DES part2 episode3
109) A 34-year-old obese Caucasian female complains of periodic visual obscurations. She has episodes during which she "goes blind" for several seconds when standing up or stooping forward abruptly. She also describes frequent morning headaches over the last two months for which she has had to take ibuprofen or aspirin almost every morning. She takes no other medications. Past medical history is insignificant aside from one uncomplicated vaginal delivery. She denies use of alcohol, tobacco, or illicit drugs. She is afebrile with a blood pressure of 138/88 mmHg and pulse of 93/min. Visual field testing shows enlarged blind spots. There are no other significant findings on neurologic examination. Which of the following is the most likely cause of this patient's symptoms?
Optic neuritis
Glaucoma
Cataract
Papilledema
Amaurosis fugax
110) A 30-year-old man is concerned about "floating spots" and blurred vision in his right eye. He had a serious injury of his left eye several weeks ago, which eventually led to vision loss in that eye. Inspection reveals a moderate perilimbal flush. What is the most probable cause of this patient's condition?
Reagin-mediated disease
Circulating immune complexes
. Non-caseating granulomas
Uncovering of 'hidden' antigens
Non-immune injury
115) A 65-year-old man complains of two years of persistent cough. He says that he coughs up whitish sputum almost every morning on waking, and then continues coughing throughout the day. He also complains of exertional shortness of breath that becomes disabling if he gets an upper respiratory infection. He has smoked one pack of cigarettes daily for the past 40 years. Pulmonary function testing reveals a vital capacity that is 65% of his predicted. Which of the following best explains this finding?
. Alveolar-capillary membrane thickening
Decreased functional residual capacity
Air trapping during expiration
Decreased lung distensibility
Respiratory muscle fatigue
116) A 71-year-old man is brought to the ER after a witnessed tonic-clonic seizure. He is somnolent and intermittently combative on exam. No past medical history is available. His arterial blood gas (ABG) at room air is given below: pH 7.23, pCO2 69 mmHg, pO2 57 mmHg, HCO3 28 mmHg. Which of the following best explains the acid-base disturbances in this patient
Lactic acid accumulation
Hypoventilation
. Pulmonary embolism
. Renal failure
Protracted vomiting
117) A 60-year-old white male presents to the Emergency Room with sudden onset of dyspnea. He is a truck driver and just returned from a long trip. His past medical history is insignificant. He is not taking any medications. His blood pressure is 110/70 mmHg and heart rate is 110/min. Physical examination reveals a moderately overweight man with tachypnea. Lungs are clear on auscultation. ECG shows right axis deviation. You order ventilation/perfusion scanning. Which of the following findings will help you the most to confirm the diagnosis?
An area of ventilation defect without perfusion defect
An area of perfusion defect without ventilation defect
An area of ventilation and perfusion defect
. Several small perfusion and ventilation defects
. Absence of ventilation and perfusion abnormalities
118) A 74-year-old nursing home resident is brought to the ER with a low-grade fever, cough and shortness of breath for the last two days. The cough is productive of small amounts of greenish sputum. His past medical history is significant for hypertension, diabetes mellitus type 2, COPD, hypercholesterolemia and mild dementia. His blood pressure is 152/78 mmHg and his heart rate is 89/min, regular. Physical examination reveals decreased breath sounds, coarse rhonchi, and increased fremitus over the lower left lung field. His oxygen saturation is 92% on room air when lying on his right side but drops to 84% when he lies on his left. Which of the following best explains this finding?
Increased dead space ventilation
Decreased cardiac output
Decreased oxygen diffusion capacity
Increased arterio-venous shunting
Effort-dependent hypoventilation
119) A 60-year-old man comes to the office with worsening shortness of breath over the last 5 months. He has had two episodes of bronchitis over the last 12 months. He now has a mild nonproductive cough. He denies any fever, chills, hemoptysis, chest pain, or difficulty breathing while lying on his back. His medications include an ipratropium inhaler, aspirin, and amlodipine. He was hospitalized twice in the last 3 years due to an exacerbation of his chronic obstructive pulmonary disease. He has been smoking 1 pack of cigarettes per day for the last 40 years. His temperature is 99°F (37.2°C), blood pressure is 130/86 mm Hg, pulse is 98/min, and respirations are 18/min. Examination shows a thin man in mild respiratory distress with increased anteroposterior chest diameter, diffuse expiratory wheeze and loud S2. Chest X-ray shows hyperinflation of bilateral lung fields with diaphragm flattening and small heart size. Which of the following is the most effective measure to decrease mortality in this patient?
Adding a short acting beta-agonist inhaler
. Adding an inhaled corticosteroid
. Adding a long-acting beta agonist
Adding systemic corticosteroids
Smoking cessation
120) A 64-year-old man presents to the emergency department with progressive exertional dyspnea that worsened after he contracted an upper respiratory infection. He also complains of bilateral ankle swelling. He has a 40 pack-year history of smoking. Physical examination reveals a mildly overweight patient in mild respiratory distress. Lung auscultation reveals bilateral wheezes and a prolonged expiratory phase. His white blood cell count is 14,500/mm3 and his hemoglobin level is 16 mg/dl. Arterial blood gas analysis reveals the following: pH 7.37, pO2 65mmHg, pCO2 60mmHg. Absence of marked acidosis in this patient is best explained by which of the following?
Increased minute ventilation
Increased dead space ventilation
Pulmonary vasoconstriction
Renal tubular compensation
Erythrocyte chloride shift
121) A 43-year-old woman with congestive heart failure, rheumatoid arthritis and chronic hepatitis C complains of abdominal discomfort and difficulty breathing. Physical examination shows dullness to percussion at the right lung base. Chest x-ray reveals a large right-sided pleural effusion. Thoracentesis yields pleural fluid with a glucose content of 30 mg/dl and an LDH of 192units/L. Which of the following explains the pleural fluid glucose concentration?
Increased pleural membrane permeability
Increased capillary hydrostatic pressure
. Increased permeability of the right hemidiaphragm
. High white blood cell content of the pleural fluid
High amylase content of the pleural fluid
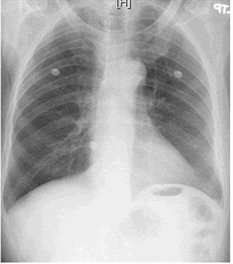
122) A 45-year-old black female presents to you because of a dry cough and has not been feeling well for the past month. She did have some pain in her shins a few weeks ago. She denies any allergies, smoking, or other medical problems. Her ECG shows normal sinus rhythm. The chest x-ray is shown below. What is the most likely pathophysiology in this patient?

For Student DES 2016-2017 last (1)

Pulmonary venous congestion
Lupus pneumonitis
Inflammatory granulomas
Malignancy of the lung
. Interstitial lung disease
123) A 42-year-old morbidly obese man is being evaluated for poor sleep. He complains of frequent awakenings due to a choking sensation and says that the resulting tiredness severely limits his physical activity. He also complains of chronic leg swelling. He denies cigarette, alcohol, or drug use. On physical examination, his blood pressure is 160/100 mmHg and his heart rate is 110/min. Which of the following additional findings is most likely to be present in this patient?
Anemia due to low erythropoietin
Decreased chloride due to bicarbonate retention
Decreased sodium due to increased ADH secretion
Decreased C02 due to persistent hypoxia
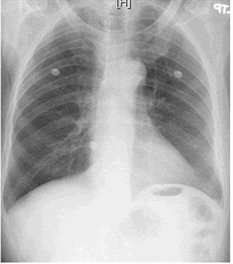
124) A 38-year -old male is brought to the emergency room with high-grade fever, shaking chills, productive cough and shortness of breath that started two days ago. His medical history is significant for two hospital admissions for alcohol withdrawal seizures. He continues to drink alcohol every day. He has no other medical problems and does not take any medications. On admission, his temperature is 39.7°C (103.5°F), pulse is 110/min, blood pressure is 100/70 mmHg, and respirations are 20/min. His skin and mucous membranes are dry. Physical examination reveals crackles and bronchial breath sounds in the right lower lobe. Chest x-ray demonstrates right lower lobe consolidation. He is started on ceftriaxone, azithromycin and intravenous normal saline at 200 ml/hr. Six hours later the nurse calls you because he is breathing at 38/min and requiring 100% oxygen. Emergent intubation is performed. A repeat chest x-ray is shown below. Which of the following is now most likely to be present in this patient?
