999 Questions Pediatrie-MCQ-(301-600) Part 1 NR
You admitted to the hospital the previous evening a 1-year-old boy who presented with cough, fever, and mild hypoxia. At the time of his admission, he had evidence of a right upper lobe consolidation on his chest radiograph. A blood culture has become positive in less than 24 hours for Staphylococcus aureus. Approximately 20 hours into his hospitalization, the nurse calls you because the child has acutely worsened over the previous few minutes, with markedly increased work in breathing, increasing oxy- gen requirement, and hypotension. As you move swiftly to the child’s hospital room, you tell the nurse to order which of the following?
A large-bore needle and chest tube kit for aspiration of a probable tension pneumothorax
A second chest radiograph to evaluate for pneumatocele formation
A change in antibiotics to include gentamicin
A sedative to treat the child’s attack of severe anxiety
A thoracentesis kit to drain his probable pleural effusion
A 15-year-old boy has been immobilized in a double hip spica cast for 6 weeks after having fractured his femur in a skiing accident. He has become depressed and listless during the past few days and has complained of nausea and constipation. He is found to have microscopic hematuria and a blood pressure of 150/100 mm Hg. Which of the following is the most appropriate course of action?
Collect urine for measurement of the calcium to creatinine ratio
Request a psychiatric evaluation
Check blood pressure every 2 hours for 2 days
Order a renal sonogram and intravenous pyelogram (IVP)
Measure 24-hour urinary protein
An adolescent with type 1 diabetes returns for a follow-up visit after his annual checkup last week. You note that his serum glucose is elevated and his glycosylated hemoglobin (hemoglobin A1C) is 16.7%. This finding suggests poor control of his diabetes over at least which of the following time periods?
2 months
8 hours
1 week
1 month
6 months
A 6-year-old male presents to the physician with eyelid swelling. His mother noted an insect bite on his left cheek yesterday, and states that this morning his left eyelid was completely swollen shut and painful. He has not had a fever, fatigue, headache, or rhinorrhea. On examination, he is afebrile. The left eyelid is erythematous, tender to palpation, and swollen shut. When trying to clinically distinguish between preseptal and orbital cellulitis, which of the following findings is most likely to be seen with preseptal cellulitis?
Eyelid discoloration
Decreased eye movements
Decreased visual acuity
Proptosis
Fever
A 41-year-old woman who is 32-weeks pregnant presents to the emergency department in labor. Her pregnancy has been complicated by gestational hypertension. Her medical history is otherwise unremarkable. She does not abuse alcohol, tobacco, or illicit drugs. Despite medical interventions, her preterm labor cannot be arrested, and she delivers a 2 kg (41b, 5oz) female infant. Both she and the child do well after delivery. Which of the following is true regarding immunizations for this infant?
Immunizations should be given according to the chronologic age
Immunizations should be given according to the gestational age
Toxoid and polysaccharide vaccines should be given according to chronologic age, but live attenuated vaccines should be given according to the gestational age
Immunizations should be started after she reaches 3 kg.
Immunizations should be given when allergen testing confirms an immune response
As you are about to step out of a newly delivered mother’s room, she mentions that she wants to breast-feed her healthy infant, but that her obstetrician was concerned about one of the medicines she was taking. Which of the woman’s medicines, listed below, is clearly contraindicated in breast-feeding?
Amphetamines for her attention deficit disorder
Ibuprofen as needed for pain or fever
Labetalol for her chronic hypertension
Carbamazepine for her seizure disorder
Acyclovir for her HSV outbreak
A recovering premature infant who weighs 950 g (2 lb, 1 oz) is fed breast milk to provide 120 cal/kg/d. Over the ensuing weeks, the baby is most apt to develop which of the following?
Hypocalcemi
Hypernatremia
Blood in the stool
Hyperphosphatemia
Vitamin D toxicity
A 15-year-old female presents to your office with secondary amenorrhea. As part of your evaluation, you find that she is pregnant. After informing her of the pregnancy, you continue to explain that young mothers have a higher risk of several pregnancy-related complications, including which of the following?
Low-birth weight infants
Twin gestation
Hypotension
Excessive weight gain
Infants with genetic defects
A 16-year-old boy who is the backup quarterback for the local high school team is in your office complaining of worsening acne. For the last few months he has noted more acne and more oily hair. On his examination, you note gynecomastia and small testicular volume. He is SMR 5. Which of the following drugs of abuse is the likely explanation for all of his findings?
Oxandrolone
Cocaine
Marijuana
Toluene
Methylenedioxymethamphetamine
A 4-year-old Caucasian boy is brought to his physician's office for a health maintenance exam. He will be starting preschool soon, and his parents want to make sure that he is in optimal health. The child has no complaints, and is generally happy. His medical history is significant for pneumonia as a newborn, and three episodes of otitis media since birth. He does not take any medications on a regular basis. His newborn screening test results are normal. His developmental milestones are at par with his age. He lives with his parents in a middle-class, suburban house built in 1981. Which of the following is the most appropriate next step for this child's primary care?
Vision exam
Screen him for inguinal hernias
Serum lead level
Meningococcal vaccine
Rotavirus vaccine
A term infant is born to a known HIV-positive mother. She has been taking antiretroviral medications for the weeks prior to the delivery of her infant. Routine management of the healthy infant should include which of the following?
A course of zidovudine for the infant
Admission to the neonatal intensive care unit for close cardiovascular monitoring
HIV ELISA on the infant to determine if congenital infection has occurred
Chest radiographs to evaluate for congenital Pneumocystis carinii
Administration of IVIG to the baby to decrease the risk of perinatal HIV infection
Initial examination of a full-term infant weighing less than 2500 g (5 lb, 8 oz) shows edema over the dorsum of her hands and feet. Which of the following findings would support a diagnosis of Turner syndrome?
Redundant skin folds at the nape of the neck
A liver palpable to 2 cm below the costal margin
Tremulous movements and ankle clonus
A transient, longitudinal division of the body into a red half and a pale half
Softness of the parietal bones at the vertex
A 3-year-old boy is brought to the office by his Caucasian mother because his speech is difficult to understand. He is a very slow learner, is unusually calm, stays to himself, doesn't hug his parents, prefers to play by himself, speaks in mumbles, and repetitively tries to make towers with cubes. He becomes very aggressive if he is stopped from his activities. He was born at term from an uncomplicated pregnancy and delivery, and his physical growth has been normal. His brother used to be aggressive as a child, and was diagnosed with attention deficit hyperactivity disorder. In the office, the patient is sitting quietly and trying to make towers with cubes. He seems to be oblivious of his environment. On calling his name thrice, he turns towards you once and then resumes playing with the cubes. What do you tell his mother?
He has autism and will need special behavioral and educational programs
He has attention deficit hyperactivity disorder and would benefit from methylphenidate
This could be autism and would benefit from antipsychotics
He has hearing problems and he needs ear, nose and throat evaluation
His diagnosis is Asperger syndrome
A father brings his 3-year-old daughter to the emergency center after noting her to be pale and tired and with a subjective fever for several days. Her past history is significant for an upper respiratory infection 4 weeks prior, but she had been otherwise healthy. The father denies emesis or diarrhea, but does report his daughter has had leg pain over the previous week, waking her from sleep. He also reports that she has been bleeding from her gums after brushing her teeth. Examination reveals a listless pale child. She has diffuse lymphadenopathy with splenomegaly but no hepatomegaly. She has a few petechiae scattered across her face and abdomen and is mildly tender over her shins, but does not have associated erythema or joint swelling. A CBC reveals a leukocyte count of 8,000/L with a hemoglobin of 4 g/dL and a platelet count of 7,000/L. The automated differential reports an elevated number of atypical lymphocytes. Which of the following diagnostic studies is the most appropriate next step in the management of this child?
Bone marrow biopsy
Epstein-Barr virus titers
Serum haptoglobin
Antiplatelet antibody assay
Reticulocyte count
While bathing her newly-received 2-year-old son, a foster mother feels a mass in his abdomen. A thorough medical evaluation of the child reveals aniridia, hypospadias, horseshoe kidney, and hemihypertrophy. Which of the following is the most likely diagnosis for this child?
Wilms tumor
Neuroblastoma
Hepatoblastoma
Rhabdomyosarcoma
Testicular cancer
A 7 -year-old Caucasian male with a history of peanut allergy develops sudden shortness of breath after lunch at school. On physical examination, his blood pressure is 70/50 mmHg and his heart rate is 130/min. Inspirations and expirations are labored and noisy. Which of the following is the best initial treatment?
Subcutaneous epinephrine injection
Albuterol nebulizer
Intravenous steroids
Intravenous diphenhydramine
Endotracheal intubation
A 1-year-old boy is brought to the pediatrician for a routine visit. While talking to his mother, she reports that they moved into an old house several months ago and are in the process of renovating. The child eats table food and drinks whole milk. His height, weight, and head circumference are all at the 50th percentile for his age. Physical examination is normal. The results of a fingerstick blood test are shown below: Hemoglobin 1 0.5 g/dL Hematocrit 30.0% Lead level 12 μg/dL (Normal < 10 μg/dL) Which of the following is the most appropriate next step in management?
Check a serum lead level
Remove the child from the house
Initiate chelation therapy with dimercaprol
Initiate chelation therapy with dimercaptosuccinic acid (DMSA, succimer)
Recheck lead level in one month
A 7-day-old boy is admitted to a hospital for evaluation of vomiting and dehydration. Physical examination is otherwise normal except for minimal hyperpigmentation of the nipples. Serum sodium and potassium concentrations are 120 mEq/L and 9 mEq/L (without hemolysis), respectively; serum glucose is 40 mg/dL. Which of the following is the most likely diagnosis?
Congenital adrenal hyperplasia
Pyloric stenosis
Secondary hypothyroidism
Hyperaldosteronism
Panhypopituitarism
A 14-year-old boy presents with the complaint of “breast swelling.” The boy reports that he has been in good health and without other problems, but has noticed over the past month or so that his left breast has been “achy” and that he has now noticed some mild swelling under the nipple. He has never seen discharge; the other breast has not been swelling; and he denies trauma. Your examination demonstrates a quarter-sized area of breast tissue under the left nipple that is not tender and has no discharge. The right breast has no such tissue. He has a normal genitourinary examination, and is Tanner stage 3. Which of the following is the best next course of action?
