Pediactic. kb 1

Pediatric Health Knowledge Quiz
Test your knowledge on pediatric health concepts with this comprehensive quiz designed for healthcare professionals and students alike.
Whether youŌĆÖre preparing for an examination or simply want to refresh your understanding, this quiz features:
- 150 thought-provoking questions
- Relevant multiple-choice options
- A variety of pediatric topics
1. Two weeks after a viral syndrome, a 9-year-old boy presents to your clinic with a complaint of several days of weakness of his mouth. In addition to the drooping of the left side of his mouth, you note that he is unable to completely shut his left eye. His smile is asymmetric, but his examination is otherwise normal. Which of the following is the most likely diagnosis?
A. Guillain-Barre╠Ø syndrome
B. Botulism
C. Cerebral vascular accident
D. Brainstem tumor
E. Bell palsy
2. An infant can regard his parentŌĆÖs face, follow to the midline, lift his head from the examining table, smile spontaneously, and respond to a bell. He does not yet regard his own hand, follow past the midline, nor lift his head to a 45┬░ angle off the examining table. Which of the following is the most likely age of the infant?
A. 1 month
B. 3 months
C. 6 months
D. 9 months
E. 12 months
3. A child is brought to your clinic for a routine examination. She can put on a T-shirt but requires a bit of help dressing otherwise. She can copy a circle well but has diffic ulty in copying a square. Her speech is understandable and she knows four colors. She balances proudly on each foot for 2 seconds but is unable to hold the stance for 5 seconds. Which of the following is the most likely age of this child?
A. 1 year
B. 2 years
C. 3 years
D. 4 years
E. 5 years
4. A 4-year-old girl is noticed by her grandmother to have a limp and a some-what swollen left knee. The parents report that the patient occasionally com- plains of pain in that knee. An ophthalmologic examination reveals findings as depicted in the photograph. Which of the following conditions is most likely to be associated with these findings?
A. Juvenile rheumatoid arthritis
B. Slipped capital femoral epiphysis
C. Henoch-Scho╠łnlein purpura
D. Legg-Calve╠Ø-Perthes disease
E. Osgood-Schlatter disease
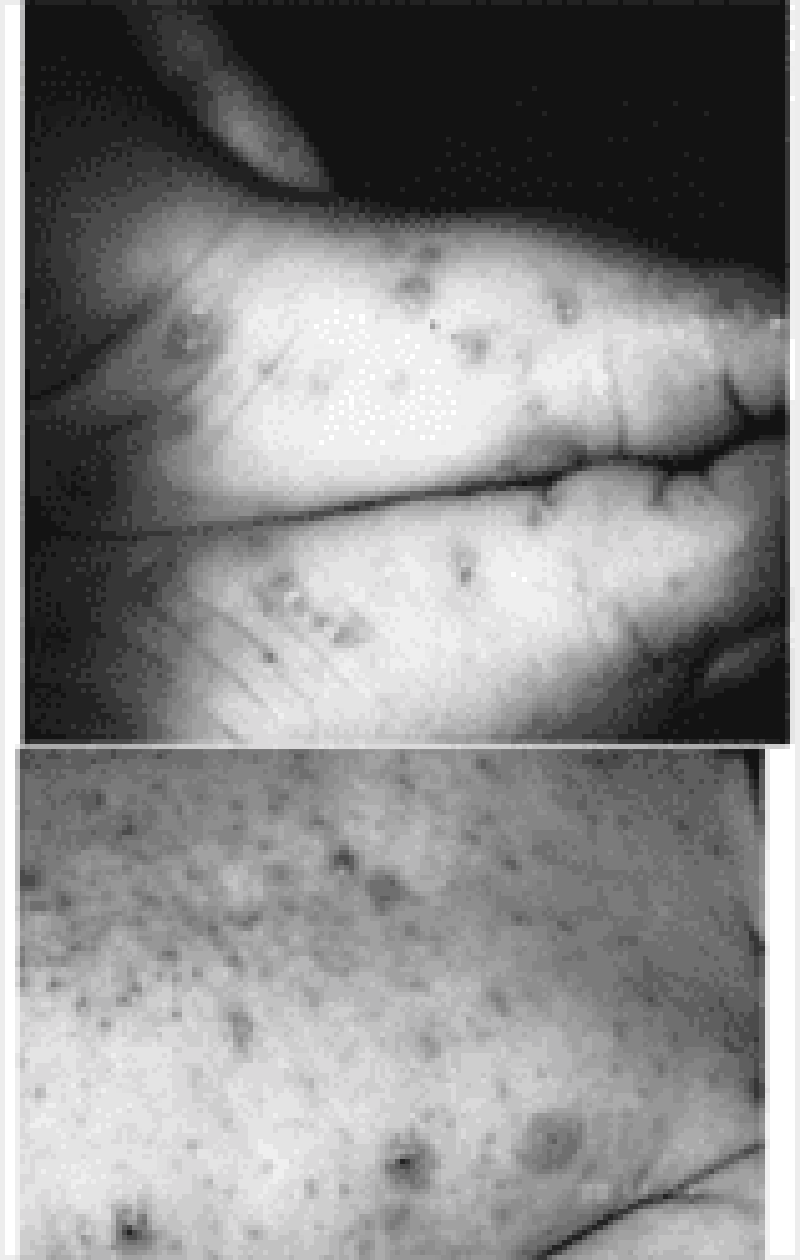
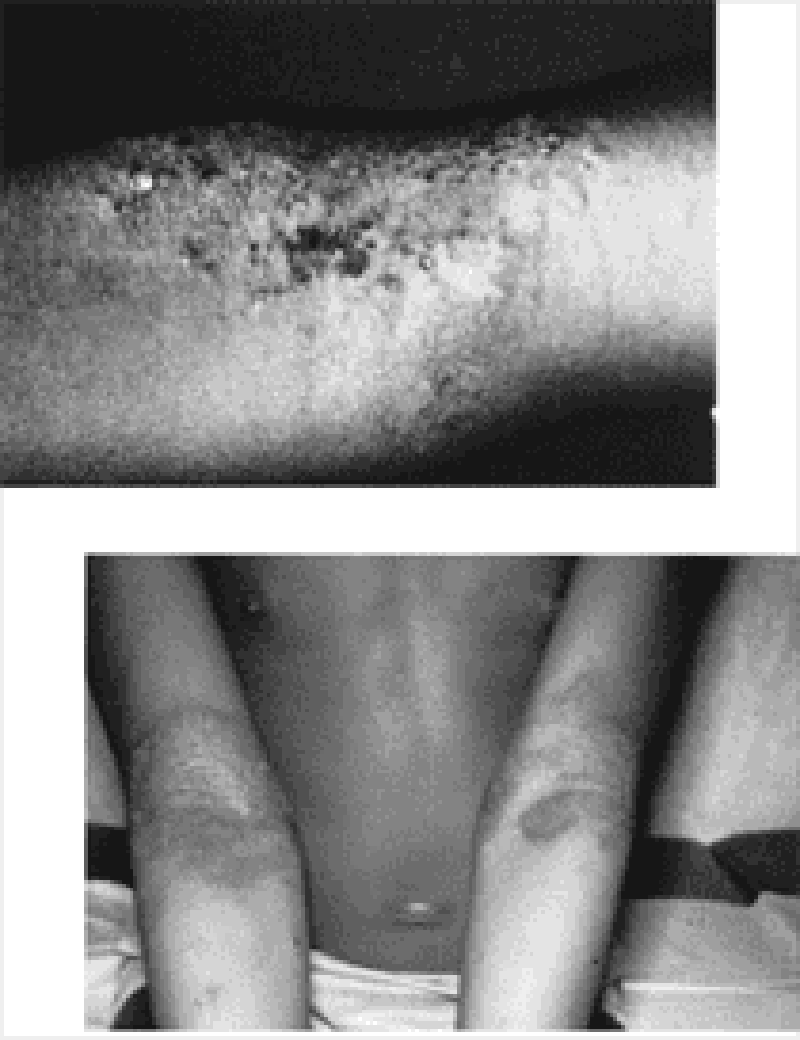
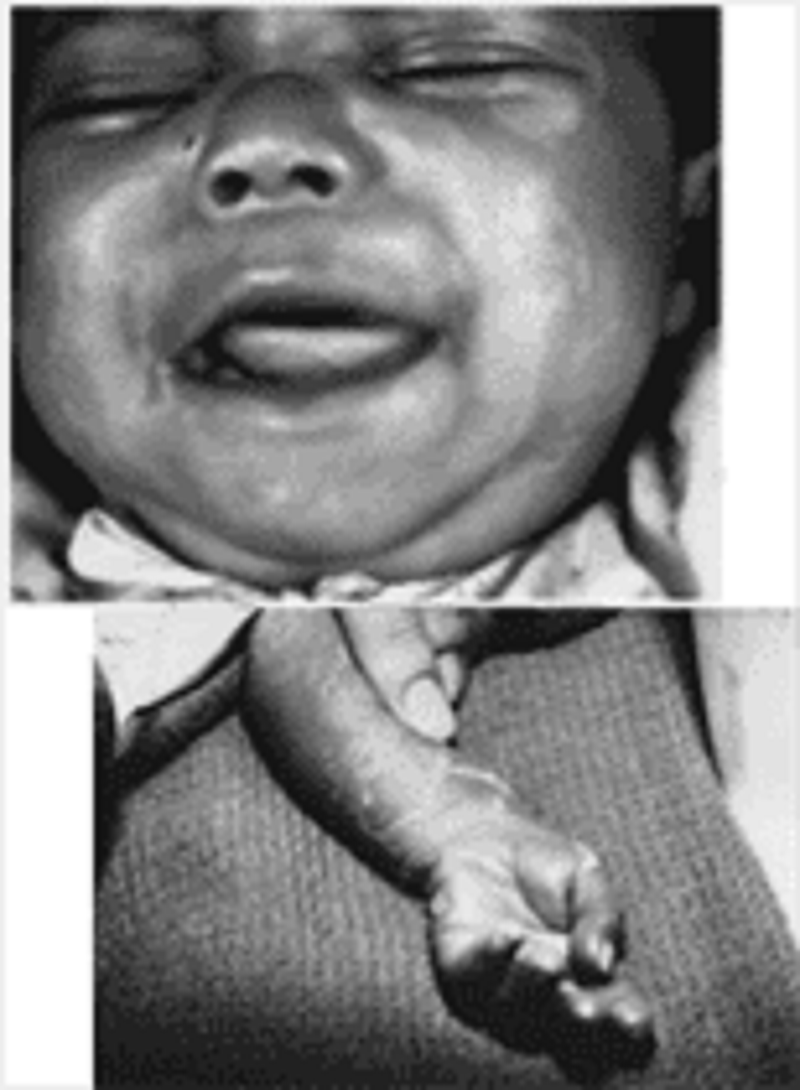
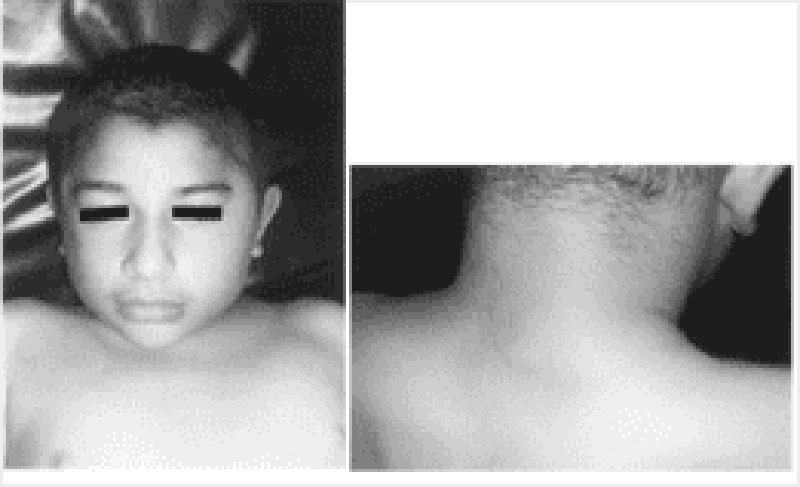
5. A previously healthy 4-year-old child pictured below presents to the emergency room (ER) with a 2-day history of a brightly erythematous rash and temperature of 40°C (104°F). The exquisitely tender, generalized rash is worse in the flexural and perioral areas. The child is admitted and over the next day develops crusting and fissuring around the eyes, mouth, and nose. The desquamation of skin shown in the photograph occurs with gentle traction. Which of the following is the most likely diagnosis?
A. Epidermolysis bullosa
B. Staphylococcal scalded skin syndrome
C. Erythema multiforme
D. Drug eruption
E. Scarlet fever
6. A patient comes to your office for a hospital follow-up. You had sent him to the hospital 3 weeks earlier for persistent fevers but no other symptoms; he was diagnosed with endocarditis and is currently being treated appropriately. Advice to this family should now include which following?
Restrict the child from all strenuous activities.
Give the child a no-salt-added diet.
Provide the child with antibiotic prophylaxis for dental procedures
Test all family members in the home with repeated blood cultures.
Avoid allowing the child to get upset or agitated.
7. A mother calls you on the telephone and says that your 4-year-old son bit the hand of her 2- year-old son 48 hours previously. The area around the injury has become red, indurated, and swollen, and he has a temperature of 39.4┬░C (103┬░F). Which of the following is the most appropriate response?
A) Arrange for a plastic surgery consultation at the next available appointment.
B) Admit the child to the hospital immediately for surgical debridement and antibiotic treatment.
C) Prescribe penicillin over the telephone and have the mother apply warm soaks for 15 minutes four times a day.
D) Suggest purchase of bacitracin ointment to apply to the lesion three times a day.
E) See the patient in the ER to suture the laceration.
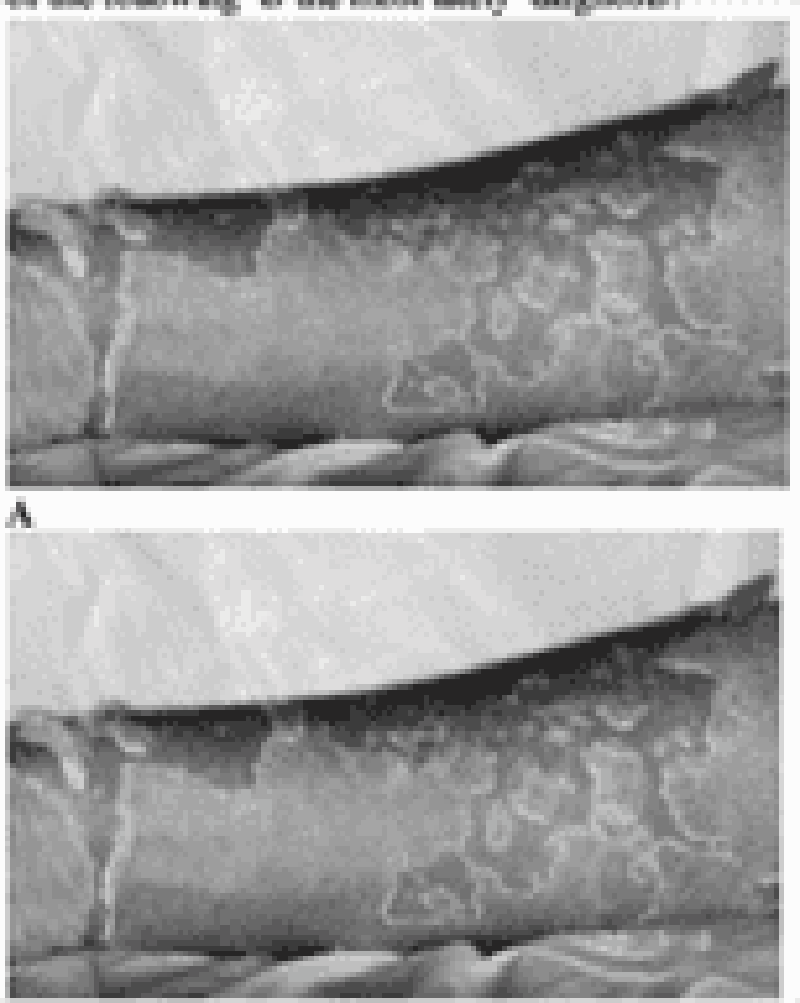
8) The adolescent shown presents with a 14-day history of multiple oval lesions over her back. The rash began with a single lesion over the lower abdomen (A); the other lesions developed over the next days (B). These lesions are slightly pruritic. Which of the following is the most likely diagnosis?
A) Contact dermatitis
B) Pityriasis rosea
C) Seborrheic dermatitis
D) Lichen planus
E) Psoriasis
9) A chubby 6-month-old baby boy is brought to the clinic by his father. His father is concerned that his penis is too small (see photograph). The child is at the 95% for weight and the 50% for length; he has been developing normally and has had no medical problems. Which of the following is the most appropriate first step in management of this child?
A) Surgical consultation
B) Evaluation of penile length after retracting the skin and fat lateral to the penile shaft
C) Ultrasound for uterus and ovaries
D) Weight loss
E) Serum testosterone levels
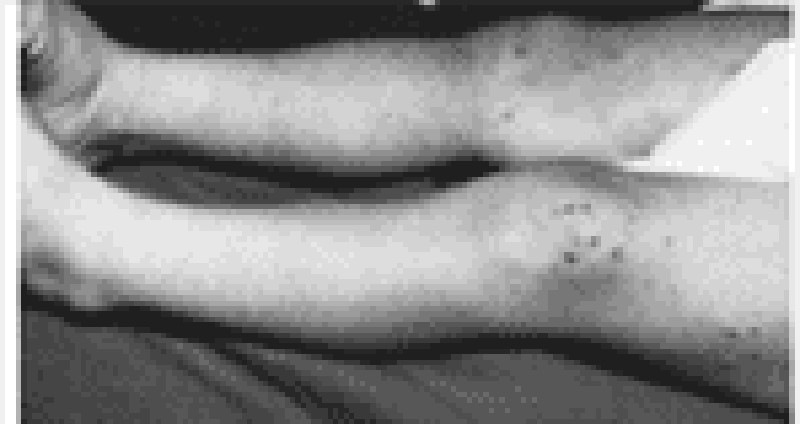
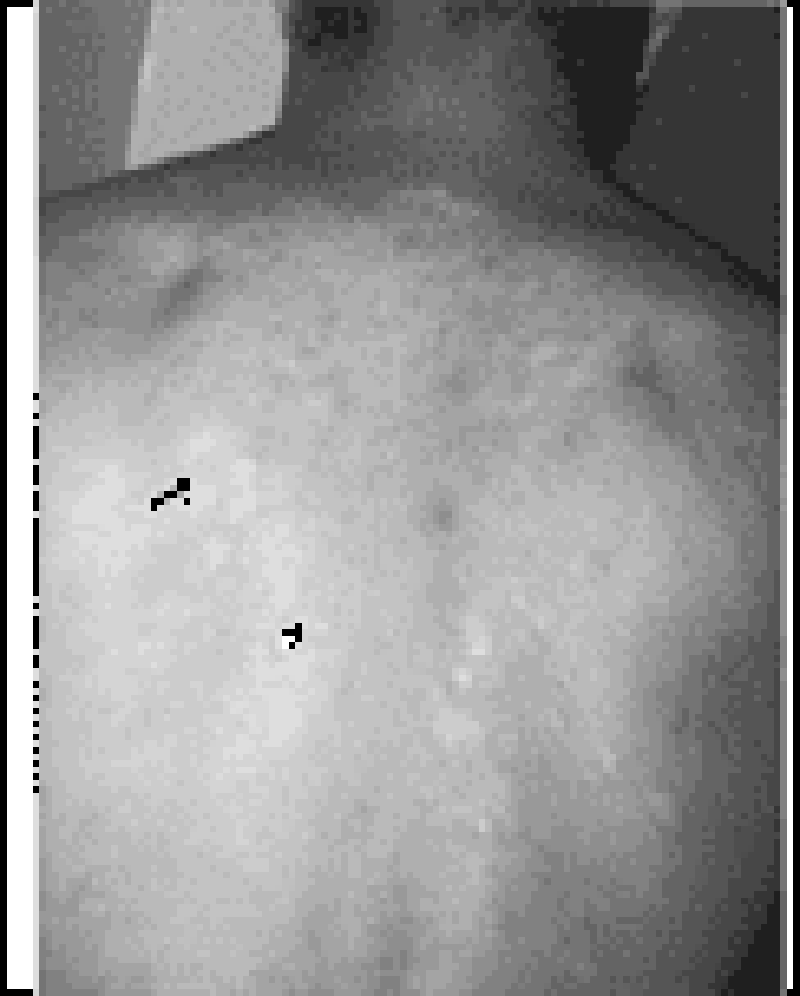
10) A previously healthy 5-year-old boy has a 1-day history of low-grade fever, colicky abdominal pain, and a rash. He is well-appearing and alert. His vital signs, other than a temperature of 38°C (100.5°F) are completely normal. A diffuse, erythematous, maculopapular, and petechial rash is present on his buttocks and lower extremities, as shown in the photograph. He has no localized abdominal tenderness or rebound; bowel sounds are active. Laboratory data demonstrate i) Urinalysis: 30 red blood cells (RBCs) per high-powered field, 2+ protein Stool: Guaiac positive Platelet count: 135,000/μL ii) These findings are most consistent with which of the following?
A) Anaphylactoid purpura
B) Meningococcemia
C) Child abuse
D) Leukemia
E) Hemophilia B

