DES 3 ep6
234) A 24-year-old man with chronic schizophrenia is brought to the emergency room after his parents found him in his bed and were unable to communicate with him. On examination, the man is confused and disoriented. He has severe muscle rigidity and a temperature of 39.4°C (103°F). His blood pressure is elevated, and he has a leucocytosis. Which of the following is the best first step in the pharmacologic treatment of this man?
. Haloperidol
. Lorazepam
. Benztropine
. Bromocriptine
. Lithium
235) A 30-year-old man is brought to the emergency room after he was found wandering on the streets with no shoes on in the middle of winter. He is admitted to the inpatient psychiatric unit and stabilized on antipsychotic medication. Looking at past records, his psychiatrist notes that he is repeatedly noncompliant with his medication postdischarge, and each time he relapses within 6 months. Which of the following medications is the best one for this patient to be maintained on?
. Clozapine
. Haloperidol decanoate
. Thioridazine
. Chlorpromazine
. Quetiapine
236) A 23-year-old woman was diagnosed with schizophrenia after a single episode of psychosis (hallucinations and delusions) that lasted 7 months. She was started on a small dose of olanzapine at the time of diagnosis, which resulted in the disappearance of all her psychotic symptoms. She has now been symptom free for the past 3 years. Which of the following treatment changes should be made first?
. Her olanzapine should be decreased, but not stopped
. Her olanzapine should be decreased and then stopped if she remains symptom free
. Her olanzapine should be maintained at a constant level, but she can stretch out the time between her appointments with the psychiatrist
. Her diagnosis should be reexamined as she is likely not schizophrenic at all
. Her olanzapine should be switched to a long-acting depot antipsychotic medication such as haloperidol decanoate
237) A 28-year-old woman is diagnosed with bipolar disorder, manic type, when she was hospitalized after becoming psychotic, hypersexual, severely agitated, and unable to sleep. She is started on a medication in the acute phase of her illness. Which of the following medications, recommended for acute use in manic patients, is recommended to be continued on into maintenance therapy?
. Lamotrigine
. Aripiprazole
. Olanzepine
. Lithium
. Ziprasidone
238) A 30-year-old man comes to the psychiatrist for the evaluation of a depressed mood. He states that at least since his mid-20s he has felt depressed. He notes poor self-esteem and low energy, and feels hopeless about his situation, though he denies suicidal ideation. He states he does not use drugs or alcohol, and has no medical problems. His last physical examination by his physician 1 month ago was entirely normal. Which of the following treatment options should be tried first?
. Hospitalization
. ECT
. Venlafaxine
. Psychoanalysis
. Amoxapine
239) A 22-year-old college student calls his psychiatrist because for the past week, after cramming hard for finals, his thoughts have been racing and he is irritable. The psychiatrist notes that the patient’s speech is pressured as well. The patient has been stable for the past 6 months on 500 mg of valproate twice a day. Which of the following is the most appropriate first step in the management of this patient’s symptoms?
. Hospitalize the patient
Increase the valproate by 500 mg/day
. Start haloperidol 5 mg qd
. Prescribe clonazepam 1 mg qhs
. Tell the patient to begin psychotherapy one time per week
240) A 38-year-old woman with bipolar disorder has been stable on lithium for the past 2 years. She comes to her psychiatrist’s office in tears after a 2-week history of a depressed mood, poor concentration, loss of appetite, and passive suicidal ideation. Which of the following is the most appropriate next step in the management of this patient?
. Start the patient on a long-acting benzodiazepine
. Start the patient on a second mood stabilizer
. Stop the lithium and start an antidepressant
. Start an antidepressant and continue the lithium
. Stop the lithium and start an antipsychotic
241) A 42-year-old woman sees her physician because she has been depressed for the past 4 months. She also notes that she has gained 20 lb without trying to. She notes that she does not take pleasure in the activities that she once enjoyed and seems fatigued most of the time. These symptoms have caused the patient to withdraw from many of the social functions that she once enjoyed. The physician diagnoses the patient with hypothyroidism and starts her on thyroid supplementation. Six weeks later, the patient’s thyroid hormone levels have normalized, but she still reports feeling depressed. Which of the following is the most appropriate next step in the management of this patient?
. Increase the patient’s thyroid supplementation
. Recommend that the patient begin psychotherapy
. Start the patient on an antidepressant medication
. Tell the patient that she should wait another 6 weeks, during which time her mood will improve
. Take a substance abuse history from the patient
242) A 54-year-old man sees a physician complaining of a depressed mood and inability to sleep for the past 3 weeks. He tells the physician that in the past when he has had similar episodes, he was placed on a monoamine oxidase inhibitor, which proved effective. The physician diagnoses the patient with major depression and agrees to use an MAOI. Which of the following foods must be completely avoided by this patient while on this medication?
. Coffee
. Licorice
. Cheddar cheese
. Chocolate
. Soy sauce
243) A 10-year-old boy is brought to the psychiatrist by his mother. She states that for the past 2 months he has been increasingly irritable, withdrawn, and apathetic. He has been refusing to do his homework, and his grades have dropped. Which of the following is the best next step in management?
The child should be hospitalized
. The child should be started in supportive psychotherapy
. The child should receive an antidepressant medication
. The mother should be warned that the child will likely turn out to be bipolar (67% chance)
. The child should receive lithium and an antidepressant
244) A 35-year-old woman is seeing a psychiatrist for treatment of her major depression. After 4 weeks on fluoxetine at 40 mg/day, her psychiatrist decides to try augmentation. Which of the following is the most appropriate medication?
. Lithium
. Sertraline
. An MAO inhibitor
. Clonazepam
. Haloperidol
245) While working as the medical resident on call, you are paged to see a 72-year-old woman who complains of a headache. Upon seeing you, she snaps, "You look young and foolish. I hope you're more efficient than you seem." While you are performing a basic physical examination on her, she says, "I'm going to complain to the hospital administrators about you because you have no idea how to properly deal with a patient." Which of the following is the best response to her threat?
. "Feel free to do as you please."
. "Please allow me to complete the physical examination first."
. "You're hurting me with your comments."
. "You seem to be angry, and I don't know why."
. "Would you prefer that my attending see you instead?"
246) A colleague who works as a pediatrician in your group practice comes to your office to inquire about a patient you examined earlier this morning. The colleague says that he recognized the patient as a former neighbor of his who is also a good friend of the family. The patient was recently diagnosed as HIV-positive and is now on antiretroviral medication. Your colleague asks what the patient is being treated for. What is the most appropriate response to such an inquiry?
. "Actually, we've not been able to diagnose his condition."
. "He is on anti-retrovirals because he is HIV positive.”
. "I don't think it would be appropriate for me to discuss this with you."
. "It is unprofessional of you to ask me this question."
. "I don't think it is necessary for me to discuss this with you."
247) A 35-year-old female presents to your office complaining of knee pain. She has a long history of rheumatoid arthritis affecting her hand and knee joints. The stiffness and pain has persisted over the last several months and has responded poorly to NSAIDs. Over the last two days the pain in her right knee has been interfering with her sleep. She had an episode of chills this morning. Her blood pressure is 120/70 mmHg, pulse is 90/min, temperature is 38.7°C (102°F) and respiratory rate is 18/min. Physical examination reveals swelling in the joints of her hand and wrist. The right knee is red and swollen; active and passive range of motion at the right knee is limited due to pain. This patient's current condition can be best treated with which of the following?
. Corticosteroids
. Colchicine
. Antibiotics
. Anti-cytokine agents
. Antimetabolites
248) A 68-year-old African-American woman presents to the ER in acute distress. She complains of a sudden onset of complete visual loss in her right eye. Her vision had been blurry for the past few days and acutely worsened one hour ago. She also describes right-sided headaches of two months duration for which she has taken ibuprofen without relief. She has no nausea or vomiting. She has diabetes, hypertension, and degenerative joint disease. Her temperature is 37.2°C (98.9°F) and blood pressure is 146/86 mmHg. Examination reveals complete loss of vision in the right eye. Her pupils are 4 mm bilaterally. Fundoscopy shows a swollen pale disc with blurred margins. A bruit is heard in the right subclavicular area. Motor and sensory examination is within normal limits. Which of the following is the most appropriate next step in management?
. Low dose prednisone
. Temporal artery biopsy
. MRI of the brain with contrast
. Methotrexate therapy
. High dose prednisone
249) A 45-year-old woman presents to your office complaining of one week of fatigue and weakness in her shoulders and hips. She reports difficulty performing household tasks, climbing the stairs, or rising from a chair. She denies any facial weakness or blurry vision. She has a history of gastroesophageal reflux disease and takes over the counter ranitidine. Her family history is positive for breast cancer in her mother. Her vital signs are within normal limits and examination shows normal sensation and deep tendon reflexes. Strength is 4 out of 5 in the proximal muscles groups of the arms and legs, and there is no limitation in the range of motion. Other physical examination is within normal limits. The ESR is 80 mm/hour and her serum creatine kinase is elevated. The TSH is within normal limits. Which of the following is the best initial treatment for this patient?
