DES C_Management (8) Prepared : CHILLY
A 45-year-old man is brought to the emergency department after being involved in a motor vehicle collision. He is conscious but in severe pain. His blood pressure is 90/60 mm Hg, pulse is 100/min and respirations are 17/min. Physical examination shows marked swelling and some bruising over the right thigh; the skin is intact. An x-ray film of the leg shows a fracture of the mid shaft of the femur. After hemodynamically stabilizing the patient, which of the following is the most appropriate next step in management?
Closed intramedullary fixation of the femoral shaft
Internal fixation of the fracture with plates and screw
Open intramedullary nailing of the femur
Place a plaster cast
External fixation of the fracture
A 45-year-old man is brought to the emergency department after being involved in a motor vehicle collision. He is unable to void. Examination shows blood at the urethral meatus and a scrotal hematoma. His temperature is 37C (98.6F), blood pressure is 100/50, pulse is 100/min and respirations are 16/min. Examination shows a high-riding prostate with no other signs of trauma. Which of the following is the most appropriate next step in management?
Diuretic to increase the urine output
Retrograde cystogram with post-void films
Immediate surgical repair of urethra
Retrograde urethrogram
Foley catheterization
A 45-year-old man is brought to the emergency department after being involved in an automobile crash. He is alert and oriented, with a normal neurologic examination. His respiratory rate is 20/min, with clear lungs, pulse rate of 120/min, and blood pressure of 80/40 mmHg. On examination, he is noted to have a distended abdomen, with decreased bowel sounds, and a fracture of the right ankle. IV access is established, and the patient receives a rapid infusion of 2 L of saline, without changes to pulse rate or blood pressure. Which of the following is the most appropriate next step in his management?
Focused abdominal sonography for trauma (FAST)
Diagnostic peritoneal lavage
Insertion of a Swan-Ganz catheter
Exploratory laparotomy
Abdominal CT scan
A 45-year-old man is brought to the emergency department following a serious motor vehicle collision. Despite heroic attempts to save him, the physician caring for him believes he is brain dead. Unfortunately, the patient does not have an advanced directive or durable medical power of attorney. What step is necessary in order to remove the patient from the ventilator?
Notify the county medical examiner
No further steps are necessary
Ask the hospital ethics committee
Confirm brain death with another physician
Ask his family members
A 45-year-old man presents after a high-speed motor vehicle collision. He has a seatbelt sign across his neck and chest with an ecchymosis over his left neck. He is hemodynamically stable and neurologically intact. A CT angiogram shows a left carotid dissection. In the absence of other significant injuries, what is the next step in his management?
Neck exploration and left intra-extracranial bypass
Angiography and left carotid artery stenting
Neck exploration and left carotid artery repair
Antiplatelet therapy
Systemic anticoagulation with heparin
A 45-year-old man presents to the physician’s office complaining of dysphagia and retrosternal pressure and pain of 2-year duration. The symptoms have worsened over the last 3 months. He has a 30 pack-year smoking history and drinks beer on weekends. Vital signs include a BP of 150/90 mmHg, pulse rate of 90/min, and respiratory rate of 12/min, with a normal temperature. Examination reveals a thin man with a normal heart, lung, and abdomen examination. An esophagogram reveals a 6-cm, smooth, concave defect in the mid-esophagus with sharp borders. Esophagoscopy reveals intact overlying mucosa and a mobile tumor. Which of the following is the most appropriate next step?
Thoracotomy with esophageal resection
Radiation therapy
Chemotherapy
Thoracotomy with extramucosal resection
Repeat esophagoscopy with biopsy
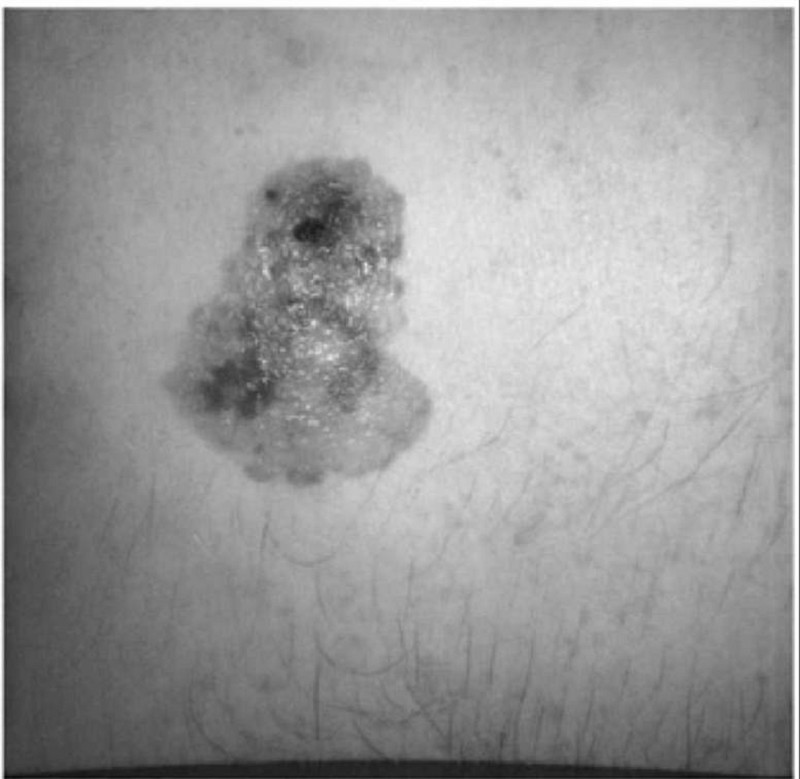
A 45-year-old man presents to the physician’s office for evaluation of a skin lesion on his abdomen. He states that the lesion has been present for 1 year, but has recently enlarged over the last 2 months. The mass is nontender, and he is otherwise asymptomatic. Past history is unremarkable. Examination reveals a 3-cm, pigmented, irregular skin lesion located in the left lower quadrant of the abdomen, as shown in Figure 6-12. Heart, lung, and abdominal examination are normal. There are no palpable cervical, axillary, or inguinal lymph nodes. Chest x-ray and liver fun
Wide excision with 2 cm margin
Mohs’ surgical excision
Excisional biopsy with 1–2 mm margins
Shave biopsy
Wide excision with 2 cm margin and SLN mapping
A 45-year-old man presents with right upper quadrant abdominal pain and fever. CT scan shows a large, calcified cystic mass in the right lobe of the liver. Echinococcus is suggested by the CT findings. Which of the following is the most appropriate management of echinococcal liver cysts?
Medical treatment with steroids
Total pericystectomy
Medical treatment with metronidazole
Percutaneous catheter drainage
Medical treatment with albendazole
A 45-year-old man shows up in the emergency department with a pale, pulseless, paresthetic, painful, and paralytic right lower extremity. The process began suddenly 2 hours ago. On examination, no pulses are apparent in the right lower extremity. Pulse at the wrist is 95/min and grossly irregular. Treatment would likely be based on which of the following?
Heparin and dicumarol
Selective sympathetic blocks medical
Saphenous vein bypasses
Dacron prosthetic vascular conduits
Fogarty balloon tipped catheters
A 45-year-old man was discovered to have a hepatic flexure colon cancer during a colonoscopy for anemia requiring transfusions. Upon exploration of his abdomen in the operating room, an unexpected discontinuous 3-cm metastasis is discovered in the edge of the right lobe of the liver. Preoperatively, the patient was counseled of this possibility and the surgical options. Which of the following is the most appropriate management of this patient?
Right hemicolectomy with postoperative radiation therapy to the liver
Closure of the abdomen followed by chemotherapy
Right hemicolectomy with local resection of the liver metastasis
A diverting ileostomy should be performed and further imaging obtained
Right hemicolectomy
A 45-year-old man with a history of chronic peptic ulcer disease undergoes a truncal vagotomy and antrectomy with a Billroth II reconstruction for gastric outlet obstruction. Six weeks after surgery, he returns, complaining of postprandial weakness, sweating, light-headedness, crampy abdominal pain, and diarrhea. Which of the following would be the best initial management strategy?
Preparation for revision to Roux-en-Y gastrojejunostomy
Workup for neuroendocrine tumor (eg, carcinoid)
Dietary advice and counseling that symptoms will probably not abate but are not dangerous
Dietary advice and counseling that symptoms will probably abate within 3 months of surgery
Treatment with a long-acting somatostatin analog
A 45-year-old man with advanced chronic renal failure comes to the physician because of edema of his feet. His temperature is 37°C (99°F), blood pressure is 150/100mm Hg, pulse is 78/min, and respirations are 15/min. Examination shows bilateral ankle edema. Laboratory studies show BUN of 62 mg/dl, serum creatinine of4.2 mg/dl, serum potassium of 5.6 meq/l, serum sodium of 146 meq/l, and total plasma cholesterol of 260 mg/dl. Which of the following is most likely to improve the prognosis of his disease?
Captopril
Potassium restriction
Salt restriction
Simvastatin
Protein restriction
A 45-year-old man with alcoholic cirrhosis is bleeding from a duodenal ulcer. He has required 6 units of blood over the past 8 hours, and all conservative measures to stop the bleeding, including irrigation with cold saline, IV vasopressin, and endoscopic use of the laser have failed. He is being considered for surgical intervention. Laboratory studies done at the time of admission, when he had received only one unit of blood, showed a bilirubin of 4.5 mg/dL, a prothrombin time of 22 seconds, and a serum albumin of 1.8 g/dL. He was mentally clear when he came in, but has since then developed encephalopathy and is now in a coma. Which of the following best describes his operative risk?
Prohibitive regardless of attempts to improve his condition
Prohibitive unless he is dialyzed to normalize his bilirubin
Amenable to improvement if he receives vitamin K
Acceptable as he now is
Amenable to improvement if he is given albumin
A 45-year-old man with known cirrhosis due to hepatitis C is admitted to the hospital for abdominal discomfort and confusion. Physical examination reveals a distended abdomen, leg edema, and deep yellow discoloration of the skin and sclerae. Bibasilar crackles are heard on chest auscultation. His serum sodium level is 127 mEq/L, potassium level is 2.9 mEq/L, and creatinine level is 1.3 mg/dl. On day 3 of his hospitalization, the serum creatinine is 4.2mg/dl. A urinalysis reveals: Protein negative, Glucose negative, WBC 4-5/hpf, RBC 0-1/hpf. Renal ultrasound is normal and the post-void residual urinary volume is less than 50 ml. He is given 2 L of normal saline intravenously with no change in his serum creatinine concentration. This patient's kidney dysfun
High-dose spironolactone
Pegylated interferon
Broad spectrum antibiotics
Liver transplantation
ACE inhibitors
A 45-year-old man with poorly controlled hypertension presents with severe chest pain radiating to his back. An ECG demonstrates no significant abnormalities. A CT scan of the chest and abdomen is obtained, which demonstrates a descending thoracic aortic dissection extending from distal to the left sub-clavian take off down to above the iliac bifurcation. A Foley catheter is placed, and urine output is 30 to 40cc/h. His feet are warm, with less than 2-second capillary refill. Which of the following is the most appropriate initial management?
