DES C_Basic (5) Prepared : CHILLY
A 63-year-old male is admitted for sudden onset severe chest pain. His ECG reveals ST elevation in leads V2-V6. He is treated with thrombolytic therapy, heparin, aspirin, metoprolol, morphine, and nitrates. A coronary angiogram performed after thrombolytic therapy reveals 50% obstruction of the left anterior descending artery. On the third day of hospitalization, the patient suddenly develops severe shortness of breath at rest and hypotension. Examination reveals a soft S1, an apical pansystolic murmur radiating to the axilla, and bibasilar crackles. His temperature is 37.8°C (100°F), blood pressure is 92/58 mmHg, heart rate is 102/min, and respirations are 31/min. An echocardiogram performed on the second hospital day reveals an akinetic region of the anterior wall. What is the most likely explanation for this patient's deterioration?
Pericardial tamponade
Rupture of ventricular septum
Pulmonary embolism
Papillary muscle dysfunction
Acute aortic dissection
A 63-year-old man presents to the ER with substernal chest pain and diaphoresis. The pain stated one hour ago and did not remit with antacids. He has a past medical history of asthma for which he uses inhaled fluticasone and peptic ulcer disease for which he takes omeprazole. His family history is significant for prostate cancer in his father and breast cancer in his mother. Physical examination reveals a blood pressure of 160/100 mmHg and a heat rate of 90/min. A bruit is heard over the right carotid artery and a mild systolic murmur is present at the cardiac apex. Sublingual nitroglycerin and aspirin are administered in the. Within minutes, the patient reports decreased pain. Which of the following most likely accounts for this improvement in his symptoms?
Decreased left ventricular volume
Increased systemic afterload
Increased left ventricular compliance
Increased cardiac preload
Decreased left ventricular contractility
A 63-year-old man with a 40-pack per year smoking history undergoes a low anterior resection for rectal cancer and on postoperative day 5 develops a fever, new infiltrate on chest x-ray, and leukocytosis. He is transferred to the ICU for treatment of his pneumonia because of clinical deterioration. Which of the following is a sign of early sepsis?
Respiratory acidosis
Hypoglycemia
Decreased cardiac output
Increased arteriovenous oxygen difference
Peripheral vasodilation
A 63-year-old woman with a long history of hypertension faints after experiencing the sudden onset of severe chest pain that radiates to her back. She is rushed to the emergency room. Upon arrival she is agitated and demands quick pain relief. Her heart rate is 110/min and blood pressure is 90/50 mmHg. Jugular veins are distended. An intra-arterial catheter shows significant variation of systolic blood pressure related to the respiratory cycle. Chest x-ray reveals widening of the mediastinum. Which of the following is the most likely cause of this patient's syncope?
Papillary muscle dysfunction
Pericardial fluid accumulation
Intravascular volume loss
Vagal hyperactivity
Cardiac tachyarrhythmia
A 64-year-old man complains of palpitations and progressive shortness of breath over the past several hours. He says that he also develops a choking sensation every time he tries to lie down. His medical history is significant for hypertension for the past 20 years and medication non-compliance. He also has a 35-year smoking history. He reports that his father died of a heart attack at age 70 and his mother suffered from asthma. On physical examination, his blood pressure is 170/100 mmHg and his heat rate is 130/min and irregularly irregular. Lung exam reveals bibasilar crackles. There is 2+ pitting edema of the lower extremities. Bedside echocardiography shows a left ventricular ejection fraction of 55%. Which of the following is most likely responsible for his symptoms?
Cardiogenic shock
Small airway bronchoconstriction
High-output heat failure
Increased lung compliance
Diastolic dysfunction
A 64-year-old man presents to the emergency department with progressive exertional dyspnea that worsened after he contracted an upper respiratory infection. He also complains of bilateral ankle swelling. He has a 40 pack-year history of smoking. Physical examination reveals a mildly overweight patient in mild respiratory distress. Lung auscultation reveals bilateral wheezes and a prolonged expiratory phase. His white blood cell count is 14,500/mm3 and his hemoglobin level is 16 mg/dl. Arterial blood gas analysis reveals the following: pH 7.37, pO2 65mmHg, pCO2 60mmHg. Absence of marked acidosis in this patient is best explained by which of the following?
Increased minute ventilation
Pulmonary vasoconstriction
Increased dead space ventilation
Renal tubular compensation
Erythrocyte chloride shift
A 64-year-old woman is admitted to the hospital with right lobar pneumonia and sepsis syndrome. She becomes progressively more short of breath and hypoxemic requiring intubation and mechanical ventilation. Her repeat CXR in the intensive care unit now shows diffuse pulmonary infiltrates and a diagnosis of acute respiratory distress syndrome (ARDS) is made. Which of the following mechanisms is the most likely cause for the early exudative phase of ARDS?
Increased interstitial fibrosis
Decreased pulmonary perfusion
Increased lung compliance
Increased vascular permeability to fluid and proteins
Decreased ventilatory dead space
A 64-year-old woman presents to your office after falling in the grocery store earlier today. She says she was doing her usual shopping when she felt weak in her legs and fell down. She denies hitting her head, headache, or loss of consciousness, but does complain of low back pain. Her past medical history is significant for diabetes mellitus, hypertension, severe osteoporosis, chronic neck pain and congestive heart failure. She has had three transient ischemic attacks, each lasting 15-20 minutes and characterized by slurred speech, in the past. Her medications include insulin, lisinopril, carvedilol, alendronate, aspirin, and acetaminophen. Her blood pressure is 160/90 mmHg and her heart rate is 73/min. Physical exam reveals muscular weakness, increased deep tendon reflexes, and mildly decreased pinprick sensation in both lower extremities. Which of the following is most likely responsible?
Ischemic stroke
Spinal cord compression
Intracranial bleeding
Polyneuropathy
Neuromuscular junction disease
A 65-year-old bedridden woman is brought in with complaints of weight loss, weakness and malaise. Her past medical history includes chronic obstructive pulmonary disease (diagnosed fifteen years ago) and hypertension of ten years' duration. She quit smoking two years ago, but previously smoked three packs of cigarettes daily since she was 20 years of age. Her vital signs are stable. Her physical examination reveals severe weakness in her proximal muscles, and loss of deep tendon reflexes. Chest x-ray shows a right upper lung mass with mediastinal lymphadenopathy. Which of the following is the most likely cause of her weakness?
Multicentric CNS inflammation and demyelination
Antibodies to voltage gated calcium channels
Upper and lower motor neuron degeneration
Immune mediated muscle inflammation
Autoantibodies against post synaptic receptors
A 65-year-old Caucasian male had undergone cardiac catheterization followed by aortic valve replacement for severe aortic stenosis and coronary artery bypass grafting for three-vessel disease. His postoperative course was complicated by atrial fibrillation and a urinary tract infection. His other medical problems include hypertension, diabetes, and hypercholesterolemia. He is also receiving heparin, ciprofloxacin, and amiodarone. On postoperative day five, he developed prolonged bleeding from the venipuncture site. His labs show: Hb 11.5 g/dL, MCV88 fl, Platelet count 50,000/cmm, Leukocyte count 7,500/cmm, Segmented neutrophils 68%, Bands 1%, Eosinophils 1%, Lymphocytes 24%, Monocytes 6%, Prothrombin time 12 sec (INR=1.0), Partial thromboplastin time 65 sec. His preoperative labs were unremarkable. What is the most likely cause of these findings in this patient?
Thrombotic thrombocytopenic purpura
Idiopathic thrombocytopenia purpura
Hemolytic uremic syndrome
Vitamin deficiency
Medication effect
A 65-year-old Caucasian male presents to your office complaining of an episode of slurred speech and clumsiness of his right hand. The episode lasted 15 minutes and resolved spontaneously. He had a similar episode one week ago. His past medical history is significant for moderate hypertension, diabetes mellitus (OM) type 2 and osteoarthritis of the right knee. He has smoked one pack of cigarettes daily for 35 years, and drinks 1-2 glasses of wine daily. His current medications include metoprolol, glyburide and naproxen. His blood pressure is 160/95 mmHg, pulse is 65/min, respirations are 16/min, and temperature is 36.7°C (98°F). The physical findings are within normal limits. The lab studies show: Fasting blood glucose 200 mg/dl, Total cholesterol 240 mg/dl, LDL cholesterol 140 mg/dl, HDL cholesterol 76 mg/dl. What is the most important risk factor for a stroke in this patient?
Hypertension
Smoking
Elevated cholesterol level
Alcohol consumption
Diabetes mellitus
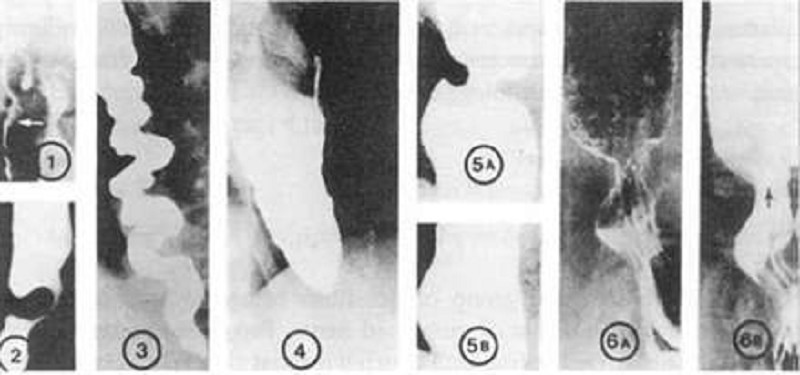
A 65-year-old Caucasian male presents to your office with a several month history of difficulty swallowing. He has noticed a right-sided neck mass which increases in size while drinking fluids. His past medical history is significant for hypertension, gastroesophageal reflux disease, and osteoarthritis of his right knee. His current medications include hydrochlorothiazide, ranitidine, and occasional naproxene. You order a barium examination of the esophagus to visualize the abnormality. Which of the following is the most important pathogenetic factor in the development of this patient's problem?
