GASTROINTESTINALE I
An 82-year-old woman presents 1-hour after the sudden onset of moderate-to-severe epigastric pain. The pain radiates to her back, both scapulae, and both arms. She has been nauseated and vomited three times in the past hour. Her past medical history is remarkable for peptic ulcer disease 10-years ago, cholelithiasis for the past 6-years, and stable angina pectoris for the past 3-years. She has had occasional episodes of biliary colic and two bouts of acute cholecystitis which were treated conservatively. Her temperature is 36.8C (98.2F), blood pressure is 120/70 mm Hg, pulse is 90/min, and respirations are 14/min. The lungs are clear to auscultation. Abdominal examination shows a soft abdomen with mild tenderness to palpation in the epigastrium. Murphy's sign is negative. Which of the following studies should be done first?
Abdominal ultrasound
Upper Gl endoscopy
Electrocardiogram
Upright abdominal x-ray
Serum amylase and lipase
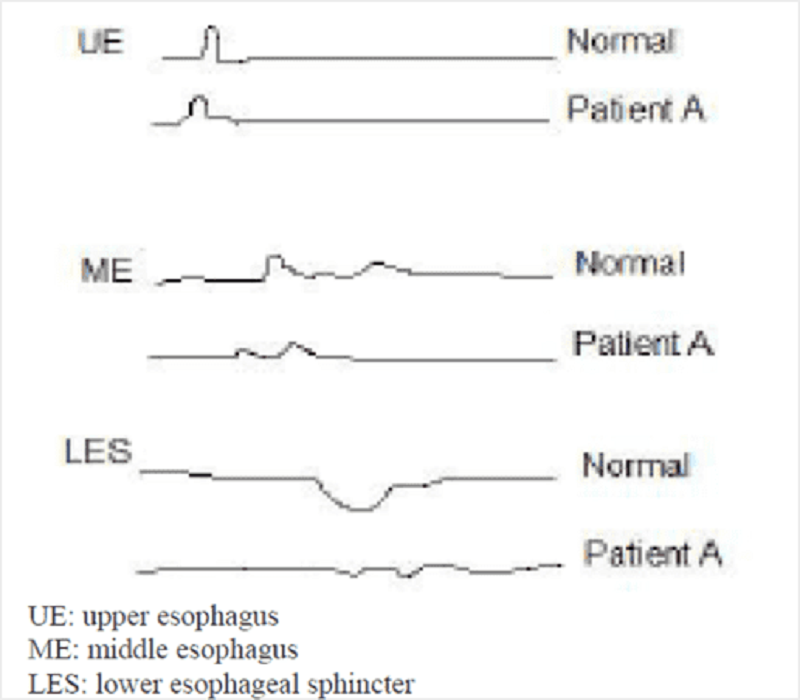
A 43-year-old male (Patient A) is being evaluated for an esophageal disorder. Esophageal manometry tracings after a single swallow of 5 ml of water are shown on the slide below. Which of the following is the most likely diagnosis in this patient?
Cricopharyngeal dysfunction
Diffuse esophageal spasm
Achalasia
Gastroesophageal reflux
Mallory-Weiss syndrome
A 45-year-old nurse practitioner presents to the emergency department due to painful abdominal cramps and watery diarrhea. She has about 10 to 20 bowel movements a day. She also has nocturnal bowel movements. She has had multiple hospitalizations in the past for similar problems without a definite diagnosis. A lower GI endoscopy during a previous hospitalization showed dark brown discoloration of the colon with lymph follicles shining through as pale patches. Which of the following is the most likely diagnosis?
Factitious diarrhea
Irritable bowel syndrome
Celiac disease
Infectious diarrhea
Non-Hodgkin's lymphoma
A 65-year-old woman presents with a 2-month history of fatigue and dyspnea on exertion. She takes no medication. Her temperature is 36.7C (98F), blood pressure is 162/83 mm Hg, pulse is 100/min, and respirations are 21/min. Auscultation shows a 2/6 systolic murmur in the 2nd right intercostal space. No peripheral edema is noted. Rectal examination shows no abnormalities. Test of the stool for occult blood is negative. EKG shows sinus tachycardia and non-specific ST-T changes. Laboratory studies show: Hemoglobin 8.1 g/L MCV 73 fl Platelets 360,000/mm3 Leukocyte count 4,500/mm3 Neutrophils 56% Eosinophils 1% Lymphocytes 33% Monocytes 10%. Which of the following is the most appropriate next step in management?
Echocardiography
Bone marrow biopsy
Gastro-duodenoscopy
Colonoscopy
Isotope-labeled erythrocytes scintigraphy
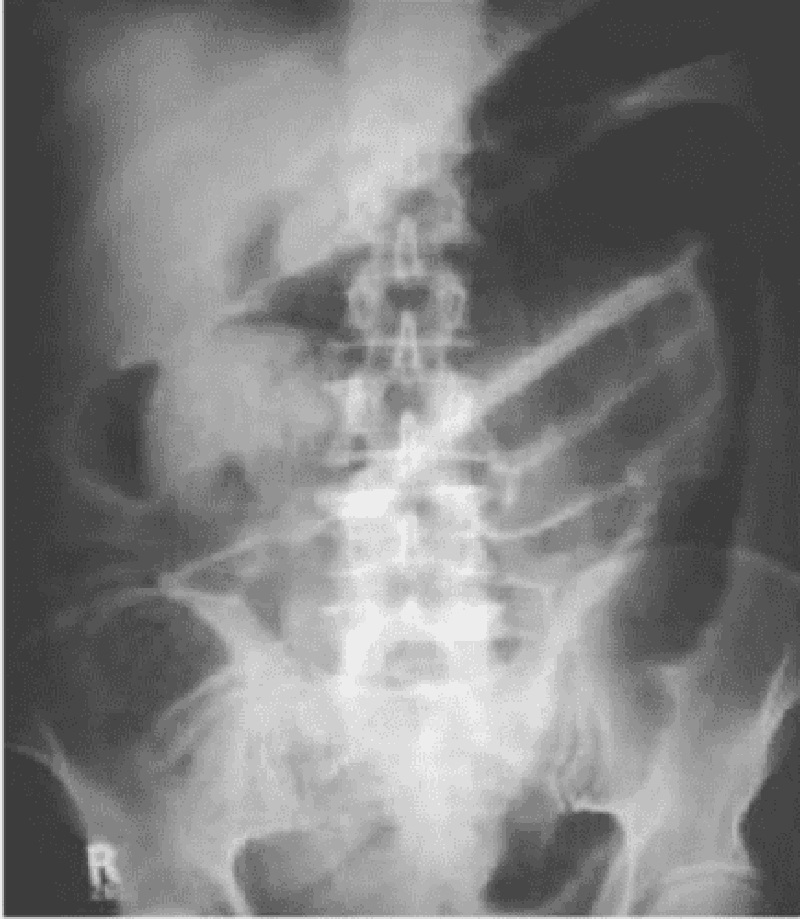
A 44-year-old white female presents with a 2-month history of low-grade fever, abdominal pain and bloody diarrhea. Over the past two days, her symptoms have increased. She does not use medications and she has no allergies. She has had a 10 lb (4.5 kg) weight loss over the past four weeks. Her temperature is 38.9C (102F), blood pressure is 102/70 mm Hg, pulse is 118/min, and respirations are 22/min. Examination shows pale and dry mucus membranes. Abdominal examination shows diffuse tenderness and distention. Laboratory studies show: Hb 9.5 g/dl WBC 16,000/cmm Serum Na 145 mEq/L Serum K 3.0 mEq/L An x-ray film of the abdomen is shown below: Which of the following is the most likely diagnosis?
Crohn's disease
Pseudomembranous colitis
Toxic megacolon from ulcerative colitis
S. Aureus gastroenteritis
Obstructed colon cancer
A 45-year-old Mexican male presents with a 2-day history of traces of blood on the tissue paper after he wipes. He does not have gross blood mixed with stool, but on one occasion there were drops of blood in the toilet after defecation. He has no past medical history or family history of cancer or other significant disease. Which of the following is the most appropriate next step in management?
Colonoscopy
Fecal occult blood test
Anoscopy
Sigmoidoscopy
Barium enema
A 65-year-old man comes to the physician's office with a 2-month history of dysphagia. He initially had difficulty swallowing solids, but now this includes liquids. He has occasional heartburn, which usually responds well to antacids. He has lost 20 lbs of weight in the past 2 months. He has a 40 pack-year history of smoking. He has been a chronic alcoholic for 20 years. His temperature is 36.7C(98F), blood pressure is 110/80 mm Hg, pulse is 66/min, and respirations are 14/min. Physical examination shows no abnormalities. Barium studies show a minimally dilated esophagus with beak-shaped narrowing. Manometry shows increased lower esophageal sphincter tone. Which of the following is the most likely diagnosis?
Achalasia
Esophageal cancer
Scleroderma
Peptic stricture
Diffuse esophageal spasm
A 73-year-old woman is transferred to the hospital from the nursing home because of diverticulitis. A prior CT scan showed inflamed sigmoid colon. Transferred records indicate a 2-day history of fever and abdominal pain. On admission, her white count is 22,000/cmm, and she is started on IV antibiotics and IV fluids. Over the ensuing few days, her white count starts to come down and she has no nausea, vomiting or fever; however, she suddenly develops a cough and increasing abdominal pain. Abdominal examination shows guarding and tenderness in the left lower quadrant. An upright x-ray film of the chest shows free air under the left diaphragm. Which of the following is the most appropriate next step in management?
CT scan of the abdomen
Colonoscopy
Barium enema
Continue antibiotics and observe
Laparotomy
A 51-year-old obese male presents to your office complaining of difficulty swallowing solids but not liquids. His medical history is significant for GERD. Six months ago he was diagnosed with Barrett's esophagus. He reports that three months after the diagnosis of Barrett's esophagus, his heartburn resolved. Barium swallow now reveals an area of symmetric, circumferential narrowing affecting the distal esophagus. Which of the following best explains this finding?
Esophageal adenocarcinoma
Hiatal hernia
Achalasia
Peptic stricture
Vascular ring
Ms. Lee, a 62-year-old Chinese woman, comes with yellowness in her eyes for the past 6 weeks. She is generally feeling tired, has lost some weight, and occasionally had some nausea. She denies any altered bowel habits. She is a non-smoker but drinks 2-3 beers each night. Her dad is suffering from high cholesterol and also has had stroke. She had a dilatation and curettage for an abnormal pap smear 15 years ago. Her vitals are stable and she is afebrile. She has marked scleral icterus. An abdominal examination reveals normal bowel sounds and no organomegaly. Her stools were occult blood negative. Her liver function tests and enzymes were ordered and the results are Total protein 6.1 g/dl Albumin 39 g/dl AST 67U/L ALT 52U/L Alkaline phosphatase 290 U/L Total bilirubin 96 mg/dl Direct bilirubin 89 mg/dl Serum lipase is 46 U/L Anti-mitochondrial antibodies negative. Which of the following is the most likely cause of these findings?
Primary biliary cirrhosis
Chronic pancreatitis
Viral hepatitis
Pancreatic carcinoma
Hepatocellular carcinoma
A 23-year-old man comes to the physician because of a two-month history of loose stools, decreased appetite, and weight loss. He has no history of medical problems. He takes no medications. His temperature is 36.7C (98F), blood pressure is 120/76 mmHg, pulse is 90/min, and respirations are 16/min. Laboratory studies show: Hemoglobin 11.2 g/dL MCV 80 fl Leukocyte count 9,500/cmm Segmented Neutrophils 65% Bands 3% Eosinophils 1% Basophils 0% Lymphocytes 25% Monocytes 6% Platelets 550,000/cmm ESR 50 mm/hr Serum sodium 145 mEq/L Serum potassium 4.0 mEq/L Test of the stool for occult blood is positive. Which of the following is the most likely type of diarrhea in this patient?
Inflammatory
Secretory
Osmotic
Motor
Factitial
A 35-year-old Hispanic male comes to the office because of excruciating pain during defecation for the past week. The pain is so severe that he avoids using the toilet. He also adds that he has noticed bright red blood in his stool. The caliber of his stool has not changed. His past medical history is significant for chronic constipation. Rectal examination shows a posterior mucosal tear of the anus. Which of the following is the most appropriate next step in management?
