DES 2016. Final (Part24)
278) A 65-year-old man complains of periodic back pain radiating to his thigh and buttock. The pain is related to walking or climbing the stairs but is promptly relieved by leaning forward. He also has noticed tingling and numbness in both lower extremities. He has a history of hypertension and takes hydrochlorothiazide. He does not use tobacco, alcohol, or illicit drugs. His pulse is 76/min, respirations are 14/min, and blood pressure is 140/80 mmHg. Lumbar extension reproduces the pain and tingling, while lumbar flexion relieves the symptoms. Which of the following is the most likely cause of this patient's condition?
. Iliac artery atherosclerosis
. Abdominal aortic aneurysm
. Degenerative central canal stenosis
. Lumbar disk herniation
. Spina bifida occulta
279) A 51-year-old Caucasian female complains of low-back pain radiating to the buttocks. She also complains of persistent muscle pain that gets worse with exercise. Physical examination reveals normal muscle strength. Her joints are not swollen, but palpation over the outer upper quadrants of the buttocks and the medial aspect of the knees elicits tenderness. Her ESR is 12mm/hr. Which of the following is the most likely diagnosis?
. Seronegative spondyloarthropathy
. Polymyalgia rheumatica
. Polymyositis
. Rheumatoid arthritis
. Fibromyalgia
280) A 27-year-old male presents to the physician's office because of pain on the medial side of the tibia just below the knee. The pain does not radiate and is continuous. He relates the onset of his pain to falling on the ground while playing football two weeks ago. He denies fever, malaise and weight loss. His past medical history is not significant. On examination, a well-defined area of tenderness is present on the upper tibia below the medial knee joint. There is no redness, warmth or swelling. His gait is normal. A valgus stress test has no effect on his pain. X-ray of the knee and tibia shows no abnormalities. Which of the following is the most likely cause of his current symptoms?
. Anserine bursitis
. Prepatellar bursitis
. Medial collateral ligament strain
. Medial compartment osteoarthritis
. Patellofemoral syndrome
281) A 16-year-old boy presents with a seven-month history of intermittent right knee pain and swelling. He states that his discomfort first began after a baseball injury. This injury was associated with pain, swelling, and restriction of movement in his right knee. He has had three subsequent episodes of pain and swelling in his right knee, not precipitated by trauma. The last episode occurred three days ago. He denies history of fevers or chills. There is no history of recent travel, other than a camping trip with his friends to Long Island, New York a few months ago. On physical examination, he has a marked effusion of his right knee and is unable to fully flex or extend his leg. X-ray reveals no bony abnormalities. What is the most probable diagnosis?
. Rheumatoid arthritis
. Septic arthritis
. Lyme arthritis
. Reactive arthritis
. Osteomyelitis
282) A 75-year-old female comes to the emergency room with acute onset of severe back pain. The pain started while lifting a turkey from the freezer. She had no obvious trauma preceding the pain. She denies weakness or sensory loss in the legs. Her past medical history is significant for temporal arteritis diagnosed several months ago and has been taking prednisone. She does not smoke or consume alcohol. Her temperature is 36.7°C (98°F), blood pressure is 140/70 mmHg, pulse is 80/min, and respirations are 16/min. Physical examination reveals local tenderness of the lumbar spine area. Bilateral ankle reflex is absent. Knee reflex is 2+ in both legs. Babinski's sign is absent bilaterally. Muscle power is 5/5 in both legs. Bilateral straight-leg raising to 90 degrees does not increase the pain What is the most probable diagnosis in this patient?
. Multiple myeloma
. Ankylosing spondylitis
. Compression fracture of the vertebrae
. Lumbosacral strain
. Herniated disk
283) A 66-year-old man complains of a 1-year history of low-back and buttock pain that worsens with walking and is relieved by sitting or bending forward. He has hypertension and takes hydrochlorothiazide but has otherwise been healthy. There is no history of back trauma, fever, or weight loss. On examination, the patient has a slightly stooped posture, pain on lumbar extension, and has a slightly wide base gait. Pedal pulses are normal and there are no femoral bruits. Examination of peripheral joints and skin is normal. What is the most likely cause for this patient’s back and buttock pain?
. Lumbar spinal stenosis
. Herniated nucleus pulposus
. Atherosclerotic peripheral vascular disease
. Facet joint arthritis
. Prostate cancer
284) A 22-year-old man develops the insidious onset of low-back pain improved with exercise and worsened by rest. There is no history of diarrhea, conjunctivitis, urethritis, rash, or nail changes. On examination, the patient has loss of mobility with respect to lumbar flexion and extension. He has a kyphotic posture. A plain film of the spine shows sclerosis of the sacroiliac joints. Calcification is noted in the anterior spinal ligament. Which of the following best characterizes this patient’s disease process?
. He is most likely to have acute lumbosacral back strain and requires bed rest.
. The patient has a spondyloarthropathy, most likely ankylosing spondylitis.
. The patient is likely to die from pulmonary fibrosis and extrathoracic restrictive lung disease.
. A rheumatoid factor is likely to be positive.
. A colonoscopy is likely to show Crohn disease.
285) A 20-year-old man complains of arthritis and eye irritation. He has a history of burning on urination. On examination, there is a joint effusion of the right knee and a rash of the glans penis. Which of the following is correct?
. The patient is likely to be rheumatoid factor—positive.
. An infectious process of the GI tract may precipitate this disease.
. An ANA is very likely to be positive.
. CPK will be elevated.
. Neisseria gonorrhoeae is likely to be cultured from the glans penis.
286) Last week a 20-year-old college student developed acute wrist pain and swelling. This resolved in four days. Yesterday, he developed pain and swelling in his left knee. Two months ago he went on a backpacking trip in Rhode Island. A week or so later he developed an enlarging circular red spot that persisted for 2 weeks and then resolved. What is the most likely diagnosis?
. Acute rheumatoid arthritis
. Parvovirus infection
. Psoriatic arthritis
. Lyme disease
. Inflammatory bowel disease
287) A 38-year-old man has pain and stiffness of his right knee. This began 2-weeks ago after he fell while skiing. On two occasions he had the sense that his knee was locked in a semiflexed position for a few seconds. He has noted a popping sensation when he bends his knee. On examination there is tenderness over the medial joint line of the knee. Marked flexion and extension of the knee are painful. The Lachman test (anterior displacement of the lower leg with the knee at 20°of flexion) and the anterior drawer test are negative. What is the most likely diagnosis?
. Medial meniscus tear
. Osteoarthritis
. Anterior cruciate ligament tear
. Chondromalacia patella
. Lumbosacral radiculopathy
288) A 63-year-old painter complains of severe right shoulder pain. The pain is located posteriorly over the scapula. These symptoms began after he fell from a ladder 2 weeks ago. The pain is especially bad at night and makes it difficult for him to sleep. In addition, he has had some pain in the right upper arm. Treatment with acetaminophen and ibuprofen has been unsuccessful in controlling his pain. On examination the patient appears uncomfortable. The right shoulder has full range of motion. Movement of the shoulder is not painful. There is no tenderness to palpation of the scapula. What is the most likely diagnosis?
. Subdeltoid bursitis
. Rotator cuff tendonitis
. Adhesive capsulitis
. Osteoarthritis
. Cervical radiculopathy
289) A 50-year-old woman with rheumatoid arthritis has been treated with meloxicam (Mobic). You add hydroxychloroquine. Six weeks later her arthritis is mildly improved. The same joints are still involved but she now reports only 1-hour morning stiffness. She has, however, developed epigastric burning and melena for the past 3 days. Stool is strongly positive for occult blood. Which of the following is the most likely cause for the melena in this case?
. Emotional stress over her illness resulting in acid peptic disease
. Hydroxychloroquine-induced acid peptic disease
. Gastric lymphoma associated with autoimmune disease
. NSAID gastropathy
. Meckel diverticulum
290) A 55-year-old woman with long-standing rheumatoid arthritis is on prednisone 5 mg daily and etanercept (Enbrel) 50 mg subcutaneously once a week. Her arthritis is well-controlled. However, she complains of a 2-day history of headaches, chills, and spiking fevers to 39.4°C (103°F). You suspect which of the following?
. An allergic febrile reaction to etanercept
. Fever related to her underlying autoimmune disease
. A serious infection
. A viral syndrome
. An occult malignancy
291) A 32-year-old Japanese woman has a long history of recurrent aphthous oral ulcers. In the last 2 months she has had recurrent genital ulcers. She now presents with a red painful eye that was diagnosed as anterior uveitis. What is the most likely diagnosis?
. Herpes simplex
. HIV infection
. Behçet disease
. Diabetes mellitus
. Systemic lupus erythematosus
292) A 53-year-old man presents with arthritis and bloody nasal discharge. Urinalysis reveals 4+proteinuria, RBCs, and RBC casts. ANCA is positive in a cytoplasmic pattern. Antiproteinase 3 (PR3) antibodies are present, but antimyeloperoxidase (MPO) antibodies are absent. Which of the following is the most likely diagnosis?
. Behçet syndrome
. Sarcoidosis
. Wegener granulomatosis
. Henoch-Schönlein purpura
. Classic polyarteritis nodosa
293) A 35-year-old right-handed construction worker presents with complaints of nocturnal numbness and pain involving the right hand. Symptoms wake him and are then relieved by shaking his hand. There is some atrophy of the thenar eminence. Tinel sign is positive. Which of the following is the most likely diagnosis?
. Carpal tunnel syndrome
. De Quervain tenosynovitis
. Amyotrophic lateral sclerosis
. Rheumatoid arthritis of the wrist joint
. Guillain-Barré syndrome
294) A 50-year-old white woman presents with aching and stiffness in the trunk, hip, and shoulders. There is widespread muscle pain after mild exertion. Symptoms are worse in the morning and improve during the day. They are also worsened by stress. The patient is always tired and exhausted. She has trouble sleeping at night. On examination, joints are normal. ESR is normal, and Lyme antibody and HIV test are negative. A diagnosis is best made by which of the following?
