute with an oxygen saturation of 96% on room air. The patient appears to be in mild distress with some intercostal retractions. Upon chest auscultation, there are minimal wheezes localized over bilateral lower lung fields. The patient’s symptoms completely resolve after two more nebulizer treatments. Which of the following medications, in addition to a rescue β2-agonist inhaler, should be prescribed for outpatient use?
Corticosteroids
Magnesium sulfate
Epinephrine injection (EpiPen)
Cromolyn sodium
Ipratropium
A 22-year-old woman is brought to the ED by paramedics who state that they found the patient hunched over on a park bench barely breathing. The patient is rousable only to painful stimuli. Her initial vitals include an HR of 78 beats per minute, a BP of 125/58 mmHg, and a respiratory rate of 6 breaths per minute with an oxygen saturation of 94% on 2-L nasal cannula. Upon physical examination, the patient has clear breath sounds bilaterally and no signs of trauma. Her pupils are 2 mm bilaterally and reactive to light. Which of the following agents may be used to restore this patient’s respirations?
Naloxone
Oxygen
Flumazenil
Anticholinergic inhaler treatment
β2-Agonist nebulized treatment
A 43-year-old undomiciled man is brought to the ED after being found intoxicated on the street. He is currently rousable and expresses a request to be left alone. Initial vitals include an HR of 92 beats per minute, a BP of 125/80 mm Hg, and an RR of 14 breaths per minute with an oxygen saturation of 93% on room air. His rectal temperature is 101.2°F. A chest radiograph shows infiltrates involving the right lower lobe. Given this clinical presentation, what initial antibiotic coverage is most appropriate for this patient?
Broad-spectrum with anaerobic coverage
Gram-negative coverage only
Gram-positive coverage only
PCP coverage
Antifungal therapy
A 32-year-old man is brought into the ED by EMS with fever, shortness of breath, and stridor. The patient was treated yesterday in the ED for a viral syndrome. His BP is 90/50 mmHg, HR is 110 beats per minute, temperature is 101.2°F, and his RR is 28 breaths per minute. A chest radiograph reveals a widened mediastinum. The patient is endotracheally intubated, given a 2-L bolus of normal saline, and started on antibiotics. His BP improves to 110/70 mmHg and he is transferred to the intensive care unit (ICU). You see a friend that accompanied the patient to the hospital and ask him some questions. You find out that the patient is a drum maker and works with animal hides. What is the most likely organism that is responsible for the patient’s presentation?
Bacillus anthracis
Streptococcus pneumoniae
Corynebacterium diphtheriae
Coxiella burnetii
Haemophilus influenzae
A 62-year-old man presents to the ED with gradual dyspnea over the last few weeks. He reports that he is a daily smoker and has not seen a physician in years. Upon physical examination, there are decreased breath sounds on the right as compared to the left. A chest radiograph indicates blunting of the right costophrenic angle with a fluid line. A thoracentesis is performed. Given this patient’s history, which of the following most likely describes his effusion?
Exudative effusion
Transudative effusion
Transudative and exudative effusion
Lactate dehydrogenase < 200 units
Fluid-to-blood protein ratio < 0.5
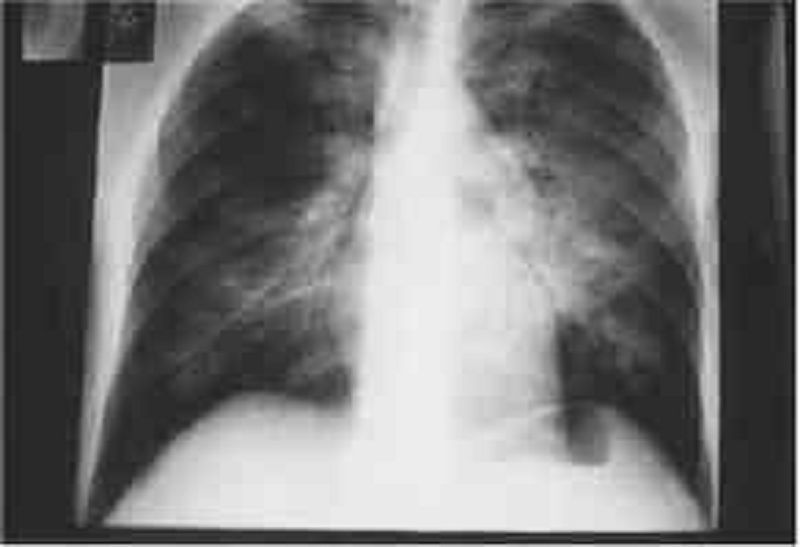
A 40-year-old man with a history of untreated HIV for 8 years comes into the ED complaining of cough, fever, and malaise for 3 days. He is tachypneic and diaphoretic. Chest radiograph reveals bilateral infiltrates. Arterial blood gas (ABG) analysis is significant for a PaO2 of 62 on room air. His chest radiograph is seen below. Which of the following is the most appropriate initial management?