Motor dysfunction
Acid reflux
Inflammation
Abnormal proliferation
Metabolic abnormalities
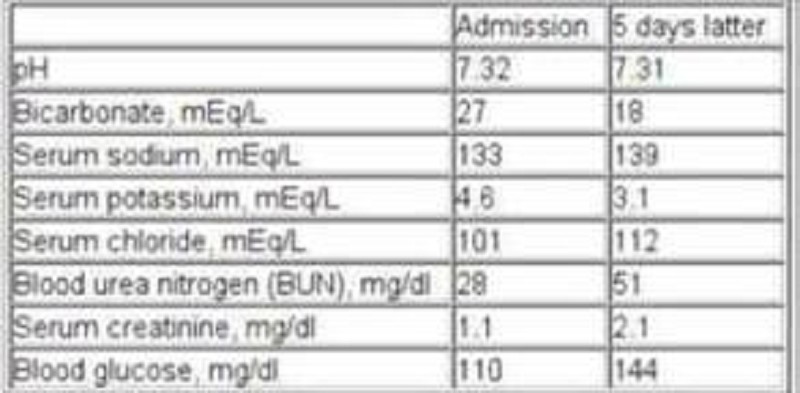
A 65-year-old chronic smoker presents to the hospital with increasing shortness of breath for the past few hours. He has been using albuterol occasionally, but it has not been helping him. He has been non-adherent to doctor's appointments and continues to smoke. He is afebrile. His oxygen saturation on room air is 86%. Examination shows elevated jugular venous pressure and lung auscultation reveals diffuse wheezing with no crackles. His heart sounds are muffled. Mild hepatomegaly and bilateral pitting pedal edema is present. Chest x-ray reveals hyperinflated lungs and a flattened diaphragm with no infiltrates. He is started on systemic steroids, bronchodilator nebulization and furosemide. His laboratory studies are shown below at the time of admission and five days later. Which of the following best explains the acid-base status change in this patient?
Acute renal failure
Glucocorticoid treatment
Development of ketoacidosis
Obstructive sleep apnea
Worsening respiratory failure
A 65-year-old diabetic man with a creatinine of 1.6 was started on an angiotensin-converting enzyme inhibitor for hypertension and presents to the emergency room with weakness. His other medications include atorvastatin for hypercholesterolemia, metoprolol and spironolactone for congestive heart failure, insulin for diabetes, and aspirin. Laboratory studies include: K: 7.2 mEq/L, Creatinine: 1.8 mg/dL, Glucose: 250 mg/dL, CK: 400 IU/L. Which of the following is the most likely cause of hyperkalemia in this patient?
Worsening renal function
Uncontrolled diabetes
Statin-induced rhabdomyolysis
Drug-induced effect on the renin-angiotensin-aldosterone system
High-potassium diet
A 65-year-old female complains of difficulty eating over the last two days. She states that food drops out of her mouth. She has also been having some discharge in her left ear recently. She denies any sore throat, nasal discharge, chest pain, cough, or difficulty breathing. Her past medical history is significant for type 2 diabetes mellitus, hypertension, and hyperlipidemia. She has been poorly complaint with follow-up appointments. Her temperature is 38.8°C (101.7°F), pulse is 96/min, blood pressure is 140/90 mmHg, and respirations are 18/min. Examination of the left ear canal shows granulations. There is facial asymmetry, and the angle of the mouth on the left is deviated downward. Which of the following is the most likely causative organism for this patient's condition?
Rhizopus species
Pseudomonas aeruginosa
Staphylococcus aureus
Aspergillus niger
Herpes zoster

A 65-year-old female presents with 6 months of worsening dyspnea and dry cough. Whereas she had previously enjoyed an active lifestyle, she now becomes breathless after walking just a few steps. The patient denies fever or chest pain and does not use tobacco, alcohol or illicit drugs. Her only medicine is hydrochlorothiazide for hypertension. She is retired and lives with her husband. She has never travelled abroad and denies any history of exposure to pets. On physical examination, her temperature is 37.2°C (98.9°F), blood pressure is 140/86 mm Hg, pulse is 84/min and respirations are 18/min. Examination shows dry, late inspiratory crackles and finger clubbing. Her chest x-ray is shown below. Which of the following abnormalities is most likely to be present in this patient?
Increased diffusing capacity of carbon monoxide
Increased residual volume
Increased PaCO2
Increased A-a gradient
Decreased FEV1/FVC ratio
A 65-year-old male comes to the physician's office after noticing blood in his urine. He denies any abdominal pain or dysuria. He denies any recent illness. The review of systems is otherwise unremarkable. His past medical history is significant for hypertension and a transient ischemic attack. He takes a baby aspirin and hydrochlorothiazide daily. His temperature is 36.7°C (98°F), blood pressure is 130/86 mm Hg, pulse is 80/min and respirations are 16/min. A complete physical examination is unremarkable. Which of the following is the most likely cause of his symptoms?
Polycystic kidney disease
Renal cell carcinoma
Bladder mass
Acute glomerulonephritis
Schistosoma infection
A 65-year-old male has been having a non-productive, hacking cough for over a week. He takes an over-the-counter medication containing guaifenesin and diphenhydramine in an effort to improve his symptoms. The next day, he complains of lower abdominal discomfort and difficulty voiding. Which of the following most likely accounts for this patient's new complaint?
Detrusor inactivity
Detrusor-sphincter dyssynergia
Overactive bladder
Abdominal muscle weakness
Urethral obstruction
A 65-year-old man comes to the emergency room complaining of 2 days of severe pain and swelling of his right knee. He denies any recent respiratory illness, diarrhea or urinary symptoms. He has a history of severe degenerative joint disease and underwent total knee replacement four years ago. He drinks one can of beer every night and does not use tobacco or illicit drugs. His temperature is 40°C (104°F), blood pressure is 120/60 mmHg, and pulse is 110/min. Examination shows warmth, swelling, and tenderness over the knee. His range of motion is restricted. Synovial fluid white blood cell count is 98,000/microl. Which of the following is the most likely cause of his current condition?
Streptococcus species
Staphylococcus aureus
Neisseria gonorrhoea
Chlamydia trachomatis
Borrelia burgdorferi
A 65-year-old man comes to the office and complains of pain and a rash with blisters over the left side of his chest. He has experienced pain over the area for the past 2 days. This morning, he noticed blisters while changing his shirt. He also complains of malaise and headache. His pulse is 82/min, blood pressure is 140/90 mmHg, respirations are 14/min and temperature is 36.8°C (98.4°F). Physical examination reveals grouped, tense vesicles arranged in a band along the left side of his chest. Which of the following is the most likely etiology of his condition?
Herpes simplex virus
Varicella zoster virus
Poison ivy
Human papilloma virus
Poxvirus
A 65-year-old man comes to the office with a six-month history of a non-healing ulcer on his right forearm. Physical examination demonstrates a scaling plaque with central ulceration and 1.5 cm diameter. The biopsy shows polygonal cells with atypical nuclei at all levels of the epidermis with zones of keratinization. What is the single most important risk factor for this condition?
Sunlight
Arsenic
Aromatic hydrocarbons
Chronic osteomyelitis
Chronic scars
A 65-year-old man complains of lower leg swelling, fatigue and poor appetite. His past medical history is significant for recurrent chest infections, wheezing, cough, recent pyelonephritis, and arterial hypertension. He smokes 1 pack of cigarettes a day but denies alcohol or intravenous drug use. His physical examination reveals a barrel-shaped chest with bilateral scattered wheezes. His abdomen is distended and his liver edge is palpated 4 cm below the right costal margin. You note pitting edema and dilated, tortuous, superficial veins over the bilateral lower extremities. Manual pressure on the abdomen causes persistent distention of the jugular veins. The patient's serum sodium level is 135 mEq/L and his creatinine concentration is 1.2 mg/dl. An abnormality of which of the following is most likely to explain his edema?
Serum albumin level
Pulmonary capillary wedge pressure
Pulmonary artery systolic pressure
Portal venous resistance
Urinary protein excretion
A 65-year-old man complains of two years of persistent cough. He says that he coughs up whitish sputum almost every morning on waking, and then continues coughing throughout the day. He also complains of exertional shortness of breath that becomes disabling if he gets an upper respiratory infection. He has smoked one pack of cigarettes daily for the past 40 years. Pulmonary function testing reveals a vital capacity that is 65% of his predicted. Which of the following best explains this finding?
Alveolar-capillary membrane thickening
Air trapping during expiration
Decreased functional residual capacity
Decreased lung distensibility
Respiratory muscle fatigue
A 65-year-old man has an enterocutaneous fistula originating in the jejunum secondary to inflammatory bowel disease. Which of the following would be the most appropriate fluid for replacement of his enteric losses?
D5W
3% normal saline
Ringer lactate solution
0.9% sodium chloride
6% sodium bicarbonate solution
A 65-year-old man undergoes a technically difficult abdominal–perineal resection for a rectal cancer during which he receives 3 units of packed red blood cells. Four hours later, in the intensive care unit (ICU), he is bleeding heavily from his perineal wound. Emergency coagulation studies reveal normal prothrombin, partial thromboplastin, and bleeding times. The fibrin degradation products are not elevated, but the serum fibrinogen content is depressed and the platelet count is 70,000/μL. Which of the following is the most likely cause of his bleeding?
Autoimmune fibrinolysis
Factor VIII deficiency
Delayed blood transfusion reaction
Hypothermic coagulopathy
A bleeding blood vessel in the surgical field
A 65-year-old man was brought to the emergency department after his wife and son were unable to wake him up this morning. His past medical history is significant for hypertension for the past 7 years. For the past year, he has had several episodes of chest pain, which was triggered by physical activity and relieved by rest. His current medications are nitrates and "baby aspirin." His blood pressure is 140/80 mm Hg, heart rate is 85/min, and respirations are 15/min. The physical examination reveals an obese man with impaired consciousness. He has a Glasgow score of 6, asymmetric pupils, and brisk deep tendon reflexes in the left extremities. Plantar stimulation provokes extension of the left great toe. The EKG shows no abnormalities. His CK-MB serum levels are within the normal range, and his LDL cholesterol level is 150 mg/dl. What is the most likely etiopathology of this patient's symptoms?
Atherosclerotic emboli obstructing a major cerebral artery
Acute left ventricular failure with decreased cerebral perfusion
Hemorrhagic stroke resulting from hypertensive crisis
Chronic subdural hematoma
Thrombus migration from the left side of the heart
A 65-year-old woman comes to the office for a health maintenance visit. She has been your patient for the last 15 years. When you ask how she has been, she replies with, "Well, I'm very health-conscious now. I read all the health magazines regularly, and exercise for 30 minutes daily. I eat a lot of garlic to control my cholesterol, and drink cranberry juice to keep my kidneys strong. I don't smoke, but I drink alcohol during social events. I've been compliant with regular screening colonoscopies, mammograms, and pap smears. Doc, since my mother died from ovarian cancer, do you think I can have an abdominal ultrasound every 6 months, plus any additional necessary tests, so that any cancer can be detected early?" What is the best response to this patient's concerns?