. Trial of glucocorticoid
. Muscle biopsy
. Demonstration of 11 tender points
. Psychiatric evaluation
. Trial of an NSAID
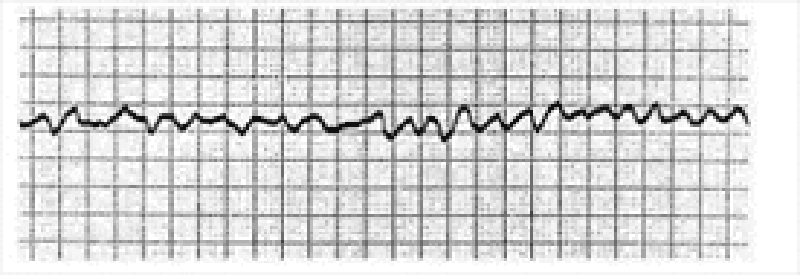
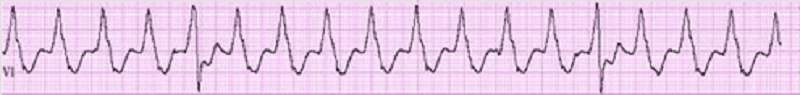
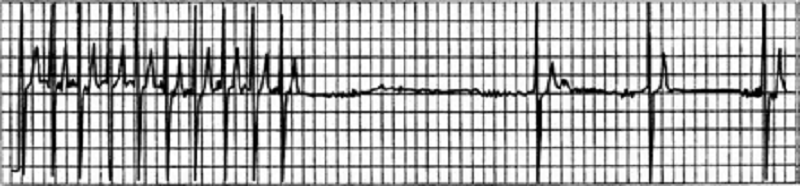
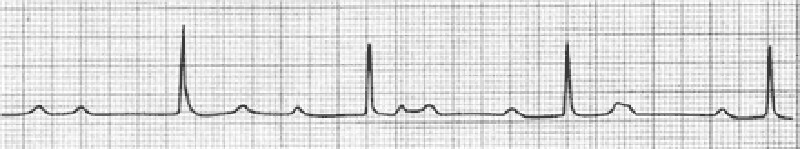
1) A 72-year-old female is admitted to the ICU with severe chest pain. The initial set of cardiac enzymes is positive and her EKG reveals an anterior wall myocardial infarction. She receives treatment with aspirin clopidogrel, metoprolol nitroglycerine drip, and morphine. Two hours later, her telemetry monitor displays the following rhythm. Which of the following is the best next step in managing this patient?
. Lidocaine
. Defibrillation
. Digoxin
. Amiodarone
. Immediate echocardiogram
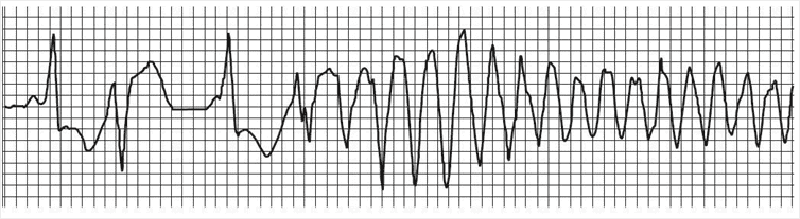
2) A 46-year-old man collapsed while getting out of his bed. He has been feeling weak over the last several days and has complained of vague chest discomfort. He ascribed the symptoms to a recent respiratory infection and did not visit a doctor. His mother died of a stroke and his father suffered from recurrent myocardial infarctions. He eats a balanced diet and takes a multivitamin daily. His most recent blood cholesterol level was 200 mg/dl. An ECG strip taken by EMS is shown below. Which of the following is the best initial management of this patient?
. Procainamide
. Synchronized DC cardioversion
. Thrombolytic therapy
. Beta-blockers and aspirin
. Pericardiocentesis
3) A 67-year-old Caucasian male is hospitalized in the intensive care unit (ICU) with an episode of prolonged hypotension and shortness of breath. His skin is cold and clammy. Intra-arterial blood pressure monitoring is established, and pulmonary artery catheterization is performed to control basic hemodynamic parameters. His blood pressure is 70/40 mmHg, and heart rate is 100/min. Cardiac output (CO) measured by thermodilution method is 2.3 L/min. Pulmonary capillary wedge pressure (PCWP) is estimated to be 22 mmHg. Systemic vascular resistance (SVR) calculated using data on mean arterial pressure, right atrial pressure and cardiac output is 2000 dynes*s/cm5 (N= 700 -1200 dynes*s/cm5). Which of the following is the most likely underlying problem in this patient?
. Cardiogenic shock
. Volume depletion
. Septic shock
. Volume overload
. Right ventricular infarction
4) A 59-year-old man comes to visit his friend in the hospital and collapses in the parking lot. He had been feeling unwell all day due to vague chest discomfort. A bystander witnesses his collapse, finds no pulse, and immediately calls for help. Which of the following is the most important factor for survival in this patient?
. Time to chest compressions
. Time to defibrillation
. Time to endotracheal intubation
. Time to epinephrine injection
. Time to cardiac catheterization lab
5) A 59-year-old male presents to the ER with sudden onset severe chest pain associated with vomiting and diaphoresis. The pain radiates to the left shoulder and is not relieved by sublingual nitroglycerine. His past medical history is significant for diabetes mellitus for seven years and hypercholesterolemia for six years. His medications include metformin, glipizide and simvastatin. On physical examination, his blood pressure is 150/98 mmHg and pulse is 86/min. An EKG obtained in the ER shows ST segment elevations in leads aVL and I. Cardiac troponin and CK-MB are elevated. Which of the following medications should be avoided in this patient at this time?
. Heparin
. Captopril
. Nifedipine
. Metoprolol
. Aspirin
6) A 69-year-old male undergoes coronary artery bypass and aortic valve replacement surgery. The procedure goes well, and he is extubated and discharged to the step-down unit on postoperative day 2. That night, he complains of weakness, chest tightness and shortness of breath. His blood pressure is 70/30 mmHg, respiratory rate is 26/min, and heart rate is 148 beats per minute. Lung auscultation reveals bibasilar crackles. An EKG rhythm strip is obtained. Which of the following is the best next step in the management of this patient?
. Amiodarone
. Transcutaneous pacing
. DC cardioversion
. Lidocaine
. Digoxin
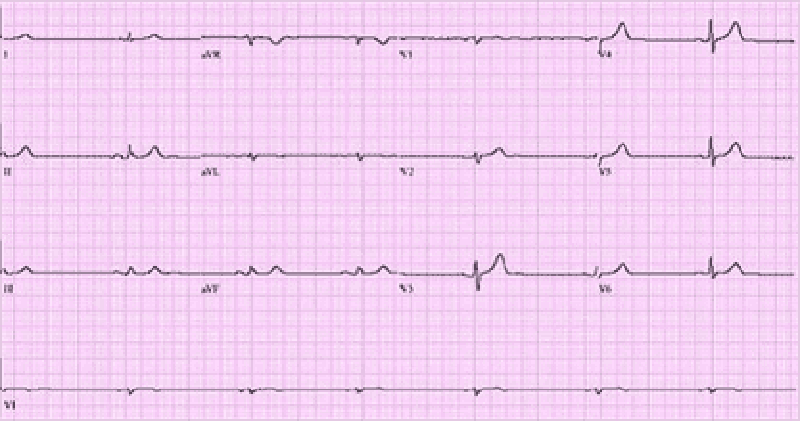
7) A 66-year-old male is rushed to the emergency department because he feels dizzy and light-headed. He denies chest pain or palpitations. He has a history of hypertension and diabetes. His blood pressure is 116/62 mmHg and his pulse is 35-40/min. He is alert, awake, and fully oriented. He is breathing comfortably and does not appear to be in any distress. His extremities are slightly cold and capillary refill is 3 seconds. His EKG is shown below. Which of the following is the most appropriate next step in management?
. Intravenous adenosine push
. Intravenous atropine
. Intravenous epinephrine
. Intravenous amiodarone
. Transcutaneous pacing
8) A 68-year-old male was intubated in the emergency room because of pulmonary edema. Stat echocardiogram reveals an ejection fraction of 45% and severe mitral regurgitation. In spite of aggressive diuresis with furosemide, the patient continues to require mechanical ventilation secondary to pulmonary edema. What is the best next step in treating this patient?
. Arrange for mitral valve replacement surgery
. Place an intra-aortic balloon pump
. Begin metoprolol
. Begin a second loop diuretic
. Begin intravenous enalapril
9) A 45-year-old male is brought to the ER with sudden onset palpitations and chest tightness. His past medical history is significant for hypertension, gout and diabetes mellitus. Cardiac monitoring shows atrial fibrillation at a rate of 120-140/min. As the nurse is attempting to establish IV access, the patient becomes unresponsive. There is no palpable pulse over the carotids or femoral arteries. The cardiac monitor still shows atrial fibrillation at the same rate. What is the best next step in management?
. Synchronized cardioversion
. Defibrillation
.IV lidocaine
. Chest compressions
. Arterial blood gas analysis
10) A 64-year-old male presents to the emergency department with chest pain. An ECG reveals ST elevations in leads II, III, and aVF. Thrombolytic therapy and heparin are administered, and the pain resolves. Eight hours after admission, the patient develops hypotension. He denies recurrence of chest pain. His temperature is 37.5°C (99.6°F), blood pressure is 84/55 mm Hg, pulse is 90/min, and respirations are 15/min. His medications include a nitroglycerin drip, beta-blocker, aspirin, heparin, and simvastatin. Examination reveals an elevated jugular venous pressure of 14 cm, cold clammy extremities, and clear lung fields. Based on this information, what is the next best step in this patient's management?
. Start dopamine
. Administer normal saline bolus and stop nitroglycerin
. Administer intravenous furosemide
. Initiate temporary cardiac pacing
. Stop nitroglycerin and start dobutamine drip
11) Neighbors find a 65-year-old male unconscious in his garden and immediately call EMS. The man is intubated at the scene. In the ER, he develops sustained ventricular tachycardia and requires cardioversion. He is started on an antiarrhythmic agent and, once recovered, is discharged to home. Three months later he returns to his physician complaining of dyspnea on exertion. Chest x-ray reveals bilateral lung fibrosis. All cultures are negative and lung biopsy reveals lipoid pneumonitis. Which of the following medications is most likely responsible for his current condition?
. Procainamide
. Amiodarone
. Lidocaine
. Quinidine
. Digoxin
12) A 36-year-old female presents to the emergency room complaining of chest pain that started suddenly while she was shopping at the mall. She also reports shortness of breath, palpitations and diaphoresis. The pain is retrosternal and radiates to the left arm. There are no aggravating or relieving factors. On review of systems, the patient reports having had a runny nose, sore throat and dry cough for the past 3 days. Her past medical history is significant for panic attacks, for which she takes paroxetine, and dysfunctional uterine bleeding, for which she takes estrogen. Her family history is significant for the sudden death of her father at age 44 from a heart attack. Social history reveals that she has smoked one pack of cigarettes per day for the past 15 years. Which of the following is the most appropriate initial therapy for this patient?