Treat with corticosteroid prior to antibiotic therapy
Treat immediately with IV trimethoprim/sulfamethoxazole (TMP/SMX)
Administer antibiotics after a rapid sputum Gram stain is obtained
Treat with nebulizer
Treat with racemic epinephrine
A 34-year-old Caucasian female comes to the emergency department and complains that her heart is "racing out of control." She began to feel this way only this morning. She denies any chest pain or shortness of breath. Over the past few months, she has unintentionally lost 10 pounds. Her past medical history is significant for panic attacks, but she claims she has not had an attack for over 10 years. She is very concerned because her father died of a heart attack at the age of 40. The EKG reveals sinus tachycardia at a rate of 120/min. The initial labs show: CBC: Hb 12.9g/dL, Ht 39%, MCV 88 fl, Platelet count 200,000/cmm, Leukocyte count 8,500/cmm, Neutrophils 67%, Eosinophils 1%, Lymphocytes 24%, Monocytes 8%. Serum: Serum Na 139 mEq/L, Serum K 4.2 mEq/L, Chloride 100 mEq/L, Bicarbonate 25 mEq/L, BUN 10 mg/dL, Serum Creatinine 1.0 mg/dL, Calcium 9.1 mg/dL, Blood Glucose 102 mg/dL, TSH < 0.1 microU/mL, Free T4 4.6 ng/dL (N0.9-24). Which of the following is the best immediate step to control this patient's symptoms?
Propanolol
Propylthiouracil
Subtotal thyroidectomy
Alprazolam
Radioactive Iodine
A 45-year-old male, found unconscious, is brought to the emergency room. His airway is maintained, and oxygen is administered. His temperature is 39.0°C (102.5°F), pulse is 102/min, blood pressure is 90/65 mmHg and respirations are 23/min. Intravenous access is secured and blood and urine samples are drawn. Lab results are as follows: Sodium 134 mEq/L, Potassium 5.9 mEq/L, Chloride 101 mEq/L, Bicarbonate 22 mEq/L, Blood urea nitrogen 110 mg/dl, Glucose 1000 mg/dl, Serum calcium 10.2 mg/dl, Amylase 100 U/L, Aspartate aminotransferase 15 U/L, Alanine aminotransferase 17 U/L, Ammonia 15 micro-moi/L (Normal is 9-33 micro-moi/L), PT 13 sec, APTT 30 sec. Arterial blood gases: PH 7.40, PaCO2 38 mm Hg, PaO2 90 mm Hg. Which of the following is the most appropriate initial infusion you should order for this patient?
Normal saline
0.45% saline
5% dextrose
Regular insulin
Potassium
A 24-year-old woman comes into the emergency department with recurrent episodes of palpitations, headache, and tremor. Her blood pressure is 155/95 mmHg, heart rate is 135/min, temperature is 37.9°C (100.2°F), and respiratory rate is 12/min. A CT of the abdomen shows a suprarenal mass. After confirming the diagnosis with a laboratory test, the physician informs the patient that she will require immediate therapy and surgical resection of the mass within the next few weeks. In order to achieve short-term control of her blood pressure, which of the following agents is most appropriate?
Prazosin
Furosemide
Hydralazine
Phenelzine
Propanolol
An 18-year-old woman presents to the emergency department with acute mental status changes, rapid and deep breathing, abdominal pain, and vomiting. On examination she is tachypneic and tachycardic, her abdomen is soft and nontender, and her mucous membranes are dry. Laboratory values are notable for a potassium level of 5.5 mEq/L, bicarbonate of 12 mEq/L, and serum glucose of 400 mg/dL. Which of the following is the most appropriate strategy during the first 24 hours?
Intravenous fluids, insulin, and potassium
Diuresis and ventilatory support
Diuresis, strict potassium restriction, and insulin
Intravenous fluids, insulin, and strict potassium restriction
Intravenous fluids, loop diuretic, and potassium
A 13-year-old boy is brought to the pediatrician by his mother because of increasing body hair. Several months earlier he had been diagnosed with 17α-hydroxylase deficiency and treated with hydrocortisone. Physical examination reveals an overweight boy with a moderate amount of both chest and genital hair, and some facial hair growth. His physical examination is otherwise unremarkable. Which of the following is the best treatment for this patient?
Add dexamethasone
Add cosyntropin
Add spironolactone
Increase hydrocortisone
Keep the current dose of hydrocortisone
A 72-year-old man with atrial fibrillation presents with complaints of fatigue and feeling cold. He also notes constipation and dry skin. His daughter states he has seemed more forgetful over the past several months. His temperature is 37.3°C (99.1°F), heart rate is 48/min, and blood pressure is 130/82 mmHg. Cardiac examination shows bradycardia but normal rhythm, and normal S1 and S2 with no murmurs; the lungs are clear to auscultation bilaterally and the abdomen is soft and nontender. The patient’s extremities are cool and puffy with dry, coarse skin. Laboratory studies show a thyroid-stimulating hormone level of 32 μU/L, free thyroxine of 0.3 ng/dL, and total tri-iodothyronine of 30 ng/dL. What medication is the patient likely taking for his atrial fibrillation?
