USMLE Pédiatrie (501-810) GD
501. A mentally retarded 14-year-old boy has a long face, large ears, micropenis, and large testes. Chromosome analysis is likely to demonstrate which of the following?
Trisomy 21
Trisomy 18
Trisomy 13
Fragile X syndrome
Williams syndrome
502. A 5-month-old child with poor growth presents to the ER with generalized tonicclonic seizure activity of about 30-minute duration that stops upon the administration of lorazepam. Which of the following historical bits of information gathered from the mother is most likely to lead to the correct diagnosis in this patient?
The child has had congestion without fever for the past 3 days
The child is developmentally normal, as are his siblings
The mother has been diluting the infant’s formula to make it last longer
The mother reports there are two dogs and one cat at home.
The mother previously worked as an attorney in an energy-trading firm
503. A 13-year-old girl presents with parental concerns of poor posture. She has not had any back pain. On examination, she has unequal shoulder height, asymmetric flank creases, and a forward-bending test that shows rib asymmetry. The physical examination is otherwise normal. Which of the following is the most likely cause of her condition?
Congenital scoliosis
Leg length inequality
Idiopathic scoliosis
Postural roundback
Scheuermann kyphosis
504. After 10 days of nasal congestion and rhinorrhea, a 3-month-old infant develops a severe hacking cough during which he repeatedly turns dusky and appears to choke on or to vomit profuse thick, clear nasopharyngeal mucus. For 7 days, the coughing continues unabated. On physical examination, he is afebrile and his lungs are clear. His chest x-ray is normal. His WBC count is 24,000/mm3, with 15% polymorphonuclear cells, 82% lymphocytes, and 3% monocytes. Which of the following antibiotics should be used to treat this patient?
Amoxicillin
Amoxicillin-clavulanic acid
Erythromycin
Tetracycline
No antibiotics are necessary
505. An 18-month-old boy presents with a history of fever to 39.0°C for 5 days. He has also been irritable and has not been drinking well. Associated symptoms include red eyes, a rash, and some trouble walking. On physical examination, he has a temperature of 39.5°C. He has bilateral bulbar conjunctivitis, a strawberry tongue, an inflamed oral pharynx, edema of the hands and feet, a morbilliform rash, and cervical lymphadenopathy. He is very irritable. His CBC shows a WBC of 15,000/mm3 with 60% neutrophils, 35% lymphocytes, and 5% monocytes. His hemoglobin is 12.0 g/dL and platelet count is 500,000/ mm3. Which of the following is the most likely diagnosis?
Erythema infectiosum (fifth disease)
Kawasaki disease
Rubella
Rubeola (measles)
Rheumatic fever
506. A 6 month old male is brought in to the Emergency Room by his mother who states that when she picked him up from the baby-sitter he was not acting right. The baby-sitter stated that he was sleeping more and was fussy. On examination the baby is stuporous. His temperature is 37.8 C (99.9 F), pulse is 140/min, and respirations are 36/min. A 4 cm ecchymosis is noted on his right cheek. The remainder of the physical examination is unremarkable. The physician suspects possible physical abuse. He orders a CT scan of the head, skeletal survey, chemistry panel and complete blood count. Which of the following diagnostic tests should also be ordered?
Ammonia level
Coagulation studies
Lipid panel
Thyroid studies
Urine electrolytes
507. An infant is delivered at full term by a spontaneous vaginal delivery to a 29-year-old primigravida. At delivery, the infant is noted to have subcostal retractions and cyanosis despite good respiratory effort. The abdomen is scaphoid. On bag and mask ventilation, auscultation of the lungs reveals decreased breath sounds on the left, with heart sounds louder on the right. Which of the following is the most likely diagnosis?
Dextrocardia with situs inversus
Diaphragmatic hernia
Pneumonia
Pulmonary hypoplasia
Spontaneous pneumothorax
508. A 12-year-old girl comes to the physician for an annual examination. She has been in good health for the past year and has no complaints. She began having menses this year and, after a few irregular cycles, is now having a monthly period. Past medical history is significant for multiple episodes of otitis media as a child. Past surgical history is unremarkable. She takes no medications and has no known drug allergies. Physical examination is unremarkable. If not currently immune, which of the following immunizations should this patient most likely receive?
Hepatitis B virus immunization
HIV immunization
Japanese encephalitis virus immunization
Rabies virus immunization
Salmonella typhi immunization
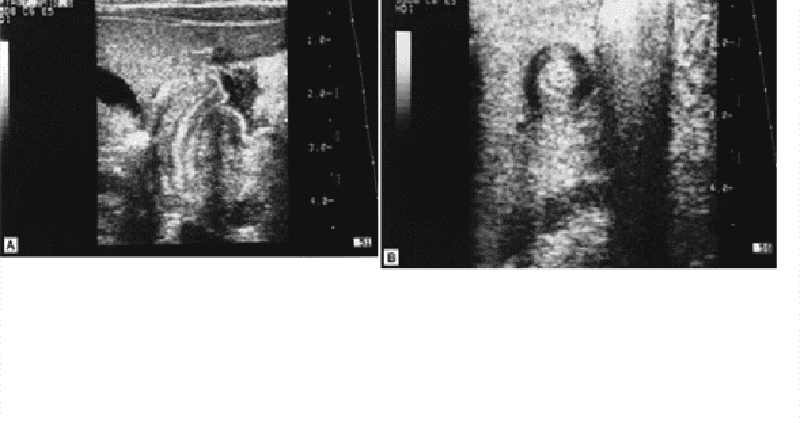
509. A 4-week-old boy presents with a 10-day history of vomiting that has increased in frequency and forcefulness. The vomitus is not bile stained. The child feeds avidly and looks well, but he has been losing weight. An ultrasound of the abdomen is shown. Which of the following is the most likely diagnosis?
Surgical consultation for pyloromyotomy
Upper GI with small-bowel follow through
Intravenous (IV) fluids alone to maintain hydration
Air contrast enema
Computed tomography (CT) of the brain
510. A 12-month-old girl has been spitting up her meals since 1 month of age. Her growth is at the 95th percentile, and she is otherwise asymptomatic and without findings on physical examination. Which of the following is the most likely diagnosis?
Pyloric stenosis
Partial duodenal atresia
Hypothyroidism
Gastroesophageal reflux
Tracheoesophageal fistula
511. A 14-year-old girl has a 9-month history of diarrhea, abdominal pain (usually periumbilical and postprandial), fever, and weight loss. She has had several episodes of blood in her stools. Which of the following is the most likely diagnosis?
Chronic appendicitis
Chronic pancreatitis
Crohn disease
Bulimia
Gallstones
512. A 12-year-old girl complains of intermittent palpitations. She had previously been in excellent health and has met all development milestones. There is no family history of heart disease. She is on no medications and takes no drugs. She states that the palpitations begin and end suddenly and usually last a couple of hours. She is otherwise asymptomatic between episodes. The physical examination is normal. An ECG reveals a shortened PR interval and a slow upstroke of the QRS wave in lead III. Which of the following is the most likely diagnosis?
Anxiety attack
Lown-Ganong-Levine syndrome
Nodal reentrant tachycardia
Sinus tachycardia
Wolff-Parkinson-White syndrome
513. An 11-year-old boy is brought to the office by his mother because "he is sick." He has had headaches for the past several weeks, and has vomited 4 times in the past 5 days. He drinks large amounts of water and goes to the bathroom all the time. He is no longer interested in playing football and going out with his friends. His temperature is 37.0C (98.6F), blood pressure is 11 8/78 mm Hg, pulse rate is 84/min, and respirations are 16/min. On examination, there is loss of peripheral visual fields. His laboratory findings are as follows: W BC 7,800/mm3 Hemoglobin 12.6 g/dl Hematocrit 35% Platelets 199,000/mm3 Sodium 145 mEq/L Potassium 3.6 mEq/L Bicarbonate 24 mEq/L Blood urea nitrogen 18 mg/dl Serum creatinine 1.0 mg/dl Blood glucose 88 mg/dl X-rays of the head reveal a calcified lesion above the sella. What is the most likely diagnosis?
Pituitary adenoma
Meningioma
Empty sella syndrome
Craniopharyngioma
Ependymoma
514. A 4-week-old male infant is brought to the office due to several episodes of projectile vomiting for the last few days. The vomitus contains milk and doesn't contain bile or blood. The child's appetite has increased for the last few days. He has been fed with goat's milk since birth, but doesn't seem to tolerate it anymore for the last few days. He vomits a few minutes after feedings. He appears dehydrated, and abdominal examination reveals no mass. Blood tests reveal macrocytosis. What is the most appropriate next step in the management of this patient?
Barium swallowing
Ultrasound of the abdomen
Substitute goat's milk with another form of milk
Divide his feedings
Add folic acid to relieve his vomiting
515. A 6-year-old Hispanic boy is brought to your office by his mother because of severe pain in his right hip and refusal to walk for the last 2 days. His blood pressure is 100/70 mm Hg, pulse is 90/min, respirations are 18/min, and temperature is 38.7C (102.7F). His WBC count is 19,000/mm3 and ESR is 55 mm at one hour. On examination, he keeps his right hip externally rotated, and cries out in pain on any movement involving the right hip. Joint aspiration reveals a turbid fluid with total WBC: 90,000/mm3 and numerous bacteria. What is the most appropriate management in this patient?
Salicylates, rest and physical therapy.
Intravenous antibiotics.
Oral antibiotics.
Emergency surgical drainage
E. Splint the hip joint and administer intravenous antibiotics
516. A 6-week-old child arrives with a complaint of “breathing fast” and a cough. On examination you note the child to have no temperature elevation, a respiratory rate of 65 breaths per minute, and her oxygen saturation to be 94%. Physical examination also is significant for rales and rhonchi. The past medical history for the child is positive for an eye discharge at 3 weeks of age, which was treated with a topical antibiotic drug. Which of the following organisms is the most likely cause of this child’s condition?
Neisseria gonorrhoeae
Staphylococcus aureus
Group B streptococcus
Chlamydia trachomatis
Herpesvirus
517. A full-term neonate presents with hypotonia, lethargy and poor feeding over the past three hours. The pregnancy was uneventful, but during delivery, the neonate presented with shoulder dystocia and subsequently obtained a fracture of the clavicle. His Apgar scores are 7 and 8 at one and five minutes, respectively. His birth weight is 4000g. His vital signs are normal. Physical examination reveals an enlarged tongue, mild microcephaly, prominent occiput, prominent eyes and omphalocele. Abdominal palpation reveals an enlarged liver and kidneys. The initial work-up reveals hypoglycemia and hyperinsulinemia. What is the most likely diagnosis?
Congenital hypothyroidism
Maternal diabetes
Beckwith-Wiedemann syndrome
WAGR syndrome
Denys-Drash syndrome
518. A 4-year-old child is brought to the emergency department after he ingested liquid oven cleaner. His vital signs are stable. He is crying and drooling with blood-tinged secretions. His lips and chin are swollen and erythematous. His clothes are contaminated with the material. His breathing appears normal. His lungs are clear. Based on these findings, what is the best next step in the management of this patient?
Upper gastrointestinal endoscopy
Barium swallow
High dose corticosteroids
Antibiotics
Nasogastric lavage
519. A male infant is born to a primigravid woman whose pregnancy was uneventful. The delivery was uncomplicated. Physical examination of the newborn reveals deformity of the feet, specifically adduction of the anterior aspect of the foot with a convex lateral border and concave medial border. The ankle movements are normal, and passive and active movement of the foot overcorrects the deformity into abduction. AP radiographs reveal mild adduction of the metatarsals at the tarsometatarsal articulation, and an increased angle between the 1st and 2nd metatarsals. What is the best next step in the management of this patient?
Reassurance
Immediate casting
Surgical correction at age two
Surgical correction within the first month of life
Orthosis
520. You are called to a delivery of a term infant, about to be born via cesarean section to a mother with multiple medical problems, including a 1-month history of a seizure disorder, for which she takes phenytoin; rheumatic heart disease, for which she must take penicillin daily for life; hypertension, for which she takes propranolol; acid reflux, for which she takes aluminum hydroxide; and a deep venous thrombosis in her left calf diagnosed 2 days ago, for which she was started on a heparin infusion. The obstetrician is concerned about the possible effects of the mother’s multiple medications on the newborn infant. Which of the following medications is most likely to cause harm in this newborn infant at delivery?
Propranolol
Penicillin
Aluminum hydroxide
Phenytoin
Heparin
521. Your older sister, her husband, their 2-day-old infant, and their pet Chihuahua arrive at your door. The parents of the child are concerned because the pediatrician noted the child was “yellow” and ordered some studies. They produce a wad of papers for you to review. Both the mother and baby have O-positive blood. The baby’s direct serum bilirubin is 0.2 mg/dL, with a total serum bilirubin of 11.8 mg/dL. Urine bilirubin is positive. The infant’s white blood cell count is 13,000/μL with a differential of 50% polymorphonuclear cells, 45% lymphocytes, and 5% monocytes. The hemoglobin is 17 g/dL, and the platelet count is 278,000/μL. Reticulocyte count is 1.5%. The peripheral smear does not show fragments or abnormal cell shapes. Which of the following is the most likely explanation for this infant’s skin color?
Rh or ABO hemolytic disease
Physiologic jaundice
Sepsis
Congenital spherocytic anemia
Biliary atresia
522. A 14-day-old male infant is brought to the emergency department due to spasms involving the whole body. He has been having very poor suckling over the last couple of days. He was delivered vaginally by an untrained birth attendant, and his mother never sought any pre- or antenatal care. The pertinent physical finding is a swollen and erythematous umbilical cord. What is the most likely diagnosis of this patient?
Congenital syphilis
Group B streptococcal infection
Congenital rubella
Toxoplasmosis
Tetanus
523. A 4-year-old boy falls from the jungle gym at preschool. He sustains minor abrasions and contusions, and is taken care of by the school nurse. His parents take him that same afternoon to his regular pediatrician and demand "a thorough check-up" for possible internal injuries. The pediatrician complies, and a complete physical examination is normal. His hemoglobin is 14 g/dL, and a urinalysis shows the presence of microhematuria. Which of the following is the most appropriate next step in management?
CT scan of the abdomen and pelvis
Reassure the parents that microhematuria from minor trauma will resolve spontaneously
Serial hemoglobin and hematocrit determinations
Urologic workup, starting with a sonogram
Retrograde ureterogram and cystogram
524. A 9-year-old boy is brought to the pediatric clinic by his mother, who noticed that the left side of his mouth has started to droop over the past several days. In addition, he is unable to close his left eye completely and complains of it burning. Review of systems reveals a cold approximately two weeks ago and recent decreased taste sensation. Physical examination reveals a well nourished male with normal vital signs. There is left eye ptosis and mild erythema of the left conjunctiva. His smile is asymmetrical on the left. Laboratory evaluation, including a complete blood count and chemistry profile, are normal. Which of the following infections is most closely associated with this patient's condition?
Epstein-Barr Virus
Group A Streptococcus
Human Immunodeficiency Virus
Influenza
Measles

525. A 5-year-old girl is brought to the physician with low grade fever and rhinorrhea. Her symptoms began ten days ago. She has also had persistent purulent rhinorrhea, nasal congestion, and a dry cough during the day that worsens at night. Her symptoms do not seem to be improving. On examination, the child has erythema and swelling of the nasal turbinates with purulent nasal drainage. She has evidence of drainage in the posterior pharynx as well. The remainder of her examination is unremarkable. Computed topography of her face is shown below. Which of the following is the most common predisposing factor for her condition?
Allergic rhinitis
Septal deformities
Adenoidal hypertrophy
Environmental mucosal irritants
Viral upper respiratory infection
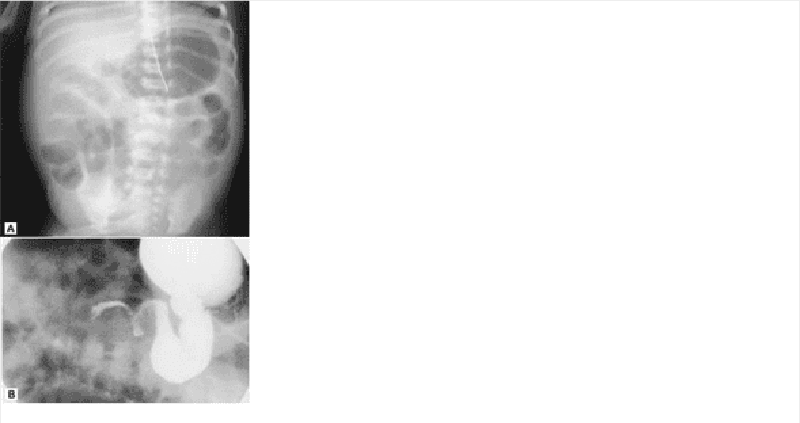
526. A 1-week-old previously healthy infant presents to the emergency room with the acute onset of bilious vomiting. The abdominal plain film in the emergency department (A) and the barium enema done after admission (B) are shown. Which of the following is the most likely diagnosis for this patient?
Jejunal atresia
Hypertrophic pyloric stenosis
Malrotation with volvulus
Acute appendicitis
Intussusception
527. A 3-year-old child presents to your office for an evaluation of constipation. The mother notes that since birth, and despite frequent use of stool softeners, the child has only about one stool per week. He does not have fecal soiling or diarrhea. He was born at term and without pregnancy complications. The child stayed an extra day in the hospital at birth because he did not pass stool for 48 hours, but has not been in the hospital since. Initial evaluation of this child should include which of the following?
A child psychiatry evaluation for stool retention and parenting assistance
A barium enema and rectal manometry
Plain films of the abdomen
Dietary log and observation
Beginning oral antispasmodic medication
528. A 3-month-old boy is brought to the pediatrician because of a red growth on his arm. The pregnancy had been uncomplicated, and the infant has been meeting all development milestones. He has been healthy so far and has received all scheduled immunizations. He is currently being breast-fed. His skin was clear at birth, but when he was 2 months old, his mother noted a light red growth on his arm. Within the past month, it has increased in size and has turned bright red. Which of the following is the most appropriate treatment for this disorder?
Observation
Topical corticosteroids
Argon laser therapy
Radiation therapy
Surgery
529. A 2-year-old boy is hospitalized for severe pneumonia requiring endotracheal intubation and mechanical ventilation. His hemoglobin level is 13.2 mg/dl and his WBC count is 3,200/mm3. The absolute level of CD3- positive lymphocytes is normal but the level of CD 19-positive lymphocytes is very low. This patient would benefit most from which of the following as a maintenance therapy?
Antiretroviral therapy
Intravenous infusion of immune globulin
Administration of live attenuated vaccines
White blood cell transfusion
Enzyme replacement therapy
530. A 14-year-old African-American boy presents to your office with difficulty walking for the past several weeks. He complains of pain in the right hip. He describes two episodes of severe hip pain and one previous episode of abdominal pain requiring hospitalization. Physical examination reveals motion restriction in the right hip joint. His joint is not erythematous or tender to palpation. His hematocrit is 22%. This patient's difficulty walking is most likely secondary to which of the following:
Osteoarthritis
Septic arthritis
Gouty arthritis
Osteonecrosis
Osteoporosis
531. A 2-week-old boy in the neonatal intensive care unit had a birth weight of 1200 g. Ultrasound of the head reveals grade II intraventricular hemorrhage and periventricular leukomalacia. An ophthalmologic examination reveals retinopathy of prematurity of both eyes. In addition, a hearing screen demonstrates bilateral hearing deficits. Which of the following is the most important determinant of this child's neurodevelopmental outcome?
Length of gestation
Maternal education
Outcome of the mother's previous pregnancies
Quality of prenatal care
Socioeconomic status of the family
532. A 2-year-old girl is brought to her pediatrician by her parents because of increasing lethargy and irritability. She has just started walking, and is teething and likes to chew on the woodwork around the windows. Physicalexamination reveals a tender abdomen. Laboratory studies indicate high iron and ferritin levels. The peripheral blood smear shows basophilic stippling. Which of the following is the most likely diagnosis?
Cobalamin deficiency
Diphyllobothriasis
Iron deficiency
Lead poisoning
Porphyria
533. A 15-month-old boy is brought to the ER because of fever and a rash. Six hours earlier he was fine, except for tugging on his ears; another physician diagnosed otitis media and prescribed amoxicillin. During the interim period, the child has developed an erythematous rash on his face, trunk, and extremities. Some of the lesions, which are of variable size, do not blanch on pressure. The child is now very irritable, and he does not interact well with the examiner. Temperature is 39.5C (103.1F). He continues to have injected, immobile tympanic membranes, but you are concerned about his change in mental status. Which of the following is the most appropriate next step in the management of this infant?
Begin administration of IV ampicillin
Begin diphenhydramine
Discontinue administration of ampicillin and begin trimethoprim with sulfamethoxazole
Perform bilateral myringotomies
Perform a lumbar puncture
534. The 3-year-old sister of a newborn baby develops a cough diagnosed as pertussis by nasopharyngeal culture. The mother gives a history of having been immunized as a child. Which of the following is a correct statement regarding this clinical situation?
The mother has no risk of acquiring the disease because she was immunized
Hyperimmune globulin is effective in protecting the infant.
The risk to the infant depends on the immune status of the mother.
Erythromycin should be administered to the infant
The 3-year-old sister should be immediately immunized with an additional dose of pertussis vaccine
535. A 10-hour-old newborn is noted to have a swelling in the scalp which was not present at birth. The swelling is limited to the surface of one cranial bone. There are no visible pulsations, indentations of the skull, or discoloration of the overlying scalp. What is the most likely diagnosis?
Cephalohematoma
Caput succedaneum
Cranial meningocele
Intracranial hemorrhage
Depressed skull fracture
536. A 3-year-old boy is brought by his father to the Emergency Department with fever, headache and neck pain that developed over the past several hours. The father states he is not the birth father, and that he and his wife adopted the boy at 18 months of age after his birth mother abandoned him. Physical examination reveals a lethargic male with a temperature of 39.7 C (103.5 F). There is photophobia, and mildly injected conjunctiva are appreciated. Pupils are equal and reactive and funduscopic examination is unremarkable. The patient has neck stiffness with a positive Kernig's sign. A complete blood count reveals a leukocyte count of 24,000/mm3 with 64 segmented neutrophils and 25 bands. A lumbar puncture is performed that reveals elevated CSF pressure, decreased glucose, and elevated protein. A Gram's stain shows gram-negative pleomorphic rods. There is no growth on blood agar. Growth on chocolate agar reveals white colonies. Which of the following is the most likely pathogen?
Haemophilus ducreyi
Haemophilus influenzae type b
Neisseria meningitidis
Listeria monocytogenes
Streptococcus pneumoniae
537. A 16-month-old girl is brought to medical attention because of irritability, poor feeding, and temperatures up to 39.4 C (103 F). Careful history and physical examination fail to disclose any identifiable cause of her fever. There is some degree of abdominal tenderness on palpation. Which of the following is the most appropriate next step in diagnosis?
Microscopic examination and culture of stool
Renal ultrasound
Chest x-ray films
Voiding cystourethrogram
Culture of urine obtained by transurethral catheterization
538. A premature neonate with respiratory distress syndrome is maintained on mechanical ventilation in a neonatal intensive care unit. Two weeks after delivery, the nurses in the intensive care unit notice that higher ventilation settings are needed and that more secretions are being suctioned from the endotracheal tube. A chest x-ray film shows questionable new infiltrates. Which of the following is the most likely pathogen?
Coagulase-negative oxacillin-resistant Staphylococcus
Coagulase-negative oxacjllin-sensitive Staphylococcus
Group B Streptococcus
Methkillin-resistant Staphylococcus aureus
Methicillin-sensitive Staphylococcus aureus
539. A 2-year-old boy is brought to the emergency department (ED) in acute respiratory distress. He is afebrile, and has a heart rate of 100/min, respiratory rate of 80/min, and Sa02 of 84% on room air. He is sitting upright, and has significant nasal flaring and intercostal retractions. He is given supplemental oxygen in the ED. Chest x-ray reveal hyperinflation of the right lung, mediastinal shift to the left, and a severely hypoinflated left lung Which of the following is the most appropriate next step in management?
Bronchodilator therapy
Direct laryngoscopy and rigid bronchoscopy
Direct laryngoscopy and flexible bronchoscopy
Segmental lung resection
CT scan of the chest
540. A 2-year-old presents to the emergency center with several days of rectal bleeding. The mother first noticed reddish-colored stools 2 days prior to arrival and has since changed several diapers with just blood. The child is afebrile, alert, and playful, and is eating well without emesis. He is slightly tachycardic, and his abdominal examination is normal. Which of the following is the best diagnostic study to order to confirm the diagnosis?
Exploratory laparotomy
Barium enema
Ultrasound of the abdomen
Radionucleotide scan
Stool culture
541. A 4-year-old boy is brought to the office because his school teacher thinks that his dusky blue appearance may have something to do with his inability to participate in regular school activities. His mother says that he has always appeared slightly out of breath. He has no history of any trauma, past surgery or medical conditions. His birth history is unremarkable. Physical examination reveals perioral cyanosis and a systolic murmur along the left sternal border. When the child squats, the murmur disappears and the cyanosis slightly improves. What is the most likely diagnosis of this patient?
Ventricular septal defect
Atrial septal defect
Coarctation of aorta
Tetralogy of Fallot
Eisenmenger syndrome
The 1-year-old brother of a child with known abetalipoproteinemia is evaluated by a pediatrician for the disease. The 1 -year-old has been exhibiting steatorrhea and ataxia. Which of the following would most strongly support the suspected diagnosis?
Acanthocytes on peripheral smear
"Crumpled silk" histiocytes on bone marrow biopsy
Globoid cells on brain biopsy
Metachromatic deposits on sural nerve biopsy
"Sea-blue" histiocytes on bone marrow biopsy
543. A 2-month-old infant is evaluated by a pediatric cardiologist. The infant was noted at birth to have an upper left sternal border ejection murmur. The infant at that time was not cyanotic, but slowly developed cyanosis over the next two months. At the time of the pediatric cardiologist's examination, an ECG showed right axis deviation and right ventricular hypertrophy. A chest x-ray film showed a small heart with a concave main pulmonary artery segment and diminished pulmonary blood flow. Which of the following is the most likely diagnosis?
Complete atrioventricular canal defect
Hypoplastic left ventricle
Isolated atrial septal defect
Tetralogy of Fallot
Transposition of the great arteries
544. A 6-year-old boy is brought to the emergency department because of the acute onset of headache, nausea, and vomiting. On arrival, physical examination reveals marked nuchal rigidity and funduscopic evidence of papilledema. A head CT scan reveals a solid tumor in the posterior fossa, centered in the cerebellar vermis and extending to the fourth ventricle. An emergency craniotomy is performed, during which a small sample of the tumor is sent to the pathologist for a frozen section consultation. Which of the following is the most likely diagnosis?
Ependymoma
Glioblastoma multiforme (GBM)
Hemangioblastoma
Medulloblastoma
Oligodendroglioma
545. A 15-month-old girl is brought to the office by her mother due to failure to thrive. For the past three months, the child has had foul-smelling, non-bloody, loose stools 7 to 8 times daily. On examination, she is irritable and has a protruding belly and trace pre-tibial edema. There are erythematous vesicles symmetrically distributed over the extensor surfaces of her elbows and knees. Preliminary laboratory investigations are significant for hypochromic microcytic anemia, and stool examination is negative for ova or parasites. What is the most likely cause of failure to thrive in this child?
Lactose intolerance
Laxative abuse
Giardiasis
Celiac disease
Shigella gastroenteritis

