USMLE PART3.1 (OPTHALMO)
A 1-year-old boy is brought to the clinic by his 28-year-old Caucasian mother for the evaluation of his eyes. For the past several months, he has been bumping into objects. His perinatal history is unremarkable. Physical examination of the eyes reveals a bilateral white reflex. The retina cannot be visualized properly. Fundal reflection is absent, and the pupil is white. What is the most likely diagnosis?
Congenital glaucoma
Congenital cataract
Retinoblastoma
Pterygium
Glocoma
A 53-year-old man comes to the office because of difficulty reading fine print over the last year. He now has to hold books, menus, and magazines at an arm’s length in order to read them. He has never had visual problems before. Which of the following is most likely abnormal in this patient?
Corneal shape
Lens elasticity
Lens opacity
Macula
Peripheral retina
A 65-year-old white man is complaining of a sudden loss of vision in his left eye which resolved after 15 minutes. "It seemed like a curtain was falling down in my eye!" said the patient. He recalls having a similar episode 3 months ago. His past medical history is significant for hypertension, for which he takes lisinopril (20mg) and hydrochlorothiazide (25mg) daily. His pulse is 82/min, blood pressure is 140/90 mm Hg, respirations are 14/min, and temperature is normal. Fundoscopy reveals zones of whitened, edematous retina following the distribution of the retinal arterioles. What is the most likely diagnosis?
Central retinal artery occlusion
Amaurosis fugax
Central retinal vein occlusion
Vitreous hemorrhage
Hypertensive retinopathy
A 3-day-old female infant is noticed to have copious, purulent discharge from both eyes. Lid edema and chemosis are also noted. She was born by normal vaginal delivery. Her mother is a 20-year-old primigravida who had no prenatal care. Which of the following is the most likely diagnosis?
Chlamydia trachomatis
Staphylococcus aureus conjunctivitis
Chemical conjunctivitis
Nasolacrimal duct obstruction
Gonococcal conjunctivitis
A 22-year-old Caucasian female presents to the office with several months history of decreased visual acuity and decreased brightness sensation in the right eye. Slight exophthalmos of the right eye is present on physical examination, and ophthalmoscopy shows pallor of the right optic disk. Several cafe-au-lait spots and intensive axillary freckling are present. Which of the following is the most likely cause of this patient's visual problems?
Pigment retinitis
Retinal hamartoma
Optic glioma
Pituitary adenoma
Optic neuritis
A 65-year-old African American man comes to the emergency department due to a sudden loss of vision in his right eye. He has had diabetes, and has been treated with metformin and glyburide for the past 10 years. Visual acuity is reduced to light perception in his right eye, and normal in his left. His vital signs are normal. Ophthalmoscopy reveals loss of fundus details, floating debris and a dark red glow. What is the most likely diagnosis?
Retinal detachment
Diabetic retinopathy
Vitreous haemorrhage
Central retinal vein occlusion
Age related macular degeneration
A 62-year-old female is brought in by EMS due to a severe right-sided headache, nausea and eye pain. She was fixing a light bulb, when she suddenly felt pain in her right eye. She decided to rest, but the eye pain only got worse. In the next few minutes, she developed loss of vision, photophobia and redness in the same eye. She took medications to relieve the accompanying headache, but the eye pain persisted. She denies any trauma. Her past medical history is significant for diabetes and hypertension. She appears to be in intense pain with bouts of nausea. Her right eye is red, with conjunctival flushing and visual acuity of 20/200. Her right pupil is mid-dilated and non-reactive to light. The same eye feels hard on palpation. The one treatment that should be avoided in this patient is:
Mannitol
Acetazolamide
Pilocarpine
Timolol
Atropine
A 60-year-old woman complains of decreasing vision and a dull ache over her left eye for the past 12 hours. She had a successful surgical cataract extraction in her left eye five days ago. Her blood pressure is 140/90 mmHg, pulse is 92/min, respirations are 14/min, and temperature is 38.1C (101.7F). Examination of the left eye reveals a swollen eyelid, edematous conjunctiva, and exudates in the anterior chamber. Testing with Snellen's chart demonstrates decreased visual acuity in her left eye. What is the most likely diagnosis?
