Pediatric USMLE 1-100
1. A 16-year-old female presents to the emergency room with severe right- sided abdominal pain. Her last menstrual period was 2 weeks ago and felt to be normal. She displays painful difficulty in positioning herself on the examination table. Her temperature is 38.5 C (101.3 F), blood pressure is 128/75 mm Hg, pulse is 80/min, and respirations are 22/min. Examination of the throat reveals mild pharyngitis. Her abdomen is diffusely tender, especially the lower abdomen. Rectal examination reveals tenderness anteriorly on the right side. Stool guaiac is negative. A pelvic examination is performed, and there is evidence of cervical tenderness and questionable fullness in the right adnexal area. Which of the following is the most likely diagnosis?
A. Ovarian cyst
B. Pyelonephritis
C. Pelvic inflammatory disease
D. Constipation
E. Endometriosis
2. Your sister who lives in another state sends via e-mail photographs of her 6-month-old infant. You note the child has a white reflection from one of his eyes. You hastily assist in arranging an urgent pediatric ophthalmologic evaluation. Your sister immediately accesses the Internet and begins to ask questions of you. Which of the following statements found by your sister is correct?
A. Most cases of retinoblastoma are unilateral and hereditary.
B. Cure rates for retinoblastoma treated in the United States exceed 90%.
C. Biopsy is usually performed to confirm the diagnosis.
D. Intraocular calcifications are an unusual finding and suggest worse prognosis.
E. Patients with the hereditary form of retinoblastoma are at significantly increased risk of leukemia in later years.
3. A 2950-g (6.5-lb) black baby boy is born at home at term. On arrival at the hospital, he appears pale, but the physical examination is otherwise normal. Laboratory studies reveal the following: mother’s blood type A, Rh-positive; baby’s blood type O, Rh-positive; hematocrit 38%; and reticulocyte count 5%. Which of the following is the most likely cause of the anemia?
A. Fetomaternal transfusion
B. ABO incompatibility
C. Physiologic anemia of the newborn
D. Sickle-cell anemia
E. Iron-deficiency anemia
4. A 5-year-old boy is brought to the physician's office because of a cough. He has episodes of successive and rapid coughs, which seems like he is choking, followed by a deep and loud inspiratory sound. He has vomited a few times after these bursts of cough. His symptoms have been progressively worsening for the past week, and were preceded by congestion, serous rhinorrhea and sneezing. His past medical history is insignificant. His vital signs are stable. Lung auscultation is unremarkable. Which of the following is the most appropriate pharmacotherapy for this patient?
A. Erythromycin
B. Ampicillin
C. Rifampin
D. Treatment is ineffective at this stage
E. Cephalexin
5. A 1-week-old male newborn is seen in the office for "noisy breathing." The mother says that the "noisy breathing" is more prominent when the infant is lying on his back, and improves when he is in a prone position with his chin up. The newborn is afebrile and has no cough, vomiting, or cyanosis. There are no inspiratory retractions or wheezes. On direct laryngoscopy, the epiglottis is rolled in from side to side. Which of the following statements is true about the child's condition?
A. The child should be held in an upright position for 30 minutes after feeding and never fed while lying down
B. The child requires immediate tracheostomy
C. The child should be treated with intravenous ceftriaxone
D. The child's condition is likely to deteriorate as the age advances
E. In this condition the stridor improves when the child cries
6. A 2-month-old infant comes to the emergency center with fever for 2 days, emesis, a petechial rash, and increasing lethargy. In the ambulance he had a 3-minute generalized tonic/clonic seizure that was aborted with lorazepam. He does not respond when blood is drawn or when an IV is placed, but he continues to ooze blood from the skin puncture sites. On examination, his anterior fontanelle is open and bulging. His CBC shows a WBC of 30,000 cells/ΠL with 20% band forms. Which of the infant’s problems listed below is a contraindication to lumbar puncture?
A. Uncorrected bleeding diathesis
B. Bulging fontanelle
C. Dehydration
D. History of recent seizure
E. Significantly elevated WBC count consistent with bacteremia
7. The mother of one of your regular patients calls your office. She reports that her daughter has a 3-day history of subjective fever, hoarseness, and a bad barking cough. You arrange for her to be seen in your office that morning. Upon seeing this child, you would expect to find which of the following?
A. A temperature greater than 38.9θC (102θF)
B. Expiratorystridor
C. Infection with parainfluenza virus
D. Hyperinflation on chest x-ray
E. A child between 6 and 8 years of age
8. A 2-week-old baby girl is brought to the clinic for the evaluation of vaginal discharge. Her mother has noticed a cloudy white vaginal discharge mixed with blood since yesterday. She was born by normal vaginal delivery at term, and no congenital anomalies were noted at birth. Physical examination reveals a blood-stained, odorless vaginal discharge. Her vital signs are stable. What is the most appropriate next step in the management of this patient?
A. Treatment for Chlamydia
B. Treatment for HSV-2
C. Rule out vaginal cancer
D. Reassurance
E. Treatment for Trichomonas vaginalis
9. A 6-month-old male infant is brought to the physician's office by his mother due to failure to thrive. According to the mother, the child always regurgitates shortly after feedings, and has even had a few episodes of blood-stained projectile vomiting. During the vomiting episodes, the child tilts his head to the left and arches his back. On examination, the child is afebrile. His abdomen is soft and non-tender to palpation. Laboratory evaluation shows hypochromic microcytic anemia. What is the most appropriate test to confirm the most likely diagnosis of this child?
A. Chest x-ray
B. 24-hour esophageal pH monitoring
C. Esophageal manometry
D. Barium swallow
E. Technetium (Tc) sulfur colloid gastroesophageal scan
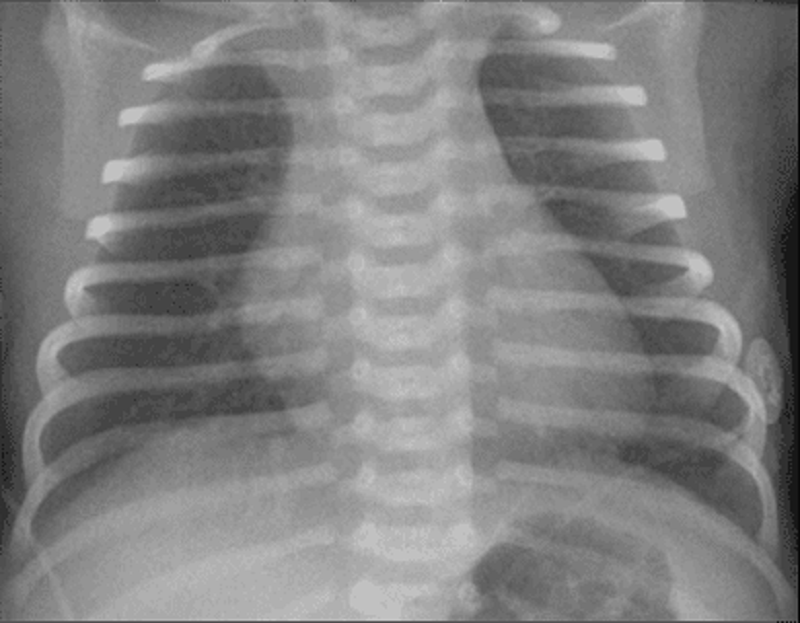
10. An infant weighing 1400 g (3 lb) is born at 32 weeks’ gestation. Initial evaluation was benign, and the infant was transferred to the level 2 nursery for prematurity. The nurse there calls at 1 hour of life and reports the infant is tachypneic. Vital signs include a heart rate of 140 beats per minute, a respiratory rate of 80 breaths per minute, a temperature of 35°C (95°F), and a peripheral oxygen saturation of 98%. The lungs are clear with bilateral breath sounds and there is no murmur; the infant is in no dis- tress. The child’s chest radiograph is shown. Which of the following is the most appropriate next step in evaluating the infant?
A. Obtain a complete blood count and differential.
B. Perform a lumbar puncture.
C. Administer intravenously 5cc of D50W.
D. Place the infant under a warmer.
E. Administer supplemental oxygen.
11. A 14-year-old boy is evaluated for short stature. He has no significant past medical history and is considered otherwise healthy by his parents. He eats a normal diet and has regular meals. His height and weight have been consistently at the 5th percentile since early childhood. His physical examination is normal, with genitalia at Tanner stage 3. Which of the following is the most likely laboratory finding for this boy?
A. Bone age that is equivalent to chronologic age
B. Decreased complement C3 level
C. Decreased serum albumin concentration
D. Decreased thyroid stimulating hormone
E. Increased serum creatinine concentration
12. A 2-month-old infant is brought to the emergency department with irritability and lethargy. The parents state that he was well until he rolled off the couch on to the floor yesterday. On examination, he is inconsolable and afebrile. The fontanels are full and tense. He has a generalized tonic-clonic seizure. Which of the following is the most important initial diagnostic study to order?