11) A 4-month-old baby boy arrives to the ER cold and stiff. The parents report that he had been healthy and that they put him to bed as usual for the night at the regular time. When they next saw him, in the morning, he was dead. Physical examination is uninformative. A film from a routine skeletal survey is shown below. Which of the following is the most likely diagnosis?
A) Scurvy
B) Congenital syphilis
C) Sudden infant death syndrome (SIDS)
D) Osteogenesis imperfecta
E) Abuse

12) A 6-year-old boy is often teased at school because he has stooled in his underwear almost daily for the last 3 months. He was toilet trained at 2 years of age without difficulty, but over the last 2 years he had developed ongoing constipation. His family is frustrated because they cannot believe him when he says ŌĆĢI didn’t know I had to go.ŌĆ¢ He is otherwise normal; school is going well, and his home life is stable. His only finding on examination is significant for stool in the rectalvault. The plain radiograph of his abdomen is shown. Initial management of this problem should include which of the following?
A) Barium enema and rectal biopsy
B) Family counseling
C) Time-out when he stools in his underwear
D) Clear fecal impaction and short-term stool softener use
E) Daily enemas for 4 weeks

13) A 2-year-old child presents to the office with a paternal complaint of “bowlegs.” The girl has always had bowlegs; her previous pediatrician told the family she would grow out of it. Now, however, it seems to be worsening. Her weight is greater than 95% for age, and she has i) significant bowing out of her legs and internal tibial torsion; otherwise, her examination is normal. A radiograph of her lower leg is shown. Which of the following is the most likely diagnosis?
B) Osgood-Schlatter disease
C) Physiologic genu varum
D) Slipped capital femoral epiphysis
E) Legg-Calv├®-Perthes disease
F) Blount disease
14) A very concerned mother brings a 2-year-old child to your office because of two episodes of a brief, shrill cry followed by a prolonged expiration and apnea. You have been following this child in your practice since birth and know the child to be a product of a normal pregnancy and delivery, to be growing and developing normally, and to have no chronic medical problems. The first episode occurred immediately after the mother refused to give the child some juice; the child became cyanotic, unconscious, and had generalized clonic jerks. A few moments later the child awakened and had no residual effects. The most recent episode (identical in nature) occurred at the grocery store when the childŌĆÖs father refused to purchase a toy for her. Your physical examination reveals a delightful child without unexpected physical examination findings. Which of the following is the most likely diagnosis?
A) Seizure disorder
B) Drug ingestion
C) Hyperactivity with attention deficit
D) Pervasive development disorder
E) Breath-holding spell
15) A 10-year-old child arrives with the complaint of new-onset bed-wetting. He has had no fever, his urine culture is negative, and he has had no new stresses in his life. He is well above the 95th percentile for weight as is much of his family. Which of the following is most helpful in making a diagnosis
A) Fasting plasma glucose of 135 mg/dL
B) Random plasma glucose of 170 mg/dL
C) Two-hour glucose during glucose tolerance test of 165 mg/dL
D) Acanthosis nigricans on the neck
E) Symptoms alone are enough to make the diagnosis
16) You are called to the ER to see one of your patients. The father of this 14-year-old mildly retarded child says that he found the child about 20 minutes ago in the neighborŌĆÖs garden shed with an unknown substance in his mouth. The child first had a headache, but then became agitated and confused; while you are talking to the father in the ER the child begins to have a seizure and dysrhythmia on the cardiac monitor. The blood gas demonstrates a severe metabolic acidosis. Which of the following agents is most likely the culprit?
A) Organophosphate
B) Chlorophenothane (DDT)
C) Sodium cyanide
D) Warfarin
E) Paraquat

17) The mother of a 3-day-old infant brings her child to your office for an early follow-up visit. The mom notes that the child has been eating well, has had no temperature instability, and stools and urinates well. She notes that over the previous 3 days the child has had a progressive rash on the face as pictured here. Which of the following is the most likely diagnosis?
A) Herpes
B) Neonatal acne
C) Milia
D) Seborrheic dermatitis
E) Eczema
18) A 2-year-old child (A) presents with a 4-day history of a rash limited to the feet and ankles. The papular rash is both pruritic and erythematous. The 3-month-old sibling of this patient has similar lesions also involving the head and neck. The most appropriate treatment for this condition includes which of the following?
A) Coal-tar soap
B) Permethrin
C) Hydrocortisone cream
D) Emollients
E) Topical antifungal cream

