Cardiovascular 3
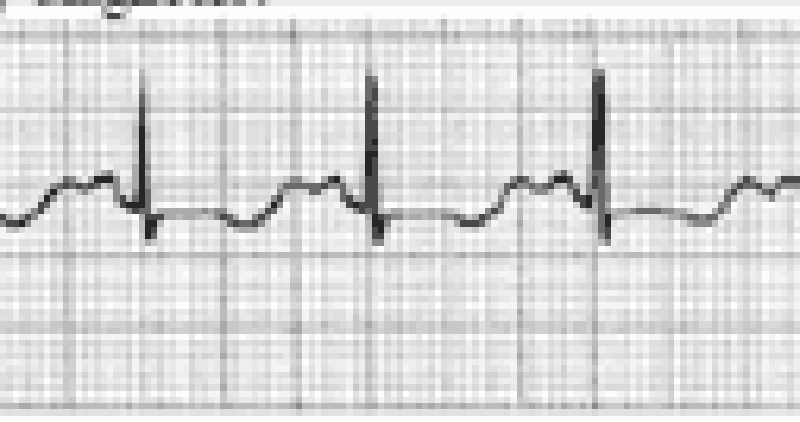
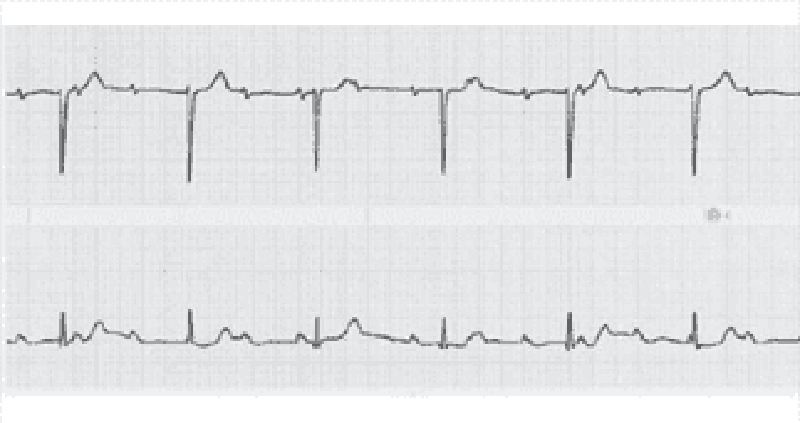
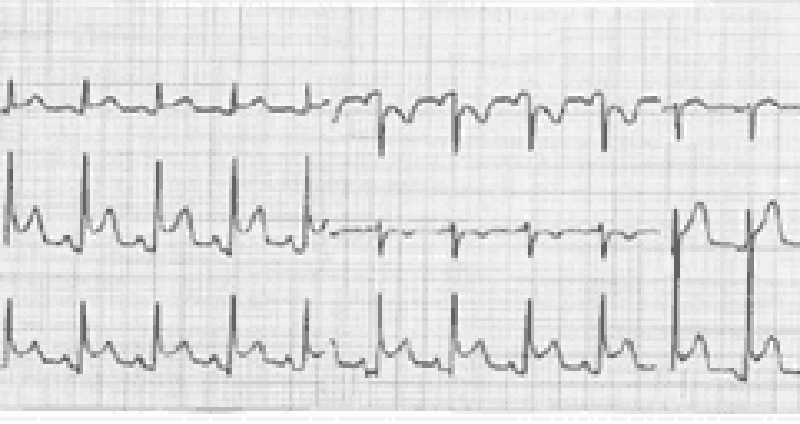
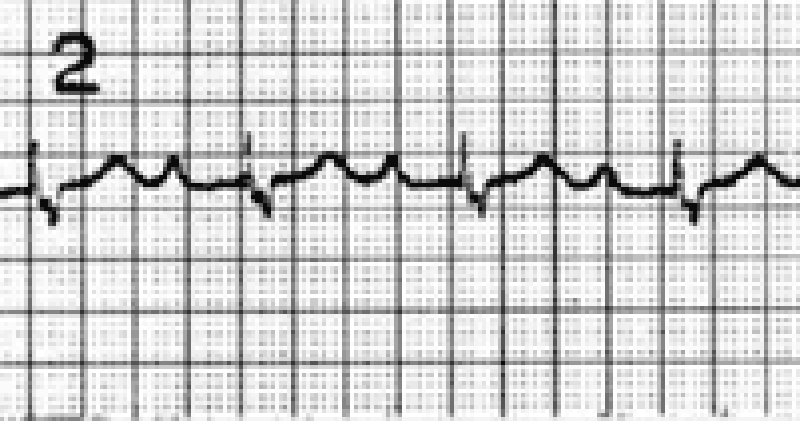
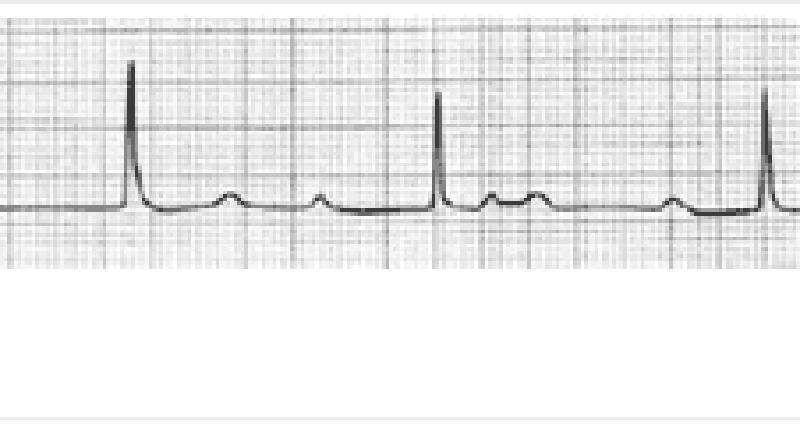
A 23-year-old woman who is an elementary school teacher is brought to the ED after syncopizing in her classroom while teaching. Prior to passing out, she describes feeling light-headed and dizzy and next remembers being in the ambulance. There was no evidence of seizure activity. She has no medical problems and does not take any medications. Her father died of a “heart problem” at 32 years of age. She does not smoke or use drugs. BP is 120/70 mm Hg, pulse rate is 71 beats per minute, RR is 14 breaths per minute, and oxygen saturation is 100% on room air. Her physical examination and laboratory results are all normal. A rhythm strip is seen below. Which of the following is the most likely diagnosis?
Wolff-Parkinson-White syndrome
Long QT syndrome
Lown-Ganong-Levine syndrome
Complete heart block
Atrial flutter
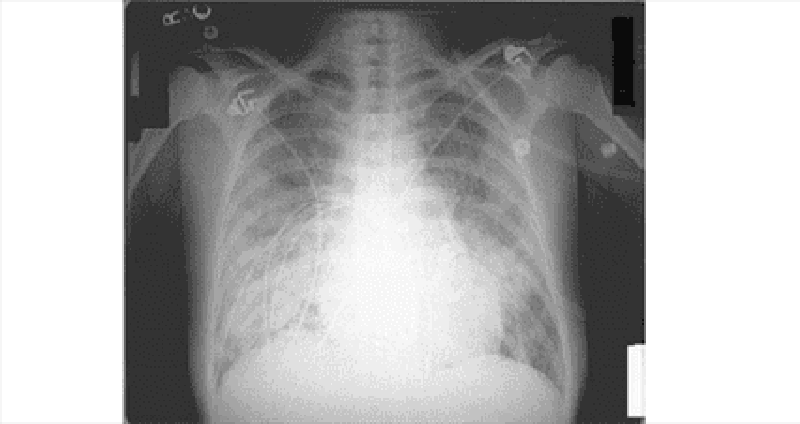
A 55-year-old man presents to the ED with chest pain and shortness of breath. His BP is 170/80 mm Hg, HR is 89 beats per minute, and oxygen saturation is 90% on room air. Physical examination reveals crackles midway up both lung fields and a new holosystolic murmur that is loudest at the apex and radiates to the left axilla. ECG reveals ST elevations in the inferior leads. Chest radiograph shows pulmonary edema with a normalsized cardiac silhouette. Which of the following is the most likely cause of the cardiac murmur?
Critical aortic stenosis
Papillary muscle rupture
Pericardial effusion
CHF
Aortic dissection
A 22-year-old man presents to the ED with a history consistent with an acute MI. His ECG reveals ST elevations and his cardiac biomarkers are positive. He has been smoking half a pack of cigarettes per day for the last 3 months. He drinks alcohol when hanging out with his friends. His grandfather died of a heart attack at 80 years of age. The patient does not have hypertension or diabetes mellitus and takes no prescription medications. A recent cholesterol check revealed normal levels of total cholesterol, lowdensity lipoprotein (LDL), and high-density lipoprotein (HDL). Which of the following is the most likely explanation for his presentation?
Cigarette smoking
Family history of heart attack at age 80 years
Incorrectly placed leads on the ECG
Undisclosed cocaine use
Alcohol use
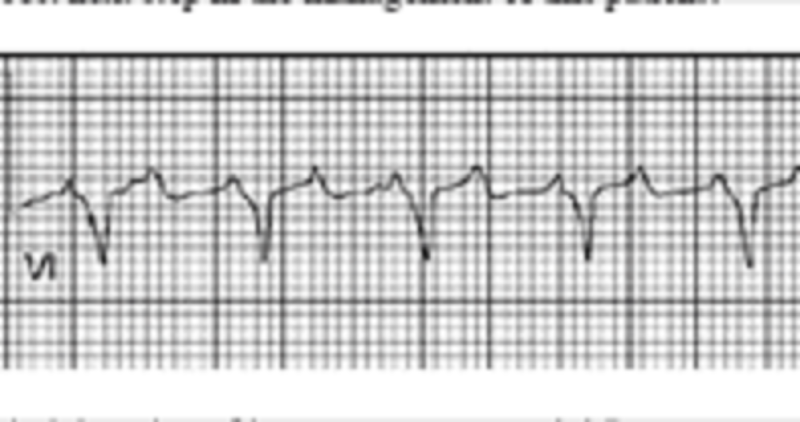
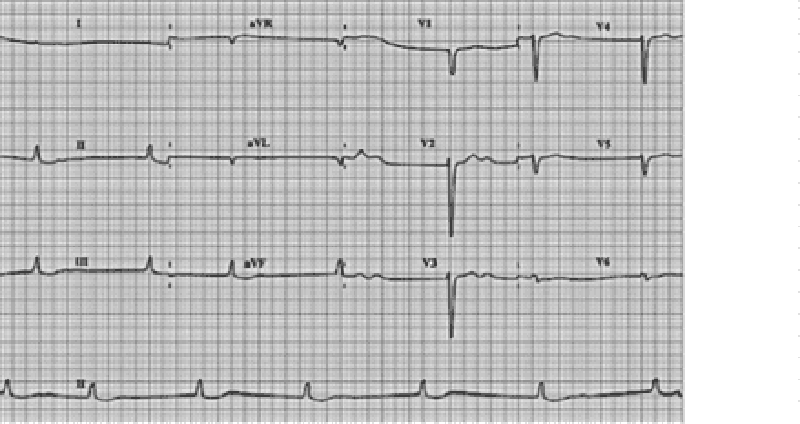
A 70-year-old male with a history of mild chronic kidney disease, diabetes mellitus, and CHF is admitted to your inpatient service with decreased urine output, weakness, and shortness of breath. He takes several medications but cannot remember their names. Labs are pending; his ECG is shown below. Based on the information available, what is the best initial step in management?
Administration of intravenous insulin
Administration of intravenous sodium bicarbonate
Administration of intravenous 3% hypertonic saline
Administration of oral sodium polystyrene sulfonate
Administration of intravenous calcium gluconate
A 59-year-old man presents to the emergency department (ED) complaining of new-onset chest pain that radiates to his left arm. He has a history of hypertension, hypercholesterolemia, and a 20-pack-year smoking history. His electrocardiogram (ECG) is remarkable for T-wave inversions in the lateral leads. Which of the following is the most appropriate next step in management?
Give the patient two nitroglycerin tablets sublingually and observe if his chest pain resolves
Place the patient on a cardiac monitor, administer oxygen, and give aspirin.
Call the cardiac catheterization laboratory for immediate percutaneous coronary intervention
Order a chest x-ray; administer aspirin, clopidogrel, and heparin.
Start a β-blocker immediately
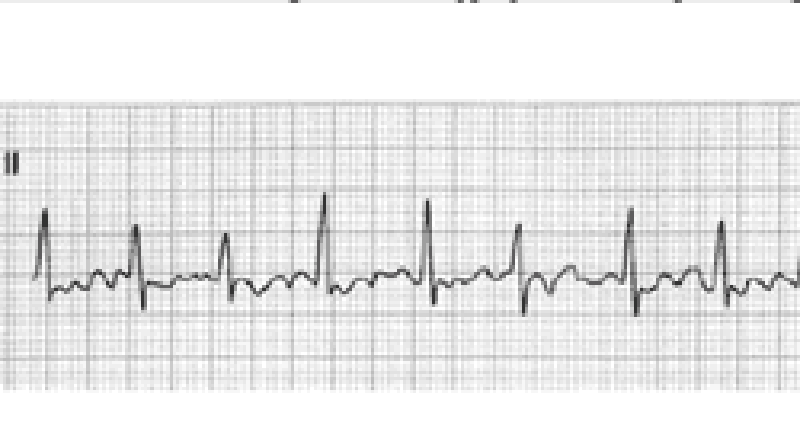
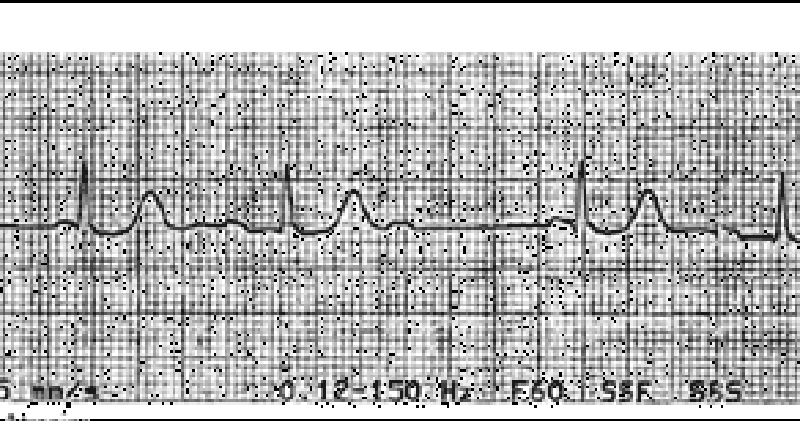
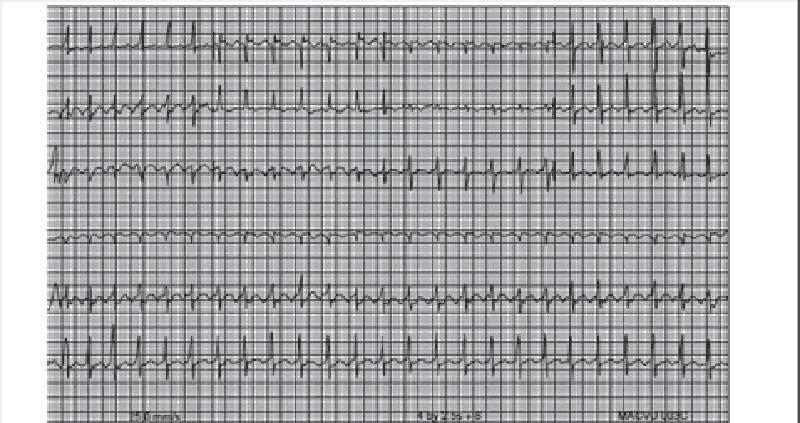
A 51-year-old man with a long history of hypertension presents to the ED complaining of intermittent chest palpitations lasting for a week. He denies chest pain, shortness of breath, nausea, and vomiting. He recalls feeling similar episodes of palpitations a few months ago but they resolved. His blood pressure (BP) is 130/75 mm Hg, heart rate (HR) is 130 beats per minute, respiratory rate (RR) is 16 breaths per minute, and oxygen saturation is 99% on room air. An ECG is seen below. Which of the following is the most appropriate next step in management?
Sedate patient for immediate synchronized cardioversion with 100 J.