Initiation of a vasodilator such as nitroprusside
Echocardiography to rule out cardiac complications
Initiation of a β-blocker
Angiography to confirm the diagnosis of aortic dissection
Emergent operation for repair of the aortic dissection
A 45-year-old white man presents to your office complaining of daytime somnolence, increased fatigability, and morning headaches. He says that his wife complains that he snores loudly. He is not taking any medications and does not smoke or consume alcohol. His blood pressure is 145/90 mmHg and heart rate is 90/min. Physical examination reveals a well-nourished man with BMI = 31 kg/m2. What is the next best step in the management of this patient?
Weight reduction
Tracheostomy
A thiazide diuretic for hypertension
A benzodiazepine to improve sleep
Advise to sleep in supine position
A 45-year-old woman has an incidental finding of a liver mass on a CT scan. Magnetic resonance imaging (MRI) is suggestive of a hemangioma. Which of the following is the most appropriate management strategy for this patient?
Resection of the hemangioma
Liver transplantation
Percutaneous biopsy of the lesion to confirm the diagnosis
Discontinuation of oral contraceptive pills
Observation
A 45-year-old woman is found to have suspicious appearing calcifications in the right breast on a screening mammogram. Stereotactic biopsy of the calcifications shows lobular carcinoma in situ (LCIS). On examination both breasts are dense without palpable masses. The neck and bilateral axilla are negative for lymphadenopathy. Which of the following is the most appropriate management of this patient?
Right total mastectomy with sentinel lymph node biopsy
Bilateral modified radical mastectomy
Frequent self-breast examinations and yearly screening mammograms
Chemotherapy
Radiation
A 45-year-old woman is undergoing chemotherapy for breast cancer. She presents 10 days after her last chemotherapy with fever (temperature > 38.5°C), but no other symptoms except a sore throat and mouth. On examination, she looks well, there is oral mucositis, ears are normal, lungs are clear, and the central line site is clean. The CXR, urinalysis, and biochemistry are normal. Her WBC is 800/mL and the absolute neutrophil count is low ( < 500). Which of the following is the most appropriate next step in management?
Start antiviral medications for HSV-1
Start antiviral and bacterial antibiotics
Acetaminophen alone until culture results are available
Start empiric bacterial antibiotics
Start empiric antifungal and bacterial antibiotics
A 45-year-old woman presents to the ED with 1 day of painful rectal bleeding. Review of systems is negative for weight loss, abdominal pain, nausea, and vomiting. On physical examination, you note an exquisitely tender swelling with engorgement and a bluish discoloration distal to the anal verge. Her vital signs are HR 105 beats per minute, BP 140/70 mm Hg, RR 18 breaths per minute, and temperature 99°F. Which of the following is the next best step in management?
Recommend warm sitz baths, topical analgesics, stool softeners, a high-fiber diet, and arrange for surgical follow-up
Incision and drainage under local anesthesia or procedural sedation followed by packing and surgical follow-up
Obtain a complete blood cell (CBC) count, clotting studies, type and cross, and arrange for emergent colonoscopy
Surgical consult for immediate operative management
Excision under local anesthesia followed by sitz baths and analgesics
A 45-year-old woman presents to your office complaining of one week of fatigue and weakness in her shoulders and hips. She reports difficulty performing household tasks, climbing the stairs, or rising from a chair. She denies any facial weakness or blurry vision. She has a history of gastroesophageal reflux disease and takes over the counter ranitidine. Her family history is positive for breast cancer in her mother. Her vital signs are within normal limits and examination shows normal sensation and deep tendon reflexes. Strength is 4 out of 5 in the proximal muscles groups of the arms and legs, and there is no limitation in the range of motion. Other physical examination is within normal limits. The ESR is 80 mm/hour and her serum creatine kinase is elevated. The TSH is within normal limits. Which of the following is the best initial treatment for this patient?
Indomethacin
Colchicine
Riluzole
Amitriptyline
Corticosteroids
A 45-year-old woman presents with a 7-cm renal cell carcinoma with radiologic evidence of abdominal lymph node involvement with no distant metastases. Which of the following is the most appropriate management of this patient?
Radiation followed by nephrectomy
Radical nephrectomy
Radiation
Chemotherapy
Chemotherapy followed by nephrectomy
A 45-year-old woman presents with dysphagia, regurgitation of undigested food, and weight loss. She had x-rays shown here as part of her workup. Upper endoscopy reveals no evidence of malignancy and esophageal motility studies show incomplete lower esophageal sphincter relaxation. Which of the following is the next best step in the treatment of this patient?
Laparoscopic 360 (Nissen) fundoplication
Laparoscopic anterior 180 (Dor) fundoplication
Laparoscopic posterior 180 (Toupet) fundoplication
Laparoscopic myotomy of the lower esophageal sphincter (Heller)
Transhiatal esophagectomy
A 45-year-old woman presents with left-sided weakness. A CT scan of the head demonstrates a well-circumscribed mass abutting the skull in the right hemisphere. Workup of the mass reveals a meningioma. Which of the following is the best next step in treatment?
Surgical excision
Chemoradiation
Chemotherapy with adriamycin
Preoperative radiation therapy followed by surgical excision
Cerebral angiography with tumor embolization
A 45-year-old woman presents with right eye pain and redness for 1 day. She has photophobia and watery discharge from the eye. She does not wear glasses or contact lenses and has no prior eye problems. On examination, the patient’s visual acuity is 20/20 in the left eye and 20/70 in the right eye. She has conjunctival injection around the cornea and clear watery discharge. On slit-lamp examination, the lids, lashes, and anterior chamber are normal. When fluorescein is applied, a branching, white-colored epithelial defect is seen. The remainder of the head examination is normal and the patient has no cutaneous lesions. Which of the following is the most appropriate treatment for this patient?
Topical steroids
Immediate ophthalmology consultation
Topical antiviral medication
Admission for intravenous (IV) antibiotics
Admission for IV antiviral agents
A 45-year-old woman with cirrhosis secondary to autoimmune hepatitis is seeing her hepatologist for routine follow-up. She reports that she has been feeling relatively well lately, and complains only of mild fatigue. Her medical history is otherwise unremarkable. Her medications include lactulose, spironolactone, propranolol and furosemide. Her vital signs are stable and the remainder of her physical exam is consistent with compensated cirrhosis. Her laboratory values are given below: Sodium 132 mEq/L, Potassium 4.1 mEq/L, Chloride 100 mEq/L, Bicarbonate 24 mEq/L, Glucose 102 mg/dl, Creatinine 0.9 mg/dl, Calcium 7.4 mg/dl, Total protein 6.1 g/dl, Albumin 2.5 g/dl, Total bilirubin 2.1 mg/dl, AST 80 units/L, ALT 102 units/L. What is the most appropriate next step in the management of this patient's hypocalcemia?
Initiate oral calcium and vitamin D replacement
No intervention is required
Replace furosemide with hydrochlorothiazide (HCTZ)
Calcium gluconate infusion
Measurement of vitamin D levels
A 45-year-old woman with history of heavy nonsteroidal anti-inflammatory drug ingestion presents with acute abdominal pain. She undergoes exploratory laparotomy 30 hours after onset of symptoms and is found to have a perforated duodenal ulcer. Which of the following is the procedure of choice to treat her perforation?
Highly selective vagotomy with omental patch
Hemigastrectomy
Truncal vagotomy and pyloroplasty
Truncal vagotomy and antrectomy
Simple closure with omental patch
A 45-year-old woman with no PMH presents to the office for an increase in abdominal fullness and bloating, worsening over the past 3 or 4 months. The patient states that she feels nauseous all the time, although has not had any vomiting. She states because of the constant nausea, she has not been eating as much. She has had a 10-lb weight loss in the last 4 months. BP, 110/70 mm Hg; P, 97; R, 18; T, 98.6°F. ROS: Denies fever and chills, Weight loss has occurred (10 lb in 4 months), Denies chest pain, shortness of breath, and abdominal pain, Nausea is present with no vomiting, No diarrhea or constipation. PE: Gen: Awake, alert, oriented x3, Abd: Soft, nontender, distended bowel sounds are present, shifting dullness to percussion is present, Pelvic: Cervix normal, no cervical motion tenderness, right adnexal enlargement is present. Which of the following is the next step in the management of this patient?
Abdominal US
Pelvic US
CA-125
BHCG
Hepatitis panel
A 45-year-old woman with previously documented urge incontinence continues to be symptomatic after following your advice for conservative self-treatment. Which of the following is the best next step in management?
Refer her to a urologist for urethral dilation
Schedule a voiding cystourethrogram
Schedule a retropubic suspension of the bladder neck
Prescribe Ditropan (oxybutynin chloride)
Prescribe Estrogen therapy
A 46-year-old female is brought to the emergency department because of visual blurring and altered mental status. She was recently treated for gout. Physical examination shows moderate to severe splenomegaly and positive sternal tenderness. Laboratory studies reveal a WBC count of 120, 000/uL with left shifted myeloid series and basophilia. Bone marrow exam shows 3% blasts. Repeat CBC is ordered. The hematologist-on-call decides to start leukophereses emergently. What another drug should be given to this patient?
Cladribine
Interferon alpha
Imatinib mesylate
Hydroxyurea
Cyclophosphamide
A 46-year-old male comes to the emergency department because of an abrupt onset of worsening epigastric pain radiating to the back and vomiting. His temperature is 36.5C (97.6F), blood pressure is 100/70 mm of Hg, pulse is 100/min and respirations are 20/min. Examination shows a mildly distended abdomen that is very tender to palpation in the epigastric region without rebound; bowel sounds are absent; rectal examination shows no abnormalities. An x-ray film of the abdomen shows gaseous distention of the small bowel in the upper abdomen. CT with contrast shows diffuse hypodense enlargement of the pancreas and peripancreatic and perirenal fluid collections. Nasogastric suction, intravenous normal saline, analgesics and antibiotics are started. Laboratory studies show: Hemoglobin 15.0 g/L, Platelets223,000/mm3, Leukocyte count14,500/mm3, Serum sodium,134mEq /L, Serum potassium 3.6 mEq/L, Chloride 93 mEq/L, Bicarbonate 29 mEq/L, Blood urea nitrogen (BUN) 30 mg/dL, Serum creatinine 0.8 mg/dL, Calcium 10.3 mg/dL, Blood glucose 168 mg/dL, Total bilirubin 1.4 mg/dL, Alkaline phosphatase 220 U/L, Aspartate aminotransferase (SGOT) 88 U/L, Alanine aminotransferase (SGPT) 155 U/L, Lipase 523 U/L. Which of the following is the most appropriate next step in management?