Colonoscopy
Local anesthetic and stool softeners
Lateral sphincterotomy
Antibiotics
Gradual dilatation of the sphincter
A 27 -year-old man complains of episodic abdominal pain. The pain is concentrated in the epigastrium and is gnawing in quality. It wakes him up during the night and is promptly relieved by a glass of water and a piece of bread. He denies vomiting or diarrhea, but has experienced an occasional "dark stool." He has no significant past medical history and does not take any medications. His family history is significant for biliary disease in his mother and stomach cancer in his father. He smokes one pack of cigarettes a day and consumes a can of beer almost every day. His vital signs are with in normal limits. Physical examination shows mild epigastric discomfort on deep palpation. Which of the following is most likely to provide long-term symptom relief in this patient?
Four weeks of omepra zole
Antibiotics and pantoprazole
NSAIDs as needed
Smoking cessation
No alcohol consumption
A 66-year-old man presents with a four-week history of increasing back pain and severe constipation. He has no weakness or sensory symptoms in his legs. He takes acetaminophen for back pain, metoprolol for high blood pressure, and an over-the-counter fiber supplement for constipation. A screening colonoscopy 5-year ago was unremarkable. Rectal examination shows no abnormalities. Examination of the stool for occult blood is negative. His blood pressure is 135/80 mmHg and heart rate is 80/min. Abdominal examination shows no abnormalities. Laboratory studies show: Hb 9.5 g/dl WBC 7,000/cmm Platelets 300,000/cmm BUN 28 mg/dl Serum Creatinine 1.9 mg/dl ESR 80/hr Which of the following is the best explanation for this patient's constipation?
Mechanical obstruction
Medication effect
Electrolyte disturbances
Hormonal disturbances
Neurologic dysfunction
A 26-year-old man presents with a 1-week history of intermittent, crampy, lower abdominal pain accompanied by rectal urgency, bloody diarrhea, nausea and vomiting. His symptoms have become more severe over the past 24 hours. His past medical history is unremarkable. He denies any recent travel or antibiotic use. His temperature is 38.5C (102.0F), blood pressure is 120/80 mm Hg, pulse is 95/min, and respirations are 15/min. Abdominal examination reveals distension and tenderness to palpation without rebound or guarding. The bowel sounds are decreased. Rectal examination shows marked rectal tenderness and mucus mixed with blood in the vault. An x-ray film of the abdomen shows distended colon filled with gas. Laboratory studies show: Hb 10.8 g/dl WBC 19,600/cmm Platelet count 459,000/cmm ESR 54/hr Which of the following is the most appropriate next step in management?
Stool for ova, parasites and culture
Barium enema
Proctosigmoidoscopy and biopsy
Serology for Entamoeba histolytica
CT scan of the abdomen
A 64-year-old white male with a history of severe stable angina and peripheral vascular disease undergoes coronary artery bypass surgery. His post-operative course is complicated by hypotension, which is treated successfully; however, a few hours later, he experiences abdominal pain followed by bloody diarrhea. His temperature is 37.8C (100 F), blood pressure is 110/60 mmHg, pulse is 110/min, and respirations are 20/min. Abdominal examination is benign. Laboratory studies show a WBC count of 15,000/cmm with 7% bands. The lactic acid level is elevated. A CT scan is ordered. Which of the following areas of the colon will most likely show abnormal findings?
Sigmoid colon
Splenic flexure
Ascending colon
Mid transverse colon
Hepatic flexure
A 49-year-old woman presents to the emergency department (ED) with profuse, foul-smelling, watery diarrhea and abdominal pain. Five days ago, she was hospitalized for urosepsis and treated with amoxicillin and sulbactam. She recovered well, and was discharged three days ago with a prescription for oral amoxicillin plus clavulanic acid. Her current temperature is 38.8C (101.9F), blood pressure is 110/70 mm Hg, pulse is 102/min, and respirations are 15/min. Abdominal examination shows tenderness in the left lower quadrant. CBC shows a WBC count of 25,000/microl. She is started on intravenous normal saline in the ED. Which of the following is the most appropriate next step in management?
Continue rehydration
Start oral metronidazole
Discontinue antibiotics
Discontinue antibiotics and start oral metronidazole
Discontinue antibiotics and start oral vancomycin
A 52-year-old man presents to your office after passing a black stool. He also describes occasional abdominal discomfort and nausea but denies hematemesis. He says that food seems to help his abdominal pain, so he eats frequently during the day and keeps some snacks on his night stand. As a consequence, he has gained 5 pounds over the last year. He admits that his diet is lacking in vegetables and fruit. He drinks one to two cans of beer nightly, but does not smoke or use illicit drugs. He says that his father died of colon cancer and his mother died from a stroke. Physical examination reveals a right-sided carotid bruit. The fecal occult blood test is positive. Which of the following is the most likely cause of his condition?
Mesenteric ischemia
Mallory-Weiss tear
Lnflammatory bowel disease
Erosive gastritis
Peptic ulcer disease
A 35-year-old Caucasian female presents to your office with several months history of heartburn. She also describes a periodic 'sticking sensation' in her throat during the meal. Her past medical history is significant for asthma that is controlled with inhaled steroids, and acoustic neuroma that was removed 2 years ago. She does not smoke or consume alcohol. She denies any recreational drug use. She is not allergic to any medications. She works as a secretary at a private firm, and considers her work moderately stressful. Her family history is significant for breast cancer in her mother and prostate cancer in her father. Endoscopic evaluation shows mild hyperemia in the distal esophagus. Esophageal manometry reveals absent peristaltic waves in the lower two-thirds of the esophagus and a significant decrease in lower esophageal sphincter tone. Which of the following is the most likely cause of this patient's complaints?
Achalasia
GERD with or without hiatal hernia
Scleroderma
Non-ulcer dyspepsia
Diffuse esophageal spasm
A 34-year-old woman complains of occasional diarrhea and crampy lower abdominal pain. She says that at times her symptoms hamper her performance in important business meetings. The pain sometimes occurs after meals but is not always preceded by eating. The pain is often accompanied by diarrhea with small amounts of stool and mucus. Her past medical history is significant for bleeding hemorrhoids. Her mother died of colon cancer. Which of the following findings is most likely in this patient?
Normal colonic mucosa
Crypt abscesses
Folic acid deficiency
Duodenal ulcer
Intestinal villous atrophy
A 55-year-old obese male presents to his physician for a routine annual physical examination. A review of systems is insignificant, except for constipation which has been present for several years. He does not have major medical problems and is not on any prescription or over-the-counter medications. He has smoked one and- a-half packs of cigarettes daily for 30 years. He drinks 4 oz of alcohol daily. Physical examination is unremarkable. As part of the routine screening, a colonoscopy is performed, which shows multiple diverticuli at the sigmoid colon. He is concerned about the diverticulosis. Which of the following is the most appropriate next step in the management of this patient's diverticulosis?
Advise him to stop smoking
Advise him to stop drinking alcohol
Increase dietary fiber intake
Explain his surgical options
Educate about prophylactic antibiotics
A 40-year-old female presents with abdominal discomfort. The discomfort is localized to the center of the upper abdomen and is not related to meals or fatty food. She has a history of similar symptoms. She has not had gastrointestinal bleeding, fatigue, dysphagia, or weight loss. Her mother has a history of gastric ulcer. Her vital signs are within normal limits. Complete physical examination is unremarkable. Stool for heme occult is negative. Complete blood count and serum chemistries are within normal limits. Which of the following is the most appropriate next step in management?
Barium swallow
Endoscopy
Empiric trial of H2 blockers
H. Pylori breathe test
Empirical antibiotic trial
A 64-year-old man is brought to the ER after an episode of coffee ground emesis followed by lightheadedness. He has been having black, tarry stools for the past few days. He has a history of coronary artery disease and he underwent coronary artery bypass surgery three years ago. He is currently taking aspirin, metoprolol, lisinopril, and pravastatin. He drinks 2-3 beers over the weekend but he quit smoking after the bypass surgery. His temperature is 36.7C (98F), pulse is 110/min, respirations are 16/min, and blood pressure is 90/60 mmHg. Examination shows coffee ground-like material in the oropharynx. His lungs are clear. Abdomen is slightly tender in the epigastrium. Laboratory studies show Complete blood count: Leukocyte count 9,500/mm3 Hemoglobin 8.1 g/L Platelets 130,000/mm3 Chemistry panel: Serum sodium 140 mEq/L Serum potassium 3.5 mEq/L Bicarbonate 27 mEq/L Blood urea nitrogen (BUN) 54 mg/dL Serum creatinine 1.2 mg/dL Which of the following is the most appropriate next step in management of this patient?
Whole blood transfusion
Packed red blood cell transfusion
Fresh frozen plasma infusion
Hemodialysis
Platelet transfusion
A 12-year-old girl comes to the physician for chronic weight loss and fatigue. She has a history of bulky, floating, foul-smelling stools, flatulence and meteorism. She also has bone pain and easy bruising. Laboratory studies show anemia with serum iron: 25 mg/dl, ferritin: 25 mg/dl and serum total iron binding capacity 600 mg/dl (normal 300-360 mg/dL); PT is 16 sec. Physical examination shows loss of subcutaneous fat, pallor, hyperkeratosis and abdominal distention; bowel sounds are increased. Which of the following is most likely associated with this patient's condition?
Anti-endomysial antibodies
Anti-Scl-70 antibodies
Antinuclear antibodies
Anticentromere antibodies
Anti-mitochondrial antibodies
A 30-year-old woman presents with a 5-month history of episodic retrosternal pain that radiates to the interscapular region. The pain episodes typically last 15 minutes, and are precipitated by emotional stress and hot or cold food. Her relative gave her sublingual nitroglycerine tablets, which alleviated the pain. Her past medical history is unremarkable, and she does not take any other medications. There is no family history of coronary artery disease. Her vital signs are within normal limits. Physical examination shows no abnormalities. A lipid profile is within normal limits. An EKG shows a normal sinus rhythm. A stress test fails to reproduce the symptoms or to induce ST/T wave changes. Chest x-ray, upper GI endoscopy, and echocardiography show no abnormalities. Which of the following is the most appropriate next step in diagnosis?
CT scan of the chest with contrast
Esophageal motility studies (manometric recordings)
Coronary angiogram
Acid perfusion (Bernstein) test
Pulmonary perfusion/ventilation scintigraphy
A 45-year-old male comes to the physician for epigastric pain and diarrhea. His past medical history is significant for chronic duodenal ulcers. He has been smoking 2 packs of cigarettes daily for the past 10 years. He occasionally drinks alcohol. He denies illegal drug use or multiple sexual partners. Physical examination shows abdominal tenderness without rebound or rigidity. Endoscopy shows prominent gastric folds, chronic duodenal ulcer, and upper jejunal ulceration. Which of the following is the most appropriate next step in the diagnosis of this patient?
Secretin stimulation test
Gastric acid secretion study
Serum chromogranin A
Calcium infusion study
Serum gastrin concentration
A 42-year-old male comes to the physician's office for evaluation of skin rash and hair loss. He has a long history of Crohn's disease and has had extensive small bowel resection resulting in short bowel syndrome. He is currently receiving total parenteral nutrition. When he does try to eat, he complains that the food does not taste good. His vital signs are stable. Examination shows alopecia and bullous, pustular lesions around the perioral and periorbital areas. Which of the following is the most likely cause of his current symptoms?
Celiac disease
Zinc deficiency
Vitamin A deficiency
Vitamin B 12 deficiency
Systemic lupus erythematosus
A 32-year-old female from South America presents with a 3-month history of progressive difficulty with swallowing for both liquids and solids. At night she has a bitter taste in her mouth. Over the past two months, she has had a 10 lb (4.54 kg) weight loss. She has not had any previous illnesses, and does not take any medication. Physical examination is unremarkable. A lateral x-ray film of the chest shows extreme dilatation of the esophagus with an air fluid level. Which of the following is the diagnostic test for this patient's condition?
Barium swallow
Endoscopy
PH monitoring
Manometry
CTscan
A 45-year-old Hispanic male comes to the emergency department because of a two-day history of intermittent abdominal pain and bloody diarrhea. He has had four similar episodes in the past year. He is subsequently admitted to the floor. Radiographic and endoscopic evaluations show extensive disease from the terminal ileum to the rectum with multiple ulcerations and pseudopolyps. Biopsy of the lesion shows noncaseating granulomas and crypt abscess. Which of the following is the most characteristic feature which favors the diagnosis of Crohn's disease against that of ulcerative colitis?
