DES 3 ep 5
133) A 54-year-old male presents to the office with several months history of hand tremors that are unresponsive to over-the-counter medication. The tremors always become worse when he is in public places. Sometimes, the hand tremors are so bad that he is unable to grasp. He denies trauma, fever, loss of muscle function or any prior stroke. His past medical history is significant for vague abdominal pains, the cause of which was never found. He is given some medication. A month later, he comes back and says, "The tremor is gone, but now I have colicky abdominal pain, confusion, headaches, hallucinations and dizziness." What is the drug that caused this patient's new symptoms?
. Alcohol
. Propranolol
. Diazepam
. Primidone
. Lithium
134) A 44-year-old male has been abusing drugs for many years. Recently he started using the agent MPTP and he now presents to you in the ER. He says that he is not feeling well and wonders what is going on. He says he has a persistent tremor in his fingers and his body has become rigid. At times has had difficulty in walking. The CT scan of his brain is normal and all the blood work is within normal limits. You decide to treat him. Two years later you see him and he tells you that his symptoms have improved. He also noticed that he had a significant relief from the recurrent and persistent upper respiratory tract viral infections that he was so prone to. The agent you gave him was?
. Bromocriptine
. Levodopa-Carbidopa
. Benztropine
. Amantadine
. Acyclovir
135) A 5-year-old boy is brought to the office by his frustrated mother because, "he just can't seem to concentrate!" He has episodes that are characterized by frequent blinking and indifference to his surroundings. He does not remember anything after an episode. An episode does not last long, but he usually has 50-80 "daydreaming accidents" daily. His school performance has deteriorated lately, and his teacher has complained about his decreased concentration. Which of the following is the drug of choice for this patient's condition?
. Phenytoin
. Carbamazepine
. Phenobarbital
. Ethosuximide
. Lamotrigine
136) A 27-year-old white female comes to the office and complains of ptosis, diplopia and difficulty in chewing. Her symptoms worsen in the evening. She is asymptomatic when she wakes up in the morning. She denies any sensory complaints or limb weakness. The Tensilon test is positive. Serological testing shows positive acetylcholine receptor antibodies. Which of the following is the best treatment to induce remission and provide long-term benefits in this patient?
. Pyridostigmine
. Prednisolone
. Plasmapheresis
. Intravenous immunoglobulins
. Thymectomy
137) A 62-year-old male is brought to the emergency department with a chief complaint of weakness. He says that he was walking his dog 1 hour ago when he began to limp and noticed some weakness in his left arm. His past medical history is significant for hypertension treated with hydrochlorothiazide, and type II diabetes mellitus managed with metformin. He denies nausea, vomiting, chest pain, fever or chills. He does note occasional palpitations and tension headaches at baseline. On physical examination, his blood pressure is 170/95 mmHg and his heart rate is 76/min and regular. His blood glucose level is 190 mg/dl and his HbA1c is 7.6%. The neurological examination is significant for profound left-sided weakness and an up going Babinski reflex on the left. Non-contrast head CT is negative for any intracranial bleed. Which of the following is most likely to affect his chance of neurological recovery?
. Insulin for tight glucose control
. Labetalol
. Fibrinolytic
. Aspirin
. Heparin
138) A 62-year-old female is brought in by EMS due to a severe right-sided headache, nausea and eye pain. She was fixing a light bulb, when she suddenly felt pain in her right eye. She decided to rest, but the eye pain only got worse. In the next few minutes, she developed loss of vision, photophobia and redness in the same eye. She took medications to relieve the accompanying headache, but the eye pain persisted. She denies any trauma. Her past medical history is significant for diabetes and hypertension. She appears to be in intense pain with bouts of nausea. Her right eye is red, with conjunctival flushing and visual acuity of 20/200. Her right pupil is mid-dilated and non-reactive to light. The same eye feels hard on palpation. The one treatment that should be avoided in this patient is:
. Mannitol
. Acetazolamide
. Timolol
. Pilocarpine
. Atropine
139) A 65-year-old male comes to the emergency department because of a sudden, painless loss of vision in his right eye that occured a half an hour ago. Five hours ago, he experienced a similar but transient loss of vision in the same eye, which lasted for five minutes. He has hypertension, diabetes, hypercholesterolemia, and peripheral vascular disease. He had an anterior wall myocardial infarction six years ago. His medications include glyburide, captopril, atenolol, simvastatin and aspirin. His temperature is 36.7°C (98.0°F), respirations are 16/min, pulse is 88/min, and blood pressure is 146/88 mmHg. Examination of the right eye reveals visual acuity of 20/60 and subtle retinal whitening. A right carotid bruit is heard. Which of the following is the most appropriate next step in the management of this patient?
. Acetazolamide IV
. Ocular massage and high flow oxygen
. Instillation of topical beta blocker
. Administer systemic steroids
. Administer thrombolytics
140) A 33-year-old man presents with a 1-day history of localized, small swelling along the margin of the upper eyelid. He feels pain, which does not seem to come from the conjunctival surface. He has a 10-pack year smoking history. He occasionally drinks alcohol. He is sexually active, and does not use condoms regularly. He is worried about the swelling. What is the best next step in the management of this patient?
. Use warm compresses
. Incision and drainage
. Take biopsy of the lesion
. Incision and curettage
. Oral Penicillin
141) A 72-year-old man presents with right eye pain for 1 day. The patient has a history of diabetes, hypertension, and “some type of eye problem.” He does not recall the name of his eye problem or the name of his ophthalmic medication. However, he does remember that the eye drop has a yellow cap. Which class of ophthalmic medication is the patient taking?
. Antibiotic
β-Blocker
Mydriatic/cycloplegic agent
. Miotic
. Anesthetic
142) A 45-year-old woman presents with right eye pain and redness for 1 day. She has photophobia and watery discharge from the eye. She does not wear glasses or contact lenses and has no prior eye problems. On examination, the patient’s visual acuity is 20/20 in the left eye and 20/70 in the right eye. She has conjunctival injection around the cornea and clear watery discharge. On slit-lamp examination, the lids, lashes, and anterior chamber are normal. When fluorescein is applied, a branching, white-colored epithelial defect is seen. The remainder of the head examination is normal and the patient has no cutaneous lesions. Which of the following is the most appropriate treatment for this patient?
. Admission for IV antiviral agents
. Admission for intravenous (IV) antibiotics
Topical antiviral medication
. Topical steroids
. Immediate ophthalmology consultation
143) A 21-year-old man presents to the ED with a red eye. The patient complains of rhinorrhea and a nonproductive cough but has no eye pain or discharge. He also has no associated ecchymosis, bony tenderness of the orbit, or pain on extraocular eye movement. His vision is normal, extraocular movements are intact, and intraocular pressure (IOP) is 12. A picture of his eye is shown below. What is the most appropriate management of this condition?

jj

. Reassurance only
. Administer ophthalmic timolol
. Elevate patient’s head
Administer 1% atropine
. Call ophthalmology immediately
144) A 28-year-old mechanic with no past medical history presents to the ED after a small amount of battery acid was splashed in his right eye. He is complaining of extreme pain and tearing from his eye. Which of the following is the most appropriate next step in management?
. Call ophthalmology now
. Check visual acuity
. Irrigate with normal saline
. Check the pH of the tears
. Apply erythromycin ointment
145) A 33-year-old white female complains of repeated episodes of fever, malaise, chills, breathlessness and dry cough over the past 6 months. She says that each episode starts suddenly and lasts for several days. She otherwise has no significant past medical history and does not take any medications. There is no family history of lung disorders. She does not smoke cigarettes or drink alcohol. She has never been abroad, and has had no sick contacts. She breeds budgerigars (a small Australian parrot) as a hobby. Chest x-ray shows diffuse generalized haziness in both lower lung fields. Pulmonary function tests reveal reduced lung volumes and an FEV1/FVC ratio of 87%. PPD test is negative. Serology shows antibodies to budgerigar antigens. What is the best treatment for this disease?
. Inhaled beclomethasone
. Oral prednisolone
. Inhaled cromolyn
. Avoid exposure to birds
. Reassurance
146) A 44-year-old male is involved in a serious motor vehicle accident. He is admitted to the intensive care unit with multiple fractures and internal bleeding, and is placed on mechanical ventilation. Over the next two days, his oxygen saturation repeatedly drops below 90%, requiring gradual increases in the FiO2. On day three of his admission, the patient's chest x-ray, which was initially clear, shows bilateral fluffy infiltrates. He has no prior medical problems and does not take any medications. Skin examination reveals no rashes. Lab studies show: Hemoglobin 10.1 g/L, Platelets 160,000/mm3, Leukocyte count 13,500/mm3. Sputum cultures are negative. The ventilator settings are: FiO2 90%, Tidal volume 400 ml (body weight 60 kg), Respiratory rate 12/min, PEEP 5cmH2O. The patient's oxygenation continues to drop below 90%. Which of the following interventions would be best for improving the patient's oxygenation?
. Increase the tidal volume
Increase the respiratory rate
. Increase the intravenous fluids
. Increase the PEEP
. Administer packed red blood cells
147) A 65-year-old white man comes to the Emergency Room complaining of headache, insomnia, palpitations, and vomiting. His past medical history is significant for chronic obstructive pulmonary disease (COPD) treated with theophylline, ipratropium, and occasional albuterol. He had a puncture wound of the foot one week ago, and it is being treated effectively with amoxicillin-clavulanate and ciprofloxacin. For the past three days, his shortness of breath is worsening, and his primary care physician gave oral prednisone. His blood pressure is 150/80 mmHg and heart rate is 105/min with frequent ectopic beats. You suspect that drug toxicity may be responsible for this patient's complaints. Which of the following drugs is most likely responsible for his condition?
