Part 36

Medical Knowledge Challenge
Test your understanding of various medical conditions, diagnoses, and management strategies with our comprehensive quiz. This engaging quiz features carefully curated questions suitable for both medical students and professionals looking to refresh their knowledge.
Prepare to answer questions on:
- Diagnostics
- Joint and Muscle Disorders
- Infectious Diseases
- Rheumatology
- Clinical Presentations
255) A 35-year-old African-American woman comes to the physician's office complaining of blurred vision, cough and shortness of breath. For the past few days she has had mild fevers, malaise and easy fatigability. She has never had these symptoms before and is anxious to uncover a diagnosis. She was recently incarcerated for two months. She practices unprotected sex with her new boyfriend. Her temperature is 37.2°C (98.9°F) and her blood pressure is 116/80 mmHg. On exam, her right eye is red and slit lamp examination shows leukocytes in the anterior chamber. Lungs have patchy rales. Chest x-ray shows bilateral reticulonodular infiltrates and hilar adenopathy. Which of the following is the most likely diagnosis in this patient?
. Acute HIV infection
. Disseminated tuberculosis
. Sarcoidosis
. Histoplasmosis
. Ankylosing spondylitis

256) A 60-year-old Caucasian woman comes to the physician because of joint pains in both hands. Her other medical problems include obesity and gastroesophageal reflux disease. She does not use tobacco, alcohol, or drugs. Family history is not significant. Her medications include omeprazole and acetaminophen. Her vital signs are within limits. X-ray of the joints is shown below. Which of the following is the most likely diagnosis?
. Rheumatoid arthritis
. Systemic lupus erythematosus
. Osteoarthritis
. Reactive arthritis
. Gouty arthritis
257) A 67-year-old male hospitalized after elective hernia repair complains of severe right knee pain. Physical examination reveals redness and swelling of the right knee with limited motion due to pain. His temperature is 38.9°C (102°F), blood pressure is 160/110 mm Hg, pulse is 80/min, and respirations are 16/min. Synovial fluid analysis reveals the following findings: WBC count 30,000mm3, Neutrophils 90%, Crystals rhomboid-shaped, positively birefringent, Gram stain negative. Which of the following is most likely associated with this patient's current condition?
. Tophi
. Transient bacteremia
. Chondrocalcinosis
. Rheumatoid factor
. Heberden nodes
258) A 43-year-old Caucasian female presents to your office complaining of joint pain and swelling in her hand. On history, she endorses easy fatigability and loss of energy that has been worsening insidiously. It is especially difficult for her to do daily activities in the morning due to prolonged stiffness. She also describes frequent knee pain accompanied by a low-grade fever. She takes ibuprofen and naproxen to relieve her symptoms. Her hematocrit is 33%. The patient is at the greatest risk of which of the following?
. Osteitis fibrosis cystica
. Osteitis deformans
. Avascular bone necrosis
. Osteomalacia
. Osteoporosis
259) A 32-year-old Caucasian male complains of inability to grip his cup of coffee and hold a pen in the morning. He says that he is 'fully functional' in the afternoon. His ESR is 45 mml hr. Which of the following is most likely to be affected by this patient's disease?
. Sacral spine
. Sacroiliac joints
. Lumbar spine
. Thoracic spine
. Cervical spine
260) A 21-year-old woman presents with 4 months of slowly progressive low back pain. Her back pain is associated with early morning stiffness that improves as the day progresses. She has no fever or gastrointestinal complains. She denies any recent illness. On examination, there is limited range of motion of her back. Other examination is unremarkable. Plain X-ray films show bilateral sacroiliitis. Which of the following conditions is this patient at greatest risk of developing?
. Aortic coarctation
. Thoracic aortic aneurysm
. Renal failure
. Oral ulcers
. Anterior uveitis
261) A 30-year-old female comes to your office with a complaint of pain over the lateral side of her wrist for the last four days. She is two months postpartum and notes that her pain is most severe when she lifts her infant from a crib. On examination, there is tenderness over the radial side of wrist and first dorsal compartment. Passive stretching of the thumb tendons over the radial styloid while the thumb is held in flexion aggravates the pain. She denies any recent trauma over the tender area. Which of the following is the most likely diagnosis in this patient?
. Osteoarthritis of first metacarpophalangeal joint
. Trigger thumb
. De Quervain tenosynovitis
. Scaphoid fracture
. Flexor carpi radialis tenosynovitis
262) A 44-year-old female complains of generalized weakness, low-grade fever and joint pain. Her daily activities are limited due to joint stiffness, especially in the morning. Her hand joints are swollen symmetrically. The inferior pole of the spleen is palpable on physical examination. Her hematocrit is 34%. Liver and renal function tests are normal. Two months after the initial visit, the patient develops painful oral ulcers. Her laboratory values are: Hematocrit 33%, AST 120 U/L, ALT 90 U/L, Alkaline phosphatase 90 U/L, Bilirubin 1.1 mg/dl, Creatinine 0.8 mg/dl, BUN 16 mg/dl. Which of the following is the most likely cause of this patient's current complaints?
. Viral hepatitis
. Felty syndrome
. Lymphoid cell proliferation
. Antimetabolite agent
. Corticosteroid treatment
263) A 35-year-old woman presents with complaints of aching pain and stiffness over her entire body for the past 3 months. She also reports, easy fatigability, poor sleep and frequent headaches. She has been using over the counter pain medications with no relief. While examining her, she complains of extreme pain to gentle palpation over her neck, shoulders and back. Her vital signs are stable. What is your diagnosis?
Chronic fatigue syndrome.
Polymyalgia rheumatica.
Rheumatoid arthritis.
Polymyositis.
Fibromyalgia.
264) A 25-year-old immigrant from Eastern Europe is being evaluated for right shoulder pain and swelling. He also complains of heel pain while walking. Palpation over the heels, iliac crests and tibial tuberosities elicits tenderness. Which of the following additional findings is most likely in this patient?
. Positive rheumatoid factor
. Proteinuria
. Limited spine mobility
. Subcutaneous nodules
. Hand joint deformities
265) A 9-year-old Caucasian male complains of fever, sore throat and difficulty swallowing. Small tender lymph nodes are palpated in the cervical region. The symptoms subside quickly on penicillin therapy. Ten days later, the patient presents again with fever, skin rash and fleeting joint pain in the lower extremities. Physical examination reveals scattered urticaria and palpable lymph nodes in the cervical, axillary and inguinal regions. Which of the following is the most likely cause of this patient's current complaints?
