USLME medecine interne
A 72-year-old Hispanic man comes to the clinic with complains of mild headache, and lethargy for the past several days. He complains of cough for the past 12 years, the cough has been bothering him more lately. The cough is mucoid, he has noticed blood in it once in a while. He has smoked 1 pack/day for 29 years. His vitals are, Temperature 37.0°C (98.6°F); BP 120/84 mm Hg; PR 78/min; RR 24/min. On examination of lungs, adventitious sounds are heard over all the lobes and scant crackles at the base. Laboratory studies show: WBC 7,600/mm3, Hemoglobin 13.6, Hematocrit 40%, Platelets 214,000mm3, Sodium 130 mEq/L, Potassium 3.6 mEq/L, Bicarbonate 18 mEq/L, Blood urea nitrogen 16 mg/dl, Creatinine 0.6 mg/dl, Glucose 95 mg/dl, Serum osmolality 260 mOsm/kg (normal 280), Urine osmolality 310 mOsm/kg. A chest x-ray shows a 2-centimeter left upper lobe mass and mediastinal adenopathy. What will be the next best step in management of this patient?
Prescribe demeclocycline
Restrict the patient water intake
Start an infusion of hypertonic saline
Start furosemide
A CT of head
You are called by the hospice nurse to evaluate a 74-year-old man who refuses to eat. He has terminal colon cancer, which was diagnosed 8 months ago and has metastasized to his liver. He has already gone through chemotherapy with 5-Fiourouracil + oxaliplatin. During the past 4 months, his condition has gotten extremely worse. He has lost 501bs (27.6kg), and currently appears totally wasted. As you approach him, he says, "I don't feel like eating anything, and I don't want any more procedures, but I'll drink any pill that can make me feel better." His abdomen is distended with positive fluid thrills. His liver has several palpable nodules. What is the best pharmacological agent of choice for this patient's anorexia?
Megestrol acetate
Dexamethasone
Dimenhydrinate
Ondansetron
Metoclopramide
A 67 -year-old man presents to your office with a one month history of progressive fatigue and exertional dyspnea. He has no significant past medical history. Physical examination reveals enlarged, non-tender axillary lymph nodes bilaterally. His abdomen is soft and non-tender and the liver span is 10 cm. Serial fecal occult blood tests are negative. Laboratory values are as follows: Hemoglobin 7.8 mg/dl, MCV 90 fl, MCHC 33 g/dl, Reticulocytes 7%, WBC count 22,000/mm3, Platelets 200,000/mm3. Which of the following is most likely to improve this patient's symptoms?
Folic acid
Iron
Prednisone
Pyridoxine
Erythropoietin
A 22-year-old woman comes to the office for the evaluation of a breast mass which she discovered while taking a shower 2 months ago. She experiences severe pain in this mass during her menses. She looks very anxious because her 45-year-old friend was diagnosed with breast cancer last year, and who "now has all sorts of medicines that have made her lose her hair." She has no other problems. She has never been pregnant. She is an occasional smoker, and drinks 3-4 beers a week. There is no family history of breast cancer. Her vital signs are stable. Physical examination reveals a 4 x 5 x 6 cm firm, moveable, rubbery mass in her left breast. Ultrasound shows a cystic mass. Needle aspiration yields clear fluid, after which the mass disappears. What is the best approach in the management of this patient?
Send the fluid for cytology
Perform a core biopsy
Observe for 4 weeks
Order a mammogram to look for other lesions
Breath CT scan
A 28-year-old male comes for complete physical examination for a new job he is starting next week. He is healthy and has no complaints. He smokes 1 pack/day cigarettes for the last 10 years. He drinks 4 oz of alcohol daily. His mother has hypertension and father has heart problems. Vitals signs are with in normal limits. Physical examination is within normal limits except for a painless, hard mass in left testicle. Ultrasound shows high likelihood of a testicular tumor. What is the next best step in management?
Observe and recheck the mass after one month
Platinum based chemotherapy
Trans-scrotal biopsy
Fine needle aspiration cytology
Radical orchiectomy
A 41-year-old woman comes to the office for the evaluation of a lump on her left breast. She feels, "generally well," and denies having any medical problems. She takes a multivitamin and Tums daily. She stopped smoking after getting married 21 years ago. She drinks wine only on weekends. Her only surgery was a bilateral tubal ligation last year, after giving birth to her fourth child. Physical examination of the left breast reveals a 4 cm lump at the 11 O'clock position and two axillary nodes on the left side. Mammography shows irregular micro-calcifications. The result of the FNA is suggestive for infiltrating ductal carcinoma. Which of the following is the single most important prognostic factor in this patient?
TNM staging
Estrogen and progesterone receptor status
Her-2/neu oncogene expression
Histological grade of the tumor
Irregular micro calcifications in mammogram
A 29-year-old woman comes to the office of a primary care physician complaining of pain in her right knee for the last 3 months. The pain is getting progressively worse and is not moving anywhere. She has tried ibuprofen but found little comfort. She is a housewife and unable to do household work because of this pain. She does not smoke nor drink and has hypertension well controlled by hydrocholorothiazide. Her vitals are stable and she is afebrile. On examination her right knee is a little swollen and tender with reduced range of motion. On x-ray, there is soap-bubble appearance in the epiphysis of distal femur. What is the next best step in the management of this patient?
Refer to an orthopedic surgeon
Perform biopsy in the office
Order bone scan
Start antibiotics
Do rheumatoid factor and anti-nuclear antibody
A 55-year-old man has undergone renal transplantation due to end-stage renal failure. His postoperative course was uncomplicated. He is currently taking prednisone and cyclosporine. He is afebrile and his pulse is 80/min, respirations are 14/min, and blood pressure is 130/65 mm Hg. Physical examination is unremarkable. Which of the following should be added to his current medication regimen to prevent opportunistic infections?
Trimethoprim-sulfamethoxazole
Oseltamivir
Itraconazole
Azithromycin
Penicillin
A 24-year-old man is found to be HIV positive. He is asymptomatic. Physical examination is unremarkable. Laboratory tests show: CD4 count 400/micro-L, HIV viral load 9,000 copies/mL, VDRL negative, Toxoplasma serology negative, PPD test 6mm induration. His chest x-ray is unremarkable. What is the most appropriate next step in the management of this patient?
Reassurance and repeat testing in 2 months
Isoniazid and pyridoxine for 9 months
Rifampin for 9 months
Rifampin, isoniazid, pyrazinamide, and ethambutol for 2 months, then isoniazid and rifampin for 4 months
Rifampin, isoniazid, and pyrazinamide for 6 months
A very worried 25-year-old woman comes to the office, presents a positive pregnancy test, and says, "I'm six weeks pregnant. Two months ago, I received the rubella vaccine and my doctor told me to avoid getting pregnant for the next three months. I'm very concerned about the health of my unborn baby. I'd like to know all the available options to prevent any harm to my baby." What is the most appropriate next step in the management of this patient?
Reassurance
Explain the risks and benefits of abortion
Advise abortion
Serological testing for rubella
Ultrasonography
A 30-year-old male has recently been diagnosed with HIV infection. He denies drug abuse. He is currently asymptomatic, and physical examination is unremarkable. He is in a stable heterosexual relationship. Laboratory studies show a CD4 count of 350/microL, HIV viral load of 15,000 copies/mL, negative VDRL, negative toxoplasma serology, tuberculin skin test of 7 mm induration, negative HBsAg, and positive anti-HBsAg antibodies. Hepatitis C antibodies are negative. Complete blood count, serum chemistries, and liver function tests are within normal limits. He has not received any vaccinations since being diagnosed with HIV. Which of the following vaccines is indicated in this patient?
BCG vaccine
Hepatitis A vaccine
Hepatitis B vaccine
Pneumococcal vaccine
Meningococcal vaccine
A 42-year-old man with advanced HIV infection has a two-week history of pain and difficulty with swallowing. He was given fluconazole for these symptoms one week ago, but his pain has worsened. His current medications include tenofovir, emtricitabine, efavirenz, and trimethoprim-sulfamethoxazole. His CD4 count is 90/microl and viral load is 300,000copies/ml. Endoscopy reveals large, irregular, linear ulcers in the esophagus. A biopsy of the abnormal mucosa reveals tissue destruction and the presence of intranuclear and intracytoplasmic inclusions. Which of the following is the most appropriate pharmacotherapy for this patient?
Prednisone
Acyclovir
Pentamidine
Ganciclovir
Itraconazole
A 26-year-old man presents to the physician's office with a two-day history of multiple symptoms, including rash on his trunk, headache, fatigue, malaise, myalgias, and high-grade fever. The rash is not associated with pain, itching, or burning. It has expanded over the last two days. He went on a camping trip in Vermont two weeks ago, and recalls a tick bite at that time. There is a single lesion on his trunk, which is erythematous with central clearing. The rest of the examination is unremarkable. What is the most appropriate next step in the management of this patient?
Perform ELISA for confirmation of Lyme disease
Perform western blot for confirmation of Lyme disease
Give him oral doxycycline
Give him oral amoxicillin
Give him intravenous ceftriaxone
A 35-year-old HIV-positive male comes to the physician's office because of pain on swallowing and substernal burning for the last 3 days. Examination of the oral cavity is unremarkable. Lungs are clear to auscultation and percussion. His current medications include zidovudine, didanosine, indinavir, trimethoprim-sulfamethoxazole, and azithromycin. His last CD4 count is 40cells/microl. What is the most appropriate next step in the management of this patient?
