Cardiology part2(101-200)ronaldo
101. A 54-year-old woman presents for a routine physical. She has no complaints. She has no history of hypertension, diabetes, hypercholesterolemia, or heart disease, and she does not use tobacco, alcohol or drugs. On physical examination, her pulse is irregular. There are no murmurs. Her lungs are clear to auscultation and her legs are free of edema. An EKG shows atrial fibrillation with a heart rate of 72 beats per minute. An echocardiogram is unremarkable except for evidence of atrial fibrillation. What is the most appropriate management of this patient?
D. Aspirin alone
A. Warfarin and clopidogrel
B. Heparin followed by warfarin
C. Low-molecular weight heparin
E. Warfarin to maintain an INR of 2 to 3
102. A middle-aged man was recently diagnosed with hypertension. The antihypertensive medication prescribed to him enhances natriuresis, decreases serum angiotensin II concentration, and decreases aldosterone production. This medication most likely belongs to which of the following drug classes?
B. Direct renin inhibitor
A. Angiotensin receptor blocker
C. Aldosterone receptor antagonist
D. Loop diuretic
E. Alpha-adrenergic blocker
103. A 63-year-old woman complains of leg swelling that is especially bothersome in the evening. She also complains of chronic cough and exertional dyspnea. She has been smoking one pack of cigarettes per day for the past 30 years. She also drinks one or two cans of beer on weekends. Her medical history is significant for a hospitalization for a "chest infection" two years ago, for which she was treated with antibiotics, steroids, and inhalers. She also reports having been diagnosed with hypertension, but says that she has never taken medications for it. On physical examination, her blood pressure is 160/90 mmHg and her heart rate is 80/min. Chest examination reveals bilateral scattered wheezes and prolonged expirations. Her jugular venous pulsation is seen 2 cm above the sternal angle with the head of the bed elevated 30•. Her abdomen is soft and non-distended. On examination of her lower extremities, you note bilateral pitting edema and dilated, tortuous, superficial veins. Which of the following is most likely to relieve this patient's edema?
B. Frequent leg elevation
A. Smoking cessation
C. Dietary sodium restriction
D. Control of hypertension
E. Oxygen therapy
104. A 32-year-old man develops severe nausea and vomiting after returning from a party. He also complains of chest pain that is more intense than any pain he has previously experienced. His past medical history is significant for HIV infection, alcohol abuse, and alcoholic hepatitis. He admits to using cocaine regularly. His temperature is 37.8C (100.F), pulse is 120/min, respirations are 24/min, and blood pressure is 100/60 mmHg. Examination reveals injected conjunctivae and bilateral dilated pupils. Chest X-ray demonstrates a widened mediastinum and left-sided pleural effusion. EKG is unremarkable. The pleural fluid is found to have an elevated amylase content. Which of the following is the most likely diagnosis in this patient?
C. Esophageal perforation
A. Acute pancreatitis
B. Peptic ulcer disease
D. Myocardial ischemia
E. Pulmonary embolism
105. A 45-year-old male is brought to the ER with sudden onset palpitations and chest tightness. His past medical history is significant for hypertension, gout and diabetes mellitus. Cardiac monitoring shows atrial fibrillation at a rate of 120-140/min. As the nurse is attempting to establish IV access, the patient becomes unresponsive. There is no palpable pulse over the carotids or femoral arteries. The cardiac monitor still shows atrial fibrillation at the same rate. What is the best next step in management?
D. Chest compressions
A. Synchronized cardioversion
B. Defibrillation
C.IV lidocaine
E. Arterial blood gas analysis
106. A 24-year-old male experiences syncope while shoveling snow. He regained consciousness within one minute. He has been having some shortness of breath and chest pains recently, mostly related to exercise. He denies any illicit drug use. His temperature is 37.2 C (98.9 F), and blood pressure is 126/76 mm Hg, pulse is 76/min and respirations are 14/min. Physical examination shows a well-built male in no apparent distress. Lungs are clear. A crescendo-decrescendo systolic murmur is heard along the left sternal border without carotid radiation. Chest X-ray is normal. Which of the following is the most likely cause of his syncopal episode?
B. Left ventricular hypertrophy
A. Atrioventricular conduction delay
C. Aortic dissection
D. Coronary atherosclerosis
E. Mitral valve degeneration
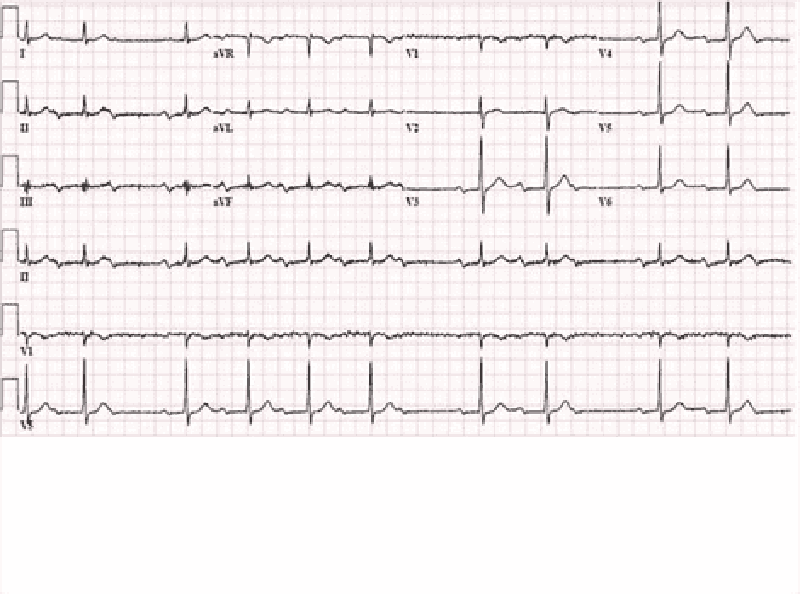
107. A 56-year-old diabetic female comes to the clinic with complaints of dizziness which has been going on for 3 weeks. She denies any dyspnea or diaphoresis. She says her blood glucose is well controlled and denies any allergy. Her BP is 155/90 mm Hg. Her chest-x ray is unremarkable and her blood work is normal. The ECG is recorded below. What is the most likely diagnosis?
A Mobitz type I heart block
B. Mobitz type II heart block
C. Complete heart block
D. Atrial fibrillation
E. First degree heart block
108. A 54-year-old overweight man wakes up in the middle of the night with substernal discomfort that he describes as a burning sensation. He also complains of left-sided neck pain and feels sweaty and short of breath. He has never had similar pain before. Prior to going to bed he had eaten a big meal. His past medical history is significant for diabetes and hypertension. Which of the following physical findings is most consistent with this patient's clinical presentation?
D. Fourth heart sound
A Fixed splitting of S2
B. Ejection-type systolic murmur
C. Friction rub
E. Pulsus paradoxus
109. A 56-year-old male is hospitalized following an acute anterior wall myocardial infarction that was treated with thrombolytic therapy 4 days ago. On day 4 of his hospitalization, he develops recurrent chest pain, similar in quality and severity to his previous pain. Sublingual nitroglycerin is administered but does not help. His blood pressure is now 140/90 mmHg and his heart rate is 82/min. S 1 and S2 are normal, and there are no cardiac murmurs or rubs. Lungs are clear to auscultation. Which of the following laboratory tests would be most useful to send in this setting?
C. CK-MB
A Troponin T
B. Lactate dehydrogenase (LDH)
D. Alkaline phosphatase
E. Dobutamin
110. A 64-year-old male presents to the emergency department with chest pain. An ECG reveals ST elevations in leads II, Ill, and aVF. Thrombolytic therapy and heparin are administered, and the pain resolves. Eight hours after admission, the patient develops hypotension. He denies recurrence of chest pain. His temperature is 37.5°c (99.6.F), blood pressure is 84/55 mm Hg, pulse is 90/min, and respirations are 15/min. His medications include a nitroglycerin drip, beta-blocker, aspirin, heparin, and simvastatin. Examination reveals an elevated jugular venous pressure of 14 cm, cold clammy extremities, and clear lung fields. Based on this information, what is the next best step in this patient's management?
B. Administer normal saline bolus and stop nitroglycerin
A. Start dopamine
C. Administer intravenous furosemide
D. Initiate temporary cardiac pacing
E. Stop nitroglycerin and start dobutamine drip
111. A 33-year-old woman is undergoing an elective, open cholecystectomy after 2 episodes of acute calculous cholecystitis. She suddenly becomes hypotensive, and a generalized rash is noted. Her past medical history is significant for a hypotensive episode 8 weeks ago while having protected sex with her new partner. Which of the following is the most probable cause of this patient's condition?
C. Allergic reaction
A. Acute blood loss
B. Coagulation abnormality
D. Septic shock
E. Pulmonary embolism
112. A 68-year-old man presents to the emergency department complaining of left lower extremity pain. He says that he first noticed a tingling sensation in his leg 3 hours ago, and since that time it has become increasingly painful. Over the past hour, he says, the skin on his leg has started to change color. His medical history is significant for hypertension, diabetes mellitus, atrial fibrillation, and major depressive disorder. He cannot remember his medication list at this time. On physical examination, his blood pressure is 127/74 mm Hg and his heart rate is 102/min. His left lower extremity is cool and pale below the level of the knee. Neither the posterior tibial nor the dorsalis pedis pulse is palpable. Which medication could have prevented this acute problem?
D. Warfarin
A. Aspirin
B. Metoprolol
C. Clopidogrel
E. Diltiazem
113. A 75-year-old patient presents to the ER after a syncopal episode. He is again alert and in retrospect describes occasional substernal chest pressure and shortness of breath on exertion. His blood pressure is 110/80 and lungs have a few bibasilar rales. Which auscultatory finding would best explain his findings?
A. A harsh systolic crescendo-decrescendo murmur heard best at the upper right sternal border
B. A diastolic decrescendo murmur heard at the mid-left sternal border
C. A holosystolic murmur heard best at the apex
D. A midsystolic click
E. A pericardial rub
114. A 72-year-old male comes to the office with intermittent symptoms of dyspnea on exertion, palpitations, and cough occasionally productive of blood. On cardiac auscultation, a low-pitched diastolic rumbling murmur is faintly heard at the apex. What is the most likely cause of the murmur?
