DES part2 episode4
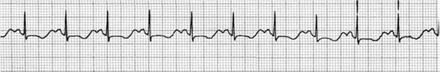
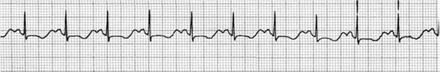
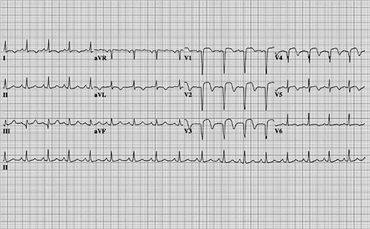
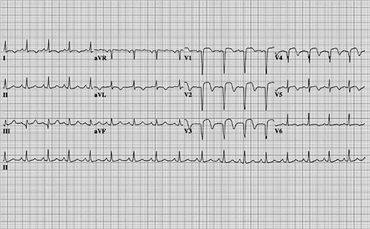
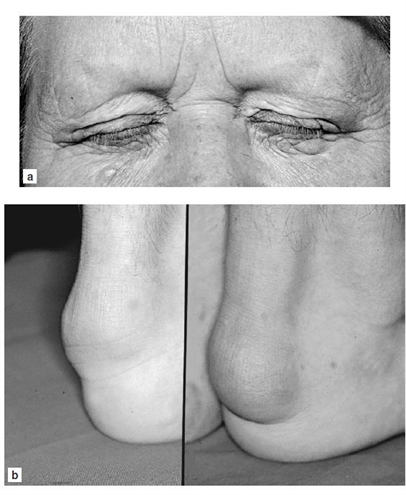
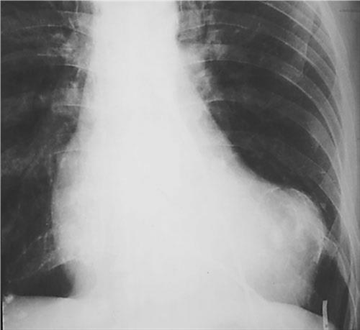
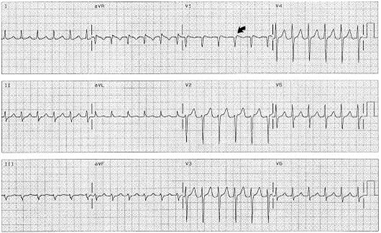
49) A 23-year-old woman who is an elementary school teacher is brought to the ED after syncopizing in her classroom while teaching. Prior to passing out, she describes feeling light-headed and dizzy and next remembers being in the ambulance. There was no evidence of seizure activity. She has no medical problems and does not take any medications. Her father died of a “heart problem” at 32 years of age. She does not smoke or use drugs. BP is 120/70 mmHg, pulse rate is 71 beats per minute, RR is 14 breaths per minute, and oxygen saturation is 100% on room air. Her physical examination and laboratory results are all normal. A rhythm strip is seen below. Which of the following is the most likely diagnosis?
For Student DES 2016-2017 last (1)
Long QT syndrome
Complete heart block
Wolff-Parkinson-White syndrome
Atrial flutter
Lown-Ganong-Levine syndrome
50) A 22-year-old man presents to the ED with a history consistent with an acute MI. His ECG reveals ST elevations and his cardiac biomarkers are positive. He has been smoking half a pack of cigarettes per day for the last 3 months. He drinks alcohol when hanging out with his friends. His grandfather died of a heart attack at 80 years of age. The patient does not have hypertension or diabetes mellitus and takes no prescription medications. A recent cholesterol check revealed normal levels of total cholesterol, low-density lipoprotein (LDL), and high-density lipoprotein (HDL). Which of the following is the most likely explanation for his presentation?
Cigarette smoking
Incorrectly placed leads on the ECG
. Family history of heart attack at age 80 years
Undisclosed cocaine use
. Alcohol use
51) A 29-year-old woman presents to the emergency department with a 3-week history of being awakened by a dull, prolonged chest pain that occurs 3–4 times a week. She is a smoker but has never suffered a myocardial infarction (MI) or had chest pain before and has no family history of early MI. Results of a 12-lead ECG are normal. Her first set of cardiac enzyme measurements (creatine kinase, creatine kinase-MB fraction, troponin I) are negative. If coronary angiography were taken at the time of her chest pain, which of the following findings is most like?
Coronary artery spasm
No abnormal findings
Greater than 80% stenosis in at least two coronary arteries
Plaque rupture and thrombosis
Coronary artery dissection
52) A 42-year-old man presents to the emergency department with a complaint of increasing shortness of breath when walking to get his newspaper, difficulty breathing while lying fl at, and a 4.5-kg (10-lb) weight gain over the past month. He is afebrile, his pulse is 75/min, and his blood pressure is 98/50 mmHg. On examination he smells of alcohol and has 2+ pitting edema in the lower extremities and a third heart sound. X-ray of the chest reveals cardiomegaly. What additional findings must be present to confirm this man’s underlying diagnosis?
Hepato-jugular reflux and pulmonary congestion
Left ventricular dilation and aortic insufficiency
Left ventricular dilation and systolic dysfunction
Myocardial thickening and diastolic dysfunction
Pulmonary congestion and diastolic dysfunction
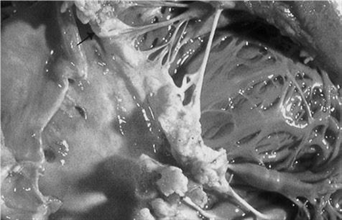
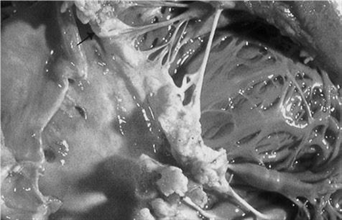
53) A 69-year-old man with rheumatic heart disease presents to the emergency department complaining of a fever and weakness on his left side. On physical examination the patient is weak in his left upper extremity and he draws only the right half of a clock. Shortly after his presentation, the patient dies, and an autopsy is performed. A gross view of the patient’s heart is shown in the image. Which of the following is a risk factor for the type of lesion pictured?
For Student DES 2016-2017 last (1)
Coronary artery disease
Hypertension
Mitral valve prolapse
Prosthetic valve replacement
Prolonged bedrest
54) A 42-year-old man with known valvular heart disease develops a fever for 1 week. He appears unwell; findings include a pansystolic murmur at the apex that radiates to the axilla and a soft S1 sound. He has petechiae on his conjunctival sac, linear hemorrhages under a few fingernails, and painful, tender, and erythematous nodules on some of the distal fingertips. Which of the following is the most responsible mechanism for these physical findings?
Direct bacterial invasion
Vascular phenomena
Immune response
Preexisting cardiac dysfunction
Valvular damage
55) A 67-year-old man presents with an anterior myocardial infarction (MI) and receives thrombolytic therapy. Three days later, he develops chest pain that is exacerbated by lying down, and his physical findings are normal except for a friction rub. His ECG shows evolving changes from the anterior infarction but new PR-segment depression and 1-mm ST-segment elevation in all the limb leads. Which of the following is the most likely diagnosis?
Reinfarction
Post-MI pericariditis
Pulmonary embolus
Dissecting aneurysm
Viral infection
56) A 77-year-old man, complaining of abdominal pain, anorexia, and nausea and vomiting over the past 24 hours, presents to the clinic with his son. The son reveals that his father has also complained of blurred vision. The patient’s vital signs are stable and his abdomen is soft, but he appears to be somewhat confused. He is currently taking metoprolol, digoxin, and hydrochlorothiazide for ischemic congestive heart failure. His son says that sometimes his father confuses his medications. The patient also has renal insufficiency with a baseline serum creatinine of 2.6 mg/dL. The ECG reveals a widened QRS complex and a new first-degree heart block. Which of the following is the most likely cause of this patient’s symptoms?
Digoxin toxicity
Myocardial infarction
Gastroenteriti
Hypovolemia secondary to thiazide diuretic overuse
Hypocalcemia
57) Two and a half weeks after coronary artery bypass grafting, a 63-year-old man returns to the emergency department acutely short of breath. The patient states that he began having chest pain and shortness of breath approximately 1 hour earlier. He has a history of hypertension, diabetes, and two myocardial infarctions. On examination he is hypoxic with an oxygen saturation of 86% on room air. Other vital signs and results of a physical examination are normal. ECG shows no interval change from his most recent ECG. CT of the chest is shown in the image. What is the most likely etiology of this patient’s shortness of breath?

For Student DES 2016-2017 last (1)