Prepare patient for the cardiac catheterization laboratory
Administer warfarin
Administer amiodarone
Administer diltiazem
A 63-year-old insurance agent is brought to the ED by paramedics for shortness of breath and an RR of 31 breaths per minute. The patient denies chest pain, fever, vomiting, or diarrhea. His wife says he ran out of his “water pill” 1 week ago. His BP is 185/90 mm Hg, HR is 101 beats per minute, oxygen saturation is 90% on room air, and temperature is 98.9°F. There are crackles midway up both lung fields and 2+ pitting edema midway up his legs. An ECG shows sinus tachycardia. The patient is sitting up and able to speak to you. After placing the patient on a monitor and inserting an IV, which of the following is the most appropriate next step in management?
Obtain blood cultures and complete blood cell (CBC) count, and begin empiric antibiotic therapy
Order a statim (STAT) portable chest x-ray
Administer oxygen via nasal cannula and have the patient chew an aspirin
Administer oxygen via non-rebreather, furosemide, nitroglycerin, and consider noninvasive respiratory therapy
Rapid sequence endotracheal intubation
Emergency department with sudden onset of crushing substernal chest pain, nausea, diaphoresis and shortness of breath. His initial ECG revealed ST segment elevation in the anterior-septal leads. Cardiac enzymes were normal. The patient underwent emergent cardiac catheterization, which revealed only a 25% stenosis of the left anterior descending (LAD) artery. No percutaneous intervention was performed. Which of the following interventions would most likely reduce his risk of similar episodes in the future?
Placement of a percutaneous drug-eluting coronary artery stent
Placement of a percutaneous non-drug-eluting coronary artery stent
Beginning therapy with an ACE inhibitor
Beginning therapy with a beta-blocker
Beginning therapy with a calcium-channel blocker
A 15-year-old male presents to your office on the advice of his football coach. The patient started playing football this year and suffered a syncopal episode at practice yesterday. He reports that he was sprinting with the rest of the team and became lightheaded. He lost consciousness and fell to the ground, regaining consciousness within one or two minutes. He suffered no trauma during the event. He has no prior history of head injury or recent illness. He has had no prior episodes of syncope. The patient is adopted and family history unavailable. Physical examination is unremarkable. What is the best course of action regarding this patient’s syncopal episode?
Perform an ECG and echocardiogram. The patient may not return to competitive sports until results are available
Perform an ECG. The patient may not return to competitive sports until results are available
Perform an ECG. The patient may return to competitive sports pending the results
Reassurance. The patient may return to competitive sports provided he increases his water consumption during practice times
Reassurance. The patient may return to competitive sports with no restrictions
An 82-year-old white female is admitted to the hospital for observation after presenting to the emergency department with dizziness. After being placed on a cardiac monitor in the ER, the rhythm strip below was recorded. There is no past history of cardiac disease, diabetes, or hypertension. With prompting, the patient discloses several prior episodes of transient dizziness and one episode of brief syncope in the past. Physical examination is unremarkable. Which of the following is the best plan of care?
Reassurance. This is a benign condition, and no direct therapy is needed
Reassurance. The patient may not drive until she is symptom free, but otherwise no direct therapy is needed
Nuclear cardiac stress testing; treatment depending on results
Begin therapy with aspirin
Arrange placement of a permanent pacemaker
29-year-old woman presents to the emergency department with a 3-week history of being awakened by a dull, prolonged chest pain that occurs 3–4 times a week. She is a smoker but has never suffered a myocardial infarction (MI) or had chest pain before and has no family history of early MI. Results of a 12-lead ECG are normal. Her first set of cardiac enzyme measurements (creatine kinase, creatine kinase-MB fraction, troponin I) are negative. If coronary angiography were taken at the time of her chest pain, which of the following findings is most like?
Coronary artery spasm
Greater than 80% stenosis in at least two coronary arteries
No abnormal findings
Plaque rupture and thrombosis
Coronary artery dissection
A 42-year-old man presents to the emergency department with a complaint of increasing shortness of breath when walking to get his newspaper, difficulty breathing while lying fl at, and a 4.5-kg (10-lb) weight gain over the past month. He is afebrile, his pulse is 75/min, and his blood pressure is 98/50 mm Hg. On examination he smells of alcohol and has 2+ pitting edema in the lower extremities and a third heart sound. X-ray of the chest reveals cardiomegaly. What additional findings must be present to confirm this man’s underlying diagnosis?
Hepatojugular reflux and pulmonary congestion
Left ventricular dilation and aortic insufficiency
Left ventricular dilation and systolic dysfunction
Myocardial thickening and diastolic dysfunction
Pulmonary congestion and diastolic dysfunction
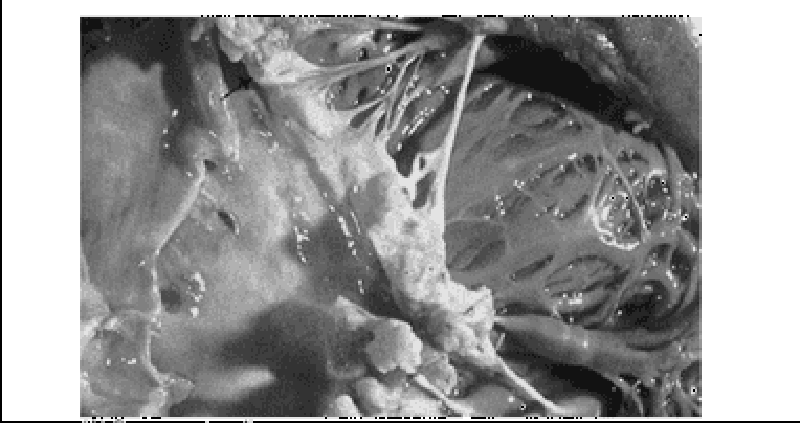
A 69-year-old man with rheumatic heart disease presents to the emergency department complaining of a fever and weakness on his left side. On physical examination the patient is weak in his left upper extremity and he draws only the right half of a clock. Shortly after his presentation, the patient dies, and an autopsy is performed. A gross view of the patient’s heart is shown in the image. Which of the following is a risk factor for the type of lesion pictured?
Coronary artery disease
Hypertension
Mitral valve prolapse@
Prolonged bedrest
Prosthetic valve replacement
An 83-year-old woman is being evaluated for confusion. She was admitted 3 days ago after having an acute MI. Her hospital course has been complicated by narrow-complex ventricular tachycardia, which has finally been stabilized on an antiarrhythmic medication. She was also started on a post-MI protocol and an antidepressant. One day after beginning these medications, she begins to develop confusion and slurred speech. Her temperature is 36.7°C (98.1°F), blood pressure is 138/60 mm Hg, pulse is 88/min, and respiratory rate is 14/min. She is alert and oriented to person, but she does not realize she is in the hospital. Additionally, she exhibits difficulty with word articulation, although she speaks fluently, and she demonstrates a mild resting tremor. The remainder of her examination is normal. Which of the following medications is most likely to cause these central nervous system effects?
Aspirin
Enalapril
Fluoxetine
Lidocaine
Metoprolol
Two weeks after hospital discharge for documented myocardial infarction, a 65-year-old returns to your office concerned about low-grade fever and pleuritic chest pain. There is no associated shortness of breath. Lungs are clear to auscultation and the heart is free of murmur, gallop, or rub. ECG is unchanged from the last one in the hospital. Which therapy is most likely to be effective?
Antibiotics
Anticoagulation with warfarin (Coumadin
An anti-inflammatory agent
An increase in antianginal medication
An anxiolytic agent
A 42-year-old man develops shortness of breath (SOB) and chest pain 7 days after an open cholecystectomy. His blood pressure is 145/86 mm Hg, pulse is 120/min, respirations 24/min, and oxygen saturation of 97%. Pulmonary embolism is clinically suspected. Which of the following is the most common ECG finding of pulmonary embolism?
A deep S wave in lead I
Depressed ST segments in leads I and II
Prominent Q wave in lead I, and inversion of T wave in lead III
Sinus tachycardia
Clockwise rotation in the precordial leads
A 42-year-old man with known valvular heart disease develops a fever for 1 week. He appears unwell; findings include a pansystolic murmur at the apex that radiates to the axilla and a soft S1 sound. He has petechiae on his conjunctival sac, linear hemorrhages under a few fingernails, and painful, tender, and erythematous nodules on some of the distal fingertips. Which of the following is the most responsible mechanism for these physical findings?
Direct bacterial invasion
Immune response
Vascular phenomena
Valvular damage
Preexisting cardiac dysfunction
A 67-year-old man presents with an anterior myocardial infarction (MI) and receives thrombolytic therapy. Three days later, he develops chest pain that is exacerbated by lying down, and his physical findings are normal except for a friction rub. His ECG shows evolving changes from the anterior infarction but new PR-segment depression and 1-mm ST-segment elevation in all the limb leads. Which of the following is the most likely diagnosis?
Reinfarction
Pulmonary embolus
Viral infection
Post-MI pericariditis
Dissecting aneurysm
A 55-year-old patient presents to you after a 3-day hospital stay for gradually increasing shortness of breath and leg swelling while away on a business trip. He was told that he had congestive heart failure, but is asymptomatic now, with normal vital signs and physical examination. An echocardiogram shows an estimated ejection fraction of 38%. The patient likes to keep medications to a minimum. He is currently on aspirin and simvastatin. Which would be the most appropriate additional treatment?
Begin an ACE inhibitor and then add a beta-blocker on a scheduled basis
Begin digoxin plus furosemide on a scheduled basis
Begin spironolactone on a scheduled basis.
Begin furosemide plus nitroglycerin
Given his preferences, no other medication is needed unless shortness of breath and swelling recur
Hemiparesis. Cardiac monitoring reveals atrial fibrillation. She had been in sinus rhythm on checkup 3 months earlier. Optimal management at discharge includes a review of antihypertensive therapy, a ventricular rate control agent, and which of the following?
Automated implanted cardioverter-defibrillator (AICD)/permanent pacemaker to avoid the need for anticoagulation
Immediate direct-current cardioversion
Antiplatelet therapy such as aspirin, without warfarin
Antiplatelet therapy plus warfarin with a target INR of 1.5
Warfarin with a target INR of 2.0 to 3.0
A 72-year-old male with a history of poorly controlled hypertension develops a viral upper respiratory infection. On his second day of symptoms he experiences palpitations and presents to the emergency room. His blood pressure is 118/78. The following rhythm strip is obtained. What is the best next step in the management of this patient?
Administration of intravenous metoprolol
Administration of intravenous adenosine
Administration of intravenous amiodarone
Emergent electrical cardioversion
Initiation of chest compressions and preparation for semielective intubation
A 48-year-old man presents to the emergency department complaining of crushing substernal chest pain. He is diaphoretic, anxious, and dyspneic. His pulse is 110/min, blood pressure is 175/112 mm Hg, respiratory rate is 30/min, and oxygen saturation is 94%. Aspirin, oxygen, sublingual nitroglycerin, and morphine are given, but they do not relieve his pain. ECG shows ST-segment elevation in leads V2 to V4. The duration of symptoms is now approximately 30 minutes. What is the most appropriate treatment for this patient at this time?
Calcium channel blocker
Intravenous angiotensin-converting enzyme inhibitor
Intravenous β-blocker
Magnesium sulfate
Tissue plasminogen activator
A 70-year-old woman presents to the emergency department complaining of dizziness. She is disoriented to the date and her location and it is difficult to gather an accurate history. Her pulse is 48/min, blood pressure is 84/60 mm Hg, and respiratory rate is 12/min. On examination her extremities are cool and clammy. Her capillary refill time is 5 seconds. What is the most appropriate therapy?
Adenosine
Miodarone
Atropine
Isoproterenol
Metoprolol
A 77-year-old man, complaining of abdominal pain, anorexia, and nausea and vomiting over the past 24 hours, presents to the clinic with his son. The son reveals that his father has also complained of blurred vision. The patient’s vital signs are stable and his abdomen is soft, but he appears to be somewhat confused. He is currently taking metoprolol, digoxin, and hydrochlorothiazide for ischemic congestive heart failure. His son says that sometimes his father confuses his medications. The patient also has renal insufficiency with a baseline serum creatinine of 2.6 mg/dL. The ECG reveals a widened QRS complex and a new first-degree heart block. Which of the following is the most likely cause of this patient’s symptoms?
Digoxin toxicity
Gastroenteritis
Hypocalcemia
Hypovolemia secondary to thiazide diuretic overuse
Myocardial infarction
An otherwise asymptomatic 65-year-old man with diabetes presents to the ER with a sports-related right shoulder injury. His heart rate is noted to be irregular, and this ECG is obtained. Which of the following is the best immediate therapy?
Atropine
Isoproterenol
Pacemaker placement
Electrical cardioversion
Observation
A patient has been in the coronary care unit for the past 24 hours with an acute anterior myocardial infarction. He develops the abnormal rhythm shown below, although blood pressure remains stable at 110/68. Which of the following is the best next step in therapy?
Perform cardioversion.
Arrange for pacemaker placement
Give digoxin.
Give propranolol.
Give lidocaine.
A 70-year-old male with a history of coronary artery disease presents to the emergency department with 2 hours of substernal chest pressure, diaphoresis, and nausea. He reports difficulty “catching his breath.” An electrocardiogram shows septal T-wave inversion. The patient is given 325-mg aspirin and sublingual nitroglycerin while awaiting the results of his blood work. His troponin I is 0.65 ng/mL (normal < 0.04 ng/mL). The physician in the emergency department starts the patient on low-molecular-weight heparin. His pain is 3/10. Blood pressure is currently 154/78 and heart rate is 72. You are asked to assume care of this patient. What is the best next step in management?
Arrange for emergent cardiac catheterization
Begin intravenous thrombolytic therapy.
Admit the patient to a monitored cardiac bed and repeat cardiac enzymes and ECG in 6 hours.
Begin intravenous beta-blocker therapy
Begin clopidogrel 300 mg po each day
You are volunteering with a dental colleague in a community indigent clinic. A nurse has prepared a list of patients who are scheduled for a dental procedure and may need antibiotic prophylaxis beforehand. Of the patients listed below, who would be most likely to benefit from antibiotic prophylaxis to prevent infective endocarditis?
17-year-old male with coarctation of the aorta
26-year-old female with a ventricular septal defect repaired in childhood
42-year-old female with mitral valve prolapse
65-year-old male with prosthetic aortic valve
72-year-old female with aortic stenosis
An 80-year-old woman was admitted to your service for dizziness. Cardiac monitoring initially revealed atrial fibrillation with rapid ventricular response. Her ventricular rate was controlled with beta-blocker. An echocardiogram revealed an enlarged left atrium and an ejection fraction of 50%. No evidence of diastolic heart dysfunction was noted. She is now asymptomatic, with blood pressure 130/80, heart rhythm irregularly irregular, and heart rate around 80/minute. Which of the following is the best management strategy of this patient’s arrhythmia?
Electrical cardioversion plus prolonged anticoagulation
Electrical cardioversion without anticoagulation
Chemical cardioversion plus prolonged anticoagulation
Chemical cardioversion without anticoagulation
Continued rate control plus prolonged anticoagulation
You are seeing a 45-year-old female patient of your partner for the first time in your clinic. A quick review of the patient’s medical record shows that her systolic blood pressure was greater than 140 mm Hg at both of her last clinic appointments. Her medical history is otherwise significant only for diabetes mellitus. Her blood pressure today is 164/92. What is the best next step in her blood pressure management?
Ask the patient to keep a written record of her blood pressure and bring with her to a return appointment
Advise the patient to begin a heart healthy, low sodium diet and refer to a nutritionist
Prescribe an ACE inhibitor in addition to heart healthy diet
Prescribe a dihydropyridine calcium-channel blocker in addition to a heart healthy diet
Arrange for echocardiogram to assess for end-organ damage.
A 68-year-old male complains of pain in his calves while walking. He notes bilateral foot pain, which awakens him at night. His blood pressure is 117/68. Physical examination reveals diminished bilateral lower extremity pulses. An ankle: brachial index measures 0.6. The patient’s current medications include aspirin and hydrochlorothiazide. Which of the following is the best initial management plan for this patient’s complaint?