. Rheumatic fever
. Drug-induced reaction
. Lymphoproliferative disorder
. Henoch-Schonlein purpura
. Infective endocarditis
266) A 66-year-old man comes to the physician's office complaining of progressive lower back pain. Over-the-counter ibuprofen has provided him with moderate relief. The back pain is associated with bilateral leg pain that is precipitated by walking. The pain improves upon lying down or sitting. He has no pain at night, and no problems with bowel and bladder function. He underwent coronary artery bypass grafting (CABG) 6 years ago for a 3-vessel coronary artery disease. His medications include aspirin, enalapril, atenolol, and lovastatin. Physical examination shows normal strength, reflexes and sensation in his legs. A straight leg raise test fails to reproduce pain. His femoral, popliteal and pedal pulses are full bilaterally and he has no bruits. Plain films of the lumbosacral spine show degenerative changes of the vertebrae. Ankle brachial index measurement is within normal limits. Which of the following is most likely responsible for his current condition?
. Atherosclerosis
. Spinal canal narrowing
. Bulging disc
. Vertebral metastasis
. Spinal cord compression
267) A 35-year-old female presents with a complaint of oral ulcers that are extremely painful. She had a similar presentation three months ago and the ulcers healed without any scarring. Her medical history includes a recent visit to the ophthalmologist with complaints of blurred vision and she is now being treated for anterior uveitis. She has also had recurrent painful ulcers in her genital area for which she has regular follow-up with her gynecologist. On examination, you notice many hyper-pigmented areas over her extremities and few painful, nodular lesions. What is the most likely diagnosis?
. Sarcoidosis
. Reiter's Syndrome
. Herpes simplex infection
. Behcet's syndrome
. Systemic lupus erythematosus

268) A 71-year-old female is brought to your clinic by her daughter with a complaint of severe pain in her fingers. Her daughter says, "Mom has horrible problems with her joints and she has never tried to get help". The patient adds that her fingers have been swollen and painful for a few weeks. She claims that she had a similar condition in her foot last year. She was given a pain pill, but it was ineffective. She takes a water pill for her blood pressure. What is the most likely diagnosis in this patient?
. Rheumatoid nodules
. Gouty arthritis
. Severe osteoarthritis
. Bone tumor
. Severe psoriatic arthritis

269) A 52-year-old male presents with a long history of joint pain. He describes pain and stiffness of the small joints of his hand that is worse in the morning and can last several hours. He also complains of occasional digit swelling. A picture of the patient's hands is shown on the slide below. Which of the following is the most likely diagnosis?
. Enteropathic arthritis
. Rheumatoid arthritis
. Psoriatic arthritis
. Crystalline arthritis
. Sarcoidosis
270) A 30-year-old white male presented to your office with low back pain and stiffness. His pain is worse in the morning and is improved with activity. He has also been having bloody diarrhea for the past few days. On examination, he has painful erythematous nodules over his shins. Pain and stiffness is present in his lower back. Plain radiographs show sacroiliac joint inflammation. Stool cultures are negative. Laboratory studies show anemia and thrombocytosis. P-ANCA is positive in high titers. Which of the following is the most likely cause of his symptoms?
. Reactive arthritis from diarrhea
. Inflammatory bowel disease
Infection with T ropheryma whippelii
. Gluten-sensitive enteropathy
. Infection with Giardia Iamblia
271) A 42-year-old male presents to your office complaining of back pain that started two days ago after carrying heavy packages. He denies any weakness or sensory changes in his legs. His past medical history is insignificant. He is not taking any medications and denies drug abuse. His temperature is 36.7°C (98°F), blood pressure is 120/76 mmHg, pulse is 80/min, and respirations are 16/min. Physical examination reveals paravertebral tenderness. Lower extremity power is 5/5 and the deep tendon reflexes are 2+. Babinski's sign is negative. Straight-leg raising test is negative at 90 degrees. What is the most probable diagnosis in this patient?
. Multiple myeloma
. Ankylosing spondylitis
. Compression fracture of the vertebrae
. Lumbosacral strain
. Herniated disk
272) A 30-year-old obese woman comes to the emergency department complaining of four days of progressive pain, swelling and redness of her right leg. She has no obvious trauma or insect bites. She does not use tobacco, alcohol or illicit drugs. Her temperature is 38.7°C (103.0°F), pulse is 106/min, and blood pressure is 130/80 mmHg. Her right calf is swollen, erythematous, and extremely tender and warm to the touch over a 6 x 3 cm region. There is a tender, palpable mass in her right groin. There is no overlying crepitus and no bullae are seen. The toe webs are fissured and macerated. Laboratory studies show: Complete blood count: Hemoglobin 14.0 g/L, Platelets 222,000/mm3, Leukocyte count 14,500/mm3, Neutrophils 86%, Lymphocytes 14%, Which of the following is the most likely cause of her current leg condition?
. Cellulitis
. Arterial thrombosis
. Deep venous thrombosis
. Necrotizing fascitis
. Ruptured Baker's cyst
273) A 27-year-old African-American woman presents with several complaints. She has had pain and swelling of her hands and wrists for the past few days. She also complains of easy fatigability and frequent mouth ulcers. She has no significant past medical history and does not take any medications. Her temperature is 37.1°C (98.9°F), blood pressure is 140/90mmHg, and pulse is 76/min. Examination reveals swollen, tender metacarpophalangeal and proximal interphalangeal joints. There are superficial ulcers on her buccal mucosa. X-ray of hands and wrists shows no bony erosions. Laboratory studies show: Hemoglobin 11.0 g/L, Platelets 90,000/mm3, Leukocyte count 4,500/mm3. Urinalysis shows 2+ protein and red blood cell casts. Which of the following is the most likely cause of her joint pains?
. Systemic lupus erythematosus
. Dermatomyositis
. Sarcoidosis
. Neuropathic joint disease
. Systemic iron overload
274) A 63-year-old painter presents with pain in his right shoulder for the past few weeks. He experiences pain when he tries to reach for objects and he is unable to lift his arm above his head. He denies trauma to the shoulder, fevers, chills and weight loss. Vital signs are within normal limits. On exam, the physician raises the patient's arm while asking him to relax the shoulder. At 60 degrees, the patient begins to shrug his shoulder and complain of pain. In spite of the pain, his range of motion is normal. A lidocaine injection into the shoulder leads to a significant decrease in pain upon lifting the arm. Which of the following is most likely responsible for his current condition?
