USMLE (part2)
101. A 56-year-old Caucasian male complains of chronic exertional dyspnea for the past several years that has progressively worsened. He cannot remember the last time that he saw a doctor, and does not take any medications regularly. It is difficult for him to climb two flights of stairs without having to rest. His dyspnea has gotten so bad that it has severely limited his activity level, and he now spends most of his time on the couch. He also describes recurrent episodes of nocturnal dyspnea, during which he wakes up at around 2:00 AM with difficulty breathing, coughing, and wheezing that improve when he sits up. He usually coughs up some yellowish sputum before being able to go back to sleep. He has had no fever, chills, or chest pain. Which of the following is the most likely cause of this patient's complaints?
A. Left ventricular failure
B. Bronchial asthma
C. Chronic bronchitis
D. Pulmonary thromboembolism
E. Pulmonary fibrosis
102. A 62-year-old man presents to his primary care physician's office with progressive exertional dyspnea. His past medical history is significant for hypertension treated with hydrochlorothiazide and diabetes mellitus treated with metformin. He was an industrial worker for 30 years and retired one year ago. He smokes one pack of cigarettes per day and consumes alcohol occasionally. His blood pressure is 150/100 mmHg and his heart rate is 80/min. His BMI is 31 kg/m2. Chest x-ray reveals pleural calcifications. Pulmonary function studies show the following: FEV1 70% of predicted FVC 65% of predicted Residual volume 70% of predicted DLCO decreased Which of the following is the most likely cause of this patient's symptoms?
A. Impaired lung expansion due to pleural calcifications
B. Emphysema from smoking
C. Interstitial lung disease from occupational exposure
D. Impaired lung expansion due to obesity
E. Increased pulmonary capillary wedge pressure
103. A 32-year-old woman comes to the emergency department complaining of sudden onset shortness of breath accompanied by a non-productive cough and left-sided chest discomfort that increases on inspiration. She denies subjective fever, coughing up blood, wheezing, palpitations, leg pain, and swelling of the lower extremities or any recent travel. Past medical history is significant for an appendectomy at age 15. Her medications include birth control pills and over- the-counter vitamins. She is a known carrier of sickle cell trait. Her father, age 65, has had diabetes for 20 years; mother, age 58, has coronary artery disease. She has never been pregnant, drinks alcohol socially and does not smoke. Her temperature is 99 F (38C), blood pressure is 110/70 mmHg, pulse 130/min and respirations are 33/min. Pulse oximetry shows an oxygen saturation of 85% on 6 liters of oxygen. Her BMI is 30 kg/m2. She is alert and cooperative without cyanosis or jaundice. Her lungs are clear to auscultation. Her abdomen is soft, nondistended and non-tender. Which of the following is the best test to confirm this patient's diagnosis?
A. EKG and cardiac enzymes
B. Echocardiogram
C. Doppler ultrasound of lower extremities
D. Spiral CT-Scan of the chest
E. Chest-x ray and sputum cultures
104. A 53-year-old male presents with progressively worsening dyspnea over a 4-month period. He also complains of decreased appetite, weight loss, and nagging epigastric discomfort. His past medical history is significant for a chronic duodenal ulcer for which he takes ranitidine on and off. He does not use tobacco, alcohol or illicit drugs. He has worked as a plumber for the past 30 years. On physical examination, his temperature is 36.9°C (98.4.F), blood pressure is 140/86 mm Hg, pulse is 80/min, and respirations are 15/min. Physical exam reveals fingernail clubbing and bibasilar endinspiratory crackles on lung auscultation. Chest x-ray demonstrates ground glass opacities of the lower lung fields, multiple pleural plaques, and one 3x3 cm mass in the right lung periphery. CT guided biopsy of the mass is planned. Biopsy is most likely to show which of the following?
A. Metastatic stomach cancer
B. Metastatic colon cancer
C. Metastatic pancreatic cancer
D. Bronchogenic carcinoma
E. Peritoneal mesothelioma
105. A 50-year-old female comes into your office complaining of four-month history of dry cough. She denies dyspnea or hemoptysis. Past medical history is significant for hypertension, diabetes, and gout. Her current medications include enalapril, metformin, hydrochlorothiazide, and allopurinol. She does not smoke or consume alcohol. Her vital signs are BP 130/80 mmHg, HR 80/min, T 36.7C (98F) and RR 16/min. Physical examination is within normal limits. The best next step in the management of this patient is:
Chest radiograph
B. Reevaluation of drug therapy
C. Pulmonary function testing
D. Barium esophagography
E. Bronchoscopy
106. A 47-year-old African American woman presents with two days of shortness of breath and leftsided chest pain. Her past medical history is significant for a mastectomy six months ago for breast cancer, for which she also received adjuvant chemotherapy. Her mobility has been limited recently due to progressive back pain. Her current medications include tamoxifen. On chest x-ray, there is an infiltrate obscuring the right heart border as well as a right-sided pleural effusion. Pleural fluid analysis reveals the following: pH 5.75 Nucleated cells 10,050/mm3 RBC 1,500/mm3 Protein 3.9 g/dl LDH 620 units/L Glucose 38 mg/dl Her serum chemistries are notable for an LDH of 310 units/L and protein of 6.1 g/dl. Which of the following is the most likely cause of her effusion?
A. Heart failure
C. Drug-induced lupus
B. Pneumonia
D. Pulmonary embolism
E. Hypoalbuminemia
107. A 45-year-old white man presents to your office complaining of daytime somnolence, increased fatigability, and morning headaches. He says that his wife complains that he snores loudly. He is not taking any medications and does not smoke or consume alcohol. His blood pressure is 145/90 mmHg and heart rate is 90/min. Physical examination reveals a well-nourished man with BMI = 31 kg/m2. What is the next best step in the management of this patient?
A. A benzodiazepine to improve sleep
B. Advise to sleep in supine position
C. Weight reduction
D. A thiazide diuretic for hypertension
E. Tracheostomy
108. A 64-year-old male presents to the ER with shortness of breath. The symptoms started one week ago with a dry cough and mild fever. His past medical history includes hypertension and exertional angina. He was hospitalized six months ago for pneumonia. He has a 35 pack-year smoking history. His blood pressure is 140/90 mmHg and heart rate is 90 and regular. On examination, the patient is in mild respiratory distress. He uses some accessory respiratory muscles for breathing, but he can speak in full sentences. Chest auscultation reveals bilateral wheezes and crackles at the left lung base. His ABG shows: pH 7.36 pO2 72mmHg pCO2 51mmHg Which of the following is the most likely cause of this patient's current symptoms?
A Congestive heart failure (CHF)
B. COPD exacerbation
C. Pulmonary embolism
D. Pneumothorax
E. Adult respiratory distress syndrome
109. A 37-year-old female with a long history of multiple sclerosis presents to her primary care physician complaining of dyspnea. She denies cough and fever but admits to right-sided chest pain. Her medical history is significant for an episode of atrial fibrillation diagnosed in the emergency department two weeks ago, which resolved spontaneously without intervention. She is wheelchairbound due to spastic paraparesis and has saccadic speech. Her only allergy is to penicillin. On physical examination, her blood pressure is 120/70 mmHg and her heart rate is 110/min and regular. Chest x-ray demonstrates a right-sided pleural effusion. Therapeutic thoracocentesis is performed, and pleural fluid analysis reveals the following: Protein 3.1 g/L RBC count 230/mm3 WBC count 150/mm3 LDH 220 IU/L Glucose 100 mg/dl Which of the following is the most likely cause of this patient's pleural effusion?
A. Congestive heart failure
B. Hypoalbuminemia
C. Pulmonary embolism
D. Aspiration pneumonia
E. Malignancy
110. A 43-year-old previously healthy male is hospitalized for acute pancreatitis. On day 3 of his admission, he develops respiratory distress. He is transferred to the intensive care unit and intubated. His initial ventilator settings are: FiO2 0.8 (80%) Respiratory rate 10/min Tidal volume 500 ml PEEP 5 mm H20 Ten minutes after being intubated, the man's blood pressure is 110/70 mmHg and his heart rate is 90/min. His arterial blood gases are: pH 7.42 pO2 105 mmHg pCO2 37 mmHg Which of the following is the best next step in the management of this patient?
A. Decrease the positive end expiratory pressure (PEEP)
B. Decrease the tidal volume
C. Decrease the FiO2
D. Decrease the respiratory rate
E. Increase the respiratory rate
111. A 35-year-old male from Wisconsin presents to his physician complaining of fever, night sweats, productive cough, and an unintentional 17-lb weight loss over the past 3 months. Several days ago, he also began to notice multiple skin lesions. He has no known medical problems and does not take any medications, nor does he use tobacco, alcohol or illicit drugs. He works outdoors in wood cutting and construction. Physical examination reveals a man of medium build in no apparent distress. His temperature is 38.4°C (101.1°F), blood pressure is 120/68 mm Hg, pulse is 86/min, and respirations are 14/min. Skin examination reveals multiple, well-circumscribed, verrucous, crusted lesions. Chest x-ray shows left upper lobe consolidation and two lytic lesions in the anterior ribs. Which of the following is the most likely cause of his current symptoms?
A. Disseminated tuberculosis
B. Sarcoidosis
C. Metastatic osteosarcoma
D. Blastomycosis
E. Coccidioidomycosis
112. A 35-year-old male was involved in a motor vehicle injury and suffered serious chest trauma. A chest tube was placed for a hemothorax. 800 cc of blood was evacuated from the chest, and, after ten days, the patient was discharged home. He returns again with a low-grade fever and dyspnea. CT scan reveals a complex loculated effusion with a thick surrounding peel. A chest tube is placed; however, after 24 hours, there is little drainage, and the patient continues to have a low-grade fever. What is the next step in his management?
A Surgery
B. Streptokinase into the chest tube
C. Increase the dose of IV antibiotics
D. Place a second chest tube
E. Pulmonary consult for bronchoscopy
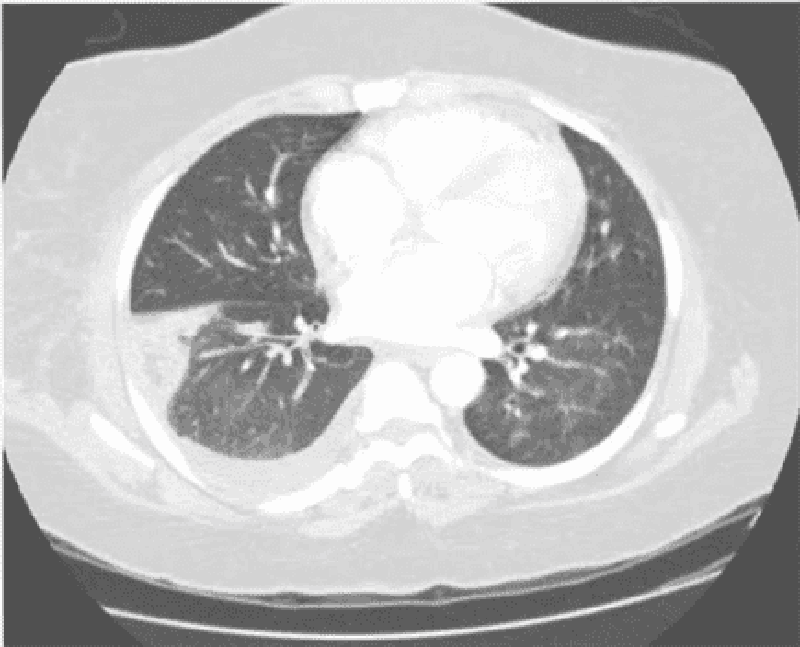
113. A 34-year-old woman presents with one week of low-grade fever, diarrhea, and lethargy plus two days of hemoptysis and severe pleuritic-type chest pain. In the past she abused heroin but is currently in a methadone program. She has a 20 pack-year cigarette smoking history. Her medical history is significant for HIV and hepatitis C infections. Her last CD4 count was 350/µl two months ago. PPD testing revealed 2 mm of induration at the same time. On physical examination today, her blood pressure is 130/80 mmHg, heart rate is 100/min, and temperature 38.1°C (100.6.F). Breath sounds are diminished at the base of the right lung. Chest CT is shown below. Which of the following is the most likely diagnosis?