546. The 4-year-old child pictured below is noted to have the tooth decay as shown. This characteristic pattern of tooth decay is caused by which of the following?
Excessive use of fluoride
Tetracycline
Use of bottled water that lacks fluoride
Prolonged use of a baby bottle
Consumption of too much candy
547. A 5-month-old infant is brought to the office for the evaluation of persistent vomiting, failure to thrive, and developmental delay. His antenatal and postnatal histories are not known to his Caucasian foster parents, who adopted him when he was 4 months old. The physical examination reveals an infant with blonde hair, fair skin and blue eyes. His urine has a peculiar musty odor. His plasma phenylalanine level is 40 mg/dl and tyrosine level is normal. His urinary phenylpyruvic and a-hydroxy phenylacetic acid levels are both increased. What is the most likely etiology of this child's symptoms?
Classic phenylketonuria
Benign hyperphenylalaninemia
Transient hyperphenylalaninemia
Tyrosinemia
Alcaptonuria
548. A 2 1/2-year-old child is evaluated by a neurologist because of difficulty walking. Neurological examination documents ataxia and mental retardation. The neurologist notes the presence of multiple telangiectasias involving the conjunctiva, ears, and antecubital fossae. The child also has a history of multiple respiratory tract infections. Immunoglobulin studies on the child would most likely demonstrate an absence of which of the following?
IgA and IgE
IgA and IgG
IgE and IgG
IgE and IgM
IgM and IgG
549. A 15-year-old boy with Duchenne muscular dystrophy is brought to the emergency department with increasing respiratory distress and cyanosis. On examination, he is diaphoretic, with gasping respirations, poor air entry, and diminished responsiveness. He is tachycardic at 160 beats/min. His chest x-ray film shows a lingular pneumonia, and he is intubated. He improves over the next 10 days with antibiotics but is not extubated secondary to hypoventilation on weaning because of muscle weakness. Which of the following modalities will most likely help wean him off the ventilator?
Nasopharyngeal tube
Pressure controlled ventilation
Pressure supported ventilation
Supplemental oxygen
Tracheostomy
550. A 2-year-old child presents to the office with a paternal complaint of “bowlegs.” The girl has always had bowlegs; her previous pediatrician told the family she would grow out of it. Now, however, it seems to be worsening. Her weight is greater than 95% for age, and she has significant bowing out of her legs and internal tibial torsion; otherwise, her examination is normal. A radiograph of her lower leg is shown. Which of the following is the most likely diagnosis?
Osgood-Schlatter disease
Physiologic genu varum
Slipped capital femoral epiphysis
Legg-Calvé-Perthes disease
Blount disease
551. A 14-year-old high school student arrives to your clinic for well-child care. In reviewing his records you determine that his most recent immunization for tetanus was at 4 years of age. Which of the following should you recommend?
Tetanus toxoid
Adult tetanus and diphtheria toxoid (Td)
Diphtheria toxoid, whole cell pertussis, and tetanus toxoid (DPT) booster
Tetanus toxoid and tetanus immune globulin
Tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine adsorbed (Tdap) @
552. A 20-month-old male is brought to ER with high fever, confusion and a skin rash suggestive of measles. He has a history of recurrent respiratory infections over the last 6 months. The patient's family has recently emigrated from a rural Russian province. Which of the following forms of vitamin supplementation should be considered in this patient?
Vitamin A
Vitamin K
Vitamin D
Vitamin E
Vitamin B 12
553. A 3-year-old male is brought to the emergency department for evaluation of right neck swelling. His parents noticed a lump on his right neck yesterday, which has since increased in size and is now erythematous and tender. He has been previously healthy except for mild upper respiratory tract symptoms last week. His temperature is 38.0 0C (100.4 0F), pulse is 90/min, and respiratory rate is 25/min. On examination, he is nontoxic appearing. A 5-cm anterior cervical lymph node is palpated on the right side. It is poorly mobile, warm, erythematous, and tender to palpation. There is no fluctuance or induration. What is the most likely organism causing these symptoms?
Staphylococcus aureus
Francisella tularensis
Peptostreptococcus
Nontuberculous mycobacteria
Epstein-Barr virus
554. A 5-year-old boy is brought into the ER immediately after an unfortunate altercation with a neighbor’s immunized Chihuahua that occurred while the child was attempting to dress the dog as a superhero. The fully immunized child has a small, irregular, superficial laceration on his right forearm that has stopped bleeding. His neuromuscular examination is completely normal, and his perfusion is intact. Management should include which of the following?
Irrigation and antimicrobial prophylaxis
Tetanus booster immunization and tetanus toxoid in the wound
Copious irrigation
Primary rabies vaccination for the child
Destruction of the dog and examination of brain tissue for rabies
555. Aunt Mary is helping her family move to a new apartment. During the confusion, 3year-old Jimmy is noted to become lethargic. The contents of Aunt Mary’s purse are strewn about on the floor. In the ER, the lethargic Jimmy is found to have miosis, bradycardia, and hypotension. He develops apnea, respiratory depression, and has to be intubated. His condition would most likely benefit from which of the following therapies?
Deferoxamine
Pediatric intensive care unit (PICU) support and trial of naloxone
N-acetylcysteine (Mucomyst)
Atropine
Dimercaptosuccinic acid (DMSA, succimer)
556. As a city public health officer, you have been charged with the task of screening high-risk children for lead poisoning. Which of the following is the best screen for this purpose?
Careful physical examination of each infant and child
Erythrocyte protoporphyrin levels (EP, FEP, or ZPP)
CBC and blood smear
Blood lead level
Environmental history
557. An infant is born at terrn to a 27-year-old Caucasian female. The prenatal course was uncomplicated. The amniotic fluid is clear. Immediately after the delivery, the infant starts crying and is moving all four extremities actively. Heart rate is 140/rnin. He is making a grimace on the attempt to put the suction catheter into his nostrils. His body is pink, but extremities are cyanotic. Which of the following is the next best step in the management of the infant?
Intubate the child
Dry the infant and keep warm
Apply silver nitrate solution to the eyes
Administer vitamin K (IM)
Place umbilical catheter
558. A 25-year-old woman brings her 5-day-old infant to the emergency room after noticing that he bruises very easily. Her pregnancy was normal, and the baby was born at term via vaginal delivery at home. This is the child's first visit to the doctor. He is exclusively breast-fed, and there is no family history of bleeding disorders. On physical examination, his vital signs are within normal limits. You note several ecchymotic skin lesions, but his exam is otherwise normal. Laboratory studies show the following: Prothrombin time 20 sec Partial thromboplastin time 37 sec Platelets 200,000/mm3 Which of the following is the most likely cause of his current condition?
Factor VIII deficiency
Impaired synthesis of von Willebrand factor
Excessive destruction of platelets
Consumption of coagulation factors
Vitamin K deficiency
559. A 7-year-old girl is brought to the physician because of an exanthematous rash associated with malaise and headache for 2 days. On examination, the child shows a fiery red facial rash with a characteristic "slapped cheek" pattern and pallor around the mouth. There is no fever. In immunocompromised patients, the pathogen that causes this condition may result in which of the following manifestations?
Aplastic anemia
Encephalitis
Non-Hodgkin lymphoma
Progressive multifocal leukoencephalopath (PML)
Symmetric polyarthritis
560. In the 2nd week of life, a previously healthy newborn develops diarrhea. The stools are watery and voluminous and continue even when the infant is fasting. Which of the following is the most likely pathogen?
Campylobacter jejuni
Enteroinvasive Escherichia coli
Rotavirus
Salmonella species
Shigella species
561. A 17-year-old girl presents to the office with a 5-day history of a malodorous vaginal discharge. She is sexually active and uses condoms for sexual intercourse. On examination, a thin, white discharge is seen. A "fishy" odor is produced when KOH is added to the discharge. The vaginal fluid has a pH of 5. Which of the following is the most likely finding on a microscopic examination of the vaginal fluid?
Clue cells
Gram-negative diplococci
Lactobacilli
Pseudohyphae
Trichomonads
562. A 9-month-old child comes in for a routine visit. She has had several episodes of otitis media in the past, but no major illnesses or hospitalizations. Her mother is concerned because the child was previously happy and social around other people, but now cries if her mother is not in the room. The child constantly wants to be held by her mother and becomes upset if her mother walks into the next room. Her grandmother keeps her during the day, and she now cries when her mother leaves her in the morning. Developmentally, she is crawling and waves bye-bye. She does not yet respond to her name or say words. She previously babbled but stopped several months ago. When you hide a toy with your hand, she lifts your hand to look for the toy. Which of the following is the best next step in the management of this child?
Psychological evaluation
Audiology evaluation
Physical therapy evaluation
Social services referral
Reassure the mother that the child's development is normal.
563. A 14-year-old boy is seen in the ER because of a 3-week history of fever between 38.3C and 38.9C (101F and 102F), lethargy, and a 2.7-kg (6-lb) weight loss. Physical examination reveals marked cervical and inguinal adenopathy, enlarged tonsils with exudate, small hemorrhages on the soft palate, a WBC differential that has 50% lymphocytes (10% atypical), and a palpable spleen 2 cm below the left costal margin. Which of the following therapies should be initiated?
Initiation of zidovudine
IV acyclovir
IV infusion of immunoglobulins and high-dose aspirin
Intramuscular penicillin
Avoidance of contact sports

564. A 2-year-old child is seen in the emergency center with a 10-day complaint of fever and a limp. The child has an elevated erythrocyte sedimentation rate (ESR) and the radiograph shown below. Which of the following statements about this child’s condition is correct?
Itismostcommonlycausedby Streptococcus pyogenes
It can arise following development of deep cellulitis
It usuallyresultsin tendernessin the region of infection that is diffuse, notlocalized.
It causes diagnostic radiographic changes on plain films within 48 hours of the beginning of symptoms.
It requires antibiotic therapy usually for 10 to 14 days
565. A 12-year-old boy with cystic fibrosis presents to the emergency department with a 3day history of severe coughing, which is productive of a yellow-greenish purulent sputum. He had fever and chills at home. He also complains of chest congestion and chest pain that is worse with coughing. On physical examination, his temperature is 39.6 C (103.2 F), blood pressure is 98/68 mm Hg, pulse is 102/min, and respirations are 24/min. He is noted to be lethargic. He has rales on the left lower lung field on auscultation, and chest radiography shows an infiltrate in the left lower lobe. Which of the following is the most appropriate initial antimicrobial therapy for this patient?
Amoxicillin-clavulanate and gentamicin
Azithromycin and ceftriaxone
Ceftazidime and tobramycin
Levofloxacin and metronidazole
Trimethoprim-sulfamethoxazole and vancomycin
566. A 12-year-old boy is brought to the physician because of pain in his right leg for the past 3 weeks. The pain frequently occurs at night and is localized to the tibia, a few centimeters below the knee. The mother reports that the pain is promptly relieved by aspirin and that the child has had no fever. Examination reveals no tissue swelling or redness about the site of pain. X-ray films show a 1-cm radiolucent focus in the tibial cortex surrounded by marked bone sclerosis. Which of the following is the most likely diagnosis?
Aneurysmal bone cyst
Enchondroma
Ewing sarcoma
Osteoid osteoma
Osteosarcoma
567. A 16-year-old African American male with sickle cell anemia presents complaining of a 1-week history of exertional dyspnea, fatigue, and generalized weakness. He denies fevers, chills, night sweats, or cough. His only medication is oxycodone for chronic pain. On physical examination, he weighs 68 kg (150 lbs) and is 168cm (66 in) tall His temperature is 36.7 0C (98 0F), blood pressure is 120/70 mm Hg, pulse is 76/min, and respirations are 18/min. All organ systems appear normal Laboratory studies show: Hematocrit 20% Mean corpuscular volume 110 fl Reticulocyte count 1.0% Which of the following is the most likely mechanism underlying these findings?
Adverse drug reaction
Gastric mucosal atrophy
Bacterial overgrowth in the small intestine
Increased demand for folic acid
Increased demand for vitamin B 12
A 15-year-old female with a history of bipolar disorder and psychosis presents to her physician's office requesting a pregnancy test. Her last menstrual period was 2 months ago. She states that her menses usually occur every 30 days. She is sexually active with one partner and occasionally uses condoms. She is concerned because she has gained 10 pounds in the last two months, and also complains of breast tenderness and milky white discharge from both nipples. She denies headaches, nausea, vomiting, diarrhea, or fever. Her vital signs are normal. Physical examination is unremarkable. A urine pregnancy test is negative. Which of the following is most likely responsible for this patient's symptoms?
Valproic acid
Risperidone
Aripiprazole
Lithium
Lamotrigine
A 7-year-old boy is brought to the physician because of recurrent headaches. The child feels nauseated before and during each attack, and derives some relief from lying down in a dark room. Noises, bright light, and fatigue seem to trigger the episodes. The child frequently complains of headaches at school, and his mother has been occasionally compelled to take him home. The mother is worried about the possibility of a serious illness. She reports that the child's father has similar headaches. The child's growth is normal, and a neurologic examination fails to reveal any abnormality. Which of the following is the most likely
Brain tumor
Cluster headache
Conduct disorde
Migraine
Tension headache
A 17 -year-old boy is brought to the emergency department by his father after the boy began threatening him at home. Over the last several months, the father reports, the boy has been increasingly abusive. He was recently involved in a fist fight at school. The boy states that there is nothing wrong. He is otherwise healthy. He denies alcohol use, but does admit to occasional marijuana use. On examination he has acne on his forehead and back and his hairline is receding. There is palpable tissue underneath his nipples bilaterally Heart and lung exams are normal. What substance is this boy most likely abusing?
Anabolic steroids
Cocaine
Heroin
Methamphetamine
Phencyclidine
A 9-month-old infant is brought to the emergency department with lethargy and tachypnea. He was healthy before developing fever and diarrhea four days ago. He has been taking some formula, but has had two to three episodes of diarrhea with each bottle. He has lost three pounds (1 .4 kg) since his routine check-up two weeks ago. He has had one wet diaper in the past twenty four hours. On examination, his temperature is 102.5F (39.1c), pulse is 200/min, respiratory rate is 42/min, and blood pressure is 70/45 mm Hg. He is lethargic with decreased tone and decreased deep tendon reflexes. His mucous membranes are dry. Cardiopulmonary exam reveals tachycardia and tachypnea. His abdominal exam is unremarkable. Capillary refill is four seconds. Laboratory results are shown below. Chemistry panel Serum sodium 165 mEq/L Serum potassium 4.5 mEq/L Chloride 108 mEq/L Bicarbonate 14 mEq/L Blood urea nitrogen (BUN) 20 mg/dl Serum creatinine 0.8 mg/dl Calcium 10.0 mg/dl Blood glucose 98 mg/dl Which of the following fluids should be used as a bolus in the resuscitation of this infant?
0.9% saline
0.45% saline
5% dextrose
5% albumin
Packed red blood cells
A 15-year-old otherwise healthy boy presents with a complaint of intermittent abdominal distention, crampy abdominal pain, and excessive flatulence. He first started noticing these symptoms when he moved into his father’s house, and his stepmother insisted on milk at dinner every night. He has normal growth, has not lost weight, and has no travel history. Which of the following is the most appropriate study to diagnose his condition?
Barium swallow and upper GI
Hydrogen excretion in breath after oral administration of lactose
Esophageal manometry
Stool pH after one to 2 weeks of a lactose-free diet
Fasting serum lactose levels
A 6-week-old infant is admitted to the hospital with jaundice. Her outpatient blood work demonstrated a total bilirubin of 12 mg/dL with a direct portion of 3.5 mg/dL. Which of the following disorders is most likely to be responsible?
ABO incompatibility
Choledochal cyst
Rh incompatibility
Gilbert disease
Crigler-Najjar syndrome
A 12-year boy is brought to the emergency room by his parents after a several day history of progressive weakness. He has been a healthy child who has met all development milestones and all his immunizations are up to date. He reports that he had an upper respiratory infection 2 weeks ago. On physical examination, his vital signs are labile with a pulse range of 60-100/ min and systolic blood pressure ranging from 80-120 mm Hg. He is alert and oriented. Neurologic examination is impressive for bilateral weakness in the upper and lower extremities. Deep tendon reflexes are absent and sensation is intact. Which of the following is the most likely diagnosis?
Guillain-Barré syndrome
Myasthenia gravis
Polymyositis
Transverse myelitis
Viral encephalitis
A 15-year-old boy with tall stature presents with decreased exercise tolerance over the past 2 months. He states that he used to play two games of basketball with no problem, but he now can play only one game. On physical examination, his weight is at the 25th percentile, and his height higher than the 95th percentile. He is thin and has a gangly body habitus. His fingers are long and thin. There is pectus deformity in his chest. His joints are hyperextensible. An ophthalmologic examination reveals mild subluxation of the lens. Which of the following is the most likely finding on an echocardiogram?
Aortic root dilatation
Aortic stenosis
Bicuspid aortic valve
Dextrocardia
Pulmonary stenosis
A 2-year-old arrives in the emergency center after having swallowed a button battery from one of her toys. She is breathing comfortably, without stridor. Radiographs show the battery to be lodged in the esophagus. Which of the following is the correct next step?
Induce emesis with syrup of ipecac.
Admit for observation, and obtain serial radiographs to document movement of the battery
Discharge home with instructions to monitor the stool for the battery
Immediate removal of the battery via endoscopy
Encourage oral intake to assist in passage of the battery
A 2-year-old boy is brought to the office due to recurrent skin and soft tissue infections. When he was 2- months-old, he had a perianal furuncle that was incised and drained because it was unresponsive to oral antibiotics. At 7 months of age, he had a left inguinal Klebsiella pneumoniae lymphadenitis. His other past infections include a left calf cellulitis that grew Serratia marcescens and a left inguinal abscess that grew Staphylococcus epidermidis. On examination, he has hepatosplenomegaly, and enlarged axillary and inguinal lymph nodes. The screening tests for humoral, cell-mediated, and complement-mediated immunity are normal. The nitroblue tetra zolium (NBT) slide test is abnormal. What is the most likely diagnosis?
Wiskott-Aidrich syndrome (WAS)
Chediak-Higashi syndrome
Chronic granulomatous disease (CGD)
Leukocyte adhesion defect I
Hyper-lgE (Job's) syndrome
A previously healthy 2-year-old male is brought to the emergency department after experiencing a seizure-like episode. His parents report that he has been healthy with the exception of mild upper respiratory symptoms for the past 24 hours. During the episode, his parents state that he fell down and had rhythmic, jerking movements of his arms and legs. The episode lasted about three minutes. The patient was sleepy when the emergency personnel arrived. Vital signs are temperature 39 .2 c (102 .5 F), pulse 120/min, and respiratory rate 25/min. The patient is alert and oriented in the emergency department. On examination, there is mild rhinorrhea and the left tympanic membrane is erythematous, bulging, and poorly mobile. The neck is supple. A complete neurological exam is unremarkable. After treating this patient's fever, which of the following is the next best step in the management of this patient?
Electroencephalogram
Magnetic resonance imaging of the brain
Lumbar puncture
Discharge home with education
Admit for further observation
An awake, alert infant with a 2-day history of diarrhea presents with a depressed fontanelle, tachycardia, sunken eyes, and the loss of skin elasticity. Which of the following is the correct percentage of dehydration?
Less than 1%
1% to 5%
5% to 9%
10% to 15%
More than 20%
A newborn infant is brought to the nursery for evaluation after delivery. The mother reports that the pregnancy was uncomplicated, but she had only two prenatal visits. The infant was born via normal spontaneous vaginal delivery and required no resuscitation. The infant has hepatosplenomegaly on examination. While in the hospital, the infant requires treatment for anemia and hyperbilirubinemia. On subsequent examinations, the infant has clear rhinorrhea and ulcerative lesions on his feet. Which of the following congenital infections is most likely in this patient?
Toxoplasmosis
Syphilis
Rubella
Cytomegalovirus infection
Human immunodeficiency virus infection
A 2 week post mature baby is born and immediately exhibits severe respiratory distress. Previously, green-tinged meconium was noted in the amniotic fluid. Which of the following is the most appropriate next step?
Emergency tracheostomy
Intubation with mechanical ventilation
Chest x-ray film
Oxygen supplementation by face mask
Suction the mouth and nasopharynx
A fetus is delivered at 40 weeks' gestation. During labor, the fetal heart monitor shows late decelerations and loss of short- and long-term variability. The membranes are ruptured to expedite the delivery. The fluid is noted to contain meconium. The infant is delivered 45 minutes later. At delivery, the infant appears to be cyanotic and limp. He has poor tone and deep reflexes. Moro's reflex is absent. Ten hours later, he experiences a seizure. Which of the following best explains this infant's perinatal course?
Encephalopathy from asphyxia
Inborn error of metabolism
Respiratory distress
Subarachnoid hemorrhage
Werdnig-Hoffman disease
An 18-month-old infant is found with the contents of a bottle of drain cleaner in his mouth. Which of the following treatment options is most appropriate?
Immediate emesis
Endoscopic examination within the first 12 to 24 hours
Decontamination by activated charcoal
Neutralization by drinking a solution of the opposite pH
Have the patient drink copious amounts of milk or water
A 16-year-old male, despondent over a recent breakup, tries to commit suicide by taking an unknown quantity of an unknown material he found at home. He is brought to the emergency center by his parents within 30 minutes of the ingestion. For which of the following household materials and medications should he be given activated charcoal as part of his emergency center treatment?
Drain cleaner
Ethylene glycol
Bleach
Phenobarbital
Lithium
A 3-year-old African American boy is brought to the emergency department with sudden onset of difficulty walking. His mother reports that his right hand also seems "clumsy." The boy's past medical history is significant for a hospitalization one year ago for severe upper extremity pain and hand swelling. On physical examination, he has a blood pressure of 90/60 mmHg, heart rate of 120/min, temperature of 36.7°C (98°F), and respiratory rate of 22/min. Which of the following would be most helpful in diagnosing his condition?
Carotid ultrasonography
CBC and reticulocyte count
Antineutrophil cytoplasmic antibodies
Temporal artery biopsy
Lumbar puncture
A 25-year-old woman comes to your office for counseling. She says that her husband has cystic fibrosis, and that she has no family history of this disease. They are planning to have a child. She wonders what the probability is for their baby to have cystic fibrosis. Which of the following is your best response in this situation?
Cystic fibrosis is an autosomal dominant disease, so the child will have the disease
Cystic fibrosis is an autosomal recessive disease, so the child has 25% probability of getting the disease
Cystic fibrosis is an autosomal recessive disease, so the child has 50% probability of getting the disease
The probability cannot be determined because her carrier status is unknown
The probability cannot be determined because cystic fibrosis does not follow Mendelian transmission
A 7-year-old boy is brought to the physician because of persistent nasal obstruction for 6 months. There is no: personal or family history of allergic disorders, Examination of the nasal fossae reveals bilateral ethmoidal polyps that protrude into the middle meatus and nasal cavity. Which of the following is the most appropriate next step in diagnosis?
Cutaneous allergen testing
Excisional biopsy
Nasal provocation testing
Pilocarpine iontophoresis sweat test
Radioallergosorbent test (RAST)
A neonate is very small for gestational age, shows hypotonia, marked skeletal muscle, and subcutaneous fat hypoplasia. During delivery, a large volume of amniotic fluid was released at rupture of membranes. The placenta was small, and only a single umbilical artery was noted. The face has a pinched appearance with hypoplastic orbital ridges, short palpebral fissures, and a small mouth and jaw. The head is small with prominence of the occiput. The ears are low set and malformed. The infant's fists are clenched, with overlapping of the third and fourth fingers. The feet are clubbed, and the great toe is shortened. Which of the following is most likely diagnosis?
47,XXY
TripleX
Trisomy 13
Trisomy 18
Trisomy 21