Conjunctivitis
Corneal ulceration
Uveitis
Postoperative endophthalmitis
Cavernous sinus thrombosis

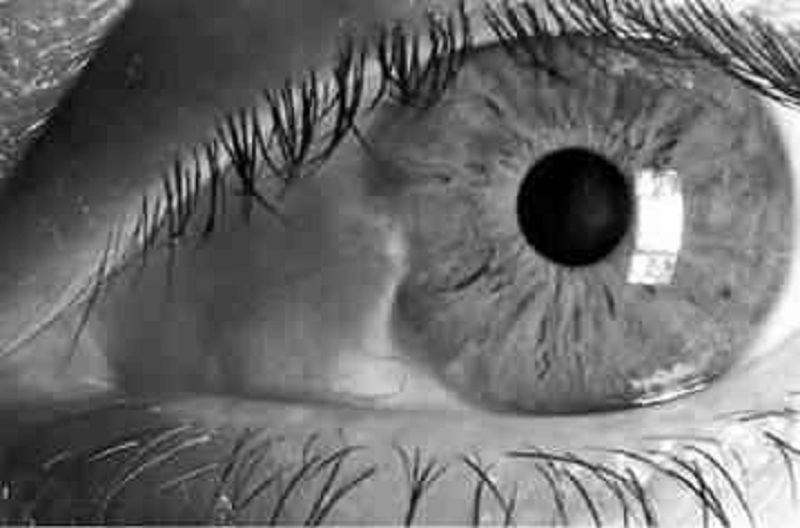
A 34-year-old male presents to the emergency department with a red eye. He says, "I just woke up this morning and saw that my right eye was red." He denies any itching, pain or discharge. He has no known drug or environmental allergies. He takes no medication. His vital signs are stable. The photo of his eye is shown below. What is the best next step in his management?
Check intraocular pressure
Refer to ophthalmologist
Check coagulation parameters
Observation
Antibiotics
A 65-year-old male comes to the emergency department because of a sudden, painless loss of vision in his right eye that occured a half an hour ago. Five hours ago, he experienced a similar but transient loss of vision in the same eye, which lasted for five minutes. He has hypertension, diabetes, hypercholesterolemia, and peripheral vascular disease. He had an anterior wall myocardial infarction six years ago. His medications include glyburide, captopril, atenolol, simvastatin and aspirin. His temperature is 36.7C (98.0F), respirations are 16/min, pulse is 88/min, and blood pressure is 146/88 mmHg. Examination of the right eye reveals visual acuity of 20/60 and subtle retinal whitening. A right carotid bruit is heard. Which of the following is the most appropriate next step in the management of this patient?
Acetazolamide IV
Ocular massage and high flow oxygen
Administer systemic steroids
Instillation of topical beta blocker
Administer thrombolytics
A 26-year-old male complains of itching and excessive watering of both eyes since this morning. He denies blurring of vision. He uses albuterol inhaler regularly for his bronchial asthma. His vital signs are normal. On examination, both eyes are noted to have conjunctival edema, hyperemia, swollen eyelids, and profuse watery discharge. What is the most likely diagnosis?
Atopic keratoconjunctivitis
Allergic conjunctivitis
Toxic conjunctivitis
Blepharitis
Dacryocystitis.
A 4-year-old boy is brought by his mother to a Medical Camp for the Uninsured for the evaluation of his inflamed right eye. He has had a nasal discharge for the past 10 days. His brother has similar symptoms. His vital signs are stable. There are follicles and inflammatory changes in the conjunctiva of his right eye. The cornea shows neovascularization. What is the most likely diagnosis?
Herpes simplex keratitis
Orbital cellulitis
Trachoma
Gonococcal conjunctivitis
Viral conjunctivitis
A 60-year-old woman comes to the emergency department due to a sudden onset of severe pain in her left eye with blurred vision, nausea, and vomiting. The symptoms began a few minutes ago, while she was watching a movie in a nearby theatre. Her blood pressure is 140/90 mm Hg, pulse is 82/min, respirations are 14/min, and temperature is 98.4 F. Examination reveals decreased visual acuity. Her left eye appears red, with a hazy cornea, shallow anterior chamber, and dilated, fixed pupil. Her left eye is stony hard to touch. What is the most likely diagnosis?
