Cardiovascular 2
A 54-year-old woman presents for a routine physical. She has no complaints. She has no history of hypertension, diabetes, hypercholesterolemia, or heart disease, and she does not use tobacco, alcohol or drugs. On physical examination, her pulse is irregular. There are no murmurs. Her lungs are clear to auscultation and her legs are free of edema. An EKG shows atrial fibrillation with a heart rate of 72 beats per minute. An echocardiogram is unremarkable except for evidence of atrial fibrillation. What is the most appropriate management of this patient?
Warfarin and clopidogrel
Heparin followed by warfarin
Low-molecular weight heparin
Aspirin alone
Warfarin to maintain an INR of 2 to 3
A middle-aged man was recently diagnosed with hypertension. The antihypertensive medication prescribed to him enhances natriuresis, decreases serum angiotensin II concentration, and decreases aldosterone production. This medication most likely belongs to which of the following drug classes?
Angiotensin receptor blocker
Direct renin inhibitor
Aldosterone receptor antagonist
Loop diuretic
Alpha-adrenergic blocker
A 63-year-old woman complains of leg swelling that is especially bothersome in the evening. She also complains of chronic cough and exertional dyspnea. She has been smoking one pack of cigarettes per day for the past 30 years. She also drinks one or two cans of beer on weekends. Her medical history is significant for a hospitalization for a "chest infection" two years ago, for which she was treated with antibiotics, steroids, and inhalers. She also reports having been diagnosed with hypertension, but says that she has never taken medications for it. On physical examination, her blood pressure is 160/90 mmHg and her heart rate is 80/min. Chest examination reveals bilateral scattered wheezes and prolonged expirations. Her jugular venous pulsation is seen 2 cm above the sternal angle with the head of the bed elevated 30•. Her abdomen is soft and non-distended. On examination of her lower extremities, you note bilateral pitting edema and dilated, tortuous, superficial veins. Which of the following is most likely to relieve this patient's edema?
Smoking cessation
Frequent leg elevation
Dietary sodium restriction
Control of hypertension
Oxygen therapy
A 32-year-old man develops severe nausea and vomiting after returning from a party. He also complains of chest pain that is more intense than any pain he has previously experienced. His past medical history is significant for HIV infection, alcohol abuse, and alcoholic hepatitis. He admits to using cocaine regularly. His temperature is 37.8C (100.F), pulse is 120/min, respirations are 24/min, and blood pressure is 100/60 mmHg. Examination reveals injected conjunctivae and bilateral dilated pupils. Chest X-ray demonstrates a widened mediastinum and left-sided pleural effusion. EKG is unremarkable. The pleural fluid is found to have an elevated amylase content. Which of the following is the most likely diagnosis in this patient?
Acute pancreatitis
Peptic ulcer disease
Esophageal perforation
Myocardial ischemia
Pulmonary embolism
A 45-year-old male is brought to the ER with sudden onset palpitations and chest tightness. His past medical history is significant for hypertension, gout and diabetes mellitus. Cardiac monitoring shows atrial fibrillation at a rate of 120-140/min. As the nurse is attempting to establish IV access, the patient becomes unresponsive. There is no palpable pulse over the carotids or femoral arteries. The cardiac monitor still shows atrial fibrillation at the same rate. What is the best next step in management?
Synchronized cardioversion
Defibrillation
IV lidocaine
Chest compressions
Arterial blood gas analysis
A 24-year-old male experiences syncope while shoveling snow. He regained consciousness within one minute. He has been having some shortness of breath and chest pains recently, mostly related to exercise. He denies any illicit drug use. His temperature is 37.2 C (98.9 F), and blood pressure is 126/76 mm Hg, pulse is 76/min and respirations are 14/min. Physical examination shows a well-built male in no apparent distress. Lungs are clear. A crescendo-decrescendo systolic murmur is heard along the left sternal border without carotid radiation. Chest X-ray is normal. Which of the following is the most likely cause of his syncopal episode?
Atrioventricular conduction delay
Left ventricular hypertrophy
Aortic dissection
Coronary atherosclerosis
Mitral valve degeneration
A 56-year-old diabetic female comes to the clinic with complaints of dizziness which has been going on for 3 weeks. She denies any dyspnea or diaphoresis. She says her blood glucose is well controlled and denies any allergy. Her BP is 155/90 mm Hg. Her chest-x ray is unremarkable and her blood work is normal. The ECG is recorded below. What is the most likely diagnosis?
Mobitz type I heart block
Mobitz type II heart block
Complete heart block
Atrial fibrillation
First degree heart block
A 54-year-old overweight man wakes up in the middle of the night with substernal discomfort that he describes as a burning sensation. He also complains of left-sided neck pain and feels sweaty and short of breath. He has never had similar pain before. Prior to going to bed he had eaten a big meal. His past medical history is significant for diabetes and hypertension. Which of the following physical findings is most consistent with this patient's clinical presentation?
Fixed splitting of S2
Ejection-type systolic murmur
Friction rub
Fourth heart sound
Pulsus paradoxus
A 56-year-old male is hospitalized following an acute anterior wall myocardial infarction that was treated with thrombolytic therapy 4 days ago. On day 4 of his hospitalization, he develops recurrent chest pain, similar in quality and severity to his previous pain. Sublingual nitroglycerin is administered but does not help. His blood pressure is now 140/90 mmHg and his heart rate is 82/min. S 1 and S2 are normal, and there are no cardiac murmurs or rubs. Lungs are clear to auscultation. Which of the following laboratory tests would be most useful to send in this setting?
Troponin T
Lactate dehydrogenase (LDH)
CK-MB
Alkaline phosphatase
Dobutamin
A 64-year-old male presents to the emergency department with chest pain. An ECG reveals ST elevations in leads II, Ill, and aVF. Thrombolytic therapy and heparin are administered, and the pain resolves. Eight hours after admission, the patient develops hypotension. He denies recurrence of chest pain. His temperature is 37.5°c (99.6.F), blood pressure is 84/55 mm Hg, pulse is 90/min, and respirations are 15/min. His medications include a nitroglycerin drip, beta-blocker, aspirin, heparin, and simvastatin. Examination reveals an elevated jugular venous pressure of 14 cm, cold clammy extremities, and clear lung fields. Based on this information, what is the next best step in this patient's management?
Start dopamine
Administer normal saline bolus and stop nitroglycerin
Administer intravenous furosemide
Initiate temporary cardiac pacing
Stop nitroglycerin and start dobutamine drip
A 33-year-old woman is undergoing an elective, open cholecystectomy after 2 episodes of acute calculous cholecystitis. She suddenly becomes hypotensive, and a generalized rash is noted. Her past medical history is significant for a hypotensive episode 8 weeks ago while having protected sex with her new partner. Which of the following is the most probable cause of this patient's condition?
Acute blood loss
Coagulation abnormality
Allergic reaction
Septic shock
Pulmonary embolism
A 68-year-old man presents to the emergency department complaining of left lower extremity pain. He says that he first noticed a tingling sensation in his leg 3 hours ago, and since that time it has become increasingly painful. Over the past hour, he says, the skin on his leg has started to change color. His medical history is significant for hypertension, diabetes mellitus, atrial fibrillation, and major depressive disorder. He cannot remember his medication list at this time. On physical examination, his blood pressure is 127/74 mm Hg and his heart rate is 102/min. His left lower extremity is cool and pale below the level of the knee. Neither the posterior tibial nor the dorsalis pedis pulse is palpable. Which medication could have prevented this acute problem?
Aspirin
Metoprolol
Clopidogrel
Warfarin
Diltiazem
A 75-year-old patient presents to the ER after a syncopal episode. He is again alert and in retrospect describes occasional substernal chest pressure and shortness of breath on exertion. His blood pressure is 110/80 and lungs have a few bibasilar rales. Which auscultatory finding would best explain his findings?
A harsh systolic crescendo-decrescendo murmur heard best at the upper right sternal border
A diastolic decrescendo murmur heard at the mid-left sternal border
A holosystolic murmur heard best at the apex
A midsystolic click
A pericardial rub
A 72-year-old male comes to the office with intermittent symptoms of dyspnea on exertion, palpitations, and cough occasionally productive of blood. On cardiac auscultation, a low-pitched diastolic rumbling murmur is faintly heard at the apex. What is the most likely cause of the murmur?
Rheumatic fever as a youth
Long-standing hypertension
A silent MI within the past year
A congenital anomaly
Anemia from chronic blood loss
You are helping with school sports physicals and see a 16-year-old boy who has had trouble keeping up with his peers. Which of the following auscultatory findings suggests a previously undiagnosed ventricular septal defect?
A systolic crescendo-decrescendo murmur heard best at the upper right sternal border with radiation to the carotids; the murmur is augmented with exercise
A systolic murmur at the pulmonic area and a diastolic rumble along the left sternal border. c. A holosystolic murmur at the mid-left sternal border
Systolic crescendo-decrescendo murmur heard best at the upper right sternal border with radiation to the carotids; the murmur is augmented with exercise.
A diastolic decrescendo murmur at the mid-left sternal border
A continuous murmur through systole and diastole at the upper left sternal border
Describes the pain as constant and states that it is exacerbated by knee flexion. He has a history of past IV drug abuse, endocarditis, and stroke. He is currently wheelchair-bound secondary to stroke-related left-sided hemiparesis. On physical examination, his blood pressure is 140/90 mmHg and his heart rate is 100/min. There is no jugular venous distention or hepatojugular reflux. His chest is clear to auscultation but his abdomen is enlarged with shifting dullness and a fluid wave, suggestive of ascites. His liver is palpable 3 cm below the right costal margin. His spleen is also palpable. On examination of his lower extremities, you note right-sided calf swelling and tenderness. Which of the following is the most likely cause of this patient's ascites?
Right-sided heart failure
Pulmonary embolism
Protein C deficiency
Chronic liver disease
Paradoxical embolism
46-year-old man comes to the ER because of weakness and chest tightness. He has had these symptoms for the past one hour. He denies any past medical history. He does not smoke or drink alcohol. His father had a myocardial infarction at 68 years of age and his mother has myasthenia gravis. His EKG is shown on the slide below.The patient should be evaluated for which of the following?