Reassurance of the normalcy of the condition
CT scan of the pituitary
Measurement of serum luteinizing hormone (LH) and follicle-stimulating hormone (FSH)
Measurement of serum testosterone
Chromosomes
A 12-week-old female infant is brought to the office by her mother due to a three-week history of weakness, poor appetite, and choking spells during feeding. Other accompanying symptoms include excessive sleeping, constipation and apathy. Her prenatal history is unremarkable. She was delivered vaginally at 38 weeks of gestation. Her weight and length at birth were within normal range. She is exclusively breastfed. Her mother's family history is unremarkable. The identity and family history of her father are unknown. The pertinent physical findings include apathy, weakness, hypotonia, large tongue, sluggish movement, abdominal bloating, and an umbilical hernia. Based on the given information, what is the most likely diagnosis?
Congenital hypothyroidism
Infant botulism
Werdnig-Hoffmann syndrome
Myotonic congenital myopathy
Myasthenia gravis
While making rounds in the newborn nursery, the nurses ask you to examine a 2-day-old infant who is not feeding well. The nurse reports that the infant is irritable, is not sleeping well, and has had several episodes of vomiting and loose stools today. A review of the maternal history reveals that she had poor prenatal care and the pregnancy was complicated by intrauterine growth restriction. On examination, the infant is diaphoretic and has a high-pitched cry. The infant is also noted to have occasional sneezing and is mildly tachypneic. No dysmorphic features are noted and the remainder of the examination is unremarkable. This infant's symptoms are most likely caused by prenatal exposure to which of the following?
Heroin
Valproic acid
Phenytoin
Alcohol
Cocaine
A 2-year-old boy is being followed for congenital cytomegalovirus (CMV) infection. He is deaf and developmentally delayed. The child’s mother informs you that she has just become pregnant and is concerned that the new baby will be infected and may develop serious consequences. Which of the following is true?
The mother has antibodies to CMV that are passed to the fetus
The mother’s infection cannot become reactivated
The likelihood that the new baby will become clinically ill is approximately 80%.
Termination of pregnancy is advised
The new infant should be isolated from the older child
A full-term infant is born after a normal pregnancy; delivery, however, is complicated by marginal placental separation. At 12 hours of age, the child, although appearing to be in good health, passes a bloody meconium stool. For determining the cause of the bleeding, which of the following diagnostic procedures should be performed first?
An Apt test
A barium enema
Gastric lavage with normal saline
An upper gastrointestinal series
A platelet count, prothrombin time, and partial thromboplastin time
A 1 0-year-old boy is brought to the emergency department due to abdominal pain and bloody diarrhea. The mother says that he was "fine" a few days ago, and then suddenly became ill. Physical examination shows a pale and jaundiced child. There is diffuse abdominal tenderness and 2+ pedal edema. Laboratory studies show anemia, thrombocytopenia and renal insufficiency. What is the most likely cause of the patient's symptoms?
A 1 0-year-old boy is brought to the emergency department due to abdominal pain and bloody diarrhea. The mother says that he was "fine" a few days ago, and then suddenly became ill. Physical examination shows a pale and jaundiced child. There is diffuse abdominal tenderness and 2+ pedal edema. Laboratory studies show anemia, thrombocytopenia and renal insufficiency. What is the most likely cause of the patient's symptoms?
Vibrio cholera
Crohn's disease
Lactose intolerance
Salmonella poisoning
A 2-year-old boy presents to the emergency department (ED) with severe wheezing. His symptoms have not improved even after three treatments with nebulizers. This is his third trip to the ED in the past two weeks. In the ED, he is given a dose of intravenous steroids, but continues to wheeze. On auscultation, there is no air entry bilaterally. His chest x-ray result is normal. His oxygen saturation is 91% on 6 liters of oxygen. What is the next best step in the management of this patient?
Mechanical ventilation
Start theophylline
Tracheostomy
Racemic epinephrine
Intravenous antibiotics
A 16-year-old girl is brought to the office due to abdominal pain and bloody diarrhea for the past two days. Her immunizations are up to date. Her past medical history is unremarkable. On examination, she appears lethargic and weak. Her skin turgor is poor, face and extremities are swollen, and skin appears yellow. Abdominal examination shows moderate non-localized, abdominal pain. Laboratory studies show: Hb 64 g/dl Hct 26.9% Platelets 45,000/mm3 Creatinine 2.3 mg/dl Total bilirubin 5.0 mg/dl What is the most common complication of the patient's condition?
Renal damage
Liver damage
Bone marrow failure
Pneumonia
Bowel obstruction
A fully immunized 2-year-old presents to the emergency room with several days of low-grade fever, barking cough, and noisy breathing. Over the past few hours he has developed a fever of 40°C (104°F) and looks toxic. He has inspiratory and expiratory stridor. The family has not noticed drooling, and he seems to be drinking without pain. Direct laryngoscopy reveals a normal epiglottis. The management of this disease process includes which of the following?
Intubation and intravenous antibiotics
Inhaled epinephrine and oral steroids
Inhaled steroids
Observation in a cool mist tent
Oral antibiotics and outpatient follow-up
An obese Caucasian father brings his 1 0-year-old obese son to your office. The father states that he was recently diagnosed with high cholesterol levels and coronary artery disease. Even though his son is asymptomatic, he is worried about the obesity. Which of the following best explains the next best step in management?
Get a screening test for total cholesterol level
Get a fasting lipid profile
Advise parents to start him on a low cholesterol diet
Evaluate him for coronary artery disease
Advise parents to start him on a regular physical exercise schedule

A 24-year-old woman arrives in the emergency center in active labor. She is at term, but received no prenatal care after 16 weeks of gestation when she lost her insurance coverage. The mother has an uncomplicated vaginal delivery. You are paged shortly after birth when the baby is noted to have respiratory distress. The infant has diminished breath sounds on the left, and the PMI is shifted toward the right. A chest radiograph is shown. The NG tube you placed earlier reveals the stomach to be below the diaphragm. Which of the following is the most likely diagnosis at this point?
Congenital cystic adenomatoid malformation
Congenital diaphragmatic hernia
Bronchogenic cysts
Congenital lobar emphysema
Congenital pneumonia
A 4-year-old boy, whose past medical history is positive for three urinary tract infections, presents with a blood pressure of 135/90 mm Hg. He is likely to exhibit which of the following symptoms or signs?
Headache
Multiple cranial nerve palsy
Hyporeflexia
Increased urine output
Right ventricular hypertrophy

The 1-year-old boy in the photograph below, who recently had a circumcision, requires an additional operation on his genitalia that will probably eliminate his risk of which of the following?
Torsion of testes
Testicular malignancy
Decreased sperm count
Urinary tract infection
Epididymitis
A previously healthy 3-year-old boy brought in by his parents for help with potty training. The boy refuses to use the toilet. If his parents try to place him on the toilet, he becomes upset and cries. He has regular urination in his diaper. He has 1-2 soft bowel movements a day. In the office, you note that the child speaks in short sentences that are mostly understandable. He runs well and can climb up on the examination table without help. His physical examination is unremarkable. Which of the following is the next best step in the management of this patient?
Stop potty training attempts for several months
Increase fiber in his diet
Put him on the toilet at regularly scheduled times
Use a positive reward system
Perform a urinalysis
A 6-year-old boy is brought to the ER with a two-day history of difficulty walking. He is dragging his right leg and seems to have weakness in his right arm. He also complains of headaches. The family just emigrated from Eastern Europe. According to his parents, the child suffers from delayed growth compared to his peers and does not like to engage in active play. His lips and fingers turn blue when he cries. His vital signs today are a blood pressure of 100/70 mmHg, pulse of 90/min, temperature of 38.3 0C (102.0 0F), and respiratory rate of 22/min. Which of the following is most likely responsible for his current complaints?
Brain abscess
Glycogen storage disorder
Demyelinating disorder
Malignancy
Malformation of the central nervous system
A 15-year-old is participating in high school football practice in August in Texas. He had complained of headache and nausea earlier in practice, but kept playing after a cup of water. He is now confused and combative. He is dizzy and sweating profusely. His temperature is 41°C (105.8°F). Therapy should consist of which of the following?
Initiate whole body cold water immersion
Provide oral rehydration solutions
Administer acetaminophen rectally
Order to rest on the bench until symptoms resolve
Tell him to go take a shower and rest until the next day’s practice

The term infant pictured below weighs 2200 g (4 lb, 14 oz). He is found to have a ventricular septal defect on cardiac evaluation. This infant appears to have features consistent with which of the following?
Fetal alcohol syndrome
Perinatal phenytoin exposure
Trisomy 21
Alport syndrome
Infant of diabetic mother
A previously healthy 4-year-old child is brought to the physician for a school physical for kindergarten. His mother has brought in his immunization record and reports that received all his immunizations prior to age 2. He has received only a yearly influenza vaccine since age 2. His physical examination is unremarkable. Which of the following immunizations should he be given during this visit?
Inactivated polio #4
Haemophilus influenza type B #4
Pneumococcal #3
Measles-mumps-rubella #1
Hepatitis B #3
A 6-week-old child is being evaluated for a fever of unknown etiology. As part of the laboratory evaluation, a urine specimen was obtained that grew E coli with a colony count of 2000/L. These findings would be definite evidence of a urinary tract infection if which of the following is true about the sampled urine?
It is from a suprapubic tap
It has a specific gravity of 1.008.
It is from a bag attached to the perineum of an uncircumcised boy.
It is from an ileal-loop bag.
It is the first morning sample.
A previously healthy 16-year-old girl presents to the emergency center with the complaint of “falling out.” She was with her friends at a local fast food restaurant when she felt faint and, according to her friends, lost consciousness for about a minute. There was no seizure activity noted, but the friends did notice her arms twitching irregularly. She is now acting normally. She denies chest pain or palpitations, and her electrocardiogram (ECG) is normal. Further management of this patient should include which of the following?
Encourage adequate fluid and salt intake
Obtain an EEG
Refer to a child psychiatrist
Begin -blocker therapy
Obtain serum and urine drug screens
A female infant is born by vaginal delivery at 39 weeks' gestational age without any significant complications. There is no history of any genetic diseases in the family. She is noted to have a port-wine stain on the right side of her face that is 4 cm in length and 3 cm in width. Which of the following treatment modalities offers the best palliation for cosmetic purposes?
Pulsed dye laser
Cryosurgery
Radiation therapy with gamma particles
Skin grafting
Topical corticosteroid therapy
A 4-year-old, apparently healthy child is examined by a pediatrician. The pediatrician hears a loud systolic ejection murmur with a prominent systolic ejection click. He also hears a soft, early diastolic murmur. Both murmurs are heard best at the upper right sternal border. ECG shows left ventricular hypertrophy. Which of the following is the most likely diagnosis?