(A) serum calcium, phosphorus, and magnesium levels
(B) analysis of cerebrospinal fluid (CSF)
(C) cranial computed tomography (CT) scan
(D) serum ammonia level
(E) serum acetaminophen level
13. Two weeks after a viral syndrome, a 2-year-old child develops bruising and generalized petechiae, more prominent over the legs. No hepatosplenomegaly or lymph node enlargement is noted. The examination is otherwise unremarkable. Laboratory testing shows the patient to have a normal hemoglobin, hematocrit, and white blood cell (WBC) count and differential. The plateletcount is 15,000/L. Which of the followingis the most likely diagnosis?
A. Von Willebrand disease (vWD)
B. Acute leukemia
C. Idiopathic (immune) thrombocytopenic purpura (ITP)
D. Aplastic anemia
E. Thrombotic thrombocytopenicpurpura
14. An 11-month-old African American boy has a hematocrit of 24% on a screening laboratory done at his well-child checkup. Further testing demonstrates: hemoglobin 7.8 g/dL; hematocrit 22.9%; leukocyte count 12,200/L with 39% neutrophils, 6% bands, 55% lymphocytes; hypochromia on smear; free erythrocyte protoporphyrin (FEP) 114 g/dL; lead level 6 g/dL whole blood; platelet count 175,000/L; reticulocyte count 0.2%; sickle-cell preparation negative; stool guaiac-negative; and mean corpuscular volume (MCV) 64 fL. Which of the following is the most appropriate recommendation?
A. Blood transfusion
B. Oral ferrous sulfate
C. Intramuscular iron dextran
D. An iron-fortified cereal
E. CalciumEDTA
15. A 7-year-old girl presents with hives, which developed after a bee sting. She has no other symptoms. The hives resolve with diphenhydramine. Which of the following is the most appropriate management?
(A) Write a prescription for diphenhydramine in case she is bitten again.
(B) Provide an Epi-pen Jr (epinephrine auto injector) to be carried at all times, as well as a prescription for diphenhydramine.
(C) Admit to the hospital for observation for delayed hypersensitivity symptoms.
(D) Refer her to an allergist for desensitization.
(E) Order a skin-prick test with hymenoptera venom.

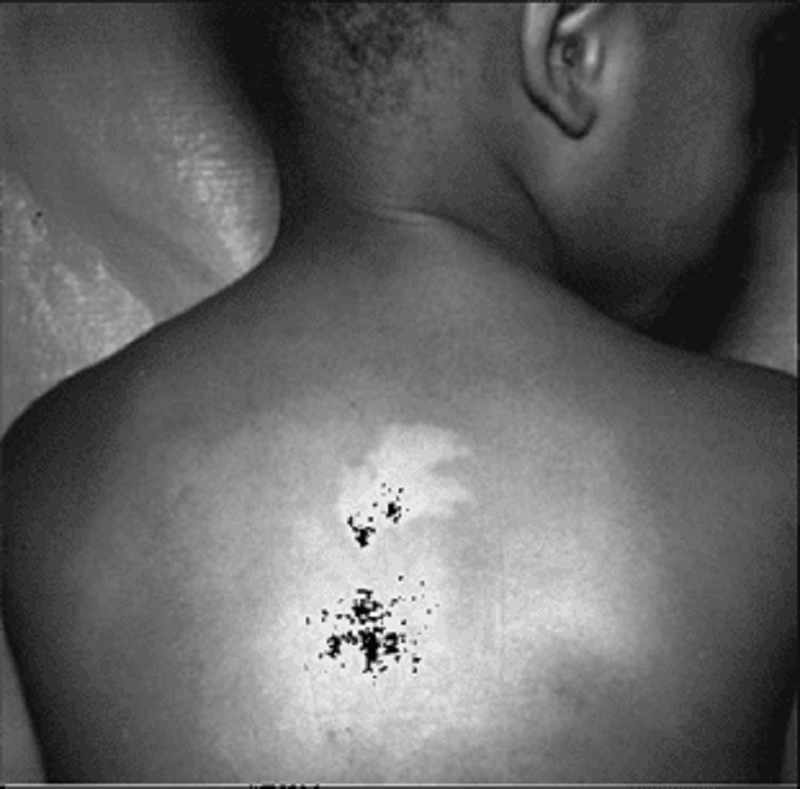
16. A 15-year-old presents with the complaint of a rash, as pictured below. Which of the following statements is correct concerning the management of this common condition?
A. Fried foods must be avoided.
B. Frequent scrubbing of the affected areas is key.
C. Topical antibiotics are of no value.
D. Topical benzoyl peroxide is the mainstay of treatment.
E. This rash is solely a disease of the adolescent.
17. The recent suicide of a well-known high school cheerleader in your community has generated an enormous amount of community concern and media coverage. A girl who was close friends with the deceased makes an appointment and comes in to your office to discuss the event with you. You ask, and she denies suicidal ideation, but she has many questions about suicide. Correct statements about adolescent suicide include which of the following?
A. Girls tend to use more lethal means.
B. The number of attempted suicides is much higher among boys.
C. Those who are successful have a history of a prior attempt or prior serious suicidal ideation.
D. Inquiry by pediatricians, high school teachers, parents, or friends about suicidal thoughts typically precipitates the act.
E. The number of suicides in adolescents 10 to 19 years of age has decreased significantly since the 1950s.
18. A 2-month-old male is brought to the emergency department for evaluation of cyanosis, which occurred earlier in the day while the infant was taking his bottle. Initially, he became fussy and sweaty, then his mother noticed that his lips turned blue. He became intermittently tachypneic and continued to cry. As the crying continued, the cyanosis worsened. His temperature is 3 0C (98.6 0F), blood pressure is 80/50 mmHg, pulse is 150/min, and respiratory rate is 45/min. On examination, the child is alert, cyanotic, and tachypneic. Cardiac auscultation reveals a normal S 1 followed by a systolic ejection click. A grade 2/6 crescendo-decrescendo systolic ejection murmur is heard at the left upper sternal border. The patient is immediately placed in a knee-chest position. This maneuver will improve this patient's condition by which of the following mechanisms?
A. Increased systemic venous return
B. Decreased pulmonary blood flow
C. Increased systemic vascular resistance
D. Increased respiratory drive
E. Increased right to left shunting
19. A 2-year-old child is brought to the physician for a routine visit. He is growing and developing appropriately. He drinks 3-4 glasses of whole milk each day. He is starting to put words together into short sentences. His mother has no concerns. Physical examination shows mild pallor. Laboratory studies show the following: Hemoglobin 9.5 g/dL RDW 21% MCV 70 fl Platelet count 284,000/mm3 Leukocyte count 6,500/mm3 Which of the following additional findings is most likely in this patient?
A. Abnormal hemoglobin electrophoresis
B. Low reticulocyte count
C. Low serum total iron binding capacity
D. High indirect bilirubin
E. Positive fecal occult blood test
20. A 10-year-old child arrives with the complaint of new-onset bed-wetting. He has had no fever, his urine culture is negative, and he has had no new stresses in his life. He is well above the 95th percentile for weight as is much of his family. Which of the following is most helpful in making a diagnosis?
A. Fasting plasma glucose of 135 mg/dL
B. Random plasma glucose of 170 mg/dL
C. Two-hour glucose during glucose tolerance test of 165 mg/dL
D. Acanthosis nigricans on the neck
E. Symptoms alone are enough to make the diagnosis
21. You are called to the ER to see one of your patients. The father of this 14-year-old mildly retarded child says that he found the child about 20 minutes ago in the neighbor’s garden shed with an unknown substance in his mouth. The child first had a headache, but then became agitated and confused; while you are talking to the father in the ER the child begins to have a seizure and dysrhythmia on the cardiac monitor. The blood gas demonstrates a severe metabolic acidosis. Which of the following agents is most likely the culprit?
A. Organophosphate
B. Chlorophenothane (DDT)
C. Sodium cyanide
D. Warfarin
E. Paraquat
22. An 8-year-old boy is brought to his physician by his mother, who is worried by the child's frequent episodes of daydreaming, which have apparently resulted in a decline in school performance. The child's psychomotor development appears normal. EEG recording reveals bilateral and symmetric 3 Hz spike-and-wave discharges, which begin and end abruptly on a normal background. Which of the following is the most likely diagnosis?
(A) Absence seizures (petit mal)
(B) Complex partial seizures
(C) Pseudoseizures
(D) Simple partial seizures
(E) Tonic-clonk seizures (grand mal)
23. A pregnant woman has premature rupture of membranes. Her baby is born 3 days later, at 37 weeks' gestation. The 5-minute APGAR score is 4. Lung sounds are reduced, and the infant appears to be in respiratory distress. Peripheral blood smear with differential counts demonstrates a neutrophil count of 30,000/mL, with toxic granules evident in many neutrophils. Gram stain of buffy coat demonstrates small gram-positive cocci in chains. Which of the following is the most likely causative organism?
