QCU/DES/USMLE/CADIOVASCULAR 1-200

Cardiovascular Mastery Quiz
Test your knowledge of cardiovascular conditions and their management with our comprehensive 200-question quiz. Ideal for students, healthcare professionals, and anyone interested in enhancing their understanding of cardiovascular health.
Key Features:
- 200 meticulously crafted multiple-choice questions
- Covers a wide range of cardiovascular topics
- Helpful for both study and certification preparation
1. A 74-year-old man presents to your office for a routine He has no present complaint His medical history is significant for right knee osteoarthritis He takes naproxen occasionally, to relieve knee pain. He does not smoke or consume alcohol His BP is 165/75 mm Hg and PR is 70/min. The physical examination showed a mild systolic ejection type murmur at the base of the heat to the right. An EKG revealed left ventricular hypertrophy and secondary ST segment and T wave change Moderate left ventricular hypertrophy, without any flow abnormalities, was demonstrated on echocardiography. The ejection fraction was 60%. What is the most probable cause of hypertension in this patient?
B. Elevated plasma renin activity
A. Rigidity of the arterial wall
D. Increased cardiac output
C. Aortic insufficiency
E. Increased intravascular volume
2. A 32-year-old Caucasian female comes to the physician because of a one-week history of fatigue, progressive worsening of shortness of breath and swelling of feet. She denies any chest pain She has no other medical problems except a recent cold two weeks ago. She is not taking any medication Her temperature is 36 7 C (98 F), blood pressure is 110/65 mmHg, pulse is g0/min, and respirations are 20/min Bilateral basal crackles, elevated jugular venous pressure, and 2+ bilateral pitting edema of the ankles are noted Complete blood count is unremarkable. Transthoracic echocardiogram of her heat will most likely show?
B. Eccentric hypertrophy of the heart
A. Concentric hypertrophy of the heart
D. Hypokinesia of the inferior wall
C. Mitral stenosis
E. Dilated ventricles with diffuse hypokinesia
8. A 47-year-old male presents to your office with a two-month history of lethargy and decreased libido His medical records reveal that he has been treated for joint pain and swelling over the last six months and was diagnosed with diabetes mellitus one year ago Physical examination reveals hepatomegaly and testicular atrophy Which of the following cardiac abnormalities is most likely to also be present in this patient?
B. Aortic stenosis
A. Atrial septal defect
D. Cardiac conduction block
C. Hypertrophic cardiomyopathy
E. Endocardial fibroelastosis
3. A 47-year-old woman loses consciousness for 2 minutes while shopping in a supermarket. In the emergency room, she recounts feeling nausea and warmth spreading over her body immediately before passing out She has never had a similar episode before. She has not seen a doctor for several years and does not take any medications, nor does she use tobacco, alcohol or drug. Her family history is unremarkable. Which of the following most likely caused this episode?
B. Seizure
A. Cardiac arrythmia
D. Heat valve disease
C. Neurocardiogenic syncope
E. Orthostatic hypotension
4. A 25-year-old woman experiences sudden-onset palpitations and generalized weakness. During this episode, her blood pressure is 100/60 mmHg and her heat rate is 160/min and regular. She has no significant past medical history and does not take any medications She reports having a few similar episodes in the past which she has self-treated by immersing her face in cold water Generally, she says, cold water immersion relieves her symptoms within several minutes. This cold water therapy works by affecting which of the following?
B. Sinoatrial node automatism
A. Vascular tone
D. Purkinje fiber conduction
C. Atrioventricular node conductivity
E. Ventricular myocardium contractility
5. A 67-year-old man is evaluated for hypertension He complains of occasional morning headaches. His past medical history is also significant for type 2 diabetes mellitus, coronary artery disease, and a stroke with residual left-sided weakness. He underwent coronary artery bypass surgery seven years ago and carotid endarterectomy five years ago. His current medication list includes lisinopril hydrochlorothiazide, amlodipine, metoprolol, aspirin, metformin and glyburide His blood pressure is 190/120 mmHg on the right arm and 170/110 mmHg on the left arm. His heat rate is 65/min Physical examination reveals a periumbilical systolic-diastolic bruit. The latter finding is best explained by which of the following?
B. Aortic dissection
A. Abdominal aortic aneurysm
D. Renal artery stenosis
C. Aortic coarctation
E. Aorto-enteric fistula
6. A 67-year-old male is brought to the emergency department after a syncopal episode. He lost consciousness while shopping in the mall. He denies any nausea, diaphoresis, chest pain, or shortness of breath. He has had two episodes of lightheadedness over the last month but has not seen a doctor. His past medical history is significant for long-standing hypertension, which is being treated with enalapril. His blood pressure is 135/90 mmHg while supine, and 130/85 mmHg while standing His heat rate is 64/min ECG shows a sinus rhythm with high voltage, prolonged PR interval, prolonged QRS interval, normal QT interval and occasional premature ventricular contractions (PVC) Echocardiography reveals left ventricular hypertrophy and an ejection fraction (EF) of 55% Which of the following is the most likely cause of this patient's syncope?
C. Torsades de pointes
B. Decreased myocardial contractility
D. Autonomic dysfunction
A. Bradyarrhythmia
E. Ventricular premature beats
7. A 60-year-old male is 2 days status post primary percutaneous coronary intervention (PCI) with stent placement. He had previously suffered from an antero-lateral myocardial infarction. His cardiac enzymes have been trending down since admission He has recovered well and is ready for discharge He is currently asymptomatic. His temperature is 37.5 C (99.5 F), blood pressure is 130/70 mm Hg, pulse is 66/min, and respirations are 14/min He is discharged with instructions to take the following medications aspirin simvastatin, lisinopril metoprolol and sublingual nitroglycerine. In addition to the medications listed above, which of the following medications should this patient also be taking after discharge?
B. Low molecular weight heparin
A. Isosorbide mononitrate
D. Clopidogrel
C. Waffarin
E. Amlodipine
9. A 35-year-old Caucasian male is being evaluated for poor exercise tolerance and muscle weakness He has no past medical history His blood pressure ranges from 175-185 mmHg systolic and 105-1 15 mmHg diastolic on repeat measurement His heat rate is 78-g5/min His serum chemistry is significant for blood glucose of 95 mg/dL serum creatinine of 0.7mg/dL serum Na of 146 mEq/L and serum K of 2.4 mEq/l_ CT scan of the abdomen reveals a 3 cm mass in the left adrenal gland. Which of the following additional findings would you expect in this patient? Plasma renin activity, Serum aldosterone, Serum bicarbonate
B. High High High
A. High High Low
D. low High Low
C. low High High
E. High Low High
10. A 67-year-old homeless male presents 24 hours after the onset of substernal chest pain and is diagnosed with an anterior wall myocardial infarction. There is no history of previous chest pain, dyspnea, palpitations, syncope or leg swelling. He has no hypertension or diabetes mellitus. He does acknowledge a 40 pack-year smoking history. Upon discharge, echocardiography shows normal left ventricular size, left ventricular anterior wall hypokinesis and an ejection fraction of 50%. Two years later, the patient is found dead in the street. Autopsy reveals a dilated left ventricle with a globular shape and thinned walls along with a scar on the anterior wall. Which of the following would have most likely prevented this patient's pathologic findings?
B. Enalapril
A. Aspirin
D. Isosorbide dinitrate
C. Amlodipine
E. Digoxin
11. A 50-year-old woman presents to your office complaining of lower extremity edema that stated several weeks ago, and slowly progressed thereafter. Her past medical history is significant for hypertension, treated with metoprolol for 2 years. Amlodipine was added recently because of inadequate control of BP with metoprolol alone. She does not smoke or consume alcohol. She has no known drug allergies. Her blood pressure is 130/80mm Hg and her heart rate is 64/min. The physical examination reveals bilateral symmetric 3+ pitting edema of both lower extremities, without any skin changes or varicosities Her neck vein pulsation is normal. Other physical findings are within normal limits. Her laboratory studies reveal the following: Serum albumin 4.5 g/dL Total serum bilirubin 0.8 mg/dL Serum sodium 140 mEq/L Serum potassium 4.0 mEq/L Serum creatinine 0.8 mg/dL Urinalysis is within normal limite. What is the most likely cause of the edema in this patient?
B. Liver disease
A. Heart failure
D. Venous insufficiency
C. Renal disease
E. Side effect of her medications
12. A 64-year-old male who has not seen a doctor for the past 20 years presents to the emergency room with excruciating chest pain that stated suddenly about three hours ago. He describes the pain as tearing in quality and says that it radiates to his back. On physical examination, you hear an early diastolic decrescendo murmur at the sternal border. Chest x ray shows widening of the superior mediastinum. EKG is normal. Which of the following medical conditions most likely accounts for this patients presentation?
B. Marfan's syndrome
A. Systemic hypertension
D. Bicuspid aortic valve
C. Ehlers-Darlos syndrome
E. Giant cell arteritis
13. A 40-year-old female presents to the emergency room with palpitations and lightheadedness of acute onset. Also, she has experienced insomnia, fatigability, and weight loss lately. She does not smoke or consume alcohol. She is not taking any medication. Her blood pressure is 110/80 mmHg and heat rate is 120/min, irregular. Physical examination reveals lid lag and fine tremor of the outstretched hands. ECG shows atrial fibrillation with rapid ventricular response. What is the next best step in the management of this patient?
B. Propranolol
A. Digoxin
D. Quinidine
C. Lidocaine
E. Immediate cardioversion
14. A 43-year-old Caucasian man with a two-year history of diabetes mellitus presents to your office for a routine. He has no complaint His medications are metformin and aspirin. He works as a computer programmer and has a sedentary lifestyle. He drinks one to two cans of beer on weekends and smokes one pack of cigarettes per day. On physical examination, his blood pressure is 153/94 mm Hg and his heat rate is 82/min His BMI is 32.5 kg/m2. The remainder of the physical examination is unremarkable Laboratory studies reveal an HbA1c of 7.6%. At his check-up one month ago, his blood pressure was 149/92 mmHg. Which of the following interventions would be most effective for controlling his blood pressure?
B. Weight loss
A. Aerobic exercise
D. Better diabetes control
C. Smoking cessation
E. Quitting alcohol
15. A 38-year-old woman presents to the emergency room complaining of chest pain for the past several hours She describes it as sharp, centrally located and non-radiation. The pain worsens somewhat with inspiration and movement. The patient denies having fevers, chills, dyspnea, swelling, or difficulty breathing at night. She says she first noticed the pain while exercising three weeks ago, but has experienced it at rest as well. She says that she has been exercising heavily in an attempt to lose weight. Her BMI is currently 34kg/m2. Her father had a myocardial infarction at age 60. Her medical history is significant for two normal vaginal deliveries. She smokes a half-pack of cigarettes daily. On physical examination, her blood pressure is 112/69 mm Hg and her heat rate is 72/min. Cardiac exam reveals a regular Sl and S2 without extra sounds or murmurs There is tenderness to palpation over the sternum. What is the most likely cause of her chest pain?
B. Pulmonary embolism
A. Gastroesophageal reflux disease
D.Pericarditis
C. Unstable angina
E. Costochondritis
16. A 63-year-old man presents to the ER with substernal chest pain and diaphoresis. The pain stated one hour ago and did not remit with antacids. He has a past medical history of asthma for which he uses inhaled fluticasone and peptic ulcer disease for which he takes omeprazole. His family history is significant for prostate cancer in his father and breast cancer in his mother. Physical examination reveals a blood pressure of 160/100 mmHg and a heat rate of 90/min. A bruit is heard over the right carotid artery and a mild systolic murmur is present at the cardiac apex Sublingual nitroglycerin and aspirin are administered in the. Within minutes, the patient reports decreased pain. Which of the following most likely accounts for this improvement in his symptoms?
B. Decreased left ventricular volume
A. Increased left ventricular compliance
C. Decreased left ventricular contractility
D. Increased systemic afterload
E. Increased cardiac preload
17. A 38-year-old female comes to your office complaining of occasional palpitations She describes feeling a fast and irregular heartbeat Over the past two months, she has had three such episodes, each lasting about two hours She denies any associated chest pain, shortness of breath cough or ankle swelling. She drinks alcohol on social occasions and does not smoke cigarettes She has no other medical problems and is not taking any medications On physical examination, her temperature is 37.1 C (98.9F), pulse is 80/min, blood pressure is 130/70mmHg, and respirations are 14/min. On auscultation of her heat the apical impulse is displaced and there is an S3. You also hear a pansystolic murmur, which is loudest at the apex and radiates to the axilla. Which of the following is the most likely cause of her symptoms?
A. Mitral valve prolapse
B. Myocardial ischemia
D. Mitral annular calcification
C. Rheumatic heat disease
E. Infective endocarditis
18. A 42-year-old woman is evaluated for depression, mood swings and poor. She also complains of mild headaches and muscle weakness. She has had two ER Visits for kidney stones over the past year. She denies any illicit drug use. Her blood pressure is 160/105 mmHg and her heat rate is 85/min. Her laboratory findings are shown below: Sodium 140mEq/L Potassium 3.6 mEq/L Chloride 101 mEq/L Bicarbonate 24 mEq/L BUN 13 mEq/L Creatinine 0.9 mEq/L Glucose 98 mEq/L Calcium 11.7 mg/dL Which of the following is the most likely cause of this patient's hypertension?
B. Renal vascular stenosis
A. Renal parenchymal disease
D. Hypothyroidism
C. Aortic dissection
E. Parathyroid gland disease
19. A 14-year-old African American male is referred to your office after his older brother experienced sudden cardiac arrest during hiking trip. He has no current complaints. He denies any illicit drug use His blood pressure is 110/60 mmHg and his heat rate is 75/min. Neck is supple, no jugular venous distention is appreciated. Carotid pulse seems to have dual upstroke. Lungs are clear. There is strong apical impulse and a systolic ejection type murmur along the left sternal border. Which of the following is most likely to increase the murmur intensity in this patient?
B. Valsalva maneuver
A. Squatting
D. Recumbency
C. Sustained handgrip
E. Leg raising
20. A 60-year-old male is brought to ER by his son because he had an episode of syncope. He was watching TV in an arm-chair when suddenly lost his consciousness without any warning sign. He had several clonic jerks while unconscious He never had such an episode before. His past medical history is significant for acute myocardial infarction six months ago and well-controlled hypertension. His current medications include captopril metoprolol hydrochlorothiazide, clopidogrel and aspirin. His blood pressure is 130/85 mmHg and heat rate is 80/min with frequent ectopic beat. Physical examination revealed mild holosystolic apical murmur radiating to the axilla. Which of the following is the most probable pathophysiologic mechanism for his syncopal episode?
B. Arrhythmia
A. Vasovagal reaction
D. Seizure
C. Autonomic dysfunction
E. Postural hypotension
21. A 45-year-old recently immigrated Mexican farmer comes to your office complaining of dyspnea, fatigue and abdominal distention for the past two months. On physical exam, his temperature is 37 C (98F), blood pressure is 126/80 mmHg, pulse is 80/min, and respirations are16/min. You note pedal edema, elevated jugular venous pressure with positive Kussmaul's sign, and increased abdominal girth with free fluid. Chest auscultation reveals decreased heart sound intensity at the apex and an early heart sound following S2 The jugular venous pressure tracing shows prominent 'x and 'y' descents. Which of the following is the most likely cause of this patient's symptoms?
B. Tuberculosis
A. Cor pulmonale
D. Psittacosis
C. Trypanosoma cruzi infection
E. Pneumoconiosis
22. A 25-year-old G2, PI at 28 weeks gestation is brought to the emergency department by her boyfriend, who found her lying on her bed in a pool of blood She is very drowsy, but denies any pain or uterine contractione Her temperature is 38 C (100.4 F) and respirations are 18/min Physical examination is suggestive of a transverse lie Inspection of the perineum reveals gross blood and active bleeding per vagina. Which of the following set of parameters would most likely be seen in this patient? CO PCWP SVR BP HR Set A Decreased Increased Increased Decreased Increased set B Decreased Decreased Increased Decreased Decreased Set C Decreased Decreased Increased Decreased Increased set D Decreased Decreased Decreased Decreased Increased set E Increased Decreased Increased Decreased Increased
B. set B
A. Set A
D. set D
C. Set C
E. set E
23. A 54 year-old male comes to the physician because of abdominal distention He thinks his big belly is making it hard for him to breathe He received radiation therapy for Hodgkin lymphoma several years ago and was told that he is cured He drinks alcohol on a regular basis His temperature is 36.7C (98F), blood pressure is 120/76 mm Hg, pulse is 80/min and respirations are 20/min Examination shows a jugular venous pressure7 cm above the sternal angle Dullness to percussion and decreased breath sounds are noted in the right lung base The abdomen is quite distended with an obvious fluid wave Mild hepatomegaly is present Extremities have 2+ lower extremity edema. Initial laboratory studies are shown below: Serum creatinine 08 mg/dL Alburnin 4.0 mg/dL Total bihrubin 1.0 mg/dl Prothrombin time 11 sec Urinalysis is within normal limits. Which of the following is the most likely cause of his condition?
B. Portal vein thrombosis
A. Urinary protein loss
D. Inelastic pericardium
C. Portal vein compression
E. Thoracic duct obstruction
24. A 32-year-old woman presents with progressively worsening dyspnea on exertion one month after returning from a vacation in Texas. She says that her symptoms have progressed to the point that she now wakes during the night with a choking sensation that improves only with sitting up. Recently her shortness of breath has required her to significantly limit her physical activity. She denies having associated chest pain, skin rash or joint pain She has no significant past medical history. Family history is significant for thyroid cancer in her aunt and lung cancer in her father, a heavy smoker. On physical examination, her temperature is 37.20C (99 F), pulse is g6/min, blood pressure is 110/70 mmHg, and respirations are 14/min. Bilateral pitting ankle edema is present. Her liver is enlarged 2 cm below the right costal marginal. Lung auscultation reveals decreased breath sounds at the bilateral bases. Cardiac exam reveals the presence of a third heat sound. Chest x ray shows an enlarged cardiac silhouette and small bilateral pleural effusion. EKG is unremarkable. Which of the following is the most likely cause of her symptoms?
B. Viral infection
A. Atherosclerosis
D. Coccidioidomycosis
C. Lyme disease
E. Autoimmune disease
25. A 45-year-old mildly overweight male recovering from an anterior wall myocardial infarction develops sudden onset of sharp pain in the left side of his chest He presented five days earlier with substernal chest pain and diaphoresis. He has had no dyspnea, extremity swelling or palpitations since admission. His past medical history is significant for diabetes mellitus type 2. He seems mildly restless, especially in the supine position. The pain improves when sitting up and leaning forward. His breathing is fast and shallow due to the pain. His lungs are clear on auscultation. His blood pressure is 120/78 mmHg and his heart rate is 60/min There is no change in blood pressure upon deep inspiration. ECG shows sinus rhythm with new diffuse ST segment elevation. Which of the following is the most likely diagnosis?
B. Ventricular free wall rupture
A. Interventricular wall rupture
D. Recurrent ischemia
C. Pulmonary infarction
E. Acute pericarditis
26. An 88-year-old female nursing home resident is brought to the hospital with a one-week history of moaning, decreased oral intake and decreased ambulation. Physical examination reveals a very thin female who is moaning and appears to be in pain. She opens her eyes spontaneously but does not respond to questions. Her blood pressure is 75/43 mmHg, pulse is 105/min, temperature is 35.5°C (96°F), and respirations are 22/min. Oxygen saturation (pulse oximetry) is 97% on room air. Her skin and oral mucosa are dry and her neck veins are flat. There is no lymphadenopathy. On chest auscultation, there are crackles in the right upper lung lobe. Abdomen is soft and non-distended. There is 2+ pitting presacral and lower extremity edema, and a deep pressure ulcer in the sacral area. Laboratory analysis reveals the following: Sodium 155mEq/L Potassium 5.3 mEq/L Glucose 88mg/dL Bicarbonate 14mEq/L BUN 151mg/dL Creatinine 3.1mg/dl Which of the following is the most likely cause of her lower extremity edema?
B. Decreased plasma oncotic pressure
A. Increased plasma hydrostatic pressure
D. Increased interstitial oncotic pressure
C. Renal water and sodium retention
E. Decreased lymphatic drainage
27. A 64-year-old man complains of palpitations and progressive shortness of breath over the past several hours. He says that he also develops a choking sensation every time he tries to lie down. His medical history is significant for hypertension for the past 20 years and medication non-compliance. He also has a 35-year smoking history. He reports that his father died of a heart attack at age 70 and his mother suffered from asthma. On physical examination, his blood pressure is 170/100 mmHg and his heat rate is 130/min and irregularly irregular. Lung exam reveals bibasilar crackles. There is 2+ pitting edema of the lower extremities. Bedside echocardiography shows a left ventricular ejection fraction of 55%. Which of the following is most likely responsible for his symptoms?
