Part 30 (89-177)

Clinical Knowledge Challenge
Test your medical knowledge with our comprehensive quiz designed for healthcare professionals and students alike. With 88 challenging questions covering a wide range of topics, you'll have the opportunity to deepen your understanding of clinical scenarios and improve your diagnostic skills.
Key Features:
- Covering diverse topics from pediatrics to geriatrics
- Designed for both learning and assessment
- Perfect for medical students, residents, and practicing clinicians
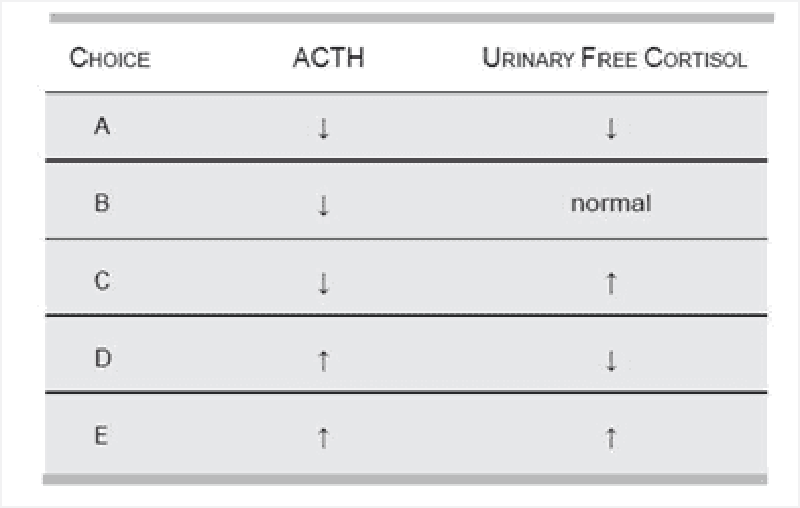
89) A 14-year-old boy presents at the pediatric clinic for a routine check-up. The patient had developed end-stage renal disease over the previous 2 years, and was successfully treated with a renal transplant 6 months prior. Since his operation, he has developed purple striae on his back and arms, central obesity, and an increasingly round face. During the subsequent blood analysis, which of the following results would be most likely?
A
D
B
E
C
90) A 64-year-old man presents to the emergency department after a motor vehicle crash and receives a CT of the abdomen that shows a finding of a unilateral mass in the left adrenal gland. He is unharmed from the accident, feels well, and has never smoked. His blood pressure is 155/90 mmHg, deep tendon reflexes are 3/4, and muscle strength is 4/5. Laboratory studies show: Na+: 150 mEq/L, K+: 3.0 mEq/L, Cl−: 105 mEq/L, HCO −: 36 mEq/L. Plasma renin activity is also decreased. Which of the following is most likely to be increased?
Aldosterone
Troponin
Anion gap
Carcinoembryonic antigen
Prostate-specific antigen
91) A 19-year-old man with insulin-dependent diabetes mellitus is taking 30 units of NPH insulin each morning and 15 units at night. Because of persistent morning glycosuria with some ketonuria, the evening dose is increased to 20 units. This worsens the morning glycosuria, and now moderate ketones are noted in urine. The patient complains of sweats and headaches at night. Which of the following is the most appropriate next step in management?
Measure blood glucose levels at bedtime
Add lispro via a calculated scale to each meal; continue NPH
Increase the evening dose of NPH insulin further
Add regular insulin to NPH at a ratio of 2/3 NPH to 1/3 regular
Obtain blood sugar levels between 2:00 and 5:00 AM
92) A 48-year-old high school teacher with no prior medical history presents to his primary care physician after feeling extremely fatigued for > 1 month. Previously an avid runner, he has recently experienced dyspnea on moderate exertion. Although he denies vomiting, he admits to intermittent episodes of diarrhea. His blood pressure is 73/37 mmHg and he is afebrile. On physical examination his skin is warm and erythematous, and his jugular venous pressure is elevated. Cardiac examination reveals a systolic murmur near the right border of the sternum that is accentuated with inspiration. Which of the following is most consistent with these findings?
Elevated urinary excretion of 5-hydroxyin- doleacetic acid
Peaked T waves on ECG
Elevated urinary excretion of vanillylman- delic acid
Pseudomonas species grown from blood cultures
Severe pulmonary congestion on x-ray of the chest
93) A 3010-g (6.6-lb) boy was born to a 37-year-old primagravida by spontaneous vaginal delivery after an uncomplicated pregnancy. On examination he has cyanotic extremities and a significant right precordial heave, a single S2, and a harsh systolic ejection murmur along the sternal border. He also has a prominent squared nose and cleft palate. An echocardiogram is subsequently performed and demonstrates tetralogy of Fallot. Corrective surgery is performed without complications. At 2 months of age the infant is diagnosed with Pneumocystis jiroveci pneumonia, and at 3 months he is diagnosed with fungal septicemia. Additional work-up of this child should include which of the following tests?
Hemoglobin electrophoresis
Serum calcium
Nitroblue tetrazolium
Quantitative immunoglobulin levels
Renal ultrasound
94) A 50-year-old female is evaluated for hypertension. Her blood pressure is 130/98 mmHg. She complains of polyuria and mild muscle weakness. She is on no blood pressure medication. On physical examination, the PMI is displaced to the sixth intercostal space. There is no sign of congestive heart failure and no edema. Laboratory values are as follows: Na+: 147 mEq/dL, K +: 2.3 mEq/dL, Cl−: 112 mEq/dL, HCO3: 27 mEq/dL. The patient denies the use of diuretics or over-the-counter agents to decrease fluid retention or promote weight loss. She does not eat licorice. Which of the following tests is most useful in establishing a diagnosis?
24-hour urine for cortisol
Ratio of serum aldosterone to plasma renin activity
Urinary metanephrine
Plasma renin activity
Renal angiogram
95) A 36-year-old female complains of inability to lose weight despite low-calorie diet and daily exercise. She has also noticed that she is cold intolerant. She is wearing a jacket even though it is summer. She also reports constipation and hair loss. These symptoms have been worsening over the past 2 to 3 months. An elevated TSH and low total and free T4 confirm your suspicion of hypothyroidism. You suspect the etiology of this patient’s hypothyroidism to be autoimmune thyroiditis. What is the best test to confirm the diagnosis of autoimmune thyroiditis?
Thyroid peroxidase antibody (TPOAb)
Thyroid aspiration
Antinuclear antibody
24-hour radioactive iodine uptake
Thyroid ultrasound
96) A 72-year-old man with end stage renal disease secondary to hypertension presents with several months of back pain. He denies fever, weight loss, difficulty walking, altered sensation in his legs, or incontinence. He was diagnosed with renal disease 20 years ago and was managed medically for many years. However, 2 years ago he began hemodialysis because of a progressive decline in renal function. There is no family history of renal disease or malignancy. Physical examination is unremarkable. X-ray of the chest shows ill-defined bands of increased bone density adjacent to the vertebral endplates. What laboratory abnormalities is most likely in this patient?
Bence-Jones protein in urine
Elevated parathyroid hormone
Decreased parathyroid hormone
Decreased phosphate
Elevated bone-specific alkaline phosphatase
97) An 82-year-old woman presents 1-hour after the sudden onset of moderate-to-severe epigastric pain. The pain radiates to her back, both scapulae, and both arms. She has been nauseated and vomited three times in the past hour. Her past medical history is remarkable for peptic ulcer disease 10-years ago, cholelithiasis for the past 6-years, and stable angina pectoris for the past 3-years. She has had occasional episodes of biliary colic and two bouts of acute cholecystitis which were treated conservatively. Her temperature is 36.8°C (98.2°F), blood pressure is 120/70 mmHg, pulse is 90/min, and respirations are 14/min. The lungs are clear to auscultation. Abdominal examination shows a soft abdomen with mild tenderness to palpation in the epigastrium. Murphy's sign is negative. Which of the following studies should be done first?
Abdominal ultrasound
Serum amylase and lipase
Upper GI endoscopy
Electrocardiogram
Upright abdominal x-ray
98) A 65-year-old woman presents with a 2-month history of fatigue and dyspnea on exertion. She takes no medication. Her temperature is 36.7°C (98°F), blood pressure is 162/83 mmHg, pulse is 100/min, and respirations are 21/min. Auscultation shows a 2/6 systolic murmur in the 2nd right intercostal space. No peripheral edema is noted. Rectal examination shows no abnormalities. Test of the stool for occult blood is negative. EKG shows sinus tachycardia and non-specific ST-T changes. Laboratory studies show: Hemoglobin 8.1 g/L, MCV 73 fl, Platelets 360,000/mm3, Leukocyte count 4,500/mm3, Neutrophils 56%, Eosinophils 1%, Lymphocytes 33%, Monocytes 10%. Which of the following is the most appropriate next step in management?
