(EXAM) Part 4 (765-865) (765-1019) NR 5
A 54-year-old male comes to the emergency department with complaints of cough and bloody sputum. He used to smoke 2 packs of cigarettes daily for 22 years, but states that he quit last month. He also complains of weight loss, anorexia, constipation, increased thirst, and easy fatigability, which he attributes to depression. He lost his wife 4 months ago and "life never felt the same after that." He is sure that he cannot have cancer because he does not smoke anymore. His vital signs are stable. He appears slim, pale, slightly irritable, and short of breath. The laboratory studies and chest x-ray results are as follows: Sodium 144 mEq/dL, Potassium 4.3 mEq/dL, Chloride 98 mEq/dL, Bicarbonate 21 mEq/dL, Calcium 14.5 mg/dl, BUN 48 mg/dl, Creatinine 2.0 mg/dl, Chest x-ray hilar mass in the left lung. While in the ED, he becomes more somnolent and vomits twice. What is the best next step in the management of this patient?
IV normal saline
IV furosemide
CT scan of the head
Emergency hemodialysis
IV pamidronate
A 75-year-old Caucasian male who was diagnosed with carcinoma of the prostate presents to ER with worsening back pain for the past 2-3 days. He never had this pain before. He denies any weakness of the legs. On examination, his muscle power in the lower extremities is 4.5/5 and has brisk reflexes. Rectal sphincter tone is weak. He has point tenderness over the L5 and S1 region. His vital signs are, BP: 122/80 mm Hg, PR 80/min, RR 16/min and Temperature 37°C (98°F). What is the most appropriate next step in management of this patient?
Intravenous dexamethasone
Radiotherapy
Immediate MRI of spine
Decompression surgery of spine
CT myelogram
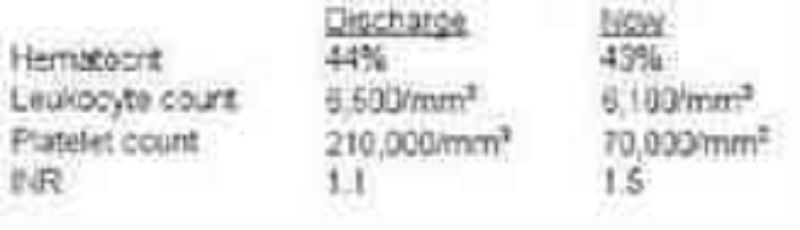
A 55-year-old woman complains of right leg swelling and tenderness following an international flight. A venous scan of the right lower extremity showed thrombosis of the right popliteal vein. She is sent home with oral warfarin and subcutaneous enoxaparin. One week later, she returns to the office for a follow-up appointment. Laboratory studies at the time of discharge and now are shown below: This patient's current condition predisposes her to which of the following?
Arterial thrombosis
Acute interstitial nephritis
Hemarthrosis
Pneumothorax
Fat embolism
A 22-year-old African American male suffering from sickle cell anemia presents in the emergency department with a sustained painful penile erection for the last 4 hours. Previously, he had one episode of acute chest syndrome that was treated with oxygenation, hydration and blood transfusion. His pulse is 76/min, respirations are 16/min, blood pressure is 115/76 mm Hg, and temperature is 37°C (98.6°F). Examination of all his systems is unrevealing. What is the best next step in the management of this patient?
Exchange transfusion
Observation
Hyperbaric oxygen therapy
Surgical intervention
Hydroxyurea
A 65-year-old man presents to the emergency department with a two-day history of fever, headache, altered mental status, and vomiting. His past medical history is significant for renal transplantation secondary to polycystic kidney disease, hypertension, and diabetes. He takes aspirin, insulin, nifedipine, cyclosporine, and prednisone. He has no known drug allergies. His temperature is 39.2°C (102.5°F), pulse is 102/min, respirations are 18/min, and blood pressure is 120/75 mm Hg. He is alert but confused. Fundoscopy does not show any abnormalities. His neck is stiff. Lungs are clear to auscultation. He has a normal S1 and S2 with a II/IV systolic ejection murmur heard best in the right infraclavicular area. Complete blood count shows a WBC count of 17,000/cm3 with neutrophilic leukocytosis. His blood is drawn and sent for culture. Lumbar puncture is performed and the results are pending. Which of the following is the most appropriate empiric antibiotic therapy for this patient?
Ceftriaxone, vancomycin, and ampicillin
Ceftriaxone
Ceftriaxone and vancomycin
Cefotaxime and ampicillin
Ceftazidime and vancomycin
A 7-year-old Caucasian boy with a history of cystic fibrosis presents to the emergency department with a two-day history of high-grade fever and cough productive of purulent, green-colored sputum. He also complains of chest pain, which is worsened by breathing. His temperature is 39.6°C (103.2°F), pulse is 112/min, respirations are 26/min, and blood pressure is 90/60 mm Hg. Chest examination shows dullness on percussion and increased tactile fremitus in the right lung base. Chest x-ray shows a right lower lobe infiltrate. Which of the following is the most appropriate pharmacotherapy for this patient?
Piperacillin and tobramycin
Ceftriaxone and gentamicin
Azithromycin
Piperacillin and ciprofloxacin
Dicloxacillin
A 28-year-old man presents to ER with fever, chills, and generalized weakness for the past one week. He has no history of pre-existing heart disease, but he was admitted to the hospital six months ago for cellulitis of the right arm. His temperature is 40.0°C (104°F), pulse is 110/min, respirations are 22/min, and blood pressure is 110/65 mmHg. Oropharynx is clear. Lungs are clear to auscultation. A holosystolic murmur is heard at the lower sternum which increases in intensity with inspiration. His blood is drawn and sent for culture. What is the most appropriate initial antibiotic therapy for this patient?
Vancomycin
Ampicillin-sulbactam
Clindamycin
Oxacillin
Penicillin G and gentamycin
A 45-year-old female presents to emergency room complaining of urinary frequency, burning during urination, and weakness. Her last menstrual period was one year ago, and she is not sexually active. She is not taking any medications. Her temperature is 37.8°C (100°F), blood pressure is 120/76 mmHg, pulse is 80/min, and respirations are 14/min. Very mild costovertebral angle tenderness is present. IV ceftriaxone is started. Two days later, the patient feels much better. Antibiotic susceptibility testing returned with an uropathogen (E.coli) highly sensitive to ceftriaxone, gentamicin, ciprofloxacin and trimethoprim/sulfamethoxazole (TMP/SMX). Which of the following is the most reasonable next step in the management of this patient?
Switch to TMP/SMX
Add ciprofloxacin to the regimen
Switch to gentamicin
Continue ceftriaxone
Discontinue antibiotic therapy
A 65-year-old man presents to the emergency department with a two-day history of fever, headache, altered mental status, and vomiting. His past medical history is significant for renal transplantation secondary to polycystic kidney disease, hypertension, and diabetes. He takes aspirin, insulin, nifedipine, cyclosporine, and prednisone. He has no known drug allergies. His temperature is 39.2°C (102.5°F), pulse is 102/min, respirations are 18/min, and blood pressure is 120/75 mm Hg. He is alert but confused. Fundoscopy does not show any abnormalities. His neck is stiff. Lungs are clear to auscultation. He has a normal S1 and S2 with a II/IV systolic ejection murmur heard best in the right infraclavicular area. Complete blood count shows a WBC count of 17,000/cm3 with neutrophilic leukocytosis. His blood is drawn and sent for culture. Lumbar puncture is performed and the results are pending. Which of the following is the most appropriate empiric antibiotic therapy for this patient?
Ceftriaxone, vancomycin. And ampicillin
Ceftriaxone
Ceftriaxone and vancomycin
Cefotaxime and ampicillin
Ceftazidime and vancomycin
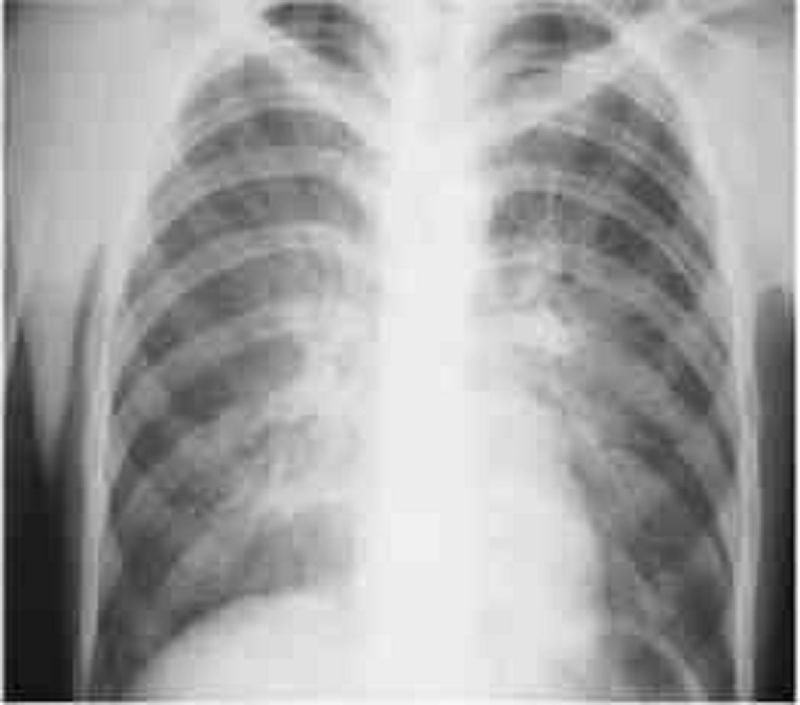
A 29-year-old male, known intravenous drug user presents to the emergency department with a chief complaint of dyspnea. Over the last few days, he has become short of breath and he has very little exercise tolerance. His other symptoms are a persistent dry cough, low-grade fever for the past two days, watery diarrhea, abdominal cramps, and general malaise. He self-treated his fever with acetaminophen. He has a history of anaphylaxis with sulfonamides. Physical examination reveals an emaciated man with numerous needle marks on his hands. Arterial blood gas analysis reveals a PCO2 of 32 mm Hg and PO2 of 64 mm Hg on room air. The chest x-ray is shown below. Which of the following is the most appropriate initial treatment regimen for this patient?