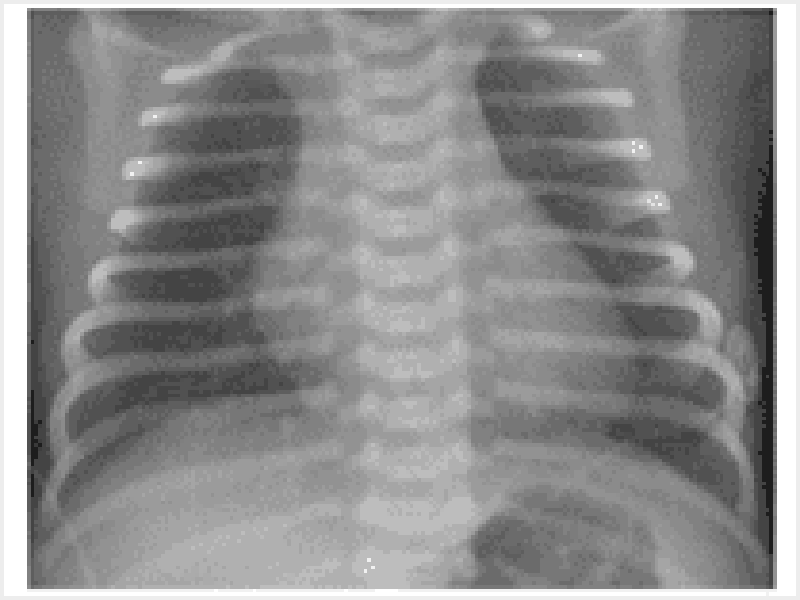
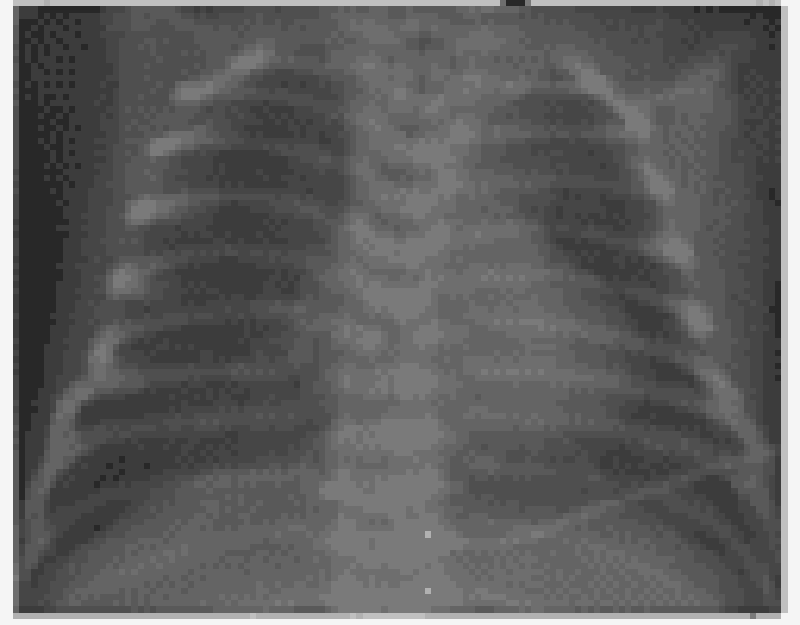
19) An 8-hour-old infant develops increased respiratory distress, hypothermia, and hypotension. A complete blood count (CBC) demonstrates a white blood cell (WBC) count of 2500/μL with 80% bands. The chest radiograph is shown below. Which of the following is the most likely diagnosis?
A) Congenital syphilis
B) Diaphragmatic hernia
C) Group B streptococcalpneumonia
D) Transient tachypnea of the newborn
E) Chlamydial pneumonia
20) A 16-year-old arrives to your office soon after beginning basketball season. He states that he has had progressive pain in his knees. A physical examination reveals, in addition to tenderness, a swollen and prominent tibial tubercle. Radiographs of the area are unremarkable. Which of the following is the most likely diagnosis?
A) Osgood-Schlatter disease
B) Popliteal cyst
C) Slipped capital femoral epiphysis
D) Legg-Calv├®-Perthes disease
E) Gonococcal arthritis
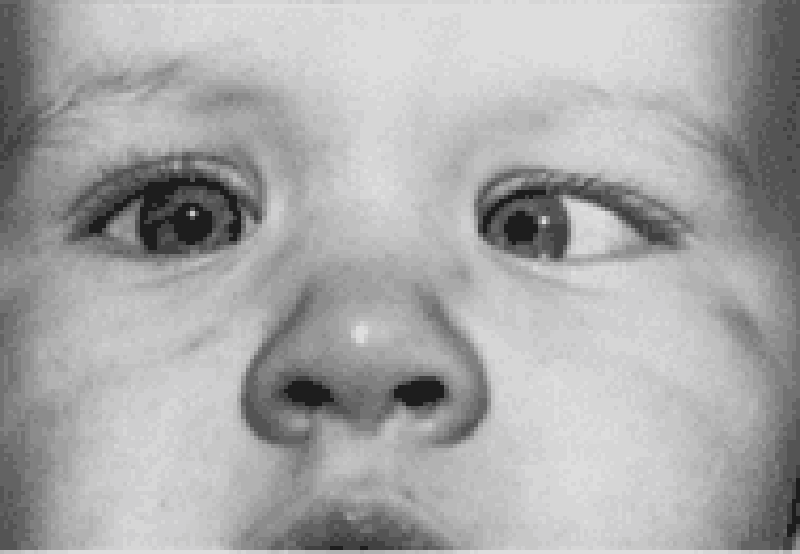
21) You are performing a well-child examination on the 1-year-old child shown in the picture. For this particular problem, which of the following is the most appropriate next step in management?
A) Patch the eye with the greater refractive error
B) Patch the eye that deviates
C) Defer patching or ophthalmologic examination until the child is older and better able to cooperate
D) Reassure the mother that he will outgrow it
E) Refer immediately to ophthalmology
22) You are seeing a 2-year-old child, brought by his father for a well-child examination. In providing age-appropriate anticipatory guidance, you should tell him which of the following?
A) He should set his water heater to 71┬░C (160┬░F) to ensure the sterility of dishes and clothes, thereby decreasing the risk of infections.
B) Milk should be switched from whole to skim or low fat.
C) Continue rear facing car seats.
D) Purchase a bed alarm to assist with the childŌĆÖs nocturnal enuresis.
E) Teach the child to swim so that the parents have the ability to allow the child to be alone in pools.
23) A child can walk well holding on to furniture but is slightly wobbly when walking alone. She uses a neat pincer grasp to pick up a pellet, and she can release a cube into a cup after it has been demonstrated to her. She tries to build a tower of two cubes with variable success. She is most likely at which of the following age?
A) 2 months
B) 4 months
C) 6 months
D) 9 months
E) 1 year
24) You are called by a general practitioner to consult on a patient admit- ted to the hospital 4 days ago. The patient is a 7-month-old white boy with poor weight gain for the past 3 months, who has not gained weight in the hospital despite seemingly adequate nutrition. You take a detailed diet his- tory from his foster mother, and the amounts of formula and baby food intake seem appropriate for age. Physical examination reveals an active, alert infant with a strong suck reflex who appears wasted. You note generalized lymphadenopathy with hepatomegaly. In addition, you find a severe case of oral candidiasis that apparently has been resistant to treatment. Which of the following is the most appropriate next step in the evaluation or treatment of this child?
A) Increase caloric intake because this is probably a case of underfeeding.
B) Order human immunodeficiency virus (HIV) polymerase chain reaction (PCR).Testing because this is likely the presentation of congenitally acquired HIV.
C) Draw blood cultures because this could be sepsis.
D) Perform a sweat chloride test because this is probably cystic fibrosis.
E) Send stool for fecalfat because this is probably a malabsorption syndrome.
25) A 5-year-old boy presents with the severe rash shown in the photographs. The rash is pruritic, and it is especially intense in the flexural areas. The mother reports that the symptoms began in infancy (when it also involved the face) and that her 6-month-old child has similar symptoms. Which of the following is the most appropriate treatment of this condition?
A) Coal-tar soaps and shampoo
B) Topical antifungal cream
C) Ultraviolet light therapy
D) Moisturizers and topical steroids
E) Topical antibiotics
26) A 1-year-old presents for a well-child checkup, but the parents are concerned about giving the child his immunizations. Which of the following is a true contraindication to the administration of the fourth DTaP (diphtheria and tetanus toxoid and acellular pertussis) vaccine?
A) Child is currently on amoxicillin for an otitis media
B) Positive family history of adverse reactions to DTaP vaccine
C) A past history of infantile spasms
D) Child is currently febrile to 39┬░C (102.2┬░F)
E) Prolonged seizures 6 days after the last DTaP vaccine
27) A mother arrives to the clinic with her three children (ages 2 months, 18 months, and 36 months). The 18-month-old has an intensely pruritic scalp, especially in the occipital region, with 0.5-mm lesions noted at the base of hair shafts, as shown in the picture. Which of the following therapies should be avoided in this situation?
A) Treatment of all household contacts with 1% lindane (Kwell)
B) Use of 1:1 vinegar-water rinse for hair for nit removal
C) Washing of all clothing and bedding in very hot water
D) Replacement of all commonly used brushes
E) Advice to the mother that treatment will again be necessary in 7 to 10 days
28) A 2-year-old boy has been vomiting intermittently for 3 weeks and has been irritable, listless, and anorectic. His use of language has regressed to speaking single words. In your evaluation of this patient, which of the following is the most reasonable diagnosis to consider?
A) Expanding epidural hematoma
B) Herpes simplex virus (HSV) encephalitis
C) Tuberculous meningitis
D) Food allergy
E) Bacterial meningitis
29) You find a discrete, whitish polyp that extends through the tympanic membrane in a child with a history of recurrent otitis media. This most likely represents which of the following?
A) A cholesteatoma
B) Tympanosclerosis
C) Acute otitis media with perforation and drainage
D) Dislocation of the malleus from its insertion in the tympanic membrane
E) Excessive cerumen production
30) An 8-month-old infant arrives to the emergency department (ED) with a 2-day history of diarrhea and poor fluid intake. Your quick examination reveals a lethargic child; his heart rate is 180 beats per minute, his respiratory rate is 30 breaths per minute, and his blood pressure is low for age. He has poor skin turgor, 5-second capillary refill, and cool extremities. Which of the following fluids is most appropriate management for his condition?
A) Dextrose 5% in 1/4 normal saline (D5 1/4 NS)
B) Dextrose 5% in 1/2 normal saline (D5 1/2 NS)
C) Normal saline
D) Whole blood
E) Dextrose 10% in water (D10W)
31) During the examination of a 2-month-old infant, you note that the infantŌĆÖs umbilical cord is still firmly attached. This finding prompts you to suspect which of the following?
A) Occult omphalocele
B) Leukocyte adhesion deficiency
C) IgG subclass deficiency
D) Umbilical granuloma
E) Persistent urachus (urachal cyst)
32) You are seeing an established patient, a 4-year-old girl brought in by her mother for vaginal itching and irritation. She is toilet trained and has not complained of frequency or urgency, nor has she noted any blood in her urine. Her mother noted she has been afebrile and has not complained of abdominal pain. Mom denies the risk of inappropriate contact; the girl also denies anyone ŌĆ£touching her there.ŌĆØ Your physical examination of the perineum is significant for the lack of foul odor or discharge. You do note some erythema of the vulvar area but no evidence of trauma. Which of the following is the most appropriate course of action?
A) Refer to pediatric gynecology for removal under anesthesia of a suspected foreign body in the vagina.
B) Counsel mother to stop giving the girl bubble baths, have the girl wear only cotton underwear, and improve hygiene.
C) Refer to social services for suspected physical or sexual abuse.
D) Swab for gonorrhea and plate on chocolate agar, and send urine for Chlamydia.
E) Treat with an antifungal cream for suspected yeast infection.
33) A 20-month-old child is brought to the ED because of fever and irritability and refusal to move his right lower extremity. Physical examination reveals a swollen and tender right knee that resists passive motion. Which of the following is the most likely to yield the diagnosis in this patient?
A) Examination of joint fluid
B) X-ray of the knee
C) Erythrocyte sedimentation rate (ESR)
D) CBC and differential
E) Blood culture
34) A 14-year-old high school student arrives to your clinic for well-child care. In reviewing his records you determine that his most recent immunization for tetanus was at 4 years of age. Which of the following should you recommend?
A) Tetanus toxoid
B) Adult tetanus and diphtheria toxoid (Td)
C) Diphtheria toxoid, whole cell pertussis, and tetanus toxoid (DPT) booster
D) Tetanus toxoid and tetanus immune globulin
E) Tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine adsorbed (Tdap)
35) A 5-year-old boy is brought into the ER immediately after an unfortunate altercation with a neighborŌĆÖs immunized Chihuahua that occurred while the child was attempting to dress the dog as a superhero. The fully immunized child has a small, irregular, superficial laceration on his right forearm that has stopped bleeding. His neuromuscular examination is completely normal, and his perfusion is intact. Management should include which of the following?
A) Irrigation and antimicrobial prophylaxis
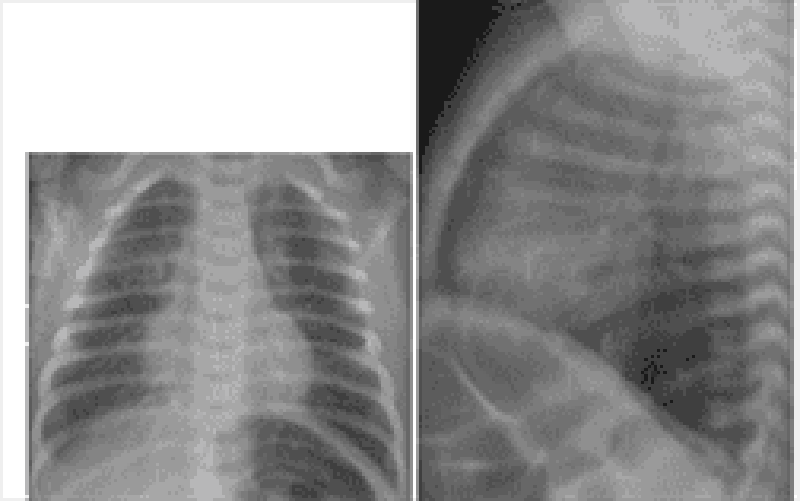
B) Tetanus booster immunization and tetanus toxoid in the wound
C) Copious irrigation
D) Primary rabies vaccination for the child
E) Destruction of the dog and examination of brain tissue for rabies
36) Aunt Mary is helping her family move to a new apartment. During the confusion, 3-year-old Jimmy is noted to become lethargic. The contents of Aunt MaryŌĆÖs purse are strewn about on the floor. In the ER, the lethargic Jimmy is found to have miosis, bradycardia, and hypotension. He develops apnea, respiratory depression, and has to be intubated. His condition would most likely benefit from which of the following therapies?
A) Deferoxamine
B) Pediatric intensive care unit (PICU) support and trial of naloxone
C) N-acetylcysteine (Mucomyst)
D) Atropine
E) Dimercaptosuccinic acid (DMSA, succimer)
37) As a city public health officer, you have been charged with the task of screening high-risk children for lead poisoning. Which of the following is the best screen for this purpose?
A) Careful physical examination of each infant and child
B) Erythrocyte protoporphyrin levels (EP, FEP, or ZPP)
C) CBC and blood smear
D) Blood lead level
E) Environmental history
38) A 15-year-old is participating in high school football practice in August in Texas. He had complained of headache and nausea earlier in practice, but kept playing after a cup of water. He is now confused and combative. He is dizzy and sweating profusely. His temperature is 41┬░C (105.8┬░F). Therapy should consist of which of the following?
A) Provide oral rehydration solutions
B) Administer acetaminophen rectally
C) Order to rest on the bench until symptoms resolve
D) Initiate whole body cold water immersion
E) Tell him to go take a shower and rest until the next dayŌĆÖs practice
39) As part of your anticipatory guidance to new parents of a healthy new- born, you suggest putting the child in which of the following positions for sleep?
A) Supine position
B) Prone position
C) Seated position
D) Trendelenburg position
E) A hammock
40) A mentally retarded 14-year-old boy has a long face, large ears, micropenis, and large testes. Chromosome analysis is likely to demonstrate which of the following?
A) Trisomy 21
B) Trisomy 18
C) Trisomy 13
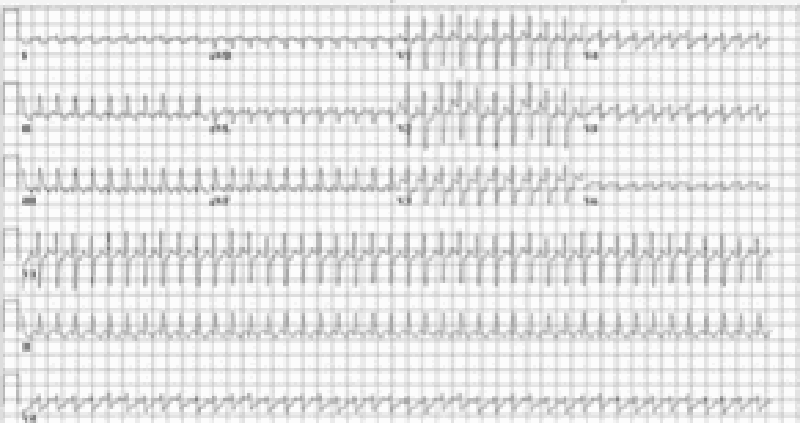
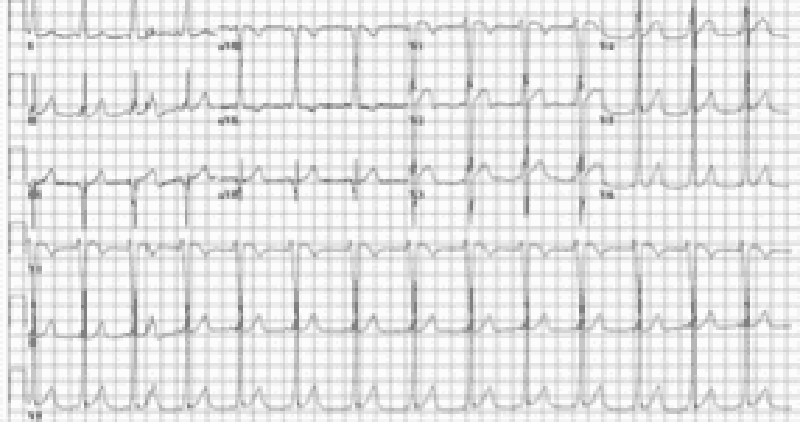
D) Fragile X syndrome
E) Williams syndrome
41) A 5-month-old child with poor growth presents to the ER with generalized tonic-clonic seizure activity of about 30-minute duration that stops upon the administration of lorazepam. Which of the following historical bits of information gathered from the mother is most likely to lead to the correct diagnosis in this patient?
A) The child has had congestion without fever for the past 3 days
B) The child is developmentally normal, as are his siblings
C) The mother has been diluting the infantŌĆÖs formula to make it last longer
D) The mother reports there are two dogs and one cat at home.
E) The mother previously worked as an attorney in an energy-trading firm