Obtain a right upper quadrant ultrasound
Administer intramuscular carbachol to treat ileus
Add intravenous pancreatic protease inhibitor
Colonoscopic decompression
Add intravenous sodium bicarbonate
A 46-year-old male comes to your office for a routine health examination. He has no current physical complaints and says he is compliant with his medications. His past medical history is significant for type 2 diabetes diagnosed two years ago that he has been able to control with diet, exercise and metformin. The patient also takes a daily aspirin. On physical examination, he has a temperature of 36.7°C (98°F), a blood pressure of 140/86 mmHg, a pulse of 80/min, and respirations of 14/min. His laboratory studies show: Total cholesterol 170 mg/dl, High density lipoprotein (HDL) 50 mg/dl, Low density lipoprotein (LDL) 65 mg/dl, Triglycerides (TG) 150 mg/dl, HbA1C 7.0. Serum chemistries are with in normal limits. Which of the following is the most appropriate next step in the management of this patient?
Add niacin
Add ezetimibe
Add insulin
Add gemfibrozil
Add lisinopril
A 46-year-old male is brought to the ER because of coffee ground emesis. He has a history of chronic hepatitis C and alcohol abuse. His temperature is 36.6C (97.9F), blood pressure is 120/70 mm Hg, pulse is 90/min and respirations are 14/min. He is oriented to time, place and person but somewhat sleepy. A flapping tremor is noted. His abdomen is soft, non-tender, and mildly-distended; liver and spleen are palpated below the costal margins; shifting dullness is present. Nasogastric tube aspiration shows bright red blood that was easily cleared with saline lavage. Endoscopy shows a fresh ulcer with a small adherent clot located high on the lesser curvature near the gastroesophageal junction. Non bleeding esophageal and gastric varices are also seen. Laboratory studies show: Hemoglobin 10.2 g/L, MCV 105 fl, Platelets 105,000/mm3, Leukocyte count 4,500/mm3, Prothrombin time 17 sec, Aspartate aminotransferase (SGOT) 78 U/L, Alanine aminotransferase (SGPT) 50 U/L, Which of the following is the most appropriate next step in management?
Gastric resection, selective vagotomy and pyloroplasty
Conservative medical management
Esophageal and proximal gastric devascularization and splenectomy
Sclerotherapy of the varices
Porto-systemic shunt
A 46-year-old male is hospitalized with severe acute pancreatitis. Because of progressive respiratory difficulty, he is intubated and placed on mechanical ventilation. His weight is 70 kg (152 lb), blood pressure is 110/70 mmHg, and heart rate is 90/min. Chest x-ray shows patchy opacities bilaterally, consistent with pulmonary edema. His current ventilator settings are: assist control mode, respiratory rate of 12/min, tidal volume of 450 ml, FiO2 of 40%, and positive end-expiratory pressure (PEEP) of 5 cm H20. His blood gas readings are: pH 7.51, pCO2 22mmHg, pO2 121mmHg. Which of the following is the best next step in managing this patient?
Decrease FiO2
Incentive spirometry
Bronchodilator therapy
Decrease respiratory rate
Increase tidal volume
A 46-year-old male was admitted with epigastric pain radiating to the back. He has a previous history of endocarditis from intravenous drug use and cellulitis of the arm. Serum lipase is elevated. He was admitted and treated conservatively. Two days later he started to have a fever. He is awake but slightly disoriented. His temperature is 38.7C (101.6F), blood pressure is 120/76 mm Hg, pulse is 110/min and respirations are 16/min. He is tremulous and says bugs are crawling on him. His blood cultures are positive for gram negative rods. Empiric antibiotic therapy is started. CT scan of the abdomen shows a new 6 x 6 cm cystic lesion attached to the pancreatic head. Laboratory results show: Hematocrit 44.0 g/L, MCV 105fl, Leukocyte count 18,500/mm3, Amylase 255 U/L. Which of the following is the most appropriate next step in management?
Continue conservative management
External drainage of the cystic lesion
Perform lumbar puncture to rule out meningitis
Obtain Ca 19-9 level for pancreatic cancer
Obtain echocardiogram to evaluate for endocarditis
A 46-year-old man comes to the emergency department because of abrupt onset of epigastric pain radiating to the back and associated vomiting. He has had these symptoms for the past 1 day. The symptoms are progressively getting worse. He has no other medical problems or previous surgeries. He does not use tobacco, alcohol, or illicit drugs. His temperature is 36.5°C (97.6°F), blood pressure is 100/70 mm Hg, pulse is 100/min, and respirations are 20/min. Abdomen is mildly distended and very tender to palpation in the epigastric region; bowel sounds have decreased. There is no rebound tenderness or organomegaly. Rectal examination shows no abnormalities. Laboratory findings reveal: CBC: Hb 15.0 g/dL, Platelet count 223,000/mm3, Leukocyte count 14,500/mm3, Serum Chemistry: Serum Na 134 mEq/L, Serum K 3.6 mEq/L, Chloride 93 mEq/L, Bicarbonates 29 mEq/L, BUN 30 mg/dL, Serum creatinine 0.8 mg/dL, Calcium 10.3 mg/dL, Blood glucose 168 mg/dL, LFT 1.4 mg/dL. Total bilirubin: Alkaline phosphatase 220 U/L, Aspartate aminotransferase 88 U/L, Alanine aminotransferase 155 U/L, Lipase 523 U/L. Abdominal x-ray shows gaseous distention of the small bowel in the upper abdomen. Computed tomography (CT) scan with contrast shows diffuse hypodense enlargement of the pancreas and peripancreatic and perirenal fluid collections. Nasogastric suction, intravenous normal saline, analgesics, and antibiotics are started. Which of the following is the most appropriate next step in management?
Administer intramuscular carbachol to treat ileus
Obtain a right upper quadrant ultrasound
Add intravenous pancreatic protease inhibitor
Perform colonoscopic decompression
Add intravenous sodium bicarbonate
A 46-year-old man comes to the physician because of a two day history of worsening abdominal discomfort and persistent vomiting. He has not had a bowel movement or passed flatus for 3 days. He had an appendectomy for appendicitis 20 years ago. Examination shows a distended abdomen that is tympanic on percussion. High-pitched bowel sounds and splashing are heard on auscultation. The abdomen is diffusely tender on palpation without rebound or guarding. An x-ray film of the abdomen shows distended small bowel loops with air-fluid levels; no gas is seen in the colon. IV rehydration is started. Which of the following is the most appropriate next step in management?
Nasogastric suction and intravenous fluids
Start total parenteral nutrition
Barium enema under fluoroscopic control
Administer bethanechol
Emergency laparotomy
A 46-year-old woman presents to your office complaining of something bulging from her vagina for the past year. It has been getting progressively more prominent. She has started to notice that she leaks urine with laughing and sneezing. She still has periods regularly every 26 days. She is married. Her husband had a vasectomy for contraception. After appropriate evaluation, you diagnose a second-degree cystocele. She has no uterine prolapse or rectocele. Which of the following is the best treatment plan to offer this patient?
Surgical correction with a bladder neck suspension procedure
Use of vaginal estrogen cream
Antibiotic therapy with
Le Fort colpocleisis
Anticholinergic medications
A 46-year-old woman suffering from systemic lupus erythematosus (SLE) develops hematuria and proteinuria. She was diagnosed with SLE four years ago and has been treated with hydroxychloroquine. A renal biopsy is performed and shows diffuse proliferative glomerulonephritis. She is started on cyclophosphamide and prednisone and hydroxychloroquine is stopped. She continues these two medications for several weeks because of the low therapeutic response. This new therapeutic regimen puts her at an increased risk for which of the following conditions?
Cochlear dysfunction
Digital vasospasm
Peripheral neuropathy
Bladder carcinoma
Optic neuritis
A 46-year-old woman who was recently diagnosed with Crohn disease asks about the need for surgery. Which of the following findings would be an indication for an immediate exploratory laparotomy?
Enterovesical fistula
Free perforation
Enterovaginal fistula
Ileum-ascending colon fistula
Intestinal obstruction
A 46-year-old woman, who had always been in good health, comes in because of the sudden onset of very severe back and leg pain that she experienced 2 hours ago when attempting to lift a heavy object. She says that she felt "a bolt of lightning" running down the back of her leg, and she still has very severe pain that prevents her from walking or moving. The pain is exacerbated by coughing, sneezing, or straining. She keeps the affected leg flexed; straight leg rising gives her excruciating pain. She has good sphincter tone and intact sensation in the perineum. Once the diagnosis is confirmed with the appropriate studies, which of the following will be the most appropriate treatment?
Body cast for 3-6 months
Surgical decompression
Radiotherapy to the affected area
Analgesics and bed rest for about 3 weeks
Appropriate antibiotics
A 47-year old woman comes to the clinic because of worsening left breast swelling and pain. She had mastitis when she nursed her first child 20 years ago. She has not seen a doctor since that time. She is afebrile. Breast examination shows the left breast is enlarged with a 7 x 6 cm area of edema and erythema. A poorly localized mass without fluctuation is palpated in that area. Scant non-bloody discharge is noted on the nipple, and several large axillary nodes are palpated. Which of the following is the most appropriate next step in management?
Biopsy for histology and treatment depending on the findings of the histology
Biopsy for culture and treatment depending on the findings of the culture
Drainage, culture of the drained exudate and treatment depending on the findings of the culture
Culture of the discharge and treatment depending on the findings of the culture
Antibiotic active against Streptococci and Staphylococci
A 47-year-old asymptomatic woman is incidentally found to have a 5-mm polyp and no stones in her gallbladder on ultrasound examination. Which of the following is the best management option?