Echocardiography
Isotope-labeled erythrocytes scintigraphy
Bone marrow biopsy
Gastro-duodenoscopy
Colonoscopy
99) A 45-year-old Mexican male presents with a 2-day history of traces of blood on the tissue paper after he wipes. He does not have gross blood mixed with stool, but on one occasion there were drops of blood in the toilet after defecation. He has no past medical history or family history of cancer or other significant disease. Which of the following is the most appropriate next step in management?
Colonoscopy
Barium enema
Fecal occult blood test
Anoscopy
Sigmoidoscopy
100) A 26-year-old man presents with a 1-week history of intermittent, crampy, lower abdominal pain accompanied by rectal urgency, bloody diarrhea, nausea and vomiting. His symptoms have become more severe over the past 24 hours. His past medical history is unremarkable. He denies any recent travel or antibiotic use. His temperature is 38.5°C (102.0°F), blood pressure is 120/80 mmHg, pulse is 95/min, and respirations are 15/min. Abdominal examination reveals distension and tenderness to palpation without rebound or guarding. The bowel sounds are decreased. Rectal examination shows marked rectal tenderness and mucus mixed with blood in the vault. An x-ray film of the abdomen shows distended colon filled with gas. Laboratory studies show: Hb 10.8 g/dl, WBC 19,600/cmm, Platelet count 459,000/cmm, ESR 54/hr. Which of the following is the most appropriate next step in management?
Stool for ova, parasites and culture
CT scan of the abdomen
Barium enema
Proctosigmoidoscopy and biopsy
Serology for Entamoeba histolytica
101) A 34-year-old woman complains of occasional diarrhea and crampy lower abdominal pain. She says that at times her symptoms hamper her performance in important business meetings. The pain sometimes occurs after meals but is not always preceded by eating. The pain is often accompanied by diarrhea with small amounts of stool and mucus. Her past medical history is significant for bleeding hemorrhoids. Her mother died of colon cancer. Which of the following findings is most likely in this patient?
Normal colonic mucosa
Intestinal villous atrophy
Crypt abscesses
Folic acid deficiency
Duodenal ulcer
102) A 40-year-old female presents with abdominal discomfort. The discomfort is localized to the center of the upper abdomen and is not related to meals or fatty food. She has a history of similar symptoms. She has not had gastrointestinal bleeding, fatigue, dysphagia, or weight loss. Her mother has a history of gastric ulcer. Her vital signs are within normal limits. Complete physical examination is unremarkable. Stool for heme occult is negative. Complete blood count and serum chemistries are within normal limits. Which of the following is the most appropriate next step in management?
Barium swallow
Empirical antibiotic trial
Endoscopy
Empiric trial of H2 blockers
H. Pylori breathe test
103) A 30-year-old woman presents with a 5-month history of episodic retrosternal pain that radiates to the interscapular region. The pain episodes typically last 15 minutes, and are precipitated by emotional stress and hot or cold food. Her relative gave her sublingual nitroglycerine tablets, which alleviated the pain. Her past medical history is unremarkable, and she does not take any other medications. There is no family history of coronary artery disease. Her vital signs are within normal limits. Physical examination shows no abnormalities. A lipid profile is within normal limits. An EKG shows a normal sinus rhythm. A stress test fails to reproduce the symptoms or to induce ST/T wave changes. Chest x-ray, upper GI endoscopy, and echocardiography show no abnormalities. Which of the following is the most appropriate next step in diagnosis?
CT scan of the chest with contrast
Acid perfusion (Bernstein) test
Esophageal motility studies (manometric recordings)
Coronary angiogram
Pulmonary perfusion/ventilation scintigraphy
104) A 45-year-old male comes to the physician for epigastric pain and diarrhea. His past medical history is significant for chronic duodenal ulcers. He has been smoking 2 packs of cigarettes daily for the past 10 years. He occasionally drinks alcohol. He denies illegal drug use or multiple sexual partners. Physical examination shows abdominal tenderness without rebound or rigidity. Endoscopy shows prominent gastric folds, chronic duodenal ulcer, and upper jejunal ulceration. Which of the following is the most appropriate next step in the diagnosis of this patient?
Secretin stimulation test
Serum gastrin concentration
Gastric acid secretion study
Serum chromogranin A
Calcium infusion study
105) A 32-year-old female from South America presents with a 3-month history of progressive difficulty with swallowing for both liquids and solids. At night she has a bitter taste in her mouth. Over the past two months, she has had a 10 lb (4.54 kg) weight loss. She has not had any previous illnesses, and does not take any medication. Physical examination is unremarkable. A lateral x-ray film of the chest shows extreme dilatation of the esophagus with an air fluid level. Which of the following is the diagnostic test for this patient's condition?
Barium swallow
CTscan
Endoscopy
PH monitoring
Manometry
106) A 50-year-old man presents with a 3-hour history of right arm pain. Two weeks ago, he was treated for superficial thrombophlebitis of the right cephalic and right saphenous veins. For the past two months, he has had significant back pain, which is being treated with NSAIDs. His temperature is 37.0°C (98.6°F), blood pressure is 140/80 mmHg, pulse is 70/min, and respirations are 10/min. Physical examination shows a swollen, ruddy and warm right arm, but is otherwise unremarkable. Cervical and chest x-ray films show no abnormalities. Laboratory studies show: Hct 50%, Platelets 120,000/cmm, WBC 9,600/cmm, Neutrophils 60%, Eosinophils 2%, Basophils 0%, Lymphocytes 31%, Monocytes 7%, PT 25 sec, PTT 39 sec, Fibrinogen 300 mg/dL, Fibrin split products positive. Which of the following is the most appropriate next step in management?
Protein C, S and antithrombin III levels
Perfusion scintigraphy of the lungs
Venography of right brachial, axillary and subclavian veins
CT of the chest abdomen and pelvis
CT of the thoracic outlet
107) A 45-year-old Asian-American female comes to the physician due to bloating, flatulence, abdominal cramps and explosive watery diarrhea. These symptoms occur after ingesting dairy products. She has not had any weight loss. She has not had bone pain or easy bruising. Physical examination shows abdominal distention and borborygmi. You decide to investigate the patient further. Which of the following test results is most likely to be observed
Positive urine test for reducing substances
Positive acid steatocrit test
Decreased stool osmotic gap
Positive hydrogen breath test
Alkaline stool pH
108) A 50-year-old male undergoes vagotomy and pyloroplasty for a peptic ulcer perforation. His early postoperative course is complicated by fever and hypotension, which are treated with broad-spectrum antibiotics and IV fluid support. He then recovers well; however, on post-operative day 6 he develops nausea, vomiting, abdominal pain, and profuse, watery diarrhea. His temperature is 38.9°C (102° F), blood pressure is 110/70 mmHg, pulse is 120/min, and respirations are 18/min. Abdominal examination shows tenderness in the sigmoidal area. Test of the stool for occult blood is negative. Laboratory studies show: Hb 11.5g/dL, Platelet count 180, 000/cmm, Leukocyte count 17, 500/cmm, segmented neutrophils 75%, Bands 10%, Eosinophils 1%, Lymphocytes 14%. Which of the following is the most appropriate next step in management?
Blood cultures
Colonoscopy
Stool cultures
Cytotoxin assay in the stool
Observation
109) A 68-year-old woman with a history of heavy alcohol use and chronic pancreatitis presents with a several month history of recurrent epigastric pain. The pain is occasionally associated with nausea and vomiting. She has lost 15 lbs (6.8 kg) over the past 3 months. She is afebrile. Physical examination shows scleral icterus. Laboratory studies show: Albumin 3.0 mgldl, Total bilirubin 3.5 mgldl, Direct bilirubin 24 mgldl, Alkaline phosphatase 220 U/L, Aspartate aminotransferase (SGOT) 28 U/L, Alanine aminotransferase (SGPT) 25 U/L, Amylase 145 U/L, Lipase 100 U/L. Which of the following is the most appropriate next step in management?
ERCP
Upper GI endoscopy
CT scan of the abdomen
MRI of the abdomen
Plain abdominal radiography
110) A 56-year-old man comes to the emergency department due to a one day history of abdominal pain and increasing distension. He has not passed flatus during this time. He has had nausea without vomiting. He has a history of cirrhosis secondary to chronic alcoholism. He is taking spironolactone and furosemide. His temperature is 38.0°C (101.3°F), blood pressure is 120/70 mm Hg, pulse is 100/min, and respirations are 24/min. Physical examination shows a slightly confused man with a flapping tremor. Breathing is labored and lungs are clear to auscultation. Abdominal examination shows distension, tenderness to palpation with rebound, and no guarding; a fluctuating wave and shifting dullness are present. Abdominal auscultation shows splashing and markedly decreased bowel sounds. An x-ray film of the chest shows no abnormalities. An x-ray film of the abdomen shows gas in the small and large bowels without air-fluid levels. Which of the following is the most appropriate next step in management?
