DES C_ParaClinic (5) Prepared : CHILLY
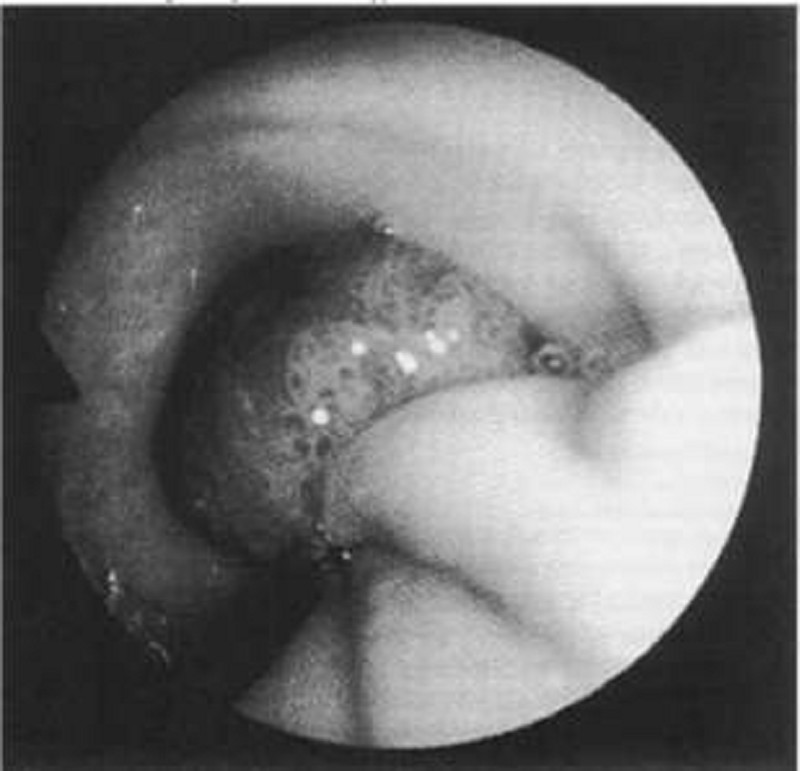
A 58-year-old white man complains of intermittent rectal bleeding and, at the time of colonoscopy, is found to have internal hemorrhoids and the lesion shown at the splenic flexure. Pathology shows tubulovillous changes. Repeat colonoscopy should be recommended at what interval?
In 1 to 2 months
In 1 year
In 3 years
In 10 years
Repeat colonoscopy is not necessary
A 59-year-old man is referred for evaluation because he has been fainting at his job, where he operates heavy machinery. He is pale and gaunt, but otherwise his physical examination is remarkable only for 4+ occult bloods in the stool. Laboratory studies show haemoglobin of 5gm/dL with microcytosis, as well as decreased levels of serum iron and increased iron binding capacity. Which of the following will most likely establish the diagnosis?
Colonoscopy
Upper gastrointestinal endoscopy
Upper gastrointestinal series (swallowed barium studies)
Visceral angiogram
Flexible sigmoidoscopy to 45 cm
A 59-year-old man presents for his routine colonoscopy and during his visit he has numerous large adenomas removed from his colon. Which of the following is the most effective strategy for follow-up of this patient?
Elective colectomy
Repeat colonoscopy in 3 years
Repeat colonoscopy in 10 years
Sigmoidoscopy in 10 years
Urgent colectomy
A 59-year-old man presents to the ED complaining of vomiting and sharp abdominal pain in the epigastric area that began abruptly this afternoon. He describes feeling nauseated and has no appetite. Laboratory results reveal WBC 18,000/μL, hematocrit 48%, platelets 110/μL, AST 275 U/L, ALT 125 U/L, alkaline phosphatase 75 U/L, amylase 1150 U/L, lipase 1450 IU, LDH 400 U/L, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 110 mEq/L, bicarbonate 20 mEq/L, BUN 20 mg/dL, creatinine 1.5 mg/dL, and glucose 250 mg/dL. Which of the following laboratory results correlate with the poorest prognosis?