. Theophylline
. Ipratropium
. Ciprofloxacin
. Albuterol
. Steroids
148) A 67-year-old woman with a past medical history significant for hypertension, hypercholesterolemia, and type 2 diabetes calls 911 for severe shortness of breath. Her symptoms started 2 hours ago with chest pain and progressed rapidly to orthopnea and shortness of breath. Her blood pressure is 170/ 100 mmHg and heart rate is 120/min and regular. A third heart sound is present. Bilateral crackles are heard on chest auscultation. Her oxygen saturation is 78% with 40% inspired oxygen. She is intubated in the field by paramedics for progressive respiratory failure and is treated with nitrates and diuretics. After the initial resuscitation, breath sounds on the left side are markedly decreased. Which of the following is most likely to restore breath sounds to this hemithorax?
. Left-sided chest tube
. Left-sided needle thoracostomy
. Pericardiocentesis
. Endotracheal tube withdrawal
. Tidal volume increase
149) A 55-year-old chronic smoker comes to you because of worsening shortness of breath. He says that he has had lung problems due to smoking for the past five years. He has hypertension controlled with hydrochlorothiazide, and type 2 diabetes mellitus, controlled with diet. He has smoked two packs of cigarettes daily for 25 years. Physical examination shows bilateral decrease in breath sounds with prolonged expiration and wheezing in both the lung fields. He is hypoxic on room air. An x-ray film of the chest shows hyperinflation of both lung fields. His pulmonary function tests showed moderate obstructive disease, with very little bronchodilator response. The patient is started on bronchodilators. He is being considered for home oxygen therapy. Which of the following is a criterion for initiating home oxygen in such patients?
. Worsening of shortness of breath
. Patients with SaO2 less than 88% on room air
. Patients with SaO2 less than 92% on room air
. Patients with PaO2 1ess than 65 mmHg on room air
. Development of pulmonary osteoarthropathy
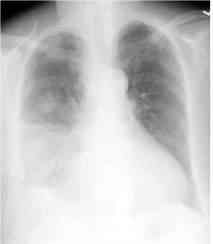
150) A 65-year-old white male who has a history of chronic obstructive pulmonary disease, congestive heart failure, and coronary artery disease presented with a three-day history of worsening shortness of breath, cough with yellowish expectoration, and fever. He is not on steroids and does not use oxygen at home. He takes ipratropium, albuterol, aspirin, digoxin, furosemide, metoprolol, and lisinopril. He lives at home with his wife. His temperature is 39.4°C (103°F), blood pressure is 110/70 mmHg, pulse is 110/min, and respirations are 24/min. He is saturating 88% on room air. He was started on 3-liters of oxygen to keep the saturations above 92%. The chest x-ray of the patient is shown below. What is the most appropriate next step in the management of this patient?
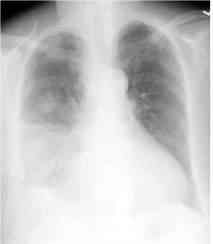
kk
. Admit the patient and give ampicillin
. Outpatient trimethoprim-sulfamethoxazole
. Admit the patient and start ciprofloxacin
. Admit the patient and start levofloxacin
. Admit the patient and start vancomycin
151) A 76-year-old male nursing home resident is hospitalized with confusion, fever and decreased oral intake. His past medical history is significant for type 2 diabetes mellitus, hypertension, osteoarthritis and gout. Blood cultures are positive for E coli. Despite antibiotic therapy, he slips into respiratory failure. He is intubated and placed on mechanical ventilation with an FiO2 of 70%, tidal volume of 500 ml and respiratory rate of 14/min. His current arterial blood gases are: pH 7.45, pO2 59 mmHg, pCO2 30 mmHg, HCO3 21 mEq/L. Which of the following is the best next step in managing this patient?
. Increase tidal volume
. Increase respiratory rate
. Add positive end-expiratory pressure
. Increase the fraction of inspired oxygen
. Decrease the fraction of inspired oxygen
152) A 45-year-old male with mild persistent asthma comes to you for a routine checkup. He is taking a low-dose beclomethasone inhaler daily and inhaled albuterol, as needed, for the last year. His past medical history is otherwise not significant. His family history is significant for diabetes mellitus type 2, hypertension and obesity. His blood pressure is 136/90 mmHg and his heart rate is 80/min. His BMI is 26 kg/m2. Which of the following is the most likely complication of chronic beclomethasone use in this patient?
. Cushing's syndrome
. Thrush
. Adrenal suppression
. Osteoporosis
. Purpura
153) A 56-year-old morbidly obese man twisted his ankle five days ago and has been bed-ridden since. Today he presents to the emergency department with acute-onset shortness of breath and chest tightness. His past medical history is significant for diabetes mellitus, hypertension, right knee osteoarthritis, and a deep venous thrombosis. His current medications are lisinopril, metoprolol, and metformin. His blood pressure is 110/60 mmHg and his heart rate is 110/min. A CT scan of the chest with contrast is consistent with pulmonary thromboembolism. Which of the following is the best treatment for this patient?
. Start both heparin and warfarin now, and stop heparin in 1-2 days
. Start heparin now, and in 5-6 days stop heparin and start warfarin
. Start heparin now and continue for 3-4 weeks
. Start heparin and warfarin now, and stop heparin in 5-6 days
. Start warfarin now and continue for at least 6 months
154) A 35-year old male presents to your office complaining of nocturnal wheezing and chest tightness for the past three months. He has also noticed new hoarseness, particularly in the morning. He has no history of bronchial asthma, hypertension or diabetes. He is a non-smoker but occasionally drinks alcohol. On examination, he is an obese male in no acute distress. His pulse is 84/min, blood pressure is 130/80 mmHg, and respirations are 16/min. His chest is clear to auscultation and percussion. Laryngoscopy reveals a red and inflamed posterior pharynx and larynx. Which of the following pharmacotherapies would be most helpful for this patient?
. Bedtime fluticasone inhaler
. Bedtime albuterol inhaler
. Oral omeprazole
. Oral theophylline
. Oral prednisone
155) A 38-year-old female comes to your office with a recent episode of hemoptysis. The symptoms started one week ago with malaise, throat pain and dry cough. The cough progressed becoming productive of yellowish sputum. She started noticing speckles of red blood in her sputum as of yesterday. Her past medical history is significant for peptic ulcer disease. She has a 5 pack-year smoking history, but she quit 10 years ago. Her temperature is 98°F (36.7°C), blood pressure is 130/80 mmHg and heart rate is 87/min. Physical examination reveals scattered bilateral wheezes. Chest X-ray shows clear lung fields. Which of the following is the most appropriate next step in management?
. CT scan of the chest
. Pulmonary function tests
. Observation
. Sputum Gram stain and culture
. Sputum cytology
156) A 34-year-old male presents to his physician's office for a routine health maintenance examination. He has a five-year history of bronchial asthma for which he uses an albuterol inhaler. He says that he uses the inhaler an average of two times per week during the day. In addition, he states that his asthma symptoms wake him from sleep approximately 3-4 times per month. He does not use tobacco, alcohol or illicit drugs. His family history is significant for asthma in his grandfather. Physical examination is unremarkable. Which of the following is the most appropriate next step in his management?
. Add inhaled corticosteroids
. Add long-acting beta-2 agonist inhaler
. Add oral prednisone
. Add oral theophylline
. Continue current medical regimen
157) A 19-year woman presents to her physician's office for a routine health maintenance examination. She notes experiencing occasional wheezing and breathlessness following aerobic exercise, but has no symptoms at other times of the day or night. Her medical history is otherwise significant for allergic rhinitis and acne, for which she uses topical benzoyl peroxide and erythromycin cream. She does not use tobacco, alcohol or illicit drugs. On physical examination, her vital signs are within normal limits and chest auscultation is unremarkable. Which of the following is the most appropriate next step in her management?
Beta-adrenergic agonists before exercise
. Daily oral steroids
. Daily oral theophylline
. Daily steroid inhalers
. Lpratropium inhalers before exercise
158) A 57-year-old male was involved in a motor vehicle accident and was immediately brought to the Emergency Room. He suffered minor head and neck injury, but was found to have a broken tibia. He underwent repair of the tibial fracture the following day. Five days later, he suddenly develops tachycardia and is tachypneic. He complains of increasing chest discomfort and has a syncopal episode. His blood pressure is 80/55 mmHg, pulse is 130/min, and respirations are 24/min. Pulse oximetry showed 82% on room air. Stat echocardiogram reveals obstruction in the main pulmonary artery. Which of the following choices is the most appropriate course of action?
. Heparin infusion
. Fibrinolytic therapy
. Inferior vena cava filter
. Embolectomy
. A CT scan of the lung
159) A 68-year-old female comes to the Emergency Room with increased shortness of breath and cough for 12 hours. She has a history of chronic obstructive pulmonary disease for the past 14 years and has been oxygen dependent for two years. Twelve hours ago, she felt unable to get her breath. She took two extra nebulizer treatments and used her as-needed inhaler with no relief of symptoms. She denies any fever, chills, sweating, nausea or vomiting, and hemoptysis. She rarely uses alcohol, but had smoked two packs/day for 45 years. She quit smoking about six years ago. Her medications include ipratropium, albuterol, multivitamins, and oxygen 2 liters/min by nasal cannula. She is a thin, frail female in moderate distress. Her temperature is 36.7°C (98°F), blood pressure is 110/65 mmHg, pulse is 110/min, and respirations are 28/min. Pulse oximetry shows 84% on 2 liters oxygen by nasal cannula. The patient is given oxygen, methyl prednisolone, aerosolized ipratropium, and albuterol; however, the patient remains dyspneic and bedridden. ABGs are ordered and the results show: pH 7.32, PCO2 60 mmHg, and PO2 52 mmHg on 4-liters O2. What is the next best step in the management of this patient?