Cushing syndrome
Hyperthyroidism
Aortic dissection
High-frequency deafness
High-range proteinuria
A 64-year-old male presents to the ER with chest pain. His history is significant for a hospitalization 2 weeks ago for an acute myocardial infarction. The patient reports that he is afraid his heart attack is recurring. He localizes the pain to the middle of the chest, and says that he can only take shallow breaths because deep breaths make the pain worse. Leaning forward in his chair makes the pain somewhat better. He notes some associated neck pain and general malaise, but denies shortness of breath, palpitations, syncope or cough. His temperature is 36.7C (98.F), blood pressure is 135/84 mmHg and heart rate is 90/min. EKG shows ST segment elevations in all limb and precordial leads except in aVR, where ST depression is seen. Which of the following is the best next step in the management of this patient?
Anticoagulation with heparin
Anticoagulation with warfarin
Nitroglycerin and beta-blockers
Broad-spectrum antibiotics
Non-steroidal antiinflammatory agent
A 15-year-old female, who has recently emigrated from Asia, is found to have a heart murmur during her routine physical examination. She has no current complaints. She had a febrile illness with joint swelling and pain approximately one year ago. She plays table tennis and swims every weekend. Her blood pressure is 120/70 mmHg and her heart rate is 70/min, regular. Cardiac auscultation shows a loud first heart sound and mid-diastolic rumble at the apex. Her lungs are clear to auscultation. Which of the following is the best treatment for this patient at this point?
Penicillin
Metoprolol
Enalapril
Digoxin
Digoxin
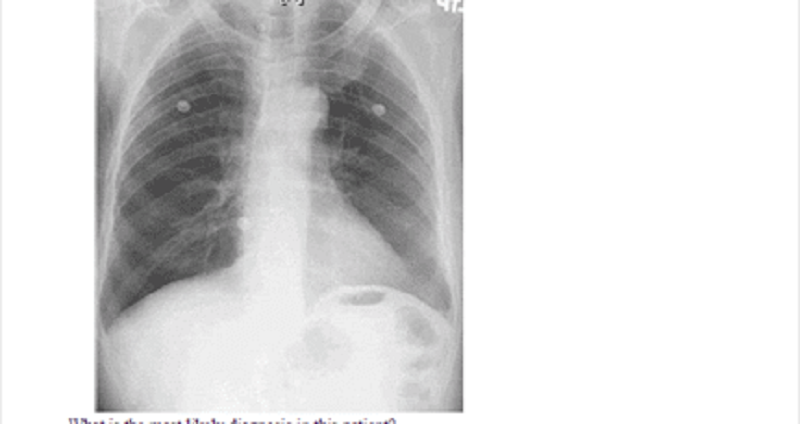
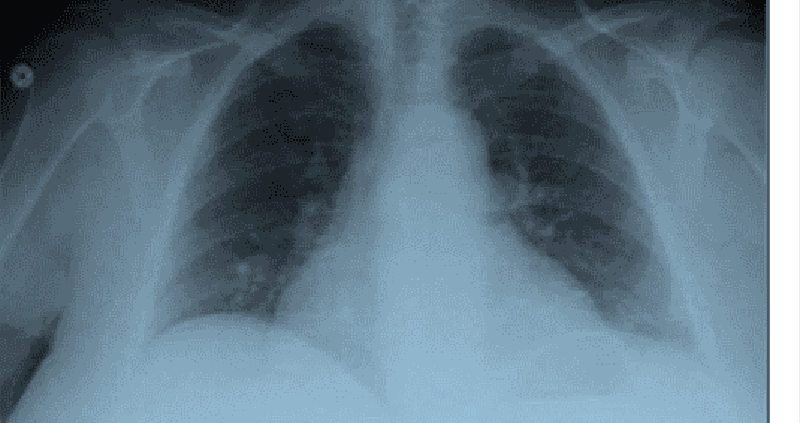
A 46-year-old man presents to the emergency department with difficulty breathing and chest discomfort. His pain worsens with inspiration but does not radiate. He says that he has never had symptoms like this before. His past medical history is unremarkable. He works as a long-haul truck driver. On physical examination, his blood pressure is 110/70 mmHg, his heart rate is 110/min, his respiratory rate is 31/min, and his temperature is 36.7C (98.F). ECG reveals sinus tachycardia but no ischemic ST-segment or T-wave changes. His chest X-ray is shown below. What is the most likely diagnosis in this patient?
Ascending aortic dissection
Myocardial infarction
Pneumothorax
Pulmonary embolism
Pulmonary embolism
Began ten minutes ago. He has never had such pain before. His past medical history is significant for diabetes mellitus, type 2, controlled with diet His blood pressure is 150/95 mmHg and HR is 80/min. You give him one chewable tablet of aspirin and two sublingual tablets of nitroglycerin with a 5-minute interval. After the second tablet of nitroglycerin, the pain is greatly relieved. What is the most important mechanism responsible for pain relief in this patient?
Increase in coronary blood flow
Increased cardiac contractility
Dilation of resistance vessels
Dilation of capacitance vessels
Change in the activity of baroreceptors
A 34-year-old male who recently immigrated from Brazil presents with a 5-month history of exertional dyspnea without associated chest pain, palpitations, dizziness, or syncope. His past medical history is significant for an episode of megacolon, which was treated 2 years ago. On physical examination, there is 1+ pedal edema and mild jugular venous distention. Cardiac exam is significant for the presence of an S3, but no murmurs are heard. Chest x-ray reveals prominent cardiomegaly. Based on these findings, which of the following is most likely causing his symptoms?
Diphtheric myocarditis
Coronary artery disease
Protozoal disease
Giant cell myocarditis
Rickettsial myocarditis
A 54-year-old male with a past medical history of type 2 diabetes mellitus comes to the emergency department complaining of shortness of breath. His blood pressure is 146/92 mmHg, respiratory rate is 26/min, and oxygen saturation is 87% on room air. Cardiac auscultation findings over the apex are given below. Based on the physical findings, which of the following is the best initial therapy for this patient?
Inhaled bronchodilators
Intravenous beta-blockers
Intravenous diltiazem
Intravenous diuretics
Pericardiocentesis
Neighbors find a 65-year-old male unconscious in his garden and immediately call EMS. The man is intubated at the scene. In the ER, he develops sustained ventricular tachycardia and requires cardioversion. He is started on an antiarrhythmic agent and, once recovered, is discharged to home. Three months later he returns to his physician complaining of dyspnea on exertion. Chest-x ray reveals bilateral lung fibrosis. All cultures are negative and lung biopsy reveals lipoid pneumonitis. Which of the following medications is most likely responsible for his current condition?
Procainamide
Amiodarone
Lidocaine
Quinidine
Digoxin
A 12-year-old African American male is found to have a murmur during a routine sports physical. He has a family history of sudden death at a young age. It is a harsh crescendo-decrescendo murmur that begins after S1 and is best heard at the left lower sternal border. Valsalva maneuver intensifies the murmur. Which of the following is the most likely mitral valve abnormality in this patient?
Dilated mitral valve annulus
Rupture of chordae tendinae
Abnormal mitral leaflet motion
Mitral annulus calcifications
Prolapse of the mitral valve
A 36-year-old female presents to the emergency room complaining of chest pain that started suddenly while she was shopping at the mall. She also reports shortness of breath, palpitations and diaphoresis. The pain is retrosternal and radiates to the left arm. There are no aggravating or relieving factors. On review of systems, the patient reports having had a runny nose, sore throat and dry cough for the past 3 days. Her past medical history is significant for panic attacks, for which she takes paroxetine, and dysfunctional uterine bleeding, for which she takes estrogen. Her family history is significant for the sudden death of her father at age 44 from a heart attack. Social history reveals that she has smoked one pack of cigarettes per day for the past 15 years. Which of the following is the most appropriate initial therapy for this patient?
Lorazepam
Aspirin
Ibuprofen
Acetaminophen
Heparin
A 65-year-old female is admitted to the hospital with increasing shortness of breath, weight gain and lower extremity edema. She has a history of hypertension, nonischemic cardiomyopathy with an ejection fraction of 30%, and hyperlipidemia. Her home medications include oral aspirin, digoxin, furosemide, metoprolol, lisinopril and atorvastatin. She is started on intravenous furosemide. On day three of hospitalization telemetry reveals six beats of wide complex ventricular tachycardia. Physical examination now shows decreased leg edema and clear lungs. Which of the following is the most appropriate next step in the management of this patient's tachycardia?
Add spironolactone
Add metolazone
Measure serum electrolytes
Discontinue atorvastatin
Discontinue metoprolol
A 34-year-old male presents with palpitations for the past 4 hours without associated chest pain, shortness of breath, fevers, or chills. His medical history is significant for Wolff-Parkinson-White syndrome for the past ten years and three prior episodes of supraventricular tachycardia. He does not smoke cigarettes, and drinks alcohol on social occasions. He does report having had five cans of beer while at a party last night. On examination, his blood pressure is 120/80 mmHg and his pulse is irregularly irregular. EKG shows atrial fibrillation with a rate of 160/min. What is the best next step in the management of this patient?
Digoxin
Verapamil
Lidocaine
Procainamide
Adenosine
A 45-year-old male presents to your clinic with complaints of pleuritic chest pain. He says he is a heavy smoker and has been having intermittent cough for the past 2 weeks. His blood work is normal and his chest x ray is clear. EKG reveals a normal sinus rhythm with a heart rate of 68. He does have a PR interval > 0.2 seconds. The next step in the management of his arrhythmia is:
Observation
Atenolol
Pacemaker
Electrophysiology study
Cardiac catheterization
A 21-year-old man comes to the ER with palpitations and dizziness that began suddenly one hour ago. He notes having similar past episodes provoked by fatigue or strong emotions. He says he can usually stop the episodes by putting his head into cold water or squatting and taking a deep breath. However, these techniques are not working this time. Presently, his blood pressure is 60/30 mmHg and his heart rate is 240/min. He is diaphoretic with cold extremities. An EKG rhythm strip shows a regular, narrow complex tachycardia. Which of the following is the best next step in managing his condition?