Pentamidine and azithromycin
Penicillin and acyclovir
Tetracycline and azithromycin
Acyclovir and azithromycin
Ganciclovir and azithromycin
A 54-year-old diabetic woman comes to the emergency department because of increasing neck and facial pain, fever, and chills. A few weeks ago, she developed an infection on the side of her neck. She thought it would go away with over-the-counter medication, but the infection has now started to drain. For the past twenty years, she has had diabetes, which is well-controlled with an oral hypoglycemic. She denies trauma, travel, and smoking. Physical examination reveals an area of erythema and induration at the base of the neck. Serosanguineous fluid is draining from a small defect in the skin near the center of the lesion. There is no crepitus. Histological analysis of the discharge reveals the presence of gram positive, branching bacteria. The treatment for this patient is?
Intravenous penicillin
Surgical debridement
Start triple combination TB therapy
Start amphotericin
Hyperbaric oxygenation
A 72-year-old man presents to the ED during the month of January complaining of non-productive cough, fever, malaise, runny nose, and severe body aches. The symptoms came on suddenly last night. He has no other medical problems. Physical examination reveals a temperature of 38.9°C (102.0°F) and oxygen saturation of 88% on room air. His lung exam reveals diffuse crackles with occasional wheezes. Laboratory values are: Hematocrit 44%, Platelets 219,000/mm3, Leukocyte count 4,100/mm3, Neutrophils 65%, Lymphocytes 32%. His chest x-ray reveals diffuse interstitial infiltrates bilaterally. What is the most appropriate initial therapy for this patient?
Oseltamivir
Ganciclovir
Tenofovir
Valacyclovir
Nevirapine
A 23-year-old man is brought to the emergency room because of confusion and hallucinations. While in ER, he has an episode of generalized tonic-clonic seizures. His past medical history is significant for illicit drug use. His temperature is 40.0°C (104.0°F), pulse is 95/min, and blood pressure is 120/80 mm Hg. He is confused and disoriented. Fundoscopy is with in normal limits. There is no neck stiffness. The neurological examination shows upgoing plantar reflexes bilaterally. Lumbar puncture is performed and CSF analysis shows the following: Glucose 35mg/dl, Protein 80mg/dl, WBC count 150/cm3, Neutrophils 10%, Lymphocytes 90%, Gram stain Negative. CT scan of the brain without contrast is normal. Which of the following is the most appropriate next step in the management of this patient?
Intravenous acyclovir
MRI of the brain
Intravenous ceftriaxone and vancomycin
CSF culture for herpes simplex virus
Urine toxicology screen
A 65-year-old female who lives in nursing home and is bed ridden due to severe right hemiparesis is brought to the ER because of altered mental status and decreased oral intake. Her past medical history includes hypertension, diabetes, hyperlipidemia, and myocardial infarction. She has a chronic indwelling Foley catheter to avoid contamination of a sacral decubitus ulcer. She is febrile in the ER. Examination shows dry mucus membranes and clear lungs. She is disoriented. The decubitus ulcer has good granulation tissue and does not appear infected. Labs show: Hemoglobin 12.0 g/L, Leukocyte count 12 500/mm3, Blood urea nitrogen (BUN) 28 mg/dL, Serum creatinine 0.8 mg/dL, Serum bicarbonate 24 mg/dL. Urinalysis: Specific gravity 1.036, Protein 1+, pH 8.5, Blood negative, Glucose 1+, Ketones negative, Leukocyte esterase positive, WBC 50-100/hpf, Bacteria few. Which of the following is the most likely cause of her altered mental status?
Urinary tract infection from Proteus species
Urinary tract infection from Escherichia coli
Urinary tract infection from Klebsiella species
Urinary tract infection from Pseudomonas aeruginosa
Urinary tract infection from Candida species
A 21-year-old man presents with symptoms of headache, fever, chills, and discomfort in both sides of his jaw. He has also noticed discomfort in his testes, but no dysuria or urethral discharge. Physical examination reveals bilateral enlargement of the parotid glands, as well as bilateral testicular enlargement and tenderness on palpation. His temperature is 38.5°C pulse rate of 92/min, and the remaining examination is normal. Laboratory data show hemoglobin 15 g/dL; hematocrit 40%; WBC 12000/mL, with 30% segmented neutrophils, 8% monocytes, and 62% lymphocytes. Which of the following statements concerning this dis- ease is true?
The most common complication of this disease in post pubertal boys and men is orchitis
The disease is caused by a herpesvirus
The incubation period is 3–5 days
Recurrent infections may occur
An increased serum amylase is proof of the existence of pancreatitis as a complication
An 8-year-old boy from an impoverished inner- city area has never been vaccinated appropriately. He develops fever, cough, and coryza. The next day, blue white spots develop on the buccal mucosa. On the third day, an erythematous, nonpruritic maculopapular rash develops on the face and spreads over the entire body. Which of the following is the most likely complication?
Otitis media
Pneumonia
Encephalitis
Bronchitis
Mastoiditis
A 6-year-old boy develops symptoms of cough, fever, and malaise followed by a generalized maculopapular rash that has spread from the head downwards. A clinical diagnosis of measles is made. A few days after the onset of the rash he is drowsy, lethargic, and complaining of headache. A lumbar puncture, electroencephalogram (EEG), and computerized tomography (CT) of the brain exclude other etiologies and confirm the diagnosis of encephalitis. Which of the following is the most likely delayed neurologic complication of measles virus encephalitis?
Mental retardation or epilepsy
Meningitis
Pure motor paralysis
Autonomic neuropathy
Stocking-glove peripheral neuropathy
A 24-year-old man complains of fatigue, malaise, fever, and a sore throat. He was previously well, but now feels tired all the time and has to rest multiple times a day. Physical examination shows enlarged tonsils and palpable anterior and posterior cervical, axillary, and inguinal lymph nodes. There is also tenderness in the right upper quadrant with a liver span of 10 cm. Laboratory data is significant for a heterophil antibody (sheep cell agglutination) test that is positive. Which of the following rare complications can be associated with this condition?
Splenic rupture
Retinitis
Esophagitis
Kaposi sarcoma
Hemorrhage
A 65-year-old male presents to the emergency department complaining of fever, chills, and a productive cough for the past 3 days. He also complains of right-sided chest pain and shortness of breath. He says that his chest pain worsens with deep breathing. The patient's past medical history is significant for diabetes and hyperlipidemia. He takes aspirin, simvastatin, metformin, glipizide and rosiglitazone. He does not use tobacco, alcohol or drugs. On physical exam, he has a temperature of 39.2°C (102.5°F), a blood pressure of 110/70 mm Hg, a pulse of 112/min, and respirations of 24/min. His mucus membranes are dry. Chest x-ray reveals a right lower lobe pneumonia. Laboratory studies show: Hemoglobin 17.0 g/L, Platelets 250,000/mm3, Leukocyte count 16,500/mm3, Serum sodium 140 mEq/L, Serum potassium 4.5 mEq/L, Blood urea nitrogen (BUN) 48 mg/dL, Serum creatinine 2.0 mg/dL, Serum calcium 10.3 mg/dL, Blood glucose 128 mg/dL. Blood cultures are obtained and antibiotics are administered. What is the appropriate next step in the management of this patient?
Discontinue metformin
Add lisinopril
Discontinue rosiglitazone
Discontinue glipizide
Begin bisphosphonate therapy
A 70-year-old woman is brought to the emergency department by her daughter because of altered mental status. She lives alone and is able to perform all daily activities. She experienced a minor febrile illness with decreased appetite several days ago, but has otherwise been in good health. She takes no medications. Her temperature is 37.2°C (99°F), blood pressure is 92/50 mm Hg, pulse is 100/min, and respirations are 18/min. Physical examination shows dry oral mucosa. Laboratory studies show: Hematocrit 45%, Serum sodium 147 mEq/L, Serum potassium 5.2 mEq/L, BUN 70 mg/dl, Serum creatinine 1.8 mg/dl. Which of the following is the most appropriate next step in management?
Intravenous crystalloids
Intravenous colloids
Order packed red blood cells
Intravenous antibiotics
Diuretics
A 45-year-old woman presents to the emergency department (ED) with vomiting and severe right flank pain that radiates to her groin. She has been to the ED twice in the past due to similar episodes of renal colic, and was subsequently discharged on both occasions. She admits to not seeking further medical care because she has no insurance. KUB shows a renal stone. 24-hour urine collection shows a urinary calcium excretion of 350 mg (normal is less than 250 mg in women). Laboratory studies show a serum calcium concentration of 8.9 mg/dL; serum PTH is normal. An x-ray film of the chest shows no abnormalities. Further investigations fail to reveal the cause of her hypercalciuria. Apart from advising her to increase her fluid intake, which of the following interventions will benefit this patient?
Thiazide diuretics
Restriction of calcium in her diet
Low dose furosemide
High sodium intake
Potassium citrate
A 65-year-old man is brought to the emergency department due to the sudden onset of weakness. He was lying on the floor for several hours before he was brought in. His other medical problems include hypertension, diabetes mellitus, coronary artery disease, transient ischemic attacks and osteoarthritis. CT scan of the head shows evidence of a right middle cerebral artery territory stroke. Laboratory studies show: Serum Na 137 mEq/L, Serum K 64 mEq/L, Chloride 104 mEq/L, Bicarbonate 18 mEq/L, BUN 36 mg/dl, Serum creatinine 3.0 mg/dl, Calcium 8.3 mg/dl, Blood glucose 178 mg/dl. His serum creatinine level one month ago was 1.4 mg/dl. EKG shows tall 'T' waves. CK level is pending. Which of the following is the most appropriate next step in management?