42) The term infant pictured below weighs 2200 g (4 lb, 14 oz). He is found to have a ventricular septal defect on cardiac evaluation. This infant appears to have features consistent with which of the following?
A) Perinatal phenytoin exposure
B) Trisomy 21
C) Alport syndrome
D) Fetal alcohol syndrome
E) Infant of diabetic mother
43) A newborn is noted to be quite jaundiced at 3 days of life. Laboratory data demonstrate his total bilirubin to be 17.8 mg/dL (direct bilirubin is 0.3 mg/dL). Which of the following factors is associated with an increased risk of neurologic damage in a jaundiced newborn?
A) Metabolic alkalosis
B) Increased attachment of bilirubin to binding sites caused by drugs such as sulfisoxazole
C) Hyperalbuminemia
D) Neonatal sepsis
E) Maternal ingestion of phenobarbital during pregnancy
44) A 2-hour-old full-term newborn infant is noted by the nursing staff to be having episodes of cyanosis and apnea. Per nursery protocol they place an oxygen saturation monitor on him. When they attempted to feed him, his oxygen levels drop into the 60s. When he is stimulated and cries, his oxygen levels increase into the 90s. Which of the following is the most important next step to quickly establish the diagnosis?
A) Echocardiogram
B) Ventilation perfusion scan
C) Passage of catheter into nose
D) Hemoglobin electrophoresis
E) Bronchoscopic evaluation of palate and larynx
45) A mother calls you frantic because she has just been diagnosed with chicken pox. She delivered 7 days ago a term infant that appears to be eating, stooling, and urinating well. The child has been afebrile and seems to be doing well. Which of the following is the most appropriate step in management?
A) Isolate the infant from the mother.
B) Hospitalize the infant in the isolation ward.
C) Administer acyclovir to the infant.
D) Administer varicella-zoster immunoglobulin to the infant.
E) Advise the mother to continue regular well-baby care for the infant.
46) A mother wishes to breast-feed her newborn infant, but is worried about medical conditions that would prohibit her from doing so. You counsel her that of her listed conditions, which of the following is a contraindication to breast-feeding?
A) Upper respiratory tract infection
B) Cracked and bleeding nipples
C) Mastitis
D) Inverted nipples
E) HIV infection
47) A mother delivers a neonate with meconium staining and Apgar scores of 3 at 1 and 5 minutes of life. She had no prenatal care and the delivery was by emergency cesarean section for what the obstetricians report as ŌĆ£severe fetal bradycardia.ŌĆØ Which of the following sequelae could be expected to develop in this intubated neonate with respiratory distress?
A) Sustained rise in pulmonary arterial pressure
B) Hyperactive bowel sounds
C) Microcephaly with micrognathia
D) Cataracts
E) Thrombocytosis
48) A 2-year-old boy is being followed for congenital cytomegalovirus (CMV) infection. He is deaf and developmentally delayed. The childŌĆÖs mother informs you that she has just become pregnant and is concerned that the new baby will be infected and may develop serious consequences. Which of the following is true?
A) The mother has antibodies to CMV that are passed to the fetus.
B) The motherŌĆÖs infection cannot become reactivated.
C) The likelihood that the new baby will become clinically ill is approximately 80%.
D) Termination of pregnancy is advised.
E) The new infant should be isolated from the older child.
49) A full-term infant is born after a normal pregnancy; delivery, however, is complicated by marginal placental separation. At 12 hours of age, the child, although appearing to be in good health, passes a bloody meconium stool. For determining the cause of the bleeding, which of the following diagnostic procedures should be performed first?
A) A barium enema
B) An Apt test
C) Gastric lavage with normal saline
D) An upper gastrointestinal series
E) A platelet count, prothrombin time, and partial thromboplastin time
50) As you are about to step out of a newly delivered motherŌĆÖs room, she mentions that she wants to breast-feed her healthy infant, but that her obstetrician was concerned about one of the medicines she was taking. Which of the womanŌĆÖs medicines, listed below, is clearly contraindicated in breast-feeding?
A) Ibuprofen as needed for pain or fever
B) Labetalol for her chronic hypertension
C) Amphetamines for her attention deficit disorder
D) Carbamazepine for her seizure disorder
E) Acyclovir for her HSV outbreak
51) A recovering premature infant who weighs 950 g (2 lb, 1 oz) is fed breast milk to provide 120 cal/kg/d. Over the ensuing weeks, the baby is most apt to develop which of the following?
A) Hypernatremia
B) Hypocalcemia
C) Blood in the stool
D) Hyperphosphatemia
E) Vitamin D toxicity
52) A primiparous woman whose blood type is O positive gives birth at term to an infant who has A-positive blood and a hematocrit of 55%. A total serum bilirubin level obtained at 36 hours of age is 12 mg/dL. Which of the following additional laboratory findings would be characteristic of ABO hemolytic disease in this infant?
A) A normal reticulocyte count
B) A positive direct Coombs test
C) Crescent-shaped red blood cells in the blood smear
D) Elevated hemoglobin
E) Petechiae

53) The nurse from the level 2 neonatal intensive care nursery calls you to evaluate a baby. The infant, born at 32 weeks’ gestation, is now 1 week old and had been doing well on increasing nasogastric feedings. This afternoon, how- ever, the nurse noted that the infant has vomited the last two feedings and seems less active. Your examination reveals a tense and distended abdomen with decreased bowelsounds. As you are evaluating the child, he has a grossly bloody stool. The plain film of his abdomen is shown. The next step in your management of this infant should include which of the following?
A) Surgical consultation for an emergent exploratory laparotomy.
B) Continued feeding of the infant, as gastroenteritis is usually self-limited.
C) Stool culture to identify the etiology of the bloody diarrhea and an infectious diseases consultation.
D) Stopping feeds, beginning intravenous fluids, ordering serial abdominal films, and initiating systemic antibiotics.
E) Removal of nasogastric tube, placement of a transpyloric tube and, after confir- mation via radiograph of tube positioning, switching feeds from nasogastric to nasoduodenal.
54) An infant weighing 1400 g (3 lb) is born at 32 weeks’ gestation. Initial evaluation was benign, and the infant was transferred to the level 2 nursery for prematurity. The nurse there calls at 1 hour of life and reports the infant is tachypneic. Vital signs include a heart rate of 140 beats per minute, a respiratory rate of 80 breaths per minute, a temperature of 35°C (95°F), and a peripheral oxygen saturation of 98%. The lungs are clear with bilateral breath sounds and there is no murmur; the infant is in no dis- tress. The child’s chest radiograph is shown. Which of the following is the most appropriate next step in evaluating the infant?
A) Obtain a complete blood count and differential.
B) Perform a lumbar puncture.
C) Administer intravenously 5cc of D50W.
D) Place the infant under a warmer.
E) Administer supplemental oxygen.
55) Two new mothers are discussing their infants outside the neonatal intensive care unit. Both were born at 36 weeksŌĆÖ gestation. One infant weighs 2600 g (5 lb, 12 oz) while the other infant weighs 1600 g (3 lb, 8 oz). The mother of the second infant should be told that her child is more likely to have which of the following conditions?
A) Congenital malformations
B) Low hematocrit
C) Hyperglycemia
D) Surfactant deficiency
E) Rapid catch-up growth
56) A 3-day-old infant, born at 32 weeksŌĆÖ gestation and weighing 1700 g (3 lb, 12 oz), has three episodes of apnea, each lasting 20 to 25 seconds and occurring after a feeding. During these episodes, the heart rate drops from 140 to 100 beats per minute, and the child remains motionless; between episodes, however, the child displays normal activity. Blood sugar is 50 mg/dL and serum calcium is normal. Which of the following is most likely true regarding the childŌĆÖs apneic periods?
A) They are due to an immature respiratory center.
B) They are a part of periodic breathing.
C) They are secondary to hypoglycemia.
D) They are manifestations of seizures.
E) They are evidence of underlying pulmonary disease.
57) You have an 11-day-old term infant in your office for a well-child visit. The mother notes that she received a letter that day from the stateŌĆÖs Department of Health reporting that her childŌĆÖs newborn screen had come back abnormal, indicating possible galactosemia. Which of the following is the most appropriate management at this point?
A) Discontinue oral feeds and begin total parenteralnutrition.
B) Supplement her breast-feeding with a multivitamin.
C) Refer to endocrinology for evaluation.
D) Discontinue breast-feeding and initiate soy formula feedings
E) Ultrasound of pancreas.
58) The father of a 1-week-old infant comes to the office in a panic. He has just noticed on his child a right anterior shoulder mass that seems ten- der. The father is an osteosarcoma survivor and fears the child has the same malignancy. In reviewing the babyŌĆÖs discharge papers, you note the child was a term, appropriate-for-gestational-age vaginal delivery with a birth weight of 3200 g (7 lb, 1 oz). Apgar scores were 9 at 1 and 5 minutes. Your examination is significant for a large firm mass on the right clavicle; the rest of the examination is normal. Management of this problem should include which of the following?
A) Magnetic resonance imaging of the right shoulder
B) Reassurance and supportive care
C) A biopsy of the mass for culture and cytology
D) Referralto an orthopedic surgeon
E) Skin biopsy to test for osteogenesis imperfecta
59) A 1-day-old infant who was born by a difficult forceps delivery is alert and active. She does not move her left arm spontaneously or during a Moro reflex. Rather, she prefers to maintain it internally rotated by her side with the forearm extended and pronated. The rest of her physical examination is normal. This clinical scenario most likely indicates which of the following?
A) Fracture of the left clavicle
B) Fracture of the left humerus
C) Left-sided Erb-Duchenne paralysis
D) Left-sided Klumpke paralysis
E) Spinal injury with left hemiparesis
60) You are examining a newborn infant in the well-baby nursery. The infant was the product of a benign pregnancy and vaginal delivery; he appears to be in no distress. Interestingly, your measurement of fronto- occipital head circumference is about 2 cm larger than the initial measurement done severalhours before. Your examination otherwise is significant for tachycardia and a ŌĆ£squishyŌĆØ feel to the entire scalp. You can elicit a fluid wave over the scalp. Management of this condition should include which of the following?
A) Transfer to the newborn ICU
B) Observation and parental reassurance
C) CT scan of the skull with bone windows
D) Surgical drainage
E) Elevation of the head of the crib
61) A 19-year-old primiparous woman develops toxemia in her last trimester of pregnancy and during the course of her labor is treated with magnesium sulfate. At 38 weeksŌĆÖ gestation, she delivers a 2100-g (4-lb, 10-oz) infant with Apgar scores of 1 at 1 minute and 5 at 5 minutes. Laboratory studies at 18 hours of age reveal a hematocrit of 79%, platelet count of 100,000/╬╝L, glucose 41 mg/dL, magnesium 2.5 mEq/L, and calcium 8.7 mg/dL. Soon after, the infant has a generalized convulsion. Which of the following is the most likely cause of the infantŌĆÖs seizure?
A) Polycythemia
B) Hypoglycemia
C) Hypocalcemia
D) Hypermagnesemia
E) Thrombocytopenia
62) An infant who appears to be of normal size is noted to be lethargic and somewhat limp after birth. The mother is 28 years old, and this is her fourth delivery. The pregnancy was uncomplicated, with normal fetalmonitoring prior to delivery. Labor was rapid, with local anesthesia and intravenous meperidine (Demerol) administered for maternal pain control. Which of the following therapeutic maneuvers is likely to improve this infantŌĆÖs condition most rapidly?
A) Intravenous infusion of 10% dextrose in water
B) Administration of naloxone (Narcan)
C) Administration of vitamin K
D) Measurement of electrolytes and magnesium levels
E) Neurologic consultation
63) At 43 weeksŌĆÖ gestation, a long, thin infant is delivered. The infant is apneic, limp, pale, and covered with ŌĆĢpea soupŌĆ¢ amniotic fluid. Which of the following is the best first step in the resuscitation of this infant at delivery?
A) Intubation and suction of the trachea; provision of oxygen
B) Artificial ventilation with bag and mask
C) Chest compressions
D) Administration of 100% oxygen by mask
E) Catheterization of the umbilical vein

