QCU/DES/USMLE/EMERGENCY

Emergency Medicine Mastery Quiz
Test your knowledge and skills in emergency medicine with our comprehensive quiz designed for medical students, healthcare professionals, and enthusiasts. Explore a range of clinical scenarios that will challenge your understanding of diagnosis, treatment, and critical care.
Whether you're preparing for exams or just want to reinforce your medical knowledge, this quiz offers:
- 150 carefully curated questions
- Diverse clinical cases from various specialties
- Immediate feedback and scoring
48. A 35-year-old man who is employed as a forklift operator was found sitting outside a warehouse. He came stumbling out complaining of dizziness and headaches. Coworkers in an adjoining warehouse also complained of headache and nausea. After collapsing outside, he regained consciousness immediately but appeared confused. In the ED, his BP is 100/54 mm Hg, HR is 103 beats per minute, temperature is 100°F, pulse ox is 91% on room air, and RR is 23 breaths per minute. Physical examination is unremarkable. Laboratory results reveal WBC 10,500/μL, hematocrit 45%, platelets 110/μL, sodium 137 mEq/L, potassium 4 mEq/L, chloride 103 mEq/L, bicarbonate 21 mEq/L, BUN 8 mg/dL, creatinine 0.5 mg/dL, and glucose 89 mg/dL. Arterial blood gas results are pH 7.32, PCO2 32 mm Hg, and PO2 124 mm Hg. Which of the following is the most likely diagnosis?
A. Methemoglobinemia
B. Hypoglycemic syncope
C. Hydrocarbon poisoning
D. Opioid overdose
E. CO poisoning
49. A 51-year-old man presents to the ED complaining of nausea and abdominal pain after drinking some “bitter stuff.” He is considered one of the “regulars” who is usually at triage with ethanol intoxication. His temperature is 97.9°F, BP is 130/65 mm Hg, HR is 90 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 97% on room air. Physical examination is unremarkable, except for slurred speech and the smell of acetone on the patient’s breath. Laboratory results reveal serum sodium 138 mEq/L, potassium 3.5 mEq/L, chloride 105 mEq/L, bicarbonate 23 mEq/L, BUN 10 mg/dL, creatinine 2.1 mg/dL, glucose 85 mg/dL, arterial blood pH 7.37, and lactate 1.4 mEq/L. Urinalysis shows moderate ketones. Which of the following is the most likely diagnosis?
A. DKA
B. Ethanol intoxication
C. Methanol intoxication
D. Isopropyl alcohol intoxication
E. Ethylene glycol intoxication
50. A 55-year-old man presents to the ED 6 hours after ingesting two bottles of his baby aspirin. He complains of nausea, vomiting, dizziness, and tinnitus. His temperature is 100.3°F, BP is 140/80 mm Hg, HR is 105 beats per minute, RR is 31 breaths per minute, and oxygen saturation is 99% on room air. Arterial blood gas on room air reveals a pH of 7.52, PCO2 10 mm Hg, and PO2 129 mm Hg. The blood salicylate level returns at 45 mg/dL. Which of the following is the most appropriate next step in management?
A. Administer activated charcoal, begin IV hydration, and administer sodium bicarbonate.
B. Administer activated charcoal, begin IV hydration, and intubate the patient for respiratory failure.
C. Administer activated charcoal, begin IV hydration, and administer NAC.
D. Arrange for immediate hemodialysis.
E. Gastric lavage, IV hydration, and repeat levels before beginning therapy.
51. A 40-year-old man with a known history of ethanol abuse states that 2 hours ago he ingested two bottles of extrastrength Tylenol. The patient has no medical complaints except for some nausea. At 4 hours postingestion, you send blood to the laboratory to measure the serum acetaminophen concentration. The level returns and falls above the treatment line when you plot it on the APAP nomogram. You administer activated charcoal and decide to start IV NAC. Which of the following is a known adverse effect of IV NAC administration?
A. Hepatic failure
B. Anaphylactoid reaction
C. Hypertensive crisis
D. Confusion
E. Change in urine color
52. A 19-year-old woman presents to the ED with abdominal pain, nausea, vomiting, diarrhea, and hematemesis after ingesting an unknown substance in a suicide attempt. Which of the following antidotes are correctly paired?
A. Organophosphate—Physostigmine
B. Iron overdose—Deferoxamine
C. Aspirin overdose—NAC
D. Acetaminophen overdose—Naloxone
E. Anticholinergic overdose—Fomepizole
53. A 34-year-old woman presents to the ED after ingesting an unknown quantity of her antidepressant pills. EMS workers found an empty bottle of amitriptyline on her apartment floor. She is awake but appears delirious. Her BP is 130/65 mm Hg, HR is 101 beats per minute, temperature is 99.1°F, RR is 16 breaths per minute, and oxygen saturation is 100% on room air. On examination, her pupils are 7 mm and reactive. Her face is flushed and mucous membranes are dry. Her lungs are clear and heart is without murmurs. The abdomen is soft, nontender, and with decreased bowel sounds. She is moving all four extremities. ECG reveals sinus rhythm at a rate of 99 and QRS just under 100 milliseconds. In a TCA overdose, which of the following is responsible for her mydriasis, dry mucous membranes, and delirium?
A. Sodium channel blockade
B. Muscarinic receptor blockade
C. Inhibition of serotonin and norepinephrine reuptake
D. Histamine receptor blockade
E. α-Receptor blockade
54. An asymptomatic young adult was brought to the ED by a police officer after his home was raided. The patient swallowed five small packets of an unknown substance before being arrested. His BP is 125/75 mm Hg, HR is 85 beats per minute, temperature is 98.7°F, and RR is 16 breaths per minute. Physical examination is unremarkable. An abdominal radiograph confirms intraluminal small bowel densities. Which of the following is the most appropriate treatment?
A. Magnesium citrate
B. Gastric lavage
C. Activated charcoal and polyethylene glycol
D. Syrup of ipecac
E. NAC
55. A 33-year-old woman presents to the ED with a painful sprained ankle. She has a past medical history of depression for which she is taking phenelzine, a monoamine oxidase inhibitor. After you place an elastic wrap on her ankle, she asks you to prescribe her some pain medication. Which of the following medications is contraindicated in patients taking a monoamine oxidase inhibitor?
A. Ibuprofen
B. Acetaminophen
C. Meperidine
D. Oxycodone
E. Hydrocodone
56. A 27-year-old woman presents to the ED 6 hours after the onset of body aches, abdominal cramping, and diarrhea. She is currently visiting relatives and normally lives in another state. She regularly takes six to eight tablets daily of hydrocodone for chronic low-back pain, sumatriptan for migraines, and amitriptyline and paroxetine for bulimia nervosa. Her BP is 130/80 mm Hg, HR is 100 beats per minute, temperature is 98.6°F, RR is 16 breaths per minute, and oxygen saturation is 99% on room air. Examination shows diaphoresis, dilated pupils, and piloerection. Neurologically she is moving all four extremities and you do not note tremors. She is alert and cooperative but seems restless. She denies hallucinations or suicidal ideations. She becomes very angry when you ask her for the phone numbers of her regular physicians. Which of the following is the most likely explanation of her symptoms?
A. Anticholinergic overdose
B. TCA intoxication
C. Ethanol withdrawal
D. Serotonin syndrome
E. Opiate withdrawal
57. A 58-year-old woman is brought to the emergency department (ED) by emergency medical service (EMS) after slipping on a patch of ice while walking to work and hitting her head on the cement pavement. Bystanders acknowledged that the patient was unconscious for approximately 1 minute. On arrival, her vital signs are blood pressure (BP) 155/75 mm Hg, heart rate (HR) 89 beats per minute, respiratory rate (RR) 18 breaths per minute, and pulse oxygenation 98% on room air. She has a 5-cm laceration to the back of her head that is actively bleeding. You ask the patient what happened but she cannot remember. You inform her that she is in the hospital as a result of a fall. Over the next 10 minutes she asks you repeatedly what happened and where she is. You do not find any focal neurologic deficits. As you bring the patient to the CT scanner, she vomits once. CT results show a normal brain scan. Which of the following is the most likely diagnosis?
A. Cerebral concussion
B. Diffuse axonal injury
C. Cerebral contusion
D. Posttraumatic epilepsy
E. Trauma-induced Alzheimer disease
58. A 41-year-old man, the restrained driver in a high-speed motor vehicle collision, is brought to the ED by EMS. The patient is breathing without difficulty with bilateral and equal breaths sounds. He has strong pulses peripherally indicating a BP of at least 90 mm Hg. The HR is 121 beats per minute. His Glasgow coma scale (GCS) is 14. A secondary survey reveals chest wall bruising. You suspect a cardiac injury. Which of the following locations most commonly involve cardiac contusions?
A. Right atrium
B. Right ventricle
C. Left atrium
D. Left ventricle
E. Septum
59. A 25-year-old man is brought into the trauma resuscitation room after his motorcycle is struck by another vehicle. EMS reports that the patient was found 20 ft away from his motorcycle, which was badly damaged. His vital signs include a BP of 90/60 mm Hg, HR 115 beats per minute, RR 22 breaths per minute, and pulse oxygenation of 100% on facemask. Which of the following is the smallest amount of blood loss that produces a decrease in the systolic BP in adults?
A. Loss of 5% of blood volume
B. Loss of 10% of blood volume
C. Loss of 15% to 30% of blood volume
D. Loss of 30% to 40% of blood volume
E. Loss of greater than 40% of blood volume
60. You are notified by the EMS dispatcher that there is a multiple-car collision on the local highway with many injuries. He states that there are two people dead at the scene, one person is critically injured and hypotensive, and three people have significant injuries but with stable vital signs. Which of the following is the leading cause of death and disability in trauma victims?
A. Abdominal injury
B. Thoracic injury
D. Cervical injury
C. Back injury
E. Head injury
61. Paramedics bring a 17-year-old high school football player to the ED on a backboard and with a cervical collar. During a football game, the patient “speared” another player with his helmet and subsequently experienced severe neck pain. He denies paresthesias and is able to move all of his extremities. A cervical spine CT scan reveals multiple fractures of the first cervical vertebra. Which of the following best describes this fracture?
A. Odontoid fracture
B. Hangman’s fracture
C. Jefferson fracture
D. Clay shoveler’s fracture
E. Teardrop fracture
62. A 20-year-old man presents to the ED with multiple stab wounds to his chest. His BP is 85/50 mm Hg and HR is 123 beats per minute. Two large-bore IVs (intravenous) are established and running wide open. On examination, the patient is mumbling incomprehensibly, has good air entry on lung examination, and you notice jugular venous distension (JVD). As you are listening to his heart, the nurse calls out that the patient has lost his pulse and that she cannot get a BP reading. Which of the following is the most appropriate next step in management?
A. Atropine
B. Epinephrine
C. Bilateral chest tubes
D. ED thoracotomy
E. Pericardiocentesis
63. A 22-year-old man calls the ED from a local bar stating that he was punched in the face 10 minutes ago and is holding his front incisor tooth in his hand. He wants to know what the best way is to preserve the tooth. Which of the following is the most appropriate advice to give the caller?
A. Place the tooth in a napkin and bring it to the ED.
B. Place the tooth in a glass of water and bring it to the ED.
C. Place the tooth in a glass of beer and bring it to the ED.
D. Pour some water over the tooth and place it immediately back into the socket.
E. Place the tooth in a glass of milk and bring it to the ED.
64. A 19-year-old man is brought into the trauma room by EMS after a head-on cycling accident. The patient was not wearing a helmet. Upon presentation his BP is 125/75 mm Hg, HR is 105 beats per minute, RR is 19 breaths per minute, and oxygen saturation is 100% on mask. His eyes are closed but open to command. He can move his arms and legs on command. When you ask him questions, he is disoriented but able to converse. What is this patient’s GCS score?
A. 11
B. 12
C. 13
D. 14
E. 15
65. An 18-year-old man presents to the ED after getting stabbed in his abdomen. His HR is 140 beats per minute and BP is 90/40 mm Hg. He is yelling that he is in pain. Two large-bore IVs are inserted into his antecubital fossa and fluids are running wide open. After 2 L of fluids, his BP does not improve. Which of the following is the most common organ injured in stab wounds?
A. Liver
B. Small bowel
C. Stomach
D. Colon
E. Spleen
66. A 61-year-old man presents to the ED with chest wall pain after a motor vehicle collision. He is speaking full sentences, breath sounds are equal bilaterally, and his extremities are well-perfused. His BP is 150/75 mm Hg, HR is 92 beats per minute, and oxygen saturation is 97% on room air. Chest radiography reveals fractures of the seventh and eighth ribs of the right anterolateral chest. He has no other identifiable injuries. Which of the following is the most appropriate treatment for this patient’s rib fractures?
A. Apply adhesive tape on the chest wall perpendicular to the rib fractures.
B. Insert a chest tube into the right thorax.
C. Bring the patient to the OR for surgical fixation.
D. Analgesia and incentive spirometry.
Observation
67. A 27-year-old man brought to the ED by paramedics after a motor vehicle collision. His RR is 45 breaths per minute, oxygen saturation is 89%, HR is 112 beats per minute, and BP is 115/75 mm Hg. You auscultate his chest and hear decreased breath sounds on the left. Which of the following is the most appropriate next step in management?
A. Order a stat chest radiograph.
B. Perform a pericardiocentesis.
C. Perform a diagnostic peritoneal lavage (DPL).
D. Perform an ED thoracotomy.
E. Perform a tube thoracostomy.
68. A 29-year-old man is brought to the ED by EMS after being stabbed in the left side of his back. His BP is 120/80 mm Hg, HR is 105 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 98% on room air. On the secondary survey, you note motor weakness of his left lower extremity and the loss of pain sensation in the right lower extremity. Which of the following is the most likely diagnosis?
A. Spinal shock
B. Central cord syndrome
C. Anterior cord syndrome
D. Brown-Sequard syndrome
E. Cauda equina syndrome
69. A 33-year-old man, who was drinking heavily at a bar, presents to the ED after getting into a fight. A bystander tells paramedics that the patient was punched and kicked multiple times and sustained multiple blows to his head with a stool. In the ED, his BP is 150/75 mm Hg, HR is 90 beats per minute, RR is 13 breaths per minute, and oxygen saturation is 100% on non-rebreather. On examination, he opens his eyes to pain and his pupils are equal and reactive. There is a laceration on the right side of his head. He withdraws his arm to pain but otherwise does not move. You ask him questions, but he just moans. Which of the following is the most appropriate next step in management?
A. Prepare for intubation.
B. Suture repair of head laceration.
C. Administer mannitol.
D. Bilateral burr holes.
E. Neurosurgical intervention.
70. A 74-year-old man presents to the ED after being involved in a motor vehicle collision. He states he was wearing his seat belt in the driver’s seat when a car hit him from behind. He thinks his chest hit the steering wheel and now complains of pain with breathing. His RR is 20 breaths per minute, oxygen saturation is 98% on room air, BP is 145/75 mm Hg, and HR is 90 beats per minute. On examination, you notice paradoxical respirations. Which of the following best describes a flail chest?
A. One rib with three fracture sites
B. Two adjacent ribs, each with two fracture sites
C. Three adjacent ribs, each with two fracture sites
D. One fractured right-sided rib and one fractured left-sided rib
E. Two fractured right-sided ribs and two fractured left-sided ribs
71. A 29-year-old man presents to the ED after being stabbed in his neck. The patient is speaking in full sentences. His breath sounds are equal bilaterally. His BP is 130/75 mm Hg, HR is 95 beats per minute, RR is 16 breaths per minute, and oxygen saturation is 99% on room air. The stab wound is located between the angle of the mandible and the cricoid cartilage and violates the platysma. There is blood oozing from the site although there is no expanding hematoma. Which of the following is the most appropriate next step in management?