. Increase oxygen by nasal cannula
. Decrease oxygen
. Noninvasive positive pressure ventilation
. Intubate and mechanically ventilate the patient
. Aminophylline
160) A 68-year-old male is hospitalized following an intracerebral hemorrhage. On hospital day 3, he develops redness, swelling, and tenderness of the left calf. There is no fever. Compression ultrasonography reveals a thrombus in the popliteal vein. Which of the following is the most appropriate next step in the management of this patient?
. Anticoagulation with heparin
. Thrombolytic therapy
. No treatment for his deep vein thrombosis
. Placement of an inferior vena cava filter
. Compression stockings
161) A 66-year-old man complains of exertional dyspnea that has progressed over the last two years. As a result, he has had to limit his physical activities to avoid becoming short of breath. He denies any significant chest pain, but does note having a recurrent cough productive of whitish sputum. His past medical history is significant for hypertension controlled with hydrochlorothiazide. He has a 40 pack-year smoking history. His family history is significant for a stroke in his mother. His blood pressure is 160/90 mmHg and his heart rate is 80/min. Physical examination reveals a mildly overweight patient in no acute distress. His anteroposterior chest diameter is markedly increased. Breath sounds are decreased bilaterally with scattered expiratory wheezes. Which of the following agents is most likely to reduce this patient's symptoms?
. Alpha-adrenergic blocker
. Beta-adrenergic blocker
. Dopamine agonist
Muscarinic antagonist
Alpha 2-adrenergic agonist
162) A 64-year-old male presents to the physician's office with increasing shortness of breath. He denies orthopnoea, paroxysmal nocturnal dyspnea, or chest pain. He was hospitalized for pneumonia four years ago but has otherwise been healthy. He has smoked one pack of cigarettes daily for the past 30 years. He does not take any medications. His temperature is 37.2°C (98.9°F), blood pressure is 124/76 mm Hg, pulse is 82/min and respirations are 16/min. Pulse oximetry reveals an oxygen saturation of 88%. On chest auscultation, breath sounds are diminished throughout, and the expiratory phase is prolonged. Heart sounds are regular and there are no murmurs or gallops. There is no peripheral edema or jugular venous distention. Laboratory studies show a hematocrit of 56% and WBC count of 6,700/mm3. Which of the following interventions will have the maximum impact on this patient's survival?
. Maintenance oral steroids
. Influenza and pneumococcal vaccinations
. Prophylactic antibiotics to reduce exacerbations
. Long-term supplemental oxygen therapy
. Long-term beta-blocker therapy
163) A 47-year-old male who has just returned from a cruise to the Bahamas presents to the hospital with a high-grade fever, productive cough and shortness of breath for the past two days. He also complains of frequent vomiting and diarrhea. He has no prior medical problems, does not take any medications, and denies using tobacco, alcohol or drugs. His temperature is 40°C (104°F), blood pressure is 110/65 mm Hg, pulse is 80/min, and respirations are 18/min. Lung examination reveals right lower lobe crackles. The abdomen is soft and non-tender. Chest x-ray demonstrates right lower lobe consolidation. Sputum Gram stain contains many neutrophils with no organisms. Which of the following antibiotics must be given to this patient?
. Vancomycin
. Clindamycin
. Amoxicillin
. Fluconazole
. Azithromycin
164) A 36-year-old female presented to the emergency room with fever and a productive cough. The physician on call suspected community acquired pneumonia and prescribed azithromycin for 5 days. After 5 days of treatment, she comes to your office with no improvement of her symptoms and complains of worsening foul smelling sputum. Further inquiry reveals that she had undergone an upper GI endoscopy 8 days ago for a long history of heartburn and suspected peptic ulcer disease. She also reports a history of manic-type bipolar disorder. In your office she has a blood pressure of 130/80 mm Hg, her pulse is 108/min, temperature is 38.7°C (101.6°F) and respirations are 26/min. Chest x-ray showed a right upper lobe infiltrate. Which of the following additional therapies would be most helpful for this patient's condition?
. Doxycycline
. Ciprofloxacin
. Clindamycin
. Trimethoprim-sulfamethoxazole
. Gentamicin+ ampicillin
165) A 45-year-old male comes to the emergency room complaining of shortness of breath that began 3 hours ago. He also has a nonproductive cough, a low-grade fever and right-sided chest pain that worsen with inspiration. He denies coughing up blood, wheezing, palpitations, leg pain or swelling of his lower extremities. He recently returned home from a trip to Singapore. He has a history of hypertension and diabetes mellitus. His takes fosinopril, metformin and glyburide. He doesn't use tobacco, alcohol or illicit drugs. His temperature is 98.0°F (36.6°C), blood pressure is 115/70 mmHg, pulse is 128/min, respirations are 32/min, and O2 saturation is 84% on room air. Physical examination shows a slightly obese man in acute respiratory distress. He is alert and cooperative without any cyanosis or jaundice. He has a slightly displaced apical impulse with a S4. Chest-x ray shows mild cardiomegaly with no infiltrates. EKG shows sinus tachycardia and left ventricular hypertrophy without ST-T wave changes. His arterial blood gas analysis shows pH 7.52, pCO2 30, pO2 55, HC03 22. What is the next best step in the management of this patient?
Pulmonary angiogram
. Lower extremity venous ultrasound
. Initiate heparin weight-based protocol
. Spiral CT scans of the chest
. Broad spectrum antibiotics
166) A 65-year-old male with oxygen-dependent chronic obstructive pulmonary disease, chronic atrial fibrillation, and depression comes into the Emergency Room, with symptoms of increased dyspnea and worsening cough pattern. His recent history had been significant for a gradual worsening of his baseline lung disease over the past month, which had been treated by his outpatient doctor with increased frequency of inhaled beta-agonist and azithromycin. This morning he had a severe shortness of breath that was unresponsive to "stacked" home nebulizer treatments. The ER physician notes that the patient is in moderate severe respiratory distress. His temperature is 37.2°C (99°F), blood pressure is 150/90 mmHg, pulse is 110/min, and respirations are 28/min. Accessory muscle use was noted. Lung exam shows diffuse rhonchi and wheezing. A pulse oximetry revealed an oxygen saturation of 80% on room air. His chest x-ray showed no new infiltrates. His WBC count is 7,000/cmm with normal differential. The ER physician had given nebulization, and the patient is on 5-liters of oxygen. Which of the following should also be considered in this patient?
. Gatifloxacin
. Methylprednisolone
. Clarithromycin
. N-acetylcysteine
. Aminophylline
167) A 32-year-old man presents to the emergency department with pain and swelling in the right leg. He was recently hospitalized for a right lower extremity deep venous thrombosis and discharged on warfarin. Today his INR is 1.12. Ultrasound reveals a right popliteal vein thrombosis extending into the deep femoral vein. What is the best initial management step for this patient?
. Increase warfarin dose for goal INR > 2.0
. Start intravenous unfractionated heparin
. Place inferior vena cava filter
. Initiate thrombolytic therapy
. Discontinue warfarin and reassure
168) A 50-year-old female comes into your office complaining of four-month history of dry cough. She denies dyspnea or hemoptysis. Past medical history is significant for hypertension, diabetes, and gout. Her current medications include enalapril, metformin, hydrochlorothia zide, and allopurinol. She does not smoke or consume alcohol. Her vital signs are BP 130/80 mmHg, HR 80/min, T 36.7°C (98°F) and RR 16/min. Physical examination is within normal limits. The best next step in the management of this patient is:
. Chest radiograph
. Reevaluation of drug therapy
. Barium esophagography
. Pulmonary function testing
. Bronchoscopy
169) A 45-year-old white man presents to your office complaining of daytime somnolence, increased fatigability, and morning headaches. He says that his wife complains that he snores loudly. He is not taking any medications and does not smoke or consume alcohol. His blood pressure is 145/90 mmHg and heart rate is 90/min. Physical examination reveals a well-nourished man with BMI = 31 kg/m2. What is the next best step in the management of this patient?
. A benzodiazepine to improve sleep
. Advise to sleep in supine position
. A thiazide diuretic for hypertension
. Weight reduction
. Tracheostomy
170) A 43-year-old previously healthy male is hospitalized for acute pancreatitis. On day 3 of his admission, he develops respiratory distress. He is transferred to the intensive care unit and intubated. His initial ventilator settings are: FiO2 0.8 (80%), Respiratory rate 10/min, Tidal volume 500 ml, PEEP 5 mm H20. Ten minutes after being intubated, the man's blood pressure is 110/70 mmHg and his heart rate is 90/min. His arterial blood gases are: pH 7.42, pO2 105 mmHg, pCO2 37 mmHg. Which of the following is the best next step in the management of this patient?
. Decrease the positive end expiratory pressure (PEEP)
. Decrease the tidal volume
. Decrease the FiO2
. Decrease the respiratory rate
Increase the respiratory rate
171) A 35-year-old male was involved in a motor vehicle injury and suffered serious chest trauma. A chest tube was placed for a hemothorax. 800 cc of blood was evacuated from the chest, and, after ten days, the patient was discharged home. He returns again with a low-grade fever and dyspnea. CT scan reveals a complex loculated effusion with a thick surrounding peel. A chest tube is placed; however, after 24 hours, there is little drainage, and the patient continues to have a low-grade fever. What is the next step in his management?