. Lorazepam
. Heparin
. Aspirin
. Ibuprofen
. Acetaminophen
13) A 21-year-old man comes to the ER with palpitations and dizziness that began suddenly one hour ago. He notes having similar past episodes provoked by fatigue or strong emotions. He says he can usually stop the episodes by putting his head into cold water or squatting and taking a deep breath. However, these techniques are not working this time. Presently, his blood pressure is 60/30 mmHg and his heart rate is 240/min. He is diaphoretic with cold extremities. An EKG rhythm strip shows a regular, narrow complex tachycardia. Which of the following is the best next step in managing his condition?
. Adenosine
. Procainamide
. Verapamil
. Digoxin
. DC cardioversion
14) A 64-year-old Caucasian male presents to the Emergency Room with a sharp, left-sided chest pain. He says that the pain is worse when he takes deep breaths, but he gets relief with leaning forward. He had an acute non-ST elevation myocardial infarction six months ago and had undergone angioplasty for the right coronary artery. His other medical problems include: diabetes, hypertension, hyperlipidemia, peripheral neuropathy, diabetic retinopathy, paroxysmal atrial fibrillation, hypothyroidism, and chronic renal insufficiency. His vital signs are BP 142/86 mmHg, PR 78/min, RR 16/min, and T 36.1°C (97°F). On examination, you find a pericardial rub. EKG shows diffuse ST elevation. Lab results are: Hb 9.0 g/dl, WBC 8,000/cmm, Platelets 210,000/cmm, Blood Glucose 248 mg/dl, Serum Na 135 mEq/L, Serum K 5.8 mEq/L, Bicarbonate 17 mEq/L, BUN 86 mg/dl, Serum Creatinine 4.4 mg/dl. Which of the following is the most appropriate management of this patient?
. NSAIDs
. Corticosteroids
. Pericardiocentesis
. Hemodialysis
. Echocardiography
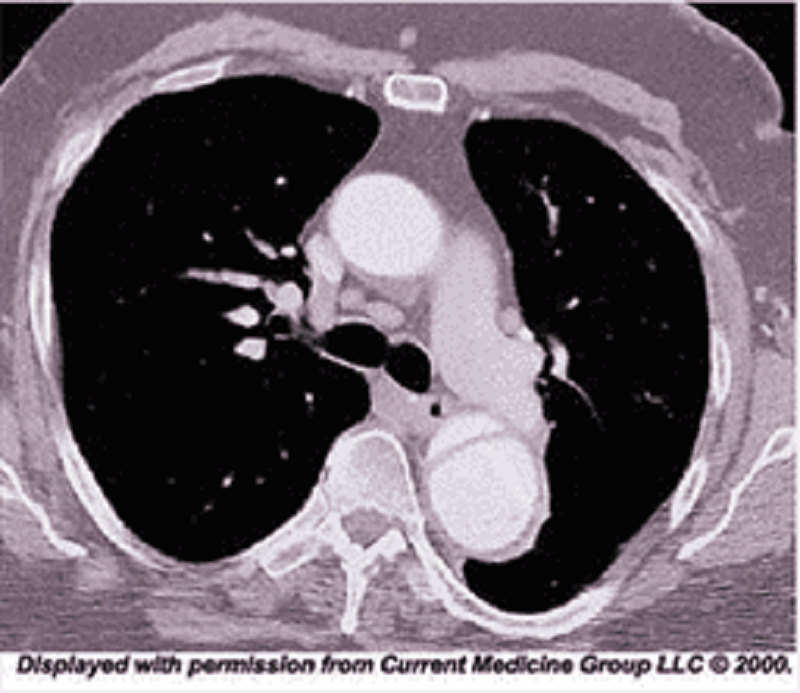
15) A 48-year-old African American man presents to the emergency room with severe retrosternal chest pain. His temperature is 36.7°C (98°F), blood pressure is 190/ 100 mmHg, pulse is 100/min, and respirations are 16/min. On physical examination, his lungs are clear to auscultation and his heart sounds are normal. EKG shows evidence of left ventricular hypertrophy. A CT image of his chest is shown below. Which of the following is the most appropriate immediate pharmacotherapy for this patient?
. Labetalol
. Nifedipine
. Heparin
. Hydrochlorothiazide
. Hydralazine
16) A 64-year-old male is admitted in ICU for acute myocardial infarction. He is on metoprolol, lisinopril, aspirin, furosemide, and potassium supplements. All of a sudden, the nurse mentions that the patient has a change in his tele monitoring. His blood pressure is 120/60 mmHg. His potassium level is 4.2. He is alert, awake and oriented time, place and person. Examination shows scattered bilateral crackles, peripheral pedal edema and elevated JVI. Which of the following is the next best step in the management of this patient?
. IV amiodarone
. IV digoxin
. Cardioversion
. IV diltiazem
. Carotid massage
17) A 56-year-old man presents to the emergency department with dyspnea. He describes waking up during the night with difficulty breathing and chest pain that kept him from falling back to sleep. He has never had these symptoms before. His past medical history is significant for long-standing hypertension and non-compliance with his antihypertensive therapy. He has smoked a pack of cigarettes per day for the past 30 years. On physical examination, his blood pressure is 170/100 mmHg and his heart rate is 120/min and regular. Lung auscultation reveals bibasilar rales and scattered wheezes. Which of the following is most likely to relieve this patient's dyspnea?
. Metoprolol
. Hydralazine
. Nitroglycerin
. Dopamine
. Amiodarone
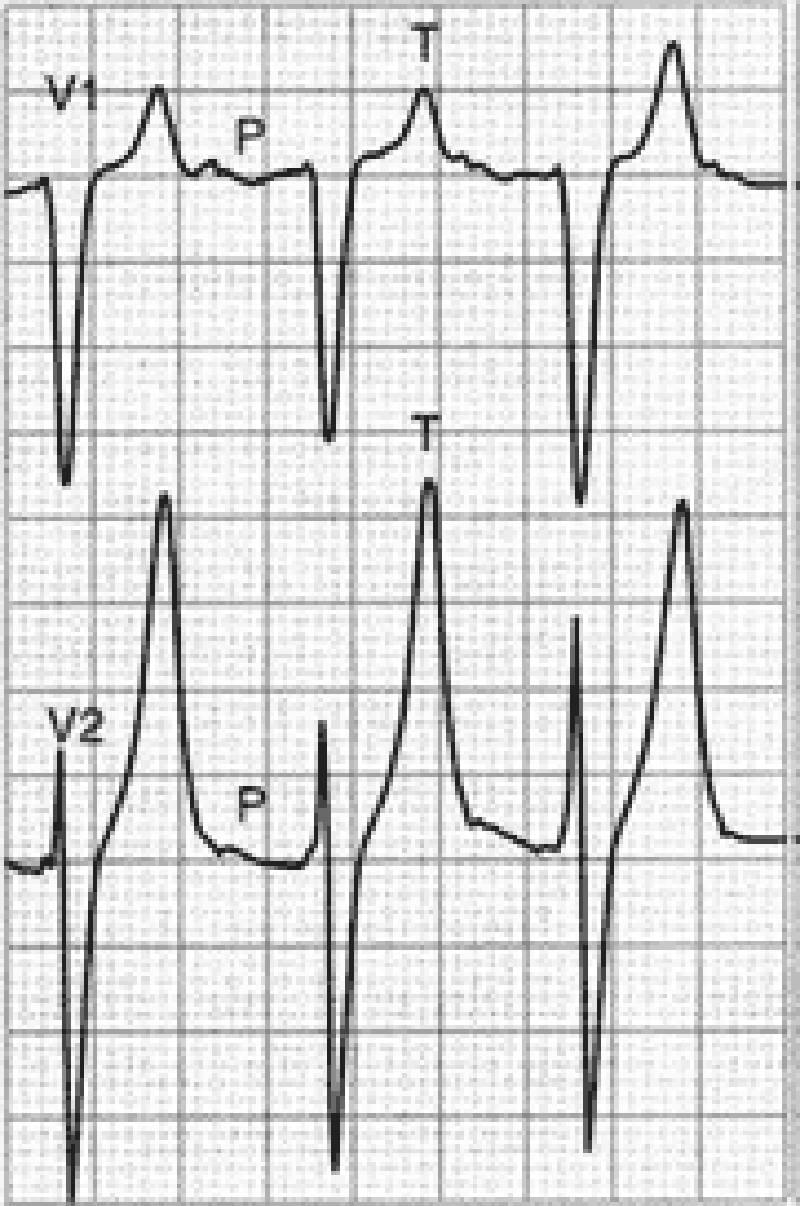
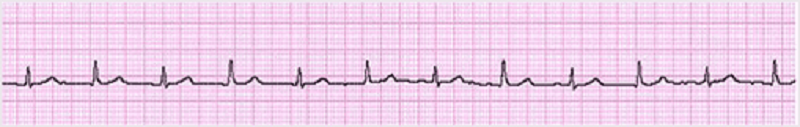
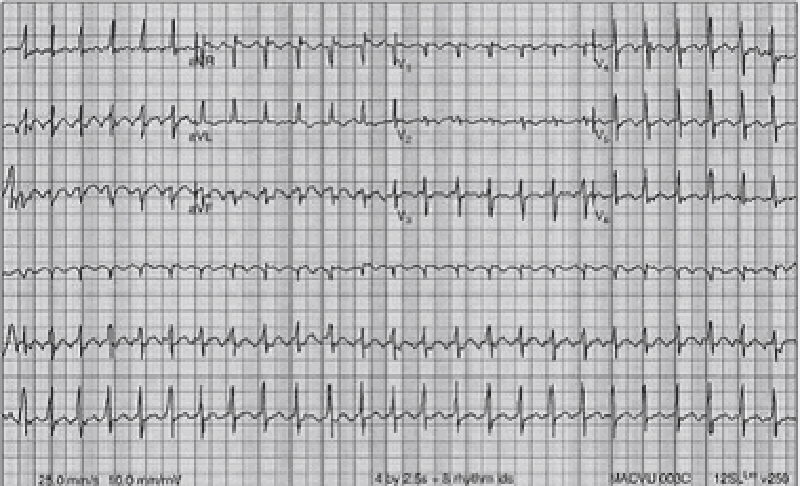
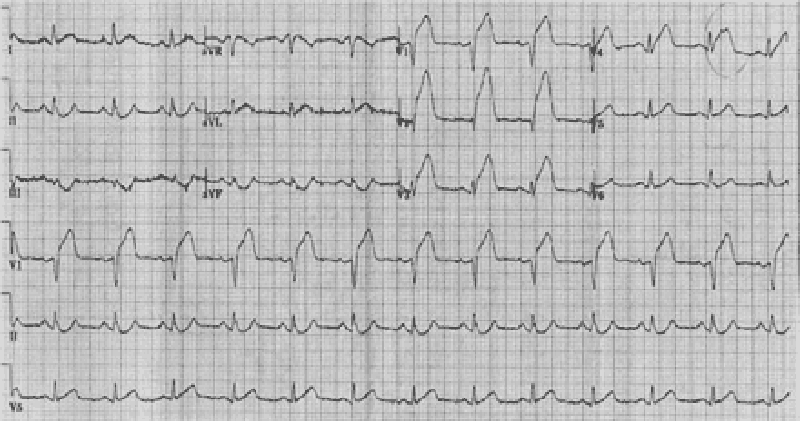
18) A 70-year-old male with a history of mild chronic kidney disease, diabetes mellitus, and CHF is admitted to your inpatient service with decreased urine output, weakness, and shortness of breath. He takes several medications but cannot remember their names. Labs are pending; his ECG is shown below. Based on the information available, what is the best initial step in management?