The delivery of a newborn boy is remarkable for oligohydramnios. The infant (pictured) is also noted to have undescended testes and clubfeet, and to be in respiratory distress. Which of the following is the most likely diagnosis to explain these findings?
Surfactant deficiency
Turner syndrome
Prune belly syndrome
Hermaphroditism
Congenital adrenal hyperplasia
A 17-year-old boy is brought to the emergency department by his parents with the complaint of coughing up blood. He is stabilized, and his hemoglobin and hematocrit levels are 11 mg/dL and 33%, respectively. During his hospitalization, he is noted to have systolic blood pressure persistently greater than 130 mm Hg and diastolic blood pressure greater than 90 mm Hg. His urinalysis is remarkable for hematuria and proteinuria. You are suspicious the patient has which of the following?
Hemolytic-uremic syndrome
Goodpasture syndrome
Nephrotic syndrome
Poststreptococcal glomerulonephritis
Renal vein thrombosis
A 10-year-old presents with 2months history of heavy menstrual-like bleeding. Menarche occurred 6 months ago and this first menses consisted of spotting for 3-4 days without cramps. Subsequent periods were light in flow but lasted 6 to 8 days. Which of the following is the most likely cause of her bleeding?
Von Willebrand disease
Ovarian tumor
Thyroid disease
Dysfunctional uterine bleeding
Pregnancy
A 4-year-old boy presents with 5-day history of fever and increased irritability. His temperature is 40. 2 C (104. 3 F), blood pressure is 98/68 mm Hg, pulse is 112/min, and respirations are 24/min. On physical examination, he is noted to have bilateral cervical lymphadenopathy, cracked lips, strawberry tongue, and bilateral conjunctival injection. His palms and soles are erythematous. There is a polymorphous macular rash generalized on his body. Which of the following is the most appropriate pharmacotherapy?
Amoxicillin
Aspirin and corticosteroid
Aspirin and IV immune globulin
Corticosteroid
IV immune globulin

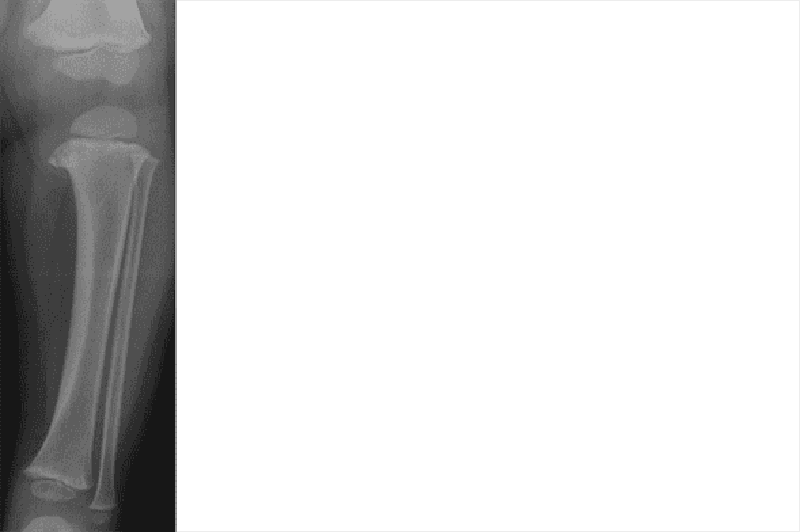
A 13-year-old male is brought to the physician for evaluation of intermittent left knee pain that arose three months ago. He does not remember any trauma to his knee. The pain worsens after basketball games, but improves some with rest. He has been taking nonsteroidal anti-inflammatory medications with some relief. On physical examination, he has edema and tenderness over the proximal tibia at the site of the patellar tendon insertion. Examination of the knee joint is normal and no effusion is present. His knee pain is reproducible by extending the knee against resistance. A lateral radiograph of his knee is shown below. Which of the following is the most likely cause of this patient's knee pain?
Prepatellar bursitis
Traction apophysitis
Patellar tendonitis
Tibial osteomyelitis
Patellofemoral stress syndrome
A 4-day-old infant is brought to the physician for an outpatient follow-up visit. The mother's pregnancy and delivery were uncomplicated. The infant weighed 3.4kg (7 .5 lb) and was 19 in (48.2 cm) long at birth. He did well in the newborn nursery and was discharged from the hospital on day 2 of life. Today his mother reports that he is exclusively breastfed, and nurses for 10 minutes every 3 hours. He has 3-4 wet diapers a day, and has not had a bowel movement for two days. On examination, he weighs 2.95 kg (6.5 lb) and is 19 in (48.2 cm) long. He appears jaundiced on the face and chest. The remainder of the physical examination is unremarkable. Laboratory values are shown below. Total bilirubin 15 mg/dl Direct bilirubin 1 mg/dl Infant's blood type O positive Mother's blood type A positive Which of the following is the most likely cause of this infant's hyperbilirubinemia?
Biliary atresia
Breast milk jaundice
Breastfeeding jaundice
Galactosemia
ABO incompatibility
A 16-year-old boy with a history of ulcerative colitis presents to the physician complaining of diarrhea and a rash. He states that his appetite has been decreased recently, and also complains of nausea and abdominal pain in addition to watery diarrhea. He has an erythematous rash on his distal arms and legs that "burns". His mother reports that he has had poor concentration and has been irritable lately. Vital signs are stable. Examination reveals a beefy red tongue that appears swollen. Abdominal examination is normal. The rash resembles a sunburn and is located on his distal arms and legs. It is symmetrical and tender to palpation. Neurological examination is normal. This patient's symptoms are most likely due to a deficiency of which of the following vitamins?
Thiamine
Riboflavin
Niacin
Pyridoxine
Cyanocobalamin
You are called by a general practitioner to consult on a patient admit- ted to the hospital 4 days ago. The patient is a 7-month-old white boy with poor weight gain for the past 3 months, who has not gained weight in the hospital despite seemingly adequate nutrition. You take a detailed diet his- tory from his foster mother, and the amounts of formula and baby food intake seem appropriate for age. Physical examination reveals an active, alert infant with a strong suck reflex who appears wasted. You note generalized lymphadenopathy with hepatomegaly. In addition, you find a severe case of oral candidiasis that apparently has been resistant to treatment. Which of the following is the most appropriate next step in the evaluation or treatment of this child?
Increase caloric intake because this is probably a case of underfeeding
Order human immunodeficiency virus (HIV) polymerase chain reaction (PCR). Testing because this is likely the presentation of congenitally acquired HIV.
Draw blood cultures because this could be sepsis
Perform a sweat chloride test because this is probably cystic fibrosis
Send stool for fecal fat because this is probably a malabsorption syndrome

A 5-year-old boy presents with the severe rash shown in the photographs. The rash is pruritic, and it is especially intense in the flexural areas. The mother reports that the symptoms began in infancy (when it also involved the face) and that her 6-month-old child has similar symptoms. Which of the following is the most appropriate treatment of this condition?
Coal-tar soaps and shampoo
Topical antifungal cream
Ultraviolet light therapy
Moisturizers and topical steroids
Topical antibiotics
A 13-year-old girl returns to her physician for followup of a strep throat, for which she had been treated 3 weeks previously. After performing a throat culture, the physician asks how school is going. There is dead silence. Her mother says that her daughter has missed the last 4 weeks of school. Which of the following is the most appropriate initial step in management?
Contract with the girl to go back to school as you explore the problem
Write a medical excuse for her until the throat culture results come back
Tell them you must report her to the school authorities for truancy
Send the mother for supportive counseling
Send the girl for psychotherapy
A 1 -year old child is brought in for a well baby check-up. His parents report that he has been of good health and began walking a few weeks earlier. They are concerned that he tends to bump into things and falls more than his older sister did. Family history is significant for retinoblastoma. On examination, the pediatrician notes leukocoria of the left eye. No significant lymphadenopathy is present, and there is no enlargement of the liver or spleen. The child's height and weight are normal for age. Which of the following is the most appropriate next step in management?
Explain to parents what leukocoria is and reassure them that it is temporary
Return visit in 1 month
Refer to neurologist
Refer to ophthalmologist
Treat the eye with erythromycin ophthalmic ointment for 10 days
A 4-year-old boy is being evaluated for short stature. He has a history of multiple bone fractures in the past. He requires a wheelchair to ambulate and has hearing difficulty. On physical examination, his height is below the 5th percentile. His sclerae are blue in color. There is marked deformity of his lower extremities. Which of the following is the most likely diagnosis?
Achondroplasia
Constitutional delay of growth
Developmental dysplasia of the hip
Familial short stature
Osteogenesis imperfecta
A 6-month-old infant presents to the emergency department with the new onset of weak cry, decreased activity, and poor feeding. The mother also states that the infant has been constipated for the past 2 days. On physical examination, the infant has a very weak cry, poor muscle tone, and absent deep tendon reflexes. Which of the following is the most likely diagnosis?
Congenital hypothyroidism
Guillain-Barré syndrome
Infant botulism
Myasthenia gravis
Vaccine-associated poliomyelitis
You are called to examine a 2-day-old male, newborn after he was noted to be cyanotic. He was born at term. His antenatal and birth histories are unremarkable. Auscultation reveals a holosystolic murmur at the left, lower sternal border and a single S2. No rales or rhonchi are heard. Chest radiograph reveals decreased pulmonary vascular markings and a normal-sized heart. EKG reveals left axis deviation. What is the most likely diagnosis?
Tetralogy of Fallot
Truncus arteriosus
Common atrioventricular canal
Ebstein's anomaly
Tricuspid atresia
A 6-year-old Asian boy is brought by his parents to the office due to high-grade fever and rash for the last 9 days. A brick-red, maculopapular rash first appeared on his face and subsequently spread to his trunk and extremities. Prior to the outbreak of the rash, he had a non-productive cough, tearing of eyes, runny nose, sneezing, and intermittent nasal obstruction. Laboratory findings are as follows: Hct 46% WBC 2,000/mm3 Platelets 160,000/mm3 Which of the following has been shown to reduce the morbidity and mortality rates of patients with this kind of infection?
Vitamin A
Vitamin B 6
Vitamin B 12
Vitamin E
Vitamin K
A 2-year-old boy has been vomiting intermittently for 3 weeks and has been irritable, listless, and anorectic. His use of language has regressed to speaking single words. In your evaluation of this patient, which of the following is the most reasonable diagnosis to consider?
Expanding epidural hematoma
Herpes simplex virus (HSV) encephalitis
Tuberculous meningitis
Food allergy
Bacterial meningitis
A 15-year-old boy is seen in the pediatrician's office for a health maintenance physical examination. The boy reports a heavy, dragging sensation in his left scrotum. The sensation is more pronounced after exercise. He denies any scrotal pain. He is not sexually active. Examination of his genitalia indicates Tanner stage 4. There is a palpable fullness over his left scrotum. Both testes are normal in size and smooth in contour. Which of the following is the most likely explanation of these findings?
Hydrocele
Inguinal hernia
Orchitis
Testicular tumor
Varicocele
A 5-year-old child undergoes a school entrance physical examination. The pediatrician notices grey-brown pigmentation on the skin of his forehead, hands, and pretibial regions. Subconjunctival areas near the corneoscleral junction show wedge-shaped, yellow-brown discoloration (pingueculae). Enlargement of both the spleen and the liver are noted on abdominal examination. Needle biopsy of the spleen demonstrates the presence of unusually large (20- to 100-mm diameter) reticuloendothelial histiocytes with a "crumpledsilk" appearance. Bone marrow biopsy demonstrates the presence of the same type of cells. Which of the following is the most likely diagnosis?
Abetalipoproteinemia
Fabry disease
Gaucher disease
Niemann-Pick disease
Tangier disease
A term male infant is found to be cyanotic shortly after birth and requires endotracheal intubation. On physical examination, his blood pressure is 68/34 mm Hg (equal in all four extremities), pulse is 180/min, and respirations are 32/min. His precordium is dynamic, has a grade III systolic murmur, and a single S2. Chest radiography shows a normal heart size and increased pulmonary vascular markings. An arterial blood gas on an FiO2 of 100% shows pH 7.34; PaCO2, 47 mm Hg; PaO2, 46 mm Hg. Which of the following diagnoses is most consistent with these findings?
Atrial septal defect
Hypoplastic left heart syndrome
Patent ductus arteriosus
Tetralogy of Fallot
Total anomalous pulmonary venous return
A 6-month-old boy is found to have bilateral metaphyseal fractures of both proximal and distal ends of the tibia. The mother says that her boyfriend takes care of the infant while she is at work. Her boyfriend explains the injuries as the result of multiple falls from bed. Which of the following is the most likely diagnosis?
Accidental trauma
Osteogenesis imperfecta
Osteopetrosis
Physical abuse
Rickets
A 15-year-old African-American girl has a facial rash and vague joint pains. Her temperature is 37.2C (99F). On examination, a malar erythematous rash is noted. Her laboratory evaluation is significant for anemia, leukopenia, and a normal platelet count. Her antinuclear antibody and Rapid Plasma Reagin (RPR) tests are positive. Which of the following tests is confirmatory for this patient's condition?
VORL (Veneral Disease Research Laboratory) test
FTA (Fluorescent T reponemal Antibody) test
Anti-Smith antibody test
Coomb's test
Bone marrow examination
A 7 -year-old boy is rushed to the emergency department after falling on his outstretched hand. He immediately complained of right arm pain after the accident, and he currently cannot move his arm due to the pain. He is crying and holding his right arm in flexion. There is ecchymosis just above his elbow. He cries out in pain when his arm is moved. An x-ray reveals a supracondylar fracture. What secondary injury is most commonly associated with this patient's fracture?
Median nerve injury
Axillary nerve injury
Ulnar artery injury
Brachial artery injury
Brachial plexus injury

A patient with hair loss is shown below. The lesion does not fluoresce with a Wood lamp and has not responded well to a variety of topical agents. The lesion is boggy, is spreading, and has tiny pinpoint black dots throughout. Which of the following is the most likely diagnosis?
Traction alopecia from tight hair braids
Infection with Trichophyton tonsurans
Alopecia areata
Biotinidasedeficiency
Hypothyroidism
An 8-year-old sickle-cell patient arrives at the emergency room (ER) in respiratory distress. Over the previous several days, the child has become progressively tired and pale. The child’s hemoglobin concentration in the ER is 3.1 mg/dL. Which of the following viruses commonly causes such a clinical picture?
Roseola
Parvovirus B19
Coxsackie A16
Echovirus11
Cytomegalovirus
A 2-year-old child has had red, weeping, crusted lesions of the face, scalp, diaper area, and extremities since about age 2 months, with multiple periods of exacerbation and improvement. Attempts to remove potentially irritating substances have not modified the course of the rashes. The child is noted to be constantly scratching and rubbing involved areas. There is a strong family history of hay fever and asthma. Which of the following is the most likely diagnosis?
Atopic dermatitis
Cellulitis
Contact dermatitis
Lichen simplex chronicus
Seborrheic dermatitis
A 5-year-old boy is brought to clinic with increasing right lower foot pain. He stepped on a nail several days ago. At that time, the family had sought medical attention. The child was given a tetanus shot, and the wound was extensively irrigated. On examination, the foot is tender, swollen, warm, and erythematous. Osteomyelitis is suspected. Which of the following is the most appropriate next step in diagnosis?
White cell count
CT scan of the foot
Gallium scan
Technetium bone scan
X-ray of the foot
A 16-year-old girl with an incomplete vaccination record received one dose of the measles, mumps, and rubella (MMR) vaccine during a doctor's visit. One month later, she learns that she is 9 weeks pregnant, and she is concerned about potential birth defects resulting from the MMR vaccine. Which of the following most closely approximates the risk of birth defects secondary to MMR vaccine exposure during the first trimester?
<1%
3%
5%
8%
10%
A 6-week-old male infant who was born at 32 weeks' gestation with a birth weight of 1500 g, has had an average weight gain of 8 g/day since birth. He takes an iron-fortified formula that is 24 kcal/oz. His calorie intake is about 125 kcal/day. It is noted that his stool is poorly formed and bulky. Which of the following dietary modifications will most likely result in decreased steatorrhea and improved weight gain?
Add pancreatic enzymes to the formula
Change to a lactose-free formula
Increase calorie intake to 175 kcal/day by increasing volume per feed
Substitute medium-chain triglycerides for long-chain triglycerides
Supplement with vitamins A and E
A previously healthy 4-year-old girl is brought to the office due to a 12-day history of persistent, thick, nasal discharge, nasal congestion, headache, cough, and intermittent lowgrade fever. The cough is worse at night, but there is no wheezing. Her temperature is 37.2C (99F), pulse is 90/min, and respirations are 15/min. Examination shows an alert, interactive child breathing comfortably. She has clear tympanic membranes, congested posterior nasal pharynx with thick and purulent mucus, and red, swollen nasal turbinates. Her maxillary sinuses are mildly tender. Her lungs are clear on auscultation. What is the most appropriate next step in the management of this patient?
X-ray paranasal sinuses
CT scan of sinuses
Sinus aspiration
Start the patient on decongestants
Start the patient on oral amoxicillin
A 7-year-old Caucasian boy is brought to the clinic because of poor performance in school. His mother says that his teachers have been complaining about his poor attention in the classroom for the past 8 months. They have also complained that he is out of his seat often, fidgets, and talks excessively, gets distracted easily, and interrupts class and other students. His mother has noticed that he often loses his things, and she is having more and more difficulty disciplining him at home. His antenatal and postnatal history is insignificant. His parents never had any similar problems with his 10-year-old sister. What is your clinical diagnosis?
Autistic disorder
Attention deficit hyperactivity disorder
Oppositional defiant disorder
Conduct disorder
Learning disorder
A 13-year-old comes to your office expressing concern about his height. He had first seen you a year prior for his routine checkup and a preparticipation sports physical for soccer (see growth curve). Now in the eighth grade, al of his friends are taller than he is, and he is at a disadvantage on the soccer field playing against much larger boys. After obtaining height information from his parents shown here, you order a skeletal bone age radiograph. Which of the following results would allow you to assure him of an excellent prognosis for normal adult height?
A bone age of 9 years
A bone age of 13 years
A bone age of 15 years
Being at the 50th percentile for weight
Being at the 3rd percentile for weight