There is no evidence that ultrasound surveillance has any role in decreasing mortality from ovarian cancer
CXR, EGO, and abdominal ultrasound can be done to help detect cancers early
Abdomen ultrasound is not effective for detecting ovarian cancer early, but CXR surveillance has helped decrease the mortality of lung cancer
Perform an ultrasound every six months since it is a non-invasive procedure that can save you from any risk of being sued for malpractice
Reassure her that with a healthy lifestyle, cancer is unlikely
A 65-year-old woman complains of periodic headaches in the temporal region, visual disturbances, and neck stiffness. Treatment is initiated early and biopsy of a scalp artery is consistent with arteritis. Two months later, the patient presents to your office with weakness. She says that her headaches are gone but she has difficulty climbing stairs and getting up from a chair. Her serum CK level and ESR are normal. Which of the following is the most likely cause of this patient's current complaints?
Polymyalgia rheumatica
Symmetric polyneuropathy
Mononeuritis multiplex
Inflammatory myositis
Drug-induced myopathy
A 65-year-old woman presents to your office for evaluation of genital prolapse. She has a history of chronic hypertension, well controlled with a calcium channel blocker. She has had three full-term spontaneous vaginal deliveries. The last baby weighed 9 lb and required forceps to deliver the head. She says she had a large tear in the vagina involving the rectum during the last delivery. She has a history of chronic constipation and often uses a laxative to help her have a bowel movement. She has smoked for more than 30 years and has a smoker’s cough. She entered menopause at age 52 but has never taken hormone replacement therapy. Which of the following factors is least important in the subsequent development of genital prolapse in this patient?
Chronic cough
Chronic constipation
Chronic hypertension
Childbirth trauma
Menopause
A 65-year-old woman presents with a 1-cm lesion with a pearly border on her nose, and punch biopsy is consistent with a basal cell carcinoma. She is scheduled to undergo Mohs surgery. Which of the following is a benefit of Mohs surgery over wide local excision?
Mohs surgery results in a smaller cosmetic defect while obtaining negative margins circumferentially
Mohs surgery results in less recurrence and metastases
Mohs surgery can be performed on many different types of skin cancers
Mohs surgery offers a shorter operating time
Mohs surgery does not depend on intraoperative evaluation of specimen margins with frozen sections
A 66-year old female has been your patient for the last 8 years. She was diagnosed with colorectal carcinoma 2 years ago, and eventually underwent an endoscopic resection. Since then, she has been healthy, and has been coming to the office regularly for follow-up visits. She is very grateful, and has stated many times that she owes her life to you. You are currently a co-investigator of a retrospective observational study of patients with colon cancer, and you believe that including her medical information will be extremely beneficial. What course of action must you take so that you can include this patient's data in your study?
Include the data, as she has been your patient for so many years
Include the data and inform her whenever she comes next time
Include the data only after taking informed consent
Have the data de-identified by a colleague, then include it in the study
Call her and obtain verbal consent to include her data
A 66-year-old female comes for removal of a lipoma from her elbow. She wants the swelling out because it looks ugly when she wears sleeveless tops. Her only complaints are general malaise and fatigue for the past 8 months, which she attributes to her "being alone all the time." Her vital signs are within normal limits. Physical examination reveals mild pallor and both cervical and supraclavicular lymphadenopathy. Her preoperative blood count reveals the following: Hemoglobin 10.0 g/dL, Hematocrit 32%, Platelets 126,000/cmm, WBC 31,600/cmm. Leukocyte distribution: Segmented neutrophils 18%, Lymphocytes 77%, Bands 4%, Monocytes 1%. The pathologist reports the presence of "leukocytes that have undergone partial breakdown during preparation of a stained smear or tissue section, because of their greater fragility." Lymph node biopsy confirms the diagnosis. What is the correct statement about the above patient?
The prognosis is extremely bad
This is a form of plasma cell leukemia
The presence of thrombocytopenia is a poor prognostic factor
The most common cause of death is renal failure
This is a classic T-cell disease
A 66-year-old man presents with a four week history of increasing back pain and severe constipation. He has no weakness or sensory symptoms in his legs. He takes acetaminophen for back pain, metoprolol for high blood pressure, and an over-the-counter fiber supplement for constipation. A screening colonoscopy 5-year ago was unremarkable. Rectal examination shows no abnormalities. Examination of the stool for occult blood is negative. His blood pressure is 135/80 mmHg and heart rate is 80/min. Abdominal examination shows no abnormalities. Laboratory studies show: Hb 9.5 g/dl, WBC 7,000/cmm, Platelets 300,000/cmm, BUN 28 mg/dl, Serum Creatinine 1.9 mg/dl, ESR 80/hr. Which of the following is the best explanation for this patient's constipation?
Mechanical obstruction
Electrolyte disturbances
Medication effect
Hormonal disturbances
Neurologic dysfunction
A 66-year-old retired carpenter presents with chronic shortness of breath upon exertion. He has smoked one pack of cigarettes per day for the past 5 years and drinks alcohol regularly. Physical examination reveals a displaced point of maximal impulse and hepatosplenomegaly. His medications include pantoprazole for gastroesophageal reflux and sertraline for depression. Echocardiogram reveals an ejection fraction of 30% and dilated left and right ventricles. Laboratory tests show: Na+: 129 mEq/L, K+: 5.2 mEq/L, Cl−: 101 mEq/L, Blood urea nitrogen: 45 mg/dL, Creatinine: 1.3 mg/dL, Glucose: 134 mg/dL, Aspartate aminotransferase: 220 U/L, Alanine aminotransferase: 140 U/L, Alkaline phosphatase: 280 U/L. Which of the following is the most likely cause of his cardiac findings?
Borrelia burgdorferi
Cigarette smoking
Coxsackie B virus
Ethanol
Pantoprazole toxicity
A 67 -year-old male presents to the emergency department with severe dizziness and the inability to walk. He complains of repetitive vomiting and occipital headache. The symptoms started two hours ago when he was playing golf in sunny weather with his friends. His past medical history is significant for hypertension and diabetes. He underwent coronary stenting two years ago for recurrent chest pain. His current medications are aspirin, glipizide, enalapril and metoprolol. His blood pressure is 210/110 mmHg, heart rate is 78/min, temperature is 37.8°C (100°F), and respirations are 18/min. Muscle strength is preserved in all four extremities, and there are no sensory abnormalities. Which of the following is the most likely cause of this patient's symptoms?
Heat stroke
Posterior cerebral artery occlusion
Vestibular neuronitis
Cerebellar haemorrhage
Meniere disease
A 67-year-old Caucasian male complains of progressive visual loss in his right eye over the past several months. He has a history of hypertension and type 2 diabetes mellitus. Current medications include a daily baby aspirin, hydrochlorothiazide, lisinopril, and metformin. There is no family history of visual problems. He has a 35 pack year smoking history and admits to occasional alcohol use. He is afebrile with a blood pressure of 137/82 mmHg and pulse of 73/min. Cardiac and pulmonary examinations are unremarkable. A neurologic examination demonstrates no focal motor or sensory abnormalities. The patient is asked to cover his left eye and to look at a small spot on a grid made of parallel vertical and horizontal lines. He describes the vertical lines as being bent and wavy. Which of the following is the most likely cause of this patient's complaints?
Lens opacity
Macular degeneration
Increased intraocular pressure
Peripheral retinal degeneration
Enlarged blind spot
A 67-year-old male is brought to the emergency department after a syncopal episode. He lost consciousness while shopping in the mall. He denies any nausea, diaphoresis, chest pain, or shortness of breath. He has had two episodes of lightheadedness over the last month but has not seen a doctor. His past medical history is significant for long-standing hypertension, which is being treated with enalapril. His blood pressure is 135/90 mmHg while supine, and 130/85 mmHg while standing. His heat rate is 64/min. ECG shows a sinus rhythm with high voltage, prolonged PR interval, prolonged QRS interval, normal QT interval and occasional premature ventricular contractions (PVC). Echocardiography reveals left ventricular hypertrophy and an ejection fraction (EF) of 55%. Which of the following is the most likely cause of this patient's syncope?
Bradyarrhythmia
Torsades de pointes
Decreased myocardial contractility
Autonomic dysfunction
Ventricular premature beats
A 67-year-old male presents with a one-month history of dyspnea on exertion and chest pain. He denies hemoptysis, cough, fever, night sweats or weight loss. His past medical history is significant for hypertension and chronic obstructive pulmonary disease. He has a 48 pack-year smoking history but quit six years ago. He works as a salesman. On physical examination, the patient has a temperature of 38.2°C (100.8°F), blood pressure of 128/72 mm Hg, pulse of 92/minute, and respirations of 20 breaths/minute. His complete blood count, chemistry panel, and hepatic fun
Elevation of hydrostatic pressure
Decreased plasma osmotic pressure
Increased capillary permeability
Passage of fluid through openings in the diaphragm
Reduction of pleural space pressures
A 67-year-old man is evaluated for hypertension. He complains of occasional morning headaches. His past medical history is also significant for type 2 diabetes mellitus, coronary artery disease, and a stroke with residual left-sided weakness. He underwent coronary artery bypass surgery seven years ago and carotid endarterectomy five years ago. His current medication list includes lisinopril hydrochlorothiazide, amlodipine, metoprolol, aspirin, metformin and glyburide. His blood pressure is 190/120 mmHg on the right arm and 170/110 mmHg on the left arm. His heat rate is 65/min Physical examination reveals a periumbilical systolic-diastolic bruit. The latter finding is best explained by which of the following?
Abdominal aortic aneurysm
Aortic dissection
Aortic coarctation
Renal artery stenosis
Aorto-enteric fistula
A 67-year-old man presents to his primary care provider in January with fever and a productive cough. The patient had been seen ten days earlier with complaints of fever to 102°F (39.0°C), myalgias, rhinorrhea, and dry cough. At that time, his lung exam revealed occasional crackles. He was given a medication and told to follow up if his symptoms worsened. The symptoms did remit over the first five days, but he began to feel worse again two days ago. He smokes a half-pack of cigarettes per day and drinks alcohol several times a week. On exam today, his temperature is 102.3°F (39.3°C), and lung exam reveals increased tactile fremitus in the left lower lobe. What is the most likely pathogen responsible for his current condition?
Pneumocystis jiroveci
Pseudomonas aeruginosa
Klebsiella pneumoniae
Mycoplasma pneumoniae
Staphylococcus aureus
A 67-year-old man presents to your office with two days of back pain. He was moving boxes in the garage when the pain started. The pain is not relieved by lying down and increases in intensity upon straining and coughing. He could not sleep during the night due to pain and took several tablets of acetaminophen without relief. He has never had such pain before. Physical examination reveals symmetric knee reflexes. Plantar reflexes are flexor bilaterally. Straight leg raise is negative. Local tenderness is evident upon percussion of the fourth lumbar vertebra. Which of the following is the most likely cause of this patient's condition?