Esophagoscopy with biopsy, cytology and culture
Oral Fluconazole
Oral Famotidine
Oral Acyclovir
Oral Ganciclovir
A 25-year-old HIV-positive male comes to a physician with complaints of headache and left-sided weakness of recent onset. His temperature is 38°C (100.8°F), blood pressure is 115/70mm Hg, respirations are 14/min, and pulse is 73/min. Neurological examination reveals decreased power, hyperreflexia, and upgoing plantars in the left upper and lower limb. Neuroimaging by CT shows multiple ring-enhancing lesions. What is the most appropriate next step in management?
Trimethoprim-sulfamethoxazole
Sulfadiazine and pyrimethamine
Brain irradiation
Brain biopsy
Anti-tuberculous therapy
An 18-year-old young man comes to your clinic with complaints of fatigue, malaise, fever, and sore throat for the past few days. His temperature is 38.8°C (101°F), pulse is 90/min, respirations are 18/min, and blood pressure is 135/70 mm Hg. Physical examination reveals cervical lymphadenopathy, pharyngeal hyperemia, and splenomegaly. Complete blood count shows leukocytosis with predominant atypical lymphocytes. The heterophile antibody test is positive. When you ask if he has any questions, he replies with, "Well, I'm a rugby player in school, so I need to know when I can start playing again." What is the most appropriate advice for this patient?
He can start playing when he becomes afebrile
He can start playing when he is no longer fatigued
He can start playing when his labs normalize
He can start playing when his physical examination is normal
He can start playing whenever he wants
A 25-year-old man presents to the physician's office because of a clenched fist injury ("fight bite") incurred during a gang fight. The injury occurred two days ago and he has now started to develop pain, swelling, and redness around the wound. His immunizations are up to date. His wounds are cleaned in the clinic. Plain films of hand do not show evidence of foreign body or osteomyelitis. Which of the following is the most appropriate antibiotic for his current condition?
Amoxicillin-clavulanate
Clindamycin
Ampicillin
Erythromycin
Ciprofloxacin
A 30-year-old white, HIV-infected male from Ohio presents with low-grade fever, anorexia and weight loss of 3.6kg (Bib) for the past 3 weeks. His baseline PPD test was negative. His pulse is 87/min, blood pressure is 126/76 mm Hg, temperature is 38.3°C (101°F), and respirations are 18/min. Examination shows oropharyngeal ulcers and hepatosplenomegaly. Lab testing shows: Hematocrit 36%, Platelet count 50,000/microL, WBC count 3,100/microL. Blood culture establishes the diagnosis of histoplasmosis. What is the most appropriate next step in the management of this patient?
IV amphotericin B followed by lifelong treatment with itraconazole
IV amphotericin B till the cultures become negative
Itraconazole till the cultures become negative
IV amphotericin B plus itraconazole till the cultures become negative
Lifelong treatment with itraconazole
A 7-year-old boy is brought to the office by his mother due to anal pruritus for the past month. His symptoms are most severe at night. Physical examination is normal, except for mild perianal erythema. Stool examination is normal. "Scotch tape test" is positive. Which of the following is the most appropriate treatment for this child's condition?
Pyrantel pamoate
Albendazole
Metronidazole
Thiabendazole
Ivermectin
A 37-year-old man comes to his primary care physician for the evaluation of slightly pruritic skin lesions around his anus. He denies fever, malaise, and anorexia. He is sexually active with multiple male partners and occasionally uses condoms. He has never been tested for HIV or other sexually transmitted diseases. He has no drug allergies. Examination shows skin-colored, verrucous, papilliform lesions around his anus. Which of the following is the most appropriate treatment for this patient?
Podophyllin
Penicillin
Erythromycin
Doxycycline
Tetracycline
A 28-year-old, HIV-infected female from Michigan is admitted with Pneumocystis jirovecii pneumonia (PCP) secondary to noncompliance with prophylaxis. She was diagnosed with HIV infection three years ago. Her C04 count on admission is 30/microl, and viral load is 300,000copies/ml. Her pneumonia is adequately treated with IV antibiotics, and she subsequently receives zidovudine, lamivudine, nelfinavir, and trimethoprim-sulfamethoxazole. What is the most appropriate drug to be added to her current regimen?
Azithromycin
Rifabutin
Fluconazole
Itraconazole
Ganciclovir
A 65-year-old Connecticut resident calls your office after finding a 3 mm red-brown tick attached to his right leg. He just returned from a hiking trip and was about to a take a shower when he discovered the tick. Which of the following is the best advice to give this patient?
Crush the tick with your fingers
Remove the tick with tweezers
Ly petroleum jelly over the tick
Come to the office tomorrow for tick removal
Let the tick detach spontaneously

A 27-year-old man presents with fever, malaise, anorexia, and fatigue for the last three days. He denies cough, chest pain, arthralgias, and diarrhea. He has history of rheumatic heart disease and recently underwent a dental cleaning. His temperature is 38.5°C (101.3°F), pulse is 90/min, respirations are 18/min, and blood pressure is 135/76 mm Hg. Examination of his fingernail is shown below. Cardiovascular examination reveals an early diastolic murmur in the mitral area. The chest x-ray is negative. Urinalysis shows microscopic hematuria. What is the most appropriate next step in the management of this patient?
Start antibiotics immediately and then obtain blood cultures
Start antibiotics after drawing blood for culture
Do transesophageal echocardiography
Do transthoracic echocardiography
Give aspirin and start his penicillin prophvlaxis
A 65-year-old African-American man is hospitalized after a car accident. He has a vertebral fracture at the level of the fifth thoracic vertebra and is unable to move his lower extremities. Since his injury, he has needed a catheter for micturition. Which of the following is the most effective measure for decreasing the risk of a urinary tract infection in patients requiring bladder catheterization?
Antibacterial creams applied to the urethral meatus
Prophylactic antibiotics
Antibacterial washes of external genitalia
Bladder irrigation with antibacterial solutions
Intermittent catheterization
A 32-year-old man from Arkansas presents to physician with a two-day history of fever, headache, malaise, and myalgias. His family says that he seems slightly confused. He recalls having a tick bite two weeks ago after walking through the woods. His temperature is 39°C (102°F), pulse is 90/min, and blood pressure is 125/80 mm Hg. Neck is supple and there is no lymphadenopathy noted. Oropharynx is clear. Chest auscultation is unremarkable. Abdomen is soft and non-tender. There is no rash evident. Neurologic examination is nonfocal. Laboratory testing shows: Complete blood count:Hemoglobin 14.0 g/L, MCV 88 fL, Platelets 78,000/mm3, Leukocyte count 2,500/mm3, Neutrophils 56%, Eosinophils 1%, Lymphocytes 33%, Monocytes 10%. Liver studies:Total protein, serum 6.5 g/dL, Total bilirubin 1.0 mg/dL, Direct bilirubin 0.8 mg/dL, Alkaline phosphatase 110 U/L, Aspartate aminotransferase (SGOT) 98 U/L, Alanine aminotransferase (SGPT) 105 U/L. What is the most appropriate next step in the management of this patient?
Doxycycline
Chloramphenicol
Erythromycin
Ceftriaxone
Hepatitis serology
A 22-year-old woman presents to the emergency department after she is bitten on her right arm by her neighbor's dog. She provoked the dog while it was eating. The dog is not immunized against rabies, but does not show any signs of rabies. Her right forearm shows a deep bite wound. Her last tetanus booster was 3 years ago. Her wound is cleaned with soap, water, and povidone-iodine solution. What is the most appropriate next step in the management of this patient?
Kill the dog and do brain biopsy
Observe the dog for 10 days
Active immunization for rabies
Passive immunization for rabies
Active and passive immunization for rabies
A 25-year-old male comes to the clinic because of a painless ulcer on his penis. He denies fever or urethral discharge, but admits to recent sexual activity with a prostitute. He describes severe rash and face swelling with penicillin. Physical examination reveals a shallow, non-tender ulcer. There is no lymphadenopathy. Darkfield microscopy reveals spirochetes. Which of the following is the most appropriate treatment for this patient?
