Surgery USMLE (927-1022)
Your hospital is conducting an ongoing research study involving the hormonal response to trauma. Blood is drawn regularly (with Institutional Review Board [IRB] approval) for various studies. Which of the following values are likely to be seen after a healthy 36-year-old man is hit by a bus and sustains a ruptured spleen and a lacerated small bowel?
Increased secretion of insulin
Increased secretion of thyroxine
Decreased secretion of vasopressin (antidiuretic hormone [ADH])
Decreased secretion of glucagon
Decreased secretion of aldosterone
A 29-year-old man sustained a gunshot wound to the right upper quadrant. He is taken to the operating room and, after management of a liver injury, is found to have a complete transection of the common bile duct with significant tissue loss. Which of the following is the optimal surgical management of this patient’s injury?
Choledochoduodenostomy
Loop choledochojejunostomy
Primary end-to-end anastomosis of the transected bile duct
Roux-en-Y choledochojejunostomy
Bridging of the injury with a T tube
You evaluate an 18-year-old man who sustained a right-sided cervical laceration during a gang fight. Your intern suggests nonoperative management and observation. Which of the following is a relative, rather than an absolute, indication for neck exploration?
Expanding hematoma
Dysphagia
Dysphonia
Pneumothorax
Hemoptysis
Following blunt abdominal trauma, a 12-year-old girl develops upper abdominal pain, nausea, and vomiting. An upper gastrointestinal series reveals a total obstruction of the duodenum with a coiled spring appearance in the second and third portions. In the absence of other suspected injuries, which of the following is the most appropriate management of this patient?
Gastrojejunostomy
Nasogastric suction and observation
Duodenal resection
TPN (total parental nutrition) to increase the size of the retroperitoneal fat pad
Duodenojejunostomy
A 45-year-old man presents after a high-speed motor vehicle collision. He has a seatbelt sign across his neck and chest with an ecchymosis over his left neck. He is hemodynamically stable and neurologically intact. A CT angiogram shows a left carotid dissection. In the absence of other significant injuries, what is the next step in his management?
Antiplatelet therapy
Systemic anticoagulation with heparin
Neck exploration and left carotid artery repair
Neck exploration and left intra-extracranial bypass
Angiography and left carotid artery stenting
An 18-year-old man was assaulted and sustained significant head and facial trauma. Which of the following is the most common initial manifestation of increased intracranial pressure?
Change in level of consciousness
Ipsilateral (side of hemorrhage) pupillary dilation
Contralateral pupillary dilation
Hemiparesis
Hypertension
A 28-year-old man is brought to the ER for a severe head injury after a fall. He was intubated in the field for his decreased level of consciousness. He is tachycardic and hypotensive. On examination, he is noted to have an obvious skull fracture and his right pupil is dilated. Which of the following is the most appropriate method for initially reducing his intracranial pressure?
Elevation of the head of the bed
Saline-furosemide (Lasix) infusion
Mannitol infusion
Intravenous dexamethasone (Decadron)
Hyperventilation
A 45-year-old man was an unhelmeted motorcyclist involved in a high-speed collision. He was ejected from the motorcycle and was noted to be apneic at the scene. After being intubated, he was brought to the ER, where he is noted to have a left dilated pupil that responds only sluggishly. What is the pathophysiology of his dilated pupil?
Infection within the cavernous sinus
Herniation of the uncal process of the temporal lobe
Laceration of the corpus callosum by the falx cerebri
Occult damage to the superior cervical ganglion
Cerebellar hypoxia
A 31-year-old man is brought to the ER following an automobile accident in which his chest struck the steering wheel. Examination reveals stable vital signs and no evidence of respiratory distress, but the patient exhibits multiple palpable rib fractures and paradoxical movement of the right side of the chest. Chest x-ray shows no evidence of pneumothorax or hemothorax. Which of the following is the most appropriate initial management of this patient?
Intubation, mechanical ventilation, and positive end-expiratory pressure
Stabilization of the chest wall with sandbags
Stabilization with towel clips
Immediate operative stabilization
Pain control, chest physiotherapy, and close observation
A 30-year-old man is stabbed in the arm. There is no evidence of vascular injury, but he cannot flex his three radial digits. Which of the following structures has he most likely injured?
Flexor pollicis longus and flexor digitus medius tendons
Radial nerve
Median nerve
Thenar and digital nerves at the wrist
Ulnar nerve
Following a 2-hour firefighting episode, a 36-year-old fireman begins complaining of a throbbing headache, nausea, dizziness, and visual disturbances. He is taken to the ER, where his carboxyhemoglobin (COHb) level is found to be 31%. Which of the following is the most appropriate next step in his treatment?
Begin an immediate exchange transfusion.
Transfer the patient to a hyperbaric oxygen chamber.
Begin bicarbonate infusion and give 250 mg acetazolamide (Diamox) intravenously
Administer 100% oxygen by mask
Perform flexible bronchoscopy with further therapy determined by findings
A 75-year-old man with a history of coronary artery disease, hypertension, and diabetes mellitus undergoes a right hemicolectomy for colon cancer. On the second postoperative day, he complains of shortness of breath and chest pain. He becomes hypotensive with depressed mental status and is immediately transferred to the intensive care unit. After intubation and placement on mechanical ventilation, an echocardiogram confirms cardiogenic shock. A central venous catheter is placed that demonstrates a central venous pressure of 18 mm Hg. Which of the following is the most appropriate initial management strategy?
Additional liter fluid bolus
Inotropic support
Mechanical circulatory support with intra-aortic balloon pump (IABP)
Cardiac catheterization
Heart transplant
An 18-year-old man climbs up a utility pole to retrieve his younger brother’s kite. An electrical spark jumps from the wire to his metal belt buckle and burns hisabdominal wall, knocking him to the ground. Which of the following should guide your treatment of this patient?
Injuries are generally more superficial than those from thermal burns.
Intravenous fluid replacement is based on the percentage of body surface area burned
Electric burns often result in a transient traumatic optic neuropathy.
Evaluation for fracture of the other extremities and visceral injury is indicated
Cardiac conduction abnormalities are unlikely
A 22-year-old man is examined following a motor vehicle accident. He has a right knee dislocation which is reduced in the emergency room. He has palpable pedal pulses and is neurologically intact. Which of the following is an appropriate next step in his workup and management?
Measurement of ankle-brachial indices
Angiography of the right lower extremity
Prophylactic below-knee 4-compartment fasciotomies
Surgical exploration of the right popliteal artery
Observation with serial pulse checks
A 23-year-old, previously healthy man presents to the ER after sustaining a single gunshot wound to the left chest. The entrance wound is 3 cm inferior to the nipple and the exit wound is just below the scapula. A chest tube is placed that drains 400 mL of blood and continues to drain 50 to 75 mL/h during the initial resuscitation. Initial blood pressure of 70/0 mm Hg has responded to 2L crystalloid and is now 100/70 mm Hg. Abdominal examination is unremarkable. Chest x-ray reveals a reexpanded lung and no free air under the diaphragm. Which of the following is the best next step in his management?
Admission and observation
Peritoneal lavage
Exploratory thoracotomy
Exploratory celiotomy
Local wound exploration
A patient is brought to the ER after a motor vehicle accident. He is unconscious and has a deep scalp laceration and one dilated pupil. His heart rate is 120 beats per minute, blood pressure is 80/40 mm Hg, and respiratory rate is 35 breaths per minute. Despite rapid administration of 2 L normal saline, the patient’s vital signs do not change significantly. Which of the following is the most appropriate next step in the workup of his hypotension?