Crypt abscess
Abdominal pain and bloody diarrhea
Non-caseating granulomas
Pseudopolyps
Disease from terminal ileum to rectum
A 50-year-old female presents with heartburn and gnawing abdominal pain. She was diagnosed with peptic ulcer disease 3 years ago, but she has been non-adherent to her medications. She asks you if her nonadherence puts her at increased risk of any complications. Which of the following is the most common complication of peptic ulcer disease?
Perforation
Penetration
Gastric outlet obstruction
Hemorrhage
Atrophic gastritis
A 56-year-old woman with cirrhosis presents with a 2-week history of increasing abdominal distension. She has mild encephalopathy and esophageal varices without bleeding. Her cirrhosis is due to chronic hepatitis type B. She has a past history of ascites treated successfully with conservative management. She is currently on sodium, water and protein restriction, maximal doses of spironolactone and furosemide, and lactulose. Her temperature is 36.6C (97.9F), blood pressure is 120/70 mm Hg, pulse is 80/min, and respirations are 30/min. She has a flapping tremor and labored breathing. Abdominal examination shows marked abdominal distension. An x-ray film of the chest is unremarkable. Abdominal ultrasound shows peritoneal fluid and splenomegaly, liver hyperechogenicity and nodularity, and portal vein width of 16 mm; no masses are evident. Which of the following is the most appropriate next step in the management of this patient's ascites?
Intravenous furosemide therapy
Tapping of some amount of ascitic fluid
Peritonea-jugular shunt
Distal spleno-renal shunt (selective shunt)
Side-to-side porto-caval shunt (non-selective shunt)
A 44-year-old male who has had an extensive small bowel resection for Crohn's disease has been on total parenteral nutrition for two years. He presented to the hospital with epigastric and right upper quadrant pain. He has been taking azathioprine. His vital signs are within normal limits. Physical examination shows mild right upper quadrant tenderness. An ultrasonogram shows several gallstones; an ultrasonogram performed two years ago did not demonstrate gall stones. Which of the following is the most likely cause of his gallstones?
Increased cholesterol secretion
Increased red blood cell destruction
Impaired gallbladder contraction
Increased enterohepatic recycling of bile acids
Increased calcium absorption
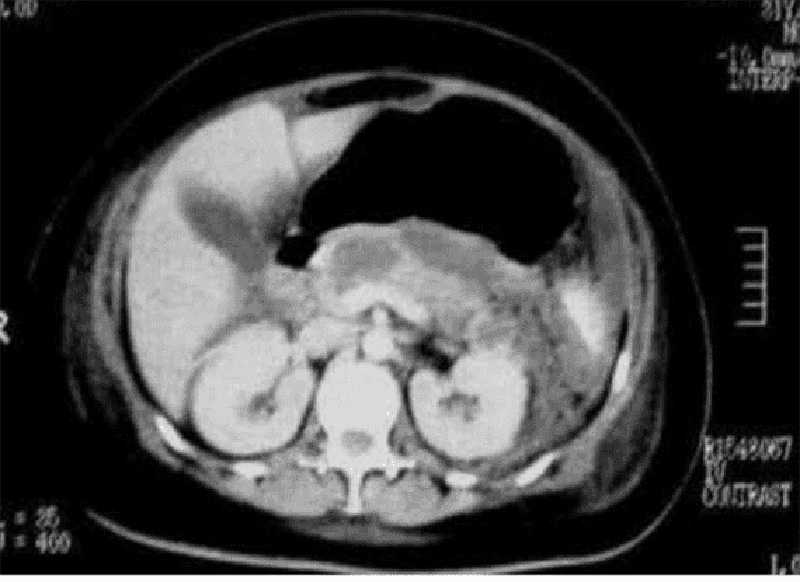
A 54-year-old male presents to the emergency department with a 1-week history of abdominal pain. His other symptoms are nausea, vomiting, low-grade fever, and loss of appetite. He does not use alcohol. He has a seizure disorder, for which he takes a "prescription drug." X-ray films of his chest and abdomen show no abnormalities. His abdominal CT scan is shown below. Which of the following is the most likely explanation for this patient's abdominal symptoms?
Gall bladder pathology
Kidney pathology
Pancreas pathology
Air in the stomach
Liver pathology
A 50-year-old man presents with a 3-hour history of right arm pain. Two weeks ago, he was treated for superficial thrombophlebitis of the right cephalic and right saphenous veins. For the past two months, he has had significant back pain, which is being treated with NSAIDs. His temperature is 37.0C (98.6F), blood pressure is 140/80 mm Hg, pulse is 70/min, and respirations are 10/min. Physical examination shows a swollen, ruddy and warm right arm, but is otherwise unremarkable. Cervical and chest x-ray films show no abnormalities. Laboratory studies show: Hct 50% Platelets 120,000/cmm WBC 9,600/cmm Neutrophils 60% Eosinophils 2% Basophils 0% Lymphocytes 31% Monocytes 7% PT 25 sec PTT 39 sec Fibrinogen 300 mg/dL Fibrin split products positive Which of the following is the most appropriate next step in management?
Protein C, S and antithrombin III levels
Perfusion scintigraphy of the lungs
Venography of right brachial, axillary and subclavian veins
CT of the chest abdomen and pelvis
CT of the thoracic outlet

A 70-year-old male presents to the emergency room complaining of weakness, dizziness and back pain. He denies nausea, vomiting, diarrhea, chest pain, palpitations, shortness of breath, urinary symptoms, or black stools. His past medical history is significant for diabetes mellitus, diabetic nephropathy and retinopathy, hypertension, atrial fibrillation and chronic leg cellulitis. He takes warfarin for chronic anticoagulation. On physical examination, his blood pressure is 139/75 mmHg and his heart rate is 110 and irregular. His WBC count is 10,500/mm3, hemoglobin level is 7.0 mg/dl and platelet count is 170,000/mm3. An abdominal CT image is shown on the slide below. Which of the following is the most likely diagnosis?
Renal cell carcinoma
Vertebral fracture
Retroperitoneal hematoma
Hydronephrosis
Mesenteric ischemia
A 43-year-old man is evaluated for a one-year history of chronic abdominal pain. He describes episodes of epigastric and left upper quadrant pain that last for hours and are not relieved by antacids. Certain foods can precipitate the pain. He also complains of occasional diarrhea. The patient has lost 10 pounds over the last 6 months. Four years ago he was hospitalized for three days with acute abdominal pain. He smokes one pack of cigarettes a day and consumes alcohol regularly. His family history is significant for diabetes mellitus in his mother and prostate cancer in his father. Which of the following is most likely to diagnose this patient's condition?
D -xylose absorption test
Serum amylase and lipase
Radioisotope (HIDA) scans
CA 19-9 and CEA levels
Stool elastase
A 50-year-old woman comes to clinic due to several episodes of severe watery diarrhea for the past 15 days. There is 4/10 pain all over her abdomen but she has not noticed any blood in her stools. She has normal diet and has not travelled anywhere recently. She denies any one around her having similar complaints. She also had occasional cramps in her leg muscles and feels dehydrated. She smokes one to two cigarettes a day and drinks socially. Her temperature is 36.8C (98.1F), blood pressure is 108/64 mm Hg, pulse is 118/min, and respirations are 18/min. On examination her abdomen is slightly tender. Laboratory results are as follows. WBC 5600mm3 Hemoglobin 13.6 Hematocrit: 41%, Platelets 209,000mm3 Sodium 138mEq/L Potassium: 2.1mEq/L Bicarbonate: 35mEq/L Blood urea nitrogen: 16 mg/dl Creatinine: 0.8 mg/dl Glucose 106 mg/dl A CT abdomen is ordered which shows a mass in the head of pancreas. What is the most probable diagnosis?
Pancreatic adenocarcinoma
Glucagonoma
Lnsulinoma
VIPoma
Gastrinoma
A 37 -year-old male is brought to the emergency department due to an episode of hematemesis. He has a history of peptic ulcer disease. A nasogastric tube lavage yields coffee-ground-like material. Physical examination reveals pallor and delayed capillary refill, without cyanosis. His temperature is 36.7C (98F), blood pressure is 85/40 mm Hg, pulse is 125/min, and respirations are 18/min. Which of the following is the most appropriate first step in management?
Intravenous octreotide
Upper GI endoscopy
Surgical intervention
Intravenous pantoprazole
Fluid resuscitation
A 35-year-old Caucasian male presents to the emergency department with two episodes of bloody vomiting which occurred one-half hour ago. He has a history of migraines. For the past two days, he has been having severe headaches and has taken 20 tablets of aspirin without relief. He then resorted to heavy drinking and forgot about the pain. He drinks alcohol "occasionally" and has been smoking 1 pack of cigarettes daily for the past 18 years. Which of the following is the most likely explanation for this patient's hematemesis?
Esophageal variceal bleeding
Acute erosive gastritis
Mallory Weiss syndrome
Fulminant hepatic failure
Acute platelet dysfunction
A 52-year-old woman with cirrhosis presents with increasing abdominal distension. Her treatment regimen was amended three days ago, when furosemide was added to spironolactone and sodium/water restriction. However, her distension persists, and today she is very somnolent and has passed very little urine. Her past medical history is remarkable for chronic hepatitis type B, cirrhosis, encephalopathy, and 2 bleeding episodes from esophageal varices; the bleeding was controlled with sclerotherapy. Her temperature is 36.5C (97.6F), blood pressure is 90/60 mm Hg, pulse is 80/min, and respirations are 18/min. Abdominal examination shows distension, shifting dullness, and no tenderness; bowel sounds are present. Laboratory studies show: Hemoglobin 11.0 g/L Leukocyte count 3,500/mm3 Serum sodium 125 mEq/L Serum potassium 5.5 mEq/L Chloride 103 mEq/L Blood urea nitrogen 60 mg/dL Serum creatinine 1.8 mg/dL Prothrombin time 18 sec Partial thromboplastin time 35 sec Urinalysis shows no abnormalities. Ultrasound of the kidney is unremarkable. Which of the following is the most appropriate next step in management?
Increase the dose of furosemide to its maximum
Careful volume loading and discontinuation of furosemide and spironolactone
Tapping of ascites
Renal biopsy
Intravenous pyelography
An 83-year-old woman presents with a 1-year history of progressively severe crampy abdominal pain after eating. She has started avoiding food because of the pain. The pain is often associated with bloating, nausea, and occasional diarrhea. She has had a 15 kg (331b) weight loss over the past year. Her other medical problems include hypertension, diabetes mellitus-type 2, hypercholesterolemia, peripheral vascular disease, coronary artery disease and myocardial infarction. Social history is not significant. Abdomen is soft, nontender and non-distended. Abdominal x-ray and CT scan are unremarkable. Which of the following is the most likely diagnosis?
Chronic pancreatitis
Atherosclerosis of the mesenteric arteries
Crohn' s disease
Irritable bowel syndrome
Celiac disease
A 45-year-old Asian-American female comes to the physician due to bloating, flatulence, abdominal cramps and explosive watery diarrhea. These symptoms occur after ingesting dairy products. She has not had any weight loss. She has not had bone pain or easy bruising. Physical examination shows abdominal distention and borborygmi. You decide to investigate the patient further. Which of the following test results is most likely to be observed?
Positive urine test for reducing substances
Decreased stool osmotic gap
Positive hydrogen breath test
Alkaline stool pH
Positive acid steatocrit test
A 50-year-old male undergoes vagotomy and pyloroplasty for a peptic ulcer perforation. His early postoperative course is complicated by fever and hypotension, which are treated with broad-spectrum antibiotics and IV fluid support. He then recovers well; however, on post-operative day 6 he develops nausea, vomiting, abdominal pain, and profuse, watery diarrhea. His temperature is 38.9 C (102 F), blood pressure is 110/70 mmHg, pulse is 120/min, and respirations are 18/min. Abdominal examination shows tenderness in the sigmoidal area. Test of the stool for occult blood is negative. Laboratory studies show: Hb 11.5g/dL Platelet count 180, 000/cmm Leukocyte count 17, 500/cmm Segmented neutrophils 75% Bands 10% Eosinophils 1% Lymphocytes 14% Which of the following is the most appropriate next step in management?
Blood cultures
Colonoscopy
Stool cultures
Cytotoxin assay in the stool
Observation
A 65-year-old woman presents with painless intermittent rectal bleeding. The bleeding is bright red in color. She does not have abdominal pain, nausea, or vomiting. She has a history of hypertension, diabetes mellitus, and hypercholesterolemia. Her temperature is 36.7C (98 F), blood pressure is 140/80 mmHg, pulse is 80/min, and respirations are 16/min. Physical examination shows a systolic ejection murmur in the right second intercostal space; examination is otherwise unremarkable. Sigmoidoscopy shows no abnormalities. Which of the following is the most likely diagnosis?