(A) Group A Streptococcus
(B) Group B Streptococcus
(C) Methicillin-resistant Staphylococcus aureus
(D) Methicillin-sensitive Staphylococcus aureus
(E) Neisseria meningitides
24. A 15-year-old girl is seen in your clinic with a sprained ankle, which occurred the previous day while she was exercising in her room. You realize that you have not seen her for quite some time, and begin to expand your examination beyond the ankle. You find relatively minimal swelling on her right ankle. She has dental decay, especially of anterior teeth and a swollen, reddened, irritated uvula. She seems to be somewhat hirsute on her arms and legs, but has thinning of her hair of the head. She has a resting heart rate of 60 beats per minute, and her oral temperature is 35.5°C (96θF). Further questioning suggests that she has developed secondary amenorrhea. Which of the following is the most appropriate next step in the management of this girl?
A. Human immunodeficiency virus (HIV) testing
B. Radiograph of ankle
C. Thyroid function panel
D. Comparison of current and past weights
E. Pregnancy testing
25. A 17-year-old sexually active girl comes to your office complaining of acne that is unresponsive to the usual treatment regimen. Physical examination reveals severe nodulocystic acne of her face, upper chest, and back. You consider prescribing isotretinoin (Accutane), but you are concerned about side effects. Reviewing the literature, you find which of the following to be true about isotretinoin?
A. Its efficacy can be profound and permanent.
B. It is not known to be a teratogen.
C. Most patients experience excessive tearing and salivation.
D. Severe arthritis necessitating cessation of the drug occurs in about 15% of patients. e. Significant decrease in serum triglyceride levels are noted in 25% of patients.
26. A 6-year-old boy has multiple, honey-colored, crusted lesions on his face, periungual areas, and forearms. The first lesion appeared 2 weeks ago on his philtrum. Since then the lesions have spread to his hands and arms. Each began as a small pustule on an erythematous base and eventually ruptured to form the crusted lesions now present. His temperature is 100.6 F, pulse is 100/min, and respirations are 14/min. The remainder of the physical examination is unremarkable. Which of the following is the most appropriate treatment?
(A) Clarithromycin
(B) Dicloxacillin
(C) Penicillin G
(D) Penicillin V
(E) Vancomycin
27. A 30-minute-old male newborn is noted to have central cyanosis. He was born to a 16-year-old white female at 28 weeks gestation. His respirations are rapid and shallow at 70/min. His other vital signs are stable. On examination, there is audible grunting, intercostal and subcostal retractions, nasal flaring, and duskiness. On auscultation, fine rales are heard over the lung bases. Nasal oxygenation does not improve his cyanosis. A chest roentgenogram shows fine reticular granularity, predominantly in the lower lobes. Arterial blood gas analysis shows evidence of hypoxemia and metabolic acidosis. What is the most likely diagnosis of this patient?
A. Transient tachypnea of the newborn
B. Hyaline membrane disease (HMO)
C. Persistent pulmonary hypertension of the newborn (PPHN)
D. Meconium aspiration syndrome
E. Lntracranial hemorrhage
28. A 16-year-old Asian boy presents with a two-day history of fever, malaise, and painful enlargement of his parotid glands. He has no significant past medical history. He was born in India, and has not received any childhood vaccinations. He recently returned from a one-week vacation in India. His vital signs are stable, except for a mild fever. Examination shows bilateral parotid enlargement. The rest of the examination is unremarkable. Which of the following organs is most likely to be affected by this patient's illness?
A. Testes
B. Pancreas
C. Liver
D. Kidney
E. Spleen
29. The parents of a 14-year-old boy are concerned about his short stature and lack of sexual development. By history, you learn that his birth weight and length were 3 kg and 50 cm, respectively, and that he had a normal growth pattern, although he was always shorter than children his age. The physical examination is normal and his growth curve is shown on the next page. His upper-to-lower segment ratio is 0.98. A small amount of fine axillary and pubic hair is present. There is no scrotal pigmentation; his testes measure 4.0 cm3 and his penis is 6 cm in length. In this situation, which of the following is the most appropriate course of action?
A. Measure pituitary gonadotropin
B. Obtain a computed tomographic (CT) scan of the pituitary area
C. Biopsy his testes
D. Measure serum testosterone levels
E. Reassure the parents that the boy is normal
30. Friends are considering adopting a “special needs” child from another country. The family has few details, but the information they have received so far suggests the 4-year-old child has had surgery for an endocardial cushion defect, is short for his age, and had a history of what sounds like surgically repaired duodenal atresia at birth. You are suspicious this child may have which of the following syndromes?
A. Kleinfelter
B. Waardenberg
C. Marfan
D. Down
E. Turner
31. The parents of a 1-month-old infant bring him to the emergency center in your local hospital for emesis and listlessness. Both of his parents wanted a natural birth, so he was born at home and has not yet been to see a physician. On examination, you find a dehydrated, listless, and irritable infant. Although you don’t have a birth weight, the parents do not feel that he has gained much weight. He has significant jaundice. His abdominal examination is significant for both hepatomegaly and splenomegaly. Laboratory values include a total bilirubin of 15.8 mg/dL and a direct bilirubin of 5.5 mg/dL. His liver function tests are elevated and his serum glucose is 38 mg/dL. Serum ammonia is normal. A urinalysis is negative for glucose, but it has a “mouse-like” odor. These findings are consistent with which of the following conditions?
A. Homocystinuria
B. Maple syrup urine disease
C. Galactosemia
D. Ornithine transcarbamylase deficiency
E. Phenylketonuria
32. An 8-year-old African American boy is brought in for evaluation of a mass on the scalp. On examination, he is afebrile and nontoxic. There is a boggy mass on his scalp with alopecia. His posterior cervical lymph nodes are enlarged but nontender. Which of the following is the most appropriate treatment?
(A) incision and drainage
(B) oral amoxicillin
(C) IV naficillin
(D) selenium sulfide shampoo twice a week
(E) oral griseofulvin and selenium sulfide shampoo twice weekly
33. A 4-year-old child presents to your office in July with a history of a low-grade fever (38.1°C) and “sores” in his mouth for 2 days. He has been refusing to eat but has been drinking an adequate amount of liquids. On examination, he is afebrile and seems well hydrated. He has ulcers on his tongue and posterior pharynx, which are 4 mm in diameter. You also note a few vesicles on his hands and feet, which are 3–4 mm in size and mildly tender. Which of the following is the most likely diagnosis?
(A) herpes simplex virus (HSV)
(B) coxsackie virus
(C) aphthous ulcers
(D) Behçet syndrome
(E) traumatic ulcers
34. A 6-year-old obese girl is brought to the clinic by her mother, who is concerned that the child does not exercise and constantly eats. The mother has tried to enroll her in gym and fitness classes, but without success. The mother seems helpless and asks for your help. Which of the following is not a complication of obesity later in life?
A Slipped capital femoral epiphysis
B. Type I diabetes
C. Hypertension
D. Decreased self esteem
E. Uterine cancer
35. After an uneventful labor and delivery, an infant is born at 32 weeks’ gestation weighing 1500 g (3 lb, 5 oz). Respiratory difficulty develops immediately after birth and increases in intensity thereafter. At 6 hours of age, the child’s respiratory rate is 60 breaths per minute. Examination reveals grunting, intercostal retraction, nasal flaring, and marked cyanosis in room air. Auscultation reveals poor air movement. Physiologic abnormalities compatible with these data include which of the following?
A. Decreased lung compliance, reduced lung volume, right-to-left shunt of blood
B. Decreased lung compliance, increased lung volume, left-to-right shunt of blood
C. Normal lung compliance, reduced lung volume, left-to-right shunt of blood
D. Normal lung compliance, increased lung volume, right-to-left shunt of blood
E. Decreased lung compliance, reduced lung volume, left-to-right shunt of blood
36. You have been recently named as the medical director of the normal newborn nursery in your community hospital and have been asked to write standardized admission orders for all pediatricians to follow. Which of the following vaccines will you include on these orders?
A. Hepatitis A vaccine
B. Hepatitis B vaccine
C. Combination diphtheria, tetanus, and acellular pertussis vaccine
D. Inactivated polio virus
E. Haemophilus influenza B vaccine
37. A 30-minute-old male newborn is noted to have central cyanosis. He was born to a 16-year-old white female at 28 weeks gestation. His respirations are rapid and shallow at 70/min. His other vital signs are stable. On examination, there is audible grunting, intercostal and subcostal retractions, nasal flaring, and duskiness. On auscultation, fine rales are heard over the lung bases. Nasal oxygenation does not improve his cyanosis. A chest roentgenogram shows fine reticular granularity, predominantly in the lower lobes. Arterial blood gas analysis shows evidence of hypoxemia and metabolic acidosis. What is the most likely diagnosis of this patient?