Calcium gluconate
Insulin with dextrose
Kayexalate
Sodium bicarbonate
Regular insulin
A 3-year-old girl is brought to the emergency department because of fever, chills, vomiting, and abdominal pain. Her temperature is 39.5°C (103.1°F), blood pressure is 70/40 mm Hg, pulse is 110/min, and respirations are 20/min. She is restless and diaphoretic. The abdominal examination shows right costovertebral tenderness. Laboratory studies show: Hemoglobin 15.0 g/L, Platelets 260,000/mm3, Leukocyte count 16,500/mm3, BUN 20 mg/dL, Serum creatinine 1.1 mg/dL. Urinalysis: Blood Negative, Glucose Negative, Ketones Negative, Leukocyte esterase Positive, Nitrites Positive, WBC 40-50/hpf, RBC 5-9/hpf. Blood and urine cultures are taken. Which of the following is the most appropriate next step in management?
Empiric therapy with intravenous antibiotics
Empiric therapy with oral antibiotics
Renal ultrasound
Voiding cystoureterogram
Plain abdominal x-ray
A 45-year-old man comes to the emergency department (ED) with severe right flank pain. He is tossing in bed due to the pain. KUB done in the ED shows no abnormalities; however, abdominal ultrasound shows a 5 mm stone in the right ureter. Urinalysis shows: Urine pH 4.5 (normal is 5-6), WBC Absent, RBC 2-3/HPF, Bacteria Absent, Nitrites Negative, Esterase Negative. Which of the following is the most beneficial next step in management?
Oral sodium bicarbonate
Hydrochlorothiazide
Furosemide
High-protein diet
Calcium-restricted diet
A 35-year-old man comes to the physician due to a one-month history of weight gain and facial edema. The facial edema resolves at the end of the day, but ankle edema develops. His temperature is 37.2°C (99°F), blood pressure is 142/80 mm Hg, pulse is 80/min, and respirations are 16/min. Examination shows 2+ ankle edema. Laboratory studies show: Hb 11.0 g/dl, WBC 8,000/cmm, Platelets 200,000/cmm, Serum Na 135 mEq/L, Serum albumin 2.2 g/dl, BUN 16 mg/dl, Serum creatinine 1.0 mg/dl. Urinalysis: Glucose Absent, Protein 4+, WBC 1-2/HPF, RBC Absent, Casts Fatty casts. This patient is most likely at risk for developing which of the following?
Hypercoagulability
Rupture of brain aneurysm
Abdominal aortic aneurysm
Pulmonary hemorrhage
Gall stone pancreatitis
A 73-year-old man presents to the emergency department complaining of lower abdominal pain and nausea. He denies any vomiting or diarrhea, and his last bowel movement was two days ago. The patient also notes that several days ago he began taking amitriptyline for chronic neck pain. He does not smoke or consume alcohol. On physical examination, his blood pressure is 160/70 mmHg and his heart rate is 100/min. His lung fields are clear to auscultation. Palpation of the abdomen reveals fullness and tenderness along the midline below the umbilicus. Which of the following is the best initial management for this patient?
Urinary catheterization
Abdominal CT scan
Upright abdominal x-ray
Barium enema
Broad spectrum antibiotics
A 34-year-old woman comes to the physician's office because of occasional headaches and palpitations. She has no other medical problems. She takes no medications. She smokes one and a half packs of cigarettes daily. Her blood pressure is 170/100 mm Hg in both arms, and heart rate is 80/min. Physical examination shows bilateral flank masses. Laboratory studies show: Serum sodium 140 mEq/L, Serum potassium 4.4 mEq/L, BUN 26 mg/dL, Serum creatinine 1.3 mg/dL. Urinalysis shows 10-12 red blood cells/hpf, but otherwise shows no abnormalities. The most likely complication that can occur in this patient is which of the following?
Intracranial aneurysms
Liver necrosis
Restrictive cardiomyopathy
Pancreatic cancer
Aortic dissection
A 47-year-old HIV-positive man is brought to the emergency room because of weakness. The patient has HIV nephropathy and adrenal insufficiency. He takes trimethoprim-sulfamethoxazole for PCP prophylaxis and is on triple-agent antiretroviral treatment. He was recently started on spironolactone for ascites due to alcoholic liver disease. Physical examination reveals normal vital signs, but his muscles are diffusely weak. Frequent extrasystoles are noted. He has mild ascites and 1+ peripheral edema. Laboratory studies show a serum creatinine of 2.5 with a potassium value of 7.3 mEq/L. An EKG shows peaking of the T waves and QRS duration of 0.14. What is the most important immediate treatment?
IV calcium gluconate
Sodium polystyrene sulfonate (Kayexalate)
Acute hemodialysis
IV normal saline
IV furosemide 80 mg stat
A 69-year-old man is brought to the ER by his family for increasing confusion. At baseline the patient is interactive and pleasant, but he has become withdrawn and confused over the last several months. He has also complained of abdominal pain, nausea, vomiting and back pain over the same period of time. His medical history is significant for diabetes controlled with metformin and hypertension treated with hydrochlorothiazide. Exam reveals normal vital signs and a disheveled, confused man. His neurologic exam is otherwise normal. Examination of the heart and lungs is unremarkable and no neck masses or nodes are appreciated. Laboratory results are given below: Sodium 139 mEq/L, Potassium 4.2 mEq/L, Chloride 111 mEq/L, Bicarbonate 26 mEq/L, Creatinine 1.4 mg/dl, Glucose 142 mgldl, Calcium 12.8 mEq/L, WBC 3,200/mm3, Hematocrit 32%, Platelets 47,000/mm3. What is the most appropriate next step for this patient?
0.9% saline infusion
Hemodialysis
Pamidronate
Calcitonin
Furosemide
A 38-year-old woman presents to the emergency department and complains of persistent vomiting that has increased in severity over the last week. Her other complaints are muscular weakness, twitching and cramps. Her urine output has decreased over the last 20 hours. Her past medical history is significant for a previously diagnosed prepyloric peptic ulcer. Her pulse is 100/min, blood pressure is 100/60 mmHg, respirations are 12/min, and temperature is 37.2°C (99°F). Physical examination reveals dry oral mucosa and decreased skin turgor. Abdominal examination reveals hypoactive bowel sounds and mild tenderness on palpation of the epigastrium. Nasogastric suction is started, and intravenous normal saline is given. Laboratory studies show: Serum sodium 135 mEq/L, Serum potassium 2.8 mEq/L, Chloride 81 mEq/L, Bicarbonate 40 mEq/L, Blood urea nitrogen (BUN) 42 mg/dl, Serum creatinine 1.3 mg/dl, Calcium 8.6 mg/dl, Ionized calcium 0.7 mmoi/L (1.1-1.3 mmoi/L), Serum pH 7.54. Which of the listed agents should be added to the patient's current therapy?
Potasium chloride
Ammonium chloride
Calcium chloride
Furosemide
Sodium bicarbonate
A 22-year-old man presents to the emergency department complaining of fever, nausea, vomiting, and right lower quadrant pain. He has no significant medical history and does not take any medications. He is a senior in college and denies cigarette smoking or drug use. He drinks alcohol occasionally. Physical examination reveals a temperature of 38.6°C, with all other vital signs within normal limits. ACT scan of his abdomen confirms acute appendicitis. Laboratory analyses reveal a leukocytosis but no electrolyte abnormalities. He is taken to the operating room and undergoes a successful laparoscopic appendectomy. Following the procedure, he is given intravenous fluids containing 5% dextrose in a 0.45% (½normal) saline solution at a rate of 150 ml/hr. The next morning the patient feels well but he then becomes progressively confused throughout the afternoon. You are called to his bedside after he has two grand mal seizures lasting 30 seconds apiece. Serum chemistries drawn at that time reveal a sodium concentration of 115mEq/L. What is the most appropriate therapy for this patient?
3% saline
Fosphenytoin
Normal saline
Phenobarbital
Lorazepam
A 71-year-old man with inclusion body myositis is brought to the emergency department from his nursing home after becoming less interactive. His temperature is 37.1°C, blood pressure is 90/60, heart rate is 98/min, and respiratory rate is 16/min. He has orthostatic vital signs. Physical examination reveals a frail man with dry oral mucosa and decreased axillary perspiration. Laboratory studies reveal the following: Sodium 164 mEq/L, Potassium 4.9 mEq/L, Bicarbonate 29 mEq/L, Chloride 122 mEq/L. What is the most appropriate next step in the management of this patient?
IV 0.9% saline
Oral free water
IV 5% dextrose in water
IV 5% dextrose in 04 5% saline
IV free water
A 55-year-old male is brought to the emergency department with a gunshot wound to his abdomen. He went to the operating room for repair of his injuries. On postoperative day 4, he develops a waxing and waning fever, tachypnea and shortness of breath. His temperature is 40°C (104°F), blood pressure is 90/60 mm Hg, pulse is 110/min and respirations are 22/min. Physical examination reveals an altered sensorium, crackles at the right lung base and a well healing abdominal wound. His urine output over the last 12 hours is 100ml. His laboratory profile shows: Blood pH 7.23, PaO2 60 mm Hg, PaCO2 32 mmHg, HCO3- 16 mEq/L. Broad-spectrum antibiotics are started. Which of the following additional treatments is most appropriate in this patient?
Intravenous 0.9% saline
Intravenous sodium bicarbonate
Intravenous Dextrose in water (D5W)
Intravenous 3% saline
Intravenous dopamine
A 34-year-old Mexican male comes to the emergency department and complains of severe episodic headache, especially at night, for the past month. He also complains of unilateral, sharp, stabbing pain in the eye, which wakes him from sleep. The pain often starts suddenly just behind the right eye, and spreads to his face and temple region. It is not associated with nausea or visual disturbances, but is associated with watering of the eyes and nose, and with red eye. He had a similar episode one year ago, and it lasted for 2 months. Which of the following is the best treatment regimen for aborting the patient's pain during an acute attack?