A. Rheumatic fever as a youth
B. Long-standing hypertension
C. A silent MI within the past year
D. A congenital anomaly
E. Anemia from chronic blood loss
115. You are helping with school sports physicals and see a 16-year-old boy who has had trouble keeping up with his peers. Which of the following auscultatory findings suggests a previously undiagnosed ventricular septal defect?
C. A holosystolic murmur at the mid-left sternal border
A. A systolic crescendo-decrescendo murmur heard best at the upper right sternal border with radiation to the carotids; the murmur is augmented with exercise.
B. A systolic murmur at the pulmonic area and a diastolic rumble along the left sternal border
D. A diastolic decrescendo murmur at the mid-left sternal border
E. A continuous murmur through systole and diastole at the upper left sternal border
116. A 53-year-old male presents to your office with a two-day history of right calf pain and swelling. He describes the pain as constant and states that it is exacerbated by knee flexion. He has a history of past IV drug abuse, endocarditis, and stroke. He is currently wheelchair-bound secondary to stroke-related left-sided hemiparesis. On physical examination, his blood pressure is 140/90 mmHg and his heart rate is 100/min. There is no jugular venous distention or hepatojugular reflux. His chest is clear to auscultation but his abdomen is enlarged with shifting dullness and a fluid wave, suggestive of ascites. His liver is palpable 3 cm below the right costal margin. His spleen is also palpable. On examination of his lower extremities, you note right-sided calf swelling and tenderness. Which of the following is the most likely cause of this patient's ascites?
D. Chronic liver disease
A. Right-sided heart failure
B. Pulmonary embolism
C. Protein C deficiency
E. Paradoxical embolism
117. A 46-year-old man comes to the ER because of weakness and chest tightness. He has had these symptoms for the past one hour. He denies any past medical history. He does not smoke or drink alcohol. His father had a myocardial infarction at 68 years of age and his mother has myasthenia gravis. His EKG is shown on the slide below. The patient should be evaluated for which of the following?
B. Hyperthyroidism
A. Cushing syndrome
C. Aortic dissection
D. High-frequency deafness
E. High-range proteinuria
118. A 64-year-old male presents to the ER with chest pain. His history is significant for a hospitalization 2 weeks ago for an acute myocardial infarction. The patient reports that he is afraid his heart attack is recurring. He localizes the pain to the middle of the chest, and says that he can only take shallow breaths because deep breaths make the pain worse. Leaning forward in his chair makes the pain somewhat better. He notes some associated neck pain and general malaise, but denies shortness of breath, palpitations, syncope or cough. His temperature is 36.7C (98.F), blood pressure is 135/84 mmHg and heart rate is 90/min. EKG shows ST segment elevations in all limb and precordial leads except in aVR, where ST depression is seen. Which of the following is the best next step in the management of this patient?
E. Non-steroidal antiinflammatory agent
A. Anticoagulation with heparin
B. Anticoagulation with warfarin
C. Nitroglycerin and beta-blockers
D. Broad-spectrum antibiotics
119. A 15-year-old female, who has recently emigrated from Asia, is found to have a heart murmur during her routine physical examination. She has no current complaints. She had a febrile illness with joint swelling and pain approximately one year ago. She plays table tennis and swims every weekend. Her blood pressure is 120/70 mmHg and her heart rate is 70/min, regular. Cardiac auscultation shows a loud first heart sound and mid-diastolic rumble at the apex. Her lungs are clear to auscultation. Which of the following is the best treatment for this patient at this point?
A. Penicillin
B. Metoprolol
C. Enalapril
D. Digoxin
E. Warfarin
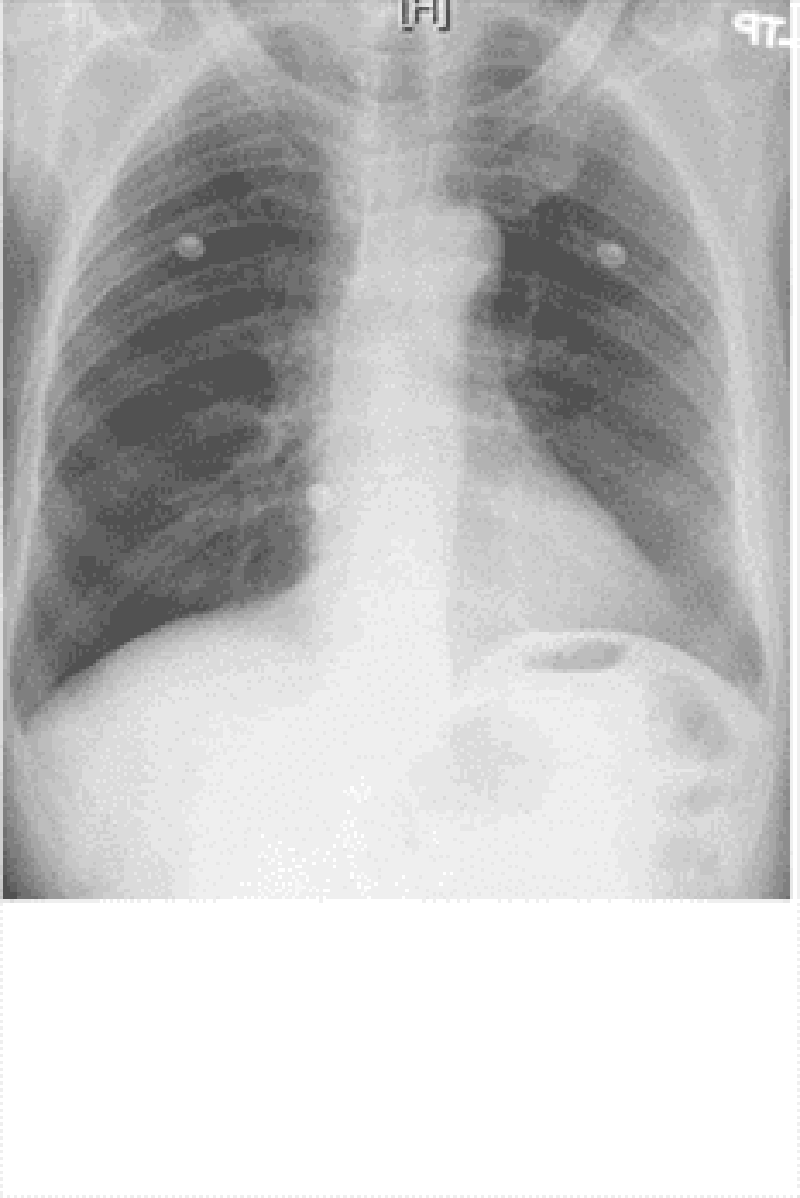
120. A 46-year-old man presents to the emergency department with difficulty breathing and chest discomfort. His pain worsens with inspiration but does not radiate. He says that he has never had symptoms like this before. His past medical history is unremarkable. He works as a long-haul truck driver. On physical examination, his blood pressure is 110/70 mmHg, his heart rate is 110/min, his respiratory rate is 31/min, and his temperature is 36.7C (98.F). ECG reveals sinus tachycardia but no ischemic ST-segment or T-wave changes. His chest X-ray is shown below. What is the most likely diagnosis in this patient?
D. Pulmonary embolism
A. Ascending aortic dissection
B. Myocardial infarction
C. Pneumothorax
E. Pleural effusion
121. A 60-year-old white man comes into the Emergency Room with intensive retrosternal pain that began ten minutes ago. He has never had such pain before. His past medical history is significant for diabetes mellitus, type 2, controlled with diet His blood pressure is 150/95 mmHg and HR is 80/min. You give him one chewable tablet of aspirin and two sublingual tablets of nitroglycerin with a 5-minute interval. After the second tablet of nitroglycerin, the pain is greatly relieved. What is the most important mechanism responsible for pain relief in this patient?
D. Dilation of capacitance vessels
A. Increase in coronary blood flow
B. Increased cardiac contractility
C. Dilation of resistance vessels
E. Change in the activity of baroreceptors
122. A 34-year-old male who recently immigrated from Brazil presents with a 5-month history of exertional dyspnea without associated chest pain, palpitations, dizziness, or syncope. His past medical history is significant for an episode of megacolon, which was treated 2 years ago. On physical examination, there is 1+ pedal edema and mild jugular venous distention. Cardiac exam is significant for the presence of an S3, but no murmurs are heard. Chest x-ray reveals prominent cardiomegaly. Based on these findings, which of the following is most likely causing his symptoms?
C. Protozoal disease
A Diphtheric myocarditis
B. Coronary artery disease
D. Giant cell myocarditis
E. Rickettsial myocarditis
123. A 54-year-old male with a past medical history of type 2 diabetes mellitus comes to the emergency department complaining of shortness of breath. His blood pressure is 146/92 mmHg, respiratory rate is 26/min, and oxygen saturation is 87% on room air. Cardiac auscultation findings over the apex are given below. Based on the physical findings, which of the following is the best initial therapy for this patient?
D. Intravenous diuretics
A. Inhaled bronchodilators
B. Intravenous beta-blockers
C. Intravenous diltiazem
E. Pericardiocentesis
124. Neighbors find a 65-year-old male unconscious in his garden and immediately call EMS. The man is intubated at the scene. In the ER, he develops sustained ventricular tachycardia and requires cardioversion. He is started on an antiarrhythmic agent and, once recovered, is discharged to home. Three months later he returns to his physician complaining of dyspnea on exertion. Chest-x ray reveals bilateral lung fibrosis. All cultures are negative and lung biopsy reveals lipoid pneumonitis. Which of the following medications is most likely responsible for his current condition?
B. Amiodarone
A. Procainamide
C. Lidocaine
D. Quinidine
E. Digoxin
125. A 12-year-old African American male is found to have a murmur during a routine sports physical. He has a family history of sudden death at a young age. It is a harsh crescendo-decrescendo murmur that begins after S1 and is best heard at the left lower sternal border. Valsalva maneuver intensifies the murmur. Which of the following is the most likely mitral valve abnormality in this patient?