Adenosine
Procainamide
Verapamil
Digoxin
DC cardioversion
A 64-year-old Caucasian male presents to the Emergency Room with a sharp, left-sided chest pain. He says that the pain is worse when he takes deep breaths, but he gets relief with leaning forward. He had an acute non-ST elevation myocardial infarction six months ago and had undergone angioplasty for the right coronary artery. His other medical problems include: diabetes, hypertension, hyperlipidemia, peripheral neuropathy, diabetic retinopathy, paroxysmal atrial fibrillation, hypothyroidism, and chronic renal insufficiency. His vital signs are BP 142/86 mmHg, PR 78/min, RR 16/min, and T 36.1 C (97F). On examination, you find a pericardial rub. EKG shows diffuse ST elevation. Lab results are: Hb 9.0 g/dl WBC 8,000/cmm Platelets 210,000/cmm Blood Glucose 248 mg/dl Serum Na 135 mEq/L Serum K 5.8 mEq/L Bicarbonate 17 mEq/L BUN 86 mg/dl Serum Creatinine 4.4 mg/dl Which of the following is the most appropriate management of this patient?
NSAIDs
Corticosteroids
Pericardiocentesis
Hemodialysis
Echocardiography
A 63-year-old woman with a long history of hypertension faints after experiencing the sudden onset of severe chest pain that radiates to her back. She is rushed to the emergency room. Upon arrival she is agitated and demands quick pain relief. Her heart rate is 110/min and blood pressure is 90/50 mmHg. Jugular veins are distended. An intraarterial catheter shows significant variation of systolic blood pressure related to the respiratory cycle. Chest x-ray reveals widening of the mediastinum. Which of the following is the most likely cause of this patient's syncope?
Papillary muscle dysfunction
Intravascular volume loss
Pericardia! Fluid accumulation
Vagal hyperactivity
Cardiac tachyarrhythmia
A 32-year-old woman is brought to the emergency department with excruciating chest and neck pain. She is 6'2" and has long extremities. Her hand joints show significant extensibility. Which of the following additional findings is also likely in this patient?
Fourth heart sound
Early diastolic murmur
Opening snap
Fixed splitting of the second heart sound
Kussmaul's sign
A 53-year-old Caucasian woman comes to the physician for a routine health maintenance examination. Recently, she noticed a mild hand tremor while performing some fine tasks, like pouring out the tea. She says that the tremor disappears for a while after drinking a glass of wine. Her past medical history is insignificant. Her blood pressure is 160/90 mmHg and heart rate is 80/min. Physical examination is insignificant. Which of the following medications is the best choice to treat this patient's hypertension?
Propranolol
Verapamil
Amlodipine
Hydrochlorothiazide
Enalapril
A 47-year-old male was brought to the emergency room with chest pain of acute onset. The pain was associated with nausea, vomiting, and diaphoresis. He has a history of diabetes, hypertension, and hyperlipidemia. ECG reveals ST segment elevation in the anterolateral leads and ventricular premature beats (VPBs). The patient dies within the first hour after the arrival to emergency room. What is the most likely pathophysiologic mechanism responsible for this patient's death?
Electro-mechanic dissociation
Reentry
Full conduction block
Increased automaticity
Asystole
A 60-year-old Caucasian man presents to the office with a 2-week history of worsening shortness of breath and decreased exercise tolerance. His breathlessness is worse at night. He thinks his legs are swelling up. He has hypertension, coronary artery disease and chronic obstructive pulmonary disease. He used to drink heavily and smoke 1 pack of cigarettes daily but has quit recently, although he still reports occasionally drinking a "few beers." He currently denies any chest pain, palpitations or cough. His temperature is 37.5C (99.5 F), blood pressure is 110/70 mm Hg, pulse is 96/min and respirations are 22/min. The pertinent physical findings are an S3, bibasilar crackles, JVP 10 cm above the sternal angle, mild hepatomegaly, and 4+ pitting lower extremity edema. The patient is immediately treated with oxygen, intravenous furosemide, and nitrates Which of the following markers is most likely elevated in this patient?
B-type natriuretic peptide
Mean corpuscular volume
Ejection fraction
Urine sodium
Neutrophil count
A 69-year-old male presents to the emergency department with severe pain in the back of his chest that began suddenly 6 hours ago, and 2 hours of difficulty walking due to leg weakness. He has never had such symptoms before. His past medical history is significant for hypertension, bleeding peptic ulcers, and deep vein thrombosis requiring inferior vena cava filter placement. He drinks 6-8 cans of beer each weekend and does not smoke cigarettes or use illicit drugs. Blood pressure taken from his right arm is 210/120 mmHg. His heart rate is 120/min and regular. Chest x-ray reveals a right-sided pleural effusion. EKG shows sinus tachycardia. What is the most likely diagnosis?
Angina pectoris
Myocardial infarction
Acute pericarditis
Aortic dissection
Pulmonary embolism
A 34-year-old male with a history of mitral valve prolapse and mitral regurgitation presents with one week of intermittent fevers and increasing fatigue. He was punched in the face during a street fight two weeks ago. On admission he receives empiric intravenous vancomycin and gentamicin. Three days later, three out of four blood cultures grow Streptococcus viridans highly sensitive to penicillin. Which of the following is the best next step in managing this patient?
Continue current regimen
Switch antibiotics to IV ceftriaxone
Switch antibiotics to oral penicillin V
Switch antibiotics to oral amoxicillin/clavulanate
Switch antibiotics to IV aminoglycosides
A 10-year-old boy is brought to the ER by his mother because he has lost consciousness, while playing in the yard. He regained his consciousness quickly without following confusion. He never had such an episode before. His past medical history is significant for impaired hearing since birth and one episode of pneumonia three years ago, which required hospitalization. The family history is significant for a sudden cardiac death, in his cousin, at the age of 13. Physical examination is unremarkable. Blood pressure is 110/70 mmHg. Heart rate is 70/min, regular. Which of the following medication is most appropriate for this patient?
Propranolol
Verapamil
Quinidine
Ethosuximide
Phenobarbital
A 57-year-old male presents to your office with a two-week history of fever, chills, and generalized weakness. His medical history is significant for a hospitalization for pyelonephritis requiring IV antibiotics six months ago. He also recently underwent cystoscopy for evaluation of persistent dysuria. His past medical history is also significant for an episode of rheumatic fever as a child and Hodgkin's lymphoma treated with chemotherapy 10 years ago. On examination, his temperature is 37.8°C (100°F), blood pressure is 150/86 mmHg, pulse is 98/min and regular, and respirations are 16/min. The patient appears slightly diaphoretic. You note a new II/VI systolic murmur and tender erythematous lesions affecting several fingertips. The remainder of the physical examination is unremarkable. Which of the following bacteria is most likely responsible for his present illness?
Streptococcus pyogenes
Staphylococcus epidermidis
Enterococci
Viridans streptococci
Coxiella burnetii
A 57-year-old male presents to the emergency department with recent-onset dyspnea and cough. He reports that his symptoms began earlier this morning while he was jogging, when he suddenly started feeling short of breath and very weak. In the emergency department, laboratory analysis reveals a markedly elevated serum b-type natriuretic peptide level. Which of the following clinical signs best correlates with this finding?
Wheezing
Cyanosis
Third heart sound
Extremity edema
Periumbilical bruit
A 68-year-old Caucasian male presents to the emergency room with a three-week history of progressive dyspnea, orthopnea, and lower extremity edema. His past medical history is significant for hypertension, type 2 diabetes mellitus, myocardial infarction experienced eight years ago, and congestive heart failure. His current medications include metoprolol, digoxin, enalapril, furosemide, spironolactone, and aspirin. His blood pressure is 145/90 mmHg, and heart rate is 75/min. Symmetric 2+ pitting edema of the lower extremities is present. Point of maximal impulse is displaced to the left and soft holosystolic murmur is heard on the apex. Bilateral crackles are present over the lower lobes. His laboratory values are: Hemoglobin 11.0 g/dl Leukocyte count 7,500/cmm Platelets 300,000/cmm Serum sodium 128 mEq/L Serum potassium 5.3 mEq/L Serum calcium 9.0 mg/dl Serum phosphorus 4.0 mg/dl Serum creatinine 1 .9 mg/dl ECG does not reveal acute ischemic changes. Which of the following is most likely correct concerning this patient's condition?
Serum norepinephrine level is low
The combination of furosemide and enalapril is the cause of hyperkalemia
Hyponatremia indicates severe heart failure
Increasing the dose of digitalis may be indicated
Increasing sodium intake will help to control the electrolyte abnormalities
A 76-year-old man presents to your office with progressively worsening fatigue over the past several months. He denies associated chest pain, dyspnea, nausea, cough, or ankle swelling. He has smoked a pack of cigarettes per day for the past 30 years. His past medical history is significant for hypertension for which he takes hydrochlorothiazide and type 2 diabetes mellitus controlled with metformin. He had a medical check-up five months ago which did not uncover any new abnormalities or medical issues. On physical examination today, his blood pressure is 130/80 mmHg and his heart rate is 110 and irregularly irregular. His lab values are: Hematocrit 41% WBC count 4,700/mm3 Platelets 200,000/mm3 Sodium 137 mEq/L Potassium 4.1 mEq/L Creatinine 0.8 mg/dl Fasting glucose 85 mg/dl Which of the following is the best treatment for this patient?
Captopril
Salmeterol
Amlodipine
Warfarin
Spironolactone
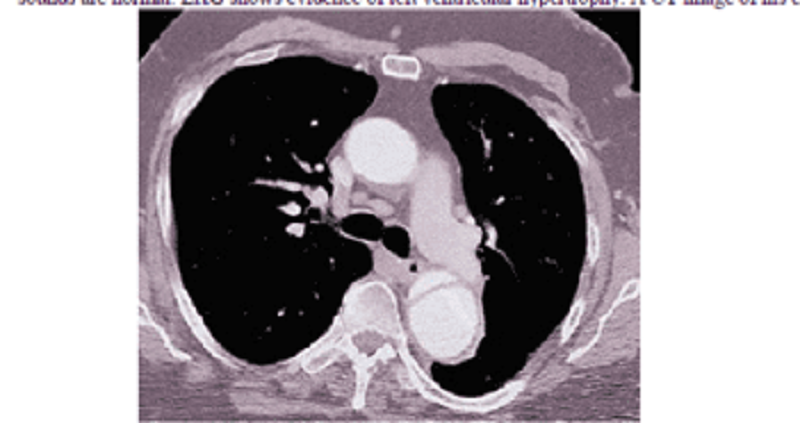
A 48-year-old African American man presents to the emergency room with severe retrosternal chest pain. His temperature is 36.7C (98.F), blood pressure is 190/100 mm Hg, pulse is 100/min, and respirations are 16/min. On physical examination, his lungs are clear to auscultation and his heart sounds are normal. EKG shows evidence of left ventricular hypertrophy. A CT image of his chest is shown below. Which of the following is the most appropriate immediate pharmacotherapy for this patient?