Amylase 950, lipase 1250, LDH 400
WBC 18,000, LDH 400, glucose 250
WBC 18,000, amylase 950, lipase 1250
Lipase 1250, creatinine 1.5, potassium 3.5
Lipase 1250, LDH 400, bicarbonate 20
A 6 month old male is brought in to the Emergency Room by his mother who states that when she picked him up from the baby-sitter he was not acting right. The baby-sitter stated that he was sleeping more and was fussy. On examination the baby is stuporous. His temperature is 37.8 C (99.9 F), pulse is 140/min, and respirations are 36/min. A 4 cm ecchymosis is noted on his right cheek. The remainder of the physical examination is unremarkable. The physician suspects possible physical abuse. He orders a CT scan of the head, skeletal survey, chemistry panel and complete blood count. Which of the following diagnostic tests should also be ordered?
Ammonia level
Coagulation studies
Lipid panel
Thyroid studies
Urine electrolytes
A 6-month-old child was noted to be normal at birth, but over the ensuing months you have been somewhat concerned about his slowish weight gain and his mild delay in achieving developmental milestones. The family calls you urgently at 7:00 AM noting that their child seems unable to move the right side of his body. Which of the following conditions might explain this child’s condition?
Phenylketonuria
Homocystinuria
Cystathioninuria
Maple syrup urine disease
Histidinemia
A 6-month-old male infant is brought to the physician's office by his mother due to failure to thrive. According to the mother, the child always regurgitates shortly after feedings, and has even had a few episodes of blood-stained projectile vomiting. During the vomiting episodes, the child tilts his head to the left and arches his back. On examination, the child is afebrile. His abdomen is soft and non-tender to palpation. Laboratory evaluation shows hypochromic microcytic anemia. What is the most appropriate test to confirm the most likely diagnosis of this child?
Chest x-ray
Barium swallow
Technetium (Tc) sulfur colloid gastroesophageal scan
24-hour esophageal pH monitoring
Esophageal manometry
A 6-week-old child is being evaluated for a fever of unknown etiology. As part of the laboratory evaluation, a urine specimen was obtained that grew E coli with a colony count of 2000/µL. These findings would be definite evidence of a urinary tract infection if which of the following is true about the sampled urine?
It has a specific gravity of 1.008
It is from a bag attached to the perineum of an uncircumcised boy
It is the first morning sample
It is from an ileal-loop bag
It is from a suprapubic tap
A 6-week-old infant is admitted to the hospital with jaundice. Her outpatient blood work demonstrated a total bilirubin of 12 mg/dL with a direct portion of 3.5 mg/dL. Which of the following disorders is most likely to be responsible?
ABO incompatibility
Choledochal cyst
Rh incompatibility
Gilbert disease
Crigler-Najjar syndrome
A 6-year-old boy has had a fever for 8 days. He just finished a 5-day course of amoxicillin for otitis media. On examination, his temperature is 38.6 C (101.4 F). He has meningismus and palsy of the left sixth cranial nerve. Cerebrospinal fluid (CSF) analysis reveals 200 white cells per mL with 80% lymphocytes and 20% polymorphonuclear leukocytes, glucose of 18 mg/dL, protein of 260 mg/dL, and a negative Gram stain. There is basilar enhancement without focal lesions on CT. Which of the following CSF tests will most likely identify the cause of meningitis?
Antigen test for Cryptococcus
Latex agglutination test for pneumococcus
Culture for mycobacteria
Bacterial culture
Test for Treponema pallidum
A 6-year-old boy presents to his pediatrician for a routine physical examination. His mother reports no problems over the past year except that he seems to be shorter than the other boys in his class. His mother is 163 cm (5'4") tall and experienced menarche at age 12 years, and his father is 178 cm (5'10") tall and went through puberty at approximately age 14 years. On his growth curve, the boy’s height was at the 10th percentile at birth, at the sixth percentile by age 3 years, and at the third percentile now. His weight is currently at the 25th percentile. Which of the following is most important in this patient’s evaluation?
Chromosomal analysis
Insulin-like growth factor-1 level
Growth hormone level
No further evaluation is necessary
Colonoscopy
A 6-year-old boy with mental retardation has recently been diagnosed with Fragile X syndrome. His 9-year-old sister appears to be of normal intelligence but has symptoms of attention deficit hyperactivity disorder (ADHD). What is the first test that is indicated in her work-up for ADHD?
