V. GASTROINTESTINALE Part II (101-236) Na
101. A 70-year-old woman with a history of hypertension, congestive heart failure, and atrial fibrillation presents to the ED with several hours of acute onset diffuse abdominal pain. She denies any nausea or vomiting. The pain is constant, but she is unable to localize it. She was diagnosed with a renal artery thrombosis several years ago. Vital signs include HR of 95 beats per minute, BP of 110/70 mm Hg, and temperature of 98°F. Her abdomen is soft and mildly tender, despite her reported severe abdominal pain. Her WBC count is 12,000/μL, hematocrit 38%, platelets 250/μL, and lactate 8 mg/dL. The stool is traced heme-positive. You are concerned for acute mesenteric ischemia. What is the best way to diagnose this condition?
A. Serum lactate levels
B. Abdominal radiograph (supine and upright)
C. CT scan
D. Angiography
E. Barium contrast study
102. An 81-year-old diabetic woman with a history of atrial fibrillation is transferred to your emergency department (ED) from the local nursing home. The note from the facility states that the patient is complaining of abdominal pain, having already vomited once. Her vital signs in the ED are temperature 100.1°F, blood pressure (BP) 105/75 mm Hg, heart rate (HR) 95 beats per minute, and respiratory rate (RR) 18 breaths per minute. You examine the patient and focus on her abdomen. Considering that the patient has not stopped moaning in pain since arriving to the ED, you are surprised to find that her abdomen is soft on palpation. You decide to order an abdominal radiographic series. Which of the findings on plain abdominal film is strongly suggestive of mesenteric infarction?
A. Sentinel loop of bowel
B. No gas in the rectum
C. Presence of an ileus
D. Pneumatosis intestinalis
E. Air fluid levels
103. As you palpate the right upper quadrant (RUQ) of a 38-year-old woman’s abdomen, you notice that she stops her inspiration for a brief moment. During the history, the patient states that over the last 2 days she gets pain in her RUQ that radiates to her back shortly after eating. Her vitals include a temperature of 100.4°F, HR of 95 beats per minute, BP of 130/75 mm Hg, and RR of 16 breaths per minute. What is the initial diagnostic modality of choice for this disorder?
A. Plain film radiograph
B. Computed tomography (CT) scan
C. Magnetic resonance imaging (MRI)
D. Radioisotope cholescintigraphy (HIDA scan)
E. Ultrasonography
104. An undomiciled 41-year-old man walks into the ED complaining of abdominal pain, nausea, and vomiting. He tells you that he has been drinking beer continuously over the previous 18 hours. On examination, his vitals are BP 150/75 mm Hg, HR 104 beats per minute, RR 16 breaths per minute, oxygen saturation 97% on room air, temperature of 99.1°F rectally, and finger stick glucose 81 mg/dL. The patient is alert and oriented, his pupils anicteric. You notice gynecomastia and spider angiomata. His abdomen is soft but tender in the RUQ. Laboratory tests reveal an AST of 212 U/L, ALT 170 U/L, alkaline phosphatase of 98 U/L, total bilirubin of 1.9 mg/dL, international normalized ratio (INR) of 1.3, WBC 12,000/μL. Urinalysis shows 1+ protein. Chest x-ray is unremarkable. Which of the following is the most appropriate next step in management?
A. Place a nasogastric tube in the patient’s stomach to remove any remaining ethanol.
B. Order a HIDA scan to evaluate for acute cholecystitis.
C. Administer hepatitis B immune globulin.
D. Send viral hepatitis titers.
E. Provide supportive care by correcting any fluid and electrolyte imbalances
105. A 23-year-old woman presents to the ED complaining of lower abdominal pain and vaginal spotting for 2 days. Her menstrual cycle is irregular. She has a history of ovarian cysts and is sexually active but always uses condoms. Her BP is 115/75 mm Hg, HR is 75 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. Which of the following tests should be obtained next?
A. Chlamydia antigen test.
B. β-Human chorionic gonadotropin (β-hCG).
C. Transvaginal ultrasound.
D. Abdominal radiograph.
E. Observe her abdominal pain, if it resolves discharge her with a diagnosis of menstruation.
106. A 71-year-old obese man is brought to the ED complaining of constant left mid quadrant (LMQ) abdominal pain with radiation into his back. His past medical history is significant for hypertension, peripheral vascular disease, peptic ulcer disease, kidney stones, and gallstones. He smokes a pack of cigarettes and consumes a pint of vodka daily. His BP is 145/80 mm Hg, HR is 90 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. Abdominal examination is unremarkable. An ECG is read as sinus rhythm with an HR of 88 beats per minute. An abdominal radiograph reveals normal loops of bowel and curvilinear calcification of the aortic wall. Which of the following is the most likely diagnosis?
a. Biliary colic
B. Nephrolithiasis
C. Pancreatitis
D. Small bowel obstruction (SBO)
E. Abdominal aortic aneurysm

107. A 73-year-old man is seen in the ED for abdominal pain, nausea, and vomiting. His symptoms have progressively worsened over the past 2 to 3 days. The pain is diffuse and comes in waves. He denies fever or chills, but has a history of constipation. He reports no flatus for 24 hours. Physical examination is notable for diffuse tenderness and voluntary guarding. There is no rebound tenderness. An abdominal radiograph is seen below. Which of the following is the most likely diagnosis?
A. Constipation
B. SBO
C. Cholelithiasis
D. Large bowel obstruction
E. Inflammatory bowel disease
108. For which of the following patients is an abdominal CT scan contraindicated?
A. A 52-year-old man with abdominal pain after blunt trauma, negative focused assessment with sonography for trauma (FAST) examination, BP 125/78 mm Hg, and HR 109 beats per minute
B. A 22-year-old woman with RLQ pain, negative ƒÀ-hCG, temperature 100.6‹F
C. A 45-year-old man with abdominal pain, temperature 100.5‹F, WBC 11,200/ƒÊL, BP 110/70 mm Hg, HR 110 beats per minute, and lipase 250 IU
D. A 70-year-old man with abdominal pain, an 11-cm pulsatile mass in the epigastrium, BP of 70/50 mm Hg, and HR of 110 beats per minute
E. A 65-year-old woman with right flank pain that radiates to her groin, microhematuria, BP 165/85 mm Hg, and HR 105 beats per minute
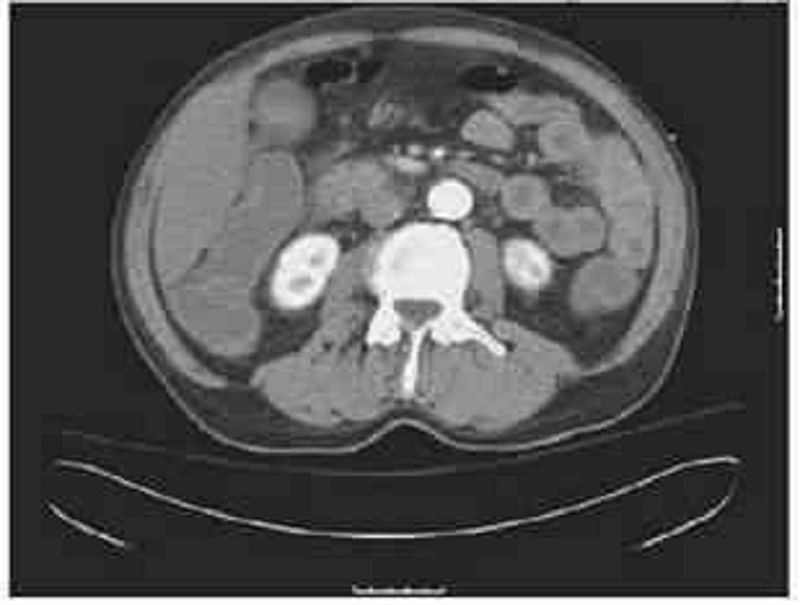
109. A 63-year-old man is brought to the ED by EMS complaining of severe abdominal pain that began suddenly 6 hours ago. His BP is 145/75 mm Hg and HR is 105 beats per minute and irregular. On examination, you note mild abdominal distention and diffuse abdominal tenderness without guarding. Stool is heme positive. Laboratory results reveal WBC 12,500/ƒÊL, haematocrit 48%, and lactate 4.2 U/L. ECG shows atrial fibrillation at a rate of 110. A CT scan is shown below. Which of the following is the most likely diagnosis?
A. Abdominal aortic aneurysm
B. Mesenteric ischemia
C. Diverticulitis
D. SBO
E. Crohn disease
110. A 21-year-old woman presents to the ED complaining of diarrhea, abdominal cramps, fever, anorexia, and weight loss for 3 days. Her BP is 127/75 mm Hg, HR is 91 beats per minute, and temperature is 100.8‹F. Her abdomen is soft and nontender without rebound or guarding. WBC is 9200/ƒÊL, ƒÀ-hCG is negative, urinalysis is unremarkable, and stool is guaiac positive. She tells you that she has had this similar presentation four times over the past 2 months. Which of the following extraintestinal manifestations is associated with Crohn disease but not ulcerative colitis?
A. Ankylosing spondylitis
B. Erythema nodosum
C. Nephrolithiasis
D. Thromboembolic disease
E. Uveitis
111. An 84-year-old woman with coronary artery disease, congestive heart failure, peripheral vascular disease, and atrial fibrillation presents to the emergency department with dizziness, weakness, and sudden-onset crampy periumbilical pain. The pain is associated with one episode of diarrhea and one episode of emesis. The patient notes she has been having similar pain after meals for gseveral monthsh but never this severe. Her temperature is 37.2‹C (98.9‹F), heart rate is 135/min, blood pressure is 96/60 mm Hg, and respiratory rate is 16/min. Physical examination is notable for a slightly distended abdomen that is extremely tender to palpation with diminished bowel sounds. There is no rigidity or rebound tenderness noted on the abdominal examination. In addition, the patient has heme positive stool. Her WBC count is 19,500/mm3, hemoglobin is 10.9 g/dL, and platelet count is 159,000/mm3. Liver function testing results are normal. After stabilizing the patient, what is the best next step in management?
(A) Barium enema
(B) Colonoscopy
(C) Laparotomy
(D) Obstruction series
(E) Warfarin therapy

112. A 2-year-old boy is brought to the emergency department. His mother reports that the patient had been well until 3 days ago, when he developed a fever and nasal congestion. He was diagnosed with otitis media in his right ear, and was started on amoxicillin with clavulanic acid by his pediatrician. He appeared to be improving until this morning, when he began to complain of abdominal pain. The pain has been intermittent, with episodes occurring every 20 minutes for several minutes each time. However, the episodes appear to be worsening and lasting longer with increasing pain. Thirty minutes ago he had an episode of nonbloody, nonbilious emesis that was followed by passage of blood- and mucus-stained stools. He is currently in no acute distress, and his vital signs are normal. A firm sausage-shaped mass is palpable in the RUQ of his abdomen. A rectal examination yields bloody mucus. He does not have any skin lesions or rashes. X-ray of the abdomen is shown in the image. Which of the following is the most likely diagnosis?
(A) Cystic fibrosis
(B) Enterocolitis
(C) Henoch-Schonlein purpura
(D) Idiopathic intussusception
(E) Meckelfs diverticulum
113. A 59-year-old man presents for his routine colonoscopy and during his visit he has numerous large adenomas removed from his colon. Which of the following is the most effective strategy for follow-up of this patient?
(A) Elective colectomy
(B) Repeat colonoscopy in 10 years
(C) Repeat colonoscopy in 3 years
(D) Sigmoidoscopy in 10 years
(E) Urgent colectomy
114. A 67-year-old woman is currently postoperative day 8 after an emergent laparoscopic cholecystectomy for acute cholecystitis. On postoperative day 2 she spiked a temperature of 40‹C (101.4‹F) and began to complain of some shortness of breath. X-ray of the chest revealed right lower lobe pneumonia, and the patient was started on clindamycin. Today she is experiencing multiple episodes of foul-smelling, watery diarrhea that is green tinged but non-bloody. She also complains of lower abdominal cramping. Her temperature is 37.8‹C (100‹F), pulse is 90/min, respiratory rate is 15/min, and blood pressure is 110/70 mm Hg. Which of the following is the most likely explanation for these findings?
(A) Ingestion of preformed enterotoxins, cytotoxins, and/or neurotoxins
(B) Production of cytotoxins within the gastro- intestinal tract
(C) Production of enterotoxins and cytotoxins within the gastrointestinal tract
(D) Production of enterotoxins within the gastrointestinal tract
(E) Viral invasion and damage of villous epithelial cells within the gastrointestinal tract

115. A male infant is delivered at 37 weeksf gestation via cesarean section for breech presentation. The pregnancy was complicated by polyhydramnios. The 34-year-old mother is rubella immune and has blood type B. She is negative for Rh antibody, Group B streptococci, rapid plasma reagin, hepatitis B surface antigen, gonorrhea, and Chlamydia. At delivery there is no meconium. He has a birth weight of 2.7 kg (6 lb). The baby has a weak cry and is pale and frothing at the nose and mouth. He has nasal flaring and retractions, with a respiratory rate of 56/min. Heart rate is 140/min and he has a regular rhythm and a harsh 2/6 holosystolic murmur that is best heard at the left sternal border. On auscultation he has fine diffuse crackles in his lungs bilaterally. The infant is missing both thumbs and has fusion of the remaining digits of his upper extremities bilaterally. The pediatric resident is able to suction secretions from the patientfs nasopharynx and oropharynx; however, she is unable to pass a nasogastric or orogastric tube more than 10 cm down. X-ray of the chest is shown in the image. Which of the following is the most likely diagnosis?