. Corticosteroids
. Indomethacin
. Colchicine
. Riluzole
. Amitriptyline
250) A 55-year-old man presents to his physician with 6 months of mild intermittent pain in both knees. The pain is aggravated by walking and weight bearing, and is partially relieved by rest. He also complains of morning stiffness that lasts for 10 minutes. He does not smoke but drinks alcohol occasionally. His BMI is 25 Kg/m2, temperature is 37°C (98.6°F), pulse is 75/min, and blood pressure is 130/80 mmHg. Examination reveals crepitus over both knee joints. Which of the following is the most appropriate initial treatment for this patient?
. Ketorolac
. Antibiotics
. Colchicine
. Acetaminophen
. Oxycodone
251) A 38-year-old woman complains of chronic aching pain and stiffness around the neck, shoulders, low back and hips. She fatigues easily and has been having problems with sleep. Even minor exertion worsens her pain. She has no muscle weakness, fever, malaise, weight loss or rash. She has a history of irritable bowel syndrome. Her vital signs are within normal limits. Examination shows multiple tender spots over specific points on her body. Power is 5/5 in all extremities and deep tendon reflexes are 2+. No sensory abnormalities are noted. Labs show: ESR 9 mm/hr, Hematocrit 43%, WBC count 7,000/microL, Platelet count 200,000/microL, TSH 3 microU/L, CPK 100 IU/L. Which of the following is the most appropriate pharmacotherapy for this patient?
. Amitriptyline
. Naproxen
. Colchicine
. Prednisone
. Oxycodone
252) A 35-year-old man presents to your office with severe back pain. The pain started three days ago when the patient was carrying a heavy pack. The pain radiates to the posterior surface of the right thigh. The straightleg raise test is positive. There is no bladder or bowel incontinence. Pain and temperature perception is preserved in the affected extremity, as well as in the perineal area. Anal reflex is normal. Which of the following is the best next step in the management of this patient?
. MRI of the spine
. CT scan of the spine
. Plain roentgenogram
. Early mobilization and NSAIDs
. Surgical decompression
253) A 31-year-old Caucasian male complains of joint pains. He describes right knee pain, right heel pain and lowback pain. He was recently treated for urethral discharge at an outside clinic. He has no history of trauma or illicit drug use. He is afebrile, and his vital signs are stable. His right knee is swollen, tender and warm to touch; tenderness is also present over the Achilles tendon. Oral examination shows mouth ulcers. Synovial fluid analysis from the right knee shows a white blood cell count of 10,000/mm3 with many polymorphonuclear leukocytes but a negative Gram stain. Which of the following is the most appropriate initial pharmacotherapy for this patient?
. NSAIDs
. Antihistamines
. Antibiotics
. Colchicine
. Allopurinol
254) A 70-year-old male presents with malaise, pain and stiffness of his neck, shoulders and hips for the last 3 months. His stiffness is worse in the morning and lasts about 30-40 minutes. He also complains of a recent weight loss of 7 1bs and mild fevers. He has no headache, scalp tenderness, visual symptoms or jaw claudication. Examination shows no swelling or tenderness of the involved joints with normal range of motion on active and passive movement. The arteries of the scalp, neck and extremities are normally palpable without any tenderness. Labs show a hematocrit of 31% and an ESR of 65 mm/hr. Blood cultures are negative. Which of the following is the most appropriate next step in management of this patient?
. Temporal artery biopsy
. Treatment with nonsteroidal anti-inflammatory agents
. Treatment with high-dose prednisone
. Treatment with low-dose prednisone
. Measure antinuclear antibodies and rheumatoid factor levels
255) A 43-year-old construction worker presents to your office 2 weeks after an episode of acute back pain. The pain started after lifting a heavy box, was localized to the lower back with little radiation to the buttocks, and quickly responded to conservative treatment. His past medical history is insignificant. He smokes 2 packs a day and consumes alcohol occasionally. He is concerned about the possibility of recurrence of the pain. Which of the following would be most helpful in preventing another episode of back pain in this patient?
. Sleep on the stomach
. Limiting the physical activity as much as possible
. Regular exercise with repetitive twisting and bending
. Bend at the waist, not at the knees
. Keep the back straight while lifting an object
256) A 54-year-old woman comes to the physician's office complaining of chronic, bilateral knee and hip pain. The pain increases with activity and is relieved by rest. She denies fever, chills or weight loss. The review of systems is unremarkable. She currently weighs 80 kg (180 lb) and is 146 cm (59 in) tall. Her knee joints are tender but there is no warmth, erythema or effusion. X-rays show narrow joint space, subchondral bone cysts, and bony spurs in both knees. Which of the following interventions would provide the greatest long-term benefit to this patient?
. Non-steroidal antiinflammatory agents
. Muscle strengthening exercise
. Chondroitin sulfate
. Weight loss
. Acetaminophen with codeine
257) A 45-year-old man complains of sudden pain and swelling in his left first metatarsophalangeal joint. He is undergoing high dose induction chemotherapy for acute leukemia. Joint fluid aspiration reveals negative birefringent crystals and elevated white cell count. Which of the following prophylactic measures would most likely have prevented this condition?
. Urine acidification
. N-acetylcysteine
. Mesna
Allopurinol
. Adequate hydration
258) A 30-year-old Caucasian female patient is seen at the rheumatology clinic. She has a 4-year history of rheumatoid arthritis. Over the past year, she has noticed an improvement in her symptoms. Examination of her joints reveals less swelling and erythema than on the previous visit Laboratory studies show: CBC: Hb 10.8 g/dL, Ht 32%, MCV 104 fl, Platelet count 226,000/cmm, Leukocyte count 7,500/cmm, Neutrophils 65%, Eosinophils 1%, Lymphocytes 28%, Monocytes 6%. Serum: Serum Na 140 mEq/L, Serum K 3.9 mEq/L, Chloride 100 mEq/L, Bicarbonate 18 mEq/L, BUN 16 mg/dL, Serum Creatinine 1.1 mg/dL, Calcium 9.8 mg/dL, Blood Glucose 98 mg/dL. Which of the following medications is this patient most likely taking?
. Prednisone
. Hydroxychloroquine
. Azathioprine
. Cyclosporin
. Methotrexate
259) A 46-year-old woman suffering from systemic lupus erythematosus (SLE) develops hematuria and proteinuria. She was diagnosed with SLE four years ago and has been treated with hydroxychloroquine. A renal biopsy is performed and shows diffuse proliferative glomerulonephritis. She is started on cyclophosphamide and prednisone and hydroxychloroquine is stopped. She continues these two medications for several weeks because of the low therapeutic response. This new therapeutic regimen puts her at an increased risk for which of the following conditions?
. Optic neuritis
. Cochlear dysfunction
. Peripheral neuropathy
. Bladder carcinoma
. Digital vasospasm
260) A 35-year-old white female presents with pain and stiffness of her wrist and hand joints for the last several months. Her morning stiffness lasts for more than an hour. She also complains of redness and joint swelling. Her past medical history is significant only for a similar episode one year ago. That episode resolved with over the counter ibuprofen. Examination of her joints shows redness, warmth, swelling and tenderness of proximal interphalangeal joints, metacarpophalangeal joints and wrists. X-ray shows periarticular osteopenia and erosions of the proximal interphalangeal and metacarpophalangeal joints. She started taking indomethacin with good relief. Which of the following is the most appropriate next step in the management of this patient?
. Methotrexate
. Glucocorticoids
. Azathioprine
. Celecoxib
. Etanercept
261) A 40-year-old man complains of exquisite pain and tenderness in the left ankle. There is no history of trauma. The patient is taking hydrochlorothiazide for hypertension. On examination, the ankle is very swollen and tender. There are no other physical examination abnormalities. Which of the following is the best next step in management?
. Perform arthrocentesis.
. Begin colchicine and broad-spectrum antibiotics.
. Obtain ankle x-ray to rule out fracture.
. Begin allopurinol if uric acid level is elevated.
. Apply a splint or removable cast.
262) A 48-year-old woman complains of joint pain and morning stiffness for 4 months. Examination reveals swelling of the wrists and MCPs as well as tenderness and joint effusion in both knees. The rheumatoid factor is positive, antibodies to cyclic citrullinated protein are present, and subcutaneous nodules are noted on the extensor surfaces of the forearm. Which of the following statements is correct?
. The patient has RA and should be evaluated for disease-modifying antirheumatic therapy
. Prednisone 60 mg per day should be started.
. A nonsteroidal anti-inflammatory drug should be added to aspirin
. The patient’s prognosis is highly favorable.
. The patient should receive a 3-month trial of full-dose nonsteroidal anti-inflammatory agent before determining whether and/or what additional therapy is indicated
263) A 60-year-old man complains of pain in both knees coming on gradually over the past 2 years. The pain is relieved by rest and worsened by movement. The patient is 5ft 9 in. Tall and weighs 210 lb. There is bony enlargement of the knees with mild warmth and small effusions. Crepitation is noted on motion of the knee joint bilaterally. There are no other findings except for bony enlargement at the distal interphalangeal joint. Which of the following is the best way to prevent disease progression?