Primary open angle glaucoma
Conjunctivitis
Acute angle closure glaucoma
Anterior uveitis
Corneal abrasion
A 32-year-old male construction worker presents with complaints of pain, watering, and redness in his left eye for the past 2 days. He reports having similar symptoms in the same eye a few months ago. Examination of his left eye reveals vesicles and dendritic ulcers in the cornea. His vital signs are stable. What is the most likely diagnosis?
Bacterial retinitis
Herpes simplex keratitis
Herpes zoster ophthalmicus
Corneal abrasion
Fungal keratitis
A 30-year-old male comes to the emergency department screaming, "Something blew into my right eye while I was drilling I' He complains of a foreign body sensation in the right eye, photophobia, and excessive lacrimation. Gross examination of the right eye with a penlight after the application of a topical anesthetic is insignificant. What is the best next step in the management of this patient?
Tonometry
Fluorescein examination
Topical antibiotic
Ultrasonography
MRI of the orbits
A 35-year-old HIV-positive male is complaining of deterioration of his vision over the past week. He initially experienced eye pain and mild conjunctivitis, followed by rapid progressive visual loss. Examination of his eyes reveals marked keratitis. Funduscopy shows widespread, pale, peripheral retinal lesions and central necrosis of the retina. Which of the following is the most likely causative organism of this patient's condition?
Pseudomonas
Cytomegalovirus
Herpes simplex
Candida albicans
Epstein Barr virus
A 38-year-old man with AIDS (Acquired Immune Deficiency Syndrome) is complaining of diminished vision in both eyes. His CD4 count last month was 50 ells/uL. He has been on highly active antiretroviral therapy for the past several months. He is afebrile, and his vital signs are stable. Ophthalmoscopic examination reveals yellow-white patches of retinal opacification and retinal hemorrhages. What is the most likely diagnosis?
Ocular toxoplasmosis.
Herpes simplex keratitis.
Herpes-zoster ophthalmicus.
CMV Retinitis.
HIV retinopathy.
A 65-year-old man presents with complaints of decreased vision in both eyes. His visual impairment has been progressively worsening over the past five months. He was diagnosed with diabetes ten years ago. His current medications are metformin and glyburide. His blood pressure is 140/90 mm Hg, pulse is 82/min, respirations are 14/min, and temperature is 98.4F (36.88C). Examination shows decreased visual acuity in both eyes. Ophthalmoscopy reveals microaneurysms, dot and blot hemorrhages, hard exudates, and macular edema. Which of the following is the most likely diagnosis?
Central retinal vein occlusion
Diabetic retinopathy
Macular degeneration
Retinal detachment
Open angle glaucoma
A 69-year-old white male presents to your office complaining of progressive bilateral loss of vision over the past several months. He only has problems with his central vision. His peripheral field and navigational vision are not affected. He denies smoking and alcohol intake. He does not have any history of diabetes or hypertension Two years ago, he had cataracts removed from both eyes. What is the most likely diagnosis?
Open angle glaucoma
Macular degeneration
Recurrent cataracts
Central retinal artery occlusion
Retinal detachment
A 57-year-old female with a history of type 2 diabetes mellitus complains of fatigue, urinary frequency, increasingly blurred vision and worsening leg cramps over the past week. She reports that the symptoms all began following an upper respiratory infection 7 or 8 days ago. She does not take any medications, but adheres to a diet low in saturated fat and simple carbohydrates to manage her diabetes. On physical examination, her blood pressure is 160/90 mmHg and her heart rate is 90/min. Her mucous membranes are dry. Her urine is positive for glucose but negative for ketones. Which of the following is the most likely cause of this patient's vision impairment?
Cataracts
Diabetic retinopathy
Arterial hypertension
Hyperosmolarity
Eye infection
An 80-year-old white male comes to the emergency department due to a sudden loss of vision in his left eye that occurred this morning upon waking up. He has had hypertension for the past several years. Current medications include ramipril and atenolol. His blood pressure is 140/90 mm Hg, pulse is 86/min, respirations are 14/min, and temperature is 36.8°C (98.4.F). Examination of the left eye reveals no abnormalities. Funduscopic examination shows swelling of the optic disk, retinal hemorrhages, dilated and tortuous veins, and cotton wool spots. Which of the following is the most likely diagnosis?