Barium enema
Diagnostic paracentesis
Sigmoidoscopy
Ultrasound of abdomen
Diagnostic peritoneal lavage
111) A 42-year-old male presents with a 2-year history of heartburn. The heartburn occurs after heavy meals and while supine. Over time, his symptoms have been increasing in severity and frequency. His symptoms used to be alleviated with the use of over-the-counter antacids, but these have become ineffective in the past two months. He also complains of epigastric pain and occasional vomiting, both of recent onset, especially in the morning. He denies dysphagia or odynophagia. He eats junk food and drinks two cups of coffee daily. He regularly drinks grape brandy and smokes 1 pack of cigarettes/day. Abdominal examination shows epigastric tenderness. Abdominal ultrasound is unremarkable. Test of the stool for occult blood is negative. Which of the following is the most appropriate next step in management?
Treatment with ranitidine
Reassurance
Upper GI endoscopy
Barium swallow
Manometric studies
112) A 66-year-old man returns to the emergency department (ED) for a second time because of persistent left lower quadrant pain and developing fever, despite 48 hours of oral antibiotics. He had presented to the ED 2 days ago because of left lower quadrant pain. He was able to tolerate a diet and had no fever; he was then sent home on antibiotics, and instructed to return if there was no improvement. He has a 2-week history of constipation without regular bowel movements. Laxatives have not relieved his symptoms. His diet consists of meat with very few vegetables. His vital signs are within normal limits, except for a low-grade fever. Abdominal examination shows left lower quadrant tenderness and guarding. Rectal examination shows no abnormalities. Laboratory studies show a WBC of 16,400/cmm. He is admitted and started on IV antibiotics. Forty-eight hours later, his symptoms persist without any improvement. Which of the following is the most appropriate next step in management?
Abdominal x-rays
Barium enema
Flexible sigmoidoscopy
Colonoscopy
CT scan
113) A 58-year-old woman presents to the emergency department with right subcostal heaviness, intermittent pain, food intolerance, and 13.2 lbs-weight loss (6kg) over the past 2 months. Her pain has been worsening for the past 2 days; it was initially localized to the right upper quadrant, but has now shifted to her back. Her past medical history is remarkable for appendicitis, which was complicated by perforation and peritonitis 20 years ago. Abdominal examination shows epigastric tenderness. There is a palpable mass below the right costal margin. Murphy's sign is negative. Abdominal ultrasound shows an enlarged gallbladder and dilation of the hepatic ducts. Laboratory studies show: WBC 11,000/cmm, Total bilirubin 24 mg/dl, Direct bilirubin 1.6 mg/dl, Alkaline phosphatase 310 U/L, Aspartate aminotransferase (SGOT) 87 U/L, Alanine aminotransferase (SGPT) 56 U/L, Amylase 140 U/L. Which of the following is the most appropriate next step in management?
Plain abdominal film
CT scan of the abdomen
Endoscopic retrograde cholangiopancreatography
Percutaneous transhepatic cholangiography
HIDA scan for cystic duct obstruction
114) A 50-year-old white male presents with complaints of bitter taste and central chest pain. He further describes he pain as moderate-to-severe, occurring during or after meals, non-radiating, and burning. The pain is relieved with antacids, and worsened by lying supine. He has lost 10 lbs (4.5kg) over the past 5-months (unintentional). He has smoked 2 packs of cigarettes daily for 20 years. His vital signs are stable, and he is afebrile. The physical examination is unremarkable. Chest x-ray and EKG show no abnormalities. Which of the following is the most appropriate next step in management?
Treatment with antacids
Esophageal pH monitoring
Treatment with famotidine
Treatment with omeprazole
Esophagoscopy
115) A 63-year-old man presents with a 2-month history of dysphagia for both solids and liquids. He has had a 6.6 lb (3kg) weight loss over this time. His past medical history is remarkable for a transient ischemic attack 6 months ago, two bouts of pneumonia in the past 3 months, and chronic heartburn treated with over-the-counter antacids. Physical examination shows a supple neck without masses. Abdominal examination shows mild epigastric tenderness to deep palpation. Chest x-ray is normal for his age. Which of the following is the most appropriate next step in diagnosis?
Endoscopy
Motility studies
Barium swallow
Video fluoroscopy
24-hour pH monitoring
116) A 47 -year-old male comes to the emergency department complaining of an intense burning pain in his abdomen. The pain started a couple of hours ago and is getting worse. He also has nausea and vomited twice. The vomitus is described as dark red-brown in color. He drank "quite a bit of alcohol' last night. He has had several episodes of this type of pain before, and was diagnosed with peptic ulcer disease five years ago. Several courses of H. Pylori eradication therapy have been prescribed in the past, but the patient admits to being non-compliant. He admits to smoking and drinking heavily. His temperature is 36.8° C (98.2° F), blood pressure is 126/88 mm Hg, pulse is 98/min, and oxygen saturation is 96% on room air. The physical examination is remarkable for marked epigastric tenderness. No masses or rebound tenderness are appreciated. IV fluids are administered, blood tests are taken, and upper Gl endoscopy is being arranged. Which of the following serum markers is most likely to be elevated in this patient?
Platelet count
Creatinine
Blood urea nitrogen
Prothrombin time
Potassium
117) A 65-year-old Asian male presents to the physician with a four-week history of weakness and vague postprandial epigastric pain. His past medical history is insignificant. He does not take any medications. He smokes 1½packs of cigarettes daily and drinks alcohol occasionally. The fecal occult blood test is positive. Gastroduodenoscopy shows an antral ulcer. Four of seven biopsies taken from the margins of the ulcer are consistent with adenocarcinoma. Which of the following is the most appropriate next step in management
Helicobacter pylori testing
Exploratory laparotomy
Serologic markers
A CT scan
Laparoscopy
118) A 45-year-old male presents to the office with complaints of progressive difficulty in swallowing both solids and liquids. His other complaints include occasional regurgitation of undigested food, and a nighttime cough which disturbs his sleep. The physical examination is unremarkable. Barium studies show a dilated esophagus, loss of esophageal peristalsis, and smooth tapering of the distal esophagus. Which of the following is the most appropriate next step in management?
Esophagoscopy
Pneumatic dilation
Esophageal manometry
Esophageal pH monitoring
Botulinum toxin injection
119) A 76-year-old man with multi-infarct dementia is brought to the emergency department because of lethargy. For the past 6 months, he has had difficulties with feeding and occasionally regurgitates undigested food. In recent days, his condition has deteriorated, and he has become lethargic. He has a history of hypertension for 15 years, chronic atrial fibrillation for 7 years, dementia for 5 years, and frequent respiratory tract infections for the past year. His temperature is 37.8°C (101.5°F), blood pressure is 150/95 mm Hg, pulse is 120/min, and respirations are 26/min. Physical examination shows foul-smelling breath; there is a fluctuating mass in the left side of his neck. Auscultation shows crackles in the right lung base. An x-ray film of the chest shows multiple infiltrates without cavitation in the right lower lung field. The patient is admitted, sputum and blood cultures are sent, and antibiotics are started. Which of the following is the most appropriate next step in management?
Puncture of the neck mass
Esophagoscopy
Esophagography
Bronchoscopy
CT of the neck
120) A 69-year-old man has had pain in left lower quadrant (LLQ) for 3 days. The pain was intermittent, but since yesterday it has been constant. He also had sweating and chills for the last 2 days. He hasn't had a bowel movement for 4 days, but has passed flatus. He vomited once and still has nausea. His past medical history is remarkable for constipation and nephrolithiasis. His vital signs are: PR: 110/min; BP: 122/80mm Hg; RR: 24/min; Temperature: 38.6°C (101.3°F). His abdomen is soft and tender to palpation in the left lower quadrant. Deep palpation is difficult but reveals no masses or organomegaly. Bowel sounds are decreased. Rectal exam is positive for enlarged prostate. Costovertebral angle tenderness is absent. Ultrasound shows bilateral hydronephrosis and stones in the kidneys. His laboratory test results are: WBC 14,500/cmm, Hb 11.7gm/dl, Hct 34%, ESR 40/hour, BUN43 mg/dl, Creatinine 2.0 mg/dl. Urinalysis RBC 4-10/hpf; WBC 3/hpf; few hyaline casts; many oxalate crystals. The next step should be?
Intravenous pyelography
Upright abdominal film
Sigmoidoscopy
Contrast enema
CT of abdomen
121) A 46-year-old white male presents with chronic diarrhea, abdominal distention, flatulence, and weight loss. He also has arthralgias and bulky, frothy stools. He has never had blood transfusions, tattooing or highrisk sexual behaviors. His temperature is 38.3°C (101°F), blood pressure is 130/90 mm Hg, pulse is 84/min, and respirations are 16/min. Physical examination shows generalized lymphadenopathy and skin hyperpigmentation. Which of the following is the most appropriate diagnostic test?