A. Pulmonary tuberculosis
B. Pulmonary thromboembolism
C. Pneumocystis pneumonia
D. Bacterial pneumonia
E. Lung cancer
114. A 40-year-old white male develops a proximal deep vein thrombosis in the left lower extremity. Detailed history, examination and lab testing fail to reveal any obvious cause or risk factor for his deep venous thrombosis. Idiopathic deep vein thrombosis is diagnosed and the patient starts a 6month course of warfarin anticoagulation. What is the goal INR therapeutic range in this patient?
A 1.0 to 1.5
B. 1.5to2.0
C. 2.0 to 3.0
D. 2.5 to 3.5
E. Greater than 4
115. A 25-year-old man presents to the emergency room with shortness of breath and cough productive of blood tinged sputum for the past few days. He denies associated fever, arthralgias or weight loss. He has never had these symptoms before, and is extremely concerned. He has no history of recent travel or sick contacts. He smokes half a pack of cigarettes daily, and has had two sexual partners in the past six months. On physical examination, his temperature is 37.2°C (98.9.F), blood pressure is 120/70 mm Hg, pulse is 102/min, and respirations are 22/min. Lung auscultation reveals patchy bilateral rales. Chest x-ray demonstrates bilateral pulmonary infiltrates. His serum creatinine is 2.6 mg/dl and urinalysis shows dysmorphic red cells. Which of the following is the most likely cause of his current condition?
A. Basement membrane antibodies
B. Pneumocystis pneumonia
C. Infection with acid fast bacilli
D. Pulmonary thromboembolism
E. Cardiac valve infection
116. A 32-year-old female complains of a 'nagging' dry cough over the last 4 weeks. She says that the cough is present during the day and also wakes her from sleep at night. There is no associated shortness of breath, chest pain or wheezing. Her past medical history is significant for chronic rhinorrhea and an occasional itching skin rash. She takes no medications. Chest x-ray shows no abnormalities. One week of treatment with chlorpheniramine significantly improves her symptoms. Decrease in which of the following is most likely responsible her symptom relief?
A. Airway hyperreactivity
B. Bronchial inflammation
C. Acid aspiration
D. Nasal secretions
E. Bradykinin production
117. A 50-year-old male presents to his physician complaining of daytime somnolence. He reports that yesterday, he fell asleep while stopped at a red light. His wife adds that he is a habitual snorer, and sometimes seems to stop breathing for seconds at a time while sleeping. His past medical history is significant for hypertension, a 25 pack-year smoking history, and a two beer per day drinking habit. Physical examination reveals an obese, middle-aged man in no apparent distress. His pulse is 88/min, blood pressure is 160/100 mm Hg, and respirations are 14/min. The remainder of the physical examination, including chest auscultation, is within normal limits. Which of the following is the most appropriate next step in the management of this patient?
A. Prescribe methylphenidate
B. Pulmonary function testing
C. MRI of the upper airways
D. Nocturnal polysomnography
E. Dexamethasone suppression test
118. A 37-year-old male is being evaluated after a motor vehicle accident. He complains of right sided chest pain. Physical examination reveals mild bruising over the right chest wall, and is otherwise unremarkable. Chest x-ray shows no rib fractures but a solitary round lesion is seen in the right upper lobe of the lung. Upon further questioning the patient denies recent weight loss or appetite change. He has never smoked cigarettes. Which of the following is the most appropriate next step in the management of his lung lesion?
CT-guided biops
B. CT scan of the chest
C. Bronchoscopy
D. Obtain previous x-rays to compare
E. Obtain whole body CT scan
119. An obese 56-year-old female presents to her physician concerned that her asthma is worsening. She describes night-time cough and wheezing that have been increasing over recent months. She also reports feeling tired each morning because she works late hours and has no time to relax after dinner. On review of systems, the patient denies dyspnea on exertion, but acknowledges that her throat has been sore lately. Her past medical history is significant for bronchial asthma, type2 diabetes and hypertension. Her medications include an albuterol inhaler which she uses occasionally, lisinopril and aspirin. Her vital signs are within normal limits, and there are no abnormalities on physical exam. Which of the following is the most appropriate next step in the management of this patient?
. Discontinue lisinopril
B. Discontinue aspirin
C. Add inhaled fluticasone
D. Add pantoprazole
E. Add salmeterol
120. A 66-year-old male presents to the emergency room with shortness of breath. The symptoms started one week ago with a dry cough and exertional dyspnea. His past medical history includes hypertension and recent stenting for double-vessel coronary artery disease. He was hospitalized six months ago for pneumonia. He has a 35 pack-year smoking history. His temperature is 37.2 C (98.9F), blood pressure is 160/90 mmHg, and heart rate is 90 and regular. On examination, the patient is in mild respiratory distress, but he can speak in full sentences. Chest auscultation reveals decreased breath sounds at the lung bases, bilateral crackles and occasional wheezes. His ABG shows: pH 7.46 pO2 73mmHg pCO2 31mmHg Which of the following is the most likely explanation for this patient's symptoms?
A. Congestive heart failure
B. COPD exacerbation
C. Pulmonary embolism
D. Pneumothorax
E. Adult respiratory distress syndrome
121. A 55-year-old Caucasian man comes to the emergency department because of fever and productive cough, with foul-smelling sputum. He also complains of shortness of breath. His other medical problems include hypertension and hypercholesterolemia. In the past three months, he was admitted in the hospital two times for pneumonia. He has smoked one pack of cigarettes daily for 28 years and drinks 5-6 beers daily. Family history is not significant. His medications include hydrochlorothiazide and simvastatin. His temperature is 38.9 C (102 F), blood pressure is 120/70 mmHg, pulse is 112/min, and respirations are 24/min. The patient's pulse oximetry showed 89% at room air. Examination shows crackles at the right lung base. His chest x-ray shows right, lower lobe infiltrate. A CT scan of the chest shows no mass or obstruction. Which of the following is most likely responsible for this patient's symptoms?
A. Excessive smoking
B. Excessive alcohol intake
C. Depressed humoral immunity
D. Depressed cell-mediated immunity
E. Underlying malignancy
122. A 45-year-old female presents to the emergency department because of increasing somnolence and shortness of breath. Her past medical history is significant for hyperlipidemia, hypertension and type2 diabetes. She has never smoked and does not use drugs or alcohol. Her temperature is 36.7°C (98.F), blood pressure is 160/80 mm Hg, pulse is 80/min, and respirations are 16/min. Her BMI is 55 kg/m2. On physical examination, she is drowsy but able to respond to commands. Jugular venous distention is difficult to visualize due to a thick neck. Lungs are clear to auscultation. Heart sounds are distant. Abdomen is obese and non-tender. Lower extremities have edema bilaterally. There are no obvious focal deficits on neurologic examination. Chest x-ray is poor in quality but no obvious abnormalities are noted. EKG shows low voltage QRS complexes but no significant ST-segment or T-wave abnormalities. Laboratory studies show: Complete blood count: Hemoglobin 16.0 g/L Hematocrit 48% Mean corpuscular volume 85 fl Platelet count 224,000/mm3 Leukocyte count 6,600/mm3 Arterial blood gas: pH 7.30 pO2 60mmHg pCO2 69mm Hg Which of the following is the most likely cause of her condition?
A. Venous thromboembolism
B. Aspiration pneumonia
C. Pneumocystis pneumonia
D. Impaired chest wall compliance
E. Pulmonary edema
123. A 60-year-old Caucasian female comes to the physician because of progressive shortness of breath for the past month. She has had a 13.6 kg (30 lb) weight loss during this period. She has a history of hypertension and hypothyroidism and takes metoprolol and levothyroxine. She has smoked two packs of cigarettes daily for 35 years. Her temperature is 36.7 C (98 F), blood pressure is 130/70 mmHg, pulse is 80/min, and respirations are 20/min. On examination, decreased breath sounds and dullness to percussion are noted on the right, middle and lower lobes of the lung. Her chest x-ray is shown below. Which of the following is the most appropriate next step in the management?
A. Bronchoscopy
B. Mediastinoscopy
C. Thoracentesis
D. Video-assisted thoracoscopy
E. Open pleural biopsy
124. A 60-year-old male with a history of hypertension, diabetes, coronary artery disease, asthma, and cigarette smoking undergoes emergent laparotomy for a perforated peptic ulcer. He receives 4 liters of intravenous normal saline intraoperatively. Following the procedure, he is extubated without complication, but subsequently develops respiratory distress. Immediate arterial blood gas analysis on room air shows: PaO2 60mmHg pH 7.46 PaCO2 37mmHg HCO3 22mmHg His temperature is 37.2°C (98.9.F) and blood pressure is 126/76 mm Hg. Lung auscultation reveals bilateral rales. His arterial blood gas fails to improve with administration of 100% oxygen. What is the most likely cause of his respiratory distress?
A. Excessive anesthesia
B. Pulmonary edema
C. Pulmonary embolism
D. Aspiration pneumonia
E. Exacerbation of bronchial asthma
125. A 40-year-old man presents to the emergency room with shortness of breath, cough and hemoptysis for the past two days. He says he has never had symptoms like these before. His medical history is significant for a non-healing leg ulcer and chronic purulent nasal discharge. He has smoked a pack of cigarettes daily for the past 20 years. On physical examination, his temperature is 37.6°C (99.7°F), blood pressure is 130/90 mm Hg, pulse is 94/min and respiratory rate is 18/min. Lung auscultation reveals patchy rales bilaterally. Heart sounds are regular. A 2x3cm ulcer with rolled, undermined borders is noted on the right lower leg. Which of the following is the most likely explanation for his hemoptysis?
A. Pulmonary tuberculosis
B. Bronchogenic carcinoma
C. Wegener's granulomatosis
D. Mitral stenosis
E. Pulmonary embolism
126. A 62-year-old Caucasian male presents to your office because of a non-productive cough that is 'quite disturbing.' The cough has been present for several weeks. He visited your office two times before for poorly controlled hypertension, and was started on lisinopril. He usually takes aspirin, amlodipine, and metoprolol. He does not smoke or consume alcohol. His blood pressure is 130/90 mmHg and heart rate is 60/min. Physical examination reveals a bruit over the right carotid artery, but is otherwise normal. Which of the following is the most likely cause of this patient's complaint?
