Circulatory System Quiz: Test Your Knowledge of Heart and Vessels
Quick, free circulatory system test with instant feedback and score tracking.
Use this circulatory system quiz to check what you know about the heart, blood flow, and major vessels, with instant feedback as you go. When you want a deeper dive, try our blood vessels quiz, explore NCLEX cardiovascular questions if you're studying nursing, or broaden your review with cardiology quiz questions and answers.
Study Outcomes
- Identify Heart Anatomy -
Pinpoint major chambers, valves, and vessels of the heart to strengthen your foundational knowledge.
- Trace Blood Flow Pathways -
Follow the journey of blood through the systemic and pulmonary circuits to understand circulation dynamics.
- Differentiate Vessel Types -
Compare and contrast arteries, veins, and capillaries based on structure and function in blood circulation.
- Interpret Circulatory System Processes -
Analyze blood pressure, cardiac output, and flow rate concepts to grasp cardiovascular function.
- Apply Knowledge in Quiz Scenarios -
Use critical thinking to answer questions in the circulatory system quiz, reinforcing your understanding.
- Assess Learning Gaps -
Review your blood circulation quiz score to identify areas for further study and improvement.
Cheat Sheet
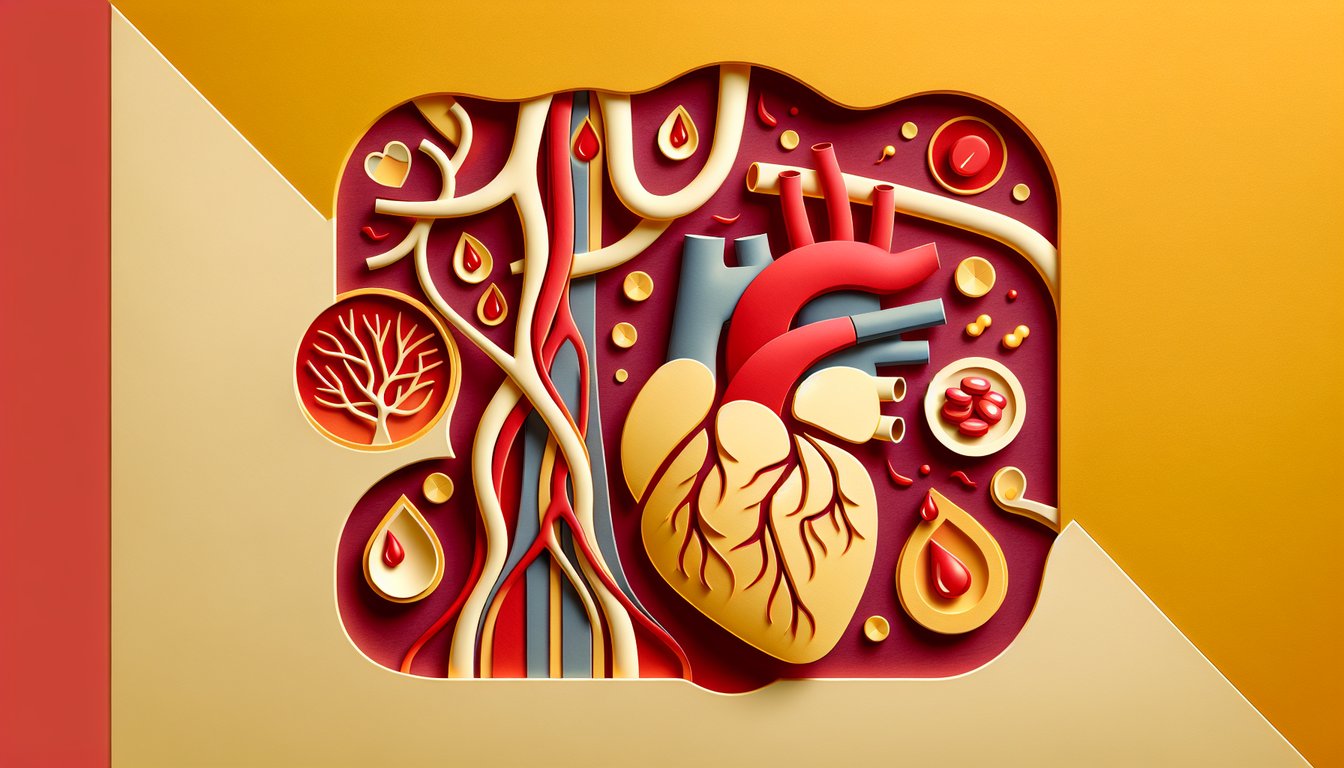
- Heart anatomy and blood flow -
Review the four chambers (RA → RV → lungs → LA → LV) in sequence for pulmonary and systemic circuits. This circuit is a staple on circulatory system quizzes, so use the mnemonic "RA RV LA LV" to keep your order tight. The American Heart Association details this pathway in its anatomy guides.
- Cardiac conduction system -
Understand the pathway: SA node → AV node → Bundle of His → Purkinje fibers, which coordinates atrial and ventricular contraction. Remember "Some Atria Always Validate Heartbeats" as a mnemonic for SA, AV, His, Purkinje. University cardiology guidelines highlight this for ECG interpretation.
- Vessel types and flow resistance -
Differentiate arteries, veins, and capillaries by wall thickness and function; arteries handle high pressure while capillaries facilitate exchange. Apply Poiseuille's law (Flow = ΔP·πr❴ / 8ηl) to see how small radius changes massively affect flow, per NIH physics research.
- Blood pressure and mean arterial pressure -
Memorize systolic vs. diastolic pressures (e.g., 120/80 mmHg in a healthy adult) and calculate MAP ≈ diastolic + ⅓(systolic - diastolic) to assess tissue perfusion. This formula is standard in American College of Cardiology reviews and ACLS protocols confirm its clinical relevance.
- Oxygen transport and the Bohr effect -
The oxyhemoglobin dissociation curve shifts right with increased CO₂, acidity, temperature, and 2,3-DPG (mnemonic "CADET, face Right"). This facilitates O₂ unloading in tissues, as detailed by Guyton and Hall's physiology texts. Study curve graphs to predict oxygen delivery under varying conditions.