Intramuscular benzathine penicillin
Ciprofloxacin
IV aqueous crystalline penicillin
Oral clindamycin
Oral doxycycline
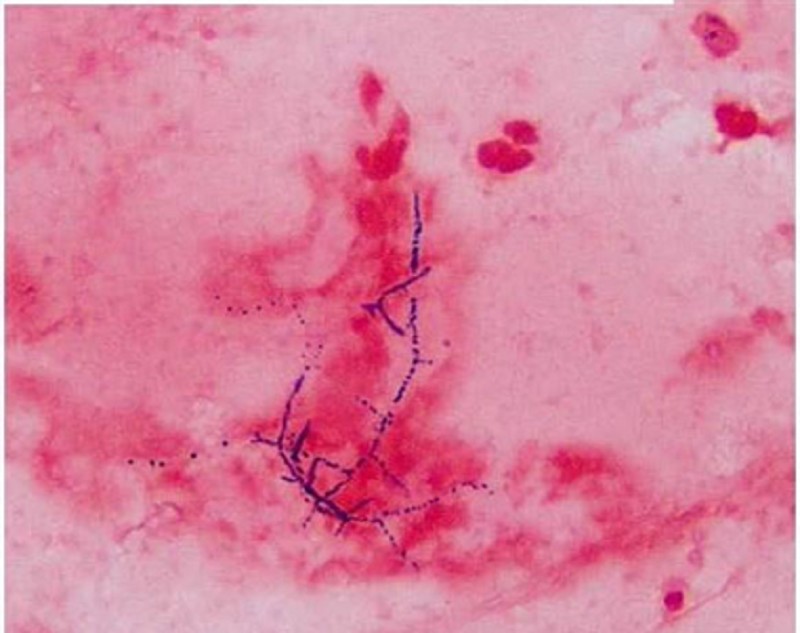
A 40-year -old man who underwent a renal transplant six months ago comes to the clinic with fever, chills, and a productive cough. His temperature is 39.4°C (103°F), pulse is 110/min, respirations are 22/min, and blood pressure is 110/65 mmHg. Chest x-ray shows a right lower lobe nodule with a cavity. Sputum gram stain is shown below. What is the most appropriate treatment of this patient's condition?
Penicillin
Trimethoprim-sulfamethoxazole
Vancomycin
Gentamycin
Metronidazole
A 36-year-old woman who lives in the suburbs of a large city comes to your office for a tuberculin skin test. She will be volunteering in her daughter's school cafeteria and the school district requires tuberculin testing. You inject a small amount of Mycobacterium tuberculosis purified protein derivative (PPD) in the skin and 2 days later she returns for a reading. You measure 12 mm of induration. She reports no history of tuberculosis exposure and no underlying medical conditions. She has never before been tested for tuberculosis. She was born in the United States, is not a healthcare worker, and has never spent time in prison. What is the best next step in her management?
Chest X-ray
Observation
Isoniazid for 6 months
Isoniazid with pyridoxine for 9 months
Isoniazid, rifampin and pyrazinamide for 8 weeks

A 22-year-old female presents to the office with a three-day history of rash, fever, and malaise. There is no burning or itching associated with the rash. Two weeks ago, she had been camping in northern Massachusetts, and noted a tick bite after walking through the woods. She is twelve weeks pregnant. The rash is shown below. The examination is otherwise unremarkable. What is the most appropriate treatment for this patient?
Doxycycline
Amoxicillin
Azithromycin
Ceftriaxone
Penicillin G
A 5-year-old Hispanic girl is brought to the emergency department (ED) due to a cat bite on her right upper extremity. She was bitten after rambunctiously playing for several minutes with the cat, which had just been given to her as a birthday gift. Her most recent booster tetanus vaccine was one year ago. Her temperature is 36.7°C (98°F), blood pressure is 108/70 mm Hg, pulse is 107/min, and respirations are 21/min. Physical examination reveals a deep puncture wound on the volar aspect of her right forearm. Before going to the ED, her mother cleaned the wound with hydrogen peroxide. There is no visible debris in the wound, and little bleeding is evident. Neurovascular function is intact. Her wound is cleaned in the ED with Betadine and lavaged with saline solution. What is the best next step in managing this girl's care?
Bandage with dry gauze and discharge home
Prescribe amoxicillin
Prescribe amoxicillin/clavulanate
Prescribe erythromycin
Prescribe levofloxacin
A 57-year-old male comes to your office in the middle of January. He complains of a 4-day history of a nonproductive cough and coryza. He also has vague muscle aches and a mild headache. He denies any shortness of breath or chest pain. His past medical history is significant for hyperlipidemia and impaired glucose tolerance. He takes aspirin and simvastatin 40 mg at bedtime. He has no known drug allergies. His medical records show that he did not show up for his scheduled annual influenza vaccine this year. His temperature is 38.5°C (101.3°F), blood pressure is 135/80 mm Hg, and pulse is 88/min. Physical examination shows conjunctival redness and an erythematous oropharynx. The tympanic membranes are clear. The heart sounds are audible with no added murmurs, rubs or gallops. His breath sounds are vesicular in quality and equal bilaterally. Which of the following is the most appropriate next step in management?
Administer influenza vaccination now
Write a prescription for amantidine
Write a prescription for oseltamivir
Advise bed rest and symptomatic treatment with acetaminophen
Empiric trial of oral antibiotics
A 60-year-old Caucasian woman undergoes elective coronary artery bypass surgery and aortic valve replacement. Her postoperative course is complicated by acute renal failure, atrial fibrillation, and pulmonary edema. On the third postoperative day, extubation is attempted but not tolerated, thus warranting reintubation. On the fifth postoperative day, she develops a fever to 38.9°C (102°F). Her pulse is 110-120/min and irregular, respirations are 36/min, and blood pressure is 110/65 mmHg. Her chest x-ray shows right middle and lower lobe infiltrates. WBC count is elevated with bandemia. Gram stain of her sputum shows gram-negative rods. She is given intravenous ceftriaxone; however, she deteriorates over the next 24 hours. Which of the following is the most appropriate next step in the management of this patient?
Stop ceftriaxone and start piperacillin-tazobactam
Continue ceftriaxone and add vancomycin
Stop ceftriaxone and start clindamycin
Continue ceftriaxone and add ceftazidime
Continue ceftriaxone and add amphotericin
A 34-year-old man is traveling in Southeast Asia on business. He is staying in Western-style hotels and eating food in large restaurants. He has not eaten from street vendors. One week after arrival, he develops symptoms of anorexia, nausea, and abdominal cramps followed by the sudden onset of watery diarrhea. He has no fever or chills and there is no blood or pus in the stools. Which of the following is the most appropriate therapy for his condition?
Amoxicillin
Symptomatic therapy with loperamide
Doxycycline
Oral rehydration only
Specific antitoxin
A 45-year-old woman is undergoing chemotherapy for breast cancer. She presents 10 days after her last chemotherapy with fever (temperature > 38.5°C), but no other symptoms except a sore throat and mouth. On examination, she looks well, there is oral mucositis, ears are normal, lungs are clear, and the central line site is clean. The CXR, urinalysis, and biochemistry are normal. Her WBC is 800/mL and the absolute neutrophil count is low ( < 500). Which of the following is the most appropriate next step in management?
Start empiric bacterial antibiotics
Start empiric antifungal and bacterial antibiotics
Acetaminophen alone until culture results are available
Start antiviral medications for HSV-1
Start antiviral and bacterial antibiotics
A 74-year-old man residing in a nursing home develops symptoms of high fever, diarrhea, chest pain, and nonproductive cough. His temperature is 40°C, blood pressure 120/80 mm Hg, respiration 24/min, and oxygen saturation 90%. He has bibasilar crackles, normal heart sounds, and a soft nontender abdomen. His CXR reveals bilateral lower lobe infiltrates. He is not able to provide any sputum, and the urine is positive for legionella antigen. Which of the following is the most appropriate antibiotic choice?
Trimethoprim-sulfamethoxazole
Azithromycin
Ceftriaxone
Cefuroxime
Gentamicin
A 28-year-old female presents to her internist with a 2-day history of low-grade fever and lower abdominal pain. She denies nausea, vomiting, or diarrhea. On physical examination, there is temperature of 38.3°C (100.9°F) and bilateral lower quadrant tenderness, without point or rebound tenderness. Bowel sounds are normal. On pelvic examination, an exudate is present and there is tenderness on motion of the cervix. Her white blood cell count is 15,000/μL and urinalysis shows no red or white blood cells. Serum β-hCG is undetectable. Which of the following is the best next step in management?
Treatment with ceftriaxone and doxycycline
Endometrial biopsy
Surgical exploration
Dilation and curettage
Aztreonam
Two students from a university dormitory building have contracted meningitis due to Neisseria meningitides. Which of the following students in the dormitory are most likely to benefit from chemoprophylaxis?
Everybody in the dormitory, with oral amoxicillin
Close contacts only, with oral amoxicillin
Everybody in the dormitory, with oral rifampin
Close contacts only, with oral rifampin
Everybody in the dormitory, with meningococcal vaccine
You are a physician in charge of patients who reside in a nursing home. Several of the patients have developed influenza-like symptoms, and the community is in the midst of influenza A outbreak. None of the nursing home residents have received the influenza vaccine. Which course of action is most appropriate?
Give the influenza vaccine to all residents who do not have a contraindication to the vaccine (ie, allergy to eggs)
Give the influenza vaccine to all residents who do not have a contraindication to the vaccine; also give oseltamivir for 2 weeks to all residents
Give amantadine alone to all residents
Give azithromycin to all residents to prevent influenza-associated pneumonia
Do not give any prophylactic regimen
A 22-year-old university student complains of fatigue and malaise for the past 2 weeks. She also reports feeling feverish, and recently had a sore throat. Physical examination reveals enlarged tonsils and palpable cervical lymph nodes. There is also tenderness in the right upper quadrant on deep palpation, and minimal splenomegaly. Laboratory data show hemoglobin 13 g/dL; hematocrit 40%; platelets 340,000/mL; WBC 9400/mL, with 35% segmented neutrophils, 1% eosinophils, and 64% lymphocytes, of which 36% were atypical. A heterophil antibody (sheep cell agglutination) test is positive. Which of the following is the most appropriate initial treatment for this condition?