Aortic dissection
Pleural effusion
Exacerbation of chronic obstructive pulmonary disease
Pulmonary embolus
Myocardial infarction
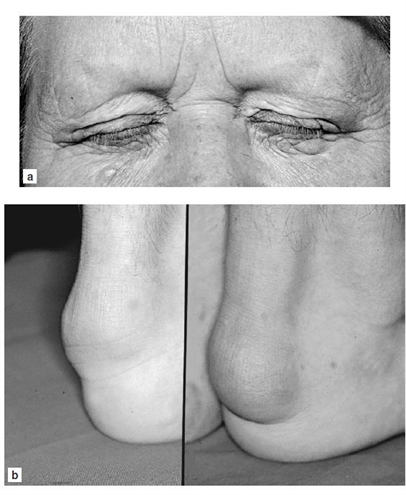
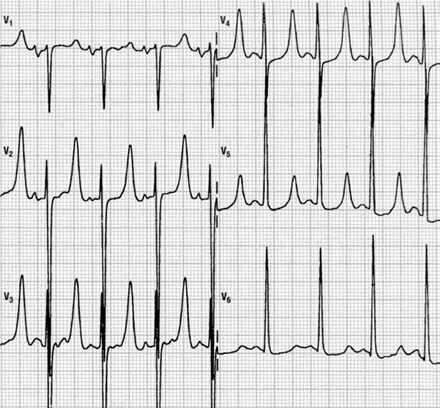
58) A 35-year-old woman presents to the clinic because of visual problems. She states that she has always had difficulty looking up, and over the past few years her overall vision has become blurry. Review of symptoms is notable for several recent episodes of “near fainting.” She takes no medication and has no other medical history, and has not seen a physician for 7 years. Because she was adopted as a child, she does not know her family history, but her son has required special tutoring at school. The patient also remarks that her son seems to have been dropping objects lately. Physical examination reveals bilateral ptosis. Her extraocular movements are intact and the pupils are equal, round, and reactive. Her corrected visual acuity is 20/100 in the right eye and 20/120 in the left eye. The view of the fundus is obscured. On ambulation she raises her knees and makes a slapping sound on the floor as she walks. ECG indicates heart block. What is the pathogenesis of this patient’s disorder?
Borrelia burgdorferi infection
Trinucleotide repeat expansion
Deletion mutation in dystrophin
X-linked emerin deficiency
Frameshift mutation in dystrophin
59) A college sophomore is found by his roommate emergency department. After resuscitation, the man complains of a severe headache and photophobia that is accompanied by dizziness, nausea, vomiting, and neck pain. Physical examination is noteworthy for positive Kernig’s and Brudzinski’s signs as well as petechiae on the trunk and mucocutaneous bleeding. Laboratory studies show: WBC count: 17,000/mm3, Hemoglobin: 11 g/dL, Platelet count: 70,000/mm3, Bleeding time: 10 min, Prothrombin time: 17 sec, Activated partial thromboplastin time: 47 sec, Thrombin time: 18 sec. A peripheral blood smear is shown in the image. Which of the following is the most likely diagnosis?
For Student DES 2016-2017 last (1)
Disseminated intravascular coagulation
Thrombotic thrombocytopenic purpura
Factor V Leiden
Protein C deficiency
Immune thrombocytopenic purpura
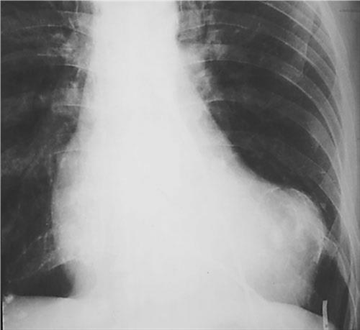
60) A 43-year-old woman presents to the emergency department because of chest pain, shortness of breath, and worsening fatigue for the past day. The chest pain initially worsened with lying down and improved with leaning forward, but now it seems equal in intensity over all positions. On physical examination she has labored, fast breathing and appears to be in pain. She has jugular venous distention. She is tachycardic, has a regular rhythm, and has distant heart sounds with a friction rub. Her lungs are clear to auscultation bilaterally, her abdominal examination is benign, and she has no peripheral edema. Her temperature is 39.0°C (102.2°F), pulse is 126/min, blood pressure is 89/66 mmHg, respiratory rate is 32/min, and oxygen saturation is 98% on room air. X-ray of the chest is shown in the image. Which of the following is the most likely diagnosis?
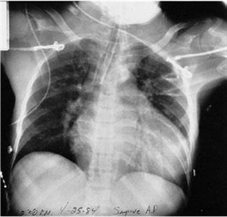
For Student DES 2016-2017 last (1)
Cardiac tamponade
Pericarditis
Decompensated congestive heart failure
Tension pneumothorax
Panic attack
61) A 37-year-old woman with sarcoidosis presents to her primary care physician complaining of progressive fatigue and shortness of breath over the past 3 months. She also reports that her socks and shoes do not fit the way they used to and that she fainted a few weeks ago for the first time in many years. She denies any recent illness and only takes medications to control her sarcoid. She states that she is more comfortable sitting than lying down. She has jugular venous distension, which increases with inspiration. Her blood pressure is 134/87 mmHg, respiratory rate is 17/min, pulse is 96/min, and temperature is 37.2°C (98.9°F). She also has decreased breath sounds bilaterally at the bases. ECG shows decreased QRS voltage. An echocardiogram shows a thick left ventricle. Which of the following is the most likely diagnosis?
Aortic stenosis
Hypertensive heart disease
Cardiac tamponade
Restrictive cardiomyopathy
Pericarditis
62) A 1-week-old infant presents to her general pediatrician’s office for a well-child visit. She was born at 37 weeks’ gestation without complications. Her temperature is 37.0°C (98.6°F), pulse is 130/min, blood pressure is 72/54 mmHg, and respiratory rate is 28/min. She is currently at the 50th percentile for weight and 75th percentile for height. She is acyanotic and has a wide, fixed split S2, with a 2/6 systolic ejection murmur at the left upper sternal border. The remainder of the examination is unremarkable. Which of the following is the most likely diagnosis?
Atrial septal defect
Dextratransposition of the great arteries
Coarctation of the aorta
Tetralogy of Fallot
Ventricular septal defect
63) Which of the following patients has the lowest clinical probability for the diagnosis of pulmonary embolism (PE)?
A 21-year-old woman 2 days after a cesarean delivery
. A 62-year-old man with pancreatic cancer
A 55-year-old woman on estrogen replacement therapy who underwent a total hip replacement procedure 3 days ago
. A 45-year-old man with factor V Leiden deficiency
A 39-year-old man who smokes cigarettes occasionally and underwent an uncomplicated appendectomy 2 months ago
64) A 72-year-old man presents with shortness of breath and increased home oxygen requirement. The patient has coronary artery disease, he has had two previous myocardial infarctions, and he has a history of chronic obstructive pulmonary disease requiring 2 L of continuous home oxygen. The patient has a 45-pack-year history of smoking. He is unable to walk more than a block and the swelling in his legs has worsened. The physician suggests measuring a brain natriuretic peptide (BNP) level to distinguish a cardiac from a pulmonary cause of his symptoms. Which of the following statements regarding BNP is true?
BNP acts to decrease venous capacitance and increase preload
BNP is decreased in the setting of left ventricular dysfunction
BNP is secreted by the cardiac atria
BNP is secreted in response to hypovolemia
BNP levels cannot differentiate systolic and diastolic dysfunction
65) A 77-year-old man with a history of hypertension, hypercholesterolemia, chronic obstructive pulmonary disease, and a 90-pack-year smoking history presents to the emergency department with lethargy and abdominal pain. His temperature is 36.9°C (98.5°F), blood pressure is 82/54 mmHg, pulse is 125/min, and respiratory rate is 16/min. A pulsatile abdominal mass is palpable just superior to the umbilicus. There is diffuse abdominal tenderness, although rebound tenderness and guarding are absent. There is also slight skin discoloration noted in the left lower back. Which of the following is the most likely diagnosis?
Aortic dissection
Mesenteric ischemia
Perforated gastric ulcer
Ruptured abdominal aortic aneurysm
Stroke
66) A 52-year-old African-American man with a history of smoking and asthma presents to the emergency department complaining of shortness of breath. He has alcohol on his breath and admits to drinking 3–4 beers each night plus an occasional “mixed drink.” He denies drug use and states that he has been feeling well until recently, when he began to sleep with more pillows and to become out of breath when walking. His blood pressure is 143/89 mmHg, respiratory rate is 21/min, pulse is 112/min, and he is afebrile. On physical examination he has a laterally displaced point of maximal impulse and an S3 gallop, as well as rales over his right lung base. X-ray of the chest shows cardiomegaly and a pleural effusion. Echocardiogram reveals an ejection fraction of 25%. Which of the following is the most likely diagnosis?
Asthma exacerbation
Delirium tremens
Dilated cardiomyopathy
Hypothyroidism
Endocarditis
67) A cardiologist is called to consult on the care of a 2-day-old girl delivered at 33 weeks’ gestation. The infant is lying supine in her isolette. She is acyanotic, but has a heart rate of 192/min and a respiratory rate of 60/min. She has a nonradiating continuous machinery murmur at the left upper sternal border that remains the same with compression of the ipsilateral, then contralateral jugular veins. S1 and S2 are normal. Her peripheral pulses are bounding. Which of the following is the most likely diagnosis?
Aortic stenosis with aortic regurgitation
Patent ductus arteriosus
Systemic arteriovenous fistula
Venous hum
Ventricular septal defect
68) A 59-year-old man presents to his internist for a routine visit. He has no complaints, and review of symptoms is negative. His past medical history is significant for poorly controlled hypertension for 15 years due to noncompliance with antihypertensive medications. He takes hydrochlorothiazide 25 mg orally four times a day. His family history is significant for hypertension, heart failure, and stroke. He has a 30-pack-year smoking history and drinks two beers a day. On physical examination he is a mildly obese man in no acute distress. He has a normal jugular venous pressure. He has a prominent point of maximum impulse, regular rate and rhythm, normal S1, loud S2, and audible S4 with no murmurs. His lungs are clear to auscultation bilaterally, and he has no signs of edema. His abdominal and neurologic examinations are within normal limits. His temperature is 37.0°C (98.6°F), pulse is 81/min, respiratory rate is 12/min, blood pressure is 165/96 mmHg, and oxygen saturation is 100% on room air. His ECG shows normal sinus rhythm with large amplitude of the S wave in V1 and V2 and of the R wave in V5 and V6. Also present are diffuse ST segment/T wave changes, widened bifid P waves, and prolonged QRS waveforms. Which of the following is the most likely diagnosis?
Acute myocardial infarction
Cerebrovascular accident
Dilated cardiomyopathy
Pericarditis
Left ventricular hypertrophy
69) A 60-year-old woman is transferred to a physician from an outside hospital following a motor vehicle collision. Her medical history is notable for Osler-Weber-Rendu syndrome. She is otherwise healthy. Which of the following triads is most likely to characterize her medical history prior to the collision?