A. Inhibition of beta-adrenoreceptors
B. Inhibition of prostaglandin synthesis
C. Increased serum renin level
D. Low level of circulating catecholamines
E. High kinin level
127. A 46-year-old male is hospitalized with severe acute pancreatitis. Because of progressive respiratory difficulty, he is intubated and placed on mechanical ventilation. His weight is 70 kg (152 lb), blood pressure is 110/70 mmHg, and heart rate is 90/min. Chest x-ray shows patchy opacities bilaterally, consistent with pulmonary edema. His current ventilator settings are: assist control mode, respiratory rate of 12/min, tidal volume of 450 ml, FiO2 of 40%, and positive end-expiratory pressure (PEEP) of 5 cm H20. His blood gas readings are: pH 7.51 pCO2 22mmHg pO2 121mmHg Which of the following is the best next step in managing this patient?
A. Bronchodilator therapy
B. Decrease Fi02
C. Decrease respiratory rate
D. Increase tidal volume
E. Incentive spirometry
128. A 69-year-old male presents to the ER with severe shortness of breath for the past 12 hours. He reports that he has used his albuterol inhaler many times without relief. On review of systems he notes having had a mild fever yesterday that resolved with acetaminophen. The patient quit smoking 2 years ago but has a 100 pack year smoking history. On physical examination, his blood pressure is 150/90 mmHg and heart rate is 110/min. The patient is using accessory muscles of respiration. Expirations are prolonged, and there are wheezes bilaterally. Arterial blood gas (ABG) analysis reveals the following: pH 7.36 pO2 64 mmHg pCO2 57 mmHg HCO3 32 mEq/L The patient is treated with ipratropium and albuterol nebulizers and moxifloxacin. Which of the following additional therapies is most likely to benefit this patient?
A. Corticosteroids
B. Loop diuretic
C. Mucolytic agents
D. Aminophylline
E. Diltiazem
129. A 28-year-old male presents to the physician's office for a routine health maintenance examination. He has a two-year history of bronchial asthma for which he uses an albuterol inhaler. He states that he experiences asthma symptoms an average of 2 times per week, for which his albuterol inhaler provides relief. He has not had nighttime awakenings over the past month. He does not use tobacco, alcohol or illicit drugs. His family history is significant for asthma in his grandfather. Physical examination is unremarkable. Which of the following is the most appropriate next step in his management?
A. Add long-acting beta-2 agonist inhale
B. Add inhaled corticosteroids
C. Add oral theophylline
D. Add oral prednisone
E. Continue current medical regimen
130. A 25-year-old female presents to the emergency department with sudden-onset severe shortness of breath and wheezing. She has a history of asthma. On examination, she is unable to speak in full sentences and is using accessory muscles of respiration. She is intubated, mechanically ventilated and treated with continuous albuterol nebulization and intravenous methylprednisolone. Within six hours, her condition is improved. She is extubated and treated with hourly nebulizer treatments. The next morning, she complains of muscle weakness. On physical examination, she has difficulty lifting her arms over her head and mild hand tremors. Her vital signs are stable What should be the immediate next step in her management?
A. Check peak expiratory flow rate
B. Check chest x-ray, PA view
C. Check serum TSH level
D. Check serum electrolyte panel
E. Obtain electromyography (EMG)
131. A 26-year-old white female comes to the Emergency Room with severe shortness of breath. She has a long history of asthma with periodic exacerbations. She is taking an inhaled albuterol, inhaled steroid, salmeterol and cromolyn. Her temperature is 37.2C (99F), blood pressure is 150/90 mmHg, pulse is 110/min, and respirations are 24/min. On examination, she has moderate respiratory distress, prolonged expiratory phase, and significant wheezing all over the lung fields. Patient is admitted and is given nebulized albuterol, intravenous methyl prednisone, and oxygen. The next day her respiratory status improved. Her vital signs did not change much, except normalization of respiratory rate. Still scattered bilateral wheezes are heard on lung auscultation. The next day her laboratory values are: Hemoglobin 14 g/dL MCV 95 fL Leukocyte count 19,000/cmm Segmented Neutrophils 80% Bands 5% Lymphocytes 13% Eosinophils 0% Basophils 0% Monocytes 2% Chest x-ray obtained at the time of admission is normal, except for hyperinflated lung fields. What is the most probable cause of the abnormal lab findings in this patient?
A. Pneumonia
B. Hypersensitivity reaction
C. Myeloproliferative state
D. Metabolic disorder
E. Drug reaction
132. A 40-year-old black male presents with dyspnea and tachypnea of sudden onset. He says that he was diagnosed with deep venous thrombosis (DVT) of the lower extremities three times before. Ventilation/perfusion scan reveals mismatched perfusion defect. Venous ultrasonography is positive for DVT. You suspect that inherited predisposition to hypercoagulation may be present. Which of the following is the most common form of such a predisposition?
A. Protein C deficiency
B. Protein S deficiency
C. Antithrombin Ill deficiency
D. Factor V Leiden
E. Plasminogen disorders
133. A 45-year-old male immigrant from Haiti complains of cough and tenacious mucopurulent sputum for several months. He denies fever or chest pain, but notes shortness of breath and occasional blood-tinged sputum. He has received antibiotic treatment for similar symptoms twice in the past year. He has smoked 1 pack of cigarettes daily for the past 20 years. On physical examination, his temperature is 37.2°C (98.9.F), blood pressure is 120/68 mm Hg, pulse is 80/min, and respirations are 14/min. On lung auscultation there are coarse crepitations at the bilateral bases. Chest x-ray reveals prominent bronchioles in the lower lobes but is otherwise unremarkable. What is the most appropriate next step in the management of this patient?
A. High resolution CT scan of the chest
B. Bronchoscopy and alveolar lavage
C. Bronchography using non-iodinated contrast medium
D. Check sputum for acid fast bacillus (AFB)
E. Echocardiography
134. A 32-year-old male presents to your office complaining of daytime sleepiness and frequent nighttime awakenings. He says that his sleep gets disrupted by a choking sensation, sometimes accompanied by cough and dyspnea. After such episodes he typically has trouble falling back to sleep. The patient notes that his symptoms are somewhat improved when he sleeps with multiple pillows. Physical examination is unremarkable except for a BMI of 29 Kg/m2. What is the most likely diagnosis?
A. Restless leg syndrome
B. Asthma
C. Left ventricular failure
D. Obstructive sleep apnea
E. Gastroesophageal reflux disease
135. A 78-year-old man is seen in the doctor’s office for a nonproductive cough, 9-kg (20-lb) unintentional weight loss, and bilateral breast enlargement, all occurring within the past 6 months. He has smoked two packs per day for the past 40 years. His past medical history is otherwise unremarkable, and he takes no medications. His temperature is 36.7°C (98.1°F), blood pressure is 125/85 mm Hg, pulse is 68/ min and regular, respiratory rate is 15/min, and oxygen saturation is 99% on room air. There are crackles at the left lower lung field and a ridge of symmetric glandular tissue (1 cm in diameter) around the nipple-areolar complexes of both breasts. Complete blood cell count shows a WBC count of 6000/mm³ hemoglobin of 14.7 g/dL, and platelet count of 210,000/ mm³. All other laboratory results are normal. X-ray of the chest shows a focal 5-cm mass lesion in the left lower lung corroborated by CT scan. Which of the following is most likely histologic type of lung cancer present in this patient?
(A) Adenocarcinoma
(B) Bronchoalveolar cell carcinoma
(C) Large cell carcinoma
(D) Small cell carcinoma
(E) Squamous cell carcinoma
136. A 30-year-old patient with a history of mild persistent asthma (baseline peak expiratory flow rate of 85%) presents to the emergency department with shortness of breath and wheezing that has not relieved by her albuterol inhaler for the past 12 hours. She was able to tolerate pulmonary function tests and a set was performed. Which of the following is the most likely test result?
(A) Decreased FEV1, normal/increased FVC, decreased FEV1: FVC ratio, with post- bronchodilator FEV1 increased by 13%
(B) Decreased residual volume and total lung capacity
(C) Increased FEV1, increased FVC, normal FEV1: FVC ratio
(D) Increased residual volume, increased total lung capacity, increased FEV1
(E) Normal FEV1, decreased FVC, increased FEV1: FVC ratio
137. A 3-year-old boy presents to the emergency department with a fever and difficulty breathing. He is the product of a normal pregnancy and has been healthy since birth. His immunizations are up to date. This morning he appeared to be in his usual state of health and was dropped off at day care by his father. Later on, his teacher noticed that he had suddenly become fussy and flushed and could not be consoled with toys, rocking, or hearing a story. He also felt warm to the touch and was drooling more than usual. When she took his temperature, it was 39°C (102.2°F). His parents were contacted immediately, and the patient was brought to the emergency department. He appears toxic and anxious, and has loud labored breathing. He is sitting upright, bracing himself on his arms, with his neck hyperextended and mouth open. His temperature is 40°C (104°F), respiratory rate is 50/min, pulse is 140/min, blood pressure is 102/62 mm Hg, and oxygen saturation is 100% on room air. Lateral x-ray of the neck is shown in the image. Laryngoscopy reveals a large cherryred epiglottitis. What is the most appropriate next step in management?
(A) Antibiotic therapy
(B) Corticosteroids
(C) Nasotracheal intubation
(D) Observation
(E) Tracheostomy
138. A 27-year-old woman is 7 months pregnant with her first child. Her pregnancy has been uncomplicated to date. She presents to the emergency department complaining of sudden-onset, rightsided chest pain that is exacerbated with deep breathing and shortness of breath, which began 1 hour ago. She denies leg pain and notes that her legs began swelling during the sixth month of her pregnancy but the swelling has not worsened. Her temperature is 37.9°C (100.3°F), blood pressure is 130/87 mm Hg, pulse is 107/min and regular, respiratory rate is 24/min, and oxygen saturation is 90% on room air, increasing to 98% with 4 L oxygen via nasal cannula. Physical examination is significant for crackles at the lower right lung field and a negative Homans’ sign bilaterally. X-ray of the chest appears nor- mal. The D-dimer level is elevated. ECG shows sinus tachycardia, right-axis deviation, S wave in lead I, Q wave in lead III, and an inverted T wave in lead III. Which of the following is the most appropriate next step in diagnosis?
(A) Arterial blood gas analysis
(B) Doppler ultrasound of the lower extremity
(C) MRI of the lower extremity
(D) Pulmonary angiography
(E) Ventilation/perfusion scans
139. A 20-year-old African American woman presents with mild dyspnea on exertion and joint discomfort in her knees, wrists, and ankles. She also has a fever and red tender rash on her shins. Physical examination reveals hepatosplenomegaly, generalized lymphadenopathy, corneal opacities, and tender erythematous nodules on her legs. CXR shows bilateral symmetric hilar adenopathy. Transbronchial biopsy reveals noncaseating granulomas. Which of the following is the most likely cause for the eye lesion?
(A) uveitis
(B) diabetic complications
(C) steroids
(D) congenital origin
(E) infectious infiltration
140. A 74-year-old man with a history of smoking notices blood in his chronic daily sputum production. He has no fever or chills, but has lost 10 lb in the past 6 months. On examination, he has bilateral expiratory wheezes, and his fingers are clubbed. There are no lymph nodes and the remaining examination is normal. CXR reveals a left hilar mass. Which of the following suggests that the tumor is a small cell lung cancer?