The parents of the child pictured below bring him to the office for evaluation of short stature. At 5 years of age, he is the shortest child in his kindergarten class. His development is normal, and he is reading on a first grade level. Both parents are of normal height, and this child resembles no one in the family. Which of the following is the most likely diagnosis?
Achondrogenesis
Achondroplasia
Metatropic dysplasia
Thanatophoric dwarfism
Chondroectodermal dysplasia
A 3-day-old, full-term baby boy is brought into the emergency department because of feeding intolerance and bilious vomiting. X-rays films show multiple dilated loops of small bowel and a "ground glass" appearance in the lower abdomen. The mother has cystic fibrosis. Which of the following diagnostic tests would also have therapeutic value?
Barium enema
Gastrografin enema
Endoscopic retrograde chokngiopancreatogram (ERCP)
Full thickness rectal biopsy
Colonoscopy
A 17-year-old girl presents with a 4-week history of intermittent fever, increasing fatigue, generalized myalgia, and swelling of both her knees and ankles. There is a fine erythematous rash on her back, and she has swollen knees and ankles; the remainder of her physical examination is unremarkable. Initial laboratory evaluation shows: Leukocytes 11,400 cells/mm3 Hemoglobin 8.8 g/dL Blood urea nitrogen 4 mg/dL Creatinine 1.4 mg/dL Glucose 98 mg/dL C3 complement 36 mg/dL (normal >80 mg/dL) Antinuclear antibody titer 1:3200 Anti-double-stranded DNA titer 1:640 Antineutrophil cytoplasmic antibodies: Negative Urinalysis Moderate hematuria (50 RBC/hpf), Moderate proteinuria (400 mg/dL) Which of the following is the most likely diagnosis?
Giant cell arteritis
Henoch-Schonlein purpura
Polyarteritis nodosa
Systemic lupus erythematosus
Wegener granulomatosis
A vomiting infant is brought to the emergency room. The blood work results reveal a normal blood count, but a hyponatremic, hypochloremic, metabolic alkalosis. Which of the following would be consistent with these findings?
Diabetes mellitus
Cystic fibrosis
Ethanol poisoning
Iron ingestion
Isoniazid ingestion
A 5-year-old boy develops a headache, cough, myalgia and a fever. He has been a healthy child with all immunizations up to date. He is given a decongestant and an aspirin for his symptoms with some relief. However, 4 days later, he is brought back by his parents because of persistent vomiting and irritability. On physical examination, he is found to be semicomatose, becoming combative on stimulation. Which of the following levels should be measured to aid in the diagnosis of this patient?
Serum ammonia level
Serum blood urea nitrogen level
Serum calcium level
Serum opiate level
Serum sodium level
A 3-year-old boy is admitted for seizure-like activity. He has been a healthy child and has been meeting all development milestones. His immunization schedule is upto-date. Examination is notable for an erythematous throat and fever. His convulsions require IV administration of a benzodiazepine. Serum analysis reveals a normal white cell count with mild basophilic stippling. The lumbar puncture reveals elevated CSF pressure. Head CT scan is notable for cerebral edema. Which of the following is the next diagnostic step?
Antistreptolysin O titer
Electroencephalography
Protoporphyrin level
Rapid slide (Monospot) test
Spinal fluid culture
A 2-week postmature neonate exhibits severe respiratory distress immediately after birth. Previously, greentinged meconium was noted in the amniotic fluid. Which of the following is the most appropriate next step in management?
Chest x-ray
Suctioning of the mouth and nasopharynx
Oxygen supplementation by face mask
Intubation with mechanical ventilation
Emergency tracheostomy
A 12-year-old girl has a solitary thyroid nodule found on routine examination; she has no symptoms. Which of the following is the most appropriate next step for this patient?
Fine needle aspirate
CT scan of the neck
Serum thyroid function tests
Trial of suppressive T4 treatment to look for nodule shrinkage
Excisionalbiopsy

The 16-month-old male infant pictured below was recently brought from a developing country to the United States. The family history reveals that his father had an eye and a leg removed. Which of the following is the most likely diagnosis?
Coloboma of the choroid
Retinaldetachment
Nematode endophthalmitis
Retinoblastoma
Persistent hyperplastic primary vitreous
A 12-year-old African American boy is brought to the office due to a 2-day history of high-grade fever and chills. He was apparently well before the onset of fever. He has no bone pain. He has sickle cell disease and has had 4 hospitalizations for painful crises and one episode of osteomyelitis. His blood pressure is 90/60 mm Hg, pulse is 100/min, respirations are 22/min and temperature is 38.9 C (102F). He appears drowsy. His laboratory report shows a total WBC count of 16,000/mm3 with 12% bands and Hb of 9.0 g/dl. Which of the following is the most likely cause of this patient's condition?
Streptococcus pneumoniae
Staphylococcus aureus
Salmonella
Escherichia coli
Pseudomonas aeruginosa
A 12-year-old male is brought to your office by his mother because of a several month history of back pain. He also experienced bed wetting recently. His past medical history is insignificant. He tried acetaminophen for pain relief. He does not smoke or consume alcohol. His temperature is 36.7 C (98 F), blood pressure is 110/65 mmHg, pulse is 80/min, and respirations are 16/min. Physical examination reveals a palpable "stepoff" at the lumbosacral area. Straight-leg raising test is negative on both sides. Perianal sensation tested by pinprick test is decreased, but anal reflex is normal. What is the most probable diagnosis in this patient?
Multiple myeloma
Ankylosing spondylitis
Compression fracture of the vertebrae
Lumbosacral strain
Spondylolisthesis
A 16-month-old is taken to the emergency room after falling while learning to walk. The toddler has an enlarging, swollen bruise on his forehead, which is now over two inches across. The parents say that the bruise is noticeably larger than it was when they entered the emergency room an hour earlier. A blood sample is drawn, and the child oozes blood at the puncture site for 25 minutes. Clotting studies on the blood sample show a prolonged PTT and a normal PT. Follow-up studies show very low levels of factor VIII. Which of the following is the most likely diagnosis?
A 16-month-old is taken to the emergency room after falling while learning to walk. The toddler has an enlarging, swollen bruise on his forehead, which is now over two inches across. The parents say that the bruise is noticeably larger than it was when they entered the emergency room an hour earlier. A blood sample is drawn, and the child oozes blood at the puncture site for 25 minutes. Clotting studies on the blood sample show a prolonged PTT and a normal PT. Follow-up studies show very low levels of factor VIII. Which of the following is the most likely diagnosis?
Hemophilia A
Hemophilia B
Hyperhomocysteinemia
Von Willebrand disease
A 7-day-old boy who is the product of an uncomplicated gestation is brought to the physician because of hypospadias. The baby is otherwise healthy, and is urinating without any difficulty. On physical examination, vital signs are stable, lungs are clear and the heart is beating at a regular rate. The only abnormal physical finding is the hypospadias. Urinalysis is negative for infection. Which of the following is the most appropriate next step?
Measuring serum creatinine level
Schedule a renal ultrasound
Obtain an intravenous pyelogram
Cystography
Performing a circumcision
A 15-year-old Caucasian boy is injured during a football game. He is taken to the emergency department for x-ray films of his leg to rule out a possible fracture. The radiologist reports that the boy has evidence of an aggressive bone tumor with both bone destruction and a soft tissue mass. Later, the pathologist reports that the bone biopsy reveals a bone cancer with some of the tumor tissue displaying neural differentiation. Which of the following is the most appropriate next step in management?
Chemotherapy
Radiation therapy
Surgery
Surgery and chemotherapy
Surgery, chemotherapy, and radiation therapy
A 7-year-old boy has a history of repeated urinary tract infections that have been treated by the empiric use of antibiotics. The parents are not satisfied with the care the child is receiving, and they take him to a pediatric urologist. Evaluation by voiding cystourethrogram shows that the patient has vesicoureteral reflux without ureteral or upper tract dilatation (grade one reflux). Which of the following is the appropriate management for this child?
Alpha blockers
Long-term, low-dose antibacterial therapy
Nephrectomy on the affected site
Reassurance and observation
Surgical reimplantation of the ureter
A 10-year-old boy was healthy until about 10 days ago when he developed 7 days of fever, chills, severe muscle pain, pharyngitis, headache, scleral injection, photophobia, and cervical adenopathy. After 7 days of symptoms he seemed to get better, but yesterday he developed fever, nausea, emesis, headache and mild nuchal rigidity. Cerebrospinal fluid (CSF) shows 200 white blood cells (WBC) per microliter (all monocytes) and an elevated protein. Correct statements about this infection include which of the following?
The condition is obtained from arthropod vectors
CNS involvement is uncommon
Most cases are mild or subclinical
Appropriate treatment includes intravenous (IV) immune globulin (IVIG) and aspirin
Hepatic and renal involvement occurs in the majority of cases
A previously healthy 8-year-old boy has a 3-week history of low-grade fever of unknown source, fatigue, weight loss, myalgia, and headaches. On repeated examinations during this time, he is found to have developed a heart murmur, petechiae, and mild splenomegaly. Which of the following is the most likely diagnosis?
Rheumatic fever
Kawasaki disease
Scarlet fever
Endocarditis
Tuberculosis
A 10-year-old boy is brought by his parents to the emergency department for the evaluation of headaches, fever, chills, and a rash over his neck, chest, and axillae. The rash appeared today, and for the past two days the child was complaining of a sore throat. He has no history of allergies, and his immunizations are up-to-date. His blood pressure is 112/70 mmHg, pulse is 1 08/min, respirations are 20/min, and temperature is 38.3C (101 F). Examination reveals an erythematous rash with a sandpaper-like texture, and which blanches with pressure. There is submandibular tender lymphadenopathy, and the throat is erythematous with gray-white exudates. What is the most likely diagnosis?
Kawasaki disease
Staphylococcal scalded skin syndrome
Scarlet fever
Stevens-Johnson syndrome
Mononucleosis
A 2-year-old boy is referred to your office for the evaluation of a white eye reflex. His mother suspects a hearing problem because he does not respond when she calls out his name. The physical examination reveals a continuous, machinery murmur over the right 2nd intercostal space and purple lesions on his arms and chest. The initial investigations reveal thrombocytopenia. What is the most likely diagnosis?
Sturge Weber syndrome
Retinoblastoma
Congenital rubella infection
Congenital CMV infection
Congenital Toxoplasma infection
A 10-year-old male fell while riding his scooter down a steep hill. In the Emergency Department, his injuries included a fractured wrist and a lacerated spleen, which required surgical removal. Two years later he is diagnosed with bacterial pneumonia. Which of the following bacterial agents is the most likely pathogen for this patient's pneumonia?
Escherichia coli
Klebsiella pneumoniae
Neisseria meningitidis
Streptococcus pneumoniae
Staphylococcus aureus
A 15-year-old girl presents with diplopia after prolonged reading and ptosis that worsens in the afternoon. On examination, she is noted to have bilateral ptosis, impaired extraocular muscle movements, facial weakness, and generalized hypotonia and weakness increasing with repetition. Which of the following is the best diagnostic test for this disorder?
CT of the brain
Electromyography
Lumbar puncture
Muscle biopsy
Nerve conduction velocity
A 12-year-old boy presents to his pediatrician with frequent episodes of headache, nausea, blurry vision, and sweating. On physical examination, his temperature is 37.4 C (99.3 F), blood pressure is 148/94 mm Hg, pulse is 92/min, and respirations are 18/min. The rest of his examination is unremarkable. His 24-hour urinary vanillylmandelic acid (VMA) and metanephrines are increased. An abdominal CT reveals an extrarenal mass above the left kidney. Which of the following is the most appropriate pharmacotherapy?
Alpha-adrenergic blocker
Angiotensin-converting enzyme inhibitor
Beta-adrenergic blocker
Calcium channel blocker
Diuretics
A 12-year-old girl with mild asthma comes to the office for a health maintenance visit. Her mother states that she is using her albuterol inhaler 2-3 times a week and that she has a cough that wakes her up at night about 3 times a month. On physical examination, she has diffuse inspiratory and expiratory wheezes. She has no accessory muscle use. Pulse oximetry shows 95% oxygen saturation on room air. Which of the following is the most appropriate treatment for her at this time?
Albuterol nebulized treatment
Cromolyn sodium nebulized treatment
Oxygen via nasal cannula
IV steroids
Subcutaneous epinephrine
You find a discrete, whitish polyp that extends through the tympanic membrane in a child with a history of recurrent otitis media. This most likely represents which of the following?
A cholesteatoma
Tympanosclerosis
Acute otitis media with perforation and drainage
Dislocation of the malleus from its insertion in the tympanic membrane
Excessive cerumen production
A 20-month-old child is brought to the ED because of fever and irritability and refusal to move his right lower extremity. Physical examination reveals a swollen and tender right knee that resists passive motion. Which of the following is the most likely to yield the diagnosis in this patient?
Examination of joint fluid
X-ray of the knee
Erythrocyte sedimentation rate (ESR)
CBC and differential
Blood culture
A 6-year-old boy is brought to the office by his mother for the evaluation of a "skin disease." The physical examination reveals multiple vesiculopustular lesions on his face and neck. Some lesions are colored golden-yellow and encrusted. The crust is thick and adherent to the underlying skin. The rest of his physical examination is within normal limit. What is the most appropriate treatment for his skin condition?
Topical erythromycin
Topical mupirocin
Oral penicillin
Topical dicloxacillin
Topical cephalexin
A 5-day-old male premature infant in the NICU develops a decreased level of consciousness, hypotonia and decreased spontaneous movements. He was delivered vaginally at 32 weeks of gestation, and his birth weight was 1800g. Examination reveals a lethargic infant with a weak and high-pitched cry, prominent scalp veins, tense fontanels, and eyes directed downward, poor suckling, hypotonia. CT scan reveals dilation of the entire ventricular system, with distinct enlargement of the subarachnoid space over the cerebral cortex. What is the most likely cause of the patient's condition?
Intraventricular hemorrhage
Dandy-Walker malformation
Arnold-Chiari malformation
Intrauterine infection
Neonatal meningitis
A 12-month-old infant presents with bilious vomiting and abdominal distention for 10 hours. His mother states that the infant has been constipated since birth and failed to pass meconium during the first 48 hours of life. On examination, he is very irritable. His length and weight are both below the 5th percentile according to his age. His abdomen is moderately distended. After a digital rectal examination, a fair amount of stool ejects out from the anus. Which of the following is the most likely diagnosis?
Duodenal atresia
Intussusception
Hirschsprung disease
Malrotation
Pyloric stenosis
A 9-year-old boy is brought to the pediatrician's office for bed-wetting. His mother states that he has never been dry at night. Occasionally, he has problems controlling his bladder during the day. On physical examination, his blood pressure is 98/56 mm Hg. Both his weight and height are below the 5th percentile for his age. His bladder is enlarged and palpable above the symphysis pubis. Which of the following is the most likely cause of his problem?
Obstructive uropathy
Primary polydipsia
Reflux nephropathy
Sickle cell trait
Unstable bladder
A 4-day-old female infant presents to the emergency department with vomiting and abdominal distention. The mother states that the vomitus was green. The infant also has had difficulty feeding and has been hard to console. The mother had an uncomplicated pregnancy. The infant passed meconium within 12 hours after birth. She also had several small, seedy, yellowish stools each day since birth. On physical examination, she is very irritable, her anterior fontanelle is slightly depressed. Her abdomen is distended. Which of the following is the most likely diagnosis?
Allergic reaction to formula
Gastroesophageal reflux disease
Hirschsprung disease
Meconium ileus
Midgut volvulus
An 8-year-old boy presents to the pediatrician's office with a headache for the past 3 weeks. His mother also states that he has been more tired and has had frequent nose bleeding for the past month. On physical examination, his height and weight are both below the 5th percentile for his age. His blood pressure is 152/86 mm Hg in all four extremities. His pulse is 74/min, and respirations are 16/min. His heart examination is normal with no murmur. His peripheral pulses are strong and symmetric. Urinalysis and serum electrolytes are ordered. Which of the following is the most appropriate next step in diagnosis?
24-hour urine creatinine and protein
Blood urea nitrogen and creatinine concentration
Plasma and urine catecholamine levels
Serum aldosterone level
Serum Cortisol level
A 1-year-old presents for a well-child checkup, but the parents are concerned about giving the child his immunizations. Which of the following is a true contraindication to the administration of the fourth DTaP (diphtheria and tetanus toxoid and acellular pertussis) vaccine?
Child is currently on amoxicillin for an otitis media
Positive family history of adverse reactions to DTaP vaccine
A past history of infantile spasms
Child is currently febrile to 39°C (102.2°F)
Prolonged seizures 6 days after the last DTaP vaccine
An 11-year-old boy presents with fever and sore throat. A rapid-strep test confirms streptococcal pharyngitis. He is leaving for a summer camp in 2 days. In the past, he has had problem finishing the whole course of antibiotic treatment. Which of the following is the best treatment for his streptococcal pharyngitis?
A single dose of benzathine penicillin G intramuscularly
A single dose of ceftriaxone intramuscularly
A single dose of procaine penicillin G intramuscularly
Erythromycin orally for 5 days
Penicillin V orally for 5 days
A previously healthy 11 -year old boy presents to the physician with a fever and persistent vomiting for 4-5 days. Initially, the emesis was clear, but now it contains streaks of bright red blood. Findings on a physical examination, complete blood count, and serum electrolytes are within normal limits. Which of the following is the most likely cause of the hematemesis?
Esophageal varices
Esophagitis
Gastritis
Mallory-Weiss tear
Mallory-Weiss tear
A 7 -year-old boy is brought to the emergency department after falling on his outstretched hand. On examination, there is minimal swelling at the right elbow. The skin on the right forearm appears tense, and severe pain is present. The brachial pulses are good bilaterally, and sensations are intact in both upper limbs. X-rays of the right upper limb show a displaced anterior fat pad. Which of the following statements is true about this condition?
The presence of brachial pulse on the right side rules out the possibility of vascular compromise
Fracture of forearm bones is responsible for the swelling
The treatment should consist of immediate cast placement
Suspect child abuse and report the case to child protection services
Forearm swelling is due to ischemia of the forearm soft tissues
An 8-week-old female infant is brought to the office by her Caucasian mother for a well-baby examination. She was born at 34 weeks gestation, and weighed 2.9kg (6.51b) at birth. She has been exclusively breastfed since birth, and her growth and development are normal for her age. The physical examination is normal, except for mild pallor. At this time, what is the most appropriate nutritional intervention for this patient?
Vitamin C supplementation
Iron supplementation
Inclusion of vegetables in diet
Inclusion of fruit juices in diet
Introduce egg and meat in diet
A 6-year-old boy is brought to the clinic due to persistent leg pain. Over the last few months, he has been constantly complaining of pain in his legs. The painful episodes occur only at night, and last a few hours each. His mother has been treating him with over-thecounter medications. He is able to walk and run to school without any complaints. He has no fever, chills and history of trauma. On examination, there is no obvious trauma to his legs, and the limb exam is completely normal. His parents are very worried and ask that you "do something.” Which of the following is the most appropriate next step in management?
Plain radiographs
Bone scan
Blood cultures
Psychiatric evaluation
Observation and reassurance
Parents bring a 5-day-old infant to your office. The mother is O negative and was Coombs positive at delivery. The term child weighed 3055 g (6 lb, 1 oz) at birth and had measured baseline hemoglobin of 16 g/dL and a total serum bilirubin of 3 mg/dL. He passed a black tarlike stool within the first 24 hours of life. He was discharged at 30 hours of life with a stable axillary temperature of 36.5°C (97.7°F). Today the infant’s weight is 3000 g, his axillary temperature is 35°C (95°F), and he is jaundiced to the chest. Parents report frequent yellow, seedy stool. You redraw labs and find his hemoglobin is now 14 g/dL, and his total serum bilirubin is 13 mg/dL. The change in which of the following parameters is of most concern?
Hemoglobin
Temperature
Body weight
Bilirubin
Stool
You are called to a delivery of a woman with no prenatal care; she is in active labor but has no history of amniotic rupture. The biophysical pro- file done in the emergency center revealed severe oligohydramnios. When you get this infant to the nursery, you should carefully evaluate him for which of the following?
Anencephaly
Trisomy 18
Renal agenesis
Duodenal atresia
Tracheoesophageal fistula
A 3-month-old infant has a history of chronic constipation. A fulminant watery diarrhea develops over a period of 2 days, and the infant is taken to the emergency department in an obviously severely dehydrated state. Plain x-ray films of the abdomen demonstrate a massively dilated transverse colon. Which of the following is the most likely diagnosis?
Meconium ileus
Necrotizing enterocolitis
Neonatal listeriosis
Newcastle syndrome
Toxic enterocolitis
A mother brings her 9-month-old daughter to the pediatrician with complaints of a rash. The mother states that the infant had a high fever [temperature up to 40.0 C (104 F)] for 3 days prior to developing the rash, but is now afebrile. The mother also says that the infant has had a runny nose and a slight cough for the past 3 days. On examination, there is a fine macular rash on the infant's trunk and neck. The examination is otherwise within normal limits, and the infant is playful and smiling. Which of the following is the most likely diagnosis?
Erythema infectiosum
Roseola
Rubella
Rubeola
Varicella
A newborn infant becomes markedly jaundiced on the second day of life, and a faint petechial eruption, first noted at birth, is now a generalized purpuric rash. Hematologic studies for hemolytic diseases are negative. Acute management should include which of the following?
Liver ultrasound
Isolation of the infant from pregnant hospital personnel
Urine drug screen on the infant
Discharge with an early follow-up visit in 2 days to recheck bilirubin
Thyroid hormone assay
A 14-year-old girl, angry at her mother for taking away her MP3 player, takes an unknown quantity of a friend’s pills. Within the first hour she is sleepy, but in the emergency center she develops a widened QRS complex on her electrocardiogram (ECG), hypotension, and right bundle branch block. The therapy you would initiate for this ingestion is which of the following?
N-acetylcysteine (Mucomyst)
Naloxone
Intensive care unit (ICU) admission, close monitoring, and possible Fab anti- body fragments
Ethanol
Deferoxamine
A 3-year-old boy of African descent is brought to your office by his stepfather because of easy bruising. He says that the child bruises easily even without trauma. The child started playing games by himself recently. He has a past history of clavicular fracture, which the stepfather attributes to a fall down a set of stairs. The history of the biological father is unknown. On examination, there is a right knee effusion with decreased range of motion, and multiple soft tissue hematomas on the thigh. What is the most appropriate diagnostic step in management?
Contact child protective services
Obtain type 1 collagen assay
Obtain prothrombin time and liver function tests
Obtain factor VIII level
Obtain bleeding time
An 8-year-old boy with sickle cell disease presents with left leg pain and a high fever. He has been refusing to walk since yesterday. On physical examination, his temperature is 39.8 C (103.6 F), blood pressure is 122/68 mm Hg, pulse is 102/min, and respirations are 20/min. His left femur is tender to palpation 3 cm above the left knee, and there is marked soft tissue swelling. A plain film of his left leg is normal. A bone scan shows increased uptake around the metaphysis of the left femur. Which of the following is the most likely pathogen?
Escherichia coli
Haemophilus influenzae
Salmonella
Staphylococcus aureus
Streptococcus pneumoniae
A 20-month-old presents to the office with a 2-day history of a harsh, barking cough. His mother states that the cough sounds like a seal. She also states he has not had any fever, although he had a runny nose earlier in the week. On examination, he is notably hoarse with inspiratory stridor. He is not drooling and is sitting on his mother's lap comfortably. The rest of his examination is within normal limits. Which of the following is the most likely diagnosis?
Acute laryngotracheobronchitis
Aspiration of foreign body in the upper respiratory tract
Epiglottitis
Laryngomalacia
Subglottic stenosis
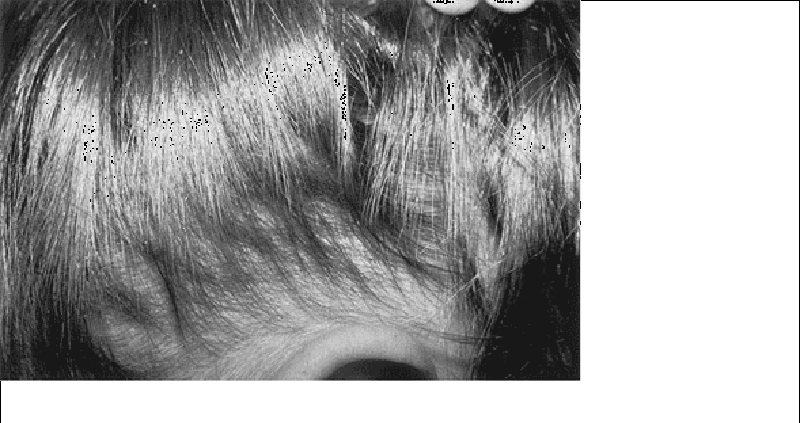
A mother arrives to the clinic with her three children (ages 2 months, 18 months, and 36 months). The 18-month-old has an intensely pruritic scalp, especially in the occipital region, with 0.5-mm lesions noted at the base of hair shafts, as shown in the picture. Which of the following therapies should be avoided in this situation?
Treatment of all household contacts with 1% lindane (Kwell)
Use of 1:1 vinegar-water rinse for hair for nit removal
Washing of all clothing and bedding in very hot water
Replacement of all commonly used brushes
Advice to the mother that treatment will again be necessary in 7 to 10 days
An infant born at term to a 22-year-old woman has a weak cry and is cyanotic at birth. His fingertips and oral mucosa appear blue. His blood pressure is 80/40 mmHg and his heart rate is 140/min. Chest x-ray shows clear lung fields bilaterally. PaO2 measured by arterial cannulation is 38 mmHg, and improves only minimally on 100% inspired oxygen. Which of the following is the best next step in managing this patient?
Loop diuretics
Packed red blood cell transfusion
Prostaglandin E1 infusion
Low dose beta-blocker
Single dose of indomethacin
An 18-year-old male undergoes elective hernia repair. During the operation, he suffers considerable blood loss, and receives a blood transfusion. He then experiences an anaphylactic transfusion reaction. He is resuscitated and further hospital course is uncomplicated. His past medical history is significant for recurrent sinopulmonary infections and intermittent episodes of diarrhea since childhood. Which of the following is the most likely cause of his symptoms?
IgA deficiency
DiGeorge Syndrome
X linked agammaglobulinemia
Wiskott-Aidrich syndrome
Cystic fibrosis
An 8-month-old previously preterm infant with bronchopulmonary dysplasia presents to the emergency department with lethargy. His regular medications include furosemide and spironolactone. His temperature is 37.4 C (99.3 F), blood pressure is 68/32 mm Hg, pulse is 110/min, and respirations are 10/min. He has poor skin turgor and dry mucous membranes. Laboratory chemistry evaluation reveals: sodium, 131 mEq/L; potassium, 3.0 mEq/L; chloride, 84 mEq/L; bicarbonate, 38 mEq/L; blood urea nitrogen, 36 mg/dL; and creatinine, 0.4 mg/dL. An arterial blood gas shows pH, 7.52; PaCO2, 49 mm Hg; and PaO2, 92 mm Hg. Which of the following is the most likely explanation for these findings?
Bartter syndrome
Primary hyperaldosteronism
Primary respiratory acidosis with metabolic compensation
Pseudohyperaldosteronism
Volume depletion
A 4-year-old girl is brought to the physician by her mother who is concerned because her child has a vaginal discharge. Starting 2 days ago, the child began scratching her vulva and complaining of burning with urination. The child is otherwise healthy and has never had a similar problem. Examination reveals normal structural anatomy for a 4-year-old girl. There is no evidence of atrophy. There is an inflammatory erythema on the medial aspects of the labia majora and excoriations. There is a mucous discharge with a few flecks of blood intermixed. Which of the following is the most likely cause of a vaginal discharge in this patient?
Lichen sclerosis
Pelvic inflammatory disease
Sarcoma botyroides (embryonal rhabdomyosarcoma)
Sexual abuse
Vaginal foreign body
A 1-year-old child presents with failure to thrive, frequent large voids of dilute urine, excessive thirst, and three episodes of dehydration not associated with vomiting or diarrhea. Over the years, other family members reportedly have had similar histories. Which of the following is the most likely diagnosis?
Water intoxication
Diabetes mellitus
Diabetes insipidus
Child abuse
Nephrotic syndrome
A 6-month-old infant has poor weight gain, vomiting, episodic fevers, and chronic constipation. Laboratory studies reveal a urinalysis with a pH of 8.0, specific gravity of 1.010, 1+ glucose, and 1+ protein. Urine anion gap is normal. Serum chemistries show a normal glucose and a normal albumin with a hyperchloremic metabolic acidosis. Serum phosphorus and calcium are low. What is the best diagnosis to explain these findings?
Renal tubular acidosis type 1
Renal tubular acidosis type 3
Renal tubular acidosis type 4
Hereditary Fanconi syndrome
Congenital nephrotic syndrome
A 2-year-old girl is taken to a pediatrician because she has developed a rash and seems unusually unsteady when she tries to walk. Physical examination demonstrates a diffuse rash on body parts exposed to sun. Also noted are short stature, possible mental retardation, and ataxia. Screening studies demonstrate increased total amino acids in the urine. Which of the following is the most likely diagnosis?
Cystinuria
Alkaptonuria
Hartnup disease
Fanconi syndrome
Phenylketonuria
A 24-month-old girl is brought to the pediatrician's office for evaluation because her mother noticed a yellowish discharge on the girl's underwear for the past 3 days. She had no fever, but her mother said she has been fussier recently. On physical examination, the girl is appears excessively anxious about contact with the physician. Her introitus is inflamed, and the hymeneal edge is jagged at the 8 o'clock position. A vaginal culture is taken. Which of the following organisms, if isolated from the vaginal vault, would constitute the most definitive evidence of sexual abuse?
Candida albicans
Chlamydia trachomatis
Gardnerella vaginalis
Pseudomonas aeruginosa
Neisseria gonorrhoeae
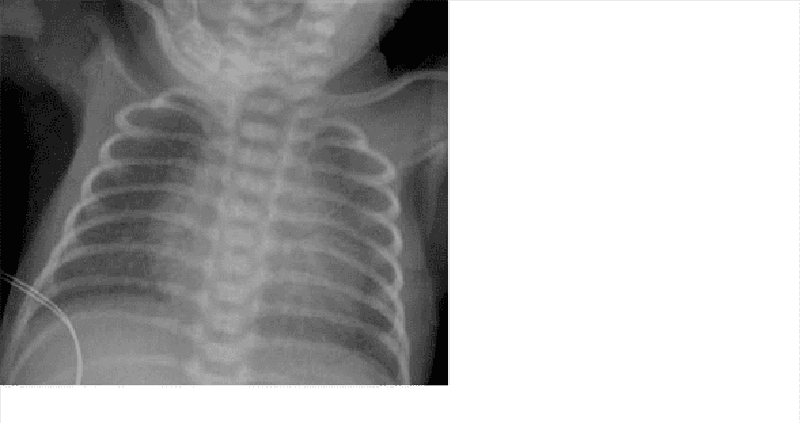
You are called to the delivery room to evaluate an infant born at 28-weeks gestational age. The infant is tachypneic and cyanotic. Examination reveals intercostal and subcostal retractions along with nasal flaring. Lungs have coarse breath sounds bilaterally. After initial resuscitation, the patient is given respiratory support with continuous positive airway pressure and admitted to the neonatal intensive care unit. The patient's respiratory status continues to worsen over the next 24 hours. A chest radiograph from the patient is shown below. In addition to prematurity, which of the following is a risk factor for the development of this disease?
Prolonged rupture of membranes
Intrauterine growth restriction
Maternal diabetes
Maternal hypertension
Antenatal corticosteroids
A 10-year-old boy, the star pitcher for the Salt Lake City Little League baseball team, had a sore throat about 2 weeks ago but did not tell anyone because he was afraid he would miss the play-offs. Since several children have been diagnosed with rheumatic fever in the area, his mother is worried that he may be at risk as well. You tell her that several criteria must be met to make the diagnosis but the most common finding is which of the following?
Carditis
Arthralgia
Erythema marginatum
Chorea
Subcutaneous nodules
You are asked to evaluate an infant born vaginally 3 hours previously to a mother whose only pregnancy complication was poorly controlled gestational diabetes. The nursing staff noticed that the infant was breathing abnormally. On examination, you find that the infant is cyanotic, has irregular, labored breathing, and has decreased breath sounds on the right side. You also note decreased tone in the right arm. You provide oxygen and order a stat portable chest radiograph, which is normal. Which of the following studies is most likely to confirm your diagnosis?
Nasal wash for viral culture
Fiberoptic bronchoscopy
Chest CT
Chest ultrasound
Induced sputum culture
A 6-year-old female is brought to the physician with a rash and joint pains. Her mother reports that she has been previously healthy except for a sore throat a few weeks ago. One week ago, the patient developed pain in her knees. The knee pain resolved after a few days, but now her ankles and wrists are tender. She has also developed a pink rash on her trunk that is non-pruritic. Vital signs are temperature 38.3 0c (101 0F), pulse 85/min, and respiratory rate 20/min. On examination, there is pain and stiffness during manipulation of the wrists and ankles. A faint, erythematous, centrifugal rash on her trunk and proximal limbs is present. Laboratory studies show: Complete blood count Hemoglobin 12.5 g/dL MCHC 32% MCV 85 fl Reticulocyte count 0.1% Platelet count 200,000/mm3 Leukocyte count 6,500/mm3 Neutrophils 56% Eosinophils 1% Lymphocytes 33% Monocytes 10% C-reactive protein 3.5 mg/dL Erythrocyte sedimentation rate 38 mm/hr Which of the following is the most likely diagnosis?
Juvenile rheumatoid arthritis
Rheumatic fever
Acute lymphoblastic leukemia
Systemic lupus erythematosus
Fibromyalgia
A 14-year-old African-American girl presents to the ER with a mild fever and severe right-sided thigh pain. She is agitated and requests quick pain relief. Her heart rate is 120/min and blood pressure is 120/70 mmHg. She says that she had a similar episode one year ago and was placed in the hospital for intravenous pain management. Her brother had similar episodes and died of an infection at 10 years of age. Which of the following would you most expect to see on this patient's peripheral blood smear?
Burr cells
Polycythemia
Reticulocytosis
Iron deficiency
Hypersegmented neutrophils
A 9-year-old African-American boy is brought to ER with high fever, poor appetite, and irritability. His heart rate is 140/min and his blood pressure is 80/60 mmHg. He has been hospitalized several times before for poorly localized abdominal pain. He also has a history of hematuria. The boy has not received several routine vaccinations because his mother is afraid that they will cause autism. His hematocrit is 22% and the reticulocyte count is 12%. The patient dies several hours after the admission. This patient's death may have been prevented by:
Folic acid supplementation
Vaccination with a live attenuated virus
Vaccination with a bacterial toxoid
Vaccination with a conjugate capsular polysaccharide
Periodic blood transfusions
A 10-month-old infant has poor weight gain, a persistent cough, and a history of several bouts of pneumonitis. The mother describes the child as having very large, foulsmelling stools for months. Which of the following diagnostic maneuvers is likely to result in the correct diagnosis of this child?
CT of the chest
Serum immunoglobulins
TB skin test
Inspiratory and expiratory chest x-ray
Sweat chloride test
A 3-year-old girl is admitted with the x-ray shown below. The child lives with her parents and a 6-week-old brother. Her grandfather stayed with the family for 2 months before his return to the West Indies 1 month ago. The grandfather had a 3-month history of weight loss, fever, and hemoptysis. Appropriate management of this problem includes which of the following?
Bronchoscopy and culture of washings for all family members
Placement of a Mantoux test on the 6-week-old sibling
Isolating the 3-year-old patient for 1 month
Treating the 3-year-old patient with isoniazid (INH) and rifampin
HIV testing for all family members
A previously healthy 18-month-old male comes to the physician for evaluation of fever. His mother reports that he has had a fever ranging from 1 02.2 0F (39.0 0c) to 104.0 0F (40.0 0c) for the past five days. He has also become increasingly irritable with decreased appetite. His mother reports that he does continue to take some liquids. There are no known sick contacts. On examination, the infant's temperature is 1 02.5 0F (39.2 0C), pulse is 120/min, and respiratory rate is 20/min. He is irritable during the examination. There is conjunctival erythema bilaterally, with serous drainage from both eyes. His oropharynx is erythematous and his lips are fissured. There is a 2 cm anterior cervical lymph node palpable on the right side. His neck is otherwise supple and he is able to flex his chin to his chest without difficulty. There is mild abdominal tenderness to palpation. His hands and feet are slightly erythematous and edematous and there is a maculopapular rash on the trunk. Which of the following is the most likely diagnosis?
Scarlet fever
Staphylococcal scalded skin syndrome
Toxic shock syndrome
Kawasaki disease
Rocky Mountain spotted fever