Hypertension, bradycardia, and irregular respirations
Telangiectasia, recurrent epistaxis, and positive family history
Jaundice, fever, and right upper quadrant pain
Venous stasis, hypercoagulability, and endothelial damage
Symptoms of hypoglycemia, low blood sugar, and relief with increase in blood sugar
70) Three months after an anterior MI, a 73-yearold man has a follow-up ECG. He is clinically feeling well with no further angina symptoms. His ECG shows Q waves in the anterior leads with persistant ST-segment elevation. The current ECG is most compatible with which of the following diagnosis?
For Student DES 2016-2017 last (1)
Ventricular aneurysm
Acute infarction
Hibernating myocardium
Early repolarization
Silent infarction
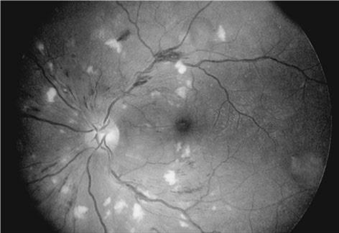
1) A 47-year-old woman develops accelerated hypertension (blood pressure 210/105 mmHg) but no clinical symptoms except frequent headaches. Which of the following findings are most likely on examination of the fundii?
For Student DES 2016-2017 last (1)
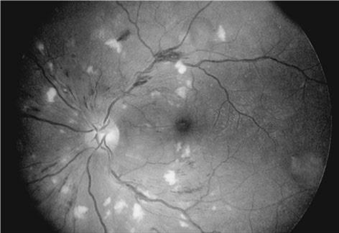
Retinitis obliterans
Cotton wool spots
Retinal detachment
Foveal blindness
Optic atrophy
2) A 32-year-old man presents for rountine evaluation. He has no symptoms but has noticed some new “nodules” on his legs. Physical examination reveals lumps on his Achillis tendon, yellow lesions around his eyes, and pigmentation of his iris. Which of the following is the most likely diagnosis?
For Student DES 2016-2017 last (1)
Familial hyperlipidemia
Diabetes
Myxedema
Chronic renal disease
An inherited defect of glycogen utilization
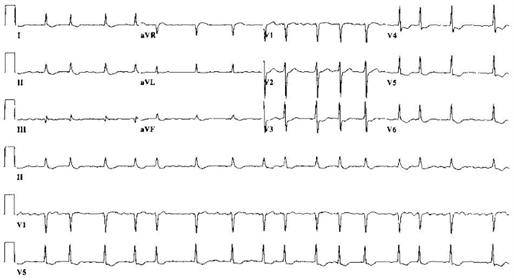
3) A 54-year-old woman presents to the ED because of a change in behavior at home. For the past 3 years, she has end-stage renal disease requiring dialysis. Her daughter states that the patient has been increasingly tired and occasionally confused for the past 3 days and has not been eating her usual diet. On examination, the patient is alert and oriented to person only. The remainder of her examination is normal. An initial 12-lead ECG is performed as seen on the following page. Which of the following electrolyte abnormalities best explains these findings?
For Student DES 2016-2017 last (1)
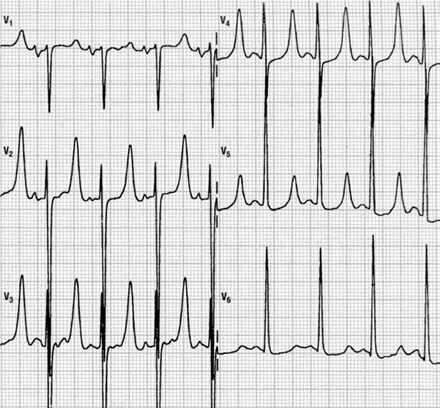
Hypokalemia
Hyperkalemia
Hypocalcemia
Hypercalcemia
Hyponatremia
4) A 42-year-old man found vomiting in the street is brought to the ED by emergency medical services (EMS). He has a known history of alcohol abuse with multiple presentations for intoxication. Today, the patient complains of acute onset, persistent chest pain associated with dysphagia, and pain upon flexing his neck. His BP is 115/70 mmHg, HR is 101 beats per minute, RR is 18 breaths per minute, and oxygen saturation is 97% on room air. As you listen to his heart, you hear a crunching sound. His abdomen is soft with mild epigastric tenderness. The ECG is sinus tachycardia without ST-T–wave abnormalities. On chest radiograph, you note lateral displacement of the left mediastinal pleura. What is the most likely diagnosis?
Aspiration pneumonia
Acute pancreatitis
Pericarditis
Esophageal perforation
Aortic dissection
5) A 65-year-old man with a history of chronic hypertension presents to the ED with sudden-onset tearing chest pain that radiates to his jaw. His BP is 205/110 mmHg, HR is 90 beats per minute, RR is 20 breaths per minute, and oxygen saturation is 97% on room air. He appears apprehensive. On cardiac examination you hear a diastolic murmur at the right sternal border. A chest x-ray reveals a widened mediastinum. Which of the following is the preferred study of choice to diagnose this patient’s condition?
Electrocardiogram (ECG)
Transthoracic echocardiography (TTE
Transesophageal echocardiography (TEE)
Magnetic resonance imaging (MRI)
Computed tomography (CT) scan
6) A 36-year-old man is seen because of palpitations. He admits to precordial discomfort, weakness, and anxiety. His pulse is 150/min, and his blood pressure is 124/70 mmHg. Heart sounds are normal. Carotid sinus pressure gradually changes the rate to 75/min, but when released, the pulse rate returns to 150/min. Which of the following is the most likely diagnosis?
Atrial flutter with 2:1 block
Paroxysmal atrial tachycardia with 2:1 block
Sinus arrhythmia
Nodal tachycardia
Atrial fibrillation
7) A 25-year-old man complains of left precordial chest pain that radiates to the left shoulder but not down the left arm. The pain is accentuated by inspiration and relieved by sitting up. The pain is accompanied by fever and chills. His blood pressure is 105/75 mmHg, pulse 110/min and regular, and temperature 37.5°C. Aside from the tachycardia, there are no abnormal physical findings in the heart or lungs. The ECG shows STsegment elevation in all leads except aVR and VI. On the third hospital day, the patient’s blood pressure falls, JVP rises, and he goes into CHF. Which of the following is the most likely diagnosis?
A second pulmonary embolus
Cardiac tamponade
Extension of a myocardial infarct
Rupture of a chordae tendineae
Secondary bacterial infection
8) Image below is an x-ray of an asymptomatic 64-year-old male executive coming in for his regular annual medical checkup. He had an anterior Q wave MI 4 years ago. What is your diagnosis?
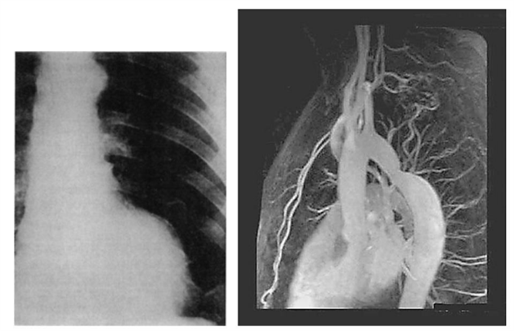
For Student DES 2016-2017 last (1)
Calcific pericarditis
Pleuropericarditis
Left ventricular aneurysm
Normal
Hydatid cyst
9) A 42-year-old female with acute pericarditis develops jugular venous distention and hypotension. The ECG shows electrical alternans. Which of the following is the most likely additional physical finding?
Basilar rales halfway up both posterior lung fields
Pulsus paradoxus
S3 gallop
Epigastric tenderness
Strong apical beat
10) A 36-year-old man presents to the clinic with complaints of a genital sore. The patient is a sexually active heterosexual involved with three partners and practices unprotected intercourse. Four days ago he noted a painless sore on his penis. He is afebrile, with a heart rate of 80/min and blood pressure of 120/77 mmHg. Physical examination reveals a solitary ulcerated lesion located on the lateral aspect of his penis. The lesion is nontender and associated with bilateral inguinal lymphadenopathy. Physical examination is otherwise normal. If left untreated, this man is at increased risk for which of the following?
Ascending aortic aneurysm
Coronary artery aneurysm
Endocarditis
Rupture of ventricular free wall
Mitral valve stenosis
11) The laboratory results shown in Table 1–1 are obtained from the investigation of a 37-year-old African-American woman who has a blood pressure at rest of 140/100 mmHg. Which of the following is the most likely diagnosis?
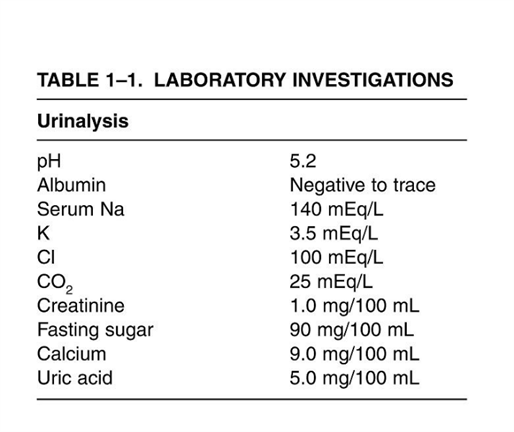
For Student DES 2016-2017 last (1)
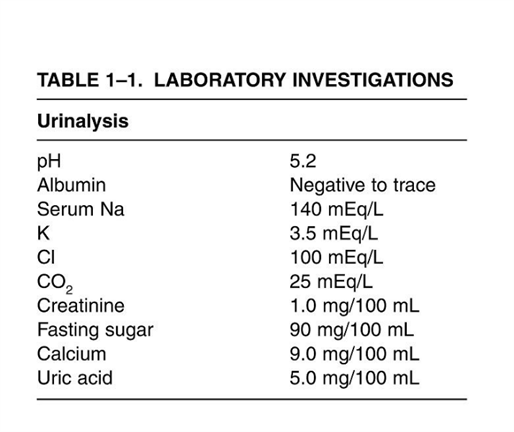
Cushing’s syndrome
Primary aldosteronism
Essential hypertension
Bilateral renal artery stenosis
Pyelonephritis
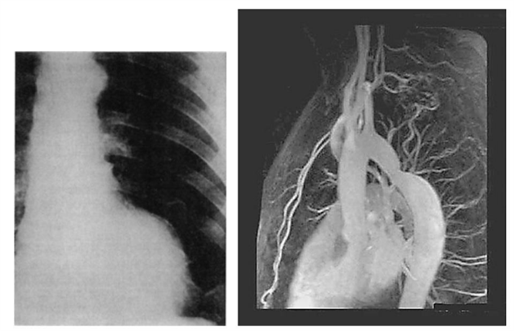
12) Image below is the x-ray and MR of an 8-year-old boy who had easy fatigability and a soft, continuous murmur in the upper back. ECG revealed minimal LVH. What is your diagnosis?
For Student DES 2016-2017 last (1)
Aortic stenosis
Patent ductus arteriosus
Coarctation of the aorta
Peripheral pulmonary stenosis
Pulmonary valvular stenosis
13) A 78-year-old woman presents to a nursing home physician complaining of palpitations over the past several months. Her episodes are not associated with any chest pain, dizziness, or loss of consciousness. The patient reports that she spent several weeks in the hospital as a child with rheumatic fever. ECG is shown in the image. Which of the following is the most likely diagnosis?
For Student DES 2016-2017 last (1)
Atrial fibrillation
Multifocal atrial tachycardia
Atrial flutter
Paroxysmal supraventricular tachycardia
Paroxysmal atrial tachycardia
14) A boy is delivered at 37 weeks gestation via spontaneous vaginal delivery. He is the product of a normal pregnancy and was delivered without complications. Prenatally the mother was blood type B and was rubella immune and negative for Rh antibody, group B streptococci, rapid plasma reagin, hepatitis B surface antigen, gonorrhea, and chlamydia. The patient appears cyanotic. He is breathing at a rate of 60/min and his heart rate is 130/min. He has a normal S1 and S2. There is a harsh holosystolic murmur that is loudest at the left lower sternal border. His examination reveals palpable nonbounding peripheral pulses bilaterally. Which of the following is the most likely diagnosis?
Coarctation of the aorta
Truncus arteriosus
Dextraposed transposition of the great arteries
Tetralogy of Fallot
Patent ductus arteriosus
15) A 75-year-old man comes into the emergency department with a 10-minute history of crushing substernal chest pain radiating to his left arm. This man is well known to the staff due to his long history of chest pain. His creatine phosphokinase level is elevated and his troponin T level is 0.4 ng/mL. Which of the following is the most likely diagnosis?
Acute myocardial infarction
Stable angina
Hypochondriasis
Unstable angina
Prinzmetal’s angina
16) A 55-year-old man with hypertension and a one-pack-per-day smoking history presents to the ED complaining of three episodes of severe heavy chest pain this morning that radiated to his left shoulder. In the past, he experienced chest discomfort after walking 20 minutes that resolved with rest. The episodes of chest pain this morning occurred while he was reading the newspaper. His BP is 155/80 mmHg, HR 76 beats per minute, and RR 15 breaths per minute. He does not have chest pain in the ED. An ECG reveals sinus rhythm with a rate of 72. A troponin I is negative. Which of the following best describes this patient’s diagnosis?
Variant angina
ST-elevation MI (STEMI
Stable angina
Non–ST-elevation MI
Unstable angina
17) Auscultation of the heart of a 17-year-old boy reveals an increased intensity of the pulmonary component of the second heart sound. He complains of dyspnea on exertion but no other cardiac or pulmonary symptoms. Which of the following explanations is the most likely cause of his dyspnea?