Ligamentous sprain
Nerve root demyelinization
Intervertebral disk degeneration
Apophyseal joint arthritis
Vertebral body demineralization
A 67-year-old woman is being evaluated for periodic confusion, insomnia, and frequent falls as well as episodes of decreased alertness and visual hallucinations. On physical examination, she has increased lower extremity muscle tone but downgoing Babinski reflexes bilaterally. Which of the following pathologic findings most likely underlies her condition?
Neurofibrillary tangle
Multiple lacunar strokes
Impaired CSF absorption
Corticospinal tract demyelinization
Lewy bodies
A 67-year-old woman is currently postoperative day 8 after an emergent laparoscopic cholecystectomy for acute cholecystitis. On postoperative day 2 she spiked a temperature of 40°C (101.4°F) and began to complain of some shortness of breath. X-ray of the chest revealed right lower lobe pneumonia, and the patient was started on clindamycin. Today she is experiencing multiple episodes of foul-smelling, watery diarrhea that is green tinged but non-bloody. She also complains of lower abdominal cramping. Her temperature is 37.8°C (100°F), pulse is 90/min, respiratory rate is 15/min, and blood pressure is 110/70 mm Hg. Which of the following is the most likely explanation for these findings?
Ingestion of preformed enterotoxins, cytotoxins, and/or neurotoxins
Production of cytotoxins within the gastro- intestinal tract
Production of enterotoxins within the gastrointestinal tract
Production of enterotoxins and cytotoxins within the gastrointestinal tract
Viral invasion and damage of villous epithelial cells within the gastrointestinal tract
A 68-year-old Caucasian man is admitted with a diagnosis of left lower lobe pneumonia, and is started on gatifloxacin. He has a long history of diabetes, hypothyroidism, hypercholesterolemia, and hypertension. He also has diabetic retinopathy, peripheral neuropathy, and nephropathy. He has an arterio-venous fistula placed for a possible dialysis. His medications are insulin, furosemide, atorvastatin, metoprolol and levothyroxine. After having his blood drawn for some laboratory studies today, he bleeds persistently. Laboratory studies show: Hb 11.5 g/dl, Platelets 160,000/cmm, Blood glucose 178 mg/dl, BUN 56 mg/dl, Serum creatinine 3.5 mg/dl. His baseline creatinine level is between 3.2-3.5 mg/dl. Which of the following is the most likely cause of his bleeding?
Disseminated intravascular coagulation
Factor VIII deficiency
Platelet dysfunction
Consumptive coagulopathy
Thrombocytopenia
A 68-year-old white female presents to the ER complaining of sudden onset chest pain associated with two episodes of vomiting. She has hypertension for which she takes atenolol and hydrochlorothiazide. Her pulse is 60/min, blood pressure is 80/50 mmHg and respirations are 14/min. Examination shows elevated jugular venous pressure and a positive Kussmaul's sign. Her lungs are clear to auscultation. Her EKG shows 2 mm ST segment elevation in leads II, III and aVF and 1 mm ST segment depression in leads I and aVL. Which of the following is the most likely cause of this patient's hypotension?
Pulmonary thromboembolism
Interventricular septum rupture
Right ventricular infarction
Variant angina
Intravascular volume depletion
A 68-year-old woman presents with a pigmented lesion on the trunk. Upon further examination the lesion has an irregular border, darkening coloration, and raised surface. An incisional biopsy is performed and confirms a melanoma with a thickness of 0.5 mm. The patient is scheduled for a wide local excision of the melanoma in the operating room. Which of the following is the smallest margi recommended for excision?
3 mm
5 mm
1 cm
2 cm
5 cm
A 7 -year-old Caucasian boy is brought to the emergency room with a severe headache, vomiting, and altered mental status of acute onset. His temperature is 36.7 C (98 F), blood pressure is 130/70 mm Hg, pulse is 60/min, and respirations are 18/min. Neurologic examination reveals nuchal rigidity, but no focal neurologic signs. A CT scan shows blood in the subarachnoid space. Which of the following is the most probable additional finding in this patient?
History of seizures
Mental retardation
Congenital heart disease
Coagulation abnormalities
Trauma
A 7-year-old boy has cramping abdominal pain and a rash mainly on the back of his legs and buttocks as well as on the extensor surfaces of his forearms. Laboratory analysis reveals proteinuria and microhematuria. You diagnose Henoch-Schönlein, or anaphylactoid, purpura. In addition to his rash and abdominal pain, what other finding is he likely to have?
Chronic renal failure
Seizures
Arthritis or arthralgia
Unilateral lymphadenopathy
Bulbar nonpurulent conjunctivitis
A 7-year-old boy presents to the physician's office with a 3-week history of left-sided anterior cervical lymph node enlargement. The enlarged nodes are not tender to palpation. A few papules developed on the left forearm at the onset of lymphadenopathy. The boy has a kitten at home. Which of the following is the most likely organism causing lymphadenopathy in this child?
Actinomyces israelii
Francisella tularensis
Bartonella henselae
Mycobacterium tuberculosis
Staphylococcus aureus
A 7-year-old boy presents with tenderness and erythema of one knee joint. He has had troubles with infections since about 3 months of age. A brother and a maternal uncle both died of infectious disease at an early age. A detailed immunologic evaluation performed at 2 years of age demonstrated plasma IgG less than 50 mg/100 mL. Normal numbers of circulating T cells and normal cellular immunity were found. The boy had been treated monthly since then with IV immunoglobulin. This therapy had markedly reduced, but not eliminated, the boy's infection rate. Which of the following is the most likely pathogen to cause infectious arthritis in this patient?
Aspergillus
Herpes
Mycobacteria
Mycoplasma
Toxoplasma
A 7 -year-old boy is rushed to the emergency department after falling on his outstretched hand. He immediately complained of right arm pain after the accident, and he currently cannot move his arm due to the pain. He is crying and holding his right arm in flexion. There is ecchymosis just above his elbow. He cries out in pain when his arm is moved. An x-ray reveals a supracondylar fracture. What secondary injury is most commonly associated with this patient's fracture?
Median nerve injury
Axillary nerve injury
Ulnar artery injury
Brachial artery injury
Brachial plexus injury
A 68-year-woman with hypertension and dyslipidemia presents with 30 minutes of retrosternal chest pain radiating to her neck. She is diaphoretic and in moderate distress. The ECG shows ST-segment elevation in the inferior leads. Which of the following mechanisms is the most likely cause of her condition?
Coronary plaque rupture
Aortic inflammation
Pericardial inflammation
Vasculitis
Myocarditis
A 69-year-old woman complains of easy fatigue and one episode of presyncope. On examination of the jugular venous pressure (JVP), there are irregular large a waves. The ECG has fixed PP and RR intervals but varying PR intervals. Which of the following conditions is this most likely caused by?
Surgical removal of an atrium
A reentry phenomenon
A drug effect
A heart rate under 60 beats/min
Independent beating of atria and ventricles
A 7-year-old girl is brought to the office by her mother. The mother is worried because she noticed some axillary hair development in her daughter. The girl appears calm, and denies the presence of headaches, visual disturbances or abdominal pain. There has been no change in her behavior. Her medical history is unremarkable. Her older sister's pubertal changes began at age 11. Physical examination reveals scarce and dark axillary hair, absent breast development and absent pubic hair. The rest of the examination is unremarkable. Activation of which of the following structures is most likely responsible for this patient's symptomatology?
Hypothalamus
Pituitary gland
Adrenal glands
Ovaries
Liver
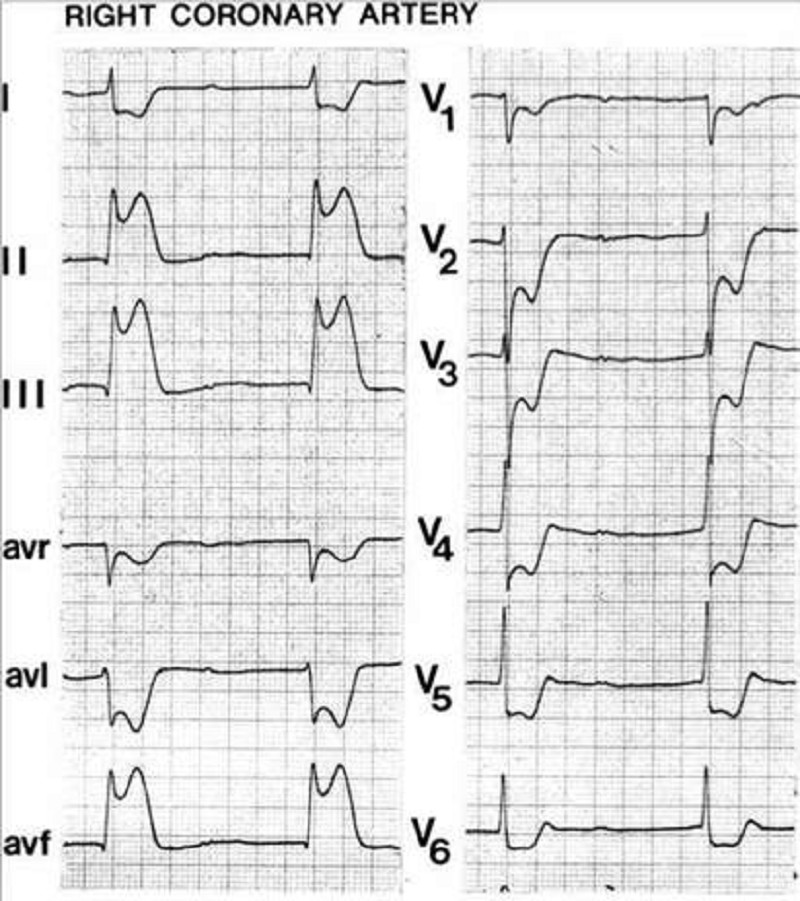
A 70-year-old Caucasian man comes to the emergency department because of the sudden onset of nausea, vomiting, diaphoresis, and chest pain. His other medical problems include hypertension, diabetes mellitus-type 2, and aortic stenosis. He has smoked one-and-a-half packs of cigarettes daily for 30 years and drinks 4 ounces of alcohol daily. His temperature is 37.2°C (99°F), blood pressure is 100/60 mmHg, pulse is 60/min, and respirations are 18/min. The patient's pulse oximetry showed 98% at room air. Examination shows normal first and second he sounds. Lungs are clear to auscultation. His EKG is shown below. Which of the following is the most likely mechanism of this patient's condition?