64) The newborn pictured below was born at home and has puffy, tense eye- lids; red conjunctivae; a copious amount of purulent ocular discharge; and chemosis 2 days after birth. Which of the following is the most likely diagnosis?
A) Dacryocystitis
B) Chemical conjunctivitis
C) Pneumococcalophthalmia
D) Gonococcal ophthalmia
E) Chlamydial conjunctivitis
65) After an uneventful labor and delivery, an infant is born at 32 weeksŌĆÖ gestation weighing 1500 g (3 lb, 5 oz). Respiratory difficulty develops immediately after birth and increases in intensity thereafter. At 6 hours of age, the childŌĆÖs respiratory rate is 60 breaths per minute. Examination reveals grunting, intercostal retraction, nasal flaring, and marked cyanosis in room air. Auscultation reveals poor air movement. Physiologic abnormalities compatible with these data include which of the following?
A) Decreased lung compliance, reduced lung volume, left-to-right shunt of blood
B) Decreased lung compliance, reduced lung volume, right-to-left shunt of blood
C) Decreased lung compliance, increased lung volume, left-to-right shunt of blood
D) Normal lung compliance, reduced lung volume, left-to-right shunt of blood
E) Normal lung compliance, increased lung volume, right-to-left shunt of blood
66) A term infant is born to a known HIV-positive mother. She has been taking antiretroviral medications for the weeks prior to the delivery of her infant. Routine management of the healthy infant should include which of the following?
A) Admission to the neonatal intensive care unit for close cardiovascular monitoring
B) HIV ELISA on the infant to determine if congenital infection has occurred
C) A course of zidovudine for the infant
D) Chest radiographs to evaluate for congenital Pneumocystis carinii
E) Administration of IVIG to the baby to decrease the risk of perinatal HIV infection
67) Initial examination of a full-term infant weighing less than 2500 g (5 lb, 8 oz) shows edema over the dorsum of her hands and feet. Which of the following findings would support a diagnosis of Turner syndrome?
A) A liver palpable to 2 cm below the costal margin
B) Tremulous movements and ankle clonus
C) Redundant skin folds at the nape of the neck
D) A transient, longitudinal division of the body into a red half and a pale half
E) Softness of the parietal bones at the vertex
68) You have been recently named as the medical director of the normal newborn nursery in your community hospital and have been asked to write standardized admission orders for all pediatricians to follow. Which of the following vaccines will you include on these orders?
A) Hepatitis A vaccine
B) Hepatitis B vaccine
C) Combination diphtheria, tetanus, and acellular pertussis vaccine
D) Inactivated polio virus
E) Haemophilus influenza B vaccine

69) A 1-week-old black infant presents to you for the first time with a large, fairly well-defined, purple lesion over the buttocks bilaterally, as shown in the photograph. The lesion is not palpable, and it is not warm nor tender. The mother denies trauma and reports that the lesion has been present since birth. This otherwise well-appearing infant is growing and developing normally and appears normal upon physical examination. Which of the following is the most appropriate course of action in this infant?
A) Report the family to child protective services
B) Reassurance of the normalcy of the condition
C) Soft tissues films of the buttocks to identify calcifications
D) Administration of vitamin K
E) Measurement of bleeding time as well as factor VII and XI levels
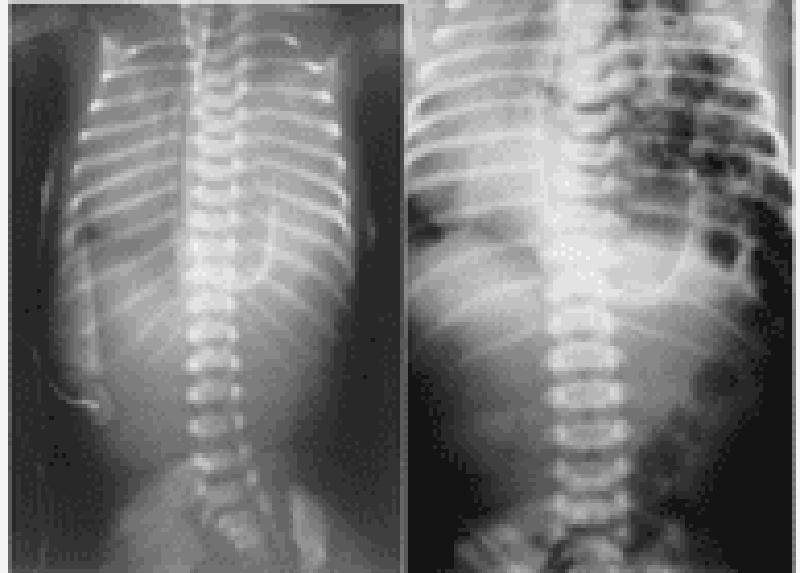
70) A newborn infant develops respiratory distress immediately after birth. His abdomen is scaphoid. No breath sounds are heard on the left side of his chest, but they are audible on the right. Immediate intubation is successfulwith little or no improvement in clinical status. Emergency chest x-ray is shown (A) along with an x-ray 2 hours later (B). Which of the following is the most likely explanation for this infant’s condition?
A) Pneumonia
B) Cystic adenomatoid malformation
C) Diaphragmatic hernia
D) Choanal atresia
E) Pneumothorax
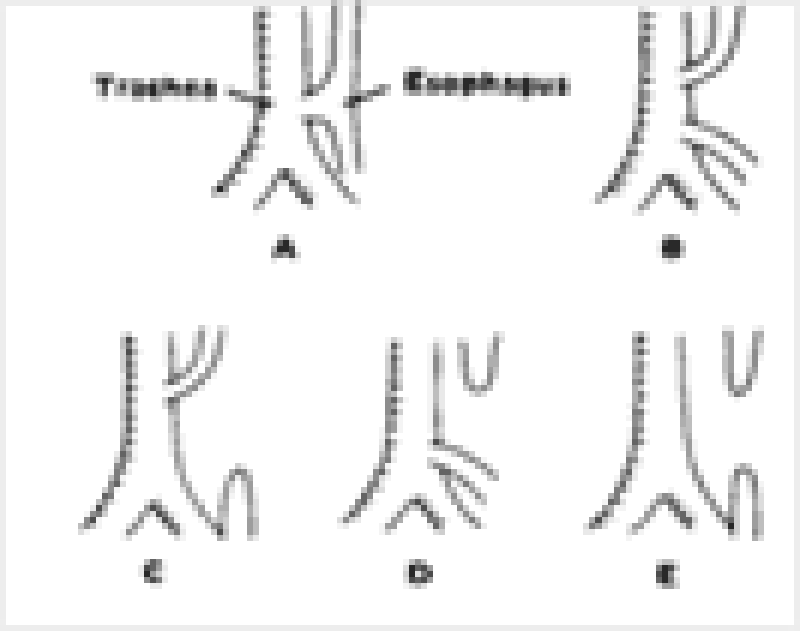
71) Shortly after birth, an infant develops abdominal distention and begins to drool. When she is given her first feeding, it runs out the side of her mouth, and she coughs and chokes. Physical examination reveals tachypnea, inter- costal retractions, and bilateral pulmonary rales. The esophageal anomaly that most commonly causes these signs and symptoms is illustrated by which of the following?
A) Figure A
B) Figure B
C) Figure C
D) Figure D
E) Figure E
72) You are advised by the obstetrician that the mother of a baby she has delivered is a carrier of hepatitis B surface antigen (HBsAg-positive). Which of the following is the most appropriate action in managing this infant?
A) Screen the infant for HBsAg.
B) Isolate the infant with enteric precautions.
C) Screen the mother for hepatitis B ŌĆ£eŌĆØantigen (HBeAg).
D) Administer hepatitis B immune globulin and hepatitis B vaccine to the infant.
E) Do nothing because transplacentally acquired antibody will prevent infection in the infant.
73) You are called to a delivery of a term infant, about to be born via cesarean section to a mother with multiple medical problems, including a 1-month history of a seizure disorder, for which she takes phenytoin; rheumatic heart disease, for which she must take penicillin daily for life; hypertension, for which she takes propranolol; acid reflux, for which she takes aluminum hydroxide; and a deep venous thrombosis in her left calf diagnosed 2 days ago, for which she was started on a heparin infusion. The obstetrician is concerned about the possible effects of the motherŌĆÖs multiple medications on the newborn infant. Which of the following medications is most likely to cause harm in this newborn infant at delivery?
A) Propranolol
B) Penicillin
C) Aluminum hydroxide
D) Phenytoin
E) Heparin
74) Your older sister, her husband, their 2-day-old infant, and their pet Chihuahua arrive at your door. The parents of the child are concerned because the pediatrician noted the child was ŌĆ£yellowŌĆØ and ordered some studies. They produce a wad of papers for you to review. Both the mother and baby have O-positive blood. The babyŌĆÖs direct serum bilirubin is 0.2 mg/dL, with a total serum bilirubin of 11.8 mg/dL. Urine bilirubin is positive. The infantŌĆÖs white blood cell count is 13,000/╬╝L with a differential of 50% polymorphonuclear cells, 45% lymphocytes, and 5% monocytes. The hemoglobin is 17 g/dL, and the platelet count is 278,000/╬╝L. Reticulocyte count is 1.5%. The peripheral smear does not show fragments or abnormal cell shapes. Which of the following is the most likely explanation for this infantŌĆÖs skin color?
A) Rh or ABO hemolytic disease
B) Physiologic jaundice
C) Sepsis
D) Congenital spherocytic anemia
E) Biliary atresia
75) At the time of delivery, a woman is noted to have a large volume of amniotic fluid. At 6 hours of age, her baby begins regurgitating small amounts of mucus and bile-stained fluid. Physical examination of the infant is normal, and an abdominal x-ray is obtained (see below). Which of the following is the most likely diagnosis of this infant’s disorder?
A) Gastric duplication
B) Pyloric stenosis
C) Esophageal atresia
D) Duodenal atresia
E) Midgut volvulus
76) The mother and father of a newborn come in for the 2-week checkup. The mother complains of ŌĆ£colicŌĆØ and asks if she can switch to goatŌĆÖs milk instead of breast milk. Which of the following should be your main concern about using goatŌĆÖs milk instead of breast milk or cowŌĆÖs milk?
A) It has insufficient calories.
B) It has insufficient folate.
C) It has insufficient whey.
D) It has insufficient casein.
E) It has insufficient fat.

77) You see the newborn baby shown below for the first time in the nursery. You consult plastic and reconstructive surgeon as well as the hospital’s speech therapist. Understandably, the parents have many questions. Which of the following statements is appropriate anticipatory guidance for this family?
A) Parenteralalimentation is recommended to prevent aspiration.
B) Surgical closure of the palatal defect should be done before 3 months of age.
C) Good anatomic closure will preclude the development of speech defects.
D) Recurrent otitis media and hearing loss are likely complications.
E) The chance that a sibling also would be affected is 1 in 1000.
78) The mother of a 2-week-old infant reports that since birth, her infant sleeps most of the day; she has to awaken her every 4 hours to feed, and she will take only an ounce of formula at a time. She also is concerned that the infant has persistently hard, pellet-like stools. On your examination you find an infant with normal weight and length, but with an enlarged head. The heart rate is 75 beats per minute and the temperature is 35┬░C (95┬░F). The child is still jaundiced. You note large anterior and posterior fontanelles, a distended abdomen, and an umbilical hernia. This clinical presentation is likely a result of which of the following?
A) Congenital hypothyroidism
B) Congenital megacolon (Hirschsprung disease)
C) Sepsis
D) Infantile botulism
E) Normal development
79) A routine prenatal ultrasound reveals a male fetus with meningomyelocele. The 24-year-old primigravid mother is told the infant will require surgery shortly after birth. You counsel her about the etiology of this defect and the risk of further pregnancies being similarly affected, and state which of the following?
A) The hereditary pattern for this condition is autosomal recessive.
B) The prenatal diagnosis can be made by the detection of very low levels of alpha- fetoprotein in the amniotic fluid.
C) Subsequent pregnancies are not at increased risk compared to the general population.
D) Supplementation of maternal diet with folate leads to a decrease in incidence of this condition.
E) Neither environmental nor social factors have been shown to influence the incidence.
80) A term, 4200-g (9-lb, 4-oz) female infant is delivered via cesarean section because of cephalopelvic disproportion. The amniotic fluid was clear, and the infant cried almost immediately after birth. Within the first 15 minutes of life, however, the infant’s respiratory rate increased to 80 breaths per minute, and she began to have intermittent grunting respirations. The infant was transferred to the level 2 nursery and was noted to have an oxygen saturation of 94%. The chest radiograph is shown. Which of the following is the most likely diagnosis?
A) Diaphragmatic hernia
B) Meconium aspiration
C) Pneumonia
D) Idiopathic respiratory distress syndrome
E) Transient tachypnea of the newborn
81) The infant in the following picture presents with hepatosplenomegaly, anemia, persistent rhinitis, and a maculopapular rash. Which of the following is the most likely diagnosis for this child?
A) Toxoplasmosis
B) Glycogen storage disease
C) Congenital hypothyroidism
D) Congenital syphilis
E) Cytomegalovirus disease

