DES C_Management (11) Prepared : CHILLY
A 65-year-old female is admitted to the hospital with increasing shortness of breath, weight gain and lower extremity edema. She has a history of hypertension, nonischemic cardiomyopathy with an ejection fraction of 30%, and hyperlipidemia. Her home medications include oral aspirin, digoxin, furosemide, metoprolol, lisinopril and atorvastatin. She is started on intravenous furosemide. On day three of hospitalization telemetry reveals six beats of wide complex ventricular tachycardia. Physical examination now shows decreased leg edema and clear lungs. Which of the following is the most appropriate next step in the management of this patient's tachycardia?
Add metolazone
Discontinue metoprolol
Discontinue atorvastatin
Measure serum electrolytes
Add spironolactone
A 65-year-old G2P2 postmenopausal woman presents to a gynecologist for the first time in many years complaining of vaginal bleeding, pelvic pain, and increased urinary frequency. She reports she is sexually active with her husband. After an appropriate work-up, a diagnosis of locally invasive squamous cell carcinoma of the cervix is made. The tumor has extended approximately 9 mm into the cervical stroma, grading the cancer as stage IB. The patient is informed of the diagnosis and wishes to undergo definitive therapy. What is the definitive therapy for this patient’s disease?
Loop electrosurgical excision procedure
Uterine artery embolization
Radical hysterectomy
Chemotherapy
Cold knife cone excision
A 65-year-old Hispanic male is brought to the emergency department after having one seizure episode. His past medical history is significant for non-small cell lung carcinoma, which was diagnosed two years ago and treated surgically. He had no residual disease at that time. CT scan of the brain with contrast now shows a solitary cortical mass in the right hemisphere of the brain at the grey-white matter junction. His chest x-ray is clear. He is admitted for further management and started on phenytoin. Which of the following is the most appropriate management for this patient?
Palliative pain therapy and seizure prophylaxis
Whole brain radiation
Combination chemotherapy
Surgical resection of the mass
Focal radiation to brain mass
A 65-year-old lady comes to the office for the evaluation of her deteriorating memory. She has become increasingly forgetful over the last several months, and now appears very concerned about her memory loss. She used to pride herself for her sharp memory, but has been forgetting the most trivial things and has become "extremely inefficient." She also complains of easy fatigability, poor appetite, and frequent awakening at night. She feels worthless and has lost interest in her favorite hobby, which is gardening. On coughing or laughing, she loses urine involuntarily, and this is adding to her misery. She lives with her husband, who says that she has become very "cranky and irritable" lately. Her medical history is significant for hypercholesterolemia, for which she refuses to take medication. She is presently not on any hormonal therapy. The physical examination is completely normal. Laboratory studies are unremarkable. CT scan of the head is normal. What is the best next step in the management of this patient?
Start selective serotonin reuptake inhibitor
Reassurance
Surgical bypass shunting
Start hormonal replacement therapy
Treat her with donepezil
A 65-year-old male comes to the emergency department because of a sudden, painless loss of vision in his right eye that occured a half an hour ago. Five hours ago, he experienced a similar but transient loss of vision in the same eye, which lasted for five minutes. He has hypertension, diabetes, hypercholesterolemia, and peripheral vascular disease. He had an anterior wall myocardial infarction six years ago. His medications include glyburide, captopril, atenolol, simvastatin and aspirin. His temperature is 36.7°C (98.0°F), respirations are 16/min, pulse is 88/min, and blood pressure is 146/88 mmHg. Examination of the right eye reveals visual acuity of 20/60 and subtle retinal whitening. A right carotid bruit is heard. Which of the following is the most appropriate next step in the management of this patient?
Ocular massage and high flow oxygen
Acetazolamide IV
Administer thrombolytics
Administer systemic steroids
Instillation of topical beta blocker
A 65-year-old male comes to the office and complains of nausea and early satiety for the past several months. His other complaints are anorexia and abdominal bloating. He denies any heartburn or epigastric pain. He has diabetes, and has been taking insulin for the last fifteen 15 years. His blood glucose readings using the home blood glucose monitor range between 40 to 400 mg/dL. Most of the low blood glucose readings occur after meals. Which of the following is the most appropriate management of this patient's symptoms?
Promethazine
Metoclopramide
Ranitidine
Ondansetron
Ibuprofen
A 65-year-old male complains of fatigue for the past one month. He has been living alone since the death of his wife one year ago. He does not like to cook, and his diet consists mostly of canned food, hot tea, and toast. He drinks one glass of white wine nightly with dinner. Examination shows pallor of the skin, nail beds and conjunctiva. Rectal exam is heme-negative. His physical examination is otherwise unremarkable. Administration of which of the following would be most helpful in treating his condition?
Vitamin B12
Vitamin C
Vitamin D
Vitamin E
Folic acid
A 65-year-old male presented to the ER with increasing shortness of breath, fever and productive cough of 2 days duration. He has smoked for several years and has been on home oxygen. Chest x-ray showed right lower lobe consolidation. His vital signs on admission were temperature 38.70 C (101.70 F), blood pressure 120/76 mm Hg, pulse 11 0/min and respirations 26/min. His condition worsened over the next several hours and required oro-tracheal intubation and mechanical ventilation. He was transferred to the intensive care unit. Placement of a central venous catheter in the right subclavian vein for IV access was attempted. After the line is successfully placed, the patient begins to deteriorate. Repeat vital signs are blood pressure 80/50 mm Hg and pulse 130/min. Examination shows absent breath sounds on the right side and distended neck veins. Which of the following is the most appropriate next step in management?
Pericardiocentesis
Intravenous fluids and dopamine
Needle thoracostomy
Stat chest x-ray
Arterial blood gas analysis
A 65-year-old male presents to the emergency department with substernal chest pain, severe shortness of breath, and diaphoresis that began suddenly 40 minutes ago. Since the pain started, the patient has vomited twice. The pain radiates to his left arm and does not remit with sublingual nitroglycerine. EKG shows 2 mm ST elevations in the anterior leads. On physical examination, the patient's temperature is 36.9°C (98.4°F), blood pressure is 110/70 mmHg, pulse is 60/min, respirations are 32/min, and oxygen saturation is 90% on 4L oxygen by nasal canula. Cardiac exam reveals a muffled S1 and S2 and the presence of an S3. Lung exam reveals basilar crackles that extend halfway up the lung fields bilaterally. Which of the following is the best next step in managing this patient?
Metoprolol
IV fluids
Spironolactone
Digoxin
Furosemide
A 65-year-old male with oxygen-dependent chronic obstructive pulmonary disease, chronic atrial fibrillation, and depression comes into the Emergency Room, with symptoms of increased dyspnea and worsening cough pattern. His recent history had been significant for a gradual worsening of his baseline lung disease over the past month, which had been treated by his outpatient doctor with increased frequency of inhaled beta-agonist and azithromycin. This morning he had a severe shortness of breath that was unresponsive to "stacked" home nebulizer treatments. The ER physician notes that the patient is in moderate severe respiratory distress. His temperature is 37.2°C (99°F), blood pressure is 150/90 mmHg, pulse is 110/min, and respirations are 28/min. Accessory muscle use was noted. Lung exam shows diffuse rhonchi and wheezing. A pulse oximetry revealed an oxygen saturation of 80% on room air. His chest x-ray showed no new infiltrates. His WBC count is 7,000/cmm with normal differential. The ER physician had given nebulization, and the patient is on 5-liters of oxygen. Which of the following should also be considered in this patient?
Gatifloxacin
Clarithromycin
Aminophylline
Methylprednisolone
N-acetylcysteine
A 65-year-old man complains of blood in his urine for the past 2 months. He has had no similar episodes in the past. He is otherwise healthy and denies abdominal pain, any trauma, fever, chills, anorexia, or dysuria. He reports having a good urinary stream and no nocturia or dribbling. He is not sexually active. He has no other medical problems and is not taking any medications. His vital signs are stable. Lung, heart, abdominal, and groin examination are unremarkable. Rectal exam reveals a nontender prostate with no masses or enlargement- Urinalysis reveals packed red cells, a few white cells, and no casts. Which of the following is the most appropriate management?
Schedule a prostatic biopsy
Schedule a pelvic CT scan
Schedule a cystoscopy
Schedule a renal angiogram
Prescribe levofloxacin
A 65-year-old man presents to the emergency department with sudden onset of pain and weakness of the left lower extremity of 2-hour duration. Past history reveals chronic atrial fibrillation following a myocardial infarction 12 months ago. On examination, he is found to have a cool, pale left lower extremity with decreased strength and absent popliteal and pedal pulses. The opposite leg has a normal appearance with palpable pulses. Following successful treatment for an embolus to the left femoral artery with no evidence of a reperfusion injury (anticoagulation with heparin and thromboembolecctomy), which of the following long-term treatments would most likely decrease the chance of recurrent embolus?
Placement of a vena cava filter
Exercise program
Aortofemoral bypass grafting
Coronary artery bypass grafting
Anticoagulation
A 65-year-old man presents to the emergency department with sudden onset of pain and weakness of the left lower extremity of 2-hour duration. Past history reveals chronic atrial fibrillation following a myocardial infarction 12 months ago. On examination, he is found to have a cool, pale left lower extremity with decreased strength and absent popliteal and pedal pulses. The opposite leg has a normal appearance with palpable pulses. Which of the following is the most appropriate first step in management of this patient?
Arteriography
Echocardiography
Anticoagulation with warfarin
Anticoagulation with heparin
Alkalinization of the urine with IV sodium bicarbonate
A 65-year-old man presents to the emergency department with sudden onset of pain and weakness of the left lower extremity of 2-hour duration. Past history reveals chronic atrial fibrillation following a myocardial infarction 12 months ago. On examination, he is found to have a cool, pale left lower extremity with decreased strength and absent popliteal and pedal pulses. The opposite leg has a normal appearance with palpable pulses. Which of the following is the treatment of choice for this patient?