Aortic valve stenosis
Atrial septal defect
Tetralogy of Fallot
Transposition of great arteries
Ventricular septal defect
A 19-year-old primiparous woman develops toxemia in her last trimester of pregnancy and during the course of her labor is treated with magnesium sulfate. At 38 weeks’ gestation, she delivers a 2100-g (4-lb, 10-oz) infant with Apgar scores of 1 at 1 minute and 5 at 5 minutes. Laboratory studies at 18 hours of age reveal a hematocrit of 79%, platelet count of 100,000/μL, glucose 41 mg/dL, magnesium 2.5 mEq/L, and calcium 8.7 mg/dL. Soon after, the infant has a generalized convulsion. Which of the following is the most likely cause of the infant’s seizure?
Polycythemia
Hypoglycemia
Hypocalcemia
Hypermagnesemia
Thrombocytopenia
An infant who appears to be of normal size is noted to be lethargic and somewhat limp after birth. The mother is 28 years old, and this is her fourth delivery. The pregnancy was uncomplicated, with normal fetal monitoring prior to delivery. Labor was rapid, with local anesthesia and intravenous meperidine (Demerol) administered for maternal pain control. Which of the following therapeutic maneuvers is likely to improve this infant’s condition most rapidly?
Administration of naloxone (Narcan)
Intravenous infusion of 10% dextrose in water
Administration of vitamin K
Measurement of electrolytes and magnesium levels
Neurologic consultation
At 43 weeks’ gestation, a long, thin infant is delivered. The infant is apneic, limp, pale, and covered with ―pea soup‖ amniotic fluid. Which of the following is the best first step in the resuscitation of this infant at delivery?
Intubation and suction of the trachea; provision of oxygen
Artificial ventilation with bag and mask
Chest compressions
Administration of 100% oxygen by mask
Catheterization of the umbilical vein
A 4-year-old child presents with an enlarged submandibular node that is 4 cm in diameter, nontender, and not fluctuant. The node has been enlarged for about 4 weeks, and there is no history of fever or contact with any person who was ill. A CBC is normal, and a Mantoux test with 5 tuberculin units of PPD shows 6 mm of induration. Which of the following is the most likely diagnosis?
Atypical mycobacteria lymphadenitis
Cat-scratch fever
Acute pyogenic lymphadenitis
Acute lymphoblastic leukemia
Tuberculous lymphadenitis
A 4-year-old child with grade III vesicoureteral reflux has recurrent UTIs despite adequate antibiotic prophylaxis. Which of the following is the most appropriate next step in the treatment of this patient?
Antireflux surgery
IV antibiotic treatment for 2 weeks
Repeat renal scan
Renal arteriogram
Addition of vitamin C (ascorbic acid) to the treatment regimen
A 2-week-old infant presents with hepatosplenomegaly and a thick, purulent, bloody nasal discharge. Coppery, oval, maculopapular skin lesions are present in an acral distribution. The neurologic examination is normal, including head circumference. Which of the following is the most likely cause of this congenital infection?
T. pallidum
Cytomegalovirus (CMV)
HSV
GBS
T. gondii
A 7-month-old patient presents with a history of 3 days of fever to 104°F, which resolved the same day that an exanthem erupted. The exanthem is prominent on the neck and trunk. It is macular, with discrete lesions 3–5 mm in diameter. Which of the following is the most likely diagnosis?
Roseola infantum
Erythema infectiosum
Measles
Rubella
Scarlet fever
A newborn infant has respiratory distress and trouble feeding in the nursery. The mother has no significant medical history, but the pregnancy was complicated by decreased fetal movement. On physical examination, you note that aside from shallow respirations and some twitching of the fingers and toes, the infant is not moving, and is very hypotonic. In the mouth there is pooled saliva and you note tongue fasciculations. Deep tendon reflexes are absent. Spinal fluid is normal. Appropriate statements about this condition include which of the following statements?
The condition is caused by the degeneration of anterior horn cells in the spinal cord
The condition is caused by the absence of the muscle cytoskeletal protein dystrophin
The condition is caused by the antibodies that bind the acetylcholine receptor at the postsynaptic muscle membrane
The condition is caused by progressive autoimmune demyelination
The condition is caused by birth trauma
A 3-year-old boy’s parents complain that their child has difficulty walking. The child rolled, sat, and first stood at essentially normal ages and first walked at 13 months of age. Over the past several months, however, the family has noticed an increased inward curvature of the lower spine as he walks and that his gait has become more “waddling” in nature. On examination, you confirm these findings and also notice that he has enlargement of his calves. Which of the following is the most likely diagnosis?
Muscular dystrophy
Occult spina bifida
Brain tumor
Guillain-Barrésyndrome
Botulism
Your 6-year-old son awakens at 1:00 AM screaming. You note that he is hyperventilating, is tachycardic, and has dilated pupils. He cannot be consoled, does not respond, and is unaware of his environment. After a few minutes, he returns to normal sleep. He recalls nothing the following morning. Which of the following is the most likely diagnosis?
Night terrors
Seizure disorder
Drug ingestion
Psychiatric disorder
Migraine headache
A 5-year-old febrile child presents with swelling of the right eyelid. Proptosis and limitation of ocular movements is noted. Which of the following is the most likely diagnosis?
Orbital cellulitis
Retinoblastoma
Periorbital cellulitis
Neuroblastoma
Hyphema
A 6-month-old infant is diagnosed with her first episode of otitis media. She does not have any allergies to medications. Which of the following medications would be the recommended initial therapy for this infant?
Amoxicillin
Amoxicillin-clavulanic acid
Cephalexin
Ceftriaxone
Erythromycin
A 10-year-old boy is brought in with a chief complaint of multiple colds. On further questioning, you elicit a history of chronic, clear nasal discharge with no seasonal variation. Other symptoms include sneezing, itching of the nose and eyes, as well as tearing and occasional eye redness. Some relief is obtained with an over-the-counter cold medicine containing antihistamine and a decongestant. His history suggests which of the following?
Allergic rhinitis
Nasal foreign body
Immunologic deficiency
Rhinitis medicamentosa
Chronic sinusitis

A 15-year-old boy comes to the physician with left shoulder joint pain and swelling. He has had these symptoms for the past 3 months and they are getting progressively worse. He has no fever, weight loss, or night sweats. The patient lifts weights and plays baseball 5 days a week. He has taken acetaminophen and ibuprofen with little relief. Examination shows a tender mass at the left proximal humerus. Range of motion is normal. Laboratory evaluation shows elevated alkaline phosphatase, erythrocyte sedimentation rate, and lactate dehydrogenase. X-ray of the shoulder is shown in the photograph below. Which of the following is the most likely diagnosis?
Osteosarcoma
Ewing sarcoma
Osteoid osteoma
Osteomyelitis
Stress fracture
A 7-year-old boy is brought to your office with a sore throat, decreased appetite, and nausea. His past medical history is insignificant. All of his vaccinations are up-to-date. He has no known allergies. His temperature is 39.0°C (102.5°F), blood pressure is 110/70 mmHg, pulse is 104/min, and respirations are 16/min. On examination, the pharynx and tonsils are red, sv1ollen, and have white exudates on their surface. There is also bilateral tender cervical lymphadenopathy. The rapid diagnostic test for streptococcal antigen is positive. What is the most appropriate next step in management?
Oral penicillin V
Throat culture
Monospot test
Antistreptolysin O antibodies
Oral azithromycin
A 4-day-old infant presents with yellow discoloration of the skin and sclera. The baby was born at term by a normal vaginal delivery. Pregnancy was uncomplicated; there were no risk factors for sepsis and no history of maternal alcohol or drug use. The baby is breast-fed and has been nursing every 2 hours, about 10 minutes at each breast. The bilirubin level is 15 mg/dL (all unconjugated), the hematocrit is 45%, and the Coombs test is negative. Which of the following is the most likely diagnosis?
Breast-feeding jaundice
Congenital biliary atresia
Isoimmune hemolytic disease
Crigler-Najjar syndrome
Breast milk jaundice
A previously healthy, active, 18-month-old African American child presents with unilateral nasal obstruction and foul-smelling discharge. The child’s examination is otherwise unremarkable. Which of the following is the most likely diagnosis?
Foreign body
Nasal polyps
Frontal sinusitis
Deviated septum
Choanal atresia
A 7-year-old child is brought by his mother for a school physical. His growth parameters show his height to be 50th percentile and his weight to be significantly higher than 95th percentile. His mother complains that he always seems sleepy during the day and that he has started complaining of headaches. His second-grade teacher has commented that he has difficulty staying awake in class. His mother complains that he wakes up the whole house with his snoring at night. Which of the following is the most appropriate next step in evaluating and managing this condition?
Arrange for polysomnography
Try steroids to decrease tonsillar and adenoid hypertrophy
Refer to an otolaryngologist for tonsillectomy and adenoidectomy
Arrange for continuous positive airway pressure (CPAP) at home
Arrange for home oxygen therapy for use at night
A 3-year-old boy is brought to the emergency department three hours after having a seizure. He has been having severe diarrhea for the last three days. His mother recently read about the importance of maintaining adequate hydration during diarrhea, so she had been giving him a lot of milk mixed with water. On examination, his vital signs are stable and mucus membranes are moist. Initial lab results are: Hb 13 g/dl WBC 6,000/mm3 Platelets 300,000/mm3 Blood Glucose 98 mg/dl Serum Na 120 mEq/L Serum K 34 mEq/L Chloride 92 mEq/L BUN 22 mg/dl Creatinine 1.2 mg/dl What is the most likely cause of this patient's seizure?
Water intoxication
SIADH
Severe dehydration
Acute renal failure
Sepsis
The state laboratory calls your office telling you that a newborn infant, now 8 days old, has an elevated thyroid stimulating hormone (TSH), and low thyroxin (T4) on his newborn screen. If this condition is left untreated, the infant is likely to demonstrate which of the following in the first few months of life?
Prolonged jaundice
Hyperreflexia
Hyperirritability
Diarrhea
Hyperphagia
A 1-year-old boy presents with the complaint from his parents of “not developing normally.” He was the product of an uneventful term pregnancy and delivery, and reportedly was normal at birth. His previous health-care provider noted his developmental delay, and also noted that the child seemed to have an enlarged spleen and liver. On your examination, you confirm the developmental delay and the hepatosplenomegaly, and also notice that the child has short stature, macrocephaly, hirsutism, a coarse facies, and decreased joint mobility. Which of the following is the most likely etiology of his condition?