EEG
Cytogenetic testing
MRI
Intelligence quotient (IQ) test
Urine for metabolic screen
A 6-year-old child is hospitalized for observation because of a short period of unconsciousness after a fall from a playground swing. He has developed unilateral pupillary dilatation, focal seizures, recurrence of depressed consciousness, and hemiplegia. Which of the following is the most appropriate management at this time?
Spinal tap
CT scan
Rapid fluid hydration
Naloxone
Gastric decontamination with charcoal
A 6-year-old girl is brought to the emergency room because her urine is red. She has been healthy her whole life, and has recently returned from an outing with her grandmother to a local amusement park. Her urine dip for heme is positive, suggesting which of the following is a possibility?
Ingestion of blackberries
Phenolphthalein catharsis
Ingestion of beets
Presence of myoglobin
Ingestion of Kool-Aid
A 6-year-old girl is brought to the office due to significant steatorrhea and failure to thrive. She has a poor appetite and general malaise. Her past medical history is significant for prolonged neonatal jaundice and numerous respiratory tract infections. On examination, she looks a little underweight and has a runny nose. Auscultation reveals mild wheezing and diminished air entry in both lungs. Clubbing is visible on both hands. What is the best diagnostic test for this patient?
Blood cultures
Sputum cultures
CT abdomen
Sweat chloride test
Liver function tests
A 6-year-old girl is brought to the office for the evaluation of "passing smoky urine." She recently had a sore throat. Her blood pressure is 150/100 mmHg. There is swelling of the face and extremities. Urinalysis reveals many red blood cells, red blood cell casts and 1 + proteinuria. Her serum C3 level and CH 50 are low. Her C4 1evel is normal. Her antistreptolysin-a (ASO) titer is 1,024 Todd units (normal ≤ 166 Todd units). In this patient, which of the following abnormal findings is most likely to become normal within 8 to 12 weeks?
ASO titer
Complement level
Hematuria
Proteinuria
Bacteremia
A 6-year-old girl is brought to the physician by her mother, who says the child has been falling behind at school. She notes that the girl did not speak until the age of 4. She is friendly at school, but is unable to complete most tasks, even when aided. She is noted to have a very short attention span and occasional temper tantrums at school and at home. Which of the following tests would be most helpful in establishing the diagnosis?
Electroencephalogram (EEG)
Hearing test
IQ testing
Complete blood count (CBC)
Lumbar punture
A 60-year-old Caucasian man presents to the office with a 2-week history of worsening shortness of breath and decreased exercise tolerance. His breathlessness is worse at night. He thinks his legs are swelling up. He has hypertension, coronary artery disease and chronic obstructive pulmonary disease. He used to drink heavily and smoke 1 pack of cigarettes daily but has quit recently, although he still reports occasionally drinking a "few beers." He currently denies any chest pain, palpitations or cough. His temperature is 37.5°C (99.5°F), blood pressure is 110/70 mm Hg, pulse is 96/min and respirations are 22/min. The pertinent physical findings are an S3, bibasilar crackles, JVP 10 cm above the sternal angle, mild hepatomegaly, and 4+ pitting lower extremity edema. The patient is immediately treated with oxygen, intravenous furosemide, and nitrates. Which of the following markers is most likely elevated in this patient?
Ejection fraction
Mean corpuscular volume
B-type natriuretic peptide
Urine sodium
Neutrophil count
A 60-year-old Hispanic laboratory technician presents with increasing fatigue and generalized weakness for the last 2 months. He also has chronic pain in the lower back and legs when he walks. He has been smoking 2-3 packs of cigarettes daily for 30 years, and drinks alcohol almost daily. His mother has diabetes, while his father died of a stroke. Physical examination reveals pallor. There is mild hepatomegaly. The neurological examination is completely normal. Complete work-up reveals: CBC: Hemoglobin 9.8 g/L, MCV 85 fl, Platelets 226,000/mm3, Leukocyte count 6,500/mm3, Neutrophils 60%, Eosinophils 1%, Lymphocytes 29%, Lvlonocytes 10%. Chemistry panel: Serum sodium 138 mEq/L, Serum potassium 4.0 mEq/L, Bicarbonate 24 mEq/L, Blood urea nitrogen (BUN) 28 mg/dL, Serum creatinine 2.1 mg/dL, Calcium 11.2 mg/dL, Blood glucose 98 mg/dL. Liver studies: Albumin 4.0 mg/dL, Total protein, serum 9.5 g/dL, Total bilirubin 1.0 mg/dL, Direct bilirubin 0.8 mg/dL, Alkaline phosphatase 110 U/L, Aspartate aminotransferase (SGOT) 58 U/L, Alanine aminotransferase (SGPT) 25 U/L. ESR is 100 mm/h. What is the best next step in the management of this patient?