Acute angle-closure glaucoma
Optic neuritis
Central retinal vein occlusion
Amaurosis fugax
Acute anterior uveitis
A 32-year-old woman comes to the office distraught because "the colors look washed out I" She has had this vision impairment since yesterday. She also complains of pain on eye movements. Her vital signs are stable, and she is afebrile. Examination reveals decreased visual acuity, sluggish afferent pupillary response to light, and changes in color perception. Fundoscopy reveals a swollen disc. What is the most likely diagnosis?
Orbital cellulitis
Optic neuritis
Acute anterior uveitis
Open angle glaucoma
Episcleritis
A 34-year-old obese Caucasian female complains of periodic visual obscurations. She has episodes during which she "goes blind" for several seconds when standing up or stooping forward abruptly. She also describes frequent morning headaches over the last two months for which she has had to take ibuprofen or aspirin almost every morning. She takes no other medications. Past medical history is insignificant aside from one uncomplicated vaginal delivery. She denies use of alcohol, tobacco, or illicit drugs. She is afebrile with a blood pressure of 138/88 mmHg and pulse of 93/min. Visual field testing shows enlarged blind spots. There are no other significant findings on neurologic examination. Which of the following is the most likely cause of this patient's symptoms?
Optic neuritis
Optic neuritis
Cataract
Papilledema
Amaurosis fugax
A 34-year-old obese Caucasian female complains of periodic visual obscurations. She has episodes during which she "goes blind" for several seconds when standing up or stooping forward abruptly. She also describes frequent morning headaches over the last two months for which she has had to take ibuprofen or aspirin almost every morning. She takes no other medications. Past medical history is insignificant aside from one uncomplicated vaginal delivery. She denies use of alcohol, tobacco, or illicit drugs. She is afebrile with a blood pressure of 138/88 mmHg and pulse of 93/min. Visual field testing shows enlarged blind spots. There are no other significant findings on neurologic examination. Which of the following is the most likely cause of this patient's symptoms?
Optic neuritis
Optic neuritis
Cataract
Papilledema
Amaurosis fugax
An 85-year-old man presents with a rash over his forehead, tip of nose and left eye. He also complains of pain and decreased vision. He has had fever, malaise, and a burning sensation around his left eye for the past 5 days. His blood pressure is 140/90 mm Hg, pulse is 92/min, respirations are 14/min, and temperature is 38.1C (101F). Physical examination reveals a vesicular rash on the periorbital region and lid margins. The left eye is red, with chemosis of the conjunctiva. Dendriform ulcers are seen on the cornea. What is the most likely diagnosis?
Herpes simplex keratitis
Dacryocystitis
Bacterial keratitis
Trigeminal neuralgia
Herpes zoster ophthalmicus
A 33-year-old man presents with a 1-day history of localized, small swelling along the margin of the upper eyelid. He feels pain, which does not seem to come from the conjunctival surface. He has a 10-pack year smoking history. He occasionally drinks alcohol. He is sexually active, and does not use condoms regularly. He is worried about the swelling. What is the best next step in the management of this patient?
Use warm compresses
Incision and drainage
Incision and curettage
Take biopsy of the lesion
Oral Penicillin
A 30-year-old man is concerned about "floating spots" and blurred vision in his right eye. He had a serious injury of his left eye several weeks ago, which eventually led to vision loss in that eye. Inspection reveals a moderate perilimbal flush. What is the most probable cause of this patient's condition?
Reagin-mediated disease
Circulating immune complexes
Non-caseating granulomas
Uncovering of 'hidden' antigens
Non-immune injury
A 65-year-old female is complaining of seeing a sudden burst of flashing lights and blurred vision in her left eye. These symptoms started this morning. She now sees small spots in her field of vision. She felt "like a curtain came down" over her eye. She had a successful cataract extraction in her left eye 4 months ago. Her vital signs are stable. Examination shows a sluggish left pupil. Ophthalmoscopy reveals retinal tears and a grayish-appearing retina. What is the most probable diagnosis?