Smoking cessation therapy, warfarin
Smoking cessation therapy, graduated exercise regimen, cilostazol
Smoking cessation therapy, schedule an arteriogram
Smoking cessation therapy, warfarin, peripherally acting calcium-channel blocker
Smoking cessation therapy, consultation with a vascular surgeon
An 82-year-old woman is brought to the ED by her daughter for worsening fatigue, dizziness, and light-headedness. The patient denies chest pain or shortness of breath. She has not started any new medications. Her BP is 140/70 mm Hg, HR is 37 beats per minute, and RR is 15 breaths per minute. An IV is started and blood is drawn. An ECG is seen below. Which of the following is the most appropriate next step in management?
Bed rest for the next 48 hours and follow-up with her primary-care physician
Administer aspirin, order a set of cardiac enzymes, and admit to the cardiac care unit (CCU).
Place a magnet on her chest to turn off her pacemaker.
Admit for Holter monitoring and echocardiogram
Place on a cardiac monitor, place external pacing pads on the patient, and admit to the CCU.
A 66-year-old retired carpenter presents with chronic shortness of breath upon exertion. He has smoked one pack of cigarettes per day for the past 5 years and drinks alcohol regularly. Physical examination reveals a displaced point of maximal impulse and hepatosplenomegaly. His medications include pantoprazole for gastroesophageal reflux and sertraline for depression. Echocardiogram reveals an ejection fraction of 30% and dilated left and right ventricles. Laboratory tests show: Na+: 129 mEq/L K+: 5.2 mEq/L Cl−: 101 mEq/L Blood urea nitrogen: 45 mg/dL Creatinine: 1.3 mg/dL Glucose: 134 mg/dL Aspartate aminotransferase: 220 U/L Alanine aminotransferase: 140 U/L Alkaline phosphatase: 280 U/L Which of the following is the most likely cause of his cardiac findings?
Borrelia burgdorferi
Cigarette smoking
Coxsackie B virus
Ethanol
Pantoprazole toxicity
A 52-year-old man presents to his primary care physician’s office for routine care. He has hypertension, hypercholesterolemia, and type 2 diabetes mellitus, and has smoked one pack of cigarettes per day for the past 30 years. Medications include hydrochlorothiazide, atorvastatin, and glipizide. There is a family history of myocardial infarction in the maternal grandfather at age 60. The patient has undergone screening for colon and prostate cancer. Physical examination reveals a pleasant, obese man who is 175 cm (5′9″) tall and weighs 108 kg (238 lb). His blood pressure is 155/81 mm Hg, heart rate is 78/min, respiratory rate is 14/min, and temperature is 36.8°C (98.3°F). What one action would most reduce the patient’s stroke risk?
Blood glucose reduction
Blood pressure reduction
Serum cholesterol reduction
Smoking cessation
Weight loss
A 29-year-old tall, thin man presents to the ED after feeling short of breath for 2 days. In the ED, he is in no acute distress. His BP is 115/70 mm Hg, HR is 81 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 98% on room air. Cardiac, lung, and abdominal examinations are normal. An ECG reveals sinus rhythm at a rate of 79. A chest radiograph shows a small right-sided (< 10% of the hemithorax) spontaneous pneumothorax. A repeat chest x-ray 6 hours later reveals a decreased pneumothorax. Which of the following is the most appropriate next step in management?
Discharge the patient with follow-up in 24 hours
Perform needle decompression in the second intercostal space, midclavicular line.
Insert a 20F chest tube into right hemithorax.
Observe for another 6 hours.
Admit for pleurodesis.
A 47-year-old man with a history of hypertension presents to the ED complaining of continuous left-sided chest pain that began while snorting cocaine 1 hour ago. The patient states he never experienced chest pain in the past when using cocaine. His BP is 170/90 mm Hg, HR is 101 beats per minute, RR is 18 breaths per minute, and oxygen saturation is 98% on room air. The patient states that the only medication he takes is alprazolam to “calm his nerves.” Which of the following medications is contraindicated in this patient?
Metoprolol
Diltiazem
Aspirin
Lorazepam
Nitroglycerin
A 32-year-old woman presents to the ED with a persistent fever of 101°F over the last 3 days. The patient states that she used to work as a convenience store clerk but was fired 2 weeks ago. Since then, she has been using drugs intravenously daily. Cardiac examination reveals a heart murmur. Her abdomen is soft and nontender with an enlarged spleen. Chest radiograph reveals multiple patchy infiltrates in both lung fields. Laboratory results reveal white blood cells (WBC) 14,000/μL with 91% neutrophils, hematocrit 33%, and platelets 250/μL. An ECG reveals sinus rhythm with first-degree heart block. Which of the following is the most appropriate next step in management?
Obtain four sets of blood cultures, order a TTE, and start antibiotic treatment.
Order a monospot test and recommend that the patient refrain from vigorous activities for 1 month.
Administer a nonsteroidal anti-inflammatory drug (NSAID) and inform the patient she has pericarditis
Administer isoniazid (INH) and report the patient to the Department of Health.
Order a Lyme antibody and begin antibiotic therapy
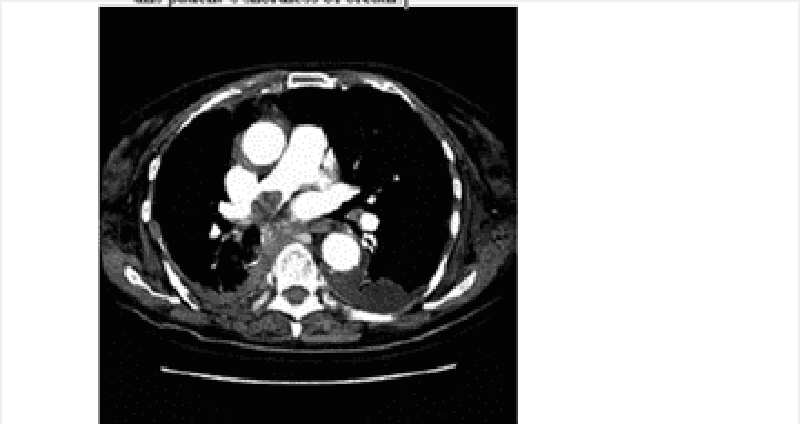
Two and a half weeks after coronary artery bypass grafting, a 63-year-old man returns to the emergency department acutely short of breath. The patient states that he began having chest pain and shortness of breath approximately 1 hour earlier. He has a history of hypertension, diabetes, and two myocardial infarctions. On examination he is hypoxic with an oxygen saturation of 86% on room air. Other vital signs and results of a physical examination are normal. ECG shows no interval change from his most recent ECG. CT of the chest is shown in the image. What is the most likely etiology of this patient’s shortness of breath?
Aortic dissection
Exacerbation of chronic obstructive pulmonary disease
Myocardial infarction
Pleural effusion
Pulmonary embolus
A 35-year-old woman presents to the clinic because of visual problems. She states that she has always had difficulty looking up, and over the past few years her overall vision has become blurry. Review of symptoms is notable for several recent episodes of “near fainting.” She takes no medication and has no other medical history, and has not seen a physician for 7 years. Because she was adopted as a child, she does not know her family history, but her son has required special tutoring at school. The patient also remarks that her son seems to have been dropping objects lately. Physical examination reveals bilateral ptosis. Her extraocular movements are intact and the pupils are equal, round, and reactive. Her corrected visual acuity is 20/100 in the right eye and 20/120 in the left eye. The view of the fundus is obscured. On ambulation she raises her knees and makes a slapping sound on the floor as she walks. ECG indicates heart block. What is the pathogenesis of this patient’s disorder?
Borrelia burgdorferi infection
Deletion mutation in dystrophin
Frameshift mutation in dystrophin
Trinucleotide repeat expansion
X-linked emerin deficiency
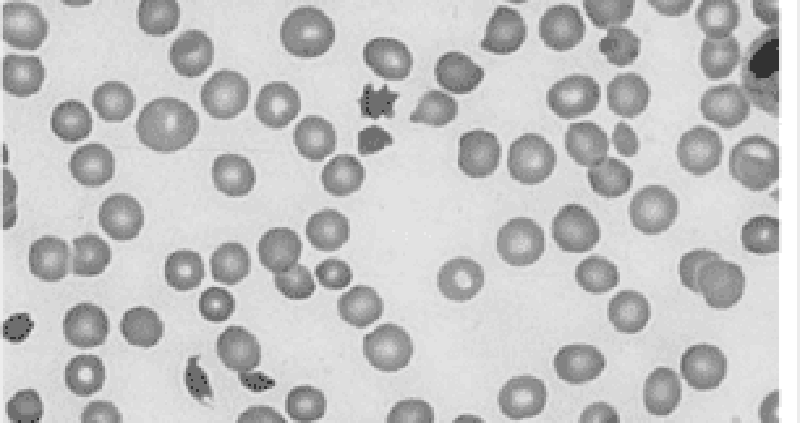
A college sophomore is found by his roommate emergency department. After resuscitation, the man complains of a severe headache and photophobia that is accompanied by dizziness, nausea, vomiting, and neck pain. Physical examination is noteworthy for positive Kernig’s and Brudzinski’s signs as well as petechiae on the trunk and mucocutaneous bleeding. Laboratory studies show: WBC count: 17,000/mm3 Hemoglobin: 11 g/dL Platelet count: 70,000/mm3 Bleeding time: 10 min Prothrombin time: 17 sec Activated partial thromboplastin time: 47 sec Thrombin time: 18 sec A peripheral blood smear is shown in the image. Which of the following is the most likely diagnosis?
Disseminated intravascular coagulation
Factor V Leiden
Immune thrombocytopenic purpura
Protein C deficiency
Thrombotic thrombocytopenic purpura
A 60-year-old man with coronary artery disease, peptic ulcer disease, and gout presents to the emergency department with a 24-hour history of abdominal pain. The pain, which is most intense in the upper abdomen, was sudden in onset and has become progressively more severe. Free air in the abdomen is detected on x-ray films. The patient is in an agitated state. His extremities are cool and capillary refill time is 3 seconds. His blood pressure is 80/40 mm Hg and heart rate is 130/min. The neck veins are flat and the lungs are clear to auscultation. His hemoglobin is 13.8 g/dL. A urinary catheter is inserted and 10 mL of urine is drained. What is the most appropriate treatment for this patient at this time?
Broad-spectrum antibiotics for presumed sepsis
Infusion of isotonic fluid
Infusion of norepinephrine
Inotropic support with dopamine, vasopressin, or dobutamine
Transfuse with 1 unit packed RBCs
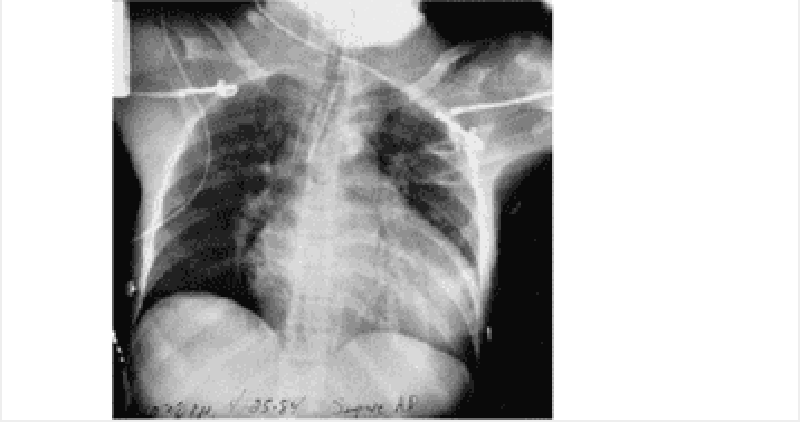
A 43-year-old woman presents to the emergency department because of chest pain, shortness of breath, and worsening fatigue for the past day. The chest pain initially worsened with lying down and improved with leaning forward, but now it seems equal in intensity over all positions. On physical examination she has labored, fast breathing and appears to be in pain. She has jugular venous distention. She is tachycardic, has a regular rhythm, and has distant heart sounds with a friction rub. Her lungs are clear to auscultation bilaterally, her abdominal examination is benign, and she has no peripheral edema. Her temperature is 39.0°C (102.2°F), pulse is 126/min, blood pressure is 89/66 mm Hg, respiratory rate is 32/min, and oxygen saturation is 98% on room air. X-ray of the chest is shown in the image. Which of the following is the most likely diagnosis?
Cardiac tamponade
Decompensated congestive heart failure
Panic attack
Pericarditis
Tension pneumothorax
An elderly man presents to the emergency department with chest pain. He has a history of stable angina and recent onset diabetes mellitus, but now the chest pain comes on with less exertion and takes longer to go away. An ECG and cardiac enzymes are ordered. If this man has unstable angina, what are the expected findings on ECG and cardiac enzyme testing?
Delta waves on the ECG and elevated cardiac enzyme levels
Low voltage ECG and elevated cardiac enzyme levels
No changes on ECG and elevated cardiac enzyme levels
ST-segment depressions on ECG and normal cardiac enzyme levels
ST-segment elevations with Q waves and normal cardiac enzyme levels
A 19-year-old man complains of chest pain while playing basketball on his high school team. Paramedics are called and he is rushed to the hospital. Physical examination reveals moderate mitral regurgitation and a crescendodecrescendo systolic ejection murmur that gets louder with Valsalva maneuver. Echocardiography reveals thickened left ventricular walls and dynamic left ventricular outflow tract obstruction. What is the best first step in management?
β-Blockers
Calcium channel blockers
Partial excision of the interventricular septum
Warfarin
Digoxin
A 47-year-old woman who is 2 weeks post triple bypass surgery presents to the emergency department with a chief complaint of sudden onset, sharp chest pain for several hours. She is fatigued and short of breath. On physical examination she has distended neck veins that grow more distended on inspiration. Muffled heart sounds are heard. Her temperature is 37.0°C (98.6°F), pulse is 133/min, blood pressure is 70/50 mm Hg, respiratory rate is 30/ min, and oxygen saturation is 100% on room air. An echocardiogram shows a large pericardial effusion and chamber collapse; therefore, pericardiocentesis is performed. Although a large amount of blood is aspirated, the patient’s clinical picture acutely worsens. Her pain level increases substantially; pulse is 150/min, blood pressure is 60/41 mm Hg, respiratory rate is 30/ min, and oxygen saturation is 100%. Repeat echocardiography shows an even larger pericardial effusion with chamber collapse. Which complication of pericardiocentesis is most likely in this patient?
Acute left ventricular failure with pulmonary edema
Aspiration of 10 mL air into the pericardium
Laceration of a coronary vessel
Pneumothorax
Puncture of the left ventricle
A 57-year-old man presents to the emergency department with worsening substernal chest pain occurring over the past 20 minutes. He has a medical history significant for a 2-packper- day smoking history, gout, obesity, hypercholesterolemia, hypertension, osteoarthritis of both knees, inflammatory bowel disease, and recently diagnosed type 2 diabetes mellitus that is well controlled on oral antiglycemics (haemoglobin A1c of 7.8%). On physical examination he is in moderate distress, diaphoretic, and nauseous. His temperature is 37.5°C (99.5°F), pulse is 112/min, blood pressure is 142/85 mm Hg, and respiratory rate is 22/min. He tests positive for MI by serial cardiac enzymes. He is started on the appropriate therapy and is ready for discharge the following evening. What is the number one preventive measure this patient can take to decrease his immediate risk for a second MI?
Decrease the amount of cholesterol in his diet
Exercise three times a week
Lower his blood pressure to the 120/80 mm Hg range
Lower his blood sugar levels to achieve a hemoglobin A1c level <7%
Quit smoking
A 31-year-old kindergarten teacher presents to the ED complaining of acute-onset substernal chest pain that is sharp in nature and radiates to her back. The pain is worse when she is lying down on the stretcher and improves when she sits up. She smokes cigarettes occasionally and was told she has borderline diabetes. She denies any recent surgeries or long travel. Her BP is 145/85 mm Hg, HR is 99 beats per minute, RR is 18 breaths per minute, and temperature is 100.6°F. Examination of her chest reveals clear lungs and a friction rub. Her abdomen is soft and nontender to palpation. Her legs are not swollen. Chest radiography and echocardiography are unremarkable. Her ECG is shown below. Which of the following is the most appropriate next step in management?
Anticoagulate and CT scan to evaluate for a PE.
Prescribe a NSAID and discharge the patient
Aspirin, heparin, clopidogrel, and admit for ACS.