. Rotator cuff tear
. Adhesive capsulitis
. Rotator cuff impingement
. Crystal arthritis
. Bacterial infection
275) A 22-year-old Caucasian female comes to your office complaining of difficulty swallowing. She says that solid food sticks in the middle of her chest, and that's why she prefers liquids. She has lost 10 pounds over the last 3 months. She also complains of recent severe heartburn that does not respond well to over-the-counter antacids. On review of systems, she denies cough, shortness of breath and palpitations. She has noticed occasional swelling and pain in her small finger joints. Her fingers turn blue upon cold exposure, and she always wears gloves to keep them warm. She does not smoke or drink alcohol. She denies illegal drug use. Which of the following is the most likely diagnosis?
. CREST syndrome
. Esophageal neoplasm
. Achalasia
. Diffuse esophageal spasm
. Rheumatoid arthritis
276) A 28-year-old woman presents to her physician's office because of pain in her left knee joint. She reports having mild discomfort and pain in right wrist 4 days ago and left ankle pain two days ago. She denies any recent respiratory illness, diarrhea, or urinary symptoms. She has no vaginal discharge. She has no previous medical problems and does not take any medications. She drinks half a pint of vodka daily but denies intravenous drug abuse. She is single and sexually active. Her last menstrual period was one week ago. Her temperature is 38.5°C (101.3°F), blood pressure is 120/80 mmHg, pulse is 98/min, and respirations are 15/min. Examination of the knee reveals warmth, tenderness, decreased range of motion, and an effusion. No skin lesions are present and her pelvic examination is unremarkable. Synovial fluid analysis shows a white blood cell count of 75,000/microl. Which of the following is the most likely cause of her symptoms?
. Non-gonococcal septic arthritis
. Gonococcal septic arthritis
. Acute rheumatic fever
. Acute HIV infection
. Crystal induced arthritis
277) A 45-year-old tennis player comes to your office with a complaint of pain over the lateral side of the right elbow. He has been a professional tennis player for 15 years but has never had this kind of pain before. Range of motion at both elbows is normal. There is point tenderness over the lateral side of the distal end of right humerus. Pain is exacerbated by extension of wrist against resistance. The rest of the physical examination is normal. Which of the following is the most likely diagnosis in this patient?
. Lateral epicondylitis
. Rotator cuff injury
. Radial tunnel syndrome
. Posterior interosseous nerve entrapment
. Rupture of long head of biceps tendon
278) A 65-year-old man complains of periodic back pain radiating to his thigh and buttock. The pain is related to walking or climbing the stairs but is promptly relieved by leaning forward. He also has noticed tingling and numbness in both lower extremities. He has a history of hypertension and takes hydrochlorothiazide. He does not use tobacco, alcohol, or illicit drugs. His pulse is 76/min, respirations are 14/min, and blood pressure is 140/80 mmHg. Lumbar extension reproduces the pain and tingling, while lumbar flexion relieves the symptoms. Which of the following is the most likely cause of this patient's condition?
. Iliac artery atherosclerosis
. Abdominal aortic aneurysm
. Degenerative central canal stenosis
. Lumbar disk herniation
. Spina bifida occulta
279) A 51-year-old Caucasian female complains of low-back pain radiating to the buttocks. She also complains of persistent muscle pain that gets worse with exercise. Physical examination reveals normal muscle strength. Her joints are not swollen, but palpation over the outer upper quadrants of the buttocks and the medial aspect of the knees elicits tenderness. Her ESR is 12mm/hr. Which of the following is the most likely diagnosis?
. Seronegative spondyloarthropathy
. Polymyalgia rheumatica
. Polymyositis
. Rheumatoid arthritis
. Fibromyalgia
280) A 27-year-old male presents to the physician's office because of pain on the medial side of the tibia just below the knee. The pain does not radiate and is continuous. He relates the onset of his pain to falling on the ground while playing football two weeks ago. He denies fever, malaise and weight loss. His past medical history is not significant. On examination, a well-defined area of tenderness is present on the upper tibia below the medial knee joint. There is no redness, warmth or swelling. His gait is normal. A valgus stress test has no effect on his pain. X-ray of the knee and tibia shows no abnormalities. Which of the following is the most likely cause of his current symptoms?
. Anserine bursitis
. Prepatellar bursitis
. Medial collateral ligament strain
. Medial compartment osteoarthritis
. Patellofemoral syndrome
281) A 16-year-old boy presents with a seven-month history of intermittent right knee pain and swelling. He states that his discomfort first began after a baseball injury. This injury was associated with pain, swelling, and restriction of movement in his right knee. He has had three subsequent episodes of pain and swelling in his right knee, not precipitated by trauma. The last episode occurred three days ago. He denies history of fevers or chills. There is no history of recent travel, other than a camping trip with his friends to Long Island, New York a few months ago. On physical examination, he has a marked effusion of his right knee and is unable to fully flex or extend his leg. X-ray reveals no bony abnormalities. What is the most probable diagnosis?
. Rheumatoid arthritis
. Septic arthritis
. Lyme arthritis
. Reactive arthritis
. Osteomyelitis
282) A 75-year-old female comes to the emergency room with acute onset of severe back pain. The pain started while lifting a turkey from the freezer. She had no obvious trauma preceding the pain. She denies weakness or sensory loss in the legs. Her past medical history is significant for temporal arteritis diagnosed several months ago and has been taking prednisone. She does not smoke or consume alcohol. Her temperature is 36.7°C (98°F), blood pressure is 140/70 mmHg, pulse is 80/min, and respirations are 16/min. Physical examination reveals local tenderness of the lumbar spine area. Bilateral ankle reflex is absent. Knee reflex is 2+ in both legs. Babinski's sign is absent bilaterally. Muscle power is 5/5 in both legs. Bilateral straight-leg raising to 90 degrees does not increase the pain What is the most probable diagnosis in this patient?
. Multiple myeloma
. Ankylosing spondylitis
. Compression fracture of the vertebrae
. Lumbosacral strain
. Herniated disk
283) A 66-year-old man complains of a 1-year history of low-back and buttock pain that worsens with walking and is relieved by sitting or bending forward. He has hypertension and takes hydrochlorothiazide but has otherwise been healthy. There is no history of back trauma, fever, or weight loss. On examination, the patient has a slightly stooped posture, pain on lumbar extension, and has a slightly wide base gait. Pedal pulses are normal and there are no femoral bruits. Examination of peripheral joints and skin is normal. What is the most likely cause for this patient’s back and buttock pain?