B. Diastolic dysfunction
A. Cardiogenic shock
D. Small airway bronchoconstriction
C. High-output heat failure
E. Increased lung compliance
28. A 22-year-old Caucasian male is evaluated for an episode of syncope that occurred while playing soccer It lasted only 2 minutes without any post-syncopal confusion, sleepiness or weakness. He had prior episodes of dizziness while playing active sports as well as vague chest discomfort. His uncle died suddenly at a young age. Auscultation of his precordium reveals a III/IV systolic murmur along the left sternal border. The patient is most likely to benefit from which of the following medications?
A. Nitrates
B. Beta-blockers
D. Amlodipine
C. Disopyramide
E. Digitalis
29. A 55-year-old Caucasian male presents to your office with muscle pain of recent onset. His past medical history is significant for hypertension and an acute myocardial infarction experienced 2 months ago. His current medications include metoprolol captopril, aspirin and simvastatin. His blood pressure is 130/80 mmHg and heat rate is 60/min Liver function tests are slightly abnormal. Serum creatine kinase level is elevated. You suspect a drug-induced reaction. Which of the following is the most possible mechanism of drug-induced reaction in this patient?
B. Cell surface receptor blockage
A. Immune-mediated reaction
D. Synthetic reaction inhibition
C. Extracellular enzyme blockage
E. Damage of membrane-bound lipids
30. A 40-year-old male presents with six months of worsening dyspnea. His symptoms have progressed to the point that walking even one block causes him to become shot of breath. He has a history of cigarette smoking, but quit 10 years ago. He drinks approximately one alcoholic drink daily. His medical history is significant for peptic ulcer disease for which he takes antacids. On physical examination, he is afebrile. His pulse is 86/min, blood pressure is 140/56 mmHg, and respiratory rate is 14/min While examining his heat you note a high-pitched blowing, early diastolic, decrescendo murmur, which is heard best in the left third intercostal space and is intensified by handgrip. There is prominent cardiomegaly on chest x-ray. Which of the following medications would improve both this patient’s symptoms and cardiomegaly?
B. Metoprolol
A. Quinidine
D. Ephedrine
C. Nifedipine
E. Amiodarone
31. A 70-year-old man is brought to the Emergency Room because he lost his consciousness while working in the garden. He says that he had several episodes of near-syncope on exertion recently. His past medical history is insignificant He is not taking any medications. His blood pressure is 110/85 mmHg and heat rate is 80/min. Point of maximal impulse is increased in intensity. Cardiac auscultation reveals ejection type systolic murmur at the base of the heat with radiation to the carotid arteries. ECG demonstrates left ventricular hypertrophy, and secondary ST segment and T wave change. What is the most probable cause of this patient's condition?
B. Bacterial endocarditis
A. Rheumatic endocarditis
D. Congenital anomaly
C. Hypertension
E. Age-related sclerocalcific changes
32. A 20-year-old female presents to your office for a routine. She has no complaints and her past medical history is insignificant. She is not taking any medications and denies drug abuse. Her blood pressure is 125/65 mmHg and heat rate is 80/min. Cardiac auscultation reveals early diastolic murmur at the left sternal border. What is the next best step in the management of this patient?
B. Chest x ray
A. Electrocardiogram
D. Echocardiography
C. Coronary angiography
E. No further work-up
33. A 23-year-old woman who is 26 weeks pregnant presents to the emergency department with sudden onset severe shortness of breath and inability to lie flat. She recently emigrated from Eastern Europa. Her medical history is significant for recurrent sore throats requiring tonsillectomy as a child. Presently, her blood pressure is 110/60 mmHg and her heart rate is 120/min. An EKG rhythm strip suggests atrial fibrillation. Which of the following is the most likely diagnosis?
B. Constrictive pericarditis
A. Hypertrophic cardiomyopathy
D. Myocardial infarction
C. Mitral stenosis
E. Aortic insufficiency
34. A 68-year-old man is brought to the emergency room after he passed out for one minute during an early morning jog. He was not confused after the episode and did not have bowel or bladder incontinence. He has been having exertional chest pain and shortness of breath for the past few months. He has never had any resting chest pain. He has been healthy except for hypertension, for which he takes hydrochlorothiazide. He has a 20 pack year smoking history and occasionally drinks a glass of wine. His blood pressure is 142/90 mm Hg, pulse is 80/min, and respirations are 16/min. Carotid pulse is delayed S2 is weak and an S4 is present. A grade 3/6 systolic ejection murmur is in the right 2nd intercostal space, radiating to the carotids. Neurological examination reveals no focal findings, and there are no signs of head trauma. An EKG shows left ventricular hypertrophy. The first set of cardiac enzymes is negative. Which of the following is the most appropriate next step in management?
B. Electroencephalogram (EEG)
A. CT scan of the head
D. Echocardiogram
C. Exercise stress test
E. CT angiogram of the chest
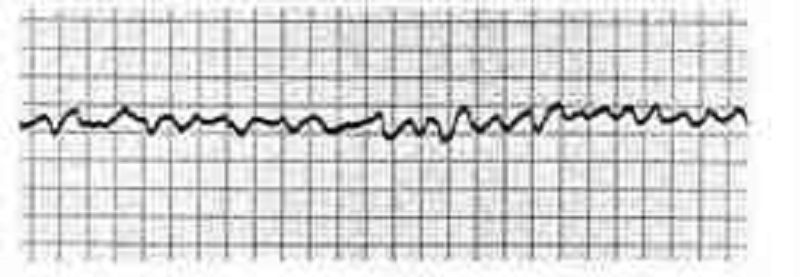
35. A 72-year-old female is admitted to the ICU with severe chest pain. The initial set of cardiac enzymes is positive and her EKG reveals an anterior wall myocardial infarction. She receives treatment with aspirin clopidogrel, metoprolol nitroglycerine drip, and morphine. Two hours later, her telemetry monitor displays the following rhythm .Which of the following is the best next step in managing this patient?
B. Defibrillation
A. Lidocaine
D. Amiodarone
C. Digoxin
E. Immediate echocardiogram
36. A 63-year-old Caucasian female presents to the emergency room with a recent onset of left-sided Weakness. She has been experiencing increased fatigability, low-grade fevers and occasional palpitations over the past two months. She has lost seven pounds during the same period. Her temperature is 37C (98.6 F), pulse is 80/min (regular), blood pressure is 120/76mmHg and respirations are 14/min. Her lungs are clear. Cardiac auscultation reveals normal first and second heat sounds and a mid-diastolic rumble at the apex. Echocardiography shows a mass in the left atrium. Which of the following is the most likely diagnosis?
B. Infective endocarditis
A. Congenital heart defect
D. Myxomatous valve degeneration
C. Intracardiac tumor
E. Rheumatic fever and atrial thrombus
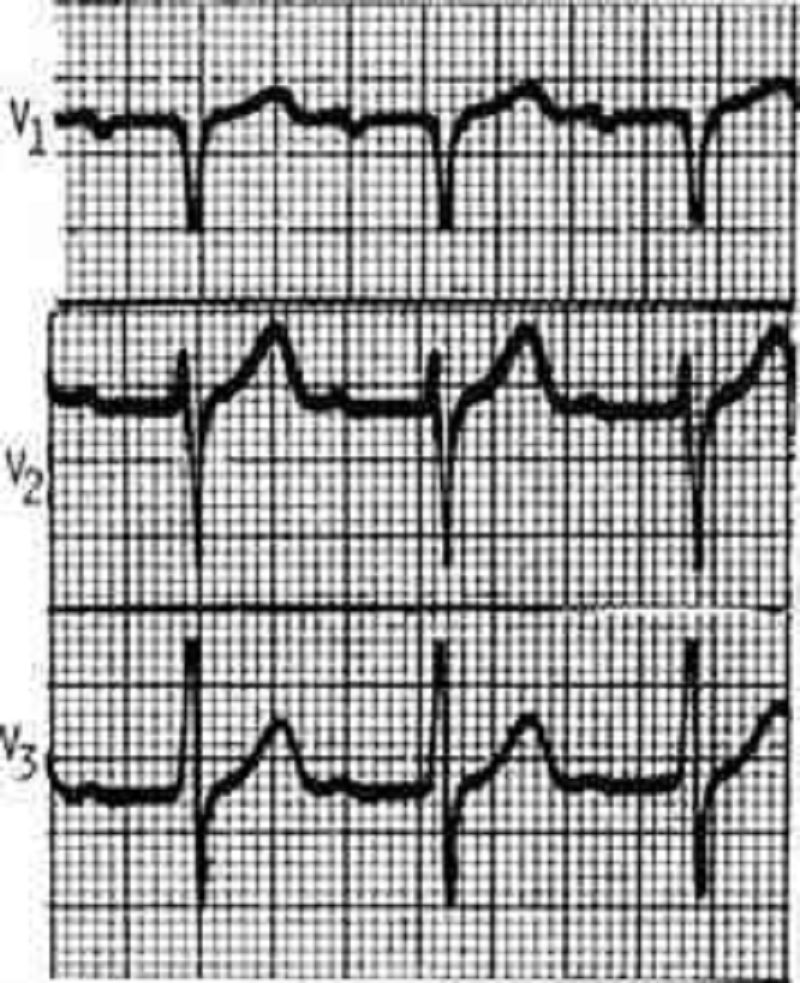
37. A 67-year-old male presents to the ER with chest pain. His medical history is significant for stable angina for which he takes aspirin and isosorbide dinitrate, as well as hypertension and bronchial asthma. Occasionally, he uses an albuterol inhaler. He is admitted to the hospital and five hours later, he begins to feel lightheaded and weak. His blood pressure is 100/60 mmHg. An EKG is obtained and is shown below.Which of the following is the best next step in managing this patient?
A. Cardiac catheterization
B. Pacemaker insertion
C. Adenosine
D. Digoxin
E. Metoprolol
38. A 56-year-old male presents with progressively worsening dyspnea and ankle edema. He denies chest pain syncope or palpitations. He does not smoke or drink alcohol. He denies diabetes mellitus, hypertension, or hyperlipidemia. His temperature is 37.1C (98.7F), pulse is 70/min, blood pressure is 136/70mmHg, and respirations are 15/min. Examination shows elevated jugular venous pressure, bilateral ankle edema, and tender hepatomegaly. Chest auscultation shows bibasilar rales. His heat sounds are distant and there is no murmur. Chest x ray shows mild cardiomegaly and a right-sided pleural effusion. ECG shows low voltage QRS complexes and nonspecific ST-T wave changes. Echocardiography shows normal left ventricular volume with symmetrical thickening of the left ventricular walls and slightly reduced systolic function. Which of the following would represent a potentially reversible cause of this patient’s heat disease?
B. Sarcoidosis
A. Amyloidosis
D. Scleroderma
C. Hemochromatosis
E. LED
39. A 43-year-old white male is found to have premature atrial complexes (PACs) on routine EKG. He denies chest pain, shortness of breath or lightheadedness. He has smoked 1-2 packs of cigarettes daily for the past 20 years. He also has a 20-year history of alcoholism, though recently he has limited his use to 1-2 beers/day The patient's family history is significant for a myocardial infarction in his mother at age 65 and a stroke in his father at age 72. He has no personal history of hypertension or diabetes. Physical examination including Vital signs, is entirely within normal limits. What is the best next step in the management of this patient?
B. 24-hour Halter monitoring
A. Reassurance
D. Start beta-blocker therapy
C. Echocardiogram
E. Advise him to stop alcohol and tobacco
40. A 60-year-old man is brought to the emergency department due to syncope. He has had similar episodes a few times during the past few weeks. These episodes usually occur after he exerts himself. He does not feel confused or tired after these episodes. He denies any chest pain or palpitation. His wife reports that when he collapses, he seems to lose consciousness for a few seconds, but then is back to being alert right away. She denies any jerking movement. His past medical history is significant diverticulosis, for which he takes fiber supplements. He is not on any other medication. His temperature is 37.1 C (98.8 F), blood pressure is 110/98 mm Hg, pulse is 88/min, and respirations are 14/min. On examination, he has a fourth heart sound and harsh 3/6 systolic murmur, best heard over the right sternal border. The murmur is accentuated on expiration. The lung fields are clear to auscultation. After performing an echocardiograph to confirm the diagnosis, which of the following management options is most appropriate?
B. Aortic valve replacement
A. Aortic valvotomy
D. Exercise test looking for arrhythmias
C. Close outpatient follow-up with serial echocardiograms
E. Observe until the patient develops breathlessness
41. A 12-year-old white male wants to participate in sports at school. He has been growing normally since birth. His immunizations are up-to-date and he is not suffering from any known medical conditions. Which of the following measures should be taken to screen him for underlying heart disease that could cause sudden cardiac death?
B. History and physical exam
A. No screening is required
D. Echocardiography
C. 12 lead ECG
E. Exercise stress testing
42. A 55-year-old male presents to the emergency room with right-sided weakness that has persisted for the past several hours. He also complains of severe central chest pain that is "ripping" in quality and radiates to his back. He has had hypertension for the past seven years and has not been taking any anti-hypertensive medication. He has been smoking one pack of cigarettes per day for the past 25 years. His father died of coronary artery disease at age 44 years. His temperature is 37.1C (98.6F), pulse is 78/min, blood pressure is 180/120 mm Hg in the right arm and 110/70 mm Hg in the left arm, and respirations are 16/min. He is diaphoretic and confuse. His neurological examination is significant for decreased power and tone in the right upper and right lower extremities. The rest of his physical examination is unremarkable ECG shows left axis-deviation and a chest x ray is normal. Based on these findings, what is the most likely diagnosis?
B. Hemorrhagic stroke
A. Subarachnoid hemorrhage
D. Myocardial infarction with thromboembolism
C. Paradoxical pulmonary embolism
E. Aortic dissection
43. A 54-year-old man is brought to the ER three hours after the onset of severe, 10/10, tearing, substernal chest pain radiating to his back. He still complains of pain and dizziness at the time of arrival. Physical examination demonstrates a pale thin male who is anxious and diaphoretic. His blood pressure is 90/60 mmHg in the right arm and 70/40 mmHg in the left arm. There is an 18 mmHg difference in systolic blood pressure between inspiration and expiration. His jugular veins are distended while sitting. Bedside echocardiogram demonstrates a moderate amount of pericardial fluid. Which of the following is the most likely diagnosis?
B. Acute pericarditis
A. Acute myocardial infarction
D. Pulmonary embolism
C. Aortic dissection
E. Tension pneumothorax
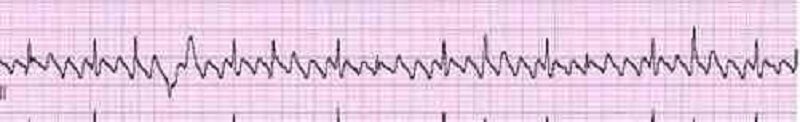
44. A 46-year-old man collapsed while getting out of his bed. He has been feeling weak over the last several days and has complained of vague chest discomfort. He ascribed the symptoms to a recent respiratory infection and did not visit a doctor. His mother died of a stroke and his father suffered from recurrent myocardial infarctions. He eats a balanced diet and takes a multivitamin daily. His most recent blood cholesterol level was 200 mg/dl. An ECG strip taken by EMS is shown below.Which of the following is the best initial management of this patient?
B. Synchronized DC cardioversion
A. Procainamide
C. Thrombolytic therapy
D. Beta-blockers and aspirin
E. Pericardiocentesis
45. A 59-year-old male suffers a myocardial infarction. He is treated medically and is discharged home ten dayslater on aspirin, atorvastatin, metoprolol, lisinopril, and sublingual nitroglycerin. One month later, he presentsto your office for a follow-up visit. He denies chest pain, dyspnea or lightheadedness. His blood pressure is120/75 mmHg. His EKG is pictured below. Echocardiogram reveals an ejection fraction of 45%. What is the best next step in his management?
B. Amiodarone
A. Observation
D. DC cardioversion
C. Digoxin
E. Verapamil
46. A 55-year-old white male presents to the Emergency Room with a four-hour history of chest pain. The pain is substernal and radiates to the left arm. He has a history of hypertension, diabetes, and hypercholesterolemia. His temperature is 36.7 C (98 F), blood pressure is 110/65 mmHg, pulse is 110/min, and respirations are 18/min. ECG is recorded and reveals ST segment elevation in the anterior leads and several ventricular premature beats (VPBs). What would the administration of lidocaine to such a patient most likely result in?
B. Improvement in overall prognosis
A. Increase in the risk of ventricular fibrillation
C. No change in frequency of VPBs
D. Increase in the risk of asystole
E. Increase in the risk of congestive heart failure
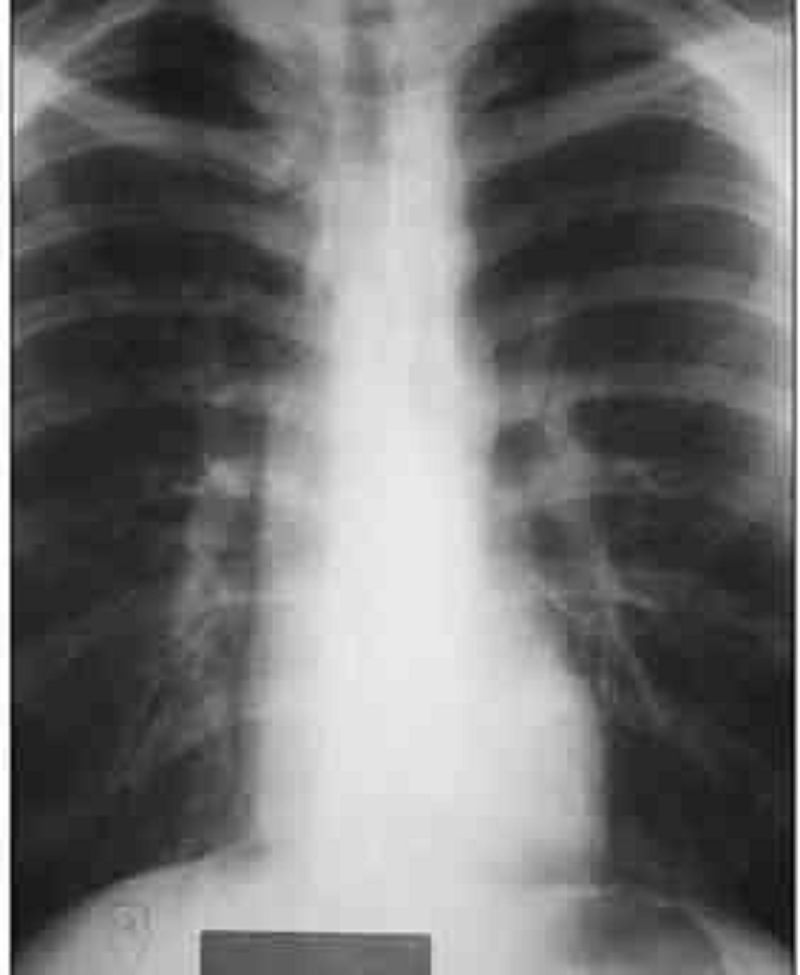
47. A 22-year-old male presents to you with feelings of general malaise. He is always tired and has noticed that he has frequent headaches. Exam reveals an elevated arm blood pressure with a radial to femoral delay. ECG shows left ventricular hypertrophy and the chest-x ray is shown below. Close examination of the x-ray reveals a "3" sign.What is the most likely diagnosis in this patient?
B. Patent ductus arteriosus
A Tetralogy of F allot
D. Atrial septal defect
C. Coarctation of aorta
E. Aortic aneurysm
48. A 67-year-old Caucasian male is hospitalized in the intensive care unit (ICU) with an episode of prolonged hypotension and shortness of breath. His skin is cold and clammy. Intra-arterial blood pressure monitoring is established, and pulmonary artery catheterization is performed to control basic hemodynamic parameters. His blood pressure is 70/40 mmHg, and heart rate is 100/min. Cardiac output (CO) measured by thermodilution method is 2.3 Umin. Pulmonary capillary wedge pressure (PCWP) is estimated to be 22 mmHg. Systemic vascular resistance (SVR) calculated using data on mean arterial pressure, right atrial pressure and cardiac output is 2000 dynes*s/cm5 (N= 700 - 1200 dynes*s/cm5). Which of the following is the most likely underlying problem in this patient?
B. Volume depletion
A. Cardiogenic shock
C. Septic shock
D. Volume overload
E. Right ventricular infarction
49. A 32-year-old male complains of progressive weakness and exertional dyspnea. His past medical history is significant for a knife injury to the right thigh two months ago. He has been arrested several times for robbery. He consumes alcohol regularly, and smokes crack occasionally. His younger brother died of cystic fibrosis. His blood pressure is 160/60 mmHg, and heart rate is 100/min. His extremities are warm and flushed. Carotid upstroke is brisk. The point of maximal impulse is displaced to the left, and a soft, holosystolic murmur is heard over the cardiac apex. The murmur does not change with the Valsalva maneuver. Which of the following is the most likely cause of this patient's symptoms?