Hurler syndrome
Beckwith-Wiedemann syndrome
Crouzon syndrome
Trisomy 18 (Edwards syndrome)
Jeune syndrome
A 22-year-old Caucasian female who has received no prenatal care experiences a stillbirth. This is her first pregnancy. The baby has multiple fractures, blue sclerae and short, bent extremities. Her past medical history is significant for a seizure disorder. She has been taking phenytoin regularly and had no seizure episodes during the pregnancy. She admits to eating poorly and occasionally drinking alcohol during the first trimester. She lives with her boyfriend who abuses her physically. She recalls several episodes of abuse during the pregnancy. Which of the following is most likely responsible for fetal abnormalities?
Collagen synthesis defect
Folic acid deficiency
Prenatal abuse
Phenytoin use
Alcohol abuse
You are awakened in the night by your 2-year-old son, who has developed noisy breathing on inspiration, marked retractions of the chest wall, flaring of the nostrils, and a barking cough. He has had a mild upper respiratory infection (URI) for 2 days. Which of the following therapies is indicated?
Inhaled epinephrine and a dose of steroids
Short-acting bronchodilators and a 5-day course of steroids
Intubation and antibiotics
Observation for hypoxia and dehydration alone
Rigid bronchoscopy
You receive a telephone call from the mother of a 4-year-old child with sickle-cell anemia. She tells you that the child is breathing fast, coughing, and has a temperature of 40°C (104°F). Which of the following is the most conservative, prudent course of action?
Admit the child to the hospital
Prescribe aspirin and ask her to call back if the fever does not respond
Make an office appointment for the next available opening
Make an office appointment for the next day
Refer the child to the laboratory for an immediate hematocrit, white blood cell count, and differential
A 7-month-old baby presents with a history of constipation for 1 month. He has one hard stool every week. He has been well otherwise. His physical examination is normal. Which of the following is the most likely cause of his problem?
Functional constipation
Hypothyroidism
Lead poisoning
Hirschsprung disease
Hypocalcemia
A specific pattern of abnormalities has been identified among infants born to mothers who consume moderate-to-large amounts of alcohol during their pregnancies. Which of the following abnormalities is characteristic of these infants?
Mental retardation
Cataracts
Developmental dysplasia of the hip
Gonadal dysgenesis
Neural tube defects

A 1-week-old black infant presents to you for the first time with a large, fairly well-defined, purple lesion over the buttocks bilaterally, as shown in the photograph. The lesion is not palpable, and it is not warm nor tender. The mother denies trauma and reports that the lesion has been present since birth. This otherwise well-appearing infant is growing and developing normally and appears normal upon physical examination. Which of the following is the most appropriate course of action in this infant?
Reassurance of the normalcy of the condition
Report the family to child protective services
Soft tissues films of the buttocks to identify calcifications
Administration of vitamin K
Measurement of bleeding time as well as factor VII and XI levels

A newborn infant develops respiratory distress immediately after birth. His abdomen is scaphoid. No breath sounds are heard on the left side of his chest, but they are audible on the right. Immediate intubation is successful with little or no improvement in clinical status. Emergency chest x-ray is shown (A) along with an x-ray 2 hours later (B). Which of the following is the most likely explanation for this infant’s condition?
Diaphragmatic hernia
Pneumonia
Cystic adenomatoid malformation
Choanal atresia
Pneumothorax
A 9-month-old infant is brought to the pediatrician's office because his weight is persistently below the 10th percentile. His mother states that the infant seems to be hungry all the time and usually consumes 8-12 oz of formula every 2-3 hours in addition to some table food. He also has frequent, bulky, and malodorous stools. A malabsorption syndrome is suspected. The results of which of the following tests will most likely be abnormal?
Fecal fat quantification
Abdominal radiography
Serum albumin
Stool culture for Clostridium difficile toxins
Stool smear for leukocytes and eosinophils
The parents of a previously healthy 2-year-old child note her to be pale and bring her to your clinic for evaluation. She currently has no fever, nausea, emesis, bone pain, or other complaints. Her examination is significant for pallor, tachycardia, and a systolic ejection murmur, but she has no organomegaly. Her complete blood count (CBC) reveals a hemoglobin of 4 g/dL, normal indices for age, a WBC count of 6.5/L, and a platelet count of 750,000/L. Her reticulocyte count is 0%. Coombs test is negative. Her peripheral blood smear shows no blast forms and no fragments. Red blood cell (RBC) adenosine deaminase levels are normal. A bone marrow reveals markedly decreased erythroid precursors. Which of the following is this child’s likely diagnosis?
Transient erythroblastopenia of childhood
Diamond-Blackfan anemia
Sickle-cell anemia
Pearson marrow-pancreas syndrome
Iron deficiency anemia
On a routine-screening CBC, a 1-year-old is noted to have a microcytic anemia. A follow-up hemoglobin electrophoresis demonstrates an increased concentration of hemoglobin A2. The child is most likely to have which of the following?
ρ�-Thalassemia trait
Iron deficiency
Sickle-cell anemia
Chronic systemic illness
Lead poisoning
A 2-year-old child is brought to the office by his parents for the evaluation of failure to thrive and chronic diarrhea. His diarrhea is "almost continuous", and he also has recurrent episodes of fever. He was initially quite well and was on the 60th percentile for weight; however, for the past seven months, he didn't seem to grow and failed to gain weight. Over the past three months, he fell to the 3rd percentile for weight. His parents deny any use of drugs, but they drink occasionally. His mother mentions that her former boyfriend was a heroin addict. Physical examination reveals oral thrush, generalized lymphadenopathy and eczema. What is the most likely diagnosis in this patient?
HIV infection
Congenital Toxoplasmosis
Non-Hodgkin lymphoma infiltrating small intestine
Miliary tuberculosis
Malabsorptive disease
A 3-year-old girl is brought to the emergency department because she became partially unconscious, lethargic and febrile. Her mother claims that "she suddenly took a turn for the worse" 24 hours ago after an upper respiratory tract infection. She has no allergies, and was not taking oral antibiotics. Her blood pressure is 60/45mm Hg and pulse is 120/min. On examination, she appears emaciated and lethargic. Despite numerous attempts, it is impossible to start a peripheral intravenous line, and the child's condition continues to deteriorate. What is the best next step to obtain IV access in this patient?
Lntraosseous
Subclavian central line
Jugular cut down
Femoral vein
Fluids down endotracheal tube
After being delivered following a benign gestation, a newborn infant is noted to have a platelet count of 35,000/L, decreased fibrinogen, and elevated fibrin spilt products. On examination you note a large cutaneous hemangioma on the abdomen that is purple and firm. Which of the following anomalies might also be expected in this infant?
Kaposiform hemangioendothelioma
Nevus simplex
Nevus flammeus
PHACE(S) syndrome
Infantile fibrosarcoma
A 4-year-old previously well African American boy is brought to the office by his aunt. She reports that he developed pallor, dark urine, and jaundice over the past few days. He stays with her, has not traveled, and has not been exposed to a jaundiced person, but he is taking trimethoprim sulfamethoxazole for otitis media. The CBC in the office shows a low hemoglobin and hematocrit, while his “stat” serum electrolytes, blood urea nitrogen (BUN), and chemistries are remarkable only for an elevation of his bilirubin levels. His aunt seems to recall his 8-year-old brother having had an “allergic reaction” to aspirin, which also caused a short-lived period of anemia and jaundice. Which of the following is the most likely cause of this patient’s symptoms?
Glucose-6-phosphate dehydrogenase deficiency
Hepatitis B
Hepatitis A
Hemolytic-uremic syndrome
Gilbert syndrome
A 24-month-old child is seen in the pediatrician's office for a regular health supervision visit. He has no history of developmental delay. He was born by an uncomplicated normal vaginal delivery at term, and he has not had any significant illness or injury prior to this visit. Which of the following motor milestones is most consistent with his age?
Throwing a ball overhead
Building a tower of two cubes
Copying a circle
Scribbling
Walking backward
A 2-year-old girl has severe dental caries of the upper and lower incisors. Her teeth are brushed twice daily with a small amount of fluoride-containing toothpaste. What is the feeding practice most likely to result in this pattern of dental caries?
Drinking a bottle of juice in bed
Drinking juice from a cup at snack time
Drinking juice from a bottle at snack time
Drinking milk from a bottle at meal time
Prolonged breast-feeding beyond the first year
A 6-year-old girl has a low-grade fever, headache, and nasal congestion. She has a flushed face and has developed a lacy reticular rash on the trunk and extensor surface of her arms and legs. Palms and soles are spared. Her mother has been ill with a low-grade fever and some joint stiffness and pain. Which of the following is the most likely diagnosis?
Erythema infectiosum (fifth disease)
Rubella
Measles
Scarlet fever
Roseola infantum
A 3-year-old boy has had fever for 4 days. On physical examination he has bilateral cervical lymphadenopathy, injected pharynx, and dry cracked lips. A throat swab is done and the rapid strep test is negative. The child is sent home and advised to follow-up if symptoms worsen. The child is brought back 2 days later with all previous findings including a maculopapular rash, swollen hands, and conjunctivitis. Which of the following is the most likely diagnosis?
Kawasaki disease
Scarlett fever
Toxic shock syndrome
Infectious mononucleosis
Erythema infectiosum

An 8-year-old girl is brought to the emergency department with fever for the past 6 days. Her parents report that she has been very "cranky" and has developed a new rash. Six weeks ago, she completed a 10-day course of amoxicillin for streptococcal pharyngitis. She has no other medical problems and takes no medications. Her temperature is 39.4° C (103° F), blood pressure is 110/60 mm Hg, pulse is 120/min, and respirations are 24/min. Physical examination shows injected lips and pharynx. Bilateral conjunctivae are also injected, with no exudates. A 1.7-cm mobile lymph node is palpated on the left neck. A blanching erythematous rash is present across her face, trunk, and extremities, including the palms and soles. Her mouth is shown below. What is the most appropriate next step in management of this patient?