A. Explore the wound and blind clamp any bleeding site.
B. Probe the wound looking for injured vessels.
C. Apply direct pressure and bring the patient immediately to the OR to explore the zone I injury.
D. Apply direct pressure and bring the patient immediately to the OR to explore the zone II injury.
E. Apply direct pressure and bring the patient immediately to the OR to explore the zone III injury.
72. A 45-year-old man is brought to the ED after a head-on motor vehicle collision. Paramedics at the scene tell you that the front end of the car is smashed. The patient’s BP is 130/80 mm Hg, HR is 100 beats per minute, RR is 15 breaths per minute, and oxygen saturation is 98% on room air. Radiographs of the cervical spine reveal bilateral fractures of the C2 vertebra. The patient’s neurologic examination is unremarkable. Which of the following best describes this fracture?
A. Colles fracture
B. Boxer’s fracture
C. Jefferson fracture
D. Hangman’s fracture
E. Clay shoveler’s fracture
73. A 71-year-old man is found lying on the ground one story below the balcony of his apartment. Paramedics bring the patient into the ED. He is cool to touch with a core body temperature of 96°F. His HR is 119 beats per minute and BP is 90/70 mm Hg. His eyes are closed, but they open when you call his name. His limbs move to stimuli, and he answers your questions but is confused. On examination, you note clear fluid dripping from his left ear canal and an area of ecchymosis around the mastoid bone. Which of the following is the most likely diagnosis?
A. Le Fort fracture
B. Basilar skull fracture
C. Otitis interna
D. Otitis externa
E. Tripod fracture
74. A 34-year-old construction worker is brought to the ED by EMS after falling 30 ft from a scaffold. His vital signs are HR 124 beats per minute, BP 80/40 mm Hg, and oxygen saturation 93% on 100% oxygen. He has obvious head trauma with a scalp laceration overlying a skull fracture on his occiput. He does not speak when asked his name, his respirations are poor, and you hear gurgling with each attempted breath. Auscultation of the chest reveals diminished breath sounds on the right. There is no JVD or anterior chest wall crepitus. His pelvis is unstable with movement laterally to medially and you note blood at the urethral meatus. His right leg is grossly deformed at the knee and there is an obvious fracture of his left arm. Which of the following is the most appropriate next step in management?
A. Insert a 32F chest tube into the right thoracic cavity.
B. Perform a DPL to rule out intra-abdominal hemorrhage.
C. Create two Burr holes into the cranial vault to treat a potential epidural hematoma.
D. Immediately reduce the extremity injuries and place in a splint until the patient is stabilized.
E. Plan for endotracheal intubation of the airway with in-line stabilization of the cervical spine.
75. A 20-year-old man was found on the ground next to his car after it hit a tree on the side of the road. Bystanders state that the man got out of his car after the collision but collapsed within a few minutes. Paramedics subsequently found the man unconscious on the side of the road. In the ED, his BP is 175/90 mm Hg, HR is 65 beats per minute, temperature is 99.2°F, RR is 12 breaths per minute, and oxygen saturation is 97% on room air. Physical examination reveals a right-sided fixed and dilated pupil. A head CT is shown below. Which of the following is the most likely diagnosis?
A. Epidural hematoma
B. Subdural hematoma
C. Subarachnoid hemorrhage (SAH)
D. Intracerebral hematoma
E. Cerebral contusion
76. 81-year-old woman presents to the ED after tripping over the sidewalk curb and landing on her chin causing a hyperextension of her neck. She was placed in a cervical collar by paramedics. On examination, she has no sensorimotor function of her upper extremities. She cannot wiggle her toes, has 1/5 motor function of her quadriceps, and only patchy lower extremity sensation. Rectal examination reveals decreased rectal tone. Which of the following is the most likely diagnosis?
A. Central cord syndrome
B. Anterior cord syndrome
C. Brown-Sequard syndrome
D. Transverse myelitis
E. Exacerbation of Parkinson disease
77. A 22-year-old man presents to the ED after being ejected from his vehicle following a high-speed motor vehicle collision. Upon arrival, his BP is 85/55 mm Hg and HR is 141 beats per minute. Two large-bore IVs are placed in the antecubital veins and lactated Ringer solution is being administered. After 3 L of crystalloid fluid, the patient’s BP is 83/57 mmHg. Which of the following statements is most appropriate regarding management of a hypotensive trauma patient who fails to respond to initial volume resuscitation?
A. It is important to wait for fully cross-matched blood prior to transfusion.
B. Whole blood should be used rather than packed red blood cells (RBCs).
C. Blood transfusion should begin after 4 L of crystalloid infusion.
D. Type O blood that is Rh-negative should be transfused.
E. Type O blood that is Rh-positive should be transfused.
78. A 24-year-old man is brought into the ED by paramedics after being run over by a car. His systolic BP is 90 mm Hg by palpation, HR is 121 beats per minute, RR is 28 breaths per minute, and oxygen saturation is 100% on non-rebreather. The airway is patent and breath sounds are equal bilaterally. You establish large-bore access and fluids are running wide open. Secondary survey reveals an unstable pelvis upon movement with lateral to medial force. Bedside focused abdominal sonography for trauma (FAST) is negative for intraperitoneal fluid. Which of the following is the most appropriate immediate next step in management?
A. Bilateral chest tubes
B. Application of external fixator
C. Application of pelvic binding apparatus
D. Venographic embolization
E. Angiographic embolization
79. A 32-year-old man is brought to the ED by paramedics after a diving accident. The lifeguard on duty accompanies the patient and states that he dove head first into the shallow end of the pool and did not resurface. On examination, the patient is speaking but cannot move his arms or legs and cannot feel pain below his clavicle. He is able to feel light touch and position of his four extremities. A cervical spine radiograph does not reveal a fracture. Which of the following is the most likely diagnosis?
A. Spinal cord injury without radiographic abnormality (SCIWORA)
B. Central cord syndrome
C. Anterior cord syndrome
D. Cauda equina syndrome
E. Brown-Sequard syndrome
80. A 22-year-old man is brought to the ED 20 minutes after a head-on motor vehicle collision in which he was the unrestrained driver. On arrival, he is alert and coherent but appears short of breath. His HR is 117 beats per minute, BP is 80/60 mm Hg, and oxygen saturation is 97% on a nonrebreather. Examination reveals bruising over the central portion of his chest. His neck veins are not distended. Breath sounds are present on the left but absent on the right. Following administration of 2 L of lactated Ringer solution, his systolic BP remains at 80 mm Hg. Which of the following is the most appropriate next step in management?
A. Sedate, paralyze, and intubate.
B. Perform a needle thoracostomy.
C. Perform a DPL.
D. Perform a FAST examination.
E. Perform a pericardiocentesis.
81. An 87-year-old man is brought to the ED on a long board and in a cervical collar after falling down a flight of steps. He denies losing consciousness. On arrival, his vital signs include an HR of 99 beats per minute, BP of 160/90 mm Hg, and RR of 16 breaths per minute. He is alert and speaking in full sentences. Breath sounds are equal bilaterally. Despite an obvious right arm fracture, his radial pulses are 2+ and symmetric. When examining his cervical spine, he denies tenderness to palpation and you do not feel any bony deformities. Which of the following is a true statement?
A. Epidural hematomas are very common in the elderly age population.
B. Cerebral atrophy in the elderly population provides protection against subdural hematomas.
C. Increased elasticity of their lungs allows elderly patients to recover from thoracic trauma more quickly than younger patients.
D. The most common cervical spine fracture in this age group is a wedge fracture of the sixth cervical vertebra.
E. Despite lack of cervical spine tenderness, imaging of his cervical spine is warranted.
82. A 45-year-old man is brought into the ED after a head-on motor vehicle collision. His BP is 85/45 mm Hg and HR is 130 beats per minute. He is speaking coherently. His breath sounds are equal bilaterally. After 2 L of fluid resuscitation, his BP is 80/40 mm Hg. A FAST examination reveals fluid in Morison pouch. Which of the following organs is most likely to be injured in blunt abdominal trauma?
A. Liver
B. Spleen
D. Small bowel
C. Kidney
E. Bladder
83. A 47-year-old man is brought into the ED after falling 20 ft from a ladder. His HR is 110 beats per minute, BP is 110/80 mm Hg, RR is 20 breaths per minute, and oxygen saturation is 100% on face mask. He is able to answer your questions without difficulty. His chest is clear with bilateral breath sounds, abdomen is nontender, pelvis is stable, and the FAST examination is negative. You note a large scrotal hematoma and blood at the urethral meatus. Which of the following is the most appropriate next step in management?
A. Scrotal ultrasound
B. Kidney-ureter-bladder (KUB) radiograph
C. IV pyelogram
D. Retrograde cystogram
E. Retrograde urethrogram
84. A 17-year-old man presents to the ED after getting hit in the right eye with a tennis ball during a tennis match. On arrival to the ED, you note periorbital swelling and ecchymosis. The patient’s visual acuity is 20/20. When you are testing his extraocular muscles, you note that his right eye cannot look superiorly but his left eye can. He also describes pain in his right eye when attempting to look upward. Which of the following is the most likely diagnosis?
A. Zygomatic arch fracture
B. Orbital floor fracture
C. Retrobulbar hematoma
D. Ruptured globe
E. Mandible fracture with entrapment of the pterygoid
85. A 24-year-old man is brought to the ED after being shot once in the abdomen. On arrival, his BP is 100/60 mm Hg, HR is 115 beats per minute, and RR is 22 breaths per minute. His airway is patent and you hear breath sounds bilaterally. On abdominal examination, you note a single bullet entry wound approximately 1 cm to the right of the umbilicus. During the log roll, you see a single bullet exit wound approximately 3 cm to the right of the lumbar spine. His GCS score is 15. The patient’s BP is now 85/65 mmHg and HR is 125 beats per minute after 2L of fluid. Which of the following is the most appropriate next step in management?
A. Probe the entry wound to see if it violates the peritoneum.
B. Perform a FAST examination.
C. Perform a DPL.
D. Take the patient directly to the CT scanner.
E. Take the patient directly to the OR.
86. A 43-year-old man, who currently uses drugs intravenously (IV), presents to the emergency department (ED) with 2 weeks of fever, back pain, and progressive weakness in his legs bilaterally. He denies any history of trauma or prior surgery. His blood pressure (BP) is 130/75 mm Hg, heart rate (HR) is 106 beats per minute, temperature is 103°F, and respiratory rate (RR) is 16 breaths per minute. On physical examination, he has tenderness to palpation in the mid-lumbar spine, increased patellar reflexes, and decreased strength in the lower extremities bilaterally, with normal range of motion. Laboratory results reveal a white blood cell (WBC) count of 15,500/μL, hematocrit 40%, and platelets 225/μL. Urinalysis and spinal x-rays are unremarkable. Which of the following is the most likely diagnosis?
A. Fibromyalgia
B. Ankylosing spondylitis
C. Spinal epidural abscess
E. Spinal metastatic lesion
D. Vertebral compression fracture
87. An 81-year-old woman is brought to the ED by her children who state that the patient is acting more tired than usual, has had fever for the last 2 days, and is more confused. Ordinarily, the patient is high functioning: she is ambulatory, cooks for herself, and walks on a treadmill 30 minutes a day. Her vital signs are BP 85/60 mm Hg, HR 125, RR 20, temperature 101.3°F, and pulse oxygenation 97% on room air. On examination, the patient has dry mucous membranes but is otherwise unremarkable. She is oriented to person and place but states that the year is 1925. Her laboratory results show a WBC 14,300/μL, hematocrit 31%, and platelets 350/μL. Her electrolytes are within normal limits. Blood glucose is 92 mg/dL. A chest radiograph does not show any infiltrates. Urinalysis reveals 2+ protein, trace ketones, WBC > 100/hpf, red blood cell (RBC) 5 to 10/hpf, nitrite positive, and leukocyte esterase positive. After administering a 500-cc normal saline fluid bolus and broad-spectrum antibiotics through her peripheral IV line, the patient’s BP is 82/60 mm Hg. You suspect that the patient is in septic shock due to an acute urinary tract infection. Which of the following is the next most appropriate course of action to manage this patient with earlygoal-directed therapy (EGDT)?
A. Immediately start a norepinephrine infusion to increase the blood pressure given the low systolic blood pressure.
B. Prepare to transfuse uncrossed matched packed RBC to increase oxygen-carrying capacity given the low hematocrit.
c. Place a central venous line into the right internal jugular vein to measure central venous pressure (CVP)
D. Transport the patient to radiology for a stat CT scan of her head given the acute change in mental status.
E. Place a central venous line into the right internal jugular vein to measure mixed venous oxygen saturation (SVO2).
88. A 23-year-old man presents to the ED with left lower abdominal pain and left testicular pain that started 1 to 2 weeks ago and has gradually worsened. He has some nausea and vomiting. His HR is 98 beats per minute, BP is 125/65 mm Hg, temperature is 100.9°F, and RR is 18 breaths per minute. Physical examination reveals a tender left testicle with a firm nodularity on the posterolateral aspect of the testicle. Pain is relieved slightly with elevation of the testicle and the cremasteric reflex in normal. You make the presumptive diagnosis of epididymitis. Which of the following is the next best step?
A. Prescribe pain medications and penicillin for coverage of syphilis, the most likely causative organism.
B. Recommend bed rest, ice, and scrotal elevation with prompt urology follow-up.
C. Give ceftriaxone 125 mg intramuscularly (IM), plus a one-time dose of azithromycin 1g orally.
D. Give ceftriaxone 250 mg intramuscularly (IM), plus a 10-day course of oral doxycycline.
E. Confirm the diagnosis with transillumination of the testicle, and then consult urology for surgical drainage.
89. A 40-year-old man with insulin-dependent diabetes presents to the ED with complaints of 2 days of increasingly severe perineal pain and subjective fevers. His HR is 118 beats per minute, BP is 95/55 mm Hg, temperature is 103.4°F, and RR is 22 breaths per minute. The bedside sugar reading is “high.” Physical examination demonstrates crepitus over the medial thigh and widespread erythema and purple discoloration with sharp demarcation over the scrotum. The scrotum is markedly tender, warm, and edematous. Which of the following is the most likely diagnosis?
A. Cutaneous candidiasis
B. Fournier syndrome
C. Phimosis
D. Paraphimosis
E. Testicular torsion
90. A 55-year-old man with a history of diabetes presents with complaints of developed left knee pain several days following a fall from standing height. The patient was brought to the ED by ambulance after being found on a park bench stating he was unable to walk because of the pain. On physical examination, there are no rashes or external signs of trauma. His left knee is warm, diffusely tender, and swollen with a large effusion. He has pain on passive range of motion and is refusing to walk. His BP is 150/85 mm Hg, HR is 105 beats per minute, temperature is 102.7°F, RR is 16 breaths per minute, and fingerstick glucose is 89 mg/dL. Which of the following is the most appropriate diagnostic test?
A. Knee radiographs
B. Magnetic resonance imaging (MRI)
C. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
D. Arthrocentesis
E. Bone scan
91. A 35-year-old woman with systemic lupus erythematosus (SLE) is brought to the ED by her brother after he found her febrile and confused. Physical examination reveals fever, tachycardia, a waxing and waning mental status, petechiae over her oral mucosa, pallor, and mildly heme-positive stool. Her urinalysis is positive for blood, red cell casts, and proteinuria. Laboratory results reveal blood urea nitrogen (BUN) of 40 mg/dL and creatinine of 2 mg/dL. Her bilirubin is elevated (unconjugated > conjugated) and her international normalized ratio (INR) is 0.98. Her complete blood count reveals WBC 12,000/μL, hematocrit 29%, and platelet count 17,000/μL with schistocytes on the peripheral smear. Which of the following is the most appropriate next step in management?