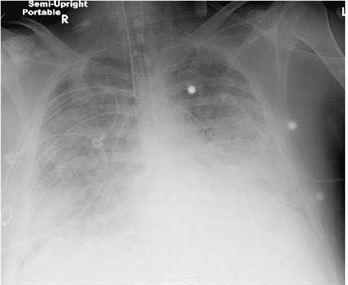
For Student DES 2016-2017 last (1)
Normal pulmonary capillary wedge pressure
Increased lung compliance
Increased left ventricular end diastolic pressure
Normal pulmonary arterial pressure
Normal alveolar-arterial oxygen gradient
125) A 53-year-old homosexual man comes to the ER with shortness of breath and dry cough over the past week. You note that he was hospitalized for Candida esophagitis one month ago, but left against medical advice. On physical examination, his blood pressure is 120/70 mmHg, heart rate is 120/min and regular, oxygen saturation is 89% on 2Umin of oxygen by nasal cannula, and temperature is 38.3°C (101°F). There are extensive white plaques over the oral mucosa and there is a soft 2/6 systolic murmur over the cardiac apex. Lung auscultation is remarkable for faint bilateral crackles. Which of the following is most likely responsible?
Increased pulmonary capillary wedge pressure
Alveolar hypoventilation
. Increased alveolar-arterial oxygen gradient
Increased lung compliance
Pulmonary hypertension
126) A 56-year-old male presents with progressively worsening dyspnea over a 4 month period. He denies fever, chest pain, cough or ankle swelling and does not use tobacco, alcohol or drugs. He works for a home insulation and plumbing company. He has never been abroad and does not own any pets. His only medications are hydrochlorothiazide and metoprolol for blood pressure control. On physical examination, his temperature is 36.8°C (98.2°F), pulse is 76/min, blood pressure is 130/78 mmHg, and respirations are 15/min. Examination shows digital clubbing and fine bibasilar end-inspiratory crackles. Jugular venous pressure is 7 cm and there is no peripheral edema. Which of the following additional findings is most likely in this patient?
. Increased pulmonary capillary wedge pressure
Decreased diffusion lung capacity (DLCO
. Decreased pulmonary arterial pressure
Increased residual lung volume
Reduced FEV1/FVC ratio
127) An 80-year-old Caucasian female is brought to the emergency room by her son with a three-day history of fever and a foul-smelling, productive cough. Her past medical history is significant for advanced dementia, diabetes, and hypertension. She takes aspirin, metformin, insulin, and atenolol. She was admitted two times with pneumonia during the past two months. Her temperature is 38.3°C (101°F), blood pressure is 100/70mmHg, pulse is 105/min, and respirations are 20/min. The patient is not oriented in time and place. Physical examination reveals dry mucus membranes and decreased skin turgor. Breath sounds are decreased to the right. A chest x-ray revealed right, lower lobe infiltrate. Which of the following is the most important predisposing factor for this condition in this patient?
Decreased lung elasticity
Gastro-esophageal reflux
. Impaired epiglottic reflex
. Decreased thyroid function
. Depressed cell-mediated immunity
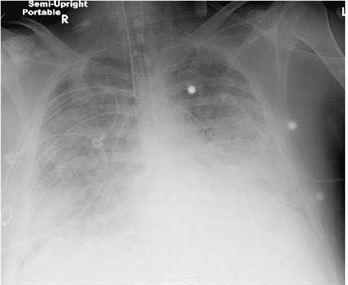
128) A 65-year-old female presents with 6 months of worsening dyspnea and dry cough. Whereas she had previously enjoyed an active lifestyle, she now becomes breathless after walking just a few steps. The patient denies fever or chest pain and does not use tobacco, alcohol or illicit drugs. Her only medicine is hydrochlorothiazide for hypertension. She is retired and lives with her husband. She has never travelled abroad and denies any history of exposure to pets. On physical examination, her temperature is 37.2°C (98.9°F), blood pressure is 140/86 mm Hg, pulse is 84/min and respirations are 18/min. Examination shows dry, late inspiratory crackles and finger clubbing. Her chest x-ray is shown below. Which of the following abnormalities is most likely to be present in this patient?

For Student DES 2016-2017 last (1)

. Increased diffusing capacity of carbon monoxide
. Decreased FEV1/FVC ratio
Increased residual volume
Increased PaCO2
Increased A-a gradient
129) A 44-year-old woman presents with increased shortness of breath, cough, and sputum production. She has had asthma since childhood and uses her medications as directed. Recently, she noticed that her peak flow readings were decreasing after the symptoms started. On examination, she is in moderate respiratory distress, respirations 25/min, there are bilateral wheezes and oxygen saturation is 90% on room air. On her blood gas, the PCO2 is 50 mm Hg. Which of the following is the most likely mechanism for her carbon dioxide retention?
Impaired diffusion syndromes
Right-to-left shunt
Hyperventilation
Ventilation-perfusion ratio inequality
Mechanical ventilation at fixed volume
130) A 57-year-old man with a 40-pack-per-year history of smoking experiences symptoms of shortness of breath on exertion. He has bilateral wheezes on expiration and increased resonance to percussion of the chest. Pulmonary function tests confirm the diagnosis of chronic obstructive lung disease (COPD). Which of the following is the best definition of this condition?
It is caused by bronchial asthma
It is preceded by chronic bronchitis
It is airflow limitation that is not fully reversible
It is due to destruction and dilatation of lung alveoli
Is due to small airways disease only
131) A 38-year-old man is being seen in his physician’s office after being involved in a car accident. He has a vague pain along his right sternal border, where he crashed into the steering wheel. His temperature is 36.6°C (97.8°F), pulse is 80/min, blood pressure is 123/75 mm Hg, respiratory rate is 14/min, and oxygen saturation is 99% on room air. Physical examination is significant for point tenderness over the right sternal border. X-ray of the chest shows no broken ribs but a single, well-circumscribed pulmonary nodule, 1.5 cm in diameter, located in the left lower lung field. A search through the patient’s electronic medical file reveals that he had an x-ray of the chest taken 2 years ago. The radiology report from that time reveals that the nodule was only 0.75 cm in diameter. To characterize the lesion, CT of the chest is performed and shows dense, flocculated calcification within the lesion. Which of the following risk factors most increases the chances of malignancy in this patient?
Increased doubling time of tumor
Increased patient age
Nodule diameter of 1.5 cm or higher
Presence of discrete border
Presence of flocculated calcification
132) A 32-year-old man develops symptoms of wheezing, cough, and shortness of breath. He has bilateral expiratory wheezes, and the rest of the examination is normal. Further evaluation with pulmonary function tests reveals a reduced FEV1/FVC ratio that corrects with bronchodilators. Which of the following statements about a diagnosis of idiosyncratic asthma (also called nonatopic) is correct
Known antigenic stimulus
Adult onset
History of atopy
High immunoglobulin E (IgE) levels
Positive skin tests
133) A 25-year-old man is recovering in the hospital from an open repair of his broken femur, which he suffered during an automobile accident. On postoperative day 3 he develops sudden onset shortness of breath and vague chest discomfort. His temperature is 37.6°C (99.6°F), heart rate is 108/min, blood pressure is 95/62 mm Hg, respiratory rate is 42/min, and oxygen saturation is 89% on room air. Physical examination is significant for jugular venous distention to 9 cm and an accentuated pulmonic component of S2. A pulmonary angiogram is shown in the image. Which of the following is most likely to be decreased?

For Student DES 2016-2017 last (1)

Airway resistance
Alveolar ventilation
Alveolar dead space
Pulmonary vascular resistance
Pulmonary compliance
134) A 64-year-old woman is admitted to the hospital with right lobar pneumonia and sepsis syndrome. She becomes progressively more short of breath and hypoxemic requiring intubation and mechanical ventilation. Her repeat CXR in the intensive care unit now shows diffuse pulmonary infiltrates and a diagnosis of acute respiratory distress syndrome (ARDS) is made. Which of the following mechanisms is the most likely cause for the early exudative‖ phase of ARDS?
Increased lung compliance
Increased interstitial fibrosis
Increased vascular permeability to fluid and proteins
Decreased pulmonary perfusion
Decreased ventilatory dead space
135) A 55-year-old woman is in the intensive care unit on a ventilator for hypoxemia following “flash” pulmonary edema. Her PO2 on the blood gas prior to intubation was 44 mm Hg, and now while breathing 100% oxygen on the ventilator her repeat blood gas reveals a PO2 of 80 mm Hg. Hypoxemia while receiving 100% oxygen indicates which of the following problems?
Ventilation-perfusion ratio inequality
Right-to-left shunt
Hypoventilation
Impaired diffusion
Interstitial lung disease
136) You are the internist caring for a 26-year-old male who is stricken with alcoholic gastritis. The man has remained absent from his work as a waiter for several days due to his illness. His employer calls you for more information about the illness and the prognosis. He says that he just spoke with his employee on the phone and was granted permission to talk with you. What is the most appropriate response to this request?
"I'm sorry, but I cannot share such information with you at this point."
"The diagnosis is alcoholic gastritis, and I expect it will clear up spontaneously at some point in the near future
"I can assure you that the illness does not pose a health risk to any of your employees or customers
"I will need to have a release of information document signed by my patient before we can discuss this matter."