Aspirin and intravenous immunoglobulin
Amoxicillin
Doxycycline
Lymph node biopsy
Reassurance and close follow-up
A 6-year-old African-American child is brought in by his father for complaints of easy fatigability and pallor. These symptoms occurred after the son was treated with "some medication" for a recent diarrhea. Physical examination is normal except for pallor and multiple petechiae. Laboratory values are as follows: Hb 8.0 g/dL WBC 12,000/cmm Platelets 50,000/cmm Blood glucose 118 mg/dL Serum Na 135 mEq/L Serum K 5.3 mEq/L Chloride 110 mEq/L Bicarbonate 18 mEq/L BUN 38 mg/dL Serum creatinine 2.5 mg/dL Total bilirubin 3 mg/dL Direct bilirubin 0.5 mg/dL PT 12 seconds APTT 30 seconds LDH 900 IU/L Reticulocyte count 6% A peripheral blood smear reveals giant platelets and multiple schistocytes. What is the most likely underlying pathophysiology for this boy's pallor?
Microangiopathic hemolytic anemia
Sickle cell anemia
Thalassemia
Vitamin B12 deficiency
Folate deficiency
A 13-year-old boy’s scrotum is shown below. He complains of several months of swelling but no pain just above his left testicle. He is sexually active but states that he uses condoms. On physical examination, the area in question feels like a “bag of worms.” Which of the following is the most appropriate management for this condition?
Reassurance and education only at this time
Doppler flow study of testes
Radionuclide scan of testes
Urinalysis and culture
Ceftriaxone intramuscularly and doxycycline orally

A 3-day-old infant’s scrotum is shown below. Palpation reveals a tense, fluid-filled area surrounding the right testicle. The scrotum transil luminates well, and the amount of fluid does not vary with mild pressure. Which of the following is the most appropriate approach to this condition?
Observe only
Request a surgical consultation
Incision and drainage
Administer prophylactic antibiotics
Perform a chromosome determination
A 1-week-old infant is brought to the emergency department due to vomiting and poor feeding. The prenatal and birth histories are unremarkable. The infant's pulse is 140/min, temperature is 37 C (98.7 F), and capillary refill is 2 sec. He has sunken eyes, depressed anterior fontanel, and dry mucus membranes; skin elasticity is reduced. Heart and lungs are clear. There is no abdominal mass. Genital examination shows enlarged clitoris, and fusion of the labioscrotal folds. The initial laboratory work-up reveals the following: Sodium 128 mEq/L Potassium 5.8 mEq/L BUN 25 mg/dl If this patient's karyotype is 46 XX, which of the following is most likely to be increased in this patient's serum?
17 -alpha-hydroxyprogesterone
18-hydroxycorticosterone
11-deoxycorticosterone
11-deoxycortisol
Corticosterone
An 8-year-old Caucasian boy is brought to the office for the evaluation of high-grade fever, flank pain and burning micturition for the last two days. He has had two previous episodes of acute pyelonephritis. Physical examination reveals costovertebral angle tenderness. Urinalysis shows pyuria, significant bacteriuria, WBC casts, positive nitrite and esterase. The voiding cystourethrogram (VCUG) reveals vesicoureteral reflux. What is the most likely complication of this condition, if left untreated?
Renal scarring
Hydronephrosis
Renal stones
Renal abscess
Renal cell carcinoma
A woman comes to an emergency department because she is in labor. She has had no prenatal care. Her baby is delivered and appears to be of about 32 weeks' gestation. The newborn is very pale and shows severe, generalized edema. Cord-blood hematocrit is 22%, and cord-blood bilirubin is 7 mg/dl. Ultrasound examination demonstrates pleural effusions, ascites, cardiomegaly, and hepatomegaly. Which of the following is the most likely diagnosis?
Rh incompatibility
ABO incompatibility
Beta thalassemia
Congenital spherocytosis
Sickle cell anemia
A neonate is examined following a protracted breech delivery. One of the infant's arms is partially paralyzed. The affected arm is adducted and internally rotated at the shoulder, and the forearm is pronated. Which of the following is the most likely diagnosis?
Erb palsy
Bell palsy
Klumpke palsy
Pseudobulbar palsy
Supranuclear palsy
A 2-year-old boy presents with refusal to use his right arm for 1 day. He is otherwise well. His mother states she pulled upward on his arm the previous evening to keep him from tripping down the stairs. Which of the following is the most likely diagnosis?
Subluxation of the radial head
Colles fracture
Fractured clavicle
Greenstick fracture of the humerus
Rotator cuff injury
A 3-year-old male presents after having a tonicclonic seizure lasting about 1 minute. On examination, the child now has no neurologic abnormalities. He has a temperature of 40.3°C and has an obvious otitis media on the left but no other abnormalities on physical examination. You correctly counsel the family with which one of the following statements?
There is a slight increase in risk for development of epilepsy
The child will need hospitalization, a lumbar puncture, and antibiotics
An EEG and CNS imaging must be done
Anticonvulsants must be stated and continued for 6 months
The child must be monitored carefully for long-term neurologic damage
A 1-day-old infant who received silver nitrate eye drops in the delivery room is suffering from bilateral purulent conjunctival discharge. Which of the following is the most likely cause of this child’s condition?
Chemical irritation
N. Gonorrhoeae infection
Herpes simplex infection
Nasolacrimal duct obstruction
Pseudomonas infection
A 10-month-old girl is seen in clinic for a routine checkup. She weighs 11 kg (24.2 lb). The infant's mother reports that she drinks whole cow's milk and takes solid food poorly. The infant's activity is decreased, but her muscle tone is good and her developmental milestones are up to date. The only significant abnormal physical finding is parlor. Which of the following is the most appropriate next step in management?
Dietary advice and oral iron treatment
Hemoglobin electrophoresis
Intravenous pyelogram
Skeletal survey with x-rays
Bone marrow biopsy
A 2-year-old boy is brought to the clinic because of a swelling at the base of his neck on the left side. The family indicates that since he was born, they suspected he had some kind of a mass in his left supraclavicular area and behind the sternomastoid on that same side, but the area felt soft and mushy, was not always evident, and seemed to be painless, so they did nothing about it. Two weeks ago the child had an upper respiratory infection, and within a day or two the mass became larger and quite obvious. On physical examination he indeed has a soft, mushy, ill-defined mass occupying the entire left supraclavicular area and extending into the posterior triangle of the neck. He has no enlarged lymph nodes anywhere, and his spleen and liver are not palpable. Which of the following is the most appropriate next step in the evaluation?
MRI of the neck and chest
Bone marrow biopsy
Multiple percutaneous needle biopsies
Open surgical excisional biopsy
Panendoscopy under general anesthesia
A 14-year-old girl has a history of red eyes with clear discharge that she suffers from in a seasonal pattern. Together with these symptoms, she reports itching, which is her most bothersome complaint. Physical examination shows conjunctival redness, tearing, and swelling, but there is no purulent discharge. This clinical picture is most compatible with a diagnosis of which of the following conditions?
Allergic conjunctivitis
Bacterial conjunctivitis
Blepharitis
Corneal abrasion
Trachoma
A 4-day-old boy is brought to the physician for an outpatient follow-up visit. His mother's pregnancy and delivery were uncomplicated. The patient weighed 3.4 kg (7.5 lb) and was 48.2 cm (1'7") long at birth. He did well in the newborn nursery and was discharged from the hospital on day 2 of life. His mother reports that he is now exclusively breastfed and nurses for 10 minutes on each breast every 3 hours. He has two wet diapers/day and has not had a bowel movement for 2 days. He weighs 2.95 kg (6.5 lb) and is 48.2 cm (1'7'') long. He appears jaundiced on the face and chest. The remainder of the physical examination shows no abnormalities. Laboratory studies reveal: Total bilirubin 15 mg/dl Direct bilirubin 1 mg/dl Infant's blood type 0 positive Mother's blood type A positive Which of the following is the most likely cause of this infant's hyperbilirubinemia?
Breastfeeding failure jaundice
Biliary atresia
Breast milk jaundice
Galactosemia
ABO incompatibility
A 6-year-old female is brought to the physician with a rash and joint pains. Her mother reports that she has been previously healthy except for a sore throat a few weeks ago. One week ago, the patient developed pain in her knees. The knee pain resolved after a few days, but now her ankles and wrists are tender. She has also developed a pink rash on her trunk that is non-pruritic. Vital signs are temperature 38.3°C (101°F), pulse 85/min, and respiratory rate 20/min. On examination, there is pain and stiffness during manipulation of the wrists and ankles. A faint, ery1hematous, centrifugal rash on her trunk and proximal limbs is present. Laboratory studies show: Complete blood count Hemoglobin 12.5 g/dL MCHC 32% MCV 85 fl Reticulocyte count 0.1% Platelet count 200,000/mm3 Leukocyte count 6,500/mm3 Neutrophils 56% Eosinophils 1% Lymphocytes 33% Monocytes 10% C-reactive protein 3.5 mg/dL Erythrocyte sedimentation rate 38 mm/hr Which of the following is the most likely diagnosis?
Rheumatic fever
Juvenile rheumatoid arthritis
Acute lymphoblastic leukemia
Systemic lupus ery1hematosus
Fibromyalgia
A young Hispanic couple brings their first child to their physician for a well-child examination. The child is a 3-month-old healthy-appearing infant, whose weight is at the 45th percentile of the normal growth curve. During examination, the physician observes an area of blue-black pigmentation over the buttocks. The parents say that it was present from the time of birth. Which of the following is the most appropriate next step in management?
Tell parents that this is a normal finding
Tell parents that this is a bruise caused by trauma
Order CT/MRI scans to rule out dysraphism
File a report of suspected child abuse
Tell parents that this is a severe condition finding
A 14-year-old boy presents with decreased exercise tolerance. He is noted to have a grade III/VI systolic ejection murmur best heard at the left upper sternal border and a grade II/VI mid-diastolic murmur at the lower left sternal border. The first heart sound is normal. The second heart sound is widely split and fixed. A right ventricular impulse is palpated. On a chest roentgenogram, the pulmonary artery segment is enlarged, and pulmonary vascular markings are increased. An ECG shows right axis deviation. Which of the following congenital heart diseases does this boy most likely have?
Atrial septal defect
Aortic stenosis
Coarctation of the aorta
Patent ductus arteriosus
Ventricular septal defect
A 7-year-old boy presents with a rash. His mother states that he was well until 3 days ago when he developed fever and malaise. The next day, the rash started as papules on the trunk, which rapidly changed to vesicles. The lesions have spread all over the body. On physical examination, he has no fever and seems well. You note numerous vesicles all over the body, some of which have crusted over. Which of the following is the most likely diagnosis?
Chicken pox
Kawasaki disease
Measles
Rubella
Staphylococcal scalded skin syndrome
A 7-year-old child is scheduled for an elective tonsillectomy. The most important instruction to the parents should be to make sure that the child does which of the following?