. Lumbar spinal stenosis
. Herniated nucleus pulposus
. Atherosclerotic peripheral vascular disease
. Facet joint arthritis
. Prostate cancer
284) A 22-year-old man develops the insidious onset of low-back pain improved with exercise and worsened by rest. There is no history of diarrhea, conjunctivitis, urethritis, rash, or nail changes. On examination, the patient has loss of mobility with respect to lumbar flexion and extension. He has a kyphotic posture. A plain film of the spine shows sclerosis of the sacroiliac joints. Calcification is noted in the anterior spinal ligament. Which of the following best characterizes this patient’s disease process?
. He is most likely to have acute lumbosacral back strain and requires bed rest.
. The patient has a spondyloarthropathy, most likely ankylosing spondylitis.
. The patient is likely to die from pulmonary fibrosis and extrathoracic restrictive lung disease.
. A rheumatoid factor is likely to be positive.
. A colonoscopy is likely to show Crohn disease.
285) A 20-year-old man complains of arthritis and eye irritation. He has a history of burning on urination. On examination, there is a joint effusion of the right knee and a rash of the glans penis. Which of the following is correct?
. Neisseria gonorrhoeae is likely to be cultured from the glans penis.
. The patient is likely to be rheumatoid factor—positive.
. An infectious process of the GI tract may precipitate this disease.
. An ANA is very likely to be positive.
. CPK will be elevated.
286) Last week a 20-year-old college student developed acute wrist pain and swelling. This resolved in four days. Yesterday, he developed pain and swelling in his left knee. Two months ago he went on a backpacking trip in Rhode Island. A week or so later he developed an enlarging circular red spot that persisted for 2 weeks and then resolved. What is the most likely diagnosis?
. Acute rheumatoid arthritis
. Parvovirus infection
. Psoriatic arthritis
. Lyme disease
. Inflammatory bowel disease
287) A 38-year-old man has pain and stiffness of his right knee. This began 2-weeks ago after he fell while skiing. On two occasions he had the sense that his knee was locked in a semiflexed position for a few seconds. He has noted a popping sensation when he bends his knee. On examination there is tenderness over the medial joint line of the knee. Marked flexion and extension of the knee are painful. The Lachman test (anterior displacement of the lower leg with the knee at 20°of flexion) and the anterior drawer test are negative. What is the most likely diagnosis?
. Medial meniscus tear
. Osteoarthritis
. Anterior cruciate ligament tear
. Chondromalacia patella
. Lumbosacral radiculopathy
288) A 63-year-old painter complains of severe right shoulder pain. The pain is located posteriorly over the scapula. These symptoms began after he fell from a ladder 2 weeks ago. The pain is especially bad at night and makes it difficult for him to sleep. In addition, he has had some pain in the right upper arm. Treatment with acetaminophen and ibuprofen has been unsuccessful in controlling his pain. On examination the patient appears uncomfortable. The right shoulder has full range of motion. Movement of the shoulder is not painful. There is no tenderness to palpation of the scapula. What is the most likely diagnosis?
. Subdeltoid bursitis
. Rotator cuff tendonitis
. Adhesive capsulitis
. Osteoarthritis
. Cervical radiculopathy
289) A 50-year-old woman with rheumatoid arthritis has been treated with meloxicam (Mobic). You add hydroxychloroquine. Six weeks later her arthritis is mildly improved. The same joints are still involved but she now reports only 1-hour morning stiffness. She has, however, developed epigastric burning and melena for the past 3 days. Stool is strongly positive for occult blood. Which of the following is the most likely cause for the melena in this case?
. Emotional stress over her illness resulting in acid peptic disease
. Hydroxychloroquine-induced acid peptic disease
. Gastric lymphoma associated with autoimmune disease
. NSAID gastropathy
. Meckel diverticulum
290) A 55-year-old woman with long-standing rheumatoid arthritis is on prednisone 5 mg daily and etanercept (Enbrel) 50 mg subcutaneously once a week. Her arthritis is well-controlled. However, she complains of a 2-day history of headaches, chills, and spiking fevers to 39.4°C (103°F). You suspect which of the following?
. An allergic febrile reaction to etanercept
. Fever related to her underlying autoimmune disease
. A serious infection
. A viral syndrome
. An occult malignancy
291) A 32-year-old Japanese woman has a long history of recurrent aphthous oral ulcers. In the last 2 months she has had recurrent genital ulcers. She now presents with a red painful eye that was diagnosed as anterior uveitis. What is the most likely diagnosis?
. Herpes simplex
. HIV infection
. Behçet disease
. Diabetes mellitus
. Systemic lupus erythematosus
292) A 53-year-old man presents with arthritis and bloody nasal discharge. Urinalysis reveals 4+proteinuria, RBCs, and RBC casts. ANCA is positive in a cytoplasmic pattern. Antiproteinase 3 (PR3) antibodies are present, but antimyeloperoxidase (MPO) antibodies are absent. Which of the following is the most likely diagnosis?
. Behçet syndrome
. Sarcoidosis
. Wegener granulomatosis
. Henoch-Schönlein purpura
. Classic polyarteritis nodosa
293) A 35-year-old right-handed construction worker presents with complaints of nocturnal numbness and pain involving the right hand. Symptoms wake him and are then relieved by shaking his hand. There is some atrophy of the thenar eminence. Tinel sign is positive. Which of the following is the most likely diagnosis?
. Carpal tunnel syndrome
. De Quervain tenosynovitis
. Amyotrophic lateral sclerosis
. Rheumatoid arthritis of the wrist joint
. Guillain-Barré syndrome
294) A 50-year-old white woman presents with aching and stiffness in the trunk, hip, and shoulders. There is widespread muscle pain after mild exertion. Symptoms are worse in the morning and improve during the day. They are also worsened by stress. The patient is always tired and exhausted. She has trouble sleeping at night. On examination, joints are normal. ESR is normal, and Lyme antibody and HIV test are negative. A diagnosis is best made by which of the following?