C. Abnormal mitral leaflet motion
A. Dilated mitral valve annulus
B. Rupture of chordae tendinae
D. Mitral annulus calcifications
E. Prolapse of the mitral valve
126. A 36-year-old female presents to the emergency room complaining of chest pain that started suddenly while she was shopping at the mall. She also reports shortness of breath, palpitations and diaphoresis. The pain is retrosternal and radiates to the left arm. There are no aggravating or relieving factors. On review of systems, the patient reports having had a runny nose, sore throat and dry cough for the past 3 days. Her past medical history is significant for panic attacks, for which she takes paroxetine, and dysfunctional uterine bleeding, for which she takes estrogen. Her family history is significant for the sudden death of her father at age 44 from a heart attack. Social history reveals that she has smoked one pack of cigarettes per day for the past 15 years. Which of the following is the most appropriate initial therapy for this patient?
C Aspirin
A. Lorazepam
B. Heparin
D. Ibuprofen
E. Acetaminophen
127. A 65-year-old female is admitted to the hospital with increasing shortness of breath, weight gain and lower extremity edema. She has a history of hypertension, nonischemic cardiomyopathy with an ejection fraction of 30%, and hyperlipidemia. Her home medications include oral aspirin, digoxin, furosemide, metoprolol, lisinopril and atorvastatin. She is started on intravenous furosemide. On day three of hospitalization telemetry reveals six beats of wide complex ventricular tachycardia. Physical examination now shows decreased leg edema and clear lungs. Which of the following is the most appropriate next step in the management of this patient's tachycardia?
C. Measure serum electrolytes
A. Add spironolactone
B. Add metolazone
D. Discontinue atorvastatin
E. Discontinue metoprolol
128. A 34-year-old male presents with palpitations for the past 4 hours without associated chest pain, shortness of breath, fevers, or chills. His medical history is significant for Wolff-Parkinson-White syndrome for the past ten years and three prior episodes of supraventricular tachycardia. He does not smoke cigarettes, and drinks alcohol on social occasions. He does report having had five cans of beer while at a party last night. On examination, his blood pressure is 120/80 mmHg and his pulse is irregularly irregular. EKG shows atrial fibrillation with a rate of 160/min. What is the best next step in the management of this patient?
D. Procainamide
A Digoxin
B. Verapamil
C. Lidocaine
E. Adenosine
129. A 45-year-old male presents to your clinic with complaints of pleuritic chest pain. He says he is a heavy smoker and has been having intermittent cough for the past 2 weeks. His blood work is normal and his chest x ray is clear. EKG reveals a normal sinus rhythm with a heart rate of 68. He does have a PR interval > 0.2 seconds. The next step in the management of his arrhythmia is:
A. Observation
B. Atenolol
C. Pacemaker
D. Electrophysiology study
E. Cardiac catheterization
130. A 21-year-old man comes to the ER with palpitations and dizziness that began suddenly one hour ago. He notes having similar past episodes provoked by fatigue or strong emotions. He says he can usually stop the episodes by putting his head into cold water or squatting and taking a deep breath. However, these techniques are not working this time. Presently, his blood pressure is 60/30 mmHg and his heart rate is 240/min. He is diaphoretic with cold extremities. An EKG rhythm strip shows a regular, narrow complex tachycardia. Which of the following is the best next step in managing his condition?
E. DC cardioversion
A. Adenosine
B. Procainamide
C. Verapamil
D. Digoxin
131. A 64-year-old Caucasian male presents to the Emergency Room with a sharp, left-sided chest pain. He says that the pain is worse when he takes deep breaths, but he gets relief with leaning forward. He had an acute non-ST elevation myocardial infarction six months ago and had undergone angioplasty for the right coronary artery. His other medical problems include: diabetes, hypertension, hyperlipidemia, peripheral neuropathy, diabetic retinopathy, paroxysmal atrial fibrillation, hypothyroidism, and chronic renal insufficiency. His vital signs are BP 142/86 mmHg, PR 78/min, RR 16/min, and T 36.1 C (97F). On examination, you find a pericardial rub. EKG shows diffuse ST elevation. Lab results are: Hb 9.0 g/dl WBC 8,000/cmm Platelets 210,000/cmm Blood Glucose 248 mg/dl Serum Na 135 mEq/L Serum K 5.8 mEq/L Bicarbonate 17 mEq/L BUN 86 mg/dl Serum Creatinine 4.4 mg/dl Which of the following is the most appropriate management of this patient?
D. Hemodialysis
A. NSAIDs
B. Corticosteroids
C. Pericardiocentesis
E. Echocardiography
132. A 63-year-old woman with a long history of hypertension faints after experiencing the sudden onset of severe chest pain that radiates to her back. She is rushed to the emergency room. Upon arrival she is agitated and demands quick pain relief. Her heart rate is 110/min and blood pressure is 90/50 mmHg. Jugular veins are distended. An intraarterial catheter shows significant variation of systolic blood pressure related to the respiratory cycle. Chest x-ray reveals widening of the mediastinum. Which of the following is the most likely cause of this patient's syncope?
C. Pericardia! Fluid accumulation
A. Papillary muscle dysfunction
B. Intravascular volume loss
D. Vagal hyperactivity
E. Cardiac tachyarrhythmia
133. A 32-year-old woman is brought to the emergency department with excruciating chest and neck pain. She is 6'2" and has long extremities. Her hand joints show significant extensibility. Which of the following additional findings is also likely in this patient?
B. Early diastolic murmur
A Fourth heart sound
C. Opening snap
D. Fixed splitting of the second heart sound (S2)
E. Kussmaul's sign
134. A 53-year-old Caucasian woman comes to the physician for a routine health maintenance examination. Recently, she noticed a mild hand tremor while performing some fine tasks, like pouring out the tea. She says that the tremor disappears for a while after drinking a glass of wine. Her past medical history is insignificant. Her blood pressure is 160/90 mmHg and heart rate is 80/min. Physical examination is insignificant. Which of the following medications is the best choice to treat this patient's hypertension?
A. Propranolol
B. Verapamil
C. Amlodipine
D. Hydrochlorothiazide
E. Enalapril
135. A 47-year-old male was brought to the emergency room with chest pain of acute onset. The pain was associated with nausea, vomiting, and diaphoresis. He has a history of diabetes, hypertension, and hyperlipidemia. ECG reveals ST segment elevation in the anterolateral leads and ventricular premature beats (VPBs). The patient dies within the first hour after the arrival to emergency room. What is the most likely pathophysiologic mechanism responsible for this patient's death?
B. Reentry
A. Electro-mechanic dissociation
C. Full conduction block
D. Increased automaticity
E. Asystole
136. A 60-year-old Caucasian man presents to the office with a 2-week history of worsening shortness of breath and decreased exercise tolerance. His breathlessness is worse at night. He thinks his legs are swelling up. He has hypertension, coronary artery disease and chronic obstructive pulmonary disease. He used to drink heavily and smoke 1 pack of cigarettes daily but has quit recently, although he still reports occasionally drinking a "few beers." He currently denies any chest pain, palpitations or cough. His temperature is 37.5C (99.5 F), blood pressure is 110/70 mm Hg, pulse is 96/min and respirations are 22/min. The pertinent physical findings are an S3, bibasilar crackles, JVP 10 cm above the sternal angle, mild hepatomegaly, and 4+ pitting lower extremity edema. The patient is immediately treated with oxygen, intravenous furosemide, and nitrates Which of the following markers is most likely elevated in this patient?
C. B-type natriuretic peptide
A. Ejection fraction
B. Mean corpuscular volume
D. Urine sodium
E. Neutrophil count
137. A 69-year-old male presents to the emergency department with severe pain in the back of his chest that began suddenly 6 hours ago, and 2 hours of difficulty walking due to leg weakness. He has never had such symptoms before. His past medical history is significant for hypertension, bleeding peptic ulcers, and deep vein thrombosis requiring inferior vena cava filter placement. He drinks 6-8 cans of beer each weekend and does not smoke cigarettes or use illicit drugs. Blood pressure taken from his right arm is 210/120 mmHg. His heart rate is 120/min and regular. Chest x-ray reveals a right-sided pleural effusion. EKG shows sinus tachycardia. What is the most likely diagnosis?
D. Aortic dissection
A. Angina pectoris
B. Myocardial infarction
C. Acute pericarditis
E. Pulmonary embolism
138. A 34-year-old male with a history of mitral valve prolapse and mitral regurgitation presents with one week of intermittent fevers and increasing fatigue. He was punched in the face during a street fight two weeks ago. On admission he receives empiric intravenous vancomycin and gentamicin. Three days later, three out of four blood cultures grow Streptococcus viridans highly sensitive to penicillin. Which of the following is the best next step in managing this patient?
B. Switch antibiotics to IV ceftriaxone
A. Continue current regimen
C. Switch antibiotics to IV aminoglycosides
D. Switch antibiotics to oral penicillin V
E. Switch antibiotics to oral amoxicillin/clavulanate
139. A 10-year-old boy is brought to the ER by his mother because he has lost consciousness, while playing in the yard. He regained his consciousness quickly without following confusion. He never had such an episode before. His past medical history is significant for impaired hearing since birth and one episode of pneumonia three years ago, which required hospitalization. The family history is significant for a sudden cardiac death, in his cousin, at the age of 13. Physical examination is unremarkable. Blood pressure is 110/70 mmHg. Heart rate is 70/min, regular. Which of the following medication is most appropriate for this patient?
A. Propranolol
B. Verapamil
C. Quinidine
D. Ethosuximide
E. Phenobarbital
140. A 57-year-old male presents to your office with a two-week history of fever, chills, and generalized weakness. His medical history is significant for a hospitalization for pyelonephritis requiring IV antibiotics six months ago. He also recently underwent cystoscopy for evaluation of persistent dysuria. His past medical history is also significant for an episode of rheumatic fever as a child and Hodgkin's lymphoma treated with chemotherapy 10 years ago. On examination, his temperature is 37.8°C (100°F), blood pressure is 150/86 mmHg, pulse is 98/min and regular, and respirations are 16/min. The patient appears slightly diaphoretic. You note a new II/VI systolic murmur and tender erythematous lesions affecting several fingertips. The remainder of the physical examination is unremarkable. Which of the following bacteria is most likely responsible for his present illness?