(A) Congenital diaphragmatic hernia
(B) Pyloric stenosis
(C) Respiratory distress syndrome
(D) Tracheoesophageal fistula
(E) Transient tachypnea of the new-born
116. A 51-year-old man is brought to the emergency department (ED) by emergency medical services (EMS) with a blood pressure (BP) of 90/60 mm Hg, heart rate (HR) of 110 beats per minute, respiratory rate (RR) of 18 breaths per minute, and oxygen saturation of 97% on room air. The patient tells you that he has a history of bleeding ulcers. On examination, his abdomen is tender in the epigastric area. He is guaiac positive, with black stool. He has a bout of hematemesis and you notice that his BP is now 80/50 mm Hg, HR is 114 beats per minute, as he is slowly starting to drift off. Which of the following is the most appropriate next step in therapy?
A. Assess airway, establish two large-bore intravenous (IV) lines, cross-match for two units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy.
B. Assess airway, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor.
C. Place two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy.
D. Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy.
E. Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor.
117. A 19-year-old woman presents to the ED with 1 hour of acute-onset progressively worsening pain in her RLQ. She developed nausea shortly after the pain and vomited twice over the last hour. She had similar but less severe pain 2 weeks ago that resolved spontaneously. Her BP is 123/78 mm Hg, HR is 99 beats per minute, temperature is 99.1‹F, and her RR is 16 breaths per minute. On physical examination, the patient appears uncomfortable, not moving on the gurney. Her abdomen is nondistended, diffusely tender, worst in the RLQ. Pelvic examination reveals a normal-sized uterus and moderate right-sided adnexal tenderness. Laboratory results reveal WBC 10,000/ƒÊL, hematocrit 38%, and a negative urinalysis and ƒÀ-hCG. Pelvic ultrasound reveals an enlarged right ovary with decreased flow. Which of the following is the most appropriate management for this patient?
A. Admit to the gynecology service for observation.
B. Administer IV antibiotics and operate once inflammation resolves.
C. Attempt manual detorsion.
D. Order an abdominal CT.
E. Go for immediate laparoscopic surgery.
118. A 23-year-old woman presents to the ED with RLQ pain for the last 1 to 2 days. The pain is associated with nausea, vomiting, diarrhea, anorexia, and a fever of 100.9‹F. She also reports dysuria. The patient returned 1 month ago from a trip to Mexico. She is sexually active with one partner but does not use contraception. She denies vaginal bleeding or discharge. Her last menstrual period was approximately 1 month ago. She has a history of pyelonephritis. Based on the principles of emergency medicine, what are the three priority considerations in the diagnosis of this patient?
A. Perihepatitis, gastroenteritis, cystitis
B. Ectopic pregnancy, appendicitis, pyelonephritis
C. Pelvic inflammatory disease (PID), gastroenteritis, cystitis
D. Ectopic pregnancy, PID, menstrual cramps
E. Gastroenteritis, amebic dysentery, menstrual cramps
119. A 73-year-old woman presents to the emergency room with black tarry stools and symptoms of presyncope when standing up. Digital rectal examination confirms the presence of melena. She recently started using ibuprofen for hip discomfort. Upper endoscopy confirms the diagnosis of a gastric ulcer. Which of the following is the most likely explanation for the gastric ulcer?
A. Increasing acid production
B. Causing direct epithelial cell death
C. Promoting replication of Helicobacter pylori
D. An antiplatelet effect
E. Inhibiting mucosal repair
120. A 52-year-old woman is experiencing abdominal discomfort after meals as well as early in the morning. There is no weight loss or constitutional symptoms, and she has tried antacids but experienced minimal relief. Upper endoscopy reveals a duodenal ulcer and the biopsy is negative for malignancy. Which of the following is the most appropriate next step in management?
A. 6.8 weeks of omeprazole or ranitidine
B. long-term acid suppression with omeprazole
C. Antibiotic therapy
D. Antibiotic therapy with omeprazole
E. Bismuth citrate therapy
121. A 28-year-old man presents with symptoms of frequent bowel movements, crampy abdominal pain, and the passage of mucus. There is no history of any bloody diarrhea, but recently, he developed joint discomfort in his hands, knees, and back. On examination he is thin, and his abdomen is soft with voluntary guarding in the left lower quadrant. His joints are not actively inflamed and there is an asymmetric distribution. Which of the following is the most likely diagnosis?
A. Lymphoma of the bowel
B. Amyloid infiltration
C. Chronic pancreatitis
D. Ulcerative colitis
E. Tropical sprue
122. A 64-year-old white woman presents to her primary care physician complaining of difficulty and pain with swallowing, as well as occasional chest pain. She has a history of breast cancer treated with lumpectomy and radiation, hyper- tension, high cholesterol, and ovarian polyps. She indicates that her current problem started with liquids, but has progressed to solids, and that the food gjust gets stuck in my throat.h The chest pain was once so bad that she took one of her husbandfs nitroglycerin pills and the pain subsided, but it has since occurred many times. The physician orders an x-ray of the chest, but it is not diagnostic. Manometry is conducted, and it shows uncoordinated contractions. Which of the following is the most likely diagnosis?
(A) Breast cancer relapse
(B) Diffuse esophageal spasm
(C) Esophageal cancer
(D) Myocardial infarction
(E) Nutcracker esophagus
123. A 22-year-old woman is brought to the ED by ambulance complaining of sudden onset of severe abdominal pain for 1 hour. The pain is in the RLQ and is not associated with nausea, vomiting, fever, or diarrhea. On the pelvic examination you palpate a tender right adnexal mass. The patientfs last menstrual period was 6 weeks ago. Her BP is 95/65 mm Hg, HR is 124 beats per minute, temperature is 99.8‹F, and RR is 20 breaths per minute. Which of the following are the most appropriate next steps in management?
A. Provide her oxygen via face mask and administer morphine sulfate.
B. Administer morphine sulfate, order an abdominal CT with contrast, and call an emergent surgery consult.
C. Send the patientfs urine for analysis and order an abdominal CT.
D. Bolus 2 L NS, order a type and crossmatch and ƒÀ-hCG, and call gynecology for possible surgery.
E. Provide oxygen via face mask, give morphine sulfate, and order a transvaginal ultrasound.
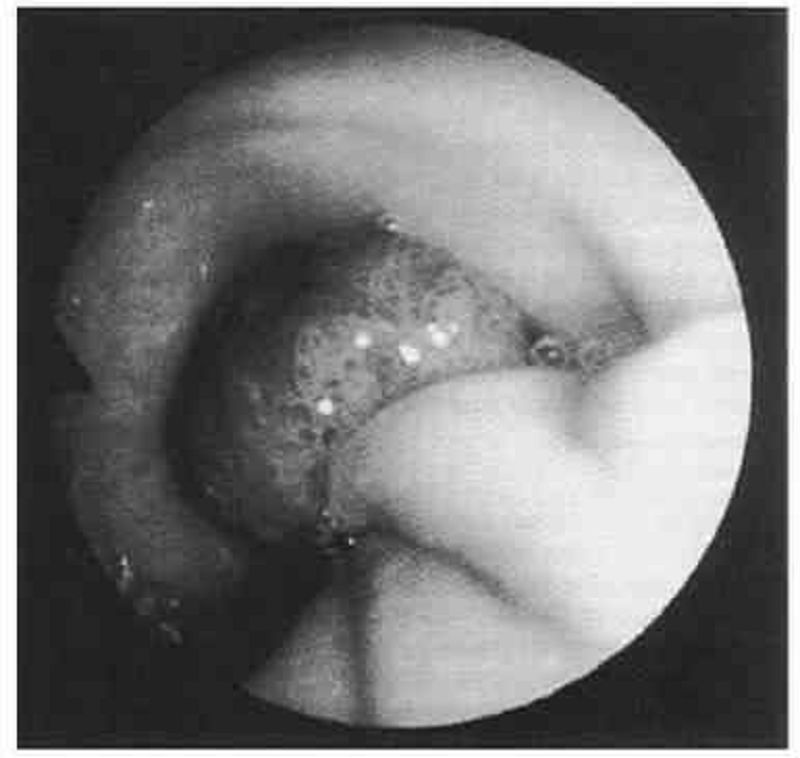
124. A 58-year-old white man complains of intermittent rectal bleeding and, at the time of colonoscopy, is found to have internal hemorrhoids and the lesion shown at the splenic flexure. Pathology shows tubulovillous changes. Repeat colonoscopy should be recommended at what interval?
A. In 1 to 2 months
B. In 1 year
C. In 3 years
D. In 10 years
E. Repeat colonoscopy is not necessary
125. A 36-year-old man presents for a well-patient examination. He gives a history that, over the past 20 years, he has had three episodes of abdominal pain and hematemesis, the most recent of which occurred several years ago. He was told that an ulcer was seen on a barium upper GI radiograph. You obtain a serum assay for H Pylori IgG, which is positive. What is the most effective regimen to eradicate this organism?
A. Omeprazole 20 mg orally once daily for 6 weeks
B. Ranitidine 300 mg orally once daily at bedtime for 6 weeks
C. Omeprazole 20 mg twice daily, amoxicillin 1000 mg twice daily, and clarithromycin 500 mg twice daily for 14 days
D. Pepto-Bismol and metronidazole twice daily for 7 days
E. Benzathine penicillin, 1.2 million units intramuscularly weekly for three doses
126. An otherwise healthy 40-year-old woman sees you because of recurrent abdominal pain. In the past month she has had four episodes of colicky epigastric pain. Each of these episodes has lasted about 30 minutes and has occurred within an hour of eating. Two of the episodes have been associated with sweating and vomiting. None of the episodes have been associated with fever or shortness of breath. She has not lost weight. She does not drink alcohol or take any prescription or over-the-counter medications. Other than three previous uneventful vaginal deliveries, she has never been hospitalized. Her examination is negative except for mild obesity (BMI = 32). A complete blood count and multichannel chemistry profile that includes liver function test is normal. A gallbladder sonogram reveals multiple gallstones. What is the next best step in the treatment of this patient?
A. Omeprazole, 20 mg daily for eight weeks.
B. Ursodeoxycholic acid
C. Observation without specific therapy
D. Laparoscopic cholecystectomy
E. Weight reduction
127. A 56-year-old chronic alcoholic has a 1-year history of ascites. He is admitted with a 2-day history of diffuse abdominal pain and fever. Examination reveals scleral icterus, spider angiomas, a distended abdomen with shifting dullness, and diffuse abdominal tenderness. Paracentesis reveals slightly cloudy ascitic fluid with an ascitic fluid PMN cell count of 1000/ƒÊL. Which of the following statements about treatment is true?
A. Antibiotic therapy is unnecessary if the ascitic fluid culture is negative for bacteria.
B. The addition of albumin to antibiotic therapy improves survival
C. Repeated paracenteses are required to assess the response to antibiotic treatment.
D. After treatment of this acute episode, a recurrent episode of spontaneous bacterial peritonitis would be unlikely.
E. Treatment with multiple antibiotics is required because polymicrobial infection is common.
128. A 60-year-old man with known hepatitis C and a previous liver biopsy showing cirrhosis requests evaluation for possible liver transplantation. He has never received treatment for hepatitis C. Though previously a heavy user of alcohol, he has been abstinent for over 2 years. He has had 2 episodes of bleeding esophageal varices. He was hospitalized 6 months ago with acute hepatic encephalopathy. He has a 1-year history of ascites that has required repeated paracentesis despite treatment with diuretics. Medications are aldactone 100 mg daily and lactulose 30 cc 3 times daily. On examination he appears thin, with obvious scleral icterus, spider angiomas, palmar erythema, gynecomastia, a large amount ascites, and small testicles. There is no asterixis. Recent laboratory testing revealed the following: hemoglobin = 12.0 mg/dL (normal 13.5-15.0), MCV = 103 fL (normal 80-100), creatinine = 2.0 mg/dL (normal 0.7-1.2), bilirubin = 6.5 mg/dL (normal 0.1-1.2), AST = 25 U/L (normal < 40), ALT= 45 U/L (normal < 40), INR = 3.0 (normal 0.8-1.2). What is the next best step?
A. Repeat liver biopsy.
B. Start treatment with interferon and ribavirin.
C. Refer the patient for hospice care.
D. Continue to optimize medical treatment for his ascites and hepatic encephalopathy and tell the patient he is not eligible for liver transplantation because of his previous history of alcohol abuse.
E. Refer the patient to a liver transplantation center.
129. A 32-year-old white woman complains of abdominal pain off and on since the age of 17. She notices abdominal bloating relieved by defecation as well as alternating diarrhea and constipation. She has no weight loss, GI bleeding, or nocturnal diarrhea. On examination, she has slight LLQ tenderness and gaseous abdominal distension. Laboratory studies, including CBC, are normal. Which of the following is the most appropriate initial approach?
A. Recommend increased dietary fiber, antispasmodics as needed, and follow-up examination in 2 months.
B. Refer to gastroenterologist for colonoscopy.
C. Obtain antiendomysial antibodies.
D. Order UGI series with small bowel follow-through.
E. Order small bowel biopsy.
130. A 27-year-old female is found to have a positive hepatitis C antibody at the time of plasma donation. Physical examination is normal. Liver enzymes reveal ALT of 62 U/L (normal < 40), AST 65 U/L (normal < 40), bilirubin 1.2 mg/dL (normal), and alkaline phosphatase normal. Hepatitis C viral RNA is 100,000 copies/mL. Hepatitis B surface antigen and HIV antibody are negative. Which of the following statements is true?
A. Liver biopsy is necessary to confirm the diagnosis of hepatitis C.
B. Most patients with hepatitis C eventually resolve their infection without permanent sequelae.
C. This patient should not receive vaccinations against other viral forms of hepatitis.
D. Serum ALT levels are a good predictor of prognosis.
E. Patients with hepatitis C genotype 2 or 3 are more likely to have a favourable response to treatment with interferon and ribavirin.