Labetalol
Nifedipine
Heparin
Hydrochlorothiazide
Hydralazine
A 70-year-old male is brought to the ER, by his wife, because he lost consciousness while getting up in the morning. The syncopal episode lasted for several minutes, and the patient rapidly recovered consciousness. He had diarrhea and a decreased appetite one day earlier, which resolved spontaneously. His past medical history is significant for hypertension that is effectively controlled with the combination of hydrochlorothiazide/amiloride. His blood pressure is 120/70 mm Hg, while supine, and 98/50 mm Hg, while standing. The physical examination revealed a mucosal dryness. The EKG is normal. Which of the following laboratory values is the most sensitive indicator of the patient's underlying condition?
Decreased sodium concentration in the urine
Hypokalemia
Increased BUN/creatinine ratio
Metabolic acidosis
Decreased haematocrit
A 65-year-old man complains of lower leg swelling, fatigue and poor appetite. His past medical history is significant for recurrent chest infections, wheezing, cough, recent pyelonephritis, and arterial hypertension. He smokes 1 pack of cigarettes a day but denies alcohol or intravenous drug use. His physical examination reveals a barrel-shaped chest with bilateral scattered wheezes. His abdomen is distended and his liver edge is palpated 4 cm below the right costal margin. You note pitting edema and dilated, tortuous, superficial veins over the bilateral lower extremities. Manual pressure on the abdomen causes persistent distention of the jugular veins. The patient's serum sodium level is 135 mEq/L and his creatinine concentration is 1.2 mg/dl. An abnormality of which of the following is most likely to explain his edema?
Serum albumin level
Pulmonary artery systolic pressure
Pulmonary capillary wedge pressure
Portal venous resistance
Urinary protein excretion
A 60-year-old male presents to the emergency room with the chief complaint of progressive exertional dyspnea and fatigue. He denies any chest pain, syncope, cough, or edema. He suffered an acute anterior wall myocardial infarction one month ago. Chest auscultation reveals bilateral crackles in his lower chest. Cardiac auscultation reveals a pansystolic murmur at the apex with radiation to the axilla. ECG shows previously present unchanged Q waves and a persistent ST segment elevation in the anterior leads. Based on these findings, what is the most likely underlying cause of his symptoms?
Interventricular wall rupture
Ventricular free wall rupture
Ventricular aneurysm
Recurrent ischemia
Right ventricular infarction
A 65-year-old male presents to your office with a six-month history of periodic substernal pain. The pain episodes are experienced during strong emotion, last for 10-15 minutes, and resolve spontaneously. He has a long history of hypertension and diabetes mellitus, type 2. His right foot was amputated two years ago due to diabetes-related complications. You suspect angina pectoris and decide to perform myocardial perfusion scanning. It reveals uniform distribution of isotope at rest, but inhomogenesity of the distribution after dipyridamole injection. You conclude that the patient has ischemic heart disease. Which of the following effects of dipyridamole helped you in making the diagnosis?
Increased heart contractility
Coronary steal
Dilation of diseased vessels
Inhibition of platelet aggregation
Placebo effect
A 37-year-old healthy Caucasian male is seen in your office for a routine physical examination. He denies any symptoms or illness. He says he smokes a pack a day and drinks one to two beers every weekend. He has no allergies. Examination is unremarkable. The EKG reveals normal sinus rhythm with a heart rate of 72; there are frequent premature atrial beats present. The blood pressure is 120/65mm Hg. The next step in his management is:
Digoxin
Lidocaine
Order potassium levels
Complete electrophysiological study
Observation
A 56-year-old white male presents with dyspnea for the last 3 months. His dyspnea was initially exertional but it has worsened progressively and now he is breathless even at rest. He denies any chest pain or ankle swelling. He has been smoking one-pack/day cigarettes for the last 30 years and has been drinking alcohol heavily for the last 10 years. He is not taking any medication. His mother died of breast cancer at 57. His vitals are, PR 86/min, BP 113/76mm of Hg; Temperature 37.1C (98.9F); RR 13/min. On auscultation of his precordium an S3 is heard, but there are no murmurs. Chest auscultation reveals bilateral basal crepitations. Chest x-ray shows marked cardiac silhouette enlargement and pulmonary venous congestion. EKG shows non-specific ST-T wave changes. Echocardiography shows a dilated left ventricle and systolic dysfunction (EF of 25-30%). CBC shows hematocrit of 32%, WBC count of 6,000/microl, and platelet count of 60,000/microl. Peripheral blood smear shows MCV of 101 fl. LFTs show AST of 180U/L and AL T of 66 U/L. The findings of cardiac catheterization and coronary angiography are not compatible with the diagnosis of ischemic cardiomyopathy. Which of the following measures is most likely to reverse his heart failure?
Cessation of cigarette smoking
Abstinence from alcohol
Reduced salt intake
Use of ACE inhibitors
Use of digoxin
A 55-year-old Caucasian male presents to your office for a routine check-up. His past medical history is significant for gout, hypertension, and hypercholesterolemia. His current medications include enalapril and pravastatin. He does not smoke or consume alcohol. His blood pressure is 156/94 mmHg and heart rate is 80/min. Physical examination reveals that the patient is moderately overweight (BMI = 27 kg/m2) with increased waist-to-hip ratio. You consider adding hydrochlorothiazide to the treatment regimen to improve the control of hypertension. Which of the following metabolic effects do you expect to emerge after this correction?
Hypocalcemia
Hyperkalemia
Decreased LDL cholesterol
Decreased plasma triglycerides
Hyperglycemia
Sociated symptoms. His past medical history is significant for hypertension, type 2 diabetes, hypercholesterolemia and hypothyroidism. His medications include aspirin, metformin, glipizide, hydrochlorothiazide, lisinopril, low dose atorvastatin and levothyroxine. He has smoked 1-2 packs of cigarettes daily for the past 40 years, and he drinks 1-2 glasses of wine daily. On physical examination, his blood pressure is 160/90 mmHg and his pulse is 80/min. Heart sounds are normal and his lungs are clear. Laboratory studies show: Serum creatinine 1.7 mg/dL Low density lipoprotein (LDL) 150 mg/dL HbA1C 8.5% Serum TSH 3.0 Which of the following interventions would most reduce the likelihood of his aortic aneurysm enlarging?
Better control of hypertension
Better control of hypercholesterolemia
Better control of diabetes
Smoking cessation
Alcohol cessation
A 68-year-old white female presents to the ER complaining of sudden onset chest pain associated with two episodes of vomiting. She has hypertension for which she takes atenolol and hydrochlorothiazide. Her pulse is 60/min, blood pressure is 80/50 mmHg and respirations are 14/min. Examination shows elevated jugular venous pressure and a positive Kussmaul's sign. Her lungs are clear to auscultation. Her EKG shows 2 mm ST segment elevation in leads II, Ill and aVF and 1 mm ST segment depression in leads I and aVL. Which of the following is the most likely cause of this patient's hypotension?
Pulmonary thromboembolism
Right ventricular infarction
Interventricular septum rupture
Variant angina
Intravascular volume depletion
A 72-year-old male is admitted to the hospital with chest pain. EKG and cardiac enzymes confirm a myocardial infarction and he is started on nitroglycerine, aspirin, simvastatin and low molecular weight heparin. Four days later, he complains of leg pain. Physical examination reveals a cold, pale leg. The angiogram is shown below. What is the best next step in his management?
Intravenous streptokinase
Clopidogrel
Cilosta zol
Leg elevation and warm compress
Embolectomy
A 53-year-old man presents to your office complaining of weakness and exertional dyspnea over the last week. He denies chest pain and palpitations. He has no other past medical history. His father died of a myocardial infarction at age 55. On exam, his heart rate is 100/min and blood pressure is 90/60 mmHg. Internal jugular venous pulsation is observed 7 cm above the sternal angle. Lungs are clear to auscultation. Heart sounds are muffled. Which of the following is the most likely cause of this patient's complaints?
Decreased cardiac contractility
Left ventricular outflow obstruction
Decreased left ventricular preload
Pulmonary hypertension
Increased right ventricular compliance
A 24-year-old military recruit is brought to the emergency room after suddenly collapsing while at training camp. Witnesses say he lost consciousness, and in the ER he appears confused. He had apparently been in his usual state of good health until this incident. His medical history includes allergic rhinitis for which he takes chlorpheniramine. On physical examination, his temperature is 41°C (106.F), blood pressure is 90/60 mm Hg, respiratory rate is 22/min, and pulse is 130/min and regular. He appears restless. His pupils are 4mm in size, symmetric, and reactive to light. Lung exam reveals a few rales at both lung bases. His abdomen is soft, non-tender and bowel sounds are present. There is no neck stiffness. His skin is dry and hot. He has 2+ symmetric reflexes in the upper and lower extremities. Muscle tone and bulk are normal. Initial laboratory studies show: Hemoglobin 16.0 g/L Platelets 120,000/mm3 Leukocyte count 18,500/mm3 Blood urea nitrogen (BUN) 40 mg/dL Prothrombin time 17 sec Partial thromboplastin time 40 sec Which of the following is the most likely cause of his current condition?
Heat stroke
Meningitis
Anticholinergic toxicity
Serotonin syndrome
Neuroleptic malignant syndrome
56-year-old man presents to your office complaining of progressively worsening fatigue. He also reports difficulty concentrating and increasing forgetfulness over the past several weeks. On review of systems, the patient reports having unintentionally gained 6 pounds over the last three months. His past medical history is significant for hypertension and atrial fibrillation. On physical examination, he has a blood pressure of 140/90 mmHg and a heart rate of 75/min. His lung fields are clear to auscultation. There is no ankle edema. His skin is dry. Which of the following drugs is most likely responsible for this patient's complaints?
Hydralazine
Metoprolol
Verapamil
Enalapril
Amiodarone
A 33-year-old Russian male reports concern over recurrent episodes of a "pounding" and "racing" heart over the last several months. He says his symptoms are worst while lying supine and while lying on his left side. On physical examination, his blood pressure is 150/55 mmHg and heart rate is 73/min. Which of the following is most likely responsible for his symptoms?