Neurosurgical consultation for emergent ventriculostomy to manage his intracranial pressure
Neurosurgical consultation for emergent craniotomy for suspected subdural hematoma
Emergent burr hole drainage at the bedside for suspected epidural hematoma
Administration of mannitol and hyperventilation to treat his elevated intracranial pressure
Abdominal ultrasound (focused assessment with sonography in trauma [FAST])
A 25-year-old man is involved in a gang shoot-out and sustains an abdominal gunshot wound from a .22 pistol. At laparotomy, it is discovered that the left transverse colon has incurred a through-and-through injury with minimal fecal soilage of the peritoneum. Which of the following is the most appropriate management of this patient?
A colostomy should be performed regardless of the patient’s hemodynamic status to decrease the risk of an intraabdominal infection.
Primary repair should be performed, but only in the absence of hemodynamic instability
Primary repair should be performed with placement of an intra-abdominal drain next to the repair
Primary repair should be performed and intravenous antibiotics administered for 14 days
The patient should undergo a 2-stage procedure with resection of the injured portion and reanastomosis 48 hours later when clinically stabilized
A 1-year-old child has repeated episodes of vomiting and abdominal distention. An x-ray shows obstruction at the second portion of the duodenum. Laparotomy is performed and an annular pancreas is discovered. For a symptomatic partial duodenal obstruction secondary to an annular pancreas, which of the following is the operative treatment of choice?
A Whipple procedure
Gastrojejunostomy
Vagotomy and gastrojejunostomy
Partial resection of the annular pancreas
Duodenostomy
Approximately 2 weeks after a viral respiratory illness, an 18-month-old child complains of abdominal pain and passes some bloody mucus per rectum. A long, thin mass is palpable in the right upper quadrant of the abdomen. No peritoneal signs are present. Intussusception is suspected. Which of the following is the most appropriate next step?
Diagnostic air enema with subsequent observation and serial abdominal examinations
Hydrostatic reduction with air enema
Diagnostic laparoscopy with laparoscopic reduction
Exploratory laparotomy with bowel resection
Decompressive colonoscopy with placement of a rectal tube

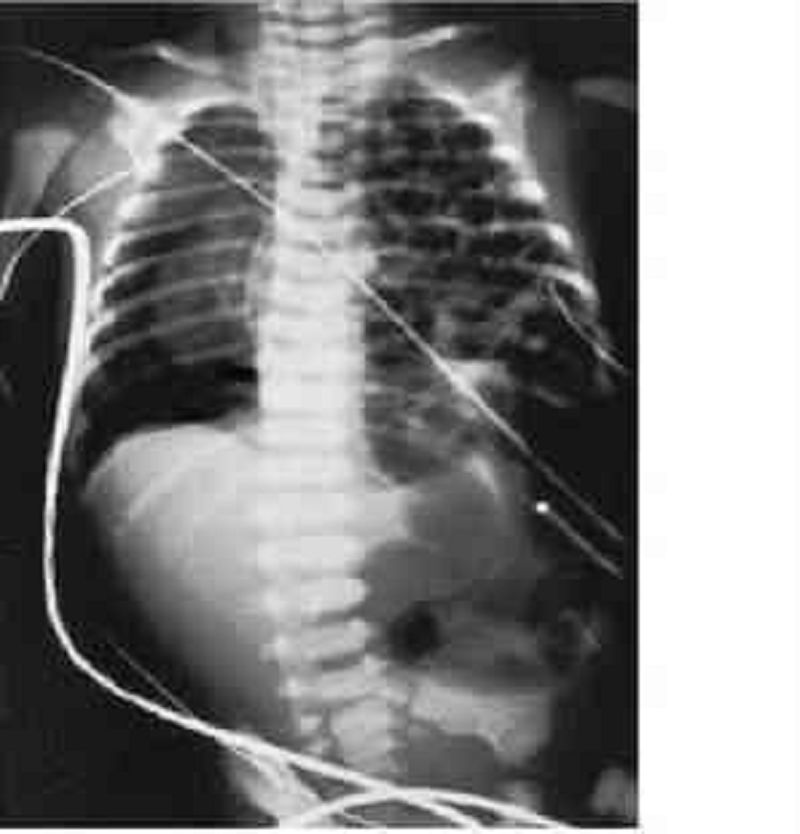
A 34-year-old prostitute with a history of long-term intravenous drug use is admitted with a 48-hour history of pain in her left arm. She is tachycardic to 130 and her systolic blood pressure is 80 mm Hg. Physical examination is remarkable for crepitus surrounding needle track marks in the antecubital space with a serous exudate. The plain x-ray of the arm is shown here. Which of the following is the most appropriate next step in her management?
Treatment with penicillin G and close observation
MRI of the arm
CT scan of the arm
Surgical exploration and debridement
Hyperbaric oxygen therapy
A 47-year-old man is extricated from an automobile after a motor vehicle accident. He is hypotensive with a systolic blood pressure of 80. The patient has a steering wheel bruise on the anterior chest. His electrocardiogram (ECG) shows some premature ventricular complexes, and his cardiac isoenzymes are elevated. Which of the following is the best next test for evaluation for a blunt cardiac injury?
Measurement of serial creatinine phosphokinase and creatinine kinase (including the myocardial band) levels
Thallium stress test
Echocardiography
Single photon emission computed tomography (SPECT)
Multiple acquisition scans (MUGA)
A 70-year-old man presents to the ER with several fractures and a ruptured spleen after falling 20 ft. Which of the following will occur in response to the injury?
Decreased liver gluconeogenesis
Inhibition of skeletal muscle breakdown by interleukin 1 and tumor necrosis factor (TNF, cachectin)
CT scan of the abdomen and pelvis
Angiography
Sigmoidoscopy in the ER
A 27-year-old man presents to the ER after a high-speed motor vehicle collision with chest pain and marked respiratory distress. On physical examination, he is hypotensive with distended neck veins and absence of breath sounds in the left chest. Which of the following is the proper initial treatment?
Intubation
Chest x-ray
Pericardiocentesis
Chest decompression with a needle
Emergent thoracotomy
A 48-year-old man sustains a gunshot wound to the right upper thigh just distal to the inguinal crease. He is immediately brought to the ER. Peripheral pulses are palpable in the foot, but the foot is pale, cool, and hypesthetic. The motor examination is normal. Which of the following statements is the most appropriate next step in the patient’s management?
The patient should be taken to the operating room immediately to evaluate for a significant arterial injury
A neurosurgical consult should be obtained and somatosensory evoked potential monitoring performed
A fasciotomy should be performed prophylactically in the emergency room
A duplex examination should be obtained to rule out a venous injury
The patient should be observed for at least 6 hours and then reexamined for changes in the physical examination
A 62-year-old woman is seen after a 3-day history of fever, abdominal pain, nausea, and anorexia. She has not urinated for 24 hours. She has a history of previous abdominal surgery for inflammatory bowel disease. Her blood pressure is 85/64 mm Hg, and her pulse is 136. Her response to this physiologic state includes which of the following?
Increase in sodium and water excretion
Increase in renal perfusion
Decrease in cortisol levels
Hyperkalemia
Hypoglycemia
A 46-year-old man is brought to the emergency department after being involved in a motor vehicle collision. He is unresponsive and his injuries include a basilar skull fracture, brain contusion, fractures of ribs 7-10, hemopneumothorax on the right, and a pelvic fracture. After placement of a chest tube and pelvis fixation, his condition stabilizes. On the fifth day of his hospital stay, he is still unresponsive with a Glasgow Coma Scale of 8 and spontaneous respirations. Examination shows an abnormal facial reaction with palpation of the right upper quadrant of the abdomen and diminished bowel sounds. Rectal examination shows no abnormalities. Nasogastric tube aspiration shows retention of gastric contents. An abdominal CT scan shows gaseous distention of the small and large bowels without air-fluid levels. The gall bladder is distended with pericholecystic fluid but no gallstones. Which of the following is the most likely diagnosis for this patient's abdominal findings?