100 % oxygen
Oral NSAIDs
Verapamil
Nasal sumatriptan
Ergotamine
A 63-year-old man presents to the emergency department with a 6-hour history of slurred speech and right hand weakness. His past medical history is significant for chronic hypertension and a myocardial infarction 2 years ago. His current medications include enalapril and aspirin. He smokes 2 packs of cigarettes daily and consumes alcohol occasionally. His blood pressure is 165/95 mmHg, pulse is 80/min, and respirations are 14/min. Physical examination reveals right hand weakness and mild motor aphasia without sensory abnormalities Which of the following is the most probable cause of this patient's condition?
Hypertension
Large artery atherosclerosis
Cardiac embolus
Berry aneurysm
Arterial dissection
A 37-year-old white female with myasthenia gravis presents to the office with a fever and cough productive of yellow-green sputum. She has been on pyridostigmine for the past few months. She refuses to have a thymectomy. Her pulse is 90/min, blood pressure is 120/76 mm Hg, respirations are 18/min, and temperature is 38.9°C (102°F). Her respiratory effort is weak. Pulse oximetry reveals 86% oxygen saturation on room air. There is a consistent decline on serial measurement of vital capacity. Which of the following is the most appropriate next step in management?
Endotracheal intubation
Increase the dose of pyridostigmine
Treatment with edrophonium
Treatment with atropine
Treatment with prednisolone
A 36-year-old white female is brought to the emergency department due to paraplegia and bladder incontinence. She immediately tells you that she has, "multiple sclerosis in remission." She has a history of optic neuritis and internuclear ophthalmoplegia, and both resolved with treatment. At that time, MRI showed plaques in the periventricular region. She is currently not taking any medications. Which of the following is the most appropriate next step in the management of this patient?
Corticosteroids
Plasmapheresis
Interferon
Cyclophosphamide
Intravenous Immunoglobulins

A 64-year-old Caucasian female is rushed to the emergency department (ED) due to a sudden onset of severe headache and altered mental status. By the time she arrived at the ED, she had deteriorated to a stuporous state. She developed a fever and severe dry cough yesterday, but did not take any medicine nor consult her physician. Her medical problems include hypertension, coronary artery disease, atrial fibrillation, mitral valve regurgitation, and psoriasis. Her medications include aspirin, metoprolol, warfarin, amiodarone, and multivitamin tablets. Her blood pressure is 162/80 mm Hg, pulse is 80/min, respirations are 16/min and temperature is 37°C (98°F). Her lab results are: Hb 13 g/dl, WBC 11,000/cmm, Platelets 180,000/cmm, Blood Glucose 118 mg/dl, Serum Na 138 mEq/L, Serum K 4.5 mEq/L, BUN 16 mg/dl, Serum Creatinine 1.0 mg/dl, PT 25.0sec, INR 4.0. Which of the following is the most appropriate next step in management?
Give fresh frozen plasma
IV infusion of vitamin K
Order t-PA
Stop warfarin and start heparin
Obtain liver function panel
A 24-year-old male is brought to the emergency room after he fainted while practicing football on a bright sunny day. He complained of dizziness and headache before he collapsed. He was in his usual state of health until today and has no medical problems. He takes no medication. On arrival to the emergency room, his temperature is 41°C (105.8°F), blood pressure is 90/60 mm Hg, pulse is 140/min, and respirations are 22/min. He is not oriented. Skin is dry and hot. Neck is supple. Auscultation of the chest is unremarkable. Abdomen is soft and non-tender. Muscle tone and reflexes are within normal limits. Intravenous hydration is started. Which of the following is the most appropriate next step in management?
Evaporation cooling of the patient
Empirical antibiotic therapy
Gastric lavage with cold water
Immersion of the patient in cold water
High dose acetaminophen therapy
A 23-year-old male with a history of drug abuse is brought to the emergency department (ED) by an ambulance while having a tonic-clonic seizure. His mother soon arrives at the ED and says that she found him on the floor, where "he must have fallen." She says his seizure has lasted for more than 30 minutes now, and that he never regained consciousness since she found him. In the ED, he is unresponsive and cyanotic. He is biting his tongue and is incontinent. Despite resuscitation and administration of intravenous lorazepam, phenytoin, and glucose, the seizures continue. What is the best next step in the management of this patient?
Anesthesia with midazolam and intubation
Obtain CBC and electrolytes as soon as possible
Stat electroencephalogram (EEG)
Obtain CT scan of the head
Do a drug screen and attempt detoxification
A 27 -year-old white female comes to the office and complains of a headache for the last two weeks. She characterizes the headache as intermittent, "feels like a dull ache", 5/10 in severity, and associated with nausea and vomiting. She is afebrile and never had such a headache before. She has no visual complaints. She is a non-smoker and drinks alcohol only on weekends. Her only drugs are oral contraceptive pills (OCPs). Her menses are regular, and she has never conceived. She has no family history of similar problem. Her pulse is 80/min, temperature is 37.1°C, blood pressure is 120/75mmHg and respirations are 15/min. She is 5 feet 10 inches tall, and her weight is 210 lbs. The neurological examination is non-focal, and there are no signs of meningeal irritation. Funduscopy reveals papilledema. MRI of the brain is normal. Which of the following complications is likely to develop if this patient is left untreated?
Blindness
Seizures
Intracranial bleed
Paralysis
Urinary incontinence
A 64-year-old male is brought to the emergency department (ED) due to a sudden onset of lower extremity weakness. He was swimming in the pool, when he suddenly felt his legs become weak. He then felt that his legs had no more strength, and he was not able to move them. He struggled out of the pool, called EMS, and was rushed to the ED. He denies any trauma, loss of consciousness, visual or speech problems. He cannot pass urine. He has a long history of back problems. The physical examination reveals significant motor weakness in both legs, and numbness from the buttocks to the soles of the feet. He has no sensation in the perineal area. The rectal tone is absent. A Foley catheter is placed, and 800 cc of urine is collected. What is the best treatment for this patient?
Emergency surgery
CT head without contrast
Complete bed rest for 24 hours
Physiotherapy and NSAIDs
Nerve conduction studies
A 78-year-old woman is brought to the emergency department with agitation and insomnia. She screams out loudly and tries to run away while being examined. She is a nursing home resident and has a recent medical history that includes severe memory loss, gait disturbance and urinary incontinence. Her chronic medical issues include hypertension, diabetes mellitus, atrial fibrillation, peptic ulcer disease and chronic pyelonephritis. Her blood pressure is 160/100 mmHg and heart rate is 95/min and irregular. ECG reveals atrial fibrillation but no acute ischemic changes. Laboratory investigations reveal the following: Hematocrit 41%, WBC count 9,000/mm3, Platelets 160,000/mm3, Sodium 137 meq/L, Potassium 5.5 meq/L, Chloride 95 meq/L, Creatinine 1.4 mg/dl, BUN 25 mg/dl. Urinalysis shows trace protein, numerous leukocytes and occasional erythrocytes. Which of the following is the best initial treatment for this patient?
Haloperidol
Heparin
Aspirin
Lorazepam
Amitriptyline
A 79-year-old woman is brought to the emergency department due to a suspected cerebrovascular accident on her right side. She complains of diffuse paresthesias and tingling in her right hand. She did not lose consciousness. The physical examination reveals normal speech, symmetric deep tendon reflexes (2/4 on both upper extremities, 2/4 both patellar reflexes, and 0/4 both Achilles reflexes), a cold right hand, and undetectable arterial radial pulse. Tinel and Phalen's signs are negative. The rest of the examination is normal. What is the most appropriate next step in the management of this patient?
Immediate vascular surgery consultation for intervention
CT scan of the brain without contrast
MRI scan of the brain with diffusion images
Doppler of the carotid arteries
Schedule for EMG, and nerve conduction studies

A 34-year-old male presents to the emergency department with a red eye. He says, "I just woke up this morning and saw that my right eye was red." He denies any itching, pain or discharge. He has no known drug or environmental allergies. He takes no medication. His vital signs are stable. The photo of his eye is shown below. What is the best next step in his management?
Observation
Check intraocular pressure
Refer to ophthalmologist
Check coagulation parameters
Antibiotics
A 24-year-old woman presents to the emergency department (ED) complaining of right eye pain and blurry vision since waking up this morning. She states that the pain began after taking out contact lenses that were in her eyes for over 1 week. Her blood pressure (BP) is 120/75 mm Hg, heart rate (HR) is 75 beats per minute, temperature is 99.1°F, and respiratory rate (RR) is 16 breaths per minute. Her right and left eye visual acuity is 20/60 and 20/20, respectively. Her conjunctivae are injected. The slitlamp examination reveals a large area of fluorescein uptake over the visual axis. Which of the following is the most appropriate therapy?
Prescribe ciprofloxacin eye drops, oral analgesia, update tetanus prophylaxis, and arrange for ophthalmology follow-up
Call the ophthalmology consult for an emergent corneal transplant
Prescribe a systemic analgesic for pain control and advise the patient to not wear her contact lenses for the next week
Prescribe oral amoxicillin, a topical anesthetic, such as tetracaine, and have patient follow-up with an ophthalmologist
Prescribe ciprofloxacin eye drops and have patient strictly wear an eye patch until her pain resolves
A 60-year-old woman presents to the ED complaining of pain in her right eye and burning sensation over half of her forehead and scalp. On physical examination, you notice a patch of grouped vesicles on an erythematous base located in a dermatomal distribution on her scalp and forehead. There are also a few vesicles located at the tip of the patient’s nose. Her visual acuity is 20/20 bilaterally, heart is without murmurs, lungs are clear, abdomen is soft, and there are no gross findings on neurologic examination. Which of the following is the most concerning complication of this patient’s clinical presentation?