Four-compartment fasciotomy
Anticoagulation and close observation
Thromboembolectomy
Administration of vasodilators
R-TPA (tissue plasminogen activator) infusion following anticoagulation
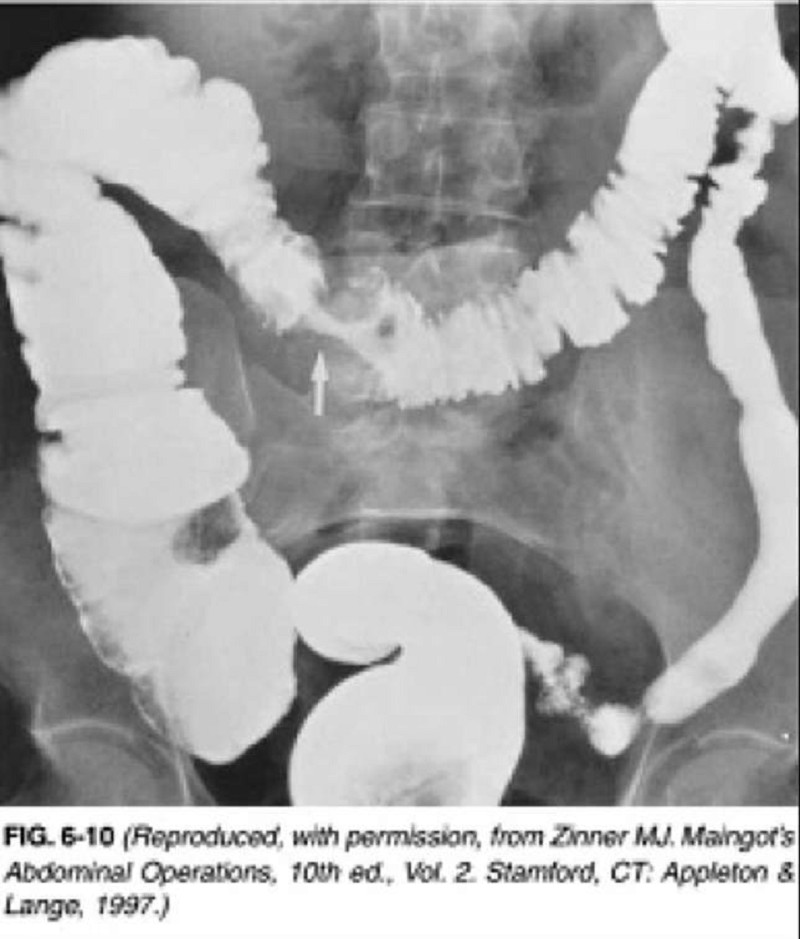
A 65-year-old man presents to the physician’s office for his yearly physical examination. His only complaint relates to early fatigue while playing golf. Past history is pertinent for mild hypertension. Examination is unremarkable except for trace hematest-positive stool. Blood tests are normal except for a hematocrit of 32. A UGI series is performed and is normal. A barium enema is performed, and one view is shown in Figure 6-10. Which of the following is the most appropriate therapy following colonoscopy?
Surgical resection and primary anastomosis
Surgical bypass (colocolostomy)
Proximal colostomy with mucous fistula
Radiation therapy
Chemotherapy
A 65-year-old man sustains a 50% TBSA burn while burning trash in the backyard. The patient is resuscitated with lactated Ringer (LR) solution using the Parkland formula and a weight of 80 kg. What is the rate of LR given in the first 8 hours?
100 mL/h
5000 mL/h
10,000 mL/h
500 mL/h
1000 mL/h

A 65-year-old man who is hospitalized with pancreatic carcinoma develops abdominal distention and obstipation. The following abdominal radiograph is obtained. Which of the following is the most appropriate initial management of this patient?
Urgent colostomy or cecostomy
Detorsion of volvulus and colopexy or resection
Diagnostic and therapeutic colonoscopy
Digital disimpaction of fecal mass in the rectum
Discontinuation anticholinergic medications and narcotics and correction of metabolic disorders
A 65-year-old man who smokes cigarettes and has chronic obstructive pulmonary disease falls and fractures the third, fourth, and fifth ribs in the left anterolateral chest. Chest x-ray is otherwise normal. Which of the following would be the most appropriate next step in his management?
Surgical fixation of the fractured ribs
Placement of an epidural for pain management
Admission to the hospital and treatment with oral analgesia
Tube thoracostomy
Strapping the chest with adhesive tape
A 65-year-old man with a history of occasional painless rectal bleeding presents with 2 to 3 days of constant, dull RLQ pain. He also complains of fever, nausea, and decreased appetite. He had a colonoscopy 2 years ago that was significant for sigmoid and cecal diverticula but was otherwise normal. On physical examination he has RLQ tenderness with rebound and guarding. His vitals include HR of 95 beats per minute, BP of 130/85 mm Hg, and temperature of 101.3°F. The abdominal CT demonstrates the presence of sigmoid and cecal diverticula, inflammation of pericolic fat, thickening of the bowel wall, and a fluid-filled appendix. Which of the following is the most appropriate next step in management?
Begin IV hydration and broad-spectrum antibiotics, keep the patient npo (nothing by mouth), and admit the patient to the hospital
Discharge the patient with broad-spectrum oral antibiotics and surgical follow-up
Begin sulfasalazine 3 to 4 g/d along with IV steroid therapy
Arrange for an emergent barium enema to confirm the diagnosis
Begin IV antibiotics and call a surgical consult for an emergent operative procedure
A 65-year-old smoker previously diagnosed with chronic obstructive pulmonary disease presents to the emergency department complaining of worsening cough and sputum production. She reports feeling breathless when climbing the stairs to her first floor walk-up apartment, and has moderate difficulty in providing her history in complete sentences. X-ray of the chest shows hyper inflated lungs with flattened diaphragms, attenuated vascular markings, and a narrow mediastinum. What agent(s) will provide the greatest relief of symptoms in the emergency department?
Albuterol and ipratropium bromide
N-acetylcysteine
Theophylline
Antibiotics
Magnesium sulfate

A 65-year-old white male who has a history of chronic obstructive pulmonary disease, congestive heart failure, and coronary artery disease presented with a three-day history of worsening shortness of breath, cough with yellowish expectoration, and fever. He is not on steroids and does not use oxygen at home. He takes ipratropium, albuterol, aspirin, digoxin, furosemide, metoprolol, and lisinopril. He lives at home with his wife. His temperature is 39.4°C (103°F), blood pressure is 110/70 mmHg, pulse is 110/min, and respirations are 24/min. He is saturating 88% on room air. He was started on 3-liters of oxygen to keep the saturations above 92%. The chest x-ray of the patient is shown below. What is the most appropriate next step in the management of this patient?
Admit the patient and start vancomycin
Admit the patient and start levofloxacin
Admit the patient and start ciprofloxacin
Admit the patient and give ampicillin
Outpatient trimethoprim-sulfamethoxazole
A 65-year-old white man comes to the Emergency Room complaining of headache, insomnia, palpitations, and vomiting. His past medical history is significant for chronic obstructive pulmonary disease (COPD) treated with theophylline, ipratropium, and occasional albuterol. He had a puncture wound of the foot one week ago, and it is being treated effectively with amoxicillin-clavulanate and ciprofloxacin. For the past three days, his shortness of breath is worsening, and his primary care physician gave oral prednisone. His blood pressure is 150/80 mmHg and heart rate is 105/min with frequent ectopic beats. You suspect that drug toxicity may be responsible for this patient's complaints. Which of the following drugs is most likely responsible for his condition?
Theophylline
Steroids
Albuterol
Ciprofloxacin
Ipratropium
A 65-year-old woman has a life-threatening pulmonary embolus 5 days following removal of a uterine malignancy. She is immediately heparinized and maintained in good therapeutic range for the next 3 days, then passes gross blood from her vagina and develops tachycardia, hypotension, and oliguria. Following resuscitation, an abdominal CT scan reveals a major retroperitoneal hematoma. Which of the following is the best next step in management?
Reverse heparin with protamine, explore and evacuate the hematoma, and ligate the vena cava below the renal veins
Immediately reverse heparin by a calculated dose of protamine and place a vena caval filter (eg, a Greenfield filter)
Stop heparin, give fresh-frozen plasma (FFP), and begin warfarin therapy
Switch to low-dose heparin
Stop heparin and observe closely
A 65-year-old woman is found to have osteoporosis on DEXA scan. She underwent right knee surgery five years ago and developed post-operative deep venous thrombosis, for which she was treated with 6 months of warfarin therapy. She also has severe gastroesophageal reflux disease and takes lansoprazole daily. Her mother died of breast cancer, her maternal aunt has endometrial cancer, and her paternal aunt has a history of ovarian cancer. She does not want to use bisphosphonates because of her reflux symptoms, and would like to consider raloxifene. Which of the following is a contraindication to raloxifene in this patient?
History of deep vein thrombosis
History of colon cancer
History of ovarian cancer in her paternal aunt
History of endometrial cancer in her maternal aunt
History of breast cancer in her mother
A 65-year-old woman is very worried because she recently had a close family member and friend die, one after the other. First, her 85-year-old mother died of an ovarian cancer that was diagnosed 3 years ago. Last week, she lost her best friend to lung cancer that metastasized to the liver and brain. Today, her 58-year-old sister learned that she has breast cancer. She has regular pap smears and breast examinations. She has read in the paper that there are a few ways that have proved to be very successful in preventing breast cancer. Which of the following measures has the best evidence of preventing breast cancer in high-risk women?