Weight reduction
Calcium supplementation
. Long-term nonsteroidal anti-inflammatory drug (NSAID) administration
. Total knee replacement
. Oral prednisone
264) A 20-year-old woman has developed low-grade fever, a malar rash, and arthralgias of the hands over several months. High titers of anti-DNA antibodies are noted, and complement levels are low. The patient’s white blood cell count is 3000/μL, and platelet count is 90,000/μL. The patient is on no medications and has no signs of active infection. Which of the following statements is correct?
If glomerulonephritis, severe thrombocytopenia, or hemolytic anemia develops, high-dose glucocorticoid therapy would be indicated
Central nervous system symptoms will occur within 10 years.
. Joint deformities will likely occur.
. The patient can be expected to develop Raynaud phenomenon when exposed to cold
. The disease process described is an absolute contraindication to pregnancy
265) A 75-year-old man complains of headache. On one occasion he transiently lost vision in his right eye. He also complains of aching in the shoulders and neck. There are no focal neurologic findings. Carotid pulses are normal without bruits. Laboratory data show a mild anemia. Erythrocyte sedimentation rate (ESR) is 85. Which of the following is the best approach to management?
Begin glucocorticoid therapy and arrange for temporal artery biopsy.
. Schedule temporal artery biopsy and begin corticosteroids based on biopsy results and clinical
. Schedule carotid angiography.
. Follow ESR and consider further studies if it remains elevated
. Start aspirin and defer any invasive studies unless further symptoms develop.
266) A 55-year-old man with psoriasis has been troubled by long-standing destructive arthritis involving the hands, wrists, shoulders, knees, and ankles. Hand films demonstrate pencil-in-cup deformities. He has been treated with naproxen 500 mg bid, sulfasalazine 1 g bid, prednisone 5 mg qd, and methotrexate 17.5 mg once a week without substantive improvement. Which of the following treatments is most likely to provide long-term benefit?
. Cyclophosphamide
. Addition of folic acid supplementation
. Tumor necrosis factor alpha inhibitor
. Oral cyclosporine
. Higher-dose steroids in the range of 20 mg of prednisone per day
267) A 35-year-old woman complains of aching all over. She says she sleeps poorly and all her muscles and joints hurt. Her symptoms have progressed over several years. She reports she is desperate because pain and weakness often cause her to drop things. Physical examination shows multiple points of tenderness over the neck, shoulders, elbows, and wrists. There is no joint swelling or deformity. A complete blood count and erythrocyte sedimentation rate are normal. Rheumatoid factor is negative. Which of the following is the best therapeutic option in this patient?
. Graded aerobic exercise
. Prednisone
. Hydroxychloroquine
. Weekly methotrexate
. A nonsteroidal antiinflammatory drug
1) A 32-year-old Caucasian female comes to the physician because of a one-week history of fatigue, progressive worsening of shortness of breath and swelling of feet. She denies any chest pain. She has no other medical problems except a recent cold two weeks ago. She is not taking any medication. Her temperature is 36.7°C (98°F), blood pressure is 110/65 mmHg, pulse is 90/min, and respirations are 20/min. Bilateral basal crackles, elevated jugular venous pressure, and 2+ bilateral pitting edema of the ankles are noted. Complete blood count is unremarkable. Transthoracic echocardiogram of her heat will most likely show?
. Eccentric hypertrophy of the heart
. Concentric hypertrophy of the heart
. Hypokinesia of the inferior wall
. Mitral stenosis
. Dilated ventricles with diffuse hypokinesia
2) A 35-year-old Caucasian male is being evaluated for poor exercise tolerance and muscle weakness. He has no past medical history. His blood pressure ranges from 175-185 mmHg systolic and 105-115 mmHg diastolic on repeat measurement. His heat rate is 78-95/min His serum chemistry is significant for blood glucose of 95 mg/dL serum creatinine of 0.7mg/dL serum Na of 146 mEq/L and serum K of 2.4 mEq/L. CT scan of the abdomen reveals a 3 cm mass in the left adrenal gland. Which of the following additional findings would you expect in this patient? ( Plasma renin activity, Serum aldosterone, Serum bicarbonate )
High High High
High High Low
Low High Low
Low High High
High Low High
3) A 25-year-old G2, PI at 28 weeks gestation is brought to the emergency department by her boyfriend, who found her lying on her bed in a pool of blood. She is very drowsy, but denies any pain or uterine contraction. Her temperature is 38°C (100.4°F) and respirations are 18/min. Physical examination is suggestive of a transverse lie. Inspection of the perineum reveals gross blood and active bleeding per vagina. Which of the following set of parameters would most likely be seen in this patient?
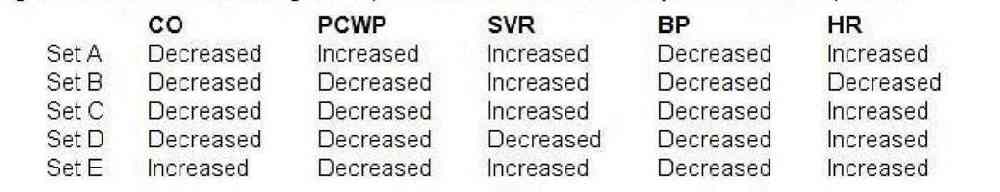
qq
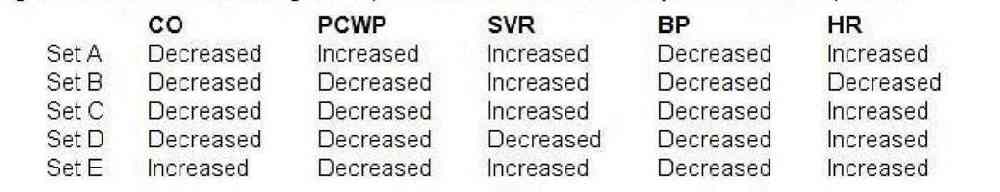
. set B
. Set C
. set D
. Set A
. set E
4) A 20-year-old female presents to your office for a routine. She has no complaints and her past medical history is insignificant. She is not taking any medications and denies drug abuse. Her blood pressure is 125/65 mmHg and heat rate is 80/min. Cardiac auscultation reveals early diastolic murmur at the left sternal border. What is the next best step in the management of this patient?
. Electrocardiogram
. Echocardiography
. Chest x ray
Coronary angiography
. No further work-up
5) A 68-year-old man is brought to the emergency room after he passed out for one minute during an early morning jog. He was not confused after the episode and did not have bowel or bladder incontinence. He has been having exertional chest pain and shortness of breath for the past few months. He has never had any resting chest pain. He has been healthy except for hypertension, for which he takes hydrochlorothiazide. He has a 20 pack year smoking history and occasionally drinks a glass of wine. His blood pressure is 142/90 mm Hg, pulse is 80/min, and respirations are 16/min. Carotid pulse is delayed S2 is weak and an S4 is present. A grade 3/6 systolic ejection murmur is in the right 2nd intercostal space, radiating to the carotids. Neurological examination reveals no focal findings, and there are no signs of head trauma. An EKG shows left ventricular hypertrophy. The first set of cardiac enzymes is negative. Which of the following is the most appropriate next step in management?
. Exercise stress test
. CT scan of the head
. Echocardiogram
Electroencephalogram (EEG)
. CT angiogram of the chest
6) A 61-year-old woman with a history of diabetes and hypertension is brought to the ED by her daughter. The patient states that she started feeling short of breath approximately 12 hours ago and then noticed a tingling sensation in the middle of her chest and became diaphoretic. An ECG reveals ST depression in leads II, III, and aVF. You believe that the patient had a non–ST-elevation MI (NSTEMI). Which of the following cardiac markers begins to rise within 3 to 6 hours of chest pain onset, peaks at 12 to 24 hours, and returns to baseline in 7 to 10 days?
. Myoglobin
. Creatinine kinase (CK)
. Troponin I
. Creatinine kinase-MB (CK-MB)
. Lactic dehydrogenase (LDH)
7) A 71-year-old man is playing cards with some friends when he starts to feel a pain in the left side of his chest. His fingers in the left hand become numb and he feels short of breath. His wife calls the ambulance and he is brought to the hospital. In the ED, an ECG is performed. Which of the following best describes the order of ECG changes seen in an MI?
. Hyperacute T wave, ST-segment elevation, Q wave
. Q wave, ST-segment elevation, hyperacute T wave
. Hyperacute T wave, Q wave, ST-segment elevation
. ST-segment elevation, Q wave, hyperacute T wave
. ST-segment elevation, hyperacute T wave, Q wave
8) While playing a match of tennis, a 56-year-old man with a medical history significant only for acid reflux disease starts to feel substernal chest pain that radiates into his left arm and shortness of breath. His pain feels better after drinking antacid, but since it is not completely resolved, his partner calls 911. Upon arrival, EMS administers aspirin and sublingual nitroglycerin. After 20 minutes, the man’s symptoms resolve. He is brought to the ED for further evaluation where his ECG shows sinus rhythm without any ischemic abnormalities. You order a chest radiograph and send his blood work to the laboratory for analysis. Which of the following statements regarding the diagnosis of acute MI is most accurate?