A. Transient tachypnea of the newborn
B. Hyaline membrane disease (HMD)
C. Persistent pulmonary hypertension of the newborn (PPHN)
D. Meconium aspiration syndrome
E. Intracranial hemorrhage
38. A 9-year-old girl is seen in the office for unsteady gait and weakness in the lower limbs. On examination she is found to have a wide-based gait with constant shifting of position to maintain her balance. There is decreased vibratory and position sense in the lower extremities, and ankle jerks are absent bilaterally. Her feet are deformed with high plantar arches. MRI of the brain and spinal cord shows marked atrophy of the cervical spinal cord and minimal cerebellar atrophy. Nerve conduction velocity results are within normal limits. EKG shows T-wave inversions in the inferior and lateral chest leads. The mother says that her other child, a 3-year-old boy, is completely normal. He shares toys with his sister and plays well with other children at playschool. He is able to copy squares and crosses but is unable to copy a triangle. Which of the following statements would you advance while discussing the girl's condition with her mother?
A. There is nothing to worry about since it's a non-progressive condition
B. It is most likely a result of spontaneous mutation & the chances of your boy developing the same condition are minimal
C. The EKG abnormalities are most likely due to myocardial ischaemia
D. The inability of your boy to copy a triangle worries me since it may be an early manifestation of the same condition your daughter is suffering from
E. I advise you to go for prenatal counseling if you desire any future pregnancies

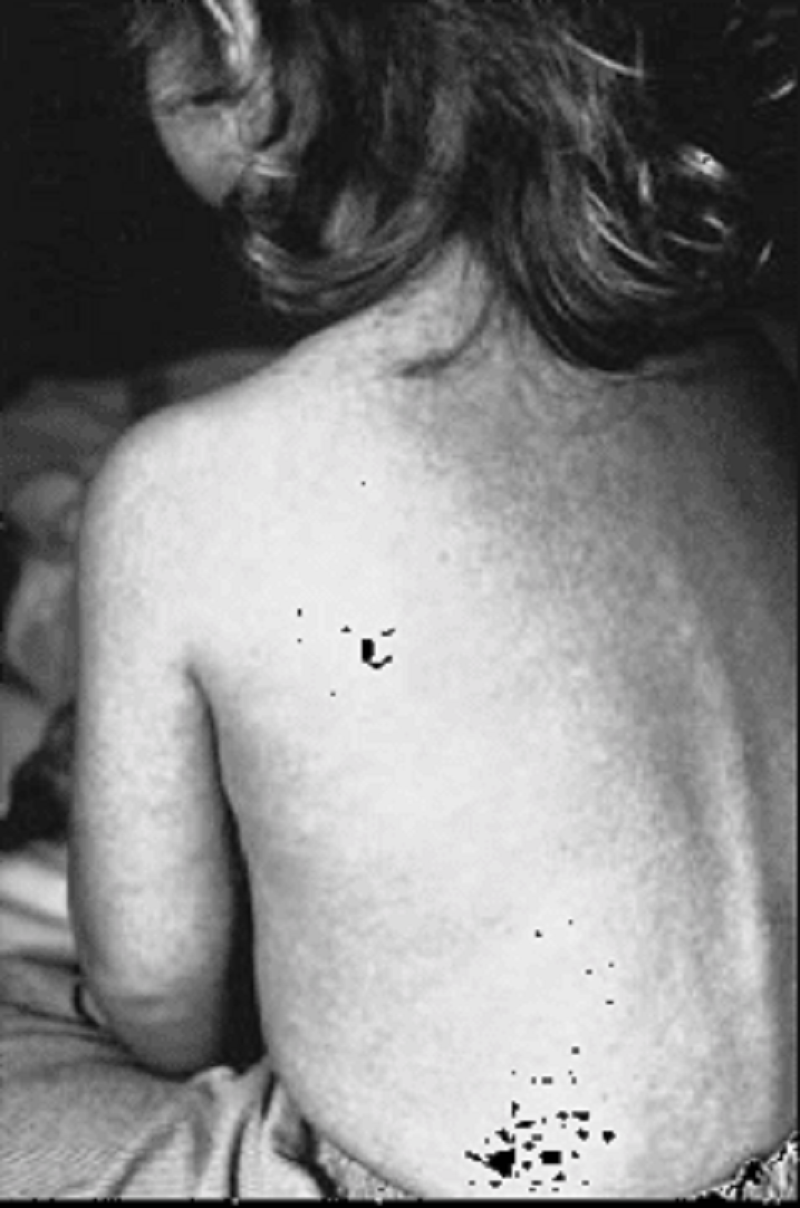
39. A 10-year-old patient (pictured below) calls his parents from summer camp to state that he has had fever, muscular pain (especially in the neck), headache, and malaise. He describes the area from the back of his mandible toward the mastoid space as being full and tender and that his earlobe on the affected side appears to be sticking upward and outward. Drinking sour liquids causes much pain in the affected area. When his father calls your office, you remind him that he had refused immunizations for his child on religious grounds. Which of the following preventable diseases has this child acquired?
A. Mumps
B. Varicella
C. Rubella
D. Measles
E. Diphtheria
40. A healthy 1-year-old child comes to your office for a routine checkup and for immunizations. His parents have no complaints or concerns. The next day, the CBC you performed as customary screening for anemia returns with the percentage of eosinophils on the differential to be 30%. Which of the following is the most likely explanation?
A. Bacterial infections
B. Chronic allergic rhinitis
C. Fungal infections
D. Helminthinfestation
E. Tuberculosis
41. A 1400-g infant, born at 35 weeks' gestation, is 42 cm in length and a head circumference of 28 cm. One day after birth, she becomes very irritable, tremulous, and inconsolable. Her cry is high-pitched. Her pulse is 174/min. There are no dysmorphic facial features. To which of the following substances was this newborn most likely exposed in utero?
A. Alcohol
B. Barbiturates
C. Cocaine
D. Marijuana
E. Opiates
42. A 9-month-old infant is seen in the pediatrician's office because of failure to gain weight. Her length and weight are both below the 5th percentile at her age. The patient's chart indicates that at the age of age of 6 months, her length and weight were at the 50th percentile. A careful history reveals that the mother returned to work when the infant was 6 months old, and the grandmother assumed the care of the infant most of the time since then. She is receiving 6-8 oz of iron-fortified, cow protein-based formula every 4 hours. Which of the following is the best initial step in the management of this infant?
A. Ask how the formula is mixed
B. Obtain a detailed family history for lactose intolerance
C. Obtain a stool specimen
D. Obtain a sweat chloride test
E. Obtain a urinalysis

A very upset mother brings her 8-month-old child to the emergency room because he will not move his leg. She reports that when she was carrying him to the car about half an hour ago, she slipped on some ice and fell on top of him. The mother, an 18-year-old African American woman, has been exclusively breast-feeding her child. She has only recently started him on cereals, and has not supplemented his diet with vitamins. A radiograph of the child’s leg is shown below. Which of the following laboratory findings would be expected?
A. Hypocalcemia
B. Hypophosphaturia
C. Reduced serum alkaline phosphatase
D. Hypocalciuria
E. Hyperphosphatemia
44. A small-for-gestational-age infant is born at 30 weeks’ gestation. At 1 hour of age, his serum glucose is noted to be 20 mg/dL (normally greater than 40 mg/dL). Which of the following is the most likely explanation for hypoglycemia in this infant?
A. Inadequate stores of nutrients
B. Adrenal immaturity
C. Pituitary immaturity
D. Insulin excess
E. Glucagondeficiency
45. A 30-hour-old infant has not passed meconium since birth. He was full term with a birth weight of 3856 g (8 lb 8 oz). The pregnancy was uncomplicated. The baby appears well with no respiratory distress. Slight abdominal distention is noted. Rectal examination reveals a slightly tight rectum and results in a greenish gush of stool. Which of the following tests will probably confirm the likely diagnosis?
A. A stool culture
B. A rectal biopsy
C. A barium enema
D. An alpha1-antitrypsin level
E. A serum TSH level
46. A 2-month-old girl presents to her pediatrician's office for well-child care. Her mother complains of excessive tearing of the baby's left eye for the past 4 weeks. Each morning, a yellow crusty discharge is noted along the lashes of the left eye. The conjunctiva appears uninflamed. The right eye is not affected. On physical examination, the infant is otherwise well and achieving adequate weight gain on an exclusive breast milk diet. She is developmentally appropriate, including visually tracking 180 degrees. Which of the following is the most likely diagnosis?
(A) Dacryostenosis
(B) Gonococcal conjunctivitis
(C) Normal infant eye
(D)Viral conjunctivitis
(E)Vitamin A deficiency
47. A primiparous woman whose blood type is O positive gives birth at term to an infant who has A-positive blood and a hematocrit of 55%. A total serum bilirubin level obtained at 36 hours of age is 12 mg/dL. Which of the following additional laboratory findings would be characteristic of ABO hemolytic disease in this infant?