For Student DES 2016-2017 last (1)

Pulmonary stenosis
Pulmonary hypertension
Aortic stenosis
Systemic hypertension
MI
18) A 22-year-old woman complains of palpitations and has a regular heartbeat at a rate of 170/min, with a blood pressure of 110/70 mmHg. The rate abruptly changes to 75/min after applying carotid sinus pressure. Which of the following is the most likely diagnosis?
For Student DES 2016-2017 last (1)
Sinus tachycardia
Paroxysmal atrial flutter
Paroxysmal atrial fibrillation
Paroxysmal ventricular tachycardia
Paroxysmal supraventricular tachycardia (PSVT
19) A 58-year-old man with hypertension is brought to the emergency room after sudden onset chest pain that radiates to his back and arms. He is in moderate distress with a blood pressure of 160/90 mmHg in the left arm and 120/70 mm Hg in the right arm. Cardiac examination reveals a soft second heart sound and a murmur of aortic insufficiency. His ECG shows sinus tachycardia but no acute ischemic changes, and the chest x-ray (CXR). Which of the following is the most appropriate next step in confirming the diagnosis?

For Student DES 2016-2017 last (1)

Coronary angiography
Computerized tomography (CT) chest
Transthoracic echocardiography
Cardiac troponin level
Exercise stress test
20) A 38-year-old woman presents to the emergency room complaining of chest pain for the past several hours. She describes it as sharp, centrally located and non-radiation. The pain worsens somewhat with inspiration and movement. The patient denies having fevers, chills, dyspnea, swelling, or difficulty breathing at night. She says she first noticed the pain while exercising three weeks ago, but has experienced it at rest as well. She says that she has been exercising heavily in an attempt to lose weight. Her BMI is currently 34kg/m2. Her father had a myocardial infarction at age 60. Her medical history is significant for two normal vaginal deliveries. She smokes a half-pack of cigarettes daily. On physical examination, her blood pressure is 112/69 mmHg and her heat rate is 72/min. Cardiac exam reveals a regular S1 and S2 without extra sounds or murmurs. There is tenderness to palpation over the sternum. What is the most likely cause of her chest pain?
Gastroesophageal reflux disease
. Unstable angina
Pulmonary embolism
Costochondritis
. Pericarditis
21) A 12-year-old white male wants to participate in sports at school. He has been growing normally since birth. His immunizations are up-to-date and he is not suffering from any known medical conditions. Which of the following measures should be taken to screen him for underlying heart disease that could cause sudden cardiac death?
No screening is required
History and physical exam
12 lead ECG
. Echocardiography
Exercise stress testing
22) A 22-year-old female is referred to the dermatology clinic. Over the past few years, she has noticed small areas of depigmentation on her arms and legs. Some of these areas are well-circumscribed, as shown in the picture below. She is otherwise well. Her only medication is the oral contraceptive pill. She is currently sexually active with more than one partner. Which of the following diseases is most likely to be associated with her skin condition?

For Student DES 2016-2017 last (1)

. Type-2 diabetes mellitus
. Pernicious anemia
Hypoparathyroidism
HIV infection
Zollinger-EIIison syndrome
23) A 28-year-old Caucasian woman comes to the office for a routine skin exam. On exam, you encounter a dark-colored lesion. The patient states that she has had a spot there her whole life. She does state that it has recently "been a little itchy and hurts sometimes." She gives a history of sunburns during childhood, and says that she is very "sun-sensitive." A picture of the mole is shown below. Which of the following is the most likely diagnosis?

For Student DES 2016-2017 last (1)

. Keratoacanthoma
Melanocytic nevus
. Blue nevus
Lentigo simplex
. Melanoma
24) An 80-year-old woman comes to the office and appears very upset. She requests removal of a lesion on her neck because "it is greasy and unsightly." She is tired of people constantly staring at her neck. The lesion has been present "for quite a while," and has been gradually darkening. Aside from occasional itching, there are no other symptoms. A picture of the lesion is shown below. What is the most likely diagnosis?

For Student DES 2016-2017 last (1)

. Basal cell carcinoma
. Seborrheic keratosis
Melanoma .
. Acrochordon
Actinic keratosis
25) An 18-year-old girl comes to the emergency department for sudden-onset redness and swelling of her skin over exposed areas. She had just spent 1 hour at the beach when she began to experience a burning sensation, followed by redness and swelling of those areas. Her face has a few inflammatory nodules as well as open and closed comedones, and she was recently prescribed "some medication for the past month or so" for her facial lesions. Her pulse is 82/min, blood pressure is 120/80 mmHg, respirations are 14/min and temperature is 37.2°C (99°F). On examination, you notice erythema, edema and vesicles on her face, neck, dorsal hands and upper chest. She has no mucosal lesions. Which of the following best explains her condition?
Allergic contact dermatitis
. Erythromycin-induced phototoxicity
. Stevens-Johnson syndrome
. Benzoyl peroxide induced phototoxicity
. Doxycycline-induced phototoxicity
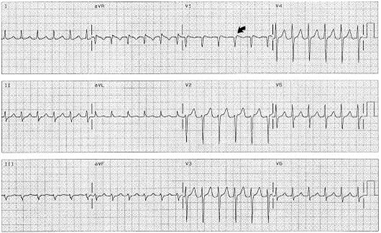
26) A 45-year-old man is brought to the office due a sudden onset of skin lesions and fever. He is unable to eat or drink due to the pain in his mouth and throat. His wife says that he was complaining of a headache, malaise, and joint pain prior to developing the skin lesions. Generally, he has been in good health, other than an episode of sinusitis, for which he was prescribed trimethoprim-sulfamethoxazole 5 days ago. His pulse is 92/min, blood pressure is 110/80 mmHg, respirations are 14/min, and temperature is 36.8°C (98.4°F). On examination, both conjunctivae are inflamed. There is erythema, blistering and ulceration over the oral mucosa. There is an erythematous rash over the trunk and cutaneous lesions over the hands, arms and feet. Some of the lesions are shown in the picture below. What is the most likely diagnosis?