Ophthalmic involvement leading to anterior uveitis or corneal scarring
Central nervous system (CNS) involvement leading to meningitis
Cardiac involvement leading to endocarditis
Permanent scarring of her face
Nasopalatine involvement leading to epistaxis
A 24-year-old woman presents to the ED at 4 AM with severe left eye pain that woke her up from sleep. She wears soft contact lenses and does not routinely take them out to sleep. She is in severe pain and wearing sunglasses in the examination room. You give her a drop of proparacaine to treat her pain prior to your examination. On examination, her vision is at baseline and she has no afferent pupillary defect. There is some perilimbic conjunctival erythema. On fluorescein examination, a linear area on the left side of the cornea is highlighted when cobalt blue light is applied. No underlying white infiltrate is visualized. No white cells or flare are visualized in the anterior chamber. What is the most appropriate treatment for this condition?
Tobramycin ophthalmic ointment
Immediate ophthalmology consult
Erythromycin ophthalmic ointment
Eye patch
Proparacaine ophthalmic drops
A 45-year-old man lacerated his right forehead after an altercation in a local bar. Instead of seeking medical attention, the patient applied super glue to his wound. He successfully stopped the bleeding, but some of the glue got into his right eye and now he comes to the ED with difficulty opening his right eye. What is the most appropriate treatment of this patient?
Apply erythromycin ointment
Call ophthalmology immediately
Wash eye with acetone
Wash eye with normal saline
Use forceps to remove all the glue from the eye
A 12-year-old girl presents to the ED for left eye pain and swelling for 2 days. The patient has had cough, congestion, and rhinorrhea for the last week that is improving. On examination, her temperature is 100.8°F, HR 115 beats per minute, RR 12 breaths per minute, and BP 110/70 mm Hg. On eye examination, there is purple-red swelling of both upper and lower eyelids with injection of the conjunctiva. Pupils are equal and reactive to light. There is restricted lateral gaze. Visual acuity is 20/70 in the left eye and 20/25 in the right eye. The rest of the physical examination is normal. What is the most appropriate next step in management?
Administer vancomycin IV
Administer diphenhydramine
Administer amoxicillin/clavulanate
Perform computed tomographic (CT) scan of orbits and sinuses
Administer artificial tears
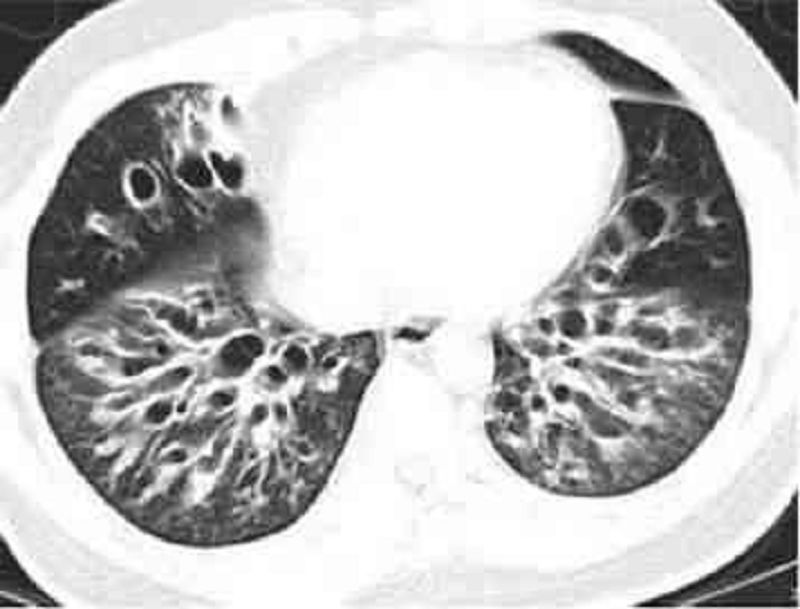
A 48-year-old male presents to the doctor with a history of persistent cough, tenacious mucopurulent sputum, and intermittent chills. He has been treated with several courses of antibiotics without resolution of his symptoms. On examination, he has an emaciated appearance and there is decreased air entry in the right lung base. His sputum has a foul smell. High resolution CT scan of the chest is shown below. Which of the following is the most feared complication of this patient's condition?
Hemoptysis
Pneumonia
Respiratory failure
Pneumothorax
Pulmonary embolism

A 67-year-old white male with a long history of bronchial asthma and chronic obstructive pulmonary disease (COPD) presents to the emergency room complaining of acute onset of shortness of breath for the last 30 minutes. He says that for the past 2 or 3 days he has been having some difficulty breathing and a productive cough with thick phlegm, but nothing as bad as the current episode. He also has a history of congestive heart failure after suffering a myocardial infarction for which he is taking furosemide and lisinopril. While talking to you in halting sentences, you note that he appears cyanotic, confused and are sweating profusely. He normally takes albuterol, ipratropium and budesonide inhalers for his breathing difficulties, but they have not relieved his current symptoms. On examination, he is found to be markedly dyspneic and his PaO2 is 55 mm Hg. A chest x-ray done in the ER is shown below. Which of the following is the most appropriate next step in the management of this patient?
Urgent bronchoscopy
Start intravenous theophylline
Urgent thoracocentesis
Place central venous line
Increase furosemide and start digoxin
A 32-year-old man presented to the emergency department five hours ago with an acute asthma exacerbation. He has been receiving continuous albuterol nebulizer treatments since that time. He has a 20-year history of asthma but notes that recently the frequency of his attacks has increased. Presently, his blood pressure is 110/70 mmHg and heart rate is 120 and regular. On physical exam, the patient appears drowsy. Breath sounds are diminished bilaterally but there are no wheezes. The most recent ABG reveals: pH 7.32, pO2 65mmHg, pCO2 50mmHg. Which of the following is the best next step in managing this patient?
Endotracheal intubation
Inhaled corticosteroids
Ipratropium inhalation
Intravenous theophylline
Oral prednisone
A 75-year-old man develops increased ventilatory requirements several days after requiring intubation for respiratory failure. X-ray of the chest shows bilateral infiltrates, and based on his ventilatory settings, the ratio of the partial arterial pressure of oxygen to the fraction of inspired oxygen (PaO2:FiO2) is 190. Which of the following is the most common underlying etiology of acute respiratory distress syndrome?
Sepsis
Aspiration of gastric contents
Drug overdose
Lung or bone marrow transplantation
Massive blood transfusion
A 25-year-old Caucasian woman presents as a new patient after having recently moved to the neighborhood. She says that she was diagnosed with anorexia nervosa two years ago, and that her disorder resolved after intensive psychotherapy. Although her eating pattern is normal now, she is still underweight. Her menstrual cycles have been regular for the past year. She recently married and is now interested in starting a family with her husband. She asks whether her history of anorexia nervosa will affect her ability to conceive or carry a healthy child to term. Given this clinical presentation, which of the following complications is most likely?
Small for gestational age baby
Congenital anomalies
Macrosomia
Infertility
Postpartum psychosis
A 22-year-old woman is seen in the emergency room after a suicide attempt. She swallowed 10 aspirin in the presence of her mother, with whom she had just had an argument. The patient has a long history of cutting herself superficially with razor blades, which her psychiatrist of the last 5 years confirms by telephone. The patient currently lives in a stable environment (a halfway house) where she has been for 3 years. Which of the following option is the best course of action for the physician in the emergency room?
Discharge the patient back to outpatient therapy and the halfway house
Admit the patient involuntarily
Admit the patient voluntarily
Admit the patient to a medical floor
Discharge the patient to outpatient therapy after meeting with the patient’s mother
A 62-year-old Caucasian female complains of frequent headaches, fatigue and recent weight loss. Her shoulder muscles feel stiff in the morning. Her ESR is 85 mm/hr. Which of the following will be the most likely complication of this patient's condition?
Aortic aneurysm
Chronic lymphocytic leukemia
Hypothyroidism
Ulcerative colitis
Membranous glomerulonephritis
A 40-year-old female presents to the emergency room with palpitations and lightheadedness of acute onset. Also, she has experienced insomnia, fatigability, and weight loss lately. She does not smoke or consume alcohol. She is not taking any medication. Her blood pressure is 110/80 mmHg and heat rate is 120/min, irregular. Physical examination reveals lid lag and fine tremor of the outstretched hands. ECG shows atrial fibrillation with rapid ventricular response. What is the next best step in the management of this patient?
Propranolol
Digoxin
Lidocaine
Quinidine
Immediate cardioversion
A 43-year-old Caucasian man with a two-year history of diabetes mellitus presents to your office for a routine. He has no complaint His medications are metformin and aspirin. He works as a computer programmer and has a sedentary lifestyle. He drinks one to two cans of beer on weekends and smokes one pack of cigarettes per day. On physical examination, his blood pressure is 153/94 mmHg and his heat rate is 82/min. His BMI is 32.5 kg/m2. The remainder of the physical examination is unremarkable. Laboratory studies reveal an HbA1c of 7.6%. At his check-up one month ago, his blood pressure was 149/92 mmHg. Which of the following interventions would be most effective for controlling his blood pressure?
Weight loss
Aerobic exercise
Smoking cessation
Better diabetes control
Quitting alcohol
A 60-year-old male is 2 days status post primary percutaneous coronary intervention (PCI) with stent placement. He had previously suffered from an antero-lateral myocardial infarction. His cardiac enzymes have been trending down since admission. He has recovered well and is ready for discharge. He is currently asymptomatic. His temperature is 37.5°C (99.5°F), blood pressure is 130/70 mmHg, pulse is 66/min, and respirations are 14/min He is discharged with instructions to take the following medications aspirin simvastatin, lisinopril metoprolol and sublingual nitroglycerine. In addition to the medications listed above, which of the following medications should this patient also be taking after discharge?