In bloc resection of the gallbladder, wedge resection of the liver, and portal lymphadenectomy
Laparoscopic cholecystectomy
Open cholecystectomy with frozen section
Observation with repeat ultrasound examinations to evaluate for increase in polyp size
Aspiration of the gallbladder with cytologic examination of the bile
A 47-year-old Caucasian female presents with occasional episodes of nocturnal substernal chest pain that wakes her up during sleep. The pain episodes last 15-20 minutes and resolve spontaneously. She denies any illicit drug use. She leads a sedentary lifestyle but states that she can climb two flights of stairs without any discomfort. She has no history of hypertension or diabetes. Her pulse is 75/min and regular, blood pressure is 134/70 mmHg and respirations are 14/min. Extended ambulatory ECG monitoring reveals transient ST segment elevation in leads I, aVL, and V4-V6 during the episodes. Which of the following is the best treatment for this patient?
Diltiazem
Propranolol
Aspirin
Heparin
Digoxin
A 47-year-old diabetic woman comes to the physician due to the recent onset of tremors. She has undergone combined pancreatic and kidney transplantation secondary to end stage renal disease and diabetes. She takes multiple medications, including immunosuppressants. Her temperature is 36.1° C (97°F), blood pressure is 152/90 mm Hg, pulse is 78/min, and respirations are 16/min. Examination shows gum hypertrophy. Laboratory studies show: Hb 13.0 g/dl, WBC 8,000/cmm, Serum Na 135 mEq/L, Serum K 5.3 mEq/L, BUN 26 mg/dl, Serum Creatinine 1.7 mg/dl. Which of the following immunosuppressants is most likely responsible for her presentation?
Cyclosporine
Tacrolimus
Azathioprine
Mycophenolate
Diuretic
A 47-year-old male who has just returned from a cruise to the Bahamas presents to the hospital with a high-grade fever, productive cough and shortness of breath for the past two days. He also complains of frequent vomiting and diarrhea. He has no prior medical problems, does not take any medications, and denies using tobacco, alcohol or drugs. His temperature is 40°C (104°F), blood pressure is 110/65 mm Hg, pulse is 80/min, and respirations are 18/min. Lung examination reveals right lower lobe crackles. The abdomen is soft and non-tender. Chest x-ray demonstrates right lower lobe consolidation. Sputum Gram stain contains many neutrophils with no organisms. Which of the following antibiotics must be given to this patient?
Vancomycin
Fluconazole
Amoxicillin
Azithromycin
Clindamycin
A 47-year-old man comes to the office for the evaluation of a sore over his right ear. His sore bleeds and oozes, and has remained open for 3 weeks. He thinks that it has been growing slowly over the past year. He works for the postal service (USPS), and is usually out all day delivering mail. He admits to smoking approximately 2 packs of cigarettes daily for the last 13 years. Physical examination reveals a punched out 1.5 cm ulcer on his right auricle. There are no enlarged lymph nodes. Full thickness biopsy reveals proliferating malignant cells which arise from the epidermis and extend into the dermis in lobules or strands. What is the best next step in the management of this patient?
Observe for 3 weeks and then examine
Local chemotherapy with anticancer creams
Wide excision with at least 5 em margins
Scraping
Surgical excision with 1-2 mm of clear margins
A 47-year-old man with a history of hypertension presents to the ED complaining of continuous left-sided chest pain that began while snorting cocaine 1 hour ago. The patient states he never experienced chest pain in the past when using cocaine. His BP is 170/90 mmHg, HR is 101 beats per minute, RR is 18 breaths per minute, and oxygen saturation is 98% on room air. The patient states that the only medication he takes is alprazolam to “calm his nerves.” Which of the following medications is contraindicated in this patient?
Metoprolol
Aspirin
Lorazepam
Nitroglycerin
Diltiazem
A 47-year-old man with hypertensive nephropathy develops fever, graft tenderness, and oliguria 4 weeks following cadaveric renal transplantation. Serum creatinine is 3.1 mg/dL. A renal ultrasound reveals mild edema of the renal papillae but normal flow in both the renal artery and the renal vein. Nuclear scan demonstrates sluggish uptake and excretion. Which of the following is the most appropriate next step?
Performing renal biopsy, steroid boost, and immunoglobulin therapy
Decreasing steroid and cyclosporine dose
Performing an angiogram
Beginning FK 506
Beginning intravenous antibiotics
A 47-year-old woman comes to the physician for an annual examination. One year ago, she was diagnosed with endometrial carcinoma and underwent a total abdominal hysterectomy and bilateral salpingo-oophorectomy. She was found to have grade I, stage I, disease at that time. Over the past year, she has developed severe hot flashes that occur throughout the day and night and are worsening. She is also concerned because her mother and several of her aunts have severe osteoporosis. She wonders whether she can take estrogen replacement therapy. Which of the following is the most appropriate response?
Estrogen replacement therapy may be used, and there are no risks
Estrogen replacement therapy is absolutely contraindicated
Estrogen replacement therapy will lead to cancer recurrence
Estrogen replacement therapy will lead to breast cancer
Estrogen replacement therapy may be used, but there are risks
A 47-year-old woman presents to your office complaining of two days of pain and itching over her left chest. Her medical history is significant for breast cancer for which she underwent a left-sided mastectomy six months ago. She has also been receiving chemotherapy and radiation. Physical examination reveals erythema around the mastectomy scar, with excoriations and occasional vesicles. Which of the following is the best treatment for her condition?
Topical 5-fluorouracil
Acyclovir
Mupirocin
Fluconazole
Topical corticosteroids
A 48-year-old Caucasian female is undergoing a routine work-up 9 months after radical mastectomy due to right-sided breast cancer. She has no present complaints, and says that she is 'full of energy'. Chest radiograph reveals an isolated pulmonary nodule, 2.0 cm in diameter, in the middle lobe of the right lung. CT confirms that the lesion is solitary with poorly defined margins, but completely within lung parenchyma. Bone scan is negative. CT abdomen and pelvis is normal. Transthoracic biopsy demonstrates adenocarcinoma with positive estrogen receptors (ER) and no HER-2/neu overexpression. Which of the following is the best management strategy for this patient?
Combined chemotherapy and endocrine therapy
Pretreatment with monoclonal antibodies against HER-2/neu
Surgery
Hormone therapy
Systemic chemotherapy
A 48-year-old G2P2 presents for her well-woman examination. She had two uneventful vaginal deliveries. She had a vaginal hysterectomy for fibroids and menorrhagia. She denies any medical problems, but has not seen a doctor in 6 years. Her family history is significant for stroke, diabetes, and high blood pressure. On examination she is a pleasant female, stands 5 ft 3 in tall, and weighs 85 kg. Her blood pressure is 150/92 mm Hg, pulse 70 beats per minute, respiratory rate 14 breaths per minute, and temperature 37C (98.4F). Her breast, lung, cardiac, abdomen, and pelvic examinations are normal. The next appropriate step in the management of this patient’s blood pressure is which of the following?
Diet, exercise, weight loss, and repeat blood pressure in 2 months
NSAID
Beta-blocker
Diuretic
Calcium channel blocker
A 48-year-old man presents with jaundice, melena, and right upper quadrant abdominal pain after undergoing a percutaneous liver biopsy. Endoscopy shows blood coming from the ampulla of Vater. Which of the following is the most appropriate first line of therapy for major hemobilia?
Percutaneous transhepatic biliary drainage (PTBD)
Hepatic resection
Ligation of bleeding vessels
Transarterial embolization (TAE)
Correction of coagulopathy, adequate biliary drainage, and close monitoring
A 48-year-old man sustains a gunshot wound to the right upper thigh just distal to the inguinal crease. He is immediately brought to the ER. Peripheral pulses are palpable in the foot, but the foot is pale, cool, and hypesthetic. The motor examination is normal. Which of the following statements is the most appropriate next step in the patient’s management?
The patient should be observed for at least 6 hours and then reexamined for changes in the physical examination
A duplex examination should be obtained to rule out a venous injury
A fasciotomy should be performed prophylactically in the emergency room
A neurosurgical consult should be obtained and somatosensory evoked potential monitoring performed
The patient should be taken to the operating room immediately to evaluate for a significant arterial injury
A 48-year-old man with a past medical history of hepatitis C and cirrhosis presents to the ED complaining of acute-onset abdominal pain and chills. His BP is 118/75 mm Hg, HR is 105 beats per minute, RR is 16 breaths per minute, temperature is 101.2°F rectally, and oxygen saturation is 97% on room air. His abdomen is distended, and diffusely tender. You decide to perform a paracentesis and retrieve 1 L of cloudy fluid. Laboratory analysis of the fluid shows a neutrophil count of 550 cells/mm 3. Which of the following is the most appropriate choice of treatment?
Sulfamethoxazole/trimethoprim (SMX/TMP)
Cefotaxime
Neomycin and lactulose
Metronidazole
Vancomycin
A 48-year-old woman complains of joint pain and morning stiffness for 4 months. Examination reveals swelling of the wrists and MCPs as well as tenderness and joint effusion in both knees. The rheumatoid factor is positive, antibodies to cyclic citrullinated protein are present, and subcutaneous nodules are noted on the extensor surfaces of the forearm. Which of the following statements is correct?
The patient should receive a 3-month trial of full-dose nonsteroidal anti-inflammatory agent before determining whether and/or what additional therapy is indicated
The patient’s prognosis is highly favorable
A nonsteroidal anti-inflammatory drug should be added to aspirin
The patient has RA and should be evaluated for disease-modifying antirheumatic therapy
Prednisone 60 mg per day should be started
A 48-year-old woman consults with you regarding menopausal symptoms. Her periods have become less regular over the past 6 months. Her last period was 1 month ago. She started having hot flushes last year. They have been getting progressively more frequent. She has several hot flushes during the day, and she wakes up twice at night with them as well. She has done quite a lot of reading about perimenopause, menopause, and hormone replacement therapy. She is concerned about the risks of taking female hormones. She wants to know what she should expect in regard to her hot flushes if she does not take hormone replacement. You should tell her which of the following?
Hot flushes are the final manifestation of ovarian failure and menopause
Hot flushes can begin several years before actual menopause
Hot flushes usually resolve within 1 week after the initiation of HRT
Hot flushes are normal and rarely interfere with a woman’s well-being
Hot flushes usually resolve spontaneously within 1 year of the last menstrual period
A 48-year-old woman presents to her gynecologist because of vaginal bleeding. She states that after a year of hot flashes and irregular cycles, she finally stopped menstruating 4 months ago. Two days ago she began having some vaginal bleeding that was very similar to her prior menses. She is concerned because she heard that the first sign of endometrial cancer in postmenopausal women is vaginal bleeding. She is an otherwise healthy woman with no medical problems. She exercises three times a week and takes multivitamins. She had three children when she was 29–35 years old. She used oral contraceptive pills for contraception from the time she was 18 until she got married at the age of 28. Which of the following is the most appropriate next step in managing this woman’s vaginal bleeding?