"I will need to have a verbal waiver of confidentiality granted to me by telephone before we can discuss this matter. Let me call you back
137) A 34-year-old obese female is brought to the emergency department complaining of severe right upper quadrant abdominal pain that began suddenly earlier this morning. She is accompanied by her husband. An ultrasound evaluation is performed and the woman is diagnosed with acute cholecystitis. Because her symptoms worsen with conservative treatment, the decision is made to operate. The patient is discharged home five days after her successful cholecystectomy. Upon discharge, the patient and her husband request all medical records associated with her stay. What is the most appropriate response on the behalf of the physician?
. Provide a copy of the original records
. Refuse to provide the records
Politely inform the couple that it is unlawful to provide patients with their medical records
Give them the medical chart in its entirety
. Inquire as to why the records are needed
138) A long-time patient calls your office to speak with you directly. She voices frustration with your receptionist, who has repeatedly refused to allow her to schedule an appointment to see you. The patient says that at her last visit, she had a heated argument with the receptionist about a minor detail regarding her insurance coverage. When she has called since then, the receptionist always responds by saying, "I'm sorry, but there are too many patients waiting ahead of you." Which of the following defense mechanisms is the receptionist demonstrating?
Distortion
. Displacement
Acting out
Introjection
. Passive-aggressive behaviour
139) A 34-year-old woman who describes herself as a "holistic healer" brings her two children aged four years and three years to the pediatrician for routine physical examinations. This is a first visit as they have recently moved from another state. The medical records for the children indicate that no immunizations have been given. When the mother is questioned about this, she proudly replies, "My children are wonderfully healthy on their own and have no need for these artificial vaccines." The principles and benefits of immunization are discussed at length, as well as the risks inherent in not being immunized. The physician recommends that the children be given all age-appropriate vaccinations today. The mother remains convinced that immunizations cause more harm than good, and she steadfastly refuses to allow her children to be vaccinated. What is the most appropriate next step?
. Obtain a court order for immunization of children
. Proceed with immunizations today
. Inform mother that she will be reported to the local health department
Document in the medical chart that the risks and benefits of vaccination have been explained
Request to speak with her husband
140) A 48-year-old woman notices a firm, fixed mass in her right breast but chooses to ignore it. The mass is then detected on her annual physical examination eight months later. By that point, the mass has increased greatly in size. When questioned as to why she did not report the mass when she first noticed it, the woman states that she was not concerned about the mass because she does not have a family history of breast cancer This response is an example of which of the following defense mechanisms?
Repression
. Dissociation
Denial
Rationalization
Intellectualization
141) A 60-year-old physician is admitted to the hospital for jaundice and weight loss. He denies other symptoms, including abdominal pain and alterations in bowel movements. His past medical history is noncontributory. He denies any history of significant alcohol intake but admits to a 30-pack-year smoking history. A detailed work-up eventually reveals the diagnosis of pancreatic carcinoma. Shortly after his discharge, he spends several hours per day on his laptop computer so that he can obtain the latest information on his illness. Which of the following psychological defense mechanisms is this physician most likely employing?
. Intellectualization
Rationalization
Denial
. Isolation
. Resistance
142) A 54-year-old male with a history of chronic alcoholism is admitted to the hospital with hematemesis and abdominal distension. Upper gastrointestinal endoscopy reveals the presence of esophageal varices. Continued workup of his condition results in a diagnosis of cirrhosis of the liver. He is treated appropriately and strongly counseled about the need to abstain from alcohol. He is then discharged home. After discharge, he begins to work as a full-time volunteer for a non-profit organization that assists patients with alcoholic cirrhosis. Which of the following defense mechanisms is this man using?
Reaction formation
Denial
Sublimation
Altruism
. Suppression
143) A 21-year-old college junior requests an urgent appointment with her family physician to discuss a "personal concern." During her conversation with the doctor, the woman appears tense, speaks very little, and makes minimal eye contact. After gentle questioning, she breaks down and says that her father is taking lithium for a manic episode experienced two years ago. She had not realized this could have any bearing on her own situation until she encountered an article on the Internet that mentioned genetics appears to play a role in the pathogenesis of bipolar disorder. Since then, she has had disturbed sleep and has been very worried that she too will one day develop bipolar disorder. Based on clinical data, what is the likelihood that she will have a manic episode during her lifetime?
1%
. 10%
40%
. 60%
75%
144) A 25-year-old married female is brought to the emergency department by her mother for excruciating right-sided abdominal pain. A urine pregnancy test is positive and a pelvic ultrasound reveals an empty uterus. Ruptured ectopic pregnancy is suspected, and an operating room is reserved for an emergent laparotomy. The patient's medical history is unremarkable except for a psychiatric diagnosis of paranoid schizophrenia. Who should sign the informed consent paperwork for the procedure?
The patient's husband
The patient's mother
The court
. The patient
No consent is necessary as the patient is incompetent
145) A 31-year-old woman voices her anger at the increasing number of immigrants who compete for job opportunities in her chosen field of computer science. She observes that many of her friends in the local community are also experiencing difficulty in securing appealing employment because of the influx of immigrants. This woman volunteers in her spare time to provide vocational guidance to new immigrant families in the community. Which of the following psychological defense mechanisms is she demonstrating
Suppression
. Splitting
Reaction formation
. Sublimation
Altruism
146) A 57-year-old Caucasian woman presents for a follow-up visit regarding her lower back pain. She originally presented with this complaint last month and was advised to limit activity and use ibuprofen as needed. When her pain persisted, she was scheduled for an MRI of her back. The MRI report returned today and describes the presence of metastatic deposits in her spine. The source of the primary neoplasm remains undetermined. The patient has not yet been told about the findings and will need to be informed today. Which of the following is the best means of initiating a conversation about her condition?
"You have cancer, and it has metastasized to your back
"We will try our best. However, once a tumor metastasizes, the prognosis is poor
"You should have come earlier for a medical checkup. It is now too late."
"How are you feeling today?"
"You do not have a simple back strain
147) A 23-year-old man comes to the psychiatrist with a chief complaint of a depressed mood. He is very anxious and obviously uncomfortable in the physician’s office. Which of the following actions should be used to help develop rapport with this patient?
Inform the patient that his problem is simple and easily fixed
. Express compassion with the difficult position the patient is in
Tell the patient that you too are nervous when you see new patients
Ask the patient why he is so unusually anxious about seeing a psychiatrist
Get right to the patient’s complaint so that the patient can leave as soon as possible
148) A 37 year-old man with chronic schizophrenia is brought to see a new psychiatrist for treatment. While taking the history, the psychiatrist finds that the patient functions with a flat affect and circumstantial speech all the time. He has few friends. He is able to hold a menial job at the halfway house where he lives, and his behavior is not influenced by delusions or hallucinations currently. What should the psychiatrist rate the patient on Axis V (global assessment of functioning)?
>95
70
55
. 30
15
149) An 18-year-old man is brought to the emergency room by police after he is found wandering in the street, screaming loudly at passersby. In the emergency room he is placed in an examination room, and paces the floor and pounds his fist against the door repeatedly. Which of the following actions should be taken by the psychiatrist first?
Rule out an organic mental disorder
. Rule out psychosis
Give the patient 5 mg of haloperidol IM
Make sure the physical environment is safe for the interviewer
Put the patient into soft restraints
150) A 24-year-old man returns from Iraq after a 13-month tour of duty. During that tour he was involved in battle situations and saw one of his friends injured by a car bomb. What percentage of American soldiers returning home from Iraq have posttraumatic stress disorder (PTSD)?
. <1%
1% to 5%
15% to 20%
. 50% to 55%
85% to 90%
151) A 28-year-old woman is brought to see a psychiatrist by her mother. The patient insists that nothing is wrong with her, but the mother notes that the patient has been slowly but progressively isolating herself from everyone. She now rarely leaves the house. The mother says she can hear the patient talking to “people who aren’t there” while she’s in her room. On examination, the patient is noted to have auditory hallucinations and the delusional belief that her mother is going to kick her out of the house so that it can be turned into a theme park. Which of the following is the lifetime prevalence for this disorder?
1%
. 3%
. 5%
10%
. 15%
152) A 32-year-old man is admitted to the psychiatric unit after his wife brought him to the emergency room in a severe major depression. The patient signs himself in voluntarily because he “didn’t think he is safe” at home. Which of the following factors most increases a patient’s risk of suicide while on the inpatient unit?
The patient is in his first week of hospitalization
Staff morale is high on the unit
The patient is admitted in early July (new residents are on the unit
. The patient is started on an SSRI the first day on the unit
The patient is told he will be evaluated for ECT
153) A 52-year-old female presents with a rash over her face for the past few weeks. She also complains of recent-onset difficulty with rising from a seated position and climbing stairs. On examination, you notice a dusky malar rash and a violaceous periorbital edema. Her vital signs are within normal limits. Examination shows symmetric proximal muscle weakness in legs. This patient's condition is most often associated with which of the following?