. Administration of intravenous insulin
. Administration of intravenous sodium bicarbonate
. Administration of intravenous 3% hypertonic saline
. Administration of oral sodium polystyrene sulfonate
. Administration of intravenous calcium gluconate
19) A 51-year-old man with a long history of hypertension presents to the ED complaining of intermittent chest palpitations lasting for a week. He denies chest pain, shortness of breath, nausea, and vomiting. He recalls feeling similar episodes of palpitations a few months ago but they resolved. His blood pressure (BP) is 130/75 mmHg, heart rate (HR) is 130 beats per minute, respiratory rate (RR) is 16 breaths per minute, and oxygen saturation is 99% on room air. An ECG is seen below. Which of the following is the most appropriate next step in management?
. Sedate patient for immediate synchronized cardioversion with 100 J
. Prepare patient for the cardiac catheterization laboratory
. Administer warfarin
. Administer amiodarone
. Administer diltiazem
20) An 82-year-old white female is admitted to the hospital for observation after presenting to the emergency department with dizziness. After being placed on a cardiac monitor in the ER, the rhythm strip below was recorded. There is no past history of cardiac disease, diabetes, or hypertension. With prompting, the patient discloses several prior episodes of transient dizziness and one episode of brief syncope in the past. Physical examination is unremarkable. Which of the following is the best plan of care?
. Reassurance. This is a benign condition, and no direct therapy is needed
. Reassurance. The patient may not drive until she is symptom free, but otherwise no direct therapy is needed
. Nuclear cardiac stress testing; treatment depending on results
. Begin therapy with aspirin
. Arrange placement of a permanent pacemaker
21) A 48-year-old man presents to the emergency department complaining of crushing substernal chest pain. He is diaphoretic, anxious, and dyspneic. His pulse is 110/min, blood pressure is 175/112 mmHg, respiratory rate is 30/min, and oxygen saturation is 94%. Aspirin, oxygen, sublingual nitroglycerin, and morphine are given, but they do not relieve his pain. ECG shows ST-segment elevation in leads V2 to V4. The duration of symptoms is now approximately 30 minutes. What is the most appropriate treatment for this patient at this time?
Calcium channel blocker
Intravenous angiotensin-converting enzyme inhibitor
Intravenous β-blocker
Magnesium sulfate
Tissue plasminogen activator
22) A 70-year-old woman presents to the emergency department complaining of dizziness. She is disoriented to the date and her location and it is difficult to gather an accurate history. Her pulse is 48/min, blood pressure is 84/60 mmHg, and respiratory rate is 12/min. On examination her extremities are cool and clammy. Her capillary refill time is 5 seconds. What is the most appropriate therapy?
Adenosine
Amiodarone
Atropine
Isoproterenol
Isoproterenol
23) A 64-year-old man in the surgical intensive care unit goes into rapid atrial fibrillation on postoperative day one after a decortication for a loculated pulmonary empyema. He is given an appropriate loading dose of digoxin, but 4 hours after his second dose, the patient complains of increased palpitations and dizziness. The patient is conscious and hemodynamically stable. STAT serum blood tests show a potassium level of 5.0 mEq/L; all other electrolytes, including divalents, are in the normal range. The digitalis level is above the therapeutic range at 4 ng/mL (therapeutic range 0.5-2 ng/mL). Results of cardiac telemetry are shown in the image. Which of the following should be administered immediately?
Calcium
Furosemide
Magnesium
Potassium
Sodium polystyrene sulfonate
24) A 49-year-old man presents to the clinic for a health maintenance visit. He has no complaints, but he requests a prescription for his “pressure pills,” as he lost his original prescription. On physical examination his blood pressure is 220/130 mmHg. Physical examination is otherwise within normal limits. Laboratory tests show: Na+: 142 mEq/L, K+: 3.8 mEq/L, Cl−: 105 mEq/L, Carbon dioxide: 25 mEq/L, Blood urea nitrogen: 20 mg/dL, Creatinine: 1.0 mg/dL, Glucose: 133 mg/dL. Urinalysis is within normal limits, and his ECG is normal. Which of the following is the most effective management?
Administer intravenous nitroprusside for management of hypertensive emergency
Administer intravenous nitroprusside for management of hypertensive urgency
Administer oral furosemide for management of hypertensive emergency
Administer oral metoprolol for management of hypertensive urgency
Administer sublingual nifedipine for management of hypertensive emergency
25) A 65-year-old man presents to the emergency department following the acute onset of palpitations. His wife states that he was eating dinner when he noticed the palpitations, lightheadedness, and shortness of breath. The patient has a history of treated hypertension, but no other medical history. The patient is not able to relate any meaningful history. Blood pressure is 80/40 mmHg, heart rate is 126/ min, respiratory rate is 20/min, and oxygen saturation is 99% on room air; he is afebrile. His heart rate is irregularly irregular with no murmurs, clicks, or rubs. Respiratory examination is unremarkable. X-ray of the chest shows no acute disease. ECG shows no discernible P waves and an irregularly spaced QRS response. Which of the following is the best first step in management?
Administration of adenosine
Cardiac catheterization and stent placement
Cardioversion to sinus rhythm
Carotid massage
Placement of dual lead pacemaker
26) A 65-year-old man develops palpitations and dizziness. His blood pressure is 80/50 mm Hg and his pulse is regular at 150/min. His ECG shows a “saw-toothed” pattern of P waves. Which of the following procedures is most appropriate in converting him back to sinus rhythm?
Carotid sinus pressure
Gagging procedures
Valsalva maneuver
Eyeball compression
Electrical cardioversion
28) A 57-year-old man complains of chest palpitations and light-headedness for the past hour. Five years ago he underwent a cardiac catheterization with coronary artery stent placement. He smokes half a pack of cigarettes daily and drinks a glass of wine at dinner. His HR is 140 beats per minute, BP is 115/70 mmHg, and oxygen saturation is 99% on room air. An ECG reveals a wide complex tachycardia at a rate of 140 that is regular in rhythm. An ECG from 6 months ago shows a sinus rhythm at a rate of 80. Which of the following is the most appropriate medication to treat this dysrhythmia?
Digoxin
Diltiazem
Amiodarone
Adenosine
Bretylium
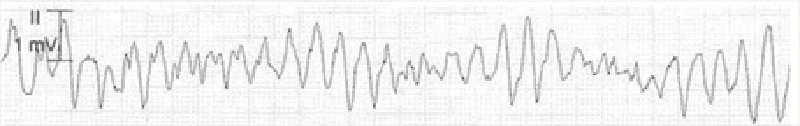
27) A 55-year-old man presents to the ED with worsening weakness, muscle cramps, and paresthesias. His past medical history is significant for hypertension and diabetes. He smokes one pack of cigarettes per day. On examination, the patient is alert and oriented and diffusely weak. An ECG is seen below. Which of the following is the most important next step in management?
Administer calcium gluconate
Administer insulin and dextrose
Administer aspirin and call the catheterization laboratory
Order an emergent head CT scan and get a neurology consult
Collect a sample of his urine to test for ketones
29) As you are examining the patient described in the previous question, he starts to complain of chest discomfort and shortness of breath and has another syncopal episode. His ECG is shown below. Which of the following is the most appropriate next step in management?
Call cardiology consult
Cardiovert the patient
Administer metoprolol
Administer amiodarone
Apply transcutaneous pacemaker
30) A 19-year-old woman was attacked while coming home from a party and is brought to the emergency department. She recalls being punched in the side of the head and stabbed in the left flank. Her speech is slow and she complains of a bad headache. Her pulse is 110/min, blood pressure is 90/50 mmHg, and respiratory rate is 25/min. On examination she has a stab wound at the left costal margin in the midaxillary line. Two large-bore intravenous lines are inserted, and after infusion of 2 L of lactated Ringer’s solution her blood pressure rises to 95/55 mmHg. What is the most appropriate next step in management?
Abdominal ultrasound
Diagnostic peritoneal lavage
Exploratory laparotomy
Noncontrast CT of the head
Peritoneal laparoscopy
31) A 20-year-old woman arrives at the emergency department actively seizing with QRS prolongation on ECG per paramedics. The patient’s roommate called emergency medical services after the patient collapsed, was not responsive to questioning, and began having clonic jerks bilaterally in her upper extremities. The patient’s roommate denies any knowledge of the patient consuming alcohol or illicit drugs. She does not believe the patient had any plan of harming herself, but does acknowledge that the patient has seemed “down” lately and was recently prescribed medication for generalized anhedonia. Which of the following is the most appropriate first-line treatment?
Activated charcoal
Diazepam
Flumazenil
Physostigmine
Sodium bicarbonate and diazepam
32) A 67-year-old woman is brought to the ED by paramedics complaining of dyspnea, fatigue, and palpitations. Her BP is 80/50 mmHg, HR is 139 beats per minute, and RR is 20 breaths per minute. Her skin is cool and she is diaphoretic. Her lung examination reveals bilateral crackles and she is beginning to have chest pain. Her ECG shows a narrow complex irregular rhythm with a rate in the 140s. Which of the following is the most appropriate immediate treatment for this patient?
Diltiazem
Metoprolol
Digoxin
Coumadin
Synchronized cardioversion
33) A 61-year-old woman with a history of congestive heart failure (CHF) is at a family picnic when she starts complaining of shortness of breath. Her daughter brings her to the ED where she is found to have an oxygen saturation of 85% on room air with rales halfway up both of her lung fields. Her BP is 185/90 mmHg and pulse rate is 101 beats per minute. On examination, her jugular venous pressure (JVP) is 6 cm above the sternal angle. There is lower extremity pitting edema. Which of the following is the most appropriate first-line medication to lower cardiac preload?