Measure serum level of follicle-stimulating hormone
Prescription of testosterone cream
Abdominal ultrasound
Follow-up examination in 6 months
Endometrial biopsy
A 49-year-old man presents to the clinic for a health maintenance visit. He has a family history of type 2 DM. His medical history is significant for gastroesophageal reflux disease, for which he takes omeprazole and over-the-counter antacids. He smokes one pack of cigarettes per day and drinks an average of two beers per night. The patient’s body mass index is 32 kg/m². Which of the following most greatly reduce(s) the patient’s risk of future coronary artery disease, renal failure, and retinopathy?
Daily multivitamin
Weight loss and exercise
Smoking cessation
Diet rich in fruit and vegetables
Alcohol avoidance
A 49-year-old man presents to the ED with nausea, vomiting, and abdominal pain that began approximately 2 days ago. The patient states that he usually drinks a six pack of beer daily, but increased his drinking to 2 six packs daily over the last week because of pressures at work. He notes decreased appetite over the last 3 days and states he has not had anything to eat in 2 days. His BP is 125/75 mm Hg, HR is 105 beats per minute, and RR is 20 breaths per minute. You note generalized abdominal tenderness on examination. Laboratory results reveal the following: White blood cells (WBC) 9000/μL Sodium 131 mEq/L Hematocrit 48% Potassium 3.5 mEq/L Platelets 210/μL Chloride 101 mEq/L Aspartate transaminase (AST) 85 U/L Bicarbonate 10 mEq/L Alanine transaminase (ALT) 60 U/L Blood urea nitrogen (BUN) 9 mg/dL Alkaline phosphatase 75 U/L Creatinine 0.5 mg/dL Total bilirubin 0.5 mg/dL Glucose 190 mg/dL Lipase 40 IU Nitroprusside test weakly positive for ketones Which of the following is the mainstay of therapy for patients with thiscondition?
Solution containing both saline and glucose (D 5/NS or D 5 NS)
The type of solution is irrelevant
Normal saline (NS) solution
Glucose solution (D5W)
Half normal saline (NS)
A 49-year-old man who underwent liver transplantation 5 years ago for alcoholic cirrhosis presents with a gradually increasing bilirubin level. He undergoes a liver biopsy, which demonstrates a paucity of bile ducts. Which of the following is his best option for treatment?
Exploratory laparotomy with thrombectomy of the portal vein
Retransplantation
Exploratory laparotomy with hepatic arterial reconstruction
Administration of a monoclonal antibody against T cells
Increase his immunosuppression
A 49-year-old obese man has become irritable, his face has changed to a round configuration, he has developed purplish lines on his flanks, and he is hypertensive. A 24-hour urine collection demonstrates elevated cortisol levels. This is confirmed with bedtime cortisol measurements of 700ng/mL. Which of the following findings is most consistent with the diagnosis of Cushing disease?
A 1-cm bronchogenic mass on magnetic resonance imaging (MRI)
Suppression with high-dose dexamethasone suppression testing
A 3-cm adrenal mass on computed tomography (CT) scan
Glucocorticoid use for the treatment of inflammatory disorders
Decreased ACTH levels
A 49-year-old woman has a firm, 2-cm mass in the right breast that has been present for 3 months. Mammogram has been read as "cannot rule out cancer," but it cannot diagnose cancer either. A fine-needle aspiration of the mass (FNA) and cytology do not identify any malignant cells. Which of the following is the most appropriate next step in management?
Core or incisional biopsies
Modified radical mastectomy
Lumpectomy and axillary dissection
Repeat mammogram and FNA in 1 month
Reassurance and reappointment in a year
A 49-year-old woman presents to her physician with dysphagia, regurgitation of undigested food eaten hours earlier, and coughing over the last 6 months. She was hospitalized 1 month ago for aspiration pneumonia and successfully treated with antibiotics. Examination reveals a thin-appearing woman with normal vital signs and unremarkable chest, heart, and abdominal examination. A UGI contrast study is performed and reveals a pharyngoesophageal (Zenker’s) diverticulum. Which of the following is the most important aspect of treatment?
Cricopharyngeal muscle myotomy
Diverticulopexy
Elevation of the head of the bed
H2 blockers
Resection of the diverticulum
A 49-year-old woman presents to her physician’s office with a long-standing history of polydipsia, polyuria, central obesity, and hyperlipidemia. She is currently taking metformin, a sulfonylurea, and an angiotensin-converting enzyme (ACE) inhibitor. ACE inhibitors are most beneficial in preventing or slowing the progression of which of the following diabetic complication?
Diabetic nephropathy
Peripheral vascular disease
Diabetic retinopathy
Diabetic neuropathy
Diabetic ketoacidosis
A 49-year-old woman undergoes surgical resection of a malignancy. The family asks about the prognosis. The histopathology is available for review. For which of the following malignancies does histologic grade best correlate with prognosis?
Melanoma
Soft tissue sarcoma
Hepatocellular carcinoma
Colonic adenocarcinoma
Lung cancer
A 5-month-old child regularly regurgitates a large portion of her feeds. A pH probe study showed significant periods of low esophageal pH. The child has normal growth and no other significant past medical history. Which of the following is the best management at this point?
Esophageal manometry
Surgical correction with fundoplication
Close observation only
Barium swallow and upper GI series
Oral reflux medications
A 5-week-old infant presents with a 1-week history of progressive nonbilious emesis, associated with a 24-hour history of decreased urine output. The infant continues to be active and eager to feed. On examination, the infant has a sunken fontanelle and decreased skin turgor. The abdomen is scaphoid, and with a test feed, there is a visible peristaltic wave in the epigastrium. Which of the following is the most appropriate next step in management of this infant?
IV fluid resuscitation, followed by surgical intervention
Change the infant’s formula and feeding regimen
Immediate surgical exploration
Initiate therapy with a prokinetic agent
Send the child home with an oral electrolyte rehydration solution
A 5-year-old African-American boy is brought to the office by his mother due to a painful right knee, fever and chills over the last 2 days. The child was diagnosed with pharyngitis 2 weeks ago, and was treated with a 10-day course of penicillin G. His temperature is 38.8 C (102F) and pulse rate is 102/min. On examination, his right knee joint is swollen and erythematous, with a decreased range of motion. The laboratory findings are significant for leukocytosis and an elevated ESR. X-rays of both the right hip and knee joints are normal. What is the most appropriate treatment for the patient's condition?
Right knee arthrocentesis & intravenous nafcillin
Repeat a ten-day course of penicillin G
Bed rest with the right knee joint in a position of comfort
Bed rest & a ten-day course of penicillin G
Bed rest & aspirin
A 5-year-old boy is brought to an emergency room because of a painful, swollen knee joint. The boy had fallen while playing, and the joint had subsequently begun to swell. The mother reports that the boy was known to have hemophilia B. Replacement of which of the following is indicated?
Factor C
Factor VII
Factor VIII
Factor IX
Factor S
A 5-year-old boy is brought to his pediatrician's office after he falls from his bicycle and strikes his head against the sidewalk. There were no witnesses to this incident, which occurred 8 hours ago. The child is otherwise healthy, up-to-date on his immunizations, and not taking any medications. On physical examination, his vital signs are stable. He has a 5 × 4 cm abrasion on his forehead. He is alert and oriented to date, place and self. His motor and sensory examinations are normal and reflexes are normal. Which of the following constitutes reasonable management?
Obtain a skull x-ray film, observe for 24 hours and discharge
Obtain a head computerized tomography scan
Admit overnight for observation
Obtain a skull x-ray film and discharge if normal
Instruct parents to observe neurological status for 24 hours
A 5-year-old boy is brought to the office by his frustrated mother because, "he just can't seem to concentrate!" He has episodes that are characterized by frequent blinking and indifference to his surroundings. He does not remember anything after an episode. An episode does not last long, but he usually has 50-80 "daydreaming accidents" daily. His school performance has deteriorated lately, and his teacher has complained about his decreased concentration. Which of the following is the drug of choice for this patient's condition?
Phenytoin
Ethosuximide
Phenobarbital
Lamotrigine
Carbamazepine
A 5-year-old boy is brought to the physician for evaluation of left hip pain after his parents saw him limping this morning. He spent time on the playground yesterday but his parents do not think he was injured then. The boy complains that the pain in his hip worsens when he moves or walks. For the past 3 days, he has had a runny nose and congestion. Review of systems is otherwise negative. His grandmother has rheumatoid arthritis treated with methotrexate. His temperature is 37.2° C (99° F), blood pressure is 100/65 mm Hg, pulse is 92/min, and respirations are 18/min. Physical examination shows a well-appearing child with clear rhinorrhea and intermittent dry cough. Lungs are clear to auscultation bilaterally. His left hip is slightly abducted and externally rotated with mildly decreased range of motion. He is able to stand and bear weight. The remainder of his examination is normal. X-rays of both hips are normal. His laboratory results are as follows: Complete blood count: Hemoglobin 12.5 g/dL, Platelets 287,000/mm3, Leukocyte count 8,500/mm3, Neutrophils 30%, Eosinophils 1%, Lymphocytes 64%, Monocytes 5%, Erythrocyte sedimentation rate 30 mm/h, C-reactive protein 9 mg/L (N: ≤ 8 mg/L). Which of the following is the best next step in management of this patient?
Serum antinuclear antibodies
Synovial fluid aspiration of the left hip
Magnetic resonance imaging of the left hip
Ibuprofen, rest, and follow-up in 1 week
Intravenous antibiotics
A 5-year-old boy is brought to the physician's office because of a cough. He has episodes of successive and rapid coughs, which seems like he is choking, followed by a deep and loud inspiratory sound. He has vomited a few times after these bursts of cough. His symptoms have been progressively worsening for the past week, and were preceded by congestion, serous rhinorrhea and sneezing. His past medical history is insignificant. His vital signs are stable. Lung auscultation is unremarkable. Which of the following is the most appropriate pharmacotherapy for this patient?