BRCA screening
Having mammograms every month
Low-fat diet
Tamoxifen
Prophylactic oophorectomy
A 65-year-old woman presents to the physician’s office for a second opinion on the management options for recently diagnosed breast cancer. She presents with a 2.5-cm mass in the upper outer quadrant of the left breast associated with a palpable axillary node suspicious for metastatic disease. The remainder of her examination is normal. Mammography demonstrates the cancer and shows no other suspicious lesions in either breast. Chest x-ray, bone scan, and blood test panel, including liver fun
Radical mastectomy
Quadrantectomy, irradiation, and axillary node dissection
Lumpectomy and axillary node dissection
Lumpectomy, irradiation, and axillary node dissection
Irradiation of the breast and axilla
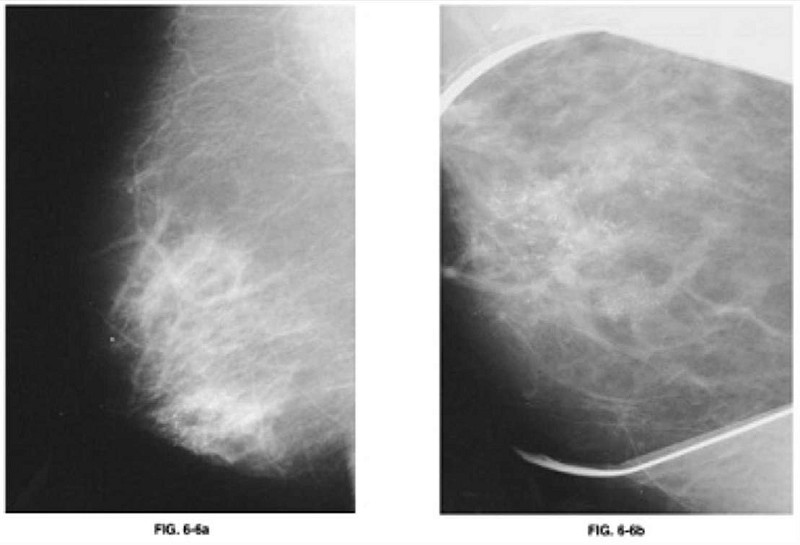
A 65-year-old woman presents to the physician’s office for evaluation of an abnormal screening mammogram. She denies any breast masses, nipple discharge, pain, or skin changes. Past history is pertinent for hypertension. Family history is positive for postmenopausal breast cancer in a sister. She has a normal breast examination and no axillary adenopathy. The remainder of her examination is unremarkable. An MLO view of the right breast is shown in Figure 6-6a along with a magnification view of the craniocaudal (CC) film (Figure 6-6b). Which of the following is the most appropriate next step in management?
Lumpectomy, radiation therapy, and SLN biopsy
Total mastectomy
Observation, with repeat mammogram on an annual basis
Biopsy
Observation, with repeat mammogram in 6 months
A 65-year-old woman with PMH of hypertension treated with lisinopril and hydrochlorothiazide (HCTZ) presents to the office for vaginal bleeding. The bleeding started last month. It was lighter than her menstruation used to be and lasted for 4 days. Vital sign: BP, 135/80 mm Hg; P, 76 beats/min; R, 18 breaths/min; T, 98.9°F. Review of system: No fever, chills, or weight loss, No chest pain or shortness of breath, No abdominal pain, nausea, vomiting, diarrhea, constipation, or distention. Physical examination: Gen: Awake, alert-oriented x3, no acute distress, CVS: S1S2 + RRR no m/r/g, Lungs: CTA bilaterally, Abd: Soft, nontender, nondistended, + bowel sounds, Ext: No edema, Pelvic: Cervix appears normal, no lacerations seen, bimanual examination findings within normal limits. What is the next step in the management of this patient?
Transabdominal US
CTscan
MRI
No further management is needed
Endometrial biopsy
A 66-year-old man complains of exertional dyspnea that has progressed over the last two years. As a result, he has had to limit his physical activities to avoid becoming short of breath. He denies any significant chest pain, but does note having a recurrent cough productive of whitish sputum. His past medical history is significant for hypertension controlled with hydrochlorothiazide. He has a 40 pack-year smoking history. His family history is significant for a stroke in his mother. His blood pressure is 160/90 mmHg and his heart rate is 80/min. Physical examination reveals a mildly overweight patient in no acute distress. His anteroposterior chest diameter is markedly increased. Breath sounds are decreased bilaterally with scattered expiratory wheezes. Which of the following agents is most likely to reduce this patient's symptoms?
Beta-adrenergic blocker
Alpha 2-adrenergic agonist
Dopamine agonist
Muscarinic antagonist
Alpha-adrenergic blocker
A 66-year-old man has progressive shortness of breath due to COPD. He is currently able to do his activities of daily living, but has trouble walking more than one block. His physical examination reveals hyperinflation, increased resonance to percussion, and bilateral expiratory wheezes. He is on appropriate medical therapy for his stage of COPD. Which of the following is also indicated in the management of this condition?
Weight reduction if obese
Pneumococcal vaccination
Haemophilus influenzae B vaccination
Meningococcal vaccination
Yearly influenza vaccination
A 66-year-old man with diabetes and generalized arteriosclerotic occlusive disease notices a gradual loss of erectile fun
Psychotherapy
Pudendal artery revascularization
Implantable penile prosthesis
Erectile nerve reconstruction
Pharmacologic therapy
A 66-year-old white male comes to the physician's office for the first time because of generalized muscle weakness. His review of systems is otherwise negative. He has a past medical history of hypertension, type- 2 diabetes, hyperlipidemia, chronic renal insufficiency and ischemic cardiomyopathy. Neurological examination shows mild weakness of the lower limbs, depressed reflexes and normal sensation. Laboratory studies show: Serum sodium 134 mEq/L, Serum potassium 6.0 mEq/L, Bicarbonate 24 mEq/L, Blood urea nitrogen (BUN) 38 mg/dl, Serum creatinine 2.8 mg/dl, Calcium 8.2 mg/dl, Blood glucose 298 mg/dl. A dose of sodium polystyrene sulfonate is given. Which of the following additional interventions is most important in this patient's management?
Start oral prednisone therapy
Obtain acetylcholine receptor antibodies
Measure serum renin and aldosterone levels
Obtain electromyography
Review all his current medications
A 66-year-old white male presents for evaluation of progressively worsening dyspnea that affects him at rest and wakes him from sleep. He also notes bilateral ankle swelling. His medical history is significant for coronary artery disease for which he has undergone angioplasty and coronary artery bypass grafting. On examination today, his pulse is 86/min, blood pressure is 110/70 mmHg, and respirations are 19/min. His neck veins are distended and there is bilaterally symmetric pitting ankle edema. On chest auscultation, you hear crackles at the bilateral lung bases and a third heart sound. Chest x-ray shows an enlarged cardiac silhouette and bilateral alveolar and interstitial pulmonary edema. Of the medications listed below, which has not been shown to improve survival in patients with the above presentation?
Captopril
Metoprolol
Digoxin
Aspirin
Losartan
A 67 -year-old man presents to your office with a one month history of progressive fatigue and exertional dyspnea. He has no significant past medical history. Physical examination reveals enlarged, non-tender axillary lymph nodes bilaterally. His abdomen is soft and non-tender and the liver span is 10 cm. Serial fecal occult blood tests are negative. Laboratory values are as follows: Hemoglobin 7.8 mg/dl, MCV 90 fl, MCHC 33 g/dl, Reticulocytes 7%, WBC count 22,000/mm3, Platelets 200,000/mm3. Which of the following is most likely to improve this patient's symptoms?
Folic acid
Prednisone
Pyridoxine
Erythropoietin
Iron
A 67-year-old homeless male presents 24 hours after the onset of substernal chest pain and is diagnosed with an anterior wall myocardial infarction. There is no history of previous chest pain, dyspnea, palpitations, syncope or leg swelling. He has no hypertension or diabetes mellitus. He does acknowledge a 40 pack-year smoking history. Upon discharge, echocardiography shows normal left ventricular size, left ventricular anterior wall hypokinesis and an ejection fraction of 50%. Two years later, the patient is found dead in the street. Autopsy reveals a dilated left ventricle with a globular shape and thinned walls along with a scar on the anterior wall. Which of the following would have most likely prevented this patient's pathologic findings?
Digoxin
Aspirin
Enalapril
Amlodipine
Isosorbide dinitrate
A 67-year-old male comes to the clinic for medical clearance prior to an elective abdominal aortic aneurysm repair. He denies any cough, shortness of breath or chest pain. He has coronary artery disease, diabetes and hypertension. He does not use tobacco, alcohol or drugs. His blood pressure is 120/76 mm Hg, pulse is 60/min, and respirations are 14/min. Examination shows no abnormalities, except prominent epigastric pulsations. Which of the following interventions would be most helpful in preventing postoperative pneumonia in this patient?
Intercostal nerve blocks for pain control
Continuous positive airway pressure
Albuterol inhalers
Incentive spirometry
Prophylactic antibiotics
A 67-year-old male comes to the office for a routine physical exam. He retired this year and wants "a clean bill of health." He has no complaints. He stopped smoking 10 years ago, but smoked for 40 years prior to that. He only takes a "water pill" for hypertension. His vital signs are normal. The physical examination reveals a bruit in his neck. His chest x-ray, EKG, and blood work have normal results. Duplex ultrasonography of his neck reveals a 70% irregular lesion at the right common carotid artery bifurcation. The left common carotid artery has a 40% lesion. What is the best next step in the management of this patient?
Long term ASA therapy
Left carotid surgery
Right carotid surgery
Temporal artery biopsy
Heparin

A 67-year-old male presents to the ER with chest pain. His medical history is significant for stable angina for which he takes aspirin and isosorbide dinitrate, as well as hypertension and bronchial asthma. Occasionally, he uses an albuterol inhaler. He is admitted to the hospital and five hours later, he begins to feel lightheaded and weak. His blood pressure is 100/60 mmHg. An EKG is obtained and is shown below. Which of the following is the best next step in managing this patient?
Cardiac catheterization
Adenosine
Digoxin
Metoprolol
Pacemaker insertion
A 67-year-old male presents with a six-month history of rigidity, gait problems, tremor and slowness of movements. His condition has progressively worsened over the last few months, and he is now unable to perform his routine daily activities due to the slowness of his movements. He is not taking any medications. On examination, he is alert and conscious. His face is without expression. There is a resting tremor of his hands. He has a stooped posture and shuffling gate. There is rigidity of his limb muscles. Which of the following is the most appropriate initial treatment for this patient?
L-dopa
Selegiline
Clozapine
Benztropine
Amantadine
A 67-year-old man presents to his primary care physician with a 1-cm skin lesion on his left forearm. On examination, it has a waxy appearance with rolled pearly borders surrounding a central ulcer. Which of the following is the most appropriate management of this patient?
Electrodesiccation of the lesion
Surgical excision
Laser vaporization of the lesion
Mohs surgery
Curettage of the lesion
A 67-year-old man with a history of gout presents with intense pain in his right great toe. He has a complex past medical history, including hypertension, coronary artery disease, congestive heart failure, myelodysplasia, and chronic kidney disease with a baseline creatinine of 3.2 mg/dL and a uric acid level of 10 mg/dL. His medications include aspirin, simvastatin, clopidogrel, furosemide, amlodipine, and metoprolol. What is the best therapy in this situation?