Occlusion of the right coronary artery
Inflammation of the pericardium
Vasospasm of the left circumflex artery
Occlusion of the left anterior descending artery
Occlusion of the left circumflex artery
A 70-year-old man comes to the physician due to a 4-6 month history of "almost continuous urinary dribbling." This symptom is present both day and night, and is progressively getting worse. He denies dysuria and hematuria. He has a 20-year history of diabetes mellitus-type 2, hypertension, alcoholic hepatitis and coronary artery disease. He had a gastric emptying study done a few weeks ago because of continuous nausea and early satiety. He had laser photocoagulation of both eyes for diabetic retinopathy. He has smoked one pack of cigarettes daily for 50 years, and drinks 4 to 6 beers daily. He takes NPH insulin, regular insulin, metformin, aspirin, metoprolol, lisinopril and metoclopramide. His vital signs are stable. Physical examination shows a well-appearing man. Pertinent physical findings are a normal sized prostate, decreased sensation in both legs below the knees, and absent Achilles tendon and knee reflexes bilaterally. Fecal occult blood test is negative. Postvoid residual volume is 550 ml. Urinalysis shows: Specific gravity 1.020, Blood trace, Glucose positive, Ketones negative, Protein moderate, Leukocyte esterase negative, Nitrites negative, WBC 1-2/hpf, RBC 3-4/hpf. Which of the following is the most likely cause of this patient's incontinence?
Multiinfarct dementia
Overflow incontinence due to detrusor weakness
Overflow incontinence from bladder outlet obstruction
Urinary tract infection
Overflow incontinence due to medication
A 70-year-old man is brought to the Emergency Room because he lost his consciousness while working in the garden. He says that he had several episodes of near-syncope on exertion recently. His past medical history is insignificant. He is not taking any medications. His blood pressure is 110/85 mmHg and heat rate is 80/min. Point of maximal impulse is increased in intensity. Cardiac auscultation reveals ejection type systolic murmur at the base of the heat with radiation to the carotid arteries. ECG demonstrates left ventricular hypertrophy, and secondary ST segment and T wave change. What is the most probable cause of this patient's condition?
Rheumatic endocarditis
Hypertension
Bacterial endocarditis
Congenital anomaly
Age-related sclerocalcific changes
A 70-year-old patient with long-standing type 2 diabetes mellitus presents with complaints of pain in the left ear with purulent drainage. On physical examination, the patient is afebrile. The pinna of the left ear is tender, and the external auditory canal is swollen and edematous. The white blood cell count is normal. Which of the following organisms is most likely to grow from the purulent drainage?
Pseudomonas aeruginosa
Streptococcus pneumoniae
Candida albicans
Haemophilus influenzae
Moraxella catarrhalis
A 71-year-old man is brought to the ER after a witnessed tonic-clonic seizure. He is somnolent and intermittently combative on exam. No past medical history is available. His arterial blood gas (ABG) at room air is given below: pH 7.23, pCO2 69 mmHg, pO2 57 mmHg, HCO3 28 mmHg. Which of the following best explains the acid-base disturbances in this patient?
Lactic acid accumulation
Hypoventilation
Pulmonary embolism
Renal failure
Protracted vomiting
A 72-year-old male comes to the office with intermittent symptoms of dyspnea on exertion, palpitations, and cough occasionally productive of blood. On cardiac auscultation, a low-pitched diastolic rumbling murmur is faintly heard at the apex. What is the most likely cause of the murmur?
Long-standing hypertension
A congenital anomaly
Rheumatic fever as a youth
A silent MI within the past year
Anemia from chronic blood loss
A 72-year-old male presents with a two-day history of intense pain in his right ear, along with ear discharge. The pain is so severe that he is unable to sleep. It radiates to his temporomandibular joint and is aggravated by chewing. His disease has worsened despite the use of topical antibiotics. He takes metformin and enalapril. On physical examination, granulation tissue is noted in the lower part of his external auditory canal. Cranial nerves are intact. Oropharynx is clear without exudate. Which of the following is the most likely causative organism of this patient's ear condition?
Pseudomonas aeruginosa
Bacteroides species
Staphylococcus aureus
Peptostreptococcus species
Aspergillus fumigatus
A 72-year-old man undergoes resection of an abdominal aneurysm. He arrives in the ICU with a core temperature of 33°C (91.4°F) and shivering. Which of the following is a physiologic consequence of the shivering?
Rising mixed venous O2 saturation
Decreased consumption of O2
Increased production of CO2
Rising base excess
Decreased minute ventilation
A 72-year-old man with coronary artery disease and hypertension is hospitalized after suffering a myocardial infarction 5 days ago. He suddenly complains of severe chest pain. His blood pressure is 90/60 mmHg and heart rate is 65/min. Auscultation reveals no murmurs or rubs. An ECG reveals sinus rhythm with an acute ST-segment elevation in the anteroseptal area. Urgent bedside echocardiography showed anteroseptal, lateral, and apical akinesis, mild left ventricular systolic dysfunction, and severe pericardial effusion. Within 20 minutes he is unconscious with undetectable pulses and blood pressure. What is the most likely cause of the patient’s sudden decompensation?
Free wall rupture
Left ventricular thrombus
Mitral regurgitation
Pericarditis
Ventricular septal rupture
A 72-year-old woman had a pacemaker inserted 4 years ago for symptomatic bradycardia because of AV nodal disease. She is clinically feeling well and her ECG shows normal sinus rhythm at a rate of 68/min but no pacemaker spikes. Her pacemaker only functions when the ventricular rate falls below a pre-set interval. Which of the following best describes her pacemaker function?
Asynchronous
Atrial synchronous
Ventricular synchronous
Ventricular inhibited
Atrial sequential
A 72-year-old woman notices progressive dysphagia to solids and liquids. There is no history of alcohol or tobacco use, and the patient takes no medications. She denies heartburn, but occasionally notices the regurgitation of undigested food from meals eaten several hours before. Her barium swallow is shown. Which of the following is the cause of this condition?
Growth of malignant squamous cells into the muscularis mucosa
Loss of intramural neurons in the esophagus
Psychiatric disease
Spasm of the lower esophageal sphincter
Scarring caused by silent gastroesophageal reflux
A 72-year-old woman who is planning to undergo ventral hernia repair is on warfarin for atrial fibrillation. She is advised to cease her warfarin several days before her surgery and is hospitalized preoperatively for heparinization. During her hospital stay, she complains of severe abdominal and flank pain. Her prothrombin time (PT) is normal, but her activated partial thromboplastin time (aPTT) is elevated. An abdominal CT scan demonstrates a large retroperitoneal hematoma. Which of the following should be administered to reverse the effects of the heparin?
Thrombin
Vitamin K
Protamine sulphate
Aprotinin
Platelet transfusion
A 73-year-old Caucasian man is brought to the office by his daughter, who is concerned that he might be depressed. He is a retired surgeon, and has lived alone ever since his wife died a year ago. His daughter visits him every 6 months; she feels bad about not being able to visit him more frequently because her job and family keep her very busy. He denies having any feelings of sadness, guilt, weight loss, loss of appetite, suicidal ideation, deafness, vertigo, and decreased or blurred vision. His medical problems include hypertension, diabetes mellitus-type 2 and a myocardial infarction 10 years ago. His current medications are glyburide, aspirin and enalapril. He denies the use of tobacco, alcohol, or drugs. His vital signs are within normal limits. He appears withdrawn, less energetic than usual, and walks stiffly. He sits with a stooped posture. He has a fixed facial expression, and his voice sounds monotonous. His deep tendon reflexes are 2+. Sensations and motor strength are normal. There is increased resistance to passive flexion. Which of the following types of gait is most likely to be present in this patient?
Cerebellar ataxia
Hypokinetic gait
Waddling gait
Spastic gait
Gait disequilibrium
A 73-year-old diabetic man presents with low-grade fever, facial pain over his right maxilla, and bloody nasal discharge for the last three days. For the last day, he has had diplopia. He was diagnosed with diabetes mellitus 10 years ago. For the last year, he has been on insulin. His most recent hemoglobinA1C was 12.0. His temperature is 39.0°C (102.2°F), pulse is 88/min, and blood pressure is 130/76mm Hg. Examination shows right-sided nasal congestion and necrosis of the right nasal turbinate with tenderness over the right maxillary sinus. There is chemosis and proptosis of his right eye. CT scan shows opacification of the right maxillary sinus. Which of the following is the most likely causative organism?
Rhizopus species
Pseudomonas aeruginosa
Staphylococcus aureus
Haemophilus influenzae
Moraxella catarrhalis
A 73-year-old man from a nursing home develops headache, fever, cough, sore throat, malaise, and severe myalgia during a community outbreak affecting numerous other residents at the home. The symptoms gradually resolve after 3 days, and he starts feeling better but then there is a reappearance of his fever, with cough and yellow sputum production. On examination, his temperature is 38.5°C, pulse 100/min, respiration 24/min, oxygen saturation 88% and crackles in the right lower lung base, bronchial breath sounds and dullness on percussion. CXR reveals a new infiltrate in the right lower lobe. Which of the following is the most likely causative organism?
Primary viral pneumonia
Mycoplasma pneumoniae
An autoimmune reaction
Streptococcus pneumoniae
Neisseria catarrhalis
A 73-year-old man presents to the ED after a syncopal episode. He had been resting in bed for approximately one week after injuring his right knee. This morning, his knee felt better and he attempted to get up from bed. However, upon attempting to stand, he sustained a brief loss of consciousness. He had no symptoms or medical history prior to the knee injury. Medications include acetaminophen and ibuprofen for knee pain. On exam, his pulse is 73/min, respirations are 14/min, and blood pressure is 136/83 mmHg. Which of the following is the most likely cause of this patient's syncope?
Cardiac arrhythmia
Orthostatic hypotension
Valvular obstruction
Vagal nerve hyperactivity
Hyperventilation
A 73-year-old woman presents to the emergency room complaining of severe epigastric pain radiating to her back, nausea, and vomiting. CT scan of the abdomen demonstrates inflammation and edema of the pancreas. A right upper quadrant ultrasound demonstrates the presence of gallstones in the gallbladder. Which of the following is an important prognostic sign in acute pancreatitis according to Ranson’s criteria?
Amylase level
Age
Total bilirubin level
Albumin level
Lipase level
A 73-year-old woman presents to the emergency room with black tarry stools and symptoms of presyncope when standing up. Digital rectal examination confirms the presence of melena. She recently started using ibuprofen for hip discomfort. Upper endoscopy confirms the diagnosis of a gastric ulcer. Which of the following is the most likely explanation for the gastric ulcer?