Aortic regurgitation
Pulmonary regurgitation
Mitral stenosis
Tricuspid stenosis
Aortic stenosis
A 34-year-old man rushes into the ER complaining of severe substernal chest pain that began abruptly 30 minutes ago. He says that he also feels as though his heart 'is racing,' but denies any shortness of breath, cough or fever. He has never experienced pain like this before. His past medical history is significant for an appendectomy one year ago. The patient reports that his father died at age 64 due to "some heart problem" and his mother died of ovarian cancer. On physical examination, the patient is agitated and sweating profusely. His pulse is 110/min, blood pressure is160/100 mm Hg, and respirations are 14/min. Physical examination is normal except for dilated pupils and a small amount of blood at the external nares. EKG shows ST elevations in leads v1_v4. What is the most likely explanation for his symptoms?
Atherosclerotic vascular disease
Acute pericarditis
Pleurodynia
Drug-induced vasospasm
Aortic dissection
A 40-year-old male presents to the Emergency Room with a two-month history of occasional severe headache and blurring of vision. His past medical history is significant for hypertension controlled with hydrochlorothiazide for two years. His family history is significant for hypertension and diabetes. He smokes two packs a day and occasionally consumes alcohol. His blood pressure is 200/140 mmHg and heart rate is 75/min. Which of the following is most consistent with a diagnosis of malignant hypertension in this patient?
Left ventricular hypertrophy on ECG
Elevated serum creatinine level
Papilledema
Oliguria
Blood pressure >/= 200/ 140 mmHg
A 62-year-old man visits his family physician because of generalized aches and pains. He denies associated fevers, headaches, chest pain, or abdominal discomfort. His past medical history is significant for an inferior wall myocardial infarction 6 years ago. His other medical problems include hypertension, diabetes, hypercholesterolemia, and gout. His current medications are aspirin, losartan, naproxen, atenolol, glipizide, colchicine, and simvastatin. On physical exam today, he is afebrile, with blood pressure 130/90 mm Hg, pulse 80/min and respirations 18/min. Lab results are as follows: Sodium 140 mEq/L Potassium 4.2 mEq/L Bicarbonate 21 mEq/L Chloride 100 mEq/l BUN 30 mg/dl Creatinine 1.6 mg/dl AST 113 IU/L ALT 120 IU/L Creatine phosphokinase 14,998 mg/dl What is the most appropriate next step in the management of this patient?
Stop losartan
Stop simvastatin
Start N-acetylcysteine
Order hepatitis panel
Obtain liver biopsy
Complaints. His past medical history is significant for hypertension controlled with a low-dose thiazide diuretic. His family history reveals non-fatal myocardial infarction in his father at the age of 47. The patient does not smoke or consume alcohol. His blood pressure is 130/75 mmHg and his heart rate is 70/min. His previous records show that his HDL level is persistently low in spite of acceptable total cholesterol and LDL levels. You prescribe niacin to raise HDL level. The patient returns in a week complaining of intensive generalized pruritis and flushing. What is the most probable cause of the patient's complaint?
Hypersensitivity reaction
Prostaglandin-related reaction
Drug interaction
Drug-induced vasoconstriction
Psychogenic reaction

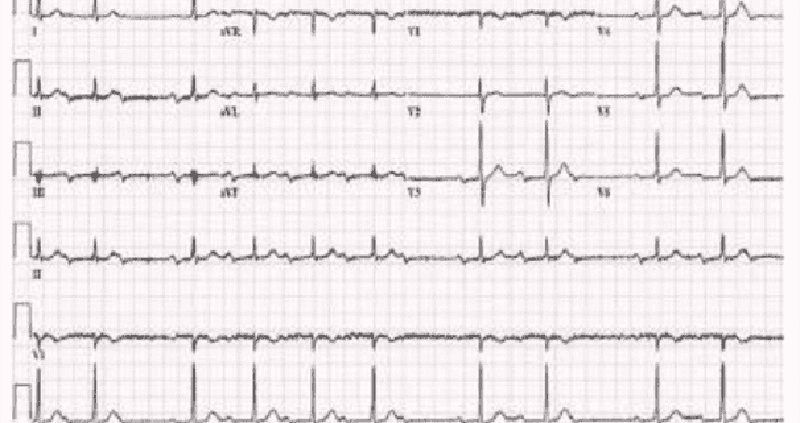
A 77-year-old woman comes to the emergency department because of feeling “light-headed and dizzy.” Except for the irregular pulse, her physical examination is normal. What is the rhythm in the lead tracing shown in Fig.?
First-degree heart block
Second-degree heart block
Third-degree heart block
Premature ventricular beats
Premature atrial beats
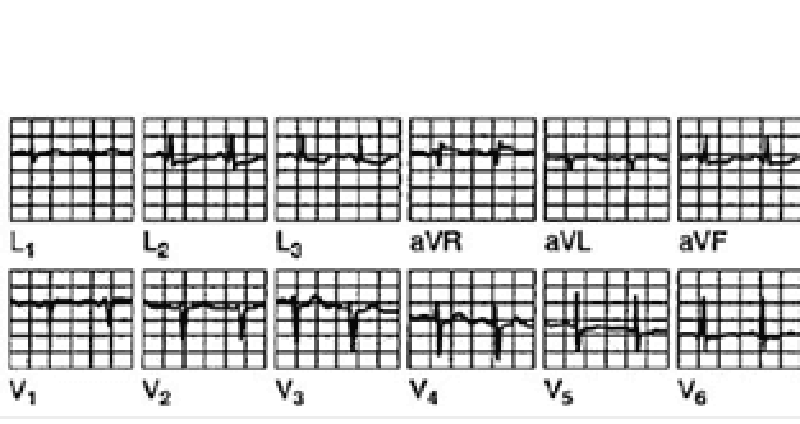
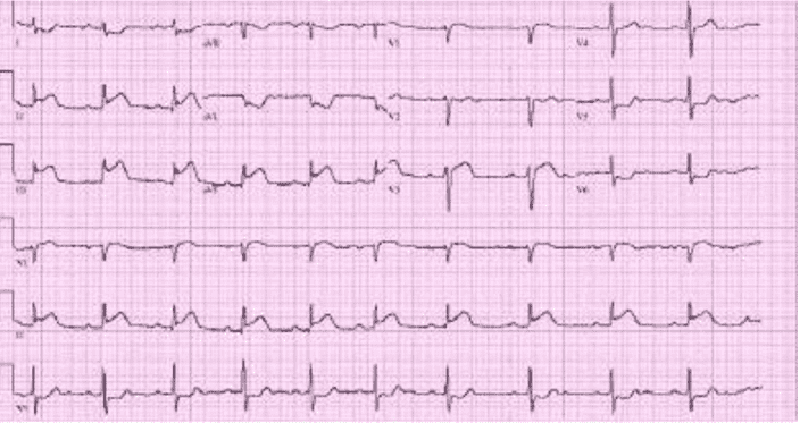
A 42-year-old woman has anterior chest pain of a somewhat atypical nature for many years. The patient’s pain has been present and relatively stable for a number of years, and the ECG shown in Fig. Is a stable one. What is the diagnosis?
Inferior wall infarction
Anterior wall infarction
Ventricular aneurysm
Nonspecific changes
Pericarditis
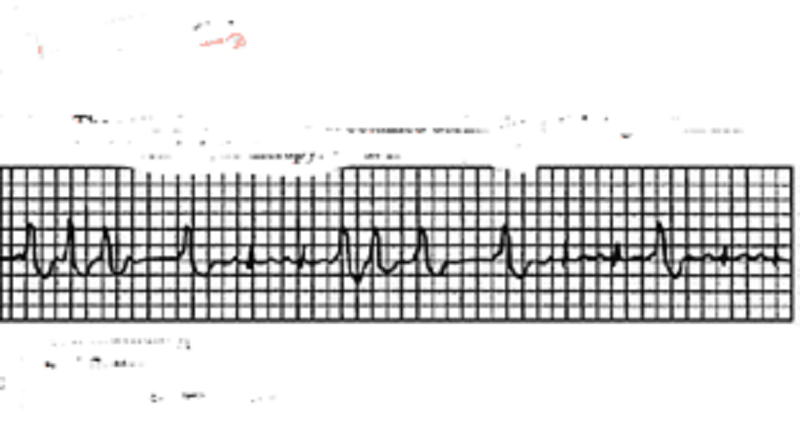
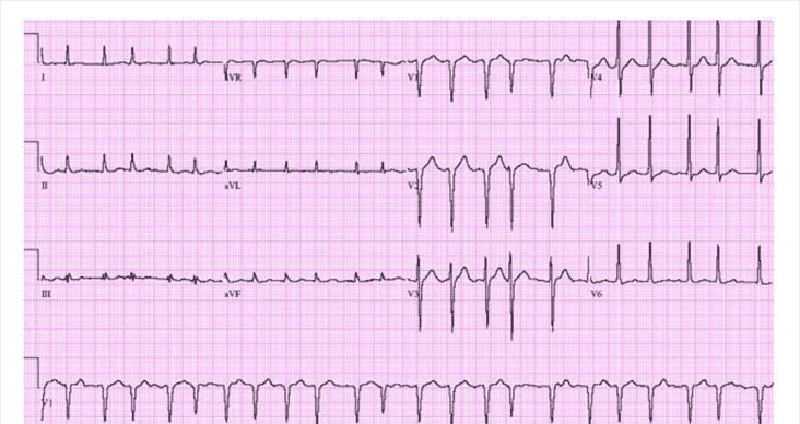
The ECG shown in Fig. Was obtained during the initial stages of an acute MI. The patient had just received thrombolytic therapy. What is the rhythm?