. Surgery
. Streptokinase into the chest tube
. Place a second chest tube
. Increase the dose of IV antibiotics
. Pulmonary consult for bronchoscopy
. Pulmonary consult for bronchoscopy
. 1.0 to 1.5
.1.5to2.0
. 2.5 to 3.5
. 2.0 to 3.0
. Greater than 4
173) An obese 56-year-old female presents to her physician concerned that her asthma is worsening. She describes night-time cough and wheezing that have been increasing over recent months. She also reports feeling tired each morning because she works late hours and has no time to relax after dinner. On review of systems, the patient denies dyspnea on exertion, but acknowledges that her throat has been sore lately. Her past medical history is significant for bronchial asthma, type2 diabetes and hypertension. Her medications include an albuterol inhaler which she uses occasionally, lisinopril and aspirin. Her vital signs are within normal limits, and there are no abnormalities on physical exam. Which of the following is the most appropriate next step in the management of this patient?
. Discontinue lisinopril
. Discontinue aspirin
. Add pantoprazole
. Add inhaled fluticasone
Add salmeterol
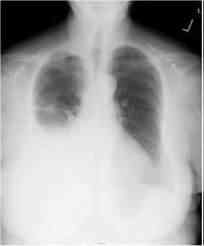
174) A 60-year-old Caucasian female comes to the physician because of progressive shortness of breath for the past month. She has had a 13.6 kg (30 lb) weight loss during this period. She has a history of hypertension and hypothyroidism and takes metoprolol and levothyroxine. She has smoked two packs of cigarettes daily for 35 years. Her temperature is 36.7°C (98°F), blood pressure is 130/70 mmHg, pulse is 80/min, and respirations are 20/min. On examination, decreased breath sounds and dullness to percussion are noted on the right, middle and lower lobes of the lung. Her chest x-ray is shown below. Which of the following is the most appropriate next step in the management?
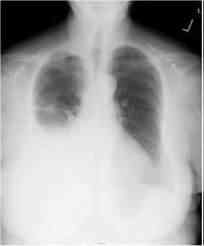
ll
. Bronchodilator therapy
. Decrease FiO2
. Increase tidal volume
. Decrease respiratory rate
Incentive spirometry
176) A 69-year-old male presents to the ER with severe shortness of breath for the past 12 hours. He reports that he has used his albuterol inhaler many times without relief. On review of systems he notes having had a mild fever yesterday that resolved with acetaminophen. The patient quit smoking 2 years ago but has a 100 pack year smoking history. On physical examination, his blood pressure is 150/90 mmHg and heart rate is 110/min. The patient is using accessory muscles of respiration. Expirations are prolonged, and there are wheezes bilaterally. Arterial blood gas (ABG) analysis reveals the following: pH 7.36, pO2 64 mmHg, pCO2 57 mmHg, HCO3 32 mEq/L. The patient is treated with ipratropium and albuterol nebulizers and moxifloxacin. Which of the following additional therapies is most likely to benefit this patient?
. Corticosteroids
. Loop diuretic
. Aminophylline
. Mucolytic agents
. Diltiazem
177) A 28-year-old male presents to the physician's office for a routine health maintenance examination. He has a two-year history of bronchial asthma for which he uses an albuterol inhaler. He states that he experiences asthma symptoms an average of 2 times per week, for which his albuterol inhaler provides relief. He has not had nighttime awakenings over the past month. He does not use tobacco, alcohol or illicit drugs. His family history is significant for asthma in his grandfather. Physical examination is unremarkable. Which of the following is the most appropriate next step in his management?
. Add long-acting beta-2 agonist inhaler
. Add inhaled corticosteroids
. Add oral prednisone
. Add oral theophylline
Continue current medical regimen
178) A 3-year-old boy presents to the emergency department with a fever and difficulty breathing. He is the product of a normal pregnancy and has been healthy since birth. His immunizations are up to date. This morning he appeared to be in his usual state of health and was dropped off at day care by his father. Later on, his teacher noticed that he had suddenly become fussy and flushed and could not be consoled with toys, rocking, or hearing a story. He also felt warm to the touch and was drooling more than usual. When she took his temperature, it was 39°C (102.2°F). His parents were contacted immediately, and the patient was brought to the emergency department. He appears toxic and anxious, and has loud labored breathing. He is sitting upright, bracing himself on his arms, with his neck hyperextended and mouth open. His temperature is 40°C (104°F), respiratory rate is 50/min, pulse is 140/min, blood pressure is 102/62 mm Hg, and oxygen saturation is 100% on room air. Lateral x-ray of the neck is shown in the image. Laryngoscopy reveals a large cherryred epiglottitis. What is the most appropriate next step in management?

zz

Antibiotic therapy
Corticosteroids
Observation
Nasotracheal intubation
Tracheostomy
179) A 35-year-old homeless man presents to the emergency department with chief complaints of a cough and fever. He is intoxicated. He admits to drinking about a fifth of vodka every day and confirms a history of delirium tremens and blackouts. X-ray of the chest is significant for an air-fluid level in the superior segment of the right lower lobe. Which of the following is the most appropriate first-line agent for treating this patient’s condition?
Azithromycin
Clindamycin
Isoniazid
Moxifloxacin
Piperacillin-tazobactam
180) An agitated and nervous 24-year-old woman has had severe wheezing and shortness of breath for 2 days. After receiving oxygen, steroids, and salbutamol (Ventolin) in the emergency room, her breathing improves. She is still wheezing and now feels tremulous and anxious with a pulse of 110/min and respirations 30/min. Arterial blood gases on oxygen reveal a pH of 7.40, PO2 340 mm Hg, PCO2 40 mm Hg, and bicarbonate of 24 mEq/L. She is hospitalized for further treatment. Which of the following treatments or medications should be avoided in her?
Theophylline
Sedatives
Sympathomimetic amines
Corticosteroids
Intravenous (IV) fluids
181) A 29-year-old woman has a long history of mild asthma. She now has a flare and experiences recurrent episodes of bronchial obstruction, fever, malaise, and expectoration of brownish mucous plug. On examination, there is bilateral wheezing. Infection is suspected and a CXR reveals upper lobe pulmonary infiltrates. The eosinophil count is 2000/mL, and serum precipitating antibodies to Aspergillus are positive. Which of the following is the most appropriate next step in management?
Antihelminthic therapy
A short course of systemic glucocorticoid therapy
High-dose glucocorticoids by puffer
Desensitization treatment
Long-term systemic glucocorticoid therapy
182) A 31-year-old African American man presents with dyspnea on exertion. He also has fever and red tender rash on his shins. Physical examination reveals fine inspiratory crackles in both lower lung lobes and tender erythematous nodules on his legs. CXR shows bilateral hilar adenopathy and reticulonodular changes in both lungs. Transbronchial biopsy reveals noncaseating granulomas. Which of the following is the most appropriate next step in management?
Aspirin
Isoniazid (INH) and streptomycin
Nitrogen mustard
Steroids
No therapy
183) A 53-year-old man with a long respiratory his- tory is admitted to the hospital because of increasing shortness of breath and sputum production. He is started on antibiotics and inhaled bronchodilators and anticholinergic agents. The next day he is found in his room confused and sleepy. A PCO2 determination reveals severe hypercarbia (PCO2 70 mmHg). Which of the following explanations regarding his elevated PCO2 is correct?
Occurs only with CO2 inhalation
Does not occur in obstructive lung disease
May worsen with oxygen administration
Does not occur in restrictive lung disease
Occurs with chronic hypocapnia
184) A 30-year-old man presents to the resuscitation bay with gunshot wounds in the anterior and posterior left chest. Although in distress and dyspneic, the patient is cooperative. He has a patent airway and is moving all extremities. His pulse is 120/min, blood pressure is 120/90 mm Hg, and respiratory rate is 30/min. He has bounding distal pulses, and no other injuries are identified on secondary examination. X-ray of the chest reveals fluid in the pleural space, and a left chest tube thoracostomy yields 600 mL of bright red fluid. Over the next hour 750 mL of blood is collected. What is the most appropriate next step in management?
Autotransfuse with the collected blood and continue to observe closely
Insert another chest tube
Remove the chest tube and suture the inci- sion closed
Left thoracotomy
Thoracentesis
185) A 22-year-old woman with mild persistent asthma comes to the primary care clinic after an emergency department visit 2 days ago for an acute asthma exacerbation. She notes an in- crease in frequency of wheezing and shortness of breath for the past 4 months, with daily symptoms, and has been symptomatic for at least 2 nights per week. She has also had three emergency department visits during the same period. Her current asthma medications include montelukast (leukotriene inhibitor) daily and an albuterol inhaler as needed. The patient’s peak flow is 75% of predicted. Which of the following is the most appropriate next step in management?
Add a long-acting inhaled β-adrenergic agonist and low-dose inhaled steroid to the regimen
Add systemic steroids to the regimen
Discontinue the leukotriene inhibitor and change the regimen to daily low-dose inhaled steroids
Admit to the hospital for further pulmonary work-up
Start cromolyn sodium
186) A 30-year-old man has episodes of wheezing and shortness of breath two to three times per week. Approximately every 2 weeks he awakens at night due to cough and difficulties breathing. He reports having similar symptoms since he was a child, but believes that they are worsening somewhat now. His symptoms are worsened by cold air and exercise and are improved by rest. Which of the following is the most appropriate treatment?