. Trial of glucocorticoid
. Muscle biopsy
. Demonstration of 11 tender points
. Psychiatric evaluation
. Trial of an NSAID
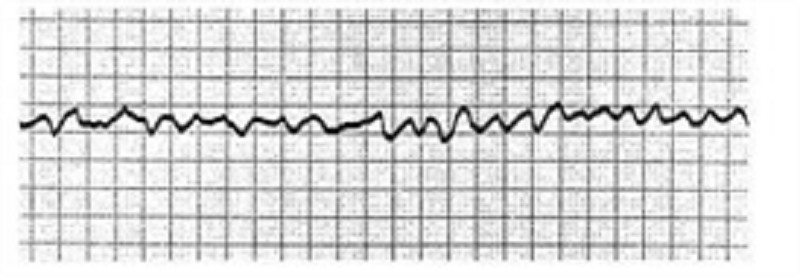
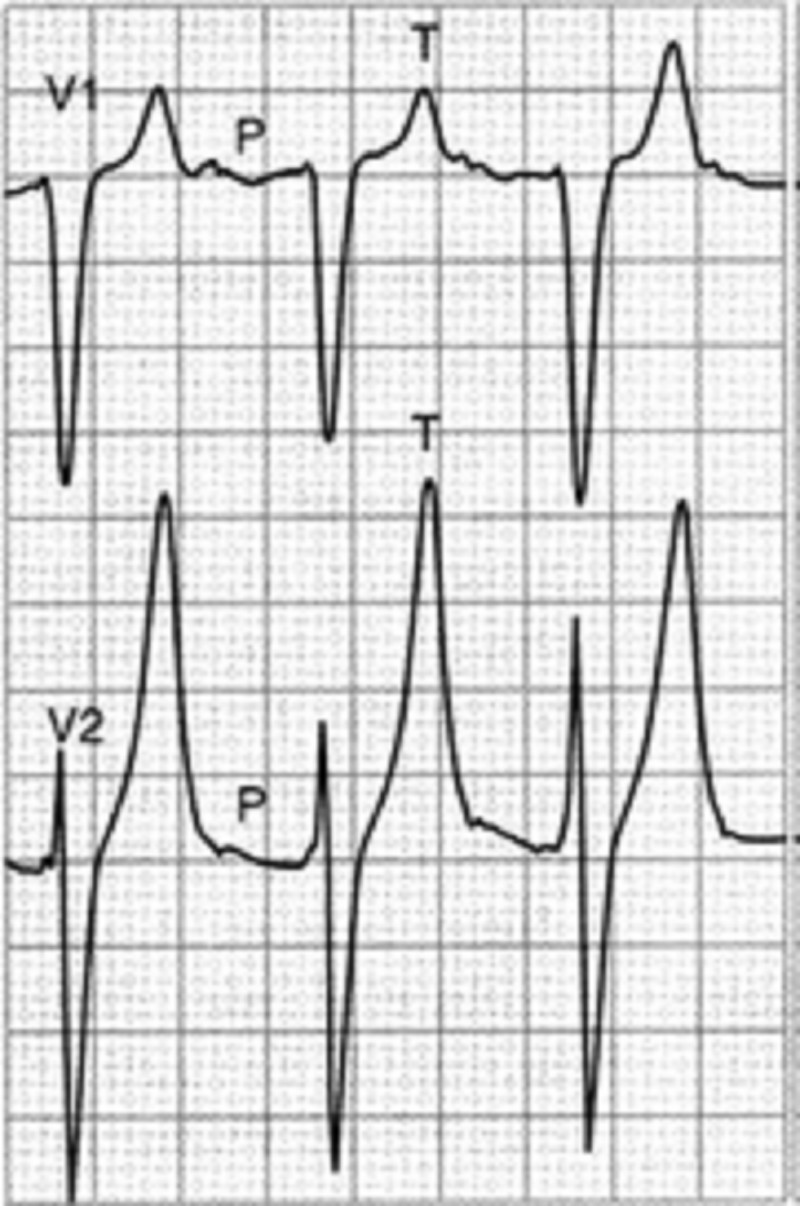
1) A 72-year-old female is admitted to the ICU with severe chest pain. The initial set of cardiac enzymes is positive and her EKG reveals an anterior wall myocardial infarction. She receives treatment with aspirin clopidogrel, metoprolol nitroglycerine drip, and morphine. Two hours later, her telemetry monitor displays the following rhythm. Which of the following is the best next step in managing this patient?
. Lidocaine
. Defibrillation
. Digoxin
. Amiodarone
. Immediate echocardiogram
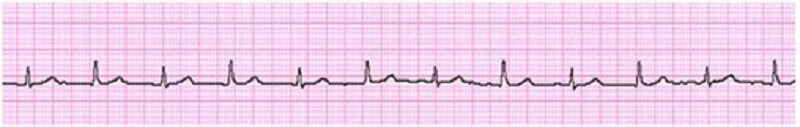
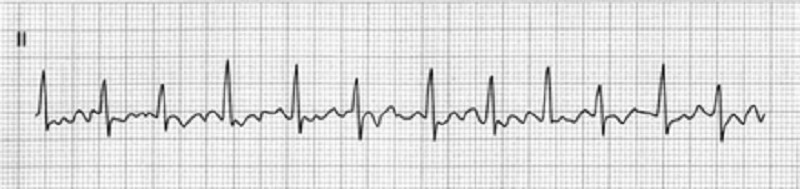
2) A 46-year-old man collapsed while getting out of his bed. He has been feeling weak over the last several days and has complained of vague chest discomfort. He ascribed the symptoms to a recent respiratory infection and did not visit a doctor. His mother died of a stroke and his father suffered from recurrent myocardial infarctions. He eats a balanced diet and takes a multivitamin daily. His most recent blood cholesterol level was 200 mg/dl. An ECG strip taken by EMS is shown below. Which of the following is the best initial management of this patient?
. Synchronized DC cardioversion
. Thrombolytic therapy
. Procainamide
. Beta-blockers and aspirin
. Pericardiocentesis
3) A 67-year-old Caucasian male is hospitalized in the intensive care unit (ICU) with an episode of prolonged hypotension and shortness of breath. His skin is cold and clammy. Intra-arterial blood pressure monitoring is established, and pulmonary artery catheterization is performed to control basic hemodynamic parameters. His blood pressure is 70/40 mmHg, and heart rate is 100/min. Cardiac output (CO) measured by thermodilution method is 2.3 L/min. Pulmonary capillary wedge pressure (PCWP) is estimated to be 22 mmHg. Systemic vascular resistance (SVR) calculated using data on mean arterial pressure, right atrial pressure and cardiac output is 2000 dynes*s/cm5 (N= 700 -1200 dynes*s/cm5). Which of the following is the most likely underlying problem in this patient?