Administer thrombolytics if the pain persists
Prescribe antibiotics and discharge the patient
A 51-year-old woman presents to the ED after 5 consecutive days of crushing substernal chest pressure that woke her up from sleep in the morning. The pain resolves spontaneously after 20 to 30 minutes. She is an avid rock climber and jogs 5 miles daily. She has never smoked cigarettes and has no family history of coronary disease. In the ED, she experiences another episode of chest pain. An ECG reveals ST-segment elevations and cardiac biomarkers are negative. The pain is relieved with sublingual nitroglycerin. She is admitted to the hospital and diagnostic testing reveals minimal coronary atherosclerotic disease. Which of the following is the most appropriate medication to treat this patient’s condition?
Aspirin
Calcium channel blocker (CCB)
β-Blocker
H2-Blocker
Antidepressant
While discussing a case presentation with a medical student, a nearby patient who just returned from getting an ankle radiograph done yells out in pain. You walk over to him and ask what is wrong. He states that since returning from the radiology suite, his automatic implantable cardioverter defibrillator (AICD) is discharging. You hook him up to the monitor and note that his rhythm is sinus. You observe a third shock while the patient is in sinus rhythm. Which of the following is the most appropriate next step in management?
Send the patient back to the radiology suite for another radiograph to desensitize his AICD.
Administer pain medication and wait until the device representative arrives at the hospital to power off the AICD.
Admit the patient to the telemetry unit to monitor his rhythm and find the cause of his AICD discharge
Place a magnet over the AICD generator to inactivate it and thereby prevent further shocks.
Make a small incision over his chest wall and remove the AICD generator and leads
A 37-year-old woman with sarcoidosis presents to her primary care physician complaining of progressive fatigue and shortness of breath over the past 3 months. She also reports that her socks and shoes do not fi t the way they used to and that she fainted a few weeks ago for the first time in many years. She denies any recent illness and only takes medications to control her sarcoid. She states that she is more comfortable sitting than lying down. She has jugular venous distension, which increases with inspiration. Her blood pressure is 134/87 mm Hg, respiratory rate is 17/min, pulse is 96/min, and temperature is 37.2°C (98.9°F). She also has decreased breath sounds bilaterally at the bases. ECG shows decreased QRS voltage. An echocardiogram shows a thick left ventricle. Which of the following is the most likely diagnosis?
Aortic stenosis
Cardiac tamponade
Hypertensive heart disease
Pericarditis
Restrictive cardiomyopathy

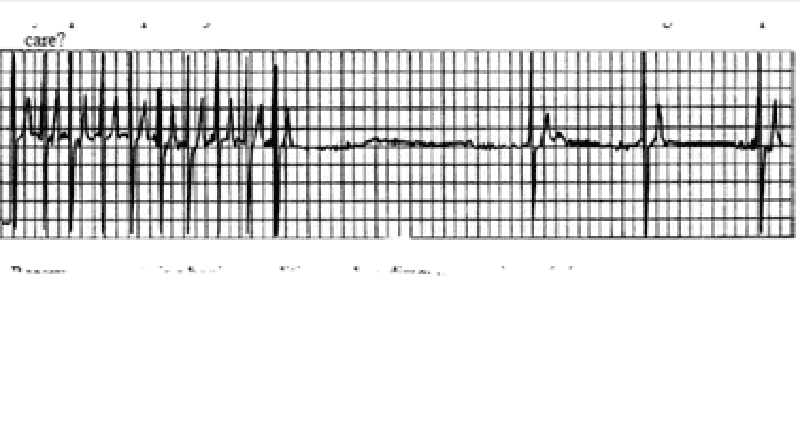
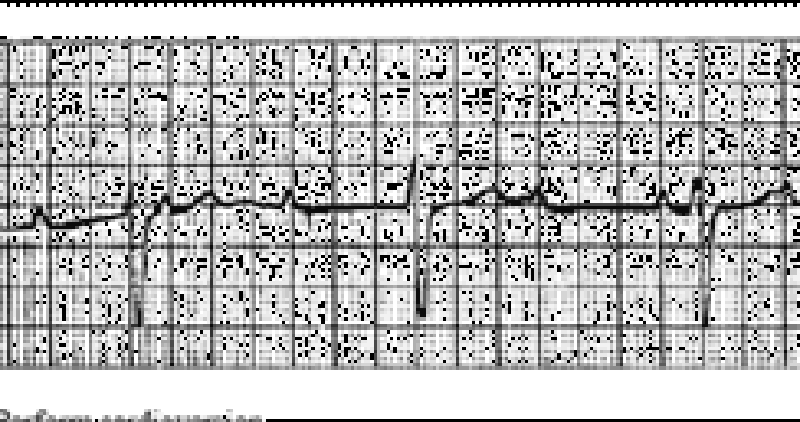
A 64-year-old man in the surgical intensive care unit goes into rapid atrial fibrillation on postoperative day one after a decortication for a loculated pulmonary empyema. He is given an appropriate loading dose of digoxin, but 4 hours after his second dose, the patient complains of increased palpitations and dizziness. The patient is conscious and hemodynamically stable. STAT serum blood tests show a potassium level of 5.0 mEq/L; all other electrolytes, including divalents, are in the normal range. The digitalis level is above the therapeutic range at 4 ng/mL (therapeutic range 0.5-2 ng/mL). Results of cardiac telemetry are shown in the image. Which of the following should be administered immediately?
Calcium
Furosemide
Magnesium
Potassium
Sodium polystyrene sulfonate
A 1-week-old infant presents to her general pediatrician’s office for a well-child visit. She was born at 37 weeks’ gestation without complications. Her temperature is 37.0°C (98.6°F), pulse is 130/min, blood pressure is 72/54 mm Hg, and respiratory rate is 28/min. She is currently at the 50th percentile for weight and 75th percentile for height. She is acyanotic and has a wide, fixed split S2, with a 2/6 systolic ejection murmur at the left upper sternal border. The remainder of the examination is unremarkable. Which of the following is the most likely diagnosis?
Atrial septal defect
Coarctation of the aorta
Dextratransposition of the great arteries
Tetralogy of Fallot
Ventricular septal defect
A 61-year-old man has a non-ST-elevation MI and is admitted to the coronary care unit. The following day, he develops bradycardia but no symptoms. His blood pressure is 126/84 mmHg, pulse 50/min, and on examination, the heart sounds are normal, with no extra sounds or rubs. His ECG has changed. Which of the following ECG findings is the best indication for this patient to receive a pacemaker?
Persistent bradycardia
Second-degree AV block Mobitz type I
First-degree AV block
New right bundle branch block
Left bundle branch block (LBBB) and second-degree AV block Mobitz type II
. A 63-year-old woman on digitalis for chronic atrial fibrillation experiences fatigue, nausea, and anorexia. Her pulse is regular at 50 beats/min, and the heart sounds, chest, and abdominal examinations are normal. On the ECG, no P waves are visible and the QRS complexes are narrow and regular. Which of the following is the most appropriate management step?
An increase in digitalis dose
Complete cessation of digitalis
Withdrawal of digitalis for one dose
Addition of a beta-blocker
Addition of a calcium channel blocker
A 26-year-old white nonsmoking woman returns for a follow-up appointment with her primary care provider. At a routine health maintenance visit 8 months earlier, her blood pressure was 179/97 mm Hg. Since then she has adhered to a low-fat diet and exercises regularly. On repeat measurement 1 month later, her blood pressure was still elevated, despite her compliance with the prescribed hydrochlorothiazide and lisinopril. She has no complaints and denies headaches, chest pain, or mental status changes. On physical examination she is a slender woman in no apparent distress. An abdominal bruit that lateralizes to the left is heard. Her blood pressure is 178/99 mm Hg in her left arm and 181/95 mm Hg in her right arm. A basic metabolic panel and complete blood count are within normal range. Which of the following is the most appropriate next step in patient care?
Add a statin to the patient’s current drug regimen to decrease fatty arterial plaques
Admit patient to the hospital and start intravenous nitroprusside
Increase the dosage of her antihypertensive regimen
Order duplex imaging of the renal arteries and proceed to percutaneous transluminal angioplasty if renal artery stenosis is found
Order duplex imaging of the renal arteries and proceed to surgical revascularization if renal artery stenosis is found
A 49-year-old man presents to the clinic for a health maintenance visit. He has no complaints, but he requests a prescription for his “pressure pills,” as he lost his original prescription. On physical examination his blood pressure is 220/130 mm Hg. Physical examination is otherwise within normal limits. Laboratory tests show: Na+: 142 mEq/L K+: 3.8 mEq/L Cl−: 105 mEq/L Carbon dioxide: 25 mEq/L Blood urea nitrogen: 20 mg/dL Creatinine: 1.0 mg/dL Glucose: 133 mg/dL Urinalysis is within normal limits, and his ECG is normal. Which of the following is the most effective management?
Administer intravenous nitroprusside for management of hypertensive emergency
Administer intravenous nitroprusside for management of hypertensive urgency
Administer oral furosemide for management of hypertensive emergency
Administer oral metoprolol for management of hypertensive urgency
Administer sublingual nifedipine for management of hypertensive emergency
A 22-year-old primagravida woman develops hypertension at 28 weeks. She is asymptomatic and the examination is normal except for 1+ pedal edema. Her complete blood count, liver enzymes, and electrolytes are normal. The urinalysis is positive for proteinuria. Which of the following is true for this type of hypertension?
Improves in the third trimester
Leads to large-birth-weight babies
Should be controlled with medications
Spares the placenta
Spares maternal kidney function
A 58-year-old man is admitted to the coronary care unit for telemetric monitoring after an episode of bradycardia. While in the unit, he suddenly loses consciousness. His pulse is undetectable and his blood pressure drops to 40 mm Hg. His airway is clear and patent, and he is still breathing on his own. An ECG shows electrical activity. Chest compressions are started and he is quickly given a bolus of intravenous sodium bicarbonate and atropine. When his tracing does not improve, the boluses are repeated twice, and finally his tracing returns to normal sinus rhythm. Moments later, when he regains consciousness, he complains of a dry mouth, blurred vision, and feeling flushed. What is the most appropriate next step in the management of this patient?
This patient has atropine toxicity and requires urgent administration of a cholinergic agonist
This patient has atropine toxicity and requires urgent administration of a muscarinic agonist
This patient has atropine toxicity and requires urgent administration of a muscarinic agonist
Patient is experiencing transient adverse effects of atropine and requires only supportive measures
This patient is experiencing transient adverse effects of bicarbonate and requires only supportive measures
A 62-year-old man with a history of benign prostatic hyperplasia and hypertension presents to his primary care provider for a routine health maintenance visit. He reports that he feels “better than ever” and explains that his daughter made him come in for his annual visit. He takes prazosin daily and occasionally some acetaminophen. He has no drug allergies and denies smoking, drinking, or the use of illicit drugs. His physical examination is within normal range except for his rectal examination, which revealed an enlarged prostate. His temperature is 36.8°C (98.2°F), respiratory rate is 13/min, pulse is 82/min, and blood pressure is 138/86 mm Hg. Which of the following is the most likely adverse effect of α1-adrenergic blockade in this patient?
Decreased urine flow
Increased blood pressure
Increased sexual drive
Rritability
Orthostatic hypotension
A 2-year-old girl is referred to the hospital for evaluation of her inability to gain weight. She is well fed by her parents, but appears to tire during feedings and has been losing weight despite frequent high-calorie meals. There is no family history of developmental delay or short stature. She is well dressed, her hair is brushed, and she is playful but tires quickly. Her temperature is 36.5°C (97.7°F), pulse is 110/min, blood pressure is 90/50 mm Hg, and respiratory rate is 24/min. She has a harsh 2/6 holosystolic murmur that is best heard at the left sternal border, which is unchanged and has been present since birth. Which of the following is the most appropriate next step in management?
Continue to monitor the patient for increased weight loss and increased shunting
PH probe for gastroesophageal refl ux disease
Refer for evaluation and possible closure of ventricular septal defect
Skeletal survey
Stool culture
Which of the following patients has the lowest clinical probability for the diagnosis of pulmonary embolism (PE)?
A 21-year-old woman 2 days after a cesarean delivery
55-year-old woman on estrogen replacement therapy who underwent a total hip replacement procedure 3 days ago
A 39-year-old man who smokes cigarettes occasionally and underwent an uncomplicated appendectomy 2 months ago
A 62-year-old man with pancreatic cancer.
A 45-year-old man with factor V Leiden deficiency
A 29-year-old man is brought to the ED by EMS for a syncopal episode that occurred during a basketball game. A friend states that the patient just dropped to the ground shortly after scoring a basket on a fast break. On examination, you note a prominent systolic ejection murmur along the left sternal border and at the apex. An ECG reveals left ventricular hypertrophy, left atrial enlargement, and septal Q waves. You suspect the diagnosis and ask the patient to perform the Valsalva maneuver while you auscultate his heart. Which of the following is most likely to occur to the intensity of the murmur with this maneuver?
Decrease
Increase
Remain unchanged
Disappear.
The intensity stays the same, but the heart skips a beat
A 72-year-old man presents with shortness of breath and increased home oxygen requirement. The patient has coronary artery disease, he has had two previous myocardial infarctions, and he has a history of chronic obstructive pulmonary disease requiring 2 L of continuous home oxygen. The patient has a 45-pack-year history of smoking. He is unable to walk more than a block and the swelling in his legs has worsened. The physician suggests measuring a brain natriuretic peptide (BNP) level to distinguish a cardiac from a pulmonary cause of his symptoms. Which of the following statements regarding BNP is true?
BNP acts to decrease venous capacitance and increase preload
BNP is decreased in the setting of left ventricular dysfunction
BNP is secreted by the cardiac atria
BNP is secreted in response to hypovolemia
BNP levels cannot differentiate systolic and diastolic dysfunction
A 77-year-old man with a history of hypertension, hypercholesterolemia, chronic obstructive pulmonary disease, and a 90-pack-year smoking history presents to the emergency department with lethargy and abdominal pain. His temperature is 36.9°C (98.5°F), blood pressure is 82/54 mm Hg, pulse is 125/min, and respiratory rate is 16/min. A pulsatile abdominal mass is palpable just superior to the umbilicus. There is diffuse abdominal tenderness, although rebound tenderness and guarding are absent. There is also slight skin discoloration noted in the left lower back. Which of the following is the most likely diagnosis?
Aortic dissection
Mesenteric ischemia
Perforated gastric ulcer
Ruptured abdominal aortic aneurysm
Stroke
A 52-year-old African-American man with a history of smoking and asthma presents to the emergency department complaining of shortness of breath. He has alcohol on his breath and admits to drinking 3–4 beers each night plus an occasional “mixed drink.” He denies drug use and states that he has been feeling well until recently, when he began to sleep with more pillows and to become out of breath when walking. His blood pressure is 143/89 mm Hg, respiratory rate is 21/min, pulse is 112/min, and he is afebrile. On physical examination he has a laterally displaced point of maximal impulse and an S3 gallop, as well as rales over his right lung base. X-ray of the chest shows cardiomegaly and a pleural effusion. Echocardiogram reveals an ejection fraction of 25%. Which of the following is the most likely diagnosis?
Asthma exacerbation
Delirium tremens
Dilated cardiomyopathy
Endocarditis
Hypothyroidism
A cardiologist is called to consult on the care of a 2-day-old girl delivered at 33 weeks’ gestation. The infant is lying supine in her isolette. She is acyanotic, but has a heart rate of 192/ min and a respiratory rate of 60/min. She has a nonradiating continuous machinery murmur at the left upper sternal border that remains the same with compression of the ipsilateral, then contralateral jugular veins. S1 and S2 are normal. Her peripheral pulses are bounding. Which of the following is the most likely diagnosis?
Aortic stenosis with aortic regurgitation
Patent ductus arteriosus
Systemic arteriovenous fistula
Venous hum
Ventricular septal defect
A 64-year-old white man with type 2 diabetes mellitus presents to the emergency department after “passing out.” While climbing the stairs, he felt dyspneic and lost consciousness as he reached the top. Before the event he experienced no palpitations or change in vision. When he awoke he felt alert and called for help immediately. He reports dyspnea on exertion for the past year. He has no history of chest pain, seizures, or recent illnesses. Medications include calcium and vitamin D supplements, glyburide, and synthroid. He is allergic to penicillin. Family history is noncontributory. He drinks wine socially and does not smoke or use illicit substances. His blood pressure is 136/92 mm Hg, heart rate is 88/min, respiratory rate is 14/min, and temperature is 36.5°C (97.7°F). Physical examination reveals a systolic crescendodecrescendo murmur best heard in the second right intercostal space with a soft S2. ECG shows nonspecific ST-segment changes and left ventricular hypertrophy with a normal heart rate and rhythm. Which of the following interventions will most likely reveal the cause of this syncopal event?