A. A normal reticulocyte count
B. A positive direct Coombs test
C. Crescent-shaped red blood cells in the blood smear
D. Elevated hemoglobin
E. Petechiae
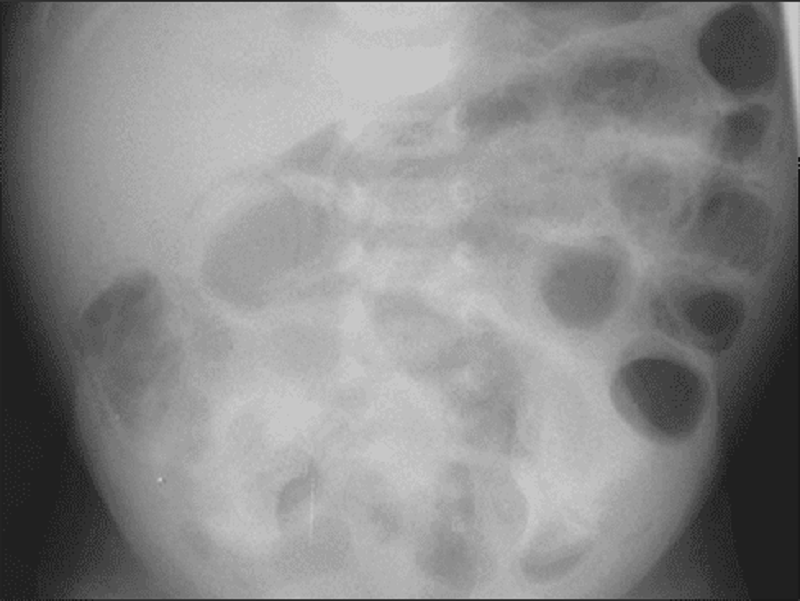
48. The nurse from the level 2 neonatal intensive care nursery calls you to evaluate a baby. The infant, born at 32 weeks’ gestation, is now 1 week old and had been doing well on increasing nasogastric feedings. This afternoon, how- ever, the nurse noted that the infant has vomited the last two feedings and seems less active. Your examination reveals a tense and distended abdomen with decreased bowel sounds. As you are evaluating the child, he has a grossly bloody stool. The plain film of his abdomen is shown. The next step in your management of this infant should include which of the following?
A. Surgical consultation for an emergent exploratory laparotomy.
B. Continued feeding of the infant, as gastroenteritis is usually self-limited.
C. Stool culture to identify the etiology of the bloody diarrhea and an infectious diseases consultation.
D. Stopping feeds, beginning intravenous fluids, ordering serial abdominal films, and initiating systemic antibiotics.
E. Removal of nasogastric tube, placement of a transpyloric tube and, after confir-mation via radiograph of tube positioning, switching feeds from nasogastric to nasoduodenal.
49. A term neonate is small for date and has a small head. Further physical examination of the infant demonstrates small eyes with short palpebral fissures, a flattened nose, and abnormal palmar creases. With which of the following maternal conditions is this presentation most likely associated?
(A) Alcohol abuse
(B) Cirrhosis
(C) Cocaine abuse
(D) Diabetes mellitus
(E) Hypothyroidism
50. The parents of a 3-year-old patient followed in your clinic recently took their child on quickly planned 5-day trip to Africa to visit an ill grandparent. Everyone did well on the trip, but since their return about 10 days ago the boy has been having intermittent, spiking fevers associated with headache, sweating, and nausea. The parents had not been too concerned since he was relatively well, except for being tired, between the fevers. Today, however, they feel that he looks a bit pale and his eyes appear “yellow.” Which of the following is likely to reveal the source of his problem?
A. Hepatitis A IgG and IgM titers
B. Complete blood count (CBC) with smear
C. Hemoglobin electrophoresis
D. Tuberculosis skin test
E. Hepatitis B IgG and IgM titers
51. A 15-year old girl presents with a 5-day history of sore throat, low-grade fever, and easy fatigability. Physical examination shows bilateral tonsillar enlargement with exudate. Her spleen is palpable 3 cm below the left costal margin. Her throat culture is negative for group A Streptococcus. Monospot test is positive. Which of the following is the most appropriate management for this patient?
(A) Abdominal ultrasound
(B) Avoidance of all contact sports
(C) Complete blood count
(D) Oral penicillin
(E) Splenectomy
52. A 4-year-old girl is brought to the office due to seizures that occurred 2 hours ago. This is her first episode. Her parents are also concerned because she is not able to carry on activities that children of her age are expected to do. On examination, there is a red flat lesion covering the left eye area and adjacent facial skin, which does not blanch on pressure, and which the parents say has been present since birth. Other pertinent findings are hemianopia, hemiparesis, and hemisensory disturbances. An x-ray of the skull shows tramline intra-cranial calcifications. What is the most likely diagnosis?
A. Sturge-Weber syndrome
B. Tuberous sclerosis
C. Capillary hemangioma
D. Epilepsy
E. Neurofibromatosis
53. An infant is born to a woman who has received very little prenatal care. The mother is anxious, complains of heat intolerance and fatigue, and reports that she has not gained much weight despite having an increased appetite. On examination the mother is tachycardic, has a tremor, and has fullness in her neck and in her eyes. The infant is most likely at risk for development of which of the following?
A. Constipation
B. Heart failure
C. Macrocephaly
D. Third-degree heart block
E. Thrombocytosis
54. An otherwise healthy 7-year-old girl is brought to your office by her father because she has some acne, breast development, and fine pubic hair. Which of the following is the most likely etiology for her condition?
A. A feminizing ovarian tumor
B. A gonadotropin-producing tumor
C. A lesion of the central nervous system (CNS)
D. Exogenous estrogens
E. Early onset of “normal” puberty (constitutional)
55. A 10-day-old infant is brought to the office by her mother for the evaluation of purulent discharge from both eyes. The discharge appeared three days ago, after which the child developed a cough. On examination, the infant's eyes appear normal, except for the presence of purulent discharge. Auscultation reveals diffuse rales without wheezing. Chest radiograph shows a hyperinflated thorax. What is the most likely diagnosis?
A. Gonococcal conjunctivitis
B. Chemical conjunctivitis
C. Congenital chlamydial infection
D. Congenital rubella infection
E. Adenovirus infection
56. A 14-year-old girl presents to clinic for an annual check up. Her parents are concerned that the child is not meeting normal milestones of adolescent growth. The patient reports no recent illnesses. She is up-to-date on her vaccines, and is not having any trouble in school. She denies drug use and is active in sports. On examination, her vital signs are stable. Her lungs are clear and heart is regular in rate and rhythm. Breast and areolar enlargement is noted with no contour separation of the areola. Pubic hair is noted to be dark. The patient also reports that she started menstruating 8 months ago. Which of the following is the most likely Tanner stage of development in this patient?
A. Stage I
B. Stage II
C. Stage III
D. Stage IV
E. Stage V
57. A 3-day-old infant, born at 32 weeks’ gestation and weighing 1700 g (3 lb, 12 oz), has three episodes of apnea, each lasting 20 to 25 seconds and occurring after a feeding. During these episodes, the heart rate drops from 140 to 100 beats per minute, and the child remains motionless; between episodes, however, the child displays normal activity. Blood sugar is 50 mg/dL and serum calcium is normal. Which of the following is most likely true regarding the child’s apneic periods?
A. They are due to an immature respiratory center.
B. They are a part of periodic breathing.
C. They are secondary to hypoglycemia.
D. They are manifestations of seizures.
E. They are evidence of underlying pulmonary disease.
58. You have an 11-day-old term infant in your office for a well-child visit. The mother notes that she received a letter that day from the state’s Department of Health reporting that her child’s newborn screen had come back abnormal, indicating possible galactosemia. Which of the following is the most appropriate management at this point?
A. Discontinue oral feeds and begin total parenteral nutrition.
B. Supplement her breast-feeding with a multivitamin.
C. Refer to endocrinology for evaluation.
D. Discontinue breast-feeding and initiate soy formula feedings
E. Ultrasound of pancreas.
59. A 3-week-old female infant born at 38 weeks' gestation through an uncomplicated vaginal delivery, presents to the emergency department with 2-day history of fever. The infant had been healthy since birth. Her temperature in the emergency department is 40.0 C (104.0 F). She appears to be quite lethargic. A culture taken from the infant grows group B Streptococcus (GBS) in 24 hours. Which of the following infections is most consistent with this presentation?
A. Endocarditis
B. Gastroenteritis
C. Meningitis
D. Pneumonia
E. Pyelonephritis
60. A 9-year-old boy is being evaluated for a syncopal episode. He was playing basketball when the syncope occurred. The episode lasted about 1-2 minutes, and then the patient woke up on his own. His mother also noticed that he has been having hearing problems. His physical examination is unremarkable. An ECG shows a prolonged Q-T interval, with a QTc of 0.49 sec. Which of the following is the most appropriate management if he has long Q-T syndrome?
A. Alpha-adrenergic blocker
B. Angiotensin converting enzyme inhibitor
C. Beta-adrenergic blocker
D. Calcium channel blocker
E. Diuretic
61. A 4-year-old child has mental retardation, shortness of stature, brachydactyly (especially of the fourth and fifth digits), and obesity with round facies and short neck. The child is followed by an ophthalmologist for subcapsular cataracts, and has previously been noted to have cutaneous an subcutaneous calcifications, as well as perivascular calcifications of the basal ganglia. This patient is most likely to have which of the following features?