Amiodarone
Flecainide
Lithium
Methimazole
Sotalol
A 75-year-old woman is brought to the emergency department after being found unresponsive at her home. She was last spoken to by her daughter on the phone 24 hours earlier, at which time she complained of chills, lethargy, and weakness. The woman has had a heart attack in the past, she has high blood pressure, and she had a total thyroidectomy performed a decade ago for cancer. The daughter had returned from several months out of town, and is unsure if the patient was taking her medications. Her temperature is 34.9°C (94.9°F), pulse is 48/min, blood pressure is 110/65 mmHg, oxygen saturation is 99% on 100% oxygen, and glucose is 85 mg/dL. On examination the patient is unresponsive, obese, and edematous with periorbital edema. Her cardiac and pulmonary examinations are normal. CT of the head reveals no signs of trauma or increased intracranial pressure, and ECG demonstrates no acute ischemic changes. Blood is drawn for laboratory testing. Which of the following is most appropriate for treating the patient’s mental status change?
Levothyroxine
Aspirin
Glucagon
Hemodialysis
Metoprolol
A family brings their 82-year-old grandmother to the emergency room stating that they cannot care for her anymore. They tell you, “She has just been getting sicker and sicker.” Now she stays in bed and won’t eat because of stomach pain. She has diarrhea most of the time and can barely make it to the bathroom because of her weakness. Her symptoms have been worsening over the past year, but she has refused to see a doctor. The patient denies symptoms of depression. Blood pressure is 90/54 mmHg with the patient supine; it drops to 76/40 mmHg when she stands. Heart and lungs are normal. Skin examination reveals a bronze coloring to the elbows and palmar creases. What laboratory abnormality would you expect to find in this patient?
Low serum Na+
Low serum Ca+
Low serum K+
Normal serum K+
Microcytic anemia
A 58-year-old woman presents to her physician because of neck discomfort and difficulty swallowing. She first began to have difficulty with swallowing solids 2 years ago, but the problem is getting progressively worse. She denies hemoptysis, hematemesis, abdominal pain, or change in bowel habits. She is a nonsmoker and past medical history is significant only for mild hypertension. Her temperature is 36.9°C (98.4°F), heart rate is 72/min, and blood pressure is 132/78 mmHg. She has an asymmetrically enlarged thyroid gland that is particularly firm on the right, with poorly palpable borders. Laboratory evaluation reveals a free thyroxine level of 4.1 ng/dL and thyroid-stimulating hormone of 5μU/mL. Based on the results of a radioisotope scan and a fine needle aspiration biopsy, the physician decides to perform surgery. For which of the following is the patient at increased risk postoperatively?
Hypocalcemia
Bone metastases
Hypercalcemia
Hypophosphatemia
Pheochromocytoma
A 53-year-old woman presents to the clinic with complaints of headache and blurred vision for the past several months. She also says her family has commented that her face looks different, and her nose is bigger than it used to be. In addition, she says her shoes feel tighter. On physical examination she has coarse facial features with a prominent mandible and widely spaced incisors. MRI of the brain reveals a mass in the pituitary. This patient may be at increased risk of developing which of the following malignancies?
Colon cancer
Hepatocellular carcinoma
Lung cancer
Malignant brain tumor
Pancreatic adenocarcinoma
A 35-year-old white female comes to her primary care physician for the evaluation of palpitations, weight loss, increased appetite and diarrhea for the past 2 months. She denies smoking cigarettes or drinking alcohol. Her temperature is 37.1°C (98°F), blood pressure is 135/80 mmHg, respirations are 14/min, and pulse is 90/min. Physical examination shows exophthalmos, lid lag, lid retraction, and a diffusely enlarged, non-tender thyroid gland. Lab studies show very low levels of serum TSH, and increased levels of serum free T4 and T3. The diagnosis of Graves' disease is established. Various treatment options are discussed with the patient, and she opts for long-term treatment with propylthiouracil. Which of the following conditions is this patient at risk for developing?
Agranulocytosis
Hypocalcemia
Permanent hypothyroidism
Recurrent laryngeal nerve palsy
Thyroid cancer
A 35-year-old white female presents with complaints of weight gain, lethargy and constipation for the last 2 months. She also complains of cold intolerance and oligomenorrhea. She is not taking any medication. She is a non-smoker, and does not drink alcohol. Her pulse is 67/min, and blood pressure is 130/90 mmHg. She is afebrile. Her hands are dry and cold. There is a non-tender, diffuse rubbery enlargement of the thyroid gland without any discrete nodularity. She does not have exophthalmos, lid lag or lid retraction. Labs show decreased serum T4 levels, elevated serum TSH levels and positive anti-thyroperoxidase (TPO) antibodies. Which of the following complications may develop in this patient?
Lymphoma of the thyroid
Papillary carcinoma of the thyroid
Follicular carcinoma of the thyroid
Anaplastic carcinoma of the thyroid
Medullary carcinoma of the thyroid
A 36-year-old female presents with weight loss, palpitations, mild shortness of breath, heat intolerance, tremors, and increased sweating. She does not have any past medical problems. Her family history is unremarkable. Her blood pressure is 140/70 mmHg, heart rate is 104/min and regular, temperature is 99.0°F (37.2°C) and respiratory rate is 22/min. Physical examination reveals a 2 x 2 cm nodule in her left thyroid lobe. The rest of her thyroid gland feels normal. There are no palpable lymph nodes in her neck. Eye examination reveals minimal lid lag, but no signs of proptosis or chemosis. She has tremors in both of her upper extremities. Her hands are moist and warm. Thyroid function testing reveals: Serum TSH < 0.03 micro IU/ml, Total T3 330 ng/dl, Total T4 14 mcg/dl. Radioactive iodine scan shows uptake only in her left-sided nodule. Which of the following disorders is this patient at risk of developing if she is left untreated?