A. Admit to the intensive care unit (ICU) for plasmapheresis and close monitoring for acute bleeds.
B. Admit to the ICU for platelet transfusion and monitoring for acute bleeds.
C. Admit to the ICU for corticosteroid infusion, transfusion of platelets, and prompt surgical consultation for emergent splenectomy.
D. Admit to the ICU for dialysis and close monitoring for acute bleeds.
E. Perform a noncontrast head computed tomography (CT) to screen for intracranial bleeding and mass effect followed by a lumbar puncture (LP) for analysis of cerebrospinal fluid (CSF). If negative, admit to telemetry for hemodynamic monitoring.
92. A 30-year-old woman presents to the ED with fever, headache, a “sunburn-like” rash, and confusion. A friend states that the patient has complained of nausea, vomiting, diarrhea, and a sore throat over the past few days. Her last menstrual period began 4 days ago. Vital signs are HR 110 beats per minute, BP 80/45 mm Hg, RR of 18 breaths per minute, and temperature of 103°F. On physical examination, you note an ill-appearing woman with a diffuse blanching erythroderma. Her neck is supple without signs of meningeal irritation. On pelvic examination, you remove a tampon. You note a fine desquamation of her skin, especially over the hands and feet, and hyperemia of her oropharyngeal, conjunctival, and vaginal mucous membranes. Laboratory results reveal a creatine phosphokinase (CPK) of 5000, WBC 15,000/μL, platelets of 90,000/μL, BUN 40 mg/dL, creatinine 2 mg/dL, and elevated liver enzymes. You suspect thediagnosis of toxic shock syndrome and initiate IV fluids. You target antibiotics at which of the following causative organism?
A. Staphylococcus aureus
B. Rickettsia rickettsii
C. Streptococcus pyogenes
D. Neisseria meningitidis
E. Neisseria gonorrhoeae
93. A 32-year-old diabetic man presents to the ED with a fever and 1 week of increasing right foot pain. He states he stepped on a nail while running barefoot 2 weeks ago but didn’t think much of it at that time. On physical examination, his heel is mildly erythematous and diffusely tender to palpation, with overlying warmth and edema. There is a small amount of purulent drainage through the puncture hole in his heel. A plain radiograph of his foot demonstrates a slight lucency of the calcaneus. He has decreased range of motion, but you are able to passively dorsiflex and plantarflex his ankle without difficulty. His vital signs include a temperature of 101.4°F, HR of 98 beats per minute, BP of 130/75 mm Hg, and RR of 16 breaths per minute. Which of the following is the most common causative organism of this condition?
A. Salmonella sp
B. Pseudomonas aeruginosa
C. Staphylococcus aureus
D. Group B streptococci
E. Pasteurella multocida
94. A 75-year-old woman is transferred to your ED from the local nursing home for fever, cough, and increasing lethargy. Over the past 3 days, the nursing home staff noticed increasing yellow sputum and decreasing urine output from the patient. Her BP is 118/75 mm Hg, RR is 20 breaths per minute, HR is 105 beats per minute, temperature is 100.9°F, and pulse oxygenation is 94% on room air. On examination, auscultation of the lungs reveals bibasilar crackles. Laboratory results reveal WBC 14,500/μL, hematocrit 39%, platelets 250/μL, sodium 132 mEq/L, potassium 3.5 mEq/L, chloride 100 mEq/L, bicarbonate 18 mEq/L, BUN 27 mg/dL, creatinine 1.5 mg/dL, and glucose 85 mg/dL. Serum lactate is 4.7 mmol/dL. Chest radiography reveals bilateral lower lobe infiltrates. Based on this patient’s presentation, which of the following is the most likely diagnosis?
A. Hospital-acquired pneumonia (HAP)
B. Community-acquired pneumonia (CAP)
C. Health care–associated pneumonia (HCAP)
D. Ventilator-associated pneumonia (VAP)
E. Atypical pneumonia
95. A 55-year-old man presents to the ED with fever, drooling, trismus, and a swollen neck. He reports a foul taste in his mouth caused by a tooth extraction 2 days ago. On physical examination, the patient appears anxious. He has bilateral submandibular swelling and elevation and protrusion of the tongue. He appears “bull-necked” with tense and markedly tender edema and brawny induration of the upper neck, and he is tender over the lower second and third molars. There is no cervical lymphadenopathy. These lungs are clear to auscultation with good air movement. His vital signs are HR 105 beats per minute, BP 140/85 mm Hg, RR 26 breaths per minute, and temperature 102°F. Which of the following is the most appropriate next step in management?
A. Obtain a sample for culture, administer a dose of IV antibiotics, and obtain a soft tissue radiograph of the neck.
B. Obtain a sample for culture, perform a broad incision and drainage at bedside, and administer a dose of IV antibiotics.
e. Secure his airway, administer a dose of IV antibiotics, and obtain an emergent ENT (ear, nose, and throat) consult
C. Administer a dose of IV antibiotics and obtain a CT scan of the soft tissues of the neck.
D. Administer a dose of IV antibiotics, obtain a CT scan of the soft tissues of the neck, and obtain an emergent ENT consult.
96. A 67-year-old woman with a history of steroid-dependent COPD, non–insulin-dependent diabetes, and hypertension presents to the ED with complaints of a painful, red, swollen left lower leg. She states she noted a “bug bite” in that area 1 week ago and since then has had gradually increasing symptoms. On examination, you note a 12 cm × 10 cm sharply demarcated area of blanching erythema, warmth, and tenderness on the medial thigh with ascending erythema to the groin. You also note tender adenopathy in the left inguinal region. Her BP is 90/55 mm Hg, RR is 24 breaths per minute, HR is 105 beats per minute, temperature is 102.4°F, and pulse oxygenation is 98% on room air. Laboratory results reveal WBC 19,500/μL, hematocrit 39%, platelets 175/μL, sodium 132 mEq/L, potassium 3.5 mEq/L, chloride 100 mEq/L, bicarbonate 14 mEq/L, BUN 32 mg/dL, creatinine 1.7 mg/dL, and glucose 455 mg/dL
A. She has systemic inflammatory response syndrome (SIRS).
B. She has sepsis.
C. She has severe sepsis.
D. She is in septic shock.
E. She has multiple organ dysfunction syndrome (MODS).
97. An 84-year-old man presents to the ED with his family due to concerns that his condition is worsening despite being placed on levofloxacin for a urinary tract infection 5 days ago by his primary care physician. His is obtunded and unable to give any additional history. Physical examination does not reveal the source of infection. His BP is 84/45 mm Hg, HR is 135 beats per minute, temperature is 102.8°F, and his RR is 28 breaths per minute. Laboratory results reveal WBC 24,500/μL, hematocrit 19%, platelets 90/μL, sodium 132 mEq/L, potassium 7.5 mEq/L, chloride 100 mEq/L, bicarbonate 12 mEq/L, BUN 37 mg/dL, creatinine 6.5 mg/dL, and glucose 255 mg/dL. Serum lactate is 11.3 mmol/dL. Cardiac enzymes and troponin are mildly elevated, and he has hyperacute T-waves on electrocardiogram (ECG). His chest radiograph shows cardiomegaly with bilateral patchy opacities and pulmonary vascular congestion. Rapid urinalysis reveals 3+ WBCs and blood and nitrates. You secure his airway with intubation, initiate broad-spectrum antibiotics, IV fluids, and other supportive therapies, and emergently consult nephrology, cardiology, and pulmonology. Which of the following best describes his clinical state?
A. He has SIRS.
B. He has sepsis.
C. He has severe sepsis.
D. He is in septic shock.
E. He has MODS.
98. A 37-year-old man presents to the ED with complaints of 2 days of a sore throat and subjective fever at home. He denies cough or vomiting. His BP is 130/75 mm Hg, HR is 85 beats per minute, temperature is 101°F, and his RR is 14 breaths per minute. He has diffuse tonsillar swelling and bilateral exudates with bilaterally enlarged and tender lymph nodes of the neck. Which of the following is the next best step in management?
A. Administer penicillin and discharge the patient without further testing.
. Perform a rapid antigen test. If it is negative, confirm with a throat culture, and administer penicillin if the results are positive.
C. Perform a rapid antigen test. If it is negative, administer penicillin and discharge the patient.
D. Perform a rapid antigen test. If it is positive, administer penicillin and discharge the patient.
E. Discharge the patient without treatment or further testing.
1. A 40-year-old man is brought to the emergency room after his wife found him alone in a confused state. He admits to overdosing in a suicide attempt, but does not specify the drug taken. En route to the hospital, he is drowsy and ataxic with blurred vision. His past medical history is significant for asthma, insomnia, depression, and substance abuse. His temperature is 38.3C (100F), blood pressure is 130/80mm Hg, pulse is 100/min, and respirations are 22/min. Examination shows dry mucus membranes and skin; pupils are 8mm bilaterally. There is no neck stiffness. Lungs are clear to auscultation. Heart sounds are within normal limits. Abdominal examination shows reduced bowel sounds with no tenderness. A Foley catheter is placed in the ER and 600 ml of urine is collected over one hour. Which of the following is the most likely diagnosis?
A. Salicylate intoxication
B. Serotonin syndrome
C. Cocaine intoxication
D. Diphenhydramine poisoning
E. Phencyclidine poisoning
2. A 46-year-old male is admitted to the hospital because of right hand cellulitis. He has a history of intravenous drug use, hepatitis C infection and septic arthritis of the knee. He smokes one pack of cigarettes and drinks one pint of vodka daily. He is started on vancomycin. On the following day, the swelling and redness of his arm decreases. However, he complains of bugs crawling on his skin. His temperature is 38.3C (100.9 F), blood pressure is 160/90 mm Hg, pulse is 110/min, and respirations are 18/min. Examination shows mild hand tremors and diaphoresis Which of the following is the most appropriate next step in management?
A. Start chlordiazepoxide
B. Give haloperidol
C. Start propranolol
D. Stop vancomycin
E. Start methadone
3. A 35-year-old woman is brought to the emergency room after an apparent suicide attempt. Her current prescription of imipramine was found at her bedside along with a suicide note. En route to the hospital, she suffered a seizure. She has been treated with many different anti-depressants over the past several years without improvement. Her temperature is 38.3C (101F), blood pressure is 90/50 mm Hg, pulse is 120/min and respirations are 24/min. EKG shows QRS widening (0.18sec). She is given sodium bicarbonate along with supportive treatment. Which of the following is the most likely mechanism that explains the beneficial effects of sodium bicarbonate?
A. Alkalinization of urine will promote diuresis of the antidepressants
B. Acidification of urine will promote diuresis of the antidepressants
C. Sodium load of sodium bicarbonate will alleviate depressant action on sodium channels
D. Sodium load of sodium bicarbonate will alleviate depressant action on potassium channels
E. Sodium load of sodium bicarbonate will alleviate depressant action on calcium channels
4. A 32-year-old male is admitted to the hospital because of confusion. He was recently diagnosed with schizophrenia His temperature is 38.6C (101.6F), blood pressure is 160/100 mm Hg, pulse is 116/min, and respirations are 22/min. He is not oriented to time, place or person. Mucus membranes are dry. Profuse diaphoresis is present. Lungs are clear to auscultation. Abdominal, neck and extremity muscles are rigid. Muscle tone is increased. Deep tendon reflexes are 2+. Laboratory studies show a serum CK of 50,000 IU/L. CSF fluid analysis shows a total white blood cell count of 5/microL. Which of the following is the most appropriate next step in management?
A. Risperidone
B. Dantrolene
C. L-Dopa
D. Prednisone
E. Antibiotics
5. A 38-year-old homeless man is brought to the emergency room. He is obtunded and unable to speak. No previous medical history is known. His temperature is 34.0C (93.2F), blood pressure is 90/60 mm Hg, pulse is 60/min and respirations are 6/min. Oxygen saturation is 86% on room air. Pupils are 5 mm in size, bilaterally. Oropharynx is dry. Lungs are clear to auscultation. Abdomen is soft; bowel sounds are decreased; there is no organomegaly. Extremities reveal several needle marks. Babinski sign is negative. Deep tendon reflexes are 2+ throughout. Which of the following is the most appropriate next step in management?
A. CT scan of the head
B. Glucagon
D. Naloxone
C. Methadone
E. Flumazenil
6. A mother brings her 16-year-old daughter to the ER after she had two episodes of coffee ground emesis. The mother reports that for the past two weeks, the teen has not been acting like herself; she has been especially isolated and has had a poor appetite and poor sleep. Her medical history is significant for anemia, for which she takes iron sulfate and folic acid. She also takes acetaminophen for occasional back pain. Presently, the patient's blood pressure is 110/70 mmHg and heart rate is 120/min. Which of the following is most likely to establish the diagnosis?
A. Liver function tests
B. Upper Gl endoscopy
D. CT scan of the head
C. Serum iron level
E. Serum acetaminophen level
7. A 47-year-old man is brought to the ED by EMS after being found wandering in the street mumbling. His BP is 150/75 mm Hg, HR is 110 beats per minute, temperature is 100.5°F, RR is 16 breaths per minute, oxygen saturation is 99% on room air, and fingerstick glucose is 98 mg/dL. On examination, the patient is confused with mumbling speech. His pupils are dilated and face is flushed. His mucous membranes and skin are dry. Which of the following toxic syndromes is this patient exhibiting?
A. Sympathomimetic syndrome
B. Anticholinergic syndrome
C. Cholinergic syndrome
D. Opioid syndrome
E. Ethanol syndrome
8. A 25-year-old man is carried into the ED by two of his friends who state that he is not breathing. The patient has a history of heroin abuse. His vital signs are BP 115/70 mm Hg, HR 99 beats per minute, temperature 98.9°F, RR 3 breaths per minute, and oxygen saturation 87% on room air. You notice fresh needle marks and miotic pupils. You begin bag-valve mask ventilation and his oxygen saturation increases to 99%. Which of the following is the most appropriate next step in management?
A. Continue bag-valve-mask ventilation until he breathes on his own.
B. Perform endotracheal intubation of the patient.
C. Evaluate response to administration of naloxone.
D. Put the patient on supplemental oxygen.
E. Place a nasogastric tube and administer activated charcoal.
9. A 42-year-old man who is actively seizing is brought to the ED by EMS after a massive ingestion of an unknown substance. The man is known to have a history of acquired immunodeficiency syndrome (AIDS). An intravenous (IV) line is established and anticonvulsant therapy is administered. After high doses of diazepam, phenobarbital, and phenytoin, it is determined that the seizures are refractory to standard anticonvulsant therapy. Which of the following substances did this patient most likely ingest?
A. Cocaine
B. Diphenhydramine
C. Tricyclic antidepressant (TCA)
D. Haloperidol
E. Isoniazid (INH)
10. A 26-year-old man is brought to the emergency room by police with depressed mental status. Out of fear of arrest, he swallowed a handful of pills as the police officers approached him. On examination, he responds to painful stimuli but is somnolent. His respiratory rate is 8/min and after naloxone bolus infusion increases to 12/min. Lungs are clear to auscultation. Which of the following additional findings is most likely to be present in this patient?
A. Miosis, bradycardia, hypertension
B. Miosis, tachycardia, hypotension
D. Miosis, tachycardia, hypertension
C. Miosis, bradycardia, hypotension
E. Mydriasis, tachycardia, hypertension
11. A 29-year-old male is brought to the emergency room because of sudden onset confusion and fever. He was recently admitted to the hospital for hallucinations and was discharged in stable condition. His temperature is 38.6C (101.6 F), blood pressure is 150/100 mm Hg, pulse is 112/min, and respirations are 24/min. Mucus membranes are dry. Profuse diaphoresis is present. Lungs are clear to auscultation. Abdominal muscles are rigid. Muscle tone is increased; "lead pipe rigidity" is noted in all four extremities. Deep tendn reflexes are 2+. Tremor is noted. Which of the following is the most likely diagnosis?