Allopurinol 100 mg po daily and titrate to uric acid less than 6 mg/dL
Colchicine 1.2 mg po initially, followed by 0.6 mg 1 hour later
Probenecid 250 mg po bid
Naproxen 750 mg po once followed by 250 mg po tid
Prednisone 40 mg po daily
A 67-year-old woman with a past medical history significant for hypertension, hypercholesterolemia, and type 2 diabetes calls 911 for severe shortness of breath. Her symptoms started 2 hours ago with chest pain and progressed rapidly to orthopnea and shortness of breath. Her blood pressure is 170/ 100 mmHg and heart rate is 120/min and regular. A third heart sound is present. Bilateral crackles are heard on chest auscultation. Her oxygen saturation is 78% with 40% inspired oxygen. She is intubated in the field by paramedics for progressive respiratory failure and is treated with nitrates and diuretics. After the initial resuscitation, breath sounds on the left side are markedly decreased. Which of the following is most likely to restore breath sounds to this hemithorax?
Pericardiocentesis
Tidal volume increase
Endotracheal tube withdrawal
Left-sided needle thoracostomy
Left-sided chest tube
A 68-year-old African-American man presents to his primary care physician for a check-up. He has not been to the physician’s office in over 15 years. He reports that he is fine but that his wife keeps telling him that he has to “go see the doctor.” He says he has never been sick, despite smoking three packs of cigarettes per day for over 40 years. He also says that he drinks 2–3 beers a night but never had a problem with that either. He’s as healthy “as a bull,” he says. His wife is in the room and says that he recently has had some problems swallowing food and that he is losing weight. He laughs and says, “I just need to chew more and eat more.” His vital signs are normal, as are his laboratory values. The physician is concerned and orders an endoscopy, which reveals a biopsy positive for squamous cell carcinoma of the esophagus. Which of the following most likely could have prevented this condition?
Taking proton pump inhibitors regularly
Getting a colonoscopy every 5 years
Eliminating smoking and alcohol consumption
Eating more meats, especially smoked meats
Avoiding fruits and vegetables
A 68-year-old African-American woman presents to the ER in acute distress. She complains of a sudden onset of complete visual loss in her right eye. Her vision had been blurry for the past few days and acutely worsened one hour ago. She also describes right-sided headaches of two months duration for which she has taken ibuprofen without relief. She has no nausea or vomiting. She has diabetes, hypertension, and degenerative joint disease. Her temperature is 37.2°C (98.9°F) and blood pressure is 146/86 mmHg. Examination reveals complete loss of vision in the right eye. Her pupils are 4 mm bilaterally. Fundoscopy shows a swollen pale disc with blurred margins. A bruit is heard in the right subclavicular area. Motor and sensory examination is within normal limits. Which of the following is the most appropriate next step in management?
Low dose prednisone
High dose prednisone
MRI of the brain with contrast
Methotrexate therapy
Temporal artery biopsy
A 68-year-old female comes to the Emergency Room with increased shortness of breath and cough for 12 hours. She has a history of chronic obstructive pulmonary disease for the past 14 years and has been oxygen dependent for two years. Twelve hours ago, she felt unable to get her breath. She took two extra nebulizer treatments and used her as-needed inhaler with no relief of symptoms. She denies any fever, chills, sweating, nausea or vomiting, and hemoptysis. She rarely uses alcohol, but had smoked two packs/day for 45 years. She quit smoking about six years ago. Her medications include ipratropium, albuterol, multivitamins, and oxygen 2 liters/min by nasal cannula. She is a thin, frail female in moderate distress. Her temperature is 36.7°C (98°F), blood pressure is 110/65 mmHg, pulse is 110/min, and respirations are 28/min. Pulse oximetry shows 84% on 2 liters oxygen by nasal cannula. The patient is given oxygen, methyl prednisolone, aerosolized ipratropium, and albuterol; however, the patient remains dyspneic and bedridden. ABGs are ordered and the results show: pH 7.32, PCO2 60 mmHg, and PO2 52 mmHg on 4-liters O2. What is the next best step in the management of this patient?
Decrease oxygen
Increase oxygen by nasal cannula
Aminophylline
Noninvasive positive pressure ventilation
Intubate and mechanically ventilate the patient
A 68-year-old hypertensive man undergoes successful repair of a ruptured abdominal aortic aneurysm. He receives 9 L Ringer lactate solution and 4 units of whole blood during the operation. Two hours after transfer to the surgical intensive care unit, the following hemodynamic parameters are obtained: systemic blood pressure (BP) 90/60 mm Hg, pulse 110 beats per minute, central venous pressure (CVP) 7 mm Hg, pulmonary artery pressure 28/10 mm Hg, pulmonary capillary wedge pressure (PCWP) 8 mm Hg, cardiac output 1.9 L/min, systemic vascular resistance 1400 (dynes)/cm5 (normal is 900-1300), PaO2 140 mm Hg (FiO2: 0.45), urine output 15 mL/h (specific gravity: 1.029), and hematocrit 35%. Given this data, which of the following is the most appropriate next step in management?
A period of observation to obtain more data
Administration of a vasodilating agent to decrease elevated systemic vascular resistance
Administration of a fluid challenge to increase urine output
Administration of a vasopressor agent to increase systemic blood pressure
Administration of a diuretic to increase urine output
A 68-year-old male complains of pain in his calves while walking. He notes bilateral foot pain, which awakens him at night. His blood pressure is 117/68 mmHg. Physical examination reveals diminished bilateral lower extremity pulses. An ankle:brachial index measures 0.6. The patient’s current medications include aspirin and hydrochlorothiazide. Which of the following is the best initial management plan for this patient’s complaint?
Smoking cessation therapy, consultation with a vascular surgeon
Smoking cessation therapy, warfarin, peripherally acting calcium-channel blocker
Smoking cessation therapy, schedule an arteriogram
Smoking cessation therapy, graduated exercise regimen, cilostazol
Smoking cessation therapy, warfarin
A 68-year-old male is hospitalized following an intracerebral hemorrhage. On hospital day 3, he develops redness, swelling, and tenderness of the left calf. There is no fever. Compression ultrasonography reveals a thrombus in the popliteal vein. Which of the following is the most appropriate next step in the management of this patient?
No treatment for his deep vein thrombosis
Compression stockings
Placement of an inferior vena cava filter
Anticoagulation with heparin
Thrombolytic therapy
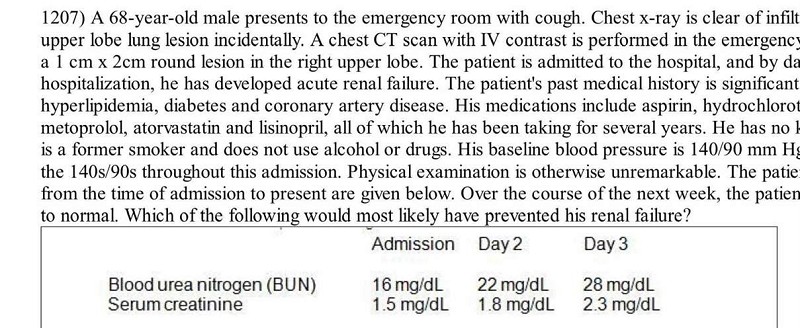
A 68-year-old male presents to the emergency room with cough. Chest x-ray is clear of infiltrates but reveals a right upper lobe lung lesion incidentally. A chest CT scan with IV contrast is performed in the emergency department and reveals a 1 cm x 2cm round lesion in the right upper lobe. The patient is admitted to the hospital, and by day 3 of his hospitalization, he has developed acute renal failure. The patient's past medical history is significant for hypertension, hyperlipidemia, diabetes and coronary artery disease. His medications include aspirin, hydrochlorothiazide, clopidogrel, metoprolol, atorvastatin and lisinopril, all of which he has been taking for several years. He has no known drug allergies. He is a former smoker and does not use alcohol or drugs. His baseline blood pressure is 140/90 mm Hg and has remained in the 140s/90s throughout this admission. Physical examination is otherwise unremarkable. The patient's laboratory values from the time of admission to present are given below. Over the course of the next week, the patient's renal fun
Prednisone
100% oxygen mask
Intravenous hydration
Furosemide
Stopping clopidogrel
A 68-year-old male undergoes colon resection surgery for diverticulosis. In the 24 hours following the surgery, he passes a total of 300 ml of urine. His past medical history is significant for coronary artery disease, right knee osteoarthritis and moderate chronic obstructive pulmonary disease. On physical examination, his blood pressure is 110/70 mm Hg and his heart rate is 90/min. His lungs are clearto auscultation and his abdomen is soft and non-distended. His current labs are given below: Hemoglobin 9.5 mg/dl, WBC count 13,000/mm3, Platelet count 160,000/mm3, Sodium 138 mg/dl, Potassium 5.1 mg/dl, Glucose 108 mg/dl, Creatinine 2.3 mg/dl, BUN 82 mg/dl, His indwelling bladder catheter is changed but no residual urine is drained. Which of the following is the best next step in managing this patient?
Furosemide
Intravenous pyelography
Low-dose dopamine infusion
Bolus of IV fluids
Mannitol
A 68-year-old man comes to the emergency department because of sudden onset back pain. He has never had back pain before and denies any trauma. He does not feel well and feels "like he is going to die". His blood pressure is 70/40 mm Hg, pulse is 110/min and respirations are 20/min. On examination, the abdomen is tender to palpation and there is a large pulsatile mass. Which of the following is the most appropriate next step in management?
CT scan of abdomen
Resuscitate and re-evaluate
Abdominal angiogram
Laparotomy
Fast track ultrasound
A 68-year-old man presents to the emergency department complaining of left lower extremity pain. He says that he first noticed a tingling sensation in his leg 3 hours ago, and since that time it has become increasingly painful. Over the past hour, he says, the skin on his leg has started to change color. His medical history is significant for hypertension, diabetes mellitus, atrial fibrillation, and major depressive disorder. He cannot remember his medication list at this time. On physical examination, his blood pressure is 127/74 mmHg and his heart rate is 102/min. His left lower extremity is cool and pale below the level of the knee. Neither the posterior tibial nor the dorsalis pedis pulse is palpable. Which medication could have prevented this acute problem?