Atrial fibrillation
Atrial flutter
Second-degree heart block
Wenckebach phenomenon
Nonsustained ventricular tachycardia
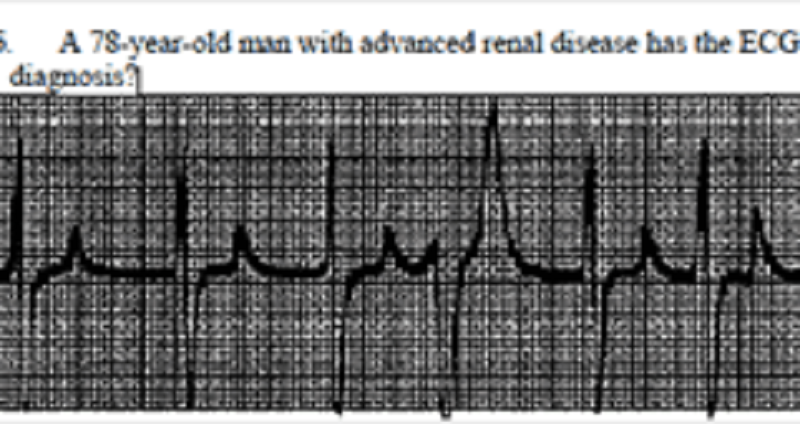
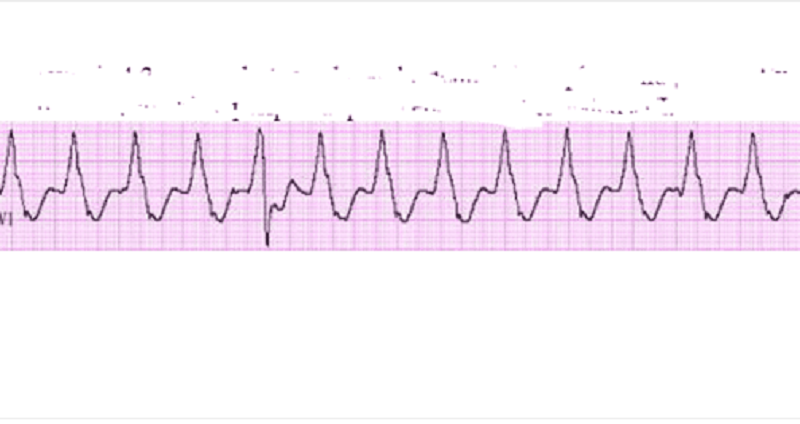
A 78-year-old man with advanced renal disease has the ECG shown in Fig. (lead II). What is the diagnosis?
Hyperkalemia
Hypercalcemia
Hypernatremia
Pericarditis
Ventricular aneurysm
A 74-year-old woman presents to your office complaining of diarrhea and decreased appetite over the past week as well as increasing fatigue and occasional palpitations over the last few days. Her past medical history is significant for chronic atrial fibrillation for which she takes metoprolol, digoxin and warfarin. She smokes cigarettes and has for the past several years. On physical examination, her blood pressure is 140/90 mmHg and her heart rate is 70/min and irregular. Lung auscultation reveals scattered wheezes. Her abdomen is soft and non-tender. The liver span is 8 cm and the spleen is not palpable. There is no ankle edema. Her last measured INR was 2.3 two weeks ago. Which of the following is the best initial test in this patient?
Echocardiography
Chest x-ray
Pulmonary function tests
Thyroid function tests
Blood drug level
A 43-year-old male complains of frequent epigastric burning not relieved by antacids. The sensation is typically brought on by heavy lifting at work and takes 10-15 minutes to go away. He denies having associated arm or neck pain, cough, shortness of breath or difficulty swallowing. His past medical history is significant for systemic lupus erythematosus (SLE) diagnosed five years ago, for which he takes low-dose prednisone daily. On physical examination, his blood pressure is 140/90 mmHg and pulse is 80/min and regular. Heart, lung, and abdomen exams are unremarkable. EKG is normal. Which of the following is the best next step in managing this patient?
Echocardiogram
Coronary angiography
Exercise EKG
Myocardial perfusion testing
Upper Gl endoscopy
A 64-year-old white female presents for evaluation of two weeks of decreased appetite and nausea. She also notes occasional palpitations, which have been especially prominent over the past two days. Her medical history is significant for an anterior wall myocardial infarction one year ago and secondary congestive heart failure with left ventricular systolic dysfunction. Her current medications include aspirin, digoxin, furosemide, enalapril and metoprolol. On physical examination, her blood pressure is 120/80 mm Hg, pulse is 106/min and respirations are 15/min. The remainder of her exam is unremarkable. Chest x-ray shows an enlarged cardiac silhouette and normal lung fields. On laboratory testing, her digoxin level is twice the upper limit of normal. You order an EKG. Which of the following arrhythmias is most specific for digitalis toxicity?
Atrial flutter
Atrial fibrillation
Mobitz type II second-degree AV block
Atrial tachycardia with AV block
Multifocal atrial tachycardia
A 63-year-old male is admitted for sudden onset severe chest pain. His ECG reveals ST elevation in leads V2-V6. He is treated with thrombolytic therapy, heparin, aspirin, metoprolol, morphine, and nitrates. A coronary angiogram performed after thrombolytic therapy reveals 50% obstruction of the left anterior descending artery. On the third day of hospitalization, the patient suddenly develops severe shortness of breath at rest and hypotension. Examination reveals a soft S1, an apical pansystolic murmur radiating to the axilla, and bibasilar crackles. His temperature is 37.8°c (100°F), blood pressure is 92/58 mm Hg, heart rate is 102/min, and respirations are 31/min. An echocardiogram performed on the second hospital day reveals an akinetic region of the anterior wall. What is the most likely explanation for this patient's deterioration?
Pericardia! tamponade
Pulmonary embolism
Rupture of ventricular septum
Papillary muscle dysfunction
Acute aortic dissection
A 34-year-old female presents to your office complaining of pressure-like, substernal chest pain that has been affecting her recently when she plays active sports. Resting consistently alleviates the pain. She denies any associated nausea, vomiting, diaphoresis, dyspnea, palpitations or syncope. Family history is non-contributory. On physical examination, her pulse is 79/min and blood pressure is 130/70 mmHg. Cardiac auscultation reveals a high-pitched 3/6 systolic murmur best heard at the second right intercostal space. The lungs are clear to auscultation. Chest x-ray shows a normal sized heart and clear lung fields. What is the most likely cause of this patient's chest pain?
Anomalous origin of the right coronary artery
Atherosclerotic narrowing of the coronaries
Increased myocardial oxygen demand
Increased myocardial oxygen extraction
Stretching of the papillary muscles
A 45-year-old mildly overweight smoker presents with occasional episodes of nocturnal substernal chest pain that wakes her up from sleep. The episodes last 15-20 minutes and resolve spontaneously. She denies any illicit drug use. She leads a sedentary lifestyle but states that she can climb two flights of stairs without any discomfort. Her pulse is 78/min and regular, blood pressure is 130/70 mmHg and respirations are 13/min. Auscultation of her heart and lungs is unremarkable. Extended ambulatory ECG monitoring reveals transient ST segment elevations in leads V4-V6 during the pain attack. The pathophysiology of this patient's condition is most similar to that of which of the following?
Lacunar stroke
Intermittent claudication
Abdominal aortic aneurysm
Raynaud phenomenon
Pulmonary embolism
An 84-year-old Caucasian male is brought to the ER with severe chest pain, dyspnea and diaphoresis. His past medical history is significant for a long history of hypertension and diabetes mellitus, type 2. He experienced a severe myocardial infarction 6 months ago. His current medications are enalapril, metoprolol, aspirin, furosemide, potassium, glyburide and pravastatin, but he says that he has not been taking some of his medications recently. Physical examination reveals acrocyanosis and symmetric 3+ lower extremity edema. Point of maximal apical impulse is displaced to the left, and a holosystolic II/VI apical murmur is heard at the apex. Non-specific ST segment and T wave changes are present on ECG. The initial set of cardiac enzymes are positive. The patient continues to deteriorate, despite aggressive diuretic and vasodilator therapy. You perform an echocardiographic evaluation of left ventricular function and decide to proceed with pulmonary artery catheterization. Cardiac index (CI), total peripheral resistance (TPR) and left ventricular enddiastolic volume (LVEDV) are determined. Which of the following is most likely to present in this patient?
Cl decreased, TPR decreased, LVEDV decreased
Cl decreased, TPR increased, LVEDV decreased
Cl decreased, TPR increased, LVEDV increased
Cl decreased, TPR increased, LVEDV normal
Cl normal, TPR decreased, LVEDV increased
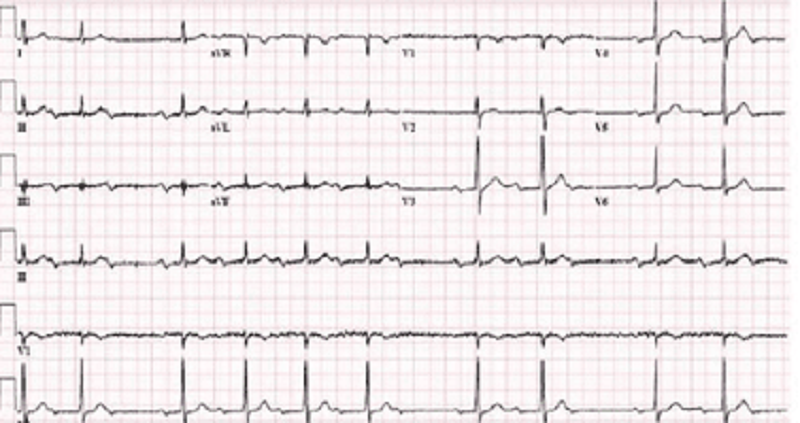
A 42-year -old male with a past medical history of bladder cancer and recurrent hematuria presents to the emergency room after "passing out" when he got out of bed this morning. The patient says that he was standing up to urinate shortly after waking when he began feeling dizzy. Fortunately, he was able to return to his bed before losing consciousness for 7-10 minutes. His EKG at the time of admission is shown below: Which of the following most likely accounts for the observed EKG changes?
Ventricular preexcitation
Impaired SA node automaticity
Impaired AV node conduction
Atrial reentry
His bundle branch block
A 65-year-old man comes to your office for a follow-up after his previous visits revealed inadequately controlled hypertension. He has no present complaints except difficulty walking uphill or climbing stairs, because of the pain in the right thigh, which makes him stop and rest. His past medical history includes stable angina, requiring coronary angioplasty and stenting 2 years ago; hypercholesterolemia; a 20-year history of hypertension; and a 10-year history of diabetes mellitus, type 2. His current medications are aspirin, metoprolol, hydrochlorothiazide, enalapril, amlodipine, pravastatin and glyburide. He smokes 1½packs of cigarettes per day and does not consume alcohol. His blood pressure is 160/100 mm Hg in his right arm and 180/110 mmHg in his left arm. Which of the following findings will point to the potential cause of the resistant hypertension in this patient?