ECG
Echocardiography
Electroencephalography
Exercise stress test with echocardiogram
Sublingual nitroglycerin and serial cardiac enzymes
A 56-year-old woman with a history of chronic renal disease presents to the emergency department because of severe, sharp, retrosternal chest pain that radiates to her jaw. The pain worsens when the patient lies down, and she is most comfortable leaning forward and hugging her knees. She takes erythropoietin, furosemide, calcitriol, and sodium polystyrene sulfonate. She is scheduled for dialysis three times per week, but she admits to sometimes missing sessions. She stopped drinking and smoking 20 years ago, and she has no family history of heart or renal problems. Auscultation of the heart reveals a friction rub. Laboratory tests show: WBC count: 12,000/mm3 Hemoglobin: 10.0 g/dL Hematocrit: 30.0% Platelet count: 150,000/mm3 Na+: 141 mEq/L K+: 4.8 mEq/L Cl: 101 mEq/L HCO3 : 22 mEq/L Blood urea nitrogen: 63 mg/dL Creatinine: 3.2 mg/dL Glucose: 111 mg/dL The emergency medicine physician urges the patient to be more compliant with her dialysis, but the patient complains that she is too tired to go to dialysis all of the time and that it is ruining her life. Which of the following is the most likely complication if the patient’s condition remains untreated?
Cardiac tamponade
Decreased jugular venous pressure
Mitral regurgitation
Restrictive cardiomyopathy
Septic shock
A 70-year-old man comes to his primary care physician for his annual check-up. He has a history of hypertension, hyperlipidemia, and coronary artery disease, and had coronary artery bypass grafting 6 years ago. On examination the physician notes a right carotid bruit. Which of the following is the most appropriate next step?
Carotid duplex ultrasound
Carotid endarterectomy
ECG
Referral to a neurologist
Transthoracic echocardiography
A 32-year-old man is brought to the emergency department by paramedics after being found wandering downtown, apparently delirious and agitated. During transport to the hospital the patient becomes diaphoretic and tremulous and has a blood pressure to 163/100 mm Hg, pulse of 102/min, and temperature of 39°C (102.2°F). On examination the patient has dilated pupils and ulcerations of his nasal septum mucosa with the residue of a white powder along the nasal alae in addition to his tachycardia, hypertension, hyperthermia, and agitation. Which of the following is the reason why nonselective β-blockers should be avoided in this patient?
Increased risk of late vasospasm
Risk of acutely worsening hypertension through vasoconstriction
Risk of causing acute hypotension
Risk of causing dyspnea
Risk of ventricular arrhythmia
A 59-year-old man presents to his internist for a routine visit. He has no complaints, and review of symptoms is negative. His past medical history is significant for poorly controlled hypertension for 15 years due to noncompliance with antihypertensive medications. He takes hydrochlorothiazide 25 mg orally four times a day. His family history is significant for hypertension, heart failure, and stroke. He has a 30-pack-year smoking history and drinks two beers a day. On physical examination he is a mildly obese man in no acute distress. He has a normal jugular venous pressure. He has a prominent point of maximum impulse, regular rate and rhythm, normal S1, loud S2, and audible S4 with no murmurs. His lungs are clear to auscultation bilaterally, and he has no signs of edema. His abdominal and neurologic examinations are within normal limits. His temperature is 37.0°C (98.6°F), pulse is 81/min, respiratory rate is 12/min, blood pressure is 165/96 mm Hg, and oxygen saturation is 100% on room air. His ECG shows normal sinus rhythm with large amplitude of the S wave in V1 and V2 and of the R wave in V5 and V6. Also present are diffuse ST segment/T wave changes, widened bifid P waves, and prolonged QRS waveforms. Which of the following is the most likely diagnosis?
Acute myocardial infarction
Cerebrovascular accident
Dilated cardiomyopathy
Left ventricular hypertrophy
Pericarditis
A 60-year-old woman is transferred to a physician from an outside hospital following a motor vehicle collision. Her medical history is notable for Osler-Weber-Rendu syndrome. She is otherwise healthy. Which of the following triads is most likely to characterize her medical history prior to the collision?
Hypertension, bradycardia, and irregular respirations
Jaundice, fever, and right upper quadrant pain
Symptoms of hypoglycemia, low blood sugar, and relief with increase in blood sugar
Telangiectasia, recurrent epistaxis, and positive family history
Venous stasis, hypercoagulability, and endothelial damage
A 65-year-old man presents to the emergency department following the acute onset of palpitations. His wife states that he was eating dinner when he noticed the palpitations, lightheadedness, and shortness of breath. The patient has a history of treated hypertension, but no other medical history. The patient is not able to relate any meaningful history. Blood pressure is 80/40 mm Hg, heart rate is 126/ min, respiratory rate is 20/min, and oxygen saturation is 99% on room air; he is afebrile. His heart rate is irregularly irregular with no murmurs, clicks, or rubs. Respiratory examination is unremarkable. X-ray of the chest shows no acute disease. ECG shows no discernible P waves and an irregularly spaced QRS response. Which of the following is the best first step in management?
Administration of adenosine
Cardiac catheterization and stent placement
Cardioversion to sinus rhythm
Carotid massage
Placement of dual lead pacemaker
A 62-year-old man with coronary artery disease (CAD) presents with presyncope. His physical examination is normal except for bradycardia (pulse 56 beats/min) and an irregular pulse. The electrocardiogram (ECG) shows Wenckebach’s type atrioventricular (AV) block. Which of the following are you most likely to see on the ECG?
Progressive PR shortening
Progressive lengthening of the PR interval
Tachycardia
Dropped beat after PR lengthening
Fixed 2:1 block
A 72-year-old woman had a pacemaker inserted 4 years ago for symptomatic bradycardia because of AV nodal disease. She is clinically feeling well and her ECG shows normal sinus rhythm at a rate of 68/min but no pacemaker spikes. Her pacemaker only functions when the ventricular rate falls below a preset interval. Which of the following best describes her pacemaker function?
Asynchronous
Atrial synchronous
Ventricular synchronous
Ventricular inhibited
Atrial sequential
A 47-year-old man is found to have edema, ascites, and hepatosplenomegaly. The examination of his neck veins reveals elevated venous pressure with a deep y descent. Heart size on x-ray is normal. Which of the following etiologies is not a possible explanation for this syndrome?
Rheumatic fever
TB
Unknown cause
Previous acute pericarditis
Neoplastic involvement of the pericardium
A 65-year-old man develops palpitations and dizziness. His blood pressure is 80/50 mm Hg and his pulse is regular at 150/min. His ECG shows a “saw-toothed” pattern of P waves. Which of the following procedures is most appropriate in converting him back to sinus rhythm?
Carotid sinus pressure
Gagging procedures
Valsalva maneuver
Eyeball compression
Electrical cardioversion
A 31-year-old man who works for a moving company presents to the ED because he thinks he was having a heart attack. He does not smoke, and jogs 3 days a week. His father died of a heart attack in his sixties. He describes a gradual onset of chest pain that is worse with activity and resolves when he is at rest. His HR is 68 beats per minute, BP is 120/70 mm Hg, and RR is 14 breaths per minute. On examination, his lungs are clear and there is no cardiac murmur. You palpate tenderness over the left sternal border at the third and fourth ribs. An ECG reveals sinus rhythm at a rate of 65. A chest radiograph shows no infiltrates or pneumothorax. Which of the following is the most appropriate next step in management?
Administer aspirin and send for a troponin
Administer aspirin, clopidogrel, and heparin, and admit for acute coronary syndrome (ACS).
Administer ibuprofen and reassure the patient that he is not having a heart att
Inject corticosteroid into the costochondral joint to reduce inflammation
Observe the patient for 6 hours
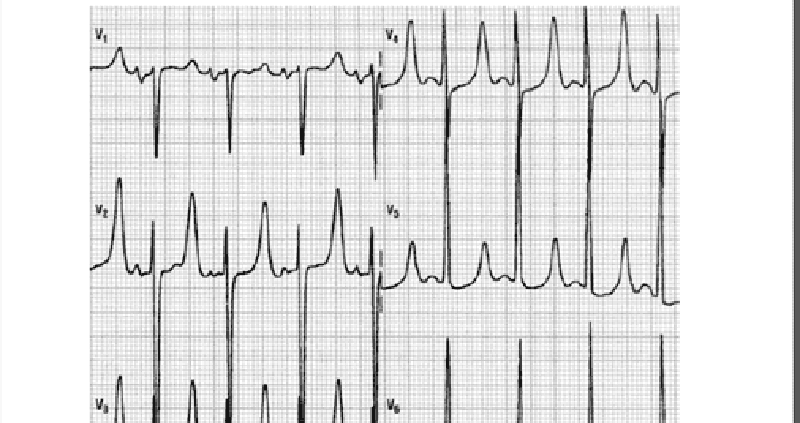
A 55-year-old man presents to the ED with worsening weakness, muscle cramps, and paresthesias. His past medical history is significant for hypertension and diabetes. He smokes one pack of cigarettes per day. On examination, the patient is alert and oriented and diffusely weak. An ECG is seen below. Which of the following is the most important next step in management?
Administer calcium gluconate
Administer insulin and dextrose
Administer aspirin and call the catheterization laboratory
Order an emergent head CT scan and get a neurology consult
Collect a sample of his urine to test for ketones
A 59-year-old man presents to the ED with left-sided chest pain and shortness of breath that began 2 hours prior to arrival. He states the pain is pressure-like and radiates down his left arm. He is diaphoretic. His BP is 160/80 mm Hg, HR 86 beats per minute, and RR 15 breaths per minute. ECG reveals 2-mm ST-segment elevation in leads I, aVL, and V3 to V6. Which of the following is an absolute contraindication to receiving thrombolytic therapy?
Systolic BP (SBP) greater than 180 mm Hg
Patient on Coumadin and aspirin
Total hip replacement 3 months ago
Peptic ulcer disease
Previous hemorrhagic stroke
A 27-year-old man who is otherwise healthy presents to the ED with a laceration on his thumb that he sustained while cutting a bagel. You irrigate and repair the wound and are about to discharge the patient when he asks you if he can receive an ECG. It is not busy in the ED so you perform the ECG, as seen below. Which of the following is the most appropriate next step in management?
Admit the patient for placement of a pacemaker
Admit the patient for a 24-hour observation period
Administer aspirin and send cardiac biomarkers
Repeat the ECG because of incorrect lead placement
Discharge the patient home
A 55-year-old man presents to the ED at 2:00 AM with left-sided chest pain that radiates down his left arm. He takes a β-blocker for hypertension, a proton pump inhibitor for gastroesophageal reflux disease, and an antilipid agent for high cholesterol. He also took sildenafil the previous night for erectile dysfunction. His BP is 130/70 mm Hg and HR is 77 beats per minute. Which of the following medications is contraindicated in this patient?
Aspirin
Unfractionated heparin
Nitroglycerin
Metoprolol
Morphine sulphate
62-year-old man has progressive symptoms of dyspnea, and more recently noticed difficulty lying supine. Examination shows an elevated JVP at 8 cm, with a third heart sound, pedal edema, and bibasilar crackles on auscultation. Which one of the following may be implicated in fluid retention for this condition?
Decreased renin
Increased aldosterone
Increased estrogen
Increased growth hormone
Decreased vasopressin
Three months after an anterior MI, a 73-yearold man has a follow-up ECG. He is clinically feeling well with no further angina symptoms. His ECG shows Q waves in the anterior leads with persistant ST-segment elevation. The current ECG is most compatible with which of the following diagnosis?
Ventricular aneurysm
Hibernating myocardium
Acute infarction
Silent infarction
Early repolarization
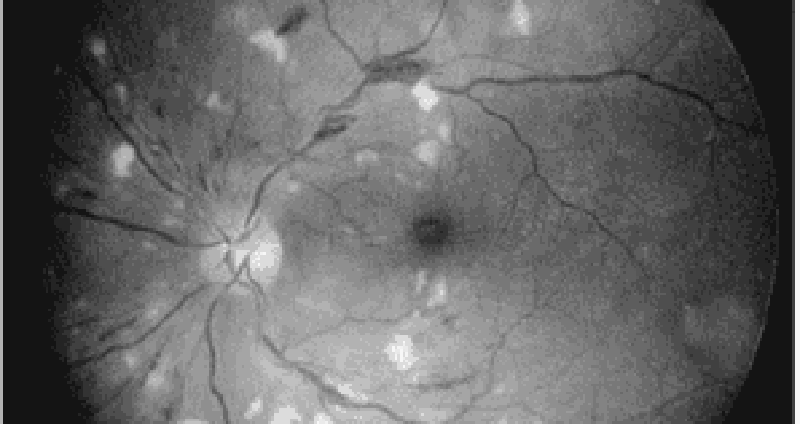
A 47-year-old woman develops accelerated hypertension (blood pressure 210/105 mm Hg) but no clinical symptoms except frequent headaches. Which of the following findings are most likely on examination of the fundii?
Retinitis obliterans
Cotton wool spots
Retinal detachment
Optic atrophy
Foveal blindness

A 32-year-old man presents for rountine evaluation. He has no symptoms but has noticed some new “nodules” on his legs. Physical examination reveals lumps on his Achillis tendon, yellow lesions around his eyes, and pigmentation of his iris. Which of the following is the most likely diagnosis?
Familial hyperlipidemia
Diabetes
Myxedema
Chronic renal disease
An inherited defect of glycogen utilization
A 36-year-old woman presents to the ED with sudden onset of left-sided chest pain and mild shortness of breath that began the night before. She was able to fall asleep without difficulty but woke up in the morning with persistent pain that is worsened upon taking a deep breath. She walked up the stairs at home and became very short of breath, which made her come to the ED. Two weeks ago, she took a 7-hour flight from Europe and since then has left-sided calf pain and swelling. What is the most common ECG finding for this patient’s presentation?
S1Q3T3 pattern
Atrial fibrillation
Right-axis deviation
Right-atrial enlargement
Tachycardia or nonspecific ST-T–wave changes
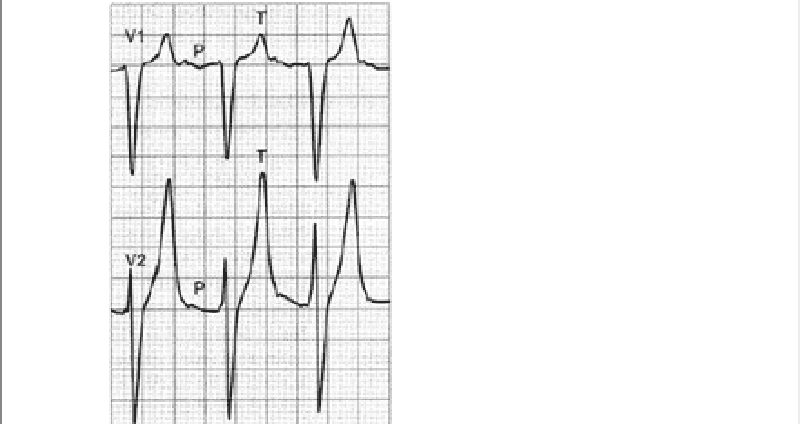
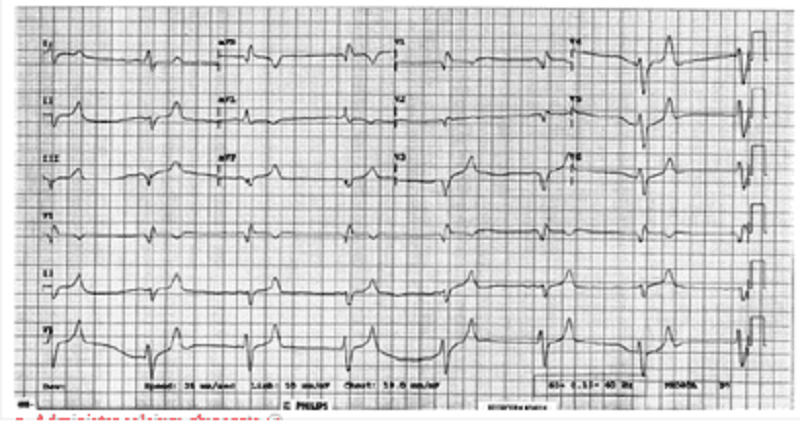
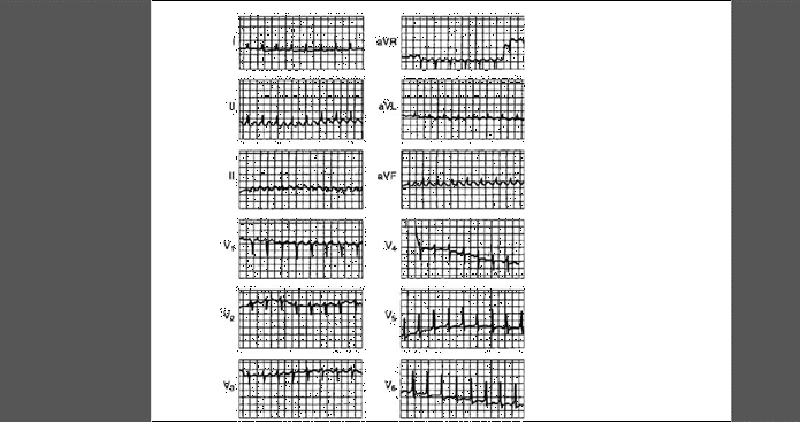
A 54-year-old woman presents to the ED because of a change in behavior at home. For the past 3 years, she has end-stage renal disease requiring dialysis. Her daughter states that the patient has been increasingly tired and occasionally confused for the past 3 days and has not been eating her usual diet. On examination, the patient is alert and oriented to person only. The remainder of her examination is normal. An initial 12-lead ECG is performed as seen on the following page. Which of the following electrolyte abnormalities best explains these findings?