Vascular ectasia
Ischemic colitis
Diverticulosis
Carcinoma colon
Hemorrhoids
A 45-year-old white male comes to your office for evaluation of diarrhea of 8-months duration. He says that he has lost almost 15 lbs during the past 8 months. He denies any blood in the stools. 24-hour stool collection reveals fecal fat of 10 gm/day. Stool microscopy reveals no pathogens and no leucocytes. D-xylose test was performed which shows that less than 2 grams of D-xylose is excreted in urine in 5 hours. D-xylose test was re-performed after 4-week treatment with antibiotics but excretion is still less than 2 grams in 5 hours. Based on these findings, what is the most likely diagnosis in this patient?
Lactose intolerance
Bacterial overgrowth
Celiac disease
Pancreatic insufficiency
Terminal ileal disease
A 27 -year-old male presents with a history of intermittent abdominal distention, flatulence and greasy stools. He also complains of fatigue. He has no other medical problems. His family history is unremarkable. He does not use tobacco, alcohol or smoking. His vital signs are within normal limits. Physical examination shows a pruritic, papulovesicular rash over the extensor surfaces of the extremities and over the trunk, scalp and neck. His abdomen is soft, nontender and non-distended. Stool for occult blood testing is negative. Lab studies show: Hemoglobin 10.0 g/L MCV 75 fl Platelets 340,000/mm3 Leukocyte count 4,500/mm3 Neutrophils 56% Eosinophils 1% Lymphocytes 33% Monocytes 10% Which of the following is the most likely diagnosis of his skin condition?
Guttate psoriasis
Dermatitis herpetiformis
Pityriasis rose a
Seborrheic dermatitis
Bullous pemphigoid
A 68-year-old woman with a history of heavy alcohol use and chronic pancreatitis presents with a several month history of recurrent epigastric pain. The pain is occasionally associated with nausea and vomiting. She has lost 15 lbs (6.8 kg) over the past 3 months. She is afebrile. Physical examination shows scleral icterus. Laboratory studies show: Albumin 3.0 mgldl Total bilirubin 3.5 mgldl Direct bilirubin 24 mgldl Alkaline phosphatase 220 U/L Aspartate aminotransferase (SGOT) 28 U/L Alanine aminotransferase (SGPT) 25 U/L Amylase 145 U/L Lipase 100 U/L Which of the following is the most appropriate next step in management?
ERCP
CT scan of the abdomen
MRI of the abdomen
Plain abdominal radiography
Upper GI endoscopy
A 29-year-old male with a 6-year history of HIV infection presents with chronic, severe diarrhea associated with malaise, nausea, anorexia and abdominal cramps. His last CD4 count was 80cells/mm3. A modified acid-fast stain of a stool specimen shows 4-6 mm oocysts. Which of the following is the most likely microorganism responsible for this condition?
Mycobacterium avium complex
Cryptosporidium parvum
Isospora belli
Pneumocystis jiroveci
Microsporidia
A 56-year-old man comes to the emergency department due to a one-day history of abdominal pain and increasing distension. He has not passed flatus during this time. He has had nausea without vomiting. He has a history of cirrhosis secondary to chronic alcoholism. He is taking spironolactone and furosemide. His temperature is 38.0C (101.3F), blood pressure is 120/70 mm Hg, pulse is 100/min, and respirations are 24/min. Physical examination shows a slightly confused man with a flapping tremor. Breathing is labored and lungs are clear to auscultation. Abdominal examination shows distension, tenderness to palpation with rebound, and no guarding; a fluctuating wave and shifting dullness are present. Abdominal auscultation shows splashing and markedly decreased bowel sounds. An x-ray film of the chest shows no abnormalities. An x-ray film of the abdomen shows gas in the small and large bowels without air-fluid levels. Which of the following is the most appropriate next step in management?
Barium enema
Sigmoidoscopy
Ultrasound of abdomen
Diagnostic peritoneal lavage
Diagnostic paracentesis
A 49-year-old woman presents with a two-week history of lower abdominal pain and severe diarrhea. The stools are watery without blood or mucus. The abdominal pain is mild and unrelated to her stools. She has had recent episodes of flushing. She has not had fever. There is no history of travel. She does not smoke or drink alcohol. Her past surgical history includes a fracture repair of her right leg 3 years ago. Her temperature is 36.6C (97.8F), blood pressure is 106/68 mm Hg, pulse is 103/min, and respirations are 20/min. Oxygen saturation is 99% on room air. Physical examination shows facial flushing, a prominent jugular venous pulse and expiratory wheezes. Which of the following is the most likely diagnosis?
Diverticulitis
Infectious gastroenteritis
Lnflammatory bowel disease
Carcinoid syndrome
Irritable bowel syndrome
A 42-year-old male presents with a 2-year history of heartburn. The heartburn occurs after heavy meals and while supine. Over time, his symptoms have been increasing in severity and frequency. His symptoms used to be alleviated with the use of over-the-counter antacids, but these have become ineffective in the past two months. He also complains of epigastric pain and occasional vomiting, both of recent onset, especially in the morning. He denies dysphagia or odynophagia. He eats junk food and drinks two cups of coffee daily. He regularly drinks grape brandy and smokes 1 pack of cigarettes/day. Abdominal examination shows epigastric tenderness. Abdominal ultrasound is unremarkable. Test of the stool for occult blood is negative. Which of the following is the most appropriate next step in management?
Treatment with ranitidine
Upper Gl endoscopy
Barium swallow
Manometric studies
Reassurance
A 45-year-old Caucasian male presents with a 2-year history of progressive heartburn which is most severe while supine. Over-the-counter antacids have not relieved his symptoms. Endoscopy shows a hiatal hernia. The patient is reluctant to accept any treatment. Which of the following is he at risk for if his condition is left untreated?
Peptic ulceration
Squamous cell carcinoma of esophagus
Aspiration pneumonia
Mallory Weiss syndrome
Adenocarcinoma of esophagus
A 34-year-old Caucasian male presents to the office with a 4-week history of diarrhea. He just returned from a trip to South America, where he developed foul-smelling stools, abdominal cramps and bloating. A three-day course of ciprofloxacin did not relieve his symptoms. His vital signs are within normal limits. Physical examination shows no abnormalities. Which of the following is the most appropriate next step in management?
Schedule colonoscopy
Obtain CT scan of the abdomen
Prescribe oral metronidazole
Prescribe another course of ciprofloxacin
Prescribe oral ampicillin
A 55-year-old male comes to the physician with a history of diarrhea, weight loss, bloating, and excessive flatulence. His symptoms began soon after having "stomach surgery" two years ago. He has a history of gastric ulcers. Physical examination shows scarring associated with past surgery, and abdominal distention with identifiable succussion splash. Laboratory studies show anemia with MCV of 100fl. Which of the following is the most likely diagnosis?
Short bowel syndrome
Bacterial overgrowth
Peptic ulcer disease
Crohn's disease
Ulcerative colitis
A 45-year-old male comes to the physician with a 6-month history of periodic abdominal pain. He tried several over-the-counter medications including H2 blockers and proton pump inhibitors with moderate success. Workup, including an upper GI series and endoscopy, showed multiple duodenal ulcers and a single jejunal ulcer. Test of the stool for occult blood is positive. Test of the stool for fat is positive. Which of the following is the best explanation for this patient's impaired fat absorption?
Pancreatic enzyme deficiency
Pancreatic enzyme inactivation
Reduced bile salt absorption
Defective intestinal absorption
Bacterial proliferation
A 66-year-old man returns to the emergency department (ED) for a second time because of persistent left lower quadrant pain and developing fever, despite 48 hours of oral antibiotics. He had presented to the ED 2 days ago because of left lower quadrant pain. He was able to tolerate a diet and had no fever; he was then sent home on antibiotics, and instructed to return if there was no improvement. He has a 2-week history of constipation without regular bowel movements. Laxatives have not relieved his symptoms. His diet consists of meat with very few vegetables. His vital signs are within normal limits, except for a low-grade fever. Abdominal examination shows left lower quadrant tenderness and guarding. Rectal examination shows no abnormalities. Laboratory studies show a WBC of 16,400/cmm. He is admitted and started on IV antibiotics. Forty-eight hours later, his symptoms persist without any improvement. Which of the following is the most appropriate next step in management?
Abdominal x-rays
Flexible sigmoidoscopy
Colonoscopy
CTscan
Barium enema
A 58-year-old man presents with a one-year history of diarrhea. The stools are watery and accompanied by abdominal cramps. He denies any fever, blood per rectum, or foul-smelling stools. He has also experienced frequent episodes of dizziness, flushing, wheezing, and a feeling of warmth. He has taken herbal medicines, which failed to relieve his symptoms. He is depressed about his illness, and feels hopeless about diagnosis and treatment. He appears ill. Auscultation of the chest shows a 2/6 systolic murmur over the left lower sternal border. Abdominal examination shows hepatomegaly 3cm below the right costal margin, mild shifting dullness, and no abdominal tenderness. Laboratory studies show: Hb 13.0gm/dl MCV 90fl WBC 6,100/cmm Platelets 210,000/cmm AST101 U/L ALT 99 U/L Alkaline phosphatase 400 mg/dl This patient is at risk of developing a deficiency of which vitamin or mineral?
Vitamin A
Lron
Niacin
Calcium
Vitamin C
A 50-year-old female presents with a 3-year history of abdominal pain and diarrhea. She has not been evaluated by a physician. Recently, her symptoms have been progressively worsening. Endoscopy shows multiple ulcerations of the duodenum and prominent gastric folds. Secretin stimulation test shows increased gastrin secretion. Which of the following is most likely associated with this patient's condition?
Medullary thyroid cancer
Pheochromocytoma
Primary hyperparathyroidism
Neuromas
Marfanoid habitus
A 58-year-old woman presents to the emergency department with right subcostal heaviness, intermittent pain, food intolerance, and 13.2 lbs-weight loss (6kg) over the past 2 months. Her pain has been worsening for the past 2 days; it was initially localized to the right upper quadrant, but has now shifted to her back. Her past medical history is remarkable for appendicitis, which was complicated by perforation and peritonitis 20 years ago. Abdominal examination shows epigastric tenderness. There is a palpable mass below the right costal margin. Murphy's sign is negative. Abdominal ultrasound shows an enlarged gallbladder and dilation of the hepatic ducts. Laboratory studies show: WBC 11,000/cmm Total bilirubin 24 mg/dl Direct bilirubin 1.6 mg/dl Alkaline phosphatase 310 U/L Aspartate aminotransferase (SGOT) 87 U/L Alanine aminotransferase (SGPT) 56 U/L Amylase 140 U/L Which of the following is the most appropriate next step in management?
Plain abdominal film
Endoscopic retrograde cholangiopancreatography
Percutaneous transhepatic cholangiography
CT scan of the abdomen
HIDA scan for cystic duct obstruction
A 50-year-old white male presents with complaints of bitter taste and central chest pain. He further describes he pain as moderate-to-severe, occurring during or after meals, non-radiating, and burning. The pain is relieved with antacids, and worsened by lying supine. He has lost 10 lbs (4.5kg) over the past 5-months (unintentional). He has smoked 2 packs of cigarettes daily for 20 years. His vital signs are stable, and he is afebrile. The physical examination is unremarkable. Chest x-ray and EKG show no abnormalities. Which of the following is the most appropriate next step in management?
Treatment with antacids
Treatment with famotidine
Treatment with omeprazole
Esophagoscopy\
Esophageal pH monitoring
A 63-year-old man presents with a 2-month history of dysphagia for both solids and liquids. He has had a 6.6 lb (3kg) weight loss over this time. His past medical history is remarkable for a transient ischemic attack 6 months ago, two bouts of pneumonia in the past 3 months, and chronic heartburn treated with over-the-counter antacids. Physical examination shows a supple neck without masses. Abdominal examination shows mild epigastric tenderness to deep palpation. Chest x-ray is normal for his age. Which of the following is the most appropriate next step in diagnosis?