Serum TSH
Endoscopy with small bowel biopsy
Antinuclear antibody (ANA) titer
Gamma-glutamyl transpeptidase levels
ELISA for anti-HIV antibodies
122) A 40-year-old male comes to the physician complaining of diarrhea with pale, voluminous, foul-smelling stools that are difficult to flush. He has had this problem sporadically for years, but has neglected medical care. He also has severe, intermittent, epigastric pain lasting 15 to 30 minutes after eating. He admits to chronic alcohol consumption. Physical examination shows no abnormalities. Which of the following is the best test to confirm fat malabsorption in this patient?
Sudan III stain
Lactose tolerance test
72-hour fecal fat collection
Acid steatocrit
D-xylose test
123) A 40-year-old man with long-standing alcohol abuse complains of abdominal swelling, which has been progressive over several months. He has a history of gastrointestinal bleeding. On physical examination, there are spider angiomas and palmar erythema. Abdominal collateral vessels are seen around the umbilicus. There is shifting dullness, and bulging flanks are noted. Which of the following is the most important first step in the patient’s evaluation?
Diagnostic paracentesis
Ethanol level
Upper GI series
CT scan of the abdomen
Examination of peripheral blood smear
124) A 70-year-old man presents with a complaint of fatigue. There is no history of alcohol abuse or liver disease; the patient is taking no medications. Scleral icterus is noted on physical examination; the liver and spleen are nonpalpable. The patient has a normocytic, normochromic anemia. Urinalysis shows bilirubinuria with absent urine urobilinogen. Serum bilirubin is 12 mg/dL, AST and ALT are normal, and alkaline phosphatase is 300 U/L (three times normal). Which of the following is the best next step in evaluation
Ultrasound or CT scan of the abdomen
Antimitochondrial antibodies
Viral hepatitis profile
Reticulocyte count
Serum ferritin
125) A 45-year-old woman presents with a 1-week history of jaundice, anorexia, and right upper quadrant discomfort. On examination she is icteric, with a tender right upper quadrant and liver span of 14 cm. There is no shifting dullness or pedal edema and the heart and lungs are normal. On further inquiry, she reports consuming one bottle of wine a day for the past 6 months. Which of the following laboratory tests are most likely to be characteristic of a patient with jaundice secondary to alcoholic hepatitis?
Ratio of AST: ALT is 3:1 and the AST is 500 U/L
Ratio of AST: ALT is 1:1 and the AST is 500 U/L
Ratio of AST: ALT is 2:1 and the AST is 250 U/L
Ratio of AST: ALT is 1:1 and the AST is 250 U/L
Ratio of AST: ALT is 1:3 and the AST is 750
126) A 60-year-old man with a history of alcohol abuse presents to the ED with hematemesis for 1 day. He denies abdominal or chest pain. On physical examination, his eyes appear reddened which he attributes to having drunken heavily the night before (he also reveals vomiting several times after this recent binge). Vital signs are HR 115 beats per minute, BP 130/85 mm Hg, RR 18 breaths per minute, and temperature 99.5°F. Chest radiograph is unremarkable. Laboratory results reveal a WBC 10,000/μL, haemoglobin 14 mg/dL, hematocrit 40%, and platelets 210/μL. Which diagnosis is endoscopic evaluation most likely to confirm?
Esophageal varices
Mallory-Weiss tear
Boerhaave syndrome
Curling ulcer
Perforated gastric ulcer
127) A 73-year-old man comes to his primary care physician for his yearly check-up. His medical history is significant for obesity, new onset diabetes mellitus, and a remote history of tobacco use. The patient has noticed that his stool has been darker for the past 3 months, although he has only seen gross blood in his stool once, a week ago. He also complains of recent fatigue and occasional light-headedness when standing up from sitting. On examination the patient has fecal occult blood and a hematocrit of 32%. Colonoscopy and upper gastrointestinal endoscopy reveal no obvious pathology. Which of the following is the best diagnostic test to locate this patient’s hemorrhage?
Angiography
Tagged RBC scan
Barium enema
Colonoscopy
CT scan with contrast
128) A 70-year-old woman with a history of hypertension, congestive heart failure, and atrial fibrillation presents to the ED with several hours of acute onset diffuse abdominal pain. She denies any nausea or vomiting. The pain is constant, but she is unable to localize it. She was diagnosed with a renal artery thrombosis several years ago. Vital signs include HR of 95 beats per minute, BP of 110/70 mm Hg, and temperature of 98°F. Her abdomen is soft and mildly tender, despite her reported severe abdominal pain. Her WBC count is 12,000/μL, hematocrit 38%, platelets 250/μL, and lactate 8 mg/dL. The stool is traced heme-positive. You are concerned for acute mesenteric ischemia. What is the best way to diagnose this condition?
Serum lactate levels
Barium contrast study
Abdominal radiograph (supine and upright)
CT scan
Angiography
129) As you palpate the right upper quadrant (RUQ) of a 38-year-old woman’s abdomen, you notice that she stops her inspiration for a brief moment. During the history, the patient states that over the last 2 days she gets pain in her RUQ that radiates to her back shortly after eating. Her vitals include a temperature of 100.4°F, HR of 95 beats per minute, BP of 130/75 mm Hg, and RR of 16 breaths per minute. What is the initial diagnostic modality of choice for this disorder?
Plain film radiograph
Ultrasonography
Computed tomography (CT) scan
Magnetic resonance imaging (MRI)
Radioisotope cholescintigraphy (HIDA scan)
130) A 23-year-old woman presents to the ED complaining of lower abdominal pain and vaginal spotting for 2 days. Her menstrual cycle is irregular. She has a history of ovarian cysts and is sexually active but always uses condoms. Her BP is 115/75 mm Hg, HR is 75 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. Which of the following tests should be obtained next?
Chlamydia antigen test
Observe her abdominal pain, if it resolves discharge her with a diagnosis of menstruation
β-Human chorionic gonadotropin (β-hCG)
Transvaginal ultrasound
Abdominal radiograph
131) For which of the following patients is an abdominal CT scan contraindicated?
A 52-year-old man with abdominal pain after blunt trauma, negative focused assessment with sonography for trauma (FAST) examination, BP 125/78 mm Hg, and HR 109 beats per minute
A 22-year-old woman with RLQ pain, negative β-hCG, temperature 100.6 F
A 45-year-old man with abdominal pain, temperature 100.5 F, WBC 11,200/μL, BP 110/70 mm Hg, HR 110 beats per minute, and lipase 250 IU
A 70-year-old man with abdominal pain, an 11-cm pulsatile mass in the epigastrium, BP of 70/50 mm Hg, and HR of 110 beats per minute
A 65-year-old woman with right flank pain that radiates to her groin, microhematuria, BP 165/85 mm Hg, and HR 105 beats per minute
132) A 59-year-old man presents for his routine colonoscopy and during his visit he has numerous large adenomas removed from his colon. Which of the following is the most effective strategy for follow-up of this patient?
Elective colectomy
Urgent colectomy
Repeat colonoscopy in 10 years
Repeat colonoscopy in 3 years
Sigmoidoscopy in 10 years
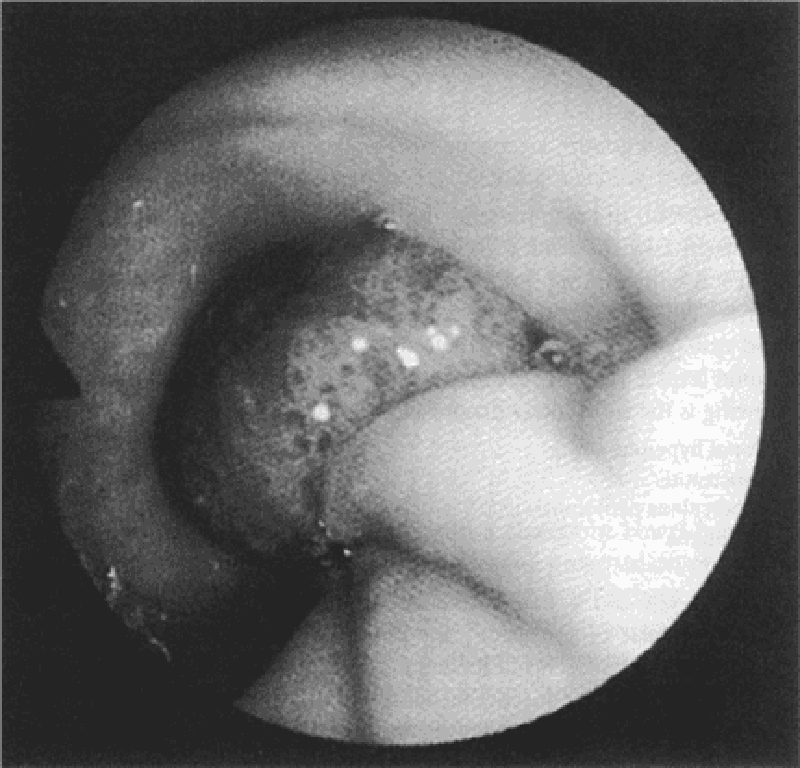
133) A 58-year-old white man complains of intermittent rectal bleeding and, at the time of colonoscopy, is found to have internal hemorrhoids and the lesion shown at the splenic flexure. Pathology shows tubulovillous changes. Repeat colonoscopy should be recommended at what interval?