131. A 45-year-old woman presents to the ED with 1 day of painful rectal bleeding. Review of systems is negative for weight loss, abdominal pain, nausea, and vomiting. On physical examination, you note an exquisitely tender swelling with engorgement and a bluish discoloration distal to the anal verge. Her vital signs are HR 105 beats per minute, BP 140/70 mm Hg, RR 18 breaths per minute, and temperature 99‹F. Which of the following is the next best step in management?
A. Recommend warm sitz baths, topical analgesics, stool softeners, a high-fiber diet, and arrange for surgical follow-up.
B. Incision and drainage under local anesthesia or procedural sedation followed by packing and surgical follow-up.
C. Obtain a complete blood cell (CBC) count, clotting studies, type and cross, and arrange for emergent colonoscopy.
D. Excision under local anesthesia followed by sitz baths and analgesics
E. Surgical consult for immediate operative management.
132. A 68-year-old man presents to the ED 4 hours after an upper endoscopy was performed for 5 months of progressive dysphagia. During the procedure, a 1-cm ulcerated lesion was found and biopsied. Now, the patient complains of severe neck and chest pain. His vitals are as follows: BP 135/80 mm Hg, HR 123 beats per minute, RR 26 breaths per minute, and temperature 101‹F. On physical examination, he appears diaphoretic and in moderate distress with crepitus in the neck and a crunching sound over the heart. You obtain an electrocardiogram (ECG), which is notable for sinus tachycardia. After obtaining a surgical consult, which of the following is the next best step in management?
A. Perform an immediate bronchoscopy.
B. Give aspirin 325 mg and obtain a cardiology consult for possible cardiac catheterization.
C. Repeat the endoscopy to evaluate the biopsy site.
D. Perform an immediate thoracotomy.
E. Order an immediate esophagram with water-soluble agent.
133. A 65-year-old man with a history of occasional painless rectal bleeding presents with 2 to 3 days of constant, dull RLQ pain. He also complains of fever, nausea, and decreased appetite. He had a colonoscopy 2 years ago that was significant for sigmoid and cecal diverticula but was otherwise normal. On physical examination he has RLQ tenderness with rebound and guarding. His vitals include HR of 95 beats per minute, BP of 130/85 mm Hg, and temperature of 101.3‹F. The abdominal CT demonstrates the presence of sigmoid and cecal diverticula, inflammation of pericolic fat, thickening of the bowel wall, and a fluid-filled appendix. Which of the following is the most appropriate next step in management?
A. Discharge the patient with broad-spectrum oral antibiotics and surgical follow-up.
B. Begin IV hydration and broad-spectrum antibiotics, keep the patient npo (nothing by mouth), and admit the patient to the hospital.
C. Begin IV antibiotics and call a surgical consult for an emergent operative procedure.
D. Arrange for an emergent barium enema to confirm the diagnosis.
E. Begin sulfasalazine 3 to 4 g/d along with IV steroid therapy.
134. A 49-year-old man presents to the ED with nausea, vomiting, and abdominal pain that began approximately 2 days ago. The patient states that he usually drinks a six pack of beer daily, but increased his drinking to 2 six packs daily over the last week because of pressures at work. He notes decreased appetite over the last 3 days and states he has not had anything to eat in 2 days. His BP is 125/75 mm Hg, HR is 105 beats per minute, and RR is 20 breaths per minute. You note generalized abdominal tenderness on examination. Laboratory results reveal the following: White blood cells (WBC) 9000/ƒÊL Sodium 131 mEq/L Hematocrit 48% Potassium 3.5 mEq/L Platelets 210/ƒÊL Chloride 101 mEq/L Aspartate transaminase (AST) 85 U/L Bicarbonate 10 mEq/L Alanine transaminase (ALT) 60 U/L Blood urea nitrogen (BUN) 9 mg/dL Alkaline phosphatase 75 U/L Creatinine 0.5 mg/dL Total bilirubin 0.5 mg/dL Glucose 190 mg/dL Lipase 40 IU Nitroprusside test weakly positive for ketones Which of the following is the mainstay of therapy for patients with thiscondition?
A. Normal saline (NS) solution
B. Half normal saline (. NS)
C. Glucose solution (D5W)
D. Solution containing both saline and glucose (D 5/NS or D 5. NS)
E. The type of solution is irrelevant
135. A 31-year-old man from Florida presents to the ED complaining of severe pain that starts in his left flank and radiates to his testicle. The pain lasts for about 1 hour and then improves. He had similar pain last week that resolved spontaneously. He noted some blood in his urine this morning. His BP is 145/75 mm Hg, HR is 90 beats per minute, temperature is 98.9‹F, and his RR is 24 breaths per minute. His abdomen is soft and nontender. As you examine the patient, he vomits and has trouble lying still in his stretcher. Which of the following is the most appropriate next step in management?
A. Call surgery consult to evaluate the patient for appendicitis.
B. Order an abdominal CT.
C. Start intravenous (IV) fluids and administer an IV nonsteroidal anti-inflammatory drug (NSAID) and antiemetic.
D. Perform an ultrasound to evaluate for an abdominal aortic aneurysm (AAA).
E. Perform an ultrasound to evaluate for testicular torsion.
136. A 24-year-old man woke up from sleep 1 hour ago with severe pain in his right testicle. He states that he is sexually active with multiple partners. On examination, the right scrotum is swollen, tender, and firm. You cannot elicit a cremasteric reflex. His BP is 145/75 mm Hg, HR is 103 beats per minute, RR is 14 breaths per minute, temperature is 98.9‹F, and oxygen saturation is 99% on room air. Which of the following is the most appropriate next step in management?
A. Administer one dose of ceftriaxone and doxycycline for 10 days and have him follow-up with a urologist.
B. Swab his urethra, send a culture for gonorrhea and Chlamydia, and treat if positive.
C. Send a urinalysis and treat for a urinary tract infection (UTI) if positive.
D. Treat the patient for epididymitis and have him return if symptoms persist.
E. Order a statim (STAT) color Doppler ultrasound and urologic consultation.
137. A 22-year-old man presents to the ED complaining of dysuria for 3 days. He states that he has never had this feeling before. He is currently sexually active and uses a condom most of the time. He denies hematuria but notes a yellowish discharge from his urethra. His BP is 120/75 mm Hg, HR is 60 beats per minute, and temperature is 98.9‹F. You send a clean catch urinalysis to the laboratory that returns positive for leukocyte esterase and 15 white blood cells per high power field (WBCs/hpf). Which of the following is the most appropriate next step in management?
A. Send a urethral swab for culture and administer 125 mg ceftriaxone intramuscularly and 1 g azithromycin orally.
B. Send urine for culture and administer SMX/TMP orally.
C. Discharge the patient with strict instructions to return if his symptoms worsen.
D. Order a CT scan to evaluate for a kidney stone.
E. Have him follow-up immediately with a urologist to evaluate for testicular cancer.
138. A 59-year-old man presents to the ED complaining of vomiting and sharp abdominal pain in the epigastric area that began abruptly this afternoon. He describes feeling nauseated and has no appetite. Laboratory results reveal WBC 18,000/ƒÊL, hematocrit 48%, platelets 110/ƒÊL, AST 275 U/L, ALT 125 U/L, alkaline phosphatase 75 U/L, amylase 1150 U/L, lipase 1450 IU, LDH 400 U/L, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 110 mEq/L, bicarbonate 20 mEq/L, BUN 20 mg/dL, creatinine 1.5 mg/dL, and glucose 250 mg/dL. Which of the following laboratory results correlate with the poorest prognosis?
A. Amylase 950, lipase 1250, LDH 400
B. Lipase 1250, LDH 400, bicarbonate 20
C. Lipase 1250, creatinine 1.5, potassium 3.5
D. WBC 18,000, LDH 400, glucose 250
E. WBC 18,000, amylase 950, lipase 1250
139. An 18-year-old woman presents to the ED complaining of acute onset of RLQ abdominal pain. She also describes the loss of appetite over the last 12 hours, but denies nausea and vomiting. Her BP is 124/77 mm Hg, HR is 110 beats per minute, temperature is 102.1‹F, RR is 16 breaths per minute, and oxygen saturation is 100% on room air. Abdominal examination reveals lower abdominal tenderness bilaterally. On pelvic examination you elicit cervical motion tenderness and note cervical exudates. Her WBC is 20,500/ƒÊL and ƒÀ-hCG is negative. Which of the following is the most appropriate next step in management?
A. Bring her to the OR for an appendectomy.
B. Begin antibiotic therapy.
C. Perform a culdocentesis.
D. Bring her to the OR for immediate laparoscopy.
E. Order an abdominal plain film.
140. A 27-year-old man is seen in the ED for a leak around a surgical G-tube that was placed 2 weeks ago and has been used for enteral feeding for 1 week. Inspection reveals the tube is pulled out from the stoma, but is still in the cutaneous tissue. The abdomen is soft and nondistended and there are no signs of skin infection. Which of the following is the most appropriate next step in management?
A. Insert a Foley catheter into the tract and aspirate. If gastric contents are aspirated the tube can be used for feeding.
B. Insert a Foley catheter into the tract, instill water-soluble contrast, and obtain an abdominal radiograph prior to using for feeding.
C. Remove the tube and admit the patient for observation.
D. Remove the tube and immediately obtain a CT scan of the abdomen.
E. Return to the OR for closure of gastrotomy and placement of a new tube.
141. A 30-year-old man presents to the ED complaining of sudden onset of abdominal bloating and back pain lasting for 2 days. The pain woke him up from sleep 2 nights ago. It radiates from his back to his abdomen and down toward his scrotum. He is in severe pain and is vomiting. His temperature is 101.2‹F and HR is 107 beats per minute. A CT scan reveals a 9-mm obstructing stone of the left ureter with hydronephrosis. Urinalysis is positive for 2+ blood, 2+ leukocytes, 2+ nitrites, 40 to 50 WBCs, and many bacteria. You administer pain medicine, antiemetics, and antibiotics. Which of the following is the most appropriate next step in management?
A. Admit for IV antibiotics and possible surgical removal of stone.
B. Observe in ED for another 6 hours to see if stone passes.
C. Discharge with antibiotics and pain medicine.
D. Discharge patient with instructions to consume large amounts of water.
E. Discharge patient with antibiotics, pain medicine, and instructions to drink large amounts of water and cranberry juice.
142. A 24-year-old woman presents to the ED after being sexually assaulted. She is a college student with no past medical history. Her BP is 130/75 mm Hg, HR is 91 beats per minute, temperature is 98.6‹F, and RR is 16 breaths per minute. On physical examination you observe vaginal trauma and scattered bruising and abrasions. Which of the following medications should be offered to the patient in this scenario?
A. Ceftriaxone, azithromycin, metronidazole, antiretrovirals, emergency contraception
B. Ceftriaxone, tetanus, metronidazole, antiretrovirals, emergency contraception
C. Ceftriaxone, azithromycin, tetanus, metronidazole, emergency contraception
D. Ceftriaxone, azithromycin, tetanus, antiretrovirals, emergency contraception
E. Ceftriaxone, azithromycin, tetanus, metronidazole, antiretrovirals, emergency contraception
143. A 43-year-old man presents to the ED complaining of progressively worsening abdominal pain over the past 2 days. The pain is constant and radiates to his back. He also describes nausea and vomiting and states he usually drinks six pack of beer daily, but has not had a drink for 2 days. His BP is 144/75 mm Hg, HR is 101 beats per minute, temperature is 99.8‹F, and RR is 14 breaths per minute. He is lying on his side with his knees flexed. Examination shows voluntary guarding and tenderness to palpation of his epigastrium. Laboratory results reveal WBC 10,500/ƒÊL, hematocrit 51%, platelets 225/ƒÊL, and lipase 620 IU. An abdominal radiograph reveals a nonspecific bowel gas pattern. There is no free air under the diaphragm. Which of the following is the most appropriate next step in management?
A. Observe in the ED.
B. Send home with antibiotic therapy.
C. Admit to the hospital for endoscopy.
D. Admit to the hospital for exploratory laparotomy.
E. Admit to the hospital for medical management and supportive care.
144. A 77-year-old woman is brought to the emergency room because of nonspecific abdominal discomfort. She has no anorexia, fever, chills, or weight loss. Her abdomen is soft and non-tender on physical examination. Abdominal x-rays show lots of stool in the colon, but no free air or air-fluid levels. The amylase is 150 U/L (25.125U/L), and the rest of her biochemistry and complete blood count are normal. Which of the following conditions can cause a false positive elevation in the serum amylase?
A. maturity-onset diabetes mellitus (DM)
B. Gastric ulcer
C. Renal failure
D. Sulfonamide therapy
E. Gastric carcinoma
145. A 76-year-old woman with a history of congestive heart failure, coronary artery disease, and an girregular heart beath is brought to the ED by her family. She has been complaining of increasing abdominal pain over the past several days. She denies nausea or vomiting and bowel movements remain unchanged. Vitals are HR of 114 beats per minute, BP 110/75 mm Hg, and temperature 98‹F. On cardiac examination, her HR is irregularly irregular with no murmur detected. The abdomen is soft, nontender, and nondistended. The stool is heme-positive. This patient is at high risk for which of the following conditions?
A. Perforated gastric ulcer
B. Diverticulitis
C. Acute cholecystitis
D. Mesenteric ischemia
E. Sigmoid volvulus
146. A 78-year-old man with a history of atherosclerotic heart disease and congestive heart failure presents with increasing abdominal pain. The pain began suddenly a day ago and has progressively worsened since then. He denies nausea, vomiting, and diarrhea, but states that he had black tarry stool this morning. He denies any history of prior episodes of similar pain. Vitals are BP 120/65 mm Hg, HR 105 beats per minute, and temperature 99‹F. The patient is at high risk for which of the following conditions?