Erythromycin
Cephalexin
Treatment is ineffective at this stage
Ampicillin
Rifampin
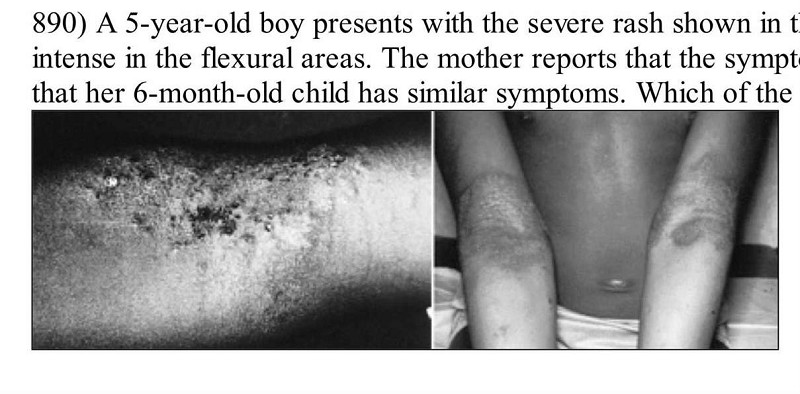
A 5-year-old boy presents with the severe rash shown in the photographs. The rash is pruritic, and it is especially intense in the flexural areas. The mother reports that the symptoms began in infancy (when it also involved the face) and that her 6-month-old child has similar symptoms. Which of the following is the most appropriate treatment of this condition?
Coal-tar soaps and shampoo
Topical antibiotics
Moisturizers and topical steroids
Ultraviolet light therapy
Topical antifungal cream
A 5-year-old boy suddenly begins coughing while eating peanuts. He is choking and gagging. When he is brought to the emergency department, but he is awake and is able to give his name. On physical examination, his vital signs are stable. On examination of the chest, inspiratory stridor and intercostal and suprasternal retractions are apparent. Which of the following is the most appropriate initial step in management?
Perform emergency tracheostomy and take to surgery
Position patient and perform back blows
Clear oropharynx with multiple blind sweeps with finger
Allow patient to clear foreign object by spontaneous coughing
Stand behind patient and perform abdominal thrusts
A 5-year-old child presents with a small mass near the anterior border of the sternocleidomastoid muscle. The mass is associated with localized erythema and induration, and the child is febrile. Which of the following is the definitive treatment of this problem?
Immediate excision followed by postoperative antibiotic therapy for 1 week
Partial excision followed by clinical observation
Incision and drainage followed by complete excision after resolution of the inflammation and infection
Antibiotic therapy
Incision and drainage
A 5-year-old child was hit in the right eye by a toy. He is rubbing at his eye, which is watering profusely. There is a small abrasion at the corner of the eye. He is mildly photophobic, but his pupils are equal, symmetric, and reactive to light and accommodation. His vision is normal. Which of the following is the most appropriate next step in the management of this patient?
Apply a patch to the eye and follow-up in a week
Discharge him to home with antibiotic eye ointment
Refer him immediately to an ophthalmologist
Perform a fluorescein dye stain of the cornea to determine if there is a corneal abrasion
Irrigate the eye with sterile normal saline
A 5-year-old girl is brought to medical attention by her parents 12 hours after the onset of generalized tonicoclonic seizures. She never had similar episodes in the past. The girl is otherwise healthy. Her temperature is 37 C (98.6 F). Physical examination is unremarkable. There is no evidence that the girl had a fever at the onset of the convulsive episode. The parents fear that seizures may damage the child's brain and may eventually recur. Which of the following is the most appropriate next step in management?
Perform CT/MW studies of the brain
Start antiepileptic medication
Admit patient to the hospital for further evaluation
Perform electroencephalographic studies
Provide reassurance to child and family
A 5-year-old girl is diagnosed with Bordetella pertussis infection after an outbreak in the day-care center. She is prescribed erythromycin for 14 days. She lives with her parents and 13-year-old sister whose immunizations are up to date. What is the most appropriate way to limit the risk of infection in household contacts?
Keep the child hospitalized until symptoms disappear
Administer pertussis immunization to the parents only
Prescribe erythromycin for 14 day to the mother and father only
Prescribe erythromycin for 14 days to all household contacts
Administer pertussis immunization to all household contacts
A 5-year-old girl without past history of UTI is in the hospital on antibiotics for Escherichia coli pyelonephritis. She is still febrile after 4 days of appropriate antibiotics. A renal ultrasound revealed no abscess, but a focal enlargement of one of the lobes of the right kidney. CT of the abdomen reveals a wedge shaped area in the right kidney distinct from the normal tissue with minimal contrast enhancement. Appropriate management of this patient includes which of the following interventions?
Surgical consultation
Renal biopsy
Dimercaptosuccinic acid (DMSA) scan
Routine treatment with 10 to 14 days of antibiotics for pyelonephritis
Prolonged antibiotic therapy
A 5-year-old Hispanic girl is brought to the emergency department (ED) due to a cat bite on her right upper extremity. She was bitten after rambunctiously playing for several minutes with the cat, which had just been given to her as a birthday gift. Her most recent booster tetanus vaccine was one year ago. Her temperature is 36.7°C (98°F), blood pressure is 108/70 mm Hg, pulse is 107/min, and respirations are 21/min. Physical examination reveals a deep puncture wound on the volar aspect of her right forearm. Before going to the ED, her mother cleaned the wound with hydrogen peroxide. There is no visible debris in the wound, and little bleeding is evident. Neurovascular fun
Bandage with dry gauze and discharge home
Prescribe levofloxacin
Prescribe erythromycin
Prescribe amoxicillin/clavulanate
Prescribe amoxicillin
A 5-year-old Mexican female child is brought to the office for the evaluation of a pruritic vulva for the past fifteen days. The pruritus is felt mostly during the night. Her 4-year-old cousin who visited them four weeks ago has a similar complaint. On examination, there is no vaginal discharge, but the vulva is erythematous. The rest of the physical examination is normal. What is the most appropriate next step in the management of this patient?
Do stool examination for parasites
Do wet mount of vaginal fluid
Do vaginal fluid gram stain
Detain the child with the suspicion of sexual abuse
Do a scotch tape test
A 50-year-old Caucasian male comes to the office for the evaluation of polyuria and polydypsia for the last two months. He also complains of weakness and fatigue. He had one episode of transient proximal muscle weakness which lasted 30 minutes. He has a 20-pack year history of smoking. He does not drink alcohol. His past medical and family histories are insignificant. His pulse is 78/min, blood pressure is 150/96 mmHg and temperature is 36.7°C (98°F). The rest of the examination, including the neurological examination, is normal. Labs show: Plasma sodium 150 mEq/L, Potassium 2.6 mEq/L, Serum creatinine 0.8 mg/dL. Which of the following is the most appropriate next step in the management of this patient?
Aldosterone suppression testing
Adrenal vein sampling
Imaging of adrenals by CT scan
Measurement of 24 hour urinary potassium excretion
Measurement of plasma renin activity and aldosterone concentration
A 50-year-old Caucasian male returns to the clinic for the evaluation of his blood pressure control. He was diagnosed with essential hypertension one year ago. He claims compliance with his reduced salt intake diet. He is currently on a thiazide diuretic and a beta-blocker. His past medical history is significant for angina, which is always relieved with sublingual nitroglycerine, but he has not had an attack of angina in over a month. He has never had a myocardial infarction. He lives with his wife and two children. He quit smoking two years ago, but previously had a 25-pack year history. He drinks 4 bottles of wine per week. His blood pressure is 150/90 mm Hg. What is the best next step in management?
Reassurance and repeat measurement in 2 weeks
Increase the dose of thiazide diuretic
Reduction in alcohol intake
Admit him to the hospital to control his blood pressure
Start an ACE inhibitor
A 50-year-old diabetic woman presents for follow-up of her hypertension. Her blood pressure is 152/96 in the office today and she brings in readings from home that are consistently in the same range over the past month. Her current medications are amlodipine 5 mg daily and hydrochlorothiazide 25 mg daily. The diuretic was added when she developed peripheral edema on the amlodipine; now she has only trace peripheral edema. A spot urine specimen shows 280 µg of albumin per mg creatinine (microalbuminuria is present if this value is between 30 and 300 µg/mg). What would be the best next therapeutic step in this patient?
Add angiotensin-converting enzyme inhibitor or angiotensin receptor blocker
Add clonidine
Add an alpha-blocker
Increase the thiazide diuretic dose
Add a beta-blocker
A 50-year-old female comes into your office complaining of four-month history of dry cough. She denies dyspnea or hemoptysis. Past medical history is significant for hypertension, diabetes, and gout. Her current medications include enalapril, metformin, hydrochlorothia zide, and allopurinol. She does not smoke or consume alcohol. Her vital signs are BP 130/80 mmHg, HR 80/min, T 36.7°C (98°F) and RR 16/min. Physical examination is within normal limits. The best next step in the management of this patient is:
Chest radiograph
Bronchoscopy
Barium esophagography
Pulmonary function testing
Reevaluation of drug therapy
A 50-year-old female is 5 ft 7 in tall and weighs 185 lb. There is a family history of diabetes mellitus. Fasting blood glucose (FBG) is 160 mg/dL and 155 mg/dL on two occasions. HgA1c is 7.8%. You educate the patient on medical nutrition therapy. She returns for reevaluation in 8 weeks. She states she has followed diet and exercise recommendations but her FBG remains between 130 and 140 and HgA1C is 7.3%. She is asymptomatic, and physical examination shows no abnormalities. Which of the following is the treatment of choice?
Observation with repeat HgA1C in 6 weeks
Encourage compliance with medical nutrition therapy
Insulin
Thiazolidinediones
Metformin

A 50-year-old male comes to the office due to an ulcer in his right foot. He has type 2 diabetes, for which he takes glyburide. Laboratory investigations reveal an HbA1c of 9%, and random blood sugar of 180 mg/dL. X-ray of the leg/foot is normal. A picture of the foot ulcer is shown below. Which of the following is the most appropriate management of this patient's foot ulcer?
Prescribe oral antibiotics and follow-up as an outpatient
Amputation
Perform thorough debridement of the wound
Prescribe tight-fitting shoes
Start aspirin and atorvastatin
A 50-year-old male patient comes to the office because he is concerned about the marked tremors of his hands. His tremors disappear with voluntary activity and worsen with emotional stress. He finds it mild difficult to initiate movements. He does not have a family history of tremors. Physical examination reveals tremors that occur at a frequency of 3-4 cycles/sec. There is rigidity of his limb musculature. His gait and posture is minimally disturbed. His higher mental fun
Benztropine
Selegiline
Clozapine
Propranolol
Amantadine
A 50-year-old man comes to the emergency department due to a sudden onset of severe, colicky pain in the right flank. He was admitted twice in the past for similar complaints; he was managed conservatively and sent home on both occasions. He has no other medical problems. He does not use tobacco, alcohol or drugs. His vital signs are stable. He is given IV fluids and narcotics. Laboratory studies show: Hb 14.5 g/dL, WBC 13,000/cmm; no bands, Platelets 300,000/cmm, BUN 16 mg/dl, Serum Creatinine 0.8 mg/dl. CT scan of the abdomen without contrast shows renal calculi. Which of the following is the best advice for the prevention of future stones in this patient?