A. Tetanus
B. Meningitis
D. Cocaine intoxication
C. Drug induced idiosyncratic reaction
E. Lithium intoxication
12. A 26-year-old man is brought to the emergency room after an attempted suicide by medication overdose. For the past hour, he has suffered two seizures. His temperature is 38.8C (102F), blood pressure is 110/85 mmHg, pulse is 90/min, and respirations are 22/min. He is not oriented to time, place, and person. Pupils are dilated, but reactive to light and accommodation; skin is flushed and dry. Abdominal examination shows reduced bowel sounds. EKG shows prolonged QRS complexes (0.19 sec). Toxicology studies are pending. Which of the following is the most appropriate indicator of severity of intoxication?
A. Serum drug levels
B. Urine drug levels
D. Pupillary size
C. Duration of QRS complex
E. Bowel sounds
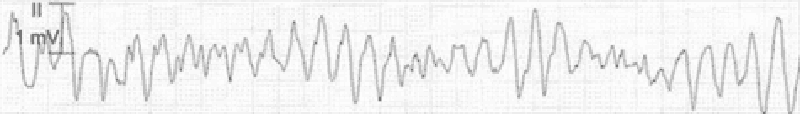
13. A 42-year-old male is admitted to the hospital with fever and shortness of breath. He has HIV infection, hepatitis C infection, and alcohol induced cardiomyopathy. His temperature is 38.6 C (101.5 F). Thrush is noted in the oropharynx. Chest x-ray reveals right lower lobe consolidation. He is started on fluconazole and moxifloxacin. His pneumonia and thrush improve over the next 2 days. However, on the third day, he develops palpitations. His EKG strip is shown below:Which of the following is the most appropriate next step in management?
A. Calcium gluconate
B. Magnesium sulphate
C. Sotalol
D. Amiodarone
E. Adenosine
14. A 34-year-old homeless man is brought to the emergency room in a confused state. He complains of epigastric pain, vomiting and blurred vision. His temperature is 36.8C (98.2F), blood pressure is 110/60 mm Hg, pulse is 110/min and respirations are 22/min. Physical examination shows poor oral hygiene and dry mucous membranes. Lungs are clear to auscultation. Abdominal exam shows mild epigastric discomfort. Funduscopic examination reveals optic disc hyperemia. Laboratory studies show: Serum sodium 136 mEq/L Serum potassium 3.0 mEq/L Chloride 93 mEq/L Bicarbonate 6 mEq/L Blood urea nitrogen (BUN) 30 mg/dL Serum creatinine 0.8 mg/dL Blood glucose 80 mg/dL Serum ketones negative Plasma lactate 2.2 mEq/L Which of the following is the most likely cause of his symptoms?
A. Ethylene glycol poisoning
B. Mesenteric ischemia
C. Septic shock
D. Diabetic ketoacidosis
E. Methanol poisoning
15. You receive notification from EMS that they are bringing in a 17-yearold adolescent boy who was found unconscious by a police officer. The police officer at the scene states that he snuck up on a group of kids that he thought were using drugs. Two of them got away and one just fell to the ground seconds after standing up. Lying on the ground next to the adolescent were plastic bags. The emergency medical technician (EMT) states that the patient was in ventricular fibrillation. He was shocked in the field and is now in a sinus rhythm. The EMT also administered IV dextrose, thiamine, and naloxone without any change in mental status. Which of the following substances was the patient most likely abusing?
A. Butane
B. Ethanol
D. Cocaine
C. Heroin
E. PCP
16. A 61-year-old man with a history of depression and hypertension is brought to the ED by EMS for altered mental status. The patient’s wife states that he stopped taking his fluoxetine 1 month ago and now only takes metoprolol for his hypertension. The patient’s BP is 75/40 mm Hg, HR is 39 beats per minute, RR is 14 breaths per minute, oxygen saturation is 99% on 100% oxygen, and fingerstick glucose is 61 mg/dL. The patient is awake and moaning, responding only to deep stimuli. His extremities are cool to the touch. You suspect an overdose of metoprolol. You endotracheally intubate the patient for airway control. Which of the following is the most appropriate next step in management?
A. Normal saline bolus, administer atropine, administer 1-g calcium gluconate bolus, then insert a transvenous cardiac pacer
B. Put the patient on pacer pads, then administer norepinephrine drip
C. Cardioversion with 200 J, then administer atropine
D. Normal saline bolus, atropine, norepinephrine
E. Normal saline bolus, atropine, glucagon
17. A 22-year-old woman presents to the ED by ambulance from a dance club. The paramedics report that the patient was agitated in the club and had a generalized seizure. Her BP is 165/100 mm Hg, HR is 119 beats per minute, temperature is 101.9 °F, RR is 17 breaths per minute, oxygen saturation is 98% on room air, and fingerstick glucose is 92 mg/dL. On examination, the patient is hyperactive and appears to be hallucinating. Her pupils are dilated to 6 mm bilaterally and reactive. Her neck is supple. Examination of the heart is unremarkable except for tachycardia. Her lungs are clear and abdomen is soft and nontender. The patient moves all four extremities. Laboratory results are as follows: Sodium 109 mEq/L WBC 12,000/mm 3 Potassium 3.5 mEq/L Hct 49% Chloride 83 mEq/L Platelets 350/μL Bicarbonate 20 mEq/L BUN 10 mg/dL Creatinine 1 mg/dL Glucose 103 mg/dL Which of the following substances did this patient most likely consume?
A. Cocaine
B. Heroin
D. Ketamine (special K)
C. 3,4-Methylenedioxymethamphetamine (MDMA)
E. PCP
18. A 32-year-old woman is brought to the emergency department by her husband because of slurred speech and difficulty walking. She has also been very drowsy for the past several hours, a non-typical behavior for a very active woman. She has a history of bipolar disorder, insomnia, migraine headaches, seizures and hypothyroidism. Her temperature is 37(98.6F), blood pressure is 110/70 mm Hg, pulse is 76/min, and respirations are 16/min. She is lethargic and falls asleep during the interview and physical examination. Pupils are 5 mm in size and reactive to light. Neck is supple. Oropharynx is clear. Chest auscultation is unremarkable. Abdomen is soft and non-tender; bowel sounds are normal. Limited neurologic examination shows 1+ deep tendon reflexes in all four extremities; there is no Babinski sign; strength is 5/5 throughout. There is no nystagmus or hand tremor. Blood sugar is 130 mg/dl. Which of the following is the most likely cause of her symptoms?
A. Cerebrovascular accident
B. Phenytoin toxicity
C. Benzodiazepine overdose
D. Ethanol intoxication
E. Lithium toxicity
19. A 31-year-old woman with a known psychiatric history presents to the ED after ingesting an unknown quantity of pills from her medication vial. In the ED, she complains of nausea, abdominal cramping, and feels unsteady on her feet. On physical examination, you observe that she is tachycardic and ataxic. Which of the following substances will best be treated by activated charcoal that could present like this?
A. Phenobarbital
B. Carbamazepine
C. Lye (sodium hydroxide)
D. Lithium
E. Acetaminophen
20. A 27-year-old man presents to the ED extremely agitated complaining of mild chest pain and dyspnea. He states that he was snorting cocaine all afternoon. You place him on a monitor and get his vital signs. His BP is 215/130 mm Hg, HR is 112 beats per minute, temperature is 100.1°F, RR is 17 breaths per minute, and oxygen saturation is 98% on room air. An ECG reveals sinus tachycardia at a rate of 116. Which of the following is the most appropriate medication to administer?
A. Haloperidol
B. Labetalol
C. Esmolol
D. Diltiazem
E. Diazepam
21. A 30-year-old man is brought to the ED by police officers. The patient is agitated, vomiting, and complaining of body aches. He states that he is withdrawing from his medication. His vital signs are BP 160/85 mm Hg, RR 20 breaths per minute, HR 107 beats per minute, and temperature 99.7°F. On examination he is diaphoretic, has rhinorrhea, piloerection, and hyperactive bowel sounds. Which of the following substances is this patient most likely withdrawing from?
A. Ethanol
B. Cocaine
C. Nicotine
D. Methadone
E. Clonidine
22. A 25-year-old man is brought into the ED by two police officers because of suspected drug use. The patient is extremely agitated and is fighting the police officers. It takes three hospital staff members and the two police officers to keep him on the stretcher. His vital signs are BP 150/80 mm Hg, HR 107 beats per minute, temperature 99.7°F, RR 18 breaths per minute, and oxygen saturation 99% on room air. Physical examination is unremarkable except for cool, diaphoretic skin, persistent vertical and horizontal nystagmus, and occasional myoclonic jerks. Which of the following is the most likely diagnosis?
A. Cocaine intoxication
B. Cocaine withdrawal
D. PCP intoxication
C. Anticholinergic toxidrome
E. Opiate withdrawal
23. A 20-year-old female is brought to the emergency room after getting struck by a motor vehicle. She appears confused. According to her parents, she has no other medical problems and does not take any prescription medications. However, they have noticed her increase in appetite recently. She occasionally drinks alcohol and smokes half a pack of cigarettes daily. Her temperature is 37.2C (99F), blood pressure is 150/90mm Hg, pulse is 110/min, and respirations are 22/min. Examination reveals dry mouth and conjunctival injection. Pupils are equal, reactive to light and accommodation. She has impaired time orientation and shortterm memory. Which of the following is the most likely explanation for this patient's symptoms?
A. Benzodiazepine overdose
B. Opioid overdose
D. Alcohol intoxication
C. Cocaine intoxication
E. Marijuana overdose
24. A 34-year-old male is brought to the emergency department by his neighbor. The neighbor found the man lying on the floor beside an empty bottle of unknown substance. At the hospital, the patient is conscious and alert, but in severe pain. His temperature is 36.8C (98.2F), blood pressure is 130/70 mm Hg, pulse is 90/min and respirations are 20/min. Abdomen is benign, with normal bowel sounds. Pupils are 5 mm, bilaterally. His tongue is white, heavy drooling of saliva is noted and he is unable to swallow. Which of the following is the most likely explanation for this patient's symptoms?
A. Anticholinergic poisoning
B. Caustic poisoning
C. Tricyclic antidepressant poisoning
D. Cyanide poisoning
E. Alcohol intoxication
25. A 35-year-old woman calls her family physician after her 7-year old son accidentally splashed an unknown liquid containing acid on his face. Some liquid likely entered his eye, as the child is complaining of severe pain in his right eye. She knows a doctor living in her immediate neighborhood but is hesitant about what to do next. Which of the following is the most appropriate initial course of action that the mother should take?
A Call 911 immediately
B. Go to local emergency room immediately
C. Go to the doctor in the neighborhood immediately
D. Wash the eye with copious amount of water
E. Do not try to wash the eye as it can enhance the damage
26. A worried and anxious pregnant mother brings her 3-year-old son to the emergency room after he experienced several episodes of vomiting and abdominal pain for the past two hours. His vomit is coffee ground in appearance. He is irritable and lethargic. His blood pressure is 80/50mmHg and pulse rate is 120/min. Examination shows a normal oropharynx; chest auscultation is within normal limits. Abdomen is soft and mildly tender at the epigastrium; there is no hepatosplenomegaly. Extremities are cold to touch. Initial laboratory studies show: Hemoglobin 10.3 g/L Leukocyte count 14,500/mm3 Bicarbonate 18 mEq/L Chest x-ray is within normal limits. Abdominal imaging shows radio opaque tablets in the stomach. Intravenous normal saline is started. Which of the following is the most appropriate next step in management?
A. Sodium bicarbonate
B. Deferoxamine
D. Hemodialysis
C. Magnesium sulphate
E. Calcium EDTA
27. A 32-year-old male comes to the hospital complaining of pain, swelling and redness of his right arm. His past medical history is significant for substance abuse. His temperature is 38.9 C (102.0 F), blood pressure is 110/60 mm Hg, pulse is 110/min and respirations are 14/min. He is started on intravenous clindamycin. The next day the swelling and pain improve, but he develops nausea, vomiting, abdominal cramps and diarrhea. He is restless and asks for pain medication to treat his aching muscles and joints. His temperature now is 37.3C (99.1F), blood pressure is 120/70 mm Hg, pulse is 80/min and respirations are 16/min. His laboratory studies at the time of admission and the following day show: Hemoglobin Leukocyte count NeutrophiIs Lymphocytes 13.0 g/L 17,500/ mm3 86% 14% 12.8 g/L 8,500/ mm3 64% 26% Which of the following is the most appropriate next step in management?
A Stool for Clostridium difficile toxin
B. Discontinue clindamycin
C. Start chlordiazepoxide
D. Start methadone
E. Start intravenous morphine
28. A 34-year-old homeless male is brought to the ER in a confused state. He complains of flank pain. His past medical history is unknown. His temperature is 36.8C (98.2F), blood pressure is 110/60 mm Hg, pulse is 110/min and respirations are 22/min. His appearance is disheveled. Pupils are equal, 4 mm in size and reactive to light. Funduscopic examination is within normal limits. Lungs have crackles at both bases. Mild costovertebral angle tenderness is present. Foley catheter is placed and urine appears red. Laboratory studies show: Serum sodium 136 mEq/L Serum potassium 3.5 mEq/L Chloride 93 mEq/L Bicarbonate 6 mEq/L Blood urea nitrogen (BUN) 34 mg/dl Serum creatinine 2.8 mg/dl Blood glucose 80 mg/dl Calcium 6.5 mg/dl Serum ketones negative Plasma lactate 2.4 mEq/L Which of the following is the most appropriate next step in management?
A. Broad spectrum antibiotics
B. Fomepizole
C. N-acetylcysteine
D. Regular insulin
E. Glucagon
29. A 26-year-old bar employee is brought to the emergency room because of agitated, combative behavior in which three people had to restrain her. She has also been hallucinating during this entire period. Her temperature is 37.7C (100F), blood pressure is 160/90 mm Hg, pulse is 126/min, and respirations are 18/min. She is confused and agitated during the examination. Pupils are 6 mm in diameter and respond to light; prominent nystagmus is present. The remainder of her examination is unremarkable. Which of the following is the most likely diagnosis?
A. Barbiturate intoxication
B. Phencyclidine intoxication
C. Cocaine intoxication
D. Marijuana Intoxication
E. Opioid intoxication
30. A 38-year-old man is brought to the emergency room by EMS after an apparent suicide attempt. En route to the hospital, he appeared confused and suffered a seizure. He has a history of hypertension and major depression. His temperature is 37.7C (100F), blood pressure is 70/40 mm Hg, pulse is 40/min, and respirations are 12/min. Examination shows normal heart sounds and diffuse wheezing. Extremities are cold and clammy. EKG shows AV block. The patient is given intravenous fluids and atropine; however, his bradycardia and hypotension do not improve. Which of the following is the most appropriate next step in management?
A. Epinephrine
B. Aminophylline
C. Digoxin specific antibody
D. Glucagon
E. Pacemaker
31. A 24-year-old woman is brought to the emergency room after ingesting 14 acetaminophen tablets, 500 mg each, two hours ago. She does not smoke but drinks alcohol on the weekends. She is alert and oriented. Her temperature is 37.2C (99F), blood pressure is 110/60mm Hg, pulse is 90/min and respirations are 18/min. Examination shows no abnormalities. Laboratory studies show: Hct 40% WBC 6,000/mm3 Platelet 390,000/mm3 Which of the following is the most appropriate next step in management?
A. Administer the loading dose of N-acetylcysteine
B. Obtain serum acetaminophen levels in two hours
C. Obtain serum acetaminophen levels now
D. Transfer to liver transplantation facility
E. Discharge her home without further work up
32. A group of teenagers attend an indoor barbecue on a cold winter night. They all ate servings of potato salad and barbecue chicken. A few hours later, they present to the local emergency room with headache, nausea, vomiting, vague abdominal discomfort and confusion. One of the teenagers mentions a pet dog that was in the room with them had similar symptoms. A quick physical examination of one patient reveals tachycardia, tachypnea and a pinkish-skin hue. Which of the following is the most likely diagnosis?