For Student DES 2016-2017 last (1)

. Stevens-Johnson syndrome
Toxic shock syndrome
. Erythema multiforme minor
. Impetigo
Staphylococcal scalded skin syndrome
27) A 55-year-old man comes to the office due to a sudden onset of blisters all over his body. He complains of pain in the involved areas. He first noticed the lesions in his mouth a few days ago. His pulse is 82/min, blood pressure is 140/90 mmHg, respirations are 14/min, and temperature is 36.8°C (98.4°F). On examination, there are crops of flaccid bullae over normal-appearing skin, and large erosions at sites where the bullae had ruptured. The oral mucosa shows erosions and ulcerations. Slight rubbing of the uninvolved skin causes easy separation of the epidermis. Immunofluorescence microscopy shows deposits of IgG inter cellularly in the epidermis. What is the most likely diagnosis?
. Bullous pemphigoid
. Erythema multiforme
. Bullous impetigo
. Dermatitis herpetiformis
Pemphigus vulgaris
28) A 45-year-old woman comes to the office for the evaluation of reddened areas over her face (flushed skin). These areas worsen every time she drinks something hot or goes out in hot, sunny weather. Her vital signs are stable. On examination, there is evident erythema over her nose, cheeks, forehead and chin with telangiectasias, pustules and papules. What is the most likely diagnosis?
Acne vulgaris
. Systemic lupus erythematosus
Seborrheic dermatitis
. Rosacea
Carcinoid syndrome
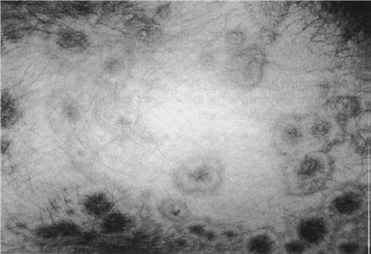
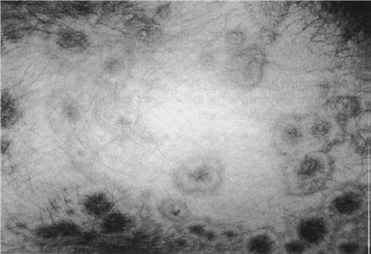
29) A 42-year-old woman presents with painful skin lesions. She is unable to eat or drink because the lesions have involved her mouth and throat. Her other complaints include malaise, headache, sore throat, cough, nausea and vomiting prior to the onset of the skin lesions. She was in perfect health in the past, other than an episode of urinary tract infection 3 days ago. She was prescribed trimethoprim-sulfamethoxazole combination for this infection. Her pulse is 92/min, respirations are 14/min, blood pressure is 140/90 mmHg, and temperature is 38.3°C (101°F). On examination, the skin is hot and tender with erythematous macules. The oral mucosa shows blistering and erosions. A picture of her back is shown below. What is the most likely diagnosis?

For Student DES 2016-2017 last (1)

Exfoliative dermatitis
Toxic epidermal necrolysis
Staphylococcal scalded skin syndrome
Stevens Johnson's syndrome
Erythema multiforme minor
30) A 28-year-old Caucasian woman presents to the primary care physician with complaints of painless blistering on the backs of her hands, accompanied by an increased fragility of the surrounding skin. She first noted the blisters one week ago, after spending some time gardening outdoors. She denies ever having similar symptoms, but suspects that her mother may occasionally have had a similar presentation that eventually resolved without treatment. Her past medical history is significant for chronic infection with Hepatitis C virus. Current medications include oral contraceptives, which were begun last month. Physical examination reveals mild hyperpigmentation of the face. Which of the following is the most likely diagnosis?
. Allergic contact dermatitis
Herpes zoster
Porphyria cutanea tarda
Lmpetigo
Dermatitis herpetiformis
31) A 36-year-old male presents to clinic complaining of a pruritic eruption on his forearms. He denies fever, chills and malaise. Physical examination reveals an erythematous rash with occasional vesicles affecting both forearms. No lymphadenopathy is appreciated. Vesicular fluid grows coagulase-negative staphylococci. His only relevant history is recent work in the woods behind his home chopping and transporting firewood. Which of the following is the most likely diagnosis?
Herpes simplex infection
S. Epidermidis cellulitis
.S. Aureus cellulitis
Contact dermatitis
Suppurative hidradenitis
32) A 64-year-old female presents with complaints of lesions over her breasts and thighs. She had been experiencing severe pain in those areas prior to developing redness and blisters. Her past medical history is significant for valvular heart disease with atrial fibrillation, ulcerative colitis diagnosed 20 years ago, and a resection of part of her colon. She is a known patient of yours, and four days ago, you started her on treatment for atrial fibrillation with antiarrhythmics and oral anticoagulants. Her pulse is 82/min, blood pressure is 140/90 mmHg, respirations are 14/min, and temperature is 36.8°C (98.4°F). On examination, you notice well-demarcated lesions with bullae and necrotic changes over her thighs and breasts. What is the most likely diagnosis?
Necrotizing fasciitis
Warfarin-induced necrosis
Venous gangrene
Cholesterol embolisation syndrome
. Pyoderrma gangrenosum
33) A mother brings her 6-month-old infant to your office for evaluation of scaly, erythematous lesions around his eyebrows and sides of his nose. She also notes a scaly scalp that improves with baby shampoo. Which of the following is the most likely diagnosis?
Atopic dermatitis
Tinea capitis
Seborrheic dermatitis
Psoriasis
Contact dermatitis
34) A 20-year-old female comes to the office and complains of rough, dry and scaly skin. Her skin was normal at birth, but gradually became dry. The dryness increases during the winter months, despite regular application of body-moisturizing lotion. An image of the patient's skin lesions is shown below. What is the most likely diagnosis?

For Student DES 2016-2017 last (1)

Atopic dermatitis
Impetigo
. Irritant contact dermatitis
. Psoriasis
. Ichthyosis vulgaris
35) A 35-year-old male presents to your office with red skin lesions on his back that were first noticed by his wife. His past medical history is not significant. Physical examination reveals the following findings (see the slide below). Which of the following is the most likely diagnosis in this patient

For Student DES 2016-2017 last (1)

. Strawberry (capillary) hemangioma
. Cavernous hemangioma
. Cherry hemangioma
. Cystic hygroma
Spider angioma
36) An 83-year-old man is brought to the office by his wife because he has had frequent falls for the past 3 months. The wife says that, "He's not his usual self these days. He needs help with everything, even everyday things." The patient has mask-like facies. He speaks very softly with a poorly modulated voice, and he has a fine tremor in both hands. The resting tremor in his hands disappears with voluntary movements. The other pertinent findings include a shuffling gait with short steps, stooped posture, tendency to fall and rigidity of both upper limbs. What skin condition is associated with this patient's neurologic diagnosis?
Tinea versicolor
Dermatophytosis
Seborrheic dermatitis
. Lichen simplex chronicus
Pityriasis rosea
37) A 43-year-old woman comes to the office because she has "finally decided to see a doctor." For the past four months, she has suffered from itching all over her body. She is tired of using over-the-counter products with no relief. Over the past two months, she has had loose stools, which "take forever to flush." Physical examination reveals jaundice, hepatomegaly and splenomegaly. The results of her blood work are as follows: Alkaline phosphatase 200 u/dL, Bilirubin 3.3 mg/dL, Anti-mitochondrial antibodies positive. Which of the following benign lesions of the eye is frequently associated with this patient's condition
Chalazion
Xanthelasma
Hordeolum
Stye
. Molluscum contagiosum
38) A 25-year-old male comes to the office due to severe itching and burning of the skin lesions on his knees, elbows and back of his neck. He gives a history of loose stools, flatulence, weight loss of more than 10 lbs, and fatigue for the past 6 months. His vital signs are stable. On examination, there are papules and vesicles over the extensor aspect of his elbows, knees, posterior neck and scalp. The laboratory studies reveal the presence of anti-endomysial antibodies. Which of the following is the most likely diagnosis?
. Erythema multiforme
. Kaposi's sarcoma
Bullous pemphigoid
Acantholytic dermatosis
. Dermatitis herpetiformis
39) A 36-year-old male comes to the office for the evaluation of a skin lesion. For the past two months, he noticed darkening and thickening of the skin over his neck and groin area. These areas occasionally feel itchy. His pulse is 82/min, blood pressure is 130/80 mmHg, respirations are 14/min, and temperature is 36.8°C (98.4°F). Physical examination reveals symmetrical, hyperpigmented, velvety plaques on the axilla, groin and posterior neck. This patient's condition should alert the physician to check for which of the following?
. Gastrointestinal malignancy
Pellagra
Diabetes mellitus
Hemochromatosis
Addison's disease
40) A 70-year-old Caucasian male presents to your office for evaluation of skin lesions on his forehead. On physical exam you find that these papules have a sandpaper texture by palpation. The lesions are illustrated in the slide below. Which of the following is the most likely diagnosis in this patient?

For Student DES 2016-2017 last (1)

. Psoriasis
Actinic keratosis
Seborrheic keratosis
Pityriasis rose a
Atopic dermatitis
41) A 17-year-old man presents with a non-pruritic rash in his periumbilical area. The rash consists of firm, dome-shaped, flesh-colored papules with central umbilication. This patient's rash is most commonly associated with which of the following conditions?
. Selective lgA deficiency
Complement deficiency
Cellular immunodeficiency
Circulating autoantibodies
. Impaired phagocytosis
42) An 8-year-old boy is brought to the office due to itchy rashes with blisters over his face, trunk and legs for the past 2 days. His vital signs are normal, except for a temperature of 37.7°C (100°F). On examination, you notice macules, pustules, vesicles, and honey-colored crusts around his mouth, nose, legs, buttocks and trunk area. What is the most likely diagnosis?
. Contact dermatitis
Herpes simplex infection
. Impetigo
Varicella zoster infection
. Erythema multiforme
43) An 18-year-old white female is brought to the emergency department due to severe vomiting, fever and rashes. She was fine until today, when she developed a fever, flu-like symptoms and dizziness. She has a history of asthma and allergic rhinitis. She denies taking drugs or alcohol, or being exposed to other sick individuals. She had her period yesterday, but did not place a tampon until today, 6 hours prior to becoming ill. Her last menstrual period was 6 weeks ago. She appears alert but listless. Her temperature is 38.8°C, pulse is 120/min, respirations are 23/min, and blood pressures are 100/66 mmHg, supine and 66/30 mmHg, standing. On examination, there are erythematous flat and raised rashes on her trunk and extremities. What is the most likely diagnosis?
Toxic shock syndrome
Meningococcemia
. Scarlet fever
Toxic epidermal necrolysis
. Stevens-Johnson syndrome
44) An 18-month-old Caucasian boy is brought to the emergency department due to a 3-day history of fever and facial rash. His past medical history is significant for atopic dermatitis, which was diagnosed 1 week ago and treated with topical steroids. Examination reveals numerous umbilicated vesicles over erythematous skin of both cheeks. Submandibular adenopathy is present. What is the most probable diagnosis?
Varicella
. Contact dermatitis
Impetigo contagiosa
. Atopic dermatitis exacerbation
. Eczema herpeticum
45) A 45-year-old male comes to you with complaints of throbbing pain over the pulp of his right index finger for the last two days. He has been feeling warm for the last three days. He denies ever having any sexually transmitted disease or cold sores in the past. On examination, he has a swollen, soft, and tender distal pulp space of the right index finger with some non-purulent vesicles. A picture of his hand is shown below. Tzanck smear of the vesicles show multinucleated giant cells. Which of the following is most likely the occupation of this patient?