Bowel obstruction
Cholecystitis
Pancreatitis
Mesenteric ischemia
Lung contusion
A 20-year-old man presents after being punched in the right eye and assaulted to the head. On a facial CT scan, he is noted to have a blowout fracture of the right orbital floor. Which of the following findings mandates immediate surgical intervention?
A fracture 25% of the orbital floor
1 mm of enophthalmos
Periorbital ecchymosis
Inability to move the right eye upward
Traumatic optic neuropathy
A 33-year-old woman is seen in the ER with severe rectal bleeding. She has a history of ulcerative colitis. Her blood pressure is 78/56 mm Hg, her pulse is 144, and she is pale and clammy. Which of the following responses is likely to occur after administration of Ringer lactate solution?
Increase in serum lactate concentration
Impairment of liver function
Improvement in hemodynamics by alleviating the deficit in the interstitial fluid compartment
Increase in metabolic acidosis
Increase in the need for blood transfusion
An 18-year-old high school football player is kicked in the left flank. Three hours later he develops hematuria. His vital signs are stable. A CT scan demonstrates a grade II renal injury based on the Urologic Injury Scale of the American Association for the Surgery of Trauma. Which of the following is the most appropriate treatment for this patient?
Resumption of normal daily activity excluding sports
Exploration and suture of the laceration
Exploration and wedge resection of the left kidney
Nephrostomy
Strict bed rest with serial hemoglobin levels
A 32-year-old man is in a high-speed motorcycle collision and presents with an obvious pelvic fracture. On examination, he has a scrotal hematoma and blood at his urethral meatus. Which of the following is the most appropriate next step in his management?
Placement of a Foley catheter
Cystoscopy
CT of the pelvis
Retrograde urethrogram
Nephrostomy tube placement
A 36-year-old man sustains a gunshot wound to the left buttock. He is hemodynamically stable. There is no exit wound, and an x-ray of the abdomen shows the bullet to be located in the right lower quadrant. Which of the following is most appropriate in the management of his suspected rectal injury?
Barium studies of the colon and rectum
Barium studies of the bullet track
CT scan of the abdomen and pelvis
Angiography
Sigmoidoscopy in the ER
A 17-year-old adolescent boy sustains a small-caliber gunshot wound to the mid- epigastrium with no obvious exit wound. His abdomen is very tender; he is taken to the operating room and the bullet appears to have tracked through the stomach, distal pancreas, and spleen. The duct appears to have been injured. Which of the following is the best strategy for the management of this patient’s pancreatic injury?
Drainage alone
Roux-en-Y pancreaticojejunostomy
Pancreaticoduodenectomy
Frey procedure
Distal pancreatectomy
A 22-year-old woman who is 4 months pregnant presents after a motor vehicle collision complaining of abdominal pain and right leg pain. She has an obvious deformity of her right femur. She is hemodynamically stable. Which of the following is the best next step in her management?
Observation with serial abdominal exams
Diagnostic peritoneal lavage
Plain film of the abdomen with a lead apron as a shield
Focused assessment with sonography for trauma (FAST) examination of the abdomen
MRI of the abdomen

An 18-year-old woman presents with abdominal pain, fever, and leukocytosis. With the presumptive diagnosis of appendicitis, a right lower quadrant (McBurney) incision is made and a lesion 60 cm proximal to the ileocecal valve is identified (see photo). Which of the following is the most likely diagnosis?
Intestinal duplication
Mesenteric cyst
Meckel diverticulum
Ileoileal intussusception
�Christmas tree” type of ileal atresia
A newborn infant born from a mother with polyhydramnios presents with excessive salivation along with coughing and choking with the first oral feeding. An xray of the abdomen shows gas in stomach and a nasogastric tube coiled in the esophagus. Which of the following is the most likely diagnosis?
Esophageal atresia
Tracheoesophageal fistula
Esophageal atresia and tracheoesophageal fistula (TEF)
Omphalocele
Gastroschisis
An infant is born with a defect in the anterior abdominal cavity. Upon examination there are abdominal contents (small bowel and liver) protruding directly through the umbilical ring. Which of the following should be considered in the management of this condition?
No further workup is indicated prior to closure of the abdominal wall defect.
A Silastic silo should be placed with immediate reduction of the viscera into the abdominal cavity.
Broad-spectrum intravenous antibiotics should be administered prophylactically
Topical antimicrobial solutions should be administered prophylactically.
Enteral feeds for nutritional support should be initiated early prior to operative management.
A 2-week-old infant presents with sudden onset of bilious emesis. Plain films of the abdomen show evidence of an intestinal obstruction. An upper gastrointestinal (UGI) contrast series reveals a midgut volvulus with the site of obstruction at the third portion of the duodenum. Which of the following is the most likely diagnosis?
Necrotizing enterocolitis (NEC)
Intussusception
Hirschsprung disease
Anomalies of intestinal rotation and fixation
Hypertrophic pyloric stenosis
A 29-week-old previously healthy male infant presents with fevers, abdominal distention, feeding intolerance, and bloody stools at 3 weeks of age. The patient undergoes x-ray and ultrasound examination for possible necrotizing enterocolitis. Which of the following findings on imaging is an indication for surgical management?
Pneumoperitoneum
Ascites
Portal venous gas
Ileus
Pneumatosis intestinalis
A newborn presents with signs and symptoms of distal intestinal obstruction. Abdominal x-rays reveal dilated loops of small bowel, absence of air-fluid levels, and a mass of meconium within the right side of the abdomen mixed with gas to give a ground-glass appearance. Which of the following should be performed as the initial management of the patient?
Administration of oral polyethylene glycol
Bowel rest with nasogastric tube decompression and broad-spectrum intravenous antibiotics
Contrast enema
Surgical evacuation of the luminal meconium
Resection of the dilated terminal ileum
A 4-week-old male infant presents with projectile, nonbilious emesis. Ultrasound of the abdomen reveals a pyloric muscle thickness of 8 mm (normal 3-4 mm). Which of the following is the best initial management of this patient?
Urgent pyloromyotomy
Urgent pyloroplasty
Urgent gastroduodenostomy
Fluid hydration and correction of electrolyte abnormalities prior to operative management
Administration of sodium bicarbonate to correct aciduria prior to operative management
A 1-month-old female infant presents with persistent jaundice. A serum direct bilirubin is 4.0 mg/dL and an ultrasound of the abdomen shows a shrunken gallbladder and inability to visualize the extrahepatic bile ducts. Which of the following is the most appropriate initial management of this patient?
NPO and total parenteral nutrition
Oral choleretic bile salts
Methylprednisolone
IV antibiotics
Exploratory laparotomy
A full-term male newborn experiences respiratory distress immediately after birth. A prenatal sonogram was read as normal. An emergency radiograph is shown here. The patient is intubated and placed on 100% O2. Arterial blood gases reveal pH 7.24, PO 2 60 kPa, and PCO2 52 kPa. The baby has sternal retractions and a scaphoid abdomen. Which of the following should be performed in the management of this patient?
Administration of intravenous steroids
Placement of bilateral tube thoracostomies
Immediate thoracotomy with lung resection
Immediate laparotomy with repair of the diaphragm
Mechanical ventilation with low tidal volumes
A 22-year-old man undergoes an exploratory laparotomy after a gunshot wound to the abdomen. The patient has multiple injuries, including a significant liver laceration, multiple small-bowel and colon injuries, and an injury to the infrahepatic vena cava. The patient receives 35 units of packed RBCs, 15 L of crystalloid, 12 units of fresh-frozen plasma (FFP), and a 12 packs of platelets. The patient’s abdomen is packed closed and he is taken to the intensive care unit for further resuscitation. Which of the following warrants a decompressive laparotomy?