Bone loss
Airway compression
Thyroid cancer
Coronary artery disease
Proptosis
A 55-year-old male presents with complaints of an ulcer over the sole of his right great toe for one week. His medical problems include a ten year history of hypertension, diabetes and hypercholesterolemia. His current medications are ramipril, aspirin, metformin, glibenclamide and pravastatin. He has a 20-pack year history of smoking and occasionally drinks alcohol. He denies illegal drug use or multiple sexual partners. Which of the following is most likely contributing to the development of his foot ulcer?
Diabetic neuropathy
History of smoking
Poor glycemic control
Peripheral vascular disease
Bony abnormality of the foot
A 49-year-old woman presents to the emergency department (ED) with profuse, foul-smelling, watery diarrhea and abdominal pain. Five days ago, she was hospitalized for urosepsis and treated with amoxicillin and sulbactam. She recovered well, and was discharged three days ago with a prescription for oral amoxicillin plus clavulanic acid. Her current temperature is 38.8°C (101.9°F), blood pressure is 110/70 mmHg, pulse is 102/min, and respirations are 15/min. Abdominal examination shows tenderness in the left lower quadrant. CBC shows a WBC count of 25,000/microl. She is started on intravenous normal saline in the ED. Which of the following is the most appropriate next step in management?
Discontinue antibiotics and start oral metronidazole
Continue rehydration
Start oral metronidazole
Discontinue antibiotics
Discontinue antibiotics and start oral vancomycin
A 64-year-old man is brought to the ER after an episode of coffee ground emesis followed by lightheadedness. He has been having black, tarry stools for the past few days. He has a history of coronary artery disease and he underwent coronary artery bypass surgery three years ago. He is currently taking aspirin, metoprolol, lisinopril, and pravastatin. He drinks 2-3 beers over the weekend but he quit smoking after the bypass surgery. His temperature is 36.7°C (98°F), pulse is 110/min, respirations are 16/min, and blood pressure is 90/60 mmHg. Examination shows coffee ground-like material in the oropharynx. His lungs are clear. Abdomen is slightly tender in the epigastrium. Laboratory studies show: Complete blood count: Leukocyte count 9,500/mm3, Hemoglobin 8.1 g/L, Platelets 130,000/mm3. Chemistry panel: Serum sodium 140 mEq/L, Serum potassium 3.5 mEq/L, Bicarbonate 27 mEq/L, Blood urea nitrogen (BUN) 54 mg/dL, Serum creatinine 1.2 mg/dL Which of the following is the most appropriate next step in management of this patient?
Packed red blood cell transfusion
Whole blood transfusion
Fresh frozen plasma infusion
Hemodialysis
Platelet transfusion
A 50-year-old female presents with heartburn and gnawing abdominal pain. She was diagnosed with peptic ulcer disease 3 years ago, but she has been non-adherent to her medications. She asks you if her nonadherence puts her at increased risk of any complications. Which of the following is the most common complication of peptic ulcer disease?
Hemorrhage
Perforation
Penetration
Gastric outlet obstruction
Atrophic gastritis
A 37 -year-old male is brought to the emergency department due to an episode of hematemesis. He has a history of peptic ulcer disease. A nasogastric tube lavage yields coffee-ground-like material. Physical examination reveals pallor and delayed capillary refill, without cyanosis. His temperature is 36.7°C (98°F), blood pressure is 85/40 mmHg, pulse is 125/min, and respirations are 18/min. Which of the following is the most appropriate first step in management?
Fluid resuscitation
Intravenous octreotide
Upper GI endoscopy
Surgical intervention
Intravenous pantoprazole
A 54-year-old man is brought to the ER because of an episode of coffee ground emesis and lightheadedness. He has a history of intravenous drug use, hepatitis C infection, and alcohol use. He says he has not had an alcoholic drink for about three days. He has been noncompliant with medications and follow-ups. He takes no medications. His temperature is 36.7°C (98°F), pulse is 110/min, respirations are 16/min, and blood pressure is 90/60 mmHg. Scleral icterus is present. Examination shows coffee ground material in the oropharynx. His lungs are clear. His abdomen is distended and a fluid wave is present. He is slightly tender to palpation in the epigastrium. Laboratory studies show: Complete blood count:Leukocyte count 9,500/mm3, Hemoglobin 10.0 g/L, Platelets 120,000/mm3. Chemistry panel:Serum sodium 140 mEq/L, Serum potassium 3.5 mEq/L, Bicarbonate 27 mEq/L, Blood urea nitrogen (BUN) 34 mg/dL, Serum creatinine 0.8 mg/dL. Coagulation studies :Prothrombin time 27 sec, Partial thromboplastin time 42 sec. Which of the following is the most appropriate next step in the management of this patient?