. Cardiogenic shock
. Volume depletion
. Septic shock
. Volume overload
. Right ventricular infarction
4) A 59-year-old man comes to visit his friend in the hospital and collapses in the parking lot. He had been feeling unwell all day due to vague chest discomfort. A bystander witnesses his collapse, finds no pulse, and immediately calls for help. Which of the following is the most important factor for survival in this patient?
. Time to chest compressions
. Time to defibrillation
. Time to endotracheal intubation
. Time to epinephrine injection
. Time to cardiac catheterization lab
5) A 59-year-old male presents to the ER with sudden onset severe chest pain associated with vomiting and diaphoresis. The pain radiates to the left shoulder and is not relieved by sublingual nitroglycerine. His past medical history is significant for diabetes mellitus for seven years and hypercholesterolemia for six years. His medications include metformin, glipizide and simvastatin. On physical examination, his blood pressure is 150/98 mmHg and pulse is 86/min. An EKG obtained in the ER shows ST segment elevations in leads aVL and I. Cardiac troponin and CK-MB are elevated. Which of the following medications should be avoided in this patient at this time?
. Heparin
. Captopril
. Nifedipine
. Metoprolol
. Aspirin

6) A 69-year-old male undergoes coronary artery bypass and aortic valve replacement surgery. The procedure goes well, and he is extubated and discharged to the step-down unit on postoperative day 2. That night, he complains of weakness, chest tightness and shortness of breath. His blood pressure is 70/30 mmHg, respiratory rate is 26/min, and heart rate is 148 beats per minute. Lung auscultation reveals bibasilar crackles. An EKG rhythm strip is obtained. Which of the following is the best next step in the management of this patient?
. Amiodarone
. DC cardioversion
. Transcutaneous pacing
. Lidocaine
. Digoxin

7) A 66-year-old male is rushed to the emergency department because he feels dizzy and light-headed. He denies chest pain or palpitations. He has a history of hypertension and diabetes. His blood pressure is 116/62 mmHg and his pulse is 35-40/min. He is alert, awake, and fully oriented. He is breathing comfortably and does not appear to be in any distress. His extremities are slightly cold and capillary refill is 3 seconds. His EKG is shown below. Which of the following is the most appropriate next step in management?
. Intravenous adenosine push
. Intravenous atropine
. Intravenous epinephrine
. Intravenous amiodarone
. Transcutaneous pacing
8) A 68-year-old male was intubated in the emergency room because of pulmonary edema. Stat echocardiogram reveals an ejection fraction of 45% and severe mitral regurgitation. In spite of aggressive diuresis with furosemide, the patient continues to require mechanical ventilation secondary to pulmonary edema. What is the best next step in treating this patient?
. Arrange for mitral valve replacement surgery
. Place an intra-aortic balloon pump
. Begin metoprolol
. Begin a second loop diuretic
. Begin intravenous enalapril
9) A 45-year-old male is brought to the ER with sudden onset palpitations and chest tightness. His past medical history is significant for hypertension, gout and diabetes mellitus. Cardiac monitoring shows atrial fibrillation at a rate of 120-140/min. As the nurse is attempting to establish IV access, the patient becomes unresponsive. There is no palpable pulse over the carotids or femoral arteries. The cardiac monitor still shows atrial fibrillation at the same rate. What is the best next step in management?
. Synchronized cardioversion
. Defibrillation
.IV lidocaine
. Chest compressions
. Arterial blood gas analysis
10) A 64-year-old male presents to the emergency department with chest pain. An ECG reveals ST elevations in leads II, III, and aVF. Thrombolytic therapy and heparin are administered, and the pain resolves. Eight hours after admission, the patient develops hypotension. He denies recurrence of chest pain. His temperature is 37.5°C (99.6°F), blood pressure is 84/55 mm Hg, pulse is 90/min, and respirations are 15/min. His medications include a nitroglycerin drip, beta-blocker, aspirin, heparin, and simvastatin. Examination reveals an elevated jugular venous pressure of 14 cm, cold clammy extremities, and clear lung fields. Based on this information, what is the next best step in this patient's management?
. Start dopamine
. Administer normal saline bolus and stop nitroglycerin
. Administer intravenous furosemide
. Initiate temporary cardiac pacing
. Stop nitroglycerin and start dobutamine drip
11) Neighbors find a 65-year-old male unconscious in his garden and immediately call EMS. The man is intubated at the scene. In the ER, he develops sustained ventricular tachycardia and requires cardioversion. He is started on an antiarrhythmic agent and, once recovered, is discharged to home. Three months later he returns to his physician complaining of dyspnea on exertion. Chest x-ray reveals bilateral lung fibrosis. All cultures are negative and lung biopsy reveals lipoid pneumonitis. Which of the following medications is most likely responsible for his current condition?
. Procainamide
. Amiodarone
. Lidocaine
. Quinidine
. Digoxin
12) A 36-year-old female presents to the emergency room complaining of chest pain that started suddenly while she was shopping at the mall. She also reports shortness of breath, palpitations and diaphoresis. The pain is retrosternal and radiates to the left arm. There are no aggravating or relieving factors. On review of systems, the patient reports having had a runny nose, sore throat and dry cough for the past 3 days. Her past medical history is significant for panic attacks, for which she takes paroxetine, and dysfunctional uterine bleeding, for which she takes estrogen. Her family history is significant for the sudden death of her father at age 44 from a heart attack. Social history reveals that she has smoked one pack of cigarettes per day for the past 15 years. Which of the following is the most appropriate initial therapy for this patient?
. Lorazepam
. Heparin
. Aspirin
. Ibuprofen
. Acetaminophen
13) A 21-year-old man comes to the ER with palpitations and dizziness that began suddenly one hour ago. He notes having similar past episodes provoked by fatigue or strong emotions. He says he can usually stop the episodes by putting his head into cold water or squatting and taking a deep breath. However, these techniques are not working this time. Presently, his blood pressure is 60/30 mmHg and his heart rate is 240/min. He is diaphoretic with cold extremities. An EKG rhythm strip shows a regular, narrow complex tachycardia. Which of the following is the best next step in managing his condition?