Choroidal rupture
Central retinal artery occlusion
Central retinal artery occlusion
Exudative macular degeneration
Retinal detachment
A 67 -year-old Caucasian male complains of progressive visual loss in his right eye over the past several months. He has a history of hypertension and type 2 diabetes mellitus. Current medications include a daily baby aspirin, hydrochlorothiazide, lisinopril, and metformin. There is no family history of visual problems. He has a 35 pack year smoking history and admits to occasional alcohol use. He is afebrile with a blood pressure of 137/82 mmHg and pulse of 73/min. Cardiac and pulmonary examinations are unremarkable. A neurologic examination demonstrates no focal motor or sensory abnormalities. The patient is asked to cover his left eye and to look at a small spot on a grid made of parallel vertical and horizontal lines. He describes the vertical lines as being bent and wavy. Which of the following is the most likely cause of this patient's complaints?
Lens opacity
Enlarged blind spot
Increased intraocular pressure
Macular degeneration
Peripheral retinal degeneration
A 35-year-old white female is complaining of blurry vision and pain with eye movements. She is on no medications and denies any trauma. Last year, she developed bladder incontinence and an episode of leg weakness, which both improved without therapy. Physical examination reveals reduced vision and swollen optic discs. The one diagnosis that may explain her symptoms is·
Parkinson disease
Myasthenia gravis
Multiple sclerosis
Subdural hematoma
Transient ischemic attacks
A 65-year-old woman presents with complaints of pain and swelling over the inner aspect of her right eye for the past two days. Examination of the eye reveals tenderness, edema, and redness over the medial canthus. Slight pressure over the area causes expression of purulent material. Visual acuity is normal. What is the most likely diagnosis?
Episcleritis
Dacryocystitis
Hordeolum
Hordeolum
Orbital cellulitis
A 65-year-old man complains of gradual onset blurred vision for the past two months. He also has difficulty driving at night and reading fine print. He has diabetes and hypertension. His medications include ramipril and metoprolol. His vital signs are stable. His best corrected vision is OD (right eye) 20/80, OS (left eye) 20/100, with full fields. Ophthalmoscopic examination with good pupillary dilatation reveals a loss of transparency of lens in both eyes. The red fundal reflex is normal, but retinal details are difficult to visualize. What is the most likely diagnosis?
Open angle glaucoma.
Retinal detachment.
Macular degeneration.
Central retinal vein occlusion.
Cataract.
A 24-year-old woman presents to the emergency department (ED) complaining of right eye pain and blurry vision since waking up this morning. She states that the pain began after taking out contact lenses that were in her eyes for over 1 week. Her blood pressure (BP) is 120/75 mm Hg, heart rate (HR) is 75 beats per minute, temperature is 99.1°F, and respiratory rate (RR) is 16 breaths per minute. Her right and left eye visual acuity is 20/60 and 20/20, respectively. Her conjunctivae are injected. The slitlamp examination reveals a large area of fluorescein uptake over the visual axis. Which of the following is the most appropriate therapy?
Call the ophthalmology consult for an emergent corneal transplant.
Prescribe ciprofloxacin eye drops and have patient strictly wear an eye patch until her pain resolves.
Prescribe ciprofloxacin eye drops, oral analgesia, update tetanus prophylaxis, and arrange for ophthalmology follow-up
Prescribe oral amoxicillin, a topical anesthetic, such as tetracaine, and have patient follow-up with an ophthalmologist.
A 60-year-old woman presents to the ED complaining of pain in her right eye and burning sensation over half of her forehead and scalp. On physical examination, you notice a patch of grouped vesicles on an erythematous base located in a dermatomal distribution on her scalp and forehead. There are also a few vesicles located at the tip of the patient’s nose. Her visual acuity is 20/20 bilaterally, heart is without murmurs, lungs are clear, abdomen is soft, and there are no gross findings on neurologic examination. Which of the following is the most concerning complication of this patient’s clinical presentation?