Fresh frozen plasma infusion
Whole blood transfusion
Hemodialysis
Pooled platelet transfusion
Plasmapheresis
An undomiciled 41-year-old man walks into the ED complaining of abdominal pain, nausea, and vomiting. He tells you that he has been drinking beer continuously over the previous 18 hours. On examination, his vitals are BP 150/75 mm Hg, HR 104 beats per minute, RR 16 breaths per minute, oxygen saturation 97% on room air, temperature of 99.1°F rectally, and finger stick glucose 81 mg/dL. The patient is alert and oriented, his pupils anicteric. You notice gynecomastia and spider angiomata. His abdomen is soft but tender in the RUQ. Laboratory tests reveal an AST of 212 U/L, ALT 170 U/L, alkaline phosphatase of 98 U/L, total bilirubin of 1.9 mg/dL, international normalized ratio (INR) of 1.3, WBC 12,000/μL. Urinalysis shows 1+ protein. Chest x-ray is unremarkable. Which of the following is the most appropriate next step in management?
Provide supportive care by correcting any fluid and electrolyte imbalances
Place a nasogastric tube in the patient’s stomach to remove any remaining ethanol
Order a HIDA scan to evaluate for acute cholecystitis
Administer hepatitis B immune globulin
Send viral hepatitis titers
An 84-year-old woman with coronary artery disease, congestive heart failure, peripheral vascular disease, and atrial fibrillation presents to the emergency department with dizziness, weakness, and sudden-onset crampy periumbilical pain. The pain is associated with one episode of diarrhea and one episode of emesis. The patient notes she has been having similar pain after meals for “several months” but never this severe. Her temperature is 37.2°C (98.9°F), heart rate is 135/min, blood pressure is 96/60 mm Hg, and respiratory rate is 16/min. Physical examination is notable for a slightly distended abdomen that is extremely tender to palpation with diminished bowel sounds. There is no rigidity or rebound tenderness noted on the abdominal examination. In addition, the patient has heme positive stool. Her WBC count is 19,500/mm³, hemoglobin is 10.9 g/dL, and platelet count is 159,000/mm³. Liver function testing results are normal. After stabilizing the patient, what is the best next step in management?
Laparotomy
Barium enema
Colonoscopy
Obstruction series
Warfarin therapy
A 51-year-old man is brought to the emergency department (ED) by emergency medical services (EMS) with a blood pressure (BP) of 90/60 mm Hg, heart rate (HR) of 110 beats per minute, respiratory rate (RR) of 18 breaths per minute, and oxygen saturation of 97% on room air. The patient tells you that he has a history of bleeding ulcers. On examination, his abdomen is tender in the epigastric area. He is guaiac positive, with black stool. He has a bout of hematemesis and you notice that his BP is now 80/50 mm Hg, HR is 114 beats per minute, as he is slowly starting to drift off. Which of the following is the most appropriate next step in therapy?
Assess airway, establish two large-bore intravenous (IV) lines, cross-match for two units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Assess airway, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor
Place two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor
A 19-year-old woman presents to the ED with 1 hour of acute-onset progressively worsening pain in her RLQ. She developed nausea shortly after the pain and vomited twice over the last hour. She had similar but less severe pain 2 weeks ago that resolved spontaneously. Her BP is 123/78 mm Hg, HR is 99 beats per minute, temperature is 99.1°F, and her RR is 16 breaths per minute. On physical examination, the patient appears uncomfortable, not moving on the gurney. Her abdomen is nondistended, diffusely tender, worst in the RLQ. Pelvic examination reveals a normal-sized uterus and moderate right-sided adnexal tenderness. Laboratory results reveal WBC 10,000/μL, hematocrit 38%, and a negative urinalysis and β-hCG. Pelvic ultrasound reveals an enlarged right ovary with decreased flow. Which of the following is the most appropriate management for this patient?
Go for immediate laparoscopic surgery
Admit to the gynecology service for observation
Administer IV antibiotics and operate once inflammation resolves
Attempt manual detorsion
Order an abdominal CT
A 22-year-old woman is brought to the ED by ambulance complaining of sudden onset of severe abdominal pain for 1 hour. The pain is in the RLQ and is not associated with nausea, vomiting, fever, or diarrhea. On the pelvic examination you palpate a tender right adnexal mass. The patient’s last menstrual period was 6 weeks ago. Her BP is 95/65 mm Hg, HR is 124 beats per minute, temperature is 99.8°F, and RR is 20 breaths per minute. Which of the following are the most appropriate next steps in management?