B. Hypertrophic cardiomyopathy
A. Decreased cardiac output
D. Papillary muscle dysfunction
C. Increased cardiac preload
E. Pulmonary hypertension
50. A 21-year-old woman presents to the ED complaining of lightheadedness. Her symptoms appeared 45 minutes ago. She has no other symptoms and is not on any medications. She has a medical history of mitral valve prolapse. Her HR is 170 beats per minute and BP is 105/55 mm Hg. Physical examination is unremarkable. After administering the appropriate medication, her HR slows down and her symptoms resolve. You repeat a 12-lead ECG that shows a rate of 89 beats per minute with a regular rhythm. The PR interval measures 100 milliseconds and there is a slurred upstroke of the QRS complex. Based on this information, which of the following is the most likely diagnosis?
B. Atrial flutter with 3:1 block
A. Ventricular tachycardia
D. Lown-Ganong-Levine (LGL) syndrome
C. Atrial fibrillation
E. Wolff-Parkinson-White (WPW) syndrome
51. A 61-year-old woman with a history of diabetes and hypertension is brought to the ED by her daughter. The patient states that she started feeling short of breath approximately 12 hours ago and then noticed a tingling sensation in the middle of her chest and became diaphoretic. An ECG reveals ST depression in leads II, III, and aVF. You believe that the patient had a non–ST-elevation MI (NSTEMI). Which of the following cardiac markers begins to rise within 3 to 6 hours of chest pain onset, peaks at 12 to 24 hours, and returns to baseline in 7 to 10 days?
B. Creatinine kinase (CK)
A. Myoglobin
D. Troponin I
C. Creatinine kinase-MB (CK-MB)
E. Lactic dehydrogenase (LDH)
52. A 71-year-old man is playing cards with some friends when he starts to feel a pain in the left side of his chest. His fingers in the left hand become numb and he feels short of breath. His wife calls the ambulance and he is brought to the hospital. In the ED, an ECG is performed. Which of the following best describes the order of ECG changes seen in an MI?
B. Q wave, ST-segment elevation, hyperacute T wave
A. Hyperacute T wave, ST-segment elevation, Q wave
C. Hyperacute T wave, Q wave, ST-segment elevation
D. ST-segment elevation, Q wave, hyperacute T wave
E. ST-segment elevation, hyperacute T wave, Q wave
53. While playing a match of tennis, a 56-year-old man with a medical history significant only for acid reflux disease starts to feel substernal chest pain that radiates into his left arm and shortness of breath. His pain feels better after drinking antacid, but since it is not completely resolved, his partner calls 911. Upon arrival, EMS administers aspirin and sublingual nitroglycerin. After 20 minutes, the man’s symptoms resolve. He is brought to the ED for further evaluation where his ECG shows sinus rhythm without any ischemic abnormalities. You order a chest radiograph and send his blood work to the laboratory for analysis. Which of the following statements regarding the diagnosis of acute MI is most accurate?
B. One set of negative cardiac enzymes is sufficient to exclude the diagnosis of MI in this patient.
A. A normal ECG rules out the diagnosis of acute MI.
C. Troponin may not reach peak levels for at least 12 hours
D. Relief of symptoms by antacids essentially rules out a cardiac cause of his chest pain.
E. Epigastric discomfort and indigestion is a rare presentation of ACS.
54. A 22-year-old college student went to the health clinic complaining of a fever over the last 5 days, fatigue, myalgias, and a bout of vomiting and diarrhea. The clinic doctor diagnosed him with acute gastroenteritis and told him to drink more fluids. Three days later, the student presents to the ED complaining of substernal chest pain that is constant. He also feels short of breath. His temperature is 100.9°F, HR is 119 beats per minute, BP is 120/75 mm Hg, and RR is 18 breaths per minute. An ECG is performed revealing sinus tachycardia. A chest radiograph is unremarkable. Laboratory tests are normal except for slightly elevated WBCs. Which of the following is the most common cause of this patient’s diagnosis?
B. Influenza A
A. Streptococcus viridans
C. Coxsackie B virus
D. Atherosclerotic disease
E. Cocaine abuse
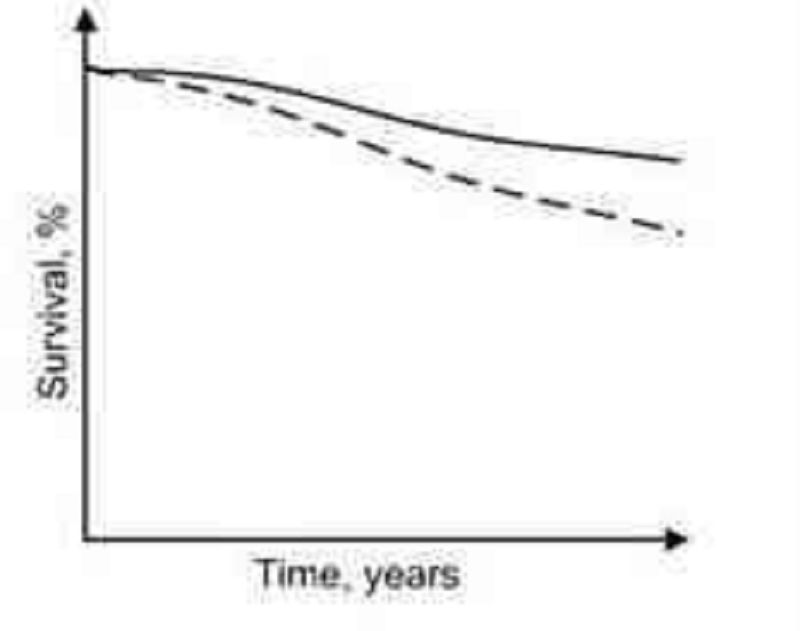
55. Diuretics, vasodilators and oxygen are standard inpatient therapy for patients hospitalized with leftsided heart failure. When patients are discharged, a different outpatient regimen is instituted. A team of researchers compares long-term cardiovascular mortality between patients treated with two different outpatient regimens. The study results are depicted below:In comparison to the patients depicted by the dashed curve, those depicted by the solid line most likely received treatment with which of the following?
B. Calcium channel blocker
A. ACE inhibitor
D. Digoxin
C. Loop diuretic
E. Dobutamine
56. A 60-year-old man is brought to the ER by his wife because he lost consciousness in the bathroom at night. He says that he woke up, went to the bathroom to urinate, and fainted there. He rapidly recovered his consciousness without any indication of disorientation. He has never had such an episode before. He admits' problems with urination,' including difficulty with initiating urination and frequent awakening to void at night. He does not take any medication. His past medical history is insignificant. He smokes 2 packs of cigarettes per day and does not consume alcohol. His blood pressure is 130/80 mm Hg while supine, and 132/80 while standing. His heart rate is 70/min. His physical examination is within normal limits. The ECG is normal. What is the most probable cause of the syncopal episode in this patient?
B. Postural hypotension
A. Arrhythmia
D. Seizure
C. Situational syncope
E. Transient ischemic attack (TIA)
57. A 76-year-old man was operated on for a strangulated inguinal hernia and had approximately 40 cm of small bowel resected. On the morning of his third post-operative day, he falls while getting out of bed. Immediately after the fall, he is responsive but his speech is slurred and he cannot explain what happened. His pulse is 122/min, blood pressure is 96/50 mm Hg, and respirations are 23/min. Lungs are clear to auscultation and his heart has a regular rate and rhythm. His neck veins are distended. An ECG is remarkable for a new onset right bundle branch block (RBBB). Immediate resuscitation is started with wide open intravenous fluids, but he becomes unresponsive. Shortly thereafter, his pupils start to dilate and his heart rate drops to 45/min. He eventually dies despite resuscitative efforts. What is the most likely cause of his death?
B. Acute ischemic stroke
A. Hypovolemia accompanied by syncope
D. Post-operative sepsis
C. Myocardial infarction
E. Massive pulmonary thromboembolism
58. A 57-year-old female with a past medical history of bronchial asthma presents to the physician's office for evaluation of high blood pressure. On her previous two visits, her blood pressure has been 154/88 and 150/90. Her blood pressure during this visit is 150/90 mmHg. She denies headaches and has no complaints. She uses fluticasone and albuterol inhalers for her chronic persistent asthma. She denies smoking or alcohol intake, and has no known drug allergies. Her family history is significant for myocardial infarction in both her mother and father. Exercise and a low salt diet have not improved her hypertension. Which of the following is the most appropriate next step in managing this patient's hypertension?
B. Prescribe propranolol
A. Discontinue asthma medications
D. Prescribe hydrochlorothiazide
C. Prescribe enalapril
E. Obtain an echocardiogram
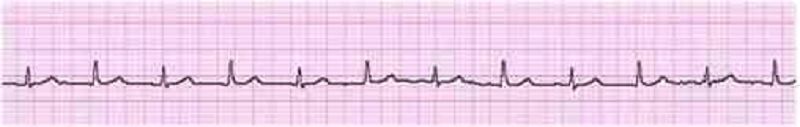
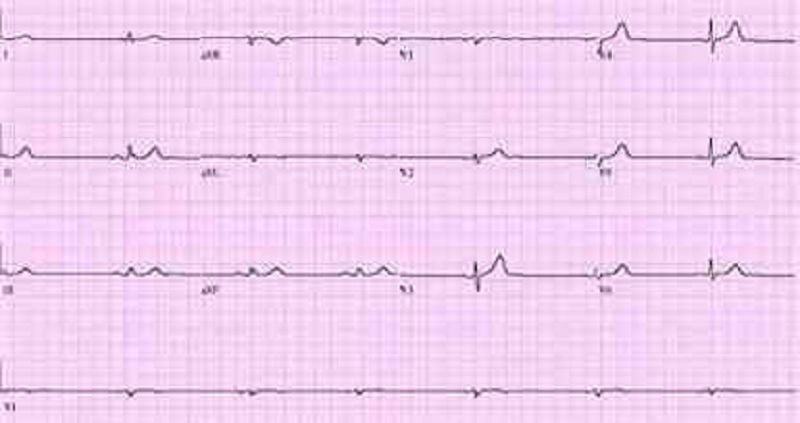
59. A 63-year-old female presents to your clinic complaining of palpitations. For the past 3 weeks, she has noticed pounding of her heart that comes and goes. Her symptoms are more frequent at night. Her only medicine is insulin for diabetes mellitus. On physical examination, she is alert and oriented, and in no distress. Her EKG is shown below.Which of the following best accounts for this patient's symptoms?
B. Irregularly irregular atrial activation
A Sinus arrhythmia
D. Atrial ectopy
C. Variable AV node conduction
E. Ventricular ectopy
60. A 53-year-old Caucasian female is admitted to the ER with hypotension. Her condition is considered very serious, and invasive hemodynamic monitoring is established. Blood pressure measured by intraarterial method is 72/46 mmHg. Her heart rate is 120/min, regular. Pulmonary capillary wedge pressure (PCWP) estimated using Swan-Ganz catheter is 6 mmHg. Mixed venous oxygen concentration (MVo2) is 16 vol% (Normal = 15.5 vol%). Which of the following is the most likely cause of this patient's condition?
B. Volume depletion
A.Cardiogenic shock
C. Septic shock
D. Hemorrhagic shock
E. Neurogenic shock
61. A 27-year-old female presents to your office for a follow-up. The previous two visits revealed an elevated blood pressure in the range of 150-155/90-95 mm Hg. She has no present complaints. Her past medical history is insignificant. She smokes 1/2 pack of cigarettes per day and does not consume alcohol. Her current medications include a combination oral contraceptive for the last 2 years, and an occasional acetaminophen for tension headache relief. There is no family history of hypertension or heart attacks. This visit, her blood pressure is 155/95 and her heart rate is 80/min. The physical examination is unremarkable. The ECG is normal. Her total cholesterol level, measured 6 months ago, was 170 mg/dL. Which of the following is the most appropriate next step in the management of this patient?
B. Discontinuation of the oral contraceptive
A Lifestyle modification
D. Intravenous pyelography
C. Low-dose thiazide diuretic
E. No intervention at this point
62. A 60-year-old female comes to your office for progressive exertional dyspnea and new-onset ankle swelling. She has been recently worked up for proteinuria and easy bruisability. Otherwise her past medical history is insignificant. She has a ten pack-year history of smoking and she drinks two to three glasses of wine every day. Her temperature is 37.1 C (98.8F), blood pressure is 130/70 mm Hg, pulse is 80/min and respirations are 14/min. There is mild jugular venous distention on physical examination. Chest auscultation shows scattered bibasilar crackles. Echocardiography reveals symmetrical thickening of the ventricular walls, normal ventricular dimensions and a slightly reduced systolic function. Which of the following is the most likely diagnosis?
B. Hemochromatosis
A. Alcohol-related heart disease
D. Amyloidosis
C. Sarcoidosis
E. Constrictive pericarditis
63. A 65-year-old male presents to the emergency department with substernal chest pain, severe shortness of breath, and diaphoresis that began suddenly 40 minutes ago. Since the pain started, the patient has vomited twice. The pain radiates to his left arm and does not remit with sublingual nitroglycerine. EKG shows 2 mm ST elevations in the anterior leads. On physical examination, the patient's temperature is 36.9°c (98.4.F), blood pressure is 110/70 mm Hg, pulse is 60/min, respirations are 32/min, and oxygen saturation is 90% on 4L oxygen by nasal canula. Cardiac exam reveals a muffled S1 and S2 and the presence of an S3. Lung exam reveals basilar crackles that extend halfway up the lung fields bilaterally. Which of the following is the best next step in managing this patient?
B. Digoxin
A Metoprolol
C. Furosemide
D. Spironolactone
E. IV fluids
64. During a routine office visit, a 62-year-old male is found to have a pulsatile non-tender mass above his umbilicus. His medical history is significant for hypertension, chronic renal insufficiency, myocardial infarction, and peripheral vascular disease. He quit smoking 10 years ago. On physical examination, his blood pressure is 160/90 mm Hg and pulse is 76/min. Laboratory analyses reveal a serum creatinine of 2.0 mg/dl. Which of the following is the most appropriate next step in evaluating this patient's abdominal mass?
B. CT scan with contrast
A. Plain abdominal x-ray
D. Abdominal MRI
C. Abdominal ultrasound
E. No testing required
65. A 20-year-old white female presents with chest pain for the past few weeks. She describes the pain as sharp, located to the left of the sternum, and lasting 5-10 seconds at a time. There is no associated fever, cough, breathlessness, palpitations, or syncope. She does not smoke or drink alcohol. On cardiac examination, there is a short systolic murmur at the apex that disappears with squatting. Which of the following is the most likely diagnosis?
B. Ventricular septal defect
A. Mitral valve prolapse
C. Rheumatic heart disease
D. Bicuspid aortic valve
E. Infective endocarditis
66. A 42-year-old man presents to the emergency department complaining of two weeks of weakness, low-grade fevers, and exertional shortness of breath. He also notes fingertip pain and urine that has been dark and cloudy recently. On physical examination, several of his proximal interphalangeal joints are swollen. Which of the following diagnoses is most consistent with his presentation?
B. Post-streptococcal glomerulonephritis
A Rheumatoid arthritis
D. Infective endocarditis
C. Adult Still's disease
E. Adrenal insufficiency
67. A 59-year-old man comes to visit his friend in the hospital and collapses in the parking lot. He had been feeling unwell all day due to vague chest discomfort. A bystander witnesses his collapse, finds no pulse, and immediately calls for help. Which of the following is the most important factor for survival in this patient?
B. Time to defibrillation
A. Time to chest compressions
D. Time to epinephrine injection
C. Time to endotracheal intubation
E. Time to cardiac catheterization lab
68. A 73-year-old man presents to the ED after a syncopal episode. He had been resting in bed for approximately one week after injuring his right knee. This morning, his knee felt better and he attempted to get up from bed. However, upon attempting to stand, he sustained a brief loss of consciousness. He had no symptoms or medical history prior to the knee injury. Medications include acetaminophen and ibuprofen for knee pain. On exam, his pulse is 73/min, respirations are 14/min, and blood pressure is 136/83 mmHg. Which of the following is the most likely cause of this patient's syncope?
B. Valvular obstruction
A Cardiac arrhythmia
D. Vagal nerve hyperactivity
C. Orthostatic hypotension
E. Hyperventilation
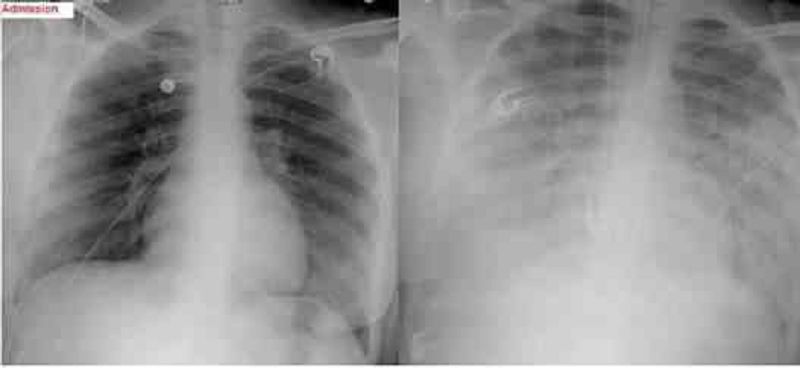
69. A 47-year-old female, who is a chronic alcoholic, is admitted to the hospital with epigastric pain, nausea, and vomiting. Her serum amylase and lipase levels are significantly elevated and the diagnosis of acute pancreatitis is made. She is maintained nothing by mouth (NPO), and receives intravenous hydration and narcotic analgesics. On the second day of hospitalization she develops progressive shortness of breath. Her temperature is 37.2 C (98.9 F), blood pressure is 110/66 mm Hg, pulse is 110/min, and respirations are 24/min. Her oxygenation is measured at 84% on 100% nonrebreather mask and the decision is made to intubate. Since the time of admission, she has received 5 liters of normal saline and has produced 3 liters of urine output. On examination, there is no evidence of jugular venous distention. Chest auscultation reveals diffuse bilateral crackles. Auscultation of the heart reveals normal heart sounds with no murmurs. A chest x-ray from the time of admission and one from the time of intubation are shown below:Based on these findings, what is the most likely diagnosis in this patient?
B. Hospital acquired pneumonia
A. Acute respiratory distress syndrome
D. Congestive heart failure from myocardial infarction
C. Iatrogenic volume overload
E. Alcoholic cardiomyopathy
70. A 59-year-old male presents to the ER with sudden onset severe chest pain associated with vomiting and diaphoresis. The pain radiates to the left shoulder and is not relieved by sublingual nitroglycerine. His past medical history is significant for diabetes mellitus for seven years and hypercholesterolemia for six years. His medications include metformin, glipizide and simvastatin. On physical examination, his blood pressure is 150/98 mmHg and pulse is 86/min. An EKG obtained in the ER shows ST segment elevations in leads aVL and I. Cardiac troponin and CK-MB are elevated. Which of the following medications should be avoided in this patient at this time?
B. Captopril
A Heparin
D. Metoprolol
C. Nifedipine
E. Aspirin
71. A 46-year-old woman is hospitalized for agitation, restlessness and poor sleep. She has been complaining of headaches recently and has gained 14 pounds over the past three months. She denies any illicit drug use. Her blood pressure is 160/110 mmHg and her heart rate is 90/min. Her laboratory findings are shown below: Sodium 142 mEq/L Potassium 3.2 mEq/L Chloride 98 mEq/L Bicarbonate 26 mEq/L BUN 12 mg/dl Creatinine 0.9 mg/dl Glucose 205 mg/dl Calcium 94 mg/dl Which of the following is the most likely cause of this patient's hypertension?
B. Adrenal medullary disease
A. Renal parenchymal disease
D. Hypothyroidism
C. Adrenal cortical disease
D. Hypothyroidism E. Parathyroid gland disease
72. A 55-year-old male with a history of rheumatoid arthritis and rheumatoid lung disease is admitted to the hospital with palpitations. His restrictive lung disease is of moderate severity, requiring use of 2 liters of oxygen by nasal cannula at all times. He has no known history of coronary artery disease, hypertension or diabetes. On physical examination, his blood pressure is 110/70 mmHg and heart rate is 120 and irregular. EKG shows atrial fibrillation with a rapid ventricular rate. Which of the following medications should be avoided in this patient?
B. Digoxin
A. Verapamil
C. Quinidine
D. Amiodarone
E. Metoprolol
73. A 37-year-old Cambodian woman presents to the emergency room with acute onset of left-sided weakness. She has been experiencing progressive exertional dyspnea, nocturnal cough and occasional hemoptysis over the past six months. She also describes frequent episodes of palpitations and irregular heartbeats. Which of the following is the most likely diagnosis?