Gamma-globulin
Adequate rest
Chlorambucil
Chloramphenicol
Radiation therapy
A 44-year-old renal transplant patient develops severe cough and shortness of breath on exertion. On examination, he appears dyspneic, respirations 24/min, pulse 110/min, and oxygen saturation 88%. His lungs are clear on auscultation and heart sounds are normal. CXR shows bilateral diffuse perihilar infiltrates. Bronchoscopy and bronchial brushings show clusters of cysts that stain with methenamine silver. Which of the following is the most appropriate next step in management?
Amphotericin B
Cephalosporins
Trimethoprim-sulfamethoxazole
Aminoglycosides
Penicillins
A businesswoman needs to make frequent trips to South America, but every time she is there, she develops traveler’s diarrhea, which requires her to change her business schedule. To prevent future episodes during business trips, she is inquiring about prophylaxis methods. Which of the following is the most helpful advice for her?
Take loperamide for symptoms
Take trimethoprim-sulfamethoxazole every day
Take azithromycin every day
Take doxycycline every day
Take ciprofloxacin only if moderate or severe symptoms develop
A 30-year-old male patient complains of fever and sore throat for several days. The patient presents to you today with additional complaints of hoarseness, difficulty breathing, and drooling. On examination, the patient is febrile and has inspiratory stridor. Which of the following is the best course of action?
Begin outpatient treatment with ampicillin
Culture throat for β-hemolytic streptococci
Admit to intensive care unit and obtain otolaryngology consultation
Schedule for chest x-ray
Obtain Epstein-Barr serology
A 35-year-old previously healthy male develops cough with purulent sputum over several days. On presentation to the emergency room, he is lethargic. Temperature is 39°C, pulse 110, and blood pressure 100/70. He has rales and dullness to percussion at the left base. There is no rash. Flexion of the patient’s neck when supine results in spontaneous flexion of hip and knee. Neurologic examination is otherwise normal. There is no papilledema. A lumbar puncture is performed in the emergency room. The cerebrospinal fluid (CSF) shows 8000 leukocytes/μL, 90% of which are polys. Glucose is 30 mg/dL with a peripheral glucose of 80 mg/dL. CSF protein is elevated to 200 mg/dL. A CSF Gram stain shows gram-positive diplococci. Which of the following is the correct treatment option?
Begin acyclovir for herpes simplex encephalitis
Obtain emergency MRI scan before beginning treatment
Begin ceftriaxone and vancomycin for pneumococcal meningitis
Begin ceftriaxone, vancomycin, and ampicillin to cover both pneumococci and Listeria
Begin high-dose penicillin for meningococcal meningitis
A young man has recently been bitten by a stray dog. He has a penetrating wound to the right forearm. The dog is nowhere to be found. In the emergency room, the wound is cleaned with water and povidone-iodine solution. Which of the following is the most appropriate next step in management?
Start postexposure prophylaxis
Contact the local public health professional for further advice
Treat with oral doxycycline
Treat with IV ceftriaxone
Start IV acyclovir
A 22-year-old male, recently incarcerated and now homeless, has received one week of clarithromycin for low-grade fever and left upper-lobe pneumonia. He has not improved on antibiotics, with persistent cough productive of purulent sputum and flecks of blood. Repeat chest x-ray suggests a small cavity in the left upper lobe. Which of the following statements is correct?
The patient has anaerobic infection and needs outpatient clindamycin therapy
The patient requires sputum smear and culture for acid fast bacilli
The patient requires glove and gown contact precautions
Isoniazid prophylaxis should be started if PPD is positive
Drug resistant pneumococci may be causing this infection
A 23-year-old woman visits your office because of headache, malaise, anorexia, pain in both sides of her jaw, and discomfort in both lower abdominal quadrants. Physical examination reveals enlarged parotid glands; bilateral lower quadrant abdominal tenderness; a temperature of 38.7°C; and a pulse rate of 92/min. Serologic testing (IgM) confirms the diagnosis of mumps. Which of the following is the most appropriate treatment for this condition?
Symptomatic
Immunization
Broad-spectrum antibiotics
Sulfonamides
Steroids
A 25-year-old woman complains of dysuria, frequency, and suprapubic pain. She has not had previous symptoms of dysuria and is not on antibiotics. She is sexually active and on birth control pills. She has no fever, vaginal discharge or history of herpes infection. She denies back pain, nausea, or vomiting. On physical examination she appears well and has no costovertebral angle tenderness. A urinalysis shows 20 white blood cells per high power field. Which of the following statements is correct?
A 3-day regimen of trimethoprim-sulfamethoxazole is adequate therapy
Quantitative urine culture with antimicrobial sensitivity testing is mandatory
Obstruction resulting from renal stone should be ruled out by ultrasound
Low-dose antibiotic therapy should be prescribed while the patient remains sexually active
The etiologic agent is more likely to be sensitive to trimethoprim-sulfamethoxazole than to fluoroquinolones
A 40-year-old woman cut her finger while cooking in her kitchen. Two days later she became rapidly ill with fever and shaking chills. Her hand became painful and mildly erythematous. Later that evening her condition deteriorated as the erythema progressed and the hand became a dusky red. Bullae and decreased sensation to touch developed over the involved hand. What is the most important next step in the management of this patient?
Surgical consultation and exploration of the wound
Treatment with clindamycin for mixed aerobic-anaerobic infection
Treatment with penicillin for clostridia infection
Vancomycin to cover community-acquired methicillin-resistant Staphylococcus
Evaluation for acute osteomyelitis
A 60-year-old man comes to the physician because of a 2-week history of worsening fatigue. He has chronic renal insufficiency, hypertension, diabetes mellitus, hypercholesterolemia, hypothyroidism, polymyalgia rheumatica and depression. He was started on lisinopril for the prevention of proteinuria from diabetic nephropathy. Physical examination shows a few basal crackles. He is being considered for dialysis. Laboratory studies show hyperkalemia with serum K + of 6.0 mEq/L. EKG shows no abnormalities. Which of the following is the best treatment to remove K+ from his body?
Sodium bicarbonate
Beta agonists
Calcium gluconate
Kayexalate
Insulin plus glucose
A 45-year-old man with advanced chronic renal failure comes to the physician because of edema of his feet. His temperature is 37°C (99°F), blood pressure is 150/100mm Hg, pulse is 78/min, and respirations are 15/min. Examination shows bilateral ankle edema. Laboratory studies show BUN of 62 mg/dl, serum creatinine of4.2 mg/dl, serum potassium of 5.6 meq/l, serum sodium of 146 meq/l, and total plasma cholesterol of 260 mg/dl. Which of the following is most likely to improve the prognosis of his disease?
Captopril
Simvastatin
Protein restriction
Salt restriction
Potassium restriction
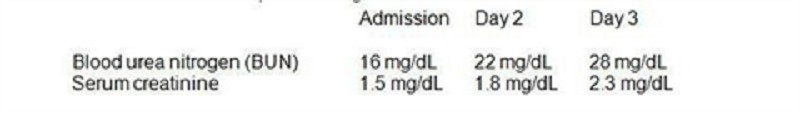
A 68-year-old male presents to the emergency room with cough. Chest x-ray is clear of infiltrates but reveals a right upper lobe lung lesion incidentally. A chest CT scan with IV contrast is performed in the emergency department and reveals a 1 cm x 2cm round lesion in the right upper lobe. The patient is admitted to the hospital, and by day 3 of his hospitalization, he has developed acute renal failure. The patient's past medical history is significant for hypertension, hyperlipidemia, diabetes and coronary artery disease. His medications include aspirin, hydrochlorothiazide, clopidogrel, metoprolol, atorvastatin and lisinopril, all of which he has been taking for several years. He has no known drug allergies. He is a former smoker and does not use alcohol or drugs. His baseline blood pressure is 140/90 mm Hg and has remained in the 140s/90s throughout this admission. Physical examination is otherwise unremarkable. The patient's laboratory values from the time of admission to present are given below. Over the course of the next week, the patient's renal function returns to normal. Which of the following would most likely have prevented his renal failure?
Prednisone
Furosemide
Stopping clopidogrel
Intravenous hydration
100% oxygen mask
A 23-year-old male hospitalized for confusion and seizures is treated with intravenous high-dose acyclovir. On the third day of hospitalization, his serum creatinine level increases to 3.4 mg/dl from a baseline of 0.9 mg/dl at admission. The observed finding could have been potentially prevented by which of the following?
Careful allergy history taking
Monitoring the blood drug levels
Pre-treatment with allopurinol
Pre-treatment with prednisone
Aggressive intravenous hydration
A 27-year-old man comes to the physician because of a 1-day history of fever and joint pains. He is being treated with cephalexin for a skin infection. His urine has turned darker. His temperature is 38.5°C (101.3°F), blood pressure is 125/70 mm Hg, pulse is 90/min, and respirations are 15/min. Examination shows a skin rash; examination otherwise shows no abnormalities. Urinalysis shows: 8 RBCs/HPF, 12 WBCs/HPF with white cell casts, eosinophiluria, and a mild degree of proteinuria. Laboratory studies show a BUN of 40 mg/dl and serum creatinine of 2.2 mg/dl. Which of the following is the most appropriate next step in management?