(A) syndrome of inappropriate antidiuretic hormone (SIADH) secretion
(B) acanthosis nigricans
Cushing’s syndrome
(D) leukemoid reaction
(E) Stevens-Johnson syndrome
141. A 44-year-old woman presents with increased shortness of breath, cough, and sputum production. She has had asthma since childhood and uses her medications as directed. Recently, she noticed that her peak flow readings were decreasing after the symptoms started. On examination, she is in moderate respiratory distress, respirations 25/min, there are bilateral wheezes and oxygen saturation is 90% on room air. On her blood gas, the PCO2 is 50 mm Hg. Which of the following is the most likely mechanism for her carbon dioxide retention?
(A) impaired diffusion syndromes
(B) right-to-left shunt
(C) hyperventilation
(D) ventilation-perfusion ratio inequality
(E) mechanical ventilation at fixed volume
142. A 35-year-old HIV-positive man (CD4+ cell count 150/mm³) is seen in the emergency department with right-sided chest pain. The patient has become progressively dyspneic over the past few days. Suddenly, 30 minutes ago he noticed a sharp pain in his chest associated with shortness of breath. His temperature is 37.7° (99.9°F), blood pressure is 128/84 mm Hg, pulse is 102/min and regular, respiratory rate is 25/min, and oxygen saturation is 90% on room air. Physical examination reveals diminished right-sided breath sounds and hyperresonance. Jugular venous distention is 5 cm and there is no tracheal deviation. ECG shows sinus tachycardia. X-ray of the chest shows a rightsided pneumothorax occupying approximately 10% of the right thoracic cavity. Which of the following most likely caused this patient’s presentation?
Intravenous drug use
Kaposi’s sarcoma
(C) Mycobacterium tuberculosis
(D) Pneumocystis jiroveci pneumonia
(E) Toxoplasmosis
143. A 55-year-old man presents to his physician’s office with increasing dyspnea on exertion. He denies chest pain, diaphoresis, nausea, or vomiting. He has been involved in eight motor vehicle accidents in the past 3 years. Past medical history is significant for hypertension, for which he takes a diuretic. His temperature is 37.2°C (99.0°F), blood pressure is 121/82 mm Hg, pulse is 85/min, respiratory rate is 14/min, and oxygen saturation is 99% on room air. Physical examination is significant for a body mass index of 35 kg/m², a diffuse and laterally displaced point of maximal intensity, and an S3 gallop. Which of the following is the most appropriate next step in diagnosing his most likely underlying condition?
(A) Cardiac catheterization
(B) Echocardiogram
(C) Exercise tolerance test
(D) Polysomnography
(E) X-ray of the chest
144. A 74-year-old man presents to his primary care physician complaining of dyspnea and cough with blood-tinged sputum for the past several weeks. He has diabetes and elevated cholesterol. Medications include a sulfonylurea and a statin. The patient has a 50-pack-year smoking history and a family history of hypertension. His vital signs are within normal limits. Physical examination reveals abdominal striae and moon facies, along with a truncal fat distribution. X-ray of the chest reveals a single central nodule, and follow-up CT again demonstrates the nodule and multiple solid hepatic masses. Which of the following is the most likely diagnosis?
(A) Adenocarcinoma of the lung
(B) Carcinoma metastatic to the lung
(C) Large cell carcinoma of the lung
(D) Small cell carcinoma of the lung
(E) Squamous cell carcinoma of the lung
145. A 35-year-old homeless man presents to the emergency department with chief complaints of a cough and fever. He is intoxicated. He admits to drinking about a fifth of vodka every day and confirms a history of delirium tremens and blackouts. X-ray of the chest is significant for an air-fluid level in the superior segment of the right lower lobe. Which of the following is the most appropriate first-line agent for treating this patient’s condition?
(A) Azithromycin
(B) Clindamycin
(C) Isoniazid
(D) Moxifloxacin
(E) Piperacillin-tazobactam
146. A 5-month-old infant has failed to gain weight despite a good appetite. The child’s mother reports that the baby has up to eight bulky, foul-smelling, oily stools per day. A sweat chloride test reveals a chloride level of 78 mEq/L (normal: <60 mEq/L). Which of the following sequelae is most likely to occur as a result of this patient’s disease?
(A) Cirrhosis and subsequent hepatic failure
(B) Dehydration, electrolyte abnormalities, and acute hypotension
(C) Esophageal ulceration or strictures and upper gastrointestinal bleeding
(D) Purple lines on the gums, red-brown discoloration of the urine, and renal tubular acidosis
(E) Recurrent airway disease with eventual respiratory insufficiency associated with bronchiectasis
147. A 33-year-old farmer complains of recurrent episodes of wheezing after working in a barn where hay is stored. On auscultation, there are bibasilar crackles and heart sounds are normal. His laboratory work is normal with no increase in eosinophils and the chest x-ray (CXR) reveals patchy lower lobe infiltrates. Which of the following is the most likely diagnosis
(A) Asthma
(B) Chronic obstructive lung disease
(C) Hypersensitivity pneumonitis
(D) Bronchiectasis
(E) Sarcoidosis
148. A 57-year-old man with a 40-pack-per-year his- tory of smoking experiences symptoms of shortness of breath on exertion. He has bilateral wheezes on expiration and increased resonance to percussion of the chest. Pulmonary function tests confirm the diagnosis of chronic obstructive lung disease (COPD). Which of the following is the best definition of this condition?
(A) It is caused by bronchial asthma
(B) It is preceded by chronic bronchitis
(C) It is airflow limitation that is not fully reversible
(D) It is due to destruction and dilatation of lung alveoli
(E) Is due to small airways disease only
149. An agitated and nervous 24-year-old woman has had severe wheezing and shortness of breath for 2 days. After receiving oxygen, steroids, and salbutamol (Ventolin) in the emergency room, her breathing improves. She is still wheezing and now feels tremulous and anxious with a pulse of 110/min and respirations 30/min. Arterial blood gases on oxygen reveal a pH of 7.40, PO2 340 mm Hg, PCO2 40 mm Hg, and bicarbonate of 24 mEq/L. She is hospitalized for further treatment. Which of the following treatments or medications should be avoided in her?
(A) Theophylline
(B) Sedatives
(C) Corticosteroids
(D) Sympathomimetic amines
(E) Intravenous (IV) fluids
150. A 29-year-old woman has a long history of mild asthma. She now has a flare and experiences recurrent episodes of bronchial obstruction, fever, malaise, and expectoration of brownish mucous plug. On examination, there is bilateral wheezing. Infection is suspected and a CXR reveals upper lobe pulmonary infiltrates. The eosinophil count is 2000/mL, and serum precipitating antibodies to Aspergillus are positive. Which of the following is the most appropriate next step in management?
(A) antihelminthic therapy
(B) A short course of systemic glucocorticoid therapy
(C) Desensitization treatment
(D) high-dose glucocorticoids by puffer
(E) Long-term systemic glucocorticoid therapy
151. A 31-year-old African American man presents with dyspnea on exertion. He also has fever and red tender rash on his shins. Physical examination reveals fine inspiratory crackles in both lower lung lobes and tender erythematous nodules on his legs. CXR shows bilateral hilar adenopathy and reticulonodular changes in both lungs. Transbronchial biopsy reveals noncaseating granulomas. Which of the following is the most appropriate next step in management?
(A) aspirin
(B) isoniazid (INH) and streptomycin
(C) steroids
(D) nitrogen mustard
(E) no therapy
152. A 53-year-old man with a long respiratory his- tory is admitted to the hospital because of increasing shortness of breath and sputum production. He is started on antibiotics and inhaled bronchodilators and anticholinergic agents. The next day he is found in his room confused and sleepy. A PCO2 determination reveals severe hypercarbia (PCO2 70 mmHg). Which of the following explanations regarding his elevated PCO2 is correct?
(A) occurs only with CO2 inhalation
(B) does not occur in obstructive lung disease
(C) does not occur in restrictive lung disease
(D) may worsen with oxygen administration
(E) occurs with chronic hypocapnia
153. A 30-year-old man presents to the resuscitation bay with gunshot wounds in the anterior and posterior left chest. Although in distress and dyspneic, the patient is cooperative. He has a patent airway and is moving all extremities. His pulse is 120/min, blood pressure is 120/90 mm Hg, and respiratory rate is 30/min. He has bounding distal pulses, and no other injuries are identified on secondary examination. X-ray of the chest reveals fluid in the pleural space, and a left chest tube thoracostomy yields 600 mL of bright red fluid. Over the next hour 750 mL of blood is collected. What is the most ap- propriate next step in management?
(A) Autotransfuse with the collected blood and continue to observe closely
(A) Autotransfuse with the collected blood and continue to observe closely
(C) Left thoracotomy
(D) Remove the chest tube and suture the inci- sion closed
(E) Thoracentesis
154. A 38-year-old man is being seen in his physician’s office after being involved in a car accident. He has a vague pain along his right sternal border, where he crashed into the steering wheel. His temperature is 36.6°C (97.8°F), pulse is 80/min, blood pressure is 123/75 mm Hg, respiratory rate is 14/min, and oxygen saturation is 99% on room air. Physical examination is significant for point tenderness over the right sternal border. X-ray of the chest shows no broken ribs but a single, wellcircumscribed pulmonary nodule, 1.5 cm in diameter, located in the left lower lung field. A search through the patient’s electronic medical file reveals that he had an x-ray of the chest taken 2 years ago. The radiology report from that time reveals that the nodule was only 0.75 cm in diameter. To characterize the lesion, CT of the chest is performed and shows dense, flocculated calcification within the lesion. Which of the following risk factors most increases the chances of malignancy in this patient?
(A) Increased doubling time of tumor
(B) Increased patient age
(C) Nodule diameter of 1.5 cm or higher
(D) Presence of discrete border
(E) Presence of flocculated calcification
155. A 21-year-old nonsmoking college student comes to the local emergency department because pf cough, weight loss, and low-grade fever. Occasionally his sputum is tinged with blood. X-ray of the chest is shown in the image. He reports traveling to Haiti on a “medical mission” trip several years ago. Which of the following is the most likely diagnosis?
(A) Aspergillosis
(B) Klebsiella infection
(C) Lung cancer
(D) Sarcoidosis
(E) Tuberculosis
156. A 63-year-old woman is seen in the emergency room with acute shortness of breath. There is no history of heart or lung problems in the past. She was recently diagnosed with breast cancer and is undergoing active treatment. On examination, her blood pressure is 120/80 mm Hg, pulse 100/min, and heart and lungs are normal. There are no clinical signs of deep venous thrombosis (DVT). Which of the following investigations is most likely to rule out a pulmonary embolism (PE)?
(B) normal electrocardiogram (ECG)
(C) normal ventilation-perfusion lung scan @
normal CXR
Normal ventilation scan
Normal magnetic resonance image (MRI)
157. A 53-year-old man presents to the clinic with complaints of increasing shortness of breath, a nagging cough, and weight loss over several months. He reports no history of cigarette smoking but has worked underground in the New York City subway system for the past 20 years. Spirometry demonstrates an FEV1: FVC ratio of 0.7 and an FEV1 value that is 60% of expected. The FEV1 improves to 70% of expected with bronchodilator treatment. Which of the following is the most likely diagnosis?