Hypokalemia
Hyperkalemia
Hypocalcemia
Hypercalcemia
Hyponatremia
A 42-year-old man found vomiting in the street is brought to the ED by emergency medical services (EMS). He has a known history of alcohol abuse with multiple presentations for intoxication. Today, the patient complains of acute onset, persistent chest pain associated with dysphagia, and pain upon flexing his neck. His BP is 115/70 mm Hg, HR is 101 beats per minute, RR is 18 breaths per minute, and oxygen saturation is 97% on room air. As you listen to his heart, you hear a crunching sound. His abdomen is soft with mild epigastric tenderness. The ECG is sinus tachycardia without ST-T–wave abnormalities. On chest radiograph, you note lateral displacement of the left mediastinal pleura. What is the most likely diagnosis?
Aspiration pneumonia
Acute pancreatitis
Pericarditis
Esophageal perforation
Aortic dissection
A 65-year-old man with a history of chronic hypertension presents to the ED with sudden-onset tearing chest pain that radiates to his jaw. His BP is 205/110 mm Hg, HR is 90 beats per minute, RR is 20 breaths per minute, and oxygen saturation is 97% on room air. He appears apprehensive. On cardiac examination you hear a diastolic murmur at the right sternal border. A chest x-ray reveals a widened mediastinum. Which of the following is the preferred study of choice to diagnose this patient’s condition?
Electrocardiogram (ECG)
Transthoracic echocardiography (TTE)
Transesophageal echocardiography (TEE)
Computed tomography (CT) scan
Magnetic resonance imaging (MRI)
36-year-old man is seen because of palpitations. He admits to precordial discomfort, weakness, and anxiety. His pulse is 150/min, and his blood pressure is 124/70 mm Hg. Heart sounds are normal. Carotid sinus pressure gradually changes the rate to 75/min, but when released, the pulse rate returns to 150/min. Which of the following is the most likely diagnosis?
Atrial flutter with 2:1 block
Paroxysmal atrial tachycardia with 2:1 block
Sinus arrhythmia
Atrial fibrillation
Nodal tachycardia
A 25-year-old man complains of left precordial chest pain that radiates to the left shoulder but not down the left arm. The pain is accentuated by inspiration and relieved by sitting up. The pain is accompanied by fever and chills. His blood pressure is 105/75 mm Hg, pulse 110/min and regular, and temperature 37.5°C. Aside from the tachycardia, there are no abnormal physical findings in the heart or lungs. The ECG shows STsegment elevation in all leads except aVR and VI. On the third hospital day, the patient’s blood pressure falls, JVP rises, and he goes into CHF. Which of the following is the most likely diagnosis?
A second pulmonary embolus
Extension of a myocardial infarct
Cardiac tamponade
Secondary bacterial infection
Rupture of a chordae tendineae
A 80-year-old man with Type II diabetes and hypertension presents with increasing dyspnea. He appears short of breath, blood pressure is 170/95 mm Hg, pulse 100/min and regular. The JVP is at 7 cm; there is a loud second heart sound and a systolic ejection murmur at the right sternal border, which does not radiate. The lungs have bibasilar crakles up to the scapula. The CXR has bilateral infiltrates and vascular redistribution. His echocardiogram reports aortic sclerosis, concentric left ventricular hypertrophy (LVH), and normal ejection fraction. Which of the following is the most likely mechanism for this condition?
Valvular heart disease
Diastolic dysfunction
Systolic dysfunction
Hibernating myocardium
Hypertrophic obstructive cardiomyopathy (HOCM)
A 68-year-woman with hypertension and dyslipidemia presents with 30 minutes of retrosternal chest pain radiating to her neck. She is diaphoretic and in moderate distress. The ECG shows ST-segment elevation in the inferior leads. Which of the following mechanisms is the most likely cause of her condition?
Coronary plaque rupture
Aortic inflammation
Pericardial inflammation
Vasculitis
Myocarditis
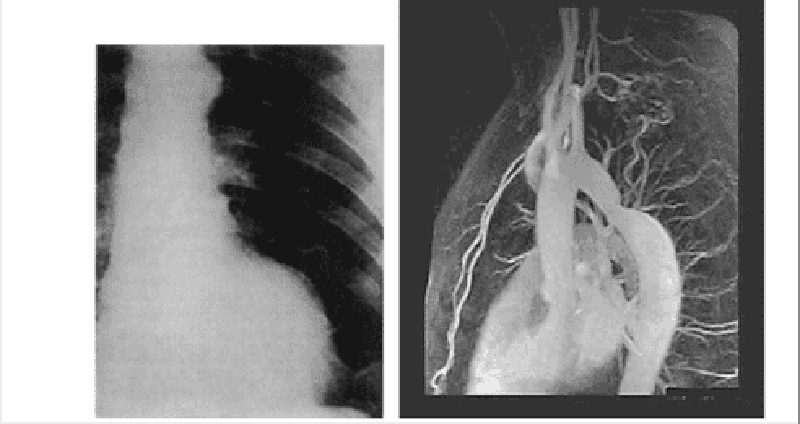
Image below is an x-ray of an asymptomatic 64- year-old male executive coming in for his regular annual medical checkup. He had an anterior Q wave MI 4 years ago. What is your diagnosis?
Calcific pericarditis
Left ventricular aneurysm
Hydatid cyst
Pleuropericarditis
Normal
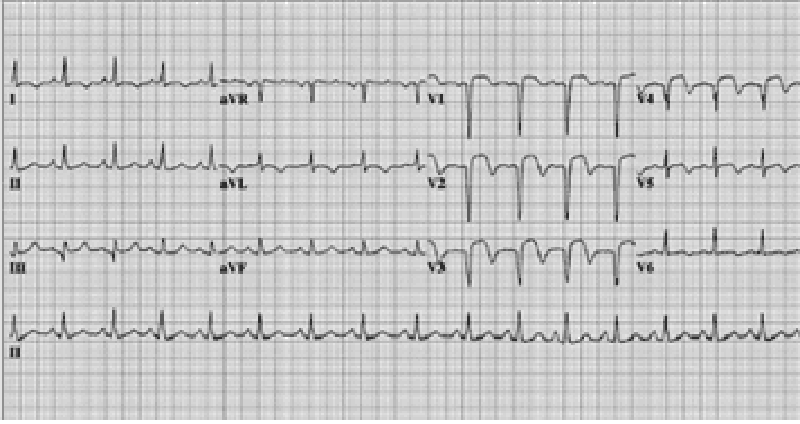
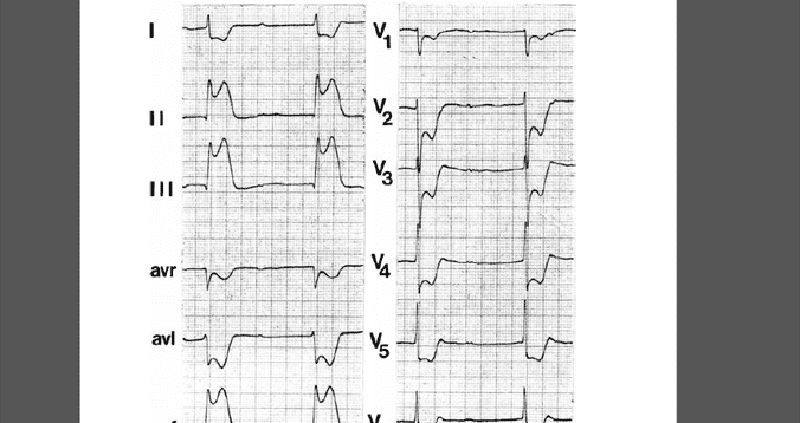
A 70-year-old man has dyspnea, orthopnea, and paroxysmal nocturnal dyspnea. He has generalized cardiomegaly and pulmonary and systemic venous hypertension. The ECG is shown in Fig.What is the cardiac rhythm?
Ectopic atrial tachycardia
Atrial flutter with 2:1 AV conduction
Sinus tachycardia
Supraventricular tachycardia
Atrial fibrillation with rapid ventricular response
A 72-year-old man with coronary artery disease and hypertension is hospitalized after suffering a myocardial infarction 5 days ago. He suddenly complains of severe chest pain. His blood pressure is 90/60 mm Hg and heart rate is 65/min. Auscultation reveals no murmurs or rubs. An ECG reveals sinus rhythm with an acute ST-segment elevation in the anteroseptal area. Urgent bedside echocardiography showed anteroseptal, lateral, and apical akinesis, mild left ventricular systolic dysfunction, and severe pericardial effusion. Within 20 minutes he is unconscious with undetectable pulses and blood pressure. What is the most likely cause of the patient’s sudden decompensation?
Free wall rupture
Left ventricular thrombus
Mitral regurgitation
Pericarditis
Ventricular septal rupture
A 56-year-old woman was recently started on medication for high blood pressure. At her next office visit her hypertension is under good control, but she now complains of “feeling strange” since she started the medication. On further questioning, she reports feeling chest tightness several times over the past 2 weeks, and has also noticed pain in her elbows and knees. Her blood pressure is 124/78 mm Hg (146/82 mm Hg on last visit), heart rate is 102/min, and respiratory rate is 14/min. Her examination is notable for several erythematous plaques on the malar distribution of the face, arms, and upper torso. What medication was she most likely started on during her last visit?
Captopril
Furosemide
Hydralazine
Metoprolol
Verapamil
A 62-year-old woman presents to the ED with general weakness, shortness of breath, and substernal chest pain that radiates to her left shoulder. Her BP is 155/80 mm Hg, HR is 92 beats per minute, and RR is 16 breaths per minute. You suspect that she is having an acute MI. Which of the following therapeutic agents has been shown to independently reduce mortality in the setting of an acute MI?
Nitroglycerin
Aspirin
Unfractionated heparin
Lidocaine
Diltiazem
A 57-year-old man complains of chest palpitations and light-headedness for the past hour. Five years ago he underwent a cardiac catheterization with coronary artery stent placement. He smokes half a pack of cigarettes daily and drinks a glass of wine at dinner. His HR is 140 beats per minute, BP is 115/70 mm Hg, and oxygen saturation is 99% on room air. An ECG reveals a wide complex tachycardia at a rate of 140 that is regular in rhythm. An ECG from 6 months ago shows a sinus rhythm at a rate of 80. Which of the following is the most appropriate medication to treat this dysrhythmia?
A. Digoxin
Diltiazem
Amiodarone
Adenosine
Bretylium
As you are examining the patient described in the previous question, he starts to complain of chest discomfort and shortness of breath and has another syncopal episode. His ECG is shown below. Which of the following is the most appropriate next step in management?
Call cardiology consult
Cardiovert the patient
Administer metoprolol
Administer amiodarone
Apply transcutaneous pacemaker
A 19-year-old woman was attacked while coming home from a party and is brought to the emergency department. She recalls being punched in the side of the head and stabbed in the left flank. Her speech is slow and she complains of a bad headache. Her pulse is 110/min, blood pressure is 90/50 mm Hg, and respiratory rate is 25/min. On examination she has a stab wound at the left costal margin in the midaxillary line. Two large-bore intravenous lines are inserted, and after infusion of 2 L of lactated Ringer’s solution her blood pressure rises to 95/55 mm Hg. What is the most appropriate next step in management?
Abdominal ultrasound
Diagnostic peritoneal lavage
Exploratory laparotomy
Noncontrast CT of the head
Peritoneal laparoscopy
34-year-old woman presents to your office complaining of several months of chest pain. She says that the pain is left-sided, does not change with deep inspiration, and typically lasts several hours. The pain has no relation to physical activity, but worsens with emotional stress. The patient has no significant family history, and does not use tobacco, alcohol or drugs. She takes no medications and has no drug allergies. On exam, her blood pressure is 110/70 mmHg and her heart rate is 78/min. ECG is normal. Which of the following is the best next step in her management?
Reassurance
Stress ECG testing
Transthoracic echocardiography
Lower extremity venous ultrasonography
Chest X-ray
60-year-old male patient is receiving aspirin, an angiotensin-converting enzyme inhibitor, nitrates, and a beta-blocker for chronic stable angina. He presents to the ER with an episode of more severe and long-lasting angina chest pain each day over the past 3 days. His ECG and cardiac enzymes are normal. Which of the following is the best course of action?
Admit the patient and add intravenous digoxin.
Admit the patient and begin low-molecular-weight heparin
Admit the patient for thrombolytic therapy
Admit the patient for observation with no change in medication.
Increase the doses of current medications and follow closely as an outpatient
While palpating the pulse of a patient, you note that the pulse wave has two peaks. You auscultate the heart and are certain that there is only one heartbeat for each two pulse waves. Which of the following best describes this finding?
Pulsus alternans
Dicrotic pulse
Pulsus parvus et tardus
Pulsus bigeminus
Pulsus bisferiens
A 42-year-old female with acute pericarditis develops jugular venous distention and hypotension. The ECG shows electrical alternans. Which of the following is the most likely additional physical finding?
Basilar rales halfway up both posterior lung fields
S3 gallop
Pulsus paradoxus
Strong apical beat
Epigastric tenderness
Yesterday you admitted a 55-year-old white male to the hospital for an episode of chest pain, and you are seeking to rule out MI plus assess for any underlying coronary artery disease. The patient tends to be anxious about his health. On admission, his lungs were clear, but his heart revealed a grade 1/6 early systolic murmur at the upper left sternal border without radiation. Blood pressure readings have consistently been in the 140/90 to 150/100 range. Cardiac enzymes are normal. A resting ECG shows only left ventricular hypertrophy with secondary ST-T changes (“LVH with strain”). Why would a treadmill ECG stress test not be an appropriate test in this patient?
Anticipated difficulty with the patient’s anxiety (ie, he might falsely claim chest pain during the test)
Increased risk associated with high blood pressure readings
Concern about the heart murmur, a relative contraindication to stress testing
The presence of LVH with ST-T changes on baseline ECG
Concern that this represents the onset of unstable angina with unacceptable risk of MI with stress testing
A 67-year-old male presents to your office after community ultrasound screening revealed an aortic aneurysm measuring 3.0 x 3.5 cm. Physical examination confirms a palpable, pulsatile, nontender abdominal mass just above the umbilicus. The patient’s medical conditions include hypertension, hyperlipidemia, and tobacco use. What is the best recommendation for the patient to consider?
Watchful waiting is the best course until the first onset of abdominal pain.
Surgery is indicated except for the excess operative risk represented by the patient’s risk factors.
Serial follow-up with ultrasound, CT, or MRI is indicated, with the major determinant for surgery being aneurysmal size greater than 5 to 6 cm
Serial follow-up with ultrasound, CT, or MRI is indicated, with the major determinant for surgery being involvement of a renal artery
Unlike stents in coronary artery disease, endovascular stent grafts have proven unsuccessful in the management of AAAs.