In 1 to 2 months
Repeat colonoscopy is not necessary
In 1 year
In 3 years
In 10 years
134) A 68-year-old man presents to the ED 4 hours after an upper endoscopy was performed for 5 months of progressive dysphagia. During the procedure, a 1-cm ulcerated lesion was found and biopsied. Now, the patient complains of severe neck and chest pain. His vitals are as follows: BP 135/80 mm Hg, HR 123 beats per minute, RR 26 breaths per minute, and temperature 101°F. On physical examination, he appears diaphoretic and in moderate distress with crepitus in the neck and a crunching sound over the heart. You obtain an electrocardiogram (ECG), which is notable for sinus tachycardia. After obtaining a surgical consult, which of the following is the next best step in management?
Perform an immediate bronchoscopy
Perform an immediate thoracotomy
Give aspirin 325 mg and obtain a cardiology consult for possible cardiac catheterization
Repeat the endoscopy to evaluate the biopsy site
Order an immediate esophagram with water-soluble agent
135) A 24-year-old man woke up from sleep 1 hour ago with severe pain in his right testicle. He states that he is sexually active with multiple partners. On examination, the right scrotum is swollen, tender, and firm. You cannot elicit a cremasteric reflex. His BP is 145/75 mm Hg, HR is 103 beats per minute, RR is 14 breaths per minute, temperature is 98.9°F, and oxygen saturation is 99% on room air. Which of the following is the most appropriate next step in management?
Administer one dose of ceftriaxone and doxycycline for 10 days and have him follow-up with a urologist
Send a urinalysis and treat for a urinary tract infection (UTI) if positive
Swab his urethra, send a culture for gonorrhea and Chlamydia, and treat if positive
Treat the patient for epididymitis and have him return if symptoms persist
Order a statim (STAT) color Doppler ultrasound and urologic consultation
136) A 59-year-old man presents to the ED complaining of vomiting and sharp abdominal pain in the epigastric area that began abruptly this afternoon. He describes feeling nauseated and has no appetite. Laboratory results reveal WBC 18,000/μL, hematocrit 48%, platelets 110/μL, AST 275 U/L, ALT 125 U/L, alkaline phosphatase 75 U/L, amylase 1150 U/L, lipase 1450 IU, LDH 400 U/L, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 110 mEq/L, bicarbonate 20 mEq/L, BUN 20 mg/dL, creatinine 1.5 mg/dL, and glucose 250 mg/dL. Which of the following laboratory results correlate with the poorest prognosis?
Amylase 950, lipase 1250, LDH 400
Lipase 1250, creatinine 1.5, potassium 3.5
Lipase 1250, LDH 400, bicarbonate 20
WBC 18,000, LDH 400, glucose 250
WBC 18,000, LDH 400, glucose 250
137) A 27-year-old man is seen in the ED for a leak around a surgical G-tube that was placed 2 weeks ago and has been used for enteral feeding for 1 week. Inspection reveals the tube is pulled out from the stoma, but is still in the cutaneous tissue. The abdomen is soft and nondistended and there are no signs of skin infection. Which of the following is the most appropriate next step in management?
Insert a Foley catheter into the tract and aspirate. If gastric contents are aspirated the tube can be used for feeding
Remove the tube and admit the patient for observation
Insert a Foley catheter into the tract, instill water-soluble contrast, and obtain an abdominal radiograph prior to using for feeding
Remove the tube and immediately obtain a CT scan of the abdomen
Return to the OR for closure of gastrotomy and placement of a new tube
138) A 23-year-old woman presents with weight loss and chronic diarrhea. She appears unwell and cachectic. Routine laboratory tests reveal a low hemoglobin level and an increased international normalized ratio (INR) even though she is not taking any anticoagulants. The liver enzymes are normal, but the albumin and calcium levels are low, suggesting generalized malnutrition. Which of the following is the most appropriate initial diagnostic test for malabsorption?
Xylose absorption
Small intestinal biopsy
Schilling test
X-ray studies
Stool fat quantitation
139) A 50-year-old man with a history of alcohol and tobacco abuse has complained of difficulty swallowing solid food for the past 2 months. More recently, swallowing fluids has also become a problem. He has noted black, tarry stools on occasion. The patient has lost 10 lb. Which of the following statements is correct?
A CT scan of the abdomen and pelvis is the best next test
Herpes simplex virus infection of the esophagus is likely
Barium contrast esophagram will likely establish a diagnosis
The most likely diagnosis is peptic ulcer disease
The patient has achalasia
140) A 48-year-old woman presents with a change in bowel habit and 10-lb weight loss over the past 2 months despite preservation of appetite. She notices increased abdominal gas, particularly after fatty meals. The stools are malodorous and occur 2 to 3 times per day; no rectal bleeding is noticed. The symptoms are less prominent when she follows a clear liquid diet. Which of the following is the most likely histological abnormality associated with this patient’s symptoms?
Signet ring cells on gastric biopsy
Periportal inflammation on liver biopsy
Mucosal inflammation and crypt abscesses on sigmoidoscopy
Villous atrophy and increased lymphocytes in the lamina propria on small bowel biopsy
Small, curved gram-negative bacteria in areas of intestinal metaplasia on gastric biopsy
141) A 62-year-old woman is transferred to the medical service with an appendiceal mass serendipitously picked up at the edge of an x-ray taken of a broken femur in the emergency department. Otherwise, the patient has no significant past medical history and no current symptoms. Which of the following studies is most likely to be useful?
Arterial blood gas
Room air oxygen saturation
CT of the chest and abdomen
Immediate ECG
MRI of the chest and abdomen
142) A 60-year-old woman complains of fever and constant left lower quadrant pain of 2 days duration. She has not had vomiting or rectal bleeding. She has a history of hypertension but is otherwise healthy. She has never had similar abdominal pain, and has had no previous surgeries. Her only regular medication is lisinopril. On examination blood pressure is 150/80, pulse 110, and temperature 38.9°C (102°F). She has normal bowel sounds and left lower quadrant abdominal tenderness with rebound. A complete blood count reveals WBC = 28,000. Serum electrolytes, BUN, creatinine and liver function tests are normal. What is the next best step in evaluating this patient’s problem?
Colonoscopy
CT scan of the abdomen and pelvis
Barium enema
Exploratory laparotomy
Ultrasound of the abdomen
143) A 37-year-old woman presents for evaluation of abnormal liver chemistries. She has long-standing obesity (current BMI 38) and has previously taken anorectic medications but not for the past several years. She takes no other medications and has not used parenteral drugs or had high risk sexual exposure. On examination, her liver span is 13 cm; she has no spider angiomas or splenomegaly. Several sets of liver enzymes have shown transaminases two to three times normal. Bilirubin and alkaline phosphatase are normal. Hepatitis B surface antigen and hepatitis C antibody are normal, as are serum iron and total iron-binding capacity. Which of the following is the likely pathology on liver biopsy?
Macrovesicular fatty liver
Cirrhosis
Microvesicular fatty liver
Portal triaditis with piecemeal necrosis
Copper deposition
144) A 55-year-old man from China is known to have chronic liver disease, secondary to hepatitis B infection. He has recently felt unwell, and his hemoglobin level has increased from 130 g/L, 1 year ago, to 195 g/L. Which of the following is the most appropriate initial diagnostic test?
Alkaline phosphatase
Alanine transaminase (ALT)
Alpha-fetoprotein (AFP)
Aspartate transaminase (AST)
Unconjugated bilirubin
145) A 42-year-old previously well woman presents with pruritus. She is not taking any medications, and only drinks alcohol on a social basis. Her physical examination is entirely normal with no signs of chronic liver disease or jaundice. Laboratory evaluation reveals an alkaline phosphatase level of three times normal, and an ultrasound of the liver and gallbladder is normal. Which of the following is the most appropriate next step in diagnosis?
INR or prothrombin time
Antimitochondrial antibodies
Antinuclear antibodies
Protein immunoelectrophoresis
Abdominal ultrasound

146) A 22-year-old man with inflammatory bowel disease is noted to have a “string sign” in the ileal area on barium enema. In which of the following conditions is this sign most often seen?