Metoprolol
Morphine sulfate
Nitroprusside
Nitroglycerin
Oxygen
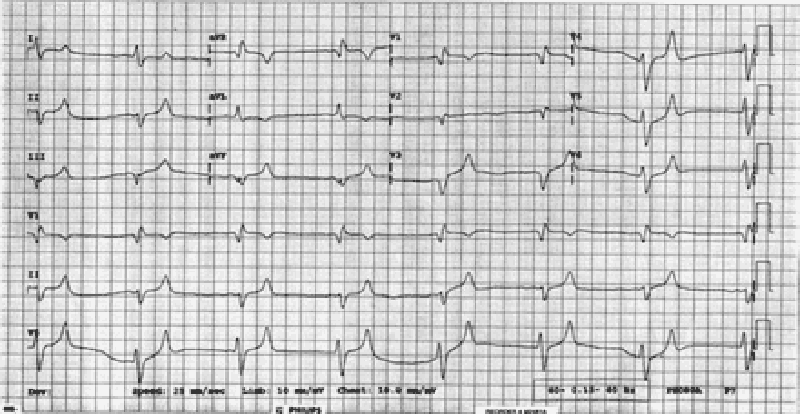
34) A 59-year-old man presents to the ED with left-sided chest pain and shortness of breath that began 1 hour ago. Initial vital signs are BP 85/45 mmHg, HR 105 beats per minute, RR 20 breaths per minute, and oxygen saturation 94% on room air. An ECG is seen below. Which of the following is the most appropriate definitive treatment?
Administer metoprolol or diltiazem
Electrical cardioversion
Administer calcium gluconate
Thrombolytic therapy
Percutaneous angioplasty
35) A 32-year-old man is stabbed in the left chest and presents to the emergency department in distress. His pulse is 130/min, blood pressure is 70/50 mmHg, and respiratory rate is 39/min. The stab wound is in the left fifth intercostal space in the midaxillary line. On examination his trachea is deviated to the right, jugular veins are distended bilaterally, and he has absent breath sounds and hyperresonance to percussion on the left side. Subcutaneous emphysema is palpated on the left thoracic wall. What is the best next step in management?
Chest tube thoracotomy
Diagnostic peritoneal lavage
Needle thoracostomy
Pericardiocentesis
Surgical exploration
36) In the ICU, a patient suddenly becomes pulseless and unresponsive, with cardiac monitor indicating ventricular tachycardia. The crash cart is immediately available. What is the best first therapy?
Amiodarone 150-mg IV push
Lidocaine 1.5-mg/kg IV push
Epinephrine 1-mg IV push
Defibrillation at 200 J
Defibrillation at 360 J
37) A 55-year-old African American female presents to the ER with lethargy and blood pressure of 250/150 mmHg. Her family members indicate that she was complaining of severe headache and visual disturbance earlier in the day. They report a past history of asthma but no known kidney disease. On physical examination, retinal hemorrhages are present. Which of the following is the best approach?
Intravenous labetalol therapy
Continuous-infusion nitroprusside
Clonidine by mouth to lower blood pressure
Nifedipine sublingually to lower blood pressure
Intravenous loop diuretic
38) A 36-year-old male presents with the sensation of a racing heart. His blood pressure is 110/70 mmHg, respiratory rate 14/minute, and O2 saturation 98%. His ECG shows a narrow QRS complex tachycardia with rate 180, which you correctly diagnose as paroxysmal atrial tachycardia. Carotid massage and Valsalva maneuver do not improve the heart rate. Which of the following is the initial therapy of choice?
Adenosine 6-mg rapid IV bolus
Verapamil 2.5 to 5 mg IV over 1 to 2 min
Diltiazem 0.25-mg/kg IV over 2 min
Digoxin 0.5 mg IV slowly
Electrical cardioversion at 50 J
39) A 56-year-old woman with a history of chronic renal disease presents to the emergency department because of severe, sharp, retrosternal chest pain that radiates to her jaw. The pain worsens when the patient lies down, and she is most comfortable leaning forward and hugging her knees. She takes erythropoietin, furosemide, calcitriol, and sodium polystyrene sulfonate. She is scheduled for dialysis three times per week, but she admits to sometimes missing sessions. She stopped drinking and smoking 20 years ago, and she has no family history of heart or renal problems. Auscultation of the heart reveals a friction rub. Laboratory tests show: WBC count: 12,000/mm3, Hemoglobin: 10.0 g/dL, Hematocrit: 30.0%, Platelet count: 150,000/mm3, Na+: 141 mEq/L, K+: 4.8 mEq/L, Cl: 101 mEq/L, HCO3 : 22 mEq/L, Blood urea nitrogen: 63 mg/dL, Creatinine: 3.2 mg/dL, Glucose: 111 mg/dL. The emergency medicine physician urges the patient to be more compliant with her dialysis, but the patient complains that she is too tired to go to dialysis all of the time and that it is ruining her life. Which of the following is the most likely complication if the patient’s condition remains untreated?
Cardiac tamponade
Decreased jugular venous pressure
Mitral regurgitation
Restrictive cardiomyopathy
Septic shock
40) A 39-year-old white man with essential hypertension presents for a routine health maintenance visit. He has no complaints and reports compliance with his hydrochlorothiazide. His pulse is 70/min, blood pressure is 145/92 mmHg, and respiratory rate is 16/min. His body mass index is 24 kg/m2. His physical examination is within normal limits. For which condition is the patient at increased risk?
End-stage renal disease
Hypercholesterolemia
Hypertrophic cardiomyopathy
Second-degree Mobitz I atrioventricular block
Type 2 diabetes mellitus
41) A 40-year-old man is brought to the emergency room after his wife found him alone in a confused state. He admits to overdosing in a suicide attempt, but does not specify the drug taken. En route to the hospital, he is drowsy and ataxic with blurred vision. His past medical history is significant for asthma, insomnia, depression, and substance abuse. His temperature is 38.3°C (100°F), blood pressure is 130/80mmHg, pulse is 100/min, and respirations are 22/min. Examination shows dry mucus membranes and skin; pupils are 8mm bilaterally. There is no neck stiffness. Lungs are clear to auscultation. Heart sounds are within normal limits. Abdominal examination shows reduced bowel sounds with no tenderness. A Foley catheter is placed in the ER and 600 ml of urine is collected over one hour. Which of the following is the most likely diagnosis?
. Salicylate intoxication
. Serotonin syndrome
. Cocaine intoxication
. Diphenhydramine poisoning
. Phencyclidine poisoning
42) A 46-year-old male is admitted to the hospital because of right hand cellulitis. He has a history of intravenous drug use, hepatitis C infection and septic arthritis of the knee. He smokes one pack of cigarettes and drinks one pint of vodka daily. He is started on vancomycin. On the following day, the swelling and redness of his arm decreases. However, he complains of bugs crawling on his skin. His temperature is 38.3°C (100.9°F), blood pressure is 160/90 mmHg, pulse is 110/min, and respirations are 18/min. Examination shows mild hand tremors and diaphoresis. Which of the following is the most appropriate next step in management?
. Start chlordiazepoxide
. Give haloperidol
. Start propranolol
. Stop vancomycin
. Start methadone
43) A 35-year-old woman is brought to the emergency room after an apparent suicide attempt. Her current prescription of imipramine was found at her bedside along with a suicide note. En route to the hospital, she suffered a seizure. She has been treated with many different anti-depressants over the past several years without improvement. Her temperature is 38.3°C (101°F), blood pressure is 90/50 mmHg, pulse is 120/min and respirations are 24/min. EKG shows QRS widening (0.18sec). She is given sodium bicarbonate along with supportive treatment. Which of the following is the most likely mechanism that explains the beneficial effects of sodium bicarbonate?
. Alkalinization of urine will promote diuresis of the antidepressants
. Acidification of urine will promote diuresis of the antidepressants
. Sodium load of sodium bicarbonate will alleviate depressant action on sodium channels
. Sodium load of sodium bicarbonate will alleviate depressant action on potassium channels
. Sodium load of sodium bicarbonate will alleviate depressant action on calcium channels
44) A 32-year-old male is admitted to the hospital because of confusion. He was recently diagnosed with schizophrenia His temperature is 38.6°C (101.6°F), blood pressure is 160/100 mmHg, pulse is 116/min, and respirations are 22/min. He is not oriented to time, place or person. Mucus membranes are dry. Profuse diaphoresis is present. Lungs are clear to auscultation. Abdominal, neck and extremity muscles are rigid. Muscle tone is increased. Deep tendon reflexes are 2+. Laboratory studies show a serum CK of 50,000 IU/L. CSF fluid analysis shows a total white blood cell count of 5/microL. Which of the following is the most appropriate next step in management?
. Risperidone
. Dantrolene
. L-Dopa
. Prednisone
. Antibiotics
45) A 38-year-old homeless man is brought to the emergency room. He is obtunded and unable to speak. No previous medical history is known. His temperature is 34.0°C (93.2°F), blood pressure is 90/60 mmHg, pulse is 60/min and respirations are 6/min. Oxygen saturation is 86% on room air. Pupils are 5 mm in size, bilaterally. Oropharynx is dry. Lungs are clear to auscultation. Abdomen is soft; bowel sounds are decreased; there is no organomegaly. Extremities reveal several needle marks. Babinski sign is negative. Deep tendon reflexes are 2+ throughout. Which of the following is the most appropriate next step in management?
. CT scan of the head
. Glucagon
. Methadone
. Naloxone
. Flumazenil
46) A mother brings her 16-year-old daughter to the ER after she had two episodes of coffee ground emesis. The mother reports that for the past two weeks, the teen has not been acting like herself; she has been especially isolated and has had a poor appetite and poor sleep. Her medical history is significant for anemia, for which she takes iron sulfate and folic acid. She also takes acetaminophen for occasional back pain. Presently, the patient's blood pressure is 110/70 mmHg and heart rate is 120/min. Which of the following is most likely to establish the diagnosis?
. Liver function tests
. Upper GI endoscopy
. Serum iron level
. CT scan of the head
. Serum acetaminophen level
47) A 47-year-old man is brought to the ED by EMS after being found wandering in the street mumbling. His BP is 150/75 mmHg, HR is 110 beats per minute, temperature is 100.5°F, RR is 16 breaths per minute, oxygen saturation is 99% on room air, and fingerstick glucose is 98 mg/dL. On examination, the patient is confused with mumbling speech. His pupils are dilated and face is flushed. His mucous membranes and skin are dry. Which of the following toxic syndromes is this patient exhibiting?
. Sympathomimetic syndrome
. Anticholinergic syndrome
. Cholinergic syndrome
. Opioid syndrome
. Ethanol syndrome
48) A 25-year-old man is carried into the ED by two of his friends who state that he is not breathing. The patient has a history of heroin abuse. His vital signs are BP 115/70 mmHg, HR 99 beats per minute, temperature 98.9°F, RR 3 breaths per minute, and oxygen saturation 87% on room air. You notice fresh needle marks and miotic pupils. You begin bag-valvemask ventilation and his oxygen saturation increases to 99%. Which of the following is the most appropriate next step in management?