Bolus 2 L NS, order a type and crossmatch and β-hCG, and call gynecology for possible surgery
Provide her oxygen via face mask and administer morphine sulfate
Administer morphine sulfate, order an abdominal CT with contrast, and call an emergent surgery consult
Send the patient’s urine for analysis and order an abdominal CT
Provide oxygen via face mask, give morphine sulfate, and order a transvaginal ultrasound
A 67-year-old man is brought to the ED by emergency medical service (EMS). His wife states that the patient was doing his usual chores around the house when all of a sudden he started complaining of severe abdominal pain. He has a past medical history of coronary artery disease and hypertension. His BP is 85/70 mm Hg, HR is 105 beats per minute, temperature is 98.9°F, and his RR is 18 breaths per minute. On physical examination, he is diaphoretic and in obvious pain. Upon palpating his abdomen, you feel a large pulsatile mass. An electrocardiogram (ECG) reveals sinus tachycardia. You place the patient on a monitor, administer oxygen, insert two largebore IVs, and send his blood to the laboratory. His BP does not improve after a 1-L fluid bolus. Which of the following is the most appropriate next step in management?
Call surgery and have them prepare the operating room (OR) for an exploratory laparotomy
Order a CT scan to evaluate his aorta
Call the angiography suite and have them prepare the room for the patient
Order a portable abdominal radiograph
Call the cardiac catheterization laboratory to prepare for stent insertion
A 32-year-old man with Crohn’s disease presents to the emergency department with acute-onset diffuse abdominal pain and emesis. The patient states these symptoms are different than his usual Crohn’s disease flare-ups. The pain is severe (10/10) and is cramping in nature. He says his abdomen feels larger than usual. His Crohn’s disease has been well managed on 6-mercaptopurine for the past 6 months. The patient denies any recent sick contacts or eating underprepared foods. He states he had a bowel movement and flatus since the abdominal pain began. In addition to Crohn’s disease, the patient had appendicitis for which he underwent an appendectomy 12 years ago. His temperature is 37.1°C (98.7°F), blood pressure is 135/86 mm Hg, pulse is 84/min, and respiratory rate is 14/ min. On physical examination the abdomen is distended and diffusely tender with high-pitched bowel sounds. There is rebound tenderness throughout the abdomen along with guarding. The remainder of the physical examination is noncontributory. An x-ray of the abdomen shows dilated small loops of bowel along with absence of gas in the colon. What is the best next step in management?
Laparotomy
Bowel rest only
Intravenous fluids and antibiotics only
MRI of the abdomen
Ultrasound
A 24-year-old man with a history of depression is brought to the emergency room because of a drug overdose. He is experiencing some nausea and vomiting, but no other symptoms. Physical examination and vital signs are normal. Six hours prior to presentation, he intentionally took 40 tablets of acetaminophen (500mg/tablet). Which of the following is the most appropriate next step in management?
Give N-acetylcysteine to allow binding of the toxic metabolite
Give ethanol to compete with the parent drug for metabolism, therefore preventing formation of toxic metabolites
Give Narcan to block its actions directly
Give intravenous prostacyclins to maintain cellular integrity
Give glucocorticoids to block the immune cascade

A 58-year-old man comes to the emergency department complaining of colicky abdominal pain over the past 3 days that suddenly became more severe and constant over the past 6 hours. A contrast study is performed and results are shown in the image. What is the first-line treatment after fluid resuscitation and nasogastric tube placement?
Hemicolectomy
Colonoscopy
Proximal colostomy with delayed resection
Sigmoid colectomy
Sigmoidoscopy
A 59-year-old woman with renal cell carcinoma presents to the emergency department with severe right upper quadrant (RUQ) pain. She is afebrile, acutely tender in the RUQ, and has shifting dullness and a palpable liver edge. Murphy’s sign is negative. Laboratory studies show: Na+: 138 mEq/L, K+: 3.6 mEq/L, Glucose: 80 mg/dL. Aspartate aminotransferase: 50 U/L Alanine aminotransferase: 43 U/L Alkaline phosphatase: 138 U/L Total protein: 6.4 g/dL, Albumin: 3.8 g/dL, Total bilirubin: 1.1 mg/dL. Imaging demonstrates a spider web of collateral veins in the liver. Although extensive measures are taken, the patient dies 6 hours after arriving. Which of the following was the most likely initial treatment?
Tissue plasminogen activator followed by anticoagulation
β-Blocker followed by lactulose
Cholecystectomy
Endoscopic retrograde cholangiopancreatography with dilation of the common bile duct
Exploratory laparotomy
A 67-year-old woman with a history of hypertension and congestive heart failure presents with “burning” epigastric pain that began 2 hours after eating a meal. She states that she has had similar pain over the past several weeks, and has been taking antacids and a medication that her primary care physician had prescribed with moderate relief. The pain has occurred with increasing frequency and now awakens her from sleep. She states she came to the ED today because the pain was not relieved with her usual medications. She denies nausea, vomiting, diarrhea, or fever. She also denies hematemesis, black stool, or bright red blood per rectum. On physical examination, she is tender at the epigastrium, with an otherwise normal abdominal, pulmonary, and heart examination. Stool guaiac tests positive for occult blood. Which of the following is the most common serious complication of peptic ulcer disease?
GI haemorrhage
GI perforation
GI penetration
Gastric outlet obstruction
Pernicious anemia
A 70-year-old man with a history of constipation has been experiencing intermittent left-sided abdominal pain and fevers for 2 days. He came to the emergency department immediately after he noticed blood in his toilet this morning. His heart rate is 110/min, blood pressure is 90/50 mm Hg, respiratory rate is 18/ min, and oxygen saturation is 95% on room air. On physical examination the physician notes copious amounts of bright red blood per rectum. The physician immediately places two large bore intravenous lines, administers fluid, and sends blood for type and screen. Which of the following is the best next step in management?