. Aortic aneurysms
Renal failure
Alveolar hemorrhage
Malignancy
. Carpal tunnel syndrome
154) A 50-year-old man presents to your office complaining of pain and swelling of the right knee. He bumped his right knee into a pole 2 days ago while working. He had one episode of similar pain two years ago that resolved with over-the-counter analgesics. He denies any illicit drug use. He has no other medical problems and does not take any medications. His temperature is 37.2°C (98.9°F), and blood pressure is 126/76 mmHg. Examination reveals swelling, warmth and decreased range of motion of the right knee. All other joints are within normal limits. Synovial fluid analysis shows positive birefringent crystals and negative Gram stain. These crystals are most likely composed of?
Hydroxyapatite
Monosodium urate
Calcium pyrophosphate
Calcium oxalate
Ammonium phosphate
155) A 53-year-old Caucasian man comes to the emergency department at 2 am because of severe pain in his right great toe for the past 2 hours. He complains that the pain began suddenly as a dull, aching pain, and has worsened over time to a severe throbbing pain, not relieved by acetaminophen. His other medical problems include hypertension, diabetes mellitus-type 2, hypercholesterolemia, and peptic ulcer disease. He has smoked 2 packs of cigarettes daily for 30 years. He drinks 5-6 ounces of alcohol daily. He eats a lot of junk food and exercises infrequently. Both his father and mother have diabetes and hypertension. His older brother died of a myocardial infarction 2 years ago. His medications include glyburide, lisinopril, atenolol, simvastatin and famotidine. His temperature is 37.8°C (100°F), blood pressure is 160/90 mm Hg, pulse is 88/min and respirations are 16/min. On examination, the right great toe appears markedly swollen, red, and is warm to touch. Aspiration of the joint fluid reveals negatively birefringent needle shaped crystals. Apart from prescribing oral indomethacin, what other intervention would be most important to prevent the development of further attacks?
Smoking cessation
Alcohol cessation
Stopping lisinopril
Stopping simvastatin
Stopping glyburide
156) A 32-year old woman comes to the physician because of pain and paresthesias in her thumb, first two fingers and the radial-half of the ring finger. Her pain is worse at night and interferes with sleep. She feels tired and unable to work effectively in her office lately. She takes an over-the-counter stool softener for constipation but otherwise has no known medical problems. Her vital signs are within normal limits. When you ask the patient to maintain acute wrist flexion for 30seconds she experiences severe pain and paresthesias. Her skin is dry. Which of the following is the most likely cause of her hand symptoms?
Amyloid fibril deposition
Tenosynovial inflammation
Accumulation of matrix substances
. Synovial tendon hyperplasia
. Accumulation of fluid in carpal tunnel
157) A 51 -year-old man complains of difficulty walking and mild right-sided foot pain for the past several weeks. His medical history is significant for type 1 diabetes mellitus, hypertension and hypercholesterolemia. Physical examination reveals a significantly deformed right foot and a mildly deformed left foot. X-rays suggest effusions in several of the tarsometatarsal joints, large osteophytes, and several extra articular bone fragments. Which of the following is the most likely cause of this patient's complaints?
Hyperuricemia
Poor vascular supply
Nerve damage
Rheumatoid arthritis
Bone demineralization
158) A 24-year-old Caucasian female complains of weakness, skin rash, low-grade fever and joint pain. She describes pain and swelling of the hand joints and pain in her knees. Her mother suffers from rheumatoid arthritis. Her blood pressure is 145/90 mmHg, and her heart rate is 90/min. Her hematocrit is 40% and ESR is 43 mm/hr. Urinalysis is 2+ for protein. Which of the following is the best statement about this patient's joint symptoms?
. Excessive bony growth is characteristic
. Permanent deformity is uncommon
Subluxation and tendon damage cause permanent deformity
. Cartilage degradation and muscle atrophy cause deformity
Bone resorption of the distal phalanges may result
159) A 67-year-old man presents to your office with two days of back pain. He was moving boxes in the garage when the pain started. The pain is not relieved by lying down and increases in intensity upon straining and coughing. He could not sleep during the night due to pain and took several tablets of acetaminophen without relief. He has never had such pain before. Physical examination reveals symmetric knee reflexes. Plantar reflexes are flexor bilaterally. Straight leg raise is negative. Local tenderness is evident upon percussion of the fourth lumbar vertebra. Which of the following is the most likely cause of this patient's condition?
. Ligamentous sprain
Intervertebral disk degeneration
. Apophyseal joint arthritis
Nerve root demyelinization
. Vertebral body demineralization
160) A 38-year-old male with steroid-dependent sarcoidosis presents to the physician's office because of progressive right hip pain. He localizes the pain to right groin and states that the pain is present on weight bearing and at rest. His temperature is 37.2°C (98.9°F) and blood pressure is 156/86 mm Hg. Examination shows decreased range of motion due to pain. He also has a round face and fullness in supraclavicular area. Purple striae are present on skin. Muscle power is slightly decreased in the proximal thigh muscles in both legs. Reflexes are 2+, and there are no sensory deficits. Plain films of the right hip show no significant abnormalities ESR is 10 mm/hr. Which of the following is the most likely cause of his hip pain?
Inflammatory arthritis
Cartilage degeneration
Disruption of bone vasculature
Inflammation of the trochanteric bursa
Aortoiliac occlusion
161) A 65-year-old man comes to the emergency room complaining of 2 days of severe pain and swelling of his right knee. He denies any recent respiratory illness, diarrhea or urinary symptoms. He has a history of severe degenerative joint disease and underwent total knee replacement four years ago. He drinks one can of beer every night and does not use tobacco or illicit drugs. His temperature is 40°C (104°F), blood pressure is 120/60 mmHg, and pulse is 110/min. Examination shows warmth, swelling, and tenderness over the knee. His range of motion is restricted. Synovial fluid white blood cell count is 98,000/microl. Which of the following is the most likely cause of his current condition?
Streptococcus species
Staphylococcus aureus
. Neisseria gonorrhoea
Chlamydia trachomatis
Borrelia burgdorferi
162) A 24-year-old woman comes to the physician complaining of a skin rash and pain in her wrists, ankles and elbows over the past 4 days. She has also had a fever and sweats, but denies headache, nausea or vomiting. She has no significant past medical history and does not take any medications. She recently took a vacation with her new boyfriend. She denies any previous sexually transmitted diseases but acknowledges having unprotected sex with her new boyfriend. She does not use tobacco, alcohol or illicit drugs. Her temperature is 38.5°C (101.3°F) and her pulse is 98/min. Her oropharynx is clear and there is no thrush or lymphadenopathy. Her abdomen is benign and the pelvic examination is within normal limits. She has pain along the tendon sheaths with active and passive hand movement. A photo of her skin rash is shown below. Which of the following is the most likely cause of her symptoms?

For Student DES 2016-2017 last (1)

. Lyme disease
Syphilis
Gonococcemia
. Meningococcemia
Acute HIV infection
163) A 43-year-old Caucasian female has a long history of polyarthritis. She also complains of fatigue, low-grade fever, weakness and recent weight loss. Her current medications are methotrexate, naproxen and ranitidine. Physical examination reveals deformed hand joints and a soft, tender mass palpated in the right popliteal fossa. The latter finding is best explained by:
Subcutaneous abscess
Inflamed synovium
Lymphedema
Venous thrombosis
Bony growth
164) A 45-year-old woman with long-standing, well-controlled rheumatoid arthritis develops severe pain and swelling in the left elbow over 2 days. She is not sexually active. Arthrocentesis reveals cloudy fluid. Synovial fluid analysis reveals >100,000 cells/mL; 98% of these are PMNs. What is the most likely organism to cause this scenario?
Streptococcus pneumoniae
Neisseria gonorrhoeae
. Escherichia coli
Staphylococcus aureus
Pseudomnonas aeruginosa
1) A 64-year-old male who has not seen a doctor for the past 20 years presents to the emergency room with excruciating chest pain that stated suddenly about three hours ago. He describes the pain as tearing in quality and says that it radiates to his back. On physical examination, you hear an early diastolic decrescendo murmur at the sternal border. Chest X-ray shows widening of the superior mediastinum. EKG is normal. Which of the following medical conditions most likely accounts for this patients presentation?
Systemic hypertension
. Marfan's syndrome
. Ehlers-Darlos syndrome
Giant cell arteritis
. Bicuspid aortic valve
2) A 45-year-old recently immigrated Mexican farmer comes to your office complaining of dyspnea, fatigue and abdominal distention for the past two months. On physical exam, his temperature is 37°C (98°F), blood pressure is 126/80 mmHg, pulse is 80/min, and respirations are16/min. You note pedal edema, elevated jugular venous pressure with positive Kussmaul's sign, and increased abdominal girth with free fluid. Chest auscultation reveals decreased heart sound intensity at the apex and an early heart sound following S2. The jugular venous pressure tracing shows prominent 'x’ and 'y' descents. Which of the following is the most likely cause of this patient's symptoms?