Avoids aspirin and antihistamines for 2 weeks before surgery
Avoids contact with other children
Discontinues antibiotics 72 hour before surgery
Does not drink from siblings’ cups
Eats iron-laden foods for 3 weeks before surgery
A 4-month-old baby is in for a well-child check and routine immunizations. The baby had a fever of 39°C the day he received his 2-month immunizations. The parents have read about the vaccine on the Internet and express their concerns. Which of the following is an absolute contraindication to giving the diphtheria and tetanus toxoids and acellular pertussis (DTaP)?
Encephalopathy within 7 days of administration of previous dose of vaccine
History of fever >38C after previous vaccination
History of local reaction after previous vaccination (redness, soreness, swelling)
Family history of seizures
Current antibiotic therapy
The mother and father of a newborn come in for the 2-week checkup. The mother complains of “colic” and asks if she can switch to goat’s milk instead of breast milk. Which of the following should be your main concern about using goat’s milk instead of breast milk or cow’s milk?
It has insufficient folate
It has insufficient calories
It has insufficient whey
It has insufficient casein
It has insufficient fat.

You see the newborn baby shown below for the first time in the nursery. You consult plastic and reconstructive surgeon as well as the hospital’s speech therapist. Understandably, the parents have many questions. Which of the following statements is appropriate anticipatory guidance for this family?
Recurrent otitis media and hearing loss are likely complications
Parenteral alimentation is recommended to prevent aspiration
Surgical closure of the palatal defect should be done before 3 months of age
Good anatomic closure will preclude the development of speech defects
The chance that a sibling also would be affected is 1 in 1000
The mother of a 2-week-old infant reports that since birth, her infant sleeps most of the day; she has to awaken her every 4 hours to feed, and she will take only an ounce of formula at a time. She also is concerned that the infant has persistently hard, pellet-like stools. On your examination you find an infant with normal weight and length, but with an enlarged head. The heart rate is 75 beats per minute and the temperature is 35°C (95°F). The child is still jaundiced. You note large anterior and posterior fontanelles, a distended abdomen, and an umbilical hernia. This clinical presentation is likely a result of which of the following?
Congenital hypothyroidism
Congenital megacolon (Hirschsprung disease)
Sepsis
Infantile botulism
Normal development
A routine prenatal ultrasound reveals a male fetus with meningomyelocele. The 24-year-old primigravid mother is told the infant will require surgery shortly after birth. You counsel her about the etiology of this defect and the risk of further pregnancies being similarly affected, and state which of the following?
Supplementation of maternal diet with folate leads to a decrease in incidence of this condition
The hereditary pattern for this condition is autosomal recessive
The prenatal diagnosis can be made by the detection of very low levels of alpha- fetoprotein in the amniotic fluid
Subsequent pregnancies are not at increased risk compared to the general population
Neither environmental nor social factors have been shown to influence the incidence
A term, 4200-g (9-lb, 4-oz) female infant is delivered via cesarean section because of cephalopelvic disproportion. The amniotic fluid was clear, and the infant cried almost immediately after birth. Within the first 15 minutes of life, however, the infant’s respiratory rate increased to 80 breaths per minute, and she began to have intermittent grunting respirations. The infant was transferred to the level 2 nursery and was noted to have an oxygen saturation of 94%. The chest radiograph is shown. Which of the following is the most likely diagnosis?
Transient tachypnea of the newborn
Diaphragmatic hernia
Meconium aspiration
Pneumonia
Idiopathic respiratory distress syndrome
A 7 -year-old African American boy is brought to your clinic with complaints of bedwetting. He was toilet trained at the age of 4. He has been able to pass urine normally in daytime, but has never been dry at night. There is no history of urgency or frequency during daytime. There is no history suggestive of child abuse. He had two episodes of urinary tract infections (UTI) from birth until he was 2-years-old, but he has not had any episodes ever since. What is the next best step in the management of this patient?
Urinalysis
Intravenous pyelogram
Ultrasound of the kidneys
Prescription of Imipramine
Behavioral modification
A 1-month-old male infant is brought to the emergency department by his mother due to a 3-day history of projectile vomiting. He has been formula- fed since birth, and his bowel movements are normal. He has never been ill before. His parents and 4-year-old sister are all healthy. One of his maternal uncles is mentally retarded. He weighs 3.1 kg (7 Ib). Physical examination reveals fair hair and skin, blue eyes, eczematous rash, and mild signs of dehydration. His urine has a mousy odor. What is the most appropriate screening test for this patient's early diagnosis and treatment?
Guthrie test in urine
Aminolevulinic acid and porphobilinogen in the urine
SerumTSH
Blood level of alfa 1-antiprotease
Serum LDH
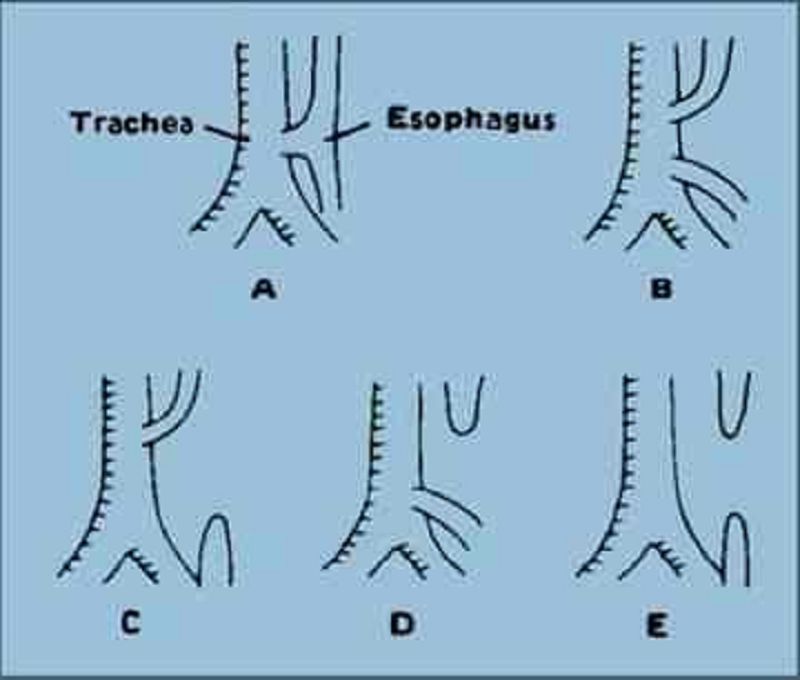
Shortly after birth, an infant develops abdominal distention and begins to drool. When she is given her first feeding, it runs out the side of her mouth, and she coughs and chokes. Physical examination reveals tachypnea, inter- costal retractions, and bilateral pulmonary rales. The esophageal anomaly that most commonly causes these signs and symptoms is illustrated by which of the following?
Figure D
Figure A
Figure B
Figure C
Figure E
You are advised by the obstetrician that the mother of a baby she has delivered is a carrier of hepatitis B surface antigen (HBsAg-positive). Which of the following is the most appropriate action in managing this infant?
Administer hepatitis B immune globulin and hepatitis B vaccine to the infant
Screen the infant for HBsAg
Isolate the infant with enteric precautions
Screen the mother for hepatitis B “e”antigen (HBeAg).
Do nothing because transplacentally acquired antibody will prevent infection in the infant.
You are asked to evaluate a 4-year-old boy admitted to your local children’s hospital with a diagnosis of pneumonia. The parents state that the child has had multiple, intermittent episodes of fever and respiratory difficulty over the past 2 years, including cyanosis, wheezing, and dyspnea; each episode lasts for about 3 days. During each event he has a small amount of hemoptysis, is diagnosed with left lower lobe pneumonia, and improves upon treatment. Repeat radiographs done several days after each event are reportedly normal. His examination on the current admission is significant for findings similar to those described above, as well as digital clubbing. Which of the following is the most appropriate primary recommendation?
Bronchoalveolar lavage
Intravenous cephalosporin and oral macrolide therapy
Modified barium swallow study to evaluate for aspiration
Nasal swab for viral culture
Incentive spirometry
A male infant, born to a 32-year-old white female, develops a bluish discoloration of the extremities and oral mucous membranes at 30 minutes of life. On examination, the infant is found to have tachypnea, nasal flaring and respiratory grunting. Auscultation reveals poor air entry on the left with a shift of cardiac sounds to the right. The abdomen has a scaphoid shape. The antenatal history is significant for polyhydramnios in the mother. The neonatologist on call suspects a diagnosis of congenital diaphragmatic hernia. What is the most appropriate next step in the management of this neonate?
Orogastric tube placement
Chest X-ray (anteroposterior view)
Cardiac ultrasonography
Bag-and-mask ventilation
Chest tube placement
A few weeks after a presumed viral respiratory infection, a 4-year-old girl presents with bruising and petechiae. Bone marrow examination reveals increased numbers of megakaryocytes but is otherwise normal. Hb is 13.5 g/100 mL. Platelet count is 30,000/mm3. Which of the following would be appropriate for this child at this time?
No specific therapy
Daily prednisone
A transfusion of packed RBCs and platelets
IV gamma globulin
Splenectomy
An 18-month-old child presents to the emergency center having had a brief, generalized tonic-clonic seizure. He is now postictal and has a temperature of 40C (104F). During the lumbar puncture (which ultimately proves to be normal), he has a large, watery stool that has both blood and mucus in it. Which of the following is the most likely diagnosis in this patient?
Shigella
Salmonella
Enterovirus
Rotavirus
Campylobacter
A 6-year-old Caucasian boy is brought to the emergency room by his mother with hemiplegia of acute onset. She states that she found the boy unconscious in his room where she had left him playing several minutes ago; and, he slowly gained consciousness, but could not move his right arm and leg. His past medical history is insignificant. Physical examination reveals right hemiparesis with little sensory abnormalities. No meningeal signs are present. The motor function restored spontaneously during 24-hour observation in the hospital. A CT scan of the head is normal. What is the most probable cause of this patient's problem?
Seizure
Homocystinemia
Nephrotic syndrome
Antiphospholipid antibodies
Congenital heart disease
A 6-year-old female with Down syndrome is brought to the physician for behavioral changes. Over the past few weeks, she has begun refusing to do her usual activities. Her parents also report that she seems dizzy and state that she has developed urinary incontinence. On examination, she is hypotonic but hyperreflexic with a positive Babinski reflex. Her gait is ataxic. Which of the following is the most likely diagnosis?