Daily high-dose inhaled corticosteroid and β-agonist when needed
Daily high-dose inhaled corticosteroid with oral steroids for exacerbations and short-acting β- agonist when needed
Daily low-dose inhaled corticosteroid and short-acting β-agonist when needed
Daily oral steroids and long-acting β-agonist
Short-acting β-agonist when needed
187) A 63-year-old woman presents with dyspnea and coughing up foul smelling purulent sputum. She has had many similar episodes in the past. There are no other constitutional symptoms and she denies excessive alcohol intake. On physical examination, she appears chronically ill with clubbing of the fingers. Heart sounds are normal, JVP is measured at 4 cm, and there are inspiratory crackles heard at the lung bases posteriorly. There is no hepatosplenomegaly or any palpable lymph nodes. CXR shows scaring in the left lower lobe, which on chest CT scan is identified as cystic changes with airway dilatation and bronchial wall thickening. Which of the following is the most appropriate initial next step in management?
Steroids
Antibiotics and postural drainage
Aerosols
Radiotherapy
INH
188) A 65-year-old smoker previously diagnosed with chronic obstructive pulmonary disease presents to the emergency department complaining of worsening cough and sputum production. She reports feeling breathless when climbing the stairs to her first floor walk-up apartment, and has moderate difficulty in providing her history in complete sentences. X-ray of the chest shows hyper inflated lungs with flattened diaphragms, attenuated vascular markings, and a narrow mediastinum. What agent(s) will provide the greatest relief of symptoms in the emergency department?
Albuterol and ipratropium bromide
Antibiotics
N-acetylcystein
Magnesium sulfate
Theophylline
189) A 51-year-old man presenting to the clinic for routine examination mentions that he has not been able to get over the flu. Further questioning clarifies that he has had a nonproductive cough for the past 3–4 months and is unable to sustain his normal walking pace for prolonged periods. He reports feeling more fatigued than he recalls feeling last year. His medical history is significant for hypertension, alcoholism, and obesity. His blood pressure is well controlled on losartan and hydrochlorothiazide. He has no known drug allergies. His mother died of complications of type 2 diabetes mellitus. His father had a fatal myocardial infarction at age 56 years. The patient smokes half a pack of cigarettes per day and has done so for the past 7 years. He has worked all his adult life as an accountant and has no known exposures to asbestos or organic dusts. His blood pressure is 134/96 mm Hg, heart rate is 78/min, respiratory rate is 16/min, temperature is 37°C (98.6°F), and oxygen saturation is 94% on room air. Lung examination reveals bilateral inspiratory crackles in the lung bases. High-resolution CT shows patchy areas of ground glass, reticular abnormalities, and traction bronchiectasis. Laboratory findings are normal except for an elevated erythrocyte sedimentation rate of 54 mm/hr. What is the recommended treatment for this patient’s cough?
Change the antihypertensive agent
Prescribe amantadine
Prescribe glucocorticoids
Prescribe bronchodilators and long-term domiciliary oxygen therapy
Resect diseased lung fields
190) A 38-year-old woman has been complaining of a 2-year history of increasing dyspnea and fatigue. Physical examination reveals increased JVP and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests show a slight restrictive pattern. Primary pulmonary hypertension is diagnosed. Which of the following treatments is helpful in this condition?
Nitrates
Corticosteroids
Calcium channel blockers
Alpha-adrenergic blockers
Angiotensin-converting enzyme (ACE) inhibitors
191) A 1-year-old child with cerebral palsy secondary to perinatal asphyxia presents to her general pediatrician for a well-child visit. She was delivered at 37 weeks’ gestation by emergency cesarean section for a tight nuchal chord. The patient has severe spastic quadriparesis that is limiting her movements. She also has mental retardation and is unable to speak. She has received physical and occupational therapy since early infancy; however, her parents are concerned by her lack of improvement. Which of the following is the best choice for treatment of spasticity in this child?
Baclofen
Botulinum toxin
Discontinue physical therapy
Carbamazepine
Hyperbaric oxygen
192) A 66-year-old man has progressive shortness of breath due to COPD. He is currently able to do his activities of daily living, but has trouble walking more than one block. His physical examination reveals hyperinflation, increased resonance to percussion, and bilateral expiratory wheezes. He is on appropriate medical therapy for his stage of COPD. Which of the following is also indicated in the management of this condition?
Yearly influenza vaccination
Meningococcal vaccination
Haemophilus influenzae B vaccination
Weight reduction if obese
Pneumococcal vaccination
193) A 52-year-old man develops sudden-onset shortness of breath on postoperative day 4 after a hemicolectomy for colon cancer. His surgery went well with no operative complications. He reports no cough, sputum, or pleuritic chest pain. His blood pressure is 155/90 mm Hg, pulse 100/min, temperature 37.8°C, lungs are clear, and heart sounds normal. He has bilateral pedal edema, but no discomfort in his legs. His CXR and ECG are normal. A chest CT with contrast reveals a thrombus in his right upper lobe artery. Which of the following statements concerning the management of this condition is most likely correct?
Continuous IV heparin or subcutaneous low-molecular-weight heparin (LMWH) therapy is indicated
Urgent thrombolytic therapy is indicated
Filter insertion is indicated
Urgent inferior vena cava (IVC)
Confirmation of the diagnosis with bilateral ultrasound leg Dopplers
194) A 23-year-old man is seen in the emergency department for sudden onset, right-sided pleuritic chest pain that developed 30 minutes ago while he was watching television. The patient also complains of difficulty breathing. He has no prior medical history, denies smoking and intravenous drug use, and does not take any medications. His temperature is 37.3°C (99.1°F), blood pressure is 130/82 mm Hg, pulse is 92/ min and regular, respiratory rate is 20/min and shallow, and oxygen saturation is 98% on room air. His body mass index is 18 kg/m². Diminished breath sounds, hyperresonance, and decreased tactile fremitus are prominent in the right lung field. The trachea is midline. X-ray of the chest shows a 10% pneumothorax on the right. Which of the following is the most appropriate initial management?
Needle decompression
Observation with supplemental oxygen
Thoracoscopy with stapling of blebs
Open thoracotomy with oversewing of the pleural blebs and scarification of the pleura
Tube thoracostomy with doxycycline pleurodesis
195) A 57-year-old Caucasian man presents complaining of "feeling overwhelmed by life." He has felt depressed for the past six months, and states that he has difficulty focusing on daily activities. His sleep is poor and he wakes frequently at night. Further inquiry reveals that he is a Vietnam War veteran and that he experiences flashbacks and nightmares about his combat experiences. He notes that the flashbacks began prior to his feelings of depression. He avoids watching war movies and refuses to discuss with anyone his time spent in Vietnam. This is his first visit to a psychiatrist and he asks to be started on some medication. Which of the following should be avoided in this patient?
. Lorazepam
. Nortriptyline
. Exposure therapy
. Paroxetine
. Cognitive therapy
196) A 58-year-old woman has a history of major depressive disorder that has been in remission for the past ten years. She takes phenelzine daily and sees her psychiatrist every other month. While on vacation, the patient and her husband indulge in a gourmet meal. Afterward, the patient becomes concerned as she believes one of the dishes may have contained aged cheese, which her psychiatrist had warned her about eating. She comes to the emergency department of the local hospital to express her concerns. Which of the following is most appropriate to monitor?
. Blood pressure
. Blood urea nitrogen and creatinine
. Liver function tests
. Creatine phosphokinase
. Temperature
197) While working as the attending pediatrician in the neonatai ICU, you are called by nursing to examine a two-day-old male child who has recently begun vomiting. The child has failed to pass meconium since birth. Physical examination demonstrates significant abdominal distention. A rectal examination reveals no stool in the vault. You strongly suspect Hirschsprung disease and inform the child's mother that an abdominal radiograph and barium enema are necessary. The mother forbids you from proceeding with any further testing or procedures because she does not believe "there is anything wrong." What is the most appropriate next step?
. Agree not to perform the tests
. Obtain a court order to authorize testing
. Contact the hospital's ethics committee for guidance
. Proceed with tests
. Wait until the mother provides consent
198) A 24-year-old female veterinary assistant is referred to a psychiatrist for the presumptive diagnosis of dysthymia. She reports having a three-year history of low energy levels and gradual worsening in her ability to focus on her work. She feels "sad, hopeless," and experiences little pleasure. She denies any suicidal thoughts. She has never been on any psychotropic medications before, and denies any family history of psychiatric illness. She has gastroesophageal reflux disease, for which she takes omeprazole. She has no known allergies, and does not drink alcohol or smoke cigarettes. The psychiatrist decides to treat her dysthymia with bupropion. Which of the following is a contraindication to the use of bupropion?
Narcolepsy
. Attention deficit hyperactivity disorder
. Anorexia nervosa
Smoking cessation
. Bipolar disorder
199) A 35-year-old woman has chronic auditory hallucinations in which she hears her father's voice. His voice said encouraging things to her in the past, but it has recently been scolding her and saying derogatory things about her. The woman is started on risperidone, and she returns two weeks later for a follow-up visit. Although she states that the hallucinations are much better, you notice that she is walking much slower than usual and is not swinging her arms. Also, the patient's facial expressions are rather flat and unchanging, and she admits that her writing has become smaller since starting the medication. Which of the following pharmacologic changes would be most appropriate?
. Start dantrolene
. Start benztropine
. Start sertraline
. Start propranolol
Discontinue risperidone and start haloperidol
200) A 29-year-old gravida 1, para 0 Caucasian female with a history of bipolar disorder presents at eight weeks of gestation for prenatal counseling. She has been taking a stable dose of lithium for the past year. Her last depressive episode was 16 months ago. Her family history is significant for bipolar disorder in her mother, which was successfully controlled with lithium. She does not smoke cigarettes or consume alcohol. She asks whether her baby will have any congenital abnormalities. Which of the following complications is her fetus at increased risk for?