ANA and anti-Smith antibodies
Serum immunoelectrophoresis
Bone marrow biopsy
Kidney biopsy
Bone scan
A 60-year-old male complains of low back pain, which has intensified over the past 3 months. He had experienced some fever at the onset of the pain. He was treated for acute pyelonephritis about 4 months ago. Physical examination shows tenderness over the L2-3 vertebra and paraspinal muscle spasm. Laboratory data show an erythrocyte sedimentation rate of 80 mm/h and elevated C-reactive protein. Which of the following statements is correct?
Hematogenous osteomyelitis rarely involves the vertebra in adults
The most likely initial focus of infection was soft tissue
Blood cultures will be positive in most patients with this process
Surgery will be necessary if the patient has osteomyelitis
An MRI scan is both sensitive and specific in defining the process
A 60-year-old male farmer presents to the office for the evaluation of a slightly painful ulcer on the top of his lower lip. The ulcer has not healed since he first noticed it three months ago. He has always been healthy and denies any sexual activity during the past year. He is afebrile. Physical examination shows a 3x7 mm, partially encrusted ulcer in the vermilion zone near the moist line (mucocutaneous junction) of the lower lip, surrounded by a 6 x 12 mm area of induration. There are no palpable submental or submandibular lymph nodes. The remainder of the physical examination is unremarkable. Complete blood count and differential are normal. Biopsy of the ulcer will most likely to show:
Invasive clusters of spindle cells surrounded by palisaded basal cells
Granulomatous inflammation
Invasive cords of squamous cells with keratin pearls
Shallow fibrin-coated ulceration with an underlying mononuclear infiltrate
Giant cells in a Tzanck preparation
A 60-year-old male presents to the emergency room with a two-week history of low back pain and low-grade fever. His past medical history is insignificant. He tried several over-the-counter pain medications with little success. His temperature is 38.3°C (101°F), blood pressure is 120/76 mmHg, pulse is 90/min, and respirations are 16/min. Physical examination reveals percussion tenderness over the lumbar vertebrae and local paravertebral muscular spasm. Neurological examination shows 2+ deep tendon reflexes and 5/5 muscle power. The straight-leg raising test is negative at 90 degrees. Laboratory values are: Hemoglobin 12.2 g/dL, Leukocyte count 10,700/cmm, Segmented Neutrophils 63%, Bands 4%, Eosinophils 3%, Basophils 0%, Lymphocytes 23%, Monocytes 6%, Platelets 400,000/cmm, ESR 75 mm/hr. What is the next step in the management of this patient?
Plain radiograph
Bone scan
MRI of the spine
Serum rheumatoid factor
Physiotherapy
A 60-year-old male presents to your office complaining of right-sided neck pain and numbness over the posterior surface of the forearm. He had several such episodes over the last two years that responded to NSAIDs and physical therapy. Physical examination reveals limited neck rotation and lateral bending. There is decreased pinprick sensation on the posterior aspect of the right forearm, but no muscle weakness is present. Triceps reflex is normal. Which of the following is the most likely finding on the neck radiography of this patient?
Reversed lordotic curve
Bony spurs
Vertebral body osteoporosis
Osteolytic lesions
Compression fracture
A 60-year-old male who emigrated from Russia comes to you with complaints of dizziness, fatigue and weight loss. A review of systems reveals that the patient experiences daily fevers and cough. He does not use tobacco, alcohol or drugs. He does not take any medication. His blood pressure is 108/64 mmHg while standing. His respiratory rate is 14/min and is unlabored. Laboratory studies reveal the following: Chemistry panel: Serum sodium 130 mEq/L, Serum potassium 5.9 mEq/L, Chloride 102 mEq/L, Serum creatinine 0.8 mg/dL, Blood glucose 58 mg/dL. Complete blood count: Hemoglobin 10.0g/L, Platelets 430,000/mm3, Leukocyte count 4,500/mm3, NeutrophiIs 46%, Lymphocytes 45%, Eosinophils 9%. Chest x-ray shows a right upper lobe cavity. Which of the following acid-base disturbances is expected in this patient?