You are seeing a 4-year-old girl with the physical examination finding shown below. She has no significant past history. The most appropriate management is which of the following?
Surgical consultation for correction
Topical estrogen cream daily for a week
Topical steroid cream for a week
Referral to social services for possible sexual abuse
Karyotypestudies
At the 2-week checkup of a term female infant, the mother reports a grayish and sometimes bloody vaginal discharge since birth. The infant’s mother and grandmother are the only caretakers. Examination of the external genitalia reveals an intact hymen with a thin grayish mucous discharge. Which of the following is the most appropriate next step?
Parental reassurance
MRI of the brain
Ultrasound of the abdomen
Gonorrhea and chlamydial swabs
Referral to social services for possible sexual abuse
A 4196 g (9 lb 4 oz) infant is delivered via vaginal delivery to a 31 -year-old mother with gestational diabetes. The delivery was complicated by shoulder dystocia. He is taken to the newborn nursery where his initial plasma glucose level is 20 mg/dL. The initial spun hematocrit is 65%. Which of the following congenital anomalies is this baby most likely to have?
Aniridia
Cleft palate
Macroglossia
Omphalocele
Small left colon
A 2-week-old infant is brought to the office for a newborn visit. His mother states that the he has been a very slow eater and that he is constipated, not having had a bowel movement in 3 days. On physical examination, the infant has poor muscle tone, an enlarged tongue, an umbilical hernia, an enlarged anterior fontanelle, and hypothermia. He also looks slightly jaundiced, with slightly dry skin and brittle hair. Which of the following is the most likely diagnosis?
Beckwith-Wiedemann Syndrome
Congenital hypothyroidism
Hurler syndrome
Trisomy 21
Turner syndrome
A 4-year-old male is brought to the physician with fever and headache. His symptoms began two days ago with low-grade fever, cough, and congestion. Last night, he developed a temperature of 102 F (38.9 C) and became fussy and less active. Today, he is crying and complaining of a headache. His parents report that he has vomited twice today. In the office, his temperature is 102.5 F (39.o c), pulse is 110/min, and respiratory rate is 20/min. On examination, he is irritable and shows signs of photophobia. His oropharynx is erythematous. Nuchal rigidity is present and when the neck is flexed, the patient flexes his lower extremities. The remainder of the physical examination is normal. Lumbar puncture is performed and the results are shown below. CSF Glucose 60 mg/dL Protein 80 mg/dL RBC 10/mm3 WBC 100/mm3 Neutrophils 10% Lymphocytes 70% Monocytes 20% Gram stain negative Which of the following organisms is most likely responsible for this patient's presentation?
Streptococcus pneumoniae
Mycobacterium tuberculosis
Epstein-Barr virus
Neisseria meningitidis
Echovirus
A 12-year-old boy is brought to the emergency department with a temperature of 39.1 C (102.4 F) at home, difficulty speaking, and odynophagia for 2 days, Physical examination reveals marked erythema of the right tonsil pillar and edema of the uvula with deviation to the left. In addition to anaerobic bacteria, which of the following organisms is most likely to be isolated from a tonsillar pillar aspirate?
Beta-hemolytic Streptococcus
Enterococcus
Haemophilus influenzae type b
Staphylococcus aureus
Streptococcus pneumonia
A neonate is noted to have many abnormalities, a number of which are located in the midline. The infant has cleft lip and cleft palate. His eyes are very small and have fissures of the iris, shallow supraorbital ridges, and slanted palpebral fissures. He is deaf, and the ears are low set and malformed. Each hand has six fingers and a simian crease. Which of the following congenital abnormalities of the brain is particularly likely to be present in this infant?
Anencephaly
Encephalocele
Hydranencephaly
Holoprosencephaly
Porencephaly
A 4-year-old boy, recently adopted through an international adoption service, is noted to have intermittent watery diarrhea, nausea, belching, and abdominal pain. His weight is less than the fifth percentile for his age. Which of the following studies would be most helpful in making the diagnosis?
CBC and differential
ESR
Abdominal ultrasound
Liver function studies
Stool microscopy for ova and parasites
A 5-month-old child regularly regurgitates a large portion of her feeds. A pH probe study showed significant periods of low esophageal pH. The child has normal growth and no other significant past medical history. Which of the following is the best management at this point?
Barium swallow and upper GI series
Oral reflux medications
Esophageal manometry
Close observation only
Surgical correction with fundoplication
A 7 -year-old boy is brought to your office with a mild fever and neck swelling. His mother says that the boy has been complaining of neck pain for a couple of days and she noticed a tender neck lump yesterday. All of his vaccinations are up-to-date. He has no known allergies. Physical examination reveals a tender and fluctuant anterior cervical mass. Which of the following is the best medication for this patient?
Penicillin
Amoxicillin
Dicloxacillin
Erythromycin
Acyclovir
A 21-year-old female, G1P0, who recently emigrated from Zimbabwe presents for prenatal counseling in her 34th week of pregnancy. She received no prenatal care. Ultrasound evaluation reveals lower-than-normal fetal length and markedly reduced fetal head size. Which of the following could have prevented this condition?
Folic acid supplementation
MMR vaccination
Zidovudine treatment
Malaria prophylaxis
Smoking cessation
A 4-week-old infant presents with tachycardia, tachypnea, and poor weight gain. His arterial blood gas shows a pH of 7.34, a PaCO2 of 41 mm Hg, and a PaO2 of 74 mm Hg. A chest radiograph shows cardiomegaly. Echocardiography reveals a structurally normal heart, left ventricular dilatation, a left ventricular ejection fraction of 20%, and mild mitral and tricuspid regurgitation. IV administration of which of the following medications is the best initial step in management of this patient?
Angiotensin-converting enzyme inhibitor
Corticosteroid
Digoxin
Epinephrine
Furosemide
A 12-year-old child is brought to his pediatrician for a routine health maintenance visit. He has been well except for occasional attacks of asthma and has met all development milestones. His immunizations are up to date. He occasionally uses theophylline for his asthma. Physical examination is remarkable for a blood pressure of 150/90 mm Hg in both arms. Which of the following is the most likely cause of his hypertension?
Chronic lung disease
Coarctation of the aorta
Congenital heart disease
Renal disease
Theophylline toxicity
One of your asthmatic patients arrives for a checkup. The mother reports that the child seems to need albuterol daily, especially when exercising, and she has coughing fits that awaken her from sleep about twice a week. Her grandmother had recommended a Chihuahua as a “cure” for her asthma, but her mother has seen no difference since the arrival of the pet. Appropriate treatment measures would include which of the following?
Short-acting, inhaledβ-agonists, as needed
Daily leukotriene modifier with short-acting β-agonist
Inhaled nedocromil with short-actingβ-agonists
Medium-dose, inhaled corticosteroids with short-acting β-agonists
High-dose, inhaled corticosteroids with theophylline and short-actingβ- agonists
An infant is brought to the office for health maintenance visit. On examination, the infant turns when her name is called. She is able to say "mama." Her mother mentions that she also says "dada" at home. She is able to look for her mother when she gets frightened. She also waves bye-bye to the doctor when the doctor steps out of the examination room. What age of this child is most consistent with these developmental milestones?
3 months
5 months
7 months
9 months
11 months
A 3-month-old infant is brought to the emergency department for severe vomiting over the past 6 hours. The mother tells the physician that she has vomited at least 4 times during this period. She also noticed the infant was having difficulty feeding for 2 days. On examination, she is very fussy, and there is a swelling over the left side of the head. CT of the head shows a skull fracture of the left parietal bone with no evidence of intracranial damage. The mother explains that the baby rolled off the sofa onto the floor yesterday. Which of the following is the most appropriate next step in management?
Discharge the patient home with instructions concerning post-concussion symptoms
Monitor the infant for 12 hours for signs of increased intracranial pressure, discharge the patient home if asymptomatic thereafter
Obtain a neurosurgical consultation for the skull fracture
Obtain a skeletal survey
Repeat the CT scan of the head in 24 hours
A 5-year-old boy is brought to the emergency department due to general malaise and a swollen scrotum. His mother noticed the swollen scrotum today, and is sure that "it was not there yesterday." He had a low-grade fever and a cough two weeks ago, and "hasn't been himself ever since." He has no significant past medical history. On examination, he looks ill and lethargic. He has palpable purpura on his buttocks and lower legs. He has a swollen right scrotum which is slightly tender to palpation, and his abdomen is moderately tender to palpation. Urinalysis reveals the presence of a small amount of blood and protein. He is subsequently admitted for observation. Which of the following adverse outcomes is he most likely to develop?
Appendicitis
Cholecystitis
Volvulus
Intussusception
Diverticulitis
A term neonate develops apnea, tachypnea, and seizures in the first 2 hours of life. The infant is large for gestational age and appears obese. Physical examination is otherwise unremarkable. Serum studies demonstrate a blood glucose level of 30 mg/dL. The mother most likely has which of the following conditions?
Diabetes mellitus
Emphysema
Hepatic cirrhosis
Hyperthyroidism
Rheumatoid arthritis
You receive a call from the parents of a 1 year old who is due for his well-child visit next week. They have just received a letter from their daycare center that an employee has hepatitis A. Which of the following is the best treatment plan?
Give hepatitis A immune globulin and hepatitis A vaccine
Treat with hepatitis A immune globulin.
Obtain hepatitis A serology and give hepatitis A vaccine.
Give hepatitis A vaccine.
No treatment is needed.
A 4-year-old child was brought in for evaluation of sleep problems. He cried and screamed within an hour of falling asleep. He seemed disoriented and confused; he did not seem aware of his parents’ presence. They were unable to arouse him to comfort him. This resolved spontaneously, and he had no recollection of the event the next morning. You informed the parents that he was most likely experiencing which of the following?
Nightmares
night terrors
Somnambulism
Somniloquy
Somniloquy
Varicella vaccination is a live virus vaccine. It is generally not recommended in immunocompromised patients. Which of the following is an exception to this rule?
Children on high doses of corticosteroids
Leukemia in inducton therapy
Lymphoma
Congenital T-cell abnormalities
Leukemia in remission for >1 year and a normal lymphocyte count
A male infant was found to be jaundiced 12 hours after birth. At 36 hours of age, his serum bilirubin was 18 mg/dL, hemoglobin concentration was 12.5 g/dL, and reticulocyte count 9%. Many nucleated RBCs and some spherocytes were seen in the peripheral blood smear. The differential diagnosis should include which of the following?
Pyruvate kinase deficiency
Hereditary spherocytosis
Sickle-cell anemia
Rh incompatibility
Polycythemia
On a routine well-child examination, a 1-year-old boy is noted to be pale. He is in the 75th percentile for weight and the 25th percentile for length. Results of physical examination are otherwise normal. His hematocrit is 24%. The answer to which of the following questions is most likely to be helpful in making a diagnosis?
What is the child’s usual daily diet?
Did the child receive phototherapy for neonatal jaundice?
Has anyone in the family received a blood transfusion?
Is the child on any medications?
What is the pattern and appearance of his bowel movements?
A parent brings in a 5-year-old boy being treated for acute lymphocytic leukemia (ALL). He states a friend who is staying with them at their home has just come down with chicken pox. Your patient has not had chicken pox or received immunization with varicella vaccine. What is the appropriate treatment?
Acyclovir given IV
Varicella vaccine
Varicella immune globulin (VZIG)
Varicella vaccine and VZIG
Acyclovir given IV for 7 days, varicella vaccine, and VZIG
A young mother claims that her 4-week-old child sleeps best on his stomach. You tell her that the safest sleep position for infants is which of the following?
On the back
On the stomach
On the side
On the back with the head elevated by a pillow
In the parents’ bed
A 4-year-old boy is seen in the office for a general check-up. The child appears well nourished and has normal developmental milestones. His temperature is 36.6 C (98 F), pulse rate is 80/min, and blood pressure is 110/70 mmHg. On abdominal palpation, there is a lobular right-sided flank mass, and the kidneys are palpable bilaterally. What is the most likely cause of the flank mass in this child?
Tumor originating from the metanephros
Malignancy of neural crest cells
Polycystic kidney disease, infantile type
Renal cell carcinoma, embryonal variant
Acquired renal cystic disease
A 12-year-old boy is brought to the office by his mother due to a two-week history of generalized edema which is gradually progressing. His past medical history is insignificant. He is not taking any medications. His blood pressure is 110/80 mmHg, pulse is 85/min, respirations are 18/min, and temperature is 36.7C (98F). The laboratory findings are as follows: Serum sodium 140 mEq/L Serum potassium 3.7 mEq/L Serum albumin 2.1 g/dl Serum globulin 6.0 g/dl Serum creatinine 1.0 mg/dl Urinalysis reveals proteinuria 3+. What is the best next step in the management of this patient?
Renal biopsy
Scintigraphy
Intravenous pyelography (IVP)
Prednisone
Prednisone and cyclophosphamide