B. Hypertrophic cardiomyopathy
A. Mitral stenosis
D. Wolf-Parkinson-White syndrome
C. Aortic insufficiency
E. Primary pulmonary hypertension
74. A 32-year-old anxious-appearing male is wheeled into the emergency room with the sudden onset of excruciating left-sided chest pain. His temperature is 37.2C (99F), blood pressure is 160/88 mmHg, pulse is 125/min, regular and respirations are 20/min. Physical examination is normal, except for multiple venous track marks on his extremities and atrophic nasal mucosa. An EKG is done which shows ST depression and T wave inversion in leads V1-V6. Cardiac enzymes including CK-MB and Troponin Tare not elevated. Which of the following is the most appropriate next step in the management of this patient?
B. Administer metoprolol
A. Cardiac catheterization
D. Close observation
C. Administer thrombolytics
E. Intravenous diazepam
75. A 67-year-old man presents to the emergency department after losing consciousness while shoveling snow near his house. He reports having had a similar episode one month ago while carrying heavy bags from the grocery store. The patient has reduced his physical activity level over the last several months because of progressive exertional dyspnea and fatigue. His past medical history is significant for diabetes mellitus and hypercholesterolemia. Metformin and simvastatin are his only medications. Which of the following physical examination findings is most likely in this patient?
B. Capillary pulsations
A. Pulsus paradoxus
D. Systolic ejection murmur
C. Late diastolic murmur
E. Pleural friction rub
76. A 66-year-old white male presents for evaluation of progressively worsening dyspnea that affects him at rest and wakes him from sleep. He also notes bilateral ankle swelling. His medical history is significant for coronary artery disease for which he has undergone angioplasty and coronary artery bypass grafting. On examination today, his pulse is 86/min, blood pressure is 110/70 mmHg, and respirations are 19/min. His neck veins are distended and there is bilaterally symmetric pitting ankle edema. On chest auscultation, you hear crackles at the bilateral lung bases and a third heart sound. Chest x-ray shows an enlarged cardiacsilhouette and bilateral alveolar and interstitial pulmonary edema. Of the medications listed below, which has not been shown to improve survival in patients with the above presentation?
B. Losartan
A Captopril
D. Digoxin
C. Metoprolol
E. Aspirin

77. A 69-year-old male undergoes coronary artery bypass and aortic valve replacement surgery. The procedure goes well, and he is extubated and discharged to the step-down unit on postoperative day 2. That night, he complains of weakness, chest tightness and shortness of breath. His blood pressure is 70/30 mmHg, respiratory rate is 26/min, and heart rate is 148 beats per minute. Lung auscultation reveals bibasilar crackles. An EKG rhythm strip is obtained:Which of the following is the best next step in the management of this patient?
B. Transcutaneous pacing
A. Amiodarone
D. Lidocaine
C. DC cardioversion
E. Digoxin
78. A 53-year-old man presents to the emergency room with squeezing chest pain that started two hours ago. He also complains of shortness of breath that is worse when lying down. He has never had pain like this before. He has no significant past medical history and he takes no medications. A routine health maintenance visit two weeks ago was normal. On physical examination in the ER, his blood pressure is 140/90 mmHg and his heart rate is 100/min. Chest auscultation reveals a grade IINI blowing systolic murmur at the cardiac apex and bibasilar crackles in the lungs. ECG shows ST segment elevations in leads I, aVL, and v1-v3. Which of the following is most likely increased in this patient?
B. Left atrial size
A. Left atrial pressure
D. Left ventricular ejection fraction
C. Left ventricular compliance
E. Right ventricular preload
79. A 35-year-old woman who has recently emigrated from Asia presents to the emergency room with acute onset of dyspnea. She denies any cough, chest pain, or fever. She has a history of rheumatic heart disease as a teen. On examination, she has an irregular pulse of 97/min, blood pressure of 125/75 mm of Hg and temperature of 37.2C (98.9F). The first heart sound is loud and a mid-diastolic rumble is heard at the apex. Crackles are present in both lung fields. ECG shows an irregularly, irregular heart rhythm and the absence of 'P' waves. Which of the following is the most likely cause of this patient's abnormal heart rhythm?
B. Right atrial dilatation
A. Left atrial dilatation
D. Left ventricular hypertrophy
C. Left ventricular dilatation
E. Pulmonary hypertension
80. A 17-year-old girl is brought to the ER 30 minutes after an episode where she lost consciousness. She is accompanied by her father who witnessed the event. He says that the patient recently broke up with her boyfriend and has been under a lot of stress. Her sleep has been poor. She has had three similar episodes over the last month. On exam, her heart rate is 90/min, respirations are 13/min, and blood pressure is 120/70 mmHg. She seems sleepy but can be aroused easily. She gives her correct name but is disoriented to time and place. Pupils are symmetric and reactive to light. Blood glucose level is 100 mg/dl. Which of the following findings would you most expect in this patient?
B. Pulsus paradoxus
A. Systolic murmur that increases with standing
C. Orthostatic hypotension
D. Positive stool guaiac test
E. Bitten tongue
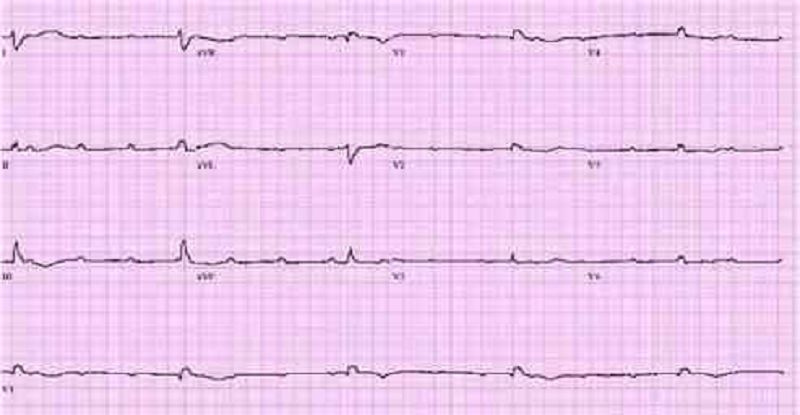
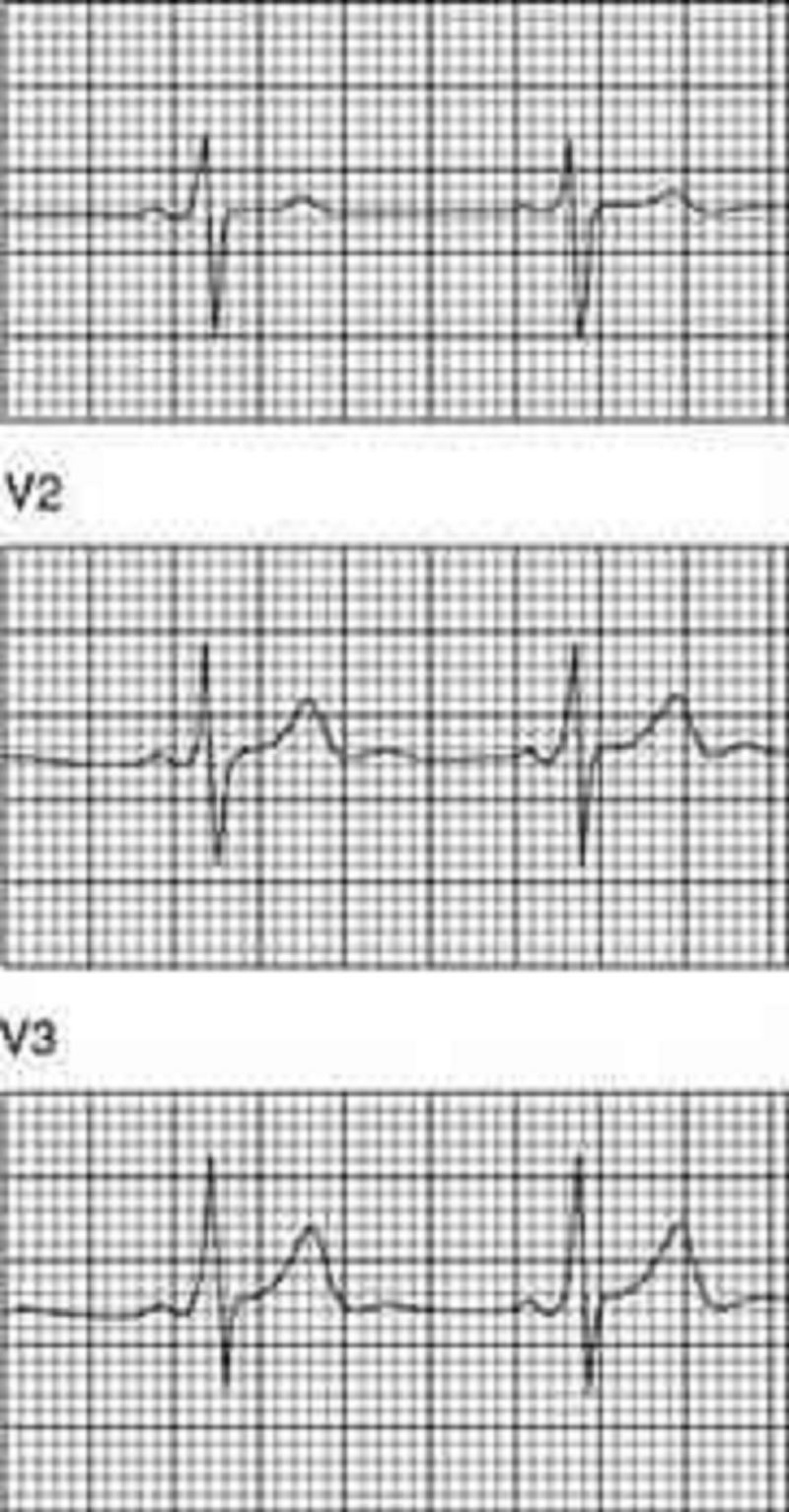
81. An 18-year-old male complains of fever and transient pain in both knees and elbows. The right knee was red and swollen for 1 day during the week prior to presentation. On physical examination, the patient has a low-grade fever. He has a III/VI, high pitched, apical systolic murmur with radiation to the axilla, as well as a soft, mid-diastolic murmur heard at the base. A tender nodule is palpated over an extensor tendon of the hand. There are pink erythematous lesions over the abdomen, some with central clearing. The following laboratory values are obtained: Hct: 42 WBC: 12,000/µL with 80% polymorphonuclear leukocytes, 20% lymphocytes ESR: 60 mm/h The patient’s ECG is shown below. Which of the following tests is most critical to diagnosis?
B. Antistreptolysin O antibody
A. Blood cultures
D. Antinuclear antibodies
C. Echocardiogram
E. Creatine kinase
82. A 50-year-old construction worker continues to have elevated blood pressure of 160/95 even after a third agent is added to his antihypertensive regimen. Physical examination is normal, electrolytes are normal, and the patient is taking no over-the-counter medications. Which of the following is the best next step for this patient?
B. Evaluate for Cushing syndrome.
A. Check pill count
D. Obtain a renal angiogram.
C. Check chest x-ray for coarctation of the aorta.
E. Obtain an adrenal CT scan.
83. A 35-year-old male complains of substernal chest pain aggravated by inspiration and relieved by sitting up. Lung fields are clear to auscultation, and heart sounds are somewhat distant. Chest x-ray shows an enlarged cardiac silhouette. Which of the following is the best next step in evaluation?
B. Cardiac catheterization
A. Right lateral decubitus chest x-ray
D. Serial ECGs
C. Echocardiogram
E. Thallium stress test
84. A 32-year-old male presents to your office with concern about progressive fatigue and lower extremity edema. He has experienced decreased exercise tolerance over the past few months, and occasionally awakens coughing at night. Past medical history is significant for sickle cell anemia and diabetes mellitus. He has had multiple admissions to the hospital secondary to vasoocclusive crises since the age of three. Physical examination reveals a displaced PMI, but is otherwise unremarkable. ECG shows a first degree AV block and low voltage. Chest x-ray shows an enlarged cardiac silhouette with clear lung fields. Which of the following would be the best initial diagnostic approach?
B. Order brain-natriuretic peptide (BNP)
A. Order serum iron, iron-binding capacity, and ferritin level.
C. Order CT scan of the chest.
D. Arrange for placement of a 24-hour ambulatory cardiac monitor.
E. Arrange for cardiac catheterization.
85. You are performing medical screening of new military recruits when an 18-year-old male reports several episodes of palpitation and syncope over the past several years. Physical examination is unremarkable. An ECG is obtained with excerpts shown below. What is the most likely diagnosis?
B. Congenital prolonged QT syndrome
A. Prior myocardial infarction secondary to coronary artery disease
C. Hypertrophic obstructive cardiomyopathy (HOCM)
D. Preexcitation syndrome (Wolff-Parkinson-White)
E. Rheumatic mitral stenosis
86. A 26-year-old primigravida at 20th week gestation presents to the emergency room with a sudden onset of tearing chest pain radiating to her back and left arm. The patient is pale and diaphoretic. Her PR: 116/min; BP: 192/ 104 in left arm, and 123/65 in right arm; RR: 36/min. Her cardiac examination reveals a diastolic murmur along the left sternal border. Her previous prenatal care is not known. She is a smoker with a 10 pack/year history and drinks alcohol. Her ECG reveals mild left axis deviation and ST segment depression in lead II, Ill, and AVF. What is the most appropriate next step in the management of this patient?
B. T ransesophageal echocardiogram (TEE)
A. Obtain CK-MB and T roponin levels
D. Antihypertensive treatment
C. Transthoracic echocardiogram (TTE)
E. CT scan of chest
87. A 45-year-old mildly overweight male recovering from an anterior wall myocardial infarction develops sudden onset of left-sided chest pain. He appears agitated and restless. Two minutes later, he is unresponsive. His pulse is not palpable and ECG monitor shows sinus tachycardia at the rate of 130/min. He presented five days earlier with substernal chest pain and diaphoresis. He has had no dyspnea, extremity swelling or palpitations since admission. His past medical history is significant for diabetes mellitus type 2. Which of the following is the most likely diagnosis?
B. Ventricular free wall rupture
A. Interventricular wall rupture
D. Recurrent ischemia
C. Pulmonary infarction
E. Right ventricular infarction
88. A 53-year-old woman presents to the physician's office with a 3-week history of burning, substernal chest pain that usually comes on with exertion and is relieved with rest. The pain does not radiate to the arms or jaw. Her past medical history is significant for bronchial asthma, type 2 diabetes, hypercholesterolemia, and hypertension. A diagnosis of stable angina is suspected, and the patient is scheduled for an exercise EKG stress test. Which of her medications should be withheld 24 hours before the test?
B. Hydrochlorothiazide
A. Atenolol
D. Ramipril
C. Simvastatin
E. Metformin
89. A 50-year-old Caucasian male returns to the clinic for the evaluation of his blood pressure control. He was diagnosed with essential hypertension one year ago. He claims compliance with his reduced salt intake diet. He is currently on a thiazide diuretic and a beta-blocker. His past medical history is significant for angina, which is always relieved with sublingual nitroglycerine, but he has not had an attack of angina in over a month. He has never had a myocardial infarction. He lives with his wife and two children. He quit smoking two years ago, but previously had a 25-pack year history. He drinks 4 bottles of wine per week. His blood pressure is 150/90 mm Hg What is the best next step in management?
B. Start an ACE inhibitor
A. Admit him to the hospital to control his blood pressure
C. Increase the dose of thiazide diuretic
D. Reduction in alcohol intake
E. Reassurance and repeat measurement in 2 weeks
90. A 34-year-old Caucasian woman presents to your office with dyspnea and severe chest pain after returning from a trip to Central Asia. The pain is localized on the left side and increases with inspiration. She also had one episode of hemoptysis. She does not smoke or consume alcohol. She is sexually active with one partner and uses oral contraceptives. Her father died of a myocardial infarction at 52 years of age. Her temperature is 36.7C (98.F), pulse is 100/min, respirations are 28/min, and blood pressure is 110/66 mmHg. Which of the following most likely accounts for this patient's chest pain?
B. Myocardial ischemia
A. Pulmonary artery distention
D. Pleural infection
C. Pericardial inflammation
E. Pulmonary infarction
91. An 82-year-old male presents for evaluation of chronic back pain. On physical examination, he is found to have a blood pressure of 160/85 mmHg while supine and 135/70 mmHg while standing. He is otherwise healthy; his only medicine is occasional ibuprofen for back pain. Which of the following age-related changes best explains the observed finding?
B. Decreased left ventricular contractility
A. Increased left ventricular wall stiffness
C. Decreased baroreceptor responsiveness
D. Decreased stress-mediated catecholamine release
E. Decreased glomerular filtration rate
92. A 64-year-old diabetic with a long history of uncontrolled hypertension is admitted for chest pain. ECG reveals elevated ST segments in the anterior wall leads. Cardiac enzymes are elevated and the patient is admitted to the ICU for supportive care. He receives low molecular weight heparin and is placed on a nitroglycerin drip. He continues to have chest pain and requires intravenous morphine. Three days later, the patient is transferred to the floor and he remains on bed rest. During the night the nurse on call informs you that the patient has a cold leg. On examination, the left leg is cold and there are no distal pulses. There is minimal swelling and the leg appears mottled. Emergency vascular surgery consult was placed and the appropriate treatment was given Which of the following should also be considered in this patient?
B. Chest x-ray
A. Venous duplex study
D. V/Q scan
C. Echocardiogram
E. D-dimer level
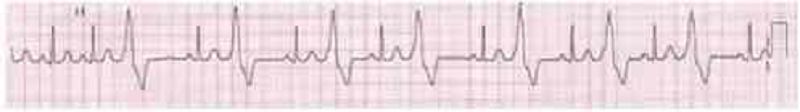
93. A 66-year-old male is rushed to the emergency department because he feels dizzy and light-headed. He denies chest pain or palpitations. He has a history of hypertension and diabetes. His blood pressure is 116/62 mm Hg and his pulse is 35-40/min. He is alert, awake, and fully oriented. He is breathing comfortably and does not appear to be in any distress. His extremities are slightly cold and capillary refill is 3 seconds. His EKG is shown below.Which of the following is the most appropriate next step in management?
B. Intravenous atropine
A. Intravenous adenosine push
C. Intravenous epinephrine
D. Intravenous amiodarone
E. Transcutaneous pacing
94. A 34-year-old woman is referred by an OB-GYN colleague for the onset of fatigue and dyspnea on exertion 1 month after her second vaginal delivery. Physical examination reveals a laterally displaced PMI, elevated jugular venous pressure and 2+pitting lower extremity edema. Echocardiogram shows systolic dysfunction with an ejection fraction of 30%. Which statement most accurately describes her condition?
B. About half of similar patients will recover completely.
A. This disease may occur unexpectedly years after pregnancy and delivery.
C. The condition is idiosyncratic; the risk of recurrence with a future pregnancy is no greater than average
D. This condition will require a different therapeutic approach than the typical dilated cardiomyopathy.
E. This condition will require endomyocardial biopsy for diagnosis.
95. A 72-year-old Caucasian male presents with shortness of breath that awakens him at night. At baseline he is able to walk less than a block before stopping to catch his breath. Physical examination findings include bilateral basilar rales and neck vein distention. The patient has a known history of congestive heart failure, and his last echocardiogram revealed an ejection fraction of 25%. The patient is compliant with a medication regimen including an ACE inhibitor, beta-blocker, and loop diuretic. Blood pressure is well controlled. What additional treatment should you begin next?
B. Aspirin
A. Spironolactone
D. Warfarin
C. Amlodipine
E. Hydralazine and isosorbide dinitrate
96. A 68-year-old male was intubated in the emergency room because of pulmonary edema. Stat echocardiogram reveals an ejection fraction of 45% and severe mitral regurgitation. In spite of aggressive diuresis with furosemide, the patient continues to require mechanical ventilation secondary to pulmonary edema. What is the best next step in treating this patient?
B. Place an intra-aortic balloon pump.
A. Arrange for mitral valve replacement surgery.
C. Begin metoprolol.
D. Begin a second loop diuretic.
E. Begin intravenous enalapril.
97. A 30-year-old female presents with a chief complaint of palpitations. A 24-hour Holter monitor shows occasional unifocal premature ventricular contractions and premature atrial contractions. Which of the following is the best management for this patient?