For Student DES 2016-2017 last (1)

. A dentist
. A tailor
. Commercial sex worker
A Pilot
A gardener
46) A 28-year-old Caucasian male presents to the office with a rash on his trunk. He complains of constant itching over the area. He has no other medical problems. He denies any family history of diabetes. He currently has two sexual partners, and he does not use condoms. His pulse is 84/min, blood pressure is 120/80 mmHg, respirations are 14/min, and temperature is 37°C (98.4°F). On his trunk, there are 4 circular patches with central clearing and scaly borders, measuring approximately 3-8cms in diameter. What is the most likely diagnosis?
Tinea corporis infection
Pityriasis rosea
Psoriasis
. Secondary syphilis
Erythema multiforme
47) A 30-year-old, Caucasian male comes to the office for the evaluation of some pale patches in a mottled distribution over his trunk area. He just returned from a 2-week summer vacation in the Bahamas, where he first noticed these lesions. His skin is generally well-tanned. Located over his central upper trunk area are multiple, velvety pink, pale macules, measuring approximately 4-5 mm in diameter. These lesions scale on scraping. What is the most likely diagnosis?
. Vitiligo
. Tinea versicolor
. Seborrheic dermatitis
Tinea corporis
. Pityriasis rose a
48) A 48-year-old Caucasian female presents to your office due to a small swelling on her left lower eyelid. She has worked outdoors her whole life. This swelling has been present for the past 6 months. Recently, she noticed a loss of eyelashes on her lower eyelid. On examination, there is a small nodular lesion on the lower eyelid margin. It is firm, painless, pearly and indurated. Loss of lashes on the left lower eyelid is confirmed. Which of the following is the most likely diagnosis?
Squamous cell carcinoma
Basal cell carcinoma
Keratoacanthoma
. Seborrheic keratosis
. Squamous papilloma
49) A 5-month-old infant is brought to the office by his mother because of a rash on his face, hands and chest. The baby is constantly scratching these areas, and his mother is having a hard time keeping his hands away from the rash. She has tried a variety of over-the-counter products and many home remedies, as advised by her mother, but has noted no improvement. On physical examination, there are erythematous lesions on his cheeks with erosion, scaling, excoriated papules and plaques. Similar lesions are also found on his trunk, scalp and forehead. The lesions are symmetrical, and the diaper area appears spared. What is the most likely diagnosis?
Contact dermatitis
Atopic dermatitis
Scabies
. Seborrheic dermatitis
Exfoliative dermatitis
50) A 48-year-old white male comes to the emergency department with complaints of severe pain and swelling in his left leg. He sustained an injury to his left leg while playing tennis five days ago. The pain worsened over the past 2-3 days, and is now unbearable. He also complains of flu-like symptoms. His temperature is 39C° (102°F), pulse is 104/min, blood pressure is 110/80 mmHg, and respirations are 18/min. Physical examination reveals an edematous limb with purplish discoloration of the injured area, along with bullae and a serosanguineous discharge. The leg is extremely tender to touch. A scalpel incision of the skin reveals yellowish green necrotic tissues. What is the most likely diagnosis?
Thrombophlebitis
Necrotizing fasciitis
Cellulitis
. Toxic shock syndrome
Erythema induratum
51) A 20-year-old woman presents with complaints of a rash for the past 2 days. She was in good health until 5-6 days ago, when she developed fever, malaise and headache. The rash first appeared on her face, and then rapidly spread to her trunk and extremities. Her pulse is 86/min, blood pressure is 110/70 mmHg, respirations are 14/min, and temperature is 37.2°C (99°F). On examination, there is a pink maculopapular rash involving her face, trunk and extremities. Tender lymph nodes are palpable in the posterior auricular and posterior cervical areas. Her soft palate reveals patchy erythema. What is the most likely diagnosis?
Secondary syphilis
Rocky mountain spotted fever
. Rubella
Erythema multiforme
Kawasaki disease
52) A 4-year-old girl is brought to the office by her parents due to a red rash and blisters. Yesterday, she had a fever and was irritable. Today, she developed the rash with blisters. Her pulse is 90/min, blood pressure is 90/60 mmHg, respirations are 14/min, and temperature is 39°C (102°F). On examination, there are superficial flaccid bullae and an erythematous rash diffusely distributed over her body. Nikolsky's sign is positive. Her face is edematous, and there is crusting around the mouth area. Her skin is warm and tender with exfoliation. What is the most likely diagnosis?
. Toxic epidermal necrolysis
. Erysipelas
Staphylococcal scalded skin syndrome
. lmpetigo
. Scarlet fever
53) A 23-year-old college student comes to the office due to itching all over her body for the past 10 days. She hardly gets to sleep at night because of it. Her roommate has similar complaints. Her vital signs are stable. Physical examination reveals vesicles and pustules arranged in short, gray wavy channels on the finger webs, heels of palms, and in wrist creases. There are papules over the nipples and areola of her breasts. What is the most likely diagnosis?
Insect bites
Scabies
Urticaria
. Bed bugs
Body lice
54) A 7-year-old girl is brought to the office by her mother due to a rash all over her body. She was apparently in good health until 4 days ago, when she developed fever, cough and eye pain. This morning, she developed a rash on her face, which later spread all over her entire body. Her pulse is 86/min, respirations are 14/min, blood pressure is 110/70 mmHg, and temperature is 37.2°C (99°F). On examination, there is an erythematous maculopapular rash covering her entire body. There are small red spots with bluish specks on her buccal mucosa. What is the most likely diagnosis?
. Roseola infantum
. Parvovirus infection
. Rubella
Paramyxovirus infection
Varicella zoster infection
55) A 17-year-old female presents with a pruritic rash localized to the wrist. Papules and vesicles are noted in a band like pattern, with slight oozing from some lesions. Which of the following is the most likely cause of the rash?
. Herpes simplex
Seborrheic dermatitis
. Shingles
. Contact dermatitis
Atopic dermatitis
56) A 50-year-old woman develops pink macules and papules on her hands and forearms in association with a sore throat. The lesions are target like, with the centers a dusky violet. What causes of this disorder are most likely in this patient?
For Student DES 2016-2017 last (1)
. Tampons and superficial skin infections
Rickettsial and fungal infections
. Drugs and herpesvirus infections
. Harsh soaps and drying agents
Anxiety and emotional stress
57) A 15-year-old girl complains of low-grade fever, malaise, conjunctivitis, runny nose, and cough. After this prodromal phase, a rash of discrete pink macules begins on her face and extends to her hands and feet. She is noted to have small red spots on her palate. What is the most likely cause of her rash?
. Toxic shock syndrome
Rubeola (measles)
Gonococcal bacteremia
. Rubella (German measles
Reiter syndrome
58) A 17-year-old girl noted a 2-cm annular pink, scaly lesion on her back. Over the next 2 weeks she develops several smaller oval pink lesions with a fine collarette of scale. They seem to run in the body folds and mainly involve the trunk, although a few occur on the upper arms and thighs. There is no adenopathy and no oral lesions. Which of the following is the most likely diagnosis?
. Tinea versicolor
Pityriasis rosea
. Psoriasis
Secondary syphilis
. Lichen planus
59) A 45-year-old man with Parkinson disease has macular areas of erythema and scaling behind the ears and on the scalp, eyebrows, glabella, nasolabial folds, and central chest. Which of the following is the most likely diagnosis?
Tinea versicolor
. Seborrheic dermatitis
. Psoriasis
Dermatophyte infection
Atopic dermatitis
60) A 33-year-old fair-skinned woman has telangiectasias of the cheeks and nose along with red papules and occasional pustules. She also appears to have conjunctivitis with dilated scleral vessels. She reports frequent flushing and blushing. Drinking red wine produces a severe flushing of the face. There is a family history of this condition. Which of the following is the most likely diagnosis?
Carcinoid syndrome
. Porphyria cutanea tarda
. Lupus vulgaris
Seborrheic dermatitis
Rosacea
61) A 50-year-old male presents for the evaluation of polyuria and polydipsia of two months duration. He also complains of weakness and fatigue. He had one episode of paralysis that resolved on its own. He has a 20 pack-year history of smoking. He does not drink alcohol. His past medical and family histories are not significant His pulse is 78/min, blood pressure is 150/96 mmHg and temperature is 37°C (98.6°F). The rest of his examination, including the neurological examination, is unremarkable. Laboratory studies show: Plasma sodium 145 mEq/L, Potassium 24 mEq/L, Serum creatinine 0.8 mg/dl, Plasma renin activity low, Plasma aldosterone concentration high. Which of the following is the most likely diagnosis?
. Primary hyperaldosteronism
Renovascular hypertension
. Hypokalemic periodic paralysis
Congestive heart failure
. Renin-secreting tumor
62) A 24-year-old Caucasian female comes to the outpatient clinic and complains of heat intolerance and increased appetite. Her past medical history is insignificant. She denies use of over-the-counter medications. Her pulse is 110/min and regular, temperature is 37.2°C (99°F), and respirations are 14/min. Swelling is noted in the front of her neck, which moves with deglutition. Lab studies show: Total T4 Increased, Free T4 Increased, TSH Decreased. Radioactive iodine uptake is decreased. The thyroid scan shows very low uptake of radioiodine. What is the most likely diagnosis?
. Multinodular goiter
. Graves’ disease