A 2-year-old child in shock has multiple nonblanching purple lesions of various sizes scattered about on the trunk and extremities; petechiae are noted, and oozing from the venipuncture site has been observed. The child’s peripheral blood smear is shown below. Clotting studies are likely to show which of the following?
Increased levels of factor V and VIII
A decreased prothrombin level
An increased fibrinogen level
The presence of fibrin split products
Normal partial thromboplastin time (PTT)
A 10-year-old boy is admitted to the hospital because of bleeding. Pertinent laboratory findings include a platelet count of 50,000/L, prothrombin time (PT) of 15 seconds (control 11.5 seconds), activated partial thromboplastin time (aPTT) of 51 seconds (control 36 seconds), thrombin time (TT) of 13.7 seconds (control 10.5 seconds), and factor VIII level of 14% (normal 38%-178%). Which of the following is the most likely cause of his bleeding?
Immune thrombocytopenic purpura (ITP)
Vitamin K deficiency
Disseminated intravascular coagulation (DIC)
Hemophilia A
Hemophilia B
A 5-month-old boy is brought to the office for a mass in his left groin area. The infant is on the examination table, quietly sucking on his pacifier. On examination, there is a fluidfilled sac that does not reach the inguinal ring and transilluminates well. Which of the following is the most likely diagnosis?
Hematoma
Hydrocele
Inguinal hernia
Testicular torsion
Testicular tumor
A 9-year-old girl is brought to the clinic with complaints of fatigue, abdominal pain and low grade fever. Four days ago her mother noticed a red rash on the tops of her daughter's feet, which has now spread to her thighs and buttocks. The rash was initially small red dots, but has now become patches. Her daughter subsequently developed periumbilical, cramping, abdominal pain. Review of systems is positive only for a respiratory viral illness three weeks ago. Her temperature is 37.7 C (99.8 F), pulse is 96/min, and respirations are 18/min. Abdominal examination is remarkable for tenderness to palpation near the umbilicus, but the abdomen is otherwise soft, with no rebound or guarding, and no organomegaly. Raised, palpable purpuric lesions are present on the buttocks and thighs. The ankles are tender and edematous bilaterally. Complete blood count reveals a leukocyte count of 9,000/mm3. Her hemoglobin 12. 6 g/dL, and platelets are 325,000/mm3. Serum electrolytes are normal. Which of the following is her urinalysis most likely to reveal?
Elevated levels of copper
Glucosuria
Red blood cells
White blood cell casts
Yeast
A 17-year-old adolescent comes to your office seeking help for “ heavy” menses. Your review of systems also reveals weekly epistaxis. Her only significant past history includes a tonsillectomy at age 6 after which she required blood transfusion for excessive bleeding. Her family history includes several people who seem to bleed and bruise more easily than others. The patient’s mother required a hysterectomy after child birth for excessive hemorrhage. You order a variety of laboratory tests. The patient has a hemoglobin of 6.5 mg/dL with an MCV of 60%; her platelet count is 350,000/L. Her von Willebrand antigen and her von Willebrand factor (vWF) activity (ristocetin cofactor activity) are decreased. Her vWF is reported as normal but in decreased amounts. You have been unable to reach her to report the findings, but when she calls about 1 week later she reports she is having a mild to moderate nosebleed. You initiate therapy with which of the following?
Aminocaproic acid (Amicar)
VWF concentrate alone
VWF with factor VIII
Desmopressin (DDAVP)
Intravenous immunoglobulin (IVIG)
A 6-month-old infant is taken to the emergency department because he had a seizure. Physical examination demonstrates premature closure of cranial sutures and markedly bowed legs. Laboratory studies demonstrate low serum phosphate levels, with normal vitamin D and parathyroid hormone levels. Urinalysis shows high phosphate levels, but no increased excretion of glucose, amino acids, or protein. The child's maternal grandfather had crippling bone disease, and his mother has mild bowing of the legs. Which of the following is most likely diagnosis?
Fanconi syndrome
Hypophosphatemic rickets
Osteogenesis imperfecta
Osteomalacia
Paget disease of bone
A 2-year-old girl is brought to the emergency department with a fever, chills, poor appetite, and vomiting. On examination, she is irritable and diaphoretic. Her temperature is 39.2 C (102.5 F), blood pressure is 80/48 mm Hg, pulse is 88/min, and respirations are 17/min. She is tender at the left costovertebral angle. Initial laboratory tests show the following: Leukocyte count 16,300/mm3 Hemoglobin 12.5 g/dL Platelet count 245,000/mm3 Blood urea nitrogen 6 mg/dL Creatinine 0.5 mg/dl Urinalysis is positive for leukocyte esterase and nitrite, with 150 white blood cells/hpf. After TV antibiotic administration and stabilization, what is the most appropriate diagnostic study?
CT of the abdomen and pelvis
IV pyelography
Plain abdominal radiography
Radionuclide imaging of the kidneys
Voiding cystourethrography
An 8-year-old male presents to the emergency department with decreased mental status. His mother states that she has noticed he has been drinking and urinating more frequently over the past several weeks. He was hard to wake up this morning and complained of abdominal pain. Physical examination reveals an afebrile drowsy male with clear airways and mild tachycardia. Mucous membranes are dry and his lips are cracked. His abdomen is mildly tender to palpation diffusely, but there is no rebound or guarding. Laboratory evaluation reveals a glucose of 560 mg/dL and potassium of 5.9 mEq/L.An arterial blood gas analysis reveals a pH of 7.18. A urinalysis is positive for ketones and glucose. CT scan of the abdomen is normal. A chest x-ray film is clear. Two hours after initiation of treatment the physician adds potassium to the patient's IV fluids. Which of the following best explains this therapeutic decision?
Acidosis causes extracellular depletion of potassium
Hyperglycemia causes potassium to shift to the extracellular space
Hyperkalemia will protect the patient against dysrhythmias
Hypokalemia will result as acidosis is corrected
Potassium should not have been added to the IV fluids
An 8-month-old girl is brought to the clinic for a well-baby checkup. Her antenatal and birth histories are unremarkable. Her vital signs are stable, and all developmental milestones are appropriate. On examination, a head tilt is noted. Ophthalmoscopic examination reveals a red reflex and normal corneal light reflex. The cover test reveals moderate esodeviation of the left eye. What is the most appropriate next step in the management of this patient?
Continuous covering of the normal eye
Continuous covering of the deviated eye
Prompt surgical correction
Measurement of intraocular pressure
Watchful waiting
A 6-year-old girl is brought to the office for the evaluation of "passing smoky urine." She recently had a sore throat. Her blood pressure is 150/100 mmHg. There is swelling of the face and extremities. Urinalysis reveals many red blood cells, red blood cell casts and 1 + proteinuria. Her serum C3 level and CH 50 are low. Her C4 1evel is normal. Her antistreptolysin-a (ASO) titer is 1,024 Todd units (normal ≤ 166 Todd units). In this patient, which of the following abnormal findings is most likely to become normal within 8 to 12 weeks?
ASO titer
Complement level
Hematuria
Proteinuria
Bacteremia
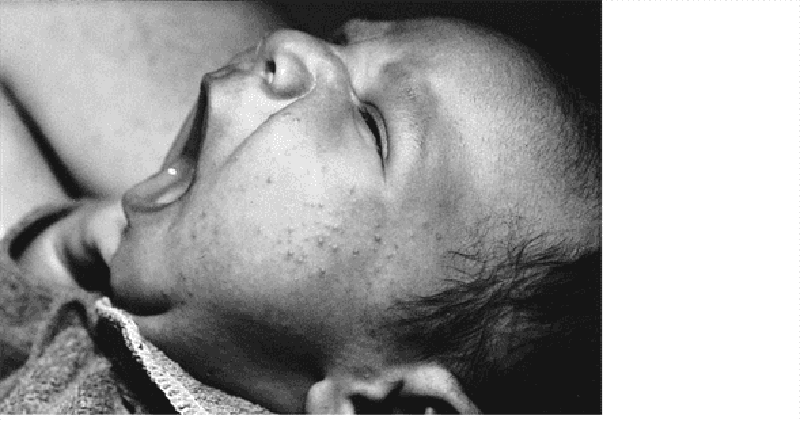
The mother of a 3-day-old infant brings her child to your office for an early follow-up visit. The mom notes that the child has been eating well, has had no temperature instability, and stools and urinates well. She notes that over the previous 3 days the child has had a progressive rash on the face as pictured here. Which of the following is the most likely diagnosis?
Herpes
Neonatal acne
Milia
Seborrheic dermatitis
Eczema
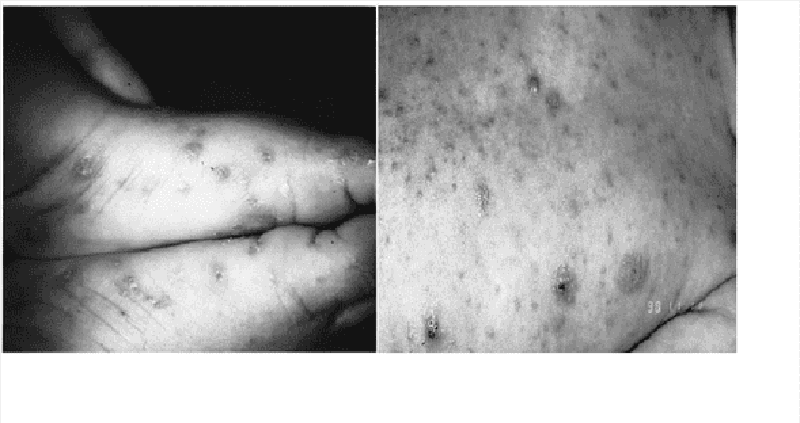
A 2-year-old child (A) presents with a 4-day history of a rash limited to the feet and ankles. The papular rash is both pruritic and erythematous. The 3-month-old sibling of this patient (B) has similar lesions also involving the head and neck. The most appropriate treatment for this condition includes which of the following?
Coal-tar soap
Permethrin
Hydrocortisone cream
Emollients
Topical antifungal cream
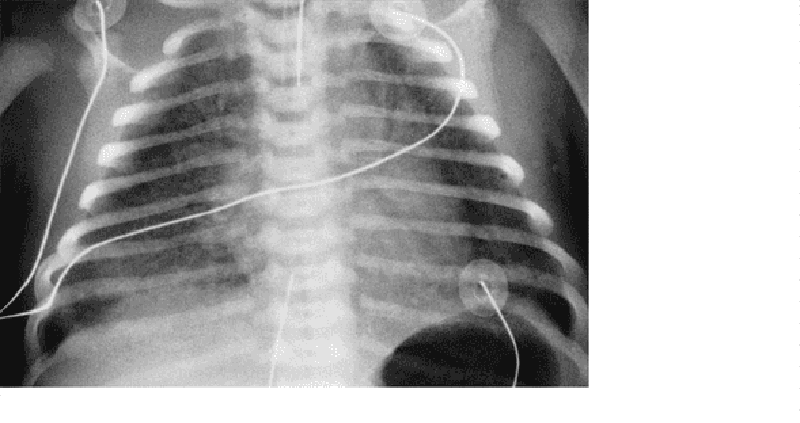
An 8-hour-old infant develops increased respiratory distress, hypothermia, and hypotension. A complete blood count (CBC) demonstrates a white blood cell (WBC) count of 2500/μL with 80% bands. The chest radiograph is shown below. Which of the following is the most likely diagnosis?
Congenital syphilis
Diaphragmatic hernia
Group B streptococcal pneumonia
Transient tachypnea of the newborn
Chlamydial pneumonia
A 3-year-old child is taken to a pediatrician because he develops burning pain, erythema, and swelling minutes after being exposed to the sun. Physical examination demonstrates erythema with swelling of the hands and arms. The skin is thickened on the backs of the hands but does not show blistering or scarring. Which of the following is the most likely diagnosis?
Acute intermittent porphyria
Erythropoietic protoporphyria
Hepatoeryfhropoietic porphyria
Porphyria cutanea tarda
Variegate porphyria
A 16-year-old girl has had a fever, vomiting, and watery diarrhea for the past 24 hours. She also complains of intermittent abdominal pain and generalized myalgia. On examination, she is slightly lethargic. Her temperature is 39.4 C (103 F), blood pressure is 75/50 mm Hg, and pulse is 150/min. Her conjunctivae and pharynx are hyperemia. She has a generalized erythematous maculopapular rash that spares the wrists. Which of the following will be the most appropriate treatment?
Amantadine
Gentamicin
Ketoconazole
Nafcillin
Prednisone
An 8-month-old infant, who is up-to-date with his immunizations, is brought to the clinic by his mother. The mother states that she overheard other mothers talking about a varicella vaccination that their children have received. She does not want her son to have the chickenpox virus and therefore, wants him to receive the vaccine today. The physician explains that the infant has not yet reached the recommended age for the vaccine. If this visit is in November, when is the earliest that this patient can return for the varicella vaccine?
February
March
April
May
June
An 11-year-old girl is brought to the office by her mother due to headaches for the last 4 hours. The headaches are bifrontal, and are accompanied by nausea, vomiting, and sensitivity to light and noise. It is her second episode, and both episodes were preceded by dark spots in her visual field. The first episode was 2 weeks ago. She doesn't report any numbness or tingling in her extremities, and no behavioral change or decline in school performance was noted. Her vital signs are stable, and she is afebrile. The physical examination is normal. What is the most appropriate next step in the management of this patient?
Reassurance and acetaminophen
Lumbar puncture
CT scan of the head
MRI of the brain
Electroencephalogram
A previously healthy one-year-old child is brought to the physician for a routine wellness visit. Her parents report that she drinks six glasses of whole milk a day, but is a very picky eater. She is developmentally appropriate. Her parents are concerned that she might be anemic because she frequently eats ice and sometimes dirt. On examination, her temperature is 88.6F (37 C), pulse is 118/min, and respiratory rate is 21 /min. Her height and weight are both at the 50th percentile for her age. She appears well nourished and her physical examination is unremarkable. Laboratory findings include the following. Complete blood count Hemoglobin 10.5 g/dL MCV 70 fl Reticulocytes 1.0% Platelets 250,000/mm3 Leukocyte count 6,500/mm3 Neutrophils 56% Lymphocytes 33% Monocytes 10% Which of the following is the most appropriate next step in the management of this child?
Hemoglobin electrophoresis
Colonoscopy
Serum creatinine
Oral iron therapy
Blood transfusion
An inner city family has been using a neighbor to care for their 3-year-old child while the parents work. The neighbor is diagnosed with pulmonary tuberculosis. PPD test of the 3- year-old is negative. Which of the following is indicated for the 3-year-old?
Ethambutol chemoprophylaxis
Isoniazid chemoprophylaxis
Rifampin chemoprophylaxis
Streptomycin chemoprophylaxis
No chemoprophylaxis
A 7 -year-old male child is brought to the office due to decreased urine output and lethargy for the past week. His birth and past medical histories are insignificant. His immunizations are up-to-date. Examination reveals no abnormalities. His BUN and creatinine levels are elevated. What is the most appropriate next step in the management of this patient?
Abdominal USG
Intravenous pyelogram
Urinalysis
CT scan of abdomen
Urine culture
A 7 -day-old male infant is brought by his mother complaining of decreased movements of his right arm. She denies any trauma or fall. Pregnancy was uneventful, but delivery was complicated with shoulder dystocia. Examination reveals the presence of crepitus and bony irregularity over the clavicular area and Mora reflex is absent on the right. Which of the following is the most appropriate management?
Reassurance
Figure-of-eight clavicle strap
Passive and active motion exercises
Nerve grafting
Casting of the right arm and shoulder
An infant born at 35 weeks’ gestation to a mother with no prenatal care is noted to be jittery and irritable, and is having difficulty feeding. You note coarse tremors on examination. The nurses report a high-pitched cry and note several episodes of diarrhea and emesis. You suspect which of the following?
Fetal alcohol syndrome
Prenatal exposure to marijuana
Heroin withdrawal syndrome
Cocaine exposure in utero
Tobacco use by the mother
A previously healthy full-term infant has several episodes of duskiness and apnea during the second day of life. Diagnostic considerations should include which of the following?
Hemolytic anemia
Congenital heart disease
Idiopathic apnea
Harlequin syndrome
Hyperglycemia
A 3-year-old girl is brought to the pediatrician with complaints of abdominal pain and fever. Her mother states that the fever started 2 days ago, with the highest temperature being 39.0 C (102.2 F). She has had no vomiting or diarrhea. The mother states that her daughter has been complaining of pain on urination. On examination, she is tender in her lower abdomen, and there is some right-sided costovertebral angle tenderness. A urinalysis confirms the suspicion of a urinary tract infection. Which of the following would be the most appropriate diagnostic procedure?
Cystoscopy
Dimercaptosuccinic acid (DMSA) scan in 1 -2 months
Intravenous pyelogram
Voiding cystourethrogram (VCUG) now
VCUG in 1 -2 months
A very concerned mother brings a 2-year-old child to your office because of two episodes of a brief, shrill cry followed by a prolonged expiration and apnea. You have been following this child in your practice since birth and know the child to be a product of a normal pregnancy and delivery, to be growing and developing normally, and to have no chronic medical problems. The first episode occurred immediately after the mother refused to give the child some juice; the child became cyanotic, unconscious, and had generalized clonic jerks. A few moments later the child awakened and had no residual effects. The most recent episode (identical in nature) occurred at the grocery store when the child’s father refused to purchase a toy for her. Your physical examination reveals a delightful child without unexpected physical examination findings. Which of the following is the most likely diagnosis?
Seizure disorder
Drug ingestion
Hyperactivity with attention deficit
Pervasive development disorder
Breath-holding spell
You are called to examine a 2-day old male infant due to difficulty in feeding. He becomes cyanotic and short of breath when he feeds, but turns pink when he cries. His prenatal, birth and family histories are unremarkable. His vital signs are normal. Chest auscultation is normal. His peripheral pulses are full and symmetric. What is the most likely diagnosis?
Cyanotic heart disease
Acyanotic heart disease with left-to-right shunt
Choanal atresia
Transient tachypnea of the newborn
Laryngomalacia
A 3-week-old female is brought into the emergency department with a fever and irritability. She was born after a normal pregnancy and delivery. Her mother had routine prenatal care and has no history of sexually transmitted infections. The infant's mother is 14 years old and the father is 17 years old. They are not married, and the father is not involved in the care of the infant. The infant lives with her mother and maternal grandparents at the maternal grandparents' home. You are concerned about meningitis and decide to do a lumbar puncture. The mother and maternal grandparents are present in the emergency department. Informed consent should be obtained from which of the following individuals?
Mother
Maternal grandparents since the mother is a minor
Mother and father must both provide consent
Mother and grandparents since the mother is a minor
Informed consent is not necessary because the mother is a minor
You are seeing a 2-year-old child, brought by his father for a well-child examination. In providing age-appropriate anticipatory guidance, you should tell him which of the following?
He should set his water heater to 71°C (160°F) to ensure the sterility of dishes and clothes, thereby decreasing the risk of infections.
Milk should be switched from whole to skim or low fat
Continue rear facing car seats
Purchase a bed alarm to assist with the child’s nocturnal enuresis.
Teach the child to swim so that the parents have the ability to allow the child to be alone in pools.
A child can walk well holding on to furniture but is slightly wobbly when walking alone. She uses a neat pincer grasp to pick up a pellet, and she can release a cube into a cup after it has been demonstrated to her. She tries to build a tower of two cubes with variable success. She is most likely at which of the following age?
2 months
4 months
6 months
9 months
1 year
A neonate has an obviously abnormal foot. The foot is in a markedly plantar flexed position, with the sole facing the adjacent leg in a position of marked adduction. No other anomalies are noted on physical examination. Which of the following is the most likely diagnosis?
Epispadias
Hypospadias
Talipes calcaneovalgus
Talipes equinovarus
Torticollis
A mentally retarded 10-year-old boy presents with arthritis, nephrolithiasis, and progressive renal failure. Since his first years of life, he manifested peculiar neurologic abnormalities consisting of self-mutilative biting of the lips and fingers, choreoathetosis, and spasticity. Two male relatives on his mother's side presented with a similar condition and died in their teens. Which of the following is the most likely diagnosis?
Chronic lead intoxication
Fragile-X syndrome
Gout
Huntington disease
Lesch-Nyhan syndrome
A previously healthy 7-year-old girl comes to the office with complaints of episodic abdominal pain over the past several months. The pain is periumbilical and sharp but does not wake her from sleep or interfere with play. She has no fever, joint complaints, or constipation or diarrhea. Growth and development have been normal. The physical examination is within normal limits. Which of the following is the most likely diagnosis?
Acute appendicitis
Acute cholecystitis
Crohn disease
Functional abdominal pain
Irritable bowel syndrome
A 4-month-old male infant is brought to the office by his parents due to progressive lethargy, poor feeding, fatigue and increasing pallor for the past four weeks. His antenatal and birth histories are unremarkable. His diet consists mainly of breast milk. His immunizations are up-to-date. His mother's blood type is O+. Physical examination reveals a webbed neck, cleft lip, shielded chest, triphalangeal thumbs, and pale mucous membranes and conjunctivae. Cardiac auscultation reveals mild tachycardia and a systolic ejection murmur over the left upper sternal border. The initial investigations reveal the following: Hb 8 g/dl Ht 26% WBCs 7,000/mm3 Platelets 300,000 /mm3 Reticulocytes 04% MCV 104 fl Blood type A Bilirubin direct 0.1 mg/dl Bilirubin total 1.0 mg/dl What is the most likely diagnosis?
Wiskott-Aidrich syndrome
Transient erythroblastopenia of childhood
Idiopathic aplastic anemia
Fanconi's anemia
Diamond-Biackfan anemia
A 15-year-old Caucasian male is brought to the office by his mother for the evaluation of a six-month history of unstable gait and speech difficulty which are getting worse over time. His past medical history is insignificant. He is not taking any medications, and denies smoking or alcohol consumption. His blood pressure is 120/70 mmHg and pulse is 80/min. Musculoskeletal examination showed scoliosis and feet deformity with 'hammer toes.' The neurologic examination showed dysarthria, dysmetria, nystagmus, and absence of deep plantar reflexes on lower extremities. What is the most common cause of death in this patient population?
Cardiomyopathy
Renal failure
Diabetes-related complication
Malignancy
Septic shock
Over the previous 2 to 3 weeks, a very active 13-year-old white boy is noted by his family to have developed deep pains in his leg that awaken him from sleep. The family brings him to your office with a complaint of a swelling over his distal leg, which he attributes to his being kicked while playing soccer about 1 week ago. He has had no fever, headaches, weakness, bruising, or other symptoms. A radiograph of the leg is shown below. Which of the following is the most likely explanation for his pain?
Growingpains
Leukemia
Osteomyelitis
Bone fracture
Osteosarcoma
An 18-month-old child is brought to the emergency department by his mother due to a one-day history of lethargy and anorexia. He had a fever the whole day yesterday, which responded to Tylenol (Acetaminophen). He then developed a petechial rash over his entire body, which worsened in the last few hours. He is up-to-date with his immunizations, and is an otherwise healthy baby. On examination, he is drowsy and lethargic. He has neck stiffness and appears septic. He flexes his hips when his neck is flexed. What is the most likely organism responsible for the patient's symptoms?
Meningococcus
Haemophilus influenza
Cytomegalo virus
Borrelia burgdorferi
Listeria monocytogenes
You are called to examine a one-day-old male neonate who gradually developed cyanosis over the past few hours. The infant was delivered vaginally at full term, assisted with forceps, and weighed 9 lbs. The Apgar scores were 7 and 8 at 1 and 5 minutes, respectively. Oxygen administration by mask does not relieve the cyanosis. Further examination reveals tachypnea, subcostal retractions, a normal S 1, single and loud S2, and no murmur. Which of the following is the most probable cause of the infant's cyanosis?
Transposition of great vessels
Atrial septal defect
Coarctation of aorta
Ventricular septal defect
Patent ductus arteriosus
A 9-month-old, chubby, healthy-appearing boy is brought to the pediatrician because of episodes of colicky abdominal pain and blood-tinged stools. The pain lasts from 1 to 10 minutes and causes the infant to double up; he then appears normal until his next bout of colic. During the examination, the infant has another episode, at which time a vague mass can be felt on the right side of the abdomen, and the right lower quadrant has an "empty" feeling to deep palpation. Which of the following is the most appropriate initial step in management?
Barium enema
Colonoscopy
Gastrografin enema
Upper gastrointestinal endoscopy
Exploratory surgery
A 29-year-old woman presents to the delivery room in labor at 35 weeks' gestation with a temperature of 40 C (104 F). She lives on a dairy farm and is in the habit of drinking unpasteurized milk from her cows before sending it to the dairy. For the past 3 days she has been unable to attend to her chores because of fever, headache, mild diarrhea, and a general feeling of illness. When her amniotic membranes rupture, the fluid is dark, cloudy, and brownish-green. At birth, the infant has no malformations or edema, but is in severe respiratory distress. Which of the following is the most likely diagnosis?
Congenital syphilis
Congenital toxoplasmosis
Fetal hydrops
Neonatal herpes
Neonatal listeriosis
A 4-year-old girl with sickle cell disease presents to the emergency department with a temperature of 39.6 C (103.2 F). Other than irritability, the physical examination is unremarkable. Laboratory evaluations reveal a white blood cell count of 18,200/mm3, with 88% polymorphonuclear neutrophils, 10% lymphocytes, and 2% monocytes, and a hemoglobin of 7.6 g/dL. Which of the following is the most appropriate next step in management?
Observe the child pending blood culture results
Administer amoxicillin orally
Administer ceftazidime and gentamicin intravenously
Administer ceftriaxone intravenously
Administer vancomycin and gentamicin intravenously
A previously healthy 13-year-old girl presents to the emergency department with an acute onset of red urine after she played soccer in the morning. Her physical examination is unremarkable. Urinalysis shows a red color; pH, 6.2; specific gravity, 1.024; glucose, negative; blood, +4; protein, trace; nitrite, negative; leukocyte esterase, negative; white blood cell, 0/hpf; red blood cell, 1/hpf. Which of the following is the most likely explanation of the red urine?
Glomerulonephritis
Hematuria
Ingestion of food coloring
Myoglobinuria
Presence of urates
A 1-month-old infant is seen in a well-baby clinic. The mother states that the baby is constipated and feeds poorly. On examination, he is jaundiced, has a large posterior fontanel and an umbilical hernia, and exhibits poor muscle tone. He has gained only 300 g since discharge from the normal newborn nursery. Which of the following is the most likely diagnosis?
Alphaj-antitrypsin deficiency
Biliary atresia
Congenital hypothyroidism
Pyloric stenosis
Syphilis
A 7-year-old boy is referred for genetic testing because his father was diagnosed with medullary cancer of the thyroid. The father underwent a total thyroidectomy, and in the preoperative workup it was determined that he also had a pheochromocytoma, and that tumor was removed also. The father did not have parathyroid hyperplasia at the time, his phenotype was normal, and his final diagnosis was MEN-2A. The child is tested and found to have RET mutations in the peripheral white blood cells. The child has normal phenotype, normal levels of calcitonin, normal levels of catecholamines, metanephrines, and VMA, and normal levels of calcium and parathyroid hormone. Which of the following is the most appropriate management?
Bilateral adrenalectomies
Continued observation
MRI of the pituitary
Parathyroid surgical exploration
Total thyroidectomy
A 3-month-old male infant is brought to the emergency department by his mother because of difficulty in breathing. His mother was admitted in the hospital ten days ago due to a urinary tract infection, and he was cared for by his grandmother during that period. His mother had just been discharged from the hospital yesterday, and noticed that he was constipated and having difficulty with breastfeeding. On examination, he is afebrile. His pulse rate is 110/min, respirations are 36/min with shallow breathing efforts, and blood pressure is 90/50mm Hg. His weight is at the 35th percentile. Examination shows ptosis, dilated pupils with sluggish reaction to light, diminished deep tendon reflexes and decreased muscle tone. What is the most likely mechanism of his illness?
Bacterial infection of the meninges
Autoimmune disease against acetylcholine receptors
Clostridium difficile toxin in the intestinal tract
Clostridium botulinum in the intestinal tract
Clostridium botulinum toxin intake
A 16-year-old College student presents to the physician's office because of a generalized malaise, sore throat and fever for the past 2 to 3 days. She is given amoxicillin prescription. Twenty-four hours later, she develops a polymorphous rash over her entire body. She has taken amoxicillin in the past for sinus disease and never had any problem. What is the most likely organism that is responsible for her symptoms?
Group B streptococcus
Epstein-Barr virus
Coxsackie virus
Escherichia coli
Nocardia
An otherwise healthy 17-year-old complains of swollen glands in his neck and groin for the past 6 months and an increasing cough over the previous 2 weeks. He also reports some fevers, especially at night, and possibly some weight loss. On examination, you notice that he has nontender cervical, supraclavicular, axillary, and inguinal nodes, no hepatosplenomegaly, and otherwise looks to be fairly healthy. Which of the following would be the appropriate next step?
Biopsy of a node
CBC and differential
Trial of antituberculosis drugs
Chest radiograph
Cat-scratchtiters
A 15-year-old girl has a round, 1 -cm cystic mass in the midline of her neck, at the level of the hyoid bone. The mass is deep to the skin and moves slightly when the patient swallows. When the mass is palpated at the same time that the tongue is pulled, there seems to be a connection between the two. The mass has been present for at least 10 years, but only recently bothered the patient because it became infected. Which of the following is the most likely diagnosis?
Branchial cleft cyst
Cystic hygroma
Epidermal inclusion cyst
Metastatic thyroid cancer
Thyrogtossal duct cyst