(A) Asthma
(B) Chronic aspiration
(C) Chronic obstructive pulmonary disease
(D) Histoplasmosis
(E) Tuberculosis
158. A 22-year-old woman with mild persistent asthma comes to the primary care clinic after an emergency department visit 2 days ago for an acute asthma exacerbation. She notes an increase in frequency of wheezing and shortness of breath for the past 4 months, with daily symptoms, and has been symptomatic for at least 2 nights per week. She has also had three emergency department visits during the same period. Her current asthma medications include montelukast (leukotriene inhibitor) daily and an albuterol inhaler as needed. The patient’s peak flow is 75% of predicted. Which of the following is the most appropriate next step in management?
(A) Add a long-acting inhaled β-adrenergic agonist and low-dose inhaled steroid to the regimen (A) Add a long-acting inhaled β-adrenergic agonist and low-dose inhaled steroid to the regimen
(B) Add systemic steroids to the regimen
(C) Admit to the hospital for further pulmonary work-up
(D) Discontinue the leukotriene inhibitor and change the regimen to daily low-dose in- haled steroids (E) Start cromolyn sodium
159. A 78-year-old woman is seen in the emergency department for difficulty breathing and cough over the past 4 hours. She has a history of congestive heart failure for which she takes hydrochlorothiazide, metoprolol, and enalapril. Her oxygen saturation is 92% on room air. On examination there is a high-pitched systolic crescendodecrescendo murmur best heard at the right upper sternal border with radiation to the carotids, and rales are present in both lung fields on inspiration. There is 2+ symmetrical pitting edema bilaterally in the lower extremities. X-ray of the chest shows an enlarged heart and prominent pulmonary vasculature. Which of the following is the most likely cause of the patient’s pulmonary edema?
(A) Decreased capillary fluid oncotic pressure
(B) Decreased interstitial fluid hydrostatic pressure
(C) Increased capillary fluid hydrostatic pressure
(D) Increased capillary permeability
(E) Increased interstitial fluid oncotic pressure
160. A 40-year-old woman has been complaining of a 3-year history of increasing dyspnea and fatigue. She has no other medical illness. Physical examination reveals increased jugular venous pressure (JVP) with prominent c-v wave, and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests show a slight restrictive pattern. Primary pulmonary hypertension is suspected. Which of the following is the most appropriate test to confirm the diagnosis?
(A) open lung biopsy
(B) pulmonary angiography
(C) cardiac catheterization
(D) noninvasive exercise testing
(E) electrophysiologic testing
161. A 56-year-old man is evaluated for chronic cough. It is present most of the time and is progressively getting worse over the past 3 years. With the cough he usually has white to yellow sputum that he has to expectorate. There is no history of wheezing, asthma, congestive heart failure (CHF), or acid reflux disease. He currently smokes one pack a day for the past 25 years. On examination, his chest is clear. CXR is normal and his forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) on spirometry are normal. Which of the following is the most likely diagnosis?
(A) chronic obstructive pulmonary disease (COPD
(B) early cor pulmonale
(C) chronic bronchitis
(D) asthma
(E) emphysema
162. A 58-year-old man is recently diagnosed with bowel cancer. He now complains of vague chest discomfort and shortness of breath. On examination, he is unwell, blood pressure 90/50 mm Hg, pulse 110/min, respirations 26/min, and oxygen saturation 88%. His lungs are normal on auscultation, the JVP is 8 cm, and P2 is loud. There is no edema or leg tenderness on palpation. A quantitative (ELISA) D-dimer assay is positive, ECG reveals sinus tachycardia, and cardiac enzymes are negative. The lung scan is read as high probability for PE. Which of the following tests is most likely to help in guiding emergent therapy?
(A) echocardiogram
(B) CT scan
(C) venous ultrasound of the legs
(D) contrast phlebography
(E) pulmonary function tests
163. A 35-year-old man is evaluated for symptoms of shortness of breath. He reports no other lung or heart disease. He smokes half pack a day for the past 10 years. On examination, his JVP is 2 cm, heart sounds normal, and lungs are clear. A CXR shows hyperinflation and increased lucency of the lung fields. A chest CT reveals bullae and emphysematous changes, while pulmonary function tests show an FEV1/FVC ratio of <70%. Evaluation of his family reveals other affected individuals. Which of the following is the most likely diagnosis?
(A) alpha1-antitrypsin deficiency
(B) beta-glycosidase deficiency
(C) glucose-6-phosphatase deficiency
(D) glucocerebrosides deficiency
(E) growth hormone deficiency
164. A 23-year-old man notices a gradual but progressive increase in breathing difficulty. He has a long history of back pain with prolonged morning stiffness. He has also had an episode of iritis in the past. On examination, there is reduced range of motion in the lumbar spine with forward flexion and pain on palpation of the sacroiliac joint and surrounding soft tissue. X-rays of the pelvis show erosions and sclerosis of the sacroiliac joint. Which of the following is the most likely pulmonary complication of this condition?
(A) fibrocavitary disease
(B) airflow obstruction
(C) bilateral lower lobe involvement
(D) pleural effusions
(E) hilar adenopathy
165. A 45-year-old Haitian immigrant presents to the emergency department with a chief complaint of productive, blood-tinged cough for 2 months. He has been in the United States for 1 month. His temperature is 40.1°C (104.2°F) and heart rate is 105/min. On physical examination he appears cachectic, and pulmonary rales are heard throughout his lung fields. X-ray of the chest reveals multiple bilateral upper lobe cavitary lesions with associated intrathoracic adenopathy. Results of sputum culture are pending. Which of the following tuberculosis medications can potentially cause optic neuritis?
(A) Ethambutol
(B) Isoniazid
(C) Levofloxacin
(D) Pyrazinamide
(E) Rifampin
166. A 30-year-old man has episodes of wheezing and shortness of breath two to three times per week. Approximately every 2 weeks he awakens at night due to cough and difficulties breathing. He reports having similar symptoms since he was a child, but believes that they are worsening somewhat now. His symptoms are worsened by cold air and exercise and are improved by rest. Which of the following is the most appropriate treatment?
(A) Daily high-dose inhaled corticosteroid and β-agonist when needed
(B) Daily high-dose inhaled corticosteroid with oral steroids for exacerbations and short-acting β-agonist when needed
(C) Daily low-dose inhaled corticosteroid and short-acting β-agonist when needed
(D) Daily oral steroids and long-acting β-agonist
(E) Short-acting β-agonist when needed
167. A 44-year-old woman has been complaining of a 4-year history of increasing dyspnea and fatigue. Physical examination reveals increased JVP and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests show a slight restrictive pattern. A diagnosis of primary pulmonary hypertension is made. Which of the following is the most likely cause of death in this condition
Intractable left ventricular failure
(B) intractable respiratory failure
(C) massive PE
(D) intractable right ventricular failure or sudden death
(E) myocardial infarction
168. A 63-year-old woman presents with dyspnea and coughing up foul smelling purulent sputum. She has had many similar episodes in the past. There are no other constitutional symptoms and she denies excessive alcohol intake. On physical examination, she appears chronically ill with clubbing of the fingers. Heart sounds are normal, JVP is measured at 4 cm, and there are inspiratory crackles heard at the lung bases posteriorly. There is no hepatosplenomegaly or any palpable lymph nodes. CXR shows scaring in the left lower lobe, which on chest CT scan is identified as cystic changes with airway dilatation and bronchial wall thickening. Which of the following is the most appropriate initial next step in management?
(A) antibiotics and postural drainage
(B) steroids
(C) radiotherapy
(D) aerosols
(E) INH
169. A 65-year-old smoker previously diagnosed with chronic obstructive pulmonary disease presents to the emergency department complaining of worsening cough and sputum production. She reports feeling breathless when climbing the stairs to her first floor walk-up apartment, and has moderate difficulty in providing her history in complete sentences. X-ray of the chest shows hyper inflated lungs with flattened diaphragms, attenuated vascular markings, and a narrow mediastinum. What agent(s) will provide the greatest relief of symptoms in the emergency department?
169. A 65-year-old smoker previously diagnosed with chronic obstructive pulmonary disease presents to the emergency department complaining of worsening cough and sputum production. She reports feeling breathless when climbing the stairs to her first floor walk-up apartment, and has moderate difficulty in providing her history in complete sentences. X-ray of the chest shows hyper inflated lungs with flattened diaphragms, attenuated vascular markings, and a narrow mediastinum. What agent(s) will provide the greatest relief of symptoms in the emergency department?
(B) Antibiotics
(C) Magnesium sulfate
(D) N-acetylcysteine
(E) Theophylline
170. A 75-year-old man develops increased ventilatory requirements several days after requiring intubation for respiratory failure. X-ray of the chest shows bilateral infiltrates, and based on his ventilatory settings, the ratio of the partial arterial pressure of oxygen to the fraction of inspired oxygen (PaO2:FiO2) is 190. Which of the following is the most common underlying etiology of acute respiratory distress syndrome?
(A) Aspiration of gastric contents
(B) Drug overdose
(C) Lung or bone marrow transplantation
(D) Massive blood transfusion
(E) Sepsis
171. After an uncomplicated pregnancy and cesarean section for breech presentation, twins are born at 32 weeks’ gestation to a 24-year-old primigravida mother. Twin A weighs 1610 g (3.5 lb) and has Apgar scores of 8 and 9 at 1 and 5 minutes, respectively. Twin B weighs 1600 g (3.5 lb) and has Apgar scores of 7 and 8 at 1 and 5 minutes, respectively. Within minutes of birth, twin B becomes mildly cyanotic and tachypneic with subcostal retractions, expiratory grunting, and nasal flaring. Twin B’s blood pressure is 58/39 mm Hg, heart rate is 130/min, respiratory rate is 100/min, and temperature is 37.0°C (98.6°F). Twin B is intubated and given 70% fraction of inspired oxygen. Compared to twin A, what is twin B at greater risk of developing?
(A) Apnea of prematurity
(B) Gastroesophageal reflux disease
(C) Hyperbilirubinemia
(D) No difference because they are both pre- mature
(E) Retinopathy of prematurity
172. A 32-year-old white man with HIV and a re- cent CD4+ cell count of 400/mm³ presents to the emergency department with a 3-day history of fever, anorexia, cough, and night sweats. He recently returned from a camping vacation in Arizona, approximately 1 month prior to presentation. He also describes diffuse joint pains. His temperature is 38.9°C (102°F), oxygen saturation is 99% on room air, and there is a rash on his arms and hands. There is dullness to percussion at the right lung base. X-ray of the chest reveals a small right-sided infiltrate and hilar lymphadenopathy. Sputum analysis does not reveal any organisms. He reportedly had a negative purified protein derivative test 2 months ago. Which of the following is the most likely diagnosis?
(A) Coccidioidomycosis
(B) Histoplasmosis
(C) Lung carcinoma
(D) Pneumocystis jiroveci pneumonia
(E) Sarcoidosis
173. A 55-year-old man was admitted to the hospital 2 weeks ago for rapid onset of cough, fatigue, and pleuritic chest pain. He has worked as a sandblaster for the past year. When first seen in the hospital, he denied hemoptysis and smoking. Currently, the patient is intubated and on assist-control ventilation. His temperature is 36.7°C (98°F), pulse is 96/min, blood pressure is 138/85 mm Hg, and respiratory rate is 18/ min. A recent arterial blood gas study showed a pH 7.42, arterial carbon dioxide pressure of 36 mm Hg, and arterial oxygen pressure of 110 mm Hg while on 100% oxygen. Physical examination is significant for diffuse crackles throughout both lung fields, a loud pulmonic component of the second heart sound, and jugular venous distention of 9 cm with a prominent A wave, a left parasternal heave, and symmetric 3+ lower extremity pitting edema. Which of the following is the most likely diagnosis?