Causing direct epithelial cell death
An antiplatelet effect
Increasing acid production
Promoting replication of Helicobacter pylori
Inhibiting mucosal repair

A 74-year-old Caucasian woman is brought to the emergency department after a fall. Her husband is concerned since she is on "blood thinners." Her other medical problems include hypertension, hearing loss, congestive heart failure, coronary artery bypass graft, transient ischemic attack, and atrial fibrillation. She does not use tobacco, alcohol, or drugs. Her medications include aspirin, metoprolol, digoxin, furosemide, and warfarin. Her temperature is 37.2°C (99°F), blood pressure is 140/90 mmHg, pulse is 72/min, and respirations are 14/min. CT scan of the head without contrast is shown below. Which of the following is the most likely cause of her condition?
Tearing of middle meningeal artery
Rupture of an aneurysm
Tumor of the arachnoid granulation
Tearing of bridging veins
Hypertensive hemorrhage
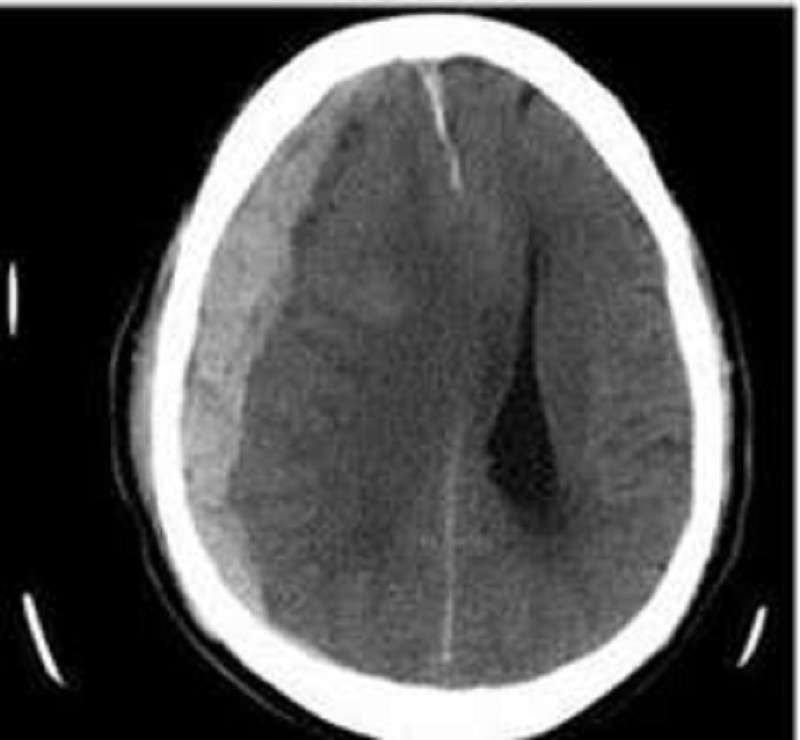
A 76-year-old man is brought to the emergency department by his son who found him confused in his apartment. The son also reports that his father has been limping for the past two days. The patient's past medical history is significant for hypertension, diabetes mellitus, and cataract surgery six months ago. His medications are metoprolol, enalapril, and glyburide. He has also been taking ibuprofen for recent headaches. A head CT scan is obtained and is shown below. Which of the following is the most likely cause of this patient's condition?
Carotid artery atherosclerosis
Blunt head trauma
Ruptured aneurysm
Recent eye surgery
Small vessel hyalinosis

A 80-year-old man with Type II diabetes and hypertension presents with increasing dyspnea. He appears short of breath, blood pressure is 170/95 mmHg, pulse 100/min and regular. The JVP is at 7 cm; there is a loud second heart sound and a systolic ejection murmur at the right sternal border, which does not radiate. The lungs have bibasilar crakles up to the scapula. The CXR has bilateral infiltrates and vascular redistribution. His echocardiogram reports aortic sclerosis, concentric left ventricular hypertrophy (LVH), and normal ejection fraction. Which of the following is the most likely mechanism for this condition?
Valvular heart disease
Hibernating myocardium
Diastolic dysfunction
Systolic dysfunction
Hypertrophic obstructive cardiomyopathy (HOCM)
A 74-year-old man presents to your office for a routine. He has no present complaint. His medical history is significant for right knee osteoarthritis. He takes naproxen occasionally, to relieve knee pain. He does not smoke or consume alcohol. His BP is 165/75 mmHg and PR is 70/min. The physical examination showed a mild systolic ejection type murmur at the base of the heat to the right. An E-KG revealed left ventricular hypertrophy and secondary ST segment and T wave change. Moderate left ventricular hypertrophy, without any flow abnormalities, was demonstrated on echocardiography. The ejection fraction was 60%. What is the most probable cause of hypertension in this patient?
Rigidity of the arterial wall
Aortic insufficiency
Elevated plasma renin activity
Increased cardiac output
Increased intravascular volume
A 74-year-old man presents with fatigue, short- ness of breath on exertion, and back and rib pain, which is made worse with movement. Investigations reveal he is anemic, calcium, urea, and creatinine are elevated. X-rays reveal multiple lytic lesions in the long bones and ribs, and protein electrophoresis is positive for an immunoglobulin G (IgG) paraprotein. Which of the following is the most likely mechanism for the renal injury?
Plasma cell infiltrates
Glomerular injury
Tubular damage by light chains
Vascular injury by light chains
Uric acid crystals
A 74-year-old nursing home resident is brought to the ER with a low-grade fever, cough and shortness of breath for the last two days. The cough is productive of small amounts of greenish sputum. His past medical history is significant for hypertension, diabetes mellitus type 2, COPD, hypercholesterolemia and mild dementia. His blood pressure is 152/78 mmHg and his heart rate is 89/min, regular. Physical examination reveals decreased breath sounds, coarse rhonchi, and increased fremitus over the lower left lung field. His oxygen saturation is 92% on room air when lying on his right side but drops to 84% when he lies on his left. Which of the following best explains this finding?
Decreased cardiac output
Increased arterio-venous shunting
Increased dead space ventilation
Effort-dependent hypoventilation
Decreased oxygen diffusion capacity
A 74-year-old woman is admitted with upper gastrointestinal (GI) bleeding. She is started on H 2 blockers, but experiences another bleeding episode. Endoscopy documents diffuse gastric ulcerations. Omeprazole is added to the H2 antagonists as a therapeutic approach to the management of acute gastric and duodenal ulcers. Which of the following is the mechanism of action of omeprazole?
Blockage of the breakdown of mucosa-damaging metabolites of nonsteroidal anti-inflammatory drugs (NSAIDs)
Provision of a direct cytoprotective effect
Buffering of gastric acids
Inhibition of parietal cell hydrogen potassium ATPase (adenosine triphosphatase)
Inhibition of gastrin release and parietal cell acid production
A 74-year-old woman with a history of a previous total abdominal hysterectomy presents with abdominal pain and distention for 3 days. She is noted on plain films to have dilated small-bowel and air-fluid levels. She is taken to the operating room for a small-bowel obstruction. Which of the following inhalational anesthetics should be avoided because of accumulation in air-filled cavities during general anesthesia?
Diethyl ether
Nitrous oxide
Halothane
Methoxyflurane
Trichloroethylene
A 75-year-old female nursing home resident complains of cough and fever. Her past medical history is significant for hypertension, myocardial infarction (experienced two years ago), and a traumatic right foot amputation. Her current medications are atenolol, hydrochlorothiazide, and aspirin. Her temperature is 39.4°C (103°F), pulse is 110/min, respirations are 22/min, and blood pressure is 110/76 mmHg. Crackles are present at right lung base. Chest x-ray reveals a right lower lobe infiltrate. Which of the following pathogens is the most likely cause of this patient's condition?
Staphylococcus aureus
Streptococcus pneumoniae
Haemophilus influenzae
Anaerobic bacteria
Gram-negative rods
A 76-year-old man presents with several months of urinary incontinence. He denies associated dysuria, nocturia, or penile discharge, and has otherwise been feeling well aside from moderate left arm pain following a fall three days ago. He denies headache or head trauma. His medical history is significant for osteoarthritis and glaucoma, which are controlled with medications. On exam, his vital signs are within normal limits. His heart, lungs, and prostate are unremarkable. The cranial nerves are all intact, fundoscopic exam is normal, and there is no tremor. His gait is wide-based and shuffling, and he scores 24/30 on the Folstein mini-mental status exam. His muscle power is 5/5 in all four extremities and the deep tendon reflexes are normal. What is the most likely cause of his current condition?
Increased CSF production
Amyloid protein deposits in the brain
Small vessel cerebral ischemia
Decreased CSF absorption
Spinal cord compression
A 76-year-old woman with a history of congestive heart failure, coronary artery disease, and an “irregular heart beat” is brought to the ED by her family. She has been complaining of increasing abdominal pain over the past several days. She denies nausea or vomiting and bowel movements remain unchanged. Vitals are HR of 114 beats per minute, BP 110/75 mm Hg, and temperature 98°F. On cardiac examination, her HR is irregularly irregular with no murmur detected. The abdomen is soft, nontender, and nondistended. The stool is heme-positive. This patient is at high risk for which of the following conditions?
Perforated gastric ulcer
Diverticulitis
Acute cholecystitis
Mesenteric ischemia
Sigmoid volvulus
A 77-year-old woman is brought to the emergency room because of nonspecific abdominal discomfort. She has no anorexia, fever, chills, or weight loss. Her abdomen is soft and non-tender on physical examination. Abdominal x-rays show lots of stool in the colon, but no free air or air-fluid levels. The amylase is 150 U/L (25–125U/L), and the rest of her biochemistry and complete blood count are normal. Which of the following conditions can cause a false positive elevation in the serum amylase?
Maturity-onset diabetes mellitus (DM)
Gastric ulcer
Renal failure
Sulfonamide therapy
Gastric carcinoma
A 78-year-old man with a history of atherosclerotic heart disease and congestive heart failure presents with increasing abdominal pain. The pain began suddenly a day ago and has progressively worsened since then. He denies nausea, vomiting, and diarrhea, but states that he had black tarry stool this morning. He denies any history of prior episodes of similar pain. Vitals are BP 120/65 mm Hg, HR 105 beats per minute, and temperature 99°F. The patient is at high risk for which of the following conditions?
Cholecystitis
Mesenteric ischemia
Cecal volvulus
Perforated peptic ulcer
Small bowel obstruction
A 78-year-old man with a history of coronary artery disease and an asymptomatic reducible inguinal hernia requests an elective hernia repair. Which of the following would be a valid reason for delaying the proposed surgery?
Coronary artery bypass surgery 3 months earlier
Jugular venous distension
A history of cigarette smoking
Hypertension
Hyperlipidemia
A 79-year-old woman presents to your office complaining of an intermittent skin rash over the last several months. She denies fever, headache, and recent weight loss. Her past medical history is significant for diet-controlled diabetes and right knee osteoarthritis treated with acetaminophen. Physical examination reveals several dark purple ecchymotic areas over the dorsum of both arms. Her abdomen is soft and non-tender. The liver span is 8 cm and the spleen is not palpable. Laboratory studies reveal: Hematocrit 47%, WBC count 5,800/mm3, Platelet count 220,000/mm3, Serum creatinine 0.8 mg/dL\, Fibrinogen 350 mg/dL, Prothrombin time 10 sec, INR 1.0, Partial thromboplastin time 25 sec. Which of the following is the most likely cause of this patient's complaint?