Discontinue cephalexin
Start ampicillin and gentamicin
Start oral ciprofloxacin
Start intravenous steroids
Start oral steroids
A 30-year-old man is admitted to the hospital with a diagnosis of acute renal failure secondary to poststreptococcal glomerulonephritis. On his fifth hospital day, he develops retrosternal, non-radiating chest pain which is relieved by leaning forward. He denies the use of tobacco or drugs. He drinks alcohol occasionally. He has no past history of any serious illness. His temperature is 37.6°C (99.8°F), blood pressure is 145/95 mm Hg, pulse is 80/min, and respirations are 20/min. A pericardial friction rub is heard on chest auscultation. The rest of the examination shows no abnormalities. EKG shows ST segment elevation in all leads, with elevation of the PR segment in lead aVR. The chest x-ray is normal. Urinalysis shows hematuria, red cell casts and mild proteinuria. Laboratory studies show a BUN level of 60 mg/dl and a serum creatinine level of 3 8 mg/dl. What is the most appropriate next step in management?
Broad spectrum antibiotics
Intravenous steroids
Hemodialysis
Thrombolytic therapy
NSAIDs
A 47-year-old diabetic woman comes to the physician due to the recent onset of tremors. She has undergone combined pancreatic and kidney transplantation secondary to end stage renal disease and diabetes. She takes multiple medications, including immunosuppressants. Her temperature is 36.1° C (97°F), blood pressure is 152/90 mm Hg, pulse is 78/min, and respirations are 16/min. Examination shows gum hypertrophy. Laboratory studies show: Hb 13.0 g/dl, WBC 8,000/cmm, Serum Na 135 mEq/L, Serum K 5.3 mEq/L, BUN 26 mg/dl, Serum Creatinine 1.7 mg/dl. Which of the following immunosuppressants is most likely responsible for her presentation?
Tacrolimus
Cyclosporine
Azathioprine
Mycophenolate
Diuretic
A 45-year-old male patient comes to the physician's office for a routine check-up. He denies any symptoms and says he feels "perfectly healthy." He was diagnosed with hypertension and mixed hypercholesterolemia a year ago. He is currently taking hydrochlorothiazide, amiloride and simvastatin daily. He does not use tobacco, alcohol or drugs. His blood pressure today is 135/85 mm Hg. Physical examination shows no abnormalities. Routine blood results reveal the following: CBC: Hb 14.2g/dL, Ht 42%, MCV 86 fl, Platelet count 260,000/cmm, Leukocyte count 8,500/cmm, Neutrophils 70%, Eosinophils 1%, Lymphocytes 24%, Monocytes 5%. Serum: Serum Na 140 mEq/L, Serum K 5.7 mEq/L, Chloride 100 mEq/L, Bicarbonate 24 mEq/L, BUN 10 mg/dL, Serum Creatinine 1.1 mg/dL, Calcium 9.0 mg/dL, Blood Glucose 118 mg/dL, Total cholesterol 220 mg/dL, LDL cholesterol 130 mg/dL. The blood sample is checked and is not hemolysed. The EKG shows normal sinus rhythm. What is the most appropriate next step in the management of this patient?
Intravenous calcium gluconate
Intravenous dextrose + insulin
Stop amiloride and recheck lab results in 1 week
Stop HCTZ and recheck lab results in 1 week
Start patient on a low potassium diet
A 50-year-old man comes to the emergency department due to a sudden onset of severe, colicky pain in the right flank. He was admitted twice in the past for similar complaints; he was managed conservatively and sent home on both occasions. He has no other medical problems. He does not use tobacco, alcohol or drugs. His vital signs are stable. He is given IV fluids and narcotics. Laboratory studies show: Hb 14.5 g/dL, WBC 13,000/cmm; no bands, Platelets 300,000/cmm, BUN 16 mg/dl, Serum Creatinine 0.8 mg/dl. CT scan of the abdomen without contrast shows renal calculi. Which of the following is the best advice for the prevention of future stones in this patient?
Decrease dietary calcium intake
Mega doses of Vitamin C
Decrease dietary protein and oxalate
Restrict fluid intake
Increase sodium intake
A 64-year-old male with a past medical history of hypertension, diabetes and chronic renal insufficiency presents with gross hematuria. His baseline serum creatinine is 1.6-1.7 mg/dl. The patient's medications include aspirin, hydrochlorothiazide, enalapril, and simvastatin. He has no known environmental, medication, or contrast allergies. On physical examination, the patient has a blood pressure of 130/80 mm Hg. The examination is otherwise unremarkable. Contrast CT scan of the abdomen is planned to evaluate his condition. Which of the following interventions would be most helpful in preventing contrast-induced kidney damage?
Prednisone
. Non-ionic contrast agent
Furosemide
100% oxygen mask
Stopping simvastatin
A 26-year-old man comes to the emergency department because of a sudden onset of severe right-sided flank pain. The pain is colicky and radiates from the flank to the scrotum. He also has nausea, vomiting and dark-colored urine. He has never had these symptoms before. His temperature is 37°C (98.6°F), blood pressure is 126/70 mm Hg, pulse is 90/min, and respirations are 18/min. Examination shows no abnormalities. He is given adequate analgesia. Non-contrast helical CT shows a 4 mm radiopaque stone in the right upper ureter. Laboratory studies show serum calcium of 9.8 mg/dl, serum creatinine of 0.9 mg/dl, and BUN of 15mg/dl. Urinalysis shows hematuria but no casts. Which of the following is the most appropriate next step in management?
24 hr urine collection for metabolic evaluation
Reassurance
Fluid intake greater than 2L/day
Intake of potassium citrate
Restriction of dietary oxalate

A healthy 54-year-old man comes to the physician for a routine health maintenance examination. He has no complaints, but he is requesting for a CT scan of the abdomen. His father died at the age of 60 due to the sudden rupture of an undiagnosed abdominal aortic aneurysm. He has a history of hypertension and gouty arthritis. His social history is not significant. His vital signs are stable. Physical examination shows no abnormalities. ACT scan of the abdomen is shown below. Which of the following is the most appropriate next step in management?
Reassurance
Surgery
CT guided biopsy
Antibiotics
Repeat CT scan in 3 months
A 72-year-old woman with poorly controlled type 2 diabetes mellitus presents to your clinic one week after being discharged from the hospital. She had been admitted with pyelonephritis secondary to a multi-drug resistant organism, and received several days of intravenous antibiotics. Her serum creatinine on admission had been 2.1 mg/dl. Today it is found to be 4.9 mg/dl. Urinalysis reveals rare epithelial casts and no white blood cells. FENa is greater than 2%. What antibiotic did she most likely receive during her hospitalization?
Nafcillin
Vancomycin
Levofloxacin
Amikacin
Doxycycline
A 58-year-old man comes to the physician and complains of "problems with erection." He has recurrent and persistently painful erections. His other medical problems include ulcerative colitis, kidney stones, insomnia, depression, hypertension, drug-induced diabetes, obesity and hypercholesterolemia. He does not use tobacco, alcohol, or drugs. He takes prednisone, mesalamine, insulin, 6-mercaptopurine, simvastatin, glyburide, enalapril, trazodone, and fluoxetine. He has no known drug allergies. His vital signs are stable. The general physical examination is unremarkable. Avoidance of which of the following medications could have prevented his condition?
Fluoxetine
Trazodone
Enalapril
Glyburide
Simvastatin
A 30-year-old woman comes to the physician due to the recent onset of occipital headaches. She has taken acetaminophen several times, but the pain returns. She has no fever or visual problems. She has not had similar episodes in the past. She has no history of serious illness. Her temperature is 36.1°C (98°F), blood pressure is 160/90 mm Hg, pulse is 88/min, and respirations are 16/min. Physical examination shows a rightsided renal bruit Which of the following is the most appropriate treatment for this patient's condition?
ACE inhibitors
Furosemide
Angioplasty with stent placement
Surgery
Oral prednisone
A 45-year-old man with known cirrhosis due to hepatitis C is admitted to the hospital for abdominal discomfort and confusion. Physical examination reveals a distended abdomen, leg edema, and deep yellow discoloration of the skin and sclerae. Bibasilar crackles are heard on chest auscultation. His serum sodium level is 127 mEq/L, potassium level is 2.9 mEq/L, and creatinine level is 1.3 mg/dl. On day 3 of his hospitalization, the serum creatinine is 4.2mg/dl. A urinalysis reveals: Protein negative, Glucose negative, WBC 4-5/hpf, RBC 0-1/hpf. Renal ultrasound is normal and the post-void residual urinary volume is less than 50 ml. He is given 2 L of normal saline intravenously with no change in his serum creatinine concentration. This patient's kidney dysfunction can be best corrected by which of the following?