A. Viral illness
B. Carbon monoxide poisoning
C. Acute gastroenteritis
D. Cyanide poisoning
E. Methemoglobinemia
33. A 40-year-old man is brought to the emergency room for retrosternal and epigastric pain after ingesting an unknown amount of "lye" (drain cleaner) 45 minutes ago. His past medical history is significant for major depression and suicide attempt. He is unable to swallow his saliva and is drooling. His temperature is 36.8C (98.2F), blood pressure is 120/70mm Hg, pulse is 110/min, and respirations are 20/min. Examination shows oropharyngeal erythema and edema. Lungs are clear to auscultation. Abdominal examination reveals tenderness at the epigastrium without rebound or guarding. Chest x-ray shows no abnormalities. Intravenous hydration is started. Which of the following is the most appropriate next step in treatment?
A. Gastric decontamination with ipecac
B. Administer activated charcoal in water
C. Neutralization and dilution of the alkali
D. Upper gastrointestinal contrast studies and endoscopy
E. Administer high dose systemic steroids
34. A 34-year-old farmer is brought to the hospital after attempting suicide. His body and clothes are soiled with vomitus. He is short of breath and appears agitated. His family reports no previous medical history or regular use of prescription medications. His temperature is 36.6C (98F), blood pressure is 110/60 mm Hg, pulse is 50/min, and respirations are 22/min. His oxygen saturation is 86% on room air. Examination shows watering of the eyes and 1 mm pupils, bilaterally. Lung examination shows widespread rhonchi with prolonged expiration. Abdominal examination shows increased bowel sounds. Neurologic examination shows muscle fasciculations. What would be the most appropriate next step in management of this patient?
A. Obtain EKG for QRS duration
B. Remove all the clothing and wash the body
C. Obtain a chest x-ray
D. Obtain a head CT scan
E. Give physostigmine
35. A 60-year-old male is found lying down on the street by police one winter morning. He has been taking ibuprofen for headaches, fluphenazine for his schizophrenia and amitriptyline for chronic painful neuropathy secondary to postherpetic neuralgia. He is also receiving cephalexin for cellulitis of the right lower leg. His temperature is 34C (90F), blood pressure is 80/50 mm Hg, pulse is 88/min, and respirations are 12/min. Which of the following medications most likely have contributed to the development of hypothermia in this patient?
A. Ibuprofen
B. Amitriptyline
C. Cephalexin
D. Fluphenazine
E. Glucagon
36. A 45-year-old woman is brought to the ER by ambulance after a neighbor found her to be in a somewhat obtunded state with an empty bottle of medication next to her. While en route to the ER she suffered a tonic clonic seizure. Her past medical history is significant for major depression. Her temperature is 38.3C (100.9F), blood pressure is 90/70 mm Hg, pulse is 120/min, and respirations are 16/min. She is able to respond to painful stimuli. Pupils are 8 mm in size bilaterally. Skin is warm and flushed. Lungs are clear to auscultation. Abdomen is soft and non-tender. Bowel sounds are decreased. There is no neck stiffness. EKG shows QRS duration of 130 msec, a change from her previous EKG a month ago. Which of the following is the most appropriate next step in management?
A. Lumbar puncture
B. Echocardiogram
C. Thyroid function tests
D. Calcium gluconate
E. Sodium bicarbonate
37. After being fired from his job, a 35-year-old man attempts suicide by drinking from a bottle labeled “insecticide.” Three hours later, emergency medical services (EMS) brings him into the emergency department (ED) and you notice that he is extremely diaphoretic, drooling, and vomiting. He is awake but confused. His vital signs include a blood pressure (BP) of 170/90 mm Hg, heart rate (HR) of 55 beats per minute, respiratory rate (RR) of 22 breaths per minute, temperature of 98.6°F, and oxygen saturation of 95% on room air. Physical examination demonstrates pinpoint pupils and crackles and wheezing on lung examination. What is the treatment to reverse this patient’s poisoning?
A. Naloxone
B. N-acetylcysteine (NAC)
C. Atropine and pralidoxime (2-PAM)
D. Flumazenil
E. Physostigmine
38. A 19-year-old man is brought to the ED by EMS after he was found lying on the floor at a dance club. EMS states that the patient seemed unconscious at the dance club, but as soon as they transferred him onto the gurney, he became combative. Upon arrival in the ED, his BP is 120/65 mm Hg, HR is 75 beats per minute, temperature is 98.9°F, RR is 12 breaths per minute, and oxygen saturation is 98% on room air. On physical examination, his pupils are midsized, equal, and reactive to light. His skin is warm and dry. Lung, cardiac, and abdominal examinations are unremarkable. As you walk away from the bedside, you hear the monitor alarm signaling zero respirations and the oxygen saturation starts to drop. You perform a sternal rub and the patient sits up in bed and starts yelling at you. As you leave him for the second time, you hear the monitor alarm again signal zero respirations. You administer naloxone, but there is no change in his condition. Which of the following is most likely the substance ingested by this patient?
A. γ-Hydroxybutyrate (GHB)
B. Diazepam
C. Cocaine
D. Phencyclidine (PCP)
E. Heroin
39. A 43-year-old woman presents to the ED with a 3-week history of intermittent headache, nausea, and fatigue. She was seen at her private doctor’s office 1 week ago along with her husband and children, who also have similar symptoms. They were diagnosed with a viral syndrome and told to increase their fluid intake. She states that the symptoms began approximately when it started to get cold outside. The symptoms are worse in the morning and improve while she is at work. Her BP is 123/75 mm Hg, HR is 83 beats per minute, temperature is 98.9°F, and oxygen saturation is 98% on room air. Physical examination is unremarkable. You suspect her first diagnosis was incorrect. Which of the following is the most appropriate next step to confirm your suspicion?
A. Order a mono spot test.
B. Perform a nasal pharyngeal swab to test for influenza.
C. Consult psychiatry to evaluate for malingering.
D. Order a carboxyhemoglobin (COHb) level.
E. Order a lead level.
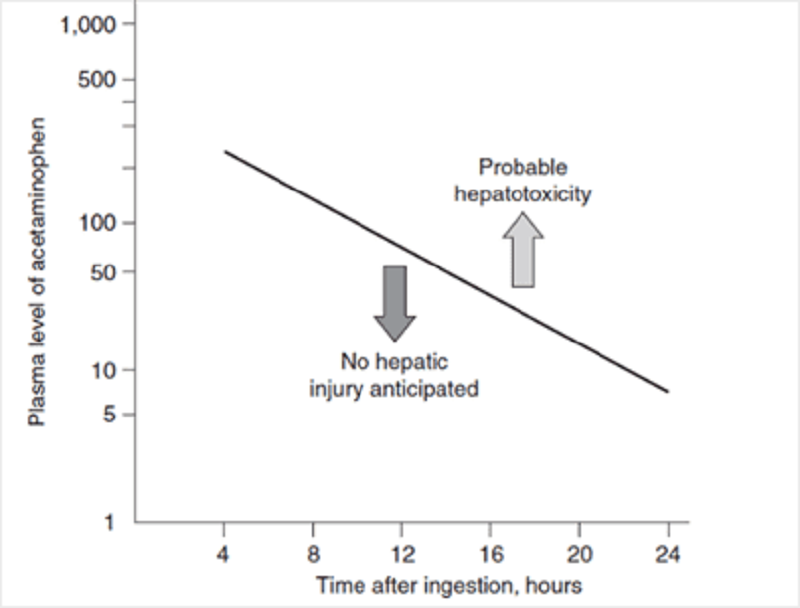
40. An 18-year-old woman is brought to the ED by her mother. The patient is diaphoretic and vomiting. Her mom states that she thinks her daughter tried to commit suicide. The patient admits to ingesting a few handfuls of acetaminophen (Tylenol) approximately 3 hours ago. Her temperature is 99.1°F, BP is 105/70 mm Hg, HR is 92 beats per minute,RR is 17 breaths per minute, and oxygen saturation is 99% on room air. On examination, her head and neck are unremarkable. Cardiovascular and pulmonary examinations are within normal limits. She is mildly tender in her right upper quadrant, but there is no rebound or guarding. Bowel sounds are normoactive. She is alert and oriented and has no focal deficits on neurologic examination. You administer 50 g of activated charcoal. At this point, she appears well and has no complaints. Her serum acetaminophen (APAP) concentration 4 hours after the reported time of ingestion returns at 350 μg/mL. You plot the level on the nomogram seen below. Which of the following is the most appropriate next step in management?
A. Discharge home with instructions to return if symptoms return.
B. Observe for 6 hours and, if the patient still has no complaints, discharge her home.
C. Repeat the acetaminophen level 4 hours after the patient arrived in the ED. Treat only if this level is above the line.
D. Admit to the psychiatry unit and keep on suicide watch while performing serial abdominal examinations.
E. Begin NAC and admit to the hospital.
41. A 60-year-old woman with a history of diabetes is brought into the ED by EMS workers who state that the patient was found on a bus in a lethargic and diaphoretic condition. Her fingerstick glucose level at the scene was 35 mg/dL. EMS workers quickly administered dextrose through an IV line. The patient became alert and responsive, stating that she just took her normal medication. Her blood sugar went up to 110 mg/dL and she remained this way throughout her trip to the ED. However, in the ED you notice that the patient is again diaphoretic and is mumbling her speech. Her fingerstick glucose is now 47 mg/dL. You administer dextrose and she perks right up. Which of the following diabetes medications commonly causes hypoglycemia for which the patient is likely to require hospital admission?
A. Regular insulin
B. Metformin
C. Glyburide
D. Sitagliptin
E. Acarbose
42. A 23-year-old woman presents to the ED complaining of abdominal pain, nausea, and vomiting. She has a history of depression but is not currently taking any antidepressant medications. Upon further questioning, the patient states that she ingested a bottle of pills in her medicine cabinet approximately 3 hours ago. Her BP is 115/65 mm Hg, HR is 101 beats per minute, temperature is 100.1°F, RR is 29 breaths per minute, and oxygen saturation is 100% on room air. Physical examination is unremarkable except for mild diffuse abdominal tenderness. Laboratory results reveal a white blood cell (WBC) count of 10,300/μL, hematocrit 46%, platelets 275/μL, aspartate transaminase (AST) 70 U/L, alanine transaminase (ALT) 85 U/L, alkaline phosphatase 75 U/L, sodium 143 mEq/L, potassium 3.7 mEq/L, chloride 98 mEq/L, bicarbonate 8 mEq/L, blood urea nitrogen (BUN) 22 mg/dL, creatinine 0.9 mg/dL, and glucose 85 mg/dL. Arterial blood gas values on room air are pH 7.51, PCO2 11 mm Hg, and PO2 134 mm Hg. Which of the following substances did this patient most likely ingest?
A. Diphenhydramine
B. Ibuprofen
C. Acetaminophen
D. Aspirin
E. Pseudoephedrine
43. A 35-year-old agitated man presents to the ED in police custody. He denies any past medical history and takes no medication. He admits to using some drugs today. His BP is 195/90 mm Hg, HR is 121 beats per minute, temperature is 100.1°F, RR is 18 breaths per minute, and oxygen saturation is 99% on room air. On examination, he is diaphoretic, and has pupils that are 8 mm in diameter, along with 3+ patella reflexes bilaterally. Electrocardiogram (ECG) reveals sinus tachycardia with a rate of 123. Which of the following toxic syndromes is this patient exhibiting?
A. Anticholinergic
B. Cholinergic
C. Sympathomimetic
D. Opioid
E. Sedative hypnotic
44. An undomiciled 49-year-old man presents to the ED with altered mental status. His BP is 149/75 mm Hg, HR is 93 beats per minute, temperature is 97.5 °F, RR is 18 breaths per minute, and O 2 saturation is 99% on room air. Physical examination reveals an unkempt man with the odor of “alcohol” on his breath. His head is atraumatic and pupils are 4 mm, equal, and reactive. The neck is supple. Cardiovascular, pulmonary, and abdominal examinations are unremarkable. There is no extremity edema and his pulses are 2+ and symmetric. Neurologically, he withdraws all four extremities to deep stimuli. ECG is sinus rhythm. Laboratory results reveal: Sodium 141 mEq/L Potassium 3.5 mEq/L Chloride 101 mEq/L Bicarbonate 14 mEq/L BUN 15 mg/dL Creatinine 0.7 mg/dL Glucose 89 mg/dL Arterial blood pH 7.26 Lactate 1.7 mEq/L Ethanol level undetectable Measured serum osmolarity 352 mOsm/L Calculated serum osmolarity 292 mOsm/kg Urinalysis: no blood, ketones, or protein Which of the following statements best describes the laboratory findings?
A. Anion gap metabolic acidosis and osmol gap
B. Anion gap metabolic acidosis without osmol gap
C. Nonanion gap metabolic acidosis and osmol gap
D. Nonanion gap metabolic acidosis without osmol gap
E. Metabolic alkalosis with secondary acidosis
45. A 26-year-old woman with a history of depression is brought into the ED. She was found lying on the floor of her apartment next to an unlabeled empty pill bottle. Her HR is 117 beats per minute, BP is 95/65 mm Hg, RR is 14 breaths per minute, and oxygen saturation is 97% on 2-L nasal cannula. On examination, the patient appears obtunded, and her pupils are 3 mm and reactive. Her oropharynx is dry and there is no gag reflex to pharyngeal stimulation. Her neck is supple. The heart is tachycardic without murmurs, the lungs are clear to auscultation, and the abdomen is soft. There is normal rectal tone and brown stool that is heme negative. Her skin is cool and moist with no signs of needle tracks. Neurologically, she is unresponsive but withdraws all extremities to deep palpation. Fingerstick blood glucose is 85 mg/dL. Her ECG reveals sinus tachycardia at 119 with a QRS complex of 140 milliseconds and a terminal R wave in lead aVR. Which of the following is the most appropriate next step in management?
A. Orotracheal intubation, administer activated charcoal through orogastric tube, and IV naloxone
B. Orotracheal intubation, administer activated charcoal through orogastric tube, and IV sodium bicarbonate
C. Orotracheal intubation, administer activated charcoal through orogastric tube, and IV NAC
D. Orotracheal intubation, administer syrup of ipecac through orogastric tube, and IV sodium bicarbonate
E. Induce vomiting prior to intubation to lower the risk of aspiration then administer IV sodium bicarbonate
46. A 37-year-old woman is brought into the ED by her friend who states that the patient swallowed approximately 50 capsules of 325-mg acetaminophen (APAP) 6 hours ago in an attempted suicide. The patient states she feels nauseated and vomits while you take her history. Her BP is 100/75 mm Hg, HR is 97 beats per minute, temperature is 98.9°F, RR is 18 breaths per minute, and oxygen saturation is 99% on room air. Examination is unremarkable except for mild epigastric tenderness. Which of the following is the correct antidote for APAP overdose?
A. NAC
B. Physostigmine
C. Flumazenil
D. Naloxone
E. Digibind
47. A 31-year-old man is brought to the ED by EMS who state that the man was found lying on the floor of his garage. He is rousable in the ED, speaks with slurred speech, and vomits. His BP is 140/85 mm Hg, HR is 94 beats per minute, temperature is 98.8°F, RR is 17 breaths per minute, and oxygen saturation is 99% on room air. You place an IV line, draw blood, and start a liter of normal saline running through the line. Laboratory results reveal serum sodium 139 mEq/L, potassium 3.5 mEq/L, chloride 101 mEq/L, bicarbonate 14 mEq/L, BUN 15 mg/dL, creatinine 1 mg/dL, glucose 105 mg/dL, arterial blood pH 7.27, COHb 4%, and lactate 2.8 mEq/L. Urinalysis shows 1+ protein, trace ketones, WBC 4/hpf (high-power field), red blood cell (RBC) 2 to 3/hpf, and multiple envelope-shaped and needle shaped crystals. Which of the following conditions would best explain his metabolic acidosis?