In the stenotic or nonstenotic phase of the disease
In the stenotic phase only
As a rigid, nondistensible phenomenon
With gastric involvement
With rectal involvement
147) A 55-year-old white man with a 20-year history of gastroesophageal reflux visits the clinic for worsening reflux symptoms over the past 18 months. His last visit was 7 years ago and he claims to be otherwise in good health. He has been compliant with his antireflux medications, including an H2-blocker and a proton pump inhibitor. Which of the following is the best next step in management?
Double the dose of his H2-blocker and schedule him for follow-up in 4 weeks
Perform an esophagoscopy
Double the dose of his proton pumps inhibitor and schedule him for follow-up in 4 weeks
Schedule him for elective esophagectomy
Schedule him for emergent Nissen fundoplication
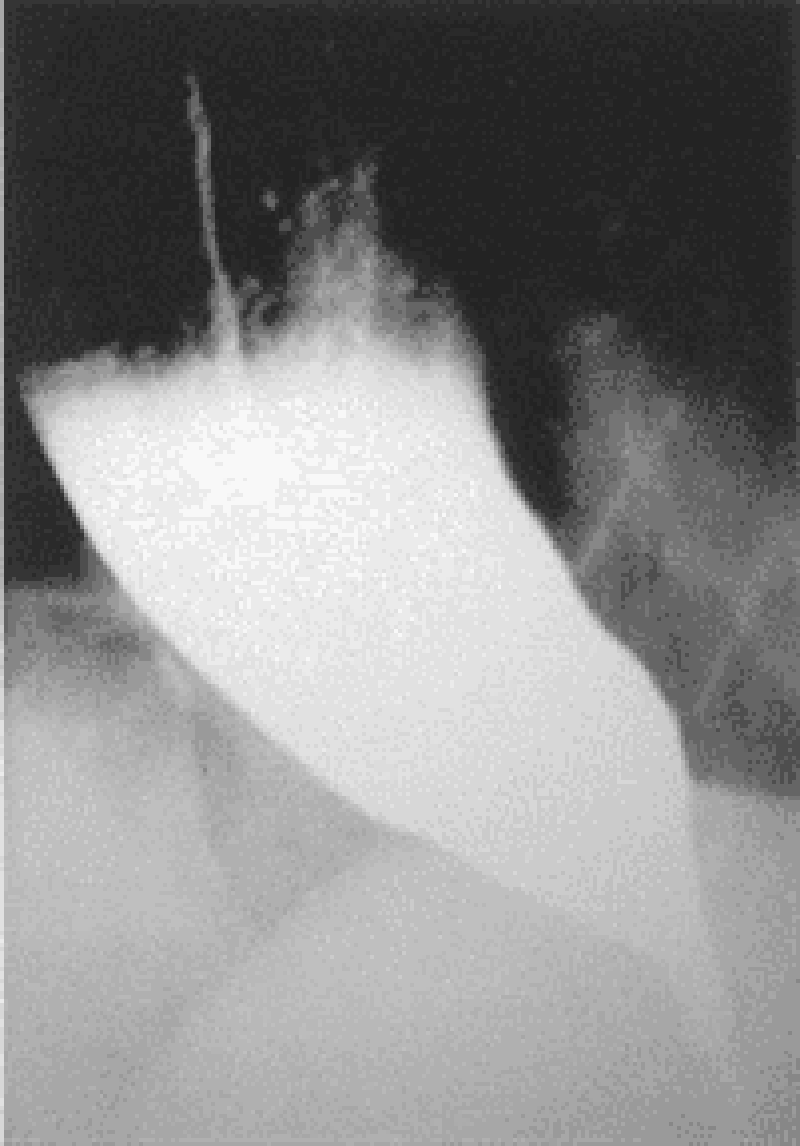
148) A 65-year-old man presents to his physician complaining of difficulty swallowing, occasional chest pain, and regurgitation of food. Over the past 2 months he has lost about 7 kg (15 lb). Results of a barium swallow study are shown in the image. What test should be performed to look for possible causes of his condition?
24-hour pH monitoring
Urease breath test
Esophageal manometry
Serum gastrin level measurement
Upper endoscopy
149) A 63-year-old man with a long history of alcohol abuse presents with ascites. He is experiencing mild abdominal discomfort and nausea. Examination reveals tense ascites and generalized tenderness but no rigidity. A diagnostic paracentesis of the fluid is performed. Which of the following ascitic fluid results is most likely to suggest an uncomplicated ascites due to portal hypertension from cirrhosis?
Hemorrhage
More than 1000 white cells/mm3
Protein >25 g/L
Bilirubin level twice that of serum
Serum to ascites albumin gradient >1.1 g/dL
150) A 21-year-old man presents to the clinic feeling tired and generally unwell. He has fallen several times over the past month and has developed a slight tremor in both hands. Physical examination is significant for scleral icterus, ankle edema, and a distended and tense abdomen. Laboratory studies show: Hemoglobin: 7 g/dL, Reticulocyte count: 7% Total bilirubin: 3.1 mg/dL, Aspartate aminotransferase: 84 U/L Alanine aminotransferase: 92 U/L Ceruloplasmin: 5 mg/dL (normal: 20–45 mg/dL). Results of a Coombs’ test are negative. Which of the following is an appropriate preventive management step after chelation therapy?
Blood protein electrophoresis
Upper endoscopy
Colonoscopy
ECG
Schilling test
151) A 35-year-old alcoholic man is admitted with nausea, vomiting, and abdominal pain that radiates to the back. He has had several previous episodes of pancreatitis presenting with the same symptoms. Which of the following laboratory values suggests a poor prognosis in this patient?
Elevated serum lipase
Diastolic blood pressure greater than 90 mm Hg
Elevated serum amylase
Leukocytosis of 20,000/μm
Diastolic blood pressure greater than 90 mm Hg
152) A 60-year-old woman with depression and poorly controlled type 2 diabetes mellitus complains of episodic vomiting over the last three months. She has constant nausea and early satiety. She vomits once or twice almost every day. In addition, she reports several months of mild abdominal discomfort that is localized to the upper abdomen and that sometimes awakens her at night. She has lost 5 lb of weight. Her diabetes has been poorly controlled (glycosylated hemoglobin recently was 9.5). Current medications are glyburide, metformin, and amitriptyline. Her physical examination is normal except for mild abdominal distention and evidence of a peripheral sensory neuropathy. Complete blood count, serum electrolytes, BUN, creatinine, and liver function tests are all normal. Gallbladder sonogram is negative for gallstones. Upper GI series and CT scan of the abdomen are normal. What is the best next step in the evaluation of this patient’s symptoms?
Barium esophagram
Small bowel biopsy
Scintigraphic gastric emptying study
Colonoscopy
Liver biopsy
153) A 63-year-old man with diabetes is called by his primary care physician because of abnormal liver function test results, as follows: Aspartate aminotransferase: 85 U/L Alanine aminotransferase: 102 U/L Alkaline phosphatases: 180 U/L Total bilirubin: 1.9 mg/dL. On physical examination his liver is enlarged. His skin has a slightly yellow hue, especially on his face. The review of symptoms is significant for some weight loss, weakness, arthritis in his hands, and inability to achieve an erection. What test would generate the most likely diagnosis and should be done first?
Blood smear
Liver biopsy
CT scan of the abdomen
Endoscopic retrograde cholangiopancreatography
Fasting transferrin saturation levels
154) A 28-year-old man presents to the ED complaining of constant vague, diffuse epigastric pain. He describes having a poor appetite and feeling nauseated ever since eating sushi last night. His BP is 125/75 mm Hg, HR is 96 beats per minute, temperature is 100.5°F, and his RR is 16 breaths per minute. On examination, his abdomen is soft and moderately tender in the right lower quadrant (RLQ). Laboratory results reveal a WBC of 12,000/ μL. Urinalysis shows 1+ leukocyte esterase. The patient is convinced that this is food poisoning from the sushi and asks for some antacid. Which of the following is the most appropriate next step in management?
Order a plain radiograph to look for dilated bowel loops
Send the patient for an abdominal ultrasound
Administer 40 cc of Maalox and observe for 1 hour
Order an abdominal CT scan
Discharge the patient home with ciprofloxacin
155) A 23-year-old woman presents to the ED in moderate pain in her left lower quadrant (LLQ). She states that the pain began suddenly and is associated with nausea and vomiting. She had a bout of diarrhea yesterday. This is the second time this month that she experienced pain in this location, however, never with this severity. Her BP is 120/75 mm Hg, HR is 101 beats per minute, temperature is 99.5°F, and RR is 18 breaths per minute. She has a tender LLQ on abdominal examination and a tender adnexa on pelvic examination. Which of the following is the most appropriate diagnostic test for the patient?