Increased peak airway pressure
Increased cardiac output
Decreased systemic vascular resistance
Decreased plasma renin and aldosterone
Increased cerebral perfusion pressure
A 10-year-old girl is the unrestrained backseat passenger in a high-speed motor vehicle collision. She is intubated in the field for unresponsiveness and on presentation to the ER, her heart rate is 160 beats per minute, and her blood pressure is 60/35 mm Hg. She weighs 30 kg. Which of the following is the most appropriate recommendation for her fluid resuscitation?
Bolus 1 L of normal saline initially.
Bolus 1 L of 5% albumin initially.
Transfuse 300 cc of packed RBCs initially.
Bolus 600 cc of normal saline initially. Transfuse if no response.
Bolus 600 cc of normal saline initially followed by a repeat bolus. Transfuse if no response
A 21-year-old woman sustains a stab wound to the middle of the chest. Upon arrival to the ER she has equal breath sounds, blood pressure of 85/46 mm Hg, distended neck veins, and pulsus paradoxus. Which of the following is the most appropriate management of this patient?
Emergent intubation and mechanical ventilation in the ER
Emergent pericardiocentesis in the ER
Emergent thoracotomy in the ER
Emergent pericardiocentesis or subxiphoid pericardial drainage after anesthetic induction in the operating room
Emergent pericardiocentesis or subxiphoid pericardial drainage under local anesthesia in the operating room
A 58-year-old man presents to the ER after falling 10 ft from a ladder. Examination reveals stable vital signs, no evidence of respiratory distress, and multiple right-sided rib fractures. Chest x-ray shows a hemothorax on the right side and a right tube thoracostomy is performed in the ER. Approximately 700 mL of blood is immediately drained with placement of the thoracostomy tube. Over the next 4 hours he continues to drain 300 mL/h after the original evacuation. Which of the following is the definitive treatment for this patient?
Platelets
Fresh-frozen plasma
Second tube thoracostomy
Thoracotomy in the operating room
Thoracotomy in the ER
A 65-year-old woman is involved in a motor vehicle collision and sustains multiple left- sided rib fractures. Upon presentation to the ER her vital signs are stable and she is in no respiratory distress. Chest x-ray reveals fractures of ribs 4 to 7 on the left side without evidence of hemothorax or pneumothorax. She is admitted for observation and a few hours later she develops shortness of breath. A repeat chest x-ray demonstrates a well-defined infiltrate in her left lung. What is the most likely diagnosis?
Pulmonary contusion
Pulmonary embolus
Pneumonia
Myocardial infarction
Cardiac tamponade
Following a head-on motor vehicle collision, a 21-year-old unrestrained passenger presents to the ER with dyspnea and respiratory distress. She is intubated and physical examination reveals subcutaneous emphysema and decreased breath sounds. Chest x-ray reveals cervical emphysema, pneumomediastinum, and a right-sided pneumothorax. What is the most likely diagnosis?
Tension pneumothorax
Open pneumothorax
Tracheobronchial injury
Esophageal injury
Pulmonary contusion
An intoxicated 22-year-old man is a restrained driver in a high-speed motor vehicle collision. Examination reveals normal vital signs, but the rest of the examination is unreliable secondary to the patient’s intoxicated state from alcohol. Which of the following sole findings on a CT scan of the abdomen and pelvis mandates an exploratory laparotomy?
Free fluid in the pelvis
Pelvic fracture
Liver hematoma
Splenic hematoma
Renal hematoma
A 23-year-old man arrives in the ER after a motor vehicle collision. Examination reveals an unstable pelvis and blood at the urethral meatus. Which of the following studies would most accurately identify a urethral injury?
CT scan of the pelvis
Intravenous pyelogram
Stress cystogram
Antegrade urethrogram
Retrograde urethrogram
A 2-year-old asymptomatic child is noted to have a systolic murmur, hypertension, and diminished femoral pulses. Which of the following should be performed as part of the preoperative workup and management of this child’s disorder?
Administration of indomethacin if there is a patent ductus arteriosus
Ligation of a patent ductus arteriosus
Echocardiography
Aortogram with bilateral lower extremity runoffs
Cardiac catheterization
A 35-week-term infant presents with cyanosis shortly after birth. His arterial oxygen saturation is only 30%. Which of the following is the most likely diagnosis?
Patent ductus arteriosus
Coarctation of the aorta
Atrial septal defect
Ventricular septal defect
Transposition of the great vessels
A 42-year-old moderately obese female complains of abdominal discomfort two days after undergoing an elective cholecystectomy. Her past medical history is significant for hypertension, diabetes mellitus and hyperlipidemia. Her blood pressure is 132/90 mmHg and her heart rate is 76/min. Physical examination reveals a distended abdomen with decreased bowel sounds. Which of the following is most likely contributing to her current condition?
Insulin for glucose control
Morphine for pain relief
Perioperative antibiotics
Metoclopramide for nausea
Absence of bile storage reservoir
A 35-year-old woman is brought to the emergency department after being rescued from a burning building by firefighters. She had a brief tonic-clonic seizure en route to the hospital. Her past medical history is unknown. She is confused and mildly agitated. Her temperature is 37° C (98.6° F), blood pressure is 100/60 mm Hg, pulse is 115/min, and respirations are 24/min. Her oxygen saturation is 96% on room air. Physical examination shows no burns and her skin color is normal. There are symmetric breath sounds bilaterally with scattered end-expiratory wheezes. Neurological examination shows no abnormalities except some confusion. The abdomen is soft and non-tender. Which of the following is the best initial treatment for the patient?
Intravenous lorazepam
Intravenous naloxone
Intravenous phenytoin
50% dextrose with thiamine
100% oxygen with facemask
A 24-year-old woman comes to the physician's office because of breast pain. She has a 2- month-old baby who she breastfeeds. Her temperature is 38.8° C (101.9° F). Examination shows a hard, red, tender and swollen area on her right breast. There is no fluctuance noted. Which of the following is the most appropriate next step in management?
Incision and drainage
Recommend mammogram
Antibiotics and lactation suppression with bromocriptine
Antibiotics, analgesics and continue breast feeding
Antibiotics, analgesics and nursing only from unaffected breast
A 22-year-old primi-gravida woman is brought to the emergency department during the 33rd week of pregnancy after a tonic-clonic seizure. She has no history of seizure disorder and has not had any complications during her pregnancy. She is given magnesium sulfate and hydralazine. One hour later, she is lethargic and complains of persistent blurry vision and headache. She also complains of muscle pain, sore joints, and inability to move her right arm. Her temperature is 37.2° C (99° F), blood pressure is 182/111 mm Hg, pulse is 112/min, and respirations are 16/min. She holds her right arm adducted and internally rotated. Examination shows no sensory loss but an inability to externally rotate the right arm. Deep tendon reflexes (DTRs) are intact bilaterally, and handgrip is preserved on both sides. Which of the following is the most likely cause of her arm weakness?
Anterior shoulder dislocation
Magnesium toxicity
Postictal (Todd) paralysis
Posterior shoulder dislocation
Radial nerve compression
A 16-year-old boy was brought to the emergency department because of left shoulder and left hand pain after falling on his outstretched hand while playing soccer. He heard a crunching sound and had intense pain in his left shoulder area following the injury. Examination shows bruising around the clavicle area. He is holding his left arm with his right hand. There is a palpable gap in the middle of the clavicle. Auscultation shows a loud bruit just beneath the clavicle. An x-ray film of the left shoulder and chest shows the middle of the clavicle is fractured and displaced. Which of the following is the most appropriate next step in management?