B. Beta-blocker therapy
A. Anxiolytic therapy
D. Quinidine
C. Digoxin
E. Reassurance, no medication
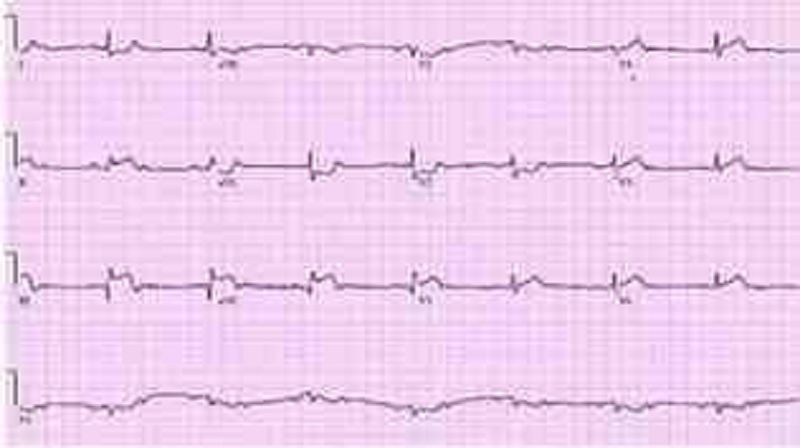
98. A 70-year-old Caucasian man comes to the emergency department because of the sudden onset of nausea, vomiting, diaphoresis, and chest pain. His other medical problems include hypertension, diabetes mellitus-type 2, and aortic stenosis. He has smoked one-and-a-half packs of cigarettes daily for 30 years and drinks 4 ounces of alcohol daily. His temperature is 37.2 C (99 F), blood pressure is 100/60 mmHg, pulse is 60/min, and respirations are 18/min. The patient's pulse oximetry showed 98% at room air. Examination shows normal first and second he sounds. Lungs are clear to auscultation. His EKG is shown below. Which of the following is the most likely mechanism of this patient's condition?
B. Occlusion of the left circumflex artery
A. Occlusion of the right coronary artery
D. Inflammation of the pericardium
C. Occlusion of the left anterior descending artery
E. Vasospasm of the left circumflex artery
99. A 36-year-old man presents to your office for a routine pre-employment physical. He has no complaints except for occasional morning headaches. His father died suddenly at the age of 54. The patient's blood pressure is 175/103 mmHg in the right arm and 180/105 in the left arm. His heart rate is 82/min. His lungs are clear bilaterally and his heart sounds are normal. Bilateral, non-tender, upper abdominal masses are palpated on exam. His hemoglobin level is 15.2 g/dl and creatinine concentration is 0.8 mg/dl. Which of the following is most likely to diagnose this patient's condition?
B. Abdominal ultrasound
A. Urine metanephrines
D. Aldosterone: renin ratio
C. Captopril-enhanced radionuclide renal scan
E. 24-hour urine cortisol
100. A 52-year-old man complains of frequent chest pain. The pain typically occurs at night and is described as retrosternal and burning in quality. He leads a sedentary lifestyle but does not smoke or drink alcohol. His past medical history includes a chronic cough and occasional hoarseness. He does not take any medications. His BMI is 28.5 kg/m2 ECG stress testing reveals 1 mm ST segment depression in the inferior leads at 90% of predicted maximal heart rate. He did not experience chest pain during the stress test. Which of the following is most likely to relieve this patient's chest pain?
B. Nitroglycerin
A. Ibuprofen
D. Alprazolam
C. Propranolol
E. Omeprazole
101. A 54-year-old woman presents for a routine physical. She has no complaints. She has no history of hypertension, diabetes, hypercholesterolemia, or heart disease, and she does not use tobacco, alcohol or drugs. On physical examination, her pulse is irregular. There are no murmurs. Her lungs are clear to auscultation and her legs are free of edema. An EKG shows atrial fibrillation with a heart rate of 72 beats per minute. An echocardiogram is unremarkable except for evidence of atrial fibrillation. What is the most appropriate management of this patient?
B. Heparin followed by warfarin
A. Warfarin and clopidogrel
D. Aspirin alone
C. Low-molecular weight heparin
E. Warfarin to maintain an INR of 2 to 3
102. A middle-aged man was recently diagnosed with hypertension. The antihypertensive medication prescribed to him enhances natriuresis, decreases serum angiotensin II concentration, and decreases aldosterone production. This medication most likely belongs to which of the following drug classes?
B. Direct renin inhibitor
A. Angiotensin receptor blocker
D. Loop diuretic
C. Aldosterone receptor antagonist
E. Alpha-adrenergic blocker
103. A 63-year-old woman complains of leg swelling that is especially bothersome in the evening. She also complains of chronic cough and exertional dyspnea. She has been smoking one pack of cigarettes per day for the past 30 years. She also drinks one or two cans of beer on weekends. Her medical history is significant for a hospitalization for a "chest infection" two years ago, for which she was treated with antibiotics, steroids, and inhalers. She also reports having been diagnosed with hypertension, but says that she has never taken medications for it. On physical examination, her blood pressure is 160/90 mmHg and her heart rate is 80/min. Chest examination reveals bilateral scattered wheezes and prolonged expirations. Her jugular venous pulsation is seen 2 cm above the sternal angle with the head of the bed elevated 30•. Her abdomen is soft and non-distended. On examination of her lower extremities, you note bilateral pitting edema and dilated, tortuous, superficial veins. Which of the following is most likely to relieve this patient's edema?
B. Frequent leg elevation
A. Smoking cessation
D. Control of hypertension
C. Dietary sodium restriction
E. Oxygen therapy
104. A 32-year-old man develops severe nausea and vomiting after returning from a party. He also complains of chest pain that is more intense than any pain he has previously experienced. His past medical history is significant for HIV infection, alcohol abuse, and alcoholic hepatitis. He admits to using cocaine regularly. His temperature is 37.8C (100.F), pulse is 120/min, respirations are 24/min, and blood pressure is 100/60 mmHg. Examination reveals injected conjunctivae and bilateral dilated pupils. Chest X-ray demonstrates a widened mediastinum and left-sided pleural effusion. EKG is unremarkable. The pleural fluid is found to have an elevated amylase content. Which of the following is the most likely diagnosis in this patient?
B. Peptic ulcer disease
A. Acute pancreatitis
C. Esophageal perforation
D. Myocardial ischemia
E. Pulmonary embolism
105. A 45-year-old male is brought to the ER with sudden onset palpitations and chest tightness. His past medical history is significant for hypertension, gout and diabetes mellitus. Cardiac monitoring shows atrial fibrillation at a rate of 120-140/min. As the nurse is attempting to establish IV access, the patient becomes unresponsive. There is no palpable pulse over the carotids or femoral arteries. The cardiac monitor still shows atrial fibrillation at the same rate. What is the best next step in management?
B. Defibrillation
A. Synchronized cardioversion
D. Chest compressions
C.IV lidocaine
E. Arterial blood gas analysis
106. A 24-year-old male experiences syncope while shoveling snow. He regained consciousness within one minute. He has been having some shortness of breath and chest pains recently, mostly related to exercise. He denies any illicit drug use. His temperature is 37.2 C (98.9 F), and blood pressure is 126/76 mm Hg, pulse is 76/min and respirations are 14/min. Physical examination shows a well-built male in no apparent distress. Lungs are clear. A crescendo-decrescendo systolic murmur is heard along the left sternal border without carotid radiation. Chest X-ray is normal. Which of the following is the most likely cause of his syncopal episode?
B. Left ventricular hypertrophy
A. Atrioventricular conduction delay
D. Coronary atherosclerosis
C. Aortic dissection
E. Mitral valve degeneration
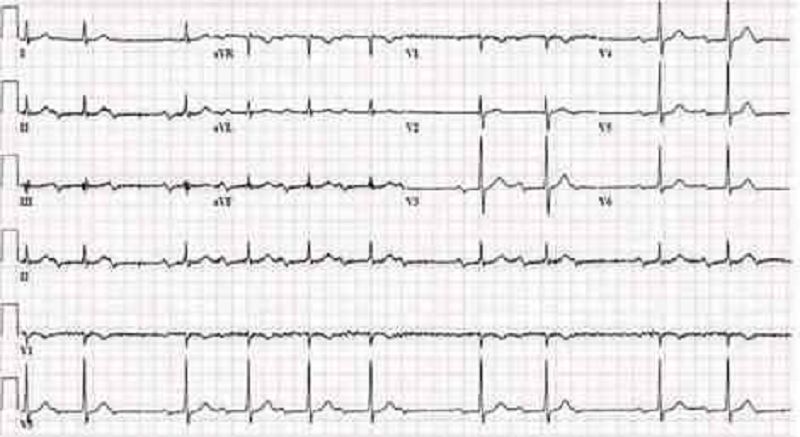
107. A 56-year-old diabetic female comes to the clinic with complaints of dizziness which has been going on for 3 weeks. She denies any dyspnea or diaphoresis. She says her blood glucose is well controlled and denies any allergy. Her BP is 155/90 mm Hg. Her chest-x ray is unremarkable and her blood work is normal. The ECG is recorded below.What is the most likely diagnosis?
B. Mobitz type II heart block
A Mobitz type I heart block
D. Atrial fibrillation
C. Complete heart block
E. First degree heart block
108. A 54-year-old overweight man wakes up in the middle of the night with substernal discomfort that he describes as a burning sensation. He also complains of left-sided neck pain and feels sweaty and short of breath. He has never had similar pain before. Prior to going to bed he had eaten a big meal. His past medical history is significant for diabetes and hypertension. Which of the following physical findings is most consistent with this patient's clinical presentation?
B. Ejection-type systolic murmur
A Fixed splitting of S2
D. Fourth heart sound
C. Friction rub
E. Pulsus paradoxus
109. A 56-year-old male is hospitalized following an acute anterior wall myocardial infarction that was treated with thrombolytic therapy 4 days ago. On day 4 of his hospitalization, he develops recurrent chest pain, similar in quality and severity to his previous pain. Sublingual nitroglycerin is administered but does not help. His blood pressure is now 140/90 mmHg and his heart rate is 82/min. S 1 and S2 are normal, and there are no cardiac murmurs or rubs. Lungs are clear to auscultation. Which of the following laboratory tests would be most useful to send in this setting?
B. Lactate dehydrogenase (LDH)
A Troponin T
D. Alkaline phosphatase
C. CK-MB
E. Dobutamin
110. A 64-year-old male presents to the emergency department with chest pain. An ECG reveals ST elevations in leads II, Ill, and aVF. Thrombolytic therapy and heparin are administered, and the pain resolves. Eight hours after admission, the patient develops hypotension. He denies recurrence of chest pain. His temperature is 37.5°c (99.6.F), blood pressure is 84/55 mm Hg, pulse is 90/min, and respirations are 15/min. His medications include a nitroglycerin drip, beta-blocker, aspirin, heparin, and simvastatin. Examination reveals an elevated jugular venous pressure of 14 cm, cold clammy extremities, and clear lung fields. Based on this information, what is the next best step in this patient's management?
B. Administer normal saline bolus and stop nitroglycerin
A Start dopamine
C. Administer intravenous furosemide
D. Initiate temporary cardiac pacing
E. Stop nitroglycerin and start dobutamine drip
111. A 33-year-old woman is undergoing an elective, open cholecystectomy after 2 episodes of acute calculous cholecystitis. She suddenly becomes hypotensive, and a generalized rash is noted. Her past medical history is significant for a hypotensive episode 8 weeks ago while having protected sex with her new partner. Which of the following is the most probable cause of this patient's condition?
B. Coagulation abnormality
A. Acute blood loss
C. Allergic reaction@ D. Septic shock
C. Allergic reaction
E. Pulmonary embolism
112. A 68-year-old man presents to the emergency department complaining of left lower extremity pain. He says that he first noticed a tingling sensation in his leg 3 hours ago, and since that time it has become increasingly painful. Over the past hour, he says, the skin on his leg has started to change color. His medical history is significant for hypertension, diabetes mellitus, atrial fibrillation, and major depressive disorder. He cannot remember his medication list at this time. On physical examination, his blood pressure is 127/74 mm Hg and his heart rate is 102/min. His left lower extremity is cool and pale below the level of the knee. Neither the posterior tibial nor the dorsalis pedis pulse is palpable. Which medication could have prevented this acute problem?
B. Metoprolol
A. Aspirin
C. Clopidogrel
D. Warfarin
E. Diltiazem
113. A 75-year-old patient presents to the ER after a syncopal episode. He is again alert and in retrospect describes occasional substernal chest pressure and shortness of breath on exertion. His blood pressure is 110/80 and lungs have a few bibasilar rales. Which auscultatory finding would best explain his findings?
B. A diastolic decrescendo murmur heard at the mid-left sternal border
A. A harsh systolic crescendo-decrescendo murmur heard best at the upper right sternal border
C. A holosystolic murmur heard best at the apex
D. A midsystolic click
E. A pericardial rub
114. A 72-year-old male comes to the office with intermittent symptoms of dyspnea on exertion, palpitations, and cough occasionally productive of blood. On cardiac auscultation, a low-pitched diastolic rumbling murmur is faintly heard at the apex. What is the most likely cause of the murmur?
B. Long-standing hypertension
A. Rheumatic fever as a youth
D. A congenital anomaly
C. A silent MI within the past year
E. Anemia from chronic blood loss
115. You are helping with school sports physicals and see a 16-year-old boy who has had trouble keeping up with his peers. Which of the following auscultatory findings suggests a previously undiagnosed ventricular septal defect?
B. A systolic murmur at the pulmonic area and a diastolic rumble along the left sternal border.
A. A systolic crescendo-decrescendo murmur heard best at the upper right sternal border with radiation to the carotids; the murmur is augmented with exercise.
C. A holosystolic murmur at the mid-left sternal border.
D. A diastolic decrescendo murmur at the mid-left sternal border.
E. A continuous murmur through systole and diastole at the upper left sternal border
116. A 53-year-old male presents to your office with a two-day history of right calf pain and swelling. He describes the pain as constant and states that it is exacerbated by knee flexion. He has a history of past IV drug abuse, endocarditis, and stroke. He is currently wheelchair-bound secondary to strokerelated left-sided hemiparesis. On physical examination, his blood pressure is 140/90 mmHg and his heart rate is 100/min. There is no jugular venous distention or hepatojugular reflux. His chest is clear to auscultation but his abdomen is enlarged with shifting dullness and a fluid wave, suggestive of ascites. His liver is palpable 3 cm below the right costal margin. His spleen is also palpable. On examination of his lower extremities, you note right-sided calf swelling and tenderness. Which of the following is the most likely cause of this patient's ascites?
B. Pulmonary embolism
A. Right-sided heart failure
D. Chronic liver disease
C. Protein C deficiency
E. Paradoxical embolism
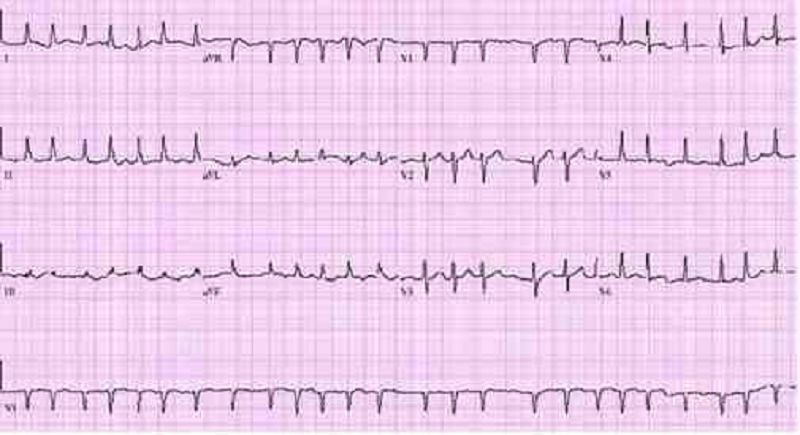
117. A 46-year-old man comes to the ER because of weakness and chest tightness. He has had these symptoms for the past one hour. He denies any past medical history. He does not smoke or drink alcohol. His father had a myocardial infarction at 68 years of age and his mother has myasthenia gravis. His EKG is shown on the slide below.The patient should be evaluated for which of the following?
B. Hyperthyroidism
A. Cushing syndrome
D. High-frequency deafness
C. Aortic dissection
E. High-range proteinuria
118. A 64-year-old male presents to the ER with chest pain. His history is significant for a hospitalization 2 weeks ago for an acute myocardial infarction. The patient reports that he is afraid his heart attack is recurring. He localizes the pain to the middle of the chest, and says that he can only take shallow breaths because deep breaths make the pain worse. Leaning forward in his chair makes the pain somewhat better. He notes some associated neck pain and general malaise, but denies shortness of breath, palpitations, syncope or cough. His temperature is 36.7C (98.F), blood pressure is 135/84 mmHg and heart rate is 90/min. EKG shows ST segment elevations in all limb and precordial leads except in aVR, where ST depression is seen. Which of the following is the best next step in the management of this patient?
B. Anticoagulation with warfarin
A. Anticoagulation with heparin
D. Broad-spectrum antibiotics
C. Nitroglycerin and beta-blockers
E. Non-steroidal antiinflammatory agent
119. A 15-year-old female, who has recently emigrated from Asia, is found to have a heart murmur during her routine physical examination. She has no current complaints. She had a febrile illness with joint swelling and pain approximately one year ago. She plays table tennis and swims every weekend. Her blood pressure is 120/70 mmHg and her heart rate is 70/min, regular. Cardiac auscultation shows a loud first heart sound and mid-diastolic rumble at the apex. Her lungs are clear to auscultation. Which of the following is the best treatment for this patient at this point?
A. Penicillin
B. Metoprolol
D. Digoxin
C. Enalapril
E. Warfarin

120. A 46-year-old man presents to the emergency department with difficulty breathing and chest discomfort. His pain worsens with inspiration but does not radiate. He says that he has never had symptoms like this before. His past medical history is unremarkable. He works as a long-haul truck driver. On physical examination, his blood pressure is 110/70 mmHg, his heart rate is 110/min, his respiratory rate is 31/min, and his temperature is 36.7C (98.F). ECG reveals sinus tachycardia but no ischemic ST-segment or T-wave changes. His chest X-ray is shown below.What is the most likely diagnosis in this patient?
B. Myocardial infarction
A. Ascending aortic dissection
D. Pulmonary embolism
C. Pneumothorax
E. Pleural effusion
121. A 60-year-old white man comes into the Emergency Room with intensive retrosternal pain that began ten minutes ago. He has never had such pain before. His past medical history is significant for diabetes mellitus, type 2, controlled with diet His blood pressure is 150/95 mmHg and HR is 80/min. You give him one chewable tablet of aspirin and two sublingual tablets of nitroglycerin with a 5minute interval. After the second tablet of nitroglycerin, the pain is greatly relieved. What is the most important mechanism responsible for pain relief in this patient?
B. Increased cardiac contractility
A. Increase in coronary blood flow
C. Dilation of resistance vessels
D. Dilation of capacitance vessels
E. Change in the activity of baroreceptors
122. A 34-year-old male who recently immigrated from Brazil presents with a 5-month history of exertional dyspnea without associated chest pain, palpitations, dizziness, or syncope. His past medical history is significant for an episode of megacolon, which was treated 2 years ago. On physical examination, there is 1+ pedal edema and mild jugular venous distention. Cardiac exam is significant for the presence of an S3, but no murmurs are heard. Chest x-ray reveals prominent cardiomegaly. Based on these findings, which of the following is most likely causing his symptoms?
B. Coronary artery disease
A Diphtheric myocarditis
D. Giant cell myocarditis
C. Protozoal disease
E. Rickettsial myocarditis
123. A 54-year-old male with a past medical history of type 2 diabetes mellitus comes to the emergency department complaining of shortness of breath. His blood pressure is 146/92 mmHg, respiratory rate is 26/min, and oxygen saturation is 87% on room air. Cardiac auscultation findings over the apex are given below. Based on the physical findings, which of the following is the best initial therapy for this patient?
B. Intravenous beta-blockers
A. Inhaled bronchodilators
D. Intravenous diuretics
C. Intravenous diltiazem
E. Pericardiocentesis
124. Neighbors find a 65-year-old male unconscious in his garden and immediately call EMS. The man is intubated at the scene. In the ER, he develops sustained ventricular tachycardia and requires cardioversion. He is started on an antiarrhythmic agent and, once recovered, is discharged to home. Three months later he returns to his physician complaining of dyspnea on exertion. Chest-x ray reveals bilateral lung fibrosis. All cultures are negative and lung biopsy reveals lipoid pneumonitis. Which of the following medications is most likely responsible for his current condition?
B. Amiodarone
A. Procainamide
D. Quinidine
C. Lidocaine
E. Digoxin
125. A 12-year-old African American male is found to have a murmur during a routine sports physical. He has a family history of sudden death at a young age. It is a harsh crescendo-decrescendo murmur that begins after S1 and is best heard at the left lower sternal border. Valsalva maneuver intensifies the murmur. Which of the following is the most likely mitral valve abnormality in this patient?
B. Rupture of chordae tendinae
A. Dilated mitral valve annulus
D. Mitral annulus calcifications
C. Abnormal mitral leaflet motion
E. Prolapse of the mitral valve
126. A 36-year-old female presents to the emergency room complaining of chest pain that started suddenly while she was shopping at the mall. She also reports shortness of breath, palpitations and diaphoresis. The pain is retrosternal and radiates to the left arm. There are no aggravating or relieving factors. On review of systems, the patient reports having had a runny nose, sore throat and dry cough for the past 3 days. Her past medical history is significant for panic attacks, for which she takes paroxetine, and dysfunctional uterine bleeding, for which she takes estrogen. Her family history is significant for the sudden death of her father at age 44 from a heart attack. Social history reveals that she has smoked one pack of cigarettes per day for the past 15 years. Which of the following is the most appropriate initial therapy for this patient?