Decrease dietary protein and oxalate
Increase sodium intake
Restrict fluid intake
Decrease dietary calcium intake
Mega doses of Vitamin C
A 50-year-old man comes to the emergency department due to acute onset respiratory difficulty. He also has periorbital, circumoral and facial edema. Two weeks ago, he experienced chest pain, profuse sweating and anxiety, and was subsequently admitted to the cardiac intensive care unit. At that time, his ECG showed ST segment elevation and Q waves in the inferior leads. He was taken to the catheterization lab and had an angioplasty with stent done for 100% occlusion of the right coronary artery. He was discharged with the following medications: aspirin, clopidogrel, metoprolol, enalapril, simvastatin and isosorbide mononitrate. In the ED, his pulse is 102/min, blood pressure is 110/70 mmHg, respirations are 24/min and temperature is 36.8°C (98.4°F). Which of the following is most likely responsible for his present symptoms?
Enalapril
Metoprolol
Lsosorbide
Clopidogrel
Aspirin
A 50-year-old man complains of loss of libido and impotence after starting treatment with leuprolide for prostatic hyperplasia. An alpha-blocker and finasteride have also been tried, but with similar adverse effects. So far, the patient has not experienced any episodes of urinary tract infection or hematuria, but he is excessively bothered by his symptoms without any medication. Digital rectal examination shows mild prostatic enlargement. At this time, his prostate-specific antigen (PSA) is 4.5 ng/mL, and his creatinine is 0.7 mg/dL. Dipstick examination shows no hematuria. Which of the following is the most appropriate alternative to his current pharmacologic treatment?
Transurethral resection of the prostate (TURP)
Open prostatectomy
Transurethral incision of the prostate (TUIP)
Watchful waiting
Megestrol acetate
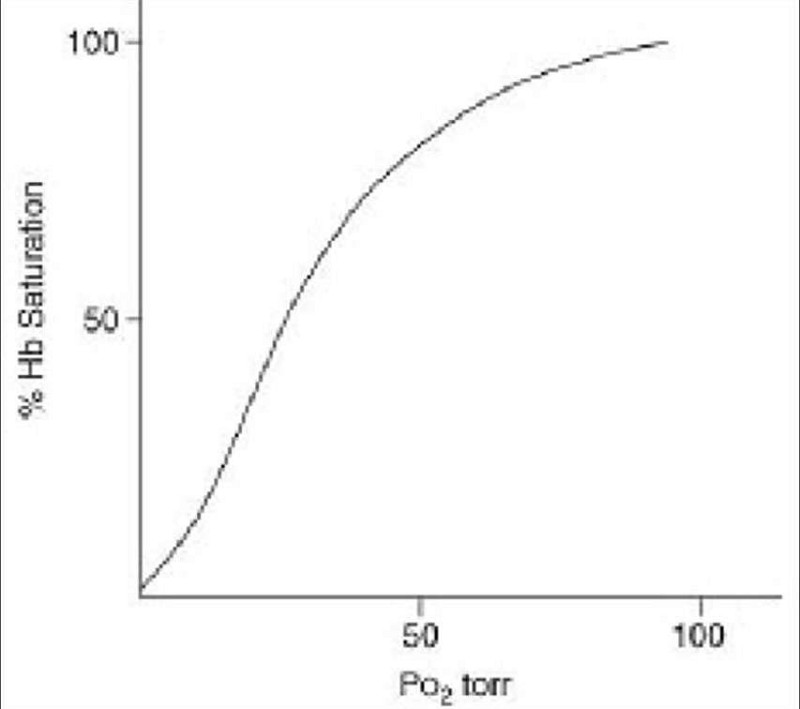
A 50-year-old man has respiratory failure due to pneumonia and sepsis after undergoing splenectomy for a traumatic injury. Which of the following management strategies will improve tissue oxygen uptake (ie, shifting the oxygen dissociation curve, depicted here, to the right)?
Transfusion of banked blood to correct acute anemia
Administration of an antipyretic to lower the patient’s temperature
Hypoventilation to increase the PaCO2
Administration of bicarbonate to promote metabolic alkalosis
Correction of acute anemia with erythropoietic stimulating agent
A 50-year-old man is admitted to the hospital with a UGI bleed from acute erosive gastritis, secondary to chronic nonsteroidal anti-inflammatory use. His hematocrit is 28%. With fluid resuscitation, his blood pressure normalizes, but he has a persistent hyperdynamic precordium, tachycardia, and flow murmur on auscultation. He complains of shortness of breath on ambulation. An ECG shows depressed ST-T segments. Which of the following is the next appropriate step in management?
Initiation of a calcium channel blocker
Blood transfusion
Initiation of iron supplementation therapy
Continued IV fluid resuscitation
Supplemental oxygen
A 50-year-old man is incidentally discovered to have a low-grade mucosa-associated lymphoid tissue (MALT) lymphoma on biopsy of the stomach during esophagogastroduodenoscopy for dyspepsia. CT scans of the chest, abdomen, and pelvis demonstrate no evidence of enlarged regional lymph nodes or distant metastases. Which of the following is the initial treatment of choice?
Chemotherapy
Steroids
Antibiotics
Total gastrectomy with esophagojejunostomy and adjuvant chemotherapy
Total gastrectomy with esophagojejunostomy
A 50-year-old postman presents with a six-month history of left calf pain that is brought on by walking and is relieved by rest. The patient reports no other symptoms. He has smoked cigarettes for the past 25 years, but does not drink alcohol or use illicit drugs. On physical examination, he has a blood pressure of 158/92 mm Hg and a pulse of 88 beats per minute. The heart and lung examinations are normal. A bruit is heard over the left femoral artery. Popliteal, dorsalis pedis and posterior tibial pulses are palpable bilaterally. The electrocardiogram shows normal sinus rhythm and Q-waves in II, Ill, and aVF. Which of the following is the best next step in management?
Duplex scan of arteries of lower limbs
Endovascular stent placement
Contrast arteriography
Ankle-brachial pressure index measurement
Reassurance
A 50-year-old woman complains of headaches and lateralizing weakness. A CT scan of the brain reveals an irregular mass in the right cerebral hemisphere. A biopsy documents that this is a glioblastoma. Which of the following is the best treatment strategy for potential cure?
Combined surgical resection, external beam radiation, and chemotherapy with temozolomide
External beam radiation alone
Surgical resection alone
Combination chemotherapy with carmustin, cisplatin, and temozolomide
Chemotherapy with temozolomide alone
A 50-year-old woman presents to your office complaining of severe insomnia, hot flashes, and mood swings. She also states that her mother had a hip fracture at 65 years of age. She is afraid of developing osteoporosis and having a similar incident. Her last menstrual period was six months ago. Her past medical history is significant for hypothyroidism diagnosed seven years ago. She takes L-thyroxine and the dose of the hormone has been stable for the last several years. Her blood pressure is 120/70 mmHg and her heart rate is 75/min. Serum TSH level is normal. You consider estrogen replacement therapy for this patient. Which of the following is most likely concerning estrogen replacement therapy in this patient?
The level of TSH would decrease
The volume of distribution of thyroxine would decrease
The requirement for L-thyroxine would increase
The metabolism of thyroid hormones would decrease
The level of total thyroid hormones would decrease
A 51-year-old man presenting to the clinic for routine examination mentions that he has not been able to get over the flu. Further questioning clarifies that he has had a nonproductive cough for the past 3–4 months and is unable to sustain his normal walking pace for prolonged periods. He reports feeling more fatigued than he recalls feeling last year. His medical history is significant for hypertension, alcoholism, and obesity. His blood pressure is well controlled on losartan and hydrochlorothiazide. He has no known drug allergies. His mother died of complications of type 2 diabetes mellitus. His father had a fatal myocardial infarction at age 56 years. The patient smokes half a pack of cigarettes per day and has done so for the past 7 years. He has worked all his adult life as an accountant and has no known exposures to asbestos or organic dusts. His blood pressure is 134/96 mm Hg, heart rate is 78/min, respiratory rate is 16/min, temperature is 37°C (98.6°F), and oxygen saturation is 94% on room air. Lung examination reveals bilateral inspiratory crackles in the lung bases. High-resolution CT shows patchy areas of ground glass, reticular abnormalities, and traction bronchiectasis. Laboratory findings are normal except for an elevated erythrocyte sedimentation rate of 54 mm/hr. What is the recommended treatment for this patient’s cough?
Prescribe glucocorticoids
Resect diseased lung fields
Prescribe bronchodilators and long-term domiciliary oxygen therapy
Change the antihypertensive agent
Prescribe amantadine
A 51-year-old man presents with a 2-cm left thyroid nodule. Thyroid scan shows a cold lesion. FNA cytology demonstrates follicular cells. Which of the following is the most appropriate initial treatment of this patient?
Prophylactic neck dissection is indicated along with a total thyroidectomy
Thyroid lobectomy
TSH suppression by thyroid hormone
External beam radiation to the neck
Multidrug chemotherapy
A 51-year-old woman G3P3 presents to your office with a 6-month history of amenorrhea. She complains of debilitating hot flushes that awaken her at night; she wakes up the next day feeling exhausted and irritable. She tells you she has tried herbal supplements for her hot flushes, but nothing has worked. She is interested in beginning hormone replacement therapy (HRT), but is hesitant to do so because of its possible risks and side effects. The patient is very healthy. She denies any medical problems and is not taking any medication except calcium supplements. She has a family history of osteoporosis. Her height is 5 ft 5 in and her weight is 115 lb. In counseling the patient regarding the risks and benefits of hormone replacement therapy, you should tell her that HRT (estrogen and progesterone) has been associated with which of the following?