C. Enterococci
A. Streptococcus pyogenes
B. Staphylococcus epidermidis
D. Viridans streptococci
E. Coxiella burnetii
141. A 57-year-old male presents to the emergency department with recent-onset dyspnea and cough. He reports that his symptoms began earlier this morning while he was jogging, when he suddenly started feeling short of breath and very weak. In the emergency department, laboratory analysis reveals a markedly elevated serum b-type natriuretic peptide level. Which of the following clinical signs best correlates with this finding?
C. Third heart sound
A Wheezing
B. Cyanosis
D. Extremity edema
E. Periumbilical bruit
142. A 68-year-old Caucasian male presents to the emergency room with a three-week history of progressive dyspnea, orthopnea, and lower extremity edema. His past medical history is significant for hypertension, type 2 diabetes mellitus, myocardial infarction experienced eight years ago, and congestive heart failure. His current medications include metoprolol, digoxin, enalapril, furosemide, spironolactone, and aspirin. His blood pressure is 145/90 mmHg, and heart rate is 75/min. Symmetric 2+ pitting edema of the lower extremities is present. Point of maximal impulse is displaced to the left and soft holosystolic murmur is heard on the apex. Bilateral crackles are present over the lower lobes. His laboratory values are: Hemoglobin 11.0 g/dl Leukocyte count 7,500/cmm Platelets 300,000/cmm Serum sodium 128 mEq/L Serum potassium 5.3 mEq/L Serum calcium 9.0 mg/dl Serum phosphorus 4.0 mg/dl Serum creatinine 1 .9 mg/dl ECG does not reveal acute ischemic changes. Which of the following is most likely correct concerning this patient's condition?
C. Hyponatremia indicates severe heart failure
A. Serum norepinephrine level is low
B. The combination of furosemide and enalapril is the cause of hyperkalemia
D. Increasing the dose of digitalis may be indicated
E. Increasing sodium intake will help to control the electrolyte abnormalities
143. A 76-year-old man presents to your office with progressively worsening fatigue over the past several months. He denies associated chest pain, dyspnea, nausea, cough, or ankle swelling. He has smoked a pack of cigarettes per day for the past 30 years. His past medical history is significant for hypertension for which he takes hydrochlorothiazide and type 2 diabetes mellitus controlled with metformin. He had a medical check-up five months ago which did not uncover any new abnormalities or medical issues. On physical examination today, his blood pressure is 130/80 mmHg and his heart rate is 110 and irregularly irregular. His lab values are: Hematocrit 41% WBC count 4,700/mm3 Platelets 200,000/mm3 Sodium 137 mEq/L Potassium 4.1 mEq/L Creatinine 0.8 mg/dl Fasting glucose 85 mg/dl Which of the following is the best treatment for this patient?
D. Warfarin
A Captopril
B. Salmeterol
C Amlodipine
E. Spironolactone
 144. A 48-year-old African American man presents to the emergency room with severe retrosternal chest pain. His temperature is 36.7C (98.F), blood pressure is 190/100 mm Hg, pulse is 100/min, and respirations are 16/min. On physical examination, his lungs are clear to auscultation and his heart sounds are normal. EKG shows evidence of left ventricular hypertrophy. A CT image of his chest is shown below. Which of the following is the most appropriate immediate pharmacotherapy for this patient?
144. A 48-year-old African American man presents to the emergency room with severe retrosternal chest pain. His temperature is 36.7C (98.F), blood pressure is 190/100 mm Hg, pulse is 100/min, and respirations are 16/min. On physical examination, his lungs are clear to auscultation and his heart sounds are normal. EKG shows evidence of left ventricular hypertrophy. A CT image of his chest is shown below. Which of the following is the most appropriate immediate pharmacotherapy for this patient?A Labetalol
B. Nifedipine
C. Heparin
D. Hydrochlorothiazide
E. Hydralazine
145. A 70-year-old male is brought to the ER, by his wife, because he lost consciousness while getting up in the morning. The syncopal episode lasted for several minutes, and the patient rapidly recovered consciousness. He had diarrhea and a decreased appetite one day earlier, which resolved spontaneously. His past medical history is significant for hypertension that is effectively controlled with the combination of hydrochlorothiazide/amiloride. His blood pressure is 120/70 mm Hg, while supine, and 98/50 mm Hg, while standing. The physical examination revealed a mucosal dryness. The EKG is normal. Which of the following laboratory values is the most sensitive indicator of the patient's underlying condition?
C. Increased BUN/creatinine ratio
A. Decreased sodium concentration in the urine
B. Hypokalemia
D. Metabolic acidosis
E. Decreased haematocrit
146. A 65-year-old man complains of lower leg swelling, fatigue and poor appetite. His past medical history is significant for recurrent chest infections, wheezing, cough, recent pyelonephritis, and arterial hypertension. He smokes 1 pack of cigarettes a day but denies alcohol or intravenous drug use. His physical examination reveals a barrel-shaped chest with bilateral scattered wheezes. His abdomen is distended and his liver edge is palpated 4 cm below the right costal margin. You note pitting edema and dilated, tortuous, superficial veins over the bilateral lower extremities. Manual pressure on the abdomen causes persistent distention of the jugular veins. The patient's serum sodium level is 135 mEq/L and his creatinine concentration is 1.2 mg/dl. An abnormality of which of the following is most likely to explain his edema?
B. Pulmonary artery systolic pressure
A. Serum albumin level
C. Pulmonary capillary wedge pressure
D. Portal venous resistance
E. Urinary protein excretion
147. A 60-year-old male presents to the emergency room with the chief complaint of progressive exertional dyspnea and fatigue. He denies any chest pain, syncope, cough, or edema. He suffered an acute anterior wall myocardial infarction one month ago. Chest auscultation reveals bilateral crackles in his lower chest. Cardiac auscultation reveals a pansystolic murmur at the apex with radiation to the axilla. ECG shows previously present unchanged Q waves and a persistent ST segment elevation in the anterior leads. Based on these findings, what is the most likely underlying cause of his symptoms?
C. Ventricular aneurysm
A. Interventricular wall rupture
B. Ventricular free wall rupture
D. Recurrent ischemia
E. Right ventricular infarction
148. A 65-year-old male presents to your office with a six-month history of periodic substernal pain. The pain episodes are experienced during strong emotion, last for 10-15 minutes, and resolve spontaneously. He has a long history of hypertension and diabetes mellitus, type 2. His right foot was amputated two years ago due to diabetes-related complications. You suspect angina pectoris and decide to perform myocardial perfusion scanning. It reveals uniform distribution of isotope at rest, but inhomogenesity of the distribution after dipyridamole injection. You conclude that the patient has ischemic heart disease. Which of the following effects of dipyridamole helped you in making the diagnosis?
B. Coronary steal
A. Increased heart contractility
C. Dilation of diseased vessels
D. Inhibition of platelet aggregation
E. Placebo effect
149. A 37-year-old healthy Caucasian male is seen in your office for a routine physical examination. He denies any symptoms or illness. He says he smokes a pack a day and drinks one to two beers every weekend. He has no allergies. Examination is unremarkable. The EKG reveals normal sinus rhythm with a heart rate of 72; there are frequent premature atrial beats present. The blood pressure is 120/65mm Hg. The next step in his management is:
E. Observation
A Digoxin
B. Lidocaine
C. Order potassium levels
D. Complete electrophysiological study
150. A 56-year-old white male presents with dyspnea for the last 3 months. His dyspnea was initially exertional but it has worsened progressively and now he is breathless even at rest. He denies any chest pain or ankle swelling. He has been smoking one-pack/day cigarettes for the last 30 years and has been drinking alcohol heavily for the last 10 years. He is not taking any medication. His mother died of breast cancer at 57. His vitals are, PR 86/min, BP 113/76mm of Hg; Temperature 37.1C (98.9F); RR 13/min. On auscultation of his precordium an S3 is heard, but there are no murmurs. Chest auscultation reveals bilateral basal crepitations. Chest x-ray shows marked cardiac silhouette enlargement and pulmonary venous congestion. EKG shows non-specific ST-T wave changes. Echocardiography shows a dilated left ventricle and systolic dysfunction (EF of 25-30%). CBC shows hematocrit of 32%, WBC count of 6,000/microl, and platelet count of 60,000/microl. Peripheral blood smear shows MCV of 101 fl. LFTs show AST of 180U/L and AL T of 66 U/L. The findings of cardiac catheterization and coronary angiography are not compatible with the diagnosis of ischemic cardiomyopathy. Which of the following measures is most likely to reverse his heart failure?
B. Abstinence from alcohol
A. Cessation of cigarette smoking
C. Reduced salt intake
D. Use of ACE inhibitors
E. Use of digoxin
151. A 55-year-old Caucasian male presents to your office for a routine check-up. His past medical history is significant for gout, hypertension, and hypercholesterolemia. His current medications include enalapril and pravastatin. He does not smoke or consume alcohol. His blood pressure is 156/94 mmHg and heart rate is 80/min. Physical examination reveals that the patient is moderately overweight (BMI = 27 kg/m2) with increased waist-to-hip ratio. You consider adding hydrochlorothiazide to the treatment regimen to improve the control of hypertension. Which of the following metabolic effects do you expect to emerge after this correction?
E. Hyperglycemia
A. Hypocalcemia
B. Hyperkalemia
C. Decreased LDL cholesterol
D. Decreased plasma triglycerides
152. An imaging study detects a 3.5 cm abdominal aortic aneurysm in a 60-year-old male. He has no associated symptoms. His past medical history is significant for hypertension, type 2 diabetes, hypercholesterolemia and hypothyroidism. His medications include aspirin, metformin, glipizide, hydrochlorothiazide, lisinopril, low dose atorvastatin and levothyroxine. He has smoked 1-2 packs of cigarettes daily for the past 40 years, and he drinks 1-2 glasses of wine daily. On physical examination, his blood pressure is 160/90 mmHg and his pulse is 80/min. Heart sounds are normal and his lungs are clear. Laboratory studies show: Serum creatinine 1.7 mg/dL Low density lipoprotein (LDL) 150 mg/dL HbA1C 8.5% Serum TSH 3.0 Which of the following interventions would most reduce the likelihood of his aortic aneurysm enlarging?