Endoscopy
Barium swallow
Motility studies
Video fluoroscopy
24-hour pH monitoring
A 27-year-old Caucasian woman presents with abdominal pain, diarrhea and a 4.5 (2kg) weight loss for the past two months. She describes the abdominal pain as intermittent, moderate-to-severe, and located in the right lower quadrant. Over the past 48 hours, the pain has intensified. Her temperature is 37.6C (99.6F), blood pressure is 120/70 mm Hg, pulse is 100/min, and respirations are 14/min. Several shallow ulcers are present in her mouth. Abdominal examination shows tenderness in the right lower quadrant without rebound. Rectal examination shows mucus. Rectosigmoidoscopy is unremarkable. An x-ray film of the abdomen shows gas in the small and large bowels. Laboratory studies show: Hb 10.2 g/dL WBC 16,500/cmm Platelet count 530,000/cmm ESR 48/hr Which of the following is the most likely diagnosis?
Diverticulitis
Celiac disease
Irritable bowel syndrome
Crohn's disease
Ulcerative colitis
A 65-year-old man treated for heart failure with enalapril and digoxin presents to the emergency department (ED) with palpitations. His blood pressure is 160/ 100 mmHg, and heart rate is 110/min. His rhythm is irregular. His lungs are clear on auscultation. His abdomen is soft and non-distended. Mild epigastric tenderness is elicited on deep palpation. ECG shows atrial fibrillation without acute ischemic changes. Cardiac enzyme levels are normal. Treatment with warfarin and verapamil is initiated, and the patient is eventually discharged home. After two weeks, he returns to the ED to complain of profound anorexia. Which of the following is the most likely cause of his current complaint?
Gastric irritation
Pancreatitis
Drug interaction
Occult carcinoma
Gastrointestinal bleeding
A 65-year-old Caucasian male presents to your office with a several month history of difficulty swallowing. He has noticed a right-sided neck mass which increases in size while drinking fluids. His past medical history is significant for hypertension, gastroesophageal reflux disease, and osteoarthritis of his right knee. His current medications include hydrochlorothiazide, ranitidine, and occasional naproxene. You order a barium examination of the esophagus to visualize the abnormality. Which of the following is the most important pathogenetic factor in the development of this patient's problem?
Motor dysfunction
Acid reflux
Lnflammation
Abnormal proliferation
Metabolic abnormalities
A 52-year-old Caucasian male comes to you for a routine health check-up. You decide to do age-appropriate screening in this patient and order a colonoscopy. The colonoscopy is normal, except for a 1.5cm polyp in the left descending colon. A colonoscopic polypectomy is done and the biopsy results are pending. The patient is anxious to know the expected biopsy results and the risk of cancer. Which of the following types of polyps is considered to be most premalignant?
Hamartomatous polyp
Hyperplastic polyp
Villous adenoma
Tubulovillous adenoma
Tubular adenoma
A 47 -year-old male comes to the emergency department complaining of an intense burning pain in his abdomen. The pain started a couple of hours ago and is getting worse. He also has nausea and vomited twice. The vomitus is described as dark red-brown in color. He drank "quite a bit of alcohol' last night. He has had several episodes of this type of pain before, and was diagnosed with peptic ulcer disease five years ago. Several courses of H. Pylori eradication therapy have been prescribed in the past, but the patient admits to being non-compliant. He admits to smoking and drinking heavily. His temperature is 36.8 C (98.2 F), blood pressure is 126/88 mm Hg, pulse is 98/min, and oxygen saturation is 96% on room air. The physical examination is remarkable for marked epigastric tenderness. No masses or rebound tenderness are appreciated. IV fluids are administered, blood tests are taken, and upper GI endoscopy is being arranged. Which of the following serum markers is most likely to be elevated in this patient?
Platelet count
Blood urea nitrogen
Prothrombin time
Potassium
Creatinine
A 65-year-old male complains of fatigue for the past one month. He has been living alone since the death of his wife one year ago. He does not like to cook, and his diet consists mostly of canned food, hot tea, and toast. He drinks one glass of white wine nightly with dinner. Examination shows pallor of the skin, nail beds and conjunctiva. Rectal exam is heme-negative. His physical examination is otherwise unremarkable. Administration of which of the following would be most helpful in treating his condition?
Vitamin 8 12
Folic acid
Vitamin C
Vitamin D
Vitamin E
A 50-year-old white male comes to the physician's office because of diarrhea, abdominal pain and weight loss. He has bulky, foul-smelling stools, abdominal distension and flatulence. He also has arthralgias and a chronic cough. His temperature is 37.8C (100F), blood pressure is 120/80 mm Hg, pulse is 80/min, and respirations are 18/min. Physical examination shows generalized lymphadenopathy, skin hyperpigmentation and a diastolic murmur in the aortic area. Small bowel biopsy shows villous atrophy with numerous PAS-positive materials in the lamina propria. Which of the following is the most likely diagnosis?
Celiac disease
Tropical sprue
Crohn's disease
Whipple's disease
Cystic fibrosis
A 65-year-old Asian male presents to the physician with a four-week history of weakness and vague postprandial epigastric pain. His past medical history is insignificant. He does not take any medications. He smokes 1½packs of cigarettes daily and drinks alcohol occasionally. The fecal occult blood test is positive. Gastroduodenoscopy shows an antral ulcer. Four of seven biopsies taken from the margins of the ulcer are consistent with adenocarcinoma. Which of the following is the most appropriate next step in management?
Helicobacter pylori testing
Serologic markers
A CTscan
Laparoscopy
Exploratory laparotomy
A 20-year-old male university student presents with a one-month history of 4 to 6 loose watery bowel movements per day with occasional tenesmus, urgency, and abdominal cramps. He also describes a two-week history of intermittent bright red blood per rectum. His appetite and energy levels are excellent and his weight is stable. He is otherwise healthy and takes no medications. His family history is unremarkable. He has not recently used antibiotics nor has he traveled outside the country. He does not use tobacco, alcohol or drugs. Sigmoidoscopy demonstrates mild erythema and rectal biopsy confirms acute mucosal inflammation. Which of the following is a potential complication of this condition requiring regular surveillance?
Toxic megacolon
Perianal fistula
Sclerosing cholangitis
Uveitis
Colorectal carcinoma
A 27 -year-old male returning home after a three-month visit to Puerto Rico presents with diarrhea for the past 6 weeks. Other accompanying symptoms include cramps, gas, fatigue and progressive weight loss. Abdominal auscultation shows hyperactive bowel sounds, and borborygmi. The family history is unremarkable for intestinal disease. Laboratory studies show anemia with a hematocrit of 25% and MCV of 105fl; stool examination for ova and parasites is negative. Small intestinal mucosal biopsy shows blunting of villi with infiltration of chronic inflammatory cells, including lymphocytes, plasma cells, and eosinophils. Which of the following is the most likely diagnosis?
Celiac disease
Amoebiasis
Tropical sprue
Bacterial overgrowth
Giardiasis
A 46-year -old alcoholic man comes to the emergency department because of several episodes of vomiting. The last episode of emesis contained blood. Five hours ago, he had a fatty meal and several alcoholic drinks. Two days ago, he had an upper GI tract endoscopy and abdominal ultrasound for the evaluation of dyspepsia. The endoscopy was unremarkable, and the ultrasound showed a hyperechogenic enlarged liver and stones in the gallbladder. His temperature is 36.6C (97.9F), blood pressure is 120/70 mm Hg, pulse is 95/min, and respirations are 15/min. Laboratory studies show: Hb 12.8 g/dl WBC 5,400/cmm BUN 26 mg/dl Creatinine 1.1 mg/dl AST 100 U/L ALT 45 U/L Bilirubin 0.7 mg/dl Nasogastric suction shows normal stomach contents mixed with bright red blood. The rectal examination shows no melena. Which of the following is the most likely explanation for this patient's bloody vomiting?
Ruptured submucosal esophageal veins
Endoscopy-related esophageal perforation
Stress gastritis
Hemobilia
Tears in the mucosa of the cardia
A 45-year-old male presents to the office with complaints of progressive difficulty in swallowing both solids and liquids. His other complaints include occasional regurgitation of undigested food, and a nighttime cough which disturbs his sleep. The physical examination is unremarkable. Barium studies show a dilated esophagus, loss of esophageal peristalsis, and smooth tapering of the distal esophagus. Which of the following is the most appropriate next step in management?
Esophagoscopy@
Esophageal manometry
Esophageal pH monitoring
Botulinum toxin injection
Pneumatic dilation
A 53-year-old woman presents to your office with right-sided abdominal pain that started two days ago. She describes the pain as constant and burning in nature. There is no associated nausea, vomiting or diarrhea. The patient reports taking over-the-counter antacids and ibuprofen, which brought no relief. Her medical history is significant for breast cancer diagnosed one year ago, for which she underwent a modified radical mastectomy and is receiving chemotherapy, the last course of which was completed two months ago. On physical examination, her temperature is 36.7C (98.F), blood pressure is 120/70 mm Hg, pulse is 80/min, and respirations are 16/min. Her lung fields are clear to auscultation and her abdomen is soft and non-distended. The liver span is 10 cm and the spleen is not palpable. Lightly touching the skin to the right of the umbilicus elicits intense pain. In one week the patient is most likely to develop:
Intestinal obstruction
Skin lesions
Ascites
Fever and jaundice
Black stool
A 76-year-old man with multi-infarct dementia is brought to the emergency department because of lethargy. For the past 6 months, he has had difficulties with feeding and occasionally regurgitates undigested food. In recent days, his condition has deteriorated, and he has become lethargic. He has a history of hypertension for 15 years, chronic atrial fibrillation for 7 years, dementia for 5 years, and frequent respiratory tract infections for the past year. His temperature is 37.8C (101.5F), blood pressure is 150/95 mm Hg, pulse is 120/min, and respirations are 26/min. Physical examination shows foul-smelling breath; there is a fluctuating mass in the left side of his neck. Auscultation shows crackles in the right lung base. An x-ray film of the chest shows multiple infiltrates without cavitation in the right lower lung field. The patient is admitted, sputum and blood cultures are sent, and antibiotics are started. Which of the following is the most appropriate next step in management?
Puncture of the neck mass
Esophagoscopy
Esophagography
Bronchoscopy
CT of the neck
A 69-year-old man has had pain in left lower quadrant (LLQ) for 3 days. The pain was intermittent, but since yesterday it has been constant. He also had sweating and chills for the last 2 days. He hasn't had a bowel movement for 4 days, but has passed flatus. He vomited once and still has nausea. His past medical history is remarkable for constipation and nephrolithiasis. His vital signs are: PR: 110/min; BP: 122/80mm Hg; RR: 24/min; Temperature: 38.6C (101.3F). His abdomen is soft and tender to palpation in the left lower quadrant. Deep palpation is difficult but reveals no masses or organomegaly. Bowel sounds are decreased. Rectal exam is positive for enlarged prostate. Costovertebral angle tenderness is absent. Ultrasound shows bilateral hydronephrosis and stones in the kidneys. His laboratory test results are: WBC 14,500/cmm Hb 11.7gm/dl Hct 34% ESR 40/hour BUN43 mg/dl Creatinine 2.0 mg/dl Urinalysis RBC 4-10/hpf; WBC 3/hpf; few hyaline casts; many oxalate crystals. The next step should be:
Intravenous pyelography
Sigmoidoscopy
Contrast enema
CT of abdomen
Upright abdominal film
A 33-year-old male is admitted to the hospital after an episode of tonic-clonic seizures. He is a known IV drug abuser. He admits 'shooting' cocaine and heroin prior to the seizure. He has never had seizures before. Fallowing the seizure, he complains of muscle pain but otherwise feels normal. His temperature is 37.2°C (98.9°F) and his blood pressure is 156/90 mm Hg. Laboratory analyses reveal the following: CPK 11,200 U/ml AST 545 U/L ALT 560U/L Troponin T normal Anti-HAV antibodies negative HBsAg negative Anti-HBsAg negative Anti-HCV antibodies positive He reports that a recent HIV test was negative. Which of the following is the best management for this patient?
Fluid restriction
Metoprolol
Hepatitis B vaccination
Life-long phenytoin therapy
No intervention
A 46-year-old white male presents with chronic diarrhea, abdominal distention, flatulence, and weight loss. He also has arthralgias and bulky, frothy stools. He has never had blood transfusions, tattooing or highrisk sexual behaviors. His temperature is 38.3C (101F), blood pressure is 130/90 mm Hg, pulse is 84/min, and respirations are 16/min. Physical examination shows generalized lymphadenopathy and skin hyperpigmentation Which of the following is the most appropriate diagnostic test?
SerumTSH
Antinuclear antibody (ANA) titer
Gamma-glutamyl transpeptidase levels
ELISA for anti-HIV antibodies
Endoscopy with small bowel biopsy
A 40-year-old male comes to the physician complaining of diarrhea with pale, voluminous, foul-smelling stools that are difficult to flush. He has had this problem sporadically for years, but has neglected medical care. He also has severe, intermittent, epigastric pain lasting 15 to 30 minutes after eating. He admits to chronic alcohol consumption. Physical examination shows no abnormalities. Which of the following is the best test to confirm fat malabsorption in this patient?