. Adenosine
. Procainamide
. Verapamil
. Digoxin
. DC cardioversion
14) A 64-year-old Caucasian male presents to the Emergency Room with a sharp, left-sided chest pain. He says that the pain is worse when he takes deep breaths, but he gets relief with leaning forward. He had an acute non-ST elevation myocardial infarction six months ago and had undergone angioplasty for the right coronary artery. His other medical problems include: diabetes, hypertension, hyperlipidemia, peripheral neuropathy, diabetic retinopathy, paroxysmal atrial fibrillation, hypothyroidism, and chronic renal insufficiency. His vital signs are BP 142/86 mmHg, PR 78/min, RR 16/min, and T 36.1°C (97°F). On examination, you find a pericardial rub. EKG shows diffuse ST elevation. Lab results are: Hb 9.0 g/dl, WBC 8,000/cmm, Platelets 210,000/cmm, Blood Glucose 248 mg/dl, Serum Na 135 mEq/L, Serum K 5.8 mEq/L, Bicarbonate 17 mEq/L, BUN 86 mg/dl, Serum Creatinine 4.4 mg/dl. Which of the following is the most appropriate management of this patient?
. NSAIDs
. Corticosteroids
. Pericardiocentesis
. Hemodialysis
. Echocardiography
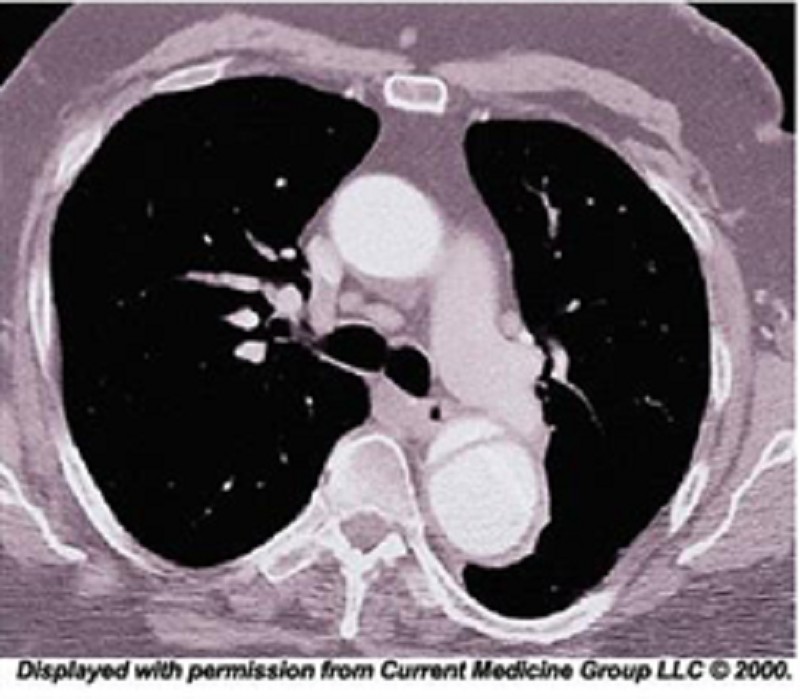
15) A 48-year-old African American man presents to the emergency room with severe retrosternal chest pain. His temperature is 36.7°C (98°F), blood pressure is 190/ 100 mmHg, pulse is 100/min, and respirations are 16/min. On physical examination, his lungs are clear to auscultation and his heart sounds are normal. EKG shows evidence of left ventricular hypertrophy. A CT image of his chest is shown below. Which of the following is the most appropriate immediate pharmacotherapy for this patient?
. Labetalol
. Nifedipine
. Heparin
. Hydrochlorothiazide
. Hydralazine
16) A 64-year-old male is admitted in ICU for acute myocardial infarction. He is on metoprolol, lisinopril, aspirin, furosemide, and potassium supplements. All of a sudden, the nurse mentions that the patient has a change in his tele monitoring. His blood pressure is 120/60 mmHg. His potassium level is 4.2. He is alert, awake and oriented time, place and person. Examination shows scattered bilateral crackles, peripheral pedal edema and elevated JVI. Which of the following is the next best step in the management of this patient?
. IV amiodarone
. IV digoxin
. Cardioversion
. IV diltiazem
. Carotid massage
17) A 56-year-old man presents to the emergency department with dyspnea. He describes waking up during the night with difficulty breathing and chest pain that kept him from falling back to sleep. He has never had these symptoms before. His past medical history is significant for long-standing hypertension and non-compliance with his antihypertensive therapy. He has smoked a pack of cigarettes per day for the past 30 years. On physical examination, his blood pressure is 170/100 mmHg and his heart rate is 120/min and regular. Lung auscultation reveals bibasilar rales and scattered wheezes. Which of the following is most likely to relieve this patient's dyspnea?
. Metoprolol
. Hydralazine
. Nitroglycerin
. Dopamine
. Amiodarone
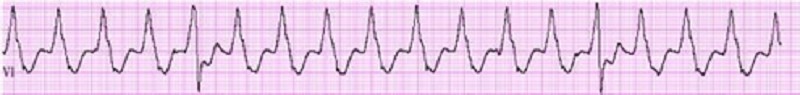
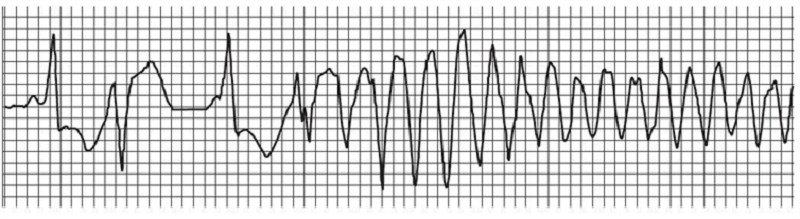
18) A 70-year-old male with a history of mild chronic kidney disease, diabetes mellitus, and CHF is admitted to your inpatient service with decreased urine output, weakness, and shortness of breath. He takes several medications but cannot remember their names. Labs are pending; his ECG is shown below. Based on the information available, what is the best initial step in management?