Aspirin
Clopidogrel
Warfarin
Diltiazem
Metoprolol
A 68-year-old woman with a history of well-managed sick sinus syndrome and osteoporosis is brought to the physician by her daughter. According to the daughter, her mother has become increasingly forgetful and irritable over the past two years. She adds that she felt less concerned about her mother's forgetfulness as "it just comes with aging," but that the "mood swings have become a problem in terms of her getting along with family members." A Folstein Mini-Mental Status Examination is performed and suggests significant cognitive decline. Dementia is strongly suspected. After potentially causative medical or psychiatric conditions have been ruled out, the diagnosis of Alzheimer's dementia is made. Which of the following medications would be most appropriate in the treatment of this woman's condition?
Sertraline
Donepezil
Lorazepam
Bupropion
Risperidone
A 69-year-old male presents to the ER with severe shortness of breath for the past 12 hours. He reports that he has used his albuterol inhaler many times without relief. On review of systems he notes having had a mild fever yesterday that resolved with acetaminophen. The patient quit smoking 2 years ago but has a 100 pack year smoking history. On physical examination, his blood pressure is 150/90 mmHg and heart rate is 110/min. The patient is using accessory muscles of respiration. Expirations are prolonged, and there are wheezes bilaterally. Arterial blood gas (ABG) analysis reveals the following: pH 7.36, pO2 64 mmHg, pCO2 57 mmHg, HCO3 32 mEq/L. The patient is treated with ipratropium and albuterol nebulizers and moxifloxacin. Which of the following additional therapies is most likely to benefit this patient?
Mucolytic agents
Corticosteroids
Loop diuretic
Aminophylline
Diltiazem

A 69-year-old man with mild hypertension and chronic obstructive pulmonary disease (COPD) presents with transient ischemic attacks and the angiogram shown here. Which of the following is the most appropriate treatment recommendation?
Medical risk factor management and carotid endarterectomy if neurologic symptoms develop
Carotid endarterectomy
Angioplasty of the carotid lesion followed by carotid endarterectomy if the angioplasty is unsuccessful
Medical therapy with warfarin
Medical therapy with aspirin 325 mg/day and medical risk factor management
A 7 -day-old male infant is brought by his mother complaining of decreased movements of his right arm. She denies any trauma or fall. Pregnancy was uneventful, but delivery was complicated with shoulder dystocia. Examination reveals the presence of crepitus and bony irregularity over the clavicular area and Mora reflex is absent on the right. Which of the following is the most appropriate management?
Casting of the right arm and shoulder
Passive and active motion exercises
Nerve grafting
Reassurance
Figure-of-eight clavicle strap
A 7 -year-old boy is brought to the office by his mother due to nocturnal enuresis. He has been wetting his bed at night for the past two years. He is otherwise healthy and has no psychological or behavioral problems. His mother is desperately asking for your help because she has tried alarms and bladder training, all to no success. What is the most appropriate next step in the management of this patient?
Insulin
Prazosin
Haloperidol
Clonidine
Desmopressin
A 7 -year-old boy is brought to your office with a mild fever and neck swelling. His mother says that the boy has been complaining of neck pain for a couple of days and she noticed a tender neck lump yesterday. All of his vaccinations are up-to-date. He has no known allergies. Physical examination reveals a tender and fluctuant anterior cervical mass. Which of the following is the best medication for this patient?
Penicillin
Dicloxacillin
Erythromycin
Acyclovir
Amoxicillin
A 7 -year-old Caucasian boy is brought to the clinic due to malaise and headache for the past 2 weeks. He was apparently normal until 3 weeks ago, when he went on a hiking trip with his family to Connecticut. His father found a tick attached to his thigh; however, a red macule remains at the site where the tick was attached. One week after the tick was removed, a red ring developed around the macule, and then the ring appeared to grow larger by expanding outward, leaving an area of central clearing. What is the most appropriate next step in the management of this patient?
Doxycycline
Ceftriaxone
Penicillin G
Erythromycin
Amoxicillin
A 7-day-old female neonate is brought to your office for a 2-day history of jaundice and poor feeding. According to the mother, she has vomited twice but doesn't appear febrile. She is regularly breastfed. Her birth history is unremarkable. On examination, she appears listless, and mild jaundice, along with signs of dehydration, are noted. Her blood pressure is 78/52mm Hg, pulse rate is 150/min, and temperature is 36 C (96 F). Her family history is insignificant. What is the most appropriate next step in the management of this patient?
Stop breast feeding
Obtain liver function tests
Obtain Coomb's test and osmotic fragility test
Obtain blood cultures and lumbar puncture
Obtain peripheral smear and reticulocyte count
A 7-month-old boy is brought to his physician because of increased agitation and restlessness. Lung examination reveals crackles and decreased breath sounds bilaterally. Chest x-ray films are notable for bilateral pneumonia. Arterial blood gas analysis reveals an oxygen tension of 45 mm Hg and a carbon dioxide tension of 60 mm Hg. Which of the following is the most appropriate next step in management?
Administer oxygen
Insert endotracheal tube
Administer antibiotics
Administer bronchodilators
Obtain blood cultures
A 7-year-old boy has a history of repeated urinary tract infections that have been treated by the empiric use of antibiotics. The parents are not satisfied with the care the child is receiving, and they take him to a pediatric urologist. Evaluation by voiding cystourethrogram shows that the patient has vesicoureteral reflux without ureteral or upper tract dilatation (grade one reflux). Which of the following is the appropriate management for this child?
Surgical reimplantation of the ureter
Nephrectomy on the affected site
Reassurance and observation
Long-term, low-dose antibacterial therapy
Alpha blockers
A 7-year-old boy is brought to the office by his mother because, "he is always daydreaming." Sometimes, he stares for a few seconds and rolls his eyes for unknown reasons. His teacher has noted a recent decline in his school performance. He has no family history of any seizure disorder, and his psychomotor development is normal. His neurological examination is unremarkable. EEG during hyperventilation shows generalized, symmetrical 3-Hz spike-and-wave activity on a normal background. Which of the following medications is the most appropriate to treat the boy's disorder?
Phenytoin
Clonazepam
Lamotrigine
Phenobarbital
Valproic acid
A 7-year-old boy is brought to the office by his mother due to anal pruritus for the past month. His symptoms are most severe at night. Physical examination is normal, except for mild perianal erythema. Stool examination is normal. "Scotch tape test" is positive. Which of the following is the most appropriate treatment for this child's condition?
Metronidazole
Pyrantel pamoate
Albendazole
Thiabendazole
Ivermectin
A 7-year-old boy is brought to the pediatrician by his mother for a routine check-up. Physical examination is normal, but during the exam the mother reveals that her son's behavior has been poor. She says that he is always running around (even during dinner), doesn't listen, and keeps his room a mess. She hopes he will grow out of this soon. Upon further questioning, the pediatrician learns that the patient's second-grade teacher has reported that he answers questions impulsively and out of turn, and that he cannot sit at his desk for a very long time without fidgeting. He also frequently forgets to bring in his homework. The mother states that her son has had these symptoms for about a year, and that his grades have been falling over the past six months. The diagnosis of attention deficit hyperactivity disorder is made and the boy is started on methylphenidate. Which of the following side effects is most likely to occur in patients who take methylphenidate?
Decreased appetite
Seizures
Weight gain
Diarrhea
Hypersomnia
A 7-year-old boy is brought to your office with a sore throat, decreased appetite, and nausea. His past medical history is insignificant. All of his vaccinations are up-to-date. He has no known allergies. His temperature is 39.0°C (102.5°F), blood pressure is 110/70 mmHg, pulse is 104/min, and respirations are 16/min. On examination, the pharynx and tonsils are red, sv1ollen, and have white exudates on their surface. There is also bilateral tender cervical lymphadenopathy. The rapid diagnostic test for streptococcal antigen is positive. What is the most appropriate next step in management?
Throat culture
Oral azithromycin
Antistreptolysin O antibodies
Oral penicillin V
Monospot test
A 7-year-old boy is referred for genetic testing because his father was diagnosed with medullary cancer of the thyroid. The father underwent a total thyroidectomy, and in the preoperative workup it was determined that he also had a pheochromocytoma, and that tumor was removed also. The father did not have parathyroid hyperplasia at the time, his phenotype was normal, and his final diagnosis was MEN-2A. The child is tested and found to have RET mutations in the peripheral white blood cells. The child has normal phenotype, normal levels of calcitonin, normal levels of catecholamines, metanephrines, and VMA, and normal levels of calcium and parathyroid hormone. Which of the following is the most appropriate management?
Continued observation
Total thyroidectomy
Parathyroid surgical exploration
MRI of the pituitary
Bilateral adrenalectomies
A 7-year-old child is brought by his mother for a school physical. His growth parameters show his height to be 50th percentile and his weight to be significantly higher than 95th percentile. His mother complains that he always seems sleepy during the day and that he has started complaining of headaches. His second-grade teacher has commented that he has difficulty staying awake in class. His mother complains that he wakes up the whole house with his snoring at night. Which of the following is the most appropriate next step in evaluating and managing this condition?
Arrange for polysomnography
Arrange for home oxygen therapy for use at night
Arrange for continuous positive airway pressure (CPAP) at home
Refer to an otolaryngologist for tonsillectomy and adenoidectomy
Try steroids to decrease tonsillar and adenoid hypertrophy
A 7-year-old child is scheduled for an elective tonsillectomy. The most important instruction to the parents should be to make sure that the child does which of the following?
Eats iron-laden foods for 3 weeks before surgery
Does not drink from siblings’ cups
Avoids aspirin and antihistamines for 2 weeks before surgery
Discontinues antibiotics 72 hour before surgery
Avoids contact with other children
A 7-year-old girl complains of increased urinary frequency, dysuria and itching on urination. Her urinalysis is consistent with a urinary tract infection. This is her 20th infection in the past year, despite adequate antibiotic coverage. Further imaging of her bladder, kidneys and ureter reveals is consistent with vesicoureteral reflux. Which of the following is the next appropriate step?
Intravenous antibiotics for two weeks
Antireflux surgery
CT scan of the pelvis
Intravenous pyelogram
Renal arteriogram
A 7-year-old girl is brought in to see you by her mother because the girl has developed breasts and has a few pubic hairs starting to show up. Which of the following is the best treatment for the girl’s condition?