Poor platelet adhesion
Perivascular connective tissue atrophy
Lupus anticoagulant
Vitamin K deficiency
Bone marrow failure
A 9-month-old African American boy is brought to the office by his parents due to swelling of the feet and hands for the past two days, accompanied by poor feeding and fussiness. His vital signs are stable, except for a temperature of 38.3C (101 F). He appears pale. On examination, the dorsal surface of his hands and feet on both sides are swollen and tender, with restricted range of movement. He is an adopted child, and his family history is not available. Radiography of the feet and hands reveal soft tissue swelling. What is the pathophysiology of this patient's presentation?
Salmonella osteomyelitis
Staphylococcus osteomyelitis
Vasa-occlusive phenomena
Hypertrophic osteoarthropathy
Autoimmune phenomena
A 9-year-old boy has a severe sore throat with fever and dysphagia. On examination, there are grayish-white papulovesicular lesions on an erythematous base that ulcerate. They are located on the soft palate, anterior pillars of the tonsils and uvula. There are no lesions on the gingiva, tongue, or lips. A clinical diagnosis of herpangina is made. Which of the following is the most likely causative organism?
Measles (Morbillivirus)
Rubella (rubivirus)
Coxsackievirus A
HSV-1
HSV-2
A 9-year-old boy is brought to the emergency department by his father due to a sudden onset of difficulty with writing and jerky movements. He recently had a mild sore throat which quickly resolved, but now seems to have recurred and have worsened. He also had a low-grade fever last week, but no chills. Physical examination reveals a pericardial friction rub and subcutaneous nodules over the hands. Laboratory studies show an elevated ESR. What is the most likely cause of this child's symptoms?
Group A streptococcus
Mycoplasma pneumoniae
Respiratory syncytial virus
Paramyxovirus
Epstein-Barr virus
A 9-year-old boy is brought to the emergency department due to an episode of seizures during class. His teacher says that the seizure started suddenly, and he fell to the ground with sustained flexion of the arms and extension of the legs, followed by clonic movements of the whole body. He has also been irritable lately, and his school performance has declined. His parents arrive shortly and say that they recently noticed he was lethargic and frequently complained of headaches, especially in the morning. His medical history is unremarkable. Physical examination reveals decreased muscle strength of the left side of the body, with brisk deep tendon reflexes in the left arm and leg. MRI of the head reveals a space-occupying lesion in the right parietal lobe. What tumor is most likely responsible for this patient's symptoms?
Benign astrocytoma
Medulloblastoma
Glioblastoma multiforme
Pinealoma
Craniopharyngioma
A 9-year-old boy is brought to the office by his mother because of itching, burning and oozing skin lesions on both of his legs. The boy appears tanned. When asked if he had been spending time outdoors, he replies with great excitement that he just returned yesterday from a camping trip in the woods with his dad. Physical examination of both lower limbs reveals vesicles with erythema arranged in a linear fashion. Weepy and crusted lesions and edema are also present. What type of reaction is responsible for this boy's lesions?
Antibody mediated hypersensitivity
Cell mediated hypersensitivity
IgE mediated hypersensitivity
Immune complex mediated hypersensitivity
Woods biopsy
A 9-year-old boy is brought to the pediatric clinic by his mother, who noticed that the left side of his mouth has started to droop over the past several days. In addition, he is unable to close his left eye completely and complains of it burning. Review of systems reveals a cold approximately two weeks ago and recent decreased taste sensation. Physical examination reveals a well-nourished male with normal vital signs. There is left eye ptosis and mild erythema of the left conjunctiva. His smile is asymmetrical on the left. Laboratory evaluation, including a complete blood count and chemistry profile, are normal. Which of the following infections is most closely associated with this patient's condition?
Epstein-Barr Virus
Group A Streptococcus
Human Immunodeficiency Virus
Influenza
Measles
A 9-year-old child has developed headaches that are more frequent in the morning and are followed by vomiting. Over the previous few months, his family has noted a change in his behavior (generally more irritable than usual) and his school performance has begun to drop. Imaging of this child is most likely to reveal a lesion in which of the following regions?
Subtentorial
Supratentorial
Intraventricular
Spinal canal
Peripheral nervous system
A 9-year-old girl has breast and pubic hair development. Evaluation demonstrates a pubertal response to a GnRH-stimulation test and a prominent increase in luteinizing hormone (LH) pulses during sleep. These findings are characteristic of patients with which of the following?
Theca cell tumors
Iatrogenic sexual precocity
Granulosa cell tumors
Constitutional precocious puberty
Premature thelarche
A 91-year-old woman presents to the emergency department with a chief complaint of shortness of breath over the past 2 days. She has a history of hypertension and coronary artery bypass surgery 25 years earlier. Her blood pressure is 178/92 mmHg and she has jugular venous distension, hepatomegaly, and 3+ lower extremity edema. ECG is remarkable for left ventricular hypertrophy, no ST-segment elevations or depressions, no Q waves, and no T wave abnormalities. Echocardiogram reveals an ejection fraction of 60% and left atrial dilatation. There is universal left ventricular thickening. No valvular regurgitation or stenosis was noted. Which of the following underlying conditions is the most likely cause of this patient’s symptoms?
Hypertensive heart disease
Ischemic heart disease
Hypertrophic obstructive cardiomyopathy
Mitral valve prolapse
Myocarditis
A blood type B infant born to a blood type O mother has clinically significant fetal-maternal blood group incompatibility with mild anemia and a weakly positive Coombs test. The infant develops jaundice a few hours after birth, with a bilirubin (measured at 12 hours after birth) of 12 mg/dL (predominately unconjugated) compared with 3.5 mg/dL in cord blood. The physician is concerned that the rising bilirubin levels will damage the infant's nervous system. Which of the following sites is most vulnerable to this injury?
Basal ganglia
Cerebellum
Cerebral cortex
Peripheral nerve
Spinal cord
A boy is brought to the office by his parents for a routine visit. During the physical examination, he can obey two-step commands, use two- to three-word phrases, and can build a tower of six blocks. According to his mother, he can walk up and down the stairs without help. What is the most likely age of this child?
15 months
4 years
2 years
3 years
18 months
A child can walk well holding on to furniture but is slightly wobbly when walking alone. She uses a neat pincer grasp to pick up a pellet, and she can release a cube into a cup after it has been demonstrated to her. She tries to build a tower of two cubes with variable success. She is most likely at which of the following age?
2 months
4 months
6 months
9 months
1 year
A child is brought to the physician for a routine visit. On examination, the child can name multiple items in the examination room, and can also combine 2 words into a short sentence. His mother estimates that he knows about 200 words. When his mother tries to help him onto the examination table, he says "me do it." Although his mother seems to understand most of what he says, you can only understand about half of his speech. Which of the following is the most likely age of this child?
12 months
15 months
18 months
24 months
36 months
A child is brought to your clinic for a routine examination. She can put on a T-shirt but requires a bit of help dressing otherwise. She can copy a circle well but has difficulty in copying a square. Her speech is understandable and she knows four colors. She balances proudly on each foot for 2 seconds but is unable to hold the stance for 5 seconds. Which of the following is the most likely age of this child?
1 year
2 years
3 years
4 years
5 years
A college student is tackled while playing football and develops severe knee pain. When examined shortly thereafter, the knee is swollen and the patient has pain on direct palpation over the lateral aspect of the knee. With the knee flexed 30 degrees, passive adduction elicits pain on the same area, and the leg can be adducted further than in the normal contralateral leg (varus stress test). The anterior drawer test, posterior drawer test, and Lachman test are negative. Which of the following is the most likely site of injury?
Anterior cruciate ligament
Lateral collateral ligament
Lateral meniscus
Medial collateral ligament
Posterior cruciate ligament
A couple presents to your office to discuss permanent sterilization. They have three children and are sure they do not want any more. You discuss the risk and benefits of surgical sterilization. Which of the following statements is true regarding surgical sterilizations?
They cannot be performed immediately postpartum
They have become the second most common method of contraception for white couples between 20 and 40 years of age in the United States
Tubal ligation should be performed in the secretory phase of the menstrual cycle
They can be considered effective immediately in males (vasectomy)
They can be considered effective immediately in females (bilateral tubal ligation)
A female infant develops cyanosis. She was delivery vaginally at 43 weeks' gestation, and the amniotic fluid had a greenish color. She has dry, peeling skin, emaciated extremities and long fingernails. Tachypnea, nasal flaring, and sub- and intercostal retractions are observed. Auscultation reveals rales and rhonchi. The chest radiograph reveals flattening of the diaphragm, hyperinflation of the lungs, and patchy opacities diffusely distributed over both lung fields. Arterial blood gases reveal hypoxia and hypercarbia. What is most likely impairing the normal respiratory function of this newborn?
Fetal lung fluid
Meconium
Poor alveolar compliance
Paralysis of the diaphragm
Fibrosis of the lungs
A football player is tackled, and he develops severe knee swelling and pain. On physical examination with the knee flexed at 90 degrees, the leg can be pulled anteriorly, like a drawer being opened. A similar finding can be elicited with the knee flexed at 20 degrees by grasping the thigh with one hand, and pulling the leg with the other. Which of the following is the most likely injured structure?
Anterior cruciate ligament
Medial collateral ligament
Medial meniscus
Posterior cruciate ligament
Lateral collateral ligament
A full-term infant is brought to the office on her 6th day of life because her mother noted that she looked "yellow". The mother states that the infant is strictly breast-fed and has been eating every 2-3 hours. On examination, she is noted to be jaundiced over her trunk and face. There is no scleral icterus. She is otherwise healthy. Both the mother and baby are Rh positive. Which of the following is the most likely cause of this infant's jaundice?
Breast-feeding jaundice
Hypothyroidism
Glucose-6-phosphate dehydrogenase (G6PD) deficiency
Physiologic jaundice
Rh incompatibility
A healthy 29-year-old gravida 2 woman at 39 weeks has been in labor for 3 hours. She had a positive vaginal-anal culture for GBS at 37 weeks’ gestation. Which one of the following statements is correct?