Atlantoaxial instability
Alzheimer disease
Hypothyroidism
Mental retardation
Spinal cord infarction
A 16-day-old infant presents with fever, irritability, poor feeding, and a bulging fontanelle. Spinal fluid demonstrates gram-positive cocci. Which of the following is the most likely diagnosis?
Group B streptococci
Listeria monocytogenes
Group A streptococci
Streptococcus pneumoniae
Staphylococcus aureus
A 16-year-old boy presents to the emergency center with a 2-day history of an abscess with spreading cellulitis. While in the emergency center, he develops a high fever, hypotension, and vomiting with diarrhea. On examination you note a diffuse erythematous macular rash, injected conjunctiva and oral mucosa, and a strawberry tongue. He is not as alert as when he first arrived. This rapidly progressive symptom constellation is likely caused by which of the following disease processes?
TSST-1–secreting S aureus
Kawasaki disease
Shiga toxin–secreting Escherichia coli
ρ�-Toxin–secreting Clostridium perfringens
Neurotoxin-secreting Clostridium tetani

A 6-month-old Hispanic boy is brought to the office for a well-baby check-up and follow-up immunizations. His mother denies any new complaints. Physical examination reveals lesions that do not fade into the surrounding skin, shown in picture below. What is the most appropriate next step in the management of this patient?
Do nothing. Since it is likely that these lesions will disappear in the next few years
Perform fundoscopy to rule out retinal hemorrhages
Coagulation tests to rule out a coagulopathy
Immediately report to the authorities for child abuse
Schedule for excisional therapy with laser
A bat is found in the bedroom of a 4-year-old patient while the boy is sleeping. The family and the patient deny close contact with or bites from the bat. Which of the following is a correct statement regarding this situation?
The patient should be started on the rabies vaccine series
Therapy is only required if the patient shows signs of rabies infection
Bats are not a natural reservoir for rabies virus; no therapy is required
The patient needs immediate treatment with acyclovir
The patient needs immediate treatment with ribavirin
An 8-year-old Cub Scout who returned from an outing 9 days ago is brought to the clinic with the rapid onset of fever, headache, muscle pain, and rash. The maculopapular rash began on the flexor surfaces of the wrist and has become petechial as it spread inward to his trunk. Which of the following is the most likely diagnosis?
Rocky Mountain spotted fever
Lyme disease
Tularemia
Measles
Toxic shock syndrome
A 10-year-old boy presents with red discoloration of the urine since the morning. He is healthy and otherwise asymptomatic. He denies dysuria, frequency, urgency, flank, or abdominal pain. His BP is normal. His examination is within normal limits including abdomen and genitourinary system. There is no rash or edema. His urine is pink in color; urinalysis is negative for hemoglobin or protein. No white cells, red cells, or bacteria are noted. Which of the following is the most appropriate next step?
Obtain a recent dietary and drug history
Obtain a urine culture
Test for myoglobin in the urine
Obtain a renal ultrasound
Obtain antistreptococcal antibodies
A 12-year-old girl has had a sore throat over 2 days. She now has a fever of 39.5°C and has difficulty opening her mouth, swallowing, or speaking. Her throat can be visualized with difficulty, the right tonsil is significantly more enlarged than the left, and the uvula is displaced to the left side. Which of the following is the most likely diagnosis?
Peritonsillar abscess
Retropharyngeal abscess
Acute uvulitis
Acute pharyngitis
Lateral pharyngeal abscess
A 2-year-old patient arrives late to your office with his father and a sign-language translator. They are very apologetic, but the father communicates that he had car trouble at his dialysis center and thus was late picking up the child from day care. The father is concerned about his child’s having intermittent red, bloody-looking urine. A gross inspection of the child’s urine in your office looks normal, but the dipstick demonstrates 3+ blood. Which of the following is the most likely cause of this child’s hematuria?
Alport syndrome
Berger nephropathy (IgA nephropathy)
Idiopathic hypercalciuria
Membranousglomerulopathy
Goodpasture syndrome
A 2-year-old boy is brought to the clinic by his mother because he is lethargic and not as active as the other kids on their block. He has difficulty walking and getting up, and he always appears tired. His mother thinks that she has a relative with a disorder that causes weakness. On examination, the child is alert but quiet. His calves appear hypertrophied. His reflexes are depressed. When he gets up from the floor, he uses his hands to climb on his legs to assume an upright position. What is the most likely diagnosis of this child?
Duchenne muscular dystrophy
Myasthenia gravis
Dermatomyositis
Polio myelitis
Fragile X syndrome
A 2-month-old male infant is rushed to the emergency department by his baby sitter. She says that the baby became unresponsive and blue while feeding. The whole episode lasted 45-60 seconds, but the baby still appears pale. She denies any history of coughing or choking. On examination, the infant appears cyanotic and tachypneic. His blood pressure is 90/60 mm of Hg; his pulse rate is 155/min and regular. On auscultation, a harsh pansystolic murmur is noted at the left sternal border, along with a single S2. Hepatomegaly is noted. Pulse oximetry shows an oxygen saturation of 80%. Based on this history and physical examination, what is the most likely diagnosis?
Tetralogy of Fallot
Truncus arteriosus
Ventricular septal defect
Patent ductus arteriosus
Transposition of great vessels
A 9-year-old boy comes to the office for a pre-participation physical examination for summer camp. His parents report that he still has episodes of bed-wetting. The boy’s father confides that he also had bed-wetting until he was 10. They are concerned about the bed-wetting, but they are more concerned about their son’s upcoming week at summer camp and that the other boys may harass him for wetting the bed. Which of the following statements about nocturnal enuresis is correct?
Spontaneous cure rates are high regardless of therapy
The condition is three times more common in girls than boys
Most patients with this condition have a psychiatric illness as the cause
Family history of this condition is uncommon
Short courses of desmopressin acetate (DDAVP) lead to permanent cure in 50% of cases
A 13-year-old asymptomatic girl is shown below. She states that the findings demonstrated began more than a year ago. Which of the following is the most likely diagnosis?
Lymphocytic (Hashimoto) thyroiditis
Iodine deficiency
Congenital hypothyroidism
Graves’ disease
Exogenous ingestion of Synthroid
During a routine well-child examination a 10-year-old girl reports that she has occasional headache, “racing heart,” abdominal pain, and dizziness. Her mother states that she has witnessed one of the episodes, which occurred during an outing at the mall, and reported the child to be pale and to have sweating as well. Other than some hypertension, she has a normal physical examination. Evaluation of this child is most likely to result in which of the following diagnoses?
Pheochromocytoma
Hysterical fainting spells
Pregnancy
Diabetesmellitus
Migraine headache

A 4-year-old boy presents to the physician with fever and a sore throat. His illness began with rhinorrhea, cough, and congestion one week ago, but in the last 24 hours he has developed fever, a sore throat, and neck pain. His mother also reports that he sounds hoarse. His appetite is decreased and he complains of dysphagia. His temperature is 39.7 C (103.5F), pulse is 10O/min, and respiratory rate is 25/min. On examination, the child appears sick. He has cervical lymphadenopathy on the right and decreased range of motion of his neck. His voice is muffled and sounds hoarse. His oropharynx is erythematous and a bulge is noted in the posterior pharyngeal wall. A lateral radiograph of the neck is shown below. Which of the following is the most likely diagnosis?
Retropharyngeal abscess
Infectious mononucleosis
Epiglottitis
Viral pharyngitis
Diphtheria
A 20-month-old male is brought to the emergency department for evaluation of rectal bleeding after his parents discovered a substantial amount of maroon colored stool when changing his diaper. He has no history of hematochezia. The patient has been otherwise healthy and has not appeared to be in any pain. He has been eating and drinking well. His temperature is 3rC (98.6.F), blood pressure is 85/50 mmHg, pulse is 130/min, and respiratory rate is 20/min. On examination, the abdomen is soft, nondistended, and nontender. On rectal examination, there are no fissures or masses present. A fecal occult blood test is positive. The remainder of the physical examination is normal. Which of the following is the best test to confirm the diagnosis?
Technetium-99m pertechnetate scan
Abdominal radiography
Superior mesenteric arteriography
Barium enema
Abdominal CT scan

A 10-year-old obese child (shown below) has central fat distribution, arrested growth, hypertension, plethora, and osteoporosis. Which of the following disorders is most likely responsible for the clinical picture that this boy presents?
Bilateral adrenal hyperplasia
Adrenaladenoma
Adrenal carcinoma
Craniopharyngioma
Ectopic adrenocorticotropin-producing tumor
A 6-year-old boy is brought to your practice by his paternal grandmother for his first visit. She has recently received custody of him after his mother entered the penal system in another state; she does not have much information about him. You note that the child is short for his age, has downslanting palpebral fissures, ptosis, low-set and malformed ears, a broad and webbed neck, shield chest, and cryptorchidism. You hear a systolic ejection murmur in the pulmonic region. His grandmother reports that he does well in regular classes, but has been diagnosed with learning disabilities and receives speech therapy for language delay. His constellation of symptoms is suggestive of which of the following?
Noonan syndrome
Congenital hypothyroidism
Turner syndrome
Congenital rubella
Down syndrome
A 2-week-old infant is noted to be jaundiced. The baby's stools are pale, and his urine darkly colored. Physical examination demonstrates hepatomegaly. Serum studies show elevations of AST, ALT, conjugated bilirubin, and unconjugated bilirubin. By 2 months of age, the baby is notably irritated by pruritus, has retarded growth, and has visible dilated veins in the periumbilical area. Ultrasound fails to demonstrate a gallbladder. Which of the following is the most likely diagnosis?
Biliary atresia
Alpha-1-antitrypsin deficiency
Cystic fibrosis
Hepatitis B
Hepatitis C
A 3-year-old girl with a ventricular septal defect (VSD) presents to the emergency department after a 15-minute focal seizure of her left arm and leg. A brief history reveals that the child has no known seizure disorder and has been having a low-grade fever at home for about 4 days. She also has been less active and has had poor appetite. On physical examination, her temperature is 40.2 C (104.3 F), and her pulse is 82/min. She is not responsive to her name, but she is responsive to painful stimuli with withdrawal of her extremities. Cardiac examination is significant for a grade 3 systolic murmur best heard at the left lower sternal border. Neurologic examination reveals anisocoria with a dilated right pupil. After stabilization, which of the following is the most appropriate next step in diagnosis?
CT of the brain
ECG
Electroencephalography
MRI of the brain
Complete blood count and blood culture
Lumbar puncture
A mother brings her 7-year-old son to the clinic because, over the past several days, his urine has become pink and bis eyes have looked puffy. About 2 weeks ago, he missed school because of fever and a sore throat. On examination, the boy's blood pressure is 130/85 mm Hg, his eyelids and scrotum appear puffy, and he has 1+ tibial edema. No rashes are noted. Which of the following is the most likely diagnosis?