Clopidogrel
Isosorbide mononitrate
Low molecular weight heparin
Waffarin
Amlodipine
A 22-year-old Caucasian male is evaluated for an episode of syncope that occurred while playing soccer. It lasted only 2 minutes without any post-syncopal confusion, sleepiness or weakness. He had prior episodes of dizziness while playing active sports as well as vague chest discomfort. His uncle died suddenly at a young age. Auscultation of his precordium reveals a III/IV systolic murmur along the left sternal border. The patient is most likely to benefit from which of the following medications?
Beta-blockers
Nitrates
Disopyramide
Amlodipine
Digitalis
A 40-year-old male presents with six months of worsening dyspnea. His symptoms have progressed to the point that walking even one block causes him to become shot of breath. He has a history of cigarette smoking, but quit 10 years ago. He drinks approximately one alcoholic drink daily. His medical history is significant for peptic ulcer disease for which he takes antacids. On physical examination, he is afebrile. His pulse is 86/min, blood pressure is 140/56 mmHg, and respiratory rate is 14/min. While examining his heat you note a high-pitched blowing, early diastolic, decrescendo murmur, which is heard best in the left third intercostal space and is intensified by handgrip. There is prominent cardiomegaly on chest x-ray. Which of the following medications would improve both this patient’s symptoms and cardiomegaly?
Nifedipine
Quinidine
Metoprolol
Ephedrine
Amiodarone

A 67-year-old male presents to the ER with chest pain. His medical history is significant for stable angina for which he takes aspirin and isosorbide dinitrate, as well as hypertension and bronchial asthma. Occasionally, he uses an albuterol inhaler. He is admitted to the hospital and five hours later, he begins to feel lightheaded and weak. His blood pressure is 100/60 mmHg. An EKG is obtained and is shown below. Which of the following is the best next step in managing this patient?
Pacemaker insertion
Cardiac catheterization
Adenosine
Digoxin
Metoprolol
A 43-year-old white male is found to have premature atrial complexes (PACs) on routine EKG. He denies chest pain, shortness of breath or lightheadedness. He has smoked 1-2 packs of cigarettes daily for the past 20 years. He also has a 20-year history of alcoholism, though recently he has limited his use to 1-2 beers/day. The patient's family history is significant for a myocardial infarction in his mother at age 65 and a stroke in his father at age 72. He has no personal history of hypertension or diabetes. Physical examination including vital signs, is entirely within normal limits. What is the best next step in the management of this patient?
Advise him to stop alcohol and tobacco
Reassurance
24-hour Halter monitoring
Echocardiogram
Start beta-blocker therapy
A 60-year-old man is brought to the emergency department due to syncope. He has had similar episodes a few times during the past few weeks. These episodes usually occur after he exerts himself. He does not feel confused or tired after these episodes. He denies any chest pain or palpitation. His wife reports that when he collapses, he seems to lose consciousness for a few seconds, but then is back to being alert right away. She denies any jerking movement. His past medical history is significant diverticulosis, for which he takes fiber supplements. He is not on any other medication. His temperature is 37.1°C (98.8°F), blood pressure is 110/98 mm Hg, pulse is 88/min, and respirations are 14/min. On examination, he has a fourth heart sound and harsh 3/6 systolic murmur, best heard over the right sternal border. The murmur is accentuated on expiration. The lung fields are clear to auscultation. After performing an echocardiograph to confirm the diagnosis, which of the following management options is most appropriate?
Aortic valve replacement
Aortic valvotomy
Close outpatient follow-up with serial echocardiograms
Exercise test looking for arrhythmias
Observe until the patient develops breathlessness

A 59-year-old male suffers a myocardial infarction. He is treated medically and is discharged home ten days later on aspirin, atorvastatin, metoprolol, lisinopril, and sublingual nitroglycerin. One month later, he presents to your office for a follow-up visit. He denies chest pain, dyspnea or lightheadedness. His blood pressure is 120/75 mmHg. His EKG is pictured below. Echocardiogram reveals an ejection fraction of 45%. What is the best next step in his management?
Observation
Amiodarone
Digoxin
DC cardioversion
Verapamil

Diuretics, vasodilators and oxygen are standard inpatient therapy for patients hospitalized with left-sided heart failure. When patients are discharged, a different outpatient regimen is instituted. A team of researchers compares long-term cardiovascular mortality between patients treated with two different outpatient regimens. The study results are depicted below. In comparison to the patients depicted by the dashed curve, those depicted by the solid line most likely received treatment with which of the following?
ACE inhibitor
Calcium channel blocker
Loop diuretic
Digoxin
Dobutamine
A 57-year-old female with a past medical history of bronchial asthma presents to the physician's office for evaluation of high blood pressure. On her previous two visits, her blood pressure has been 154/88 mmHg and 150/90 mmHg. Her blood pressure during this visit is 150/90 mmHg. She denies headaches and has no complaints. She uses fluticasone and albuterol inhalers for her chronic persistent asthma. She denies smoking or alcohol intake, and has no known drug allergies. Her family history is significant for myocardial infarction in both her mother and father. Exercise and a low salt diet have not improved her hypertension. Which of the following is the most appropriate next step in managing this patient's hypertension?
Prescribe hydrochlorothiazide
Discontinue asthma medications
Prescribe propranolol
Prescribe enalapril
Obtain an echocardiogram
A 27-year-old female presents to your office for a follow-up. The previous two visits revealed an elevated blood pressure in the range of 150- 155/90-95 mmHg. She has no present complaints. Her past medical history is insignificant. She smokes 1/2 pack of cigarettes per day and does not consume alcohol. Her current medications include a combination oral contraceptive for the last 2 years, and an occasional acetaminophen for tension headache relief. There is no family history of hypertension or heart attacks. This visit, her blood pressure is 155/95 and her heart rate is 80/min. The physical examination is unremarkable. The ECG is normal. Her total cholesterol level, measured 6 months ago, was 170 mg/dL. Which of the following is the most appropriate next step in the management of this patient?
Discontinuation of the oral contraceptive
Lifestyle modification
Low-dose thiazide diuretic
Intravenous pyelography
No intervention at this point
A 65-year-old male presents to the emergency department with substernal chest pain, severe shortness of breath, and diaphoresis that began suddenly 40 minutes ago. Since the pain started, the patient has vomited twice. The pain radiates to his left arm and does not remit with sublingual nitroglycerine. EKG shows 2 mm ST elevations in the anterior leads. On physical examination, the patient's temperature is 36.9°C (98.4°F), blood pressure is 110/70 mmHg, pulse is 60/min, respirations are 32/min, and oxygen saturation is 90% on 4L oxygen by nasal canula. Cardiac exam reveals a muffled S1 and S2 and the presence of an S3. Lung exam reveals basilar crackles that extend halfway up the lung fields bilaterally. Which of the following is the best next step in managing this patient?
Furosemide
Metoprolol
Digoxin
Spironolactone
IV fluids
A 55-year-old male with a history of rheumatoid arthritis and rheumatoid lung disease is admitted to the hospital with palpitations. His restrictive lung disease is of moderate severity, requiring use of 2 liters of oxygen by nasal cannula at all times. He has no known history of coronary artery disease, hypertension or diabetes. On physical examination, his blood pressure is 110/70 mmHg and heart rate is 120 and irregular. EKG shows atrial fibrillation with a rapid ventricular rate. Which of the following medications should be avoided in this patient?
Amiodarone
Verapamil
Digoxin
Quinidine
Metoprolol
A 32-year-old anxious-appearing male is wheeled into the emergency room with the sudden onset of excruciating left-sided chest pain. His temperature is 37.2°C (99°F), blood pressure is 160/88 mmHg, pulse is 125/min, regular and respirations are 20/min. Physical examination is normal, except for multiple venous track marks on his extremities and atrophic nasal mucosa. An EKG is done which shows ST depression and T wave inversion in leads V1-V6. Cardiac enzymes including CK-MB and Troponin Tare not elevated. Which of the following is the most appropriate next step in the management of this patient?
Intravenous diazepam
Cardiac catheterization
Administer metoprolol
Administer thrombolytics
Close observation
A 66-year-old white male presents for evaluation of progressively worsening dyspnea that affects him at rest and wakes him from sleep. He also notes bilateral ankle swelling. His medical history is significant for coronary artery disease for which he has undergone angioplasty and coronary artery bypass grafting. On examination today, his pulse is 86/min, blood pressure is 110/70 mmHg, and respirations are 19/min. His neck veins are distended and there is bilaterally symmetric pitting ankle edema. On chest auscultation, you hear crackles at the bilateral lung bases and a third heart sound. Chest x-ray shows an enlarged cardiac silhouette and bilateral alveolar and interstitial pulmonary edema. Of the medications listed below, which has not been shown to improve survival in patients with the above presentation?
Digoxin
Captopril
Losartan
Metoprolol
Aspirin
A 26-year-old primigravida at 20th week gestation presents to the emergency room with a sudden onset of tearing chest pain radiating to her back and left arm. The patient is pale and diaphoretic. Her PR: 116/min; BP: 192/ 104 mmHg in left arm, and 123/65 mmHg in right arm; RR: 36/min. Her cardiac examination reveals a diastolic murmur along the left sternal border. Her previous prenatal care is not known. She is a smoker with a 10 pack/year history and drinks alcohol. Her ECG reveals mild left axis deviation and ST segment depression in lead II, III, and AVF. What is the most appropriate next step in the management of this patient?