Toxic adenoma
. Struma ovarii
Thyroiditis
63) A 17-year-old white female comes to the office for the evaluation of fatigue which has been present for the past 4 months. Her past medical history is insignificant. She denies the use of any drugs. Her pulse is 74/min, blood pressure is 110/70 mmHg, and temperature is 36.7°C (98.0°F). Physical examination shows scars on the dorsum of her hands and dental erosions. Laboratory studies show: Plasma sodium 139 mEq/L, Serum potassium 2.3 mEq/L, Bicarbonate 40 mEq/L. Urine chloride concentration is 15 mEq/L (Normal = 80-250 mEq/L). Based on these findings, what is the most likely diagnosis?
. Chronic diarrhea
Primary hyperaldosteronism
Diuretic abuse
Bartter's syndrome
Surreptitious vomiting
64) A 56-year-old female is admitted with a diagnosis of chronic renal failure from systemic lupus erythematosus and non-steroidal anti-inflammatory drug use. She has a history of recurrent kidney stones. Laboratory studies show the following: Serum calcium 10.6 mg/dL, Serum albumin 3.9 g/L, PTH 140 pg/mL, Serum phosphorus 3.0 mg/dL. Her baseline serum creatinine level ranges from 1.6 to 1.8 mg/dL. Her bone mineral density is measured by DXA scan, revealing a T score of-2.5 at the lumbar spine, which is consistent with osteoporosis. What is the most likely cause of this patient's hypercalcemia?
. Hypercalcemia of malignancy
Chronic renal failure
Milk-alkali syndrome
Primary hyperparathyroidism
. Sarcoidosis
65) A 31-year-old Hispanic female presents with palpitations and weight loss. Her past medical history is insignificant. Her family history is unremarkable. She recently moved from South America. She does not smoke cigarettes or drink alcohol. She is married and has three children. Her last delivery was four years ago. Her blood pressure is 140/90 mmHg, pulse is 102/min, temperature is 36.7°C (98°F) and respirations are 20/min. Her eye examination is unremarkable. Thyroid examination reveals a 2 x 2 cm left-sided thyroid nodule. Her T3 and T 4 are elevated, and TSH is undetectable. Radioactive iodine scan shows uptake only in the left thyroid nodule. Uptake in the rest of the thyroid is markedly reduced. Which of the following is the most likely diagnosis?
Hashimoto's thyroiditis
Toxic adenoma
. Graves' disease
. Toxic multinodular goiter
Painless thyroiditis
66) A 36-year-old male comes to the office for the evaluation of fatigue and weakness for the last several weeks. He denies any change in appetite, change in weight, heat or cold intolerance, nausea, vomiting and constipation. He cannot recall any recent stressful events. His past medical and family histories are unremarkable. He does not have any medications. His pulse is 76/min, blood pressure is 120/70 mmHg, respirations are 14/min, and temperature is 36.7°C (98°F). He is well-oriented to time, place and person. His neurological examination is nonfocal; the deep tendon reflexes are normal. Lab tests show: Hematocrit 43%, WBC count 6,000/microl, Platelet count 200,000/microl, Serum calcium 11 mg/dL, Serum albumin 4.5 g/dL, 24-hour urinary calcium 200 mg. Which of the following is the most likely cause of his symptoms?
Primary hyperparathyroidism
Familial hypocalciuric hypercalcemia
Malignancy
Milk alkali syndrome
Increased calcium intake
67) A 46-year-old female complains of a "sandy" sensation in her eyes. Review of systems is notable for a 6 pound weight loss over the last month. A picture of her eyes is shown on the slide below. Which of the following most likely underlies this finding?
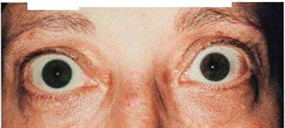
For Student DES 2016-2017 last (1)
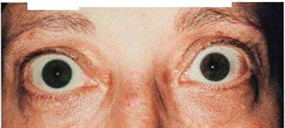
High circulating thyroxine level
Increased intraocular pressure
Periorbital lymphocytic infiltration
Increased intracranial pressure
Bilateral facial nerve compression
1) A 63-year-old white female presents with a thyroid nodule. She denies any weight loss, change in appetite, diarrhea, heat or cold intolerance, menstrual irregularities, hoarseness and dyspnea. Her past medical history is unremarkable. There is no family history of thyroid cancer. She does not take any medications. Physical examination shows a 4-5 cm, fixed, hard, and non-tender thyroid nodule. There is cervical lymphadenopathy. Her serum TSH level is normal. Fine needle aspiration (FNA) of the thyroid shows malignant cells. Which of the following is the most likely expected pathology on FNA?
Lymphoma of the thyroid
Papillary carcinoma of the thyroid
Anaplastic carcinoma of the thyroid
. Follicular carcinoma of the thyroid
. Medullary carcinoma of the thyroid
2) A 36-year-old female presents with headaches and visual problems. She also complains of palpitations, heat intolerance and weight loss. Her past medical history is unremarkable. She is currently on no medications. Her blood pressure is 130/60 mmHg, heart rate is 100/min and regular, and weight is 152 lb (weight one year ago was 170 lb). Physical examination reveals a symmetrically enlarged thyroid gland without any tenderness. Auscultation of the chest reveals tachycardia. She has bitemporal hemianopsia on confrontation. The rest of the physical examination is unremarkable. Her lab investigations show: Serum T3 222 ng/mL, Serum T4 13.9 mcg/dL, Serum TSH 7.9 IU/mL, Alpha subunit level elevated. Which of the following is the most likely diagnosis?
TSH-secreting pituitary adenoma
Toxic multinodular goiter
. Generalized resistance to thyroid hormone
Primary hypothyroidism
. Graves' disease
3) A 35-year-old male presents with complaints of weakness and fatigue of one year's duration. He is anorexic and has lost interest in all his activities. He also complains of cold intolerance and constipation. His blood pressure is 98/72 mmHg, temperature is 37.1°C (99°F), respirations are 14/min, and pulse is 50/min. His skin is dry and rough, nails are brittle, and hair is thin. There is no hyperpigmentation of the skin. Delayed deep tendon reflexes are noted on neurological examination. Lab studies show: Hemoglobin 10.2 g/dL, WBC count 5,000/micro-L, Neutrophils 45%, Monocytes 5%, Eosinophils 10%, Basophils 1%, Lymphocytes 40%, Serum sodium 135 mEq/L, Serum potassium 4.0 mEq/L. Which of the following is most consistent with this patient's findings?
Autoimmune destruction of adrenal glands
. Adrenal CMV infection
Adrenal tuberculosis
. . Pituitary tumor
. Adrenoleukodystrophy
4) A 60-year-old male is admitted to the hospital because of right lower lobe pneumonia. His medical history is significant for hypertension, diabetes mellitus, severe degenerative disease of the spine, and longstanding lower back pain. He is a chronic smoker with a 40-pack year smoking history. During his hospitalization, the laboratory report shows decreased serum calcium levels and increased phosphate levels. Further evaluation reveals increased serum intact parathyroid hormone levels. Which of the following medical conditions is most likely responsible for this patient's abnormal lab findings?
. Lung cancer
. Thyroidectomy
Primary hyperparathyroidism
. Plasma cells in marrow
Renal failure
5) A 43-year-old female presents to the physician's office with muscle cramps, polydipsia and polyuria. She has no other medical problems, and does not take any medications. She does not use tobacco, alcohol or drugs. Her father died from alcoholic liver disease at age 50. Her pulse is 75/min, respirations are 13/min, blood pressure is 160/100 mmHg, and temperature is 37°C (98.6°F). Laboratory studies show: Blood glucose 115 mg/dL, Serum sodium 142 mEq/L, Serum potassium 2.7 mEq/L. Plasma renin activity is low. What is the most likely diagnosis?
. Atherosclerosis of renal artery
Adrenal adenoma
. Fibromuscular dysplasia
Cirrhosis of liver
Congestive heart failure
6) A 30-year-old Hispanic male presents to the office with complaints of palpitations, tremor, nervousness and headache. His past history is insignificant. His mother has type 2 diabetes, which is well-controlled with medications. His temperature is 37.0°C (98.6°F), pulse is 100/min, blood pressure is 150/80 mmHg, and respirations are 16/min. He appears anxious, sweaty and shaky. His neurological examination is non-focal, and examination of other systems is unremarkable. His fingerstick blood glucose level is 38 mg/dL. Intravenous administration of a bolus of 50% dextrose leads to the improvement of his symptoms. He is then subjected to supervise prolonged fasting. After an overnight fast, laboratory studies reveal: Blood glucose 40 mg/dl, Serum insulin 15 microU/L (normal value is < 6 microU/L with hypoglycemia), Serum pro-insulin 9 microU/L (normal value is < 20% of total immunoreactive insulin), C-peptide level 0.8 nmol/L (normal value is less than 0.2 nmol/L), Sulfonylurea Negative, IGF-II Negative. Based on the above information, what is the most likely cause of this patient's hypoglycemia?
Beta cell tumor
Exogenous insulin
Non-beta cell tumor
. Glucagonoma
Sulfonylurea agents
7) A 35-year-old male presents to the family physician for bilateral gynecomastia. He observed a progressive increase in his breast size starting 6 months ago. He is sexually active and denies any drug use. Physical examination reveals bilateral gynecomastia and tenderness. The genito-urinary examination shows a 1 cm nodule in the right testis. Otherwise, the examination is within normal limits. The laboratory report shows: LH 3 U/L, FSH 2 U/L, testosterone 270 ng/dL (Normal 3-10 ng/dL), estradiol 115 pg/mL (Normal 20-60 pg/mL), beta HCG undetectable, AFP undetectable. Which is the most likely diagnosis?
Leydig cell tumor
Seminoma
Choriocarcinoma
. Endodermal sinus tumor
. Teratoma