D. Smoking cessation
A. Better control of hypertension
B. Better control of hypercholesterolemia
C. Better control of diabetes
E. Alcohol cessation
153. A 68-year-old white female presents to the ER complaining of sudden onset chest pain associated with two episodes of vomiting. She has hypertension for which she takes atenolol and hydrochlorothiazide. Her pulse is 60/min, blood pressure is 80/50 mmHg and respirations are 14/min. Examination shows elevated jugular venous pressure and a positive Kussmaul's sign. Her lungs are clear to auscultation. Her EKG shows 2 mm ST segment elevation in leads II, Ill and aVF and 1 mm ST segment depression in leads I and aVL. Which of the following is the most likely cause of this patient's hypotension?
B. Right ventricular infarction
A. Pulmonary thromboembolism
C. Interventricular septum rupture
D. Variant angina
E. Intravascular volume depletion
 154. A 72-year-old male is admitted to the hospital with chest pain. EKG and cardiac enzymes confirm a myocardial infarction and he is started on nitroglycerine, aspirin, simvastatin and low molecular weight heparin. Four days later, he complains of leg pain. Physical examination reveals a cold, pale leg. The angiogram is shown below. What is the best next step in his management?
154. A 72-year-old male is admitted to the hospital with chest pain. EKG and cardiac enzymes confirm a myocardial infarction and he is started on nitroglycerine, aspirin, simvastatin and low molecular weight heparin. Four days later, he complains of leg pain. Physical examination reveals a cold, pale leg. The angiogram is shown below. What is the best next step in his management?E. Embolectomy
A. Intravenous streptokinase
B. Clopidogrel
C. Cilosta zol
D. Leg elevation and warm compress
155. A 53-year-old man presents to your office complaining of weakness and exertional dyspnea over the last week. He denies chest pain and palpitations. He has no other past medical history. His father died of a myocardial infarction at age 55. On exam, his heart rate is 100/min and blood pressure is 90/60 mmHg. Internal jugular venous pulsation is observed 7 cm above the sternal angle. Lungs are clear to auscultation. Heart sounds are muffled. Which of the following is the most likely cause of this patient's complaints?
C. Decreased left ventricular preload
A. Decreased cardiac contractility
B. Left ventricular outflow obstruction
D. Pulmonary hypertension
E. Increased right ventricular compliance
156. A 24-year-old military recruit is brought to the emergency room after suddenly collapsing while at training camp. Witnesses say he lost consciousness, and in the ER he appears confused. He had apparently been in his usual state of good health until this incident. His medical history includes allergic rhinitis for which he takes chlorpheniramine. On physical examination, his temperature is 41°C (106.F), blood pressure is 90/60 mm Hg, respiratory rate is 22/min, and pulse is 130/min and regular. He appears restless. His pupils are 4mm in size, symmetric, and reactive to light. Lung exam reveals a few rales at both lung bases. His abdomen is soft, non-tender and bowel sounds are present. There is no neck stiffness. His skin is dry and hot. He has 2+ symmetric reflexes in the upper and lower extremities. Muscle tone and bulk are normal. Initial laboratory studies show: Hemoglobin 16.0 g/L Platelets 120,000/mm3 Leukocyte count 18,500/mm3 Blood urea nitrogen (BUN) 40 mg/dL Prothrombin time 17 sec Partial thromboplastin time 40 sec Which of the following is the most likely cause of his current condition?
A. Heat stroke
B. Meningitis
C. Anticholinergic toxicity
D. Serotonin syndrome
E. Neuroleptic malignant syndrome
157. 56-year-old man presents to your office complaining of progressively worsening fatigue. He also reports difficulty concentrating and increasing forgetfulness over the past several weeks. On review of systems, the patient reports having unintentionally gained 6 pounds over the last three months. His past medical history is significant for hypertension and atrial fibrillation. On physical examination, he has a blood pressure of 140/90 mmHg and a heart rate of 75/min. His lung fields are clear to auscultation. There is no ankle edema. His skin is dry. Which of the following drugs is most likely responsible for this patient's complaints?
E. Amiodarone
A. Hydralazine
B. Metoprolol
C. Verapamil
D. Enalapril
158. A 33-year-old Russian male reports concern over recurrent episodes of a "pounding" and "racing" heart over the last several months. He says his symptoms are worst while lying supine and while lying on his left side. On physical examination, his blood pressure is 150/55 mmHg and heart rate is 73/min. Which of the following is most likely responsible for his symptoms?
A. Aortic regurgitation
B. Pulmonary regurgitation
C. Mitral stenosis
D. Tricuspid stenosis
E. Aortic stenosis
159. A 34-year-old man rushes into the ER complaining of severe substernal chest pain that began abruptly 30 minutes ago. He says that he also feels as though his heart 'is racing,' but denies any shortness of breath, cough or fever. He has never experienced pain like this before. His past medical history is significant for an appendectomy one year ago. The patient reports that his father died at age 64 due to "some heart problem" and his mother died of ovarian cancer. On physical examination, the patient is agitated and sweating profusely. His pulse is 110/min, blood pressure is160/100 mm Hg, and respirations are 14/min. Physical examination is normal except for dilated pupils and a small amount of blood at the external nares. EKG shows ST elevations in leads v1_v4. What is the most likely explanation for his symptoms?
D. Drug-induced vasospasm
A. Atherosclerotic vascular disease
B. Acute pericarditis
C. Pleurodynia
E. Aortic dissection
160. A 40-year-old male presents to the Emergency Room with a two-month history of occasional severe headache and blurring of vision. His past medical history is significant for hypertension controlled with hydrochlorothiazide for two years. His family history is significant for hypertension and diabetes. He smokes two packs a day and occasionally consumes alcohol. His blood pressure is 200/140 mmHg and heart rate is 75/min. Which of the following is most consistent with a diagnosis of malignant hypertension in this patient?
C. Papilledema
A. Left ventricular hypertrophy on ECG
B. Elevated serum creatinine level
D. Oliguria
E. Blood pressure >/= 200/ 140 mmHg
161. A 62-year-old man visits his family physician because of generalized aches and pains. He denies associated fevers, headaches, chest pain, or abdominal discomfort. His past medical history is significant for an inferior wall myocardial infarction 6 years ago. His other medical problems include hypertension, diabetes, hypercholesterolemia, and gout. His current medications are aspirin, losartan, naproxen, atenolol, glipizide, colchicine, and simvastatin. On physical exam today, he is afebrile, with blood pressure 130/90 mm Hg, pulse 80/min and respirations 18/min. Lab results are as follows: Sodium 140 mEq/L Potassium 4.2 mEq/L Bicarbonate 21 mEq/L Chloride 100 mEq/l BUN 30 mg/dl Creatinine 1.6 mg/dl AST 113 IU/L ALT 120 IU/L Creatine phosphokinase 14,998 mg/dl What is the most appropriate next step in the management of this patient?
B. Stop simvastatin
A. Stop losartan
C. Start N-acetylcysteine
D. Order hepatitis panel
E. Obtain liver biopsy
162. A 50-year-old white male comes into your office for a routine check-up. He has no present complaints. His past medical history is significant for hypertension controlled with a low-dose thiazide diuretic. His family history reveals non-fatal myocardial infarction in his father at the age of 47. The patient does not smoke or consume alcohol. His blood pressure is 130/75 mmHg and his heart rate is 70/min. His previous records show that his HDL level is persistently low in spite of acceptable total cholesterol and LDL levels. You prescribe niacin to raise HDL level. The patient returns in a week complaining of intensive generalized pruritis and flushing. What is the most probable cause of the patient's complaint?
B. Prostaglandin-related reaction
A. Hypersensitivity reaction
C. Drug interaction
D. Drug-induced vasoconstriction
E. Psychogenic reaction
 163. A 77-year-old woman comes to the emergency department because of feeling “light-headed and dizzy.” Except for the irregular pulse, her physical examination is normal. What is the rhythm in the lead tracing shown in Fig.?
163. A 77-year-old woman comes to the emergency department because of feeling “light-headed and dizzy.” Except for the irregular pulse, her physical examination is normal. What is the rhythm in the lead tracing shown in Fig.?(B) second-degree heart block
(A) first-degree heart block
(C) third-degree heart block
(D) premature ventricular beats
(E) premature atrial beats
 164. A 42-year-old woman has anterior chest pain of a somewhat atypical nature for many years. The patient’s pain has been present and relatively stable for a number of years, and the ECG shown in Fig. Is a stable one. What is the diagnosis?
164. A 42-year-old woman has anterior chest pain of a somewhat atypical nature for many years. The patient’s pain has been present and relatively stable for a number of years, and the ECG shown in Fig. Is a stable one. What is the diagnosis?(D) nonspecific changes
(A) inferior wall infarction
(B) anterior wall infarction
(C) ventricular aneurysm
(E) pericarditis
 165. The ECG shown in Fig. Was obtained during the initial stages of an acute MI. The patient had just received thrombolytic therapy. What is the rhythm?
165. The ECG shown in Fig. Was obtained during the initial stages of an acute MI. The patient had just received thrombolytic therapy. What is the rhythm?(E) nonsustained ventricular tachycardia
(A) atrial fibrillation
(B) atrial flutter
(C) second-degree heart block
(D) Wenckebach phenomenon
 166. A 78-year-old man with advanced renal disease has the ECG shown in Fig. (lead II). What is the diagnosis?
166. A 78-year-old man with advanced renal disease has the ECG shown in Fig. (lead II). What is the diagnosis?(A) hyperkalemia
(B) hypercalcemia
(C) hypernatremia
(D) pericarditis
(E) ventricular aneurysm
167. A 74-year-old woman presents to your office complaining of diarrhea and decreased appetite over the past week as well as increasing fatigue and occasional palpitations over the last few days. Her past medical history is significant for chronic atrial fibrillation for which she takes metoprolol, digoxin and warfarin. She smokes cigarettes and has for the past several years. On physical examination, her blood pressure is 140/90 mmHg and her heart rate is 70/min and irregular. Lung auscultation reveals scattered wheezes. Her abdomen is soft and non-tender. The liver span is 8 cm and the spleen is not palpable. There is no ankle edema. Her last measured INR was 2.3 two weeks ago. Which of the following is the best initial test in this patient?