CT scan
Laparoscopy
MRI
X-ray
Doppler ultrasound
156) A 75-year-old woman comes to the emergency department with complaints of nausea and nonbilious, nonbloody vomiting over the past 4 days. The patient reports that both the nausea and vomiting come in “waves”; that is, several hours will pass during which she feels well before the vomiting suddenly recurs. A detailed history reveals that the woman was told several months ago that she “has stones in her gall-bladder,” but she has been too frightened to undergo surgery. She has not had a bowel movement for 7 days. Her temperature is 38.4°C (101.1°F) and the abdomen is distended with high-pitched bowel sounds. Which of the following is the most appropriate initial test for a patient with suspected gallstone ileus?
Abdominal ultrasound
Diagnostic laparoscopy
Endoscopic retrograde cholangiopancreatography
Hepatic iminodiacetic acid scan
Plain X-ray of the abdomen
157) An 82-year-old woman is in the surgical intensive care unit after a carotid endarterectomy. She has been taking clindamycin and ciprofloxacin for the past 13 days. On postoperative day 2 the patient is febrile and tachycardic with a high WBC count and a low RBC count. She is also noted to be dehydrated and hypotensive. On physical examination she is distended and has abdominal tenderness with rebound and guarding. Barium enema reveals colonic dilatation of 8 cm. Stool is sent for Gram stain and analysis for fecal leukocytes, fecal occult blood, and Clostridium difficile toxin. Which of the following is most likely present in the stool sample?
Clostridium difficile toxin
Spores and hyphae
Gram-negative rods
Gram-positive cocci
No fecal occult blood
158) A 51-year-old man presents to the ED complaining of epigastric pain that radiates to his back. He states that he drinks six packs of beer daily. You suspect he has pancreatitis. His BP is 135/75 mm Hg, HR is 90 beats per minute, temperature is 100.1°F, and his RR is 17 breaths per minute. Laboratory results reveal WBC 13,000/μL, hematocrit 48%, platelets 110/μL, amylase 1150 U/L, lipase 1450 IU, lactate dehydrogenase (LDH) 150 U/L, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 105 mEq/L, bicarbonate 23 mEq/L, BUN 15 mg/dL, creatinine 1.1 mg/dL, and glucose 125 mg/dL. Which of the following laboratory values are most specific for pancreatitis?
Elevated amylase
Leukocytosis
Hyperglycemia
Elevated lipase
Elevated LDH
159) A 25-year-old G3P1011 presents to the ED with a 6-hour history of worsening lower abdominal pain, mostly in the RLQ. She also noticed some vaginal spotting this morning. She is nauseated, but did not vomit. Her last menstrual period was 2 months ago, but her cycles are irregular. She is sexually active and has a history of pelvic inflammatory disease. Her BP is 120/75 mm Hg, HR is 95 beats per minute, temperature is 99.2°F, and RR is 16 breaths per minute. Her abdomen is tender in the RLQ. Pelvic examination reveals right adnexal tenderness. Her WBC count is slightly elevated and her β-hCG is positive. After establishing IV access, which of the following is the most appropriate next step in management?
Call the OR to prepare for laparoscopy
Swab her cervix and treat for gonorrhea and Chlamydia
Order an emergent CT scan of the abdomen
Perform a transvaginal ultrasound
Order a urinalysis
160) A 40-year-old Asian woman presents to the emergency department complaining of intermittent epigastric pain. The pain is severe, lasts for a few hours, and is sometimes accompanied by nausea and vomiting. Her bowel movements have been normal. Her temperature is 38.3°C (100.9°F), pulse is 100/min, blood pressure is 150/80 mm Hg, and respiratory rate is 22/min. Physical examination reveals moderate obesity and mildly icteric sclerae. Bowel sounds are normal, with an abrupt halt of inspiration upon palpation of the RUQ, and guarding is noted. Laboratory values reveal a WBC count of 13,000/mm³, total bilirubin of 3.3 mg/dL, and normal liver enzymes and alkaline phosphatase levels. Which of the following is the first diagnostic imaging study that should be performed?
CT
Ultrasound of the RUQ
Flat and upright plain x-rays of the abdomen
Hepatobiliary iminodiacetic acid scan
MRI
161) A 45-year-old white man is brought to the emergency department by ambulance. He is waving wildly, trying to hit the “flying bats” that are all around him. He is very agitated and smells strongly of alcohol. The ambulance crew said they found the patient bleeding from the mouth outside a bar. They could not find any laceration on his mouth or lips and believe that the bleeding is internal. The patient screams that he will not stand for this maltreatment any longer and tries to stand up, at which point he begins to vomit. Blood pours out of his mouth, and the patient says, “Here we go again.” The ambulance crew tells the physician that there was also a lot of vomit at the bar where he was found. The physician is able to subdue the patient to obtain his vital signs. His blood pressure is 118/78 mm Hg, pulse is 98/ min, respiratory rate is 22/min, and temperature is 37.2°C (98.9°F). The physician is unable to obtain a history on the patient or con- tact any relatives or friends. No signs of obvious trauma are observed. Which of the following is the best next step in diagnosis?
Barium swallow
X-ray of the chest
Electrocardiogram
Endoscopy
Esophageal manometry
162) A 53-year-old man presents to the emergency department with severe epigastric abdominal pain. His temperature is 37.2°C, blood pressure 110/70 mm Hg, pulse 110/min, and respirations 20/min. Examination of the heart and lungs is normal, and his abdomen is tender in the epigastric region. His white count is 15,000/mL and amylase is 450 U/L (25–125 U/L). Which of the following laboratory abnormalities is also most likely to be present?
Hypoglycemia
Hypercarbia
Hypercholesterolemia
Hyperglycemia
Hypercalcemia
163) A 34-year-old white woman is treated for a UTI with amoxicillin. Initially she improves, but 5 days after beginning treatment, she develops recurrent fever, abdominal bloating, and diarrhea with six to eight loose stools per day. What is the best diagnostic test to confirm your diagnosis?
Identification of Clostridium difficile toxin in the stool
Visualization of clue cells on microscopic examination of stool
Isolation of C difficile in stool culture
Stool positive for white blood cells (fecal leukocytes
Detection of IgG antibodies against C difficile in the serum
164) Her son brings a 50-year-old female to the emergency room because she is confused and sweating a lot. She does not have any medical problems, except hypertension for which she takes hydrochlorothiazide. She is not taking any other medication. He tells you that his mother complained of profound weakness, and inability to stand, because of lightheadedness 3 hours ago. On examination, the patient is drowsy, confused, and appears sick. Her temperature 36.8°C (98.2° F) BP 153/83mm Hg PR 128/min. Her clothes are damp from perspiration. No other abnormalities are noted on physical examination. Initial laboratory studies show: Sodium 144 mEq/L, Potassium 3.6 mEq/L, Bicarbonate 26 mEq/L, Blood urea nitrogen: 12 mg/dl, Creatinine 0.6 mg/dl. You order a few more tests and on the basis of which you diagnose insulinoma. What set of following results leads to this diagnosis? (Serum Glucose, Insulin, C-Protein
Increased, Decreased, Increased
Normal,Normal,Normal
Increased, Increased, Increased
Decreased, Increased, Increased
Decreased, Increased, Decreased
165) A 65-year-old male is brought by his wife to the emergency department because of a very high fever. He has also had a cough productive of greenish, nonbloody sputum for the past two days. He is diabetic, and had pneumonia 3 months ago. He has been smoking one pack of cigarettes daily for 27 years. His temperature is 38.4° C (101.2°F), blood pressure is 118/74 mm Hg, pulse is 98/min, and respirations are 24/min. Physical examination reveals cervical lymphadenopathy, and some scattered rales are heard on the right lung base. Chest-x ray shows a right lower lobe infiltrate. Laboratory studies reveal: Hb 12.6 gm/dL, WBC 40,000/cmm, Platelets 190,000/cmm. Peripheral smear: Segmented neutrophils 10%, Bands 4%, Lymphocytes 85%, Monocytes 1%. Some variant lymphocytes, and smudge cells are seen on the peripheral smear. What is the most appropriate way to confirm the diagnosis of this patient?
Epstein Barr virus serology
Lung biopsy
Bone marrow biopsy
Lymph node biopsy
Cytogenetic analysis
166) A father brings his 7-year-old boy to the office because "his eyes are getting yellow". The boy has no other complaints. However, he is feeling tired and does not feel like going to the next Steelers game. There is a history of diabetes and lung cancer in the family. His vitals are stable, but he has pallor, jaundice, and splenomegaly. His labs revel: WBC 10,000/cmm, Hemoglobin 10 gm/dl, Hematocrit 28%, RBC count 3.5 million, Platelets 240,000/cmm, Reticulocyte count 4%. RBC indices were as follows:MCV 90 fl, MCHC 38%, MCH 28 pg. Peripheral smear revealed anisocytosis, some spherocytosis, and polychromatophilia. Coomb's test was negative. LFTs showed: Albumin 5.2 g/dl, AST 47U/L, ALT 52U/L, Alkaline phosphatase 120 U/L, Total bilirubin 3.0 mg/dl, Direct bilirubin 0.2 mg/dl. What is the next step?