(A) Asbestosis
(B) Berylliosis
(C) Byssinosis (D) Coal worker’s pneumoconiosis
Silicosis
174. A 32-year-old man develops symptoms of wheezing, cough, and shortness of breath. He has bilateral expiratory wheezes, and the rest of the examination is normal. Further evaluation with pulmonary function tests reveals a reduced FEV1/FVC ratio that corrects with bronchodilators. Which of the following statements about a diagnosis of idiosyncratic asthma (also called nonatopic) is correct?
(A) known antigenic stimulus
(B) adult onset
(C) history of atopy
(D) positive skin tests
Igh immunoglobulin E (IgE) levels
175. A 28-year-old man presents with coughing up blood and sputum. He gives a history of recur- rent pneumonias and a chronic cough productive of foul-smelling purulent sputum. He has no other past medical history and is a lifetime nonsmoker. On physical examination, there are no oral lesions, heart sounds are normal, and wet inspiratory crackles are heard at the lung bases posteriorly. He also has clubbing of his fingers, but there is no hepatosplenomegaly or any palpable lymph nodes. CXR show fibrosis and pulmonary infiltrates in the right lower lung. Which of the following is the most appropriate initial diagnostic test?
(A) chest CT scan
(B) bronchoscopy
(C) bronchography
(D) open thoracotomy
(E) bronchoalveolar lavage

176. A 25-year-old man is recovering in the hospital from an open repair of his broken femur, which he suffered during an automobile accident. On postoperative day 3 he develops sudden onset shortness of breath and vague chest discomfort. His temperature is 37.6°C (99.6°F), heart rate is 108/min, blood pressure is 95/62 mm Hg, respiratory rate is 42/min, and oxygen saturation is 89% on room air. Physical examination is significant for jugular venous distention to 9 cm and an accentuated pulmonic component of S2. A pulmonary angiogram is shown in the image. Which of the following is most likely to be decreased?
(A) Airway resistance
(B) Alveolar dead space
(C) Alveolar ventilation
(D) Pulmonary compliance
(E) Pulmonary vascular resistance
177. A 51-year-old man presenting to the clinic for routine examination mentions that he has not been able to get over the flu. Further questioning clarifies that he has had a nonproductive cough for the past 3–4 months and is unable to sustain his normal walking pace for prolonged periods. He reports feeling more fatigued than he recalls feeling last year. His medical history is significant for hypertension, alcoholism, and obesity. His blood pressure is well controlled on losartan and hydrochlorothiazide. He has no known drug allergies. His mother died of complications of type 2 diabetes mellitus. His father had a fatal myocardial infarction at age 56 years. The patient smokes half a pack of cigarettes per day and has done so for the past 7 years. He has worked all his adult life as an accountant and has no known exposures to asbestos or organic dusts. His blood pressure is 134/96 mm Hg, heart rate is 78/min, respiratory rate is 16/min, temperature is 37°C (98.6°F), and oxygen saturation is 94% on room air. Lung examination reveals bilateral inspiratory crackles in the lung bases. High-resolution CT shows patchy areas of ground glass, reticular abnormalities, and traction bronchiectasis. Laboratory findings are normal except for an elevated erythrocyte sedimentation rate of 54 mm/hr. What is the recommended treatment for this patient’s cough?
(A) Change the antihypertensive agent
(B) Prescribe amantadine
(C) Prescribe bronchodilators and long-term domiciliary oxygen therapy
(D) Prescribe glucocorticoids
(E) Resect diseased lung fields
178. A 30-year-old woman presents to her physician’s office because of 3 months of nonproductive cough, exertional dyspnea, fatigue, malaise, and blurred vision. She denies weight loss, fever, chills, sweats, recent travel, or sick contacts. She works on the assembly line of an electronics plant. Vital signs are unremarkable. Physical examination reveals she has tender red papules over her shins. The patient said she first noticed the bumps when she changed oral contraceptive pills (her only medication), but assumed they would disappear. X-ray of the chest shows bilateral hilar lymphadenopathy with pulmonary infiltrates. Laboratory findings are: WBC count: 5600/mm3 Hemoglobin: 14.3 g/dL Platelet count: 300,000/mm3 Na+: 140 mEq/L K+: 4.2 mEq/L Cl−: 108 mEq/L Ca2+: 16 mg/dL CO2: 24 mmol/L Blood urea nitrogen: 10 mg/dL Creatinine: 1.0 mg/dL Culture of bronchoalveolar lavage fluid is neg- ative. Which of the following is the most likely diagnosis?
Berylliosis
(B) Fungal infection
(C) Lymphoma
(D) Sarcoidosis
(E) Tuberculosis
179. A 38-year-old woman has been complaining of a 2-year history of increasing dyspnea and fatigue. Physical examination reveals increased JVP and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests show a slight restrictive pattern. Primary pulmonary hypertension is diagnosed. Which of the following treatments is helpful in this condition?
A) corticosteroids
(B) nitrates
(C) alpha-adrenergic blockers
(D) calcium channel blockers
(E) angiotensin-converting enzyme (ACE) inhibitors
180. A 5-year old girl is brought to the emergency department in December by her mother, who complains that her daughter seems confused. The mother reports that her daughter has complained of intermittent headaches since the two of them moved into the first floor of an older apartment building 6 months ago. The mother has been at home with the daughter for the past 24 hours and the girl appears lethargic and is complaining of joint aches, nausea, and a headache. Her pulse is 120/min, blood pressure is 130/85 mm Hg, respiratory rate is 25/min, and oxygen saturation is 100% on room air. The girl’s mother also notes having a slight headache that started yesterday. Which of the following diagnostic tests should be most rapidly pursued?
(A) Arterial blood gas
(B) CT scan of the head
(C) Direct laryngoscopy
(D) ECG
(E) Toxicology screen
181. A 1-year-old child with cerebral palsy secondary to perinatal asphyxia presents to her general pediatrician for a well-child visit. She was delivered at 37 weeks’ gestation by emergency cesarean section for a tight nuchal chord. The patient has severe spastic quadriparesis that is limiting her movements. She also has mental retardation and is unable to speak. She has received physical and occupational therapy since early infancy; however, her parents are concerned by her lack of improvement. Which of the following is the best choice for treatment of spasticity in this child?
(A) Baclofen
(B) Botulinum toxin
(C) Carbamazepine
(D) Discontinue physical therapy
(E) Hyperbaric oxygen
182. A 58-year-old man presents to the emergency department complaining of fever and chills. The fever started last night and has not sub- sided, even though he took acetaminophen. He had a successful appendectomy 3 days ago and was discharged from the hospital 2 days ago. His only medication is ibuprofen, which is adequately controlling his pain. He is a 30-pack-year smoker with a chronic cough productive of white sputum. He has noticed increased sputum production, which has become yellowish-green. He denies dysuria, urgency, or frequency. His temperature is 38.4°C (101.1°F), heart rate is 88/min, respiratory rate is 16/min, and blood pressure is 126/74 mm Hg. On examination he appears to be tired but not in acute distress. Pulmonary examination is limited be- cause deep inhalation causes coughing and slight abdominal pain. There is no tactile fremitus or dullness to percussion. He has a slightly erythematous, appropriately tender healing incision in the right lower quadrant without exudates and normal active bowel sounds. Extremities are warm and well perfused without erythema or edema. Pulses are intact. Which of the following most likely could have prevented this condition?
(A) Aggressive incentive spirometry
(B) Early removal of the Foley catheter
(C) Early removal of the intravenous catheter
(D) Pre- and postoperative antibiotic prophylaxis
(E) Use of compression stockings and subcutaneous heparin
183. A 64-year-old woman is admitted to the hospital with right lobar pneumonia and sepsis syndrome. She becomes progressively more short of breath and hypoxemic requiring intubation and mechanical ventilation. Her repeat CXR in the intensive care unit now shows diffuse pulmonary infiltrates and a diagnosis of acute respiratory distress syndrome (ARDS) is made. Which of the following mechanisms is the most likely cause for the early exudative phase of ARDS?
(A) increased lung compliance
(B) increased interstitial fibrosis
(C) increased vascular permeability to fluid and proteins
(D) decreased pulmonary perfusion
(E) decreased ventilatory dead space
184. A 24-year-old African American woman presents with mild dyspnea on exertion, fever, and a rash on her legs. Her symptoms have come on gradually and she reports no pleuritic chest pain, hemoptysis or sputum production. She has no significant past medical history, smokes 10 cigarettes/day and is not taking any medications. Physical examination reveals generalized lymphadenopathy and tender erythematous nodules on her legs. CXR shows bilateral symmetric hilar adenopathy and reticulonodular changes in both lungs. She has a restrictive lung disease pattern on pulmonary function testing. Which of the following is the most likely diagnosis?
Hodgkin’s disease
Tuberculosis
(C) rheumatic fever
(D) sarcoidosis
(E) rheumatoid arthritis (RA)
185. A 30-year-old man presents with coughing up blood and sputum. There is no associated dyspnea, fever, or pleuritic chest pain. His past medical history is significant for recurrent pneumonias and a chronic cough productive of foul-smelling purulent sputum. The sputum production is usually worse when lying down and in the morning. He quit smoking 5 years ago and started when he was 18 years old. On physical examination, he appears chronically ill with clubbing of the fingers. Wet inspiratory crackles are heard at the lung bases posteriorly. CXR shows scaring in the right lower lobe, which on chest CT scan is identified as airway dilatation, bronchial wall thickening, and grapelike cysts. Which of the following is the most likely diagnosis?
(A) bronchiectasis
(B) chronic bronchitis
(C) disseminated pulmonary tuberculosis
(D) pulmonary neoplasm
(E) chronic obstructive emphysema
186. A 23-year-old man is experiencing a flare of his asthma. He is using his salbutamol inhaler more frequently than usual and despite increasing his inhaled steroids he is still short of breath. Previously his asthma was considered mild with no severe exacerbations requiring oral steroids or hospitalization. With his flare, he has recurrent episodes of bronchial obstruction, fever, malaise, and expectoration of brownish mucous plugs. On examination, there is bilateral wheezing. The heart, abdomen, neurologic, and skin exams are normal. CXR reveals upper lobe pulmonary infiltrates; the eosinophil count is 3000/mL, and serum precipitating antibodies to Aspergillus are positive. Which of the following is the most likely diagnosis?
(A) ascaris infestation
(B) allergic bronchopulmonary aspergillosis
(C) Churg-Strauss allergic granulomatosis
(D) Löeffler’s syndrome
(E) hypereosinophilic syndrome
187. A 34-year-old African American man presents with mild dyspnea on exertion and joint discomfort in his knees, wrists, and ankles. He also has a fever and red tender rash on his shins. Physical examination reveals hepatosplenomegaly, generalized lymphadenopathy, and tender erythematous nodules on his legs. CXR shows bilateral symmetric hilar adenopathy. Which of the following laboratory findings is not characteristic of this condition?