82) A well-appearing, 3200-g (7-lb, 1-oz) black infant is noted to have fifth finger (postaxial) polydactyly. The extra digit has no skeletal duplications and is attached to the rest of the hand by a threadlike soft tissue pedicle (see photograph). Appropriate treatment for this condition includes which of the following?
A) Chromosomal analysis
B) Excision of extra digit
C) Skeletal survey for other skeletal abnormalities
D) Echocardiogram
E) Renal ultrasound
83) An infant born at 35 weeksŌĆÖ gestation to a mother with no prenatal care is noted to be jittery and irritable, and is having difficulty feeding. You note coarse tremors on examination. The nurses report a high-pitched cry and note severalepisodes of diarrhea and emesis. You suspect which of the following?
A) Fetal alcohol syndrome
B) Prenatalexposure to marijuana
C) Heroin withdrawal syndrome
D) Cocaine exposure in utero
E) Tobacco use by the mother
84) A previously healthy full-term infant has several episodes of duskiness and apnea during the second day of life. Diagnostic considerations should include which of the following?
A) Hemolytic anemia
B) Congenital heart disease
C) Idiopathic apnea
D) Harlequin syndrome
E) Hyperglycemia
85) The signs and symptoms of meningitis in an infant can be different than those in an adult. Which of the following signs and symptoms of meningitis is more helpful in an adult patient than in a 4-month-old?
A) Lethargy
B) Jaundice
C) Vomiting
D) Brudzinski sign
E) Hypothermia
86) A woman gives birth to twins at 38 weeksŌĆÖ gestation. The first twin weighs 2800 g (6 lb, 3 oz) and has a hematocrit of 70%; the second twin weighs 2100 g (4 lb, 10 oz) and has a hematocrit of 40%. Which of the following statements is correct?
A) The second twin is at risk for developing respiratory distress, cyanosis, and congestive heart failure.
B) The first twin is more likely to have hyperbilirubinemia and convulsions.
C) The second twin is at risk for renal vein thrombosis.
D) The second twin probably has hydramnios of the amniotic sac.
E) The second twin is likely to be pale, tachycardic, and hypotensive.
87) Parents bring a 5-day-old infant to your office. The mother is O negative and was Coombs positive at delivery. The term child weighed 3055 g (6 lb, 1 oz) at birth and had measured baseline hemoglobin of 16 g/dL and a total serum bilirubin of 3 mg/dL. He passed a black tarlike stool within the first 24 hours of life. He was discharged at 30 hours of life with a stable axillary temperature of 36.5┬░C (97.7┬░F). Today the infantŌĆÖs weight is 3000 g, his axillary temperature is 35┬░C (95┬░F), and he is jaundiced to the chest. Parents report frequent yellow, seedy stool. You redraw labs and find his hemoglobin is now 14 g/dL, and his total serum bilirubin is 13 mg/dL. The change in which of the following parameters is of most concern?
A) Hemoglobin
B) Temperature
C) Body weight
D) Bilirubin
E) Stool
88) You are called to a delivery of a woman with no prenatal care; she is in active labor but has no history of amniotic rupture. The biophysical profile done in the emergency center revealed severe oligohydramnios. When you get this infant to the nursery, you should carefully evaluate him for which of the following?
A) Anencephaly
B) Trisomy 18
C) Renal agenesis
D) Duodenal atresia
E) Tracheoesophagealfistula
89) A newborn infant becomes markedly jaundiced on the second day of life, and a faint petechial eruption, first noted at birth, is now a generalized purpuric rash. Hematologic studies for hemolytic diseases are negative. Acute management should include which of the following?
A) Liver ultrasound
B) Isolation of the infant from pregnant hospital personnel
C) Urine drug screen on the infant
D) Discharge with an early follow-up visit in 2 days to recheck bilirubin
E) Thyroid hormone assay
90) A 14-year-old girl, angry at her mother for taking away her MP3 player, takes an unknown quantity of a friendŌĆÖs pills. Within the first hour she is sleepy, but in the emergency center she develops a widened QRS complex on her electrocardiogram (ECG), hypotension, and right bundle branch block. The therapy you would initiate for this ingestion is which of the following?
A) N-acetylcysteine (Mucomyst)
B) Naloxone
C) Intensive care unit (ICU) admission, close monitoring, and possible Fab anti- body fragments
D) Ethanol
E) Deferoxamine
91) A 10-year-old boy, the star pitcher for the Salt Lake City Little League baseball team, had a sore throat about 2 weeks ago but did not tell anyone because he was afraid he would miss the play-offs. Since severalchildren have been diagnosed with rheumatic fever in the area, his mother is worried that he may be at risk as well. You tell her that several criteria must be met to make the diagnosis but the most common finding is which of the following?
A) Carditis
B) Arthralgia
C) Erythema marginatum
D) Chorea
E) Subcutaneous nodules
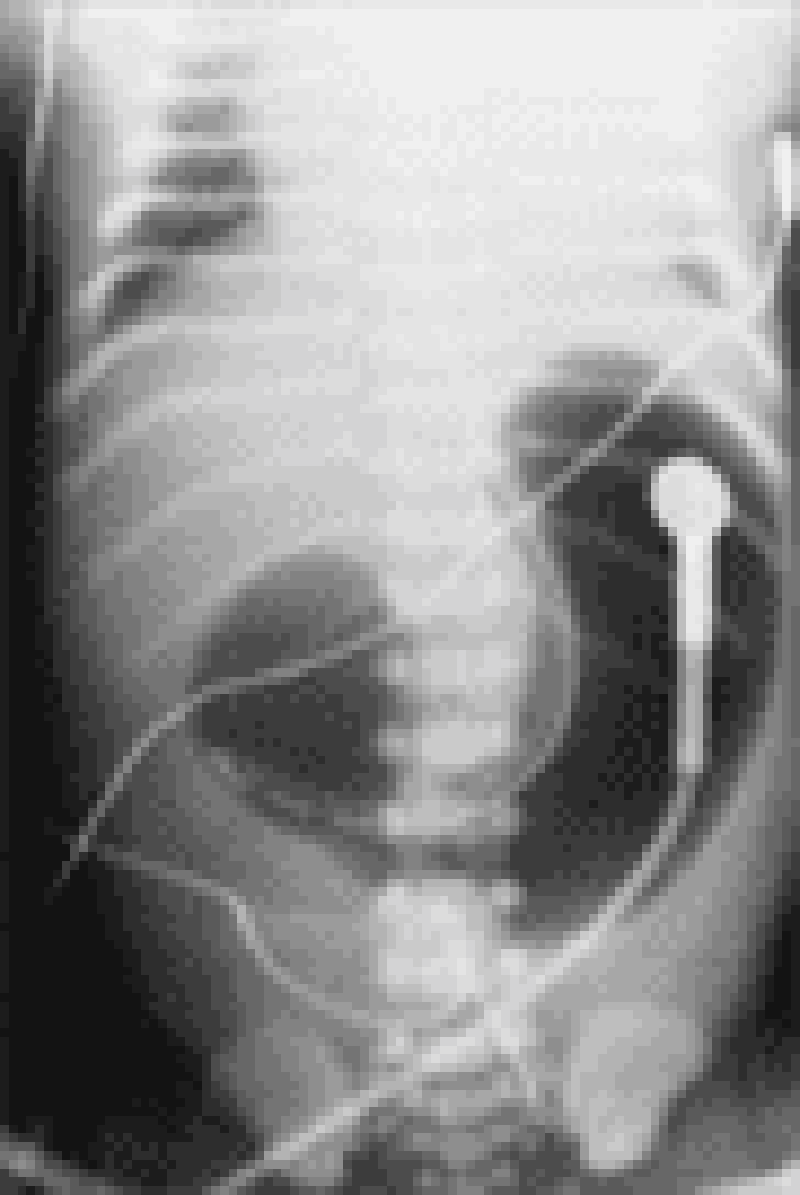
92) You are seeing a 2-year-old boy for the first time. His father denies any past medical or surgical history, but does note that the child’s day care recently sent a note home asking about severalepisodes, usually after the child does not get what he wants, when he “breathes funny” and sits in a corner with his knees under his chin for a few minutes. The day-care staffers think this “self-imposed time-out” is a good thing, but they worry about the breathing. One teacher even though he once looked blue, but decided that it was probably because of the finger paints he had been using. On examination, you identify a right ventricular impulse, a systolic thrill along the left sternal border, and a harsh systolic murmur (loudest at the left sternal border but radiating through the lung fields). His chest radio- graph and ECG are shown. Which of the following congenital cardiac lesions would you expect to find in this child?
A) Patent ductus arteriosus
B) Right ventricular outflow obstruction
C) Atrial septal defect (ASD)
D) Transposition of the great vessels with a patent foramen ovale
E) Hypoplastic left heart
93) The parents of a 2-month-old baby boy are concerned about his risk of coronary artery disease because of the recent death of his 40-year-old maternal uncle from a myocardial infarction. Which of the following is the most appropriate management in this situation?
A) Screen the parents for total cholesterol.
B) Counsel the parents regarding appropriate dietary practices for a 2-month-old infant and test him for total cholesterol at 6 months of age.
C) Reduce the infantŌĆÖs dietary fat to less than 30% of his calories by giving him skim milk.
D) Initiate lipid-lowering agents.
E) Recommend yearly ECGs for the patient.
94) For the past year, a 12-year-old boy has had recurrent episodes of swelling of his hands and feet, which has been getting worse recently. These episodes occur following exercise and emotional stress, last for 2 to 3 days, and resolve spontaneously. The last episode was accompanied by abdominal pain, vomiting, and diarrhea. The results of routine laboratory workup are normal. An older sister and a maternal uncle have had similar episodes, but they were not given a diagnosis. He presents today with another episode as shown in the photographs on the next page. Which of the following is the most likely diagnosis?
A) Systemic lupus erythematosus
B) Focal glomerulosclerosis
C) Congenital nephrotic syndrome
D) Hereditary angioedema
E) Henoch-Sch├Čnlein purpura
95) A newborn is diagnosed with congenital heart disease. You counsel the family that the incidence of heart disease in future children is which of the following?
A. 1%
B. 2% to 6%
C. 8% to 10%
D. 15% to 20%
E. 25% to 30%
96) During a regular checkup of an 8-year-old child, you note a loud first heart sound with a fixed and widely split second heart sound at the upper left sternalborder that does not change with respirations. The patient is otherwise active and healthy. Which of the following heart lesions most likely explains these findings?
A) Atrial septal defect (ASD)
B) Ventricular septal defect (VSD)
C) Isolated tricuspid regurgitation
D) Tetralogy of Fallot
E) Mitral valve prolapse