Normal anion gap metabolic acidosis
Metabolic alkalosis
Elevated anion gap metabolic acidosis
Respiratory acidosis
Respiratory alkalosis
A 60-year-old man comes to office with persistent complaints of malaise and easy fatigability, for the past 8 months. On examination, he appears pale. PR 93/min; BP 127/84mm Hg; Temperature 37°C (98.6°F); RR 16/min. Fecal occult blood test is negative. Further testing is ordered that include CBC, serum electrolytes and colonoscopy. The results are: WBC 7,600/mm3, Hemoglobin 8.8 gm/dl, Hematocrit 30%, RBC count 3.6 million, Platelets 211,000/mm3. RBC Indices were:MCV 65 fl, MCH 16.5 pg, MCHC 26%, Reticulocyte count 0.5%. Which one of the following is expected on iron studies in this patient? (Serum Iron, Ferritin, TIBC, Transferrin Saturation)
Low,High,Low,Lowto normal
High,Normai,High,Normal to High
Normal, Normal, Normal, Normal
Low,Low,High,Low
Low,Low,Low,Low
A 60-year-old man with a history of alcohol abuse presents to the ED with hematemesis for 1 day. He denies abdominal or chest pain. On physical examination, his eyes appear reddened which he attributes to having drunken heavily the night before (he also reveals vomiting several times after this recent binge). Vital signs are HR 115 beats per minute, BP 130/85 mm Hg, RR 18 breaths per minute, and temperature 99.5°F. Chest radiograph is unremarkable. Laboratory results reveal a WBC 10,000/μL, haemoglobin 14 mg/dL, hematocrit 40%, and platelets 210/μL. Which diagnosis is endoscopic evaluation most likely to confirm?
Esophageal varices
Boerhaave syndrome
Curling ulcer
Perforated gastric ulcer
Mallory-Weiss tear
A 60-year-old man with a history of hypertension and migraine headaches presents to the ED with a headache. He describes left-sided headache and eye pain that is associated with nausea and vomiting. The patient has a long history of migraines, but says his migraines do not usually include eye pain. On examination, his temperature is 97.6°F, HR 84 beats per minute, RR 12 breaths per minute, and BP 134/80 mm Hg. His neurologic examination is normal. His left eye is mid-dilated and nonreactive. His cornea is cloudy. His corrected visual acuity is 20/50 in the left eye and 20/20 in the right eye. What is the most appropriate next step in management?
Administer hydromorphone
Check IOP
Perform head CT scan
Check erythrocyte sedimentation rate (ESR)
Discharge patient
A 60-year-old white male is hospitalized due to an acute myocardial infarction. His other medical problems include type 2 diabetes mellitus, hypertension, chronic obstructive pulmonary disease, and degenerative joint disease. He admits to smoking 2 packs of cigarettes daily for the past 20 years, as well as drinking 2 bottles of beer daily for the past 15 years. His medications include aspirin, glyburide, metoprolol, enalapril, heparin, and albuterol and ipratropium inhalers. His blood pressure is 140/80 mmHg, pulse is 80/min, respirations are 16/min, and temperature is 36.7°C (98.0°F). During his stay in the hospital, a number of blood tests were ordered. Which of the following lab abnormalities is an indication for thyroid function testing?
Hyperlipidemia
Unexplained hypernatremia
Unexplained hypocalcemia
Thrombocytopenia
Neutropenia
A 60-year-old woman complains of dry mouth and a gritty sensation in her eyes. She states it is sometimes difficult to speak for more than a few minutes. There is no history of diabetes mellitus or neurologic disease. The patient is on no medications. On examination, the buccal mucosa appears dry and the salivary glands are enlarged bilaterally. Which of the following is the best next step in evaluation?
Schirmer test and measurement of autoantibodies
A therapeutic trial of prednisone for 1 month
Lip biopsy
Administration of a benzodiazepine
IgG antibody to mumps virus
A 60-year-old woman complains of fever and constant left lower quadrant pain of 2 days duration. She has not had vomiting or rectal bleeding. She has a history of hypertension but is otherwise healthy. She has never had similar abdominal pain, and has had no previous surgeries. Her only regular medication is lisinopril. On examination blood pressure is 150/80, pulse 110, and temperature 38.9°C (102°F). She has normal bowel sounds and left lower quadrant abdominal tenderness with rebound. A complete blood count reveals WBC = 28,000. Serum electrolytes, BUN, creatinine and liver function tests are normal. What is the next best step in evaluating this patient’s problem?