Central nervous system (CNS) involvement leading to meningitis
Ophthalmic involvement leading to anterior uveitis or corneal scarring
Cardiac involvement leading to endocarditis
Permanent scarring of her face
Nasopalatine involvement leading to epistaxis
31-year-old nurse in your hospital has noticed a lesion in her left eye. She denies change in vision, pain, fevers, or discharge. A picture of her eye is shown below. Which of the following is the most likely diagnosis?
Hordeolum
Chalazion
Dacryocystitis
Pinguecula
Pterygium
A 72-year-old man presents with right eye pain for 1 day. The patient has a history of diabetes, hypertension, and “some type of eye problem.” He does not recall the name of his eye problem or the name of his ophthalmic medication. However, he does remember that the eye drop has a yellow cap. Which class of ophthalmic medication is the patient taking?
Antibiotic
β-Blocker
Mydriatic/cycloplegic agent
Miotic
Anesthetic
A 35-year-old woman presents with a right-sided red eye for 3 days. She denies pain and notes that she has watery discharge from the eye. She has been coughing and congested for the past 5 days. On examination, the patient has a temperature of 98.4°F, HR of 72 beats per minute, BP of 110/70 mm Hg, and RR of 14 breaths per minute. Her visual acuity is 20/20. On inspection, the conjunctiva is erythematous with minimal chemosis and clear discharge. The slit-lamp, fluorescein, and funduscopic examinations are otherwise unremarkable. The patient has a nontender, preauricular lymph node and enlarged tonsils, without exudates. What is the most likely diagnosis?
Gonococcal conjunctivitis
Bacterial conjunctivitis
Viral conjunctivitis
Allergic conjunctivitis
Pseudomonal conjunctivitis
A 24-year-old woman presents to the ED at 4 AM with severe left eye pain that woke her up from sleep. She wears soft contact lenses and does not routinely take them out to sleep. She is in severe pain and wearing sunglasses in the examination room. You give her a drop of proparacaine to treat her pain prior to your examination. On examination, her vision is at baseline and she has no afferent pupillary defect. There is some perilimbic conjunctival erythema. On fluorescein examination, a linear area on the left side of the cornea is highlighted when cobalt blue light is applied. No underlying white infiltrate is visualized. No white cells or flare are visualized in the anterior chamber. What is the most appropriate treatment for this condition?
Immediate ophthalmology consult
Tobramycin ophthalmic ointment
Erythromycin ophthalmic ointment
Eye patch
Proparacaine ophthalmic drops
A 45-year-old woman presents with right eye pain and redness for 1 day. She has photophobia and watery discharge from the eye. She does not wear glasses or contact lenses and has no prior eye problems. On examination, the patient’s visual acuity is 20/20 in the left eye and 20/70 in the right eye. She has conjunctival injection around the cornea and clear watery discharge. On slit-lamp examination, the lids, lashes, and anterior chamber are normal. When fluorescein is applied, a branching, white-colored epithelial defect is seen. The remainder of the head examination is normal and the patient has no cutaneous lesions. Which of the following is the most appropriate treatment for this patient?
Admission for intravenous (IV) antibiotics
Admission for IV antiviral agents
Topical steroids
Topical antiviral medication
Immediate ophthalmology consultation
A 45-year-old woman presents with right eye pain and redness for 1 day. She has photophobia and watery discharge from the eye. She does not wear glasses or contact lenses and has no prior eye problems. On examination, the patient’s visual acuity is 20/20 in the left eye and 20/70 in the right eye. She has conjunctival injection around the cornea and clear watery discharge. On slit-lamp examination, the lids, lashes, and anterior chamber are normal. When fluorescein is applied, a branching, white-colored epithelial defect is seen. The remainder of the head examination is normal and the patient has no cutaneous lesions. Which of the following is the most appropriate treatment for this patient?
Admission for intravenous (IV) antibiotics
Admission for IV antiviral agents
Topical steroids
Immediate ophthalmology consultation
Topical antiviral medication

A 21-year-old man presents to the ED with a red eye. The patient complains of rhinorrhea and a nonproductive cough but has no eye pain or discharge. He also has no associated ecchymosis, bony tenderness of the orbit, or pain on extraocular eye movement. His vision is normal, extraocular movements are intact, and intraocular pressure (IOP) is 12. A picture of his eye is shown below. What is the most appropriate management of this condition?