A. Cholecystitis
B. Cecal volvulus
C. Mesenteric ischemia
D. Perforated peptic ulcer
E. Small bowel obstruction
147. A 22-year-old woman presents with chronic diarrhea. She has no abdominal discomfort, feels well, and reports no weight loss or systemic symptoms. Physical examination reveals a healthy young woman who is 5f7h tall and weighs 150 lb. The complete physical examination is normal. Which of the following is the most likely cause of a secretory diarrhea in this young woman?
A. Surreptitious use of stimulant laxatives
B. Carcinoid tumor
C. Ulcerative colitis
D. Lactose deficiency
E. Celiac disease
148. A 23-year-old woman presents with weight loss and chronic diarrhea. She appears unwell and cachectic. Routine laboratory tests reveal a low hemoglobin level and an increased international normalized ratio (INR) even though she is not taking any anticoagulants. The liver enzymes are normal, but the albumin and calcium levels are low, suggesting generalized malnutrition. Which of the following is the most appropriate initial diagnostic test for malabsorption?
A. Xylose absorption
B. Schilling test
C. x-ray studies
D. Stool fat quantitation
E. Small intestinal biopsy
149. A 29-year-old man with acquired immune deficiency syndrome (AIDS) comes to the emergency department because of progressively increasing abdominal discomfort. Examination shows voluntary guarding in the upper abdomen. His biochemistry is normal except for an elevated amylase at 370 U/L (25–125 U/L). Which of the following infections can trigger this disorder in AIDS patients?
A. toxoplasmosis
B. Mycobacterium avium complex
C. Mycobacterium tuberculosis
D. Pneumocystis carinii
E. Herpes virus
150. A full-term 5-day-old African-American girl is taken to the pediatrician because her “eyes look yellow.” She is being exclusively formula- fed with an iron-rich formula. She has six wet diapers a day and stools twice a day. The pregnancy was uncomplicated and she was delivered by spontaneous vaginal delivery. Her Apgar scores were 9 and 10 at 1 and 5 minutes, respectively. Her temperature is 37°C (98.6°F), her head circumference is in the 50th percentile, and her weight is 3420 g (3 g below her birth weight). Her sclerae are icteric. There is no hepatomegaly or splenomegaly. Her total bilirubin is 9 mg/dL and her conjugated bilirubin is 0.2 mg/dL. Hemoglobin is 15 g/dL. Which of the following is the most likely diagnosis?
(A) á1-Antitrypsin deficiency
(B) Biliary atresia
(C) Dubin-Johnson syndrome
(D) Physiologic jaundice
(E) Rotor syndrome

151. A 76-year-old man who has had multiple episodes of pancreatitis presents to his physician’s office with mild epigastric pain and 9.1-kg (20.0-lb) weight loss over the past 6 months. The patient also describes daily foul-smelling stools that “float” in the toilet bowl. The physician pulls up his electronic medical record and finds that the patient presented to the emergency department last week for the same symptoms. During that visit he had a CT of the abdomen (see image). Which of the following is the most appropriate treatment?
(A) Endoscopic retrograde cholangiopancreatography
(B) Pancreatic enzyme replacement
(C) Pancreaticogastrostomy
(D) Surgical resection of pancreas
(E) Whipple procedure
152. A 50-year-old man with a history of alcohol and tobacco abuse has complained of difficulty swallowing solid food for the past 2 months. More recently, swallowing fluids has also become a problem. He has noted black, tarry stools on occasion. The patient has lost 10 lb. Which of the following statements is correct?
A. A CT scan of the abdomen and pelvis is the best next test.
B. Barium contrast esophagram will likely establish a diagnosis
C. The most likely diagnosis is peptic ulcer disease.
D. The patient has achalasia.
E. Herpes simplex virus infection of the esophagus is likely
153. A 34-year-old man presents with substernal discomfort. The symptoms are worse after meals, particularly a heavy evening meal, and are sometimes associated with hot/sour fluid in the back of the throat and nocturnal awakening. The patient denies difficulty swallowing, pain on swallowing, or weight loss. The symptoms have been present for 6 weeks; the patient has gained 20 lb in the past 2 years. Which of the following is the most appropriate initial approach?
A. Therapeutic trial of ranitidine
B. Exercise test with thallium imaging
C. Esophagogastroduodenoscopy
D. CT scan of the chest
E. Coronary angiography
154. A 48-year-old woman presents with a change in bowel habit and 10-lb weight loss over the past 2 months despite preservation of appetite. She notices increased abdominal gas, particularly after fatty meals. The stools are malodorous and occur 2 to 3 times per day; no rectal bleeding is noticed. The symptoms are less prominent when she follows a clear liquid diet. Which of the following is the most likely histological abnormality associated with this patient’s symptoms?
A. Signet ring cells on gastric biopsy
B. Mucosal inflammation and crypt abscesses on sigmoidoscopy
C. Villous atrophy and increased lymphocytes in the lamina propria on small bowel biopsy
D. Small, curved gram-negative bacteria in areas of intestinal metaplasia on gastric biopsy
E. Periportal inflammation on liver biopsy
155. A 62-year-old woman is transferred to the medical service with an appendiceal mass serendipitously picked up at the edge of an x-ray taken of a broken femur in the emergency department. Otherwise, the patient has no significant past medical history and no current symptoms. Which of the following studies is most likely to be useful?
(A) Arterial blood gas
(B) CT of the chest and abdomen
(C) Immediate ECG
(D) MRI of the chest and abdomen
(E) Room air oxygen saturation
156. A 60-year-old woman complains of fever and constant left lower quadrant pain of 2 days duration. She has not had vomiting or rectal bleeding. She has a history of hypertension but is otherwise healthy. She has never had similar abdominal pain, and has had no previous surgeries. Her only regular medication is lisinopril. On examination blood pressure is 150/80, pulse 110, and temperature 38.9°C (102°F). She has normal bowel sounds and left lower quadrant abdominal tenderness with rebound. A complete blood count reveals WBC = 28,000. Serum electrolytes, BUN, creatinine and liver function tests are normal. What is the next best step in evaluating this patient’s problem?
A. Colonoscopy
B. Barium enema
C. Exploratory laparotomy
D. Ultrasound of the abdomen
E. CT scan of the abdomen and pelvis
157. A 72-year-old woman notices progressive dysphagia to solids and liquids. There is no history of alcohol or tobacco use, and the patient takes no medications. She denies heartburn, but occasionally notices the regurgitation of undigested food from meals eaten several hours before. Her barium swallow is shown. Which of the following is the cause of this condition?
A. Growth of malignant squamous cells into the muscularis mucosa
B. Scarring caused by silent gastroesophageal reflux
C. Spasm of the lower esophageal sphincter
D. Loss of intramural neurons in the esophagus
E. Psychiatric disease
158. A 37-year-old woman presents for evaluation of abnormal liver chemistries. She has long-standing obesity (current BMI 38) and has previously taken anorectic medications but not for the past several years. She takes no other medications and has not used parenteral drugs or had high risk sexual exposure. On examination, her liver span is 13 cm; she has no spider angiomas or splenomegaly. Several sets of liver enzymes have shown transaminases two to three times normal. Bilirubin and alkaline phosphatase are normal. Hepatitis B surface antigen and hepatitis C antibody are normal, as are serum iron and total iron-binding capacity. Which of the following is the likely pathology on liver biopsy?
A. Macrovesicular fatty liver
B. Microvesicular fatty liver
C. Portal triaditis with piecemeal necrosis
D. Cirrhosis
E. Copper deposition
159. A 20-year-old man presents to the ED with fever and severe right lower quadrant (RLQ) pain for 1 day. Prior to this episode, he reports 2 months of crampy abdominal pain, generalized malaise, a 10-lb weight loss, and occasional bloody diarrhea. On examination, his HR is 115 beats per minute, BP is 125/70 mm Hg, RR is 18 breaths per minute, and temperature is 100.8°F. His only significant past medical history is recurrent perirectal abscesses. On physical examination, the patient appears uncomfortable and has a tender mass in the RLQ, without guarding or rebound. Rectal examination is positive for trace heme-positive stool. An abdominal computed tomographic (CT) scan reveals no periappendiceal fat stranding. There is inflammation of the distal ileum and several areas of the colon. There are no rectal inflammatory changes. Which of the following is the most likely diagnosis?
A. Crohn disease (CD)
B. Ulcerative colitis (UC)
C. Appendicitis
D. Pseudomembranous enterocolitis
E. Diverticulitis
160. A 55-year-old white woman with a history of iron deficiency anemia has had intermittent trouble swallowing solids for the past few years. She denies alcohol or tobacco use. Her vital signs are stable. Her iron level is 40μg/dL and total iron binding capacity is 500 μg/dL. Other laboratory tests are within normal limits. Which of the following is the most likely diagnosis?
(A) Achalasia
(B) Barrett’s esophagus
(C) Esophageal carcinoma
(D) Mallory-Weiss syndrome
(E) Plummer-Vinson syndrome
161. A 55-year-old man from China is known to have chronic liver disease, secondary to hepatitis B infection. He has recently felt unwell, and his hemoglobin level has increased from 130 g/L, 1 year ago, to 195 g/L. Which of the following is the most appropriate initial diagnostic test?
A. Alkaline phosphatase
B. alpha-fetoprotein (AFP)
C. Aspartate transaminase (AST)
D. Alanine transaminase (ALT)
E. Unconjugated bilirubin
162. A 67-year-old man is brought to the ED by emergency medical service (EMS). His wife states that the patient was doing his usual chores around the house when all of a sudden he started complaining of severe abdominal pain. He has a past medical history of coronary artery disease and hypertension. His BP is 85/70 mm Hg, HR is 105 beats per minute, temperature is 98.9°F, and his RR is 18 breaths per minute. On physical examination, he is diaphoretic and in obvious pain. Upon palpating his abdomen, you feel a large pulsatile mass. An electrocardiogram (ECG) reveals sinus tachycardia. You place the patient on a monitor, administer oxygen, insert two largebore IVs, and send his blood to the laboratory. His BP does not improve after a 1-L fluid bolus. Which of the following is the most appropriate next step in management?
A. Order a CT scan to evaluate his aorta.
B. Call the angiography suite and have them prepare the room for the patient.
C. Order a portable abdominal radiograph.
D. Call surgery and have them prepare the operating room (OR) for an exploratory laparotomy.
E. Call the cardiac catheterization laboratory to prepare for stent insertion.
163. A 48-year-old man with a past medical history of hepatitis C and cirrhosis presents to the ED complaining of acute-onset abdominal pain and chills. His BP is 118/75 mm Hg, HR is 105 beats per minute, RR is 16 breaths per minute, temperature is 101.2°F rectally, and oxygen saturation is 97% on room air. His abdomen is distended, and diffusely tender. You decide to perform a paracentesis and retrieve 1 L of cloudy fluid. Laboratory analysis of the fluid shows a neutrophil count of 550 cells/mm 3. Which of the following is the most appropriate choice of treatment?
A. Metronidazole
B. Vancomycin
C. Sulfamethoxazole/trimethoprim (SMX/TMP)
D. Neomycin and lactulose
E. Cefotaxime
164. A 64-year-old woman develops sudden-onset abdominal discomfort after eating a large meal. The pain is constant, localizes to the epigastric area with radiation to her right scapula. She also has nausea and vomiting. It eventual subsides 1 hour later. An ultrasound of the abdomen reveals a dilated common bile duct secondary to stones. Which of the following statements regarding common bile duct stones is most likely true?
A. All originate in the gallbladder
B. Always produce jaundice
C. Produce constant level of jaundice
D. Can be painless
E. Indicate anomalies of the bile duct
165. A 29-year-old woman complains of dysphagia with both solids and liquids, worse when she is eating quickly or is anxious. Manometry reveals normal basal esophageal sphincter pressure, with no relaxation of the sphincter on swallowing. Which of the following is the most appropriate next step in management?
A. beta-blocker therapy
B. Partial esophagectomy
C. Anticholinergic drugs
D. Calcium channel blockers
E. Dietary modification
166. A 33-year-old woman develops mild epigastric abdominal pain with nausea and vomiting of 2 days duration. Her abdomen is tender on palpation in the epigastric region, and the remaining examination is normal. Her white count is 13,000/mL, and amylase is 300 U/L (25–125 U/L). Which of the following is the most common predisposing factor for this disorder?
A. drugs
B. gallstones
C. malignancy
D. alcohol
E. hypertriglyceridemia
167. A 54-year-old man complains of burning epigastric pain that usually improves after a meal, and is occasionally relieved with antacids. On examination, he appears well and besides some epigastric tenderness on palpation, the rest of the examination is normal. Upper endoscopy confirms a duodenal ulcer. Which of the following statements concerning PUD is most likely correct?
A. Duodenal ulcer is seen more often in older people than is gastric ulcer
B. clinically, gastric ulcers are more common than duodenal ulcers
C. Duodenal ulcers can frequently be malignant
D. Infection can cause both types of peptic ulcer
E. Peptic gastric ulcers are usually quite proximal in the stomach
168. A 30-year-old man complains of chronic diarrhea for the past 6 months. There is no weight loss, fever, or abdominal pain. He takes no medications and feels fine. His physical examination is completely normal. Further history reveals that this man does not take laxatives; however, in an effort to stay slim he eats a lot of sugar-free gum and sugarless candy. Which of the following explanations is the most likely cause of his diarrhea?