An increased risk of developing Alzheimer disease
An increased risk of malignant melanoma
An increased risk of thromboembolic events
An increased risk of colon cancer
An increased risk of uterine cancer
A 51-year-old woman presents to the ED after 5 consecutive days of crushing substernal chest pressure that woke her up from sleep in the morning. The pain resolves spontaneously after 20 to 30 minutes. She is an avid rock climber and jogs 5 miles daily. She has never smoked cigarettes and has no family history of coronary disease. In the ED, she experiences another episode of chest pain. An ECG reveals ST-segment elevations and cardiac biomarkers are negative. The pain is relieved with sublingual nitroglycerin. She is admitted to the hospital and diagnostic testing reveals minimal coronary atherosclerotic disease. Which of the following is the most appropriate medication to treat this patient’s condition?
Aspirin
H2-Blocker
Antidepressant
β-Blocker
Calcium channel blocker (CCB)
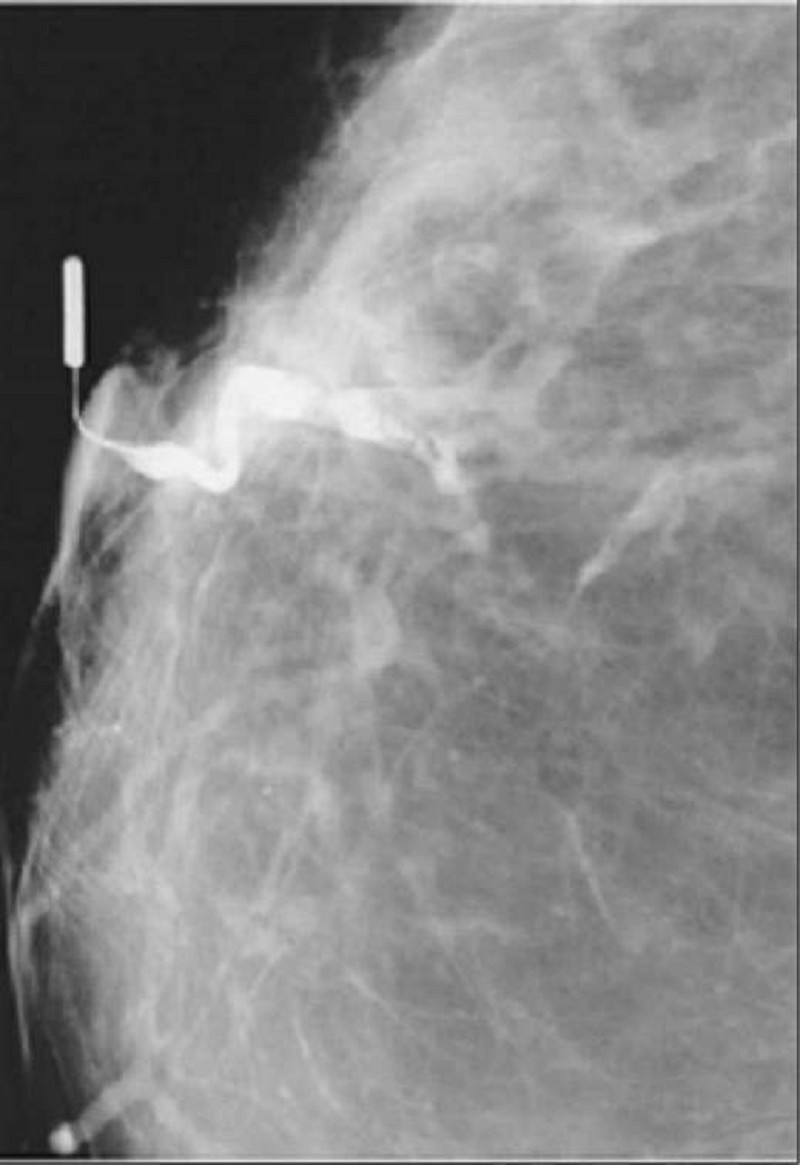
A 51-year-old woman presents to the physician’s office with a 2-month history of a right breast blood tinged nipple discharge. Past history is unremarkable. Family history is positive for postmenopausal breast cancer in a maternal grandmother. Examination reveals no palpable masses or regional adenopathy, but a serous discharge is easily elicited from a single duct in the right breast. Bilateral mammograms show no abnormalities. Cytology from the discharge was not diagnostic. A ductogram was ordered, and the results are shown in picture. Which of the following is the most appropriate next step in management?
Terminal duct excision (microdochectomy)
Central lumpectomy (including removal of the nipple/areolar complex)
Modified radical mastectomy
Observation, with repeat examination and imaging studies in 3–6 months
Collection of discharge for repeat cytologic analysis
A 52-year-old Caucasian male comes to the office for the evaluation of tremors. He has been having tremors in both hands and head over the past several months. He does not experience any tremors at rest, or any problem with his legs. He has a history of alcohol abuse. He is currently not on any medication. His father had essential tremors, and his paternal uncle has Parkinsonism. The physical examination reveals tremors, which increase in amplitude when he tries to reach for an object. Which of the following is the most appropriate next step in the management of this patient?
Benztropine
Haloperidol
Valproic acid
Clonazepam
Propranolol
A 52-year-old man complains of frequent chest pain. The pain typically occurs at night and is described as retrosternal and burning in quality. He leads a sedentary lifestyle but does not smoke or drink alcohol. His past medical history includes a chronic cough and occasional hoarseness. He does not take any medications. His BMI is 28.5 kg/m2 ECG stress testing reveals 1 mm ST segment depression in the inferior leads at 90% of predicted maximal heart rate. He did not experience chest pain during the stress test. Which of the following is most likely to relieve this patient's chest pain?
Ibuprofen
Propranolol
Alprazolam
Omeprazole
Nitroglycerin
A 52-year-old man develops sudden-onset shortness of breath on postoperative day 4 after a hemicolectomy for colon cancer. His surgery went well with no operative complications. He reports no cough, sputum, or pleuritic chest pain. His blood pressure is 155/90 mm Hg, pulse 100/min, temperature 37.8°C, lungs are clear, and heart sounds normal. He has bilateral pedal edema, but no discomfort in his legs. His CXR and ECG are normal. A chest CT with contrast reveals a thrombus in his right upper lobe artery. Which of the following statements concerning the management of this condition is most likely correct?
Urgent inferior vena cava (IVC)
Urgent thrombolytic therapy is indicated
Continuous IV heparin or subcutaneous low-molecular-weight heparin (LMWH) therapy is indicated
Confirmation of the diagnosis with bilateral ultrasound leg Dopplers
Filter insertion is indicated
A 52-year-old man is pinned against a loading dock. The patient has a fractured femur, a pelvic fracture, a tender abdomen, and no pulses in the right foot with minimal tissue damage to the right leg. Angiography discloses a popliteal artery injury with obstruction. At surgery, the popliteal vein is also transected. His blood pressure is 85/60 mm Hg. Which of the following is the best management strategy for his vascular injuries?
Amputation of the right lower extremity above the knee
Repair of the popliteal vein with a synthetic interposition graft
Ligation of the popliteal vein
Repair of the popliteal vein with saphenous vein patch
Repair of the popliteal vein with simple closure
A 52-year-old man presents to his primary care physician’s office for routine care. He has hypertension, hypercholesterolemia, and type 2 diabetes mellitus, and has smoked one pack of cigarettes per day for the past 30 years. Medications include hydrochlorothiazide, atorvastatin, and glipizide. There is a family history of myocardial infarction in the maternal grandfather at age 60. The patient has undergone screening for colon and prostate cancer. Physical examination reveals a pleasant, obese man who is 175 cm (5′9″) tall and weighs 108 kg (238 lb). His blood pressure is 155/81 mmHg, heart rate is 78/min, respiratory rate is 14/min, and temperature is 36.8°C (98.3°F). What one action would most reduce the patient’s stroke risk?
Blood pressure reduction
Smoking cessation
Weight loss
Serum cholesterol reduction
Blood glucose reduction
A 52-year-old man with Burkitt lymphoma is admitted to the hospital for chemotherapy. He is started on chemotherapy without incident. Two days into his hospitalization, he develops new peaked T-waves on his ECG. Laboratory analysis reveals a serum potassium concentration of 6.2 mEq/L, and the patient is given one ampule of calcium gluconate emergently. His renal fun
Hemodialysis
High-dose inhaled β2 agonist
Insulin and glucose
Furosemide
Sodium polystyrene sulfonate
A 52-year-old man with gastric outlet obstruction secondary to a duodenal ulcer presents with hypochloremic, hypokalemic metabolic alkalosis. Which of the following is the most appropriate therapy for this patient?
Intubation and controlled hypoventilation on a volume-cycled ventilator to further increase PCO2
Administration of acetazolamide to promote renal excretion of bicarbonate
Clamping the nasogastric tube to prevent further acid losses
Infusion of isotonic (0.15 N) HCl via a central venous catheter
Infusion of 0.9% NaCl with supplemental KCl until clinical signs of volume depletion are eliminated
A 52-year-old nurse seeks medical retirement because of a "heart condition." She complains of disabling attacks of tachycardia and palpitations. The physical examination and ECG studies confirm that indeed her pulse is between 100 and 105/min at all times, and she is in and out of atrial fibrillation. It is also noted that she is fidgety and constantly moving, and various examiners remark that she arrives for tests lightly dressed when it is rather cold outside. Thyroid fun
Fine needle aspiration cytology of the thyroid gland
Serum levels of C peptide
MRI of the pituitary area
Serum levels of tri-iodo-thyronine (T3)
Radioactive iodine uptake
{"name":"DES C_Management (8) Prepared : CHILLY", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 45-year-old man is brought to the emergency department after being involved in a motor vehicle collision. He is conscious but in severe pain. His blood pressure is 90\/60 mm Hg, pulse is 100\/min and respirations are 17\/min. Physical examination shows marked swelling and some bruising over the right thigh; the skin is intact. An x-ray film of the leg shows a fracture of the mid shaft of the femur. After hemodynamically stabilizing the patient, which of the following is the most appropriate next step in management?","img":"https://cdn.poll-maker.com/20-806587/image.jpeg?sz=1200"}
More Quizzes
Qual è la tua disciplina ideale di atletica?
630
Quanto bene conosci marco?
1169
How many People want Freedom of Choice with Vaccinations in Australia?
100
The division of labour within the family
740
Take the Fundamentals of Nursing: Test Your Skills Now!
201042275
Ultimate Donald Duck: Name His Girlfriend & More
201040122
Polygons & Quadrilaterals: Ace Your Unit 8 Test!
201055752
Childcare Safety Regulations: Test Your Knowledge
201026479
Free Employee Cybersecurity Awareness
201022061
Define: Challenge Your Vocabulary & Definitions
201048494
Free Biology EOC Study Guide & Practice
201026997
Free Topic 3 & 2 Assessment
201021748