A 67-year-old male presents to your clinic to establish primary care; he is asymptomatic. He has a history of hypertension for which he takes hydrochlorothiazide. His father had a myocardial infarction at age 62. The patient smoked until 5 years ago, but has been abstinent from tobacco since then. His blood pressure in the office today is 132/78. Aside from being overweight, the remainder of the physical examination is unremarkable. Which of the following preventive health interventions would be most appropriately offered to him today?
Carotid ultrasound to evaluate for carotid artery stenosis
Abdominal ultrasound to evaluate for aortic aneurysm
Lipoprotein(a) assay to evaluate coronary heart disease risk
Exercise (treadmill) stress testing to evaluate for coronary artery disease
Homocysteine level to evaluate coronary heart disease risk
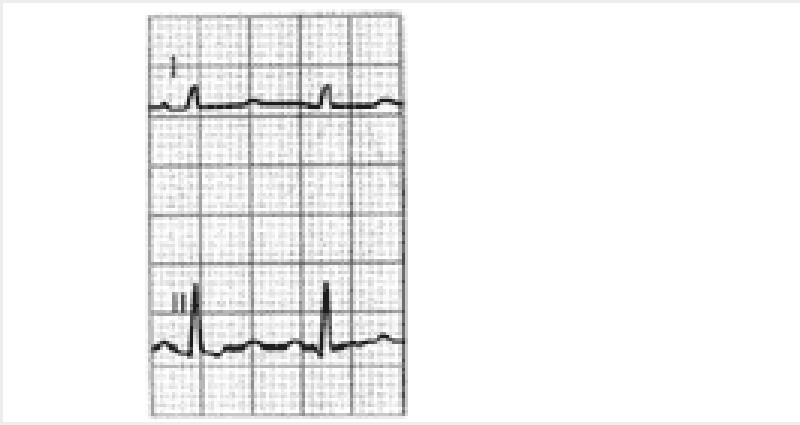
You are called by a surgical colleague to evaluate a 54-year-old woman with ECG abnormalities one day after a subtotal thyroidectomy for a toxic multinodular goiter. Her only medication is fentanyl for postoperative pain control. The patient denies any history of syncope, and has no family history of sudden cardiac death. Physical examination is unremarkable except for a clean postoperative incision at the base of the neck. Her ECG
Administration of intravenous magnesium sulfate
Measurement of serum ionized calcium
Stat noncontrast CT scan of the brain
Formal auditory testing
Reassure the patient that her ECG is normal for a woman her age
A 36-year-old man presents to the clinic with complaints of a genital sore. The patient is a sexually active heterosexual involved with three partners and practices unprotected intercourse. Four days ago he noted a painless sore on his penis. He is afebrile, with a heart rate of 80/min and blood pressure of 120/77 mm Hg. Physical examination reveals a solitary ulcerated lesion located on the lateral aspect of his penis. The lesion is nontender and associated with bilateral inguinal lymphadenopathy. Physical examination is otherwise normal. If left untreated, this man is at increased risk for which of the following?
Ascending aortic aneurysm
Coronary artery aneurysm
Endocarditis
Mitral valve stenosis
Rupture of ventricular free wall
An 81-year-old man is hospitalized for acute onset of shortness of breath and lower extremity edema. Although he lives by himself, it is very difficult for him to move around his apartment without experiencing fatigue. He has not seen his physician in years but was told in the past that he had high blood pressure. On physical examination his jugular venous pulse is palpated 9 cm above his sternal notch, inspiratory crackles are heard at his lung bases, and there is 3+ lower extremity edema. Which of the following will confirm the most likely diagnosis?
Cardiac angiography
Echocardiography
Electrocardiogram
Endomyocardial biopsy
X-ray of the chest
A 42-year-old man presents to the clinic for routine evaluation. His medical history is signifiedcant for gallstones. The patient denies smoking and drinks alcohol occasionally. His mother had a heart attack at the age of 63 years. His blood pressure is 134/77 mm Hg. The patient is overweight with well-healed laparoscopic cholecystectomy scars. Fasting laboratory tests show: Aspartate aminotransferase: 37 U/L Alanine aminotransferase: 28 U/L Alkaline phosphatase: 88 U/L Total cholesterol: 268 mg/dL LDL cholesterol: 183 mg/dL HDL cholesterol: 46 mg/dL Triglycerides: 166 mg/dL What is the most appropriate next step in management?
A trial of lifestyle modification alone (diet, exercise, and weight loss)
A trial of lifestyle modification combined with statin and niacin therapy
A trial of lifestyle modification combined with statin therapy
Niacin therapy
Statin therapy
A 62-year-old man with a prosthetic aortic valve develops fevers and malaise. His valve was replaced 5 years ago because of aortic stenosis from a bicuspid valve. He has a systolic ejection murmur but no other abnormalities on examination. Blood cultures are most likely to grow which of the following?
Fungi
Bartonella
Diptheroids
Staphylococcus epidermidis
Streptococcus bovis
A 58-year-old man with no prior cardiac history presents with retrosternal chest pain starting at rest and lasting 30 minutes. The pain radiates to the left arm and is associated with diaphoresis and dyspnea. His blood pressure is 150/90 mm Hg, pulse 100/min, the heart sounds are normal, and the lungs are clear to auscultation. Which of the following is the next most appropriate investigation?
CT scan chest
CXR
Cardiac troponin
ECG
Myocardial perfusion imaging
The laboratory results shown in Table 1–1 are obtained from the investigation of a 37-year-old African-American woman who has a blood pressure at rest of 140/100 mm Hg. Which of the following is the most likely diagnosis? TABLE 1–1. LABORATORY INVESTIGATIONS Urinalysis pH 5.2 Albumin Negative to trace Serum Na 140 mEq/L K 3.5 mEq/L Cl 100 mEq/L CO2 25 mEq/L Creatinine 1.0 mg/100 mL Fasting sugar 90 mg/100 mL Calcium 9.0 mg/100 mL Uric acid 5.0 mg/100 mL (A)
Cushing’s syndrome
Primary aldosteronism
Essential hypertension
Pyelonephritis
Bilateral renal artery stenosis
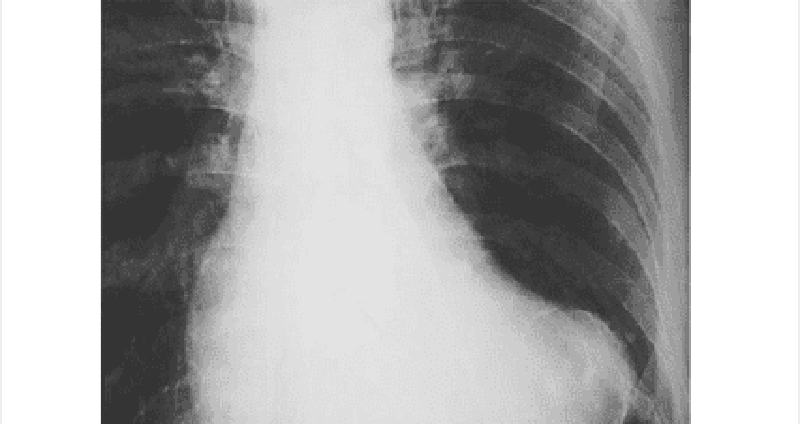
Image below is the x-ray and MR of an 8-year-old boy who had easy fatigability and a soft, continuous murmur in the upper back. ECG revealed minimal LVH. What is your diagnosis?
Aortic stenosis
Patent ductus arteriosus
Coarctation of the aorta
Pulmonary valvular stenosis
Peripheral pulmonary stenosis
A 60-year-old man with a history of congestive heart failure presents to his physician. He has a 5-year history of excessive daytime sleepiness and snoring. He also admits to three drinks of alcohol per day. His temperature is 36.6°C (98.0°F), pulse is 85/min, blood pressure is 138/82 mm Hg, respiratory rate is 14/min, and oxygen saturation is 99% on room air. His body mass index is 31 kg/m2. Physical examination is significant for macroglossia and a short neck. Polysomnography is performed and is significant for multiple nocturnal episodes of airflow cessation at the nose and mouth, despite evidence of continuing respiratory effort. Which of the following is the most effective management for this patient?
Avoidance of alcohol
Avoidance of supine posture
Nasal continuous positive airway pressure
Uvulopalatopharyngoplasty
Weight reduction
During a screening physical examination for participating in high school sports, a 14-yearold girl is found to have a late apical systolic murmur preceded by a click. The rest of the examination is unremarkable. Echocardiography shows superior displacement of the mitral leaflets of >2 mm during systole into the left atrium, with a thickness of at least 8 mm. In addition, she states that her father also has some type of heart “murmur,” but she knows nothing else about it. Which of the following is the most appropriate management at this time?
Digoxin
Instruct the patient to avoid all forms of strenuous activity
Metoprolol
Mitral valve replacement
Prophylactic antibiotics for dental procedures
A 20-year-old woman arrives at the emergency department actively seizing with QRS prolongation on ECG per paramedics. The patient’s roommate called emergency medical services after the patient collapsed, was not responsive to questioning, and began having clonic jerks bilaterally in her upper extremities. The patient’s roommate denies any knowledge of the patient consuming alcohol or illicit drugs. She does not believe the patient had any plan of harming herself, but does acknowledge that the patient has seemed “down” lately and was recently prescribed medication for generalized anhedonia. Which of the following is the most appropriate first-line treatment?
Activated charcoal
Diazepam
Flumazenil
Physostigmine
Sodium bicarbonate and diazepam
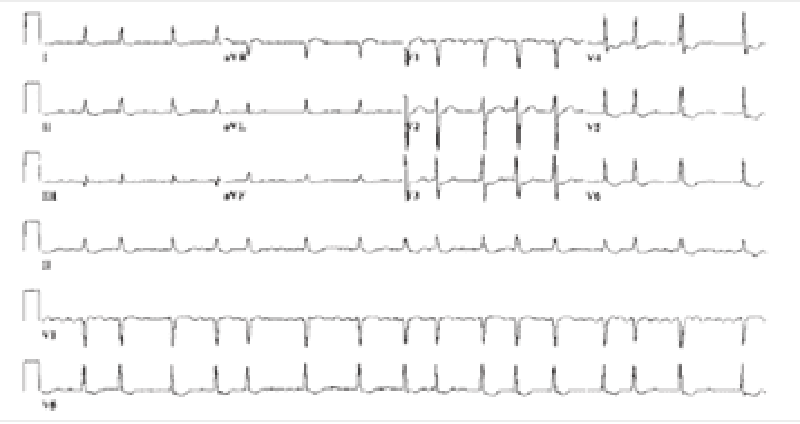
78-year-old woman presents to a nursing home physician complaining of palpitations over the past several months. Her episodes are not associated with any chest pain, dizziness, or loss of consciousness. The patient reports that she spent several weeks in the hospital as a child with rheumatic fever. ECG is shown in the image. Which of the following is the most likely diagnosis?
Atrial fibrillation
Atrial flutter
Multifocal atrial tachycardia
Paroxysmal atrial tachycardia
Paroxysmal supraventricular tachycardia
A 67-year-old woman is brought to the ED by paramedics complaining of dyspnea, fatigue, and palpitations. Her BP is 80/50 mm Hg, HR is 139 beats per minute, and RR is 20 breaths per minute. Her skin is cool and she is diaphoretic. Her lung examination reveals bilateral crackles and she is beginning to have chest pain. Her ECG shows a narrow complex irregular rhythm with a rate in the 140s. Which of the following is the most appropriate immediate treatment for this patient?
Diltiazem
Metoprolol
Digoxin
Coumadin
Synchronized cardioversion
A 61-year-old woman with a history of congestive heart failure (CHF) is at a family picnic when she starts complaining of shortness of breath. Her daughter brings her to the ED where she is found to have an oxygen saturation of 85% on room air with rales halfway up both of her lung fields. Her BP is 185/90 mm Hg and pulse rate is 101 beats per minute. On examination, her jugular venous pressure (JVP) is 6 cm above the sternal angle. There is lower extremity pitting edema. Which of the following is the most appropriate first-line medication to lower cardiac preload?
Metoprolol
Morphine sulfate
Nitroprusside
Nitroglycerin
Oxygen
A 27-year-old man complains of chest palpitations and lightheadedness for the past hour. He has no past medical history and is not taking any medications. He drinks a beer occasionally on the weekend and does not smoke cigarettes. His HR is 180 beats per minute, BP is 110/65 mm Hg, and oxygen saturation is 99% on room air. An ECG reveals an HR of 180 beats per minute with a QRS complex of 90 milliseconds with a regular rhythm. There are no discernable P waves. Which of the following is the most appropriate medication to treat this dysrhythmia?
Digoxin
Lidocaine
Amiodarone
Adenosine
Bretylium
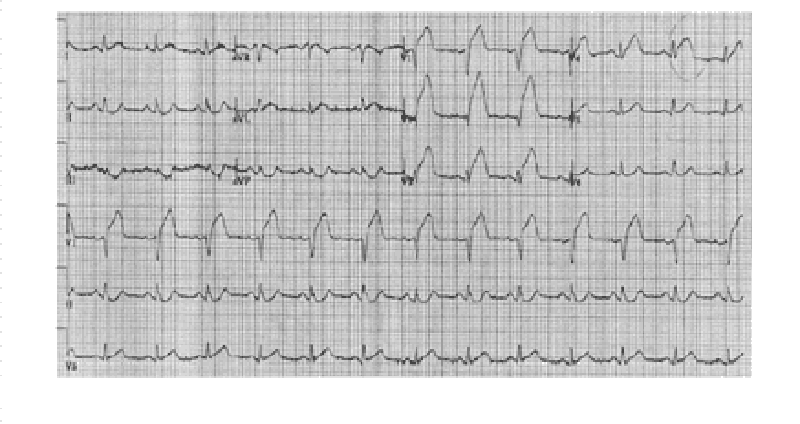
A 59-year-old man presents to the ED with left-sided chest pain and shortness of breath that began 1 hour ago. Initial vital signs are BP 85/45 mm Hg, HR 105 beats per minute, RR 20 breaths per minute, and oxygen saturation 94% on room air. An ECG is seen below. Which of the following is the most appropriate definitive treatment?
Administer metoprolol or diltiazem
Electrical cardioversion
Administer calcium gluconate
Thrombolytic therapy
Percutaneous angioplasty
A 28-year-old man with a history of intravenous drug abuse presents to the emergency department with a 2-day history of fever, chills, and shortness of breath. On physical examination the patient has a new heart murmur, small retinal hemorrhages, and subungual petechiae. Which of the following is the most likely causative organism?
Group A Streptococcus
Mycobacterium tuberculosis
Staphylococcus aureus
Streptococcus viridans
Staphylococcus epidermidis
A boy is delivered at 37 weeks’ gestation via spontaneous vaginal delivery. He is the product of a normal pregnancy and was delivered without complications. Prenatally the mother was blood type B and was rubella immune and negative for Rh antibody, group B streptococci, rapid plasma reagin, hepatitis B surface antigen, gonorrhea, and chlamydia. The patient appears cyanotic. He is breathing at a rate of 60/min and his heart rate is 130/min. He has a normal S1 and S2. There is a harsh holosystolic murmur that is loudest at the left lower sternal border. His examination reveals palpable nonbounding peripheral pulses bilaterally. Which of the following is the most likely diagnosis?
Coarctation of the aorta
Dextraposed transposition of the great arteries
Patent ductus arteriosus
Tetralogy of Fallot
Truncus arteriosus
32-year-old man is stabbed in the left chest and presents to the emergency department in distress. His pulse is 130/min, blood pressure is 70/50 mm Hg, and respiratory rate is 39/min. The stab wound is in the left fifth intercostal space in the midaxillary line. On examination his trachea is deviated to the right, jugular veins are distended bilaterally, and he has absent breath sounds and hyperresonance to percussion on the left side. Subcutaneous emphysema is palpated on the left thoracic wall. What is the best next step in management?
Chest tube thoracotomy
Diagnostic peritoneal lavage
Needle thoracostomy
Pericardiocentesis
Surgical exploration
A 75-year-old man comes into the emergency department with a 10-minute history of crushing substernal chest pain radiating to his left arm. This man is well known to the staff due to his long history of chest pain. His creatine phosphokinase level is elevated and his troponin T level is 0.4 ng/mL. Which of the following is the most likely diagnosis?