A. Direct stimulant effect of chemicals in the candies
B. Lack of fiber in his diet
C. Pancreatic insufficiency secondary to chronic protein-calorie malnutrition
D. Secondary intestinal mucosal atrophy
E. Nonabsorbed carbohydrates
169. A 32-year-old man with Crohn’s disease presents to the emergency department with acute-onset diffuse abdominal pain and emesis. The patient states these symptoms are different than his usual Crohn’s disease flare-ups. The pain is severe (10/10) and is cramping in nature. He says his abdomen feels larger than usual. His Crohn’s disease has been well managed on 6-mercaptopurine for the past 6 months. The patient denies any recent sick contacts or eating underprepared foods. He states he had a bowel movement and flatus since the abdominal pain began. In addition to Crohn’s disease, the patient had appendicitis for which he underwent an appendectomy 12 years ago. His temperature is 37.1°C (98.7°F), blood pressure is 135/86 mm Hg, pulse is 84/min, and respiratory rate is 14/ min. On physical examination the abdomen is distended and diffusely tender with high-pitched bowel sounds. There is rebound tenderness throughout the abdomen along with guarding. The remainder of the physical examination is noncontributory. An x-ray of the abdomen shows dilated small loops of bowel along with absence of gas in the colon. What is the best next step in management?
(A) Bowel rest only
(B) Intravenous fluids and antibiotics only
(C) Laparotomy
(D) MRI of the abdomen
(E) Ultrasound
170. A 39-year-old Japanese-American woman with insulin-dependent diabetes and asthma presents to her primary care physician complaining of trouble swallowing for the past few months. She explains that it started with solids, and then progressed to liquids. She states it now is hard even to swallow water and that she is often very thirsty. She says she has lost about 3.2 kg (7 lb), but says she is working out frequently. Her blood pressure is 118/76 mm Hg, pulse is 86/min, respiratory rate is 16/min, and temperature is 37.2°C (98.9°F). Laboratory tests show Na+: 144 mEq/L K+: 4.0 mEq/L Cl−: 100 mEq/L Carbon dioxide: 22 mmol/L Blood urea nitrogen: 18 mg/dL Creatinine: 1.0 mg/dL Glucose: 88 mg/dL Her hemoglobin A1c level, measured 3 months earlier, was 6.1%. A barium swallow is per- formed, which reveals a dilated esophagus, especially distally, that flares out near the lower esophageal junction. Still not completely sure of the diagnosis, esophageal manometry is performed, which reveals abnormal peristalsis and increased lower sphincter pressure. Which of the following is the most appropriate management?
(A) Cholinergic agents
(B) Glucose pharmacotherapy
(C) Instructions to elevate the bed, avoid fatty foods, and consider a histamine blocker
(D) Pneumatic dilation
(E) Surgery to remove diverticula
171. A 42-year-old previously well woman presents with pruritus. She is not taking any medications, and only drinks alcohol on a social basis. Her physical examination is entirely normal with no signs of chronic liver disease or jaundice. Laboratory evaluation reveals an alkaline phosphatase level of three times normal, and an ultrasound of the liver and gallbladder is normal. Which of the following is the most appropriate next step in diagnosis?
A. INR or prothrombin time
B. Antinuclear antibodies
C. Protein immunoelectrophoresis
D. Abdominal ultrasound
E. Antimitochondrial antibodies

172. A 22-year-old man with inflammatory bowel disease is noted to have a “string sign” in the ileal area on barium enema. In which of the following conditions is this sign most often seen?
A. In the stenotic or nonstenotic phase of the disease
B. In the stenotic phase only
C. As a rigid, nondistensible phenomenon
D. With gastric involvement
E. With rectal involvement
173. A 24-year-old man with a history of depression is brought to the emergency room because of a drug overdose. He is experiencing some nausea and vomiting, but no other symptoms. Physical examination and vital signs are normal. Six hours prior to presentation, he intentionally took 40 tablets of acetaminophen (500mg/tablet). Which of the following is the most appropriate next step in management?
A. Give ethanol to compete with the parent drug for metabolism, therefore preventing formation of toxic metabolites
B. give Narcan to block its actions directly
C. Give intravenous prostacyclins to maintain cellular integrity
D. give N-acetylcysteine to allow binding of the toxic metabolite
E. Give glucocorticoids to block the immune cascade
174. A 16-year-old girl is referred to the office because of chronic diarrhea and weight loss. She is experiencing large-volume watery diarrhea that is painless. The symptoms persist even when she is fasting, and there is no relationship to foods or liquids. She is not on any medications, and there is no travel history or other constitutional symptoms. Her physical examination is normal. Which of the following is the most likely diagnosis?
A. Partial small bowel obstruction
B. Partial large bowel obstruction
C. Osmotic diarrhea
D. Secretory diarrhea
E. Inflammatory bowel disease
175. A 55-year-old man is brought to the ED by his family. They state that he has been vomiting large amounts of bright red blood. The patient is an alcoholic with cirrhotic liver disease and a history of portal hypertension and esophageal varices. His vitals on arrival are HR 110 beats per minute, BP 80/55 mm Hg, RR 22 breaths per minute, and temperature 99°F. The patient appears pale and is in moderate distress. Which of the following is an inappropriate option in the initial management of a hypotensive patient with a history of known esophageal varices presenting with hematemesis?
a. Sengstaken-Blakemore tube placement
B. Two large-bore IV lines and volume repletion with crystalloid solutions
C. Nasogastric (NG) lavage
D. IV octreotide
E. Gastrointestinal (GI) consult
176. A 59-year-old woman presents to the ED complaining of worsening lower abdominal pain over the previous 3 days. She describes feeling constipated recently and some burning when she urinates. Her BP is 135/75 mm Hg, HR is 89 beats per minute, temperature is 101.2°F, and her RR is 18 breaths per minute. Her abdomen is mildly distended, tender in the LLQ, and positive for rebound tenderness. CT scan is consistent with diverticulitis with a 7-cm abscess. Which of the following is the most appropriate management for this condition?
A. Reserve the OR for emergent laparotomy.
B. Start treatment with ciprofloxacin and metronidazole and plan for CT-guided draining of the abscess.
C. Give an IV dose of ciprofloxacin and have the patient follow up with her primary physician.
D. Start treatment with ciprofloxacin and metronidazole and plan for an emergent barium enema.
E. Start treatment with ciprofloxacin and metronidazole and prepare for an emergent colonoscopy.
177. A 60-year-old man is brought to the ED complaining of generalized crampy abdominal pain that occurs in waves. He has been vomiting intermittently over the last 6 hours. His BP is 150/75 mm Hg, HR is 90 beats per minute, temperature is 99.8°F, and his RR is 16 breaths per minute. On abdominal examination you notice an old midline scar across the length of his abdomen that he states was from surgery after a gunshot wound as a teenager. The abdomen is distended with hyperactive bowel sounds and mild tenderness without rebound. An abdominal plain film confirms your diagnosis. Which of the following is the most appropriate next step in management?
A. Begin fluid resuscitation, bowel decompression with a nasogastric tube, and request a surgical consult.
B. Begin fluid resuscitation, administer broad-spectrum antibiotics, and admit the patient to the medical service.
C. Begin fluid resuscitation, give the patient stool softener, and administer a rectal enema.
D. Begin fluid resuscitation, administer broad-spectrum antibiotics, and observe the patient for 24 hours.
E. Order an abdominal ultrasound, administer antiemetics, and provide pain relief.
178. A 52-year-old man has suffered with chronic diarrhea for several years, but has refused to see a doctor. He finally comes because he is having trouble driving at night, because of difficulty seeing. Physical examination reveals a slender, pale, unwell-looking man. He has a microcytic anemia, low calcium, and albumin levels. Which of the following is the most likely cause for his diarrhea?
A. malabsorption
B. Osmotic diarrhea
C. Secretory diarrhea
D. Inflammatory bowel disease
E. Colonic tumor
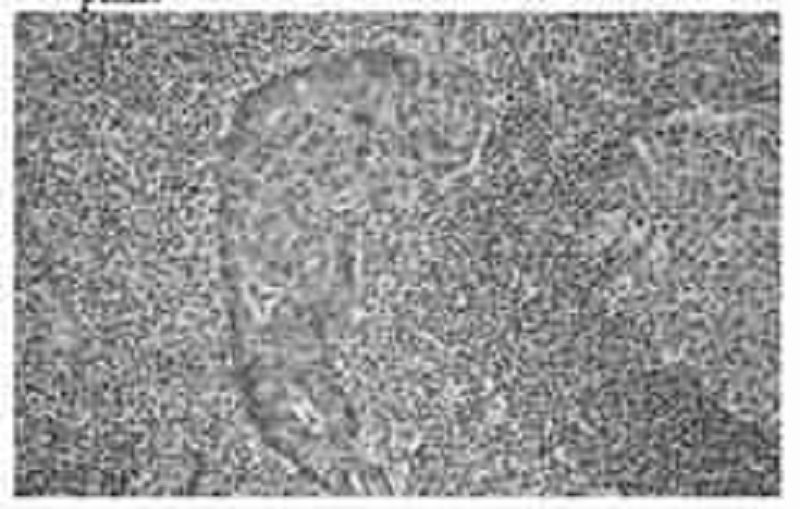
179. A 54-year-old man presents to his primary care provider with the complaint of upper abdominal fullness and pain. He states that he has lost 2.3-4.6 kg (5-10 lb), but denies other symptoms. Physical examination reveals a firm mass in the epigastric area. Ultrasonography reveals a mass in the gastric antrum. A salivary gland biopsy reveals the pathology shown in the image. Which of the following therapies is expected to be part of his treatment plan?
(A) Antibiotic therapy
(B) Bone marrow transplantation
(C) Gene therapy
(D) Liver transplantation
(E) Multiagent chemotherapy
180. A 55-year-old white man with a 20-year history of gastroesophageal reflux visits the clinic for worsening reflux symptoms over the past 18 months. His last visit was 7 years ago and he claims to be otherwise in good health. He has been compliant with his antireflux medications, including an H2-blocker and a proton pump inhibitor. Which of the following is the best next step in management?
A) Double the dose of his H2-blocker and schedule him for follow-up in 4 weeks
(B) Double the dose of his proton pumps inhibitor and schedule him for follow-up in 4 weeks
(C) Perform an esophagoscopy
(D) Schedule him for elective esophagectomy
(E) Schedule him for emergent Nissen fundoplication
181. The physician on call is paged to the well-baby nursery because a full-term, 3-hour-old boy has had green emesis twice, once after each of his feedings. He is being breast-fed. He was born by spontaneous vaginal delivery following a pregnancy complicated by polyhydramnios. His Apgar scores were 8 and 9 at 1 and 5 minutes, respectively. His temperature is 37°C (98.6°F), blood pressure is 70/50 mm Hg, pulse is 150/min, and respiratory rate is 24/ min. His upper abdomen is distended, soft, and without palpable masses. Air is visualized in the duodenum and the stomach on x-ray. Which of the following is the most likely diagnosis?
(A) Duodenal atresia
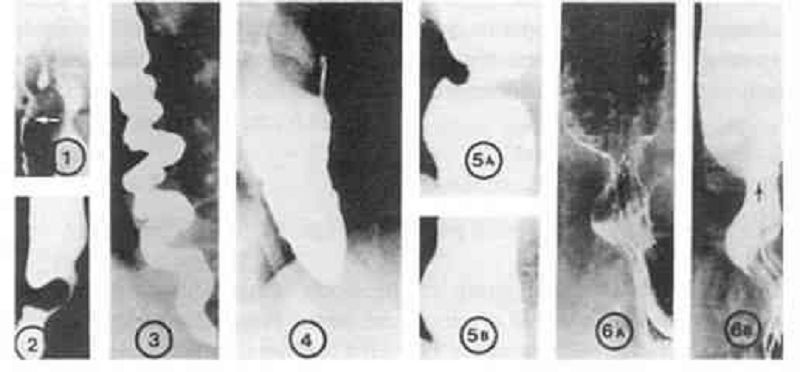
(B) Hirschsprung’s disease
(C) Intussusception
(D) Malrotation with volvulus
(E) Pyloric stenosis
182. A 68-year-old African-American man presents to his primary care physician for a check-up. He has not been to the physician’s office in over 15 years. He reports that he is fine but that his wife keeps telling him that he has to “go see the doctor.” He says he has never been sick, despite smoking three packs of cigarettes per day for over 40 years. He also says that he drinks 2–3 beers a night but never had a problem with that either. He’s as healthy “as a bull,” he says. His wife is in the room and says that he recently has had some problems swallowing food and that he is losing weight. He laughs and says, “I just need to chew more and eat more.” His vital signs are normal, as are his laboratory values. The physician is concerned and orders an endoscopy, which reveals a biopsy positive for squamous cell carcinoma of the esophagus. Which of the following most likely could have prevented this condition?
(A) Avoiding fruits and vegetables
(B) Eating more meats, especially smoked meats
(C) Eliminating smoking and alcohol consumption
(D) Getting a colonoscopy every 5 years
(E) Taking proton pump inhibitors regularly

183. A 58-year-old man comes to the emergency department complaining of colicky abdominal pain over the past 3 days that suddenly became more severe and constant over the past 6 hours. A contrast study is performed and results are shown in the image. What is the first-line treatment after fluid resuscitation and nasogastric tube placement?
(A) Colonoscopy
(B) Hemicolectomy
(C) Proximal colostomy with delayed resection
(D) Sigmoid colectomy
(E) Sigmoidoscopy
184. A full-term 6-day-old boy presents to a physician’s office for routine care. He is tolerating breast milk well. He is urinating, defecating, and sleeping normally. Physical examination reveals an alert newborn with mild eczema, good skin turgor, normal reflexes, and a musty odor. His newborn laboratory screen is notable for phenylketones in the urine. What is the best advice to give his parents regarding the boy’s diet?