. A normal ECG rules out the diagnosis of acute MI
. One set of negative cardiac enzymes is sufficient to exclude the diagnosis of MI in this patient
. Relief of symptoms by antacids essentially rules out a cardiac cause of his chest pain
. Troponin may not reach peak levels for at least 12 hours
Epigastric discomfort and indigestion is a rare presentation of ACS
9) During a routine office visit, a 62-year-old male is found to have a pulsatile non-tender mass above his umbilicus. His medical history is significant for hypertension, chronic renal insufficiency, myocardial infarction, and peripheral vascular disease. He quit smoking 10 years ago. On physical examination, his blood pressure is 160/90 mmHg and pulse is 76/min. Laboratory analyses reveal a serum creatinine of 2.0 mg/dl. Which of the following is the most appropriate next step in evaluating this patient's abdominal mass?
. CT scan with contrast
. Plain abdominal x-ray
Abdominal MRI
. Abdominal ultrasound
. No testing require
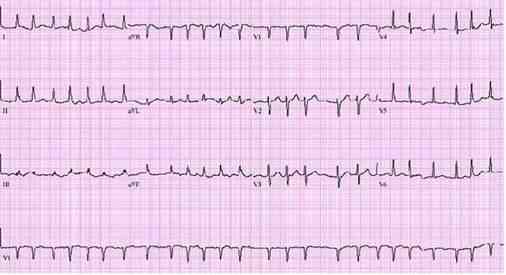
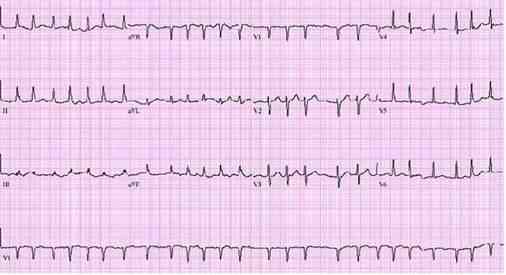
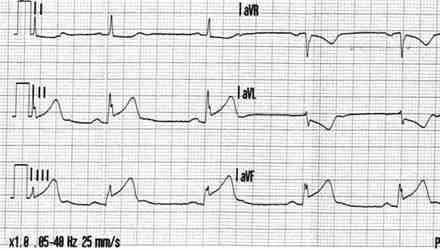
10) An 18-year-old male complains of fever and transient pain in both knees and elbows. The right knee was red and swollen for 1 day during the week prior to presentation. On physical examination, the patient has a low-grade fever. He has a III/VI, high pitched, apical systolic murmur with radiation to the axilla, as well as a soft, mid-diastolic murmur heard at the base. A tender nodule is palpated over an extensor tendon of the hand. There are pink erythematous lesions over the abdomen, some with central clearing. The following laboratory values are obtained: Hct: 42, WBC: 12,000/μL with 80% polymorphonuclear leukocytes, 20% lymphocytes, ESR: 60 mm/h. The patient’s ECG is shown below. Which of the following tests is most critical to diagnosis?
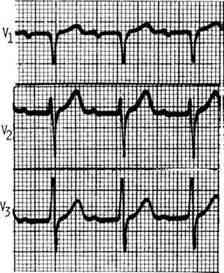
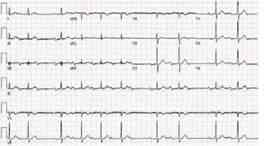
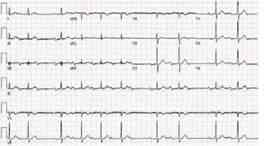
ww
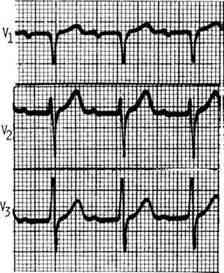
. Antistreptolysin O antibody
. Blood cultures
. Echocardiogram
Antinuclear antibodies
Creatine kinase
11) A 35-year-old male complains of substernal chest pain aggravated by inspiration and relieved by sitting up. Lung fields are clear to auscultation, and heart sounds are somewhat distant. Chest x-ray shows an enlarged cardiac silhouette. Which of the following is the best next step in evaluation?
. Cardiac catheterization
. Right lateral decubitus chest x-ray
. Echocardiogram
. Serial ECGs
. Thallium stress test
12) A 32-year-old male presents to your office with concern about progressive fatigue and lower extremity edema. He has experienced decreased exercise tolerance over the past few months, and occasionally awakens coughing at night. Past medical history is significant for sickle cell anemia and diabetes mellitus. He has had multiple admissions to the hospital secondary to vasoocclusive crises since the age of three. Physical examination reveals a displaced PMI, but is otherwise unremarkable. ECG shows a first degree AV block and low voltage. Chest x-ray shows an enlarged cardiac silhouette with clear lung fields. Which of the following would be the best initial diagnostic approach?
. Order brain-natriuretic peptide (BNP)
. Order serum iron, iron-binding capacity, and ferritin level
. Arrange for placement of a 24-hour ambulatory cardiac monitor
. Order CT scan of the chest
. Arrange for cardiac catheterization
13) A 64-year-old diabetic with a long history of uncontrolled hypertension is admitted for chest pain. ECG reveals elevated ST segments in the anterior wall leads. Cardiac enzymes are elevated and the patient is admitted to the ICU for supportive care. He receives low molecular weight heparin and is placed on a nitroglycerin drip. He continues to have chest pain and requires intravenous morphine. Three days later, the patient is transferred to the floor and he remains on bed rest. During the night the nurse on call informs you that the patient has a cold leg. On examination, the left leg is cold and there are no distal pulses. There is minimal swelling and the leg appears mottled. Emergency vascular surgery consult was placed and the appropriate treatment was given. Which of the following should also be considered in this patient?
. Chest x-ray
. Venous duplex study
. V/Q scan
. Echocardiogram
. D-dimer level
14) A 36-year-old man presents to your office for a routine pre-employment physical. He has no complaints except for occasional morning headaches. His father died suddenly at the age of 54. The patient's blood pressure is 175/103 mmHg in the right arm and 180/105 mmHg in the left arm. His heart rate is 82/min. His lungs are clear bilaterally and his heart sounds are normal. Bilateral, non-tender, upper abdominal masses are palpated on exam. His hemoglobin level is 15.2 g/dL and creatinine concentration is 0.8 mg/dL. Which of the following is most likely to diagnose this patient's condition?
. Urine metanephrines
. Abdominal ultrasound
. Aldosterone: renin ratio
. Captopril-enhanced radionuclide renal scan
. 24-hour urine cortisol
15) A 56-year-old male is hospitalized following an acute anterior wall myocardial infarction that was treated with thrombolytic therapy 4 days ago. On day 4 of his hospitalization, he develops recurrent chest pain, similar in quality and severity to his previous pain. Sublingual nitroglycerin is administered but does not help. His blood pressure is now 140/90 mmHg and his heart rate is 82/min. S1 and S2 are normal, and there are no cardiac murmurs or rubs. Lungs are clear to auscultation. Which of the following laboratory tests would be most useful to send in this setting?
. Troponin T
. Lactate dehydrogenase (LDH)
. Alkaline phosphatase
. CK-MB
. Dobutamin
16) A 46-year-old man comes to the ER because of weakness and chest tightness. He has had these symptoms for the past one hour. He denies any past medical history. He does not smoke or drink alcohol. His father had a myocardial infarction at 68 years of age and his mother has myasthenia gravis. His EKG is shown on the slide below. The patient should be evaluated for which of the following?
ee
. Cushing syndrome
. Hyperthyroidism
. Aortic dissection
. High-frequency deafness
. High-range proteinuria
17) A 60-year-old Caucasian man presents to the office with a 2-week history of worsening shortness of breath and decreased exercise tolerance. His breathlessness is worse at night. He thinks his legs are swelling up. He has hypertension, coronary artery disease and chronic obstructive pulmonary disease. He used to drink heavily and smoke 1 pack of cigarettes daily but has quit recently, although he still reports occasionally drinking a "few beers." He currently denies any chest pain, palpitations or cough. His temperature is 37.5°C (99.5°F), blood pressure is 110/70 mm Hg, pulse is 96/min and respirations are 22/min. The pertinent physical findings are an S3, bibasilar crackles, JVP 10 cm above the sternal angle, mild hepatomegaly, and 4+ pitting lower extremity edema. The patient is immediately treated with oxygen, intravenous furosemide, and nitrates. Which of the following markers is most likely elevated in this patient?
. Mean corpuscular volume
. Ejection fraction
. Urine sodium
. B-type natriuretic peptide
. Neutrophil count
18) A 68-year-old Caucasian male presents to the emergency room with a three-week history of progressive dyspnea, orthopnea, and lower extremity edema. His past medical history is significant for hypertension, type 2 diabetes mellitus, myocardial infarction experienced eight years ago, and congestive heart failure. His current medications include metoprolol, digoxin, enalapril, furosemide, spironolactone, and aspirin. His blood pressure is 145/90 mmHg, and heart rate is 75/min. Symmetric 2+ pitting edema of the lower extremities is present. Point of maximal impulse is displaced to the left and soft holosystolic murmur is heard on the apex. Bilateral crackles are present over the lower lobes. His laboratory values are: Hemoglobin 11.0 g/dl, Leukocyte count 7 ,500/cmm, Platelets 300,000/cmm, Serum sodium 128 mEq/L, Serum potassium 5.3 mEq/L, Serum calcium 9.0 mg/dl, Serum phosphorus 4.0 mg/dl, Serum creatinine 1.9 mg/dl. ECG does not reveal acute ischemic changes. Which of the following is most likely correct concerning this patient's condition?