Cardiac anomalies
Craniofacial defects
Mental retardation
Neural tube defects
. Genital anomalies
201) A 22-year-old woman is brought to the emergency department by her father because she is demonstrating "strange, disorganized behavior." Earlier that day, she had insisted that the television news anchorman was talking directly to her about the risks of "poison rays" from the moon. She was also apparently attempting to re-organize her bedroom closet when her father found her mumbling incoherently and counting the same pair of socks over and over. She is agitated when examined in the emergency department and the decision is made to admit her to the psychiatric ward. There, after a detailed interview, the diagnosis of schizophrenia is made. She is stabilized with antipsychotics and then discharged home. Her father asks what can be done to ease her return to everyday life and to decrease the likelihood of re-hospitalization. Which of the following measures would be most helpful in this regard?
Restrict the patient to home as much as possible
. Encourage the patient to return to work
. Keep family stresses and conflicts to a minimum
Minimize the patient's social interaction with others
Strongly encourage the patient to make new friends
202) A middle-aged Asian American married couple comes to clinic for a routine examination. Both the husband and wife have been known patients of yours for many years. The husband is being treated for coronary artery disease and tension headaches. Today, he mentions that he "cannot get an erection" even when he feels sexual desire. He adds that he still finds his wife physically attractive and that they are mutually compatible in every respect. This recent development has been causing him significant anxiety and has been a source of concern for his wife. After ruling out medical and psychological causes for his erectile dysfunction by taking a detailed history and pursuing a thorough workup, you agree to his request that he be started on sildenafil. One week later, his wife places an urgent call to your office, reporting that her husband developed severe chest pain "after taking the new medication you prescribed." An EKG done in the emergency department reveals new inferior wall ischemia. You immediately realize that you should not have written him the prescription for sildenafil because he was already using a nitroglycerin patch for his coronary artery disease. What is the most appropriate next step?
Admit to the patient and his wife that you made a mistake
Withhold this information as it could result in a lawsuit
. Tell the patient and his wife that you were not aware of this cross-reaction between the two drugs
Tell the patient and his wife that his chest pain was probably precipitated by anxiety
. Remove yourself as the patient's physician immediately
203) A 38-year-old male with a chronic history of schizophrenia is admitted to the hospital for deterioration in his condition. He is a known patient and was stable on risperidone for the past few years. Today, the patient does not respond when spoken to and he sits motionlessly. He makes no eye contact and his face remains expressionless. Vital signs include temperature of 37.0°C (98.6°F), blood pressure of 132/80 mm Hg, pulse of 88/min, and respirations of 14/min. Physical examination demonstrates diffuse muscle rigidity but is otherwise unremarkable. Which of the following would be the most appropriate next step?
. Increase risperidone dose
. Initiate therapy with dantrolene sodium
. Continue same dose of risperidone and add clozapine
. Replace risperidone with quetiapine
. Administer lorazepam
204) A 7-year-old boy is brought to the pediatrician by his mother for a routine check-up. Physical examination is normal, but during the exam the mother reveals that her son's behavior has been poor. She says that he is always running around (even during dinner), doesn't listen, and keeps his room a mess. She hopes he will grow out of this soon. Upon further questioning, the pediatrician learns that the patient's second-grade teacher has reported that he answers questions impulsively and out of turn, and that he cannot sit at his desk for a very long time without fidgeting. He also frequently forgets to bring in his homework. The mother states that her son has had these symptoms for about a year, and that his grades have been falling over the past six months. The diagnosis of attention deficit hyperactivity disorder is made and the boy is started on methylphenidate. Which of the following side effects is most likely to occur in patients who take methylphenidate?
Decreased appetite
. Diarrhea
. Seizures
. Hypersomnia
. Weight gain
205) A 16-year-old boy presents to his pediatrician with scattered petechiae and a three-week history of fatigue. Laboratory evaluation and a bone marrow biopsy confirm the diagnosis of acute lymphoblastic leukemia. The boy's parents are divorced and have joint custody of him. His mother consents to the proposed chemotherapy and blood transfusion and requests that his treatment be started immediately. The father, however, refuses to agree to the treatment because of his religious beliefs. What is the most appropriate means of handling this situation?
. Withhold the proposed treatment
. Proceed with the proposed treatment
. Obtain a court order to proceed
. Ask the patient his wishes
. Consult the hospital's ethics committee
206) A middle-aged married couple brings their 10-year-old daughter to the pediatrician because "she just is too tired to play nowadays and sleeps all the time." The parents say that their daughter is winded with minimal exertion. Further inquiry reveals that for the past two weeks, the girl has had bleeding gums when she brushes her teeth. Physical examination demonstrates pallor and hepatosplenomegaly. An extensive workup indicates that the girl is suffering from acute lymphoblastic leukemia, and her parents are informed that chemotherapy will be necessary. The parents firmly refuse to comply with this treatment plan, however, because they are convinced that the side effects will be too severe. Despite a lengthy discussion about the benefits of treatment and the likely consequences for their daughter if therapy is withheld, the girl’s parents insist upon taking her home. What is the most appropriate next step?
. Obtain a court order for chemotherapy
. Proceed with the chemotherapy
. Provide supportive treatment only
. Comply with parent’s wishes
. Inform the parents that if they refuse treatment for their daughter, they will need to find a new pediatrician to assume her care
207) A 72-year-old man presents for a follow-up visit regarding his depressed mood after his wife's death seven months ago. The patient complains of lethargy and episodes of tearfulness. He has attended three sessions of supportive psychotherapy so far and expresses appreciation for the referral because he likes the therapist. However, he continues to feel depressed and is now experiencing insomnia. He is also feeling very guilty about his wife's death and feels that he should have somehow done more for her in her final months. He admits that during a particularly dark moment last month he briefly contemplated committing suicide so that he could "join her," although he is adamant that he does not feel suicidal at this time and will readily contract for safety. Physical examination reveals the patient has lost 13 lbs (5.9 kg) since his wife's death. What is the most appropriate next step?
. Prescribe sertraline
. Prescribe amitriptyline and alprazolam
. Recommend electroconvulsive therapy
Increase psychotherapy sessions to twice weekly
. Provide reassurance and continue psychotherapy regimen
208) A 60-year-old Caucasian man presents to his family physician complaining of weight loss and fatigue. A review of systems is positive for a change in bowel habits. He says that in the past several weeks, he has developed pencil-thin stools. Further evaluation reveals the presence of colon carcinoma. The patient is told the diagnosis, and his treatment options and prognosis are discussed. He refuses any treatment and says he wants to die peacefully at home without any medical intervention. What would be the most appropriate means of handling the situation?
. Treat the patient against his wishes
. Contact his family and ask them to convince him to receive treatment
Ask the patient why he is reluctant to be treated
. Respect the patient's decision
. Provide the patient with some literature about the benefits of chemotherapy
209) A 20-year-old female college student is brought to the emergency department by police at 2:30 am after she was caught attempting to enter the White House. She is highly agitated and is pacing around the examination room. Upon further questioning, she states that she just flew in from Texas to meet with the president because she has a "foolproof plan for eliminating terrorism worldwide in just seven days." She adds that she has barely slept for the past ten nights because she has been working intensively on this plan. She speaks very quickly, but periodically stops to angrily shout, "I'm going to sue all of you for interfering with my right to meet with the president." The evaluation has to be stopped because she demands that she be allowed to leave. Family history is significant for major depression in her mother. Vital signs are temperature 37.0°C (98.6°F), blood pressure 148/84 mmHg, pulse 98/min, and respiratory rate 22/min. Which of the following medications should be administered to this patient immediately?
. Mirtazapine
. Desipramine
. Haloperidol
. Fluoxetine
. Lithium carbonate
210) A 52-year-old obese male presents with complaints of episodes of daytime sleepiness that prove irresistible. He reports feeling very refreshed and energized upon awakening from these "naps." A detailed history reveals he also frequently experiences a complete loss of muscle tone, especially when he laughs suddenly or feels a surge of intense emotion. Of particular concern to this patient is that he occasionally finds himself unable to move upon waking, and says he feels temporarily "frozen." His previous diagnoses include gout and external hemorrhoids. His family history is noncontributory. He does not smoke cigarettes or drink alcohol and denies recreational drug use. Physical examination reveals no abnormalities. Which of the following is the most appropriate treatment for this patient?
. Benzodiazepines
. Melatonin
. Treatment of his underlying neurological condition
. Methylphenidate
. Weight reduction
211) A 28-year-old woman is brought to the emergency department by her sister after she experiences a generalized tonic-clonic seizure. The patient appears confused and is unable to answer any questions. The sister says the patient has never had a seizure before. The patient's medical history is unremarkable except for a long history of panic disorder for which she has been taking high doses of "some medication." The sister adds that the patient missed a few doses recently because they were staying at a friend's house, but she is sure that the patient was otherwise regular in taking her medication. Which of the following medications was the patient most likely taking?
. Clonazepam
. Clomipramine
. Alprazolam
. Buspirone
. Paroxetine
212) A 27-year-old man is brought to his primary care physician by his wife because he has not been himself for the past ten days. His wife says that her formerly reserved, quiet husband has been staying up all night lately gambling their savings away while playing poker with friends that he recently met. He is also not concerned about having missed work for the past week. When asked about this recent change in behavior, the man smiles and replies proudly that he no longer needs to work because he has invested a large sum of money in a company that will soon make him rich. He speaks very quickly and it is difficult for him to focus his attention at times. Which one of the following medications would be most appropriate in the treatment of this patient?