A. Ibuprofen toxicity
B. Ethylene glycol poisoning
C. Diabetic ketoacidosis (DKA)
D. Lactic acidosis
E. Isopropyl alcohol poisoning
98. A 37-year-old man presents to the ED with complaints of 2 days of a sore throat and subjective fever at home. He denies cough or vomiting. His BP is 130/75 mm Hg, HR is 85 beats per minute, temperature is 101°F, and his RR is 14 breaths per minute. He has diffuse tonsillar swelling and bilateral exudates with bilaterally enlarged and tender lymph nodes of the neck. Which of the following is the next best step in management?
A. Administer penicillin and discharge the patient without further testing.
B. Perform a rapid antigen test. If it is negative, confirm with a throat culture, and administer penicillin if the results are positive.
C. Perform a rapid antigen test. If it is negative, administer penicillin and discharge the patient.
D. Perform a rapid antigen test. If it is positive, administer penicillin and discharge the patient.
E. Discharge the patient without treatment or further testing.
99. A 37-year-old man who just finished a full course of penicillin for pharyngitis presents to the ED requesting to be checked out again. He states he took the antibiotics exactly as prescribed and initially felt somewhat improved, but over the last 2 to 3 days has had increased pain and progressive difficulty swallowing. His BP is 130/65 mm Hg, HR is 95 beats per minute, temperature is 100.1°F, RR is 16 breaths per minute, and oxygen saturation is 99%. On examination, the patient is in no acute distress but has a fluctuant mass on the right side of his neck. You visualize a normal soft palate with swelling of the right tonsillar arch and deviation of the uvula to the left, but additional examination is limited because he is unable to open his mouth fully. Review of his records reveals a throat culture that was positive for Streptococcus. Which of the following is the most appropriate next step in management?
B. Give him morphine for pain control, give him a dose of IV antibiotics, and observe him in the ED for 6 hours.
a. Attempt needle aspiration, treat him with a new course of antibiotics (either penicillin or clindamycin),and have him return in 24 hours.
C. Admit him for incision and drainage in the OR under general anesthesia.
D. Switch his antibiotic to clindamycin and have him return in 24 hours.
E. Order a CT scan to visualize his neck, continue the penicillin, and have him return in 24 hours.
100. A 50-year-old man presents to the ED complaining of fever, headache, and neck pain for 24 hours. He states that 1 week ago he had rhinorrhea, nasal congestion, a sore throat, and occasional dry a. Attempt needle aspiration, treat him with a new course of antibiotics (either penicillin or clindamycin), and have him return in 24 hours. cough. He noted generalized weakness, myalgias, and malaise yesterday afternoon, and woke up today “feeling terrible.” His BP is 145/75 mm Hg, HR is 102 beats per minute, temperature is 101.2°F, and his RR is 16 breaths per minute. On examination, he is awake, alert, and nontoxic appearing although he has discomfort in his neck with flexion. He has a nonfocal neurologic examination without increased deep tendon reflexes or opthalmoplegia. There are no rashes. Which of the following CSF results is most consistent with your clinical diagnosis of viral meningitis?
A. Identification of viral particles on Gram stain with an elevated CSF-to-serum glucose level
B. A mildly elevated total protein level with a decreased glucose level
C. A mildly elevated total protein level with a WBC count of fewer than 500 cells/mm 3
D. Increased turbidity with marked xanthochromia
E. A markedly elevated lymphocyte count, often exceeding 100,000 cells/mm 3 with a mildly elevated total protein level
101. A 32-year-old woman presents to the ED with 7 days of vaginal discharge and pelvic pain. She is sexually active and admits to several recent “one night stands.” She denies trauma/injury and does not have any urinary or other abdominal complaints. Her HR is 85 beats per minute, BP is 135/90 mm Hg, RR is 18 breaths per minute, and temperature is 101.4°F. On bimanual examination, you note a copious, thin, white discharge with mild diffuse adnexal tenderness with significant cervical motion tenderness. There are no rashes, skin lesions, or adenopathy. Laboratory results are notable for a WBC of 18,000/μL. A urinalysis shows WBCs but is otherwise within normal limits. Which of the following is the most appropriate next step in management?
A. Prescribe her a 14-day course of levofloxacin (500 mg PO once per day) and urgent gynecology follow- up within 1 week.
B. Give her a dose of metronidazole (2 g PO) and prescribe her a 14-day course of cephalexin (500 mg) with urgent gynecology follow-up within 1 week.
C. Give her a one-time dose of oral metronidazole (2 g PO), azithromycin (1 g PO), and ceftriaxone (250 mg IM) with gynecology follow-up if she is not feeling better.
D. Give her a one-time dose azithromycin (1 g PO), and ceftriaxone (250 mg IM) with urgent gynecology follow-up within 1 week.
E. Give her a dose of ceftriaxone (250 mg IM), and prescribe her a 10-day course of doxycycline (100 mg PO BID) with urgent gynecology follow-up within 1 week
102. A 45-year-old woman presents to the ED complaining of 3 days of fever and worsening throat pain and painful odynophagia without cough or coryza. She sits on a chair, leaning forward with her mouth slightly open. She is refusing to swallow and has a cup of saliva and a box of facial tissues at her side. Vitals are HR of 120 beats per minute, BP of 110/70 mm Hg, RR of 22 breaths per minute, oxygen saturation of 99% on room air, and temperature of 102.8°F. You note a slight wheezing noise coming from her anterior neck. Her voice is hoarse and she is able to open her mouth fully, making her examination quite difficult. From what you can visualize, her posterior oropharynx is moderately hyperemic, without exudates or tonsillar enlargement. A soft tissue lateral cervical radiograph shows marked edema of the prevertebral soft tissues and absence of the vallecular space. Which of the following is the most likely diagnosis?
A. Retropharyngeal abscess
B. Peritonsillar abscess
C. Epiglottitis
D. Pharyngitis
E. Laryngotracheitis
103. A 19-year-old woman presents with 4 days of bilateral lower abdominal pain right greater than left. She also complains of a fever, nausea, vomiting, and general malaise. Her last menstrual period was 5 days ago. Vitals are HR 98 beats per minute, BP 110/65 mm Hg, RR 18 breaths per minute, e. Give her a dose of ceftriaxone (250 mg IM), and prescribe her a 10-day course of doxycycline (100 mg PO BID) with urgent gynecology follow-up within 1 week. And temperature of 102.7°F. Pelvic examination demonstrates exquisite cervical motion tenderness and right adnexal tenderness. Laboratory reports are notable for a WBC 15,000/μL, an ESR of 95 mm/h, and a negative urine β-human chorionic gonadotropin (β-hCG). Transvaginal ultrasound demonstrates a right complex mass with cystic and solid components. Which of the following is the most appropriate next step in management?
A. Prescribe her a 14-day course of levofloxacin (500 mg PO once per day) and urgent gynecology follow- up within 1 week.
B. Give her a dose of metronidazole (2 g PO) and prescribe her a 14-day course of cephalexin (500 mg) with urgent gynecology follow-up within 1 week.
C. Give her a one-time dose of oral metronidazole (2 g PO), azithromycin (1 g PO), and ceftriaxone (250 mg IM) with gynecology follow-up if she is not feeling better.
D. Given her a one-time dose with emergent gynecology consultation for possible laparoscopic drainage.
E. Give her a dose of ceftriaxone (250 mg IM), and prescribe her a 10-day course of doxycycline (100 mg PO BID) with urgent gynecology follow-up within 1 week.
104. A 42-year-old IV drug user presents to the ED with fever, chills, pleuritic chest pain, myalgias, and general malaise. The patient’s vitals include an HR of 110 beats per minute, BP of 110/65 mm Hg, RR of 18 breaths per minute, and temperature of 103.4°F. Physical examination is notable for retinal hemorrhages, petechiae on the conjunctivae and mucous membranes, a faint systolic ejection murmur, and splenomegaly. Which of the following is the most likely diagnosis?
A. Disseminated gonorrhea
B. Myocarditis
C. Pericarditis
D. Infectious mononucleosis
E. Endocarditis
105. A 51-year-old diabetic man complains of intense right-ear pain and discharge. On physical examination, his BP is 145/65 mm Hg, HR 91 beats per minute, and temperature 101°F. He withdraws when you retract the pinna of his ear. The external auditory canal is erythematous, edematous, and contains what looks like friable granulation tissue in the external auditory canal. The tympanic membrane is partially obstructed but appears to be erythematous, as well. You make the presumptive diagnosis of necrotizing (malignant) otitis externa. Which of the following statements regarding this condition is true?
A. It is an uncommon complication of otitis media in otherwise healthy patients.
B. The mainstay of treatment is outpatient with oral antibiotics.
C. Cranial nerve IX palsy is the most common complication.
D. Pseudomonas aeruginosa is the most common causative organism.
E. Hearing loss is the most common complication.
106. A 26-year-old woman presents to the ED with fever, malaise, and an evolving rash in the right axilla that she initially thought was from an insect bite that she received while hiking 1 week earlier. She complains of generalized fatigue, nausea, headache, and joint pain over the past several days. Her vitals are BP of 120/75 mm Hg, HR of 75 beats per minute, RR of 16 breaths per minute, and temperature of 101°F. On physical examination, she is awake and alert, with a nonfocal neurologic examination. Her neck is supple, but she is diffusely tender over the shoulder, knee, and hip joints bilaterally without any distinct effusions. Her abdomen is soft and nontender. She has a 9-cm erythematous annular plaque with partial central clearing and a bright red outer border and a target center under her right axilla. Which of the following is the next best step?
A. Treat empirically with broad-spectrum antibiotics and consult dermatology emergently for a biopsy of the rash.
B. Treat empirically for a cellulitis with cephalexin for 10 days and arrange follow-up with her primary care doctor.
C. Treat empirically for Lyme disease with doxycycline for 21 days and arrange follow-up with her primary-care dotor.
D. Treat empirically for an allergic dermatitis with prednisone, diphenhydramine, and famotidine for 3 days, and arrange follow-up with her primary care doctor.
E. Perform serologic testing for Borrelia burgdorferi to confirm the diagnosis of Lyme disease and arrange follow-up with her primary care doctor.
107. A 22-year-old man without medical complaints presents to the ED with a 3-day history of fever, malaise, and myalgias. He denies chest pain, shortness of breath, nausea or vomiting, abdominal pain, cough, sore throat, genitourinary symptoms, or respiratory tract complaints. On examination, the patient’s BP is 100/60 mm Hg, HR is 110 beats per minute, RR is 20 breaths per minute, and temperature is 102°F. He appears awake, alert, and comfortable. His physical examination is normal. Which of the following is the most appropriate next step in management?
b. Order a CBC, urinalysis, and chest x-ray. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination.
A. Discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination.
B. Order a CBC, urinalysis, and chest x-ray. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination.
C. Order a CBC, urinalysis, chest x-ray, and two sets of blood cultures. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination.
D. Order a CBC, urinalysis, chest x-ray, two sets of blood cultures, and perform an LP. If normal, discharge him with antipyretics and follow up with his primary care doctor in 1 or 2 days for a repeat examination.
E. Order a CBC, urinalysis, chest x-ray, two sets of blood cultures, and perform an LP. Start empiric IV antibiotics and admit him for observation.
108. A 54-year-old man with a history of hepatitis C, alcohol abuse, and cirrhotic ascites presents with increasing abdominal girth and abdominal pain. He complains of increasing difficulty breathing, especially when lying down, caused by worsening ascites. On physical examination, the patient is cachectic and appears older than his stated age. He has a diffusely tender abdomen and tense ascites. The liver is palpable 4 cm below the costal margin. Vitals include a BP of 110/65 mm Hg, HR of 110 beats per minute, RR of 22 breaths per minute, and temperature of 102°F. Which of the following is the most common organism seen in spontaneous bacterial peritonitis?a. Pseudomonas aeruginosa
A. Pseudomonas aeruginosa
B. Enterococcus
D. Enterobacteriaceae
C. Streptococcus pneumoniae
E. Streptococcus viridans
109. A 30-year-old man with type 1 diabetes presents to the emergency department (ED). His blood pressure (BP) is 100/70 mm Hg and heart rate (HR) is 140 beats per minute. His blood glucose is 750 mg/dL, potassium level is 5.9 mEq/L, bicarbonate is 5 mEq/L, and arterial pH 7.1. His urine is positive for ketones. Which of the following is the best initial therapy for this patient?
A. Give normal saline as a 2-L bolus; then administer 20 units of regular insulin subcutaneously.
B. Bolus 2 ampules of bicarbonate and administer 10 units of insulin intravenously.
C. Give him 5 mg of metoprolol to slow down his heart, start intravenous (IV) hydration, and then give 10 units of regular insulin intravenously.
D. Give normal saline in 2 L bolus and then administer 10 units of insulin intravenously followed by an insulin drip and continued hydration.
E. Give normal saline in 2 L bolus with 20 mEq/L potassium chloride (KCl) in each bag.
110. A 39-year-old woman, brought into the ED by her family, states that she has had 4 days of diarrhea and has now started acting “crazy” with mood swings and confusion. The family states that she usually takes a medication for a problem with her neck. Her BP is 130/45 mm Hg, HR is 140 beats per minute, temperature is 101.5°F, and her respiratory rate (RR) is 22 breaths per minute. An electrocardiogram (ECG) reveals atrial fibrillation with a normal QRS complex. After you address the airway, breathing, and circulation (ABCs), which of the following is the most appropriate next step in management?
A. Administer 2 ampules of bicarbonate to treat for tricyclic antidepressant overdose.
B. Administer chlordiazepoxide, thiamine, and folate.
C. Administer ceftriaxone and prepare for a lumbar puncture.
D. Administer propranolol and propylthiouracil (PTU); then wait an hour to give Lugol iodine solution.
E. Administer ciprofloxacin and give a 2-L bolus of normal saline for treatment of dehydration secondary to infectious diarrhea.
111. A 65-year-old woman, brought into the ED by her family, states that she has been weak, lethargic, and saying “crazy things” over the last 2 days. Her family also states that her medical history is significant only for a disease of her thyroid. Her BP is 120/90 mm Hg, HR is 51 beats per minute, temperature is 94°F rectally, and RR is 12 breaths per minute. On examination, the patient is overweight, her skin is dry, and you notice periorbital nonpitting edema. On neurologic examination, the patient does not respond to stimulation. Which of the following is the most likely diagnosis?
A. Apathetic thyrotoxicosis
B. Myxedema coma
C. Graves disease
D. Acute stroke
E. Schizophrenia
112. A 74-year-old woman who is a known diabetic is brought to the ED by emergency medical service (EMS) with altered mental status. The home health aide states that the patient ran out of her medications 4 days ago. Her BP is 130/85 mm Hg, HR is 110 beats per minute, temperature is 99.8°F, and RR is 18 breaths per minute. On examination, she cannot follow commands but responds to stimuli. Laboratory results reveal white blood cell (WBC) count of 14,000/L, hematocrit 49%, platelets 325/L, sodium 128 mEq/L, potassium 3.0 mEq/L, chloride 95 mEq/L, bicarbonate 22 mEq/L, blood urea nitrogen (BUN) 40 mg/dL, creatinine 1.8 mg/dL, and glucose 850 mg/dL. Urinalysis shows 3+ glucose, 1+ protein, and no blood or ketones. After addressing the ABCs, which of the following is the most appropriate next step in management?
b. Begin fluid resuscitation with a 2- to 3-L bolus of normal saline; then administer 10 units of regular insulin intravenously and begin phenytoin for seizure prophylaxis.
a. Begin fluid resuscitation with a 2- to 3-L bolus of normal saline; then administer 10 units of regular insulinee intravenously.