. The combination of furosemide and enalapril is the cause of hyperkalemia
. Serum norepinephrine level is low
. Increasing the dose of digitalis may be indicated
. Hyponatremia indicates severe heart failure
. Increasing sodium intake will help to control the electrolyte abnormalities
19) A 70-year-old male is brought to the ER, by his wife, because he lost consciousness while getting up in the morning. The syncopal episode lasted for several minutes, and the patient rapidly recovered consciousness. He had diarrhea and a decreased appetite one day earlier, which resolved spontaneously. His past medical history is significant for hypertension that is effectively controlled with the combination of hydrochlorothiazide/amiloride. His blood pressure is 120/70 mmHg, while supine, and 98/50 mmHg, while standing. The physical examination revealed a mucosal dryness. The EKG is normal. Which of the following laboratory values is the most sensitive indicator of the patient's underlying condition?
. Decreased sodium concentration in the urine
. Hypokalemia
. Metabolic acidosis
. Increased BUN/creatinine ratio
. Decreased haematocrit
20) A 77-year-old woman comes to the emergency department because of feeling “light-headed and dizzy.” Except for the irregular pulse, her physical examination is normal. What is the rhythm in the lead tracing shown in Fig.?
rr
First-degree heart block
Second-degree heart block
Premature ventricular beats
Third-degree heart block
Premature atrial beats
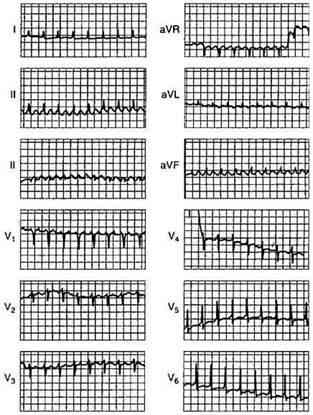
21) The ECG shown in Fig. Was obtained during the initial stages of an acute MI. The patient had just received thrombolytic therapy. What is the rhythm?
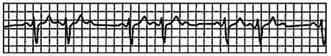
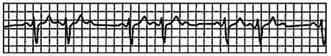
tt
Second-degree heart block
Atrial fibrillation
Wenckebach phenomenon
Atrial flutter
Nonsustained ventricular tachycardia
22) A 74-year-old woman presents to your office complaining of diarrhea and decreased appetite over the past week as well as increasing fatigue and occasional palpitations over the last few days. Her past medical history is significant for chronic atrial fibrillation for which she takes metoprolol, digoxin and warfarin. She smokes cigarettes and has for the past several years. On physical examination, her blood pressure is 140/90 mmHg and her heart rate is 70/min and irregular. Lung auscultation reveals scattered wheezes. Her abdomen is soft and non-tender. The liver span is 8 cm and the spleen is not palpable. There is no ankle edema. Her last measured INR was 2.3 two weeks ago. Which of the following is the best initial test in this patient?
. Pulmonary function tests
. Echocardiography
. Thyroid function tests
. Chest x-ray
. Blood drug level
23) A 43-year-old male complains of frequent epigastric burning not relieved by antacids. The sensation is typically brought on by heavy lifting at work and takes 10-15 minutes to go away. He denies having associated arm or neck pain, cough, shortness of breath or difficulty swallowing. His past medical history is significant for systemic lupus erythematosus (SLE) diagnosed five years ago, for which he takes low-dose prednisone daily. On physical examination, his blood pressure is 140/90 mmHg and pulse is 80/min and regular. Heart, lung, and abdomen exams are unremarkable. EKG is normal. Which of the following is the best next step in managing this patient?
. Coronary angiography
. Echocardiogram
. Myocardial perfusion testing
. Exercise EKG
. Upper Gl endoscopy
24) An 84-year-old Caucasian male is brought to the ER with severe chest pain, dyspnea and diaphoresis. His past medical history is significant for a long history of hypertension and diabetes mellitus, type 2. He experienced a severe myocardial infarction 6 months ago. His current medications are enalapril, metoprolol, aspirin, furosemide, potassium, glyburide and pravastatin, but he says that he has not been taking some of his medications recently. Physical examination reveals acrocyanosis and symmetric 3+ lower extremity edema. Point of maximal apical impulse is displaced to the left, and a holosystolic II/VI apical murmur is heard at the apex. Non-specific ST segment and T wave changes are present on ECG. The initial set of cardiac enzymes are positive. The patient continues to deteriorate, despite aggressive diuretic and vasodilator therapy. You perform an echocardiographic evaluation of left ventricular function and decide to proceed with pulmonary artery catheterization. Cardiac index (CI), total peripheral resistance (TPR) and left ventricular enddiastolic volume (LVEDV) are determined. Which of the following is most likely to present in this patient?
. Cl decreased, TPR increased, LVEDV decreased
. Cl decreased, TPR decreased, LVEDV decreased
. Cl decreased, TPR increased, LVEDV normal
. Cl decreased, TPR increased, LVEDV increased
. Cl normal, TPR decreased, LVEDV increased
25) A 42-year -old male with a past medical history of bladder cancer and recurrent hematuria presents to the emergency room after "passing out" when he got out of bed this morning. The patient says that he was standing up to urinate shortly after waking when he began feeling dizzy. Fortunately he was able to return to his bed before losing consciousness for 7-10 minutes. His EKG at the time of admission is shown below. Which of the following most likely accounts for the observed EKG changes?
. Impaired AV node conduction
. Ventricular preexcitation
. Atrial reentry
. Impaired SA node automaticity
. His bundle branch block
26) A 36-year-old male patient, who has a history of Marfan's syndrome, presents with sudden onset of severe central tearing chest pain radiating to his back. The pain is 9/10 in severity and is unrelated to exertion. He denies any history of alcohol or tobacco use. Measurement of his BP shows a difference of 35 mmHg between his two arms. Chest auscultation reveals clear lung sounds and a mid-systolic click. What is the most appropriate next diagnostic step in the management of this patient?
. Transesophageal echocardiography
. Transthoracic echocardiogram
. Coronary angiogram
. Cardiac enzymes
. Ventilation-perfusion scans
27) A 45-year-old white male presents to the ER after an episode of syncope. His medical history is unremarkable except for an upper respiratory infection one week ago. On physical examination, his temperature is 37.2°C (99°F), pulse is 90/min, blood pressure is 100/60 mmHg and respirations are 13/min. His neck veins are distended and his heart sounds are distant. His lungs are clear to auscultation bilaterally. Chest x-ray reveals small bilateral pleural effusions and an enlarged cardiac silhouette. Which of the following EKG findings is fairly specific for his condition?
. Electrical alternans
. Prolonged 'PR' interval
. Presence of 'delta' wave
. Presence of 'F' waves
. New-onset right bundle branch block
28) A 70-year-old patient presents to the ER with a 3-hour history of intensive retrosternal chest pain that radiates to the interscapular area. He states that he has never experienced this pain before. His past medical history is significant for a 20-year history of hypertension and a 10-year history of diabetes mellitus, type 2. His current medications include enalapril and hydrochlorothiazide. He does not smoke or consume alcohol. His vital signs are BP 180/110 mmHg in the right arm and 178/110 mmHg in the left arm, PR 85/min and RR 18/min. The physical examination revealed an early decrescendo-type diastolic murmur at the left sternal border. The EKG is normal. Which of the following is the best next step in the management of this patient?
. Aortography
. Magnetic resonance imaging
. CK MB and troponin T levels
Transesophageal echocardiography
. Ventilation/perfusion scanning
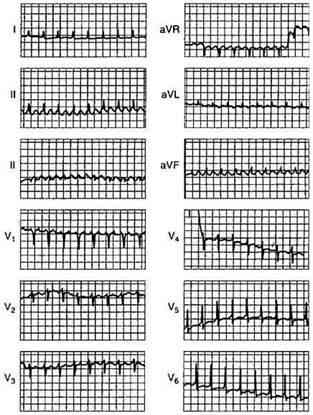
29) A 61-year-old woman was on her way to the grocery store when she started feeling chest pressure in the center of her chest. She became diaphoretic and felt short of breath. On arrival to the ED by EMS, her BP is 130/70 mmHg, HR is 76 beats per minute, and oxygen saturation is 98% on room air. The nurse gives her an aspirin and an ECG is performed as seen below. Which of the following best describes the location of this patient’s myocardial infarction (MI)?
. Anteroseptal
. Anterior
. Inferior
. Lateral
. Posterior
30) A 15-year-old male presents to your office on the advice of his football coach. The patient started playing football this year and suffered a syncopal episode at practice yesterday. He reports that he was sprinting with the rest of the team and became lightheaded. He lost consciousness and fell to the ground, regaining consciousness within one or two minutes. He suffered no trauma during the event. He has no prior history of head injury or recent illness. He has had no prior episodes of syncope. The patient is adopted and family history unavailable. Physical examination is unremarkable. What is the best course of action regarding this patient’s syncopal episode?