Colonoscopy
Ultrasound of the abdomen
Barium enema
CT scan of the abdomen and pelvis
Exploratory laparotomy
A 60-year-old woman with depression and poorly controlled type 2 diabetes mellitus complains of episodic vomiting over the last three months. She has constant nausea and early satiety. She vomits once or twice almost every day. In addition, she reports several months of mild abdominal discomfort that is localized to the upper abdomen and that sometimes awakens her at night. She has lost 5 lb of weight. Her diabetes has been poorly controlled (glycosylated hemoglobin recently was 9.5). Current medications are glyburide, metformin, and amitriptyline. Her physical examination is normal except for mild abdominal distention and evidence of a peripheral sensory neuropathy. Complete blood count, serum electrolytes, BUN, creatinine, and liver function tests are all normal. Gallbladder sonogram is negative for gallstones. Upper GI series and CT scan of the abdomen are normal. What is the best next step in the evaluation of this patient’s symptoms?
Barium esophagram
Scintigraphic gastric emptying study
Colonoscopy
Liver biopsy
Small bowel biopsy
A 60-year-old, obese, diabetic woman comes to the office and complains of "balance problems while walking." She also has tingling and paresthesias in her feet, decreased sensation below the knees, and burning and aching sensations in both legs. She has been very fatigued lately. The neurological examination reveals diminished proprioception peripherally on her feet, "stocking" distribution of hypesthesia from her knees distally, and positive signs of spinal ataxia. What is the best diagnostic test for this patient's condition?
Electroencephalography
Electromyography and conduction studies
Evoked potentials
Repetitive stimulation electromyography
Regular checking of blood sugar and diabetic diet
A 61-year-old man presents to your office with a two-week history of low back pain. He describes the pain as constant, dull, and aching. It is non-radiating. The pain is not affected by movement and cannot be fully relieved by lying down. He denies fever and urinary frequency or hesitancy. He has started taking sleeping pills because the pain disturbs him during the night. On physical examination, the paraspinal muscles are non-tender. Percussion over the lumbar vertebrae does not elicit tenderness. Knee reflexes are symmetric and he has 5/5 strength in the extremities bilaterally. A straight leg raise test is negative. Which of the following is the best test for this patient?
Electromyography
Urethral cultures
HLA genotyping
Prostate-specific antigen (PSA)
Abdominal ultrasonography
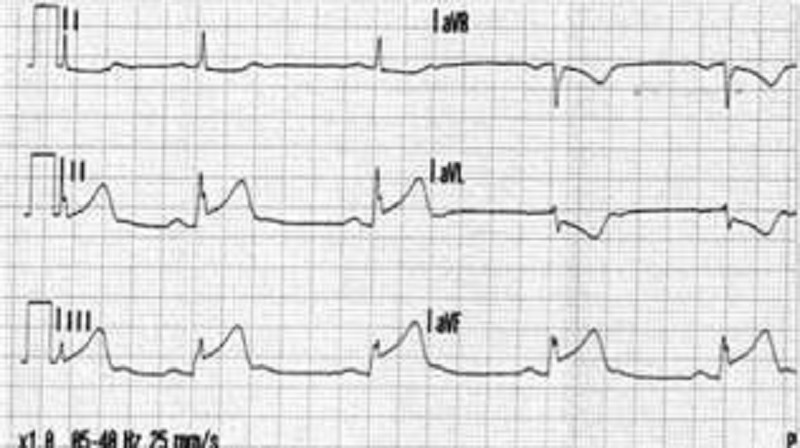
A 61-year-old woman was on her way to the grocery store when she started feeling chest pressure in the center of her chest. She became diaphoretic and felt short of breath. On arrival to the ED by EMS, her BP is 130/70 mmHg, HR is 76 beats per minute, and oxygen saturation is 98% on room air. The nurse gives her an aspirin and an ECG is performed as seen below. Which of the following best describes the location of this patient’s myocardial infarction (MI)?