Sudan Ill stain
72-hour fecal fat collection
Acid steatocrit
D-xylose test
Lactose tolerance test
A 37-year-old male prisoner has been complaining of fever, chills and abdominal pain over the last week. He vomited once before reaching the emergency room. On physical examination, his blood pressure is 112/63 mmHg and his heart rate is 115/min. Breath sounds are diminished at the left lung base and there is marked left upper quadrant tenderness. Laboratory values are given below: WBC count 23,500/mm3 Neutrophils 65% Bands 11% Hemoglobin 12.5 mg/dL Platelets 250,000/mm3 Total bilirubin 3.1 mg/dL AST 46 units/L AL T 70 units/L Alkaline phosphatase 120 units/L CT scan of the abdomen reveals a fluid collection within the spleen. Which of the following is the most likely diagnosis?
Functional asplenia
Infectious endocarditis
Lnflammatory bowel disease
Portal hypertension
Infectious mononucleosis
A 20-year-old Caucasian male presents with lower abdominal pain for the past few hours. The pain first started around the umbilicus, but then shifted to the right lower abdominal area. He has had one episode of vomiting. Physical examination shows tenderness at McBurney's point. CT scan of the abdomen confirms the diagnosis of acute appendicitis. Which of the following explains the pathophysiology of the shifting of pain from the peri-umbilical area to the right lower quadrant in acute appendicitis?
Movement of inflammed appendix with bowel movements
Visceral followed by somatic pain
Somatic followed by visceral pain
Referred pain
Rupture of appendix with pus draining into right lower quadrant
A 40-year-old female presents with a 12-month history of episodes of chest pain and dysphagia. The episodes last from a few seconds to a few minutes. She has not had weight loss, fevers or chills. Chest-x ray, ECG and barium swallow show no abnormalities. Manometric studies show simultaneous high amplitude contractions with normal relaxation of the lower esophageal sphincter. Which of the following is the most likely diagnosis?
Zenker's diverticulum
Diffuse esophageal spasm
Achalasia
Scleroderma
Infectious esophagitis
A 29-year-old man presents to the ED complaining of RLQ pain for 24 hours. He states that the pain first began as a dull feeling around his umbilicus and slowly migrated to his right side. He has no appetite, is nauseated, and vomited twice. His BP is 130/75 mm Hg, HR is 95 beats per minute, temperature is 100.9°F, and his RR is 16 breaths per minute. His WBC is 14,000/μL. As you palpate the LLQ of the patient’s abdomen, he states that his RLQ is painful. What is the name of this sign?
Blumberg sign
Psoas sign
Obturator sign
Raynaud sign
Rovsing sign
A 40-year-old man with long-standing alcohol abuse complains of abdominal swelling, which has been progressive over several months. He has a history of gastrointestinal bleeding. On physical examination, there are spider angiomas and palmar erythema. Abdominal collateral vessels are seen around the umbilicus. There is shifting dullness, and bulging flanks are noted. Which of the following is the most important first step in the patient’s evaluation?
Diagnostic paracentesis
Upper GI series
Ethanol level
CT scan of the abdomen
Examination of peripheral blood smear
A 70-year-old man presents with a complaint of fatigue. There is no history of alcohol abuse or liver disease; the patient is taking no medications. Scleral icterus is noted on physical examination; the liver and spleen are nonpalpable. The patient has a normocytic, normochromic anemia. Urinalysis shows bilirubinuria with absent urine urobilinogen. Serum bilirubin is 12 mg/dL, AST and ALT are normal, and alkaline phosphatase is 300 U/L (three times normal). Which of the following is the best next step in evaluation?
Ultrasound or CT scan of the abdomen
Viral hepatitis profile
Reticulocyte count
Serum ferritin
Antimitochondrial antibodies
A 54-year-old man is brought to the ER because of an episode of coffee ground emesis and lightheadedness. He has a history of intravenous drug use, hepatitis C infection, and alcohol use. He says he has not had an alcoholic drink for about three days. He has been noncompliant with medications and follow-ups. He takes no medications. His temperature is 36.7C (98F), pulse is 110/min, respirations are 16/min, and blood pressure is 90/60 mmHg. Scleral icterus is present. Examination shows coffee ground material in the oropharynx. His lungs are clear. His abdomen is distended and a fluid wave is present. He is slightly tender to palpation in the epigastrium. Laboratory studies show: Complete blood count: Leukocyte count 9,500/mm3 Hemoglobin 10.0 g/L Platelets 120,000/mm3 Chemistry panel: Serum sodium 140 mEq/L Serum potassium 3.5 mEq/L Bicarbonate 27 mEq/L Blood urea nitrogen (BUN) 34 mg/dL Serum creatinine 0.8 mg/dL Coagulation studies : Prothrombin time 27 sec Partial thromboplastin time 42 sec Which of the following is the most appropriate next step in the management of this patient?
Whole blood transfusion
Fresh frozen plasma infusion
Hemodialysis
Pooled platelet transfusion
Plasmapheresis
A 55-year-old man with hypertension and end-stage renal disease requiring hemodialysis presents with 2 days of painless hematochezia. He reports similar episodes of bleeding in the past, which were attributed to angiodysplasia. He denies abdominal pain, nausea, vomiting, diarrhea, and fever. His vitals include HR of 90 beats per minute, BP of 145/95 mm Hg, RR of 18 breaths per minute, and temperature of 98°F. His abdomen is soft and nontender and his stool is grossly positive for blood. Which of the following statements are true regarding angiodysplasia?
They are responsible for over 50% of acute lower GI bleeding.
Angiography is the most sensitive method for identifying angiodysplasias
They are more common in younger patients
They are less common in patients with end-stage renal disease.
The majority of angiodysplasias are located on the right side of the colon
A 70-year-old woman presents to the ED with dark stool for 3 weeks. She occasionally notes bright red blood mixed with the stool. Review of systems is positive for decreased appetite, constipation, and a 10-lb weight loss over 2 months. She denies abdominal pain, nausea, vomiting, and fever, but feels increased weakness and fatigue. She also describes a raspy cough with white sputum production over the previous 2 weeks. Examination reveals she is pale, with a supine BP of 115/60 mm Hg and HR of 90 beats per minute. Standing BP is 100/50 mm Hg, with a pulse of 105 beats per minute. Which of the following is the most likely diagnosis?
Hemorrhoids
Diverticulitis
Mallory-Weiss tear
Diverticulosis
Adenocarcinoma@
A 52-year-old man has episodes of severe chest pain associated with dysphagia. He has been seen twice in the emergency room, and both times the symptoms responded to sub-lingual nitroglycerin. He then had a full cardiac evaluation including electrocardiogram (ECG), cardiac biomarkers, and an exercise stress test, which were all normal. Which of the following is the most likely diagnosis?
Herpetic infection
Motor disorder
Midesophageal cancer
Peptic stricture
External esophageal compression
A 16-year old girl has recently been referred to your family practice. She is a recent immigrant from Southeast Asia, and has been taking isoniazid (INH) and rifampin for uncomplicated tuberculosis. Routine blood tests are unremarkable, except for an elevated direct bilirubin. Other liver enzymes and function tests are completely normal. Which of the following is the most likely diagnosis?
Hemolytic anemia
INH toxicity
Crigler-Najjar syndrome type I
Rifampin toxicity
Rotor’s syndrome
A 45-year-old woman presents with a 1-week history of jaundice, anorexia, and right upper quadrant discomfort. On examination she is icteric, with a tender right upper quadrant and liver span of 14 cm. There is no shifting dullness or pedal edema and the heart and lungs are normal. On further inquiry, she reports consuming one bottle of wine a day for the past 6 months. Which of the following lab- oratory tests are most likely to be characteristic of a patient with jaundice secondary to alcoholic hepatitis?
Ratio of AST: ALT is 3:1 and the AST is 500 U/L
Ratio of AST: ALT is 2:1 and the AST is 250 U/L
Ratio of AST: ALT is 1:1 and the AST is 500 U/L
Ratio of AST: ALT is 1:1 and the AST is 250 U/L
Ratio of AST: ALT is 1:3 and the AST is 750
A husband and wife present to the ED with 1 day of subjective fever, vomiting, watery diarrhea, and abdominal cramps. They were at a restaurant a day before for dinner and both ate the seafood special, which consisted of raw shellfish. In the ED, they are both tachycardia with temperatures of 99.8°F and 99.6°F for him and her, respectively. Which of the following is responsible for the majority of acute episodes of diarrhea?
Parasites
Viruses
Enterotoxin-producing bacteria
Anaerobic bacteria
Invasive bacteria
A 78-year-old woman is brought to the ED by EMS complaining of vomiting and abdominal pain that began during the night. EMS reports that her BP is 90/50 mm Hg, HR is 110 beats per minute, temperature is 101.2°F, and RR is 18 breaths per minute. After giving her a 500 mL bolus of NS, her BP is 115/70 mm Hg. During the examination, you notice that her face and chest appear jaundiced. Her lungs are clear to auscultation and you do not appreciate a murmur on cardiac examination. She winces when you palpate her RUQ. An ultrasound reveals dilation of the common bile duct and stones in the gallbladder. What is the most likely diagnosis?
Cholecystitis
Acute hepatitis
Cholangitis@
Pancreatic cancer
Bowel obstruction
A 62-year-old man with a history of hypertension presents to the ED with severe constant mid-epigastric pain for the past hour. Over the last several months, he has had intermittent pain shortly after eating, but never this severe. He states he now has generalized abdominal pain that began suddenly about 15 minutes ago. He has no history of trauma, has never had surgery, and takes no medications. His vitals include HR of 115 beats per minute lying supine, increasing to 135 when sitting up, BP of 170/105 mm Hg supine, falling to 145/85 mm Hg when sitting up. He appears pale. His abdomen is rigid and diffusely tender with guarding and rebound. Bowel sounds are absent and stool hemoccult is positive. The white blood cell (WBC) count is 8500/μL, hemoglobin 8.5 mg/dL, hematocrit 27%, and platelets 255/μL. Which of the following is the most likely diagnosis?
Boerhaave syndrome
Perforated gastric ulcer
Abdominal aortic aneurysm (AAA)
Inflammatory bowel disease (IBD)
Diverticulosis
A 60-year-old man with a history of alcohol abuse presents to the ED with hematemesis for 1 day. He denies abdominal or chest pain. On physical examination, his eyes appear reddened which he attributes to having drunken heavily the night before (he also reveals vomiting several times after this recent binge). Vital signs are HR 115 beats per minute, BP 130/85 mm Hg, RR 18 breaths per minute, and temperature 99.5°F. Chest radiograph is unremarkable. Laboratory results reveal a WBC 10,000/μL, haemoglobin 14 mg/dL, hematocrit 40%, and platelets 210/μL. Which diagnosis is endoscopic evaluation most likely to confirm?
Esophageal varices
Boerhaave syndrome
Curling ulcer
Perforated gastric ulcer
Mallory-Weiss tear
A 40-year-old man with a recent history of exploratory laparotomy for a stabbing injury presents to the emergency department with diffuse cramping abdominal pain for 1 day, accompanied by nausea, multiple episodes of brown colored vomitus, and lack of stool, but he reports some flatulence. He denies any fever. On physical examination, the patient has stable vital signs, and there is diffuse distention in the abdomen with guarding and tenderness but no rebound, as well as high-pitched bowel sounds. Rectal examination reveals no fecal impaction in the rectal vault, and the stool was guaiac-negative. Complete blood cell count reveals no significant abnormalities and serum chemistry shows a mild metabolic alkalosis. CT demonstrates a noticeable difference in the diameter of proximal and distal small bowel. Which of the following is the most appropriate management?
Broad-spectrum antibiotics
Colonoscopy
Exploratory laparotomy with lysis of adhesions
Give the patient nothing by mouth, insert a nasogastric tube, and perform intravenous correction of electrolyte abnormalities
Serial abdominal examinations
The physician on call is called to the well-baby nursery because a full-term, African-American boy who is 49 hours old has not passed meconium. The pregnancy was uncomplicated. The neonate’s blood pressure is 70/50 mm Hg, heart rate is 140/min, and respiratory rate is 36/ min. The neonate is crying but is easily consolable. His abdomen is markedly distended. A barium enema is ordered, which shows dilated proximal bowel and a narrowed distal segment. Which of the following would provide a definitive diagnosis in this child?