Acute myocardial infarction
Hypochondriasis
Prinzmetal’s angina
Stable angina
Unstable angina
A 91-year-old woman presents to the emergency department with a chief complaint of shortness of breath over the past 2 days. She has a history of hypertension and coronary artery bypass surgery 25 years earlier. Her blood pressure is 178/92 mm Hg and she has jugular venous distension, hepatomegaly, and 3+ lower extremity edema. ECG is remarkable for left ventricular hypertrophy, no ST-segment elevations or depressions, no Q waves, and no T wave abnormalities. Echocardiogram reveals an ejection fraction of 60% and left atrial dilatation. There is universal left ventricular thickening. No valvular regurgitation or stenosis was noted. Which of the following underlying conditions is the most likely cause of this patient’s symptoms?
Hypertensive heart disease
Hypertrophic obstructive cardiomyopathy
Ischemic heart disease
Mitral valve prolapse
Myocarditis
A 39-year-old white man with essential hypertension presents for a routine health maintenance visit. He has no complaints and reports compliance with his hydrochlorothiazide. His pulse is 70/min, blood pressure is 145/92 mm Hg, and respiratory rate is 16/min. His body mass index is 24 kg/m2. His physical examination is within normal limits. For which condition is the patient at increased risk?
End-stage renal disease
Hypercholesterolemia
Hypertrophic cardiomyopathy
Second-degree Mobitz I atrioventricular block
Type 2 diabetes mellitus
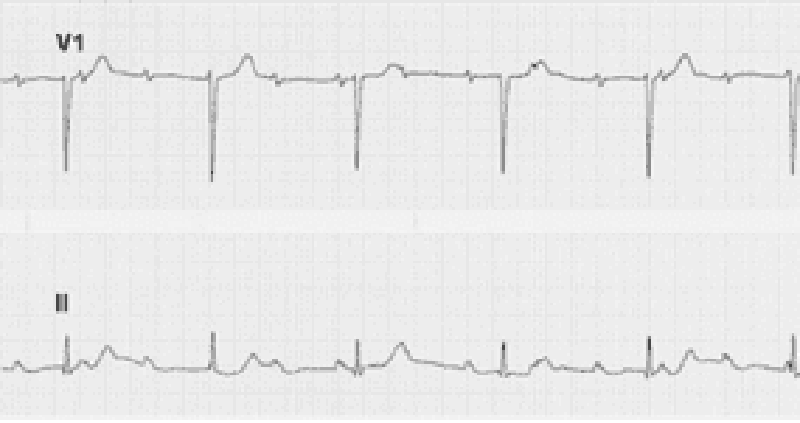
A 69-year-old woman complains of easy fatigue and one episode of presyncope. On examination of the jugular venous pressure (JVP), there are irregular large a waves. The ECG has fixed PP and RR intervals but varying PR intervals. Which of the following conditions is this most likely caused by?
Surgical removal of an atrium
Independent beating of atria and ventricles
A reentry phenomenon
A drug effect
A heart rate under 60 beats/min
A 47-year-old woman has new-onset transient right arm weakness and word finding difficulty symptoms lasting 3 hours. She is also experiencing exertional dyspnea, and had a syncopal event 1 month ago. Her echocardiogram reveals a cardiac tumor in the left atrium, it is pendunculated and attached to the endocardium. Which of the following is the most likely cause of this lesion?
Myxoma
Sarcoma
Rhabdomyoma
Fibroma
Lipoma
A 58-year-old man is undergoing cardiac catheterization for evaluation of chest pain symptoms. He is worried about the risks, and as part of obtaining informed consent, you advise him about the risks and benefits of the procedure. Which of the following aspects of angiography is true?
It is contraindicated in the presence of cyanosis
It is considered noninvasive
It is generally performed with cardiopulmonary bypass
It may cause renal failure
It requires carotid artery puncture
23-year-old man develops sharp left-sided chest pain, fever, and a friction rub heard at the lower left sternal border, unaffected by respiration. The pain is also aggevated by lying down and relieved by sitting up. He is otherwise well with no other symptoms and the remaining physical examination is normal. Which of the following is the most likely cause for his symptoms?
Rheumatic fever
Tuberculosis (TB)
Herpes simplex virus
MI
Coxsackievirus
A 55-year-old man with hypertension and a one-pack-per-day smoking history presents to the ED complaining of three episodes of severe heavy chest pain this morning that radiated to his left shoulder. In the past, he experienced chest discomfort after walking 20 minutes that resolved with rest. The episodes of chest pain this morning occurred while he was reading the newspaper. His BP is 155/80 mm Hg, HR 76 beats per minute, and RR 15 breaths per minute. He does not have chest pain in the ED. An ECG reveals sinus rhythm with a rate of 72. A troponin I is negative. Which of the following best describes this patient’s diagnosis?
Stable angina
Unstable angina
Non–ST-elevation MI
ST-elevation MI (STEMI)
Pericarditis
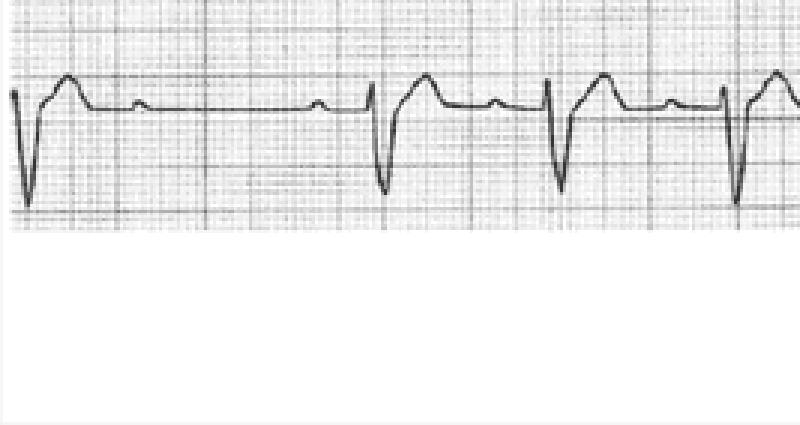
A 58-year-old man is brought to the ED for a syncopal episode at dinner. His wife states that he was well until she found him suddenly slumping in the chair and losing consciousness for a minute. The patient recalls having some chest discomfort and shortness of breath prior to the episode. His rhythm strip, obtained by EMS, is shown below. Which of the following best describes these findings?
Mobitz type I
Mobitz type II
First-degree atrioventricular (AV) block
Atrial flutter with premature ventricular contractions (PVCs)
Sinus bradycardia
In the ICU, a patient suddenly becomes pulseless and unresponsive, with cardiac monitor indicating ventricular tachycardia. The crash cart is immediately available. What is the best first therapy?
Amiodarone 150-mg IV push
Lidocaine 1.5-mg/kg IV push
Epinephrine 1-mg IV push
Defibrillation at 200 J
Defibrillation at 360 J
A 70-year-old female has been healthy except for hypertension treated with a thiazide diuretic. She presents with sudden onset of a severe, tearing chest pain, which radiates to the back and is associated with dyspnea and diaphoresis. Blood pressure is 210/94. Lung auscultation reveals bilateral basilar rales. A faint murmur of aortic insufficiency is heard. The BNP level is elevated at 550 pg/mL (Normal < 100). ECG shows nonspecific ST-T changes. Chest x-ray suggests a widened mediastinum. Which of the following choices represents the best initial management?
IV furosemide plus IV loading dose of digoxin
Percutaneous coronary intervention with consideration of angioplasty and/or stenting
Blood cultures and rapid initiation of vancomycin plus gentamicin, followed by echocardiography
IV beta-blocker to control heart rate, IV nitroprusside to control blood pressure, transesophageal echocardiogram
IV heparin followed by CT pulmonary angiography
A 55-year-old African American female presents to the ER with lethargy and blood pressure of 250/150. Her family members indicate that she was complaining of severe headache and visual disturbance earlier in the day. They report a past history of asthma but no known kidney disease. On physical examination, retinal hemorrhages are present. Which of the following is the best approach?
Intravenous labetalol therapy
Continuous-infusion nitroprusside
Clonidine by mouth to lower blood pressure
Nifedipine sublingually to lower blood pressure
Intravenous loop diuretic
A 36-year-old male presents with the sensation of a racing heart. His blood pressure is 110/70, respiratory rate 14/minute, and O2 saturation 98%. His ECG shows a narrow QRS complex tachycardia with rate 180, which you correctly diagnose as paroxysmal atrial tachycardia. Carotid massage and Valsalva maneuver do not improve the heart rate. Which of the following is the initial therapy of choice?
Adenosine 6-mg rapid IV bolus
Verapamil 2.5 to 5 mg IV over 1 to 2 min
Diltiazem 0.25-mg/kg IV over 2 min
Digoxin 0.5 mg IV slowly
Electrical cardioversion at 50 J
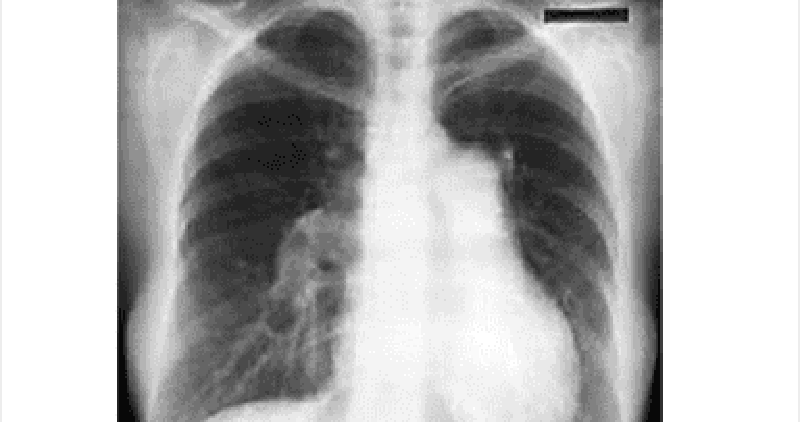
Auscultation of the heart of a 17-year-old boy reveals an increased intensity of the pulmonary component of the second heart sound. He complains of dyspnea on exertion but no other cardiac or pulmonary symptoms. Which of the following explanations is the most likely cause of his dyspnea?
Pulmonary stenosis
Aortic stenosis
MI
Pulmonary hypertension
Systemic hypertension
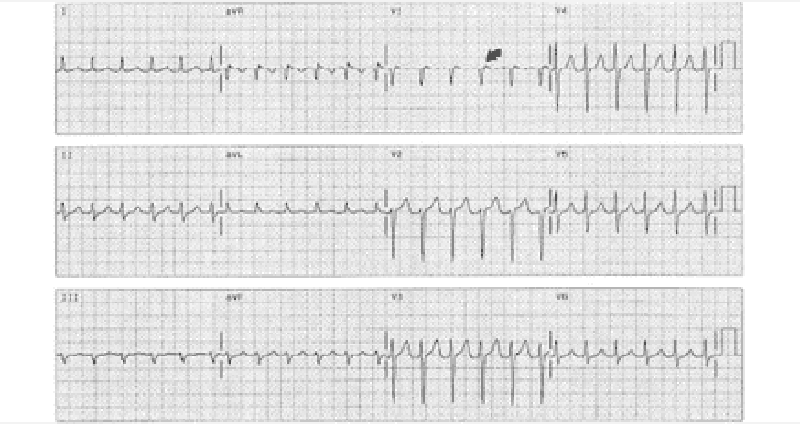
A 22-year-old woman complains of palpitations and has a regular heartbeat at a rate of 170/min, with a blood pressure of 110/70 mm Hg. The rate abruptly changes to 75/min after applying carotid sinus pressure. Which of the following is the most likely diagnosis?
Sinus tachycardia
Paroxysmal atrial fibrillation
Paroxysmal atrial flutter
Paroxysmal supraventricular tachycardia (PSVT)
Paroxysmal ventricular tachycardia
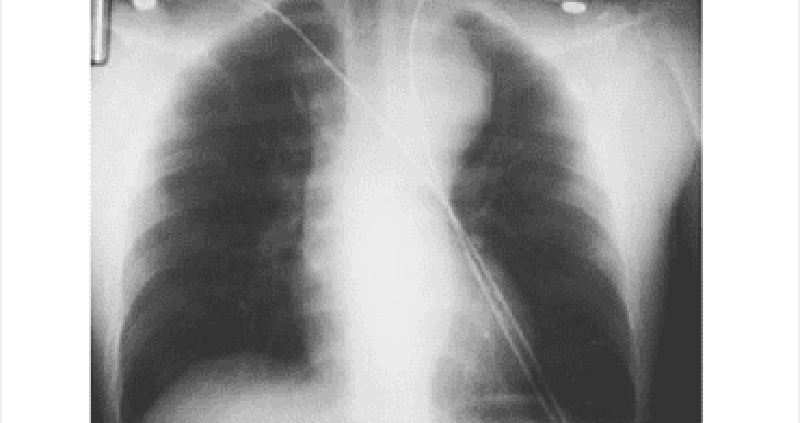
A 58-year-old man with hypertension is brought to the emergency room after suddenonset chest pain that radiates to his back and arms. He is in moderate distress with a blood pressure of 160/90 mm Hg in the left arm and 120/70 mm Hg in the right arm. Cardiac examination reveals a soft second heart sound and a murmur of aortic insufficiency. His ECG shows sinus tachycardia but no acute ischemic changes, and the chest x-ray (CXR). Which of the following is the most appropriate next step in confirming the diagnosis?
Coronary angiography
Transthoracic echocardiography
Computerized tomography (CT) chest
Exercise stress test
Cardiac troponin level
A 17-year-old girl develops exertional dyspnea, but has no cough, sputum, or wheezing symptoms. On examination, she has a fixed splitting of her second heart sound and a 3/6 systolic ejection murmur heard best over the left sternal border. An echocardiogram confirms the condition. Which of the following is the best physiologic explanation for her condition?
Pulmonary blood flow is greater than systemic blood flow
Pulmonary blood flow is less than systemic blood flow
Pulmonary blood flow is equal to systemic blood flow
The left ventricle is enlarged
The systemic blood pressure is elevated
{"name":"Cardiovascular 3", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 23-year-old woman who is an elementary school teacher is brought to the ED after syncopizing in her classroom while teaching. Prior to passing out, she describes feeling light-headed and dizzy and next remembers being in the ambulance. There was no evidence of seizure activity. She has no medical problems and does not take any medications. Her father died of a “heart problem” at 32 years of age. She does not smoke or use drugs. BP is 120\/70 mm Hg, pulse rate is 71 beats per minute, RR is 14 breaths per minute, and oxygen saturation is 100% on room air. Her physical examination and laboratory results are all normal. A rhythm strip is seen below. Which of the following is the most likely diagnosis?, A 55-year-old man presents to the ED with chest pain and shortness of breath. His BP is 170\/80 mm Hg, HR is 89 beats per minute, and oxygen saturation is 90% on room air. Physical examination reveals crackles midway up both lung fields and a new holosystolic murmur that is loudest at the apex and radiates to the left axilla. ECG reveals ST elevations in the inferior leads. Chest radiograph shows pulmonary edema with a normalsized cardiac silhouette. Which of the following is the most likely cause of the cardiac murmur?, A 22-year-old man presents to the ED with a history consistent with an acute MI. His ECG reveals ST elevations and his cardiac biomarkers are positive. He has been smoking half a pack of cigarettes per day for the last 3 months. He drinks alcohol when hanging out with his friends. His grandfather died of a heart attack at 80 years of age. The patient does not have hypertension or diabetes mellitus and takes no prescription medications. A recent cholesterol check revealed normal levels of total cholesterol, lowdensity lipoprotein (LDL), and high-density lipoprotein (HDL). Which of the following is the most likely explanation for his presentation?","img":"https://cdn.poll-maker.com/11-489431/201.png?sz=1200-010000033053"}
More Quizzes
Matter quiz
1166
Guess the Australia Test debutant from the match
1050
Ethics & Morality Quiz
15816
Quirky Preferences Quiz
10539
Qualitative Reasoning Questions - Free Practice
201023417
Midwest Landforms - Identify Western U.S. Features
201018960
What iPhone Should I Get? Free - Find Your Best Model
201019145
How Does He Feel About Me - Free & Instant Results
201019937
Animal Scientific Names - Identify Each Species
201028226
Undertale Soul: Which Soul Are You? Free Results
201020367
King Henry Doesn't Drink Chocolate Milk - Metric Prefix
201019052
Seizure Symptoms - Test Your Knowledge (Free)
201018433