Call ophthalmology immediately.
Call ophthalmology immediately.
Elevate patient’s head.
Administer ophthalmic timolol.
Reassurance only
A 28-year-old mechanic with no past medical history presents to the ED after a small amount of battery acid was splashed in his right eye. He is complaining of extreme pain and tearing from his eye. Which of the following is the most appropriate next step in management?
Call ophthalmology now
Irrigate with normal saline.
Check visual acuity.
Apply erythromycin ointment.
Check the pH of the tears.
A 45-year-old man lacerated his right forehead after an altercation in a local bar. Instead of seeking medical attention, the patient applied super glue to his wound. He successfully stopped the bleeding, but some of the glue got into his right eye and now he comes to the ED with difficulty opening his right eye. What is the most appropriate treatment of this patient?
Call ophthalmology immediately.
Wash eye with acetone
Wash eye with normal saline.
Use forceps to remove all the glue from the eye.
Apply erythromycin ointment.
The local sorority house recently installed a sun-tanning station. Two days later three sorority girls present to the ED with bilateral eye pain, tearing, and photophobia. After ophthalmic anesthesia instillation, a complete eye examination is performed. Visual acuity is normal. Extraocular eye movements are intact and pupils are equal, round, and reactive to light. IOP is normal. Slit-lamp examination is normal, but fluorescein examination under cobalt blue light illuminates small dots throughout the cornea. What is the most likely diagnosis?
Ultraviolet keratitis
Anterior uveitis
Herpes simplex keratitis
Allergic conjunctivitis
Corneal ulcer
A 12-year-old girl presents to the ED for left eye pain and swelling for 2 days. The patient has had cough, congestion, and rhinorrhea for the last week that is improving. On examination, her temperature is 100.8°F, HR 115 beats per minute, RR 12 breaths per minute, and BP 110/70 mm Hg. On eye examination, there is purple-red swelling of both upper and lower eyelids with injection of the conjunctiva. Pupils are equal and reactive to light. There is restricted lateral gaze. Visual acuity is 20/70 in the left eye and 20/25 in the right eye. The rest of the physical examination is normal. What is the most appropriate next step in management?
Administer diphenhydramine.
Administer amoxicillin/clavulanate.
Administer vancomycin IV.
Perform computed tomographic (CT) scan of orbits and sinuses.
Administer artificial tears.
A 60-year-old man with a history of hypertension and migraine headaches presents to the ED with a headache. He describes left-sided headache and eye pain that is associated with nausea and vomiting. The patient has a long history of migraines, but says his migraines do not usually include eye pain. On examination, his temperature is 97.6°F, HR 84 beats per minute, RR 12 breaths per minute, and BP 134/80 mm Hg. His neurologic examination is normal. His left eye is mid-dilated and nonreactive. His cornea is cloudy. His corrected visual acuity is 20/50 in the left eye and 20/20 in the right eye. What is the most appropriate next step in management?
Administer hydromorphone.
Perform head CT scan.
Check IOP.
Check erythrocyte sedimentation rate (ESR).
Discharge patient.
A 22-year-old man presents to the ED for left eye pain. He was in an altercation yesterday and was punched in the left eye. On examination, his left eye is ecchymotic and the eyelids are swollen shut. He has tenderness over the infraorbital rim but no step-offs. You use an eyelid speculum to examine his eye. His pupils are equal and reactive to light. His visual acuity is normal. On testing extraocular movements, you find he is unable to look upward with his left eye. He also complains of diplopia when looking upward. Funduscopic examination is normal. What is the most likely diagnosis?
Orbital blowout fracture
Ruptured globe
Retinal detachment
Cranial nerve III palsy
Traumatic retrobulbar hematoma
You are examining the pupils of a patient. On inspection, the pupils are 3 mm and equal bilaterally. You shine a flashlight into the right pupil and both pupils constrict to 1 mm. You then shine the flashlight into the left pupil and both pupils slightly dilate. What is this condition called?