No treatment; reassure the mother that pubertal symptoms at age 7 are normal
Exogenous gonadotropins
Clomiphene citrate
GnRH agonists
Ethinyl estradiol
A 7-year-old girl is seen in your office after her mother began to notice significant changes in her physical appearance. The mother says that she first noticed the development of her daughter's breasts, and she became more worried when her daughter developed both axillary and pubic hair. The patient's grandmother told the mother not to worry because two of the patient's aunts entered puberty at an early age. The patient has not had any behavioral changes or a decline in her school performance, and she denies headaches, visual changes, or vomiting. Physical examination reveals the presence of axillary hair, pubic hair at Tanner stage 3, and breast development at Tanner stage 4. The rest of the examination is unremarkable. GnRH stimulation test results in an increase of LH. Which of the following is the most appropriate management for this patient?
Medroxyprogesterone acetate therapy
Reassurance
GnRH agonist therapy
Danazol therapy
Cyproterone acetate
A 7-year-old girl presents with hives, which developed after a bee sting. She has no other symptoms. The hives resolve with diphenhydramine. Which of the following is the most appropriate management?
Provide an Epi-pen Jr (epinephrine auto injector) to be carried at all times, as well as a prescription for diphenhydramine
Write a prescription for diphenhydramine in case she is bitten again
Order a skin-prick test with hymenoptera venom
Refer her to an allergist for desensitization
Admit to the hospital for observation for delayed hypersensitivity symptoms
A 70-kg woman is to undergo nail removal from her right ring finger in the ambulatory surgery clinic. Which of the following is the most appropriate option for local anesthesia?
Digital block with 1% lidocaine without epinephrine up to 4.5 mg/kg
Local injection around the nail bed with 1% lidocaine with epinephrine up to 7 mg/kg/mL
Local injection around the nail bed with 1% lidocaine with epinephrine up to 4.5 mg/kg
Digital block with 1% lidocaine with epinephrine up to 7 mg/kg
Digital block with 1% lidocaine with epinephrine up to 4.5 mg/kg
A 70-year-old female has been healthy except for hypertension treated with a thiazide diuretic. She presents with sudden onset of a severe, tearing chest pain, which radiates to the back and is associated with dyspnea and diaphoresis. Blood pressure is 210/94 mmHg. Lung auscultation reveals bilateral basilar rales. A faint murmur of aortic insufficiency is heard. The BNP level is elevated at 550 pg/mL (Normal < 100). ECG shows nonspecific ST-T changes. Chest x-ray suggests a widened mediastinum. Which of the following choices represents the best initial management?
IV heparin followed by CT pulmonary angiography
IV beta-blocker to control heart rate, IV nitroprusside to control blood pressure, transesophageal echocardiogram
Blood cultures and rapid initiation of vancomycin plus gentamicin, followed by echocardiography
Percutaneous coronary intervention with consideration of angioplasty and/or stenting
IV furosemide plus IV loading dose of digoxin
A 70-year-old male presents with malaise, pain and stiffness of his neck, shoulders and hips for the last 3 months. His stiffness is worse in the morning and lasts about 30-40 minutes. He also complains of a recent weight loss of 7 lbs and mild fevers. He has no headache, scalp tenderness, visual symptoms or jaw claudication. Examination shows no swelling or tenderness of the involved joints with normal range of motion on active and passive movement. The arteries of the scalp, neck and extremities are normally palpable without any tenderness. Labs show a hematocrit of 31% and an ESR of 65 mm/hr. Blood cultures are negative. Which of the following is the most appropriate next step in management of this patient?
Measure antinuclear antibodies and rheumatoid factor levels
Treatment with high-dose prednisone
Treatment with low-dose prednisone
Treatment with nonsteroidal anti-inflammatory agents
Temporal artery biopsy
A 70-year-old male with a history of coronary artery disease presents to the emergency department with 2 hours of substernal chest pressure, diaphoresis, and nausea. He reports difficulty “catching his breath.” An electrocardiogram shows septal T-wave inversion. The patient is given 325-mg aspirin and sublingual nitroglycerin while awaiting the results of his blood work. His troponin I is 0.65 ng/mL (normal < 0.04 ng/mL). The physician in the emergency department starts the patient on low-molecular-weight heparin. His pain is 3/10. Blood pressure is currently 154/78 mmHg and heart rate is 72. You are asked to assume care of this patient. What is the best next step in management?
Begin clopidogrel 300 mg po each day
Begin intravenous beta-blocker therapy
Admit the patient to a monitored cardiac bed and repeat cardiac enzymes and ECG in 6 hours
Begin intravenous thrombolytic therapy
Arrange for emergent cardiac catheterization
A 70-year-old man is admitted to the ICU after repair of an abdominal aortic aneurysm. He has a prior history of hypertension and mild congestive heart failure, which were adequately controlled with digoxin and diuretics. To facilitate perioperative management, a Swan-Ganz (multilumen pulmonary artery) catheter was inserted in the operating room. During the first few hours postoperatively, the patient is noted to have a blood pressure of 140/70 mmHg, heart rate of 110/min, flat neck veins, a pulmonary arterial wedge pressure of 9 mmHg, and poor urine output. Several hours after this intervention a bolus of IV crystalloid, the patient is reassessed. The blood pressure is 150/85 mmHg, heart rate is 90/min, neck veins are distended, and the pulmonary arterial wedge pressure is 17 mmHg. Urine output is still low in volume. At this point, management should be which of the following?
IV digoxin administration
IV furosemide
A nitroprusside infusion
A dopamine infusion
A bolus of IV crystalloid
A 70-year-old man is concerned when his dentist finds a white patch on his oral mucosa during a routine examination. Proper management should include which of the following?
Application of topical antibiotics
Excisional biopsy of all lesions
Application of topical chemotherapeutic agents
Strict oral hygiene and avoidance of alcohol and tobacco
Low-dose radiation therapy
A 70-year-old man presents to the urgent care clinic complaining of extensive bruising and bleeding gums. His medical history is significant for atrial fibrillation for which he takes metoprolol and warfarin. He has been stable on his current dose of warfarin for several months. He denies any recent use of NSAIDs or other over-the-counter medications. The patient reports that he has been taking his warfarin as prescribed and has been trying to "live a healthier life" lately. On further questioning, he reports trying to exercise more often, taking numerous vitamin supplements daily, and eating more vegetables. His new diet consists mainly of vegetables like spinach, Brussels sprouts, and broccoli, as well as copious amounts of green tea. Which of the following lifestyle changes is most likely responsible for this patient's bleeding?
Brussels sprouts
Vitamin supplements
Spinach
Increased exercise
Green tea
A 70-year-old man presents with back pain and increasing difficulty with initiating a urinary stream. On rectal examination, he is found to have a hard, irregularly enlarged prostate. He has an elevated prostate-specific antigen (PSA), and osteoblastic lesions in the vertebral column and bones of the pelvis. A needle biopsy of the prostate shows well-differentiated adenocarcinoma. Which of the following is the treatment of choice?
Transurethral prostatectomy
Hormonal manipulation
Radiotherapy
Cytotoxic chemotherapy
Radical prostatectomy
A 70-year-old man with a history of congestive heart failure (CHF) secondary to nonischemic cardiomyopathy presents to the office for preoperative evaluation for total hip replacement. The previous echocardiogram revealed an ejection fration (EF) of 30%, and he occasionally has shortness of breath with exertion. His vital signs: BP 185/60 mm Hg, HR 95 beats/min, R 20 breaths/min, T0 98,60F. Which of the following factors in this patient’s history and physical examination puts him most at a high risk for perioperative mortality?
EF < 35%
JVD
Chronic alcohol use
Current smoker
History of cirrhosis
A 70-year-old woman has nausea, vomiting, abdominal distention, and episodic crampy midabdominal pain. She has no history of previous surgery but has a long history of cholelithiasis for which she has refused surgery. Her abdominal radiograph reveals a spherical density in the right lower quadrant. Which of the following is the definitive treatment for this patient’s bowel obstruction?
Nasogastric (NG) tube decompression
Ileocolectomy
Cholecystectomy
Ileotomy and extraction
Intravenous antibiotics
A 70-year-old woman undergoes a cardiac catheterization for exertional chest pain. Her pain continues to worsen and she is interested in having either surgery or percutaneous coronary intervention (PCI). Which of the following would be an indication for her to undergo either coronary artery bypass grafting or PCI?
Two-vessel coronary disease with proximal left anterior descending artery stenosis and depressed left ventricular ejection fraction
Three-vessel coronary artery disease and diabetes
Left main stenosis and additional coronary artery disease with depressed left ventricular ejection fraction
Isolated left main stenosis and diabetes
Isolated left main stenosis, no diabetes, and normal left ventricular ejection fraction
A 71-year-old man returns from the operating room (OR) after undergoing a triple coronary bypass. His initial cardiac index is 2.8 L/ (min•m2). Heart rate is then noted to be 55 beats per minute, BP is 110/80 mm Hg, wedge pressure is 15, and his cardiac index has dropped to 1.6 L/(min•m2). He has a normal left ventricle. Which of the following maneuvers will increase his cardiac output?
Increase his inspired O2 concentration
Increase his blood viscosity
Increase his heart rate to 90 by electrical pacing
Increase his peripheral vascular resistance
Increase his CVP
A 71-year-old woman with a 40-year smoking history is noted to have a peripheral nodule in her left upper lobe on chest x-ray. Workup is consistent with small cell lung cancer with ipsilateral mediastinal lymph node involvement but no extrathoracic disease. What is the best treatment option for this patient?
Neoadjuvant chemotherapy followed by thoracotomy with left upper lobectomy and mediastinal lymphnode dissection
Neoadjuvant chemoradiation followed by thoracotomy with left upper lobectomy and mediastinal lymph-node dissection
Chemoradiation
Thoracotomy with left upper lobectomy and mediastinal lymph node dissection followed by adjuvant chemotherapy
Thoracotomy with left upper lobectomy and mediastinal lymph node dissection
A 72-year-old Caucasian male presents with shortness of breath that awakens him at night. At baseline he is able to walk less than a block before stopping to catch his breath. Physical examination findings include bilateral basilar rales and neck vein distention. The patient has a known history of congestive heart failure, and his last echocardiogram revealed an ejection fraction of 25%. The patient is compliant with a medication regimen including an ACE inhibitor, beta-blocker, and loop diuretic. Blood pressure is well controlled. What additional treatment should you begin next?