. Perform an ECG and echocardiogram. The patient may not return to competitive sports until results are available
Perform an ECG. The patient may not return to competitive sports until results are available
. Reassurance. The patient may return to competitive sports provided he increases his water consumption during practice times
. Perform an ECG. The patient may return to competitive sports pending the results
. Reassurance. The patient may return to competitive sports with no restrictions
31) A 42-year-old man develops shortness of breath (SOB) and chest pain 7 days after an open cholecystectomy. His blood pressure is 145/86 mmHg, pulse is 120/min, respirations 24/min, and oxygen saturation of 97%. Pulmonary embolism is clinically suspected. Which of the following is the most common ECG finding of pulmonary embolism?
A deep S wave in lead I
Depressed ST segments in leads I and II
Prominent Q wave in lead I, and inversion of T wave in lead III
Sinus tachycardia
Clockwise rotation in the precordial leads
32) A 32-year-old woman presents to the ED with a persistent fever of 101°F over the last 3 days. The patient states that she used to work as a convenience store clerk but was fired 2 weeks ago. Since then, she has been using drugs intravenously daily. Cardiac examination reveals a heart murmur. Her abdomen is soft and nontender with an enlarged spleen. Chest radiograph reveals multiple patchy infiltrates in both lung fields. Laboratory results reveal white blood cells (WBC) 14,000/μL with 91% neutrophils, hematocrit 33%, and platelets 250/μL. An ECG reveals sinus rhythm with first-degree heart block. Which of the following is the most appropriate next step in management?
. Order a monospot test and recommend that the patient refrain from vigorous activities for 1 month
. Obtain four sets of blood cultures, order a TTE, and start antibiotic treatment
. Administer isoniazid (INH) and report the patient to the Department of Health
. Administer a nonsteroidal anti-inflammatory drug (NSAID) and inform the patient she has pericarditis
. Order a Lyme antibody and begin antibiotic therapy
33) An elderly man presents to the emergency department with chest pain. He has a history of stable angina and recent onset diabetes mellitus, but now the chest pain comes on with less exertion and takes longer to go away. An ECG and cardiac enzymes are ordered. If this man has unstable angina, what are the expected findings on ECG and cardiac enzyme testing?
Low voltage ECG and elevated cardiac enzyme levels
Delta waves on the ECG and elevated cardiac enzyme levels
ST-segment depressions on ECG and normal cardiac enzyme levels
No changes on ECG and elevated cardiac enzyme levels
ST-segment elevations with Q waves and normal cardiac enzyme levels
34) A 64-year-old white man with type 2 diabetes mellitus presents to the emergency department after “passing out.” While climbing the stairs, he felt dyspneic and lost consciousness as he reached the top. Before the event he experienced no palpitations or change in vision. When he awoke he felt alert and called for help immediately. He reports dyspnea on exertion for the past year. He has no history of chest pain, seizures, or recent illnesses. Medications include calcium and vitamin D supplements, glyburide, and synthroid. He is allergic to penicillin. Family history is noncontributory. He drinks wine socially and does not smoke or use illicit substances. His blood pressure is 136/92 mmHg, heart rate is 88/min, respiratory rate is 14/min, and temperature is 36.5°C (97.7°F). Physical examination reveals a systolic crescendodecrescendo murmur best heard in the second right intercostal space with a soft S2. ECG shows nonspecific ST-segment changes and left ventricular hypertrophy with a normal heart rate and rhythm. Which of the following interventions will most likely reveal the cause of this syncopal event?
Electroencephalography
ECG
Exercise stress test with echocardiogram
ECG Echocardiography
Sublingual nitroglycerin and serial cardiac enzymes
35) A 70-year-old man comes to his primary care physician for his annual check-up. He has a history of hypertension, hyperlipidemia, and coronary artery disease, and had coronary artery bypass grafting 6 years ago. On examination the physician notes a right carotid bruit. Which of the following is the most appropriate next step?
Carotid endarterectomy
Carotid duplex ultrasound
Referral to a neurologist
ECG
Transthoracic echocardiography
36) A 62-year-old man with coronary artery disease (CAD) presents with presyncope. His physical examination is normal except for bradycardia (pulse 56 beats/min) and an irregular pulse. The electrocardiogram (ECG) shows Wenckebach’s type atrioventricular (AV) block. Which of the following are you most likely to see on the ECG?
Progressive lengthening of the PR interval
Progressive PR shortening
Dropped beat after PR lengthening
Tachycardia
Fixed 2:1 block
37) A 36-year-old woman presents to the ED with sudden onset of left-sided chest pain and mild shortness of breath that began the night before. She was able to fall asleep without difficulty but woke up in the morning with persistent pain that is worsened upon taking a deep breath. She walked up the stairs at home and became very short of breath, which made her come to the ED. Two weeks ago, she took a 7-hour flight from Europe and since then has left-sided calf pain and swelling. What is the most common ECG finding for this patient’s presentation?
Right-axis deviation
S1Q3T3 pattern
Right-atrial enlargement
Atrial fibrillation
Tachycardia or nonspecific ST-T–wave changes
38) A 70-year-old man has dyspnea, orthopnea, and paroxysmal nocturnal dyspnea. He has generalized cardiomegaly and pulmonary and systemic venous hypertension. The ECG is shown in Fig.What is the cardiac rhythm?
ii
Ectopic atrial tachycardia
Atrial flutter with 2:1 AV conduction
Supraventricular tachycardia
Sinus tachycardia
Atrial fibrillation with rapid ventricular response
39) Yesterday you admitted a 55-year-old white male to the hospital for an episode of chest pain, and you are seeking to rule out MI plus assess for any underlying coronary artery disease. The patient tends to be anxious about his health. On admission, his lungs were clear, but his heart revealed a grade 1/6 early systolic murmur at the upper left sternal border without radiation. Blood pressure readings have consistently been in the 140/90 mmHg to 150/100 mmHg range. Cardiac enzymes are normal. A resting ECG shows only left ventricular hypertrophy with secondary ST-T changes (“LVH with strain”). Why would a treadmill ECG stress test not be an appropriate test in this patient?
Increased risk associated with high blood pressure readings
Anticipated difficulty with the patient’s anxiety (ie, he might falsely claim chest pain during the test)
The presence of LVH with ST-T changes on baseline ECG
Concern about the heart murmur, a relative contraindication to stress testing
Concern that this represents the onset of unstable angina with unacceptable risk of MI with stress testing
40) A 67-year-old male presents to your office after community ultrasound screening revealed an aortic aneurysm measuring 3.0 x 3.5 cm. Physical examination confirms a palpable, pulsatile, nontender abdominal mass just above the umbilicus. The patient’s medical conditions include hypertension, hyperlipidemia, and tobacco use. What is the best recommendation for the patient to consider?
Surgery is indicated except for the excess operative risk represented by the patient’s risk factors
Watchful waiting is the best course until the first onset of abdominal pain
Serial follow-up with ultrasound, CT, or MRI is indicated, with the major determinant for surgery being aneurysmal size greater than 5 to 6 cm
Serial follow-up with ultrasound, CT, or MRI is indicated, with the major determinant for surgery being involvement of a renal artery
Unlike stents in coronary artery disease, endovascular stent grafts have proven unsuccessful in the management of AAAs
41) A 67-year-old male presents to your clinic to establish primary care; he is asymptomatic. He has a history of hypertension for which he takes hydrochlorothiazide. His father had a myocardial infarction at age 62. The patient smoked until 5 years ago, but has been abstinent from tobacco since then. His blood pressure in the office today is 132/78 mmHg. Aside from being overweight, the remainder of the physical examination is unremarkable. Which of the following preventive health interventions would be most appropriately offered to him today?
Lipoprotein assay to evaluate coronary heart disease risk
Carotid ultrasound to evaluate for carotid artery stenosis
Exercise (treadmill) stress testing to evaluate for coronary artery disease
Abdominal ultrasound to evaluate for aortic aneurysm
Homocysteine level to evaluate coronary heart disease risk
42) You are called by a surgical colleague to evaluate a 54-year-old woman with ECG abnormalities one day after a subtotal thyroidectomy for a toxic multinodular goiter. Her only medication is fentanyl for postoperative pain control. The patient denies any history of syncope, and has no family history of sudden cardiac death. Physical examination is unremarkable except for a clean postoperative incision at the base of the neck. Her ECG is reproduced below. What is the best next step in evaluation and management of this patient?

oo

Administration of intravenous magnesium sulfate
Measurement of serum ionized calcium
Stat noncontrast CT scan of the brain
Formal auditory testing
Reassure the patient that her ECG is normal for a woman her age
43) An 81-year-old man is hospitalized for acute onset of shortness of breath and lower extremity edema. Although he lives by himself, it is very difficult for him to move around his apartment without experiencing fatigue. He has not seen his physician in years but was told in the past that he had high blood pressure. On physical examination his jugular venous pulse is palpated 9 cm above his sternal notch, inspiratory crackles are heard at his lung bases, and there is 3+ lower extremity edema. Which of the following will confirm the most likely diagnosis?