Nasogastric tube aspiration
Arteriography
Colonoscopy
Endoscopy
Surgical consultation
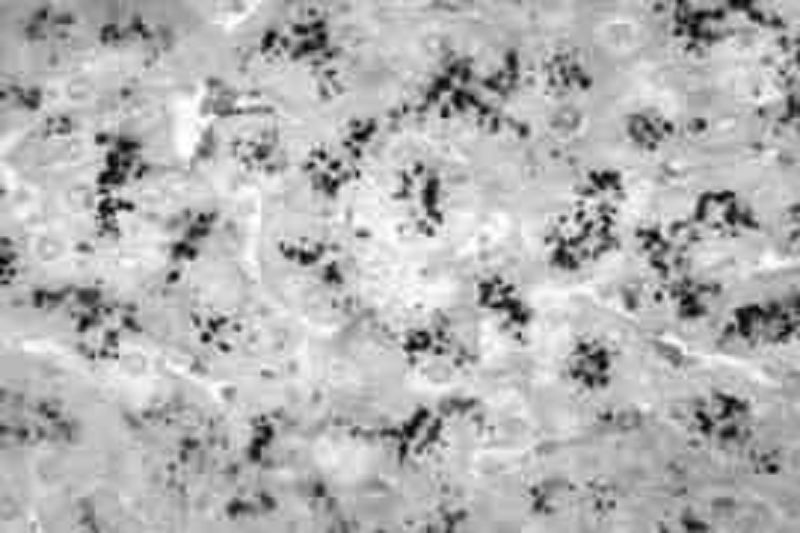
A 75-year-old woman with a history of diabetes and coronary heart failure presents to the emergency department because of increasing abdominal girth. In recent months she has been feeling increasingly fatigued, and although she has had decreased appetite, she has gained weight. Her heart rate is 100/min and blood pressure is 112/70 mm Hg. She has scleral icterus; the skin over her face, neck, and lower legs is slightly bronze in color; she has palmar erythema; and she has numerous ecchymoses over her body. Her abdominal examination is significant for ascites. Laboratory tests show: Aspartate transaminase: 102 U/L, Alanine transaminase: 97 U/L, Alkaline phosphatase: 300 U/L, Total bilirubin: 1.9 mg/dL, Albumin: 2.9 g/dL, Prothrombin time: 22 sec, Partial thromboplastin time: 42 sec. An ultrasound of her abdomen shows a shrunken and nodular liver. A liver biopsy using Perls Prussian blue stain is shown in the image. Which of the following is the most likely complication of her disease?
Hepatocellular carcinoma
Acute pancreatitis
Amyloidosis
Bone marrow failure
Splenomegaly
A 62-year-old woman with a history of diabetes mellitus presents to the emergency department complaining of severe abdominal pain for the past 12 hours, first beginning as dull pain near the umbilicus but now localized to the right lower quadrant. She initially thought she was suffering from heartburn, but decided to come to the hospital because of the unrelenting pain. The patient reports that just prior to examination by the physician, she experienced a sudden decrease in intensity of pain, but she remains feeling very uncomfortable and must remain on the stretcher. On examination the patient appears in distress secondary to pain, tachycardic, slightly hypotensive, and febrile at 39°C (102°F). She has a diffusely tender abdomen with point tenderness over her right lower quadrant, accompanied by guarding and rebound. Laboratory values showed a leukocytosis of 20,000/mm³ with 95% polymorphonuclear lymphocytes. After confirming the diagnosis with imaging, which of the following is the most appropriate management?
Emergent appendectomy and postoperative antibiotics
Give nothing by mouth with intravenous hydration
Percutaneous drainage and interval appendectomy
Serial abdominal examinations
Urgent ECG and cardiac enzymes

A 47-year-old woman presents to the emergency department with an 8-day history of left lower quadrant pain and semi-formed stools. Starting this afternoon, she has noticed blood in her stool as well as dizziness when she gets up from sitting. She denies fever, nausea, vomiting, weight loss, and night sweats. Her temperature is 37°C (98.6°F), heart rate is 104/ min, blood pressure is 120/82 mm Hg supine and 103/63 mm Hg when she sits up, and respiratory rate is 18/min. Physical examination reveals no peritoneal signs and is remarkable only for fecal occult blood on rectal examination. Laboratory results reveal a WBC count of 13,000/mm³ and hematocrit of 29%. Results of an x-ray of the abdomen are shown in the image. What is the best next step in management?
Intravenous hydration and blood transfusion
Angiography with embolization
Immediate surgery for partial colectomy
Nothing by mouth, nasogastric tube, and broad-spectrum antibiotics
Place the patient on a high-fiber diet
A 57-year-old woman presents to the ED with a basin in her hand and actively vomiting. You insert an IV catheter, start IV fluids, and administer an antiemetic agent. The patient feels much better but also complains of severe crampy abdominal pain that comes in waves. You examine her abdomen and note that it is distended and that there is a small midline scar in the lower abdomen. Upon auscultation, you hear high-pitched noises that sound like “tinkles.” Palpation elicits pain in all four quadrants but no rebound tenderness. She is guaiac negative. Which of the following is the most common cause of this patient’s presentation?