A. Hypercalcemia
B. Hypophosphatemia
C. Elevated concentrations of parathyroid hormone
D. Advanced height age
E. Decreased bone density, particularly in the skull
62. A 1-day-old normal-appearing infant develops tetany and convulsions. He was born at 34 weeks’ gestation with Apgar scores of 2 and 4 (at 1 and 5 minutes, respectively) to a woman whose pregnancy was complicated by diabetes mellitus and pregnancy-induced hypertension. Which of the following serum chemistry values is likely to be the explanation for his condition?
A. Serum bicarbonate level of 22 mEq/dL
B. Serum calcium of 6.2 mg/dL
C. Serum glucose of 45 mg/dL
D. Serum magnesium level of 5.0 mg/dL
E. Intracranial hemorrhage
63. An 11-month-old girl is brought by her mother to the office due to fever, fussiness, and irritability. The girl has a tendency to hold and pull on her left ear. For the past few days, she has had rhinorrhea and nasal congestion. Her medical history reveals nothing particular. Her temperature is 38.9C (102F). Otoscopic examination reveals a bulging, erythematous tympanic membrane with decreased mobility on air compression. What is the most likely organism responsible for the patient's condition?
A. Haemophilus influenzae
B. Streptococcus pneumoniae
C. Moraxella catarrhalis
D. Pseudomonas aeruginosa
E. Group A Streptococcus
64. A 2 and a half-year-old child is brought to the office for the evaluation of easy bruising, nosebleeds, and decreased activity over the past week. He had an upper respiratory infection that was treated with an antibiotic 2 weeks ago. On examination, he is well-developed, seems well-nourished, anicteric, and pale. Pertinent findings include some small palpable posterior cervical lymph nodes, sinus tachycardia, a grade I/VI systolic ejection murmur, ecchymoses on his left shoulder and both lower extremities, and petechiae over his extremities and groin. There is no hepatosplenomegaly. The laboratory findings are as follows: Hemoglobin 7.9 g/dl Hematocrit 24% Platelet count 12, 000/mm3 WBC 3,000/mm3 Reticulocyte count 0.5% A bone marrow biopsy reveal a markedly hypocellular marrow with decreased megakaryocytes and precursors of the erythroid and myeloid cell lines. What is the most likely diagnosis?
A. Acquired aplastic anemia
B. Fanconi's anemia
C. Diamond-Biackfan anemia
D. Transient erythroblastopenia
E. Acute myeloid leukemia
65. A 10-year-old boy is brought to clinic because of increasing weakness and dyspnea over the past 6 months. He has been previously healthy and is on no medications. There is no significant family history of illness. On examination, he appears pale. His hematocrit is 20%, mean corpuscular volume (MCV) is 60/um3, and iron level is normal. Smear reveals basophilic stippling. Hemoglobin electrophoresis is consistent with the absence of one beta-globin gene. Which of the following is the most likely diagnosis?
(A) EUiptocytosis
(B) Hemoglobin S-C disease
(C) Porphyria
(D) Sickle cell disease
(E) Thalassemia
66. The child shown below presents with a 3-day history of malaise, fever to 41.1θC (106θF), cough, coryza, and conjunctivitis. He then develops the erythematous, maculopapular rash pictured. He is noted to have white pinpoint lesions on a bright red buccal mucosa in the area opposite his lower molars. Which of the following is the most likely diagnosis?
A. Parvovirus
B. Rubella
C. Herpes
D. Rubeola
E. Varicella
67. A 3-month-old girl is brought to the pediatrician for a scheduled visit. She has been meeting all development milestones but has been vomiting after each feeding. The infant weighed 3 kg (6 lb 10 oz) at birth and now weighs 6 kg (13 lb 3 oz). She does not have diarrhea and is afebrile. The remainder of the physical examination is unremarkable. Which of the following is the most likely cause of this patient's vomiting?
(A) Adrenogenital syndrome
(B) Child abuse
(C) Inborn error of metabolism
(D) Overfeeding
(E) Pyloric stenosis
68. A neonate is noted to have aniridia of the right eye on physical examination. He was born by spontaneous vaginal delivery after an uncomplicated full-term pregnancy. The remainder of the physical examination is normal. Which of the following is the most appropriate next step before the infant is released from the hospital?
(A) An abdominal ultrasound
(B) An echocardiogram
(C) A neurology consult
(D) A rapid plasmin reagin (RPR) test
(E) TV antibiotics
69. A 7-year-old boy presents to the physician's office with a 3-week history of left-sided anterior cervical lymph node enlargement. The enlarged nodes are not tender to palpation. A few papules developed on the left forearm at the onset of lymphadenopathy. The boy has a kitten at home. Which of the following is the most likely organism causing lymphadenopathy in this child?
A. Actinomyces israelii
B. Bartonella henselae
C. Francisella tularensis
D.Mycobacterium tuberculosis
E.Staphylococcus aureus
70. A 28-year-old Caucasian female comes to the office due to fever for the past 3 days. She also complains of pain and swelling in her right breast for the past 4 days. She exclusively breastfeeds her 3-month-old baby. On examination, she is febrile. Her right breast is engorged, red and tender, without any area of fluctuation. She wants to know if she can continue to breastfeed. Which of the following is a contraindication to breastfeeding?
A Mastitis
B. Acquired immune deficiency syndrome
C. Maternal rubella infection
D. Breast milk jaundice
E. Hemolytic disease of the newborn
A female infant develops cyanosis. She was delivery vaginally at 43 weeks' gestation, and the amniotic fluid had a greenish color. She has dry, peeling skin, emaciated extremities and long fingernails. Tachypnea, nasal flaring, and sub- and intercostal retractions are observed. Auscultation reveals rales and rhonchi. The chest radiograph reveals flattening of the diaphragm, hyperinflation of the lungs, and patchy opacities diffusely distributed over both lung fields. Arterial blood gases reveal hypoxia and hypercarbia. What is most likely impairing the normal respiratory function of this newborn?
A. Fetal lung fluid
B. Poor alveolar compliance
C. Meconium
D. Paralysis of the diaphragm
E. Fibrosis of the lungs
72. A 10-year-old boy comes to the office with fever and chills for 5 days and myalgia. He has recently returned from a 2-week vacation to New England with his family. On physical examination he has mild splenomegaly. Which of the following is the most likely cause of his symptoms?
(A) Kawasaki disease
(B) pneumococcus
(C) babesiosis
(D) leptospirosis
(E) psittacosis

73. A 3-week-old infant with hypoplastic left heart syndrome comes to the physician for a follow- up visit. The infant was born at term via normal spontaneous vaginal delivery. The patient had the first of 3 palliative heart surgeries shortly after birth. He did well after surgery and was discharged home one week ago. Over the last 24 hours, the infant has difficulty feeding and one episodes of vomiting. On examination, the infant is afebrile, pulse is 160/min, respiratory rate is 55/min, blood pressure is 90/50mmHg, and pulse oximetry is 80% on room air. He is mildly cyanotic, small, but well developed. His cardiovascular exam reveals tachycardia and distant heart sounds with a systolic ejection murmur heard throughout the precordium. His chest radiographs from discharge and today are shown below. What is the most likely diagnosis ?
A. Congestive heart failure
B. Endocarditis
C. Pleural effusion
D. Pericardial effusion
E. Myocarditis
74. A 4-year-old female is brought to the emergency department for evaluation of vaginal discharge. She has had foul-smelling vaginal discharge for 1 week. Her mother has also noted a small amount of vaginal bleeding. The mother called her primary physician and was told to use an over-the-counter cream and to stop letting the child take bubble baths. However, the symptoms have not improved. The child complains of pruritis in her vaginal area. She was potty trained at age 2. While mother is at work, the baby is with her stepfather. On examination, the perineal area is erythematous with a purulent, foul-smelling vaginal discharge. Visual inspection of the vagina reveals a greenish foreign body inside the vagina. Which of the following is the next best step?
A. Irrigation with warmed fluid
B. Bimanual examination under general anesthesia
C. Cultures for gonorrhea and chlamydia
D. Notify Child Protective Services immediately
E. CT scan of the pelvis
75. A 5-month-old boy is brought in for a routine check-up. He was born at 37 weeks' gestation and has had persistent wheezing since shortly after birth despite inhaled bronchodilator and oral corticosteroid therapy. His diet consists of 32 ounces of iron-fortified cow's milk-based formula daily. On physical examination, the child appears well-nourished and happy. You note moderate relief of his wheezing with neck extension. Which of the following is the most likely mechanism of this infant's wheezing?
A. Allergic reaction to cow's milk
B. Aspiration of a foreign body
C. Compression of the airway by a vascular ring
D. Chronic upper respiratory tract infection
E. Asthma
76. A mother calls you frantic because she has just been diagnosed with chicken pox. She delivered 7 days ago a term infant that appears to be eating, stooling, and urinating well. The child has been afebrile and seems to be doing well. Which of the following is the most appropriate step in management?