97) A 2-year-old boy is brought into the emergency room with a complaint of fever for 6 days and the development of a limp. On examination, he is found to have an erythematous macular exanthem over his body as shown in image A, ocular conjunctivitis, dry and cracked lips, a red throat, and cervical lymphadenopa- thy. There is a grade 2/6 vibratory systolic ejection murmur at the lower left sternal border. A white blood cell (WBC) count and differential show predominant neutrophils with increased platelets on smear. Later, he develops the findings as seen in image B. Which of the following is the most likely diagnosis?
A) Scarlet fever
B) Rheumatic fever
C) Kawasakidisease
D) Juvenile rheumatoid arthritis
E) Infectious mononucleosis
98) An ill-appearing 2-week-old baby girl is brought to the emergency room. She is pale and dyspneic with a respiratory rate of 80 breaths per minute. Heart rate is 195 beats per minute, heart sounds are distant, a gallop is heard, and she has cardiomegaly on x-ray. An echocardiogram demonstrates poor ventricular function, dilated ventricles, and dilation of the left atrium. An ECG shows ventricular depolarization complexes that have low voltage. Which of the following is the most likely diagnosis based on this clinical picture?
A) Myocarditis
B) Endocardial fibroelastosis
C) Pericarditis
D) Aberrant left coronary artery arising from pulmonary artery
E) Glycogen storage disease of the heart
99) A newborn infant has mild cyanosis, diaphoresis, poor peripheral pulses, hepatomegaly, and cardiomegaly. Respiratory rate is 60 breaths per minute, and heart rate is 250 beats per minute. The child most likely has congestive heart failure caused by which of the following?
A) Large ASD and valvular pulmonic stenosis
B) VSD and transposition of the great vessels
C) Total anomalous pulmonary venous return
D) Hypoplastic left heart syndrome
E) Paroxysmal atrial tachycardia
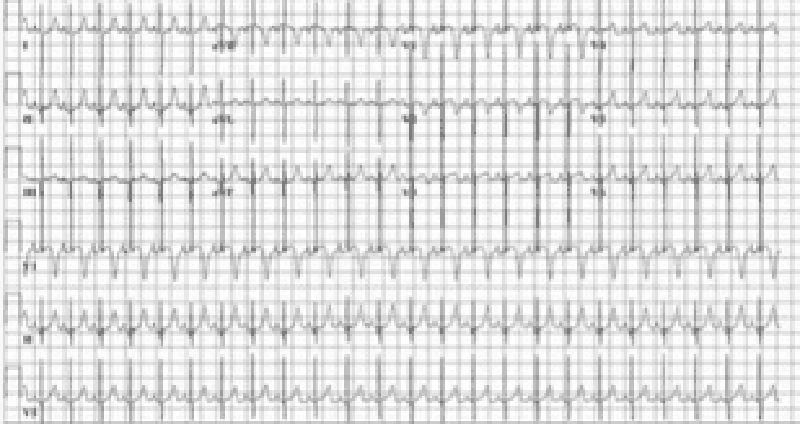
100) A 3-month-old infant is brought to your office for pallor and listless- ness. Your physical examination reveals tachycardia that is constant and does not vary with crying. He has no hepatomegaly and the lungs are clear. His ECG is shown. Which of the following is the most appropriate initial management of this patient?
A) Rapid verapamil infusion
B) Transthoracic pacing of the heart
C) Carotid massage
D) DC cardioversion
E) Precordial thump
101) A 2-year-old child with minimal cyanosis has an S3 and S4 (a quadruple rhythm), a systolic murmur in the pulmonic area, and a middiastolic murmur along the lower left sternal border. An ECG shows right atrial hypertrophy and a ventricular block pattern in the right chest leads. Which of the following is the most likely diagnosis?
A) Tricuspid regurgitation and pulmonic stenosis
B) Pulmonic stenosis and a VSD (tetralogy of Fallot)
C) Atrioventricular canal
D) Ebstein anomaly
E) Wolff-Parkinson-White syndrome
102) A 4-year-old girl is brought to the pediatrician’s office. Her father reports that she suddenly became pale and stopped running while he had been playfully chasing her and her pet Chihuahua. After 30 minutes, she was no longer pale and wanted to resume the game. She has never had a previous episode and has never been cyanotic. Her physical examination was normal, as were her chest x-ray and echocardiogram. An ECG showed the pattern seen on the next page, which indicates which of the following?
A) Paroxysmal ventricular tachycardia
B) Paroxysmal supraventricular tachycardia
C) Wolff-Parkinson-White syndrome
D) Stokes-Adams pattern
E) Excessive stress during play
103) A child has a 2-week history of spiking fevers, which have been as high as 40┬░C (104┬░F). She has spindle-shaped swelling of finger joints and complains of upper sternal pain. When she has fever, the parents note a faint salmon-colored rash that resolves with the resolution of the fever. She has had no conjunctivitis or mucositis, but her heart sounds are muffled and she has increased pulsus paradoxus. Which of the following is the most likely diagnosis?
A) Rheumatic fever
B) Juvenile rheumatoid arthritis
C) Toxic synovitis
D) Septic arthritis
E) Osteoarthritis
104) A cyanotic newborn is suspected of having congenital heart disease. He has an increased left ventricular impulse and a holosystolic murmur along the left sternal border. The ECG shows left-axis deviation and left ventricular hypertrophy (LVH). Which of the following is the most likely diagnosis?
A) Transposition of the great arteries
B) Truncus arteriosus
C) Tricuspid atresia
D) Tetralogy of Fallot
E) Persistent fetal circulation
105) A 3-day-old infant with a single second heart sound has had progressively deepening cyanosis since birth but no respiratory distress. Chest radiography demonstrates no cardiomegaly and normal pulmonary vasculature. An ECG shows an axis of 120┬░and right ventricular prominence. Which of the following congenital cardiac malformations is most likely responsible for the cyanosis?
A) Tetralogy of Fallot
B) Transposition of the great vessels
C) Tricuspid atresia
D) Pulmonary atresia with intact ventricular septum
E) Total anomalous pulmonary venous return below the diaphragm
106) During a physical examination for participation in a sport, a 16-year- old girl is noted to have a late apical systolic murmur, which is preceded by a click. The rest of the cardiac examination is normal. She states that her mother also has some type of heart ŌĆ£murmurŌĆØ but knows nothing else about it. Which of the following is the most likely diagnosis?
A) ASD
B) Aortic stenosis
C) Tricuspid regurgitation
D) Mitral valve prolapse
E) VSD
107) A previously normal newborn infant in a community hospital nursery is noted to be cyanotic at 14 hours of life. She is placed on a face mask with oxygen flowing at 10 L/min. She remains cyanotic, and her pulse oxymetry reading does not change. An arterial blood gas shows her PaO2 to be 23 mm Hg. Bilateral breath sounds are present, and she has no murmur. She is breathing deeply and quickly, but she is not retracting. While you are waiting for the transport team from the nearby childrenŌĆÖs hospital, you should initiate which of the following?
A) Indomethacin infusion
B) Saline infusion
C) Adenosine infusion
D) Prostaglandin E1 infusion
E) Digoxin infusion
108) You are asked to evaluate an infant born vaginally 3 hours previously to a mother whose only pregnancy complication was poorly controlled gestational diabetes. The nursing staff noticed that the infant was breathing abnormally. On examination, you find that the infant is cyanotic, has irregular, labored breathing, and has decreased breath sounds on the right side. You also note decreased tone in the right arm. You provide oxygen and order a stat portable chest radiograph, which is normal. Which of the following studies is most likely to confirm your diagnosis?
A) Nasalwash for viral culture
B) Fiberoptic bronchoscopy
C) Chest CT
D) Chest ultrasound
E) Induced sputum culture
109) A 10-month-old infant has poor weight gain, a persistent cough, and a history of severalbouts of pneumonitis. The mother describes the child as having very large, foul- smelling stools for months. Which of the following diagnostic maneuvers is likely to result in the correct diagnosis of this child?
A) CT of the chest
B) Serum immunoglobulins
C) TB skin test
D) Inspiratory and expiratory chest x-ray
E) Sweat chloride test
110) A previously well 1-year-old infant has had a runny nose and has been sneezing and coughing for 2 days. Two other members of the family had similar symptoms. Four hours ago, his cough became much worse. On physical examination, he is in moderate respiratory distress with nasal flaring, hyper- expansion of the chest, and easily audible wheezing without rales. His chest radiographs are shown. Which of the following is the appropriate next course of action?
A) Monitoring oxygenation and fluid status alone
B) Inhaled epinephrine and a single dose of steroids
C) Acute-acting bronchodilators and a short course of oral steroids
D) Emergent intubation and antibiotics
E) Chest tube placement
111) A 6-year-old girl presents with a 2-day history of cough and fever. At your office she has a temperature of 39.4°C (103°F), a respiratory rate of 45 breaths per minute, and decreased breath sounds on the left side. Her chest x-ray is shown below. Which of the following is the most appropriate initial treatment?
A) N-acetylcysteine chest physiotherapy
B) Vancomycin
C) Partial lobectomy
D) Postural drainage
E) Placement of tuberculosis skin test
112) A 2-year-old girl is playing in the garage with her Chihuahua, only partially supervised by her father, who is weed-whacking around the garden gnomes in the front yard. He finds her in the garage, gagging and vomiting. She smells of gasoline. In a few minutes she stops vomiting, but later that day she develops cough, tachypnea, and subcostal retractions. She is brought to your emergency center. Which of the following is the most appropriate first step in management?
A) Administer charcoal
B) Begin nasogastric lavage
C) Administer ipecac
D) Perform pulse oximetry and arterial blood gas
E) Administer gasoline-binding agent intravenously

113) A 3-year-old girl is admitted with the x-ray shown below. The child lives with her parents and a 6-week-old brother. Her grandfather stayed with the family for 2 months before his return to the West Indies 1 month ago. The grandfather had a 3-month history of weight loss, fever, and hemoptysis. Appropriate management of this problem includes which of the following?
A) Bronchoscopy and culture of washings for all family members
B) Placement of a Mantoux test on the 6-week-old sibling
C) Isolating the 3-year-old patient for 1 month
D) Treating the 3-year-old patient with isoniazid (INH) and rifampin
E) HIV testing for all family members
114) You are asked to evaluate a 4-year-old boy admitted to your local childrenŌĆÖs hospital with a diagnosis of pneumonia. The parents state that the child has had multiple, intermittent episodes of fever and respiratory difficulty over the past 2 years, including cyanosis, wheezing, and dyspnea; each episode lasts for about 3 days. During each event he has a small amount of hemoptysis, is diagnosed with left lower lobe pneumonia, and improves upon treatment. Repeat radiographs done several days after each event are reportedly normal. His examination on the current admission is significant for findings similar to those described above, as well as digital clubbing. Which of the following is the most appropriate primary recommendation?
A) Intravenous cephalosporin and oral macrolide therapy
B) Modified barium swallow study to evaluate for aspiration
C) Nasalswab for viral culture
D) Incentive spirometry
E) Bronchoalveolar lavage
115) A previously healthy, active, 18-month-old African American child presents with unilateral nasal obstruction and foul-smelling discharge. The childŌĆÖs examination is otherwise unremarkable. Which of the following is the most likely diagnosis?
A) Foreign body
B) Nasalpolyps
C) Frontal sinusitis
D) Deviated septum
E) Choanal atresia
116) A 7-year-old child is brought by his mother for a school physical. His growth parameters show his height to be 50th percentile and his weight to be significantly higher than 95th percentile. His mother complains that he always seems sleepy during the day and that he has started complaining of headaches. His second-grade teacher has commented that he has difficulty staying awake in class. His mother complains that he wakes up the whole house with his snoring at night. Which of the following is the most appropriate next step in evaluating and managing this condition?
A) Try steroids to decrease tonsillar and adenoid hypertrophy.
B) Refer to an otolaryngologist for tonsillectomy and adenoidectomy.
C) Arrange for continuous positive airway pressure (CPAP) at home.
D) Arrange for home oxygen therapy for use at night.
E) Arrange for polysomnography.
117) You admitted to the hospital the previous evening a 1-year-old boy who presented with cough, fever, and mild hypoxia. At the time of his admission, he had evidence of a right upper lobe consolidation on his chest radiograph. A blood culture has become positive in less than 24 hours for Staphylococcus aureus. Approximately 20 hours into his hospitalization, the nurse calls you because the child has acutely worsened over the previous few minutes, with markedly increased work in breathing, increasing oxy- gen requirement, and hypotension. As you move swiftly to the childŌĆÖs hospital room, you tell the nurse to order which of the following?
A) A second chest radiograph to evaluate for pneumatocele formation
B) A large-bore needle and chest tube kit for aspiration of a probable tension pneumothorax
C) A change in antibiotics to include gentamicin
D) A sedative to treat the childŌĆÖs attack of severe anxiety
E) A thoracentesis kit to drain his probable pleural effusion
118) A fully immunized 2-year-old presents to the emergency room with severaldays of low-grade fever, barking cough, and noisy breathing. Over the past few hours he has developed a fever of 40┬░C (104┬░F) and looks toxic. He has inspiratory and expiratory stridor. The family has not noticed drooling, and he seems to be drinking without pain. Direct laryngoscopy reveals a normal epiglottis. The management of this disease process includes which of the following?
A) Intubation and intravenous antibiotics
B) Inhaled epinephrine and oral steroids
C) Inhaled steroids
D) Observation in a cool mist tent
E) Oral antibiotics and outpatient follow-up
119) A 6-year-old, fully immunized boy is brought to the emergency room with a 3-hour history of fever to 39.5°C (103.1°F) and sore throat. The child appears alert, but anxious and toxic. He has mild inspiratory stridor and is drooling. He is sitting on the examination table leaning forward with his neck extended. A lateral radiograph of his neck is shown below. Which of the following is the most appropriate immediate management of this patient?
A) Examine the throat and obtain a culture.
B) Obtain an arterial blood gas and start an IV line.
C) Administer a dose of nebulized epinephrine.
D) Prepare to establish an airway in the operating room.
E) Admit the child and place him in a mist tent.
120) A 4-year-old boy was admitted to the hospital last night with the complaint of ŌĆ£difficulty breathing.ŌĆØ He has no past history of lung infection, no recent travel, and no day- care exposure; he does, however, have an annoying tendency to eat dirt. In the emergency center he was noted to be wheezing and to have hepatomegaly. He is able to talk, relaying his concern about his 6-week-old Chihuahua being left alone at home. Laboratory studies revealed marked eosinophilia (60% eosinophils). Which of the following tests is most likely to produce a specific diagnosis?
A) Tuberculin skin test
B) Histoplasmin test
C) ELISA for Toxocara
D) Silver stain of gastric aspirate
E) Stool examination for ova and parasites
121) A 10-year-old girl has had a ŌĆ£coldŌĆØ for 14 days. In the 2 days prior to the visit to your office, she has developed a fever of 39┬░C (102.2┬░F), purulent nasaldischarge, facial pain, and a daytime cough. Examination of the nose after topical decongestants shows pus in the middle meatus. Which of the following is the most likely diagnosis?
A) Brain abscess
B) Maxillary sinusitis
C) Streptococcal throat infection
D) Sphenoid sinusitis
E) Middle-ear infection
122) You are awakened in the night by your 2-year-old son, who has developed noisy breathing on inspiration, marked retractions of the chest wall, flaring of the nostrils, and a barking cough. He has had a mild upper respiratory infection (URI) for 2 days. Which of the following therapies is indicated?
A) Short-acting bronchodilators and a 5-day course of steroids
B) Intubation and antibiotics
C) Observation for hypoxia and dehydration alone
D) Inhaled epinephrine and a dose of steroids
E) Rigid bronchoscopy
123) An 8-year-old girl presents with well-controlled, moderately persistent asthma. Her therapies consist of occasional use of short-acting ╬▓-agonists, daily inhaled steroids, and a leukotriene inhibitor. She presents with white patches on her buccal mucosa. You recommend which of the following?
A) HIV testing
B) Tuberculosis skin testing
C) Measurement of serum immunoglobulins
D) Discontinuation of all her asthma medications
E) Rinse her mouth after use of her inhaled medications