Cardiac angiography
Echocardiography
Endomyocardial biopsy
Electrocardiogram
X-ray of the chest
44) A 58-year-old man with no prior cardiac history presents with retrosternal chest pain starting at rest and lasting 30 minutes. The pain radiates to the left arm and is associated with diaphoresis and dyspnea. His blood pressure is 150/90 mmHg, pulse 100/min, the heart sounds are normal, and the lungs are clear to auscultation. Which of the following is the next most appropriate investigation?
CXR
CT scan—chest
Cardiac troponin
ECG
Myocardial perfusion imaging
45) A 58-year-old man is brought to the ED for a syncopal episode at dinner. His wife states that he was well until she found him suddenly slumping in the chair and losing consciousness for a minute. The patient recalls having some chest discomfort and shortness of breath prior to the episode. His rhythm strip, obtained by EMS, is shown below. Which of the following best describes these findings?
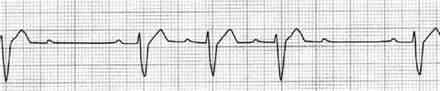
pp
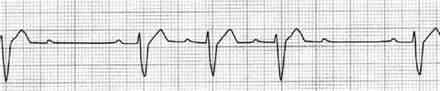
Mobitz type II
Mobitz type I
Atrial flutter with premature ventricular contractions (PVCs)
First-degree atrioventricular (AV) block
Sinus bradycardia
46) A 58-year-old man is undergoing cardiac catheterization for evaluation of chest pain symptoms. He is worried about the risks, and as part of obtaining informed consent, you advise him about the risks and benefits of the procedure. Which of the following aspects of angiography is true?
It is considered noninvasive
It is contraindicated in the presence of cyanosis
It may cause renal failure
It is generally performed with cardiopulmonary bypass
It requires carotid artery puncture
47) A 50-year-old man comes in for his annual check-up. There is a swelling on his left eyelid, which he casually acknowledges by saying that it has appeared "on-and-off for the past 2 years." It initially starts as a painful lesion which regresses with hot compresses, but then eventually reappears. On examination of his left eye, you note a nodular, painless, rubbery lesion on the eyelid without any discharge, redness or other abnormalities. What is the best next step in the management of his eye lesion?
Incision and curettage
. Anti-staphylococcal antibiotics
. Frequent hot compresses
. Direct steroid injection
. Histopathological examination
48) A 60-year-old male farmer presents to the office for the evaluation of a slightly painful ulcer on the top of his lower lip. The ulcer has not healed since he first noticed it three months ago. He has always been healthy and denies any sexual activity during the past year. He is afebrile. Physical examination shows a 3x7 mm, partially encrusted ulcer in the vermilion zone near the moist line (mucocutaneous junction) of the lower lip, surrounded by a 6 x 12 mm area of induration. There are no palpable submental or submandibular lymph nodes. The remainder of the physical examination is unremarkable. Complete blood count and differential are normal. Biopsy of the ulcer will most likely to show:
. Granulomatous inflammation
. Invasive clusters of spindle cells surrounded by palisaded basal cells
. Shallow fibrin-coated ulceration with an underlying mononuclear infiltrate
. Invasive cords of squamous cells with keratin pearls
. Giant cells in a Tzanck preparation
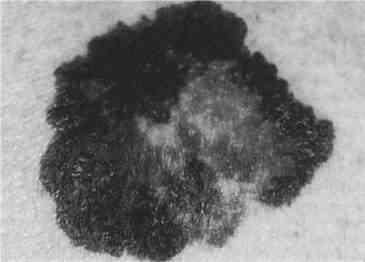
49) A 65-year-old male comes to the office on a hot summer afternoon. He complains of blisters and intense itching all over his body for the past 2 days. He has been having "itchy red swelling all over" for the past 2 months, which he thinks is due to the summer heat. His pulse is 82/min, blood pressure is 140/80 mmHg, respirations are 14/min, and temperature is 36.8°C (98.4°F). On examination, lesions are seen on both normal and erythematous skin over flexural areas of the groin, axilla and legs. An image of one of these lesions is shown below. Which of the following is most likely seen with this patient's condition? 

. IgG and C3 deposits at the dermal-epidermal junction
. IgG deposits intercellularly in the epidermis
. C3 at the basement membrane zone
. IgG deposits in a linear band at the dermal-epidermal junction
. Intradermal edema with leukocyte infiltration
50) A 30-year-old black female has a 2-month history of non-productive cough and a painful skin eruption in the lower extremities. She denies fever or weight loss. Physical examination shows several non-tenders raised plaques around the nares and scattered similar plaques around the base of the neck. In the lower extremities she has several erythematous tender non-ulcerated nodules, measuring up to 4 cm in diameter. Chest x-ray reveals bilateral hilar adenopathy and a streaky interstitial density in the right upper lobe. What is the best way to establish a histological diagnosis?
. Incisional biopsy of one of the lower extremity nodules
. Punch biopsy of one of the plaques on the neck
. Mediastinoscopy and biopsy of one of the hilar or mediastinal nodes
. Sputum studies for AFB and fungi
. Serum angiotensin-converting enzyme assay
51) A 72-year-old woman presents with pruritus for the past 6 weeks. She is careful to moisturize her skin after her daily shower and uses soap sparingly. She has never had this symptom before. The itching is diffuse and keeps her awake at night. Over this time she has lost 15 lb of weight and has noticed diminished appetite. She has previously been healthy and takes no medications. Physical examination shows no evidence of rash; a few excoriations are present. She appears fatigued and shows mild temporal muscle wasting. The general examination is otherwise unremarkable. What is the best next step in her management?
Oral antihistamines
. Topical corticosteroids
. Skin biopsy at the edge of one of the excoriations
. Psychiatric referral for management of depression
. Laboratory testing including CBC, comprehensive metabolic panel, and thyroid studies
52) A 25-year-old female with blonde hair and fair complexion complains of a mole on her upper back. The lesion is 8 mm in diameter, darkly pigmented, and asymmetric, with an irregular border (see illustration below). Which of the following is the best next step in management?
vv
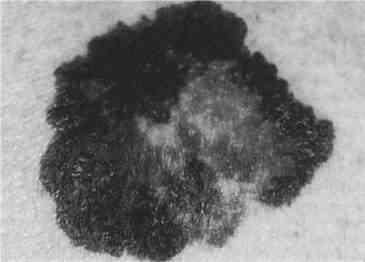
. Follow the lesion for any evidence of growth
. Tell the patient to avoid sunlight
. Obtain full-thickness excisional biopsy
. Obtain metastatic workup
. Obtain shave biopsy
53) A 39-year-old male with a prior history of myocardial infarction complains of yellow bumps on his elbows and buttocks. Yellow-colored cutaneous plaques are noted in those areas. The lesions occur in crops and have a surrounding reddish halo. Which of the following is the best next step in evaluation of this patient?
. Lipid profile
. Biopsy of skin lesions
. Chest x-ray
. Uric acid level
. Liver enzymes
54) A 20-year-old white man notes an uneven tan on his upper back and chest. On examination, he has many circular, lighter macules with a barely visible scale that coalesce into larger areas. Which test is most likely to establish the diagnosis?
. Potassium hydroxide (KOH) microscopic examination
. Punch biopsy
. Serological test for syphilis
. Dermatophyte test medium (DTM) culture for fungus
. Tzanck smear
55) A 25-year-old postal worker presents with a pruritic, nonpainful skin lesion on the dorsum of his hand. It began like an insect bite but expanded over several days. On examination, the lesion has a black, necrotic center associated with severe local swelling. The patient does not appear to be systemically ill, and vital signs are normal. Which of the following is correct?
. The patient has been bitten by Loxosceles reclusa, the brown recluse spider
. The lesion is ecthyma gangrenosum, and blood cultures will be positive for Pseudomonas aeruginosa
. The patient has the bubo of plague
A skin biopsy should be performed and Gram stain examined for gram-positive rods
. The patient has necrotizing fasciitis and needs immediate surgical debridement
56) A 25-year-old who has been living in Washington, DC, presents with a diffuse vesicular rash over his face and trunk. He also has fever. He has no history of chickenpox and has not received the varicella vaccine. Which of the following information obtained from history and physical examination suggests that the patient has chickenpox and not smallpox?
. Vesicular lesions are concentrated on the trunk
. There are vesicular lesions on the palms and soles
. All lesions are at the same stage of development
. The rash is most prominent over the face
. The patient experienced high fever several days prior to the rash
57) A 68-year-old man complains of several blisters arising over the back and trunk for the preceding 2 weeks. He takes no medications and has not noted systemic symptoms such as fever, sore throat, weight loss, or fatigue. The general physical examination is normal. The oral mucosa and the lips are normal. Several 2 to 3 cm bullae are present over the trunk and back. A few excoriations where the blisters have ruptured are present. The remainder of the skin is normal, without erythema or scale. What is the best diagnostic approach at this time?