Cor pulmonale
Tuberculosis
Trypanosoma cruzi infection
Psittacosis
. Pneumoconiosis
3) A 45-year-old mildly overweight male recovering from an anterior wall myocardial infarction develops sudden onset of sharp pain in the left side of his chest. He presented five days earlier with substernal chest pain and diaphoresis. He has had no dyspnea, extremity swelling or palpitations since admission. His past medical history is significant for diabetes mellitus type 2. He seems mildly restless, especially in the supine position. The pain improves when sitting up and leaning forward. His breathing is fast and shallow due to the pain. His lungs are clear on auscultation. His blood pressure is 120/78 mmHg and his heart rate is 60/min There is no change in blood pressure upon deep inspiration. ECG shows sinus rhythm with new diffuse ST segment elevation. Which of the following is the most likely diagnosis?
. Interventricular wall rupture
. Ventricular free wall rupture
. Pulmonary infarction
Recurrent ischemia
. Acute pericarditis
4) A 23-year-old woman who is 26 weeks pregnant presents to the emergency department with sudden onset severe shortness of breath and inability to lie flat. She recently emigrated from Eastern Europa. Her medical history is significant for recurrent sore throats requiring tonsillectomy as a child. Presently, her blood pressure is 110/60 mmHg and her heart rate is 120/min. An EKG rhythm strip suggests atrial fibrillation. Which of the following is the most likely diagnosis?
. Hypertrophic cardiomyopathy
. Constrictive pericarditis
. Mitral stenosis
. Myocardial infarction
Aortic insufficiency
5) A 63-year-old Caucasian female presents to the emergency room with a recent onset of left-sided Weakness. She has been experiencing increased fatigability, low-grade fevers and occasional palpitations over the past two months. She has lost seven pounds during the same period. Her temperature is 37°C (98.6°F), pulse is 80/min (regular), blood pressure is 120/76mmHg and respirations are 14/min. Her lungs are clear. Cardiac auscultation reveals normal first and second heat sounds and a mid-diastolic rumble at the apex. Echocardiography shows a mass in the left atrium. Which of the following is the most likely diagnosis?
. Congenital heart defect
. Infective endocarditis
Intracardiac tumor
. Myxomatous valve degeneration
Rheumatic fever and atrial thrombus
6) A 56-year-old male presents with progressively worsening dyspnea and ankle edema. He denies chest pain syncope or palpitations. He does not smoke or drink alcohol. He denies diabetes mellitus, hypertension, or hyperlipidemia. His temperature is 37.1°C (98.7°F), pulse is 70/min, blood pressure is 136/70mmHg, and respirations are 15/min. Examination shows elevated jugular venous pressure, bilateral ankle edema, and tender hepatomegaly. Chest auscultation shows bibasilar rales. His heat sounds are distant and there is no murmur. Chest x-ray shows mild cardiomegaly and a right-sided pleural effusion. ECG shows low voltage QRS complexes and nonspecific ST-T wave changes. Echocardiography shows normal left ventricular volume with symmetrical thickening of the left ventricular walls and slightly reduced systolic function. Which of the following would represent a potentially reversible cause of this patient’s heat disease?
. Amyloidosis
Hemochromatosis
Sarcoidosis
LED
Scleroderma
7) A 55-year-old male presents to the emergency room with right-sided weakness that has persisted for the past several hours. He also complains of severe central chest pain that is "ripping" in quality and radiates to his back. He has had hypertension for the past seven years and has not been taking any anti-hypertensive medication. He has been smoking one pack of cigarettes per day for the past 25 years. His father died of coronary artery disease at age 44 years. His temperature is 37.1°C (98.6°F), pulse is 78/min, blood pressure is 180/120 mm Hg in the right arm and 110/70 mm Hg in the left arm, and respirations are 16/min. He is diaphoretic and confuse. His neurological examination is significant for decreased power and tone in the right upper and right lower extremities. The rest of his physical examination is unremarkable ECG shows left axis-deviation and a chest x ray is normal. Based on these findings, what is the most likely diagnosis?
. Subarachnoid hemorrhage
Hemorrhagic stroke
. Paradoxical pulmonary embolism
Myocardial infarction with thromboembolism
Aortic dissection
8) A 54-year-old man is brought to the ER three hours after the onset of severe, 10/10, tearing, substernal chest pain radiating to his back. He still complains of pain and dizziness at the time of arrival. Physical examination demonstrates a pale thin male who is anxious and diaphoretic. His blood pressure is 90/60 mmHg in the right arm and 70/40 mmHg in the left arm. There is an 18 mmHg difference in systolic blood pressure between inspiration and expiration. His jugular veins are distended while sitting. Bedside echocardiogram demonstrates a moderate amount of pericardial fluid. Which of the following is the most likely diagnosis?
Acute myocardial infarction
. Acute pericarditis
. Aortic dissection
Pulmonary embolism
. Tension pneumothorax
9) A 22-year-old male presents to you with feelings of general malaise. He is always tired and has noticed that he has frequent headaches. Exam reveals an elevated arm blood pressure with a radial to femoral delay. ECG shows left ventricular hypertrophy and the chest-x ray is shown below. Close examination of the x-ray reveals a "3" sign. What is the most likely diagnosis in this patient?
For Student DES 2016-2017 last (1)
Tetralogy of F allot
Patent ductus arteriosus
Coarctation of aorta
Aortic aneurysm
Atrial septal defect
10) A 21-year-old woman presents to the ED complaining of lightheadedness. Her symptoms appeared 45 minutes ago. She has no other symptoms and is not on any medications. She has a medical history of mitral valve prolapse. Her HR is 170 beats per minute and BP is 105/55 mmHg. Physical examination is unremarkable. After administering the appropriate medication, her HR slows down and her symptoms resolve. You repeat a 12-lead ECG that shows a rate of 89 beats per minute with a regular rhythm. The PR interval measures 100 milliseconds and there is a slurred upstroke of the QRS complex. Based on this information, which of the following is the most likely diagnosis?
. Ventricular tachycardia
Atrial fibrillation
Atrial flutter with 3:1 block
. Wolff-Parkinson-White (WPW) syndrome
Lown-Ganong-Levine (LGL) syndrome
11) A 76-year-old man was operated on for a strangulated inguinal hernia and had approximately 40 cm of small bowel resected. On the morning of his third post-operative day, he falls while getting out of bed. Immediately after the fall, he is responsive but his speech is slurred and he cannot explain what happened. His pulse is 122/min, blood pressure is 96/50 mmHg, and respirations are 23/min. Lungs are clear to auscultation and his heart has a regular rate and rhythm. His neck veins are distended. An ECG is remarkable for a new onset right bundle branch block (RBBB). Immediate resuscitation is started with wide open intravenous fluids, but he becomes unresponsive. Shortly thereafter, his pupils start to dilate and his heart rate drops to 45/min. He eventually dies despite resuscitative efforts. What is the most likely cause of his death?
Hypovolemia accompanied by syncope
Acute ischemic stroke
. Myocardial infarction
. Post-operative sepsis
Massive pulmonary thromboembolism
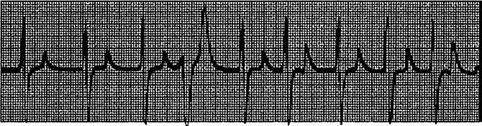
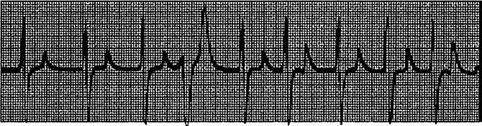
12) A 63-year-old female presents to your clinic complaining of palpitations. For the past 3 weeks, she has noticed pounding of her heart that comes and goes. Her symptoms are more frequent at night. Her only medicine is insulin for diabetes mellitus. On physical examination, she is alert and oriented, and in no distress. Her EKG is shown below. Which of the following best accounts for this patient's symptoms?
For Student DES 2016-2017 last (1)
. Sinus arrhythmia
. Irregularly irregular atrial activation
Variable AV node conduction
Atrial ectopy
Ventricular ectopy
13) A 53-year-old Caucasian female is admitted to the ER with hypotension. Her condition is considered very serious, and invasive hemodynamic monitoring is established. Blood pressure measured by intra- arterial method is 72/46 mmHg. Her heart rate is 120/min, regular. Pulmonary capillary wedge pressure (PCWP) estimated using Swan-Ganz catheter is 6 mmHg. Mixed venous oxygen concentration (MVo2) is 16 vol% (Normal = 15.5 vol%). Which of the following is the most likely cause of this patient's condition?
. Cardiogenic shock
Volume depletion
Septic shock
Hemorrhagic shock
Neurogenic shock
14) A 60-year-old female comes to your office for progressive exertional dyspnea and new-onset ankle swelling. She has been recently worked up for proteinuria and easy bruisability. Otherwise her past medical history is insignificant. She has a ten pack-year history of smoking and she drinks two to three glasses of wine every day. Her temperature is 37.1°C (98.8°F), blood pressure is 130/70 mmHg, pulse is 80/min and respirations are 14/min. There is mild jugular venous distention on physical examination. Chest auscultation shows scattered bibasilar crackles. Echocardiography reveals symmetrical thickening of the ventricular walls, normal ventricular dimensions and a slightly reduced systolic function. Which of the following is the most likely diagnosis?