E. Blood drug level
A. Echocardiography
B. Chest x-ray
C. Pulmonary function tests
D. Thyroid function tests
168. A 43-year-old male complains of frequent epigastric burning not relieved by antacids. The sensation is typically brought on by heavy lifting at work and takes 10-15 minutes to go away. He denies having associated arm or neck pain, cough, shortness of breath or difficulty swallowing. His past medical history is significant for systemic lupus erythematosus (SLE) diagnosed five years ago, for which he takes low-dose prednisone daily. On physical examination, his blood pressure is 140/90 mmHg and pulse is 80/min and regular. Heart, lung, and abdomen exams are unremarkable. EKG is normal. Which of the following is the best next step in managing this patient?
C. Exercise EKG
D. Myocardial perfusion testing
E. Upper Gl endoscopy
A. Echocardiogram
B. Coronary angiography
169. A 64-year-old white female presents for evaluation of two weeks of decreased appetite and nausea. She also notes occasional palpitations, which have been especially prominent over the past two days. Her medical history is significant for an anterior wall myocardial infarction one year ago and secondary congestive heart failure with left ventricular systolic dysfunction. Her current medications include aspirin, digoxin, furosemide, enalapril and metoprolol. On physical examination, her blood pressure is 120/80 mm Hg, pulse is 106/min and respirations are 15/min. The remainder of her exam is unremarkable. Chest x-ray shows an enlarged cardiac silhouette and normal lung fields. On laboratory testing, her digoxin level is twice the upper limit of normal. You order an EKG. Which of the following arrhythmias is most specific for digitalis toxicity?
D. Atrial tachycardia with AV block
A. Atrial flutter
B. Atrial fibrillation
C. Mobitz type II second-degree AV block
E. Multifocal atrial tachycardia
170. A 63-year-old male is admitted for sudden onset severe chest pain. His ECG reveals ST elevation in leads V2-V6. He is treated with thrombolytic therapy, heparin, aspirin, metoprolol, morphine, and nitrates. A coronary angiogram performed after thrombolytic therapy reveals 50% obstruction of the left anterior descending artery. On the third day of hospitalization, the patient suddenly develops severe shortness of breath at rest and hypotension. Examination reveals a soft S1, an apical pansystolic murmur radiating to the axilla, and bibasilar crackles. His temperature is 37.8°c (100°F), blood pressure is 92/58 mm Hg, heart rate is 102/min, and respirations are 31/min. An echocardiogram performed on the second hospital day reveals an akinetic region of the anterior wall. What is the most likely explanation for this patient's deterioration?
D. Papillary muscle dysfunction
A. Pericardia! tamponade
B. Pulmonary embolism
C. Rupture of ventricular septum
E. Acute aortic dissection
171. A 34-year-old female presents to your office complaining of pressure-like, substernal chest pain that has been affecting her recently when she plays active sports. Resting consistently alleviates the pain. She denies any associated nausea, vomiting, diaphoresis, dyspnea, palpitations or syncope. Family history is non-contributory. On physical examination, her pulse is 79/min and blood pressure is 130/70 mmHg. Cardiac auscultation reveals a high-pitched 3/6 systolic murmur best heard at the second right intercostal space. The lungs are clear to auscultation. Chest x-ray shows a normal sized heart and clear lung fields. What is the most likely cause of this patient's chest pain?
C. Increased myocardial oxygen demand
A. Anomalous origin of the right coronary artery
B. Atherosclerotic narrowing of the coronaries
D. Increased myocardial oxygen extraction
E. Stretching of the papillary muscles
172. A 45-year-old mildly overweight smoker presents with occasional episodes of nocturnal substernal chest pain that wakes her up from sleep. The episodes last 15-20 minutes and resolve spontaneously. She denies any illicit drug use. She leads a sedentary lifestyle but states that she can climb two flights of stairs without any discomfort. Her pulse is 78/min and regular, blood pressure is 130/70 mmHg and respirations are 13/min. Auscultation of her heart and lungs is unremarkable. Extended ambulatory ECG monitoring reveals transient ST segment elevations in leads V4-V6 during the pain attack. The pathophysiology of this patient's condition is most similar to that of which of the following?
D. Raynaud phenomenon
A Lacunar stroke
B. Intermittent claudication
C. Abdominal aortic aneurysm
E. Pulmonary embolism
173. An 84-year-old Caucasian male is brought to the ER with severe chest pain, dyspnea and diaphoresis. His past medical history is significant for a long history of hypertension and diabetes mellitus, type 2. He experienced a severe myocardial infarction 6 months ago. His current medications are enalapril, metoprolol, aspirin, furosemide, potassium, glyburide and pravastatin, but he says that he has not been taking some of his medications recently. Physical examination reveals acrocyanosis and symmetric 3+ lower extremity edema. Point of maximal apical impulse is displaced to the left, and a holosystolic II/VI apical murmur is heard at the apex. Non-specific ST segment and T wave changes are present on ECG. The initial set of cardiac enzymes are positive. The patient continues to deteriorate, despite aggressive diuretic and vasodilator therapy. You perform an echocardiographic evaluation of left ventricular function and decide to proceed with pulmonary artery catheterization. Cardiac index (CI), total peripheral resistance (TPR) and left ventricular enddiastolic volume (LVEDV) are determined. Which of the following is most likely to present in this patient?
C. Cl decreased, TPR increased, LVEDV increased
A. Cl decreased, TPR decreased, LVEDV decreased
B. Cl decreased, TPR increased, LVEDV decreased
D. Cl decreased, TPR increased, LVEDV normal
E. Cl normal, TPR decreased, LVEDV increased
 174. A 42-year -old male with a past medical history of bladder cancer and recurrent hematuria presents to the emergency room after "passing out" when he got out of bed this morning. The patient says that he was standing up to urinate shortly after waking when he began feeling dizzy. Fortunately, he was able to return to his bed before losing consciousness for 7-10 minutes. His EKG at the time of admission is shown below: Which of the following most likely accounts for the observed EKG changes?
174. A 42-year -old male with a past medical history of bladder cancer and recurrent hematuria presents to the emergency room after "passing out" when he got out of bed this morning. The patient says that he was standing up to urinate shortly after waking when he began feeling dizzy. Fortunately, he was able to return to his bed before losing consciousness for 7-10 minutes. His EKG at the time of admission is shown below: Which of the following most likely accounts for the observed EKG changes?C. Impaired AV node conduction
A. Ventricular preexcitation
B. Impaired SA node automaticity
D. Atrial reentry
E. His bundle branch block
175. A 65-year-old man comes to your office for a follow-up after his previous visits revealed inadequately controlled hypertension. He has no present complaints except difficulty walking uphill or climbing stairs, because of the pain in the right thigh, which makes him stop and rest. His past medical history includes stable angina, requiring coronary angioplasty and stenting 2 years ago; hypercholesterolemia; a 20-year history of hypertension; and a 10-year history of diabetes mellitus, type 2. His current medications are aspirin, metoprolol, hydrochlorothiazide, enalapril, amlodipine, pravastatin and glyburide. He smokes 1½packs of cigarettes per day and does not consume alcohol. His blood pressure is 160/100 mm Hg in his right arm and 180/110 mmHg in his left arm. Which of the following findings will point to the potential cause of the resistant hypertension in this patient?
B. Continuous murmur in the paraumbilical area to the right
A. Increased pulsation of intercostal arteries
C. Increased urinal excretion of vanillylmandelic acid (VMA)
D. High aldosterone/renin ratio
E. Increased 24-hour urinary free cortisol excretion
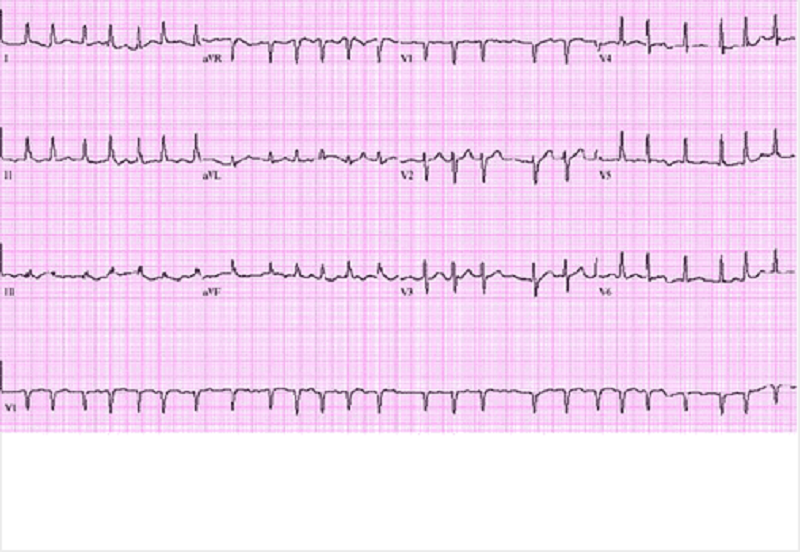
 176. A 65-year -old Hispanic male is brought to the emergency room with severe substernal chest pain and diaphoresis that began suddenly 1 hour ago. He reports that his pain started while he was at rest and radiates to his left shoulder. The patient notes having vomited twice when the pain first began. Despite administration of 2 baby aspirins and 3 tablets of sublingual nitroglycerin, the pain persists. His initial EKG is shown below. On physical examination, the patient's temperature is 36.9°C (98.4.F), blood pressure is 110/80 mmHg, pulse is 60/min, and respirations are 18/min. S1 and S2 are normal, and an S4 is heard. The lungs are clear to auscultation. There is no jugular venous distension or pedal edema. Interventions to achieve which of the following goals would most improve this patient's long-term prognosis?