C. Administer 10 units of regular insulin intravenously; then begin fluid resuscitation with a 2- to 3-L bolus of normal saline.
D. Order a computed tomographic (CT) scan of the brain; if negative for acute stroke, begin fluid resuscitation with a 2- to 3-L bolus of normal saline.
E. Arrange for urgent hemodialysis.
113. A 21-year-old man presents to the ED. He has a known history of type 1 diabetes. He is hypotensive with BP of 95/65 mm Hg, tachycardic at 120 beats per minute, and tachypneic at 30 breaths per minute. Laboratory results reveal a WBC 20,000/μL, hematocrit 45%, platelets 225/μL, sodium 131 mEq/L, potassium 5.3 mEq/L, chloride 95 mEq/L, bicarbonate 5 mEq/L, BUN 20 mg/dL,creatinine 0.9 mg/dL, and glucose 425 mg/dL. Arterial blood gas reveals a pH of 7.2. Urinalysis reveals glucosuria and ketosis. There is a fruity odor to his breath. Which of the following provides the strongest evidence for the diagnosis?
B. Glucose of 425 mg/dL, ketosis, and leukocytosis
A. Hypotension, tachycardia, and tachypnea
C. Glucose of 425 mg/dL, ketosis, pH 7.2, and bicarbonate of 5 mEq/L
D. Glucose of 425 mg/dL, hypotension, and fruity odor to breath
E. Glucosuria, hypotension, and leukocytosis
114. A 32-year-old man is brought to the ED by EMS for confusion. EMS reports that the patient was at a local pharmacy filing his prescriptions when the pharmacist noticed the patient sweating and having difficulty answering questions. In the ED, the patient’s BP is 130/68 mm Hg, HR is 120 beats per minute, temperature is 98.9°F, and RR is 12 breaths per minute. The patient is unable to explain what happened. His fingerstick glucose is 410 mg/dL and his urine is positive for ketones. An electrolyte panel reveals Na + 131 mEq/L, K + 4 mEq/L, Cl − 91 mEq/L, and Ca2+ 11 mEq/L. Which of the following electrolytes are most important to supplement during the management of his medical condition?
A. Sodium, potassium, and calcium
B. Sodium
D. Calcium
C. Potassium
E. Sodium and calcium
115. 36-year-old immigrant woman is brought to the ED from her workplace. She was found to be agitated and behaving bizarrely. The patient’s past medical history and medications are unknown. Her BP is 162/92 mm Hg, HR is 140 beats per minute, temperature is 101.8°F, and RR is 18 breaths per minute. On examination, the patient is delirious, tremulous, and has a large goiter. Which of the following is the most appropriate management of this patient?
A. Administer dantrolene.
B. Administer acetaminophen and broad-coverage antibiotics.
C. Protect airway; administer iodine.
D. Administer diazepam.
E. Protect airway; administer acetaminophen, propranolol, and PTU.
116. A 75-year-old woman is brought to the ED by EMS after she had a witnessed seizure on the street. A bystander reports that the patient fell to the ground, had tonic-clonic activity, and was drooling. Her BP is 162/85mm Hg, HR is 95 beats per minute, temperature is 99.4°F, and RR is 16 breaths per minute. On examination, the patient is unresponsive and has a bleeding superficial scalp laceration. Which of the following electrolyte disturbances is least likely to cause a seizure?
A. Hypoglycemia
B. Hyperglycemia
C. Hyponatremia
D. Hypernatremia
E. Hypokalemia
117. A 53-year-old woman is brought to the ED by her husband. He states that his wife is feeling very weak over the last 2 days, is nauseated, and vomiting at least three times. The husband states that she was taking a high-dose medication for her joint pain but ran out of her pills last week. Her vital signs are BP of 90/50 mm Hg, HR 87 beats per minute, RR 16 breaths per minute, and temperature 98.1°F. You place her on the monitor, begin IV fluids, and send her blood to the laboratory. Thirty minutes later the metabolic panel results are back and reveal the following:Na+ 126 mEq/L K+ 5 mEq/L Cl− 99 mEq/L HCO3 21 mEq/L BUN 24 mg/dL Creatinine 1.6 mg/dL Glucose 69 mg/dL Ca+ 11 mEq/L What is the most likely diagnosis?
A. Myxedema coma
B. Thyroid storm
C. Hyperaldosteronism
D. Adrenal insufficiency
E. Diabetic ketoacidosis (DKA)
118. A 44-year-old agitated woman is brought to the ED by her husband. He states that she has had fevers to 101°F and a productive cough at home for the last 3 days. Today she became labile, agitated, and complained of abdominal pain. She was recently diagnosed with Graves’ disease and started on PTU. Her BP is 156/87 mm Hg, HR is 145 beats per minute, temperature is 102.4°F, and RR is 20 breaths per minute. On examination, the patient is agitated, confused, and has rales on auscultation bilaterally. Which of the following is the most likely diagnosis?
A. Pheochromocytoma
B. Cocaine ingestion
C. Heat stroke
D. Thyroid storm
E. Neuroleptic malignant syndrome
119. An 81-year-old diabetic woman with a history of atrial fibrillation is transferred to your emergency department (ED) from the local nursing home. The note from the facility states that the patient is complaining of abdominal pain, having already vomited once. Her vital signs in the ED are temperature 100.1°F, blood pressure (BP) 105/75 mm Hg, heart rate (HR) 95 beats per minute, and respiratory rate (RR) 18 breaths per minute. You examine the patient and focus on her abdomen. Considering that the patient has not stopped moaning in pain since arriving to the ED, you are surprised to find that her abdomen is soft on palpation. You decide to order an abdominal radiographic series. Which of the findings on plain abdominal film is strongly suggestive of mesenteric infarction?
A. Sentinel loop of bowel
B. No gas in the rectum
C. Presence of an ileus
D. Pneumatosis intestinalis
E. Air fluid levels
120. A husband and wife present to the ED with 1 day of subjective fever, vomiting, watery diarrhea, and abdominal cramps. They were at a restaurant a day before for dinner and both ate the seafood special, which consisted of raw shellfish. In the ED, they are both tachycardic with temperatures of 99.8°F and 99.6°F for him and her, respectively. Which of the following is responsible for the majority of acute episodes of diarrhea?
A. Parasites
B. Viruses
C. Enterotoxin-producing bacteria
D. Anaerobic bacteria
E. Invasive bacteria
121. A 49-year-old man presents to the ED with nausea, vomiting, and abdominal pain that began approximately 2 days ago. The patient states that he usually drinks a six pack of beer daily, but increased his drinking to 2 six packs daily over the last week because of pressures at work. He notes decreased appetite over the last 3 days and states he has not had anything to eat in 2 days. His BP is 125/75 mm Hg, HR is 105 beats per minute, and RR is 20 breaths per minute. You note generalized abdominal tenderness on examination. Laboratory results reveal the following: 9000/μL Sodium 131 mEq/L Potassium 3.5 mEq/L Chloride 101 mEq/L Bicarbonate 10 mEq/L Blood urea nitrogen (BUN) 9 mg/dL Creatinine 0.5 mg/dL Glucose 190 mg/dL nitroprusside test weakly positive for ketones White blood cells (WBC) Hematocrit 48% Platelets 210/μL Aspartate transaminase (AST) 85 U/L Alanine transaminase (ALT) 60 U/L Alkaline phosphatase 75 U/L Total bilirubin 0.5 mg/dL Lipase 40 IU Which of the following is the mainstay of therapy for patients with this condition?
A. Normal saline (NS) solution
B. Half normal saline (1/2 NS)
D. Solution containing both saline and glucose (D5/NS or D5 1/2 NS)
C. Glucose solution (D5W)
E. The type of solution is irrelevant
122. As you palpate the right upper quadrant (RUQ) of a 38-year-old woman’s abdomen, you notice that she stops her inspiration for a brief moment. During the history, the patient states that over the last 2 days she gets pain in her RUQ that radiates to her back shortly after eating. Her vitals include a temperature of 100.4°F, HR of 95 beats per minute, BP of 130/75 mm Hg, and RR of 16 breaths per minute. What is the initial diagnostic modality of choice for this disorder?
A. Plain film radiograph
B. Computed tomography (CT) scan
C. Magnetic resonance imaging (MRI)
D. Radioisotope cholescintigraphy (HIDA scan)
E. Ultrasonography
123. A 31-year-old man from Florida presents to the ED complaining of severe pain that starts in his left flank and radiates to his testicle. The pain lasts for about 1 hour and then improves. He had similar pain last week that resolved spontaneously. He noted some blood in his urine this morning. His BP is 145/75 mm Hg, HR is 90 beats per minute, temperature is 98.9°F, and his RR is 24 breaths per minute. His abdomen is soft and nontender. As you examine the patient, he vomits and has trouble lying still in his stretcher. Which of the following is the most appropriate next step in management?
A. Call surgery consult to evaluate the patient for appendicitis.
B. Order an abdominal CT.
c. Start intravenous (IV) fluids and administer an IV nonsteroidal anti-inflammatory drug (NSAID) and antiemetic
d. Perform an ultrasound to evaluate for an abdominal aortic aneurysm (AAA).
E. Perform an ultrasound to evaluate for testicular torsion.
124. A 67-year-old man is brought to the ED by emergency medical service (EMS). His wife states that the patient was doing his usual chores around the house when all of a sudden he started complaining of severe abdominal pain. He has a past medical history of coronary artery disease and hypertension. His BP is 85/70 mm Hg, HR is 105 beats per minute, temperature is 98.9°F, and his RR is 18 breaths per minute. On physical examination, he is diaphoretic and in obvious pain. Upon palpating his abdomen, you feel a large pulsatile mass. An electrocardiogram (ECG) reveals sinus tachycardia. You place the patient on a monitor, administer oxygen, insert two largebore IVs, and send his blood to the laboratory. His BP does not improve after a 1-L fluid bolus. Which of the following is the most appropriate next step in management?
A. Order a CT scan to evaluate his aorta.
B. Call the angiography suite and have them prepare the room for the patient.
C. Order a portable abdominal radiograph.
D. Call surgery and have them prepare the operating room (OR) for an exploratory laparotomy.
E. Call the cardiac catheterization laboratory to prepare for stent insertion.
125. A 57-year-old woman presents to the ED with a basin in her hand and actively vomiting. You insert an IV catheter, start IV fluids, and administer an antiemetic agent. The patient feels much better but also complains of severe crampy abdominal pain that comes in waves. You examine her abdomen and note that it is distended and that there is a small midline scar in the lower abdomen. Upon auscultation, you hear high-pitched noises that sound like “tinkles.” Palpation elicits pain in all four quadrants but no rebound tenderness. She is guaiac negative. Which of the following is the most common cause of this patient’s presentation?
A. Travel to Mexico
B. Ethanol abuse
D. Hernia
C. Hysterectomy
E. Constipation
126. An undomiciled 41-year-old man walks into the ED complaining of abdominal pain, nausea, and vomiting. He tells you that he has been drinking beer continuously over the previous 18 hours. On examination, his vitals are BP 150/75 mm Hg, HR 104 beats per minute, RR 16 breaths per minute, oxygen saturation 97% on room air, temperature of 99.1°F rectally, and finger stick glucose 81 mg/dL. The patient is alert and oriented, his pupils anicteric. You notice gynecomastia and spider angiomata. His abdomen is soft but tender in the RUQ. Laboratory tests reveal an AST of 212 U/L, ALT 170 U/L, alkaline phosphatase of 98 U/L, total bilirubin of 1.9 mg/dL, international normalized ratio (INR) of 1.3, WBC 12,000/μL. Urinalysis shows 1+ protein. Chest x-ray is unremarkable. Which of the following is the most appropriate next step in management?
A. Place a nasogastric tube in the patient’s stomach to remove any remaining ethanol.
B. Order a HIDA scan to evaluate for acute cholecystitis.
C. Administer hepatitis B immune globulin.
D. Send viral hepatitis titers.
E. Provide supportive care by correcting any fluid and electrolyte imbalances.
127. A 48-year-old man with a past medical history of hepatitis C and cirrhosis presents to the ED complaining of acute-onset abdominal pain and chills. His BP is 118/75 mm Hg, HR is 105 beats per minute, RR is 16 breaths per minute, temperature is 101.2°F rectally, and oxygen saturation is 97% on room air. His abdomen is distended, and diffusely tender. You decide to perform a paracentesis and retrieve 1 L of cloudy fluid. Laboratory analysis of the fluid shows a neutrophil count of 550 cells/mm 3. Which of the following is the most appropriate choice of treatment?
A. Metronidazole
B. Vancomycin
C. Sulfamethoxazole/trimethoprim (SMX/TMP)
D. Neomycin and lactulose
E. Cefotaxime
128. A 24-year-old man woke up from sleep 1 hour ago with severe pain in his right testicle. He states that he is sexually active with multiple partners. On examination, the right scrotum is swollen, tender, and firm. You cannot elicit a cremasteric reflex. His BP is 145/75 mm Hg, HR is 103 beats per minute, RR is 14 breaths per minute, temperature is 98.9°F, and oxygen saturation is 99% on room air. Which of the following is the most appropriate next step in management?
A. Administer one dose of ceftriaxone and doxycycline for 10 days and have him follow-up with a urologist.
B. Swab his urethra, send a culture for gonorrhea and Chlamydia, and treat if positive.
C. Send a urinalysis and treat for a urinary tract infection (UTI) if positive.
E. Order a statim (STAT) color Doppler ultrasound and urologic consultation.
D. Treat the patient for epididymitis and have him return if symptoms persist.
129. A 55-year-old woman with a past medical history of diabetes walks into the emergency department (ED) stating that her tongue and lips feel like they are swollen. During the history, she tells you that her doctor just started her on a new blood pressure (BP) medication. Her only other medication is a baby aspirin. Her vitals at triage are: BP 130/70 mm Hg, heart rate (HR) 85 beats per minute, respiratory rate (RR) 16 breaths per minute, oxygen saturation 99% on room air, and temperature 98.7°F. On physical examination, you detect mild lip and tongue swelling. Over the next hour, you notice that not only are her tongue and lips getting more swollen, but her face is starting to swell, too. What is the most likely inciting agent?
A. Metoprolol
B. Furosemide
D. Lisinopril
C. Aspirin
E. Diltiazem
130. A 45-year-old woman presents to the ED immediately after landing at the airport from a transatlantic flight. She states that a few moments after landing she felt short of breath and felt pain in her chest when she took a deep breath. Her only medications are oral contraceptive pills and levothyroxine. She is a social drinker and smokes cigarettes occasionally. Her BP is 130/75 mm Hg, HR is 98 beats per minute, temperature is 98.9°F, RR is 20 breaths per minute, and oxygen saturation is 97% on room air. You send her for a duplex ultrasound of her legs, which is positive for deep vein thrombosis. What is the most appropriate management for this patient?
A. Place patient on a monitor, provide supplemental oxygen, and administer unfractionated heparin.
B. Place patient on a monitor, order a chest computed tomography (CT) scan to confirm a pulmonary embolism (PE), and then administer unfractionated heparin.
C. Place patient on a monitor and administer aspirin.
D. Instruct the patient to walk around the ED so that she remains mobile and does not exacerbate thrombus formation.
E. Place the patient on a monitor, provide supplemental oxygen, and administer warfarin.
131. A tall, thin 18-year-old man presents to the ED with acute onset of dyspnea while at rest. The patient reports sitting at his desk when he felt a sharp pain on the right side of his chest that worsened with inspiration. His past medical history is significant for peptic ulcer disease. He reports taking a 2- hour plane trip a month ago. His initial vitals include an HR of 100 beats per minute, a BP of 120/60 mm Hg, an RR of 16 breaths per minute, and an oxygen saturation of 97% on room air. On physical examination, you note decreased breath sounds on the right side. Which of the following tests should be performed next?