8) A 39-year-old woman comes to the physician because of a "pins and needles" sensation around her mouth for the last 2-3 weeks. She gets similar sensations in her feet sometimes, along with muscle cramps, especially at the end of the day. She has no similar episodes in the past and has always been healthy. She works as a waitress and has "clean habits." Her family history is not significant. She is currently not taking any medications, and is allergic to penicillin. Her vital signs are normal. Examination is unremarkable. The patient's labs reveal: CBC: Hb 12.4 g/dl, WBC 6,000/cmm. Serum: Serum Na 140 mEq/L, Serum K 4.0 mEq/L, Chloride 100 mEq/L, Bicarbonate 24 mEq/L, BUN 10 mg/dl, Serum creatinine 0.8 mg/dl, Glucose 100 mg/dl, Calcium 6.5 mg/dl, Phosphorus, inorganic 5.8 mg/dl. Protein: Total 7.0 g/dl, Albumin 3.8 g/dl, Globulins 3.0 g/dl. Which of the following is the most likely cause of her condition?
Osteoporosis
. Primary hyperparathyroidism
Osteomalacia
. Primary hypoparathyroidism
Familial hypocalciuria
9) A 56-year-old male presents in the emergency department with severe nausea, vomiting, polyuria, polydipsia, and constipation. His past medical history is significant for hypertension and type 2 diabetes mellitus. His home medications include metformin, atenolol, and hydrochlorothiazide. He has a 26-pack-year history of smoking. He drinks alcohol occasionally. He denies the use of recreational drugs. His father also has diabetes mellitus type 2. His blood pressure is 110/70 mmHg, pulse is 102/min, temperature is 36.7°C (98°F) and respirations are 16/min. His mucus membranes are dry. His lung examination reveals decreased breath sounds over the right base. The rest of the physical examination is unremarkable. The patient is subsequently admitted. Laboratory studies (obtained in the emergency department) are as follows: Serum calcium 14.8 mg/dl, Albumin 4.0 g/dl, PTH 9 pg/ml (normal 10-60 pg/ml), Serum creatinine 1.9 mg/dl, BUN 54 mg/dl, Blood glucose 180 mg/dl, 25-hydroxyvitamin D 30 ng/ml (normal 20 to 60 ng/ml), 1,25-dihydroxyvitamin D 30 pg/ml (normal 15 to 65 pg/ml). What is the most likely cause of this patient's hypercalcemia?
. Hypercalcemia of malignancy
Dehydration
Primary hyperparathyroidism
Sarcoidosis
. Hydrochlorothiazide-induced
10) A 63-year-old otherwise healthy male presents with a thyroid nodule. He denies any symptoms of anxiety, heat or cold intolerance, and recent changes in appetite or weight. He has hypertension, which is being treated with a beta-blocker. He does not have any other medical problems. He denies any family history of thyroid disease. His pulse is 79/min and blood pressure is 130/76 mmHg. Neck examination shows a hard, fixed, non-tender, 4 cm thyroid nodule in the right thyroid lobe. His serum TSH level is normal. Fine needle aspiration biopsy (FNAB) shows follicular cells. Follicular carcinoma is suspected. Which of the following is necessary to make a diagnosis of follicular thyroid cancer?
Lymph node involvement
Presence of Hurthle cells on biopsy
Invasion of the tumor capsule and blood vessels
. Presence of psammoma bodies
Secretion of calcitonin
11) A 38-year-old Caucasian female presents to the office complaining of lethargy, weight gain and fatigue. She denies headaches, pruritus or urine discoloration. She just gave birth 2 months ago via vaginal delivery; her baby is in good health and receives formula nutrition. Her delivery was complicated by vaginal bleeding that required blood transfusion, and postpartum endometritis that rapidly responded to antibiotics. She has not had any menstrual periods following delivery. Physical examination shows sparse pubic hair, dry skin and delayed tendon reflexes. Urinalysis shows no glucose or ketones. Which of the following is most likely to be responsible for this patient's condition?
Infiltrative disorder
. Ischemic necrosis
Autoimmune tissue destruction
. Drug effect
Neoplasia
12) A 56-year-old woman presents to the clinic with a 7-month history of headache and visual disturbance. Her past medical history is unremarkable. She is currently not taking any medications. She admits to smoking a pack of cigarettes daily for the last 15-years, and does not drink. On visual field examination, there is a small field defect noted in both eyes. MRI scan shows a pituitary tumor. Which of the following is the most common type of pituitary tumor?
Thyrotroph adenoma
Thyrotroph adenoma
Corticotroph adenoma
Somatotroph adenoma
Lactotroph adenoma
13) A 65-year-old Hispanic male comes to the office for a routine medical check-up. He has a history of diabetes for the past twenty years, and hypertension for the past ten years. His daily medications include insulin and ramipril. He was diagnosed with nonproliferative diabetic retinopathy at his last ophthalmologic visit. Reports from his previous laboratory studies show microalbuminuria. A detailed neurological examination is performed to check for any neuropathy. Which of the following is the most common type of neuropathy found in diabetics?
Proximal motor neuropathy
. Symmetrical distal polyneuropathy
Autonomic neuropathy
. Mononeuropathy
Mononeuropathy multiplex
14) A 65-year-old man presents with a 1-day history of hematuria and sharp flank pain (rated 10 of 10) radiating toward the groin on the right side. Past medical history is significant for three prior episodes of nephrolithiasis over the past 5 years, all of which presented with a similar clinical picture. He is not taking any medication. There is no family history of renal calculi, renal disease, or endocrine disorders. His temperature is 36.9°C (98.5°F), heart rate is 125/min, and blood pressure is 132/86 mmHg. He is in obvious distress and cannot sit still on the bed. Physical examination is significant for a soft, nontender abdomen and extreme costovertebral angle tenderness on the right. Laboratory values show: Na+: 142 mEq/L, K+: 4.8 mEq/L , Cl−: 104 mEq/L, HCO −: 24 mEq/L , Ca2+: 11.0 mg/dL , PO4: 1.4 mg/dL , Mg2+: 2.0 mg/dL , Blood urea nitrogen: 12 mg/dL, Creatinine: 1.0 mg/dL, Glucose: 118 mg/dL, Intact parathyroid hormone: 300 pg/mL. Which of the following is the most likely diagnosis?
Malignancy
Sarcoidosi
Milk-alkali syndrome
Secondary hyperparathyroidism
Primary hyperparathyroidism
15) A 90-year-old male complains of hip and back pain. He has also developed headaches, hearing loss, and tinnitus. On physical examination the skull appears enlarged, with prominent superficial veins. There is marked kyphosis, and the bones of the leg appear deformed. Serum alkaline phosphatase is elevated. Calcium and phosphorus levels are normal. Skull x-ray shows sharply demarcated lucencies in the frontal, parietal, and occipital bones. X-rays of the hip show thickening of the pelvic brim. Which of the following is the most likely diagnosis?
Multiple myeloma
Vitamin D intoxication
Paget disease
Osteitis fibrosa cystica
Metastatic bone disease
16) A 35-year-old white male presents with fatigue, decreased appetite, weight gain, constipation and cold intolerance. He cannot recall any stressful event. He does not take any medications. He is a non-smoker and non-alcoholic. His pulse is 47/min and blood pressure is 145/91 mmHg. Physical examination reveals cool, pale skin, coarse hair, and brittle nails. There is delayed relaxation of deep tendon reflexes. The thyroid gland is normal on palpation. Laboratory studies reveal increased serum free T3 and T4 levels, and normal serum TSH level. Which of the following is the most likely diagnosis?
. Primary hypothyroidism
Generalized resistance to thyroid hormones
Secondary hypothyroidism
. Graves' disease
. Subclinical hypothyroidism
{"name":"DES part2 episode4", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"49) A 23-year-old woman who is an elementary school teacher is brought to the ED after syncopizing in her classroom while teaching. Prior to passing out, she describes feeling light-headed and dizzy and next remembers being in the ambulance. There was no evidence of seizure activity. She has no medical problems and does not take any medications. Her father died of a “heart problem” at 32 years of age. She does not smoke or use drugs. BP is 120\/70 mmHg, pulse rate is 71 beats per minute, RR is 14 breaths per minute, and oxygen saturation is 100% on room air. Her physical examination and laboratory results are all normal. A rhythm strip is seen below. Which of the following is the most likely diagnosis? For Student DES 2016-2017 last (1), 50) A 22-year-old man presents to the ED with a history consistent with an acute MI. His ECG reveals ST elevations and his cardiac biomarkers are positive. He has been smoking half a pack of cigarettes per day for the last 3 months. He drinks alcohol when hanging out with his friends. His grandfather died of a heart attack at 80 years of age. The patient does not have hypertension or diabetes mellitus and takes no prescription medications. A recent cholesterol check revealed normal levels of total cholesterol, low-density lipoprotein (LDL), and high-density lipoprotein (HDL). Which of the following is the most likely explanation for his presentation?, 51) A 29-year-old woman presents to the emergency department with a 3-week history of being awakened by a dull, prolonged chest pain that occurs 3–4 times a week. She is a smoker but has never suffered a myocardial infarction (MI) or had chest pain before and has no family history of early MI. Results of a 12-lead ECG are normal. Her first set of cardiac enzyme measurements (creatine kinase, creatine kinase-MB fraction, troponin I) are negative. If coronary angiography were taken at the time of her chest pain, which of the following findings is most like?","img":"https://www.quiz-maker.com/3012/images/ogquiz.png"}
More Quizzes
Distinction between summary and Indictable offences
10517
Deutsch traduction
50250
What elemental power would you have?
8420
Erfahrungslevel
210
Which Royal Are You? King, Queen, Prince or Princess
201030650
Quiz: How Well Do You Know Nationalities in Spanish?
201051726
Free Corporate Brand Awareness
201028346
Which Choral Voice Type Are You? Find Your Perfect Part!
201033910
Free Circumcision Knowledge Assessment
201021703
Advanced Painting
15829947
National Mulligan Day Trivia - Test Your Golf Knowledge
201027762
Semicolon Practice: Master Commas, Colons & More
201096238