Increased pulsation of intercostal arteries
Continuous murmur in the paraumbilical area to the right
Increased urinal excretion of vanillylmandelic acid(VMA)
High aldosterone/renin ratio
Increased 24-hour urinary free cortisol excretion
A 65-year -old Hispanic male is brought to the emergency room with severe substernal chest pain and diaphoresis that began suddenly 1 hour ago. He reports that his pain started while he was at rest and radiates to his left shoulder. The patient notes having vomited twice when the pain first began. Despite administration of 2 baby aspirins and 3 tablets of sublingual nitroglycerin, the pain persists. His initial EKG is shown below.On physical examination, the patient's temperature is 36.9°C (98.4.F), blood pressure is 110/80 mmHg, pulse is 60/min, and respirations are 18/min. S1 and S2 are normal, and an S4 is heard. The lungs are clear to auscultation. There is no jugular venous distension or pedal edema. Interventions to achieve which of the following goals would most improve this patient's long-term prognosis?
Decrease myocardial oxygen demand
Decrease blood coagulability
Restore coronary blood flow
Prevent ischemia-induced arrhythmias
Prevent reperfusin myocardial injury
A 43-year-old man is hospitalized with chest pain, lightheadedness and nausea. He describes the pain as dull and non-radiating. He has never had chest pain before, but does report occasional episodes of dyspnea and coughing. His medical history is significant for eczema. He is not presently taking any medications. His family history is significant for prostate cancer in his father and rheumatoid arthritis in his mother. He does not smoke or consume alcohol. The patient is admitted to the hospital and is given aspirin, low-molecular weight heparin, metoprolol and captopril. On day 2 of his hospitalization he complains of shortness of breath. Physical examination reveals prolonged expirations and bilateral wheezes. There are no crackles. You estimate the jugular venous pressure to be 7 cm with the patient's head elevated at 45 degrees. Which of the following is most likely responsible for this patient's current respiratory symptoms?
Pericarditis
Bronchial infection
Recurrent myocardial ischemia
Right ventricular infarction
Drug side effect
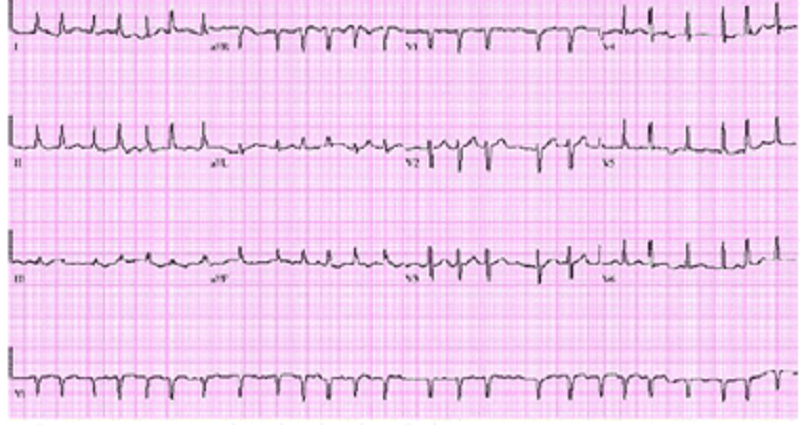
A 64-year -old male with a history of hypertension presents with general malaise and a 'funny' heart rhythm for the past 2 weeks. He had an echocardiogram done last year, which revealed mild left atrial dilatation and left ventricular hypertrophy. He has been taking hydrochlorothiazide for hypertension. His blood pressure at today's visit is 180/98 mm Hg. An EKG is obtained and is shown below. Which of the following is the most appropriate treatment for this patient?
Immediate cardioversion
Lidocaine
Adenosine
Carotid massage
Diltizem
A 53-year-old Caucasian male is admitted to the hospital with a 2-week history of fatigue and decreased exercise tolerance. He says he can hardly climb two flights of stairs without getting dyspneic. He denies palpitations or chest pain. His past medical history is insignificant, and a routine check-up 6 months ago was normal. He admits two episodes of binge drinking during the last month, but says that he 'got it under control'. He is currently not taking any medications. His blood pressure is 150/90 mmHg and heart rate is 130/min, irregular. Lungs are clear on auscultation. ECG does not reveal P waves. Echocardiography shows significant left ventricular dilation with an ejection fraction of 35% and mitral regurgitation (1+). Which of the following intervention will most likely improve the left ventricular function in this patient?
Preload optimization
Decreasing afterload
Rate or rhythm control
Inotropic support
Valve surgery
A 64-year-old male is admitted in ICU for acute myocardial infarction. He is on metoprolol, lisinopril, aspirin, furosemide, and potassium supplements. All of a sudden, the nurse mentions that the patient has a change in his tele monitoring. His blood pressure is 120/60 mm Hg. His potassium level is 4.2. He is alert, awake and oriented time, place and person. Examination shows scattered bilateral crackles, peripheral pedal edema and elevated JVI. Which of the following is the next best step in the management of this patient?
IV amiodarone
IV digoxin
Cardioversion
IV diltiazem
Carotid massage
A 48-year-old Caucasian male presents to your office complaining of progressive exertional dyspnea. It has become especially bothersome over the past two months. Presently, he becomes short of breath after climbing one flight of stairs. He denies any significant problems in the past. He is not taking any medications and he denies smoking or drinking alcohol. His temperature is 37.2°C (98.9F), pulse is 78/min, blood pressure is 130/75 mm of Hg and respirations are 14/min. Chest examination reveals a harsh systolic murmur that is best heard at the right second intercostal space with radiation along the carotid arteries. An S4 is heard at the apex. Based on these findings, what is the most likely cause of this patient's symptoms?
Hypertrophic cardiomyopathy
Myxomatous valve degeneration
Rheumatic heart disease
Bicuspid aortic valve
Senile calcific aortic stenosis
A 47-year-old Caucasian female presents with occasional episodes of nocturnal substernal chest pain that wakes her up during sleep. The pain episodes last 15-20 minutes and resolve spontaneously. She denies any illicit drug use. She leads a sedentary lifestyle but states that she can climb two flights of stairs without any discomfort. She has no history of hypertension or diabetes. Her pulse is 75/min and regular, blood pressure is 134/70 mmHg and respirations are 14/min. Extended ambulatory ECG monitoring reveals transient ST segment elevation in leads I, aVL, and V4-V6 during the episodes. Which of the following is the best treatment for this patient?
Diltiazem
Propranolol
Aspirin
Heparin
Digoxin
A 55-year-old male presents to your office with a 6-month history of periodic substernal pressure. He experiences this pressure while walking uphill or climbing two flights of stairs. His past medical history is insignificant. He smokes 1 pack a day and consumes alcohol occasionally. His blood pressure is 160/90 mmHg and heart rate is 75/min. Resting ECG is normal. You suspect stable angina and order an ECG stress test that reveals horizontal ST segment depression in leads II, III, and aVF at submaximal heart rate. What is the best medication to treat this patient's condition?
Thiazide
Verapamil
Amlodipine
Metoprolol
Enalapril
A 45-year-old man presents to the emergency department because of dyspnea, fatigue, poor appetite and weight gain over the past several weeks. He says that about four weeks ago he began to develop worsening shortness of breath with exertion and more recently has been waking at night with breathlessness. He also notes that it is sometimes difficult for him to open his eyes in the morning due to facial edema. He has no significant past medical history and he takes no medications. On physical examination, his blood pressure is 200/120 mmHg and his heart rate is 100/min. You note generalized bodily edema and distention of his jugular veins while he is sitting upright. On lung auscultation you hear bibasilar rales. Urinalysis shows trace protein, no nitrites, trace leukocyte esterase, 50+ red blood cells and occasional neutrophils. Which of the following is the most likely cause of this patient's edema?
Renal hypoperfusion
Hypoalbuminemia
Extensive glomerular damage
Portal hypertension
Hypothyroidism
Unremarkable except for an upper respiratory infection one week ago. On physical examination, his temperature is 37.2°C (99.F), pulse is 90/min, blood pressure is 100/60 mmHg and respirations are 13/min. His neck veins are distended and his heart sounds are distant. His lungs are clear to auscultation bilaterally. Chest x-ray reveals small bilateral pleural effusions and an enlarged cardiac silhouette. Which of the following EKG findings is fairly specific for his condition?
Prolonged 'PR' interval
Presence of 'F' waves
Electrical alternans
Presence of 'delta' wave
New-onset right bundle branch block
A 56-year-old man presents to the emergency department with dyspnea. He describes waking up during the night with difficulty breathing and chest pain that kept him from falling back to sleep. He has never had these symptoms before. His past medical history is significant for long-standing hypertension and non-compliance with his antihypertensive therapy. He has smoked a pack of cigarettes per day for the past 30 years. On physical examination, his blood pressure is 170/100 mmHg and his heart rate is 120/min and regular. Lung auscultation reveals bibasilar rales and scattered wheezes. Which of the following is most likely to relieve this patient's dyspnea?
Metoprolol
Hydralazine
Nitroglycerin
Dopamine
Amiodarone
A 36-year-old male patient, who has a history of Marfan's syndrome, presents with sudden onset of severe central tearing chest pain radiating to his back. The pain is 9/10 in severity and is unrelated to exertion. He denies any history of alcohol or tobacco use. Measurement of his BP shows a difference of 35 mm Hg between his two arms. Chest auscultation reveals clear lung sounds and a mid-systolic click. What is the most appropriate next diagnostic step in the management of this patient?
Transesophageal echocardiography
Transthoracic echocardiogram
Cardiac enzymes
Coronary angiogram
Ventilation-perfusion scans
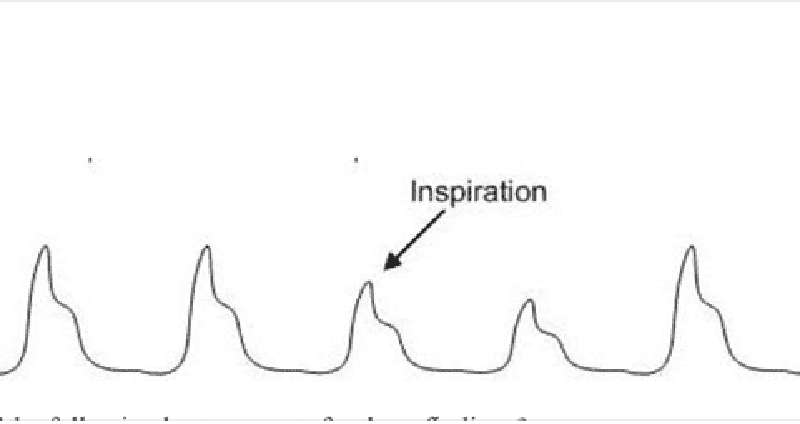
A 34-year-old female presents to the ER with difficulty breathing and dizziness. Blood pressure tracing from an arterial line placed in the ER is depicted below. Which of the following best accounts for these findings?