Hydralazine and isosorbide dinitrate
Spironolactone
Aspirin
Amlodipine
Warfarin
A 72-year-old chronic smoker with severe chronic obstructive pulmonary disease (COPD) is found to have a central hilar mass on chest x-ray. Bronchoscopy and biopsies establish a diagnosis of squamous cell carcinoma of the lung. Pulmonary fun
CT scan of the upper abdomen to rule out liver metastasis
Palliative pneumonectomy
Pneumonectomy with hope of cure
Mediastinoscopy to biopsy carinal nodes
Radiation and chemotherapy
A 72-year-old G5P5 presents to your office for well-woman examination. Her last examination was 7 years ago, when she turned 65. She has routine checks and laboratory tests with her internist each year. Her last mammogram was 6 months ago and was normal. She takes a diuretic for hypertension. She is a retired school teacher. Her physical examination is normal. Which of the following is the best vaccination to recommend to this patient?
Hepatitis B vaccine
Pneumocystis
Measles-mumps-rubella
Influenza vaccine
Diphtheria-pertussis
A 72-year-old Hispanic man comes to the clinic with complains of mild headache, and lethargy for the past several days. He complains of cough for the past 12 years, the cough has been bothering him more lately. The cough is mucoid, he has noticed blood in it once in a while. He has smoked 1 pack/day for 29 years. His vitals are, Temperature 37.0°C (98.6°F); BP 120/84 mm Hg; PR 78/min; RR 24/min. On examination of lungs, adventitious sounds are heard over all the lobes and scant crackles at the base. Laboratory studies show: WBC 7,600/mm3, Hemoglobin 13.6, Hematocrit 40%, Platelets 214,000mm3, Sodium 130 mEq/L, Potassium 3.6 mEq/L, Bicarbonate 18 mEq/L, Blood urea nitrogen 16 mg/dl, Creatinine 0.6 mg/dl, Glucose 95 mg/dl, Serum osmolality 260 mOsm/kg (normal 280), Urine osmolality 310 mOsm/kg. A chest x-ray shows a 2-centimeter left upper lobe mass and mediastinal adenopathy. What will be the next best step in management of this patient?
Start an infusion of hypertonic saline
Start furosemide
A CT of head
Prescribe demeclocycline
Restrict the patient water intake

A 72-year-old male is admitted to the hospital with chest pain. EKG and cardiac enzymes confirm a myocardial infarction and he is started on nitroglycerine, aspirin, simvastatin and low molecular weight heparin. Four days later, he complains of leg pain. Physical examination reveals a cold, pale leg. The angiogram is shown below. What is the best next step in his management?
Leg elevation and warm compress
Embolectomy
Intravenous streptokinase
Clopidogrel
Cilostazol
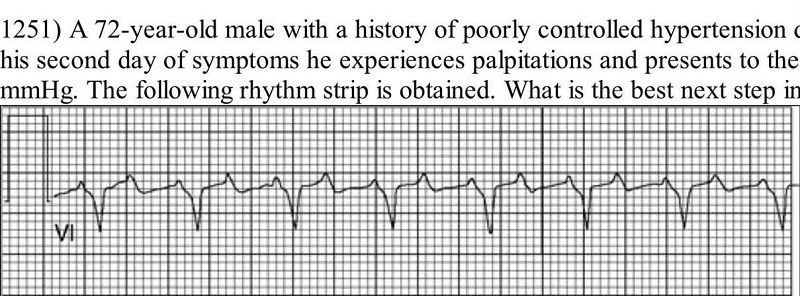
A 72-year-old male with a history of poorly controlled hypertension develops a viral upper respiratory infection. On his second day of symptoms he experiences palpitations and presents to the emergency room. His blood pressure is 118/78 mmHg. The following rhythm strip is obtained. What is the best next step in the management of this patient?
Initiation of chest compressions and preparation for semielective intubation
Emergent electrical cardioversion
Administration of intravenous amiodarone
Administration of intravenous adenosine
Administration of intravenous metoprolol
A 72-year-old man has a 3-mm ureteral stone impacted at the ureterovesical junction. He has been having mild ureteral colicky pain for about 12 hours, and he has been given fluids and analgesics in the expectation that he will spontaneously pass the stone. He then has shaking chills, and spikes a temperature of 40C (104F). When seen shortly thereafter, he has flank pain and looks quite ill. Which of the following is the most appropriate next step in management?
IV antibiotics and immediate decompression of the urinary tract above the stone
Immediate insertion of a suprapubic catheter into the bladder
Extracorporeal shock wave lithotripsy and parenteral antibiotics
Crushing and extraction of the stone via cystoscopy
Addition of IV antibiotics to the current therapeutic regimen
A 72-year-old man is scheduled to have elective sigmoid resection for diverticular disease. He has a history of heart disease, and had a documented myocardial infarction 2 years ago. He currently does not have angina, but he lives a sedentary life because "he gets out of breath" if he exerts himself. During the physical examination, it is noted that he has jugular venous distention. He has hemoglobin of 12 g/dL. If surgery is indeed needed, which of the following should most likely be done prior to the operation?
If at all possible, wait 6 months before performing surgery
Treat the patient for congestive heart failure
Order a transfusion to increase the patient's haemoglobin to 14 g/dL
Place the patient on intensive respiratory therapy
Evaluate the patient as a candidate for coronary revascularization
A 72-year-old man presents for a follow-up visit regarding his depressed mood after his wife's death seven months ago. The patient complains of lethargy and episodes of tearfulness. He has attended three sessions of supportive psychotherapy so far and expresses appreciation for the referral because he likes the therapist. However, he continues to feel depressed and is now experiencing insomnia. He is also feeling very guilty about his wife's death and feels that he should have somehow done more for her in her final months. He admits that during a particularly dark moment last month he briefly contemplated committing suicide so that he could "join her," although he is adamant that he does not feel suicidal at this time and will readily contract for safety. Physical examination reveals the patient has lost 13 lbs (5.9 kg) since his wife's death. What is the most appropriate next step?
Provide reassurance and continue psychotherapy regimen
Increase psychotherapy sessions to twice weekly
Recommend electroconvulsive therapy
Prescribe amitriptyline and alprazolam
Prescribe sertraline
A 72-year-old man presents with right eye pain for 1 day. The patient has a history of diabetes, hypertension, and “some type of eye problem.” He does not recall the name of his eye problem or the name of his ophthalmic medication. However, he does remember that the eye drop has a yellow cap. Which class of ophthalmic medication is the patient taking?
Antibiotic
Miotic
Anesthetic
Mydriatic/cycloplegic agent
β-Blocker
A 72-year-old man status post–coronary artery bypass graft (CABG) 5 years ago presents with hematochezia, abdominal pain, and fevers. Colonoscopy reveals patches of dusky-appearing mucosa at the splenic flexure without active bleeding. Which of the following is the most appropriate management of this patient?
Exploratory laparotomy with thrombectomy of the inferior mesenteric artery
Expectant management
Emergent laparotomy with left hemicolectomy and transverse colostomy
Aortomesenteric by pass
Angiography with administration of intra-arterial papaverine
A 72-year-old man undergoes coronary artery bypass graft (CABG) for severe coronary artery disease. He is extubated on the second postoperative day. His temperature is 36.6°C (97.9°F), blood pressure is 120/70 mm Hg, pulse is 80/min, and respirations are 12/min. On the third postoperative day, he complains of dyspnea and worsening retrosternal pain despite continuous analgesia with morphine. His temperature is 38.6°C (101.5°F), blood pressure is 112/52 mm Hg, pulse is 125/min and irregularly irregular and respirations are 28/min. Examination shows normal heart sounds. A small amount of cloudy fluid is present in the sternal wound drain. His ECG shows atrial fibrillation with rapid ventricular response. An x-ray film of the chest shows widening of the mediastinum. Echocardiography reveals a small amount of pericardial fluid. Laboratory studies show: Hemoglobin 8.9 mg/dl, WBC count 16,300/mm3, Platelet count 512,000/mm3, Creatinine 1.7 mg/dl, CPK 430 U/L.Which of the following will this patient most likely require?
Surgical debridement and antibiotic therapy
Pericardial puncture and nonsteroidal anti-inflammatory agents
Nonsteroidal anti-inflammatory agents alone
Broad-spectrum antibiotics alone
Anticoagulation and electrical cardioversion
A 72-year-old man underwent bypass grafting for severe coronary artery disease. On the 1st postoperative day, his temperature is 36.6C (97.9F), blood pressure is 120/70 mm Hg, pulse is 80/min and respirations are 12/min. On postoperative day 10 he is complaining of worsening retrosternal pain despite continuing analgesia with morphine. He also has dyspnea at rest. His temperature currently is 37.90 C ( 100.10 F), blood pressure is 110/70 mm Hg, pulse is 100/min and respirations are 24/min. Examination shows clear heart sounds without murmurs or rubs. EKG shows no acute changes compared to the EKG on the 1st postoperative day. An x-ray film of the chest shows widening of the mediastinum. Echocardiography shows a small amount of pericardial fluid. Laboratory studies show: Hemoglobin 11 .0 g/L, Platelets 120,000/mm3, Leukocy1e count 16,500/mm3, Neutrophils 86%, Lymphocy1es 13%, Prothrombin time 12 sec, Partial thromboplastin timeb30sec. Which of the following will this patient most likely require?
Pericardial puncture and aspirin therapy
Antibiotic therapy alone
Thoracotomy for debridement and drainage; antibiotic therapy
Thoracotomy for hemostasis
Aspirin therapy
A 72-year-old man with diabetes, renal insufficiency, and coronary artery disease presents in septic shock from emphysematous cholecystitis. His oxygen saturation is 100% on 6-L nasal cannula and his hemoglobin is 7.2 mg/dL. His mixed venous oxygen saturation is 58%. Which of the following treatment options will improve his oxygen delivery the most?
Transfuse two units of packed red blood cells 7
Administer an erythropoietic agent
Transfer him to a hyperbaric chamber
Administer ferrous sulfate
Increase his inspired oxygen concentration
A 72-year-old retired banker is brought to the ED by his daughter for increasing confusion, lethargy, cough, and fever. You remember the patient because he was discharged just 3 days earlier after being treated for urinary retention secondary to benign prostatic hypertrophy (BPH). The patient’s cough has been present since discharge and is accompanied by dark green sputum. He has not returned to work, and he has not been able to ambulate. His vital signs: BP 86/40 mm Hg, R 32 beats/min, P 121 beats/min, T0 101.90F (39.190F). What is the best next step in the management of this patient?