A 4-month-old baby boy arrives to the ER cold and stiff. The parents report that he had been healthy and that they put him to bed as usual for the night at the regular time. When they next saw him, in the morning, he was dead. Physical examination is uninformative. A film from a routine skeletal survey is shown below. Which of the following is the most likely diagnosis?
Scurvy
Congenital syphilis
Sudden infant death syndrome (SIDS)
Osteogenesis imperfecta
Abuse
A 6-year-old boy is often teased at school because he has stooled in his underwear almost daily for the last 3 months. He was toilet trained at 2 years of age without difficulty, but over the last 2 years he had developed ongoing constipation. His family is frustrated because they cannot believe him when he says (I didn’t know I had to go). He is otherwise normal; school is going well, and his home life is stable. His only finding on examination is significant for stool in the rectal vault. The plain radiograph of his abdomen is shown. Initial management of this problem should include which of the following?
Barium enema and rectal biopsy
Family counseling
Time-out when he stools in his underwear
Clear fecal impaction and short-term stool softener use
Daily enemas for 4 weeks
A 2-year-old boy who emigrated from Eastern Europe 1 year ago is brought to the physician because of fever, cough, and night sweats for 3 weeks. The child's grandmother, who lives with him, has similar symptoms. The child's temperature is 39.2 C (102.6 F), Wood pressure is 110/65 mm Hg, pulse is 90/min, and respirations are 28/min. A Mantoux test is reactive, and a chest x-ray film shows a right middle lobe infiltrate and hilar lymphadenopathy. Which of the following is the most appropriate next step in diagnosis?
Cervical lymph node biopsy
Gastric aspiration
Pleurocentesis
Sputum induction
Gastroscopy
A 4-month-old infant is evaluated by a dermatologist because of thick, erythematous skin with fine scaling, principally involving his face. The mother reports that the infant is "always scratching his face." An older brother and a maternal uncle had a similar condition. Screening hematologic studies show the following: Erythrocyte count 5.1 million/mm3 Leukocyte count 12,000/mm3 Segmented neutrophils 80% Bands 5% Eosinophils 3% Basophils 1% Lymphocytes 5% Monocytes 6% Platelet count 35,000/mm3 , with the comment that the platelets are smaller than normal Serum immunoglobulin studies demonstrate the following: IgA 120 mg/dL IgE 2300 IU/mL IgG 900 mg/dL IgM 15 mg/dL Patients with this condition have a significantly increased incidence of which of the following?
Basal cell carcinoma
Hodgkin lymphoma
Melanoma
Non-Hodgkin lymphoma
Squamous cell carcinoma of the skin
A 15-year-old athlete is in your office for his annual physical examination before the start of football season. He has no complaints, has suffered no injuries, and appears to be physically fit. On his heart examination, you note a heart rate of 100 beats per minute, and a diffuse point of maximal impulse (PMI) with a prominent ventricular lift. He has a normal S1 and S2, with an S4 gallop. He has no murmur sitting, but when he stands you clearly hear a systolic ejection murmur along the lower left sternal edge and the apex. For which of the following conditions is this examination most consistent?
Wolff-Parkinson-White syndrome
Valvular aortic stenosis
Valvular pulmonic stenosis
Myocarditis
Hypertrophic cardiomyopathy
A 16-year-old girl, accompanied by her mother, is in your office for a well-adolescent visit. The mother asks about drug and alcohol abuse. You explain that the warning signs of abuse include which of the following?
Excessive concern for weight and body configuration
Improved school performance
Recent changes from age-appropriate, acceptable friends to younger associates
Deterioration in personal habits, hygiene, dress, grooming, speech patterns, and fluency of expression
Improvement in relationships with adults, siblings, and authority figures
A 6-month-old boy presents to the Emergency Department with a three-day history of cough, congestion and low grade fever. The mother states that the baby has not been feeding well and has used only two diapers over the past 24 hours. Physical examination reveals a pale infant with a temperature of 37.8 C (100.1 F), pulse of 170/min, respirations of 60/min and oxygen saturation of 88% on room air. The patient exhibits nasal flaring, subcostal and intercostal retractions. Lung examination reveals diffuse wheezing. Cardiac examination reveals a regular but tachycardic rhythm with no murmur. Central capillary refill is four seconds. The remainder of the examination is normal. Which of the following is the most appropriate initial step in management?
Chest x-ray film
Albuterol nebulizer treatment
Bolus of intravenous fluids
Oxygen therapy
Intravenous steroids
An infant in brought to the clinic for a routine healthy visit and vaccinations. She is the product of an uncomplicated pregnancy and has been meeting development mileposts. She is feeding well, and her mother reports that the baby seems to be growing well as well. On physical examination, the infant is afebrile with stable vital signs. She can lift her head to 90 degrees, her eyes follow past the midline, she laughs, regards her own hand and has slight awareness of her mother. Which of the following is the most likely age of this infant?
2 months
4 months
6 months
12 months
18 months
A two-day old infant develops seizures, bulging fontanel, and focal neurologic signs. His temperature is 37 C (98F), pulse is 180/min, and capillary refill is> 2 seconds. The initial work-up reveals a hemoglobin level of 12g/dl. Transfontanel ultrasonography demonstrates a hemorrhage involving the germinal matrix, lateral ventricles, and brain parenchyma. Which of the following is the most significant risk factor for this newborn's condition?
Prematurity
Pelvic dystocia
Prenatal infection
Congenital anomaly
Macrosomia