Acute poststreptococcal glomerulonephritis
Hemolytic-uremic syndrome
Henoch-Schonlein purpura
Vesicoureteral reflux
Nephrotic syndrome

The examination of a child’s back is shown below. Evaluation with ultrasound of this lesion may demonstrate which of the following?
Occult spina bifida
Epsteinpearl
Mongolian spot
Cephalohematoma
Omphalocele
A 6-month-old child was noted to be normal at birth, but over the ensuing months you have been somewhat concerned about his slowish weight gain and his mild delay in achieving developmental milestones. The family calls you urgently at 7:00 AM noting that their child seems unable to move the right side of his body. Which of the following conditions might explain this child’s condition?
Homocystinuria
Phenylketonuria
Cystathioninuria
Maple syrup urine disease
Histidinemia
On a newborn boy’s first examination, you note a prominent occiput, a broad forehead, and an absent anterior fontanelle. The baby’s head is long and narrow. The remainder of the physical examination, including a careful neurological evaluation, is normal. You note that the baby was born via cesarean section for cephalopelvic disproportion. When you enter the mother’s room, the first question she asks is about her baby’s head shape. Which of the following is the most appropriate statement to the mother about this infant’s condition?
The condition requires referral to a surgeon
The condition is usually associated with other genetic defects
The condition is usually associated with hydrocephalus
Patients with this condition usually develop seizures
The condition is associated with pituitary abnormalities
An 18-month-old male infant is brought to the office by his parents for a follow-up visit. He has a congenital condition that started at the age of 6 months with repeated vomiting and hypotonia, and progressively evolved into choreoathetosis, spasticity and dystonia. Over the past month, he has started biting his hands and arms, pinching himself and banging his limbs against the wall. His family history is unremarkable. On examination, he has several scars, cuts and bruises over his arms and hands. His uric acid levels are elevated. What is the most likely deficient enzyme in this patient?
Hypoxanthine-guanine phosphoribosyl transferase
Glutamine-phosphorylase pyrophosphate aminotransferase
Xanthine oxidase
Adenyl succinate synthase
Purine nucleoside phosphorylase
You are asked by a colleague to evaluate a 5-year-old boy as a second opinion. He has a history of chronic and recurrent upper respiratory tract infections, several admissions to the hospital for pneumonia, and three surgeries for PE tubes for chronic otitis media. Of note is a right-sided heart on repeated radiographs. Convinced you know the diagnosis based on history alone, you confirm your diagnosis with a biopsy of the nasal mucosa. You expect to find which of the following?
Random orientation of cilia
Eosinophilic infiltrate
Bordetella pertussis
Absence of nasal mucous glands
Nasal polyps
A 13-year-old patient with sickle-cell anemia presents with respiratory distress; she has an infiltrate on chest radiograph. The laboratory workup of the patient reveals the following: hemoglobin 5 g/dL; hematocrit 16%; white blood cell count 30,000/μL; and arterial blood (room air) pH 7.1, PO2 35 mm Hg, and PaCO2 28 mm Hg. These values indicate which of the following?
Acidemia, metabolic acidosis, respiratory alkalosis, and hypoxia
Alkalemia, respiratory acidosis, metabolic alkalosis, and hypoxia
Acidosis with compensatory hypoventilation
Long-term metabolic compensation for respiratory alkalosis
Primary respiratory alkalosis
An otherwise healthy 7-year-old child is brought to you to be evaluated because he is the shortest child in his class. Careful measurements of his upper and lower body segments demonstrate normal body proportions for his age. Which of the following disorders of growth should remain in your differential?
Growth hormone deficiency
Achondroplasia
Morquio disease
Marfan syndrome
Hypothyroidism
A 15-year-old girl is brought to the pediatric emergency room by the lunchroom teacher, who observed her sitting alone and crying. On questioning, the teacher learned that the girl had taken five unidentified tablets after having had an argument with her mother about a boyfriend of whom the mother disapproved. Toxicology studies are negative, and physical examination is normal. Which of the following is the most appropriate course of action?
Hospitalize the teenager on the adolescent ward.
Get a psychiatry consultation
Get a social service consultation
Arrange a family conference that includes the boyfriend
Prescribe an antidepressant and arrange for a prompt clinic appointment
4-year-old immigrant boy is brought by his mother to a Medical Camp for the Uninsured for the evaluation of his inflamed right eye. He has had a nasal discharge for the past 10 days. His brother has similar symptoms. His vital signs are stable. There are follicles and inflammatory changes in the conjunctiva of his right eye. The cornea shows neovascularization. What is the most likely diagnosis?
Trachoma
Herpes simplex keratitis
Orbital cellulitis
Gonococcal conjunctivitis
Viral conjunctivitis
A previously healthy 7-year-old child suddenly complains of a headache and falls to the floor. When examined in the emergency room (ER), he is lethargic and has a left central facial weakness and left hemiparesis with conjugate ocular deviation to the right. Which of the following is the most likely diagnosis?
Acute infantile hemiplegia
Hemiplegic migraine
Supratentorial tumor
Todd paralysis
Acute subdural hematoma
An irritable 6-year-old child has a somewhat unsteady but nonspecific gait. Physical examination reveals a very mild left facial weakness, brisk stretch reflexes in all four extremities, bilateral extensor plantar responses (Babinski reflex), and mild hypertonicity of the left upper and lower extremities; there is no muscular weakness. Which of the following is the most likely diagnosis?
Pontineglioma
Cerebellar astrocytoma
Tumor of the right cerebral hemisphere
Subacute sclerosing panencephalitis
Progressivemultifocalleukoencephalopathy
A 5-year-old girl is diagnosed with Bordetella pertussis infection after an outbreak in the day-care center. She is prescribed erythromycin for 14 days. She lives with her parents and 13-year-old sister whose immunizations are up to date. What is the most appropriate way to limit the risk of infection in household contacts?
Prescribe erythromycin for 14 days to all household contacts
Administer pertussis immunization to all household contacts
Prescribe erythromycin for 14 day to the mother and father only
Administer pertussis immunization to the parents only
Keep the child hospitalized until symptoms disappear
A 2-year-old boy is rushed to the emergency department by his 21 -year-old white mother because he had a sudden-onset nosebleed which has now subsided. He never had any previous episodes. He is "sickly" and suffers from a productive cough and diarrhea that "refuses to go." His stools are greasy and foul-smelling. His appetite is normal, although his diet consists mainly of milk. His mother's boyfriend lives with them and is a chronic alcoholic. He was delivered vaginally without any complications. His weight is at the 25th percentile for his age. Physical examination reveals dry skin and dried blood at the nasal turbinates. What is the most likely cause of this child's failure to thrive?
Deficiency of pancreatic enzymes
Lactose intolerance
Parental neglect
Chronic parasitic infection
Constitutional growth delay
A 6-year-old boy had been in his normal state of good health until a few hours prior to presentation to the ER room. His mother reports that he began to have difficulty walking, and she noticed that he was falling and unable to maintain his balance. Which of the following is the most likely cause for his condition?
Drug intoxication
Agenesis of the corpus callosum
Ataxiatelangiectasia
Muscular dystrophy
Friedreich ataxia
A 9-year-old child has developed headaches that are more frequent in the morning and are followed by vomiting. Over the previous few months, his family has noted a change in his behavior (generally more irritable than usual) and his school performance has begun to drop. Imaging of this child is most likely to reveal a lesion in which of the following regions?
Subtentorial
Supratentorial
Intraventricular
Spinal canal
Peripheral nervous system
6-month-old male is brought to the office due to fussiness and tugging at his right ear for the past 2 days. He has had a fever of 39.4° C (103° F) for the past 2 days. His past medical history is significant for recurrent ear and lung infections, oral candidiasis, and persistent diarrhea by rotavirus. His temperature is 39.4° C (103° F), pulse rate is 150/min, respirations are 28/min, and blood pressure is 80/60mm Hg. Physical examination reveals an ery1hematous, bulging right tympanic membrane with poor mobility on pneumatic otoscopy. His lymph nodes are not palpable, and his tonsils are not visualized. His B and T lymphocyte levels are markedly reduced. The chest x-ray reveals an absent thymic shadow. What is the most likely etiology of this patient's condition?
Severe combined immune deficiency
Common variable immunodeficiency
Bruton's agammaglobulinemia
Wiskott-Aldrich syndrome
Chronic granulomatous disease
{"name":"999 Questions Pediatrie-MCQ-(301-600) Part 1 NR", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"You admitted to the hospital the previous evening a 1-year-old boy who presented with cough, fever, and mild hypoxia. At the time of his admission, he had evidence of a right upper lobe consolidation on his chest radiograph. A blood culture has become positive in less than 24 hours for Staphylococcus aureus. Approximately 20 hours into his hospitalization, the nurse calls you because the child has acutely worsened over the previous few minutes, with markedly increased work in breathing, increasing oxy- gen requirement, and hypotension. As you move swiftly to the child’s hospital room, you tell the nurse to order which of the following?, A 15-year-old boy has been immobilized in a double hip spica cast for 6 weeks after having fractured his femur in a skiing accident. He has become depressed and listless during the past few days and has complained of nausea and constipation. He is found to have microscopic hematuria and a blood pressure of 150\/100 mm Hg. Which of the following is the most appropriate course of action?, An adolescent with type 1 diabetes returns for a follow-up visit after his annual checkup last week. You note that his serum glucose is elevated and his glycosylated hemoglobin (hemoglobin A1C) is 16.7%. This finding suggests poor control of his diabetes over at least which of the following time periods?","img":"https://cdn.poll-maker.com/10-462816/8.jpg?sz=1200"}
More Quizzes
Part2 WUKONG 5 (385-418) 255-509
100500
Discover Your Ideal Car Journey
4222
Substance Abuse in the US
100
Balance cell bio
10519
Am I a Loner - Discover Your Solo Type (Free)
201017718
English B1 Test Online - Free Placement Level Check
201016475
European Countries: Play Free Online
201017718
Once Upon a Time Season 1 - Test Your Knowledge
201018370
Trade Coffee - Test Your Coffee Market Knowledge
201019008
Perfume - Find Your Signature Scent
201017857
Which Egyptian God Are You? - Find Your Divine Parent
201017649
Free Anatomy - Basic Human Body (15 Questions)
201018294