(A) hyperglobulinemia
(B) elevated ACE level
(C) elevated sedimentation rate (ESR)
(D) elevated serum calcium
(E) normal gallium scan
. A 66-year-old man has progressive shortness of breath due to COPD. He is currently able to do his activities of daily living, but has trouble walking more than one block. His physical examination reveals hyperinflation, increased resonance to percussion, and bilateral expiratory wheezes. He is on appropriate medical therapy for his stage of COPD. Which of the following is also indicated in the management of this condition?
(A) meningococcal vaccination
(B) yearly influenza vaccination
(C) weight reduction if obese
(D) Haemophilus influenzae B vaccination
(E) pneumococcal vaccination
. A 55-year-old woman presents with coughing up blood and sputum. She gives a history of recurrent pneumonias and a chronic cough productive of foul-smelling purulent sputum. The sputum production is worse on lying down and in the morning. On physical examination, she appears chronically ill with clubbing of the fingers. Wet inspiratory crackles are heard at the lung bases posteriorly. There are no hepatosplenomegaly or any palpable lymph nodes. CXR shows scaring in the right lower lobe, which on chest CT scan is identified as airway dilatation, bronchial wall thickening, and grapelike cysts. Which of the following is a recognized precursor to this patient’s condition?
(A) bronchial asthma
(B) cigarette smoking
(C) lung infection and impairment of drainage
(D) lung cancer
(E) silicosis
190. A 50-year-old man presents with excessive day- time sleepiness and a history of snoring. One week ago, he fell asleep while driving his car and got into a minor accident. On examination, he is obese (body mass index [BMI] >30) and his blood pressure is 160/90 mm Hg. His lungs are clear and heart sounds are distant. Which of the following is the most likely explanation for the symptoms associated with this condition?
(A) related to cardiac dysfunction
(B) neuropsychiatric and behavioral
(C) pulmonary
(D) gastrointestinal (GI)
(E) musculoskeletal
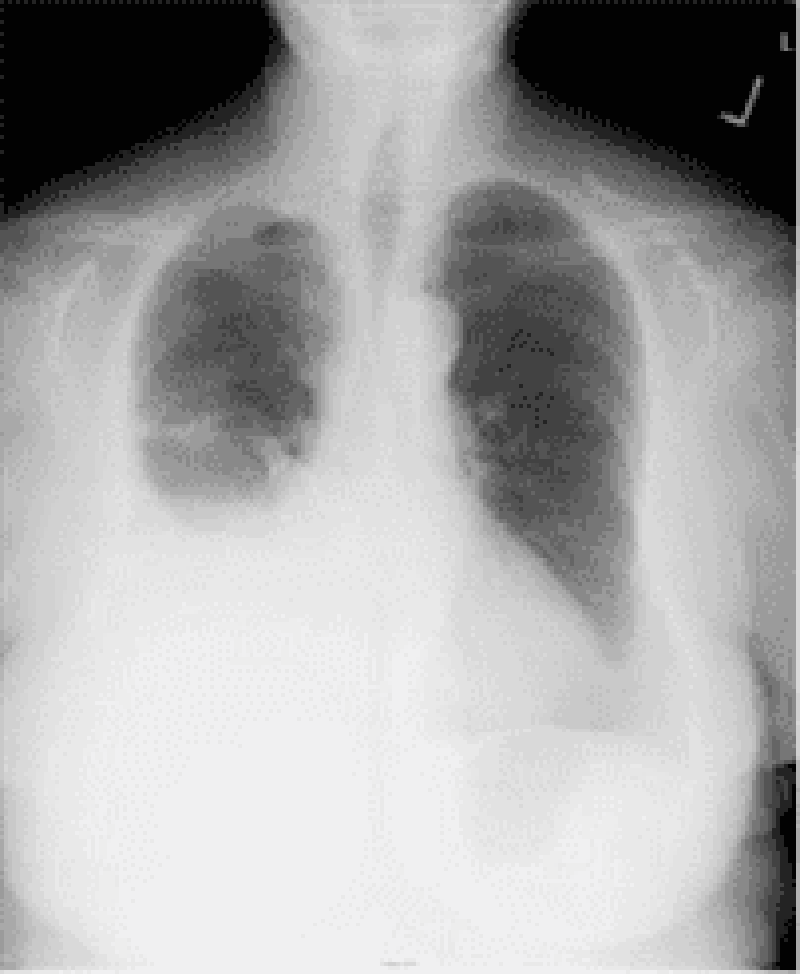
A 58-year-old steam pipe worker presents with a vague ache in the left chest and mild dyspnea of several months’ duration. There is dullness on percussion of the left chest associated with diminished breath sounds. His CXR is shown in Fig. Which of the following is the most likely diagnosis?
(A) pleural metastases
(B) Paget’s disease
(C) mesothelioma and asbestosis
(D) pleural effusion
(E) multiple myeloma
192. A 23-year-old man presents with coughing up blood and sputum. He gives a history of recurrent pneumonias and a chronic cough productive of foul-smelling purulent sputum. The sputum production is worse when lying down and in the morning. On physical examination, he appears chronically ill with clubbing of the fingers. Wet inspiratory crackles are heard at the lung bases posteriorly. There are no hepatosplenomegaly or any palpable lymph nodes. CXR shows scaring in the right lower lobe, which on chest CT scan is identified as airway dilatation, bronchial wall thickening, and grapelike cysts. Which of the following is sometimes seen in this condition? (A) lung cancer
(B) dextrocardia
(C) fungal infection
(D) carcinoid syndrome
(E) Hodgkin’s disease
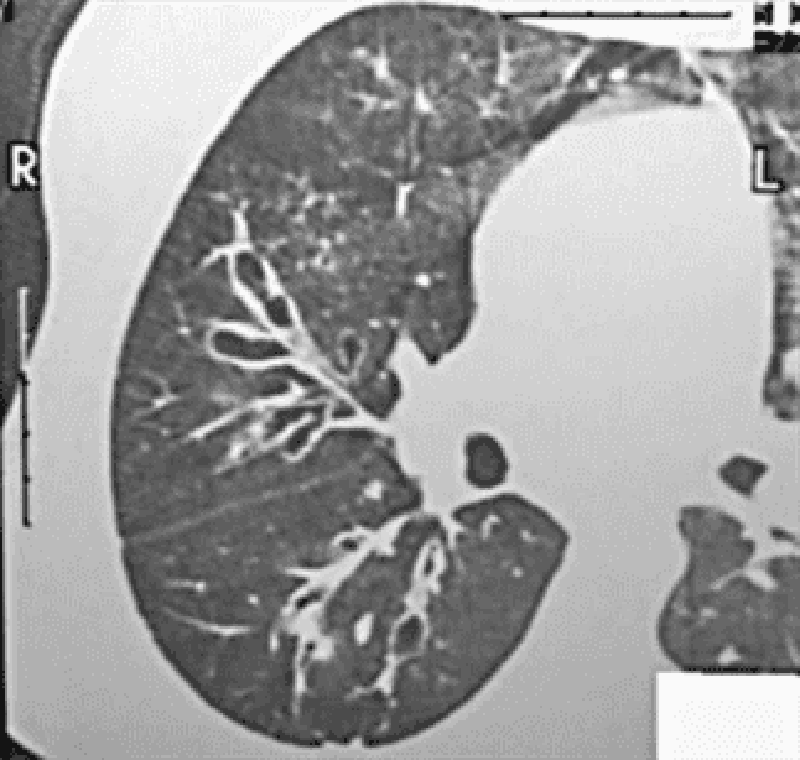
193. A 27-year-old man presents with chest pain and feeling unwell. He describes cough with bloodtinged sputum, chills, and fever of 2 days’ duration. Physical findings reveal dullness and moist rales in the left lower chest. His CXR is shown in Fig. Which of the following is the most likely diagnosis?
Pneumonia, left lower lobe
Atelectasis, left lower lobe
PE
Uberculosis
Sarcoidosis
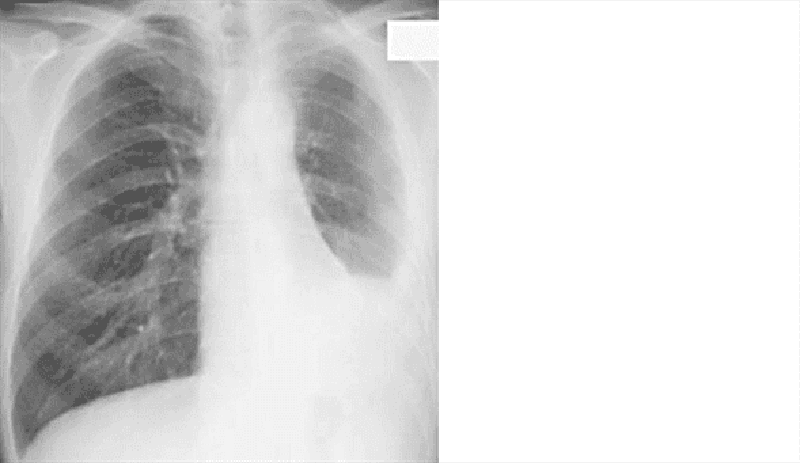
194. A 40-year-old man is seen for an insurance assessment. He has no past medical history and feels well. His compete physical examination is normal. His biochemistry, complete blood count (CBC), ECG, and urinalysis are also normal. His CXR is abnormal and presented in Fig. Which of the following is the most likely diagnosis
Hamartoma of the lung
Tuberculous granuloma of the left apex
Osteochondroma of the left 4th rib
Bronchogenic
Pulmonary metastases
195. A 21-year-old man has a nonproductive cough, shortness of breath, and chest pain, which changes with breathing. He also has pain in the left arm. On examination, there is tenderness over the left shoulder, heart sounds are normal, and the lungs are clear. CXR reveals a lytic lesion in the left humerus and reticulonodular opacities in the upper and middles lobes. The eosinophil count is normal. Which of the following is the most appropriate initial diagnostic test?
Lung biopsy
Humerus bone biopsy
CT scan of chest
Bronchoscopy
Pulmonary function tests
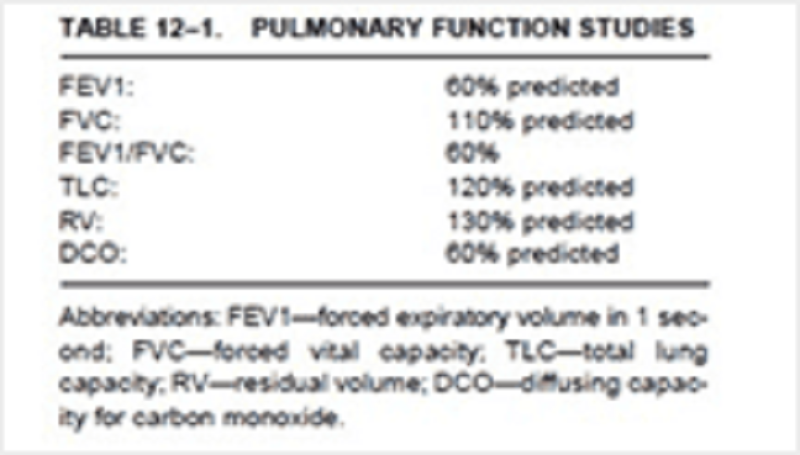
196. The pulmonary function studies shown in Table 12–1 are of a 65-year-old man with severe dyspnea and cough. Which of the following is the most likely diagnosis?