Anteroseptal
Anterior
Lateral
Inferior
Posterior
A 61-year-old woman with a history of diabetes and hypertension is brought to the ED by her daughter. The patient states that she started feeling short of breath approximately 12 hours ago and then noticed a tingling sensation in the middle of her chest and became diaphoretic. An ECG reveals ST depression in leads II, III, and aVF. You believe that the patient had a non–ST-elevation MI (NSTEMI). Which of the following cardiac markers begins to rise within 3 to 6 hours of chest pain onset, peaks at 12 to 24 hours, and returns to baseline in 7 to 10 days?
Myoglobin
Creatinine kinase-MB (CK-MB)
Creatinine kinase (CK)
Troponin I
Lactic dehydrogenase (LDH)
A 62-year-old Caucasian female complains of difficulty swallowing solid food. She needs to take sips of water during every meal to help with swallowing. Her past medical history is significant for hypertension controlled with metoprolol. She uses some over-the-counter eye drops for eye dryness. Her blood pressure is 140/90 mmHg and heart rate is 60/min. Physical examination reveals prominent dental caries. There are bilateral firm submandibular swellings present on neck palpation. Which of the following is the best test to confirm this patient's diagnosis?
Antibodies to Ro/SSA
Barium swallow test
Antimitochondrial antibodies
CT scan of the neck
Esophageal endoscopy with biopsy
A 62-year-old man comes to the office and complains of increasing fatigue and weakness for the last 4 months. He also describes a dull pain in his back and arms, which gets worse with walking. He denies any numbness or paresthesia. On examination, he appears pale. There is tenderness around the lumbar spine. CBC reveals: WBC 8,600 mm3 with normal differential, Hemoglobin 8.6 g/dl, Hematocrit 27%, Platelets 164,000 mm3. The RBC morphology is significant for a rouleaux appearance. The ESR is 55mm/hr. Bence Jones proteins are identified in the urine. Which of the following is expected in this patient's bone marrow examination?
Over proliferation of plasma cells
Increased marrow cellularity with megakaryocytic hyperplasia
Normocellular bone marrow
Hypocellular and fibrotic bone marrow
Hypoplastic fat- filled marrow with no abnormal cells
A 62-year-old man complains of right knee pain. He says that the pain started two days ago and has been limiting his daily activities. He required 2 grams of acetaminophen in order to sleep through the previous night. He has a long history of rheumatoid arthritis treated with daily low-dose prednisone. Physical examination reveals swelling, limited flexion, and tenderness to palpation of the right knee. Synovial fluid aspiration is performed. Which of the following synovial fluid characteristics would warrant immediate surgical intervention?
High viscosity
Negatively birefringent crystals
15,000 neutrophils per mcl
1500 W BC per mcl
Positive rheumatoid factor
A 62-year-old man has been noticing progressive difficulty swallowing, first solid food and now liquids as well. A barium study shows a ragged narrowing just below the carinal level. Endoscopic biopsy confirms squamous cell carcinoma. Which of the following provides the most accurate information regarding the T stage of an esophageal carcinoma?
Computed tomography
Magnetic resonance imaging
Positron emission tomography
Endoscopic ultrasound
Bronchoscopy
A 62-year-old man reports an episode of gross, painless hematuria. There is no history of trauma, and further questioning determines that he had total hematuria, rather than initial or terminal hematuria. The man does not smoke and has had no other symptoms referable to the urinary tract. He has no known allergies. Physical examination, including rectal examination, is unremarkable. His serum creatinine is 0.8 mg/dL, and, except for the presence of many red cells, his urinalysis is normal and shows no red cell casts. His hematocrit is 46%. Which of the following is the most appropriate initial step in the workup?
Intravenous pyelogram (IVP) and cystoscopy
Sonogram and CT scan of both kidneys
Coagulation studies and urinary cultures
Retrograde cystogram and pyelograms
PSA determination and prostatic biopsies
A 62-year-old man with alcoholic cirrhosis of the Uver and ascites presents with generalized abdominal pain that started 12 hours ago. He now has moderate tenderness over the entire abdomen, with minimal guarding and equivocal rebound. Bowel sounds are diminished but present. He has a temperature of 38.4 C (101.2 F) and a leukocyte count of 11,000/mm3. Although he used to be a heavy drinker, he has not touched a drop of alcohol for the past 7 years. Except for the presence of ascites, upright and flat x-ray films of the abdomen are unremarkable. Which of the following is the most appropriate next step in diagnosis?