A 6-year-old, fully immunized boy is brought to the emergency room with a 3-hour history of fever to 39.5°C (103.1°F) and sore throat. The child appears alert, but anxious and toxic. He has mild inspiratory stridor and is drooling. He is sitting on the examination table leaning forward with his neck extended. A lateral radiograph of his neck is shown below. Which of the following is the most appropriate immediate management of this patient?
Examine the throat and obtain a culture.
Obtain an arterial blood gas and start an IV line.
Administer a dose of nebulized epinephrine
Prepare to establish an airway in the operating room.
Admit the child and place him in a mist tent.
A 4-year-old boy was admitted to the hospital last night with the complaint of “difficulty breathing.” He has no past history of lung infection, no recent travel, and no daycare exposure; he does, however, have an annoying tendency to eat dirt. In the emergency center he was noted to be wheezing and to have hepatomegaly. He is able to talk, relaying his concern about his 6-week-old Chihuahua being left alone at home. Laboratory studies revealed marked eosinophilia (60% eosinophils). Which of the following tests is most likely to produce a specific diagnosis?
Histoplasmin test
ELISA for Toxocara
Silver stain of gastric aspirate
Stool examination for ova and parasites
Tuberculin skin test
A 10-year-old Caucasian boy is brought to the emergency room by his mother with right hemiplegia of sudden onset. The mother says that the child fell on a pencil in his mouth, ten hours before the onset of symptoms. His past medical history is insignificant. Family history is not significant. His blood pressure 110/60 mmHg and heart rate is 90/min. Physical examination reveals dense right hemiplegia, right hemianesthesia, and mild motor aphasia. Cardiac auscultation reveals S3. What is the most probable cause of this patient's condition?
Antiphospholipid antibodies
Migraine
Epilepsy
Congenital heart disease
Internal carotid artery dissection
A 2-day-old male infant is jaundiced. He was born at term from an uncomplicated pregnancy, and was normal at birth. He otherwise appears healthy and is feeding well. Vital signs are stable. Physical examination shows jaundice. There is no organomegaly. Laboratory investigations show: Hemoglobin 17.0 g/L MCV 88 fl Platelets 220,000/mm3 Leukocyte count 4,500/mm3 Total bilirubin 7.5 mg/dL Indirect bilirubin 6.0 mg/dL What is the most likely cause of this patient's jaundice?
Physiologic jaundice
Bacterial infection
Breast milk jaundice
Biliary atresia
Erythroblastosis fetalis
A 2-year-old child is admitted to your hospital team. The child’s primary care doctor has been following the child for several days and has noted her to have had high fever, peeling skin, abdominal pain, and a bright red throat. You are concerned because two common pediatric problems that could explain this child’s condition have overlapping presenting signs and symptoms. Which of the following statements comparing these two diseases in your differential is true?
Neither has cardiac complications.
Serologic tests are helpful in diagnosing both.
Only one of the diseases has mucocutaneous and lymph node involvement
Pharyngeal culture aids in the diagnosis of one of the conditions.
A specific antibiotic therapy is recommended for one of the conditions, but only supportive care is recommended for the other
Two new mothers are discussing their infants outside the neonatal intensive care unit. Both were born at 36 weeks’ gestation. One infant weighs 2600 g (5 lb, 12 oz) while the other infant weighs 1600 g (3 lb, 8 oz). The mother of the second infant should be told that her child is more likely to have which of the following conditions?
Congenital malformations
Low hematocrit
Hyperglycemia
Surfactant deficiency
Rapid catch-up growth
A 6-month-old male is brought to the office due to fussiness and tugging at his right ear for the past 2 days. He has had a fever of 39.4 C (103 F) for the past 2 days. His past medical history is significant for recurrent ear and lung infections, oral candidiasis, and persistent diarrhea by rotavirus. His temperature is 39.4 C (103F), pulse rate is 150/min, respirations are 28/min, and blood pressure is 80/60mm Hg. Physical examination reveals an erythematous, bulging right tympanic membrane with poor mobility on pneumatic otoscopy. His lymph nodes are not palpable, and his tonsils are not visualized. His B and T lymphocyte levels are markedly reduced. The chest x-ray reveals an absent thymic shadow. What is the most likely etiology of this patient's condition?
Severe combined immune deficiency
Common variable immunodeficiency
Bruton's agammaglobulinemia
Wiskott-Aidrich syndrome
Chronic granulomatous disease
A school teacher calls you to report that his 7-year-old student had about 10 episodes of eye blinking and gabbling today, which lasted approximately 30 seconds each. The child sat in his chair and did not have any postictal confusion. The teacher noticed several similar episodes during the last month, as well as a decline in the child's school performance. What type of seizure does this child have?
Generalized tonic-clonic seizures
Atonic seizures
Simple partial seizures
Absence seizures
Complex partial seizures
A 10-year-old girl has had a “cold” for 14 days. In the 2 days prior to the visit to your office, she has developed a fever of 39°C (102.2°F), purulent nasal discharge, facial pain, and a daytime cough. Examination of the nose after topical decongestants shows pus in the middle meatus. Which of the following is the most likely diagnosis?
Brain abscess
Maxillary sinusitis
Streptococcal throat infection
Sphenoid sinusitis
Middle-ear infection
A 16-year-old girl is being evaluated for primary amenorrhea. Her birth history is significant for low birth weight and bilateral swelling of the hands and feet. Her blood pressure is 170/96 mmHg. She has a short stature and webbed neck. Her karyotype examination results show 22 pairs of autosomes, one X, and one Y chromosome. Which of the following statements is true regarding this patient's condition?
The primary amenorrhea in this girl is most likely caused by functional uterine abnormalities
The girl should undergo bilateral abdominal gonadectomy
The webbing of the neck is caused by defects in arteriovenous communications
The inheritance for this condition is Mendelian dominant
This child will benefit from steroid hormone replacement therapy
An 8-year-old girl presents with well-controlled, moderately persistent asthma. Her therapies consist of occasional use of short-acting β-agonists, daily inhaled steroids, and a leukotriene inhibitor. She presents with white patches on her buccal mucosa. You recommend which of the following?
HIV testing
Tuberculosis skin testing
Measurement of serum immunoglobulins
Discontinuation of all her asthma medications
Rinse her mouth after use of her inhaled medications
A 4-year-old boy, who has a ventriculoperitoneal shunt for congenital hydrocephalus, develops fever, headache, irritability, lethargy, photophobia, and vomiting. His temperature is 39.6 C (103.2 F). He is noted to have nuchal rigidity, with the presence of both Kernig's and Brudzinski's signs. The shunt tract is erythematous on the surface. A lumbar puncture is performed and shows a WBC of 40,000/mm3 with 85% neutrophils, a glucose concentration of 48 mg/dL, and a protein concentration of 169 mg/dL. Which of the following is the most likely pathogen?
Haemophilus influenzae
Neisseria meningitidis
Pseudomonas aeruginosa
Staphylococcus epidermidis
Streptococcus pneumoniae
A 16-year-old boy presents with a temperature of 38.4 C (101 F) and low back, wrist, and knee pain. He had a sore throat 1 month earlier. His arthritis is diffuse. Pea-sized swellings are noted over the skin on his knees. He has a serpiginous erythematous area on his anterior trunk. His blood and throat cultures are negative, and his CBC is unremarkable. His antistreptolysin-O (ASO) titer is high. Which of the following is the most appropriate therapy?
Acetaminophen
Aspirin
Penicillin
Penicillin and aspirin
Supportive care
A 2-year-old child is brought by an anxious mother to the emergency department because of difficulty in breathing for the past 12 hours. The child has a history of runny nose that started 3 days ago. He suddenly developed a progressively increasing difficulty in breathing. The mother reports that the child "sounds like a barking dog when he coughs." The child's temperature is 37.7C (99.9F), respirations are 30/min, blood pressure is 90/60mm Hg, and pulse rate is 104/min. He is coughing and using his accessory muscles of respiration. His oxygen saturation is 98% on 2L of oxygen. He is diagnosed with laryngotracheobronchitits, started on humidified oxygen, and kept in an upright position. After 20 minutes, he becomes more irritable, his oxygen saturation drops to 92%, respirations increase to 40/min, and pulse increases to 120/min. His blood pressure and temperature are unchanged. What is the most appropriate next step in the management of this patient?
Continue the same therapy
Take the patient to the operating room
Consult the anesthesiologist
Intubate the patient in the emergency room
Start racemic epinephrine
A 5-year-old boy is brought to the clinic by his mother because he was sent home by the school nurse. The nurse claims to have heard a murmur in his chest. The child has always been healthy, and has never had any shortness of breath, chest pain, dizziness or any other illnesses. On examination, the child appears alert, and his vital signs are stable. Auscultation of the chest reveals a grade-2 systolic ejection murmur at the left sternal border, but no other extra sounds. The murmur changes with position. What is the best next step in the management of this patient?
121ead ECG
Echocardiogram
Holter monitor
Observation
Cardiology evaluation
A 13-year-old boy has a 3-day history of low-grade fever, symptoms of upper respiratory infection, and a sore throat. A few hours before his presentation to the emergency room, he has an abrupt onset of high fever, difficulty swallowing, and poor handling of his secretions. He indicates that he has a marked worsening in the severity of his sore throat. His pharynx has a fluctuant bulge in the posterior wall. A soft tissue radiograph of his neck is shown. Which of the following is the most appropriate initial therapy for this patient?
Narcotic analgesics
Trial of oral penicillin V
Surgical consultation for incision and drainage under general anesthesia
Rapid streptococcal screen
Monospot test
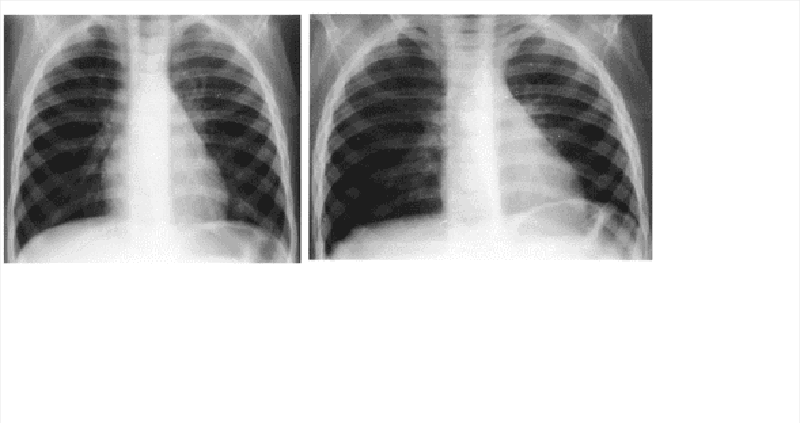
A previously healthy 2-year-old black child has developed a chronic cough during the previous 6 weeks. He has been seen in different emergency rooms on two occasions during this period and has been placed on antibiotics for pneumonia. Upon auscultation, you hear normal breath sounds on the left. On the right side, you hear decreased air movement during inspiration but none upon expiration. Inspiratory (A) and expiratory (B) radiographs of the chest are shown below. Which of the following is the most appropriate next step in making the diagnosis in this patient?
Measure the patient’s sweat chloride.
Consult pediatric surgery for bronchoscopy.
Prescribe broad-spectrum oral antibiotics.
Initiate a trial of inhaled β-agonists.
Prescribe appropriate doses of oral prednisone.
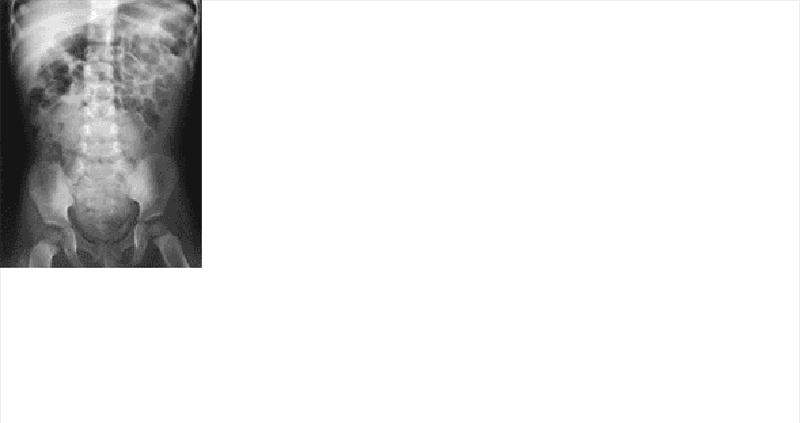
A 4-year-old boy presents with a history of constipation since the age of 6 months. His stools, produced every 3 to 4 days, are described as large and hard. Physical examination is normal; rectal examination reveals a large ampulla, poor sphincter tone but present anal wink, and stool in the rectal vault. The plain film of his abdomen is shown. Which of the following is the most appropriate next step in the management of this child?
Lower gastrointestinal (GI) barium study
Parental reassurance and dietary counseling
Serum electrolyte measurement
Upper GI barium study
Initiation of thyroid-replacement hormone
A 7 -year-old girl is brought to the physician's office by her mother due to recurrent, prolonged episodes of nausea and severe vomiting for the past 4 days. According to the mother, the vomiting starts in the early morning and recur 7 to 8 times daily. The child denies any headache, abdominal pain, diarrhea, chest pain or respiratory distress. She has had two similar episodes of vomiting and nausea in the past year, which resolved spontaneously. The mother has a history of migraines. On examination, the child is afebrile and has pallor with signs of mild dehydration. The abdomen is soft and non-tender to palpation. What is the most likely cause of this child's symptoms?
Gastroesophageal reflux disease
Gastroenteritis
Mesenteric adenitis
Cyclical vomiting
Migraine attacks
A father brings his 18-month-old daughter to the office for the evaluation of fever for the past 1 0 days. The father, who works as a phlebotomist, says that the temperature seems higher in the morning and again at night, often reaching 40.5C (105F), and is sometimes associated with shaking chills. He remembers that the child developed severe respiratory distress and skin rash when treated with penicillin in the past. He has heard about the development of 'liver toxicities' in children treated with aspirin, and he is interested in knowing everything about his daughter's condition. On examination, the child is in no acute distress. Her temperature is 39.4C (103F), pulse rate is 90/min, and blood pressure is 1 00/60 mmHg. Her sclerae are anicteric. There is bulbar conjunctival injection, and the oropharynx shows diffuse mucosal injection with fissuring and crusting of the lips. There are numerous hyperemic macules over her entire body, and her palms appear edematous. Based on the above description, which of the following is the most accurate statement?
Latex agglutination test is more accurate than streptococcal throat test in determining the etiology of this condition
Immediate desensitization & treatment with penicillin V will prevent further renal complications
Thrombocytopenia is an important marker in the second week of this illness
Acetaminophen is the drug of choice for alleviation of high temperatures in this child
She needs to be hospitalized and treated with intravenous immune globulin (IVIG) and aspirin
A term newborn is delivered vaginally following a breech presentation. On physical examination, the Barlow test is positive for bilateral subluxation of the hips. There is decreased abduction of both hips. Besides breech presentation, which of the following infants are most at risk for developmental dysplasia of the hip?
African American infants
Female infants
Second-born infants
Infants of mothers with preeclampsia
Premature infants
A 4-month-old infant boy has gained only 10 ounces since birth. He has failed to gain weight with multiple formula preparations. His stools have been loose and fatty. An older sister had similar symptoms and has been repeatedly hospitalized for failure to thrive and recurrent pulmonary infections. Which of the following is the most likely cause of this patient's gastrointestinal symptoms?
Achlorhydria
Bacterial overgrowth
Colonic inertia
Gastric hypersecretion
Pancreatic exocrine insufficiency
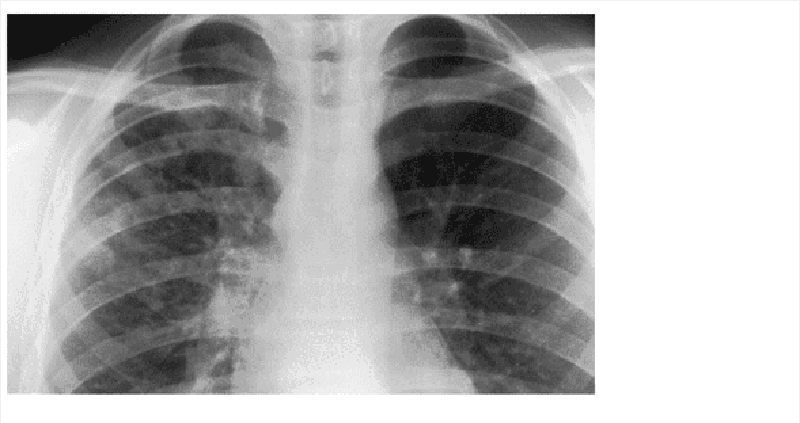
A 13-year-old develops fever, malaise, sore throat, and a dry, hacking cough over several days. He does not appear to be particularly sick, but his chest examination is significant for diffuse rales and rhonchi. The chest radio- graph is shown below. Which of the following is the most likely pathogen?
Staphylococcus aureus
Mycobacterium tuberculosis
Haemophilus influenzae
Streptococcus pneumoniae
Mycoplasma pneumoniae
A 3-month-old, previously well male infant presents to the emergency department in January with a 2-day history of clear rhinorrhea, low-grade fever, and poor appetite, but no cough. On physical examination, there are mild subcostal retractions, coarse breath sounds heard throughout the lung fields, and scattered expiratory wheezes. The child receives an intravenous fluid bolus in the emergency department and is admitted for observation. Which of the following is the most severe, life-threatening complication of this child's illness?
Apnea
Congestive heart failure
Dehydration
Hypoxemia
Wheezing
A 14-year-old boy has pain in his left leg. An x-ray shows a tumor and a biopsy reveals histopathologic features characteristic of neural origin. Which of the following is the most likely diagnosis?
Chondroblastoma
Ewing sarcoma
Neuroblastoma
Osteosarcoma
PJiabdomyosarcoma
A 7-year-old boy arrives at the emergency room in acute distress. Over the past 3 to 4 days he has become progressively ill with generalized fatigue and mild, mid-abdominal pain that have become steadily worse. On physical examination he has a maculopapular rash on his thighs and feet with some spread of the rash to his buttocks. The rash does not blanch and the some lesions near the ankles look petechial or bruised. His temperature is 39.0 C (102.2 F) and he is drawing his knees to his chest for relief of his stomach pains. He is nauseated and vomited once before coming to the hospital. He has semi-soft dark stool, which is guaiacpositive. The boy has not voided since early morning and cannot provide a urine sample. The doctor determines that he is 10% dehydrated and asks the nurse to start intravenous fluids. Which of the following is the most likely diagnosis?
Pancreatitis
Rocky Mountain spotted fever
Nephrotic syndrome
Henoch-Schönlein Purpura
Appendicitis
A newborn girl is noted to be drooling saliva, and she chokes violently when she is first fed. On physical examination, she is found to have abdominal distention and an imperforate anus. There is no fistula to the perineum or vagina. Examination of the urine reveals no meconium in it. Echocardiogram and renal sonogram are reported as negative for other congenital defects. X-ray films show abundant gas in the gastrointestinal tract. Pictures taken with a metal marker taped to the anus, and the baby hanging upside down, show that there is a significant distance (2.5 cm) between the blind end of the rectum and the anal marker. Before a diverting colostomy is performed, which of the following steps should be taken?
A soft nasogastric tube passed, and x-rays taken
Barium injected through the anal dimple
Barium swallow
Nasogastric suction for at least 24 hours
Surgical exploration of the perineum to see whether a primary repair is possible
A newborn male has oliguria and a midline mass in the lower abdomen. What is the most likely diagnosis?
Bladder exstrophy
Wilms tumor
Hypospadias
Posterior urethral valves
Cryptorchidism
A 22-month-old boy who recently immigrated from Eastern Europe with his family is brought to your office by his mother who is worried that he seems to tire easily. She describes how he becomes short of breath with even mild physical activity and cannot keep up with his peers during play. The boy is at the 40th percentile for height and 20th percentile for weight. On general examination, there is no clubbing, cyanosis, or peripheral edema, but there is a harsh 3/6 holosystolic murmur over the left lower sternal border and a rumbling diastolic murmur over the cardiac apex. Which of the following is the most likely cause of his symptoms?
Tetralogy of F allot
Atrial septal defect
Ventricular septal defec
Transposition of the great vessels
Mitral stenosis
A 15-year-old Caucasian female comes to your office because her menses have not yet started. Her breast development is Tanner stage 2 and there is scant pubic hair. Physical examination is also significant for decreased femoral pulses. Which of the following is the best next step in evaluating her condition?
Abdominal CT scan
Progesterone challenge
Serum prolactin level
Karyotype analysis
Urine 17 -hydroxyprogesterone level

A previously healthy 3-year-old male is brought to the emergency department with abdominal pain. The abdominal pain began several hours ago. Since then, he has had several episodes in which he clutches his stomach and screams. These episodes are associated with nonbloody, nonbilious vomiting and loose, watery stools. Between the episodes, the patient denies abdominal pain and is playful. On examination, his temperature is 99.o 0F (37.2 0C), pulse is 100/min, respiratory rate is 20/min, and blood pressure is 85/50 mmHg. The child is alert and in no acute distress. Abdominal examination reveals a soft, nontender, nondistended abdomen with bowel sounds present in all four quadrants. A tubular mass is felt in the right upper quadrant, and a rectal exam is hemoccult positive. An ultrasound image of the patient's abdomen is shown below. What is the best next step in the management of this patient?
Emergent laparotomy
Computed topography of the abdomen
Laparoscopic cholecystectomy
Meckel's scan
Air contrast enema
A 5-month-old child was normal at birth, but the family reports that the child does not seem to look at them any longer. They also report the child seems to “startle” more easily than he had before. Testing of his white blood cells (WBCs) identifies the absence ofhexosaminidase A activity, confirming the diagnosis of which of the following?
Niemann-Pick disease, type A
Infantile Gaucher disease
Tay-Sachsdisease
Krabbe disease
Fabry disease
The family of a 4-year-old boy has just moved into your area. The child was recently brought to the emergency department (ED) for an evaluation of abdominal pain. Although appendicitis was ruled out in the ED and the child’s abdominal pain has resolved, the ED physician requested that the family follow up in your office to evaluate an incidental finding of an elevated creatine kinase. The family notes that he was a late walker (began walking independently at about 18 months of age), that he is more clumsy than their daughter was at the same age (especially when trying to hold onto small objects), and that he seems to be somewhat sluggish when he runs, climbs stairs, rises from the ground after he sits, and rides his tricycle. A thorough history and physical examination are likely to reveal which of the following?
Hirsutism
Past seizure activity
Proximal muscle atrophy
Cataracts
Enlarged gonads
A 15-month-old boy is brought into the clinic with a 1-day history of fever, decreased oral intake, and runny nose. His vital signs are within normal limits except for a temperature of 39.5 C (103.1 F). He is active and in no distress. His ears are clear bilaterally. There is a clear nasal discharge. Multiple small (1 -2 mm) vesicular lesions are noted on the mucosa of the anterior tonsillar pillars and posterior palate. The rest of his examination is within normal limits. Which of the following is the most likely diagnosis?
Aphthous stomatitis
Hand-foot-and-mouth disease
Herpangina
Kawasaki disease
Stevens-Johnson syndrome
A nurse notices that a 1 -week-old, premature infant in the neonatal unit is experiencing migratory jerks of the extremities. She picks the infant up and can feel that the muscle jerks are continuing to happen, even when she holds an involved extremity still. After about 5 minutes, the jerking movements stop. Which of the following is the most appropriate first step in diagnosis?
CT scan of head
EEG
Serum chemistries
Skull x-rays
Ultrasound of head
A neonate develops severe cyanosis that begins within minutes of birth. Blood drawn one hour after birth shows metabolic acidosis with respiratory acidosis. A chest x-ray film shows a narrow base to the great vessels and the heart resembles an egg on its side. ECG is normal. Which of the following is the most likely diagnosis?
Aortic valve stenosis
Complete atrioventricular canal defect
Tetralogy of Fallot
Transposition of the great arteries
Underdeveloped (hypoplastic) left ventricle syndrome
A 13-year-old boy is seen for right knee pain that has persisted for the past 2 months despite the use of over-the-counter analgesics. His mother states that he has been limping since he started to have the pain. The pain is of insidious onset, but its intensity sometimes suddenly increases. On physical examination, the boy is obese; his weight is higher than the 90th percentile. Flexion of the right hip causes marked outward rotation and reproduces the pain. Internal rotation of the right hip is limited, and the right leg is slightly shortened compared with the left leg. Which of the following is the most likely diagnosis?
Juvenile rheumatoid arthritis
Legg-Calve-Perthes disease
Septic arthritis
Slipped capital femoral epiphysis
Toxic synovitis
A 2-week-old male infant is brought to the office by his mother due to fever and vomiting for the past two days. He appeared normal until two days ago. He is being breastfed. He was born at 32 weeks gestation and weighed 2.7kg (6 Ib) at birth. On examination, he is ill-looking, lethargic, and febrile. His abdomen is distended, bowel sounds are absent, and stool is guaiac-positive. An abdominal x-ray demonstrates pneumatosis intestinalis. What is the most likely diagnosis of this patient?
Intestinal obstruction
Malrotation
Meconium ileus
Necrotizing enterocolitis
Intestinal perforation
A 5-year-old Mexican female child is brought to the office for the evaluation of a pruritic vulva for the past fifteen days. The pruritus is felt mostly during the night. Her 4- year-old cousin who visited them four weeks ago has a similar complaint. On examination, there is no vaginal discharge, but the vulva is erythematous. The rest of the physical examination is normal. What is the most appropriate next step in the management of this patient?
Detain the child with the suspicion of sexual abuse
Do a scotch tape test
Do stool examination for parasites
Do vaginal fluid gram stain
Do wet mount of vaginal fluid

A 2-year-old boy is brought into the emergency room with a complaint of fever for 6 days and the development of a limp. On examination, he is found to have an erythematous macular exanthem over his body as shown in image A, ocular conjunctivitis, dry and cracked lips, a red throat, and cervical lymphadenopa- thy. There is a grade 2/6 vibratory systolic ejection murmur at the lower left sternal border. A white blood cell (WBC) count and differential show predominant neutrophils with increased platelets on smear. Later, he develops the findings as seen in image B. Which of the following is the most likely diagnosis?
Scarlet fever
Rheumatic fever
Kawasaki disease
Juvenile rheumatoid arthritis
Infectious mononucleosis
The parents of a 5-year-old boy come to the physician concerned about their child's recurrent leg pains. The boy has been complaining for several weeks about pain in both legs, usually occurring soon after going to bed. He derives relief from rubbing his legs and knees. He does not limp and is able to participate in sports activities. Which of the following is the most likely diagnosis?
"Growing" pains
Juvenile rheumatoid arthritis
Osgood-Schlatter disease (osteonecrosis of the tibial tuberosity)
Osteoid osteoma
Osteosarcoma
A young black male with sickle cell trait is preparing for his travel to West Africa from North America. While obtaining his visa, he is advised by the health inspector to obtain some immunizations, although his chances of getting a certain tropical disorder are low. What disease has the sickle cell trait been shown to convey protection against?
Tuberculosis
Malaria
Lymphoma
Histoplasmosis
Leprosy
A 5-year-old boy is brought to the emergency department by his mother. One week ago, he developed a low grade fever followed by persistent bouts of coughing that last 20-30 minutes each. The coughing spells are severe, unresponsive to antitussive medications, and appear to worsen with eating and drinking cold liquids. On physical examination, there is subconjunctival hemorrhage and extensive subcutaneous emphysema over the anterior chest. What is the most likely organism responsible for this child's illness?
Actinomyces
Haemophilus influenza
Bordetella pertussis
Pseudomonas
Rickettsia rickettsia
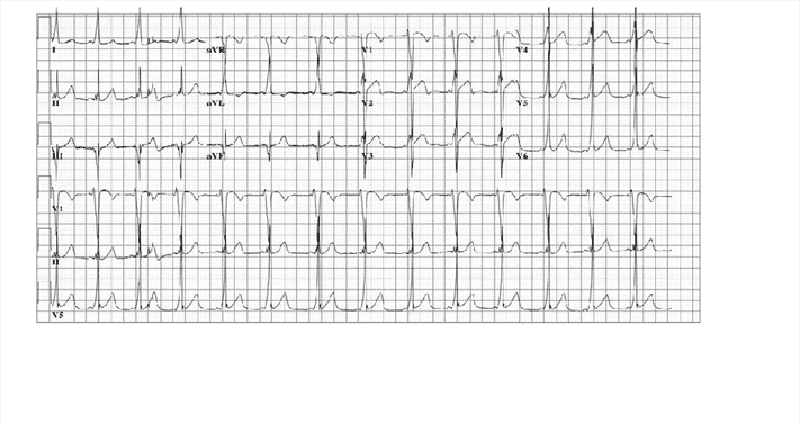
A 4-year-old girl is brought to the pediatrician’s office. Her father reports that she suddenly became pale and stopped running while he had been playfully chasing her and her pet Chihuahua. After 30 minutes, she was no longer pale and wanted to resume the game. She has never had a previous episode and has never been cyanotic. Her physical examination was normal, as were her chest x-ray and echocardiogram. An ECG showed the pattern seen on the next page, which indicates which of the following?
Paroxysmal ventricular tachycardia
Paroxysmal supraventricular tachycardia
Wolff-Parkinson-White syndrome
Stokes-Adams pattern
Excessive stress during play
{"name":"USMLE Pédiatrie (501-810) GD", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"501. A mentally retarded 14-year-old boy has a long face, large ears, micropenis, and large testes. Chromosome analysis is likely to demonstrate which of the following?, 502. A 5-month-old child with poor growth presents to the ER with generalized tonicclonic seizure activity of about 30-minute duration that stops upon the administration of lorazepam. Which of the following historical bits of information gathered from the mother is most likely to lead to the correct diagnosis in this patient?, 503. A 13-year-old girl presents with parental concerns of poor posture. She has not had any back pain. On examination, she has unequal shoulder height, asymmetric flank creases, and a forward-bending test that shows rib asymmetry. The physical examination is otherwise normal. Which of the following is the most likely cause of her condition?","img":"https://cdn.poll-maker.com/10-457719/1.png?sz=1200-000005100053"}
More Quizzes
Κεφάλαιο1 --Δεδομένα και Πληροφορία
1050
Mo Hannah
840
VERBS 6 - Centrepoint challenge
1160
How well do you know me >:3
1160
Can You Master the Venus Mutant Ninja Turtle?
201032973
Think You Know Art? Take the Famous Painters Now
201050422
Public School Policy & Services
15819912
Free IELTS Academic Writing Assessment
201022660
Free Rounding Decimals & Worksheets
201023752
Diagnostic Cytology
15823561
Injuries in Sport
15819912
Master 'Free Now' SWS Lyrics - Take the Sirens!
201030611