(A) Increase iron
(B) Increase niacin
(C) Increase phenylalanine
(D) Increase tyrosine
(E) Increase vitamin D
185. A 59-year-old woman with renal cell carcinoma presents to the emergency department with severe right upper quadrant (RUQ) pain. She is afebrile, acutely tender in the RUQ, and has shifting dullness and a palpable liver edge. Murphy’s sign is negative. Laboratory studies show: Na+: 138 mEq/L K+: 3.6 mEq/L Glucose: 80 mg/dL Aspartate aminotransferase: 50 U/L Alanine aminotransferase: 43 U/L Alkaline phosphatase: 138 U/L Total protein: 6.4 g/dL Albumin: 3.8 g/dL Total bilirubin: 1.1 mg/dL Imaging demonstrates a spider web of collateral veins in the liver. Although extensive measures are taken, the patient dies 6 hours after arriving. Which of the following was the most likely initial treatment?
(A) β-Blocker followed by lactulose
(B) Cholecystectomy
(C) Endoscopic retrograde cholangiopancreatography with dilation of the common bile duct
(D) Exploratory laparotomy
(E) Tissue plasminogen activator followed by anticoagulation
186. A 65-year-old man presents to his physician complaining of difficulty swallowing, occasional chest pain, and regurgitation of food. Over the past 2 months he has lost about 7 kg (15 lb). Results of a barium swallow study are shown in the image. What test should be performed to look for possible causes of his condition?
(A) 24-hour pH monitoring
(B) Esophageal manometry
(C) Serum gastrin level measurement
(D) Upper endoscopy
(E) Urease breath test
187. A 63-year-old man with a long history of alcohol abuse presents with ascites. He is experiencing mild abdominal discomfort and nausea. Examination reveals tense ascites and generalized tenderness but no rigidity. A diagnostic paracentesis of the fluid is performed. Which of the following ascitic fluid results is most likely to suggest an uncomplicated ascites due to portal hypertension from cirrhosis?
A. hemorrhage
B. protein >25 g/L
C. Bilirubin level twice that of serum
D. Serum to ascites albumin gradient >1.1 g/dL
E. More than 1000 white cells/mm3
188. A 67-year-old woman with a history of hypertension and congestive heart failure presents with “burning” epigastric pain that began 2 hours after eating a meal. She states that she has had similar pain over the past several weeks, and has been taking antacids and a medication that her primary care physician had prescribed with moderate relief. The pain has occurred with increasing frequency and now awakens her from sleep. She states she came to the ED today because the pain was not relieved with her usual medications. She denies nausea, vomiting, diarrhea, or fever. She also denies hematemesis, black stool, or bright red blood per rectum. On physical examination, she is tender at the epigastrium, with an otherwise normal abdominal, pulmonary, and heart examination. Stool guaiac tests positive for occult blood. Which of the following is the most common serious complication of peptic ulcer disease?
A. GI haemorrhage
B. GI perforation
C. GI penetration
D. Gastric outlet obstruction
E. Pernicious anemia
189. A 60-year-old man with no past medical history undergoes upper endoscopy and biopsy for an upset stomach that is worsened by eating. He is found to have inflammation predominantly in the antrum of the stomach. Which of the following is the most likely etiology of this condition?
(A) Alcohol abuse
(B) Cigarette smoking
(C) Iatrogenic
(D) Infection
(E) Spicy foods
190. A 21-year-old man presents to the clinic feeling tired and generally unwell. He has fallen several times over the past month and has developed a slight tremor in both hands. Physical examination is significant for scleral icterus, ankle edema, and a distended and tense abdomen. Laboratory studies show: Hemoglobin: 7 g/dL Reticulocyte count: 7% Total bilirubin: 3.1 mg/dL Aspartate aminotransferase: 84 U/L Alanine aminotransferase: 92 U/L Ceruloplasmin: 5 mg/dL (normal: 20–45 mg/dL) Results of a Coombs’ test are negative. Which of the following is an appropriate preventive management step after chelation therapy?
(A) Blood protein electrophoresis
(B) Colonoscopy
(C) ECG
(D) Schilling test
(E) Upper endoscopy
191. A 70-year-old man with a history of constipation has been experiencing intermittent left- sided abdominal pain and fevers for 2 days. He came to the emergency department immediately after he noticed blood in his toilet this morning. His heart rate is 110/min, blood pressure is 90/50 mm Hg, respiratory rate is 18/ min, and oxygen saturation is 95% on room air. On physical examination the physician notes copious amounts of bright red blood per rectum. The physician immediately places two large bore intravenous lines, administers fluid, and sends blood for type and screen. Which of the following is the best next step in management?
(A) Arteriography
(B) Colonoscopy
(C) Endoscopy
(D) Nasogastric tube aspiration
(E) Surgical consultation
192. A 23-year-old woman presents to the ED complaining of pain with urination. She has no other complaints. Her symptoms started 3 week ago. During this time, she has been to the clinic twice, with negative urine cultures each time. Her condition has not improved with antibiotic therapy with sulfonamides or quinolones. Physical examination is normal. Wet mount showed epithelial cells. Which of the following organisms is most likely responsible for the patient’s symptoms?
A. Staphylococcus aureus
B. Herpes simplex virus
C. Trichomonas vaginalis
D. Escherichia coli
E. Chlamydia trachomatis
193. A 35-year-old alcoholic man is admitted with nausea, vomiting, and abdominal pain that radiates to the back. He has had several previous episodes of pancreatitis presenting with the same symptoms. Which of the following laboratory values suggests a poor prognosis in this patient?
A. Elevated serum lipase
B. Elevated serum amylase
C. Leukocytosis of 20,000/μm
D. Diastolic blood pressure greater than 90 mm Hg
E. Heart rate of 100 beats/minute
194. A 60-year-old woman with depression and poorly controlled type 2 diabetes mellitus complains of episodic vomiting over the last three months. She has constant nausea and early satiety. She vomits once or twice almost every day. In addition, she reports several months of mild abdominal discomfort that is localized to the upper abdomen and that sometimes awakens her at night. She has lost 5 lb of weight. Her diabetes has been poorly controlled (glycosylated hemoglobin recently was 9.5). Current medications are glyburide, metformin, and amitriptyline. Her physical examination is normal except for mild abdominal distention and evidence of a peripheral sensory neuropathy. Complete blood count, serum electrolytes, BUN, creatinine, and liver function tests are all normal. Gallbladder sonogram is negative for gallstones. Upper GI series and CT scan of the abdomen are normal. What is the best next step in the evaluation of this patient’s symptoms?
A. Barium esophagram
B. Scintigraphic gastric emptying study
C. Colonoscopy
D. Liver biopsy
E. Small bowel biopsy
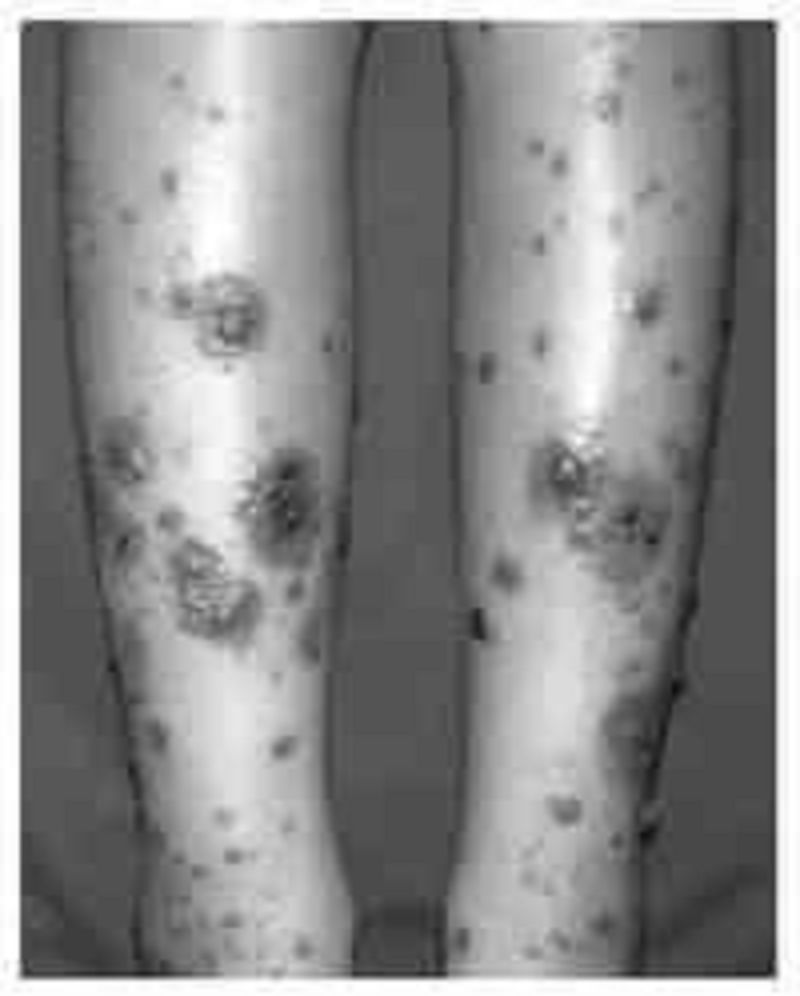
195. A 3-year-old boy is brought to the pediatrician because his mother noticed a reddish-purple rash on his buttocks and thighs (see image). She notes that he has not seemed well since he had a mild cold 2 weeks earlier; he has been complaining of aches and pains in his legs and a stomach ache. Urinalysis shows 10–20 RBCs/ mm³ and 2+proteinuria. Which of the following is associated with this patient’s disease process?
(A) Hemoptysis
(B) High antistreptolysin O titer
(C) Impaired glucose tolerance
(D) Intussusception
(E) Malar rash
196. A 63-year-old man with diabetes is called by his primary care physician because of abnormal liver function test results, as follows: Aspartate aminotransferase: 85 U/L Alanine aminotransferase: 102 U/L Alkaline phosphatases: 180 U/L Total bilirubin: 1.9 mg/dL. On physical examination his liver is enlarged. His skin has a slightly yellow hue, especially on his face. The review of symptoms is significant for some weight loss, weakness, arthritis in his hands, and inability to achieve an erection. What test would generate the most likely diagnosis and should be done first?
(A) Blood smear
(B) CT scan of the abdomen
(C) Endoscopic retrograde cholangiopancreatography
(D) Fasting transferrin saturation levels
(E) Liver biopsy
197. A 28-year-old man presents to the ED complaining of constant vague, diffuse epigastric pain. He describes having a poor appetite and feeling nauseated ever since eating sushi last night. His BP is 125/75 mm Hg, HR is 96 beats per minute, temperature is 100.5°F, and his RR is 16 breaths per minute. On examination, his abdomen is soft and moderately tender in the right lower quadrant (RLQ). Laboratory results reveal a WBC of 12,000/ μL. Urinalysis shows 1+ leukocyte esterase. The patient is convinced that this is food poisoning from the sushi and asks for some antacid. Which of the following is the most appropriate next step in management?
A. Order a plain radiograph to look for dilated bowel loops.
B. Administer 40 cc of Maalox and observe for 1 hour.
C. Send the patient for an abdominal ultrasound.
D. Order an abdominal CT scan.
E. Discharge the patient home with ciprofloxacin.
198. A 23-year-old woman presents to the ED in moderate pain in her left lower quadrant (LLQ). She states that the pain began suddenly and is associated with nausea and vomiting. She had a bout of diarrhea yesterday. This is the second time this month that she experienced pain in this location, however, never with this severity. Her BP is 120/75 mm Hg, HR is 101 beats per minute, temperature is 99.5°F, and RR is 18 breaths per minute. She has a tender LLQ on abdominal examination and a tender adnexa on pelvic examination. Which of the following is the most appropriate diagnostic test for the patient?
A. CT scan
B. MRI
C. X-ray
D. Doppler ultrasound
E. Laparoscopy
199. A 55-year-old man presents to the ED complaining of mild diffuse abdominal pain. He states that he underwent a routine colonoscopy yesterday and was told “everything is fine.” The pain began upon waking up and is associated with some nausea. He denies fever, vomiting, diarrhea, and rectal bleeding. His BP is 143/71 mm Hg, HR is 87 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. His abdomen is tense but only mildly tender. You order baseline laboratory tests. His chest radiograph is seen below. Which of the following is the most likely diagnosis?
A. Ascending cholangitis
B. Acute pulmonary edema
C. Acute liver failure
D. Pancreatitis
E. Pneumoperitoneum
200. A 34-year-old woman complains bitterly of heartburn. Physical examination reveals healing lesions of the fingertips that she says were small ulcers, and there are small areas of telangiectasias on her face. Esophageal manometry reveals a decrease in the expected amplitude of smooth muscle contraction. Lower esophageal sphincter tone is subnormal, but relaxes normally with swallowing. Which of the following statements regarding this condition is most likely correct?
A. Characterized by systemic signs of inflammation
B. Predominantly treated symptomatically
C. Characterized by a poor prognosis
D. Usually more frequent in men
E. Characterized by death secondary to a renal crisis
201. A 35-year-old White man has a long past his- tory of diarrhea, rectal bleeding, crampy abdominal pain, and the passage of mucus. He now presents with a worsening of his symptoms despite taking his medications. A barium enema is performed and is shown in Fig. Which of the following is the most likely diagnosis of this new complication?