High-dose spironolactone
ACE inhibitors
Liver transplantation
Broad spectrum antibiotics
Pegylated interferon
A 56-year-old man develops oliguria three days after having a kidney transplantation. His postoperative course was uncomplicated. His blood pressure is 160/100 mm Hg and heart rate is 90/min. Palpation of the transplant reveals mild tenderness. Laboratory studies show: Serum sodium 145 mEq/L, Serum potassium 5.5 mEq/L, Serum calcium 8.6 mg/dl, Serum creatinine 3.2 mg/dl, BUN 30 mg/dl. His serum cyclosporine level is normal. Renal ultrasonography does not detect dilatation of the calyces. Biopsy of the transplant shows heavy lymphocyte infiltration and vascular involvement with swelling of the intima. Which of the following is the most appropriate next step in management?
Decrease the dose of cyclosporine
Give IV steroids
Order ureterography
Administer IV diuretics
Prepare for surgery
A 25-year-old woman comes to the physician because of a 3-day history of burning micturition and increased urinary frequency. She has suprapubic discomfort. She denies having unusual vaginal discharge. She has been sexually active and monogamous for the past 4 years with her husband. Her temperature is 37.1°C (98.9°F), blood pressure is 110/70 mm Hg, pulse is 68/min, and respirations are 15/min. Examination shows suprapubic tenderness without flank tenderness. The rest of the examination is normal. Urinalysis shows: Specific gravity 1.020, Blood Trace, Glucose Negative, Ketones Negative, Leukocyte esterase Positive, Nitrites Positive, WBC 40-50/hpf, RBC 6-10/hpf, Bacteria 50+. Which of the following is the most appropriate next step in management?
Urine culture
Oral trimethoprim-sulfamethoxazole
Oral ciprofloxacin
Oral nitrofurantoin
Intravenous trimethoprim-sulfamethoxazole
A 34-year-old man is being evaluated for possible end-stage renal disease. He has a long history of diabetes, type 1. He previously developed chronic renal insufficiency despite being on enalapril and insulin. His renal function is getting worse day by day. A nephrologist is currently managing his renal condition. Which of the following long-term treatments would give the best survival rate for this patient?
Hemodialysis
Peritoneal dialysis
Renal transplantation from a cadaver
Renal transplantation from a living related donor
Renal transplantation from a living unrelated donor
A 50-year-old diabetic woman presents for follow-up of her hypertension. Her blood pressure is 152/96 in the office today and she brings in readings from home that are consistently in the same range over the past month. Her current medications are amlodipine 5 mg daily and hydrochlorothiazide 25 mg daily. The diuretic was added when she developed peripheral edema on the amlodipine; now she has only trace peripheral edema. A spot urine specimen shows 280 μg of albumin per mg creatinine (microalbuminuria is present if this value is between 30 and 300 μg/mg). What would be the best next therapeutic step in this patient?
Add clonidine
Add a beta-blocker
Increase the thiazide diuretic dose
Add an alpha-blocker
Add angiotensin-converting enzyme inhibitor or angiotensin receptor blocker
A 64-year-old woman develops severe diarrhea 2 weeks after finishing antibiotics for pneumonia. She has also noticed decreased urine output despite drinking lots of fluids. On examination, she has a postural drop in her blood pressure, the JVP is low, and the abdomen is soft but diffusely tender. Despite giving 4 L of normal saline, her urine output remains low. The urinalysis is positive for heme-granular casts and the urine sodium is 42mEq/L. Which of the following medications should be held during the recovery phase of this woman’s ARF?
Acetaminophen
Digoxin
Lorazepam
Enalapril
Simvastatin
A 67-year-old man with a history of gout presents with intense pain in his right great toe. He has a complex past medical history, including hypertension, coronary artery disease, congestive heart failure, myelodysplasia, and chronic kidney disease with a baseline creatinine of 3.2 mg/dL and a uric acid level of 10 mg/dL. His medications include aspirin, simvastatin, clopidogrel, furosemide, amlodipine, and metoprolol. What is the best therapy in this situation?
Colchicine 1.2 mg po initially, followed by 0.6 mg 1 hour later
Allopurinol 100 mg po daily and titrate to uric acid less than 6 mg/dL
Prednisone 40 mg po daily
Naproxen 750 mg po once followed by 250 mg po tid
Probenecid 250 mg po bid
A 60-year-old diabetic woman develops angina and will need a coronary angiogram for evaluation of coronary artery disease. She has a creatinine of 2.2. Which of the following is the most effective in reducing the risk of contrast induced nephropathy?
Administer mannitol immediately after the contrast is given
Perform prophylactic hemodialysis after the procedure
Give IV hydration with normal saline or sodium bicarbonate prior to and following the procedure
Indomethacin 25 mg the morning of the procedure
Dopamine infusion before and after the procedure
A 56-year-old man presents with hypertension and peripheral edema. He is otherwise healthy and takes no medications. Family history reveals that his father and a brother have kidney disease. His father was on hemo-dialysis before his death at age 68 of a stroke. Physical examination reveals BP 174/96 mm Hg and AV nicking on funduscopic examination. He has a soft S4 gallop. Bilateral flank masses measuring 16 cm in length are palpable. Urinalysis shows 15 to 20 RBC/hpf and trace protein but is otherwise normal; his serum creatinine is 2.4 mg/dL. Which is the most likely long-term complication of his condition?
End-stage renal disease requiring dialysis or transplantation
Malignancy
Ruptured cerebral aneurysm
Biliary obstruction owing to cystic disease of the pancreas
Dementia
A 63-year-old woman has Type II diabetes mellitus, which is well-controlled. Her physical examination is positive for peripheral neuropathy in the feet and nonproliferative retinopathy. A urinalysis is positive for proteinuria. Which of the following treatments is most likely to attenuate the course of renal disease?
Calcium channel blockers
ACE inhibitors
Hepatic hydroxymethylglutaryl- coenzyme A (HMG-CoA) inhibitors
Dietary carbohydrate restriction
Weight reduction
A 60-year-old man is brought in by ambulance and is unable to speak. The EMS personnel tell you that a neighbor informed them he has had a stroke in the past. There are no family members present. His serum sodium is 118 mEq/L. Which of the following is the most helpful first step in the assessment of this patient’s hyponatremia?
Order a chest x-ray
Place a Foley catheter to measure 24-hour urine protein
Clinical assessment of extracellular fluid volume status
CT scan of head
Serum AVP (arginine vasopressin) level
A 39-year-old woman is admitted to the gynecology service for hysterectomy for symptomatic uterine fibroids. Postoperatively the patient develops an ileus accompanied by severe nausea and vomiting; ondansetron is piggybacked into an IV of D5 ½ normal saline running at 125 cc/h. On the second postoperative day the patient becomes drowsy and displays a few myoclonic jerks. Stat labs reveal Na 118, K 3.2, Cl 88, HCO3 22, BUN 3, and creatinine 0.9. Urine studies for Na and osmolality are sent to the lab. What is the most appropriate next step?
Change the IV fluid to 0.9% (normal) saline and restrict free-water intake to 600 cc/d
Change the ondansetron to promethazine, change the IV fluid to lactated Ringer solution, and recheck the Na in 4 hours
Start 3% (hypertonic) saline, make the patient NPO, and transfer to the ICU
Change the IV fluid to normal saline and give furosemide 40 mg IV stat
Make the patient NPO and send for stat CT scan of the head to look for cerebral edema
You evaluate a 48-year-old man for chronic renal insufficiency. He has a history of hypertension, osteoarthritis, and gout. He currently has no complaints. His medical regimen includes lisinopril 40 mg daily, hydro-chlorothiazide 25 mg daily, allopurinol 300 mg daily, and acetaminophen for his joint pains. He does not smoke but drinks 8 oz of wine on a daily basis. Examination shows BP 146/86 mm Hg, pulse 76, a soft S4 gallop, and mild peripheral edema. There is no abdominal bruit. His UA reveals 1+ proteinuria and no cellular elements. Serum creatinine is 2.2 mg/dL and his estimated GFR from the MDRD formula is 42 mL/minute. What is the most important element is preventing progression of his renal disease?
Discontinuing all alcohol consumption
Discontinuing acetaminophen
Adding a calcium channel blocker to improve blood pressure control
Obtaining a CT renal arteriogram to exclude renal artery stenosis
Changing the lisinopril to losartan
A 45-year-old woman with cirrhosis secondary to autoimmune hepatitis is seeing her hepatologist for routine follow-up. She reports that she has been feeling relatively well lately, and complains only of mild fatigue. Her medical history is otherwise unremarkable. Her medications include lactulose, spironolactone, propranolol and furosemide. Her vital signs are stable and the remainder of her physical exam is consistent with compensated cirrhosis. Her laboratory values are given below: Sodium 132 mEq/L, Potassium 4.1 mEq/L, Chloride 100 mEq/L, Bicarbonate 24 mEq/L, Glucose 102 mg/dl, Creatinine 0.9 mg/dl, Calcium 7.4 mg/dl, Total protein 6.1 g/dl, Albumin 2.5 g/dl, Total bilirubin 2.1 mg/dl, AST 80 units/L, ALT 102 units/L. What is the most appropriate next step in the management of this patient's hypocalcemia?