124) A 13-year-old develops fever, malaise, sore throat, and a dry, hacking cough over severaldays. He does not appear to be particularly sick, but his chest examination is significant for diffuse rales and rhonchi. The chest radio- graph is shown below. Which of the following is the most likely pathogen?
A) Staphylococcus aureus
B) Mycobacterium tuberculosis
C) Haemophilus influenzae
D) Streptococcus pneumoniae
E) Mycoplasma pneumoniae
125) You have just given a 10-year-old boy an injection of pollen extract as prescribed by his allergist. You are about to move on to the next patient when the boy starts to complain about nausea and a funny feeling in his chest. You note that his face is flushed and his voice sounds muffled and strained. Which of the following is the first priority in managing this episode of anaphylaxis?
A) Preparation for endotracheal intubation
B) Intramuscular injection of diphenhydramine
C) Administration of oxygen
D) Subcutaneous injection of 1:1000 epinephrine
E) Administration of corticosteroids
126) A previously healthy 18-month-old has been in a separate room from his family. The family notices the sudden onset of coughing, which resolves in a few minutes. Subsequently, the patient appears to be normal except for increased amounts of drooling and refusal to take foods orally. Which of the following is the most likely explanation for this toddlerŌĆÖs condition?
A) Severe gastroesophagealreflux
B) Foreign body in the airway
C) Croup
D) Epiglottitis
E) Foreign body in the esophagus
127) You receive a telephone call from the mother of a 4-year-old child with sickle-cell anemia. She tells you that the child is breathing fast, coughing, and has a temperature of 40┬░C (104┬░F). Which of the following is the most conservative, prudent course of action?
A) Prescribe aspirin and ask her to call back if the fever does not respond.
B) Make an office appointment for the next available opening
C) Make an office appointment for the next day.
D) Refer the child to the laboratory for an immediate hematocrit, white blood cell count, and differential.
E) Admit the child to the hospital.
128) You are asked by a colleague to evaluate a 5-year-old boy as a second opinion. He has a history of chronic and recurrent upper respiratory tract infections, severaladmissions to the hospital for pneumonia, and three surgeries for PE tubes for chronic otitis media. Of note is a right-sided heart on repeated radiographs. Convinced you know the diagnosis based on history alone, you confirm your diagnosis with a biopsy of the nasal mucosa. You expect to find which of the following?
A) Eosinophilic infiltrate
B) Bordetella pertussis
C) Absence of nasal mucous glands
D) Random orientation of cilia
E) Nasalpolyps
129) A 13-year-old patient with sickle-cell anemia presents with respiratory distress; she has an infiltrate on chest radiograph. The laboratory workup of the patient reveals the following: hemoglobin 5 g/dL; hematocrit 16%; white blood cell count 30,000/╬╝L; and arterial blood (room air) pH 7.1, PO2 35 mm Hg, and PaCO2 28 mm Hg. These values indicate which of the following?
A) Acidemia, metabolic acidosis, respiratory alkalosis, and hypoxia
B) Alkalemia, respiratory acidosis, metabolic alkalosis, and hypoxia
C) Acidosis with compensatory hypoventilation
D) Long-term metabolic compensation for respiratory alkalosis
E) Primary respiratory alkalosis
130) A 24-year-old woman arrives in the emergency center in active labor. She is at term, but received no prenatal care after 16 weeks of gestation when she lost her insurance coverage. The mother has an uncomplicated vaginal delivery. You are paged shortly after birth when the baby is noted to have respiratory distress. The infant has diminished breath sounds on the left, and the PMI is shifted toward the right. A chest radiograph is shown. The NG tube you placed earlier reveals the stomach to be below the diaphragm. Which of the following is the most likely diagnosis at this point?
A) Congenital cystic adenomatoid malformation
B) Congenital diaphragmatic hernia
C) Bronchogenic cysts
D) Congenital lobar emphysema
E) Congenital pneumonia

131) A 13-year-old boy has a 3-day history of low-grade fever, symptoms of upper respiratory infection, and a sore throat. A few hours before his presentation to the emergency room, he has an abrupt onset of high fever, difficulty swallowing, and poor handling of his secretions. He indicates that he has a marked worsening in the severity of his sore throat. His pharynx has a fluctuant bulge in the posterior wall. A soft tissue radiograph of his neck is shown. Which of the following is the most appropriate initial therapy for this patient?
A) Narcotic analgesics
B) Trial of oral penicillin V
C) Surgical consultation for incision and drainage under general anesthesia
D) Rapid streptococcalscreen
E) Monospot test
132) A 6-week-old child arrives with a complaint of ŌĆ£breathing fastŌĆØ and a cough. On examination you note the child to have no temperature elevation, a respiratory rate of 65 breaths per minute, and her oxygen saturation to be 94%. Physical examination also is significant for rales and rhonchi. The past medical history for the child is positive for an eye discharge at 3 weeks of age, which was treated with a topical antibiotic drug. Which of the following organisms is the most likely cause of this childŌĆÖs condition?
A) Neisseria gonorrhoeae
B) Staphylococcus aureus
C) Group B streptococcus
D) Chlamydia trachomatis
E) Herpesvirus
133) One of your asthmatic patients arrives for a checkup. The mother reports that the child seems to need albuterol daily, especially when exercising, and she has coughing fits that awaken her from sleep about twice a week. Her grandmother had recommended a Chihuahua as a ŌĆ£cureŌĆØ for her asthma, but her mother has seen no difference since the arrival of the pet. Appropriate treatment measures would include which of the following?
A) Short-acting, inhaled╬▓-agonists, as needed
B) Daily leukotriene modifier with short-acting ╬▓-agonist
C) Inhaled nedocromil with short-acting╬▓-agonists
D) Medium-dose, inhaled corticosteroids with short-acting ╬▓-agonists
E) High-dose, inhaled corticosteroids with theophylline and short-acting╬▓-agonists
134) A previously healthy 2-year-old black child has developed a chronic cough during the previous 6 weeks. He has been seen in different emergency rooms on two occasions during this period and has been placed on antibiotics for pneumonia. Upon auscultation, you hear normal breath sounds on the left. On the right side, you hear decreased air movement during inspiration but none upon expiration. Inspiratory (A) and expiratory (B) radiographs of the chest are shown below. Which of the following is the most appropriate next step in making the diagnosis in this patient?
A) Measure the patientŌĆÖs sweat chloride.
B) Consult pediatric surgery for bronchoscopy.
C) Prescribe broad-spectrum oral antibiotics.
D) Initiate a trial of inhaled ╬▓-agonists.
E) Prescribe appropriate doses of oral prednisone.

135) A 4-year-old boy presents with a history of constipation since the age of 6 months. His stools, produced every 3 to 4 days, are described as large and hard. Physical examination is normal; rectalexamination reveals a large ampulla, poor sphincter tone but present anal wink, and stool in the rectal vault. The plain film of his abdomen is shown. Which of the following is the most appropriate next step in the management of this child?
A) Lower gastrointestinal (GI) barium study
B) Parental reassurance and dietary counseling
C) Serum electrolyte measurement
D) Upper GI barium study
E) Initiation of thyroid-replacement hormone
136) A 10-year-old boy has been having ŌĆ£bellyachesŌĆØ for about 2 years. They occur at night as well as during the day. Occasionally, he vomits after the onset of pain. Occult blood has been found in his stool. His father also gets frequent, nonspecific stomachaches. Which of the following is the most likely diagnosis?
A) Peptic ulcer
B) Appendicitis
C) Meckel diverticulum
D) Functional abdominal pain
E) Pinworm infestation
137) An 8-year-old boy presents to your office for a second opinion. He has a 2-year history of intermittent vomiting, dysphagia, and epigastric pain. His father reports he occasionally gets food ŌĆ£stuckŌĆØ in his throat. He has been on a proton pump inhibitor for 18 months without symptom relief. His past history is significant only for eczema and a peanut allergy. Endoscopy was performed 6 months ago; no erosive lesions were noted and a biopsy was not performed. You arrange for a repeat endoscopy with biopsy. Microscopy on the biopsy sample reveals many eosinophils. Treatment of this condition should include which of the following?
A) Corticosteroids
B) Prolonged acid blockade
C) Treatment for Candida sp.
D) Treatmentfor Aspergillus sp.
E) Observation
138) A 1-week-old previously healthy infant presents to the emergency room with the acute onset of bilious vomiting. The abdominal plain film in the emergency department (A) and the barium enema done after admission (B) are shown. Which of the following is the most likely diagnosis for this patient?
A) Jejunal atresia
B) Hypertrophic pyloric stenosis
C) Malrotation with volvulus
D) Acute appendicitis
E) Intussusception
139) The newborn nursery calls to notify you that a 1-day-old baby boy has developed abdominal distension and bilious emesis. Prenatalhistory was significant for areas of echogenic bowel seen on ultrasound. You order an abdominal radiograph; based on the results you order a contrast enema. Both are shown here. This infant is most likely to have which of the following?
A) Duodenal atresia
B) Cystic fibrosis
C) Gastroenteritis
D) Malrotation with volvulus
E) Hirschsprung disease
140) A 17-year-old adolescent female is 6 weeks postpartum. She presents to the emergency room with the complaints of increased jaundice, abdominal pain, nausea, vomiting, and fever. Her examination is remarkable for jaundice, pain of the right upper quadrant with guarding, and a clear chest. Chest radiographs appear normal. Which of the following tests is most likely to reveal the cause of this pain?
A) Serum chemistries
B) Complete blood count (CBC) with platelets and differential
C) Ultrasound of the right upper quadrant
D) Upper GI series
E) Hepatitis panel
141) An 8-year-old is accidentally hit in the abdomen by a baseball bat. After several minutes of discomfort, he seems to be fine. Over the ensuing 24 hours, however, he develops a fever, abdominal pain radiating to the back, and persistent vomiting. On examination, the child appears quite uncomfortable. The abdomen is tender, with decreased bowelsounds throughout, but especially painful in the midepigastric region with guarding. Which of the following tests is most likely to confirm the diagnosis?
A) Serum amylase levels
B) CBC with differential and platelets
C) Serum total and direct bilirubin levels
D) Abdominal radiograph
E) Electrolyte panel
142) A 10-month-old baby boy, recently adopted from Guyana, has a 5-hour history of crying, with intermittent drawing up of his knees to his chest. On the way to the emergency room he passes a loose, bloody stool. He has had no vomiting and has refused his bottle since the crying began. Physical examination is noteworthy for an irritable infant whose abdomen is very difficult to examine because of constant crying. His temperature is 38.8’é░C (101.8’é░F). The rectalampulla is empty, but there is some gross blood on the examining finger. Which of the following studies would be most helpful in the immediate management of this patient?
A) Stool culture
B) Examination of the stool for ova and parasites
C) Air contrast enema
D) Examination of the blood smear
E) Coagulation studies
143) A 12-month-old girl has been spitting up her meals since 1 month of age. Her growth is at the 95th percentile, and she is otherwise asymptomatic and without findings on physical examination. Which of the following is the most likely diagnosis?
A) Pyloric stenosis
B) Partial duodenal atresia
C) Hypothyroidism
D) Gastroesophageal reflux
E) Tracheoesophageal fistula
144) A 14-year-old girl has a 9-month history of diarrhea, abdominal pain (usually periumbilical and postprandial), fever, and weight loss. She has had several episodes of blood in her stools. Which of the following is the most likely diagnosis?
A) Chronic appendicitis
B) Chronic pancreatitis
C) Crohn disease
D) Bulimia
E) Gallstones
145) A 4-year-old boy, recently adopted through an international adoption service, is noted to have intermittent watery diarrhea, nausea, belching, and abdominal pain. His weight is less than the fifth percentile for his age. Which of the following studies would be most helpful in making the diagnosis?
A) CBC and differential
B) ESR
C) Abdominal ultrasound
D) Liver function studies
E) Stool microscopy for ova and parasites
146) A 5-month-old child regularly regurgitates a large portion of her feeds. A pH probe study showed significant periods of low esophageal pH. The child has normal growth and no other significant past medical history. Which of the following is the best management at this point?
A) Barium swallow and upper GI series
B) Oralreflux medications
C) Esophageal manometry
D) Close observation only
E) Surgical correction with fundoplication
147) A 2-year-old presents to the emergency center with severaldays of rectal bleeding. The mother first noticed reddish-colored stools 2 days prior to arrival and has since changed severaldiapers with just blood. The child is afebrile, alert, and playful, and is eating well without emesis. He is slightly tachycardic, and his abdominal examination is normal. Which of the following is the best diagnostic study to order to confirm the diagnosis?
A) Exploratory laparotomy
B) Barium enema
C) Ultrasound of the abdomen
D) Radionucleotide scan
E) Stool culture
148) A 15-year-old otherwise healthy boy presents with a complaint of intermittent abdominal distention, crampy abdominal pain, and excessive flatulence. He first started noticing these symptoms when he moved into his fatherŌĆÖs house, and his stepmother insisted on milk at dinner every night. He has normal growth, has not lost weight, and has no travel history. Which of the following is the most appropriate study to diagnose his condition?
A) Barium swallow and upper GI
B) Hydrogen excretion in breath after oral administration of lactose
C) Esophageal manometry
D) Stool pH after one to 2 weeks of a lactose-free diet
E) Fasting serum lactose levels
149) A 6-week-old infant is admitted to the hospital with jaundice. Her outpatient blood work demonstrated a total bilirubin of 12 mg/dL with a direct portion of 3.5 mg/dL. Which of the following disorders is most likely to be responsible?
A) ABO incompatibility
B) Choledochal cyst
C) Rh incompatibility
D) Gilbert disease
E) Crigler-Najjar syndrome
150) A 2-year-old arrives in the emergency center after having swallowed a button battery from one of her toys. She is breathing comfortably, without stridor. Radiographs show the battery to be lodged in the esophagus. Which of the following is the correct next step?
A) Induce emesis with syrup of ipecac
B) Admit for observation, and obtain serial radiographs to document movement of the battery.
C) Discharge home with instructions to monitor the stool for the battery.
D) Immediate removal of the battery via endoscopy.
E) Encourage oral intake to assist in passage of the battery.
{"name":"Pediactic. kb 1", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge on pediatric health concepts with this comprehensive quiz designed for healthcare professionals and students alike.Whether youŌĆÖre preparing for an examination or simply want to refresh your understanding, this quiz features:150 thought-provoking questionsRelevant multiple-choice optionsA variety of pediatric topics","img":"https:/images/course1.png"}
More Quizzes
(NEW)Part8 (1785-1823)..... (1785-2039)1 brettpit
111560
Paediatric HO quiz no.2
10513
Cultura general
1586
├āåŃé╣ŃāłŃé»ŃéżŃé║
100
Test Your Flash Player Skills: Adobe Flash Player
201023929
Ultimate TMNT Trivia: Test Your Ninja Turtle Knowledge
201029542
Free Simple Chemical Reactions Unit Test
201023544
HRIP Certification Exam: Test Your Knowledge Now
201071947
What Musical Instrument Are You? Discover Your Perfect Match
201031701
Free At-Home STAR, AR & ADAP Practice Test
201021830
Free TSI Reading Answer Key
201021830
What Diet Should I Do? Discover Your Perfect Plan
201027153