Asymptomatic rectovaginal colonization is present in 60% of pregnant women
The transmission rate from mother to baby is approximately 25%
Neonatal sepsis occurs in 1% of colonized mothers
A rectovaginal culture should have been obtained at the first prenatal visit
Treatment with penicillin in labor is necessary only for heavy colonized mothers
A husband and wife present to the ED with 1 day of subjective fever, vomiting, watery diarrhea, and abdominal cramps. They were at a restaurant a day before for dinner and both ate the seafood special, which consisted of raw shellfish. In the ED, they are both tachycardic with temperatures of 99.8°F and 99.6°F for him and her, respectively. Which of the following is responsible for the majority of acute episodes of diarrhea?
Parasites
Viruses
Enterotoxin-producing bacteria
Anaerobic bacteria
Invasive bacteria
A long-time patient calls your office to speak with you directly. She voices frustration with your receptionist, who has repeatedly refused to allow her to schedule an appointment to see you. The patient says that at her last visit, she had a heated argument with the receptionist about a minor detail regarding her insurance coverage. When she has called since then, the receptionist always responds by saying, "I'm sorry, but there are too many patients waiting ahead of you." Which of the following defense mechanisms is the receptionist demonstrating?
Distortion
Passive-aggressive behaviour
Displacement
Acting out
Introjection
A middle-aged man with symptomatic carotid stenosis underwent a carotid endarterectomy on the right side. The area of significant stenosis extended from die carotid bifurcation up into the internal carotid, requiring a very high dissection and clamping of the vessel. The endarterectomy was done with an in situ shunt and closed with a Dacron patch. In the postoperative period, the patient has persistent difficulty swallowing solids and even more difficulty swallowing liquids. Any attempt to do so results in violent coughing and aspiration. His lips look symmetric and move normally, he speaks in a normal tone of voice without tiring, and he has no trouble breathing. When he is asked to stick his tongue out, he does so without deviation to either side. His symptoms are due to intraoperative damage of which of the following nerves?
Main trunk of the tenth (vagus) nerve
Mandibular branch of the seventh (facial) nerve
Trunk of the twelfth (hypoglossal) nerve
Superior laryngeal branch of the tenth (vagus) nerve
Sensory fibers of the ninth (glossopharyngeal) nerve
A maternal fetal medicine specialist is consulted and performs an in-depth sonogram on a 30-year-old G1 at 28 weeks with a twin gestation. The sonogram indicates that the fetuses are both male, and the placenta appears to be diamniotic and monochorionic. Twin B is noted to have oligohydramnios and to be much smaller than twin A. Which of the following would be a finding most likely associated with twin A?
Congestive heart failure
Anemia
Hypovolemia
Hypotension
Low amniotic fluid level
A mother brings her 3-year-old son to the pediatrician because he has had 7 days of fever and a painful swollen lymph node in his right groin. This is the boy's sixth episode of lymph node swelling; previous episodes resolved after drainage and prolonged antibiotic therapy. The child also has a past medical history significant for pneumonia at 12 months of age that required chest tube placement for drainage. His maternal uncle died in childhood from recurrent infections. On examination, the boy is at the 5th percentile for both height and weight His temperature is 38.5 c (101.3 F). There is an enlarged, tender lymph node in the right inguinal area with erythema and warmth of the overlying skin. There are several healed incisions in the inguinal regions bilaterally, as well as around the neck from old drainage sites. Laboratory analyses reveal the following: Hematocrit 35%, Platelet count 350,000/mm3, Leukocyte count 17000/mm3, Segmented neutrophils 65%, Bands 10%, Lymphocytes 25%. Gram stain of fluid aspirated from the affected lymph node reveals numerous bacteria-filled segmented neutrophils. Cultures grow S. aureus. What is the most likely mechanism underlying these findings?
Adenosine deaminase deficiency
Complement consumption
Defective opsonization
Destruction of CD4+ lymphocytes
Impaired oxidative metabolism within phagocytes
A mother brings her daughter into the clinic for a routine health-care visit. On examination, you note that she walks alone, knows two words, throws objects, and comes when called. What is the most likely age of this infant?
6 months
9 months
12 months
15 months
18 months
A mother brings her infant into the clinic for a routine visit. Examination reveals nothing abnormal. Developmental assessment shows that the infant sits well unsupported, enjoys looking around, babbles, and has a raking grasp. What is the most likely age of this infant?
4 months
6 months
8 months
10 months
12 months
A mother delivers a neonate with meconium staining and Apgar scores of 3 at 1 and 5 minutes of life. She had no prenatal care and the delivery was by emergency cesarean section for what the obstetricians report as “severe fetal bradycardia.”Which of the following sequelae could be expected to develop in this intubated neonate with respiratory distress?
Sustained rise in pulmonary arterial pressure
Microcephaly with micrognathia
Hyperactive bowel sounds
Cataracts
Thrombocytosis
A neonate born at term is found to have webbed neck and swollen hands and feet. Ultrasonogram of the abdomen shows a horseshoe kidney. Which of the following is the most likely cause of edema?
Immune mediated red cell destruction
Decreased synthesis of albumin
Dysgenesis of the lymphatic network
Increased urinary loss of protein
Severe intrauterine hypoxia
A neonate is found to have an imperforate anus. As the pediatric surgeon you recommend studies to search for other anomalies. Which of the following is an associated abnormality?
Congenital pulmonary airway malformation
Duodenal atresia
Congenital heart disease
Corneal opacities
Hydrocephalus
A neonate is noted to have many abnormalities, a number of which are located in the midline. The infant has cleft lip and cleft palate. His eyes are very small and have fissures of the iris, shallow supraorbital ridges, and slanted palpebral fissures. He is deaf, and the ears are low set and malformed. Each hand has six fingers and a simian crease. Which of the following congenital abnormalities of the brain is particularly likely to be present in this infant?
Anencephaly
Encephalocele
Hydranencephaly
Holoprosencephaly
Porencephaly
A newborn has a midline defect in the anterior abdominal wall. The parents ask what, if anything, should be done. Spontaneous closure of which of the following congenital abnormalities of the abdominal wall generally occurs by the age of 4?
Umbilical hernia
Patent omphalomesenteric duct
Omphalocele
Gastroschisis
Patent urachus
A newborn infant has respiratory distress and trouble feeding in the nursery. The mother has no significant medical history, but the pregnancy was complicated by decreased fetal movement. On physical examination, you note that aside from shallow respirations and some twitching of the fingers and toes, the infant is not moving, and is very hypotonic. In the mouth there is pooled saliva and you note tongue fasciculations. Deep tendon reflexes are absent. Spinal fluid is normal. Appropriate statements about this condition include which of the following statements?
The condition is caused by the absence of the muscle cytoskeletal protein dystrophin
The condition is caused by the degeneration of anterior horn cells in the spinal cord
The condition is caused by the antibodies that bind the acetylcholine receptor at the postsynaptic muscle membrane
The condition is caused by birth trauma
The condition is caused by progressive autoimmune demyelination
A newborn infant is brought to the nursery for evaluation after delivery. The mother reports that the pregnancy was uncomplicated, but she had only two prenatal visits. The infant was born via normal spontaneous vaginal delivery and required no resuscitation. The infant has hepatosplenomegaly on examination. While in the hospital, the infant requires treatment for anemia and hyperbilirubinemia. On subsequent examinations, the infant has clear rhinorrhea and ulcerative lesions on his feet. Which of the following congenital infections is most likely in this patient?
Toxoplasmosis
Syphilis
Rubella
Cytomegalovirus infection
Human immunodeficiency virus infection
A newborn is diagnosed with congenital heart disease. You counsel the family that the incidence of heart disease in future children is which of the following?
1%
15% to 20%
25% to 30%
2% to 6%
8% to 10%
A newborn is noted to be quite jaundiced at 3 days of life. Laboratory data demonstrate his total bilirubin to be 17.8 mg/dL (direct bilirubin is 0.3 mg/dL). Which of the following factors is associated with an increased risk of neurologic damage in a jaundiced newborn?
Metabolic alkalosis
Increased attachment of bilirubin to binding sites caused by drugs such as sulfisoxazole
Maternal ingestion of phenobarbital during pregnancy
Hyperalbuminemia
Neonatal sepsis
A one-month-old infant is brought to the physician for evaluation. His mother reports that for the past two weeks, he has been crying inconsolably for several hours every evening. His mother has tried multiple methods to calm the infant down, but nothing seems to work. The infant was born full term without complications. He takes two ounces of cow's milk-based formula every two hours and is growing well. His mother reports that he is happy and alert the rest of the day. The child's physical examination is unremarkable. Which of the following is a true statement about the child's condition?
The infant should be changed to a lactose-free formula
Bloody stools are often present
The infant should be started on ranitidine for gastroesophageal reflux
The child will likely develop an anxiety disorder during childhood
This condition usually resolves by four months of age
A one-year-old girl is brought to the office for the evaluation of sickle cell anemia. Both her parents have sickle cell trait, and her elder sister has sickle cell anemia. Her vital signs are stable. Her height and weight are appropriate for age. On examination, she appears healthy and normal. Her birth and past medical histories are insignificant. Hemoglobin electrophoresis reveals 40% hemoglobin S. What is the most common presentation of this condition?
Acute painful episodes
Painless hematuria
Splenic infarction
Dactylitis
Frequent UTI
{"name":"DES C_Basic (5) Prepared : CHILLY", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 63-year-old male is admitted for sudden onset severe chest pain. His ECG reveals ST elevation in leads V2-V6. He is treated with thrombolytic therapy, heparin, aspirin, metoprolol, morphine, and nitrates. A coronary angiogram performed after thrombolytic therapy reveals 50% obstruction of the left anterior descending artery. On the third day of hospitalization, the patient suddenly develops severe shortness of breath at rest and hypotension. Examination reveals a soft S1, an apical pansystolic murmur radiating to the axilla, and bibasilar crackles. His temperature is 37.8°C (100°F), blood pressure is 92\/58 mmHg, heart rate is 102\/min, and respirations are 31\/min. An echocardiogram performed on the second hospital day reveals an akinetic region of the anterior wall. What is the most likely explanation for this patient's deterioration?","img":"https://cdn.poll-maker.com/17-719174/image.jpeg?sz=1200"}
More Quizzes
Epic Quiz By Yacob
311627
Discover Your Perfect Summer Vibe!
10530
Get to know
420
Which Stardust Crusader are you?
10511
Ultimate Stray Kids: Test Your K-Pop IQ Now
201080105
Champions League Team: Discover Your Perfect Club
201023619
Free Social Studies Praxis 5004 Review
201021595
Dare to Conquer Our Roman Empire Trivia Today?
201071879
Aesthetic Who Am I? Find Your Signature Style Now!
201026205
Free Baby Trivia: Test Your Newborn Knowledge
201069524
Free Private Pilot Theory Knowledge
201027788
Which Teen Titans Character Are You? Free
201024616