A. Isolate the infant from the mother.
B. Hospitalize the infant in the isolation ward.
C. Administer acyclovir to the infant.
D. Administer varicella-zoster immunoglobulin to the infant.
E. Advise the mother to continue regular well-baby care for the infant.
77. A mother wishes to breast-feed her newborn infant, but is worried about medical conditions that would prohibit her from doing so. You counsel her that of her listed conditions, which of the following is a contraindication to breast-feeding?
A. Upper respiratory tract infection
B. Cracked and bleeding nipples
C. Mastitis
D. Inverted nipples
E. HIV infection
78. A mother delivers a neonate with meconium staining and Apgar scores of 3 at 1 and 5 minutes of life. She had no prenatal care and the delivery was by emergency cesarean section for what the obstetricians report as “severe fetal bradycardia.”Which of the following sequelae could be expected to develop in this intubated neonate with respiratory distress?
A. Sustained rise in pulmonary arterial pressure
B. Hyperactive bowel sounds
C. Microcephaly with micrognathia
D. Cataracts
E. Thrombocytosis
79. A mother brings her 6-year-old daughter for evaluation because she has never been able to toilet train her. The child states that she perceives the sensation of having to void, and empties her bladder normally at normal intervals, but is nonetheless wet with urine all the time. Which of the following is the most likely diagnosis?
(A) Low implantation of one ureter
(B) Meatal stenosis
(C) Ureteropelvic junction obstruction
(D) Ureterovesical reflux
(E) Urethral valves
80. A neonate is noted to have an abnormally shaped face with a very small jaw. Several hours after birth, the baby develops convulsions and tetany. Serum chemistries show the following: Sodium 1 40 mEq/L Potassium 4 mEq/L Chloride 100 mEq/L Bicarbonate 24 mEq/L Magnesium 2 mEq/L Calcium 5 mg/dL Glucose 100 mg/dL This child's disorder is associated with aplasia or hypoplasia of which of the following organs?
(A) Ovaries
(B) Pancreas
(C) Pituitary
(D) Thymus
(E) Thyroid
81. A 10-year-old girl is brought to the physician because of throat pain, anorexia, and fever for 2 days. Her temperature is 38.9 C (102 F). The patient's history is negative for allergic diseases. She has had two episodes of pharyngotonsillitis over the past several years. Examination reveals a purulent exudate in the posterior oropharynx and enlarged tonsils. There is bilateral tender enlargement of anterior cervical lymph nodes. Cardiac and chest auscultation is normal. A rapid strep test is positive. Which of the following is the most appropriate next step in management?
(A) Confirmatory throat cultures before treatment
(B) Symptomatic treatment with nonsteroidal antiinflammatory drugs
(C) Symptomatic treatment and oral penicillin V
(D) Symptomatic treatment and a broad-spectrum cephalosporin
(E) Surgical referral for tonsillectomy
82. A 12-year-old girl is seen by a pediatrician for a mild case of pneumonia. She is treated with an intramuscular injection of penicillin. About 15 minutes later, she develops extreme itchiness, accompanied by the development of wheals scattered over her chest and extremities. She also begins to wheeze and complain of difficulty breathing. The color of her lips and face remains rosy. Which of the following is the most appropriate first step in management?
(A) Epinephrine injection
(B) IV corticosteroids
(C) Intubation
(D) Oral corticosteroids
(E) No specific therapy is needed
83. An 11-month-old boy is brought to the emergency department by his parents. The child has a fracture of the right femur. The father reports this was sustained as a result of falling out of the crib. The child is also noted to have bruises on his shoulders and back. The rest of his examination is unremarkable. Which of the following is the most appropriate next step in diagnosis?
(A) Social services consult
(B) Chest x-ray
(C) CT of the head
(D) Funduscopic exam
(E) Lumbar puncture
84. A 5-year-old boy is brought to the physician for evaluation of left hip pain after his parents saw him limping this morning. He spent time on the playground yesterday but his parents do not think he was injured then. The boy complains that the pain in his hip worsens when he moves or walks. For the past 3 days, he has had a runny nose and congestion. Review of systems is otherwise negative. His grandmother has rheumatoid arthritis treated with methotrexate. His temperature is 37.2° C (99° F), blood pressure is 100/65 mm Hg, pulse is 92/min, and respirations are 18/min. Physical examination shows a well-appearing child with clear rhinorrhea and intermittent dry cough. Lungs are clear to auscultation bilaterally. His left hip is slightly abducted and externally rotated with mildly decreased range of motion. He is able to stand and bear weight. The remainder of his examination is normal. X-rays of both hips are normal. His laboratory results are as follows: Complete blood count Hemoglobin 12.5 g/dL Platelets 287,000/mm3 Leukocyte count 8,500/mm3 Neutrophils 30% Eosinophils 1% Lymphocytes 64% Monocytes 5% Erythrocyte sedimentation rate 30 mm/h C-reactive protein 9 mg/L (N: ≤ 8 mg/L) Which of the following is the best next step in management of this patient?
A. Ibuprofen, rest, and follow-up in 1 week
B. Intravenous antibiotics
C. Magnetic resonance imaging of the left hip
D. Serum antinuclear antibodies
E. Synovial fluid aspiration of the left hip
85. A 2-day-old boy in the newborn nursery was born at 39 weeks gestation to a 38-year-old woman by vaginal delivery. The mother received epidural fentanyl for severe painful contractions during labor, but the delivery was uncomplicated. Since birth, the boy has shown little interest in breast or bottle feeding. He spit up the last feed but has not vomited. He has not yet passed meconium. Physical examination shows a newborn with generalized hypotonia, a flat facial profile, low-set folded earlobes, and a single transverse crease on each palm. His abdomen is firm and distended. Digital rectal examination is notable for a tight anal canal and relieves an expulsion of gas and stool. Abdominal x-ray shows markedly distended loops of bowel with no gas in the rectum. What is the mostly likely mechanism for his findings?
A. Constipation from decreased levels of thyroxine
B. Failure of neural crest cell migration during fetal intestinal development
C. Intestinal ileus from exposure to maternal epidural analgesia
D. Intestinal obstruction from inspissated meconium
E. Lnvagination of a part of the intestine into itself
86. A 6-day-old girl who was born at home is being evaluated for bruising and gastrointestinal bleeding. Laboratory findings include partial thromboplastin time and prothrombin time, greater than 2 minutes; serum bilirubin, 4.7 mg/dL; alanine aminotransferase, 18 mg/dL; platelet count, 330,000/mm3; and hemoglobin, 16.3 g/dL. Which of the following is the most likely cause of her bleeding?
A. Factor VIII deficiency
B. Factor IX deficiency
C. Idiopathic thrombocytopenic purpura
D. Liver disease
E. Vitamin K deficiency
87. A 7-year-old boy is brought to the clinic for a lifetime history of bedwetting. He has otherwise been completely healthy and has met all development milestones. His parents deny a history of trauma, and the history is not consistent with abuse. The patient has been wetting every night but not during the daytime. He has no incontinence. Which of the following is the most appropriate next step in his evaluation?
A. Intravenous pyelogram
B. Renal ultrasound
C. 24-hour urine collection
D. Urinalysis
E. CT of pelvis
88. A 1-year-old African American infant is in for well-child care. He is primarily breast-fed. His parents do not give him much solid food because he has no teeth. He receives no medications or supplements. His parents are concerned about his bowed legs. On examination, you note some other bony abnormalities including frontal bossing, enlargement of the costochondral junctions, a protuberant sternum (pigeon chest), and severe bowing of the legs. You obtain x-rays to confirm your clinical diagnosis and also note a healing fracture of the left femur. Which of the following is the most likely diagnosis?
(A) osteogenesis imperfecta
(B) scurvy
(C) congenital syphilis
(D) rickets
(E) chondrodystrophy
89. A 6-month-old infant is brought to the clinic for the evaluation of sudden episodes of jerky movements of the neck, arms, and legs onto the trunk for past month. These episodes occur in clusters, last for a few minutes, and are often preceded by a cry. Her development has been normal. Her vital signs are normal. She is at 50th percentile for height, weight and head circumference. She has multiple small 1-2 cm oval irregular hypopigmented macules on her trunk and extremities. A head CT scan reveals cortical tubers in the cerebral cortex and multiple subependymal nodules in the lateral ventricles. Her EEG shows "hypsarrhythmia." What is the best medication for this patient's seizure?
A. Vigabatrin
B. ACTH
C. Ethosuximide
D. Carbamazepine
E. Phenobarbital
90. A 3-week-old male infant is brought to the office for the evaluation of red eyes. His temperature is 37.2 C (99F), pulse is 100/min, and respirations are 34/min. On examination, the infant has conjunctival congestion and scant mucoid discharge. The rest of the physical examination is normal. What is the most appropriate next step in the management of this patient?