CT chest for pneumothorax
Nerve conduction studies
Angiogram
Open reduction of the clavicle
Closed reduction with figure of eight brace
A 60-year-old man comes to the clinic because of right calf pain. He has a history of chronic diverticular disease and has had multiple attacks of diverticulitis in the past. His most recent attack occurred 3 weeks ago, and he was treated with antibiotics and underwent left hemicolectomy. He had a stable postoperative course and was discharged from the hospital 1 week ago. He developed right calf pain 3 days ago, with swelling and difficulty bearing weight on his right leg. He currently takes no medication. He does not use tobacco, alcohol, or illicit drugs. His temperature is 36.8° C (98.2° F), blood pressure is 120/70 mm Hg, pulse is 92/min, and respirations are 14/min. Physical examination reveals the right calf slightly larger than the left calf, moderate right ankle edema, and right calf pain with dorsiflexion of the right foot. Duplex ultrasonography shows a clot in the right distal portion of the femoral vein. Which of the following is the most appropriate initial treatment?
Aspirine
Heparin
Streptokinase
Wafarin
Tissue plasminogen activator
A 78-year-old diabetic man has undergone surgical repair of a large abdominal aortic aneurysm. Postoperatively, he develops left lower quadrant abdominal pain followed by bloody diarrhea. He has a history of prostate cancer and received radiation therapy several years ago. He eats a low fiber diet. He quit smoking recently. Vital signs show a low grade fever. Examination shows tenderness in the left lower quadrant and rectal examination reveals blood in the stool. CT scan of the abdomen demonstrates thickening of the colon at the recto-sigmoid junction. On colonoscopy, ulcerations are seen in the same area while the colon above and below the lesions is completely normal. Which of the following is the most likely cause of his symptoms?
Acute diverticulitis
Radiation proctitis
Clostridium difficile colitis
lschemic colitis
Inflammatory bowel disease
A 23-year-old man is brought to the emergency department in an obtunded state following a gun-shot wound to the right upper quadrant of the abdomen. His systolic blood pressure is 60 mm Hg and unable to obtain diastolic blood pressure. His pulse is 136/min. Chest auscultation shows clear heart and breath sounds. The abdomen appears distended, and there is an obvious gun-shot wound on the right upper quadrant. The bowel sounds are decreased. Which of the following is the most appropriate next step in management?
Angiography
Diagnostic peritoneal lavage
Focused ultrasonography
Laparoscopy
Laparotomy
A 36-year-old woman presents to the physician's office after she palpated a lump in her right breast. She has no other complaints. She has not seen a doctor for 10years. She regularly performs breast self-exams after menses. She has no significant past medical history. Her mother died of breast cancer at the age of 40. Breast examination shows a 1 x 1 cm rubbery, firm, freely mobile, round mass in the upper, outer quadrant of the right breast. No axillary lymph nodes are palpable. Which of the following is the most appropriate next step in management?
Reassurance
Repeat physical exam in 6 months
Excisional biopsy
Core needle biopsy
Mammography and ultrasound
A 35-year-old woman is being evaluated for a breast mass. She had a bilateral reduction mammoplasty for mammary hyperplasia 12 years ago. She has no family history of cancer. Breast examination shows a slightly retracted right nipple. A fixed mass is palpated in the upper outer quadrant of the right breast. Mammogram shows a 3 x 3-cm spiculated mass with coarse calcifications in the upper outer quadrant of the right breast. Ultrasonogram of the breast shows a hypoechoic mass. Multiple core biopsy samples show foamy macrophages and fat globules. Which of the following is the most appropriate course of action?
Lumpectomy and axillary node dissection followed by radiation therapy
MRI of the breast
Radiation therapy of the right breast
Routine follow-up and no intervention
Simple mastectomy
A 67-year-old male comes to the clinic for medical clearance prior to an elective abdominal aortic aneurysm repair. He denies any cough, shortness of breath or chest pain. He has coronary artery disease, diabetes and hypertension. He does not use tobacco, alcohol or drugs. His blood pressure is 120/76 mm Hg, pulse is 60/min, and respirations are 14/min. Examination shows no abnormalities, except prominent epigastric pulsations. Which of the following interventions would be most helpful in preventing postoperative pneumonia in this patient?
Albuterol inhalers
Prophylactic antibiotics
Incentive spirometry
Continuous positive airway pressure
Lntercostal nerve blocks for pain control
A 33-year-old male falls while riding his bicycle in the park, and presents to the emergency department. Physical examination reveals upper abdominal bruises. His abdomen is non-distended, soft, and mildly tender in the epigastrium. Abdominal CT scan does not reveal any abnormalities. The patient is sent home with analgesic medications. He returns one week later with fever, shaking chills, poor appetite and deep abdominal pain. Which of the following is most likely related to this patient's symptoms?
Spleen rupture
Stomach perforation
Pancreatic laceration
Small bowel necrosis
Meckel diverticulitis
A 24-year-old man is brought to the emergency department after being involved in a motor vehicle collision. He complains of severe back pain and abdominal discomfort. He was placed on a board in the field for spinal immobilization. His blood pressure is 111/78 mm Hg, pulse is 55/min and regular, and respirations are 16/min. Pulse oximetry shows 96% on room air. He is alert and fully oriented. There are several lacerations on the face and anterior chest. Air entry is bilaterally symmetric. There is weakness and decreased pain sensation in both legs. Proprioceptive sensation is preserved. Chest x-ray and CT scans of the abdomen and spine are performed. Which of the following is the most appropriate next step in managing this patient?
Bladder catheterization
Femoral line placement
Intravenous atropine
Intravenous lorazepam
Nasogastric tube placement
A 25-year-old man is brought to the emergency department by ambulance after falling from a ladder for 12 m (40 ft). He was placed on a backboard for spinal stabilization. Intravenous access was obtained en route, and infusion of crystalloids was initiated. The patient is comatose on arrival to the emergency department. Examination shows facial lacerations, a depressed skull fracture, and a forearm fracture. In the emergency department, his blood pressure is 92/45 mm Hg, pulse is 127/min, and respirations are 6/min. His pulse oximetry shows 86% on 40% facemask oxygen. Which of the following is the most appropriate next step in management?
Laryngeal mask placement and manual bagging
Nasotracheal intubation
Needle cricothyroidotomy
Orotracheal intubation
Surgical tracheostomy
A 78-year-old man with Alzheimer's disease was brought to the ER because of bright red bleeding per rectum. He has chronic constipation and is being treated with bisacodyl. On admission, his temperature was 36.6° C (97.9° F), blood pressure was 130/80 mm Hg with no orthostatic change, pulse was 90/min, and respirations were 14/min. Nasogastric tube drainage showed normal stomach contents and bile but no blood. His bleeding stopped a few hours after admission, and he remained hemodynamically stable during that time. Colonoscopy showed extensive diverticulosis but no active bleeding source. Later that night he started bleeding again from the rectum. Packed red cells and intravenous fluid are started. Which of the following is the most appropriate next step in management?
Upper gastrointestinal endoscopy
Capsule endoscopy
Barium enema
Labeled erythrocyte scintigraphy
Laparotomy
A 55-year-old man comes to the physician because of a 4-month history of an ulcer on the sole of his right foot. He has had no trauma and does not remember how he got the ulcer. He states the ulcer has been difficult to heal and readily gets infected. He has multiple medical problems. He does not use tobacco, alcohol or drugs. Examination shows the ulcer is located on the sole of his foot just below the head of the first metatarsal bone. His foot is warm and dry and appears slightly deformed. Dorsalis pedis pulses are present. Which of the following is the most likely cause of his condition?