Bupropion
. Clomipramine
Haloperidol
. Clozapine
. Valproic acid
213) A 27-year-old man presents to his primary care physician complaining of feelings of inadequacy and hopelessness. In a quavering voice, he reports that he gets "extremely anxious" when he has to speak before a group of people at business meetings or other social events. He is unable to "just relax," even at small parties with friends or family, and he isolates himself as a result. He feels his social seclusion is limiting his career advancement, which bothers him greatly. Which of the following treatment combinations would be the most appropriate choice for this patient?
. Fluoxetine and chlordiazepoxide
. Assertiveness training and paroxetine
. Supportive psychotherapy and phenelzine
. Psychodynamic psychotherapy and clonazepam
. Supportive psychotherapy and propranolol
214) A 33-year-old businessman with an unremarkable past medical history presents to you complaining of fatigue and some weight loss over the past three months. He awakens at 4:00 am each morning and is unable to fall back asleep. He also mentions that he used to enjoy playing golf twice per week, but now has little interest. Although he used to excel at work, he now finds himself losing interest and "spacing out" at times. He denies considering suicide. His TSH is normal. He is diagnosed with major depression and prescribed fluoxetine, and is asked to return for a follow-up appointment in two weeks. At the return visit, he states that his symptoms have not worsened, but have not improved either. He says, "I don't feel like the medication is doing anything." What is the most appropriate next step in the management of this patient's condition?
Continue with fluoxetine at the same dose
. Increase the dose of fluoxetine
. Discontinue fluoxetine and begin amitriptyline
Discontinue fluoxetine and begin sertraline
. Continue fluoxetine and add amitriptyline
215) A 22-year-old woman presents to the emergency department in an agitated state, certain that she is "about to die." Fifteen minutes ago, she developed heart palpitations and a severe "viselike" tightness in her chest. She experienced a similar episode last week, which resolved in twenty minutes. She denies using any drugs and her medical history is unremarkable. Her father has a history of heart disease and her mother has diabetes mellitus. She takes no medications. Vital signs are temperature 37.0°C (98.6°F), blood pressure 132/74 mmHg, pulse 118/min, and respiratory rate 30/min. She is sweating profusely. EKG reveals sinus tachycardia. The most appropriate next step is administration of which of the following?
. Alprazolam
Aspirin
. Fluoxetine
. Buspirone
.lmipramine
216) As the on-call surgery resident, you are paged to see a patient on the ward who is having seizures. The patient is a 35-year-old male who underwent a cholecystectomy yesterday. His surgery was uneventful and the man appeared to be doing well until an hour ago when he developed altered sensorium. Upon arriving on the floor, you discover the patient to be confused and agitated. His vital signs include a temperature of 38°C (100.4°F), blood pressure of 134/86 mm Hg, pulse of 110/min, and respirations of 18/min. The man is diaphoretic and has tremors. His wound incisions show no evidence of inflammation, and biliary drainage appears adequate. A review of his medical record indicates his medical history to be unremarkable except for mild esophagitis. He smokes a pack of cigarettes per day and drinks 6-10 beers per night. His medications include folic acid, thiamine, and omepra zole. Laboratory results include the following: CBC: Hb 14.1 g/dL, Leukocyte count 7,100/cmm. Serum Chemistry: Sodium 137 mEq/L, Potassium 4.0 mEq/L, Chloride 101 mEq/L, Bicarbonates 24 mEq/L, BUN 12 mg/dL, Creatinine 1.0 mg/dL, Glucose 104 mg/dL. Arterial Blood Gas: PH 7.40, PO2 94 mm Hg, PCO2 40 mm Hg. Which of the following should be initiated immediately in this patient?
. Disulfiram
. Chlordiazepoxide
. Flumazenil
. Phenobarbitone
. Phenytoin
217) A 35-year-old Caucasian male with a chronic history of paranoid schizophrenia presents to the mental health clinic. He strongly believes that his wife recently stole his pill bottle of risperidone, which he feels caused him to start experiencing more frequent and intense auditory hallucinations. He says that the "voices" tell him to kill his wife because she cannot be trusted. He admits to having homicidal thoughts about his wife but denies any specific plan for harming her. He requests a refill of his risperidone. What is the most appropriate next step?
. Refill his prescription of risperidone and call his wife after he leaves
. Refill his prescription of risperidone without calling his wife as he does not have a plan to hurt her
. Call the patient's wife immediately before filling the risperidone prescription
. Admit the patient to the psychiatric ward
. Increase his dose of risperidone
218) A 37-year-old obese man returns to his doctor for a follow-up visit. One month ago, he was diagnosed with type II diabetes mellitus and was started on metformin. His fasting glucose is 122 mg/dl, and his blood pressure is 145/85 mm Hg. The patient looks rather dejected and admits it has been difficult to come to terms with his diagnosis. He has tried to exercise, watch his diet, and quit smoking as was suggested, but lately he has been feeling unmotivated and without energy. He admits to feeling sad and guilty about his weight, but is not sure he will be able to do anything about it. He continues to smoke despite attempts to cut back, and has been spending much of the day in bed watching television or sleeping. He has withdrawn from friends and family and took the last two weeks off from work, as he did not feel "up to going." Which of the following would be the best medication to prescribe at this time?
. Bupropion
. Fluoxetine
. Selegiline
. Modafinil
. Venlafaxine
219) A 28-year-old attorney presents complaining of a six-month history of extreme nervousness, irritability, and restlessness. He is "plagued" by recurrent thoughts of not being able to properly carry out his responsibilities at the office. He dreads the possibility of not being offered a position as partner in the law firm. As a result, he finds himself unable to concentrate well or perform his duties efficiently. He is also engaged to be married, and spends sleepless nights thinking about the responsibilities of married life. He worries that he will not be a good husband or father. He denies any history of alcohol intake, but has recently begun drinking two bottles of beer every night for the past month as a means of escaping from his distressing thoughts. Which of the following is the treatment of choice for this patient?
. Alprazolam
. Propanolol before a distressing situation
. Ziprasidone
. Treatment for alcohol dependence
. Buspirone
220) A 16-year-old female presents to her pediatrician's office for a routine examination. She is wearing a sweater despite the warm weather, and admits she often feels cold. She states that she has otherwise been feeling fine, except for having difficulty losing weight. She wants to lose about 10 lbs (4.5 kg) because she believes she is "too fat." She has been on a strict diet and exercises two hours daily. She is also requesting a pregnancy test because she has not had a menstrual period for the past three months. Past medical history is significant for a supracondylar fracture of her right humerus at the age of seven. She is alert, cooperative, and in no apparent distress. Vital signs are temperature 36.2°C (97.2°F), blood pressure 88/58 mmHg, pulse 56/min, and respiratory rate 16/min. Her height is 5'5" (165 cm) and weight is 90 lbs (40.9 kg). What is the most appropriate next step in the management of her symptoms?
. Advise the patient that she is underweight and needs to increase her caloric intake
. Advise the patient that her complaints likely stem from a thyroid disorder
. Recommend the patient to begin taking sertraline
. Refer the patient for cognitive-behavioral therapy to address her weight
. Hospitalize the patient
221) A 21-year-old male is admitted to the intensive care unit after attempting to commit suicide by overdosing on some pills he found in the medicine cabinet at home. A psychiatry consult is ordered. While interviewing the patient, the psychiatrist observes that the patient has a "blank" expression on his face and is minimally responsive. He refuses to make eye contact and speaks in monosyllables. An attempt is made to obtain a more detailed history from the patient's father. He describes his son as very aloof, having avoided the other children in the neighborhood and participated in few activities as a child. His son dropped out of school in ninth grade and has not been able to maintain jobs throughout the years because of his social difficulties. He adds that his son has been increasingly isolated this past year and that he has complained his deceased mother frequently asks him to "join her in heaven." Which of the following medications would provide the greatest benefit to this patient?
. Fluphenazine injections
. Risperidone
. Thioridazine
Haloperidol
. Chlorpromazine
222) A 26-year-old graduate student presents at her husband's urging, complaining of severe pain during sexual intercourse. She says that she was a virgin when she married her husband two years ago, and that she has been experiencing severe "genital pain" during sex since then. As a result, she avoids sexual intimacy with her husband, which is placing a strain upon their marriage. She also complains of intense pain with her menses and when passing stool. She admits to sporadic pelvic pain that waxes and wanes with no discernible trigger. What would be the most appropriate treatment given this woman's condition?
. Use of vaginal dilators
. Pain management training
Regularly scheduled follow-up visits
. Oral contraceptive pills
. Psychotherapy and sexual education
223) A 28-year-old male presents for a follow-up visit regarding his bipolar disorder, which has been managed with valproic acid for several years. He is accompanied by his mother who is very concerned because her son has been behaving strangely for the past two weeks, saying that he can hear the voice of his long-deceased father telling him to "come to me." The patient insists that he is able to ignore his father's voice and that he is not considering suicide at this time. The decision is made to start risperidone to treat the auditory hallucinations. This medication predominantly produces its antipsychotic effect by blocking which of the following receptors?
Alpha-1 adrenergic receptors
Dopamine-D2 receptors
. Muscarinic cholinergic receptors
. Histamine- 1 receptors
. Serotonin 2A receptors
224) A 59-year-old man well known to his primary care physician presents complaining of excessive fatigue during the daytime. He is accompanied by his wife, who says that he wakes frequently during the night and snores loudly. She worries because sometimes it sounds like he is gasping for breath at night. The only finding on physical examination is morbid obesity. The diagnosis of obstructive sleep apnea is made. Which of the following is not true about this disorder?