. Continue bag-valve-mask ventilation until he breathes on his own
. Perform endotracheal intubation of the patient
. Evaluate response to administration of naloxone
. Put the patient on supplemental oxygen
. Place a nasogastric tube and administer activated charcoal
49) A 42-year-old man who is actively seizing is brought to the ED by EMS after a massive ingestion of an unknown substance. The man is known to have a history of acquired immunodeficiency syndrome (AIDS). An intravenous (IV) line is established and anticonvulsant therapy is administered. After high doses of diazepam, phenobarbital, and phenytoin, it is determined that the seizures are refractory to standard anticonvulsant therapy. Which of the following substances did this patient most likely ingest?
. Cocaine
. Diphenhydramine
. Tricyclic antidepressant (TCA)
. Haloperidol
. Isoniazid (INH)
50) A 26-year-old man is brought to the emergency room by police with depressed mental status. Out of fear of arrest, he swallowed a handful of pills as the police officers approached him. On examination, he responds to painful stimuli but is somnolent. His respiratory rate is 8/min and after naloxone bolus infusion increases to 12/min. Lungs are clear to auscultation. Which of the following additional findings is most likely to be present in this patient?
. Miosis, bradycardia, hypertension
. Miosis, tachycardia, hypotension
. Miosis, bradycardia, hypotension
. Miosis, tachycardia, hypertension
. Mydriasis, tachycardia, hypertension
51) A 29-year-old male is brought to the emergency room because of sudden onset confusion and fever. He was recently admitted to the hospital for hallucinations and was discharged instable condition. His temperature is 38.6°C (101.6°F), blood pressure is 150/100 mmHg, pulse is 112/min, and respirations are 24/min. Mucus membranes are dry. Profuse diaphoresis is present. Lungs are clear to auscultation. Abdominal muscles are rigid. Muscle tone is increased; "lead pipe rigidity" is noted in all four extremities. Deep tendon reflexes are 2+. Tremor is noted. Which of the following is the most likely diagnosis?
. Tetanus
. Meningitis
. Drug induced idiosyncratic reaction
. Cocaine intoxication
. Lithium intoxication
52) A 26-year-old man is brought to the emergency room after an attempted suicide by medication overdose. For the past hour, he has suffered two seizures. His temperature is 38.8°C (102°F), blood pressure is 110/85 mmHg, pulse is 90/min, and respirations are 22/min. He is not oriented to time, place, and person. Pupils are dilated, but reactive to light and accommodation; skin is flushed and dry. Abdominal examination shows reduced bowel sounds. EKG shows prolonged QRS complexes (0.19 sec). Toxicology studies are pending. Which of the following is the most appropriate indicator of severity of intoxication?
. Serum drug levels
. Urine drug levels
. Duration of QRS complex
. Pupillary size
. Bowel sounds
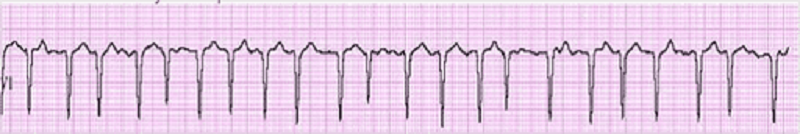
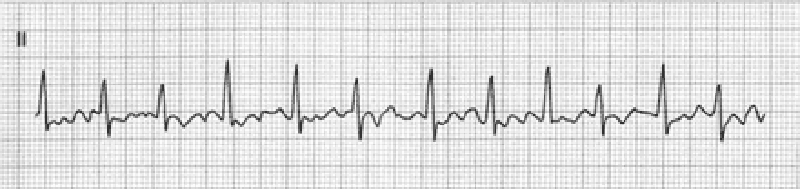
53) A 42-year-old male is admitted to the hospital with fever and shortness of breath. He has HIV infection, hepatitis C infection, and alcohol induced cardiomyopathy. His temperature is 38.6°C (101.5°F). Thrush is noted in the oropharynx. Chest x-ray reveals right lower lobe consolidation. He is started on fluconazole and moxifloxacin. His pneumonia and thrush improve over the next 2 days. However, on the third day, he develops palpitations. His EKG strip is shown below. Which of the following is the most appropriate next step in management?
. Calcium gluconate
. Magnesium sulphate
. Sotalol
. Amiodarone
. Adenosine
54) A 34-year-old homeless man is brought to the emergency room in a confused state. He complains of epigastric pain, vomiting and blurred vision. His temperature is 36.8°C (98.2°F), blood pressure is 110/60 mmHg, pulse is 110/min and respirations are 22/min. Physical examination shows poor oral hygiene and dry mucous membranes. Lungs are clear to auscultation. Abdominal exam shows mild epigastric discomfort. Funduscopic examination reveals optic disc hyperemia. Laboratory studies show: Serum sodium 136 mEq/L, Serum potassium 3.0 mEq/L, Chloride 93 mEq/L, Bicarbonate 6 mEq/L, Blood urea nitrogen (BUN) 30 mg/dL, Serum creatinine 0.8 mg/dL, Blood glucose 80 mg/dL, Serum ketones negative, Plasma lactate 2.2 mEq/L. Which of the following is the most likely cause of his symptoms?
. Ethylene glycol poisoning
. Mesenteric ischemia
. Septic shock
. Diabetic ketoacidosis
. Methanol poisoning
55) You receive notification from EMS that they are bringing in a 17-yearold adolescent boy who was found unconscious by a police officer. The police officer at the scene states that he snuck up on a group of kids that he thought were using drugs. Two of them got away and one just fell to the ground seconds after standing up. Lying on the ground next to the adolescent were plastic bags. The emergency medical technician (EMT) states that the patient was in ventricular fibrillation. He was shocked in the field and is now in a sinus rhythm. The EMT also administered IV dextrose, thiamine, and naloxone without any change in mental status. Which of the following substances was the patient most likely abusing?
. Butane
. Ethanol
. Heroin
. Cocaine
. PCP
56) A 61-year-old man with a history of depression and hypertension is brought to the ED by EMS for altered mental status. The patient’s wife states that he stopped taking his fluoxetine 1 month ago and now only takes metoprolol for his hypertension. The patient’s BP is 75/40 mmHg, HR is 39 beats per minute, RR is 14 breaths per minute, oxygen saturation is 99% on 100% oxygen, and fingerstick glucose is 61 mg/dL. The patient is awake and moaning, responding only to deep stimuli. His extremities are cool to the touch. You suspect an overdose of metoprolol. You endotracheally intubate the patient for airway control. Which of the following is the most appropriate next step in management?
. Normal saline bolus, administer atropine, administer 1-g calcium gluconate bolus, then insert a transvenous cardiac pacer
. Put the patient on pacer pads, then administer norepinephrine drip
. Cardioversion with 200 J, then administer atropine
. Normal saline bolus, atropine, norepinephrine
. Normal saline bolus, atropine, glucagon
57) A 22-year-old woman presents to the ED by ambulance from a dance club. The paramedics report that the patient was agitated in the club and had a generalized seizure. Her BP is 165/100 mmHg, HR is 119 beats per minute, temperature is 101.9°F, RR is 17 breaths per minute, oxygen saturation is 98% on room air, and fingerstick glucose is 92 mg/dL. On examination, the patient is hyperactive and appears to be hallucinating. Her pupils are dilated to 6 mm bilaterally and reactive. Her neck is supple. Examination of the heart is unremarkable except for tachycardia. Her lungs are clear and abdomen is soft and nontender. The patient moves all four extremities. Laboratory results are as follows: Sodium 109 mEq/L, WBC 12,000/mm3, Potassium 3.5 mEq/L, Hct 49%, Chloride 83 mEq/L, Platelets 350/μL, Bicarbonate 20 mEq/L, BUN 10 mg/dL, Creatinine 1 mg/dL, Glucose 103 mg/dL. Which of the following substances did this patient most likely consume?
. Cocaine
. Heroin
. 3,4-Methylenedioxymethamphetamine (MDMA)
. Ketamine (special K)
. PCP
58) A 32-year-old woman is brought to the emergency department by her husband because of slurred speech and difficulty walking. She has also been very drowsy for the past several hours, a non-typical behavior for a very active woman. She has a history of bipolar disorder, insomnia, migraine headaches, seizures and hypothyroidism. Her temperature is 37°C (98.6°F), blood pressure is 110/70 mmHg, pulse is 76/min, and respirations are 16/min. She is lethargic and falls asleep during the interview and physical examination. Pupils are 5 mm in size and reactive to light. Neck is supple. Oropharynx is clear. Chest auscultation is unremarkable. Abdomen is soft and non-tender; bowel sounds are normal. Limited neurologic examination shows 1+ deep tendon reflexes in all four extremities; there is no Babinski sign; strength is 5/5 throughout. There is no nystagmus or hand tremor. Blood sugar is 130 mg/dL. Which of the following is the most likely cause of her symptoms?
. Cerebrovascular accident
. Phenytoin toxicity
. Benzodiazepine overdose
. Ethanol intoxication
. Lithium toxicity
59) A 31-year-old woman with a known psychiatric history presents to the ED after ingesting an unknown quantity of pills from her medication vial. In the ED, she complains of nausea, abdominal cramping, and feels unsteady on her feet. On physical examination, you observe that she is tachycardic and ataxic. Which of the following substances will best be treated by activated charcoal that could present like this?
. Phenobarbital
. Carbamazepine
. Lye (sodium hydroxide)
. Lithium
. Acetaminophen
60) A 27-year-old man presents to the ED extremely agitated complaining of mild chest pain and dyspnea. He states that he was snorting cocaine all afternoon. You place him on a monitor and get his vital signs. His BP is 215/130 mmHg, HR is 112 beats per minute, temperature is 100.1°F, RR is 17 breaths per minute, and oxygen saturation is 98% on room air. An ECG reveals sinus tachycardia at a rate of 116. Which of the following is the most appropriate medication to administer?
. Haloperidol
. Labetalol
. Esmolol
. Diltiazem
. Diazepam
61) A 30-year-old man is brought to the ED by police officers. The patient is agitated, vomiting, and complaining of body aches. He states that he is withdrawing from his medication. His vital signs are BP 160/85 mmHg, RR 20 breaths per minute, HR 107 beats per minute, and temperature 99.7°F. On examination he is diaphoretic, has rhinorrhea, piloerection, and hyperactive bowel sounds. Which of the following substances is this patient most likely withdrawing from?