Venous hypertension
Arterial spasm
Peripheral neuropathy
Central spinal cord lesion
Posterior spinal cord lesion
A 72-year-old man undergoes coronary artery bypass graft (CABG) for severe coronary artery disease. He is extubated on the second postoperative day. His temperature is 36.6° C (97.9° F), blood pressure is 120/70 mm Hg, pulse is 80/min, and respirations are 12/min. On the third postoperative day, he complains of dyspnea and worsening retrosternal pain despite continuous analgesia with morphine. His temperature is 38.6° C (101.5° F), blood pressure is 112/52 mm Hg, pulse is 125/min and irregularly irregular, and respirations are 28/min. Examination shows normal heart sounds. A small amount of cloudy fluid is present in the sternal wound drain. His ECG shows atrial fibrillation with rapid ventricular response. An x-ray film of the chest shows widening of the mediastinum. Echocardiography reveals a small amount of pericardial fluid. Laboratory studies show : Hemoglobin WBC count Platelet count Creatinine CPK Which of the following will this 8.9 mg/dl 16,300/mm' 512,000/mm 1.7 mg/dl 430 U/L patient most likely require?
Anticoagulation and electrical cardioversion
Broad-spectrum antibiotics alone
Nonsteroidal anti-inflammatory agents alone
Pericardial puncture and nonsteroidal anti-inflammatory agents
Surgical debridement and antibiotic therapy
A 25-year-old man comes to the physician because of a mass in his mouth. He has had the lump for many years. He denies weight loss. He was in a motor vehicle accident several years ago and sustained a concussion of the brain. He does not use tobacco, alcohol, or illicit drugs. Physical examination shows a nontender 2 x 2-cm mass located on the hard palate of the mouth that is immobile and has a bony hard consistency. Which of the following is the most likely cause of this patient's oral finding?
Congenital
Infectious
Neoplastic
Traumatic
Vascular
A 43-year-old male complains of right shoulder pain and weakness after falling on his outstretched hands two days ago. He denies shoulder deformity. The physician passively abducts both his arms above his head and then asks him to bring his arms down slowly in an adducting motion. The right arm drops rapidly at the midpoint of its descent. What is the most likely diagnosis?
Biceps tendon tear
Long thoracic nerve injury
Lower brachial trunk injury
Rotator cuff tear
Humeral neck fracture
A 12-year-old boy is brought to the emergency department after falling from a tree. Examination shows tenderness and swelling over the left lower arm. An x-ray film of the arm shows a fracture of the distal end of the humerus with proximal and posterior displacement of the distal fracture segment. Closed reduction of the fracture is performed. However, postoperatively the patient complains of increasing pain in the left arm and forearm. Twelve hours post- operatively his forearm is pale and cold. There is marked pain on passive extension of the fingers. Which of the following is the potential dreaded complication of this condition?
Malunion with alteration of carrying angle
Non-union
Reflex sympathetic dystrophy
Sudeck's atrophy
Volkmann ischemic contracture
A 16-year-old boy is brought to the emergency department after falling off a bicycle and hitting his head on the ground. He briefly lost consciousness but had no seizures. He had two episodes of vomiting and complains of mild headache. His mother accompanies him and demands immediate evaluation. He has no other medical problems. His blood pressure is 121/67 mm Hg and pulse is 78/min. Examination shows a small bruise on his forehead but no bony abnormalities. The rest of the physical examination, including neurologic examination, shows no other abnormalities. Which of the following is the most appropriate next step in management?
Admit the patient and observe for neurologic signs every 2 hours for a total of 6-8 hours
Admit the patient, order a CT scan of the head, and observe for neurologic signs every 2 hours
Discharge the patient home and ask him to return if he develops any new symptoms
Discharge the patient home if a skull radiograph is normal and ask him to return if he develops any new symptoms
Discharge the patient home if a CT scan of the head is norn1al and ask him to return if he develops any new symptom
A 45-year-old policeman presents to your office complaining of tiredness and sleepiness. He says that his job seems tiring to him recently. It is difficult for him to get up in the morning and go to work. He goes to bed early because he feels tired and sleepy. Two months ago, he was investigating a case of mass murder. He slipped on the blood on the floor, fell and hit his head. He also describes recent abdominal pain that is constant and gnawing, interfering with his sleep. His appetite is poor, and he lost 15 pounds over the last month. Physical examination is significant only for tenderness and fullness in the epigastrium. Which of the following is the most likely diagnosis?
Duodenal ulcer
Major depressive episode
Pancreatic cancer
Post-traumatic stress disorder
Chronic subdural hematoma
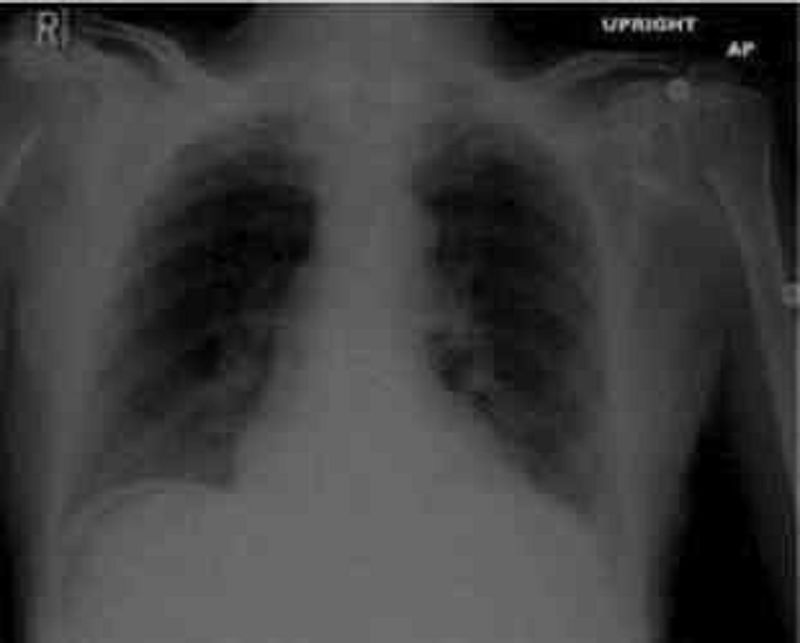
A 62-year-old man presents to the emergency department (ED} with one hour of severe epigastric pain. He has been having some epigastric pain exacerbated by eating for the last several days. He feels nauseated, and has vomited once since the pain began. His past medical history is significant for hypertension, diabetes, hyperlipidemia, and coronary artery disease. He underwent coronary bypass surgery one year back. His current medications are simvastatin, aspirin, clopidogrel, metoprolol, enalapril and metformin. His blood pressure is 140/100 mmHg, and heart rate is 65/min. His ECG is normal. Chest x-ray findings are shown on the slide below: Which of the following is the best step in the management of this patient?
Transthoracic echocardiography
Nothing by mouth (NPO) and gastric suction
Mesenteric angiography
Abdominal CT scan
Immediate surgical evaluation
A 12-year-old boy is brought to the physician because of right groin pain, knee pain, and limping. He has had these symptoms for the past 2 weeks. He is at the 90th percentile for weight and 60th percentile for height. He is afebrile, and his other vital signs are within normal limits. Examination shows that the range of motion of the right knee joint is within normal limits but hip movements are restricted and the right foot points outward. There is external rotation of the right thigh on flexion of the hip. After confirming the diagnosis, which of the following is the most appropriate management?
Aspiration and microscopic examination of the hip joint synovial fluid
Closed reduction of the hip joint
Conservative management with rest and analgesics
Immediate osteotomy of the femoral neck
Surgical pinning of the fen1oral head
A 42-year-old man is found unconscious at the scene of a motor vehicle collision. He is rushed to the emergency department, where his blood pressure is found to be 70/40 mm Hg and his respirations are 32/min. On physical examination, his trachea is deviated to the left and his breath sounds are decreased on the right side. His neck veins are distended bilaterally. The abdomen is soft and non-distended. There is significant swelling of the right thigh. Which of the following is the most appropriate next step in the management of this patient?