Hysterectomy
Travel to Mexico
Ethanol abuse
Hernia
Constipation
A 48-year-old woman comes to the office because her regular screening mammogram revealed irregular densities. Radiographic-guided needle biopsy shows evidence of invasive lobular carcinoma. The tumor is hormone receptor positive (HR +). Further investigation reveals involvement of the axillary lymph nodes; the other breast seems to be spared. No distant metastasis is detected. She undergoes modified radical mastectomy, along with radiotherapy. She is then prescribed adjuvant chemotherapy and tamoxifen for 5 years. This patient's use of tamoxifen increases her risk for developing which of the following cancers:
Endometrial cancer
Ovarian cancer
Lung cancer
Pancreatic cancer
Cervical cancer
A 54-year-old Caucasian woman presents to your office with fatigue. She also reports dizziness and palpitations after moderate physical activity. Additionally, her feet feel "numb" and are less sensitive to cold than they used to be. She has no significant past medical history. Physical examination reveals pale conjunctivae and a shiny tongue. Ankle reflex is decreased bilaterally. Laboratory findings include: Hemoglobin 7.6 mg/dL, MCV 110 fL, MCHC 36 g/dL, WBC count 3,900/mm3, Platelet count 150,000/mm3. This patient should be monitored for which of the following long-term complications?
Gastric cancer
Acute myelogenous leukemia
Hodgkin's disease
Celiac sprue
Liver cirrhosis
A 34-year-old male is brought to the emergency room after being involved in a motor vehicle accident. He suffers blunt abdominal trauma and bilateral femur fractures. He has no significant past medical history. On physical examination, his blood pressure is 80/40 mmHg and his heart rate is 110/min. He receives several units of packed red blood cells. Once stabilized, the patient begins complaining of a tingling sensation in his toes and fingers. His serum calcium level is noted to be 7.2 mg/dL. Which of the following is the most likely cause of this patient's current symptoms?
Calcium chelation by a substance in the transfused blood
Increased renal tubular secretion of calcium
Electrolyte leakage from red blood cells during pre-transfusion storage
Antibody-mediated red blood cell membrane damage
Parathyroid gland suppression due to fluid overload
An 81-year-old man is brought to the hospital due to complaints of very severe pain in his back and thighs. Seven months ago, he was diagnosed with stage IV prostate cancer which reached the spine. He has had palliative radiotherapy of his spine, and is now taking leuprolide. He is restless and very irritable, even after the nursing home staff gave him ibuprofen. He has never received any narcotics. What is the best next step in this patient's pain management?
Start with short-acting morphine
Give high dose NSAIDs
T ransdermal fentanyl patch
Long-acting opiates
Repeat radiotherapy
A 45-year-old previously healthy male is brought to the emergency room because of headaches and confusion for 2 days. He denies any focal weakness or sensory symptoms. He has no significant past medical history and does not use any medications. He does not use tobacco, alcohol or drugs. On physical exam, the patient has a temperature of 37.9°C (100.2°F), a blood pressure of 140/86 mm Hg, a pulse of 96/min, and respirations of 16/min. Mild icterus is present. The patient's oropharynx is clear and his neck is supple and without rigidity. Examination of the patient's chest and abdomen is unremarkable. Neurologic examination reveals no focal deficits. Laboratory studies show: Complete blood count: Hemoglobin 84 g/L, Platelet count 80,000/mm3, Leukocyte count 5,500/mm3. Chemistry panel:Blood urea nitrogen (BUN) 30 mg/dL, Serum creatinine 2.2 mg/dL, Serum calcium 10.0 mg/dL, Blood glucose 98 mg/dL. A peripheral blood smear shows many fragmented red blood cells. The prothrombin time is normal. Which of the following is the most appropriate next step in the management of this patient?
Plasma exchange
Hemodialysis
MRI of the brain
Electroencephalogram
Platelet transfusion
{"name":"(EXAM) Part 4 (765-865) (765-1019) NR 4", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge of emergency medicine with this comprehensive quiz designed for medical professionals and students alike. With 30 challenging questions focused on real-world clinical scenarios, you'll be able to assess your understanding and application of critical medical concepts.Topics covered include: Diagnostic proceduresManagement of acute conditionsInfectious diseasesTrauma carePharmacology","img":"https:/images/course2.png"}
More Quizzes
Part 4O
65320
USMLE_Management XIV
100500
MIS
38190
Diwali
10545
Which TommyInnit Era Are You? - Free Online
201018368
Will I Be Successful - Free Self-Assessment
201017788
Alpha Gamma Delta Initiation Test - Free Practice
201019432
Is Santa Real? Yes or No - Free
201016945
Cheboygan Day CommonLit Answers - Free Practice
201017006
Personality Plus Test Online - Free Type Assessment
201018678
Ideal Date - Find Your Perfect Date Idea (Free)
201016592
Cluster B Disorders Knowledge Test - Free with Answers
201020681