. Ethanol
. Cocaine
. Nicotine
. Methadone
. Clonidine
62) A 25-year-old man is brought into the ED by two police officers because of suspected drug use. The patient is extremely agitated and is fighting the police officers. It takes three hospital staff members and the two police officers to keep him on the stretcher. His vital signs are BP 150/80 mmHg, HR 107 beats per minute, temperature 99.7°F, RR 18 breaths per minute, and oxygen saturation 99% on room air. Physical examination is unremarkable except for cool, diaphoretic skin, persistent vertical and horizontal nystagmus, and occasional myoclonic jerks. Which of the following is the most likely diagnosis?
. Cocaine intoxication
. Cocaine withdrawal
. Anticholinergic toxidrome
. PCP intoxication
. Opiate withdrawal
63) A 20-year-old female is brought to the emergency room after getting struck by a motor vehicle. She appears confused. According to her parents, she has no other medical problems and does not take any prescription medications. However, they have noticed her increase in appetite recently. She occasionally drinks alcohol and smokes half a pack of cigarettes daily. Her temperature is 37.2°C (99°F), blood pressure is 150/90mmHg, pulse is 110/min, and respirations are 22/min. Examination reveals dry mouth and conjunctival injection. Pupils are equal, reactive to light and accommodation. She has impaired time orientation and shortterm memory. Which of the following is the most likely explanation for this patient's symptoms?
. Benzodiazepine overdose
. Opioid overdose
. Cocaine intoxication
. Alcohol intoxication
. Marijuana overdose
64) A 34-year-old male is brought to the emergency department by his neighbor. The neighbor found the man lying on the floor beside an empty bottle of unknown substance. At the hospital, the patient is conscious and alert, but in severe pain. His temperature is 36.8°C (98.2°F), blood pressure is 130/70 mmHg, pulse is 90/min and respirations are 20/min. Abdomen is benign, with normal bowel sounds. Pupils are 5 mm, bilaterally. His tongue is white, heavy drooling of saliva is noted and he is unable to swallow. Which of the following is the most likely explanation for this patient's symptoms?
. Anticholinergic poisoning
. Caustic poisoning
. Tricyclic antidepressant poisoning
. Cyanide poisoning
. Alcohol intoxication 65
65) A 35-year-old woman calls her family physician after her 7-year old son accidentally splashed an unknown liquid containing acid on his face. Some liquid likely entered his eye, as the child is complaining of severe pain in his right eye. She knows a doctor living in her immediate neighborhood but is hesitant about what to do next. Which of the following is the most appropriate initial course of action that the mother should take?
. Call 911 immediately
. Go to local emergency room immediately
. Go to the doctor in the neighborhood immediately
. Wash the eye with copious amount of water
. Do not try to wash the eye as it can enhance the damage
66) A worried and anxious pregnant mother brings her 3-year-old son to the emergency room after he experienced several episodes of vomiting and abdominal pain for the past two hours. His vomit is coffee ground in appearance. He is irritable and lethargic. His blood pressure is 80/50mmHg and pulse rate is 120/min. Examination shows a normal oropharynx; chest auscultation is within normal limits. Abdomen is soft and mildly tender at the epigastrium; there is no hepatosplenomegaly. Extremities are cold to touch. Initial laboratory studies show: Hemoglobin 10.3 g/L, Leukocyte count 14,500/mm3, Bicarbonate 18 mEq/L. Chest x-ray is within normal limits. Abdominal imaging shows radio opaque tablets in the stomach. Intravenous normal saline is started. Which of the following is the most appropriate next step in management?
. Sodium bicarbonate
. Deferoxamine
. Magnesium sulphate
. Hemodialysis
. Calcium EDTA
67) A 32-year-old male comes to the hospital complaining of pain, swelling and redness of his right arm. His past medical history is significant for substance abuse. His temperature is 38.9°C (102.0°F), blood pressure is 110/60 mmHg, pulse is 110/min and respirations are 14/min. He is started on intravenous clindamycin. The next day the swelling and pain improve, but he develops nausea, vomiting, abdominal cramps and diarrhea. He is restless and asks for pain medication to treat his aching muscles and joints. His temperature now is 37.3°C (99.1°F), blood pressure is 120/70 mmHg, pulse is 80/min and respirations are 16/min. His laboratory studies at the time of admission and the following day show: Hemoglobin 13.0 g/L (12.8 g/L), Leukocyte count 17,500/mm3 (8,500/mm3), NeutrophiIs 86% (64%), Lymphocytes 14% (26%). Which of the following is the most appropriate next step in management?
. Stool for Clostridium difficile toxin
. Discontinue clindamycin
. Start chlordiazepoxide
. Start methadone
. Start intravenous morphine
68) A 34-year-old homeless male is brought to the ER in a confused state. He complains of flank pain. His past medical history is unknown. His temperature is 36.8°C (98.2F), blood pressure is 110/60 mmHg, pulse is 110/min and respirations are 22/min. His appearance is disheveled. Pupils are equal, 4 mm in size and reactive to light. Funduscopic examination is within normal limits. Lungs have crackles at both bases. Mild costovertebral angle tenderness is present. Foley catheter is placed and urine appears red. Laboratory studies show: Serum sodium 136 mEq/L, Serum potassium 3.5 mEq/L, Chloride 93 mEq/L, Bicarbonate 6 mEq/L, Blood urea nitrogen (BUN) 34 mg/dl, Serum creatinine 2.8 mg/dl, Blood glucose 80 mg/dl, Calcium 6.5 mg/dl, Serum ketones negative, Plasma lactate 2.4 mEq/L. Which of the following is the most appropriate next step in management?
. Broad spectrum antibiotics
. Fomepizole
. N-acetylcysteine
. Regular insulin
. Glucagon
69) A 26-year-old bar employee is brought to the emergency room because of agitated, combative behavior in which three people had to restrain her. She has also been hallucinating during this entire period. Her temperature is 37.7°C (100°F), blood pressure is 160/90 mmHg, pulse is 126/min, and respirations are 18/min. She is confused and agitated during the examination. Pupils are 6 mm in diameter and respond to light; prominent nystagmus is present. The remainder of her examination is unremarkable. Which of the following is the most likely diagnosis?
. Barbiturate intoxication
. Phencyclidine intoxication
. Cocaine intoxication
. Marijuana Intoxication
. Opioid intoxication
70) A 38-year-old man is brought to the emergency room by EMS after an apparent suicide attempt. En route to the hospital, he appeared confused and suffered a seizure. He has a history of hypertension and major depression. His temperature is 37.7°C (100°F), blood pressure is 70/40 mmHg, pulse is 40/min, and respirations are 12/min. Examination shows normal heart sounds and diffuse wheezing. Extremities are cold and clammy. EKG shows AV block. The patient is given intravenous fluids and atropine; however, his bradycardia and hypotension do not improve. Which of the following is the most appropriate next step in management?
. Epinephrine
. Aminophylline
. Digoxin specific antibody
. Glucagon
. Pacemaker
71) A 24-year-old woman is brought to the emergency room after ingesting 14 acetaminophen tablets, 500 mg each, two hours ago. She does not smoke but drinks alcohol on the weekends. She is alert and oriented. Her temperature is 37.2°C (99°F), blood pressure is 110/60mmHg, pulse is 90/min and respirations are 18/min. Examination shows no abnormalities. Laboratory studies show: Hct 40%, WBC 6,000/mm3, Platelet 390,000/mm3. Which of the following is the most appropriate next step in management?
. Administer the loading dose of N-acetylcysteine
. Obtain serum acetaminophen levels in two hours
. Obtain serum acetaminophen levels now
. Transfer to liver transplantation facility
. Discharge her home without further work up
72) A group of teenagers attend an indoor barbecue on a cold winter night. They all ate servings of potato salad and barbecue chicken. A few hours later, they present to the local emergency room with headache, nausea, vomiting, vague abdominal discomfort and confusion. One of the teenagers mentions a pet dog that was in the room with them had similar symptoms. A quick physical examination of one patient reveals tachycardia, tachypnea and a pinkish-skin hue. Which of the following is the most likely diagnosis?
. Viral illness
. Carbon monoxide poisoning
. Acute gastroenteritis
. Cyanide poisoning
. Methemoglobinemia
73) A 40-year-old man is brought to the emergency room for retrosternal and epigastric pain after ingesting an unknown amount of "lye" (drain cleaner) 45 minutes ago. His past medical history is significant for major depression and suicide attempt. He is unable to swallow his saliva and is drooling. His temperature is 36.8°C (98.2°F), blood pressure is 120/70 mmHg, pulse is 110/min, and respirations are 20/min. Examination shows oropharyngeal erythema and edema. Lungs are clear to auscultation. Abdominal examination reveals tenderness at the epigastrium without rebound or guarding. Chest x-ray shows no abnormalities. Intravenous hydration is started. Which of the following is the most appropriate next step in treatment?
. Gastric decontamination with ipecac
. Administer activated charcoal in water
. Neutralization and dilution of the alkali
. Upper gastrointestinal contrast studies and endoscopy
. Administer high dose systemic steroids
74) A 34-year-old farmer is brought to the hospital after attempting suicide. His body and clothes are soiled with vomitus. He is short of breath and appears agitated. His family reports no previous medical history or regular use of prescription medications. His temperature is 36.6°C (98°F), blood pressure is 110/60 mmHg, pulse is 50/min, and respirations are 22/min. His oxygen saturation is 86% on room air. Examination shows watering of the eyes and 1 mm pupils, bilaterally. Lung examination shows widespread rhonchi with prolonged expiration. Abdominal examination shows increased bowel sounds. Neurologic examination shows muscle fasciculations. What would be the most appropriate next step in management of this patient?
. Obtain EKG for QRS duration
. Remove all the clothing and wash the body
. Obtain a chest x-ray
. Obtain a head CT scan
. Give physostigmine
75) A 60-year-old male is found lying down on the street by police one winter morning. He has been taking ibuprofen for headaches, fluphenazine for his schizophrenia and amitriptyline for chronic painful neuropathy secondary to post-herpetic neuralgia. He is also receiving cephalexin for cellulitis of the right lower leg. His temperature is 34°C (90°F), blood pressure is 80/50 mmHg, pulse is 88/min, and respirations are 12/min. Which of the following medications most likely have contributed to the development of hypothermia in this patient?
. Ibuprofen
. Amitriptyline
. Cephalexin
. Fluphenazine
. Glucagon
76) A 45-year-old woman is brought to the ER by ambulance after a neighbor found her to be in a somewhat obtunded state with an empty bottle of medication next to her. While en route to the ER she suffered a tonic clonic seizure. Her past medical history is significant for major depression. Her temperature is 38.3°C (100.9°F), blood pressure is 90/70 mmHg, pulse is 120/min, and respirations are 16/min. She is able to respond to painful stimuli. Pupils are 8 mm in size bilaterally. Skin is warm and flushed. Lungs are clear to auscultation. Abdomen is soft and non-tender. Bowel sounds are decreased. There is no neck stiffness. EKG shows QRS duration of 130 msec, a change from her previous EKG a month ago. Which of the following is the most appropriate next step in management?