Bedside echocardiography
CT scan of the chest with contrast
Intubation and mechanical ventilation
Needle thoracostomy
Two large bore IV lines and fluid resuscitation
A 32-year-old man comes to the emergency room (ER) because of acute onset left flank pain, hematuria and vomiting. His pain is relieved with analgesics in the ER. He has a history of abdominal pain due to Crohn disease, but that pain was always in the right lower quadrant and was never this severe. His temperature is 36.8°C (98.2°F), blood pressure is 120/65 mm Hg, pulse is 11 O/min and respirations are 16/min. Chest auscultation is clear. Abdomen is soft and mildly tender over the left flank. He has no rebound or rigidity. Bowel sounds are decreased. A laparotomy scar is present in right lower quadrant. Which of the following is the most likely cause of his symptoms?
Increased recycling of bile salts and fatty acids
Increased absorption of oxalate
Increased absorption of calcium
Increased parathyroid hormone activity
Recurrent bacterial infection in the kidney
While working on-site at a factory doing physical examinations for workers, a physician is suddenly called to help a worker who amputated his finger. Which of the following is the most appropriate next step in management in this situation?
Place the amputated finger in a plastic bag with water and bring it along with the patient to the emergency department
Place the amputated finger in a plastic bag with alcohol; place the bag on a bed of ice and bring it along with the patient to the emergency department
Place the amputated finger in saline moistened gauze in a plastic bag; place the bag on a bed of ice and bring it along with the patient to the emergency department
Place the amputated finger in antiseptic solution and bring it along with the patient to the emergency department
Place the amputated finger on a bed of ice and bring it along with the patient to the emergency department
A 36-year-old male presents with firm, non-tender swelling of his right cheek. He tells you that he had similar swelling at that site two years ago and was diagnosed with a tumor, which was subsequently removed without complication. Examination reveals fullness of the pre- auricular space on the right side. Repeat surgery in this patient is most likely to result in which of the following complications?
Hoarseness
Tic douloureux
Facial droop
Tongue palsy
Jaw asymmetry
A 39-year-old paleontologist complains of right-sided hip pain that makes it very difficult for him to lie on his right side while sleeping. He localizes the pain to the outer surface of his thigh. He was recently diagnosed with hypertension and hyperlipidemia. He takes hydrochlorothiazide and atorvastatin. He has smoked one pack of cigarettes daily for 15 years. He does not use alcohol or illicit drugs. Which of the following is the most likely cause of his pain?
Slipped femoral epiphysis
Paget's disease
Peripheral vascular disease
Trochanteric bursitis
Hip osteoarthritis
An 88-year-old male complains of severe right calf pain several hours after undergoing a right femoral artery embolectomy. He also complains of a burning sensation in his posterior right leg. He has a long history of atrial fibrillation and hypertension. His past medical history also includes stroke, bleeding duodenal ulcer, diabetes mellitus and diabetic nephropathy. On physical examination, his blood pressure is 160/70 mm Hg and his heart rate is 100 per minute and irregular. His right calf is swollen, tense and exquisitely tender; the pain is worsened by passive extension of the right knee. Dorsalis pedis and posterior tibial pulses are palpable in the bilateral lower extremities. Which of the following is the most likely cause of this patient's symptoms?
Recurrent embolism
Venous thrombosis
Soft tissue swelling
Bone infarction
Anaerobic infection
A 29-year-old woman is brought to the emergency department after burning her right upper extremity in a cooking accident Examination shows a circumferential burn of the right upper extremity. She is given fluids, an analgesic and a wound dressing. On day three she develops severe deep tissue pain in the right limb with edema of the hand. Examination shows a circumferential eschar over the right arm. Her right radial and ulnar pulses are faint compared to the left and she has paresthesias in her right hand. Which of the following is the most appropriate next step in management?
Increase the dose of her analgesics and discharge her
Do an angiography to assess arterial blood flow
Do an escharotomy
Look for a missed fracture of the right upper limb
Elevation of the limb
A 42-year-old man comes to the physician because of a 3-month history of burning substernal chest pain after every meal. His other medical problems include chronic alcoholism. Upper endoscopy shows mucosal irregularity and ulceration of the squamocolumnar junction above the lower esophageal sphincter. Multiple biopsies are taken. He complains of worsening substernal pain radiating to the back, left chest pain, and mild shortness of breath 4 hours later. His temperature is 37.1° C (98.9° F), blood pressure is 110/70 mm Hg, pulse is 120/min, and respirations are 34/min. A chest x-ray shows a small left pleural effusion that was not present on a chest radiograph taken 2 weeks ago. Which of the following is the most appropriate next step in management?
Repeat the endoscopy
Order water-soluble contrast esophagram
Check serum amylase and lipase levels
Wait until the pathologic diagnosis is ready
Perform thoracocentesis
A 65-year-old male is being evaluated for hip pain. The pain has been present for several months and is constant. He denies any weight loss or loss of appetite. His past medical history is significant only for high blood pressure. His temperature is 37.2° C (98.9° F), blood pressure is 150/88 mm Hg, pulse is 80/min and respirations are 12/min. Physical examination is unremarkable. Laboratory studies show: Alkaline phosphatase Elevated Gamma glutamyl transferase Normal Serum calcium Normal 2,5(OH)2 vitamin D Normal Bone scan shows increased uptake in several spots. This patient is at the highest risk of developing?
Subarachnoid hemorrhage
Carpal tunnel syndrome
Renal cell carcinoma
Pulmonary hemorrhage
Hearing loss
A 36-year-old woman presents to the emergency department with severe epigastric pain and right shoulder pain of about two hours duration. She also reports having one episode of emesis. When asked about her diet, she explains that she unintentionally fasted yesterday and had a large meal two hours ago. Her past medical history is significant for frequent heartburn for which she takes ranitidine. Several hours after presenting, the patient's pain resolves completely. Which of the following best explains this episode?
Viscus distention
Acid hypersecretion
Peritoneal irritation
Mucosal inflammation
Vascular obstruction
A 45-year-old man is brought to the emergency department after being involved in a motor vehicle collision. He is unable to void. Examination shows blood at the urethral meatus and a scrotal hematoma. His temperature is 37° C (98.6° F), blood pressure is 100/50, pulse is 100/min and respirations are 16/min. Examination shows a high-riding prostate with no other Elevated Normal Normal Normal signs of trauma. Which of the following is the most appropriate next step in management?
Immediate surgical repair of urethra
Foley catheterization
Retrograde urethrogram
Diuretic to increase the urine output
Retrograde cystogram with post-void films
A 3-year-old girl 1s brought to the emergency department because she is not moving her right arm. Her mother states that the child was perfectly normal in the morning. She remembers that she lifted the child with the child's right forearm and since then she has not been moving her right arm. Examination shows the right arm is held in pronation against the chest. The child avoids any movement of her right arm. Which of the following is the most appropriate next step in management?