Alcohol-related heart disease
. Hemochromatosis
. Sarcoidosis
Amyloidosis
Constrictive pericarditis
15) A 20-year-old white female presents with chest pain for the past few weeks. She describes the pain as sharp, located to the left of the sternum, and lasting 5-10 seconds at a time. There is no associated fever, cough, breathlessness, palpitations, or syncope. She does not smoke or drink alcohol. On cardiac examination, there is a short systolic murmur at the apex that disappears with squatting. Which of the following is the most likely diagnosis?
Mitral valve prolapse
Rheumatic heart disease
Ventricular septal defect
Infective endocarditis
. Bicuspid aortic valve
16) A 42-year-old man presents to the emergency department complaining of two weeks of weakness, low-grade fevers, and exertional shortness of breath. He also notes fingertip pain and urine that has been dark and cloudy recently. On physical examination, several of his proximal inter phalangeal joints are swollen. Which of the following diagnoses is most consistent with his presentation?
Rheumatoid arthritis
. Post-streptococcal glomerulonephritis
Adult Still's disease
Infective endocarditis
. Adrenal insufficiency
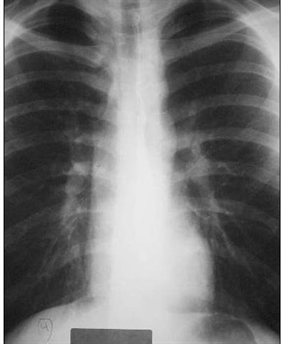
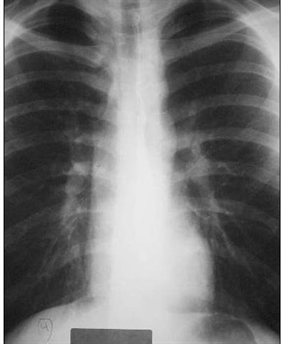
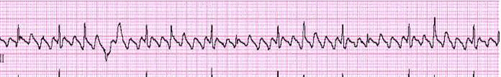
17) A 47-year-old female, who is a chronic alcoholic, is admitted to the hospital with epigastric pain, nausea, and vomiting. Her serum amylase and lipase levels are significantly elevated and the diagnosis of acute pancreatitis is made. She is maintained nothing by mouth (NPO), and receives intravenous hydration and narcotic analgesics. On the second day of hospitalization she develops progressive shortness of breath. Her temperature is 37.2°C (98.9°F), blood pressure is 110/66 mm Hg, pulse is 110/min, and respirations are 24/min. Her oxygenation is measured at 84% on 100% non-rebreather mask and the decision is made to intubate. Since the time of admission, she has received 5 liters of normal saline and has produced 3 liters of urine output. On examination, there is no evidence of jugular venous distention. Chest auscultation reveals diffuse bilateral crackles. Auscultation of the heart reveals normal heart sounds with no murmurs. A chest x-ray from the time of admission and one from the time of intubation are shown below. Based on these findings, what is the most likely diagnosis in this patient?
For Student DES 2016-2017 last (1)
Acute respiratory distress syndrome
Hospital acquired pneumonia
. Iatrogenic volume overload
Alcoholic cardiomyopathy
Congestive heart failure from myocardial infarction
18) A 37-year-old Cambodian woman presents to the emergency room with acute onset of left-sided weakness. She has been experiencing progressive exertional dyspnea, nocturnal cough and occasional hemoptysis over the past six months. She also describes frequent episodes of palpitations and irregular heartbeats. Which of the following is the most likely diagnosis?
Mitral stenosis
. Hypertrophic cardiomyopathy
. Aortic insufficiency
. Wolf-Parkinson-White syndrome
Primary pulmonary hypertension
19) A 67-year-old man presents to the emergency department after losing consciousness while shovelling snow near his house. He reports having had a similar episode one month ago while carrying heavy bags from the grocery store. The patient has reduced his physical activity level over the last several months because of progressive exertional dyspnea and fatigue. His past medical history is significant for diabetes mellitus and hypercholesterolemia. Metformin and simvastatin are his only medications. Which of the following physical examination findings is most likely in this patient?
Pulsus paradoxus
Late diastolic murmur
Capillary pulsations
Pleural friction rub
Systolic ejection murmur
20) A 17-year-old girl is brought to the ER 30 minutes after an episode where she lost consciousness. She is accompanied by her father who witnessed the event. He says that the patient recently broke up with her boyfriend and has been under a lot of stress. Her sleep has been poor. She has had three similar episodes over the last month. On exam, her heart rate is 90/min, respirations are 13/min, and blood pressure is 120/70 mmHg. She seems sleepy but can be aroused easily. She gives her correct name but is disoriented to time and place. Pupils are symmetric and reactive to light. Blood glucose level is 100 mg/dl. Which of the following findings would you most expect in this patient?
. Systolic murmur that increases with standing
. Pulsus paradoxus
Orthostatic hypotension
Positive stool guaiac test
Bitten tongue
21) A 50-year-old construction worker continues to have elevated blood pressure of 160/95 mmHg even after a third agent is added to his antihypertensive regimen. Physical examination is normal, electrolytes are normal, and the patient is taking no over-the-counter medications. Which of the following is the best next step for this patient?
Check pill count
. Evaluate for Cushing syndrome
. Check chest x-ray for coarctation of the aorta
Obtain a renal angiogram
Obtain an adrenal CT scan
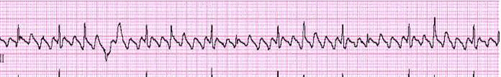
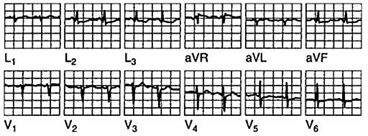
22) You are performing medical screening of new military recruits when an 18-year-old male reports several episodes of palpitation and syncope over the past several years. Physical examination is unremarkable. An ECG is obtained with excerpts shown below. What is the most likely diagnosis?
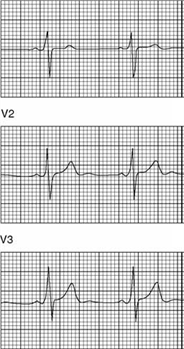
For Student DES 2016-2017 last (1)
Prior myocardial infarction secondary to coronary artery disease
Hypertrophic obstructive cardiomyopathy (HOCM)
Congenital prolonged QT syndrome
Preexcitation syndrome (Wolff-Parkinson-White
Rheumatic mitral stenosis
23) A 45-year-old mildly overweight male recovering from an anterior wall myocardial infarction develops sudden onset of left-sided chest pain. He appears agitated and restless. Two minutes later, he is unresponsive. His pulse is not palpable and ECG monitor shows sinus tachycardia at the rate of 130/min. He presented five days earlier with substernal chest pain and diaphoresis. He has had no dyspnea, extremity swelling or palpitations since admission. His past medical history is significant for diabetes mellitus type 2. Which of the following is the most likely diagnosis?
Interventricular wall rupture
Ventricular free wall rupture
Pulmonary infarction
Recurrent ischemia
Right ventricular infarction
24) A 34-year-old Caucasian woman presents to your office with dyspnea and severe chest pain after returning from a trip to Central Asia. The pain is localized on the left side and increases with inspiration. She also had one episode of hemoptysis. She does not smoke or consume alcohol. She is sexually active with one partner and uses oral contraceptives. Her father died of a myocardial infarction at 52 years of age. Her temperature is 36.7°C (98°F), pulse is 100/min, respirations are 28/min, and blood pressure is 110/66 mmHg. Which of the following most likely accounts for this patient's chest pain?
. Pulmonary artery distention
. Pericardial inflammation
. Myocardial ischemia
Pulmonary infarction
Pleural infection
25) A 32-year-old man develops severe nausea and vomiting after returning from a party. He also complains of chest pain that is more intense than any pain he has previously experienced. His past medical history is significant for HIV infection, alcohol abuse, and alcoholic hepatitis. He admits to using cocaine regularly. His temperature is 37.8°C (100°F), pulse is 120/min, respirations are 24/min, and blood pressure is 100/60 mmHg. Examination reveals injected conjunctivae and bilateral dilated pupils. Chest X-ray demonstrates a widened mediastinum and left-sided pleural effusion. EKG is unremarkable. The pleural fluid is found to have an elevated amylase content. Which of the following is the most likely diagnosis in this patient?