. Administration of intravenous insulin
. Administration of intravenous sodium bicarbonate
. Administration of intravenous 3% hypertonic saline
. Administration of oral sodium polystyrene sulfonate
Administration of intravenous calcium gluconate
19) A 51-year-old man with a long history of hypertension presents to the ED complaining of intermittent chest palpitations lasting for a week. He denies chest pain, shortness of breath, nausea, and vomiting. He recalls feeling similar episodes of palpitations a few months ago but they resolved. His blood pressure (BP) is 130/75 mmHg, heart rate (HR) is 130 beats per minute, respiratory rate (RR) is 16 breaths per minute, and oxygen saturation is 99% on room air. An ECG is seen below. Which of the following is the most appropriate next step in management?
. Sedate patient for immediate synchronized cardioversion with 100 J
. Prepare patient for the cardiac catheterization laboratory
. Administer warfarin
. Administer amiodarone
. Administer diltiazem
20) An 82-year-old white female is admitted to the hospital for observation after presenting to the emergency department with dizziness. After being placed on a cardiac monitor in the ER, the rhythm strip below was recorded. There is no past history of cardiac disease, diabetes, or hypertension. With prompting, the patient discloses several prior episodes of transient dizziness and one episode of brief syncope in the past. Physical examination is unremarkable. Which of the following is the best plan of care?
. Reassurance. This is a benign condition, and no direct therapy is needed
. Reassurance. The patient may not drive until she is symptom free, but otherwise no direct therapy is needed
. Nuclear cardiac stress testing; treatment depending on results
. Begin therapy with aspirin
. Arrange placement of a permanent pacemaker
21) A 48-year-old man presents to the emergency department complaining of crushing substernal chest pain. He is diaphoretic, anxious, and dyspneic. His pulse is 110/min, blood pressure is 175/112 mmHg, respiratory rate is 30/min, and oxygen saturation is 94%. Aspirin, oxygen, sublingual nitroglycerin, and morphine are given, but they do not relieve his pain. ECG shows ST-segment elevation in leads V2 to V4. The duration of symptoms is now approximately 30 minutes. What is the most appropriate treatment for this patient at this time?
Calcium channel blocker
Intravenous angiotensin-converting enzyme inhibitor
Intravenous β-blocker
Magnesium sulfate
Tissue plasminogen activator
22) A 70-year-old woman presents to the emergency department complaining of dizziness. She is disoriented to the date and her location and it is difficult to gather an accurate history. Her pulse is 48/min, blood pressure is 84/60 mmHg, and respiratory rate is 12/min. On examination her extremities are cool and clammy. Her capillary refill time is 5 seconds. What is the most appropriate therapy?
Adenosine
Amiodaron
Atropine
Isoprotereno
Metoprolol
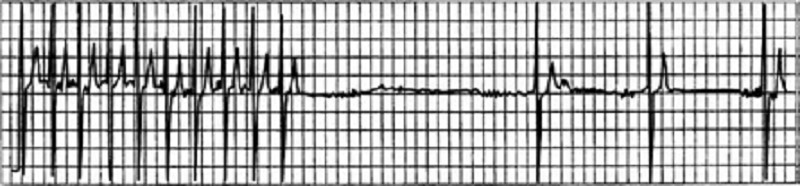
23) A 64-year-old man in the surgical intensive care unit goes into rapid atrial fibrillation on postoperative day one after a decortication for a loculated pulmonary empyema. He is given an appropriate loading dose of digoxin, but 4 hours after his second dose, the patient complains of increased palpitations and dizziness. The patient is conscious and hemodynamically stable. STAT serum blood tests show a potassium level of 5.0 mEq/L; all other electrolytes, including divalents, are in the normal range. The digitalis level is above the therapeutic range at 4 ng/mL (therapeutic range 0.5-2 ng/mL). Results of cardiac telemetry are shown in the image. Which of the following should be administered immediately?
Calcium
Magnesium
Furosemide
Potassium
Sodium polystyrene sulfonate
24) A 49-year-old man presents to the clinic for a health maintenance visit. He has no complaints, but he requests a prescription for his “pressure pills,” as he lost his original prescription. On physical examination his blood pressure is 220/130 mmHg. Physical examination is otherwise within normal limits. Laboratory tests show: Na+: 142 mEq/L, K+: 3.8 mEq/L, Cl−: 105 mEq/L, Carbon dioxide: 25 mEq/L, Blood urea nitrogen: 20 mg/dL, Creatinine: 1.0 mg/dL, Glucose: 133 mg/dL. Urinalysis is within normal limits, and his ECG is normal. Which of the following is the most effective management?
Administer intravenous nitroprusside for management of hypertensive emergency
Administer intravenous nitroprusside for management of hypertensive urgency
Administer oral furosemide for management of hypertensive emergency
Administer oral metoprolol for management of hypertensive urgency
Administer sublingual nifedipine for management of hypertensive emergency
25) A 65-year-old man presents to the emergency department following the acute onset of palpitations. His wife states that he was eating dinner when he noticed the palpitations, lightheadedness, and shortness of breath. The patient has a history of treated hypertension, but no other medical history. The patient is not able to relate any meaningful history. Blood pressure is 80/40 mmHg, heart rate is 126/ min, respiratory rate is 20/min, and oxygen saturation is 99% on room air; he is afebrile. His heart rate is irregularly irregular with no murmurs, clicks, or rubs. Respiratory examination is unremarkable. X-ray of the chest shows no acute disease. ECG shows no discernible P waves and an irregularly spaced QRS response. Which of the following is the best first step in management?
Administration of adenosine
Cardiac catheterization and stent placement
Cardioversion to sinus rhythm
Carotid massage
Placement of dual lead pacemaker
{"name":"Part 36", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your understanding of various medical conditions, diagnoses, and management strategies with our comprehensive quiz. This engaging quiz features carefully curated questions suitable for both medical students and professionals looking to refresh their knowledge.Prepare to answer questions on:DiagnosticsJoint and Muscle DisordersInfectious DiseasesRheumatologyClinical Presentations","img":"https:/images/course5.png"}
More Quizzes
Can you Solve this case?
520
M&P
351858
Pediatric nurse
320
Circles Concept
630
Ultimate Microbiology: Do You Know Cell Water Content?
201058544
Free Non Contact Forces Unit Test
201027792
Free HSPT & SHSAT Math Practice Tests
201021733
Naruto German Intro: Test Basic Conversation Skills
201028679
Which Light Skin Cute Guy Matches Your Personality?
201027237
Computer Methods
15831809
Test Your Geometry Skills: Ultimate Quadrilateral
201028376
Can You Ace This Hard TV Dads Trivia - Cartoon Dad?
201032208