Refer the child to an orthopedic surgeon for possible supracondylar fracture of humerus
Report the case to child protection agency
Gentle passive elbow flexion and forearm supinatio
Closed reduction and casting of forearm and arm
Do a skeletal survey of the child
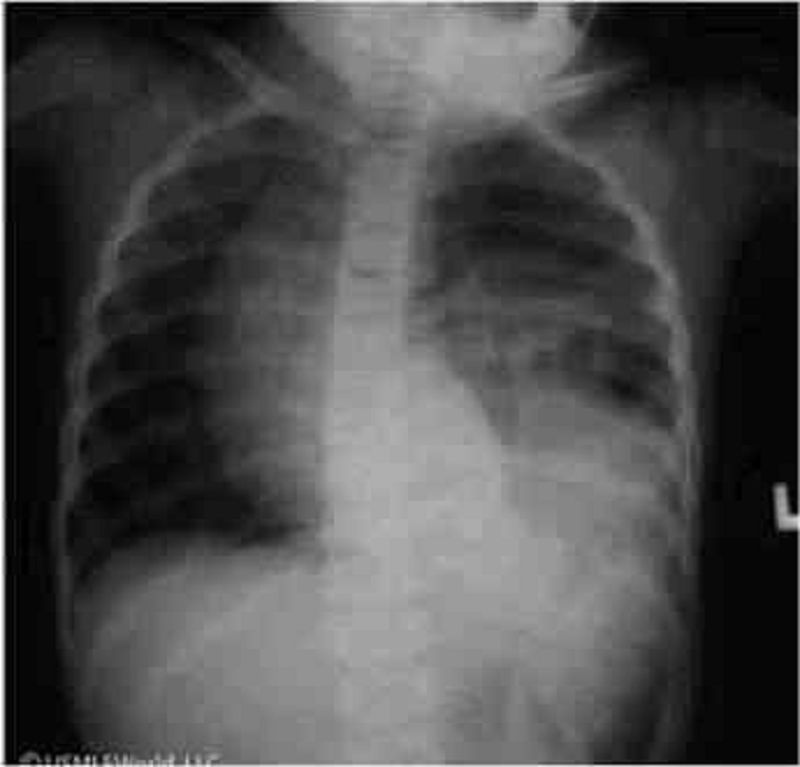
A 12-year-old boy comes to the emergency department complaining of vague left-sided chest discomfort. Two months ago, he was involved in a high-speed motor vehicle accident but sustained only minor injuries. He was observed in the emergency department overnight and discharged home. His past medical history is otherwise unremarkable. Vital signs are normal. Auscultation of the lungs shows decreased air entry into the left lower base. An x-ray of the chest is shown below: Which of the following is the most appropriate next step in management of this patient?
Chest tube placement
Computed tomography scan of the chest and abdomen
Flexible bronchoscopy
Intravenous antibiotics
Reassurance and outpatient follow-up
A 23-year-old man comes to the emergency department because of a painful swollen left knee. The pain began after he twisted his leg while playing football. Examination shows a swollen left knee with marked tenderness of the medial side of the knee. When compared to the right knee, on valgus stressing the left knee shows exaggerated laxity at the joint line. Which of the following is the most appropriate next step to confirm the diagnosis?
CT scan of the knee joint
Joint fluid aspiration
Arthroscopy
MRI of the knee joint
Plain radiographs of the knee joint
A 23-year-old male is brought to the emergency department following a motor vehicle accident (MVA) where he was the unrestrained driver. The patient was found unresponsive at the scene and was intubated by paramedics. He receives 2.5L of normal saline over the 20 minutes before he reaches the ED. His blood pressure there is 70/30 mmHg and his heart rate is 120/min. On physical examination, he responds to strong vocal and tactile stimuli by opening his eyes. His pupils are equal and reactive to light. There are multiple bruises over the anterior chest and upper abdomen. His neck veins are flat, trachea is midline and extremities are cold. Cardiac monitoring shows sinus tachycardia. Which of the following is the most likely cause of this patient's current condition?
Impaired myocardial contractility
Ventricular filling restriction
Loss of intravascular volume
Air embolism
Loss of vascular tone
A 25-year-old motorcyclist is brought to the emergency department after being involved in a collision with an automobile. On arrival he is in obvious pain. He expresses an urge to void, but is unable to do so. Genital examination shows blood at the urethral meatus and a scrotal hematoma. Rectal examination reveals a high-riding prostate. Abdominal examination is suggestive of a distended bladder. Which of the following is the most likely diagnosis?
Urethral injury
Intraperitoneal bladder rupture
Extraperitoneal bladder injury
Fracture of penis
Renal injury
A 36-year-old male comes to the emergency department because of worsening right lower quadrant (RLQ) abdominal pain. One week ago he was started on cephalexin for furunculosis. He has had type I diabetes mellitus for 1Oyears and is on insulin. His temperature is 38.83°C (101.9°F). Examination shows multiple furuncles on the inner side of both thighs; most of them are in regression. Abdominal examination shows tenderness on deep palpation in RLQ without rebound or guarding; no masses are palpated; psoas sign is positive; bowel sounds are present. Rectal examination shows no abnormalities. Laboratory studies show: Hemoglobin 13.0 g/L Leukocyte count 17,500/mm3 Which of the following is the most appropriate next step in management?
Appendectomy
Laparoscopy
CT of abdomen
Colonoscopy
AP and lateral lumbar films
A 54-year-old man is brought to the emergency department 10 minutes after being involved in a motor vehicle accident. He was an unrestrained driver and hit a car while speeding on the highway. On arrival to the emergency department, he is spontaneously breathing and noncyanotic. His temperature is 37°C (98.6°F), blood pressure is 104/50 mm Hg, pulse is 122/min, and respirations are 16/min. Examination shows facial lacerations and multiple ecchymoses on the anterior chest and abdomen. He appears obtunded. Which of the following is a component of the Glasgow coma scale (GCS) assessment for this patient?
Capillary refill
Deep tendon reflexes
Eye opening
Gag reflex
Pupillary reaction
A 46-year-old man comes to the emergency department because of abrupt onset of epigastric pain radiating to the back and associated vomiting. He has had these symptoms for the past 1 day. The symptoms are progressively getting worse. He has no other medical problems or previous surgeries. He does not use tobacco, alcohol, or illicit drugs. His temperature is 36.5° C (97.6° F), blood pressure is 100/70 mm Hg, pulse is 100/min, and respirations are 20/min. Abdomen is mildly distended and very tender to palpation in the epigastric region; bowel sounds have decreased. There is no rebound tenderness or organomegaly. Rectal examination shows no abnormalities. Laboratory findings reveal: CBC Hb15.0g/dL Platelet count 223,000/mm Leukocyte count 14,500/mm Serum Chemistry Serum Na 134mg/dL Serum K 3.6mg/dL Chloride 93mg/dL Bicarbonates 29mg/dL BUN 30mg/dL Serum creatinine 0.8mg/dL Calcium 10.3mg/dL Blood glucose 168mg/dL LFT1.4mg/dL Total bilirubin Alkaline phosphatase 220U/L Aspartate aminotransferase 88U/L Alanine aminotransferase 155 U/L Lipase Abdominal 523U/L x-ray shows gaseous distention of the small bowel in the upper abdomen. Computed tomography (CT) scan with contrast shows diffuse hypodense enlargement of the pancreas and peripancreatic and perirenal fluid collections. Nasogastric suction, intravenous normal saline, analgesics, and antibiotics are started. Which of the following is the most appropriate next step in management?
Add intravenous sodium bicarbonate
Add intravenous pancreatic protease inhibitor
Perform colonoscopic decompression
Administer intramuscular carbachol to treat ileus
Obtain a right upper quadrant ultrasound
{"name":"Surgery USMLE (927-1022)", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Your hospital is conducting an ongoing research study involving the hormonal response to trauma. Blood is drawn regularly (with Institutional Review Board [IRB] approval) for various studies. Which of the following values are likely to be seen after a healthy 36-year-old man is hit by a bus and sustains a ruptured spleen and a lacerated small bowel?","img":"https://cdn.poll-maker.com/18-741602/untitled-22.jpg?sz=1200"}
More Quizzes
Mason About Me
10522
7.klasse
331647
AIRCRAFT LANDING GEAR SYSTEM (continuation)
1470
Water conservation quiz
1050
Risk Assessment - Test Your Safety Knowledge
201018587
Arabic Grammar - Free Online Practice
201015932
French Adjectives - Agreement & Conjugation
201017986
What Pokémon Am I? Free - Find Your Best Match
201016931
First Aid Exam Questions & Answers - Free Practice
201018132
Frida Kahlo Trivia - Test Your Art Knowledge
201021212
What Kind of Toy Are You? Personality (Free)
201016636
Peach Trivia Questions and Answers - Free Online
201017775