Calcium gluconate infusion
Measurement of vitamin D levels
Replace furosemide with hydrochlorothiazide (HCTZ)
Initiate oral calcium and vitamin D replacement
No intervention is required
A 43-year-old female with history of hepatitis C, alcohol use and cirrhosis is admitted to the hospital for severe vomiting for the last 2 days. Her temperature is 36.7°C (98.2°F), pulse is 90/min, respirations are 14/min and blood pressure is 100/70 mmHg supine. Her lungs are clear to auscultation. She has mild epigastric tenderness, but there is no abdominal distention. Extremities have no edema. Her laboratory profile shows: Blood PH 7.49, PaO2 100 mmHg, PaCO2 41 mm Hg, HCO3- 30 mEq/L, Sodium 138 mEq/L, Potassium 3.0 mEq/L, Chloride 95 mEq/L. Which of the following is the most appropriate treatment for the patient's alkalosis?
Intravenous ammonium chloride and potassium
Intravenous hydrochloric acid and potassium
Intravenous mannitol
Intravenous normal saline and potassium
Dialysis
A 21-year-old woman complains of progressive weakness and loss of energy. She nearly collapsed yesterday while performing one of her routine 3 hour workouts. Additionally, she has been performing badly in college despite persistent attempts to improve her grades. Physical exam reveals a blood pressure of 102/58 mmHg, heart rate of 113/min, fine hair covering her face, and normal heart and lungs. Laboratory studies show the following findings: Sodium 140 mEq/L, Potassium 24 mEq/L, Calcium 10.1 mg/dL, Chloride 90 mEq/L, Bicarbonate 40 mEq/L, Urine chloride 14 mEq/L. Which of the following is most likely to correct the laboratory abnormalities in this patient?
Calcium gluconate infusion
Normal saline infusion
Sodium bicarbonate solution infusion
Loop diuretics
Hyperventilation
A 52-year-old man with Burkitt lymphoma is admitted to the hospital for chemotherapy. He is started on chemotherapy without incident. Two days into his hospitalization, he develops new peaked T-waves on his ECG. Laboratory analysis reveals a serum potassium concentration of 6.2 mEq/L, and the patient is given one ampule of calcium gluconate emergently. His renal function is within normal limits. Which of the following additional interventions will most rapidly correct his hyperkalemia?
Hemodialysis
Sodium polystyrene sulfonate
Furosemide
Insulin and glucose
High-dose inhaled β2 agonist
A 58-year-old man is admitted to the intensive care unit with an exacerbation of his chronic obstructive pulmonary disease (COPD) and respiratory failure. After several hours on noninvasive ventilation the patient develops worsening respiratory distress and requires endotracheal intubation. Which of the following is a contraindication to the use of succinylcholine for rapid-sequence intubation?
Hyperkalemia
COPD exacerbationq
Hepatic failure
Hypokalemia
Hypercalcemia
A 66-year-old white male comes to the physician's office for the first time because of generalized muscle weakness. His review of systems is otherwise negative. He has a past medical history of hypertension, type- 2 diabetes, hyperlipidemia, chronic renal insufficiency and ischemic cardiomyopathy. Neurological examination shows mild weakness of the lower limbs, depressed reflexes and normal sensation. Laboratory studies show: Serum sodium 134 mEq/L, Serum potassium 6.0 mEq/L, Bicarbonate 24 mEq/L, Blood urea nitrogen (BUN) 38 mg/dl, Serum creatinine 2.8 mg/dl, Calcium 8.2 mg/dl, Blood glucose 298 mg/dl. A dose of sodium polystyrene sulfonate is given. Which of the following additional interventions is most important in this patient's management?
Review all his current medications
Measure serum renin and aldosterone levels
Obtain electromyography
Obtain acetylcholine receptor antibodies
Start oral prednisone therapy
A 79-year-old female presents to your office with a three-day history of nausea, diarrhea, poor oral intake and weakness. Her past medical history is significant for hypertension treated with enalapril and diltia zem. Her serum chemistry shows the following: Sodium 139 mEq/L, Potassium 7.8 mEq/L, Bicarbonate 14 mEq/L, Chloride 95 mEq/L, Glucose 155 mg/dl, BUN 80 mg/dl, Creatinine 3.1 mg/dl. EKG reveals QRS prolongation and prominent T wave peaking in precordial leads. Which of the following pharmacologic therapies plays a role in treating this patient's electrolyte condition?
Stimulating alpha 1-adrenoreceptors
Stimulating beta 1-adrenoreceptors
Stimulating beta2-adrenoreceptors
Blocking alpha 1-adrenoreceptors
Blocking beta 1-adrenoreceptors
A 42-year-old male is brought to the emergency department immediately after having a prolonged seizure episode. His family describes a past medical history of grand mal seizures. He has been on phenytoin for the past 10 years, but stopped taking the drug six months ago because he had not had any seizures in the last nine years. He is otherwise healthy and had been doing well until this seizure episode. He does not use tobacco, alcohol or drugs. He is afebrile. His blood pressure is 136/88 mm Hg, respirations are 18/min and pulse is 96/min. He appears confused and lethargic. Chest auscultation is unremarkable, and his abdomen is soft and nontender. A limited neurologic examination is non-focal. His laboratory report shows: Serum sodium 140 mEq/L, Serum potassium 4.0 mEq/L, Chloride 103 mEq/L, Bicarbonate 17 mEq/L, Blood urea nitrogen (BUN) 20 mg/dl, Serum creatinine 0.8 mg/dl, Blood glucose 98 mg/dl. Chest x-ray and urinalysis are within normal limits, and a CT scan of the head is unremarkable. Which of the following is the most appropriate next step in the management of this patient's metabolic acidosis?
Give intravenous bicarbonate
Check serum ketones
Check serum lipase
Observe and repeat the labs after 2 hours
Start dopamine
A 50-year-old male patient comes to the office because he is concerned about the marked tremors of his hands. His tremors disappear with voluntary activity and worsen with emotional stress. He finds it mild difficult to initiate movements. He does not have a family history of tremors. Physical examination reveals tremors that occur at a frequency of 3-4 cycles/sec. There is rigidity of his limb musculature. His gait and posture is minimally disturbed. His higher mental functions are intact. Which of the following is the most appropriate treatment for this patient?
Benztropine
Amantadine
Selegiline
Clozapine
Propranolol
A 67-year-old male presents with a six-month history of rigidity, gait problems, tremor and slowness of movements. His condition has progressively worsened over the last few months, and he is now unable to perform his routine daily activities due to the slowness of his movements. He is not taking any medications. On examination, he is alert and conscious. His face is without expression. There is a resting tremor of his hands. He has a stooped posture and shuffling gate. There is rigidity of his limb muscles. Which of the following is the most appropriate initial treatment for this patient?
L-dopa
Amantadine
Selegiline
Clozapine
Benztropine
A 58-year-old woman presents to the emergency department with severe headache and agitation. She describes her pain as right-sided and retro-orbital, and also reports blurred vision, constipation, and vomiting. Her medical history is significant for Parkinson's disease, hypothyroidism, hypertension and chronic hepatitis C. Work-up reveals that her current condition is medication-induced. Which of the following agents is most likely responsible?
Levodopa
Selegiline
Bromocriptine
Trihexyphenidyl
Propranolol
A 67-year-old male comes to the office for a routine physical exam. He retired this year and wants "a clean bill of health." He has no complaints. He stopped smoking 10 years ago, but smoked for 40 years prior to that. He only takes a "water pill" for hypertension. His vital signs are normal. The physical examination reveals a bruit in his neck. His chest x-ray, EKG, and blood work have normal results. Duplex ultrasonography of his neck reveals a 70% irregular lesion at the right common carotid artery bifurcation. The left common carotid artery has a 40% lesion. What is the best next step in the management of this patient?
Left carotid surgery
Right carotid surgery
Long term ASA therapy
Temporal artery biopsy
Heparin
A middle-aged woman is found wandering the streets with an abnormal gait. Police officers bring her to the hospital. She mumbles when asked for her name and age. She is not oriented to time or place. Her blood pressure is 160/100 mmHg and her heart rate is 100/min. She is afebrile. Mucous membranes are moist and the pupils are dilated and reactive to light. She moves all of her extremities, and her deep tendon reflexes are symmetric. Which of the following is the best initial treatment for this patient?
Naloxone
Flumazenil
Thiamine
Haloperidol
Clonidine
A 61-year-old Caucasian male presents with ptosis, diplopia and limb weakness. These symptoms worsen in the evening and with exercise, and improve with rest. He also has fatigue, which is worse in the evening. He denies any tingling or numbness. On examination, he cannot sustain an upward gaze, and his eyelids tend to drift downward. Injection of edrophonium quickly restores power, and allows him to maintain an upward gaze. Which of the following is the best initial treatment for this patient?
Treatment with pyridostigmine
Treatment with edrophonium
Treatment with atropine
Treatment with prednisolone
Treatment with intravenous immunoglobulins
A 7-year-old boy is brought to the office by his mother because, "he is always daydreaming." Sometimes, he stares for a few seconds and rolls his eyes for unknown reasons. His teacher has noted a recent decline in his school performance. He has no family history of any seizure disorder, and his psychomotor development is normal. His neurological examination is unremarkable. EEG during hyperventilation shows generalized, symmetrical 3-Hz spike-and-wave activity on a normal background. Which of the following medications is the most appropriate to treat the boy's disorder?