. Hypertension is a frequent complication
. Weight loss may improve symptoms
. Cor pulmonale can develop as a complication
. Apneic episodes may increase with age
. Benzodiazepines are effective treatment
225) A 19-year-old college student presents for a first visit because she is concerned about her "abnormal behavior." She says that she worries excessively about her door being locked and that she wakes several times throughout the night to confirm that the door is properly locked. She finds these thoughts distressing. Although she agrees that her fears are not rational, she feels unable to stop from acting on them. This frequent waking grossly impairs her sleep and as a result, she is finding it increasingly difficult to perform well academically. She has no history of psychiatric conditions, but her mother was recently diagnosed with trichotillomania. Vital signs include a temperature of 37.0°C (98.6°F), blood pressure of 118/84rnrnHg, pulse of 76/min, and respirations of 12/min. Physical examination is unremarkable. Which of the following medications would be the most appropriate treatment for her condition?
. Buspirone
. Clomipramine
. Paroxetine
. Olanzapine
. Propanolol
226) A 68-year-old woman with a history of well-managed sick sinus syndrome and osteoporosis is brought to the physician by her daughter. According to the daughter, her mother has become increasingly forgetful and irritable over the past two years. She adds that she felt less concerned about her mother's forgetfulness as "it just comes with aging," but that the "mood swings have become a problem in terms of her getting along with family members." A Folstein Mini-Mental Status Examination is performed and suggests significant cognitive decline. Dementia is strongly suspected. After potentially causative medical or psychiatric conditions have been ruled out, the diagnosis of Alzheimer's dementia is made. Which of the following medications would be most appropriate in the treatment of this woman's condition?
. Sertraline
. Risperidone
. Lorazepam
. Donepezil
. Bupropion
227) A 34-year-old male calls his primary care physician's office, requesting an urgent appointment to discuss a personal problem. The receptionist informs him that the physician is preparing to leave as it is near closing time, but that an appointment is available for early the next morning. The patient declines the offer of an appointment and hangs up. Fifteen minutes later, as the physician is locking the office up, the patient arrives and insists on being seen immediately. He breathlessly says that he has "some kind of red rash" on his penis, which has him very worried. He asks again to be examined now. What is the most appropriate response?
."It is extremely inappropriate on your part to come here despite my request that you make an appointment."
. "All right, we should look at your rash now. Come inside."
. "Didn't I already inform you that it is closing time?''
. "Your rash can most certainly wait until tomorrow."
'Although I understand your concern, we should address the issue tomorrow since it is not an emergency."
228) A 19-year-old known patient with bipolar disorder presents to her psychiatrist for a follow-up visit. She experienced her first manic episode three years ago and was then immediately placed on lithium. She has had no relapses and remains asymptomatic. Today she inquires about the possibility of discontinuing her medication. Her mother is apprehensive, however, about the prospect and asks the psychiatrist to continue the medication for a longer period. Which of the following is the most appropriate management of this patient's condition?
. Continue lithium for six more months in light of mother's concerns
. Taper and discontinue lithium
. Continue lithium for her lifetime
. Order serum lithium levels
. Discontinue lithium and initiate valproic acid
229) A fourth-year medical student develops a new onset headache that he describes as "excruciating." He denies any fever or vomiting. He requests the emergency department physician to order a CT scan of his head, as he is certain that he has developed an intracranial hemorrhage. A complete workup, including an ophthalmologic evaluation, is negative. In spite of reassurance from the physician, the student continues to be excessively worried and is unable to focus on his studies due to persistent thoughts about having a "brain bleed." Which of these would be the most effective step in resolving this patient's symptoms?
. Initiate a discussion about current emotional stressors
. Provide gentle reassurance
. Prescribe a benzodiazepine
Patently explain the benign nature of the headache
. Treat the headache with a placebo
230) A 44-year-old woman presents for a follow-up visit regarding her severe depression. She has taken numerous antidepressants over the years with little symptomatic relief, and continues to spend the majority of her time in seclusion, experiencing intense feelings of worthlessness and despair. Her husband is deeply concerned about the impact her depression has had on their marriage and their two teenage children. He requests information about "all available options" to improve his wife's symptoms. The prospect of electroconvulsive therapy (ECT) is discussed, and the husband inquires about potential drawbacks to the procedure. Which of the following is a common side effect of electroconvulsive therapy?
. Elevated liver enzymes
. Amnesia
. Muscle paralysis
. Epilepsy
. Neuroleptic malignant syndrome
231) A 42-year-old Caucasian man presents to the emergency department complaining of a two-day history of fever to 40°C (104°F), headache, and vomiting. Physical examination reveals petechiae and purpura on his trunk and lower extremities. Examination of his cerebrospinal fluid is consistent with bacterial meningitis. The patient is told of his diagnosis and the need for antibiotics and hospitalization is discussed. The patient refuses to be admitted to the hospital, however, and insists upon being treated at home. What is the most appropriate next step?
. Treat the patient against his wishes
. Discuss the situation with the patient's wife and ask that she convince him to accept hospitalization
. Respect the patient's decision and arrange for home antibiotic therapy
Consult with the hospital ethics committee
. Obtain a court order to proceed with treatment
232) A 28-year-old married nurse who works with you in clinic comes to you privately, saying that she "missed a period" this month. An over-the-counter urine pregnancy test confirms that she is pregnant. The first-trimester laboratory testing is performed, and she is found also to be HIV-positive. When you reveal the news of her HIV status to her, she is devastated. She hesitantly reveals that she had unprotected sexual intercourse with a former boyfriend several months ago. You explain that her husband's HIV status must be evaluated. Upon hearing this, the nurse is horrified and says. "No, I cannot tell him about this. He would never forgive me!" What is the most appropriate next step?
Call and inform local health authorities immediately
. Call and inform local health authorities and the nurse's husband immediately
Encourage the nurse to inform her husband
. Assure the nurse that her condition will be kept absolutely confidential
Tell the nurse that if she insists on hiding her HIV status from her husband, she cannot expect your medical or moral support
233) You are seeing a 41-year-old woman and her 19-year-old daughter in the emergency room because they think that they have been poisoned. The woman states that they have not been getting along with their landlord lately because they have been late on their last few rent payments. They say that the landlord is harassing them by banging on their floor at all hours of the night, turning down their heat, and asking the other tenants to spy on them. Last month, the woman thinks the landlord tried to spy on them by installing video cameras in her living room while they were out. Today, she tasted something odd in her food, and is convinced that she and her daughter have been poisoned in an attempt to get them out of the apartment once and for all. She came immediately to the hospital for treatment and to collect evidence of the poisoning. The mother is very protective of her daughter, who seems rather submissive and passive. She completely agrees with her mother's description of the events. Which of the following is the best course of action?
. Discharge both the mother and the daughter after a complete physical examination and blood tests
. Admit the mother to the psychiatric unit for treatment, but not the daughter
. Admit the daughter to the psychiatric unit for treatment, but not the mother
. Admit the mother and the daughter to the same psychiatric unit
. Admit the mother and the daughter to different psychiatric units
{"name":"DES 3 ep 5", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"133) A 54-year-old male presents to the office with several months history of hand tremors that are unresponsive to over-the-counter medication. The tremors always become worse when he is in public places. Sometimes, the hand tremors are so bad that he is unable to grasp. He denies trauma, fever, loss of muscle function or any prior stroke. His past medical history is significant for vague abdominal pains, the cause of which was never found. He is given some medication. A month later, he comes back and says, \"The tremor is gone, but now I have colicky abdominal pain, confusion, headaches, hallucinations and dizziness.\" What is the drug that caused this patient's new symptoms?, 134) A 44-year-old male has been abusing drugs for many years. Recently he started using the agent MPTP and he now presents to you in the ER. He says that he is not feeling well and wonders what is going on. He says he has a persistent tremor in his fingers and his body has become rigid. At times has had difficulty in walking. The CT scan of his brain is normal and all the blood work is within normal limits. You decide to treat him. Two years later you see him and he tells you that his symptoms have improved. He also noticed that he had a significant relief from the recurrent and persistent upper respiratory tract viral infections that he was so prone to. The agent you gave him was?, 135) A 5-year-old boy is brought to the office by his frustrated mother because, \"he just can't seem to concentrate!\" He has episodes that are characterized by frequent blinking and indifference to his surroundings. He does not remember anything after an episode. An episode does not last long, but he usually has 50-80 \"daydreaming accidents\" daily. His school performance has deteriorated lately, and his teacher has complained about his decreased concentration. Which of the following is the drug of choice for this patient's condition?","img":"https://www.quiz-maker.com/3012/images/ogquiz.png"}
More Quizzes
PAST PERFECT vs PAST PERFECT CONTINUOUS
10519
Deel 5
10519
Most Likely To... Quiz
10526
WHO KNOW RIYA THE BEST??!!
10513
Facts About Mixtures and Solutions - Test Your Skills
201043345
Which Little Miss Am I? Take the Little Miss
201030841
Free Tooth Identification & Numbering
201023312
HACCP Online Exam: Challenge Your Team Training Knowledge
201028209
Free Parks and Recreation Knowledge
201029131
Think You Know the Plant Life Cycle? Take the
201030841
Ultimate Beowulf Poem: Test Your Epic Knowledge
201023881
Free ServSafe Practice Test: Ace Your Food Safety
201031213