Absent ganglion cells on rectal biopsy
Absent ligament of Treitz on upper gastro- intestinal series
Air bubbles in the stomach and duodenum on x-ray film of the abdomen
Positive sweat test
Telescoping of bowel on air contrast barium enema
A 73-year-old man comes to his primary care physician for his yearly check-up. His medical history is significant for obesity, new onset diabetes mellitus, and a remote history of tobacco use. The patient has noticed that his stool has been darker for the past 3 months, although he has only seen gross blood in his stool once, a week ago. He also complains of recent fatigue and occasional light-headedness when standing up from sitting. On examination the patient has fecal occult blood and a hematocrit of 32%. Colonoscopy and upper gastrointestinal endoscopy reveal no obvious pathology. Which of the following is the best diagnostic test to locate this patient’s hemorrhage?
Angiography
Barium enema
Colonoscopy
CT scan with contrast
Tagged RBC scan
A pregnant 16-year-old girl with no prior pre- natal care presents to the emergency department in labor. A male infant is delivered precipitously. Prenatal laboratory test results are unknown. There is no meconium. He has a birth weight of 3 kg (6 lb 10 oz). He is pink and is crying, heart rate is 130/min, and respiratory rate is 36/min, with good respiratory effort. The emergency medicine resident notices the infant has ascites and a membrane-covered anterior abdominal mass at the base of his umbilical cord. Which of the following is the most likely diagnosis?
Duodenal atresia
Gastroschisis
Hirschsprung’s disease
Meckel’s diverticulum
Omphalocele
A 50-year-old man is brought to the ED by ambulance with significant hematemesis. In the ambulance, paramedics placed two large-bore IVs and began infusing normal saline. In the ED, his HR is 127 beats per minute, BP is 79/45 mm Hg, temperature is 97.9°F, RR is 24 breaths per minute, and oxygen saturation is 96%. On physical examination, his abdomen is nontender, but you note spider angiomata, palmar erythema, and gynecomastia. Laboratory results reveal WBC 9000/μL, hematocrit 28%, platelets 40/μL, aspartate transaminase (AST) 675 U/L, alanine transaminase (ALT) 325 U/L, alkaline phosphatase 95 U/L, total bilirubin 14.4 mg/dL, conjugated bilirubin 12.9 mg/dL, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 110 mEq/L, bicarbonate 26 mEq/L, blood urea nitrogen (BUN) 20 mg/dL, creatinine 1.1 mg/dL, and glucose 150 mg/dL. Which of the following is the most likely diagnosis?
Perforated gastric ulcer
Diverticulosis
Splenic laceration
Esophageal varices
Ruptured AAA
A 70-year-old woman with a history of hypertension, congestive heart failure, and atrial fibrillation presents to the ED with several hours of acute onset diffuse abdominal pain. She denies any nausea or vomiting. The pain is constant, but she is unable to localize it. She was diagnosed with a renal artery thrombosis several years ago. Vital signs include HR of 95 beats per minute, BP of 110/70 mm Hg, and temperature of 98°F. Her abdomen is soft and mildly tender, despite her reported severe abdominal pain. Her WBC count is 12,000/μL, hematocrit 38%, platelets 250/μL, and lactate 8 mg/dL. The stool is traced heme-positive. You are concerned for acute mesenteric ischemia. What is the best way to diagnose this condition?
Serum lactate levels
Abdominal radiograph (supine and upright)
CT scan
Angiography
Barium contrast study
An 81-year-old diabetic woman with a history of atrial fibrillation is transferred to your emergency department (ED) from the local nursing home. The note from the facility states that the patient is complaining of abdominal pain, having already vomited once. Her vital signs in the ED are temperature 100.1°F, blood pressure (BP) 105/75 mm Hg, heart rate (HR) 95 beats per minute, and respiratory rate (RR) 18 breaths per minute. You examine the patient and focus on her abdomen. Considering that the patient has not stopped moaning in pain since arriving to the ED, you are surprised to find that her abdomen is soft on palpation. You decide to order an abdominal radiographic series. Which of the findings on plain abdominal film is strongly suggestive of mesenteric infarction?
Sentinel loop of bowel
No gas in the rectum
Presence of an ileus
Pneumatosis intestinalis
Air fluid levels
As you palpate the right upper quadrant (RUQ) of a 38-year-old woman’s abdomen, you notice that she stops her inspiration for a brief moment. During the history, the patient states that over the last 2 days she gets pain in her RUQ that radiates to her back shortly after eating. Her vitals include a temperature of 100.4°F, HR of 95 beats per minute, BP of 130/75 mm Hg, and RR of 16 breaths per minute. What is the initial diagnostic modality of choice for this disorder?
Plain film radiograph
Computed tomography (CT) scan
Magnetic resonance imaging (MRI)
Radioisotope cholescintigraphy (HIDA scan)
Ultrasonography
An undomiciled 41-year-old man walks into the ED complaining of abdominal pain, nausea, and vomiting. He tells you that he has been drinking beer continuously over the previous 18 hours. On examination, his vitals are BP 150/75 mm Hg, HR 104 beats per minute, RR 16 breaths per minute, oxygen saturation 97% on room air, temperature of 99.1°F rectally, and finger stick glucose 81 mg/dL. The patient is alert and oriented, his pupils anicteric. You notice gynecomastia and spider angiomata. His abdomen is soft but tender in the RUQ. Laboratory tests reveal an AST of 212 U/L, ALT 170 U/L, alkaline phosphatase of 98 U/L, total bilirubin of 1.9 mg/dL, international normalized ratio (INR) of 1.3, WBC 12,000/μL. Urinalysis shows 1+ protein. Chest x-ray is unremarkable. Which of the following is the most appropriate next step in management?
Place a nasogastric tube in the patient’s stomach to remove any remaining ethanol
Order a HIDA scan to evaluate for acute cholecystitis.
Administer hepatitis B immune globulin
Send viral hepatitis titers
Provide supportive care by correcting any fluid and electrolyte imbalances
A 23-year-old woman presents to the ED complaining of lower abdominal pain and vaginal spotting for 2 days. Her menstrual cycle is irregular. She has a history of ovarian cysts and is sexually active but always uses condoms. Her BP is 115/75 mm Hg, HR is 75 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. Which of the following tests should be obtained next?
Chlamydia antigen test.
β-Human chorionic gonadotropin (β-hCG)
Transvaginal ultrasound
Abdominal radiograph
Observe her abdominal pain, if it resolves discharge her with a diagnosis of menstruation
A 71-year-old obese man is brought to the ED complaining of constant left mid quadrant (LMQ) abdominal pain with radiation into his back. His past medical history is significant for hypertension, peripheral vascular disease, peptic ulcer disease, kidney stones, and gallstones. He smokes a pack of cigarettes and consumes a pint of vodka daily. His BP is 145/80 mm Hg, HR is 90 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. Abdominal examination is unremarkable. An ECG is read as sinus rhythm with an HR of 88 beats per minute. An abdominal radiograph reveals normal loops of bowel and curvilinear calcification of the aortic wall. Which of the following is the most likely diagnosis?
Biliary colic
Nephrolithiasis
Pancreatitis
Small bowel obstruction (SBO)
Abdominal aortic aneurysm
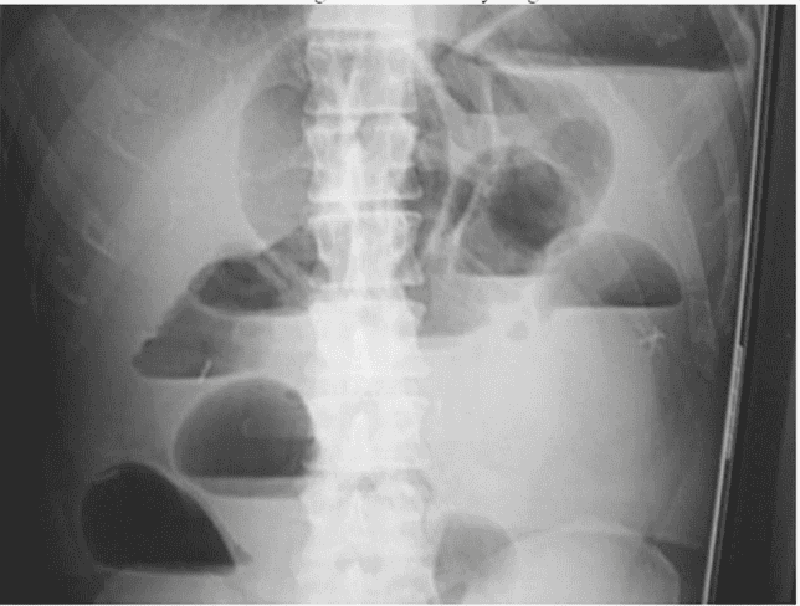
A 73-year-old man is seen in the ED for abdominal pain, nausea, and vomiting. His symptoms have progressively worsened over the past 2 to 3 days. The pain is diffuse and comes in waves. He denies fever or chills, but has a history of constipation. He reports no flatus for 24 hours. Physical examination is notable for diffuse tenderness and voluntary guarding. There is no rebound tenderness. An abdominal radiograph is seen below. Which of the following is the most likely diagnosis?
Constipation
SBO
Cholelithiasis
Large bowel obstruction
Inflammatory bowel disease
For which of the following patients is an abdominal CT scan contraindicated?
A 52-year-old man with abdominal pain after blunt trauma, negative focused assessment with sonography for trauma (FAST) examination, BP 125/78 mm Hg, and HR 109 beats per minute
A 22-year-old woman with RLQ pain, negative β-hCG, temperature 100.6°F
A 45-year-old man with abdominal pain, temperature 100.5°F, WBC 11,200/μL, BP 110/70 mm Hg, HR 110 beats per minute, and lipase 250 IU
A 70-year-old man with abdominal pain, an 11-cm pulsatile mass in the epigastrium, BP of 70/50 mm Hg, and HR of 110 beats per minute
A 65-year-old woman with right flank pain that radiates to her groin, microhematuria, BP 165/85 mm Hg, and HR 105 beats per minute
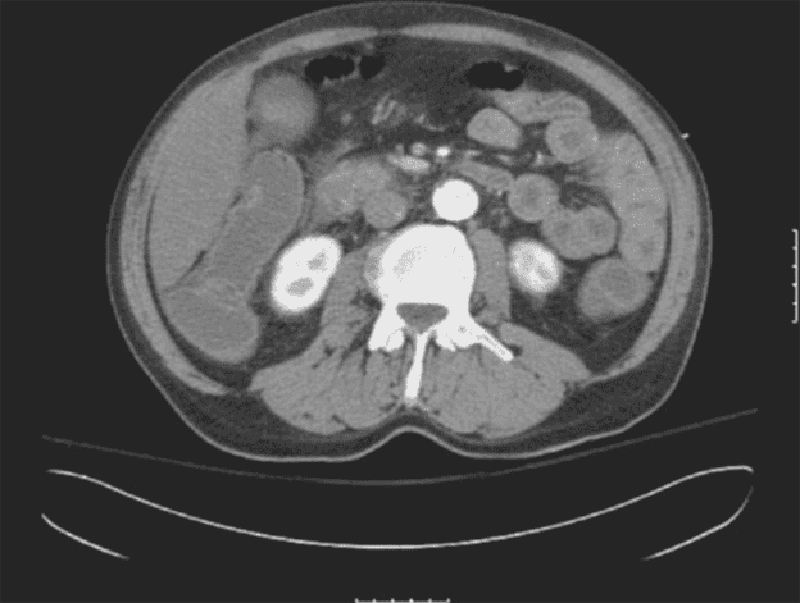
A 63-year-old man is brought to the ED by EMS complaining of severe abdominal pain that began suddenly 6 hours ago. His BP is 145/75 mm Hg and HR is 105 beats per minute and irregular. On examination, you note mild abdominal distention and diffuse abdominal tenderness without guarding. Stool is heme positive. Laboratory results reveal WBC 12,500/μL, haematocrit 48%, and lactate 4.2 U/L. ECG shows atrial fibrillation at a rate of 110. A CT scan is shown below. Which of the following is the most likely diagnosis?