Bone marrow biopsy
Bone marrow biopsy with prussian blue staining
Osmotic fragility test
Serum B12 and folate levels
Sugar water test
168) A 45-year-old white male presented to his primary care physician due to easy fatigability. He is a pure vegetarian and a known alcoholic. Physical examination revealed significant pallor. His hemoglobin level was 10.8gm/dl, and serum iron studies were within normal limits. His physician placed him on folic acid (1 mg daily), and his hemoglobin level increased to 13gm/dl over a period of several months. The patient continued to take folic acid for the next two years. On his next follow-up visit, he complained of gradual memory loss and difficulty in maintaining his balance for the past six months. Which of the following is the most likely thing to consider at this point?
He has been treated with subtherapeutic doses of folic acid
The physician should have checked his vitamin B12 levels
He should be referred for CT of the abdomen with and without contrast
Order FTA-ABS to rule out syphilis
The patient should have been started on pyridoxine
169) A 39-year-old woman comes to the office and complains of double vision. She feels "weak all over," especially at the end of the day. She had the same complaints 8 months ago that persisted for several weeks, but she didn't see a doctor because she had no insurance then. She has no past medical history. Her mother has rheumatoid arthritis, and her brother has type 1 diabetes mellitus. Her vital signs are normal. She has diplopia and mild ptosis. Her blood profile, CBC and thyroid tests are within normal limits. Electromyography and repetitive nerve stimulation reveals a decremental response in compound action potentials. Her acetylcholine receptor antibody test is positive. Which of the following tests should be ordered next?
Muscle biopsy
CT scan of chest
Edrophonium (Tensilon) test
Anti-Jo antibodies
Anti-RNP antibodies
170) A 51-year-old man comes to you complaining of increased itching, especially after bathing. He also has occasional headaches and dizziness. There is no history of smoking or alcohol use. His sister has psychiatric problems and both parents died in a car accident, many years ago. His vitals are; Temperature: 36.7°C (98.2°F); BP 148/90 mm Hg; PR 77/min; RR 12/min. On examination, his spleen is enlarged and he appears plethoric. CBC was ordered and came back as: WBC 14,500/mm3, Hemoglobin 21.5, Hematocrit 64%, Platelets 521,000/mm3, RBC count 7.6 million, MCH 30, MCHC 36, MCV 92, ROW 15.1 (n=10.3-14.1). Which of the following is expected on further work up?
Absence of measurable erythropoetin in urine
Hyponatremia and hyperkalemia
Elevated ESR
Markedly elevated serum cortisol level
Elevated brain natriureteric peptide level
171) A 35-year-old white female slipped and fell on her side 2 days ago while she was going down the stairs from her house. Since that time, she has been having pain in her right shoulder. She describes this as an ache, which has been about the same over the last couple of days. She has tried ibuprofen, with only slight relief. She denies smoking and alcohol use. Examination suggests a shoulder sprain. You order an x-ray and see a normal shoulder but incidentally a 1.5cm coin-shaped lesion, in the outer side of right lung with well-aerated surrounding lung. She denies any respiratory complaints. What is the next best step regarding her lung lesion?
Ask for an old X-ray
Open lung biopsy
CT scan chest
Fine needle aspiration
Bronchoscopy
172) A 74-year -old Caucasian man is evaluated for occasional palpitations and poor exercise tolerance. He has been living alone since his wife died two years ago. His diet consists mainly of precooked food that he heats up in the microwave oven. He has a history of degenerative joint disease and hypertension. He takes a daily aspirin, hydrochlorothiazide, and glucosamine. He quit smoking 20 years ago and occasionally drinks alcohol. His peripheral blood smear is shown below. Which of the following substances is most likely elevated in this patient's blood?
Ferritin
Homocysteine
Methionine
Cobalamin
Haptoglobin
173) A 45-year-old male with Burkitt's lymphoma is being treated with combination chemotherapy and allopurinol. On the 3rd day of treatment, he is noted to have decreased urine output and increased levels of BUN and creatinine. The patient is started on vigorous hydration. EKG reveals prolonged QT intervals. The suspected diagnosis is tumor lysis syndrome. Complete metabolic profile is ordered. Which of the following sets of results are expected in this patient? (Calcium, Phosphate, Potassium, Uric Acid)
Increased, Increased, Increased, Increased
Decreased, Increased, Decreased, Decreased
Decreased, Decreased, Decreased, Decreased
Decreased, Decreased, Increased, Increased
Decreased, Increased, Increased, Increased
174) A 55-year-old woman comes with complaints of episodes of night sweats and fever, for the last 6 weeks. She denies any cough or other respiratory complaints. She has lost 201b (9kg) and does not feel like eating anything. She denies smoking or alcohol use. Her brother was recently diagnosed with polycythemia vera. Physical examination reveals pallor and splenomegaly. Chest-X ray is within normal limits. Blood work is ordered and results are: WBC 66,100/cmm, Hemoglobin 8.70, Hematocrit 30%, Platelets 610,000/cmm. The leukocyte distribution on differential smear was: Promyelocyte 1%, Myelocyte 8%, Metamyelocyte 15%, Bands 35%, Segmented Neutrophils 25%, Lymphocytes 14%, Monocytes 2%. Further tests are ordered. Which one of the following is expected in this patient
Elevated leukocyte alkaline phosphatase
Decreased leukocyte alkaline phosphatase
Elevated leukocyte alkaline phosphatase
Absence of measurable erythropoetin in urine
Presence of auer rods
175) A 62-year-old man comes to the office and complains of increasing fatigue and weakness for the last 4 months. He also describes a dull pain in his back and arms, which gets worse with walking. He denies any numbness or paresthesia. On examination, he appears pale. There is tenderness around the lumbar spine. CBC reveals: WBC 8,600 mm3 with normal differential, Hemoglobin 8.6 g/dl, Hematocrit 27%, Platelets 164,000 mm3. The RBC morphology is significant for a rouleaux appearance. The ESR is 55mm/hr. Bence Jones proteins are identified in the urine. Which of the following is expected in this patient's bone marrow examination?
Over proliferation of plasma cells
Increased marrow cellularity with megakaryocytic hyperplasia
Hypoplastic fat- filled marrow with no abnormal cells
Normocellular bone marrow
Hypocellular and fibrotic bone marrow
176) A 27 year-old African-American woman presents to the emergency room complaining of unilateral leg swelling, pleuritic chest pain and shortness of breath. She reports a rash on her face that worsens in the sun, two previous miscarriages, and complains of recent painful swelling in both knees. A CT angiogram confirms a pulmonary embolus. Which of the following is the most likely laboratory abnormality?
Decreased prothrombin time (PT)
Absent Von Willebrand's factor
Prolonged partial thromboplastin time (PTT)
Increased bleeding time
Thrombocytosis
177) A 60-year-old man comes to office with persistent complaints of malaise and easy fatigability, for the past 8 months. On examination, he appears pale. PR 93/min; BP 127/84mm Hg; Temperature 37°C (98.6°F); RR 16/min. Fecal occult blood test is negative. Further testing is ordered that include CBC, serum electrolytes and colonoscopy. The results are: WBC 7,600/mm3, Hemoglobin 8.8 gm/dl, Hematocrit 30%, RBC count 3.6 million, Platelets 211,000/mm3. RBC Indices were:MCV 65 fl, MCH 16.5 pg, MCHC 26%, Reticulocyte count 0.5%. Which one of the following is expected on iron studies in this patient? (Serum Iron, Ferritin, TIBC, Transferrin Saturation
Low,High,Low,Lowto normal
Normal, Normal, Normal, Normal
High,Normai,High,Normal to High
Low,Low,High,Low
Low,Low,Low,Low
{"name":"Part 30 (89-177)", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your medical knowledge with our comprehensive quiz designed for healthcare professionals and students alike. With 88 challenging questions covering a wide range of topics, you'll have the opportunity to deepen your understanding of clinical scenarios and improve your diagnostic skills. Key Features: Covering diverse topics from pediatrics to geriatrics Designed for both learning and assessment Perfect for medical students, residents, and practicing clinicians","img":"https:/images/course8.png"}
More Quizzes
( Last ) Pro Paraclinique (1-74) (1-145 ) Neymar 1
74370
(New) Part 3 "510-764" Na V (678-715)
100500
Chir Ortho-traumato
115580
Magnetic Materials, Permanent magnets
10528
Cardiac Output Practice Problems - Free Online
201017963
What Type of Pizza Am I? - Find Your Slice
201018107
Teen Wolf - Test Your Beacon Hills Knowledge
201019390
Strict Parent - How Strict Are You?
201016852
Basketball IQ Test - Free NBA Knowledge Challenge
201020428
Central Nervous System Stimulant - Identify the Drug
201019938
India State Capital - Can You Name Them All?
201018963
Music Trivia Multiple Choice - 200+ Questions & Answers
201015339