. Trial of corticosteroids
. Culture of vesicular fluid for herpes viruses
. Biopsy of the edge of a bulla with some surrounding intact skin
. CT scan of the chest and abdomen looking for occult malignancy
. Combination of oral H1 and H2 antihistamines
58) A 49-year-old African-American male comes to the office and complains of headaches which have been worsening for the last three months. His other complaints include diffuse joint pains, pain on the lateral half of his right hand, difficulty getting his wedding ring out due to finger swelling, and difficulty holding and gripping objects with his right hand. His past medical history is significant for hypertension, which has not been controlled well despite compliance with medications, very low salt diet, and regular exercise. His current medications are amlodipine, lisinopril, and hydrochlorothiazide. His blood pressure is 146/98 mmHg, pulse is 90/min, temperature is 36.7°C (98°F) and respirations are 14/min. His facial features appear coarse when compared to his driver's license photo, which was taken three years ago. His palms are sweaty and have a doughy feel. His skin is oily. There are multiple skin tags, particularly around his neck area. Hand examination reveals positive Tinel's and Phalen's sign. Which of the following will be the most helpful in confirming the clinical diagnosis?
. Performing TRH stimulation test
. Measuring fasting growth hormone levels
. Measuring growth hormone following an oral glucose load
. MRI of his pituitary gland
. Measuring insulin-like growth factor (IGF-1) level
59) A 54-year-old male comes to the office for follow-up care of his foot ulcer. He has no complaints regarding the ulcer, but he has recently become polyuric and polydipsic. Fasting blood work reveals elevated glucose levels. He is prescribed oral hypoglycemics, and counseled on self-monitoring at home. On his next follow-up visit, the patient proudly states that he has been "very compliant" with his medications, and that his glucose levels are "always well-controlled." Which of the following is the best way to determine whether this patient is telling the truth?
. Fa sting urine glucose
. Random blood glucose
. Serum insulin levels
Glycosylated haemoglobin
. Serum C-peptide levels
60) A 48-year-old white male complains of generalized bone pain after undergoing bowel surgery for inflammatory bowel disease. His pain is more severe at the lower spine, pelvis, and lower extremities. Examination shows tenderness over the lower spine, pelvis, and lower extremities. Proximal muscle weakness is noted. X-rays of the lumbar spine show decreased bone density with blurring of the spine. X-rays of the femoral neck show pseudofractures, bilaterally. Which of the following lab abnormalities is consistent with this patient's diagnosis?
Increased serum calcium, low serum phosphate, increased serum parathyroid hormone
Low serum calcium, low serum phosphate, increased serum parathyroid hormone
. Low serum calcium, increased serum phosphate, low serum parathyroid hormone
. Normal serum calcium, normal serum phosphate, normal serum parathyroid hormone
. Increased serum calcium, increased serum phosphate, low serum parathyroid hormone
61) A 24-year-old white female is brought to the emergency department (ED) by her mother due to altered mental status. According to her mother, she suffered from viral gastroenteritis 4 days ago. Since then, she has been on oral fluids. Over the past 2 days, her condition had been deteriorating, but she kept refusing admission to the hospital. Her past history is not significant, except for excessive thirst, water intake and weight loss over the past two months. Her blood pressure is 100/56 mmHg, pulse is 120/min (regular and weak), temperature is 37.2°C (99°F), and respirations are 28/min (rapid and deep). Pulse oximetry is 94% on room air. She is arousable and moves all her extremities. Her mucous membranes are very dry. Her neck is supple. The chest is clear on auscultation. Which of the following is the most appropriate next step in management?
. Fingerstick glucose
. Obtain electrocardiogram
. Intubate the patient
. Obtain arterial blood gases
. Obtain CT scan of head
62) A 21-year-old female has a several month history of easy fatigability and palpitations. She also complains of excessive sweating. She follows a strict, low calorie diet in order to lose weight. Her blood pressure is 120/70 mmHg and her heart rate is 100/min. Her BMI is 19kg/m2 Thyroid function testing reveals the following findings: TSH decreased, Total T4 high, Total T3 high. Radioiodine uptake is diffusely decreased over the thyroid gland. Which of the following is the most likely pathologic finding on biopsy of this woman's thyroid gland?
. Diffuse follicular hyperplasia
. Dense lymphocytic infiltrate
. Follicular atrophy
. Orphan Annie nuclei
. Papillary neoplastic growth
63) A 45-year-old white male patient presents for the evaluation of high blood pressure. He also complains of polyuria, polydipsia and fatigue. His past medical and family histories are unremarkable. He does not use tobacco, alcohol or drugs. His blood pressure is 180/100mmHg. Physical examination shows no abnormalities. Laboratory studies show low serum potassium and high plasma aldosterone levels. CT scan of the abdomen shows a small, right adrenal mass. Which of the following additional findings is most likely to be present in this patient?
. Metabolic acidosis
. Edema
. Episodes of high blood pressure
. Increased plasma renin activity
. Mild hypernatremia
64) A 28-year-old white female presents to the office for the evaluation of goiter. She denies any recent change in appetite or weight, diarrhea, constipation, heat or cold intolerance, dyspnea and hoarseness. Her menses are normal and regular. Examination shows a symmetrically enlarged, non-tender, firm and rubbery thyroid gland. There is no lymphadenopathy. The rest of the physical examination is normal. Laboratory studies reveal an elevated serum TSH level with normal T4 and T3 levels. Serological testing for Hashimoto's thyroiditis is ordered. Which of the following are the most prevalent antibodies in patients with Hashimoto's thyroiditis?
. Anti-thyroid peroxidase antibodies
. Anti-smooth muscle antibodies
. Thyroid-stimulating immunoglobulins
. TSH-receptor blocking antibodies
. Anti-mitochondrial antibodies
65) An elderly woman is brought to the emergency department (ED) by her husband in a semiconscious state. According to her husband, she had complained of feeling unwell "over the past day or so”, but he only became very concerned when he returned from work today and found her very drowsy and difficult to arouse. Her past medical history is significant for diabetes with diabetic nephropathy and hypothyroidism. Her medications include thyroxine, metformin, gliclazide and lisinopril. Her temperature is 37.3°C (99°F), blood pressure is 110/65 mmHg, and pulse is 90/min. GCS = 13/15 (Motor 6, Verbal4, Eye3). She is confused and not oriented to time or place, but is able to follow commands. Physical examination reveals dry mucous membranes and decreased skin turgor. Neurological examination reveals weakness in the left arm. The rest of the examination is unremarkable. Urinalysis shows: Blood negative, Glucose +++, Ketones negative, Protein +, Leukocyte esterase negative, Nitrites negative, WBC 10-20/HPF. Which of the following is the most appropriate next investigation to perform?
. MRI of head
. Head CT
. Echocardiogram
. Blood glucose
. Blood cultures
66) A 45-year-old female comes to the office for the evaluation of excessive hair growth over her face and body. Her hirsutism rapidly developed over a period of 3 months. She underwent bilateral tubal ligation 4 years ago. Her menstrual cycles were regular in the past, but for the last 3 months, she has not had a menstrual period. She denies any hot flashes or vaginal discomfort. On physical examination, her height is 5'2" (169 cm) and weight is 140 lbs (63.5kg). A large amount of coarse terminal hair is noted on her face, chest and lower abdomen. She appears masculine and has an enlarged clitoris. There is significant temporal balding. Which of the following is the most appropriate next step in management?
. Serum testosterone and DHEAS
. Serum LH and FSH
. Serum 17- hydroxyprogesterone levels
. CT scan of abdomen
. Selective adrenal and ovarian vein samplings
{"name":"DES 3 ep6", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"234) A 24-year-old man with chronic schizophrenia is brought to the emergency room after his parents found him in his bed and were unable to communicate with him. On examination, the man is confused and disoriented. He has severe muscle rigidity and a temperature of 39.4°C (103°F). His blood pressure is elevated, and he has a leucocytosis. Which of the following is the best first step in the pharmacologic treatment of this man?, 235) A 30-year-old man is brought to the emergency room after he was found wandering on the streets with no shoes on in the middle of winter. He is admitted to the inpatient psychiatric unit and stabilized on antipsychotic medication. Looking at past records, his psychiatrist notes that he is repeatedly noncompliant with his medication postdischarge, and each time he relapses within 6 months. Which of the following medications is the best one for this patient to be maintained on?, 236) A 23-year-old woman was diagnosed with schizophrenia after a single episode of psychosis (hallucinations and delusions) that lasted 7 months. She was started on a small dose of olanzapine at the time of diagnosis, which resulted in the disappearance of all her psychotic symptoms. She has now been symptom free for the past 3 years. Which of the following treatment changes should be made first?","img":"https://www.quiz-maker.com/3012/images/ogquiz.png"}
More Quizzes
Oedipus Rex
1050
How to save world
100
NAIDOC Week Daily Quiz #3
840
Ytgyrg
210
Free: Which Transform Fails to Map Rectangle?
201026796
NLE Practice Exam: Free Clinical Scenario for Nurses
201033202
What State Am I In - Find Your Perfect Match
201029424
Test Your Ionic and Covalent Bonding Skills - Free
201028480
Capstone Project Synthesis
15819865
Master Various Types of Printers - Free Challenge
201068638
Free Ready Mathematics Unit 2 Assessment Key
201021781
Free Third Law of Motion Worksheet
201027891