Severe asthma@
Lobar pneumonia
Mitral stenosis
Aortic regurgitation
Panic attack
A 43-year -old man complains of progressive weakness and shortness of breath over the last two weeks. He denies any chest or muscle pain, nausea, vomiting or weight loss. He had a recent upper respiratory tract infection. His heart rate is 90/min and blood pressure is 110/70 mmHg. Jugular venous pressure is normal. Lungs are clear to auscultation. His chest x-ray is shown below. Which of the following is the most likely additional finding in this patient?
Audible fourth heart sound
Non-palpable point of maximal impulse
Pulsus bisferiens
Opening snap
Fixed splitting of the second heart sound
A 56-year-old white male presents to his primary care physician for follow-up evaluation of high blood pressure noted on each of three prior visits over a period of 6 months (systolic blood pressure ranging 140-145, diastolic blood pressure ranging 90-96 mm Hg). He has smoked a pack of cigarettes per day for the past 20 years and takes 5-6 drinks of alcohol daily. He has no other medical problems and takes no medications. There is no family history of diabetes mellitus, coronary artery disease, hyperlipidemia or hypertension. On physical examination today, his blood pressure is 146/97 mm Hg and pulse is 80/min. The remainder of the exam is unremarkable. Which of the following nonpharmacologic interventions would be expected to have the greatest impact on his high blood pressure?
Smoking cessation
Increased consumption of complex carbohydrates
Increased calcium consumption
Decreased alcohol intake
Decreased consumption of animal protein

A 55-year-old male is admitted to the ICU after being involved in a motor vehicle accident. He requires exploratory laparotomy for suspected bowel perforation. Two days after the surgery he remains hypotensive and requires both aggressive intravenous fluids and vasopressors to maintain his blood pressure. On physical examination, you note the fingertip changes pictured below: All four extremities feel cold to touch. Which of the following is most likely responsible?
Septic emboli
Raynaud's phenomenon
Norepinephrine-induced vasospasm
Cholesterol emboli
Superior vena cava syndrome
A 14-year-old African American male collapses and dies while playing basketball at a school tournament. He has no known past medical history. Which of the following is the most likely underlying disease in this patient?
Hypertrophic cardiomyopathy
Coronary atherosclerosis
Aortic aneurysm rupture
Ventricular septal defect
Bicuspid aorta
A 63-year-old female presents to your office for a routine check-up. She has no present complaints. Her past medical history includes OM, type 2, and hypertension. Her current medications include glyburide and atenolol. She does not smoke. She drinks 2-3 glasses of wine 1-2 times a week. Three consecutive BP measurements were in the range of 138-142/87-90 mmHg. Physical examination is within normal limits. Her recent fasting glucose level was 250 mg/dl. ECG recorded 1 month ago showed left ventricular hypertrophy. Which statement about the BP control in this patient is the most accurate?
BP is within acceptable range
BP is within optimal range
It is better to keep systolic pressure less than 130 mmHg to slow end-organ damage
Diastolic BP is within acceptable range, but systolic is not
Systolic BP is within acceptable range, but diastolic is not
A 70-year-old patient presents to the ER with a 3-hour history of intensive retrosternal chest pain that radiates to the interscapular area. He states that he has never experienced this pain before. His past medical history is significant for a 20-year history of hypertension and a 10-year history of diabetes mellitus, type 2. His current medications include enalapril and hydrochlorothiazide. He does not smoke or consume alcohol. His vital signs are BP 180/110 mm Hg in the right arm and 178/110 mm Hg in the left arm, PR 85/min and RR 18/min. The physical examination revealed an early decrescendo-type diastolic murmur at the left sternal border. The EKG is normal. Which of the following is the best next step in the management of this patient?
Magnetic resonance imaging
Transesophageal echocardiography
Aortography
CK MB and troponin T levels
Ventilation/perfusion scanning
A 46-year-old man complains of exertional dyspnea and dry cough. He also describes occasional episodes of a suffocating nighttime cough that is relieved only when he stands up. His medical history is significant for a myocardial infarction six months ago. His current medications are metoprolol, aspirin and simvastatin. He does not use tobacco but drinks alcohol on social occasions. His father died of a stroke and his mother suffers from diabetes mellitus. His blood pressure is 150/100 mmHg and his heart rate is 60/min. Chest examination reveals bibasilar rales. His cardiac apex is palpated in the sixth intercostal space. The liver span is 12 cm. Bilateral pitting leg edema is also present. Which of the following most likely contributes to his edema?
Constriction of the renal arterioles
High sodium delivery to the distal tubule
Increased renal blood flow
Increased renal potassium loss
High portal venous resistance
A 22-year-old white female is brought to your office by her mother because of the recurrent syncopal episodes. The first episode occurred about one year ago when her roommate committed suicide and then several similar episodes occurred usually provoked by a strong emotion. The episodes are preceded by lightheadedness, weakness, and blurred vision and last about three minutes with rapid recovery of consciousness. Past medical history is insignificant. She is not taking any medications and denies drug abuse. Her blood pressure is 110/70 mm/Hg while supine and 108/70 mmHg while standing. Physical findings are within normal limits. EKG performed one month ago was normal. Which of the following is the next best step in the management of this patient?
Chocardiography
24-hour (Holter) monitoring
Electroencephalogram
Invasive electrophysiologic testing
Upright tilt table testing
A 32-year-old man presents to the emergency department with a three-day history of fever, cough and weakness. His blood pressure is 120/80mmHg and his heart rate is 110/min. Physical examination reveals multiple needle tracks on his arms. ECG shows sinus tachycardia but is otherwise normal. Chest X-ray shows scattered round lesions in the peripheral lung fields bilaterally. Urinalysis is positive for 2+ protein. Which of the following accompanying findings is most likely in this patient?
S4 when patient is in the left lateral decubitus position
Systolic murmur that increases on inspiration
Diastolic murmur heard best with the patient sitting up
Systolic murmur that increases when the patient stands up
Paradoxical splitting of S2
41-year-old intravenous drug abuser presents with shortness of breath and pleuritic chest pain. He is febrile with a temperature of 103.5°F. He has no skin lesions and funduscopic exam is negative. He has jugular venous distension that increases with compression of the liver. The liver is pulsatile. The jugular venous pulse shows a prominent v wave. The patient has splenomegaly. Heart auscultation reveals a holosystolic murmur heard best at the left lower sternal border. The murmur increases with inspiration (Müller maneuver). Which of the following is the most likely diagnosis?
Bacterial endocarditis
Pericarditis
Rheumatic fever
Mitral valve prolapse
Pericardial effusion
A 54-year-old man with a 20-year history of chronic obstructive lung disease has a heave that is palpable at the lower left sternal border at the third, fourth, and fifth intercostal spaces. Which of the following best explains the etiology of the heave?
It is probably a displaced point of maximum impulse (PMI)
It means the patient has congestive heart failure
It means that the patient has aortic stenosis
It means the patient has right ventricular hypertrophy
It means the patient has a pericardial effusion

A 61-year-old woman was on her way to the grocery store when she started feeling chest pressure in the center of her chest. She became diaphoretic and felt short of breath. On arrival to the ED by EMS, her BP is 130/70 mm Hg, HR is 76 beats per minute, and oxygen saturation is 98% on room air. The nurse gives her an aspirin and an ECG is performed as seen below. Which of the following best describes the location of this patient’s myocardial infarction (MI)?
Anteroseptal
Anterior
Lateral
Inferior
Posterior
{"name":"Cardiovascular 2", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 54-year-old woman presents for a routine physical. She has no complaints. She has no history of hypertension, diabetes, hypercholesterolemia, or heart disease, and she does not use tobacco, alcohol or drugs. On physical examination, her pulse is irregular. There are no murmurs. Her lungs are clear to auscultation and her legs are free of edema. An EKG shows atrial fibrillation with a heart rate of 72 beats per minute. An echocardiogram is unremarkable except for evidence of atrial fibrillation. What is the most appropriate management of this patient?, A middle-aged man was recently diagnosed with hypertension. The antihypertensive medication prescribed to him enhances natriuresis, decreases serum angiotensin II concentration, and decreases aldosterone production. This medication most likely belongs to which of the following drug classes?, A 63-year-old woman complains of leg swelling that is especially bothersome in the evening. She also complains of chronic cough and exertional dyspnea. She has been smoking one pack of cigarettes per day for the past 30 years. She also drinks one or two cans of beer on weekends. Her medical history is significant for a hospitalization for a \"chest infection\" two years ago, for which she was treated with antibiotics, steroids, and inhalers. She also reports having been diagnosed with hypertension, but says that she has never taken medications for it. On physical examination, her blood pressure is 160\/90 mmHg and her heart rate is 80\/min. Chest examination reveals bilateral scattered wheezes and prolonged expirations. Her jugular venous pulsation is seen 2 cm above the sternal angle with the head of the bed elevated 30•. Her abdomen is soft and non-distended. On examination of her lower extremities, you note bilateral pitting edema and dilated, tortuous, superficial veins. Which of the following is most likely to relieve this patient's edema?","img":"https://cdn.poll-maker.com/11-487914/106.png?sz=1200-006015079053"}
More Quizzes
QUIZ o Aluminium
520
Test Your Legal Knowledge
1050
Test Your Knowledge of Rraven!
1167
Cor Java
15839
Free Brand and IP Health Assessment
201021696
Take the Ultimate Population - Test Your Geography IQ!
201044558
Ultimate Free CNA Practice Final Exam - Test Now
201055543
What Bra Type Is Best for Me? Free
201028036
Tech, Eng & Mgt Final Project
15834832
Simple Past vs Simple Present - Test Your English
201091628
String Instrument: Think You Know Your Clefs?
201067739
Enemy Pie Story Online: Test Your Book Knowledge
201072384