A Topical erythromycin
B. Topical silver nitrate
C. Topical steroids
D. Oral erythromycin
E. Oral tetracycline

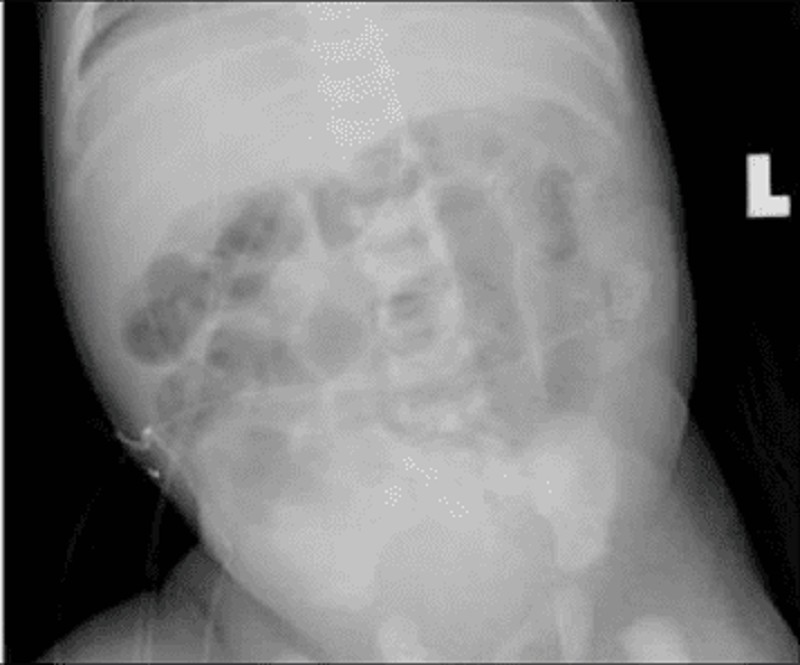
91. A 2-year-old boy is brought to the emergency department by his mother for the evaluation of a productive cough and low-grade fever. He has had ten such infections over the past year, all of which required antibiotics. He was delivered vaginally without any complications. He is an only child. His mother's siblings have a history of similar infections. He is alert and has normal vital signs, except for a mild fever. Auscultation reveals rales and rhonchi in both lungs. The chest x-ray is shown below. What is the most likely diagnosis ?
A.Cystic fibrosis
B.Foreign body
C.Kartagener's syndrome
D.Immunoglobulin deficiency
E.Congenital bronchiectasis
92. A 14-year-old boy presents with sudden onset of pain and swelling of his right testicle. There was no history of trauma, he is not sexually active, and denies any history of penile discharge. On examination, the scrotum is swollen and tender. The cremasteric reflex is absent. A testicular flow scan shows a “cold spot” or absent flow to the affected side. Which of the following is the most likely cause?
(A) inguinal hernia
(B) hydrocele
(C) epididymitis
(D) testicular torsion
(E) torsion of the appendix testis
93. Otitis media occurring during the first 8 weeks of life deserves special consideration, because the bacteria responsible for infections during this time may be different from those that affect older infants and children. Which of the following organisms is the most likely to cause otitis media in these infants?
(A) Chlamydia trachomatis
(B) E. coli
(C) Neisseria gonorrhoeae
(D) Treponema pallidum
(E) Toxoplasma gondii
94. Among the conditions that cause edema of the eyelids is orbital cellulitis. This is a serious infection that must be recognized early and treated aggressively if complications are to be avoided. Which of the following features is useful in differentiating orbital cellulitis from periorbital (preseptal) cellulitis?
(A) proptosis
(B) elevated WBC count
(C) fever
(D) lid swelling
(E) conjunctival inflammation

95. A 7-year-old boy was brought to the emergency department after falling onto his outstretched arm. He complains of pain in his left arm and refuses to move his arm at the elbow. On examination, the left arm is swollen, slightly pale, and edematous. His radial pulse is intact. The patient's radiograph is shown below. While the patient is waiting for the orthopedic resident on call to examine him, he continues to complain of increasing pain despite multiple doses of pain medication. Which of the following should you be most concerned about in this patient?
A. Displacement of the fracture
B. Transient neuropraxia
C. Brachial artery injury
D. Compartment syndrome
E. Narcotic abuse
96. A 9-year-old male is brought to the emergency department with respiratory disease after being stung by a bee. He requires resuscitation with epinephrine injection. On discharge, which of the following recommendations to the boy's mother is most appropriate?
A. Do not allow him to play outside
B. Wear colorful clothes while outside
C. Give prophylactic antihistamine agents daily
D. Provide epinephrine to carry with him
E. Use insect repellants
97. A 1-year-old boy is brought to the physician by his parents for evaluation of bruising and blood in his stool. The child has had multiple episodes of otitis media and has been hospitalized twice with pneumonia, but has never had bleeding or easy bruising in the past. He has been eating and drinking well with no vomiting or diarrhea. He is afebrile with a heart rate of 150/min and a blood pressure of 80/40 mmHg. On examination, he is well-developed, well-nourished, and has a fair complexion. There are dry, scaly patches on his cheeks and lower extremities. He also has bruising and purpura on his lower extremities. His diaper contains a small amount of occult blood positive stool, but no fissures are seen on rectal examination. The remainder of the physical examination is unremarkable. Laboratory studies show: Complete blood count Hemoglobin 11 .5 g/dL Platelet count 20,000/mm3 Leukocyte count 6,500/mm3 Neutrophils 76% Eosinophils 1% Lymphocytes 13% Monocytes 10% A peripheral smear reveals a low number of platelets, and the platelets that are seen are small. Which of the following is the most likely cause of his bleeding?
A. Bone marrow infiltration
B. Platelet antibodies
C. Nutritional deficiency
D. Platelet activation and consumption
E. Impaired platelet production

98. The developmentally delayed 6-month-old child in the picture below had intrauterine growth retardation (including microcephaly), hepatosplenomegaly, prolonged neonatal jaundice, and purpura at birth. The calcific densities in the skull x-ray shown are likely the result of which of the following?
A. Congenital cytomegalovirus (CMV) infection
B. Congenital toxoplasmosis infection
C. Congenital syphilis infection
D. Tuberculous meningitis
E. Craniopharyngioma
99. The infant pictured below develops infantile spasms. Which of the following disorders is most likely to be affecting this infant?
A.Neurofibromatosis
B. Tuberous sclerosis
C. Incontinentiapigmenti
D. Pityriasis rosea
E. Psoriasis
100. A 7 -year-old Caucasian boy is brought to the clinic due to malaise and headache for the past 2 weeks. He was apparently normal until 3 weeks ago, when he went on a hiking trip with his family to Connecticut. His father found a tick attached to his thigh; however, a red macule remains at the site where the tick was attached. One week after the tick was removed, a red ring developed around the macule, and then the ring appeared to grow larger by expanding outward, leaving an area of central clearing. What is the most appropriate next step in the management of this patient?
A Doxycycline
B. Amoxicillin
C. Ceftriaxone
D. Penicillin G
E. Erythromycin
{"name":"Pediatric USMLE 1-100", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"1. A 16-year-old female presents to the emergency room with severe right- sided abdominal pain. Her last menstrual period was 2 weeks ago and felt to be normal. She displays painful difficulty in positioning herself on the examination table. Her temperature is 38.5 C (101.3 F), blood pressure is 128\/75 mm Hg, pulse is 80\/min, and respirations are 22\/min. Examination of the throat reveals mild pharyngitis. Her abdomen is diffusely tender, especially the lower abdomen. Rectal examination reveals tenderness anteriorly on the right side. Stool guaiac is negative. A pelvic examination is performed, and there is evidence of cervical tenderness and questionable fullness in the right adnexal area. Which of the following is the most likely diagnosis?, 2. Your sister who lives in another state sends via e-mail photographs of her 6-month-old infant. You note the child has a white reflection from one of his eyes. You hastily assist in arranging an urgent pediatric ophthalmologic evaluation. Your sister immediately accesses the Internet and begins to ask questions of you. Which of the following statements found by your sister is correct?, 3. A 2950-g (6.5-lb) black baby boy is born at home at term. On arrival at the hospital, he appears pale, but the physical examination is otherwise normal. Laboratory studies reveal the following: mother’s blood type A, Rh-positive; baby’s blood type O, Rh-positive; hematocrit 38%; and reticulocyte count 5%. Which of the following is the most likely cause of the anemia?","img":"https://cdn.poll-maker.com/10-467285/10.png?sz=1200"}
More Quizzes
Where Should You Go For Spring Break?
630
SHEETMETAL & NON- SHEETMETALALIC STRUCTURE
130650
Understanding Condensation Quiz
5224
Would you survive
7427
Basic Car Knowledge - Can You Pass?
201017470
Commercial Insurance Questions - Free Policy
201017470
Am I Emo - Emo, Poser or Normal? Free Results
201018238
Maquiladora AP Human Geography - Free Industry Review
201021584
Who Should I Cosplay? - Get Your Character Match
201018779
Warrior Cats Clan: Which Clan Are You? - Free Results
201016904
5th Grade Volume Worksheets - Free Practice
201016443
Ultimate Star Wars - Episodes I - VI & The Clone Wars
201019909