B. Heparin
A. Lorazepam
D. Ibuprofen
C Aspirin
E. Acetaminophen
127. A 65-year-old female is admitted to the hospital with increasing shortness of breath, weight gain and lower extremity edema. She has a history of hypertension, nonischemic cardiomyopathy with an ejection fraction of 30%, and hyperlipidemia. Her home medications include oral aspirin, digoxin, furosemide, metoprolol, lisinopril and atorvastatin. She is started on intravenous furosemide. On day three of hospitalization telemetry reveals six beats of wide complex ventricular tachycardia. Physical examination now shows decreased leg edema and clear lungs. Which of the following is the most appropriate next step in the management of this patient's tachycardia?
B. Add metolazone
A. Add spironolactone
D. Discontinue atorvastatin
C. Measure serum electrolytes
E. Discontinue metoprolol
128. A 34-year-old male presents with palpitations for the past 4 hours without associated chest pain, shortness of breath, fevers, or chills. His medical history is significant for Wolff-Parkinson-White syndrome for the past ten years and three prior episodes of supraventricular tachycardia. He does not smoke cigarettes, and drinks alcohol on social occasions. He does report having had five cans of beer while at a party last night. On examination, his blood pressure is 120/80 mmHg and his pulse is irregularly irregular. EKG shows atrial fibrillation with a rate of 160/min. What is the best next step in the management of this patient?
B. Verapamil
A Digoxin
D. Procainamide
C. Lidocaine
D. Procainamide@ E. Adenosine
129. A 45-year-old male presents to your clinic with complaints of pleuritic chest pain. He says he is a heavy smoker and has been having intermittent cough for the past 2 weeks. His blood work is normal and his chest x ray is clear. EKG reveals a normal sinus rhythm with a heart rate of 68. He does have a PR interval > 0.2 seconds. The next step in the management of his arrhythmia is:
B. Atenolol
A. Observation
D. Electrophysiology study
C. Pacemaker
E. Cardiac catheterization
130. A 21-year-old man comes to the ER with palpitations and dizziness that began suddenly one hour ago. He notes having similar past episodes provoked by fatigue or strong emotions. He says he can usually stop the episodes by putting his head into cold water or squatting and taking a deep breath. However, these techniques are not working this time. Presently, his blood pressure is 60/30 mmHg and his heart rate is 240/min. He is diaphoretic with cold extremities. An EKG rhythm strip shows a regular, narrow complex tachycardia. Which of the following is the best next step in managing his condition?
B. Procainamide
A. Adenosine
D. Digoxin
C. Verapamil
E. DC cardioversion
131. A 64-year-old Caucasian male presents to the Emergency Room with a sharp, left-sided chest pain. He says that the pain is worse when he takes deep breaths, but he gets relief with leaning forward. He had an acute non-ST elevation myocardial infarction six months ago and had undergone angioplasty for the right coronary artery. His other medical problems include: diabetes, hypertension, hyperlipidemia, peripheral neuropathy, diabetic retinopathy, paroxysmal atrial fibrillation, hypothyroidism, and chronic renal insufficiency. His vital signs are BP 142/86 mmHg, PR 78/min, RR 16/min, and T 36.1 C (97F). On examination, you find a pericardial rub. EKG shows diffuse ST elevation. Lab results are: Hb 9.0 g/dl WBC 8,000/cmm Platelets 210,000/cmm Blood Glucose 248 mg/dl Serum Na 135 mEq/L Serum K 5.8 mEq/L Bicarbonate 17 mEq/L BUN 86 mg/dl Serum Creatinine 4.4 mg/dl Which of the following is the most appropriate management of this patient?
B. Corticosteroids
A. NSAIDs
D. Hemodialysis
C. Pericardiocentesis
E. Echocardiography
132. A 63-year-old woman with a long history of hypertension faints after experiencing the sudden onset of severe chest pain that radiates to her back. She is rushed to the emergency room. Upon arrival she is agitated and demands quick pain relief. Her heart rate is 110/min and blood pressure is 90/50 mmHg. Jugular veins are distended. An intraarterial catheter shows significant variation of systolic blood pressure related to the respiratory cycle. Chest x-ray reveals widening of the mediastinum. Which of the following is the most likely cause of this patient's syncope?
B. Intravascular volume loss
A. Papillary muscle dysfunction
D. Vagal hyperactivity
C. Pericardia! Fluid accumulation
E. Cardiac tachyarrhythmia
133. A 32-year-old woman is brought to the emergency department with excruciating chest and neck pain. She is 6'2" and has long extremities. Her hand joints show significant extensibility. Which of the following additional findings is also likely in this patient?
B. Early diastolic murmur
A Fourth heart sound (S4)
D. Fixed splitting of the second heart sound (S2)
C. Opening snap
E. Kussmaul's sign
134. A 53-year-old Caucasian woman comes to the physician for a routine health maintenance examination. Recently, she noticed a mild hand tremor while performing some fine tasks, like pouring out the tea. She says that the tremor disappears for a while after drinking a glass of wine. Her past medical history is insignificant. Her blood pressure is 160/90 mmHg and heart rate is 80/min. Physical examination is insignificant. Which of the following medications is the best choice to treat this patient's hypertension?
B. Verapamil
A. Propranolol
D. Hydrochlorothiazide
C. Amlodipine
E. Enalapril
135. A 47-year-old male was brought to the emergency room with chest pain of acute onset. The pain was associated with nausea, vomiting, and diaphoresis. He has a history of diabetes, hypertension, and hyperlipidemia. ECG reveals ST segment elevation in the anterolateral leads and ventricular premature beats (VPBs). The patient dies within the first hour after the arrival to emergency room. What is the most likely pathophysiologic mechanism responsible for this patient's death?
B. Reentry
A. Electro-mechanic dissociation
D. Increased automaticity
C. Full conduction block
E. Asystole
136. A 60-year-old Caucasian man presents to the office with a 2-week history of worsening shortness of breath and decreased exercise tolerance. His breathlessness is worse at night. He thinks his legs are swelling up. He has hypertension, coronary artery disease and chronic obstructive pulmonary disease. He used to drink heavily and smoke 1 pack of cigarettes daily but has quit recently, although he still reports occasionally drinking a "few beers." He currently denies any chest pain, palpitations or cough. His temperature is 37.5C (99.5 F), blood pressure is 110/70 mm Hg, pulse is 96/min and respirations are 22/min. The pertinent physical findings are an S3, bibasilar crackles, JVP 10 cm above the sternal angle, mild hepatomegaly, and 4+ pitting lower extremity edema. The patient is immediately treated with oxygen, intravenous furosemide, and nitrates Which of the following markers is most likely elevated in this patient?
B. Mean corpuscular volume
A. Ejection fraction
D. Urine sodium
C. B-type natriuretic peptide
E. Neutrophil count
137. A 69-year-old male presents to the emergency department with severe pain in the back of his chest that began suddenly 6 hours ago, and 2 hours of difficulty walking due to leg weakness. He has never had such symptoms before. His past medical history is significant for hypertension, bleeding peptic ulcers, and deep vein thrombosis requiring inferior vena cava filter placement. He drinks 6-8 cans of beer each weekend and does not smoke cigarettes or use illicit drugs. Blood pressure taken from his right arm is 210/120 mmHg. His heart rate is 120/min and regular. Chest x-ray reveals a right-sided pleural effusion. EKG shows sinus tachycardia. What is the most likely diagnosis?
B. Myocardial infarction
A. Angina pectoris
D. Aortic dissection
C. Acute pericarditis
E. Pulmonary embolism
138. A 34-year-old male with a history of mitral valve prolapse and mitral regurgitation presents with one week of intermittent fevers and increasing fatigue. He was punched in the face during a street fight two weeks ago. On admission he receives empiric intravenous vancomycin and gentamicin. Three days later, three out of four blood cultures grow Streptococcus viridans highly sensitive to penicillin. Which of the following is the best next step in managing this patient?
B. Switch antibiotics to IV ceftriaxone
A. Continue current regimen
D. Switch antibiotics to oral penicillin V
C. Switch antibiotics to IV aminoglycosides
E. Switch antibiotics to oral amoxicillin/clavulanate
139. A 10-year-old boy is brought to the ER by his mother because he has lost consciousness, while playing in the yard. He regained his consciousness quickly without following confusion. He never had such an episode before. His past medical history is significant for impaired hearing since birth and one episode of pneumonia three years ago, which required hospitalization. The family history is significant for a sudden cardiac death, in his cousin, at the age of 13. Physical examination is unremarkable. Blood pressure is 110/70 mmHg. Heart rate is 70/min, regular. Which of the following medication is most appropriate for this patient?
B. Verapamil
A. Propranolol
D. Ethosuximide
C. Quinidine
E. Phenobarbital
140. A 57-year-old male presents to your office with a two-week history of fever, chills, and generalized weakness. His medical history is significant for a hospitalization for pyelonephritis requiring IV antibiotics six months ago. He also recently underwent cystoscopy for evaluation of persistent dysuria. His past medical history is also significant for an episode of rheumatic fever as a child and Hodgkin's lymphoma treated with chemotherapy 10 years ago. On examination, his temperature is 37.8°C (100°F), blood pressure is 150/86 mmHg, pulse is 98/min and regular, and respirations are 16/min. The patient appears slightly diaphoretic. You note a new II/VI systolic murmur and tender erythematous lesions affecting several fingertips. The remainder of the physical examination is unremarkable. Which of the following bacteria is most likely responsible for his present illness?
B. Staphylococcus epidermidis
A. Streptococcus pyogenes
D. Viridans streptococci
C. Enterococci
E. Coxiella burnetii
141. A 57-year-old male presents to the emergency department with recent-onset dyspnea and cough. He reports that his symptoms began earlier this morning while he was jogging, when he suddenly started feeling short of breath and very weak. In the emergency department, laboratory analysis reveals a markedly elevated serum b-type natriuretic peptide level. Which of the following clinical signs best correlates with this finding?
B. Cyanosis
A Wheezing
D. Extremity edema
C. Third heart sound
E. Periumbilical bruit
142. A 68-year-old Caucasian male presents to the emergency room with a three-week history of progressive dyspnea, orthopnea, and lower extremity edema. His past medical history is significant for hypertension, type 2 diabetes mellitus, myocardial infarction experienced eight years ago, and congestive heart failure. His current medications include metoprolol, digoxin, enalapril, furosemide, spironolactone, and aspirin. His blood pressure is 145/90 mmHg, and heart rate is 75/min. Symmetric 2+ pitting edema of the lower extremities is present. Point of maximal impulse is displaced to the left and soft holosystolic murmur is heard on the apex. Bilateral crackles are present over the lower lobes. His laboratory values are: Hemoglobin 11.0 g/dl Leukocyte count 7,500/cmm Platelets 300,000/cmm Serum sodium 128 mEq/L Serum potassium 5.3 mEq/L Serum calcium 9.0 mg/dl Serum phosphorus 4.0 mg/dl Serum creatinine 1 .9 mg/dl ECG does not reveal acute ischemic changes. Which of the following is most likely correct concerning this patient's condition?
B. The combination of furosemide and enalapril is the cause of hyperkalemia
A. Serum norepinephrine level is low
C. Hyponatremia indicates severe heart failure
D. Increasing the dose of digitalis may be indicated
E. Increasing sodium intake will help to control the electrolyte abnormalities
143. A 76-year-old man presents to your office with progressively worsening fatigue over the past several months. He denies associated chest pain, dyspnea, nausea, cough, or ankle swelling. He has smoked a pack of cigarettes per day for the past 30 years. His past medical history is significant for hypertension for which he takes hydrochlorothiazide and type 2 diabetes mellitus controlled with metformin. He had a medical check-up five months ago which did not uncover any new abnormalities or medical issues. On physical examination today, his blood pressure is 130/80 mmHg and his heart rate is 110 and irregularly irregular. His lab values are: Hematocrit 41% WBC count 4,700/mm3 Platelets 200,000/mm3 Sodium 137 mEq/L Potassium 4.1 mEq/L Creatinine 0.8 mg/dl Fasting glucose 85 mg/dl Which of the following is the best treatment for this patient?
B. Salmeterol
A Captopril
D. Warfarin
C Amlodipine
E. Spironolactone
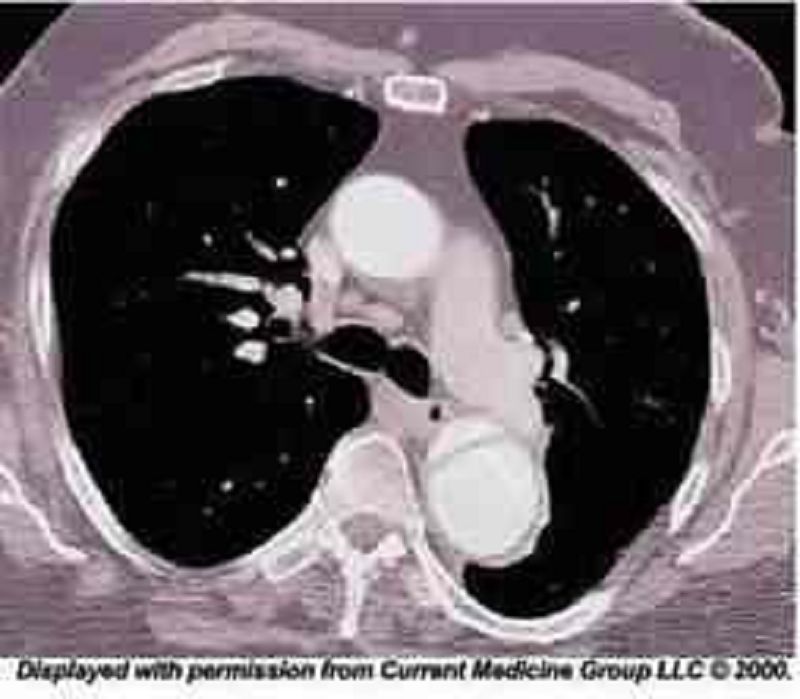
144. A 48-year-old African American man presents to the emergency room with severe retrosternal chest pain. His temperature is 36.7C (98.F), blood pressure is 190/100 mm Hg, pulse is 100/min, and respirations are 16/min. On physical examination, his lungs are clear to auscultation and his heart sounds are normal. EKG shows evidence of left ventricular hypertrophy. A CT image of his chest is shown below. Which of the following is the most appropriate immediate pharmacotherapy for this patient?
B. Nifedipine
A Labetalol
C. Heparin
D. Hydrochlorothiazide
E. Hydralazine
145. A 70-year-old male is brought to the ER, by his wife, because he lost consciousness while getting up in the morning. The syncopal episode lasted for several minutes, and the patient rapidly recovered consciousness. He had diarrhea and a decreased appetite one day earlier, which resolved spontaneously. His past medical history is significant for hypertension that is effectively controlled with the combination of hydrochlorothiazide/amiloride. His blood pressure is 120/70 mm Hg, while supine, and 98/50 mm Hg, while standing. The physical examination revealed a mucosal dryness. The EKG is normal. Which of the following laboratory values is the most sensitive indicator of the patient's underlying condition?
A. Decreased sodium concentration in the urine
B. Hypokalemia
C. Increased BUN/creatinine ratio
D. Metabolic acidosis
E. Decreased haematocrit
146. A 65-year-old man complains of lower leg swelling, fatigue and poor appetite. His past medical history is significant for recurrent chest infections, wheezing, cough, recent pyelonephritis, and arterial hypertension. He smokes 1 pack of cigarettes a day but denies alcohol or intravenous drug use. His physical examination reveals a barrel-shaped chest with bilateral scattered wheezes. His abdomen is distended and his liver edge is palpated 4 cm below the right costal margin. You note pitting edema and dilated, tortuous, superficial veins over the bilateral lower extremities. Manual pressure on the abdomen causes persistent distention of the jugular veins. The patient's serum sodium level is 135 mEq/L and his creatinine concentration is 1.2 mg/dl. An abnormality of which of the following is most likely to explain his edema?
B. Pulmonary artery systolic pressure
A. Serum albumin level
C. Pulmonary capillary wedge pressure
D. Portal venous resistance
E. Urinary protein excretion
147. A 60-year-old male presents to the emergency room with the chief complaint of progressive exertional dyspnea and fatigue. He denies any chest pain, syncope, cough, or edema. He suffered an acute anterior wall myocardial infarction one month ago. Chest auscultation reveals bilateral crackles in his lower chest. Cardiac auscultation reveals a pansystolic murmur at the apex with radiation to the axilla. ECG shows previously present unchanged Q waves and a persistent ST segment elevation in the anterior leads. Based on these findings, what is the most likely underlying cause of his symptoms?
B. Ventricular free wall rupture
A. Interventricular wall rupture
D. Recurrent ischemia
C. Ventricular aneurysm
E. Right ventricular infarction
148. A 65-year-old male presents to your office with a six-month history of periodic substernal pain. The pain episodes are experienced during strong emotion, last for 10-15 minutes, and resolve spontaneously. He has a long history of hypertension and diabetes mellitus, type 2. His right foot was amputated two years ago due to diabetes-related complications. You suspect angina pectoris and decide to perform myocardial perfusion scanning. It reveals uniform distribution of isotope at rest, but inhomogenesity of the distribution after dipyridamole injection. You conclude that the patient has ischemic heart disease. Which of the following effects of dipyridamole helped you in making the diagnosis?
B. Coronary steal
A. Increased heart contractility
D. Inhibition of platelet aggregation
C. Dilation of diseased vessels
E. Placebo effect
149. A 37-year-old healthy Caucasian male is seen in your office for a routine physical examination. He denies any symptoms or illness. He says he smokes a pack a day and drinks one to two beers every weekend. He has no allergies. Examination is unremarkable. The EKG reveals normal sinus rhythm with a heart rate of 72; there are frequent premature atrial beats present. The blood pressure is 120/65mm Hg. The next step in his management is:
B. Lidocaine
A Digoxin
D. Complete electrophysiological study
C. Order potassium levels
E. Observation
150. A 56-year-old white male presents with dyspnea for the last 3 months. His dyspnea was initially exertional but it has worsened progressively and now he is breathless even at rest. He denies any chest pain or ankle swelling. He has been smoking one-pack/day cigarettes for the last 30 years and has been drinking alcohol heavily for the last 10 years. He is not taking any medication. His mother died of breast cancer at 57. His vitals are, PR 86/min, BP 113/76mm of Hg; Temperature 37.1C (98.9F); RR 13/min. On auscultation of his precordium an S3 is heard, but there are no murmurs. Chest auscultation reveals bilateral basal crepitations. Chest x-ray shows marked cardiac silhouette enlargement and pulmonary venous congestion. EKG shows non-specific ST-T wave changes. Echocardiography shows a dilated left ventricle and systolic dysfunction (EF of 25-30%). CBC shows hematocrit of 32%, WBC count of 6,000/microl, and platelet count of 60,000/microl. Peripheral blood smear shows MCV of 101 fl. LFTs show AST of 180U/L and AL T of 66 U/L. The findings of cardiac catheterization and coronary angiography are not compatible with the diagnosis of ischemic cardiomyopathy. Which of the following measures is most likely to reverse his heart failure?
B. Abstinence from alcohol
A. Cessation of cigarette smoking
D. Use of ACE inhibitors
C. Reduced salt intake
E. Use of digoxin
151. A 55-year-old Caucasian male presents to your office for a routine check-up. His past medical history is significant for gout, hypertension, and hypercholesterolemia. His current medications include enalapril and pravastatin. He does not smoke or consume alcohol. His blood pressure is 156/94 mmHg and heart rate is 80/min. Physical examination reveals that the patient is moderately overweight (BMI = 27 kg/m2) with increased waist-to-hip ratio. You consider adding hydrochlorothiazide to the treatment regimen to improve the control of hypertension. Which of the following metabolic effects do you expect to emerge after this correction?
B. Hyperkalemia
A. Hypocalcemia
C. Decreased LDL cholesterol
D. Decreased plasma triglycerides
E. Hyperglycemia
152. An imaging study detects a 3.5 cm abdominal aortic aneurysm in a 60-year-old male. He has no associated symptoms. His past medical history is significant for hypertension, type 2 diabetes, hypercholesterolemia and hypothyroidism. His medications include aspirin, metformin, glipizide, hydrochlorothiazide, lisinopril, low dose atorvastatin and levothyroxine. He has smoked 1-2 packs of cigarettes daily for the past 40 years, and he drinks 1-2 glasses of wine daily. On physical examination, his blood pressure is 160/90 mmHg and his pulse is 80/min. Heart sounds are normal and his lungs are clear. Laboratory studies show: Serum creatinine 1.7 mg/dL Low density lipoprotein (LDL) 150 mg/dL HbA1C 8.5% Serum TSH 3.0 Which of the following interventions would most reduce the likelihood of his aortic aneurysm enlarging?