Anisocoria
Argyll Robertson pupil
Afferent pupillary defect
Horner syndrome
Normal pupil reaction
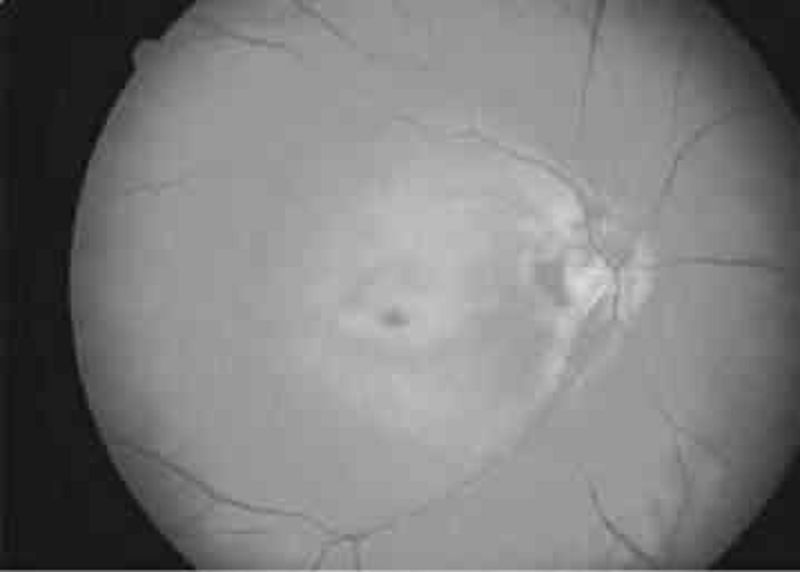
A 65-year-old man with a history of diabetes, hypertension, coronary artery disease, and atrial fibrillation presents with loss of vision in his left eye since he awoke 6 hours ago. The patient denies fever, eye pain, or eye discharge. On physical examination of the left eye, vision is limited to counting fingers. His pupil is 3 mm and reactive. Extraocular movements are intact. Slit-lamp examination is also normal. The dilated funduscopic examination is shown below. Which of the following is the most likely diagnosis?
Retinal detachment
Central retinal artery occlusion
Central retinal vein occlusion
Vitreous hemorrhage
Acute angle-closure glaucoma
{"name":"USMLE PART3.1 (OPTHALMO)", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 1-year-old boy is brought to the clinic by his 28-year-old Caucasian mother for the evaluation of his eyes. For the past several months, he has been bumping into objects. His perinatal history is unremarkable. Physical examination of the eyes reveals a bilateral white reflex. The retina cannot be visualized properly. Fundal reflection is absent, and the pupil is white. What is the most likely diagnosis?, A 53-year-old man comes to the office because of difficulty reading fine print over the last year. He now has to hold books, menus, and magazines at an arm’s length in order to read them. He has never had visual problems before. Which of the following is most likely abnormal in this patient?, A 65-year-old white man is complaining of a sudden loss of vision in his left eye which resolved after 15 minutes. \"It seemed like a curtain was falling down in my eye!\" said the patient. He recalls having a similar episode 3 months ago. His past medical history is significant for hypertension, for which he takes lisinopril (20mg) and hydrochlorothiazide (25mg) daily. His pulse is 82\/min, blood pressure is 140\/90 mm Hg, respirations are 14\/min, and temperature is normal. Fundoscopy reveals zones of whitened, edematous retina following the distribution of the retinal arterioles. What is the most likely diagnosis?","img":"https://cdn.poll-maker.com/10-459647/10.bmp?sz=1200"}
More Quizzes
The Marriage Fitness Test
22110
Gerontology
371831
Makroekonomika
1050
Random Trivia
5263
London Questions - Free Online Trivia Test Now
201016937
Black Military History - Valor Before Freedom
201016641
Guess the 80s Song - How Many Can You Name?
201017509
Genesis 1 - 50 Bible with Answers - Free Online
201019256
Spanish Expressions for Beginners - Free Practice
201022559
Neuro Linguistic Programming Test - Free Online
201016305
Am I Being Played - Free Self-Assessment
201018363
Basic English Grammar - Free Practice Online
201018517