Antihypertensive treatment
Obtain CK-MB and Troponin levels
Transesophageal echocardiogram (TEE)
Transthoracic echocardiogram (TTE)
CT scan of chest
A 53-year-old woman presents to the physician's office with a 3-week history of burning, substernal chest pain that usually comes on with exertion and is relieved with rest. The pain does not radiate to the arms or jaw. Her past medical history is significant for bronchial asthma, type 2 diabetes, hypercholesterolemia, and hypertension. A diagnosis of stable angina is suspected, and the patient is scheduled for an exercise EKG stress test. Which of her medications should be withheld 24 hours before the test?
Atenolol
Hydrochlorothiazide
Simvastatin
Ramipril
Metformin
A 50-year-old Caucasian male returns to the clinic for the evaluation of his blood pressure control. He was diagnosed with essential hypertension one year ago. He claims compliance with his reduced salt intake diet. He is currently on a thiazide diuretic and a beta-blocker. His past medical history is significant for angina, which is always relieved with sublingual nitroglycerine, but he has not had an attack of angina in over a month. He has never had a myocardial infarction. He lives with his wife and two children. He quit smoking two years ago, but previously had a 25-pack year history. He drinks 4 bottles of wine per week. His blood pressure is 150/90 mm Hg. What is the best next step in management?
Reduction in alcohol intake
Admit him to the hospital to control his blood pressure
Start an ACE inhibitor
Increase the dose of thiazide diuretic
Reassurance and repeat measurement in 2 weeks
A 34-year-old woman is referred by an OB-GYN colleague for the onset of fatigue and dyspnea on exertion 1 month after her second vaginal delivery. Physical examination reveals a laterally displaced PMI, elevated jugular venous pressure and 2+ pitting lower extremity edema. Echocardiogram shows systolic dysfunction with an ejection fraction of 30%. Which statement most accurately describes her condition?
About half of similar patients will recover completely
This disease may occur unexpectedly years after pregnancy and delivery
The condition is idiosyncratic; the risk of recurrence with a future pregnancy is no greater than average
This condition will require a different therapeutic approach than the typical dilated cardiomyopathy
This condition will require endomyocardial biopsy for diagnosis
A 72-year-old Caucasian male presents with shortness of breath that awakens him at night. At baseline he is able to walk less than a block before stopping to catch his breath. Physical examination findings include bilateral basilar rales and neck vein distention. The patient has a known history of congestive heart failure, and his last echocardiogram revealed an ejection fraction of 25%. The patient is compliant with a medication regimen including an ACE inhibitor, beta-blocker, and loop diuretic. Blood pressure is well controlled. What additional treatment should you begin next?
Spironolactone
Aspirin
Amlodipine
Warfarin
Hydralazine and isosorbide dinitrate
A 30-year-old female presents with a chief complaint of palpitations. A 24-hour Holter monitor shows occasional unifocal premature ventricular contractions and premature atrial contractions. Which of the following is the best management for this patient?
Reassurance, no medication
Anxiolytic therapy
Beta-blocker therapy
Digoxin
Quinidine
A 52-year-old man complains of frequent chest pain. The pain typically occurs at night and is described as retrosternal and burning in quality. He leads a sedentary lifestyle but does not smoke or drink alcohol. His past medical history includes a chronic cough and occasional hoarseness. He does not take any medications. His BMI is 28.5 kg/m2 ECG stress testing reveals 1 mm ST segment depression in the inferior leads at 90% of predicted maximal heart rate. He did not experience chest pain during the stress test. Which of the following is most likely to relieve this patient's chest pain?
Omeprazole
Ibuprofen
Nitroglycerin
Propranolol
Alprazolam
A 54-year-old woman presents for a routine physical. She has no complaints. She has no history of hypertension, diabetes, hypercholesterolemia, or heart disease, and she does not use tobacco, alcohol or drugs. On physical examination, her pulse is irregular. There are no murmurs. Her lungs are clear to auscultation and her legs are free of edema. An EKG shows atrial fibrillation with a heart rate of 72 beats per minute. An echocardiogram is unremarkable except for evidence of atrial fibrillation. What is the most appropriate management of this patient?
Aspirin alone
Warfarin and clopidogrel
Heparin followed by warfarin
Low-molecular weight heparin
Warfarin to maintain an INR of 2 to 3
A middle-aged man was recently diagnosed with hypertension. The antihypertensive medication prescribed to him enhances natriuresis, decreases serum angiotensin II concentration, and decreases aldosterone production. This medication most likely belongs to which of the following drug classes?
Direct renin inhibitor
Angiotensin receptor blocker
Aldosterone receptor antagonist
Loop diuretic
Alpha-adrenergic blocker
A 63-year-old woman complains of leg swelling that is especially bothersome in the evening. She also complains of chronic cough and exertional dyspnea. She has been smoking one pack of cigarettes per day for the past 30 years. She also drinks one or two cans of beer on weekends. Her medical history is significant for a hospitalization for a "chest infection" two years ago, for which she was treated with antibiotics, steroids, and inhalers. She also reports having been diagnosed with hypertension, but says that she has never taken medications for it. On physical examination, her blood pressure is 160/90 mmHg and her heart rate is 80/min. Chest examination reveals bilateral scattered wheezes and prolonged expirations. Her jugular venous pulsation is seen 2 cm above the sternal angle with the head of the bed elevated 30°. Her abdomen is soft and non-distended. On examination of her lower extremities, you note bilateral pitting edema and dilated, tortuous, superficial veins. Which of the following is most likely to relieve this patient's edema?
Frequent leg elevation
Smoking cessation
Dietary sodium restriction
Control of hypertension
Oxygen therapy
A 68-year-old man presents to the emergency department complaining of left lower extremity pain. He says that he first noticed a tingling sensation in his leg 3 hours ago, and since that time it has become increasingly painful. Over the past hour, he says, the skin on his leg has started to change color. His medical history is significant for hypertension, diabetes mellitus, atrial fibrillation, and major depressive disorder. He cannot remember his medication list at this time. On physical examination, his blood pressure is 127/74 mmHg and his heart rate is 102/min. His left lower extremity is cool and pale below the level of the knee. Neither the posterior tibial nor the dorsalis pedis pulse is palpable. Which medication could have prevented this acute problem?
Warfarin
Aspirin
Metoprolol
Clopidogrel
Diltiazem
A 64-year-old male presents to the ER with chest pain. His history is significant for a hospitalization 2 weeks ago for an acute myocardial infarction. The patient reports that he is afraid his heart attack is recurring. He localizes the pain to the middle of the chest, and says that he can only take shallow breaths because deep breaths make the pain worse. Leaning forward in his chair makes the pain somewhat better. He notes some associated neck pain and general malaise, but denies shortness of breath, palpitations, syncope or cough. His temperature is 36.7°C (98°F), blood pressure is 135/84 mmHg and heart rate is 90/min. EKG shows ST segment elevations in all limb and precordial leads except in aVR, where ST depression is seen. Which of the following is the best next step in the management of this patient?
Non-steroidal antiinflammatory agent
Anticoagulation with heparin
Anticoagulation with warfarin
Nitroglycerin and beta-blockers
Broad-spectrum antibiotics
A 15-year-old female, who has recently emigrated from Asia, is found to have a heart murmur during her routine physical examination. She has no current complaints. She had a febrile illness with joint swelling and pain approximately one year ago. She plays table tennis and swims every weekend. Her blood pressure is 120/70 mmHg and her heart rate is 70/min, regular. Cardiac auscultation shows a loud first heart sound and mid-diastolic rumble at the apex. Her lungs are clear to auscultation. Which of the following is the best treatment for this patient at this point?
Penicillin
Metoprolol
Enalapril
Digoxin
Warfarin
A 54-year-old male with a past medical history of type 2 diabetes mellitus comes to the emergency department complaining of shortness of breath. His blood pressure is 146/92 mmHg, respiratory rate is 26/min, and oxygen saturation is 87% on room air. Cardiac auscultation findings over the apex are given below. Based on the physical findings, which of the following is the best initial therapy for this patient?
Intravenous diuretics
Inhaled bronchodilators
Intravenous beta-blockers
Intravenous diltiazem
Pericardiocentesis
A 65-year-old female is admitted to the hospital with increasing shortness of breath, weight gain and lower extremity edema. She has a history of hypertension, nonischemic cardiomyopathy with an ejection fraction of 30%, and hyperlipidemia. Her home medications include oral aspirin, digoxin, furosemide, metoprolol, lisinopril and atorvastatin. She is started on intravenous furosemide. On day three of hospitalization telemetry reveals six beats of wide complex ventricular tachycardia. Physical examination now shows decreased leg edema and clear lungs. Which of the following is the most appropriate next step in the management of this patient's tachycardia?
Measure serum electrolytes
Add spironolactone
Add metolazone
Discontinue atorvastatin
Discontinue metoprolol
A 34-year-old male presents with palpitations for the past 4 hours without associated chest pain, shortness of breath, fevers, or chills. His medical history is significant for Wolff-Parkinson-White syndrome for the past ten years and three prior episodes of supraventricular tachycardia. He does not smoke cigarettes, and drinks alcohol on social occasions. He does report having had five cans of beer while at a party last night. On examination, his blood pressure is 120/80 mmHg and his pulse is irregularly irregular. EKG shows atrial fibrillation with a rate of 160/min. What is the best next step in the management of this patient?
Procainamide
Digoxin
Verapamil
Lidocaine
Adenosine
A 45-year-old male presents to your clinic with complaints of pleuritic chest pain. He says he is a heavy smoker and has been having intermittent cough for the past 2 weeks. His blood work is normal and his chest x ray is clear. EKG reveals a normal sinus rhythm with a heart rate of 68. He does have a PR interval > 0.2 seconds. The next step in the management of his arrhythmia is:
Observation
Atenolol
Pacemaker
Electrophysiology study
Cardiac catheterization
A 53-year-old Caucasian woman comes to the physician for a routine health maintenance examination. Recently, she noticed a mild hand tremor while performing some fine tasks, like pouring out the tea. She says that the tremor disappears for a while after drinking a glass of wine. Her past medical history is insignificant. Her blood pressure is 160/90 mmHg and heart rate is 80/min. Physical examination is insignificant. Which of the following medications is the best choice to treat this patient's hypertension?