Phenytoin
Phenobarbital
Valproic acid
Clonazepam
Lamotrigine
120) A 32-year-old Caucasian male comes to the emergency department due to progressive ascending paralysis, which began 18 hours ago. He initially noticed paresthesias in his lower limbs, followed by a sense of fatigue and weakness. He denies any history of headache, fever, and recent infection or illness. His blood pressure is 120/80 mm Hg, pulse is 80/min, respirations are 16/min, and temperature is 37.3°C (99.2°F). The physical examination reveals intact cranial nerves, absent deep tendon reflexes, and a normal sensory exam. Laboratory studies reveal a normal WBC count. No abnormalities are noted on CSF examination. While evaluating the patient in the hospital, he quickly deteriorates. What is the most appropriate next step in the management of this patient?
IV immunoglobulin and plasmapheresis
Administer botulinum antitoxin
IV methylprednisolone
Meticulous search for a tick
MRI of the spine
A 36-year-old Caucasian male is brought to the emergency department due to weakness of his upper and lower extremities. Neurological examination reveals weakness, atrophy, fasciculations, spasticity and hyperreflexia of the involved muscles. His sensory, bowel, bladder and cognitive functions are intact. Serum creatine kinase is normal. Cerebrospinal fluid examination is within normal limits. Electromyography shows chronic partial denervation. The patient is subsequently diagnosed with amyotrophic lateral sclerosis. Which of the following has been approved for use in patients with amyotrophic lateral sclerosis?
Riluzole
Corticosteroids
Intravenous immunoglobulins
Plasmapheresis
Donepezil
A 62-year-old Caucasian man with hypertension and chronic kidney disease complains of poor sleep. He describes a sensation of spiders crawling over both legs about 15-20 minutes after going to bed. Sometimes he has to sit up in bed and massage his legs. His wife's sleep has deteriorated as her husband's leg movements have gotten worse. Pharmacotherapy for this patient's disease is typically directed at which of the following?
Norepinephrine
Dopamine
Serotonin
Acetylcholine
GABA
A 22-year-old white obese female presents with headache for the last few weeks. Headache is worse at night and wakes her from sleep. Headache is pulsating in quality and is also associated with nausea and vomiting. She denies any weakness, sensory abnormalities or visual problems. She denies any history of trauma. She does not take any medication. Neurological examination is unremarkable. Fundoscopy shows papilledema. CT scan of head does not show any abnormality. Lumbar puncture is performed and CSF examination is normal except increased CSF pressure. Weight loss fails to control her symptoms. Which of the following is the most appropriate next step in the management of this patient?
Treatment with mannitol
Treatment with acetazolamide
Treatment with corticosteroids
Repeated lumbar punctures
Surgery
A 52-year-old Caucasian male comes to the office for the evaluation of tremors. He has been having tremors in both hands and head over the past several months. He does not experience any tremors at rest, or any problem with his legs. He has a history of alcohol abuse. He is currently not on any medication. His father had essential tremors, and his paternal uncle has Parkinsonism. The physical examination reveals tremors, which increase in amplitude when he tries to reach for an object. Which of the following is the most appropriate next step in the management of this patient?
Benztropine
Propranolol
Haloperidol
Valproic acid
Clonazepam
A 32-year-old Caucasian male is admitted to the hospital due to a 1-week history of progressive paralysis of his upper and lower extremities. He had a flu-like illness 3 weeks ago, followed by paresthesias in his fingertips and toes. The weakness initially started in his lower extremities. He denies any changes in bowel and bladder functions. His blood pressure (supine) is 130/70mm Hg, heart rate is 82/min, respirations are 18/min, and temperature is 36.9°C (98.5°F). Physical examination reveals bilateral facial paralysis, orthostatic hypotension, areflexia in all four extremities, and distal paresthesias. His CSF analysis shows: Total WBC 10/cmm, Protein 120 mg/dl, Glucose 70 mg/dl, Gram stains No organisms. What is the most appropriate next step in the management of this patient?
Intravenous methyl prednisolone
Intravenous immunoglobulin therapy
Intravenous acyclovir therapy
Botulinum antitoxin
Intravenous ceftriaxone and ampicillin
A 59-year-old white male comes to the office for the evaluation of a brief episode of right arm and leg weakness. The episode lasted for a few minutes, and was followed by a complete recovery. He had a similar episode one month ago. He has a 30 pack-year history of cigarette smoking. He has hypercholesterolemia, which is being treated with diet and exercise. His pulse is 76/min, regular, and blood pressure is 130/80 mmHg. His laboratory test results are: Hb 14.2 g/dl, WBC 7,000/cmm, Platelets 230,000/cmm, Blood Glucose 118 mg/dl, Serum Na 138 mEq/L, Serum K 4.5 mEq/L, BUN 16 mg/dl, Serum Creatinine 1.0 mg/dl. EKG shows normal sinus rhythm. CT scan of the head is unremarkable. MRI angiography of the head and neck fails to show any abnormality. Transesophageal echocardiography (TEE) is unremarkable. Which of the following is the most appropriate next step in management?
Treatment with aspirin
Treatment with heparin followed by warfarin
Treatment with clopidogrel
Treatment with combination of aspirin and dipyridamole
Treatment with ticlopidine
A 65-year-old lady comes to the office for the evaluation of her deteriorating memory. She has become increasingly forgetful over the last several months, and now appears very concerned about her memory loss. She used to pride herself for her sharp memory, but has been forgetting the most trivial things and has become "extremely inefficient." She also complains of easy fatigability, poor appetite, and frequent awakening at night. She feels worthless and has lost interest in her favorite hobby, which is gardening. On coughing or laughing, she loses urine involuntarily, and this is adding to her misery. She lives with her husband, who says that she has become very "cranky and irritable" lately. Her medical history is significant for hypercholesterolemia, for which she refuses to take medication. She is presently not on any hormonal therapy. The physical examination is completely normal. Laboratory studies are unremarkable. CT scan of the head is normal. What is the best next step in the management of this patient?
Start hormonal replacement therapy
Treat her with donepezil
Start selective serotonin reuptake inhibitorQ
Surgical bypass shunting
Reassurance
{"name":"USLME medecine interne", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 72-year-old Hispanic man comes to the clinic with complains of mild headache, and lethargy for the past several days. He complains of cough for the past 12 years, the cough has been bothering him more lately. The cough is mucoid, he has noticed blood in it once in a while. He has smoked 1 pack\/day for 29 years. His vitals are, Temperature 37.0°C (98.6°F); BP 120\/84 mm Hg; PR 78\/min; RR 24\/min. On examination of lungs, adventitious sounds are heard over all the lobes and scant crackles at the base. Laboratory studies show: WBC 7,600\/mm3, Hemoglobin 13.6, Hematocrit 40%, Platelets 214,000mm3, Sodium 130 mEq\/L, Potassium 3.6 mEq\/L, Bicarbonate 18 mEq\/L, Blood urea nitrogen 16 mg\/dl, Creatinine 0.6 mg\/dl, Glucose 95 mg\/dl, Serum osmolality 260 mOsm\/kg (normal 280), Urine osmolality 310 mOsm\/kg. A chest x-ray shows a 2-centimeter left upper lobe mass and mediastinal adenopathy. What will be the next best step in management of this patient?, You are called by the hospice nurse to evaluate a 74-year-old man who refuses to eat. He has terminal colon cancer, which was diagnosed 8 months ago and has metastasized to his liver. He has already gone through chemotherapy with 5-Fiourouracil + oxaliplatin. During the past 4 months, his condition has gotten extremely worse. He has lost 501bs (27.6kg), and currently appears totally wasted. As you approach him, he says, \"I don't feel like eating anything, and I don't want any more procedures, but I'll drink any pill that can make me feel better.\" His abdomen is distended with positive fluid thrills. His liver has several palpable nodules. What is the best pharmacological agent of choice for this patient's anorexia?, A 67 -year-old man presents to your office with a one month history of progressive fatigue and exertional dyspnea. He has no significant past medical history. Physical examination reveals enlarged, non-tender axillary lymph nodes bilaterally. His abdomen is soft and non-tender and the liver span is 10 cm. Serial fecal occult blood tests are negative. Laboratory values are as follows: Hemoglobin 7.8 mg\/dl, MCV 90 fl, MCHC 33 g\/dl, Reticulocytes 7%, WBC count 22,000\/mm3, Platelets 200,000\/mm3. Which of the following is most likely to improve this patient's symptoms?","img":"https://cdn.poll-maker.com/11-520022/4.bmp?sz=1200-00000000001000011337"}
More Quizzes
Personality quiz - system engineering edition
8425
Ben Adventures Quiz - Past Simple
84167
Melyik fiú illik hozzád a Kiszámolósból?
2211274
Toxic Traits and True Love Quiz
1168
Nerve Cell - Test Your Neuron Knowledge
201020372
Naruto Genin Exam - Ultimate Ninja Trivia
201017005
Scientist Test - Name These Famous Scientists
201017649
North & Central America Map - Name Every Country
201020575
Tennis Trivia Questions with Answers - 200+ Free
201015320
ICS 200 Final Exam Answers - Free FEMA Practice
201016206
BTS Ideal Type: Which Member's Ideal Type Are You?
201018443
Coupleszes to Take Together - Strengthen Your Bond
201016649