176. A 65-year -old Hispanic male is brought to the emergency room with severe substernal chest pain and diaphoresis that began suddenly 1 hour ago. He reports that his pain started while he was at rest and radiates to his left shoulder. The patient notes having vomited twice when the pain first began. Despite administration of 2 baby aspirins and 3 tablets of sublingual nitroglycerin, the pain persists. His initial EKG is shown below. On physical examination, the patient's temperature is 36.9°C (98.4.F), blood pressure is 110/80 mmHg, pulse is 60/min, and respirations are 18/min. S1 and S2 are normal, and an S4 is heard. The lungs are clear to auscultation. There is no jugular venous distension or pedal edema. Interventions to achieve which of the following goals would most improve this patient's long-term prognosis?C. Restore coronary blood flow
A. Decrease myocardial oxygen demand
B. Decrease blood coagulability
D. Prevent ischemia-induced arrhythmias
E. Prevent reperfusin myocardial injury
177. A 43-year-old man is hospitalized with chest pain, lightheadedness and nausea. He describes the pain as dull and non-radiating. He has never had chest pain before, but does report occasional episodes of dyspnea and coughing. His medical history is significant for eczema. He is not presently taking any medications. His family history is significant for prostate cancer in his father and rheumatoid arthritis in his mother. He does not smoke or consume alcohol. The patient is admitted to the hospital and is given aspirin, low-molecular weight heparin, metoprolol and captopril. On day 2 of his hospitalization he complains of shortness of breath. Physical examination reveals prolonged expirations and bilateral wheezes. There are no crackles. You estimate the jugular venous pressure to be 7 cm with the patient's head elevated at 45 degrees. Which of the following is most likely responsible for this patient's current respiratory symptoms?
E. Drug side effect
A. Pericarditis
B. Bronchial infection
C. Recurrent myocardial ischemia
D. Right ventricular infarction
 178. A 64-year -old male with a history of hypertension presents with general malaise and a 'funny' heart rhythm for the past 2 weeks. He had an echocardiogram done last year, which revealed mild left atrial dilatation and left ventricular hypertrophy. He has been taking hydrochlorothiazide for hypertension. His blood pressure at today's visit is 180/98 mm Hg. An EKG is obtained and is shown below. Which of the following is the most appropriate treatment for this patient?
178. A 64-year -old male with a history of hypertension presents with general malaise and a 'funny' heart rhythm for the past 2 weeks. He had an echocardiogram done last year, which revealed mild left atrial dilatation and left ventricular hypertrophy. He has been taking hydrochlorothiazide for hypertension. His blood pressure at today's visit is 180/98 mm Hg. An EKG is obtained and is shown below. Which of the following is the most appropriate treatment for this patient?E. Diltizem
A. Immediate cardioversion
B. Lidocaine
C. Adenosine
D. Carotid massage
179. A 53-year-old Caucasian male is admitted to the hospital with a 2-week history of fatigue and decreased exercise tolerance. He says he can hardly climb two flights of stairs without getting dyspneic. He denies palpitations or chest pain. His past medical history is insignificant, and a routine check-up 6 months ago was normal. He admits two episodes of binge drinking during the last month, but says that he 'got it under control'. He is currently not taking any medications. His blood pressure is 150/90 mmHg and heart rate is 130/min, irregular. Lungs are clear on auscultation. ECG does not reveal P waves. Echocardiography shows significant left ventricular dilation with an ejection fraction of 35% and mitral regurgitation (1+). Which of the following intervention will most likely improve the left ventricular function in this patient?
C. Rate or rhythm control
A. Preload optimization
B. Decreasing afterload
D. Inotropic support
E. Valve surgery
 180. A 64-year-old male is admitted in ICU for acute myocardial infarction. He is on metoprolol, lisinopril, aspirin, furosemide, and potassium supplements. All of a sudden, the nurse mentions that the patient has a change in his tele monitoring. His blood pressure is 120/60 mm Hg. His potassium level is 4.2. He is alert, awake and oriented time, place and person. Examination shows scattered bilateral crackles, peripheral pedal edema and elevated JVI. Which of the following is the next best step in the management of this patient?
180. A 64-year-old male is admitted in ICU for acute myocardial infarction. He is on metoprolol, lisinopril, aspirin, furosemide, and potassium supplements. All of a sudden, the nurse mentions that the patient has a change in his tele monitoring. His blood pressure is 120/60 mm Hg. His potassium level is 4.2. He is alert, awake and oriented time, place and person. Examination shows scattered bilateral crackles, peripheral pedal edema and elevated JVI. Which of the following is the next best step in the management of this patient?A. IV amiodarone
B.IV digoxin
C. Cardioversion
D. IV diltiazem
E. Carotid massage
181. A 48-year-old Caucasian male presents to your office complaining of progressive exertional dyspnea. It has become especially bothersome over the past two months. Presently, he becomes short of breath after climbing one flight of stairs. He denies any significant problems in the past. He is not taking any medications and he denies smoking or drinking alcohol. His temperature is 37.2°C (98.9F), pulse is 78/min, blood pressure is 130/75 mm of Hg and respirations are 14/min. Chest examination reveals a harsh systolic murmur that is best heard at the right second intercostal space with radiation along the carotid arteries. An S4 is heard at the apex. Based on these findings, what is the most likely cause of this patient's symptoms?
D. Bicuspid aortic valve
A Hypertrophic cardiomyopathy
B. Myxomatous valve degeneration
C. Rheumatic heart disease
E. Senile calcific aortic stenosis
182. A 47-year-old Caucasian female presents with occasional episodes of nocturnal substernal chest pain that wakes her up during sleep. The pain episodes last 15-20 minutes and resolve spontaneously. She denies any illicit drug use. She leads a sedentary lifestyle but states that she can climb two flights of stairs without any discomfort. She has no history of hypertension or diabetes. Her pulse is 75/min and regular, blood pressure is 134/70 mmHg and respirations are 14/min. Extended ambulatory ECG monitoring reveals transient ST segment elevation in leads I, aVL, and V4-V6 during the episodes. Which of the following is the best treatment for this patient?
A Diltiazem
B. Propranolol
C. Aspirin
D. Heparin
E. Digoxin
183. A 36-year-old male patient, who has a history of Marfan's syndrome, presents with sudden onset of severe central tearing chest pain radiating to his back. The pain is 9/10 in severity and is unrelated to exertion. He denies any history of alcohol or tobacco use. Measurement of his BP shows a difference of 35 mm Hg between his two arms. Chest auscultation reveals clear lung sounds and a mid-systolic click. What is the most appropriate next diagnostic step in the management of this patient?
A. Transesophageal echocardiography
B. Transthoracic echocardiogram
C. Cardiac enzymes
D. Coronary angiogram
E. Ventilation-perfusion scans
184. A 55-year-old male presents to your office with a 6-month history of periodic substernal pressure. He experiences this pressure while walking uphill or climbing two flights of stairs. His past medical history is insignificant. He smokes 1 pack a day and consumes alcohol occasionally. His blood pressure is 160/90 mmHg and heart rate is 75/min. Resting ECG is normal. You suspect stable angina and order an ECG stress test that reveals horizontal ST segment depression in leads II, III, and aVF at submaximal heart rate. What is the best medication to treat this patient's condition?
D. Metoprolol
A. Thiazide
B. Verapamil
C. Amlodipine
E. Enalapril
185. A 45-year-old man presents to the emergency department because of dyspnea, fatigue, poor appetite and weight gain over the past several weeks. He says that about four weeks ago he began to develop worsening shortness of breath with exertion and more recently has been waking at night with breathlessness. He also notes that it is sometimes difficult for him to open his eyes in the morning due to facial edema. He has no significant past medical history and he takes no medications. On physical examination, his blood pressure is 200/120 mmHg and his heart rate is 100/min. You note generalized bodily edema and distention of his jugular veins while he is sitting upright. On lung auscultation you hear bibasilar rales. Urinalysis shows trace protein, no nitrites, trace leukocyte esterase, 50+ red blood cells and occasional neutrophils. Which of the following is the most likely cause of this patient's edema?
C. Extensive glomerular damage
D. Portal hypertension
E. Hypothyroidism
A. Renal hypoperfusion
B. Hypoalbuminemia
186. A 45-year-old white male presents to the ER after an episode of syncope. His medical history is unremarkable except for an upper respiratory infection one week ago. On physical examination, his temperature is 37.2°C (99.F), pulse is 90/min, blood pressure is 100/60 mmHg and respirations are 13/min. His neck veins are distended and his heart sounds are distant. His lungs are clear to auscultation bilaterally. Chest x-ray reveals small bilateral pleural effusions and an enlarged cardiac silhouette. Which of the following EKG findings is fairly specific for his condition?
C. Electrical alternans
A. Prolonged 'PR' interval
B. Presence of 'F' waves
D. Presence of 'delta' wave
E. New-onset right bundle branch block
187. A 56-year-old man presents to the emergency department with dyspnea. He describes waking up during the night with difficulty breathing and chest pain that kept him from falling back to sleep. He has never had these symptoms before. His past medical history is significant for long-standing hypertension and non-compliance with his antihypertensive therapy. He has smoked a pack of cigarettes per day for the past 30 years. On physical examination, his blood pressure is 170/100 mmHg and his heart rate is 120/min and regular. Lung auscultation reveals bibasilar rales and scattered wheezes. Which of the following is most likely to relieve this patient's dyspnea?
C. Nitroglycerin
A Metoprolol
B. Hydralazine
D. Dopamine
E. Amiodarone
 188. A 34-year-old female presents to the ER with difficulty breathing and dizziness. Blood pressure tracing from an arterial line placed in the ER is depicted below. Which of the following best accounts for these findings?
188. A 34-year-old female presents to the ER with difficulty breathing and dizziness. Blood pressure tracing from an arterial line placed in the ER is depicted below. Which of the following best accounts for these findings?A. Severe asthma
B. Lobar pneumonia
C. Mitral stenosis
D. Aortic regurgitation
E. Panic attack
 189. A 43-year -old man complains of progressive weakness and shortness of breath over the last two weeks. He denies any chest or muscle pain, nausea, vomiting or weight loss. He had a recent upper respiratory tract infection. His heart rate is 90/min and blood pressure is 110/70 mmHg. Jugular venous pressure is normal. Lungs are clear to auscultation. His chest x-ray is shown below. Which of the following is the most likely additional finding in this patient?
189. A 43-year -old man complains of progressive weakness and shortness of breath over the last two weeks. He denies any chest or muscle pain, nausea, vomiting or weight loss. He had a recent upper respiratory tract infection. His heart rate is 90/min and blood pressure is 110/70 mmHg. Jugular venous pressure is normal. Lungs are clear to auscultation. His chest x-ray is shown below. Which of the following is the most likely additional finding in this patient?B. Non-palpable point of maximal impulse
A. Audible fourth heart sound
C. Pulsus bisferiens
D. Opening snap
E. Fixed splitting of the second heart sound
190. A 56-year-old white male presents to his primary care physician for follow-up evaluation of high blood pressure noted on each of three prior visits over a period of 6 months (systolic blood pressure ranging 140-145, diastolic blood pressure ranging 90-96 mm Hg). He has smoked a pack of cigarettes per day for the past 20 years and takes 5-6 drinks of alcohol daily. He has no other medical problems and takes no medications. There is no family history of diabetes mellitus, coronary artery disease, hyperlipidemia or hypertension. On physical examination today, his blood pressure is 146/97 mm Hg and pulse is 80/min. The remainder of the exam is unremarkable. Which of the following nonpharmacologic interventions would be expected to have the greatest impact on his high blood pressure?