B. Better control of hypercholesterolemia
A. Better control of hypertension
D. Smoking cessation
C. Better control of diabetes
E. Alcohol cessation
153. A 68-year-old white female presents to the ER complaining of sudden onset chest pain associated with two episodes of vomiting. She has hypertension for which she takes atenolol and hydrochlorothiazide. Her pulse is 60/min, blood pressure is 80/50 mmHg and respirations are 14/min. Examination shows elevated jugular venous pressure and a positive Kussmaul's sign. Her lungs are clear to auscultation. Her EKG shows 2 mm ST segment elevation in leads II, Ill and aVF and 1 mm ST segment depression in leads I and aVL. Which of the following is the most likely cause of this patient's hypotension?
B. Right ventricular infarction
A. Pulmonary thromboembolism
D. Variant angina
C. Interventricular septum rupture
E. Intravascular volume depletion

154. A 72-year-old male is admitted to the hospital with chest pain. EKG and cardiac enzymes confirm a myocardial infarction and he is started on nitroglycerine, aspirin, simvastatin and low molecular weight heparin. Four days later, he complains of leg pain. Physical examination reveals a cold, pale leg. The angiogram is shown below.What is the best next step in his management?
B. Clopidogrel
A. Intravenous streptokinase
D. Leg elevation and warm compress
C. Cilosta zol
E. Embolectomy
155. A 53-year-old man presents to your office complaining of weakness and exertional dyspnea over the last week. He denies chest pain and palpitations. He has no other past medical history. His father died of a myocardial infarction at age 55. On exam, his heart rate is 100/min and blood pressure is 90/60 mmHg. Internal jugular venous pulsation is observed 7 cm above the sternal angle. Lungs are clear to auscultation. Heart sounds are muffled. Which of the following is the most likely cause of this patient's complaints?
B. Left ventricular outflow obstruction
A. Decreased cardiac contractility
C. Decreased left ventricular preload
E. Increased right ventricular compliance
D. Pulmonary hypertension
156. A 24-year-old military recruit is brought to the emergency room after suddenly collapsing while at training camp. Witnesses say he lost consciousness, and in the ER he appears confused. He had apparently been in his usual state of good health until this incident. His medical history includes allergic rhinitis for which he takes chlorpheniramine. On physical examination, his temperature is 41°C (106.F), blood pressure is 90/60 mm Hg, respiratory rate is 22/min, and pulse is 130/min and regular. He appears restless. His pupils are 4mm in size, symmetric, and reactive to light. Lung exam reveals a few rales at both lung bases. His abdomen is soft, non-tender and bowel sounds are present. There is no neck stiffness. His skin is dry and hot. He has 2+ symmetric reflexes in the upper and lower extremities. Muscle tone and bulk are normal. Initial laboratory studies show: Hemoglobin 16.0 g/L Platelets 120,000/mm3 Leukocyte count 18,500/mm3 Blood urea nitrogen (BUN) 40 mg/dL Prothrombin time 17 sec Partial thromboplastin time 40 sec Which of the following is the most likely cause of his current condition?
B. Meningitis
A. Heat stroke
D. Serotonin syndrome
C. Anticholinergic toxicity
E. Neuroleptic malignant syndrome
157. 56-year-old man presents to your office complaining of progressively worsening fatigue. He also reports difficulty concentrating and increasing forgetfulness over the past several weeks. On review of systems, the patient reports having unintentionally gained 6 pounds over the last three months. His past medical history is significant for hypertension and atrial fibrillation. On physical examination, he has a blood pressure of 140/90 mmHg and a heart rate of 75/min. His lung fields are clear to auscultation. There is no ankle edema. His skin is dry. Which of the following drugs is most likely responsible for this patient's complaints?
B. Metoprolol
A. Hydralazine
D. Enalapril
C. Verapamil
D. Enalapril E. Amiodarone
158. A 33-year-old Russian male reports concern over recurrent episodes of a "pounding" and "racing" heart over the last several months. He says his symptoms are worst while lying supine and while lying on his left side. On physical examination, his blood pressure is 150/55 mmHg and heart rate is 73/min. Which of the following is most likely responsible for his symptoms?
B. Pulmonary regurgitation
A. Aortic regurgitation
D. Tricuspid stenosis
C. Mitral stenosis
E. Aortic stenosis
159. A 34-year-old man rushes into the ER complaining of severe substernal chest pain that began abruptly 30 minutes ago. He says that he also feels as though his heart 'is racing,' but denies any shortness of breath, cough or fever. He has never experienced pain like this before. His past medical history is significant for an appendectomy one year ago. The patient reports that his father died at age 64 due to "some heart problem" and his mother died of ovarian cancer. On physical examination, the patient is agitated and sweating profusely. His pulse is 110/min, blood pressure is160/100 mm Hg, and respirations are 14/min. Physical examination is normal except for dilated pupils and a small amount of blood at the external nares. EKG shows ST elevations in leads v1_v4. What is the most likely explanation for his symptoms?
B. Acute pericarditis
A. Atherosclerotic vascular disease
D. Drug-induced vasospasm
C. Pleurodynia
E. Aortic dissection
160. A 40-year-old male presents to the Emergency Room with a two-month history of occasional severe headache and blurring of vision. His past medical history is significant for hypertension controlled with hydrochlorothiazide for two years. His family history is significant for hypertension and diabetes. He smokes two packs a day and occasionally consumes alcohol. His blood pressure is 200/140 mmHg and heart rate is 75/min. Which of the following is most consistent with a diagnosis of malignant hypertension in this patient?
B. Elevated serum creatinine level
A. Left ventricular hypertrophy on ECG
D. Oliguria
C. Papilledema
E. Blood pressure >/= 200/ 140 mmHg
161. A 62-year-old man visits his family physician because of generalized aches and pains. He denies associated fevers, headaches, chest pain, or abdominal discomfort. His past medical history is significant for an inferior wall myocardial infarction 6 years ago. His other medical problems include hypertension, diabetes, hypercholesterolemia, and gout. His current medications are aspirin, losartan, naproxen, atenolol, glipizide, colchicine, and simvastatin. On physical exam today, he is afebrile, with blood pressure 130/90 mm Hg, pulse 80/min and respirations 18/min. Lab results are as follows: Sodium 140 mEq/L Potassium 4.2 mEq/L Bicarbonate 21 mEq/L Chloride 100 mEq/l BUN 30 mg/dl Creatinine 1.6 mg/dl AST 113 IU/L ALT 120 IU/L Creatine phosphokinase 14,998 mg/dl What is the most appropriate next step in the management of this patient?
B. Stop simvastatin
A. Stop losartan
C. Start N-acetylcysteine
D. Order hepatitis panel
E. Obtain liver biopsy
162. A 50-year-old white male comes into your office for a routine check-up. He has no present complaints. His past medical history is significant for hypertension controlled with a low-dose thiazide diuretic. His family history reveals non-fatal myocardial infarction in his father at the age of 47. The patient does not smoke or consume alcohol. His blood pressure is 130/75 mmHg and his heart rate is 70/min. His previous records show that his HDL level is persistently low in spite of acceptable total cholesterol and LDL levels. You prescribe niacin to raise HDL level. The patient returns in a week complaining of intensive generalized pruritis and flushing. What is the most probable cause of the patient's complaint?
B. Prostaglandin-related reaction
A. Hypersensitivity reaction
C. Drug interaction
D. Drug-induced vasoconstriction
E. Psychogenic reaction
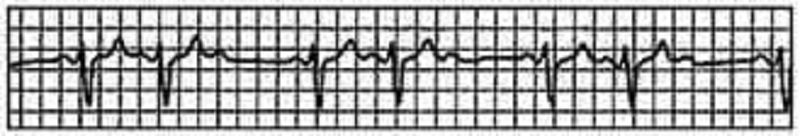
163. A 77-year-old woman comes to the emergency department because of feeling “light-headed and dizzy.” Except for the irregular pulse, her physical examination is normal. What is the rhythm in the lead tracing shown in Fig.?
(B) second-degree heart block
(A) first-degree heart block
(C) third-degree heart block
(D) premature ventricular beats
(E) premature atrial beats
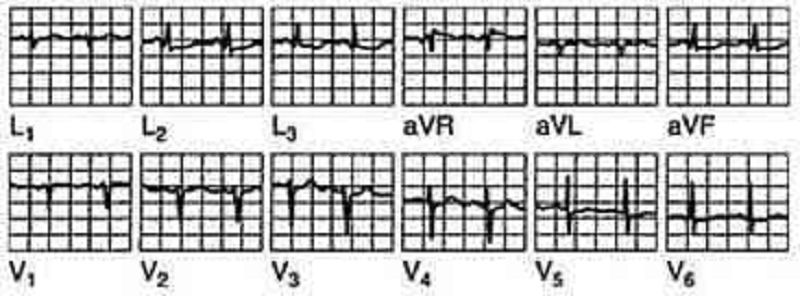
164. A 42-year-old woman has anterior chest pain of a somewhat atypical nature for many years. The patient’s pain has been present and relatively stable for a number of years, and the ECG shown in Fig. Is a stable one. What is the diagnosis?
(B) anterior wall infarction
(A) inferior wall infarction
(D) nonspecific changes
(C) ventricular aneurysm
(E) pericarditis
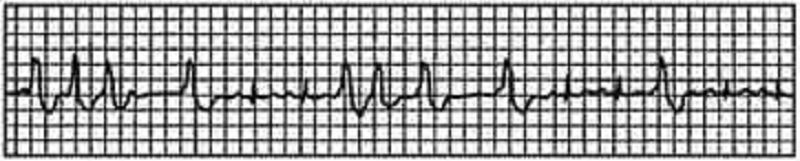
165. The ECG shown in Fig. Was obtained during the initial stages of an acute MI. The patient had just received thrombolytic therapy. What is the rhythm?
(B) atrial flutter
(A) atrial fibrillation
(D) Wenckebach phenomenon
(C) second-degree heart block
(E) nonsustained ventricular tachycardia
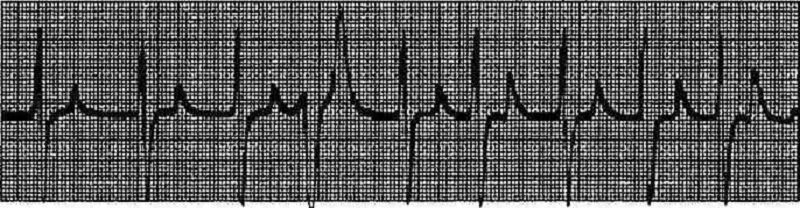
166. A 78-year-old man with advanced renal disease has the ECG shown in Fig. (lead II). What is the diagnosi
(B) hypercalcemia
(A) hyperkalemia
(C) hypernatremia
(D) pericarditis
(E) ventricular aneurysm
167. A 74-year-old woman presents to your office complaining of diarrhea and decreased appetite over the past week as well as increasing fatigue and occasional palpitations over the last few days. Her past medical history is significant for chronic atrial fibrillation for which she takes metoprolol, digoxin and warfarin. She smokes cigarettes and has for the past several years. On physical examination, her blood pressure is 140/90 mmHg and her heart rate is 70/min and irregular. Lung auscultation reveals scattered wheezes. Her abdomen is soft and non-tender. The liver span is 8 cm and the spleen is not palpable. There is no ankle edema. Her last measured INR was 2.3 two weeks ago. Which of the following is the best initial test in this patient?
B. Chest x-ray
A. Echocardiography
C. Pulmonary function tests
D. Thyroid function tests
E. Blood drug level
168. A 43-year-old male complains of frequent epigastric burning not relieved by antacids. The sensation is typically brought on by heavy lifting at work and takes 10-15 minutes to go away. He denies having associated arm or neck pain, cough, shortness of breath or difficulty swallowing. His past medical history is significant for systemic lupus erythematosus (SLE) diagnosed five years ago, for which he takes low-dose prednisone daily. On physical examination, his blood pressure is 140/90 mmHg and pulse is 80/min and regular. Heart, lung, and abdomen exams are unremarkable. EKG is normal. Which of the following is the best next step in managing this patient?
B. Coronary angiography
A. Echocardiogram
D. Myocardial perfusion testing
C. Exercise EKG
E. Upper Gl endoscopy
169. A 64-year-old white female presents for evaluation of two weeks of decreased appetite and nausea. She also notes occasional palpitations, which have been especially prominent over the past two days. Her medical history is significant for an anterior wall myocardial infarction one year ago and secondary congestive heart failure with left ventricular systolic dysfunction. Her current medications include aspirin, digoxin, furosemide, enalapril and metoprolol. On physical examination, her blood pressure is 120/80 mm Hg, pulse is 106/min and respirations are 15/min. The remainder of her exam is unremarkable. Chest x-ray shows an enlarged cardiac silhouette and normal lung fields. On laboratory testing, her digoxin level is twice the upper limit of normal. You order an EKG. Which of the following arrhythmias is most specific for digitalis toxicity?
B. Atrial fibrillation
A. Atrial flutter
C. Mobitz type II second-degree AV block
D. Atrial tachycardia with AV block
E. Multifocal atrial tachycardia
170. A 63-year-old male is admitted for sudden onset severe chest pain. His ECG reveals ST elevation in leads V2-V6. He is treated with thrombolytic therapy, heparin, aspirin, metoprolol, morphine, and nitrates. A coronary angiogram performed after thrombolytic therapy reveals 50% obstruction of the left anterior descending artery. On the third day of hospitalization, the patient suddenly develops severe shortness of breath at rest and hypotension. Examination reveals a soft S1, an apical pansystolic murmur radiating to the axilla, and bibasilar crackles. His temperature is 37.8°c (100°F), blood pressure is 92/58 mm Hg, heart rate is 102/min, and respirations are 31/min. An echocardiogram performed on the second hospital day reveals an akinetic region of the anterior wall. What is the most likely explanation for this patient's deterioration?
B. Pulmonary embolism
A. Pericardia! tamponade
C. Rupture of ventricular septum
D. Papillary muscle dysfunction
E. Acute aortic dissection
171. A 34-year-old female presents to your office complaining of pressure-like, substernal chest pain that has been affecting her recently when she plays active sports. Resting consistently alleviates the pain. She denies any associated nausea, vomiting, diaphoresis, dyspnea, palpitations or syncope. Family history is non-contributory. On physical examination, her pulse is 79/min and blood pressure is 130/70 mmHg. Cardiac auscultation reveals a high-pitched 3/6 systolic murmur best heard at the second right intercostal space. The lungs are clear to auscultation. Chest x-ray shows a normal sized heart and clear lung fields. What is the most likely cause of this patient's chest pain?
B. Atherosclerotic narrowing of the coronaries
A. Anomalous origin of the right coronary artery
C. Increased myocardial oxygen demand
D. Increased myocardial oxygen extraction
E. Stretching of the papillary muscles
172. A 45-year-old mildly overweight smoker presents with occasional episodes of nocturnal substernal chest pain that wakes her up from sleep. The episodes last 15-20 minutes and resolve spontaneously. She denies any illicit drug use. She leads a sedentary lifestyle but states that she can climb two flights of stairs without any discomfort. Her pulse is 78/min and regular, blood pressure is 130/70 mmHg and respirations are 13/min. Auscultation of her heart and lungs is unremarkable. Extended ambulatory ECG monitoring reveals transient ST segment elevations in leads V4-V6 during the pain attack. The pathophysiology of this patient's condition is most similar to that of which of the following?
B. Intermittent claudication
A Lacunar stroke
D. Raynaud phenomenon
C. Abdominal aortic aneurysm
E. Pulmonary embolism
173. An 84-year-old Caucasian male is brought to the ER with severe chest pain, dyspnea and diaphoresis. His past medical history is significant for a long history of hypertension and diabetes mellitus, type 2. He experienced a severe myocardial infarction 6 months ago. His current medications are enalapril, metoprolol, aspirin, furosemide, potassium, glyburide and pravastatin, but he says that he has not been taking some of his medications recently. Physical examination reveals acrocyanosis and symmetric 3+ lower extremity edema. Point of maximal apical impulse is displaced to the left, and a holosystolic II/VI apical murmur is heard at the apex. Non-specific ST segment and T wave changes are present on ECG. The initial set of cardiac enzymes are positive. The patient continues to deteriorate, despite aggressive diuretic and vasodilator therapy. You perform an echocardiographic evaluation of left ventricular function and decide to proceed with pulmonary artery catheterization. Cardiac index (CI), total peripheral resistance (TPR) and left ventricular enddiastolic volume (LVEDV) are determined. Which of the following is most likely to present in this patient?
B. Cl decreased, TPR increased, LVEDV decreased
A. Cl decreased, TPR decreased, LVEDV decreased
C. Cl decreased, TPR increased, LVEDV increased
D. Cl decreased, TPR increased, LVEDV normal
E. Cl normal, TPR decreased, LVEDV increased
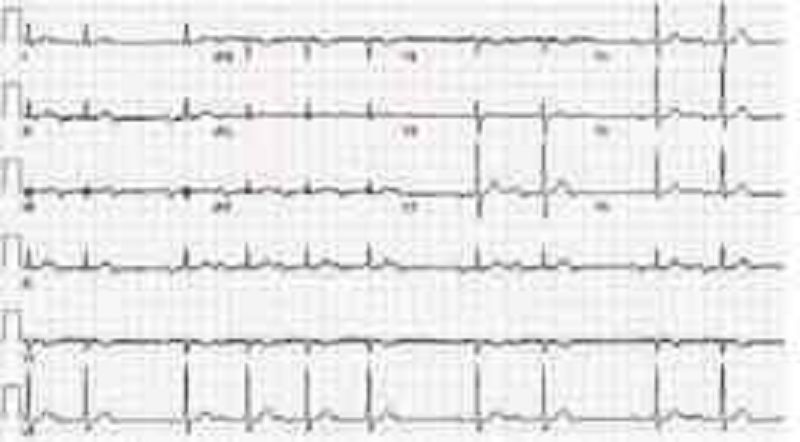
174. A 42-year -old male with a past medical history of bladder cancer and recurrent hematuria presents to the emergency room after "passing out" when he got out of bed this morning. The patient says that he was standing up to urinate shortly after waking when he began feeling dizzy. Fortunately, he was able to return to his bed before losing consciousness for 7-10 minutes. His EKG at the time of admission is shown below: Which of the following most likely accounts for the observed EKG changes?
B. Impaired SA node automaticity
A. Ventricular preexcitation
C. Impaired AV node conduction
D. Atrial reentry
E. His bundle branch block
175. A 65-year-old man comes to your office for a follow-up after his previous visits revealed inadequately controlled hypertension. He has no present complaints except difficulty walking uphill or climbing stairs, because of the pain in the right thigh, which makes him stop and rest. His past medical history includes stable angina, requiring coronary angioplasty and stenting 2 years ago; hypercholesterolemia; a 20-year history of hypertension; and a 10-year history of diabetes mellitus, type 2. His current medications are aspirin, metoprolol, hydrochlorothiazide, enalapril, amlodipine, pravastatin and glyburide. He smokes 1½packs of cigarettes per day and does not consume alcohol. His blood pressure is 160/100 mm Hg in his right arm and 180/110 mmHg in his left arm. Which of the following findings will point to the potential cause of the resistant hypertension in this patient?
B. Continuous murmur in the paraumbilical area to the right
A. Increased pulsation of intercostal arteries
C. Increased urinal excretion of vanillylmandelic acid (VMA)
D. High aldosterone/renin ratio
E. Increased 24-hour urinary free cortisol excretion

176. A 65-year -old Hispanic male is brought to the emergency room with severe substernal chest pain and diaphoresis that began suddenly 1 hour ago. He reports that his pain started while he was at rest and radiates to his left shoulder. The patient notes having vomited twice when the pain first began. Despite administration of 2 baby aspirins and 3 tablets of sublingual nitroglycerin, the pain persists. His initial EKG is shown below. On physical examination, the patient's temperature is 36.9°C (98.4.F), blood pressure is 110/80 mmHg, pulse is 60/min, and respirations are 18/min. S1 and S2 are normal, and an S4 is heard. The lungs are clear to auscultation. There is no jugular venous distension or pedal edema. Interventions to achieve which of the following goals would most improve this patient's long-term prognosis?
B. Decrease blood coagulability
A. Decrease myocardial oxygen demand
C. Restore coronary blood flow
D. Prevent ischemia-induced arrhythmias
E. Prevent reperfusin myocardial injury
177. A 43-year-old man is hospitalized with chest pain, lightheadedness and nausea. He describes the pain as dull and non-radiating. He has never had chest pain before, but does report occasional episodes of dyspnea and coughing. His medical history is significant for eczema. He is not presently taking any medications. His family history is significant for prostate cancer in his father and rheumatoid arthritis in his mother. He does not smoke or consume alcohol. The patient is admitted to the hospital and is given aspirin, low-molecular weight heparin, metoprolol and captopril. On day 2 of his hospitalization he complains of shortness of breath. Physical examination reveals prolonged expirations and bilateral wheezes. There are no crackles. You estimate the jugular venous pressure to be 7 cm with the patient's head elevated at 45 degrees. Which of the following is most likely responsible for this patient's current respiratory symptoms?