A. Electrocardiogram (ECG)
B. D-dimer
D. Upright abdominal radiograph
C. Ventilation perfusion scan (V/Q scan)
E. Chest radiograph
132. A 30-year-old obese woman with no significant past medical history presents to the ED complaining of shortness of breath and coughing up blood-streaked sputum. The patient states that she traveled to Moscow a month ago. Upon returning to the United States, the patient developed a persistent cough associated with dyspnea. She was seen by a pulmonologist, who diagnosed her with bronchitis and prescribed an inhaler. However, over the following weeks, the patient’s symptoms worsened, and she developed pleuritic chest pain. In the ED, she lets you know that she smokes half a pack per day. Her vitals include a temperature of 99°F, BP of 105/65 mm Hg, HR of 124 beats per minute, RR of 22 breaths per minute, and an oxygen saturation of 94% on room air. Physical examination is noncontributory, except for rales at the left-mid lung. Her ECG reveals sinus tachycardia with large R waves in V 1 to V 3 and inverted T waves. Given this patient’s history and presentation, what is the most likely etiology of her symptoms?
A. Mycoplasma pneumoniae (“walking” pneumonia)
B. Q fever pneumonia
D. PE
C. Pneumocystis jiroveci pneumonia (PCP)
E. Acute respiratory distress syndrome (ARDS)
133. A 24-year-old woman is brought to the ED after being found on a nearby street hunched over and in mild respiratory distress. Upon arrival, she is tachypneic at 24 breaths per minute with an oxygen saturation of 97% on face mask oxygen administration. Upon physical examination, the patient appears to be in mild distress with supraclavicular retractions. Scattered wheezing is heard throughout bilateral lung fields. Which of the following medications should be administered first?
B. Magnesium sulfate
A. Corticosteroids
D. Anticholinergic nebulizer treatment
C. Epinephrine
E. β2-Agonist nebulizer treatment
134. An 81-year-old woman presents to the ED with acute onset of shortness of breath just before arrival. She refuses to answer questions for the interview, but repeatedly states that she is feeling short of breath. Her initial vitals include an HR of 89 beats per minute, a BP of 168/76 mm Hg, and an RR of 18 breaths per minute with an oxygen saturation of 89% on room air. A portable chest x-ray appears normal. Her physical examination is unremarkable, except for a systolic ejection murmur. Intravenous (IV) access is successfully obtained. After placing the patient on oxygen and a monitor, which of the following should be performed first?
A. Evaluation of troponin level
B. Evaluation of D-dimer level
C. Rectal temperature
D. Repeat chest x-ray
E. ECG
135. As you evaluate a patient with shortness of breath, you appreciate decreased breath sounds at the left-lung base. You suspect the patient has a small pleural effusion. In which of the following views of the chest is this small pleural effusion most likely to be detected?
A. Supine
B. Lateral decubitus right-side down
C. Lateral decubitus left-side down
D. Lateral
E. Posterior-anterior (PA)
136. A 32-year-old firefighter presents to the ED in acute respiratory distress. He was taken to the ED shortly after extinguishing a large fire in a warehouse. His initial vitals include an HR of 90 beats per minute, a BP of 120/55 mm Hg, and an RR of 18 breaths per minute with an oxygen saturation of 98% on 2-L nasal cannula. An ECG shows a first-degree heart block. Upon physical examination, there are diffuse rhonchi bilaterally. The patient is covered in soot and the hairs in his nares are singed. Given this clinical presentation, which of the following may be responsible for this patient’s respiratory distress?
A. Reactive airway disease
B. Foreign body aspiration
D. Thermal burns
C. Decompression sickness
E. Pneumothorax
137. A 76-year-old man presents to the ED in acute respiratory distress, gasping for breath while on face mask. Paramedics state that he was found on a bench outside of his apartment in respiratory distress. Initial vitals include an HR of 90 beats per minute, a BP of 170/90 mm Hg, and an RR of 33 breaths per minute with an oxygen saturation of 90%. Upon physical examination, the patient is coughing up pink, frothy sputum, has rales two-thirds of the way up both lung fields, and has pitting edema of his lower extremities. A chest radiograph reveals bilateral perihilar infiltrates, an enlarged cardiac silhouette, and a small right-sided pleural effusion. After obtaining IV access and placing the patient on a monitor, which of the following medical interventions is most appropriate?
A. Morphine sulfate only
B. Nitroglycerin only
D. Aspirin
C. Nitroglycerin and a loop diuretic
E. Antibiotics
138. A 67-year-old man is brought to the ED in respiratory distress. His initial vitals include an HR of 112 beats per minute, a BP of 145/88 mm Hg, and an RR of 18 breaths per minute with an oxygen saturation of 92% on room air. He is also febrile at 102°F. After obtaining IV access, placing the patient on a monitor, and administering oxygen via nasal cannula, a chest radiograph is performed and shows patchy alveolar infiltrates with consolidation in the lower lobes. On review of systems, the patient tells you that he had five to six watery bowel movements a day for the last 2 days with a few bouts of emesis. Which of the following infectious etiologies is most likely responsible for the patient’s presentation?
A. Streptococcus pneumoniae
B. Haemophilus influenzae
D. Chlamydophila pneumoniae
C. Mycoplasma pneumoniae
E. Legionella pneumophila
139. A 32-year-old woman presents to the ED with a 1-month history of general malaise, mild cough, and subjective fevers. She states that she is human immunodeficiency virus (HIV) positive and her last CD4 count, 6 months ago, was 220. She is not on antiretroviral therapy or any other medications. Initial vitals include an HR of 88 beats per minute, a BP of 130/60 mm Hg, and an RR of 12 breaths per minute with an oxygen saturation of 91% on room air. Her chest radiograph shows bilateral diffuse interstitial infiltrates. Subsequent laboratory tests are unremarkable except for an elevated lactate dehydrogenase level. Given this patient’s history and physical examination, which of the following is the most likely organism responsible for her clinical presentation?
A. Coccidioides immitis
B. Mycobacterium tuberculosis
D. Mycoplasma pneumoniae
C. Pneumocystis jiroveci
E. Haemophilus influenzae
140. A 27-year-old woman presents to the ED complaining of an intensely pruritic rash all over her body, abdominal cramping, and chest tightness. She states that 1 hour ago she was at dinner and accidentally ate some shrimp. She has a known anaphylactic allergy to shrimp. Her BP is 115/75 mmHg, HR is 95 beats per minute, temperature is 98.9°F, RR is 20 breaths per minute, and oxygen saturation is 97% on room air. She appears anxious, and her skin is flushed with urticarial lesions. Auscultation of her lungs reveals scattered wheezes with decreased air entry. Which of the following is the most appropriate next step in management?
B. Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and administer methylprednisolone and diphenhydramine intravenously.
A. Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and administer methylprednisolone intravenously.
D. Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and start aerosolized albuterol.
E. Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, and start aerosolized epinephrine.
C. Administer oxygen via non-rebreather, place a large-bore IV, begin IV fluids, administer methylprednisolone and diphenhydramine intravenously,and give intramuscular epinephrine.
141. A 72-year-old man presents to the ED with worsening dyspnea. His initial vitals include an HR of 93 beats per minute, BP of 110/50 mm Hg, and RR of 20 breaths per minute with an oxygen saturation of 88% on room air. The patient appears thin and anxious. He is using accessory muscles to breathe. Despite distant breath sounds, you hear end-expiratory rhonchi and a prolonged expiratory phase. An ECG shows peaked P waves in leads II, III, and aVF. Given this patient’s history and physical examination, which of the following conditions does this patient most likely have?
A. Chronic bronchitis
B. Asthma
D. Congestive heart failure (CHF)
C. Emphysema
E. Pneumothorax
142. A 71-year-old woman presents to the ED after a reported mechanical fall 2 days ago. Her initial vitals include an HR of 55 beats per minute, a BP of 110/60 mm Hg, an RR of 14 breaths per minute, and an oxygen saturation of 96% on room air. The patient does not appear to be taking deep breaths. Her physical examination is significant for decreased breath sounds bilaterally and tenderness to palpation along the right side of her chest. After initial stabilization, which of the following is the diagnostic test of choice for this patient’s condition?
B. Chest CT scan
A. Chest x-ray
D. Rib radiographs
C. ECG
E. Thoracentesis
143. A 29-year-old woman presents to the ED for hyperventilation. Her initial vitals include an RR of 28 breaths per minute with an oxygen saturation of 100% on room air. She is able to speak in full sentences and tells you that she cannot breathe and that her hands and feet are cramping up. She denies any trauma, past medical history, or illicit drug use. Chest auscultation reveals clear breath sounds bilaterally. A subsequent chest radiograph is normal. Upon reevaluation, the patient reports that she is breathing better. Her vitals include an RR of 12 breaths per minute with an oxygen saturation of 100% on room air. Which of the following conditions is most likely the etiology of this patient’s symptoms?
B. Hemopneumothorax
A. Pneumothorax
C. Pleural effusion
D. Anxiety attack
E. Asthma exacerbation
144. A 42-year-old man presents to the ED via ambulance after activating EMS for dyspnea. He is currently on an oxygen face mask and was administered one nebulized treatment of a β2-agonist by the paramedics. His initial vitals include an RR of 16 breaths per minute with an oxygen saturation of 96% on room air. The patient appears to be in mild distress with some intercostal retractions. Upon chest auscultation, there are minimal wheezes localized over bilateral lower lung fields. The patient’s symptoms completely resolve after two more nebulizer treatments. Which of the following medications, in addition to a rescue β2-agonist inhaler, should be prescribed for outpatient use?
A. Magnesium sulfate
B. Epinephrine injection (EpiPen)
C. Corticosteroids
D. Cromolyn sodium
E. Ipratropium
145. A 22-year-old woman is brought to the ED by paramedics who state that they found the patient hunched over on a park bench barely breathing. The patient is rousable only to painful stimuli. Her initial vitals include an HR of 78 beats per minute, a BP of 125/58 mm Hg, and a respiratory rate of 6 breaths per minute with an oxygen saturation of 94% on 2-L nasal cannula. Upon physical examination, the patient has clear breath sounds bilaterally and no signs of trauma. Her pupils are 2 mm bilaterally and reactive to light. Which of the following agents may be used to restore this patient’s respirations?
A. Oxygen
B. Flumazenil
D. β2-Agonist nebulized treatment
C. Anticholinergic inhaler treatment
E. Naloxone
146. A 43-year-old undomiciled man is brought to the ED after being found intoxicated on the street. He is currently rousable and expresses a request to be left alone. Initial vitals include an HR of 92 beats per minute, a BP of 125/80 mm Hg, and an RR of 14 breaths per minute with an oxygen saturation of 93% on room air. His rectal temperature is 101.2°F. A chest radiograph shows infiltrates involving the right lower lobe. Given this clinical presentation, what initial antibiotic coverage is most appropriate for this patient?
A. Gram-negative coverage only
B. Gram-positive coverage only
C. Broad-spectrum with anaerobic coverage
D. PCP coverage
E. Antifungal therapy
147. A 32-year-old man is brought into the ED by EMS with fever, shortness of breath, and stridor. The patient was treated yesterday in the ED for a viral syndrome. His BP is 90/50 mm Hg, HR is 110 beats per minute, temperature is 101.2°F, and his RR is 28 breaths per minute. A chest radiograph reveals a widened mediastinum. The patient is endotracheally intubated, given a 2-L bolus of normal saline, and started on antibiotics. His BP improves to 110/70 mm Hg and he is transferred to the intensive care unit (ICU). You see a friend that accompanied the patient to the hospital and ask him some questions. You find out that the patient is a drum maker and works with animal hides. What is the most likely organism that is responsible for the patient’s presentation?
B. Corynebacterium diphtheriae
A. Streptococcus pneumoniae
C. Coxiella burnetii
D. Haemophilus influenzae
E. Bacillus anthracis
148. A 62-year-old man presents to the ED with gradual dyspnea over the last few weeks. He reports that he is a daily smoker and has not seen a physician in years. Upon physical examination, there are decreased breath sounds on the right as compared to the left. A chest radiograph indicates blunting of the right costophrenic angle with a fluid line. A thoracentesis is performed. Given this patient’s history, which of the following most likely describes his effusion?
A. Transudative effusion
B. Exudative effusion
D. Lactate dehydrogenase < 200 units
C. Transudative and exudative effusion
E. Fluid-to-blood protein ratio < 0.5
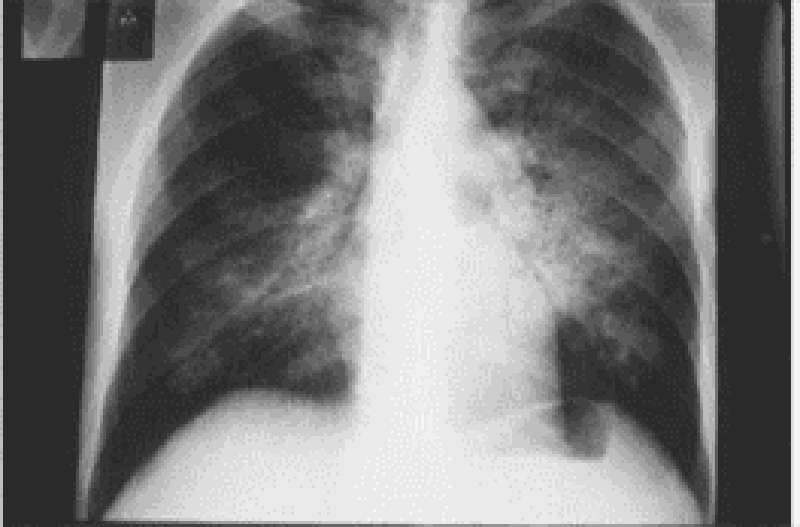
149. A 40-year-old man with a history of untreated HIV for 8 years comes into the ED complaining of cough, fever, and malaise for 3 days. He is tachypneic and diaphoretic. Chest radiograph reveals bilateral infiltrates. Arterial blood gas (ABG) analysis is significant for a PaO2 of 62 on room air. His chest radiograph is seen below. Which of the following is the most appropriate initial management?
B. Treat immediately with IV trimethoprim/sulfamethoxazole (TMP/SMX).
A. Treat with corticosteroid prior to antibiotic therapy.
D. Treat with nebulizer.
C. Administer antibiotics after a rapid sputum Gram stain is obtained.
E. Treat with racemic epinephrine.
{"name":"QCU\/DES\/USMLE\/EMERGENCY", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge and skills in emergency medicine with our comprehensive quiz designed for medical students, healthcare professionals, and enthusiasts. Explore a range of clinical scenarios that will challenge your understanding of diagnosis, treatment, and critical care.Whether you're preparing for exams or just want to reinforce your medical knowledge, this quiz offers: 150 carefully curated questionsDiverse clinical cases from various specialtiesImmediate feedback and scoring","img":"https:/images/course3.png"}
More Quizzes
(NEW) DES 2016-2017 : 2040-2299 (Fabien) 5
100500
GCS score
6335
Final 6
10559
Create account
320
Ultimate Marvel - Test Your Comics Knowledge
201021704
Which Historical Leader Are You? Free Personality
201017396
Examen TSSR Corrigé - de Révision Gratuit
201015954
Fashion Trivia: Youth Style IQ
201016659
Asia Trivia - Test Your Knowledge for Free
201017396
How Markets Work Unit Test Practice - Free Online
201016378
Am I With the Right Person? - Free Relationship Check
201017140
Am I Manic - Free Self-Assessment with Instant Results
201016955