D. Decreased alcohol intake
A. Smoking cessation
B. Increased consumption of complex carbohydrates
C. Increased calcium consumption
E. Decreased consumption of animal protein
 191. A 55-year-old male is admitted to the ICU after being involved in a motor vehicle accident. He requires exploratory laparotomy for suspected bowel perforation. Two days after the surgery he remains hypotensive and requires both aggressive intravenous fluids and vasopressors to maintain his blood pressure. On physical examination, you note the fingertip changes pictured below: All four extremities feel cold to touch. Which of the following is most likely responsible?
191. A 55-year-old male is admitted to the ICU after being involved in a motor vehicle accident. He requires exploratory laparotomy for suspected bowel perforation. Two days after the surgery he remains hypotensive and requires both aggressive intravenous fluids and vasopressors to maintain his blood pressure. On physical examination, you note the fingertip changes pictured below: All four extremities feel cold to touch. Which of the following is most likely responsible?C. Norepinephrine-induced vasospasm
A. Septic emboli
B. Raynaud's phenomenon
D. Cholesterol emboli
E. Superior vena cava syndrome
192. A 14-year-old African American male collapses and dies while playing basketball at a school tournament. He has no known past medical history. Which of the following is the most likely underlying disease in this patient?
A Hypertrophic cardiomyopathy
B. Coronary atherosclerosis
C. Aortic aneurysm rupture
D. Ventricular septal defect
E. Bicuspid aorta
193. A 63-year-old female presents to your office for a routine check-up. She has no present complaints. Her past medical history includes OM, type 2, and hypertension. Her current medications include glyburide and atenolol. She does not smoke. She drinks 2-3 glasses of wine 1-2 times a week. Three consecutive BP measurements were in the range of 138-142/87-90 mmHg. Physical examination is within normal limits. Her recent fasting glucose level was 250 mg/dl. ECG recorded 1 month ago showed left ventricular hypertrophy. Which statement about the BP control in this patient is the most accurate?
C. It is better to keep systolic pressure less than 130 mmHg to slow end-organ damage
A. BP is within acceptable range
B. BP is within optimal range
D. Diastolic BP is within acceptable range, but systolic is not
E. Systolic BP is within acceptable range, but diastolic is not
194. A 70-year-old patient presents to the ER with a 3-hour history of intensive retrosternal chest pain that radiates to the interscapular area. He states that he has never experienced this pain before. His past medical history is significant for a 20-year history of hypertension and a 10-year history of diabetes mellitus, type 2. His current medications include enalapril and hydrochlorothiazide. He does not smoke or consume alcohol. His vital signs are BP 180/110 mm Hg in the right arm and 178/110 mm Hg in the left arm, PR 85/min and RR 18/min. The physical examination revealed an early decrescendo-type diastolic murmur at the left sternal border. The EKG is normal. Which of the following is the best next step in the management of this patient?
B. Transesophageal echocardiography
A. Magnetic resonance imaging
C. Aortography
D. CK MB and troponin T levels
E. Ventilation/perfusion scanning
195. A 46-year-old man complains of exertional dyspnea and dry cough. He also describes occasional episodes of a suffocating nighttime cough that is relieved only when he stands up. His medical history is significant for a myocardial infarction six months ago. His current medications are metoprolol, aspirin and simvastatin. He does not use tobacco but drinks alcohol on social occasions. His father died of a stroke and his mother suffers from diabetes mellitus. His blood pressure is 150/100 mmHg and his heart rate is 60/min. Chest examination reveals bibasilar rales. His cardiac apex is palpated in the sixth intercostal space. The liver span is 12 cm. Bilateral pitting leg edema is also present. Which of the following most likely contributes to his edema?
A. Constriction of the renal arterioles
B. High sodium delivery to the distal tubule
C. Increased renal blood flow
D. Increased renal potassium loss
E. High portal venous resistance
196. A 22-year-old white female is brought to your office by her mother because of the recurrent syncopal episodes. The first episode occurred about one year ago when her roommate committed suicide and then several similar episodes occurred usually provoked by a strong emotion. The episodes are preceded by lightheadedness, weakness, and blurred vision and last about three minutes with rapid recovery of consciousness. Past medical history is insignificant. She is not taking any medications and denies drug abuse. Her blood pressure is 110/70 mm/Hg while supine and 108/70 mmHg while standing. Physical findings are within normal limits. EKG performed one month ago was normal. Which of the following is the next best step in the management of this patient?
E. Upright tilt table testing
A. Echocardiography
B. 24-hour (Holter) monitoring
C. Electroencephalogram
D. Invasive electrophysiologic testing
197. A 32-year-old man presents to the emergency department with a three-day history of fever, cough and weakness. His blood pressure is 120/80mmHg and his heart rate is 110/min. Physical examination reveals multiple needle tracks on his arms. ECG shows sinus tachycardia but is otherwise normal. Chest X-ray shows scattered round lesions in the peripheral lung fields bilaterally. Urinalysis is positive for 2+ protein. Which of the following accompanying findings is most likely in this patient?
B. Systolic murmur that increases on inspiration
A. S4 when patient is in the left lateral decubitus position
C. Diastolic murmur heard best with the patient sitting up
D. Systolic murmur that increases when the patient stands up
E. Paradoxical splitting of S2
198. A 41-year-old intravenous drug abuser presents with shortness of breath and pleuritic chest pain. He is febrile with a temperature of 103.5°F. He has no skin lesions and funduscopic exam is negative. He has jugular venous distension that increases with compression of the liver. The liver is pulsatile. The jugular venous pulse shows a prominent v wave. The patient has splenomegaly. Heart auscultation reveals a holosystolic murmur heard best at the left lower sternal border. The murmur increases with inspiration (Müller maneuver). Which of the following is the most likely diagnosis?
A. Bacterial endocarditis
B. Pericarditis
C. Rheumatic fever
D. Mitral valve prolapse
E. Pericardial effusion
199. A 54-year-old man with a 20-year history of chronic obstructive lung disease has a heave that is palpable at the lower left sternal border at the third, fourth, and fifth intercostal spaces. Which of the following best explains the etiology of the heave?
D. It means the patient has right ventricular hypertrophy
A. It is probably a displaced point of maximum impulse (PMI)
B. It means the patient has congestive heart failure
C. It means that the patient has aortic stenosis
E. It means the patient has a pericardial effusion
 200. A 61-year-old woman was on her way to the grocery store when she started feeling chest pressure in the center of her chest. She became diaphoretic and felt short of breath. On arrival to the ED by EMS, her BP is 130/70 mm Hg, HR is 76 beats per minute, and oxygen saturation is 98% on room air. The nurse gives her an aspirin and an ECG is performed as seen below. Which of the following best describes the location of this patient’s myocardial infarction (MI)?
200. A 61-year-old woman was on her way to the grocery store when she started feeling chest pressure in the center of her chest. She became diaphoretic and felt short of breath. On arrival to the ED by EMS, her BP is 130/70 mm Hg, HR is 76 beats per minute, and oxygen saturation is 98% on room air. The nurse gives her an aspirin and an ECG is performed as seen below. Which of the following best describes the location of this patient’s myocardial infarction (MI)?D. Inferior
A. Anteroseptal
B. Anterior
C. Lateral
E. Posterior
{"name":"Cardiology part2(101-200)ronaldo", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"101. A 54-year-old woman presents for a routine physical. She has no complaints. She has no history of hypertension, diabetes, hypercholesterolemia, or heart disease, and she does not use tobacco, alcohol or drugs. On physical examination, her pulse is irregular. There are no murmurs. Her lungs are clear to auscultation and her legs are free of edema. An EKG shows atrial fibrillation with a heart rate of 72 beats per minute. An echocardiogram is unremarkable except for evidence of atrial fibrillation. What is the most appropriate management of this patient?, 102. A middle-aged man was recently diagnosed with hypertension. The antihypertensive medication prescribed to him enhances natriuresis, decreases serum angiotensin II concentration, and decreases aldosterone production. This medication most likely belongs to which of the following drug classes?, 103. A 63-year-old woman complains of leg swelling that is especially bothersome in the evening. She also complains of chronic cough and exertional dyspnea. She has been smoking one pack of cigarettes per day for the past 30 years. She also drinks one or two cans of beer on weekends. Her medical history is significant for a hospitalization for a \"chest infection\" two years ago, for which she was treated with antibiotics, steroids, and inhalers. She also reports having been diagnosed with hypertension, but says that she has never taken medications for it. On physical examination, her blood pressure is 160\/90 mmHg and her heart rate is 80\/min. Chest examination reveals bilateral scattered wheezes and prolonged expirations. Her jugular venous pulsation is seen 2 cm above the sternal angle with the head of the bed elevated 30•. Her abdomen is soft and non-distended. On examination of her lower extremities, you note bilateral pitting edema and dilated, tortuous, superficial veins. Which of the following is most likely to relieve this patient's edema?","img":"https://cdn.poll-maker.com/10-459557/3.png?sz=1200"}
More Quizzes
ANSI Consensus Body Vote/Comment on RSTC 'Hand Signals' Standard
100
Higiene Personal 2020
11623
Indiana Latin University
10511
Baptist or Presbyterian?
1477
Which Statement About Cell Structures Is Accurate? Free
201041455
Think You Know the Ghetto Stories Film? Take the Now!
201060016
Can You Ace the Latin 3rd Declension Adjectives?
201027570
Which Fantastic Mr. Fox Character Are You? Take the
201028139
Free Medical Pathophysiology Knowledge
201028434
Master German Adjektivendungen: Free Challenge
201033979
Doberman: Are You a True Pinscher Expert?
201031860
Negative Sentiment Override: Find Your NSO Level
201023482