Acute pancreatitis
Peptic ulcer disease
Esophageal perforation
Myocardial ischemia
. Pulmonary embolism
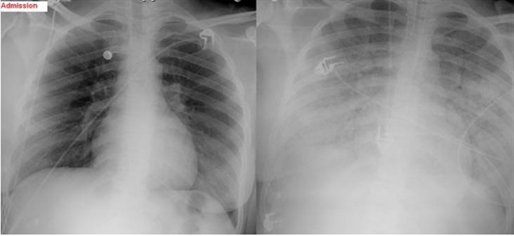
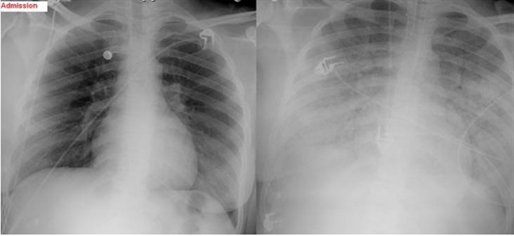
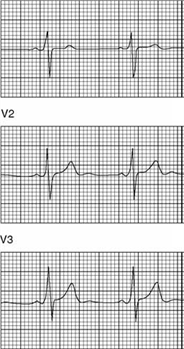
26) A 56-year-old diabetic female comes to the clinic with complaints of dizziness which has been going on for 3 weeks. She denies any dyspnea or diaphoresis. She says her blood glucose is well controlled and denies any allergy. Her BP is 155/90 mmHg. Her chest-x ray is unremarkable and her blood work is normal. The ECG is recorded below. What is the most likely diagnosis?
For Student DES 2016-2017 last (1)
. Mobitz type I heart block
Mobitz type II heart block
. Complete heart block
Atrial fibrillation
First degree heart block
27) A 54-year-old overweight man wakes up in the middle of the night with substernal discomfort that he describes as a burning sensation. He also complains of left-sided neck pain and feels sweaty and short of breath. He has never had similar pain before. Prior to going to bed he had eaten a big meal. His past medical history is significant for diabetes and hypertension. Which of the following physical findings is most consistent with this patient's clinical presentation?
. Fourth heart sound
Ejection-type systolic murmur
. Pulsus paradoxus
. Fixed splitting of S2
Friction rub
28) A 75-year-old patient presents to the ER after a syncopal episode. He is again alert and in retrospect describes occasional substernal chest pressure and shortness of breath on exertion. His blood pressure is 110/80 mmHg and lungs have a few bibasilar rales. Which auscultatory finding would best explain his findings?
A harsh systolic crescendo-decrescendo murmur heard best at the upper right sternal border
A diastolic decrescendo murmur heard at the mid-left sternal border
A holosystolic murmur heard best at the apex
A midsystolic click
. A pericardial rub
29) You are helping with school sports physicals and see a 16-year-old boy who has had trouble keeping up with his peers. Which of the following auscultatory findings suggests a previously undiagnosed ventricular septal defect?
A systolic crescendo-decrescendo murmur heard best at the upper right sternal border with radiation to the carotids; the murmur is augmented with exercise
A systolic murmur at the pulmonic area and a diastolic rumble along the left sternal border
A holosystolic murmur at the mid-left sternal border
A diastolic decrescendo murmur at the mid-left sternal border
A continuous murmur through systole and diastole at the upper left sternal border
30) A 46-year-old man presents to the emergency department with difficulty breathing and chest discomfort. His pain worsens with inspiration but does not radiate. He says that he has never had symptoms like this before. His past medical history is unremarkable. He works as a long-haul truck driver. On physical examination, his blood pressure is 110/70 mmHg, his heart rate is 110/min, his respiratory rate is 31/min, and his temperature is 36.7°C (98°F). ECG reveals sinus tachycardia but no ischemic ST-segment or T-wave changes. His chest X-ray is shown below. What is the most likely diagnosis in this patient?
For Student DES 2016-2017 last (1)
. Ascending aortic dissection
Pneumothorax
. Myocardial infarction
Pleural effusion
. Pulmonary embolism
31) A 32-year-old woman is brought to the emergency department with excruciating chest and neck pain. She is 6'2" and has long extremities. Her hand joints show significant extensibility. Which of the following additional findings is also likely in this patient?
Fourth heart sound (S4
. Early diastolic murmur
. Opening snap
Fixed splitting of the second heart sound (S2)
Kussmaul's sign
32) A 69-year-old male presents to the emergency department with severe pain in the back of his chest that began suddenly 6 hours ago, and 2 hours of difficulty walking due to leg weakness. He has never had such symptoms before. His past medical history is significant for hypertension, bleeding peptic ulcers, and deep vein thrombosis requiring inferior vena cava filter placement. He drinks 6-8 cans of beer each weekend and does not smoke cigarettes or use illicit drugs. Blood pressure taken from his right arm is 210/120 mmHg. His heart rate is 120/min and regular. Chest x-ray reveals a right-sided pleural effusion. EKG shows sinus tachycardia. What is the most likely diagnosis?
Angina pectoris
Myocardial infarction
Acute pericarditis
Aortic dissection
Pulmonary embolism
33) A 57-year-old male presents to the emergency department with recent-onset dyspnea and cough. He reports that his symptoms began earlier this morning while he was jogging, when he suddenly started feeling short of breath and very weak. In the emergency department, laboratory analysis reveals a markedly elevated serum b-type natriuretic peptide level. Which of the following clinical signs best correlates with this finding?
Wheezing
. Cyanosis
. Third heart sound
. Extremity edema
. Periumbilical bruit
34) A 65-year-old male presents to your office with a six-month history of periodic substernal pain. The pain episodes are experienced during strong emotion, last for 10-15 minutes, and resolve spontaneously. He has a long history of hypertension and diabetes mellitus, type 2. His right foot was amputated two years ago due to diabetes-related complications. You suspect angina pectoris and decide to perform myocardial perfusion scanning. It reveals uniform distribution of isotope at rest, but inhomogenesity of the distribution after dipyridamole injection. You conclude that the patient has ischemic heart disease. Which of the following effects of dipyridamole helped you in making the diagnosis?
. Increased heart contractility
. Coronary steal
Dilation of diseased vessels
Inhibition of platelet aggregation
Placebo effect
35) A 24-year-old military recruit is brought to the emergency room after suddenly collapsing while at training camp. Witnesses say he lost consciousness, and in the ER he appears confused. He had apparently been in his usual state of good health until this incident. His medical history includes allergic rhinitis for which he takes chlorpheniramine. On physical examination, his temperature is 4 1°C (106°F), blood pressure is 90/60 mmHg, respiratory rate is 22/min, and pulse is 130/min and regular. He appears restless. His pupils are 4mm in size, symmetric, and reactive to light. Lung exam reveals a few rales at both lung bases. His abdomen is soft, non-tender and bowel sounds are present. There is no neck stiffness. His skin is dry and hot. He has 2+ symmetric reflexes in the upper and lower extremities. Muscle tone and bulk are normal. Initial laboratory studies show: Hemoglobin 16.0 g/L, Platelets 120,000/mm3, Leukocyte count 18,500/mm3, Blood urea nitrogen (BUN) 40 mg/dL, Prothrombin time 17 sec, Partial thromboplastin time 40 sec. Which of the following is the most likely cause of his current condition
. Heat stroke
Meningitis
Anticholinergic toxicity
Serotonin syndrome
. Neuroleptic malignant syndrome
36) A 33-year-old Russian male reports concern over recurrent episodes of a "pounding" and "racing" heart over the last several months. He says his symptoms are worst while lying supine and while lying on his left side. On physical examination, his blood pressure is 150/55 mmHg and heart rate is 73/min. Which of the following is most likely responsible for his symptoms?
Aortic regurgitation
Pulmonary regurgitation
Mitral stenosis
Tricuspid stenosis
. Aortic stenosis
37) A 40-year-old male presents to the Emergency Room with a two-month history of occasional severe headache and blurring of vision. His past medical history is significant for hypertension controlled with hydrochlorothiazide for two years. His family history is significant for hypertension and diabetes. He smokes two packs a day and occasionally consumes alcohol. His blood pressure is 200/140 mmHg and heart rate is 75/min. Which of the following is most consistent with a diagnosis of malignant hypertension in this patient?
Left ventricular hypertrophy on ECG
Elevated serum creatinine level
. Papilledema
Oliguria
. Blood pressure ≥ 200/ 140 mmHg
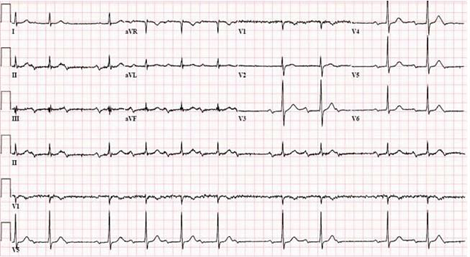
38) A 42-year-old woman has anterior chest pain of a somewhat atypical nature for many years. The patient’s pain has been present and relatively stable for a number of years, and the ECG shown in Fig. Is a stable one. What is the diagnosis?