(A) emphysema
(B) lobar pneumonia
(C) chronic bronchitis
(D) acute bronchitis
(E) CHF
197. A 33-year-old woman, otherwise perfectly well, presents with recurrent episodes of hemopty- sis. She has no fever, weight loss, cough, or sputum production. Her physical examination is entirely normal. Her CXR, biochemisty, CBC, and coagulation profile are also normal. Which of the following is the most appropriate initial diagnostic test?
(A) echocardiogram
(B) gallium scan
(C) CT scan of chest
(D) bronchoscopy
(E) pulmonary function tests
198. A 34-year-old woman is complaining of progressive and worsening shortness of breath. Her symptoms first started 3 years ago, and she now gets dyspneic and fatigued while doing her activities of daily living. Her past medical history is not significant and she not taking any medications. Physical examination reveals increased JVP and a reduced carotid pulse. Precordial examination reveals a left parasternal lift, loud P2, and right-sided S3 and S4. There are no audible murmurs. CXR reveals clear lung fields and an ECG shows evidence of right ventricular hypertrophy. Pulmonary function tests are normal. Which of the following is the most likely diagnosis?
(A) asthma (without wheezing)
Primary pulmonary hypertension
(C) pulmonary veno-occlusive disease
(C) pulmonary veno-occlusive disease
(F) disease
199. A 45-year-old woman has severe symptoms of epigastric and abdominal pain after eating. A trial of acid suppression therapy with proton pump inhibitors (PPI) only partially improved her symptoms. She undergoes elective outpatient upper endoscopy, which is positive for a small duodenal ulcer. Two hours later, she is short of breath and complaining of severe anterior chest pain, which is made worse with deep inspiration. On examination, she looks unwell, blood pressure is 150/90 mm Hg, pulse 110/min, and lungs are clear. Heart sounds are normal but an “extra crunching” type sound is intermittently heard. CXR demonstrates air surrounding the heart. Which of the following is the most likely diagnosis?
(A) acute pericarditis
(B) acute cardiac ischemia
(C) acute mediastinitis
(D) aortic dissection
(E) pneumothorax
A 55-year-old woman is in the intensive care unit on a ventilator for hypoxemia following “flash” pulmonary edema. Her PO2 on the blood gas prior to intubation was 44 mm Hg, and now while breathing 100% oxygen on the ventilator her repeat blood gas reveals a PO2 of 80 mm Hg. Hypoxemia while receiving 100% oxygen indicates which of the following problems?
(A) ventilation-perfusion ratio inequality
(B) right-to-left shunt
(C) hypoventilation
(D) impaired diffusion
(E) interstitial lung disease
201. A 31-year-old man with severe kyphoscoliosis due to cerebral palsy is experiencing worsening shortness of breath with exertion. On examination, he has a severe scoliosis to the left and decreased air entry to that side. His right lung is clear, JVP is 3 cm, and heart sounds are normal. Pulmonary function tests are performed. Which of the following is the most likely abnormality to be seen on the pulmonary function tests?
(A) increased total lung capacity (TLC)
(B) increased functional residual capacity (FRC)
(C) decreased TLC
(D) increased compliance
(E) increased vital capacity (VC)
202. A 52-year-old man develops sudden-onset shortness of breath on postoperative day 4 after a hemicolectomy for colon cancer. His surgery went well with no operative complications. He reports no cough, sputum, or pleuritic chest pain. His blood pressure is 155/90 mm Hg, pulse 100/min, temperature 37.8°C, lungs are clear, and heart sounds normal. He has bilateral pedal edema, but no discomfort in his legs. His CXR and ECG are normal. A chest CT with contrast reveals a thrombus in his right upper lobe artery. Which of the following statements concerning the management of this condition is most likely correct?
(A) continuous IV heparin or subcutaneous low-molecular-weight heparin (LMWH) therapy is indicated
(B) urgent thrombolytic therapy is indicated
(C) urgent inferior vena cava (IVC)
(D) filter insertion is indicated
(E) confirmation of the diagnosis with bilateral ultrasound leg Dopplers
203. An 83-year-old man with Parkinson’s disease presents with low-grade fever and cough for several weeks. Lately, he has been experiencing more rigidity and difficulty with his walking. He is on a levodopa/carbidopa combination for treatment for the past 5 years. On examination, his gait is shuffling and slow. He has a tremor in his left hand at rest, and there is cogwheel rigidity of the forearm. There are crackles in the left lower lung field. CXR reveals a lung abscess in the left lower lobe. Which of the following is the most likely bacteriologic diagnosis for the lung abscess?
Oropharyngeal flora
(B) tuberculosis
(C) Staphylococcus aureus
(D) Pseudomonas aeruginosa
(E) Candida albicans
204. A 31-year-old G4P3 woman gave birth via re- peat cesarean section to a full-term, 3700-gm (8.2lb) baby girl. There were no complications during the pregnancy or delivery. Two hours after the birth the resident is called to evaluate the baby girl. She is afebrile but is breathing rapidly with mild subcostal retractions. Breath sounds are equal and clear bilaterally. S1 and S2 are normal and the point of maximal intensity is not displaced. X-ray of the chest reveals flattened diaphragms, prominent vascular markings, and fluid lines in the fissures. Which of the following is the most likely diagnosis?
(A) Diaphragmatic hernia
(B) Neonatal respiratory distress syndrome
(C) Pulmonary hemorrhage
(D) Pulmonary interstitial emphysema
(E) Transient tachypnea of the newborn
205. A 67-year-old man presents to his primary care physician with complaints of dyspnea on exertion over the past 6 months that has progressively worsened to dyspnea at rest. He denies cough and wheezing and has had no fevers, night sweats, or unintentional weight loss. The man has never smoked and worked as a ship-builder for >30 years. Which of the following findings on x-ray of the chest would confirm the most likely diagnosis?
(A) Bilateral diffuse infiltrates
(B) Bilateral hilar adenopathy
(C) Consolidation of lung tissue
(D) Focal mass with air bronchograms
(E) Multiple pleural plaques with patchy parenchymal opacities
206. A 23-year-old man is seen in the emergency department for sudden onset, right-sided pleuritic chest pain that developed 30 minutes ago while he was watching television. The patient also complains of difficulty breathing. He has no prior medical history, denies smoking and intravenous drug use, and does not take any medications. His temperature is 37.3°C (99.1°F), blood pressure is 130/82 mm Hg, pulse is 92/ min and regular, respiratory rate is 20/min and shallow, and oxygen saturation is 98% on room air. His body mass index is 18 kg/m². Diminished breath sounds, hyperresonance, and decreased tactile fremitus are prominent in the right lung field. The trachea is midline. X-ray of the chest shows a 10% pneumothorax on the right. Which of the following is the most appropriate initial management?
(A) Needle decompression
(B) Observation with supplemental oxygen
(C) Open thoracotomy with oversewing of the pleural blebs and scarification of the pleura
(D) Thoracoscopy with stapling of blebs
(E) Tube thoracostomy with doxycycline pleurodesis
207. A 28-year-old African American woman presents with mild dyspnea on exertion. She reports no coughing, sputum production, or wheezing symptoms, but has noticed a red tender rash on her shins. Physical examination reveals hepatosplenomegaly, generalized lymphadenopathy, and tender erythematous nodules on her legs. CXR shows bilateral symmetric hilar adenopathy. Her pulmonary function tests reveal a mild restrictive pattern. Which of the following tests will most likely make a definitive diagnosis?
(A) tuberculin skin test
(B) bronchoscopy with transbronchial biopsy
(C) elevated ACE level
(D) serum hypercalcemia
(E) increased uptake on gallium scan
208. 69-year-old woman has recently returned on an overnight flight from Europe. She now complains of vague chest discomfort and shortness of breath. On examination, she is comfortable, blood pressure 130/80 mm Hg, pulse 90/min, respirations 18/min, and oxygen saturation 97%. Her heart and lungs are normal on auscultation, and there is no edema or leg tenderness on palpation. A quantitative (ELISA) D-dimer assay is positive. Which of the following statements regarding the Ddimer assay is correct?
(A) It is sensitive but not specific
(B) It is specific but not sensitive
(C) It is neither specific nor sensitive
(D) A negative result suggests myocardial ischemia
(E) It is both sensitive and specific
{"name":"USMLE (part2)", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"101. A 56-year-old Caucasian male complains of chronic exertional dyspnea for the past several years that has progressively worsened. He cannot remember the last time that he saw a doctor, and does not take any medications regularly. It is difficult for him to climb two flights of stairs without having to rest. His dyspnea has gotten so bad that it has severely limited his activity level, and he now spends most of his time on the couch. He also describes recurrent episodes of nocturnal dyspnea, during which he wakes up at around 2:00 AM with difficulty breathing, coughing, and wheezing that improve when he sits up. He usually coughs up some yellowish sputum before being able to go back to sleep. He has had no fever, chills, or chest pain. Which of the following is the most likely cause of this patient's complaints?, 102. A 62-year-old man presents to his primary care physician's office with progressive exertional dyspnea. His past medical history is significant for hypertension treated with hydrochlorothiazide and diabetes mellitus treated with metformin. He was an industrial worker for 30 years and retired one year ago. He smokes one pack of cigarettes per day and consumes alcohol occasionally. His blood pressure is 150\/100 mmHg and his heart rate is 80\/min. His BMI is 31 kg\/m2. Chest x-ray reveals pleural calcifications. Pulmonary function studies show the following: FEV1 70% of predicted FVC 65% of predicted Residual volume 70% of predicted DLCO decreased Which of the following is the most likely cause of this patient's symptoms?, 103. A 32-year-old woman comes to the emergency department complaining of sudden onset shortness of breath accompanied by a non-productive cough and left-sided chest discomfort that increases on inspiration. She denies subjective fever, coughing up blood, wheezing, palpitations, leg pain, and swelling of the lower extremities or any recent travel. Past medical history is significant for an appendectomy at age 15. Her medications include birth control pills and over- the-counter vitamins. She is a known carrier of sickle cell trait. Her father, age 65, has had diabetes for 20 years; mother, age 58, has coronary artery disease. She has never been pregnant, drinks alcohol socially and does not smoke. Her temperature is 99 F (38C), blood pressure is 110\/70 mmHg, pulse 130\/min and respirations are 33\/min. Pulse oximetry shows an oxygen saturation of 85% on 6 liters of oxygen. Her BMI is 30 kg\/m2. She is alert and cooperative without cyanosis or jaundice. Her lungs are clear to auscultation. Her abdomen is soft, nondistended and non-tender. Which of the following is the best test to confirm this patient's diagnosis?","img":"https://cdn.poll-maker.com/10-469385/untitled.png?sz=1200"}
More Quizzes
Varsinais-Suomi
5231
Nike the god
210
Discover Your Ideal Lifestyle
331664
Communication Ethics
7426
Free Relationship Anxiety Test - Discover Your Love Worries
201033432
CDC 2AX7X UREs Section 3: Test Your Maintenance Ops Skills
201026681
Test Your Grizzly Bear IQ: Ultimate Bear Behavior
201026426
Think You Can Ace the Chemistry Chapter 2 Test? Free!
201025935
What Kind of Impostor Are You? Free Impostor Syndrome
201033881
Free Cognitive Psychology Practice
201022191
Free Organization Founding Year
201025239
What Is AVAX Robinhood? Take the Free Now!
201032573