Abdominal aortic aneurysm
Mesenteric ischemia
Diverticulitis
SBO
Crohn disease
A 21-year-old woman presents to the ED complaining of diarrhea, abdominal cramps, fever, anorexia, and weight loss for 3 days. Her BP is 127/75 mm Hg, HR is 91 beats per minute, and temperature is 100.8°F. Her abdomen is soft and nontender without rebound or guarding. WBC is 9200/μL, β-hCG is negative, urinalysis is unremarkable, and stool is guaiac positive. She tells you that she has had this similar presentation four times over the past 2 months. Which of the following extraintestinal manifestations is associated with Crohn disease but not ulcerative colitis?
Ankylosing spondylitis
Erythema nodosum
Nephrolithiasis
Thromboembolic disease
Uveitis
An 84-year-old woman with coronary artery disease, congestive heart failure, peripheral vascular disease, and atrial fibrillation presents to the emergency department with dizziness, weakness, and sudden-onset crampy periumbilical pain. The pain is associated with one episode of diarrhea and one episode of emesis. The patient notes she has been having similar pain after meals for “several months” but never this severe. Her temperature is 37.2°C (98.9°F), heart rate is 135/min, blood pressure is 96/60 mm Hg, and respiratory rate is 16/min. Physical examination is notable for a slightly distended abdomen that is extremely tender to palpation with diminished bowel sounds. There is no rigidity or rebound tenderness noted on the abdominal examination. In addition, the patient has heme positive stool. Her WBC count is 19,500/mm³, hemoglobin is 10.9 g/dL, and platelet count is 159,000/mm³. Liver function testing results are normal. After stabilizing the patient, what is the best next step in management?
Barium enema
Colonoscopy
Laparotomy
Obstruction series
Warfarin therapy
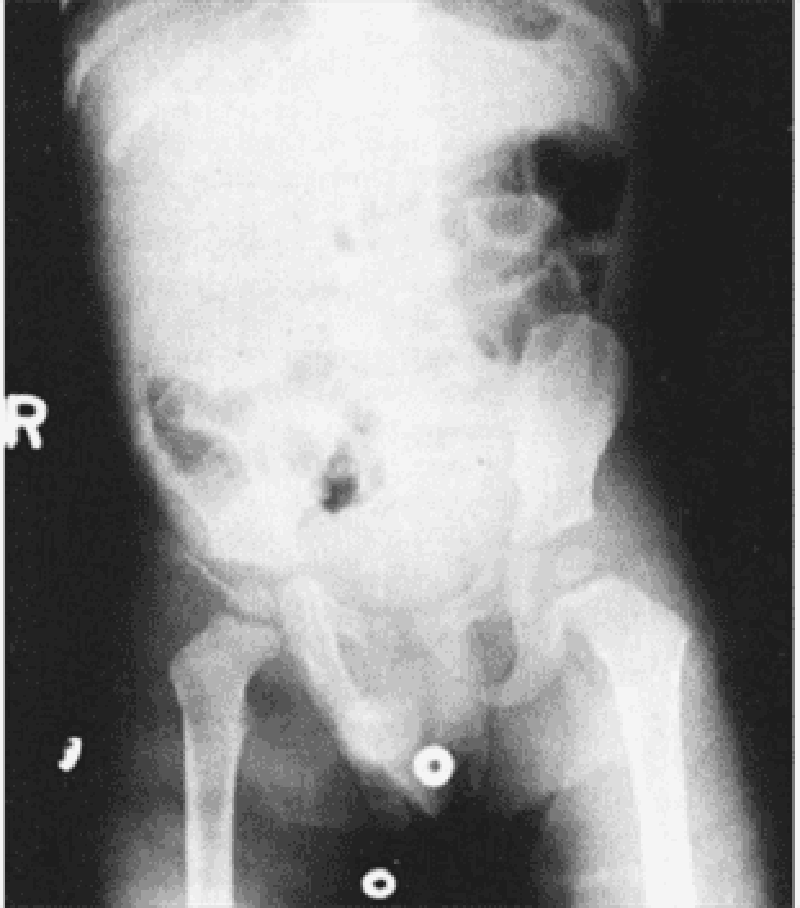
A 2-year-old boy is brought to the emergency department. His mother reports that the patient had been well until 3 days ago, when he developed a fever and nasal congestion. He was diagnosed with otitis media in his right ear, and was started on amoxicillin with clavulanic acid by his pediatrician. He appeared to be improving until this morning, when he began to complain of abdominal pain. The pain has been intermittent, with episodes occurring every 20 minutes for several minutes each time. However, the episodes appear to be worsening and lasting longer with increasing pain. Thirty minutes ago he had an episode of nonbloody, nonbilious emesis that was followed by passage of blood- and mucus-stained stools. He is currently in no acute distress, and his vital signs are normal. A firm sausage-shaped mass is palpable in the RUQ of his abdomen. A rectal examination yields bloody mucus. He does not have any skin lesions or rashes. X-ray of the abdomen is shown in the image. Which of the following is the most likely diagnosis?
Cystic fibrosis
Enterocolitis
Henoch-Schönlein purpura
Idiopathic intussusception
Meckel’s diverticulum
A 59-year-old man presents for his routine colonoscopy and during his visit he has numerous large adenomas removed from his colon. Which of the following is the most effective strategy for follow-up of this patient?
Elective colectomy
Repeat colonoscopy in 10 years
Repeat colonoscopy in 3 years
Sigmoidoscopy in 10 years
Urgent colectomy
A 67-year-old woman is currently postoperative day 8 after an emergent laparoscopic cholecystectomy for acute cholecystitis. On postoperative day 2 she spiked a temperature of 40°C (101.4°F) and began to complain of some shortness of breath. X-ray of the chest revealed right lower lobe pneumonia, and the patient was started on clindamycin. Today she is experiencing multiple episodes of foul-smelling, watery diarrhea that is green tinged but non-bloody. She also complains of lower abdominal cramping. Her temperature is 37.8°C (100°F), pulse is 90/min, respiratory rate is 15/min, and blood pressure is 110/70 mm Hg. Which of the following is the most likely explanation for these findings?
Ingestion of preformed enterotoxins, cytotoxins, and/or neurotoxins
Production of enterotoxins and cytotoxins within the gastrointestinal tract
Production of cytotoxins within the gastro- intestinal tract
Production of enterotoxins within the gastrointestinal tract
Viral invasion and damage of villous epithelial cells within the gastrointestinal tract
A male infant is delivered at 37 weeks’ gestation via cesarean section for breech presentation. The pregnancy was complicated by polyhydramnios. The 34-year-old mother is rubella immune and has blood type B. She is negative for Rh antibody, Group B streptococci, rapid plasma reagin, hepatitis B surface antigen, gonorrhea, and Chlamydia. At delivery there is no meconium. He has a birth weight of 2.7 kg (6 lb). The baby has a weak cry and is pale and frothing at the nose and mouth. He has nasal flaring and retractions, with a respiratory rate of 56/min. Heart rate is 140/min and he has a regular rhythm and a harsh 2/6 holosystolic murmur that is best heard at the left sternal border. On auscultation he has fine diffuse crackles in his lungs bilaterally. The infant is missing both thumbs and has fusion of the remaining digits of his upper extremities bilaterally. The pediatric resident is able to suction secretions from the patient’s nasopharynx and oropharynx; however, she is unable to pass a nasogastric or orogastric tube more than 10 cm down. X-ray of the chest is shown in the image. Which of the following is the most likely diagnosis?
Congenital diaphragmatic hernia
Pyloric stenosis
Respiratory distress syndrome
Tracheoesophageal fistula
Transient tachypnea of the new-born
A 51-year-old man is brought to the emergency department (ED) by emergency medical services (EMS) with a blood pressure (BP) of 90/60 mm Hg, heart rate (HR) of 110 beats per minute, respiratory rate (RR) of 18 breaths per minute, and oxygen saturation of 97% on room air. The patient tells you that he has a history of bleeding ulcers. On examination, his abdomen is tender in the epigastric area. He is guaiac positive, with black stool. He has a bout of hematemesis and you notice that his BP is now 80/50 mm Hg, HR is 114 beats per minute, as he is slowly starting to drift off. Which of the following is the most appropriate next step in therapy?
Assess airway, establish two large-bore intravenous (IV) lines, cross-match for two units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Assess airway, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor
Place two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy
Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor
A 19-year-old woman presents to the ED with 1 hour of acute-onset progressively worsening pain in her RLQ. She developed nausea shortly after the pain and vomited twice over the last hour. She had similar but less severe pain 2 weeks ago that resolved spontaneously. Her BP is 123/78 mm Hg, HR is 99 beats per minute, temperature is 99.1°F, and her RR is 16 breaths per minute. On physical examination, the patient appears uncomfortable, not moving on the gurney. Her abdomen is nondistended, diffusely tender, worst in the RLQ. Pelvic examination reveals a normal-sized uterus and moderate right-sided adnexal tenderness. Laboratory results reveal WBC 10,000/μL, hematocrit 38%, and a negative urinalysis and β-hCG. Pelvic ultrasound reveals an enlarged right ovary with decreased flow. Which of the following is the most appropriate management for this patient?
Admit to the gynecology service for observation
Administer IV antibiotics and operate once inflammation resolves
Attempt manual detorsion
Order an abdominal CT
Go for immediate laparoscopic surgery
A 23-year-old woman presents to the ED with RLQ pain for the last 1 to 2 days. The pain is associated with nausea, vomiting, diarrhea, anorexia, and a fever of 100.9°F. She also reports dysuria. The patient returned 1 month ago from a trip to Mexico. She is sexually active with one partner but does not use contraception. She denies vaginal bleeding or discharge. Her last menstrual period was approximately 1 month ago. She has a history of pyelonephritis. Based on the principles of emergency medicine, what are the three priority considerations in the diagnosis of this patient?
Perihepatitis, gastroenteritis, cystitis
Ectopic pregnancy, appendicitis, pyelonephritis
Pelvic inflammatory disease (PID), gastroenteritis, cystitis
Ectopic pregnancy, PID, menstrual cramps
Gastroenteritis, amebic dysentery, menstrual cramps
A 73-year-old woman presents to the emergency room with black tarry stools and symptoms of presyncope when standing up. Digital rectal examination confirms the presence of melena. She recently started using ibuprofen for hip discomfort. Upper endoscopy confirms the diagnosis of a gastric ulcer. Which of the following is the most likely explanation for the gastric ulcer?
Increasing acid production
Causing direct epithelial cell death
Promoting replication of Helicobacter pylori
An antiplatelet effect
Inhibiting mucosal repair
{"name":"GASTROINTESTINALE I", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"An 82-year-old woman presents 1-hour after the sudden onset of moderate-to-severe epigastric pain. The pain radiates to her back, both scapulae, and both arms. She has been nauseated and vomited three times in the past hour. Her past medical history is remarkable for peptic ulcer disease 10-years ago, cholelithiasis for the past 6-years, and stable angina pectoris for the past 3-years. She has had occasional episodes of biliary colic and two bouts of acute cholecystitis which were treated conservatively. Her temperature is 36.8C (98.2F), blood pressure is 120\/70 mm Hg, pulse is 90\/min, and respirations are 14\/min. The lungs are clear to auscultation. Abdominal examination shows a soft abdomen with mild tenderness to palpation in the epigastrium. Murphy's sign is negative. Which of the following studies should be done first?, A 43-year-old male (Patient A) is being evaluated for an esophageal disorder. Esophageal manometry tracings after a single swallow of 5 ml of water are shown on the slide below. Which of the following is the most likely diagnosis in this patient?, A 45-year-old nurse practitioner presents to the emergency department due to painful abdominal cramps and watery diarrhea. She has about 10 to 20 bowel movements a day. She also has nocturnal bowel movements. She has had multiple hospitalizations in the past for similar problems without a definite diagnosis. A lower GI endoscopy during a previous hospitalization showed dark brown discoloration of the colon with lymph follicles shining through as pale patches. Which of the following is the most likely diagnosis?","img":"https://cdn.poll-maker.com/15-640323/1.png?sz=1200"}
More Quizzes
DooSean
9420
COACH'S LEGAL RESPONSIBILITIES
10516
30150
Do you have any recommendations in new papers today?
100
Scissor Lift Safety: Challenge Your Safety Skills
201028325
Night by Elie Wiesel: Can You Ace Every Question?
201032988
CDL General Knowledge: What to Look for Ahead
201040665
Which Sword Suits You? Discover Your Best Type of Sword
201032564
Which Diet Suits You? Take the Ultimate Veg Test Now!
201030624
Free Practice: Positive Parenting Effects
201024153
Which Sailor Moon Character Are You? Take the Now!
201030989
Can You Ace the Fahrenheit 451 Salamander?
201067689