Propranolol
Verapamil
Amlodipine
Hydrochlorothiazide
Enalapril
A 34-year-old male with a history of mitral valve prolapse and mitral regurgitation presents with one week of intermittent fevers and increasing fatigue. He was punched in the face during a street fight two weeks ago. On admission he receives empiric intravenous vancomycin and gentamicin. Three days later, three out of four blood cultures grow Streptococcus viridans highly sensitive to penicillin. Which of the following is the best next step in managing this patient?
Switch antibiotics to IV ceftriaxone
Continue current regimen
Switch antibiotics to IV aminoglycosides
Switch antibiotics to oral penicillin V
Switch antibiotics to oral amoxicillin/clavulanate
A 10-year-old boy is brought to the ER by his mother because he has lost consciousness, while playing in the yard. He regained his consciousness quickly without following confusion. He never had such an episode before. His past medical history is significant for impaired hearing since birth and one episode of pneumonia three years ago, which required hospitalization. The family history is significant for a sudden cardiac death, in his cousin, at the age of 13. Physical examination is unremarkable. Blood pressure is 110/70 mmHg. Heart rate is 70/min, regular. Which of the following medication is most appropriate for this patient?
Propranolol
Verapamil
Quinidine
Ethosuximide
Phenobarbital
A 76-year-old man presents to your office with progressively worsening fatigue over the past several months. He denies associated chest pain, dyspnea, nausea, cough, or ankle swelling. He has smoked a pack of cigarettes per day for the past 30 years. His past medical history is significant for hypertension for which he takes hydrochlorothiazide and type 2 diabetes mellitus controlled with metformin. He had a medical check-up five months ago which did not uncover any new abnormalities or medical issues. On physical examination today, his blood pressure is 130/80 mmHg and his heart rate is 110 and irregularly irregular. His lab values are: Hematocrit 41%, WBC count 4,700/mm3, Platelets 200,000/mm3, Sodium 137 mEq/L, Potassium 4.1 mEq/L, Creatinine 0.8 mg/dl, Fasting glucose 85 mg/dl. Which of the following is the best treatment for this patient?
Warfarin
Captopril
Salmeterol
Amlodipine
Spironolactone
A 37-year-old healthy Caucasian male is seen in your office for a routine physical examination. He denies any symptoms or illness. He says he smokes a pack a day and drinks one to two beers every weekend. He has no allergies. Examination is unremarkable. The EKG reveals normal sinus rhythm with a heart rate of 72; there are frequent premature atrial beats present. The blood pressure is 120/65mm Hg. The next step in his management is:
Observation
Digoxin
Lidocaine
Order potassium levels
Complete electrophysiological study
A 56-year-old white male presents with dyspnea for the last 3 months. His dyspnea was initially exertional but it has worsened progressively and now he is breathless even at rest. He denies any chest pain or ankle swelling. He has been smoking one-pack/day cigarettes for the last 30 years and has been drinking alcohol heavily for the last 10 years. He is not taking any medication. His mother died of breast cancer at 57. His vitals are, PR 86/min, BP 113/76mmHg; Temperature 37.1°C (98.9°F); RR 13/min. On auscultation of his precordium an S3 is heard, but there are no murmurs. Chest auscultation reveals bilateral basal crepitations. Chest x-ray shows marked cardiac silhouette enlargement and pulmonary venous congestion. EKG shows non-specific ST-T wave changes. Echocardiography shows a dilated left ventricle and systolic dysfunction (EF of 25-30%). CBC shows hematocrit of 32%, WBC count of 6,000/microl, and platelet count of 60,000/microl. Peripheral blood smear shows MCV of 101 fl. LFTs show AST of 180U/L and AL T of 66 U/L. The findings of cardiac catheterization and coronary angiography are not compatible with the diagnosis of ischemic cardiomyopathy. Which of the following measures is most likely to reverse his heart failure?
Abstinence from alcohol
Cessation of cigarette smoking
Reduced salt intake
Use of ACE inhibitors
Use of digoxin
A 55-year-old Caucasian male presents to your office for a routine check-up. His past medical history is significant for gout, hypertension, and hypercholesterolemia. His current medications include enalapril and pravastatin. He does not smoke or consume alcohol. His blood pressure is 156/94 mmHg and heart rate is 80/min. Physical examination reveals that the patient is moderately overweight (BMI = 27 kg/m2) with increased waist-to-hip ratio. You consider adding hydrochlorothiazide to the treatment regimen to improve the control of hypertension. Which of the following metabolic effects do you expect to emerge after this correction?
Hyperglycemia
Hypocalcemia
Hyperkalemia
Decreased LDL cholesterol
Decreased plasma triglycerides
An imaging study detects a 3.5 cm abdominal aortic aneurysm in a 60-year-old male. He has no associated symptoms. His past medical history is significant for hypertension, type 2 diabetes, hypercholesterolemia and hypothyroidism. His medications include aspirin, metformin, glipizide, hydrochlorothiazide, lisinopril, low dose atorvastatin and levothyroxine. He has smoked 1-2 packs of cigarettes daily for the past 40 years, and he drinks 1-2 glasses of wine daily. On physical examination, his blood pressure is 160/90 mmHg and his pulse is 80/min. Heart sounds are normal and his lungs are clear. Laboratory studies show: Serum creatinine 1.7 mg/dL, Low density lipoprotein (LDL) 150 mg/dL, HbA1C 8.5%, Serum TSH 3.0. Which of the following interventions would most reduce the likelihood of his aortic aneurysm enlarging?
Smoking cessation
Better control of hypertension
Better control of hypercholesterolemia
Better control of diabetes
Alcohol cessation

A 72-year-old male is admitted to the hospital with chest pain. EKG and cardiac enzymes confirm a myocardial infarction and he is started on nitroglycerine, aspirin, simvastatin and low molecular weight heparin. Four days later, he complains of leg pain. Physical examination reveals a cold, pale leg. The angiogram is shown below. What is the best next step in his management?
Embolectomy
Intravenous streptokinase
Clopidogrel
Cilosta zol
Leg elevation and warm compress
A 62-year-old man visits his family physician because of generalized aches and pains. He denies associated fevers, headaches, chest pain, or abdominal discomfort. His past medical history is significant for an inferior wall myocardial infarction 6 years ago. His other medical problems include hypertension, diabetes, hypercholesterolemia, and gout. His current medications are aspirin, losartan, naproxen, atenolol, glipizide, colchicine, and simvastatin. On physical exam today, he is afebrile, with blood pressure 130/90 mmHg, pulse 80/min and respirations 18/min. Lab results are as follows: Sodium 140 mEq/L, Potassium 4.2 mEq/L, Bicarbonate 21 mEq/L, Chloride 100 mEq/l, BUN 30 mg/dl, Creatinine 1.6 mg/dl, AST 113 IU/L, ALT 120 IU/L, Creatine phosphokinase 14,998 mg/dl. What is the most appropriate next step in the management of this patient?
Stop simvastatin
Stop losartan
Start N-acetylcysteine
Order hepatitis panel
Obtain liver biopsy
{"name":"(EXAM) Part 4 (765-865) (765-1019) NR 5", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 54-year-old male comes to the emergency department with complaints of cough and bloody sputum. He used to smoke 2 packs of cigarettes daily for 22 years, but states that he quit last month. He also complains of weight loss, anorexia, constipation, increased thirst, and easy fatigability, which he attributes to depression. He lost his wife 4 months ago and \"life never felt the same after that.\" He is sure that he cannot have cancer because he does not smoke anymore. His vital signs are stable. He appears slim, pale, slightly irritable, and short of breath. The laboratory studies and chest x-ray results are as follows: Sodium 144 mEq\/dL, Potassium 4.3 mEq\/dL, Chloride 98 mEq\/dL, Bicarbonate 21 mEq\/dL, Calcium 14.5 mg\/dl, BUN 48 mg\/dl, Creatinine 2.0 mg\/dl, Chest x-ray hilar mass in the left lung. While in the ED, he becomes more somnolent and vomits twice. What is the best next step in the management of this patient?, A 75-year-old Caucasian male who was diagnosed with carcinoma of the prostate presents to ER with worsening back pain for the past 2-3 days. He never had this pain before. He denies any weakness of the legs. On examination, his muscle power in the lower extremities is 4.5\/5 and has brisk reflexes. Rectal sphincter tone is weak. He has point tenderness over the L5 and S1 region. His vital signs are, BP: 122\/80 mm Hg, PR 80\/min, RR 16\/min and Temperature 37°C (98°F). What is the most appropriate next step in management of this patient?, A 55-year-old woman complains of right leg swelling and tenderness following an international flight. A venous scan of the right lower extremity showed thrombosis of the right popliteal vein. She is sent home with oral warfarin and subcutaneous enoxaparin. One week later, she returns to the office for a follow-up appointment. Laboratory studies at the time of discharge and now are shown below: This patient's current condition predisposes her to which of the following?","img":"https://cdn.poll-maker.com/10-472575/1.jpg?sz=1200"}
More Quizzes
Movie quizzes
10525
Booking an Appointment with a Virtualist
7425
Employee Nominated GOAT Awards
10514
Which Limeade Enemy Are You?
11618
Asexual Reproduction in Plants: Test Your Skills
201023607
Think You Know Fergie With Lyrics? Prove It Now!
201024602
That Was Then, This Is Now Book: Test Your Knowledge
201028348
What's Your Chronotype? Take Our Free Chronotype Now
201025252
Free Commercial Vehicle History
201023797
Ultimate Insect Trivia: Challenge Your Bug IQ
201023797
Define a Testable Question: Scientific Method
201042032
Rhetorical Devices: Test Your Rhetoric Skills
201023607