. Lumbar puncture
. Echocardiogram
. Thyroid function tests
. Calcium gluconate
. Sodium bicarbonate
77) After being fired from his job, a 35-year-old man attempts suicide by drinking from a bottle labeled “insecticide.” Three hours later, emergency medical services (EMS) brings him into the emergency department (ED) and you notice that he is extremely diaphoretic, drooling, and vomiting. He is awake but confused. His vital signs include a blood pressure (BP) of 170/90 mmHg, heart rate (HR) of 55 beats per minute, respiratory rate (RR) of 22 breaths per minute, temperature of 98.6°F, and oxygen saturation of 95% on room air. Physical examination demonstrates pinpoint pupils and crackles and wheezing on lung examination. What is the treatment to reverse this patient’s poisoning?
. Naloxone
. N-acetylcysteine (NAC)
. Atropine and pralidoxime (2-PAM)
. Flumazenil
. Physostigmine
78) A 19-year-old man is brought to the ED by EMS after he was found lying on the floor at a dance club. EMS states that the patient seemed unconscious at the dance club, but as soon as they transferred him onto the gurney, he became combative. Upon arrival in the ED, his BP is 120/65 mmHg, HR is 75 beats per minute, temperature is 98.9°F, RR is 12 breaths per minute, and oxygen saturation is 98% on room air. On physical examination, his pupils are midsized, equal, and reactive to light. His skin is warm and dry. Lung, cardiac, and abdominal examinations are unremarkable. As you walk away from the bedside, you hear the monitor alarm signaling zero respirations and the oxygen saturation starts to drop. You perform a sternal rub and the patient sits up in bed and starts yelling at you. As you leave him for the second time, you hear the monitor alarm again signal zero respirations. You administer naloxone, but there is no change in his condition. Which of the following is most likely the substance ingested by this patient?
. γ-Hydroxybutyrate (GHB)
. Diazepam
. Cocaine
. Phencyclidine (PCP)
. Heroin
79) A 43-year-old woman presents to the ED with a 3-week history of intermittent headache, nausea, and fatigue. She was seen at her private doctor’s office 1 week ago along with her husband and children, who also have similar symptoms. They were diagnosed with a viral syndrome and told to increase their fluid intake. She states that the symptoms began approximately when it started to get cold outside. The symptoms are worse in the morning and improve while she is at work. Her BP is 123/75 mmHg, HR is 83 beats per minute, temperature is 98.9°F, and oxygen saturation is 98% on room air. Physical examination is unremarkable. You suspect her first diagnosis was incorrect. Which of the following is the most appropriate next step to confirm your suspicion?
. Order a mono spot test
. Perform a nasal pharyngeal swab to test for influenza
. Consult psychiatry to evaluate for malingering
. Order a carboxyhemoglobin (COHb) level
. Order a lead level
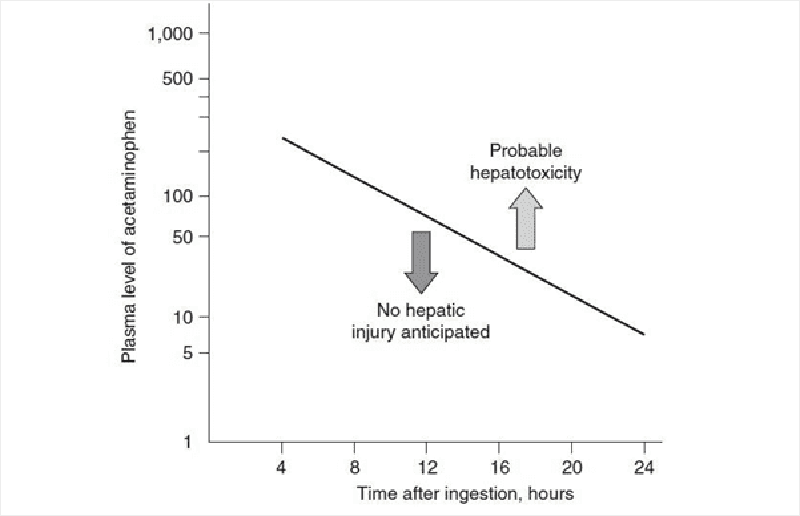
80) An 18-year-old woman is brought to the ED by her mother. The patient is diaphoretic and vomiting. Her mom states that she thinks her daughter tried to commit suicide. The patient admits to ingesting a few handfuls of acetaminophen (Tylenol) approximately 3 hours ago. Her temperature is 99.1°F, BP is 105/70 mmHg, HR is 92 beats per minute,RR is 17 breaths per minute, and oxygen saturation is 99% on room air. On examination, her head and neck are unremarkable. Cardiovascular and pulmonary examinations are within normal limits. She is mildly tender in her right upper quadrant, but there is no rebound or guarding. Bowel sounds are normoactive. She is alert and oriented and has no focal deficits on neurologic examination. You administer 50 g of activated charcoal. At this point, she appears well and has no complaints. Her serum acetaminophen (APAP) concentration 4 hours after the reported time of ingestion returns at 350 μg/mL. You plot the level on the nomogram seen below. Which of the following is the most appropriate next step in management?
. Discharge home with instructions to return if symptoms return
. Observe for 6 hours and, if the patient still has no complaints, discharge her home
. Repeat the acetaminophen level 4 hours after the patient arrived in the ED. Treat only if this level is above the line
. Admit to the psychiatry unit and keep on suicide watch while performing serial abdominal examinations.
. Begin NAC and admit to the hospital
81) A 60-year-old woman with a history of diabetes is brought into the ED by EMS workers who state that the patient was found on a bus in a lethargic and diaphoretic condition. Her fingerstick glucose level at the scene was 35 mg/dL. EMS workers quickly administered dextrose through an IV line. The patient became alert and responsive, stating that she just took her normal medication. Her blood sugar went up to 110 mg/dL and she remained this way throughout her trip to the ED. However, in the ED you notice that the patient is again diaphoretic and is mumbling her speech. Her fingerstick glucose is now 47 mg/dL. You administer dextrose and she perks right up. Which of the following diabetes medications commonly causes hypoglycemia for which the patient is likely to require hospital admission?
. Regular insulin
. Metformin
. Glyburide
. Sitagliptin
. Acarbose
82) A 23-year-old woman presents to the ED complaining of abdominal pain, nausea, and vomiting. She has a history of depression but is not currently taking any antidepressant medications. Upon further questioning, the patient states that she ingested a bottle of pills in her medicine cabinet approximately 3 hours ago. Her BP is 115/65 mmHg, HR is 101 beats per minute, temperature is 100.1°F, RR is 29 breaths per minute, and oxygen saturation is 100% on room air. Physical examination is unremarkable except for mild diffuse abdominal tenderness. Laboratory results reveal a white blood cell (WBC) count of 10,300/μL, hematocrit 46%, platelets 275/μL, aspartate transaminase (AST) 70 U/L, alanine transaminase (ALT) 85 U/L, alkaline phosphatase 75 U/L, sodium 143 mEq/L, potassium 3.7 mEq/L, chloride 98 mEq/L, bicarbonate 8 mEq/L, blood urea nitrogen (BUN) 22 mg/dL, creatinine 0.9 mg/dL, and glucose 85 mg/dL. Arterial blood gas values on room air are pH 7.51, PCO2 11 mm Hg, and PO2 134 mm Hg. Which of the following substances did this patient most likely ingest?
. Diphenhydramine
. Ibuprofen
. Acetaminophen
. Aspirin
. Pseudoephedrine
83) A 35-year-old agitated man presents to the ED in police custody. He denies any past medical history and takes no medication. He admits to using some drugs today. His BP is 195/90 mmHg, HR is 121 beats per minute, temperature is 100.1°F, RR is 18 breaths per minute, and oxygen saturation is 99% on room air. On examination, he is diaphoretic, and has pupils that are 8 mm in diameter, along with 3+ patella reflexes bilaterally. Electrocardiogram (ECG) reveals sinus tachycardia with a rate of 123. Which of the following toxic syndromes is this patient exhibiting?
. Anticholinergic
. Cholinergic
. Sympathomimetic
. Opioid
. Sedative hypnotic
{"name":"DES 2016. Final (Part24)", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"278) A 65-year-old man complains of periodic back pain radiating to his thigh and buttock. The pain is related to walking or climbing the stairs but is promptly relieved by leaning forward. He also has noticed tingling and numbness in both lower extremities. He has a history of hypertension and takes hydrochlorothiazide. He does not use tobacco, alcohol, or illicit drugs. His pulse is 76\/min, respirations are 14\/min, and blood pressure is 140\/80 mmHg. Lumbar extension reproduces the pain and tingling, while lumbar flexion relieves the symptoms. Which of the following is the most likely cause of this patient's condition?, 279) A 51-year-old Caucasian female complains of low-back pain radiating to the buttocks. She also complains of persistent muscle pain that gets worse with exercise. Physical examination reveals normal muscle strength. Her joints are not swollen, but palpation over the outer upper quadrants of the buttocks and the medial aspect of the knees elicits tenderness. Her ESR is 12mm\/hr. Which of the following is the most likely diagnosis?, 280) A 27-year-old male presents to the physician's office because of pain on the medial side of the tibia just below the knee. The pain does not radiate and is continuous. He relates the onset of his pain to falling on the ground while playing football two weeks ago. He denies fever, malaise and weight loss. His past medical history is not significant. On examination, a well-defined area of tenderness is present on the upper tibia below the medial knee joint. There is no redness, warmth or swelling. His gait is normal. A valgus stress test has no effect on his pain. X-ray of the knee and tibia shows no abnormalities. Which of the following is the most likely cause of his current symptoms?","img":"https://cdn.poll-maker.com/11-493528/defibrilla.png?sz=1200"}
More Quizzes
Sample Test 2 - English for Airlines
10519
Quiz- Schedules
11624
210
FIND THE CAR THAT MAKE YOUR HEART GO VROOMMM....
740
AFMAN 23-110 2S051 CDC EOC Vol. 1 - Free Practice
201023398
Ethnicity - Test Your Knowledge of Race and Culture
15816538
What Is My Favorite Restaurant? Free Personality
201020031
Onboarding & Integration - Free for Employees
201017410
Which One Tree Hill Character Are You? Free
201019229
Chakra Nature - Which Naruto Element Are You?
201019926
What Kind of Traveler Are You? - Find Your Type
201021418
Which Jellicle Cat Are You? Cats (Musical) Personality
201022074