B. Bronchial infection
A. Pericarditis
C. Recurrent myocardial ischemia
D. Right ventricular infarction
E. Drug side effect
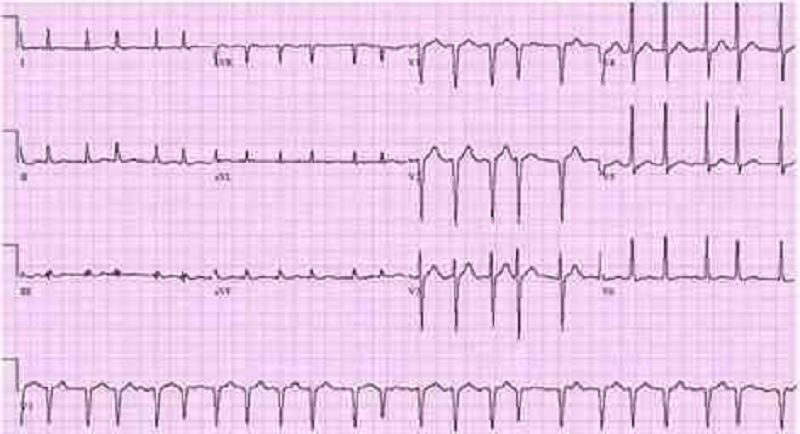
178. A 64-year -old male with a history of hypertension presents with general malaise and a 'funny' heart rhythm for the past 2 weeks. He had an echocardiogram done last year, which revealed mild left atrial dilatation and left ventricular hypertrophy. He has been taking hydrochlorothiazide for hypertension. His blood pressure at today's visit is 180/98 mm Hg. An EKG is obtained and is shown below.Which of the following is the most appropriate treatment for this patient?
B. Lidocaine
A. Immediate cardioversion
C. Adenosine
D. Carotid massage
E. Diltizem
179. A 53-year-old Caucasian male is admitted to the hospital with a 2-week history of fatigue and decreased exercise tolerance. He says he can hardly climb two flights of stairs without getting dyspneic. He denies palpitations or chest pain. His past medical history is insignificant, and a routine check-up 6 months ago was normal. He admits two episodes of binge drinking during the last month, but says that he 'got it under control'. He is currently not taking any medications. His blood pressure is 150/90 mmHg and heart rate is 130/min, irregular. Lungs are clear on auscultation. ECG does not reveal P waves. Echocardiography shows significant left ventricular dilation with an ejection fraction of 35% and mitral regurgitation (1+). Which of the following intervention will most likely improve the left ventricular function in this patient?
B. Decreasing afterload
A. Preload optimization
C. Rate or rhythm control
D. Inotropic support
E. Valve surgery

180. A 64-year-old male is admitted in ICU for acute myocardial infarction. He is on metoprolol, lisinopril, aspirin, furosemide, and potassium supplements. All of a sudden, the nurse mentions that the patient has a change in his tele monitoring. His blood pressure is 120/60 mm Hg. His potassium level is 4.2. He is alert, awake and oriented time, place and person. Examination shows scattered bilateral crackles, peripheral pedal edema and elevated JVI. Which of the following is the next best step in the management of this patient?
B.IV digoxin
A. IV amiodarone
C. Cardioversion
D. IV diltiazem
E. Carotid massage
181. A 48-year-old Caucasian male presents to your office complaining of progressive exertional dyspnea. It has become especially bothersome over the past two months. Presently, he becomes short of breath after climbing one flight of stairs. He denies any significant problems in the past. He is not taking any medications and he denies smoking or drinking alcohol. His temperature is 37.2°C (98.9F), pulse is 78/min, blood pressure is 130/75 mm of Hg and respirations are 14/min. Chest examination reveals a harsh systolic murmur that is best heard at the right second intercostal space with radiation along the carotid arteries. An S4 is heard at the apex. Based on these findings, what is the most likely cause of this patient's symptoms?
B. Myxomatous valve degeneration
A Hypertrophic cardiomyopathy
C. Rheumatic heart disease
D. Bicuspid aortic valve
E. Senile calcific aortic stenosis
182. A 47-year-old Caucasian female presents with occasional episodes of nocturnal substernal chest pain that wakes her up during sleep. The pain episodes last 15-20 minutes and resolve spontaneously. She denies any illicit drug use. She leads a sedentary lifestyle but states that she can climb two flights of stairs without any discomfort. She has no history of hypertension or diabetes. Her pulse is 75/min and regular, blood pressure is 134/70 mmHg and respirations are 14/min. Extended ambulatory ECG monitoring reveals transient ST segment elevation in leads I, aVL, and V4-V6 during the episodes. Which of the following is the best treatment for this patient?
B. Propranolol
A Diltiazem
D. Heparin
C. Aspirin
E. Digoxin
183. A 36-year-old male patient, who has a history of Marfan's syndrome, presents with sudden onset of severe central tearing chest pain radiating to his back. The pain is 9/10 in severity and is unrelated to exertion. He denies any history of alcohol or tobacco use. Measurement of his BP shows a difference of 35 mm Hg between his two arms. Chest auscultation reveals clear lung sounds and a mid-systolic click. What is the most appropriate next diagnostic step in the management of this patient?
B. Transthoracic echocardiogram
A. Transesophageal echocardiography
C. Cardiac enzymes
D. Coronary angiogram
E. Ventilation-perfusion scans
184. A 55-year-old male presents to your office with a 6-month history of periodic substernal pressure. He experiences this pressure while walking uphill or climbing two flights of stairs. His past medical history is insignificant. He smokes 1 pack a day and consumes alcohol occasionally. His blood pressure is 160/90 mmHg and heart rate is 75/min. Resting ECG is normal. You suspect stable angina and order an ECG stress test that reveals horizontal ST segment depression in leads II, III, and aVF at submaximal heart rate. What is the best medication to treat this patient's condition?
B. Verapamil
A. Thiazide
C. Amlodipine
D. Metoprolol
E. Enalapril
185. A 45-year-old man presents to the emergency department because of dyspnea, fatigue, poor appetite and weight gain over the past several weeks. He says that about four weeks ago he began to develop worsening shortness of breath with exertion and more recently has been waking at night with breathlessness. He also notes that it is sometimes difficult for him to open his eyes in the morning due to facial edema. He has no significant past medical history and he takes no medications. On physical examination, his blood pressure is 200/120 mmHg and his heart rate is 100/min. You note generalized bodily edema and distention of his jugular veins while he is sitting upright. On lung auscultation you hear bibasilar rales. Urinalysis shows trace protein, no nitrites, trace leukocyte esterase, 50+ red blood cells and occasional neutrophils. Which of the following is the most likely cause of this patient's edema?
A. Renal hypoperfusion
B. Hypoalbuminemia
C. Extensive glomerular damage
D. Portal hypertension
E. Hypothyroidism
186. A 45-year-old white male presents to the ER after an episode of syncope. His medical history is unremarkable except for an upper respiratory infection one week ago. On physical examination, his temperature is 37.2°C (99.F), pulse is 90/min, blood pressure is 100/60 mmHg and respirations are 13/min. His neck veins are distended and his heart sounds are distant. His lungs are clear to auscultation bilaterally. Chest x-ray reveals small bilateral pleural effusions and an enlarged cardiac silhouette. Which of the following EKG findings is fairly specific for his condition?
B. Presence of 'F' waves
A. Prolonged 'PR' interval
C. Electrical alternans
D. Presence of 'delta' wave
E. New-onset right bundle branch block
187. A 56-year-old man presents to the emergency department with dyspnea. He describes waking up during the night with difficulty breathing and chest pain that kept him from falling back to sleep. He has never had these symptoms before. His past medical history is significant for long-standing hypertension and non-compliance with his antihypertensive therapy. He has smoked a pack of cigarettes per day for the past 30 years. On physical examination, his blood pressure is 170/100 mmHg and his heart rate is 120/min and regular. Lung auscultation reveals bibasilar rales and scattered wheezes. Which of the following is most likely to relieve this patient's dyspnea?
B. Hydralazine
A Metoprolol
C. Nitroglycerin
D. Dopamine
E. Amiodarone
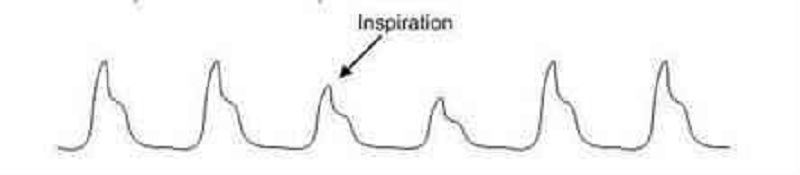
188. A 34-year-old female presents to the ER with difficulty breathing and dizziness. Blood pressure tracing from an arterial line placed in the ER is depicted below.Which of the following best accounts for these findings?
A. Severe asthma
B. Lobar pneumonia
C. Mitral stenosis
D. Aortic regurgitation
E. Panic attack
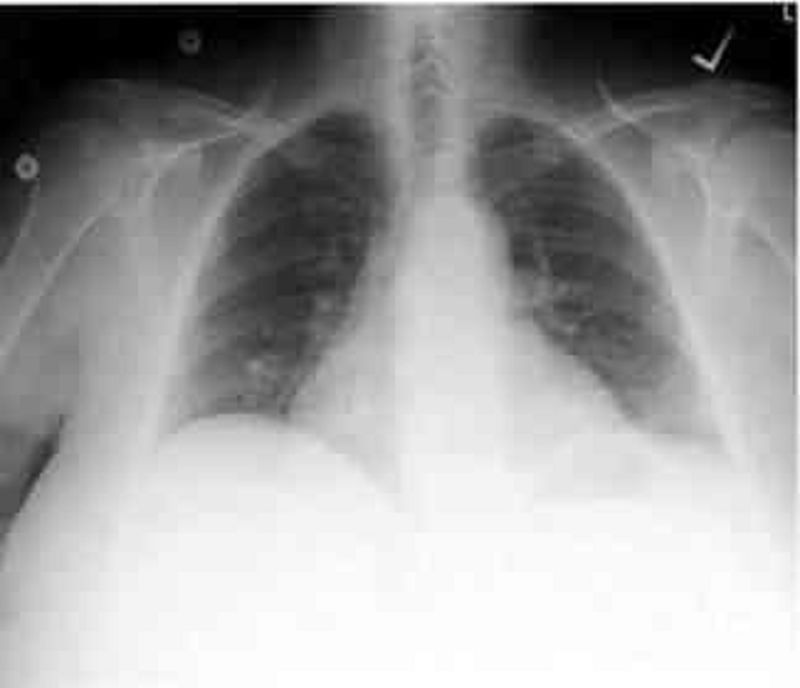
189. A 43-year -old man complains of progressive weakness and shortness of breath over the last two weeks. He denies any chest or muscle pain, nausea, vomiting or weight loss. He had a recent upper respiratory tract infection. His heart rate is 90/min and blood pressure is 110/70 mmHg. Jugular venous pressure is normal. Lungs are clear to auscultation. His chest x-ray is shown below.Which of the following is the most likely additional finding in this patient?
B. Non-palpable point of maximal impulse
A. Audible fourth heart sound
C. Pulsus bisferiens
D. Opening snap
E. Fixed splitting of the second heart sound
190. A 56-year-old white male presents to his primary care physician for follow-up evaluation of high blood pressure noted on each of three prior visits over a period of 6 months (systolic blood pressure ranging 140-145, diastolic blood pressure ranging 90-96 mm Hg). He has smoked a pack of cigarettes per day for the past 20 years and takes 5-6 drinks of alcohol daily. He has no other medical problems and takes no medications. There is no family history of diabetes mellitus, coronary artery disease, hyperlipidemia or hypertension. On physical examination today, his blood pressure is 146/97 mm Hg and pulse is 80/min. The remainder of the exam is unremarkable. Which of the following nonpharmacologic interventions would be expected to have the greatest impact on his high blood pressure?
B. Increased consumption of complex carbohydrates
A. Smoking cessation
C. Increased calcium consumption
D. Decreased alcohol intake
E. Decreased consumption of animal protein

191. A 55-year-old male is admitted to the ICU after being involved in a motor vehicle accident. He requires exploratory laparotomy for suspected bowel perforation. Two days after the surgery he remains hypotensive and requires both aggressive intravenous fluids and vasopressors to maintain his blood pressure. On physical examination, you note the fingertip changes pictured below:All four extremities feel cold to touch. Which of the following is most likely responsible?
B. Raynaud's phenomenon
A. Septic emboli
C. Norepinephrine-induced vasospasm
D. Cholesterol emboli
E. Superior vena cava syndrome
192. A 14-year-old African American male collapses and dies while playing basketball at a school tournament. He has no known past medical history. Which of the following is the most likely underlying disease in this patient?
B. Coronary atherosclerosis
A Hypertrophic cardiomyopathy
D. Ventricular septal defect
C. Aortic aneurysm rupture
E. Bicuspid aorta
193. A 63-year-old female presents to your office for a routine check-up. She has no present complaints. Her past medical history includes OM, type 2, and hypertension. Her current medications include glyburide and atenolol. She does not smoke. She drinks 2-3 glasses of wine 1-2 times a week. Three consecutive BP measurements were in the range of 138-142/87-90 mmHg. Physical examination is within normal limits. Her recent fasting glucose level was 250 mg/dl. ECG recorded 1 month ago showed left ventricular hypertrophy. Which statement about the BP control in this patient is the most accurate?
B. BP is within optimal range
A. BP is within acceptable range
C. It is better to keep systolic pressure less than 130 mmHg to slow end-organ damage
D. Diastolic BP is within acceptable range, but systolic is not
E. Systolic BP is within acceptable range, but diastolic is not
194. A 70-year-old patient presents to the ER with a 3-hour history of intensive retrosternal chest pain that radiates to the interscapular area. He states that he has never experienced this pain before. His past medical history is significant for a 20-year history of hypertension and a 10-year history of diabetes mellitus, type 2. His current medications include enalapril and hydrochlorothiazide. He does not smoke or consume alcohol. His vital signs are BP 180/110 mm Hg in the right arm and 178/110 mm Hg in the left arm, PR 85/min and RR 18/min. The physical examination revealed an early decrescendo-type diastolic murmur at the left sternal border. The EKG is normal. Which of the following is the best next step in the management of this patient?
B. Transesophageal echocardiography
A. Magnetic resonance imaging
C. Aortography
D. CK MB and troponin T levels
E. Ventilation/perfusion scanning
195. A 46-year-old man complains of exertional dyspnea and dry cough. He also describes occasional episodes of a suffocating nighttime cough that is relieved only when he stands up. His medical history is significant for a myocardial infarction six months ago. His current medications are metoprolol, aspirin and simvastatin. He does not use tobacco but drinks alcohol on social occasions. His father died of a stroke and his mother suffers from diabetes mellitus. His blood pressure is 150/100 mmHg and his heart rate is 60/min. Chest examination reveals bibasilar rales. His cardiac apex is palpated in the sixth intercostal space. The liver span is 12 cm. Bilateral pitting leg edema is also present. Which of the following most likely contributes to his edema?
B. High sodium delivery to the distal tubule
A. Constriction of the renal arterioles
C. Increased renal blood flow
D. Increased renal potassium loss
E. High portal venous resistance
196. A 22-year-old white female is brought to your office by her mother because of the recurrent syncopal episodes. The first episode occurred about one year ago when her roommate committed suicide and then several similar episodes occurred usually provoked by a strong emotion. The episodes are preceded by lightheadedness, weakness, and blurred vision and last about three minutes with rapid recovery of consciousness. Past medical history is insignificant. She is not taking any medications and denies drug abuse. Her blood pressure is 110/70 mm/Hg while supine and 108/70 mmHg while standing. Physical findings are within normal limits. EKG performed one month ago was normal. Which of the following is the next best step in the management of this patient?
B. 24-hour (Holter) monitoring
A. Echocardiography
C. Electroencephalogram
D. Invasive electrophysiologic testing
E. Upright tilt table testing
197. A 32-year-old man presents to the emergency department with a three-day history of fever, cough and weakness. His blood pressure is 120/80mmHg and his heart rate is 110/min. Physical examination reveals multiple needle tracks on his arms. ECG shows sinus tachycardia but is otherwise normal. Chest X-ray shows scattered round lesions in the peripheral lung fields bilaterally. Urinalysis is positive for 2+ protein. Which of the following accompanying findings is most likely in this patient?
B. Systolic murmur that increases on inspiration
A. S4 when patient is in the left lateral decubitus position
C. Diastolic murmur heard best with the patient sitting up
D. Systolic murmur that increases when the patient stands up
E. Paradoxical splitting of S2
198. A 41-year-old intravenous drug abuser presents with shortness of breath and pleuritic chest pain. He is febrile with a temperature of 103.5°F. He has no skin lesions and funduscopic exam is negative. He has jugular venous distension that increases with compression of the liver. The liver is pulsatile. The jugular venous pulse shows a prominent v wave. The patient has splenomegaly. Heart auscultation reveals a holosystolic murmur heard best at the left lower sternal border. The murmur increases with inspiration (Müller maneuver). Which of the following is the most likely diagnosis?
B. Pericarditis
A. Bacterial endocarditis
C. Rheumatic fever
D. Mitral valve prolapse
E. Pericardial effusion
199. A 54-year-old man with a 20-year history of chronic obstructive lung disease has a heave that is palpable at the lower left sternal border at the third, fourth, and fifth intercostal spaces. Which of the following best explains the etiology of the heave?
B. It means the patient has congestive heart failure
A. It is probably a displaced point of maximum impulse (PMI)
C. It means that the patient has aortic stenosis
D. It means the patient has right ventricular hypertrophy
E. It means the patient has a pericardial effusion
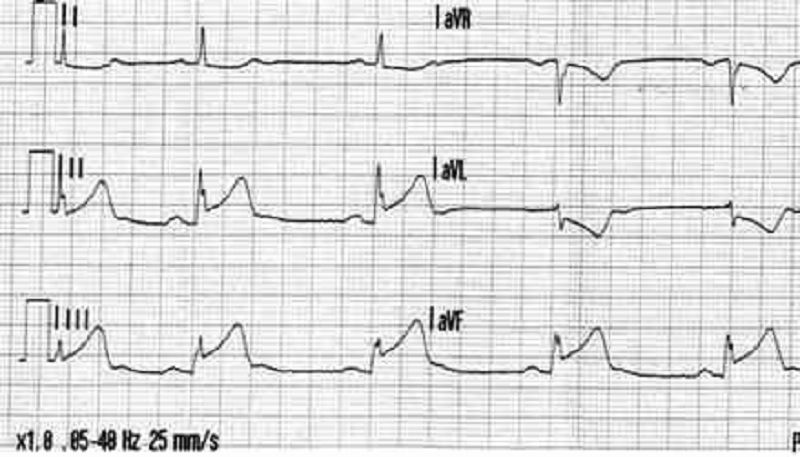
200. A 61-year-old woman was on her way to the grocery store when she started feeling chest pressure in the center of her chest. She became diaphoretic and felt short of breath. On arrival to the ED by EMS, her BP is 130/70 mm Hg, HR is 76 beats per minute, and oxygen saturation is 98% on room air. The nurse gives her an aspirin and an ECG is performed as seen below. Which of the following best describes the location of this patient’s myocardial infarction (MI)?
B. Anterior
A. Anteroseptal
C. Lateral
D. Inferior
E. Posterior
{"name":"QCU\/DES\/USMLE\/CADIOVASCULAR 1-200", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge of cardiovascular conditions and their management with our comprehensive 200-question quiz. Ideal for students, healthcare professionals, and anyone interested in enhancing their understanding of cardiovascular health.Key Features:200 meticulously crafted multiple-choice questionsCovers a wide range of cardiovascular topicsHelpful for both study and certification preparation","img":"https:/images/course8.png"}
More Quizzes
Exam part5(1132-1172) nana 4
100500
USMLE_ParaClinic II
2501250
FIRE Basics Quiz
3116338
Svenska
15810
Which Beetlejuice Character Are You? Take the Free
201017982
Logical Fallacy Game - Test Your Critical Thinking
201017499
Pest Control Test Questions & Answers - Free
201018822
Lexile Test - Check Your Reading Level Online Free
201018741
Central America Capitals - Can You Name Them All?
201018201
Which ROTTMNT Character Are You? - Free Results
201016868
US Rivers - Can You Name These American Waterways?
201018427
Free Emo: Are You Emo, Goth, Metal, Preppy or Perky?
201017175