Await blood culture results
Start anti-biotherapy
Normal saline (NS) bolus
Consult pulmonary
Dextrose 5% water colloid bolus
A 72-year-old woman presents to her physician complaining of fatigue, malaise, weight loss, and salt cravings. The patient has chronic obstructive pulmonary disease and is intermittently treated with corticosteroids but is not using home oxygen. Her oxygen saturation is 97% on room air with a blood pressure of 115/65 mmHg, which is significantly lower than her baseline of 125/78 mmHg. On auscultation she has good breath sounds bilaterally without wheeze, although the expiratory phase is slightly prolonged. Five weeks ago she received a corticosteroid treatment for an acute chronic obstructive pulmonary disease exacerbation, for which she was hospitalized and given 3 L of oxygen via nasal cannula. However, she admits that after discharge she was having continued difficulty breathing and did not follow the taper of the corticosteroids. The patient has smoked one pack of cigarettes per day for the past 51 years. Which of the following is the appropriate first step in the management of this patient?
Restart corticosteroids and follow a strict taper
3 L of oxygen via nasal cannula
Intravenous fluids
CT scan of the chest
X-ray of the chest
A 72-year-old woman undergoes a partial colectomy for adenocarcinoma of the sigmoid colon. She receives appropriate antibiotic coverage and low-dose heparin prophylaxis. On the 5th hospital day, the patient begins complaining of right chest pain, difficulty in breathing, and dry cough. Her temperature is 37.9C (100.2F), blood pressure is 134/78 mm Hg, pulse is 115/min and regular, and respirations are 20/rnin. Examination shows crackles in the right chest, but no tenderness or edema in the legs. A chest x-ray film reveals areas of opacification in the right lung. ECG reveals sinus tachycardia with nonspecific ST changes. Laboratory studies show: Arterial blood gas analysis- PaO2 74 mm Hg- PaCO2 37 mm Hg- pH 7.35- Blood/serumHematocrit 40%- Leukocytes 8300/mm3- Lactate dehydrogenase 350 U/L- Fibrin D-dimer 600 ng/mL (normal upper limit 500 ng/mL)Which of the following is the most appropriate step in diagnosis?
Ventilation-perfusion lung scanning
Contrast venography
Ultrasonography of the lower extremities
Pulmonary angiography
Bronchoalveolar lavage
A 72-year-old woman with poorly controlled type 2 diabetes mellitus presents to your clinic one week after being discharged from the hospital. She had been admitted with pyelonephritis secondary to a multi-drug resistant organism, and received several days of intravenous antibiotics. Her serum creatinine on admission had been 2.1 mg/dl. Today it is found to be 4.9 mg/dl. Urinalysis reveals rare epithelial casts and no white blood cells. FENa is greater than 2%. What antibiotic did she most likely receive during her hospitalization?
Vancomycin
Levofloxacin
Amikacin
Doxycycline
Nafcillin
A 72-year-old woman with severe COPD who requires home oxygen is unable to ambulate inside her home without experiencing severe left hip pain. She was hospitalized 1 year ago for a viral pneumonia and was ventilator-dependent at that time for 6 weeks. On examination, her blood pressure is 165/80 mm Hg. She has weakly palpable bilateral femoral pulses. An angiogram demonstrates severe aortoiliac disease involving bilateral iliac vessels. Which of the following is the most appropriate vascular procedure for this patient?
Common femoral and profunda femoral endarterectomise
Femorofemoral bypass
Aortobifemoral bypass
Femoropopliteal bypass
Axillofemoral bypass
A 73-year-old male who is a nursing home resident underwent a laparotomy for intestinal obstruction. He has advanced dementia. On the 8th postoperative day, he complains of pain and swelling on the left angle of his jaw. His temperature is 38.90 C ( 102.00 F), blood pressure is 150/80 mm Hg, pulse is 90/min, and respirations are 16/min. Examination shows swelling, erythema, and tenderness in the region of the left parotid gland. Laboratory studies show a white blood cell count of 15,600/mm. Which of the following measures would most likely have prevented this complication?
Avoiding antibiotics
Polysaccharide vaccine
Tetanus toxoid
Adequate fluid intake and oral hygiene
Incentive spirometry
A 73-year-old woman is transferred to the hospital from the nursing home because of diverticulitis. A prior CT scan showed inflamed sigmoid colon. Transferred records indicate a 2 day history of fever and abdominal pain. On admission, her white count is 22,000/cmm, and she is started on IV antibiotics and IV fluids. Over the ensuing few days, her white count starts to come down and she has no nausea, vomiting or fever; however, she suddenly develops a cough and increasing abdominal pain. Abdominal examination shows guarding and tenderness in the left lower quadrant. An upright x-ray film of the chest shows free air under the left diaphragm. Which of the following is the most appropriate next step in management?
Colonoscopy
Laparotomy
Continue antibiotics and observe
Barium enema
CT scan of the abdomen
A 73-year-old woman with a long history of heavy smoking undergoes femoral artery-popliteal artery bypass for rest pain in her left leg. Because of serious underlying respiratory insufficiency, she continues to require ventilatory support for 4 days after her operation. As soon as her endotracheal tube is removed, she begins complaining of vague upper abdominal pain. She has daily fever spikes of 39°C (102.2°F) and a leukocyte count of 18,000/mL. An upper abdominal ultrasonogram reveals a dilated gallbladder, but no stones are seen. A presumptive diagnosis of acalculous cholecystitis is made. Which of the following is the next best step in her treatment?
Provocation of cholecystokinin release by cautious feeding of the patient
Endoscopic retrograde cholangiopancreatography (ERCP) to visualize and drain the common bile duct
Percutaneous drainage of the gallbladder
Immediate cholecystectomy with operative cholangiogram
Nasogastric suction and broad-spectrum antibiotics
A 74-year-old man residing in a nursing home develops symptoms of high fever, diarrhea, chest pain, and nonproductive cough. His temperature is 40°C, blood pressure 120/80 mm Hg, respiration 24/min, and oxygen saturation 90%. He has bibasilar crackles, normal heart sounds, and a soft nontender abdomen. His CXR reveals bilateral lower lobe infiltrates. He is not able to provide any sputum, and the urine is positive for legionella antigen. Which of the following is the most appropriate antibiotic choice?
Trimethoprim-sulfamethoxazole
Ceftriaxone
Cefuroxime
Gentamicin
Azithromycin
A 75-year-old man complains of headache. On one occasion he transiently lost vision in his right eye. He also complains of aching in the shoulders and neck. There are no focal neurologic findings. Carotid pulses are normal without bruits. Laboratory data show a mild anemia. Erythrocyte sedimentation rate (ESR) is 85. Which of the following is the best approach to management?
Start aspirin and defer any invasive studies unless further symptoms develop
Follow ESR and consider further studies if it remains elevated
Schedule carotid angiography
Schedule temporal artery biopsy and begin corticosteroids based on biopsy results and clinical course
Begin glucocorticoid therapy and arrange for temporal artery biopsy
A 75-year-old thin cachectic woman undergoes a tracheostomy for failure to wean from the ventilator. One week later, she develops significant bleeding from the tracheostomy. Which of the following would be an appropriate initial step in the management of this problem?
Upsize the tracheostomy
Perform fiberoptic evaluation immediately
Attempt to reintubate the patient with an endotracheal tube
Deflate the balloon cuff on the tracheostomy
Remove the tracheostomy and place pressure over the wound
A 75-year-old woman is brought to the emergency department after falling early in the morning. She is unable to move her right leg and has severe pain in her right hip. Her temperature is 36.9C (98.6F), blood pressure is 90/50 mm Hg, pulse is 100/min and respirations are 16/min. Examination shows the right lower extremity is shortened and is externally rotated with marked limitation of hip movement on the right side. An x-ray of the hip shows a markedly displaced fracture of the neck of the right femur. After hemodynamically stabilizing the patient, which of the following is the most appropriate step in management?
Internal fixation of the fracture
Closed treatment in a spica cast
Perform a primary arthroplasty
Lower limb skeletal traction
Closed reduction and external fixation
A 75-year-old woman with history of angina is admitted to the hospital for syncope. Examination of the patient reveals a systolic murmur best heard at the base of the heart that radiates into the carotid arteries. Electrocardiogram (ECG) is notable for left ventricular hypertrophy with evidence of left atrial enlargement. ECG reveals an aortic valve area of 0.7 cm2. What is the most appropriate next step in her management?
Coronary artery bypass surgery
Aortic valve replacement
Percutaneous coronary artery angioplasty and stenting
Bilateral carotid endarterectomies
Medical management with a nitrate and an angiotensin-converting enzyme inhibitor
{"name":"DES C_Management (11) Prepared : CHILLY", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 65-year-old female is admitted to the hospital with increasing shortness of breath, weight gain and lower extremity edema. She has a history of hypertension, nonischemic cardiomyopathy with an ejection fraction of 30%, and hyperlipidemia. Her home medications include oral aspirin, digoxin, furosemide, metoprolol, lisinopril and atorvastatin. She is started on intravenous furosemide. On day three of hospitalization telemetry reveals six beats of wide complex ventricular tachycardia. Physical examination now shows decreased leg edema and clear lungs. Which of the following is the most appropriate next step in the management of this patient's tachycardia?","img":"https://cdn.poll-maker.com/20-810064/image.jpeg?sz=1200"}
More Quizzes
Spellings
15823
Find your interior aesthetic with Hallmark Stone!
630
Welcome, welcome! :p This secret quiz is made for Jeremy Hwang; it will reveal a secret date plan IF and ONLY IF you get all the answers correct. Happy playing!
840
Identify the picture shown and choose the correct answer.
105133
5 oraciones simples y 10 de modo - Prueba 2 de gramática
201019764
ESG - Free Sustainability Knowledge Check
201020981
Months of the Year in Spanish - Free Practice
201028582
Potato Trivia Questions - Free With Answers
201026447
Free Basic Plus Test - Practice Questions & Answers
201022561
Types of Irony: Identify Dramatic, Situational, Verbal
201024137
Pokemon: Ultimate Trainer Challenge (Free)
201026233
Am I a Metalhead - Are You a True Headbanger?
201021603