A. Toxic megacolon
B. Amoebic colitis
C. appendicitis
D. Ischemic colitis
E. Annular carcinoma
202. A 45-year-old man with a long history of alcohol intake comes into the emergency room with upper gastrointestinal (UGI) bleeding. Urgent endoscopy reveals the following findings. Which of the following is the most likely diagnosis?

A. Esophageal varices
B. Esophageal carcinoma
C. Foreign body
D. Tertiary waves
E. Barrett’s esophagus
203. A 50-year-old woman undergoes screening colonoscopy at her primary care physician’s recommendation. She has no family history of colorectal cancer. A single lesion is removed during the procedure and sent for pathologic examination. Which of the following findings carries the greatest risk of malignancy?
(A) Lymphoid polyp
(B) Peutz-Jeghers polyp
(C) Tubular adenoma
(D) Tubulovillous adenoma
(E) Villous adenoma
204. A 61-year-old man in previously excellent health presents to his physician with complaints of hematochezia tenesmus, and rectal pain. On work-up the physician discovers that he has a rectal tumor that is 5 cm (2.0 in) from the anal verge. Which of the following is the most appropriate treatment?
(A) Abdominoperineal resection
(B) Imatinib
(C) Low anterior resection
(D) Radiation alone
(E) Radiation plus chemotherapy
205. A 45-year-old HIV-positive woman comes to her primary care physician complaining of a 2-day history of bloody diarrhea. She states that she has been feeling well until 2 days ago, when she developed abdominal pain. She denies fevers, chills, night sweats, nausea, or vomiting. She admits to feeling tired over the last couple of weeks and has had a 2.3-kg (5-lb) weight loss over the past 2 weeks. Her stool sample shows WBCs and RBCs. Her Gram stain is shown in the image. Her CD4+ cell count is 201/mm³. Which of the following is the most likely cause of this woman’s symptoms?

(A) Escherichia coli
(B) Kaposi’s sarcoma
(C) Legionella
(D) Mycobacterium avium complex
(E) Mycobacterium tuberculosis
206. A 75-year-old woman with a history of diabetes and coronary heart failure presents to the emergency department because of increasing abdominal girth. In recent months she has been feeling increasingly fatigued, and although she has had decreased appetite, she has gained weight. Her heart rate is 100/min and blood pressure is 112/70 mm Hg. She has scleral icterus; the skin over her face, neck, and lower legs is slightly bronze in color; she has palmar erythema; and she has numerous ecchymoses over her body. Her abdominal examination is significant for ascites. Laboratory tests show: Aspartate transaminase: 102 U/L Alanine transaminase: 97 U/L Alkaline phosphatase: 300 U/L Total bilirubin: 1.9 mg/dL Albumin: 2.9 g/dL Prothrombin time: 22 sec Partial thromboplastin time: 42 sec An ultrasound of her abdomen shows a shrunken and nodular liver. A liver biopsy using Perls Prussian blue stain is shown in the image. Which of the following is the most likely complication of her disease?

(A) Acute pancreatitis
(B) Amyloidosis
(C) Bone marrow failure
(D) Hepatocellular carcinoma
(E) Splenomegaly
207. A term boy with Apgar scores of 9 and 9 at 1 and 5 minutes has failed to pass meconium at 72 hours. He has had no episodes of emesis, and his abdomen is only mildly distended to palpation. The patient’s mother reports that her older son had the same problem at birth. A plain radiograph of the abdomen shows a small bowel obstruction with numerous air-filled loops of bowel. The patient is treated with a diatrizoate meglumine (Gastrografin) enema, with good results. Which of the following is the most likely mechanism for this infant’s acute intestinal problem?
(A) Congenital aganglionosis of the colon
(B) Deficiency of pancreatic enzymes
(C) Intussusception of the large bowel
(D) Total absence of the small bowel
(E) Volvulus of the transverse colon
208. A 75-year-old woman comes to the emergency department with complaints of nausea and nonbilious, nonbloody vomiting over the past 4 days. The patient reports that both the nausea and vomiting come in “waves”; that is, several hours will pass during which she feels well before the vomiting suddenly recurs. A detailed history reveals that the woman was told several months ago that she “has stones in her gall-bladder,” but she has been too frightened to undergo surgery. She has not had a bowel movement for 7 days. Her temperature is 38.4°C (101.1°F) and the abdomen is distended with high-pitched bowel sounds. Which of the following is the most appropriate initial test for a patient with suspected gallstone ileus?
(A) Abdominal ultrasound
(B) Diagnostic laparoscopy
(C) Endoscopic retrograde cholangiopancreatography
(D) Hepatic iminodiacetic acid scan
(E) Plain X-ray of the abdomen
209. A 62-year-old woman with a history of diabetes mellitus presents to the emergency department complaining of severe abdominal pain for the past 12 hours, first beginning as dull pain near the umbilicus but now localized to the right lower quadrant. She initially thought she was suffering from heartburn, but decided to come to the hospital because of the unrelenting pain. The patient reports that just prior to examination by the physician, she experienced a sudden decrease in intensity of pain, but she remains feeling very uncomfortable and must remain on the stretcher. On examination the patient appears in distress secondary to pain, tachycardic, slightly hypotensive, and febrile at 39°C (102°F). She has a diffusely tender abdomen with point tenderness over her right lower quadrant, accompanied by guarding and rebound. Laboratory values showed a leukocytosis of 20,000/mm³ with 95% polymorphonuclear lymphocytes. After confirming the diagnosis with imaging, which of the following is the most appropriate management?
(A) Emergent appendectomy and postoperative antibiotics
(B) Give nothing by mouth with intravenous hydration
(C) Percutaneous drainage and interval appendectomy
(D) Serial abdominal examinations
(E) Urgent ECG and cardiac enzymes
210. A 24-year-old woman presents to her primary care provider because of bloody diarrhea for several months and uveitis. Complete blood cell count shows mild anemia but a normal WBC count. The erythrocyte sedimentation rate and the C-reactive protein level are not elevated. Which of the following is the most likely diagnosis?
(A) Bacterial enterocolitis
(B) Bowel ischemia
(C) Colon carcinoma
(D) Mallory-Weiss tear
(E) Ulcerative colitis
211. A 47-year-old woman presents to the emergency department with an 8-day history of left lower quadrant pain and semi-formed stools. Starting this afternoon, she has noticed blood in her stool as well as dizziness when she gets up from sitting. She denies fever, nausea, vomiting, weight loss, and night sweats. Her temperature is 37°C (98.6°F), heart rate is 104/ min, blood pressure is 120/82 mm Hg supine and 103/63 mm Hg when she sits up, and respiratory rate is 18/min. Physical examination reveals no peritoneal signs and is remarkable only for fecal occult blood on rectal examination. Laboratory results reveal a WBC count of 13,000/mm³ and hematocrit of 29%. Results of an x-ray of the abdomen are shown in the image. What is the best next step in management?

(A) Angiography with embolization
(B) Immediate surgery for partial colectomy
(C) Intravenous hydration and blood transfusion
(D) Nothing by mouth, nasogastric tube, and broad-spectrum antibiotics
(E) Place the patient on a high-fiber diet
212. A 66-year-old woman presents to her physician because of recurrent painless bleeding on defecation over the past month. She has regular, soft bowel movements and no history of constipation or diarrhea. A recent diagnosis of aortic stenosis was an incidental finding on echocardiogram. She takes calcium and vitamin D supplements daily. Her last colonoscopy (at age 60) was normal. Heart rate is 82/min, blood pressure is 133/72 mm Hg, respiratory rate is 12/min, and temperature is 36.6°C (97.8°F). Physical examination reveals her conjunctivae are pink and mucosa is moist. She has no abdominal tenderness or palpable masses and no hemorrhoids or fissures. Stool is hemoccult positive. Colonoscopy shows a spider-like lesion in the ascending colon. Which of the following is the most likely diagnosis?
(A) Angiodysplasia
(B) Crohn’s disease
(C) Diverticulosis
(D) Ischemic colitis
(E) Peptic ulcer disease
213. A 61-year-old woman is brought to the emergency department drowsy and disoriented, able only to follow simple commands. On examination her abdomen is distended and nontender, her skin has a yellow hue, and there are multiple spider nevi on her chest. In her purse, the physician finds prescriptions for peginterferon and ribavirin. When asked to raise her hands, the physician notices a coarse tremor. Laboratory tests show: Blood urea nitrogen: 17 mg/dL Creatinine kinase: 1.1 mg/dL Aspartate aminotransferase: 89 U/L Alanine aminotransferase: 93 U/L Total bilirubin: 3.1 mg/dL Ammonia: 124 μg/dL Which of the following is the most likely diagnosis?
(A) Bleeding esophageal varices
(B) Hepatic encephalopathy
(C) Hepatocellular carcinoma
(D) Hepatorenal syndrome
(E) Spontaneous bacterial peritonitis
214. A 74-year-old man presents to the emergency department with abdominal pain. The pain is deep and aching and is localized to the left lower quadrant. The man reports multiple episodes of diarrhea over the preceding week. He also reports having multiple similar episodes of abdominal pain in the past. On physical examination he is febrile and has tenderness to palpation of the left lower quadrant. His WBC count is 23,000/mm³. Results of CT are shown in the image. Which of the following is the most likely diagnosis?

(A) Angiodysplasia
(B) Carcinoid syndrome
(C) Carcinoma of the colon
(D) Diverticulitis
(E) Infectious colitis
215. A 62-year-old woman presents to her physician with complaints of heartburn, fatigue, and intermittent upper abdominal pain. The pain is often worse after meals and especially with spicy foods. She reports no recent nausea, vomiting, weight loss, dysphagia, or bright-red blood per rectum. However, her stools are darker than normal. Her last colonoscopy 2 years ago was unremarkable. Stool guaiac test result is positive. An initial complete blood cell count reveals: Hemoglobin: 10.1 g/dL Hematocrit: 33.2% Mean corpuscular volume: 74.6/mm³ Mean corpuscular hemoglobin concentration: 25.8% WBC count: 9200/mm³ Platelet count: 176,000/mm³ Ferritin: 11 ng/mL The patient undergoes upper endoscopy, which reveals erosive gastritis. She is started on omeprazole, 40 mg twice a day and oral iron sulfate supplementation, 325 mg three times a day with meals. Six months into treatment, abdominal pain and heartburn are resolved, but the patient still has fatigue and is pale. Repeat laboratory tests show: Hemoglobin: 9.9 g/dL Hematocrit: 30.2% Mean corpuscular volume: 74.2/mm³ Mean corpuscular hemoglobin concentration: 25.1% WBC count: 9800/mm³ Platelet count: 198,000/mm³ Ferritin: 10 ng/mL Repeat upper endoscopy is negative for bleeding and erosive gastritis. Stool guaiac test result is negative. Which of the following is the next best step in management?
(A) Bone marrow biopsy
(B) Determine blood type and screen for trans- fusion
(C) Discontinue omeprazole therapy
(D) Initiate darbepoetin therapy
(E) Initiate parenteral iron therapy
216. An 82-year-old woman is in the surgical intensive care unit after a carotid endarterectomy. She has been taking clindamycin and ciprofloxacin for the past 13 days. On postoperative day 2 the patient is febrile and tachycardic with a high WBC count and a low RBC count. She is also noted to be dehydrated and hypotensive. On physical examination she is distended and has abdominal tenderness with rebound and guarding. Barium enema reveals colonic dilatation of 8 cm. Stool is sent for Gram stain and analysis for fecal leukocytes, fecal occult blood, and Clostridium difficile toxin. Which of the following is most likely present in the stool sample?
(A) Clostridium difficile toxin
(B) Gram-negative rods
(C) Gram-positive cocci
(D) No fecal occult blood
(E) Spores and hyphae
217. A 51-year-old man presents to the ED complaining of epigastric pain that radiates to his back. He states that he drinks six packs of beer daily. You suspect he has pancreatitis. His BP is 135/75 mm Hg, HR is 90 beats per minute, temperature is 100.1°F, and his RR is 17 breaths per minute. Laboratory results reveal WBC 13,000/μL, hematocrit 48%, platelets 110/μL, amylase 1150 U/L, lipase 1450 IU, lactate dehydrogenase (LDH) 150 U/L, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 105 mEq/L, bicarbonate 23 mEq/L, BUN 15 mg/dL, creatinine 1.1 mg/dL, and glucose 125 mg/dL. Which of the following laboratory values are most specific for pancreatitis?
A. Elevated amylase
B. Hyperglycemia
C. Elevated lipase
D. Elevated LDH
E. Leukocytosis
218. A 51-year-old man describes 1 week of gradually worsening scrotal pain and dysuria. He is sexually active with his wife. His temperature is 100.1°F, HR 81 beats per minute, BP 140/75 mm Hg, and oxygen saturation is 99% on room air. On physical examination, his scrotal skin is warm and erythematous. A cremasteric reflex is present. The posterior left testicle is swollen and tender to touch. Color Doppler ultrasonography demonstrates increased testicular blood flow. Urinalysis is positive for leukocyte esterase. What is the most likely diagnosis?
A. Epididymitis
B. Testicular torsion
C. UTI
D. Testicular tumor
E. Varicocele
219. A 40-year-old woman presents to the ED complaining of fever and 1 day of increasingly severe pain in her RUQ. She denies nausea or vomiting and has no history of fatty food intolerance. The patient returned from a trip to Mexico 6 months ago. About 2 weeks ago she experienced intermittent diarrhea with blood-streaked mucus. Her BP is 130/80 mm Hg, HR is 107 beats per minute, temperature is 102°F, and RR is 17 breaths per minute. Physical examination reveals decreased breath sounds over the right lung base. Abdominal examination shows tenderness to percussion over the RUQ and normal active bowel sounds. There is no Murphy sign. Her WBC is 20,500/μL. Chest radiograph reveals a small right-pleural effusion. Which of the following is the most likely diagnosis?