For Student DES 2016-2017 last (1)
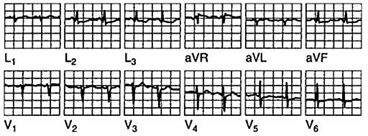
Inferior wall infarction
Anterior wall infarction
Ventricular aneurysm
Pericarditis
Nonspecific changes
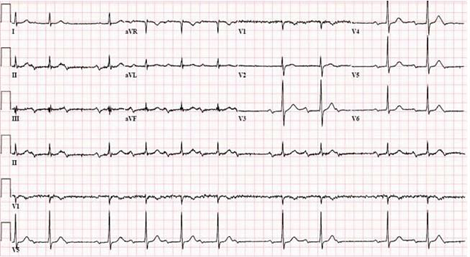
39) A 78-year-old man with advanced renal disease has the ECG shown in Fig. (lead II). What is the diagnosis?
For Student DES 2016-2017 last (1)
Hyperkalemia
Hypercalcemia
Hypernatremia
Pericarditis
Ventricular aneurysm
40) A 64-year-old white female presents for evaluation of two weeks of decreased appetite and nausea. She also notes occasional palpitations, which have been especially prominent over the past two days. Her medical history is significant for an anterior wall myocardial infarction one year ago and secondary congestive heart failure with left ventricular systolic dysfunction. Her current medications include aspirin, digoxin, furosemide, enalapril and metoprolol. On physical examination, her blood pressure is 120/80 mmHg, pulse is 106/min and respirations are 15/min. The remainder of her exam is unremarkable. Chest x-ray shows an enlarged cardiac silhouette and normal lung fields. On laboratory testing, her digoxin level is twice the upper limit of normal. You order an EKG. Which of the following arrhythmias is most specific for digitalis toxicity?
Atrial flutter
. Atrial fibrillation
Mobitz type II second-degree AV block
Multifocal atrial tachycardia
. Atrial tachycardia with AV block
41) A 45-year-old mildly overweight smoker presents with occasional episodes of nocturnal substernal chest pain that wakes her up from sleep. The episodes last 15-20 minutes and resolve spontaneously. She denies any illicit drug use. She leads a sedentary lifestyle but states that she can climb two flights of stairs without any discomfort. Her pulse is 78/min and regular, blood pressure is 130/70 mmHg and respirations are 13/min. Auscultation of her heart and lungs is unremarkable. Extended ambulatory ECG monitoring reveals transient ST segment elevations in leads V4-V6 during the pain attack. The pathophysiology of this patient's condition is most similar to that of which of the following?
. Lacunar stroke
Intermittent claudicatio
Abdominal aortic aneurysm
Pulmonary embolism
Raynaud phenomenon
42) A 65-year-old man comes to your office for a follow-up after his previous visits revealed inadequately controlled hypertension. He has no present complaints except difficulty walking uphill or climbing stairs, because of the pain in the right thigh, which makes him stop and rest. His past medical history includes stable angina, requiring coronary angioplasty and stenting 2 years ago; hypercholesterolemia; a 20-year history of hypertension; and a 10-year history of diabetes mellitus, type 2. His current medications are aspirin, metoprolol, hydrochlorothiazide, enalapril, amlodipine, pravastatin and glyburide. He smokes 1½packs of cigarettes per day and does not consume alcohol. His blood pressure is 160/100 mmHg in his right arm and 180/110 mmHg in his left arm. Which of the following findings will point to the potential cause of the resistant hypertension in this patient
. Increased pulsation of intercostal arteries
Continuous murmur in the paraumbilical area to the right
Increased urinal excretion of vanillylmandelic acid (VMA
Increased 24-hour urinary free cortisol excretion
. High aldosterone/renin ratio
43) A 43-year-old man is hospitalized with chest pain, lightheadedness and nausea. He describes the pain as dull and non-radiating. He has never had chest pain before, but does report occasional episodes of dyspnea and coughing. His medical history is significant for eczema. He is not presently taking any medications. His family history is significant for prostate cancer in his father and rheumatoid arthritis in his mother. He does not smoke or consume alcohol. The patient is admitted to the hospital and is given aspirin, low-molecular weight heparin, metoprolol and captopril. On day 2 of his hospitalization he complains of shortness of breath. Physical examination reveals prolonged expirations and bilateral wheezes. There are no crackles. You estimate the jugular venous pressure to be 7 cm with the patient's head elevated at 45 degrees. Which of the following is most likely responsible for this patient's current respiratory symptoms?
Pericarditis
. Bronchial infection
Recurrent myocardial ischemia
Right ventricular infarction
Drug side effect
44) A 34-year-old female presents to the ER with difficulty breathing and dizziness. Blood pressure tracing from an arterial line placed in the ER is depicted below. Which of the following best accounts for these findings?
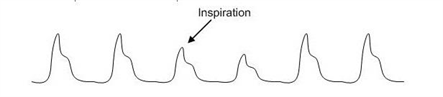
For Student DES 2016-2017 last (1)
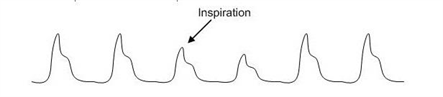
Severe asthma
. Lobar pneumonia
Mitral stenosis
Aortic regurgitation
Panic attack
45) A 43-year -old man complains of progressive weakness and shortness of breath over the last two weeks. He denies any chest or muscle pain, nausea, vomiting or weight loss. He had a recent upper respiratory tract infection. His heart rate is 90/min and blood pressure is 110/70 mmHg. Jugular venous pressure is normal. Lungs are clear to auscultation. His chest x-ray is shown below. Which of the following is the most likely additional finding in this patient?

For Student DES 2016-2017 last (1)

. Audible fourth heart sound
. Non-palpable point of maximal impulse
. Pulsus bisferiens
. Fixed splitting of the second heart sound
Opening snap
46) A 55-year-old male is admitted to the ICU after being involved in a motor vehicle accident. He requires exploratory laparotomy for suspected bowel perforation. Two days after the surgery he remains hypotensive and requires both aggressive intravenous fluids and vasopressors to maintain his blood pressure. On physical examination, you note the fingertip changes pictured below. All four extremities feel cold to touch. Which of the following is most likely responsible?

For Student DES 2016-2017 last (1)

. Septic emboli
Raynaud's phenomenon
. Norepinephrine-induced vasospasm
Cholesterol emboli
Superior vena cava syndrome
47) A 32-year-old man presents to the emergency department with a three-day history of fever, cough and weakness. His blood pressure is 120/80mmHg and his heart rate is 110/min. Physical examination reveals multiple needle tracks on his arms. ECG shows sinus tachycardia but is otherwise normal. Chest X-ray shows scattered round lesions in the peripheral lung fields bilaterally. Urinalysis is positive for 2+ protein. Which of the following accompanying findings is most likely in this patient?
. S4 when patient is in the left lateral decubitus position
Systolic murmur that increases on inspiration
. Diastolic murmur heard best with the patient sitting up
Paradoxical splitting of S2
Systolic murmur that increases when the patient stands up
48) A 41-year-old intravenous drug abuser presents with shortness of breath and pleuritic chest pain. He is febrile with a temperature of 103.5°F. He has no skin lesions and funduscopic exam is negative. He has jugular venous distension that increases with compression of the liver. The liver is pulsatile. The jugular venous pulse shows a prominent v wave. The patient has splenomegaly. Heart auscultation reveals a holosystolic murmur heard best at the left lower sternal border. The murmur increases with inspiration (Müller maneuver). Which of the following is the most likely diagnosis?
Bacterial endocarditis
Pericarditis
Rheumatic fever
. Pericardial effusion
. Mitral valve prolapse
{"name":"DES part2 episode3", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"109) A 34-year-old obese Caucasian female complains of periodic visual obscurations. She has episodes during which she \"goes blind\" for several seconds when standing up or stooping forward abruptly. She also describes frequent morning headaches over the last two months for which she has had to take ibuprofen or aspirin almost every morning. She takes no other medications. Past medical history is insignificant aside from one uncomplicated vaginal delivery. She denies use of alcohol, tobacco, or illicit drugs. She is afebrile with a blood pressure of 138\/88 mmHg and pulse of 93\/min. Visual field testing shows enlarged blind spots. There are no other significant findings on neurologic examination. Which of the following is the most likely cause of this patient's symptoms?, 110) A 30-year-old man is concerned about \"floating spots\" and blurred vision in his right eye. He had a serious injury of his left eye several weeks ago, which eventually led to vision loss in that eye. Inspection reveals a moderate perilimbal flush. What is the most probable cause of this patient's condition?","img":"https://www.quiz-maker.com/3012/images/ogquiz.png"}
More Quizzes
Guess the Heroic Architecture of the world
1470
BSW Post Tournament Survey
1470
BFF or BAEFF? Prepare a party together and we’ll reveal your true intentions.
320
QUIZ#10
100
US History Regents Practice Test - Free
201028185
What Business Should I Start? Free Startup Guide
201031563
Free Numbers: Practice Test & Study Guide
201025340
Free Classical vs Romantic Music: Test Your Knowledge
201026044
Individual Differences: B to 6
15821938
Ready for a Challenge? Take the Free Tool and Die Test
201030811
Free Supplementary Angles
201022763
Ace Dante's Inferno: Test Your Canto I Mastery
201038991