A. Amebic abscess
B. Cholecystitis
C. Cryptosporidium
D. Enterobiasis
E. Pyogenic abscess
220. A 25-year-old G3P1011 presents to the ED with a 6-hour history of worsening lower abdominal pain, mostly in the RLQ. She also noticed some vaginal spotting this morning. She is nauseated, but did not vomit. Her last menstrual period was 2 months ago, but her cycles are irregular. She is sexually active and has a history of pelvic inflammatory disease. Her BP is 120/75 mm Hg, HR is 95 beats per minute, temperature is 99.2°F, and RR is 16 breaths per minute. Her abdomen is tender in the RLQ. Pelvic examination reveals right adnexal tenderness. Her WBC count is slightly elevated and her β-hCG is positive. After establishing IV access, which of the following is the most appropriate next step in management?
A. Call the OR to prepare for laparoscopy.
B. Order an emergent CT scan of the abdomen.
C. Perform a transvaginal ultrasound.
D. Order a urinalysis.
E. Swab her cervix and treat for gonorrhea and Chlamydia.
221. A 40-year-old Asian woman presents to the emergency department complaining of intermittent epigastric pain. The pain is severe, lasts for a few hours, and is sometimes accompanied by nausea and vomiting. Her bowel movements have been normal. Her temperature is 38.3°C (100.9°F), pulse is 100/min, blood pressure is 150/80 mm Hg, and respiratory rate is 22/min. Physical examination reveals moderate obesity and mildly icteric sclerae. Bowel sounds are normal, with an abrupt halt of inspiration upon palpation of the RUQ, and guarding is noted. Laboratory values reveal a WBC count of 13,000/mm³, total bilirubin of 3.3 mg/dL, and normal liver enzymes and alkaline phosphatase levels. Which of the following is the first diagnostic imaging study that should be performed?
(A) CT
(B) Flat and upright plain x-rays of the abdomen
(C) Hepatobiliary iminodiacetic acid scan
(D) MRI
(E) Ultrasound of the RUQ
222. A 20-year-old man presents with several weeks of painful rectal bleeding. He denies fever, nausea, or vomiting. He is sexually active with women only and usually uses condoms. He denies any history of CD, UC, or malignancy. He states that the pain is most severe during and immediately after defecating. Bleeding is bright red and only enough to stain the toilet paper. Which of the following is the most common etiology of painful rectal bleeding?
a. External hemorrhoid
B. Anal fissure
C. Anorectal tumor
D. Internal hemorrhoid
E. Venereal proctitis
223. A 57-year-old woman presents to the ED with a basin in her hand and actively vomiting. You insert an IV catheter, start IV fluids, and administer an antiemetic agent. The patient feels much better but also complains of severe crampy abdominal pain that comes in waves. You examine her abdomen and note that it is distended and that there is a small midline scar in the lower abdomen. Upon auscultation, you hear high-pitched noises that sound like “tinkles.” Palpation elicits pain in all four quadrants but no rebound tenderness. She is guaiac negative. Which of the following is the most common cause of this patient’s presentation?
A. Travel to Mexico
B. Ethanol abuse
C. Hysterectomy
D. Hernia
E. Constipation
224. You are working in the ED on a Sunday afternoon when four people present with acute-onset vomiting and crampy abdominal pain. They were all at the same picnic and ate most of the same foods. The vomiting began approximately 4 hours into the picnic. They deny having any diarrhea. You believe they may have “food poisoning” so you place IV lines, administer IV fluids, and observe. Over the next few hours, the patients begin to improve, the vomiting stops, and their abdominal pain resolves. Which of the following is the most likely cause of their presentation?
A. Scombroid fish poisoning
B. Staphylococcal food poisoning
C. Clostridium perfringens food poisoning
D. Campylobacter
E. Salmonellosis
225. A premature newborn is being treated in the neonatal intensive care unit. On the sixth day of life he is noted to be lethargic and in mild respiratory distress. His heart rate is 162/min, blood pressure is 55/38 mm Hg, and respiratory rate is 56/min. In addition to a distended abdomen, he has guaiac-positive stools. X-ray of the abdomen shows gas bubbles within the bowel wall. From what potentially life-threatening condition is this patient most likely suffering?
(A) Bowel obstruction
(B) Intussusception
(C) Meconium ileus
(D) Meningitis
(E) Necrotizing enterocolitis
226. A 45-year-old white man is brought to the emergency department by ambulance. He is waving wildly, trying to hit the “flying bats” that are all around him. He is very agitated and smells strongly of alcohol. The ambulance crew said they found the patient bleeding from the mouth outside a bar. They could not find any laceration on his mouth or lips and believe that the bleeding is internal. The patient screams that he will not stand for this maltreatment any longer and tries to stand up, at which point he begins to vomit. Blood pours out of his mouth, and the patient says, “Here we go again.” The ambulance crew tells the physician that there was also a lot of vomit at the bar where he was found. The physician is able to subdue the patient to obtain his vital signs. His blood pressure is 118/78 mm Hg, pulse is 98/ min, respiratory rate is 22/min, and temperature is 37.2°C (98.9°F). The physician is unable to obtain a history on the patient or con- tact any relatives or friends. No signs of obvious trauma are observed. Which of the following is the best next step in diagnosis?
(A) Barium swallow
(B) Electrocardiogram
(C) Endoscopy
(D) Esophageal manometry
(E) X-ray of the chest
227. A 65-year-old man comes to the emergency department complaining of left lower abdominal pain that began the prior morning. He became concerned when he developed bloody diarrhea overnight. He has experienced similar pain, although to a lesser degree, over the past 2 months, especially after eating. The pain usually resolved within 1–2 hours, and he never had bloody diarrhea. His past medical history is significant for coronary artery disease and hypertension. He has smoked one pack of cigarettes per day for the past 30 years. On physical examination he is afebrile, heart rate is 90/min, and blood pressure is 135/85 mm Hg. He is visibly uncomfortable but in no apparent distress. His abdominal examination is significant for left lower quadrant tenderness but no guarding or rebound. Which of the following is the most likely diagnosis?
(A) Acute mesenteric ischemia
(B) Colon cancer
(C) Diverticulitis
(D) Infectious colitis
(E) Inflammatory bowel disease
228. A 53-year-old man presents to the emergency department with severe epigastric abdominal pain. His temperature is 37.2C, blood pressure 110/70 mm Hg, pulse 110/min, and respirations 20/min. Examination of the heart and lungs is normal, and his abdomen is tender in the epigastric region. His white count is 15,000/mL and amylase is 450 U/L (25–125 U/L). Which of the following laboratory abnormalities is also most likely to be present?
A. hypoglycemia
B. hypercholesterolemia
C. hyperglycemia
D. hypercalcemia
E. hypercarbia
229. A 43-year-old man feels vaguely unwell. Physical examination is unremarkable except for evidence of scleral icterus. The skin appears normal. Which of the following is the most likely explanation for why early jaundice is visible in the eyes but not the skin?
A. The high type II collagen content of scleral tissue
B. The high elastin content of scleral tissue
C. The high blood flow to the head with consequent increased bilirubin delivery
D. Secretion via the lacrimal glands
E. The lighter color of the sclera
230. A 25-year-old previously healthy man experiences fatigue and malaise. One week ago he had a “viral” type illness consisting of a sore throat, fever, and myalgias. He now appears jaundiced, but the rest of the physical examination is normal. His investigations reveal a total bilirubin of 4 mg/dL (0.1–1.0 mg/dL) and a direct bilirubin of 0.3 mg/dL (0.0–0.3 mg/dL). Which of the following is the most likely diagnosis?
A. hemolysis
B. gallstones
C. Alcoholic liver disease
D. Pancreatic carcinoma
E. Dubin-Johnson syndrome
231. A 49-year-old man is brought to the ED by EMS stating that he vomited approximately three cups of blood over the last 2 hours. He also complains of epigastric pain. While examining the patient, he has another episode of hematemesis. You decide to place an NG tube. You insert the tube, confirm its placement, and attach it to suction. You retrieve 200 mL of coffee-ground blood. What is the most common etiology of an upper GI bleed?
A. Varices
B. Peptic ulcer
C. Gastric erosions
D. Mallory-Weiss tear
E. Esophagitis
232. A 56-year-old woman becomes the chief financial officer of a large company and, several months thereafter, develops upper abdominal pain that she ascribes to stress. She takes an over-the-counter antacid with temporary benefit. She uses no other medications. One night she awakens with nausea and vomits a large volume of coffee grounds-like material; she becomes weak and diaphoretic. Upon hospitalization, she is found to have an actively bleeding duodenal ulcer. Which of the following statements is true?
A. The most likely etiology is adenocarcinoma of the duodenum.
B. The etiology of duodenal ulcer is different in women than in men.
C. The likelihood that she harbors Helicobacter pylori is greater than 50%.
D. Lifetime residence in the United States makes H pylori unlikely as an etiologic agent.
E. Organisms consistent with H pylori are rarely seen on biopsy in patients with duodenal ulcer.
233. A 63-year-old woman with cirrhosis caused by chronic hepatitis C is hospitalized because of confusion. She has guaiac-positive stools and a low-grade fever. She has received lorazepam for sleep disturbance. On physical examination, the patient is confused. She has no meningeal signs and no focal neurologic findings. There is hyperreflexia and a nonrhythmic flapping tremor of the wrists. Which of the following is the most likely explanation for this patient’s mental status change?
A. Tuberculous meningitis
B. Subdural hematoma
C. Alcohol withdrawal seizure
D. Hepatic encephalopathy
E. Central nervous system vasculitis from cryoglobulinemia
234. A 40-year-old white male complains of weakness, weight loss, and abdominal pain. On examination, the patient has diffuse hyperpigmentation and a palpable liver edge. Polyarthritis of the wrists and hips is also noted. Fasting blood sugar is 185 mg/dL. Which of the following is the most likely diagnosis?
A. Insulin-dependent diabetes mellitus
B. Pancreatic carcinoma
C. Addison disease
D. Hemochromatosis
E. Metabolic syndrome
235. A 55-year-old white woman has had recurrent episodes of alcoholinduced pancreatitis. Despite abstinence, the patient develops postprandial abdominal pain, bloating, weight loss despite good appetite, and bulky, foul-smelling stools. KUB shows pancreatic calcifications. In this patient, you should expect to find which of the following?
A. Diabetes mellitus
B. Malabsorption of fat-soluble vitamins D and K
C. Guaiac-positive stool
D. Courvoisier sign
E. Markedly elevated amylase
236. A 34-year-old white woman is treated for a UTI with amoxicillin. Initially she improves, but 5 days after beginning treatment, she develops recurrent fever, abdominal bloating, and diarrhea with six to eight loose stools per day. What is the best diagnostic test to confirm your diagnosis?
A. Identification of Clostridium difficile toxin in the stool
B. Isolation of C difficile in stool culture
C. Stool positive for white blood cells (fecal leukocytes)
D. Detection of IgG antibodies against C difficile in the serum
E. Visualization of clue cells on microscopic examination of stool
{"name":"V. GASTROINTESTINALE Part II (101-236) Na", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"101. A 70-year-old woman with a history of hypertension, congestive heart failure, and atrial fibrillation presents to the ED with several hours of acute onset diffuse abdominal pain. She denies any nausea or vomiting. The pain is constant, but she is unable to localize it. She was diagnosed with a renal artery thrombosis several years ago. Vital signs include HR of 95 beats per minute, BP of 110\/70 mm Hg, and temperature of 98°F. Her abdomen is soft and mildly tender, despite her reported severe abdominal pain. Her WBC count is 12,000\/μL, hematocrit 38%, platelets 250\/μL, and lactate 8 mg\/dL. The stool is traced heme-positive. You are concerned for acute mesenteric ischemia. What is the best way to diagnose this condition?, 102. An 81-year-old diabetic woman with a history of atrial fibrillation is transferred to your emergency department (ED) from the local nursing home. The note from the facility states that the patient is complaining of abdominal pain, having already vomited once. Her vital signs in the ED are temperature 100.1°F, blood pressure (BP) 105\/75 mm Hg, heart rate (HR) 95 beats per minute, and respiratory rate (RR) 18 breaths per minute. You examine the patient and focus on her abdomen. Considering that the patient has not stopped moaning in pain since arriving to the ED, you are surprised to find that her abdomen is soft on palpation. You decide to order an abdominal radiographic series. Which of the findings on plain abdominal film is strongly suggestive of mesenteric infarction?, 103. As you palpate the right upper quadrant (RUQ) of a 38-year-old woman’s abdomen, you notice that she stops her inspiration for a brief moment. During the history, the patient states that over the last 2 days she gets pain in her RUQ that radiates to her back shortly after eating. Her vitals include a temperature of 100.4°F, HR of 95 beats per minute, BP of 130\/75 mm Hg, and RR of 16 breaths per minute. What is the initial diagnostic modality of choice for this disorder?","img":"https://cdn.poll-maker.com/10-459491/107.jpg?sz=1200"}
More Quizzes
Egerg
100
Our green Earth
3272
Oracle_test
10517
Historic Dates
12613
Bleach: How Well Do You Know Renji Abarai?
201017696
AP Psychology Unit 0 Practice Test - Vocab Review
201015977
MTC Balotario A1 - Simulacro de Preguntas Gratis
201016571
¿Qué Tipo de Chica Soy? Test Gratis con Resultados
201017835
Health Canada Trivia - Test Your Knowledge
201020249
Hogwarts House - Test Your Wizarding Knowledge
201017494
7.08 Elizabethan Age Practice - Free Online
201016629
Most Accurate Aura Color Test - Free Instant Results
201018049