CT scan of the abdomen
Sonogram of the right upper quadrant
Serum amylase determinations
Culture of the ascitic fluid
Laparoscopy
A 62-year-old man with coronary artery disease (CAD) presents with presyncope. His physical examination is normal except for bradycardia (pulse 56 beats/min) and an irregular pulse. The electrocardiogram (ECG) shows Wenckebach’s type atrioventricular (AV) block. Which of the following are you most likely to see on the ECG?
Progressive PR shortening
Dropped beat after PR lengthening
Progressive lengthening of the PR interval
Fixed 2:1 block
Tachycardia
A 62-year-old woman has an eczematoid lesion in the areola of her right breast that has been present for 3 months. She has self-medicated with skin lotions and over-the-counter steroid ointments, but the area has not improved. On physical examination, the nipple is inverted, the skin of the areola is reddish and desquamated, and the entire area feels firm, with no discrete mass demarcated from the rest of the breast. Which of the following is the most appropriate next step in management?
Mammogram and punch biopsies
Skin scrapings, culture, and appropriate topical antibiotic
Estrogen cream and systemic estrogen replacement
Mammogram and galactogram
Serum levels of glucagon and CT of the pancreas
A 62-year-old woman is transferred to the medical service with an appendiceal mass serendipitously picked up at the edge of an x-ray taken of a broken femur in the emergency department. Otherwise, the patient has no significant past medical history and no current symptoms. Which of the following studies is most likely to be useful?
Arterial blood gas
Immediate ECG
CT of the chest and abdomen
MRI of the chest and abdomen
Room air oxygen saturation
A 62-year-old, right-handed man has transient episodes of paralysis of the right arm and inability to express himself. There is no associated headache. The episodes have sudden onset, last about 5-10 minutes, and leave no neurologic sequela. The patient is overweight and sedentary. He smokes one pack of cigarettes per day and has high cholesterol, but he is not hypertensive. The only abnormality in the physical examination is a bruit over the left carotid bifurcation. Which of the following is the most appropriate initial step in diagnosis?
CT scan of the head
Duplex scanning of the carotids
Echocardiogram
MRI of the brain
Aortic arch arteriogram
A 63-year-old man presents with a 2-month history of dysphagia for both solids and liquids. He has had a 6.6 lb (3kg) weight loss over this time. His past medical history is remarkable for a transient ischemic attack 6 months ago, two bouts of pneumonia in the past 3 months, and chronic heartburn treated with over-the-counter antacids. Physical examination shows a supple neck without masses. Abdominal examination shows mild epigastric tenderness to deep palpation. Chest x-ray is normal for his age. Which of the following is the most appropriate next step in diagnosis?
Endoscopy
Barium swallow
Motility studies
Video fluoroscopy
24-hour pH monitoring
A 63-year-old man with a long history of alcohol abuse presents with ascites. He is experiencing mild abdominal discomfort and nausea. Examination reveals tense ascites and generalized tenderness but no rigidity. A diagnostic paracentesis of the fluid is performed. Which of the following ascitic fluid results is most likely to suggest an uncomplicated ascites due to portal hypertension from cirrhosis?
Hemorrhage
Serum to ascites albumin gradient >1.1 g/dL
Bilirubin level twice that of serum
More than 1000 white cells/mm3
Protein >25 g/L
A 63-year-old man with diabetes is called by his primary care physician because of abnormal liver fun
CT scan of the abdomen
Fasting transferrin saturation levels
Blood smear
Liver biopsy
Endoscopic retrograde cholangiopancreatography
A 63-year-old woman is seen in the emergency room with acute shortness of breath. There is no history of heart or lung problems in the past. She was recently diagnosed with breast cancer and is undergoing active treatment. On examination, her blood pressure is 120/80 mm Hg, pulse 100/min, and heart and lungs are normal. There are no clinical signs of deep venous thrombosis (DVT). Which of the following investigations is most likely to rule out a pulmonary embolism (PE)?
Normal CXR
Normal ventilation scan
Normal electrocardiogram (ECG)
Normal ventilation-perfusion lung scan
Normal magnetic resonance image (MRI)
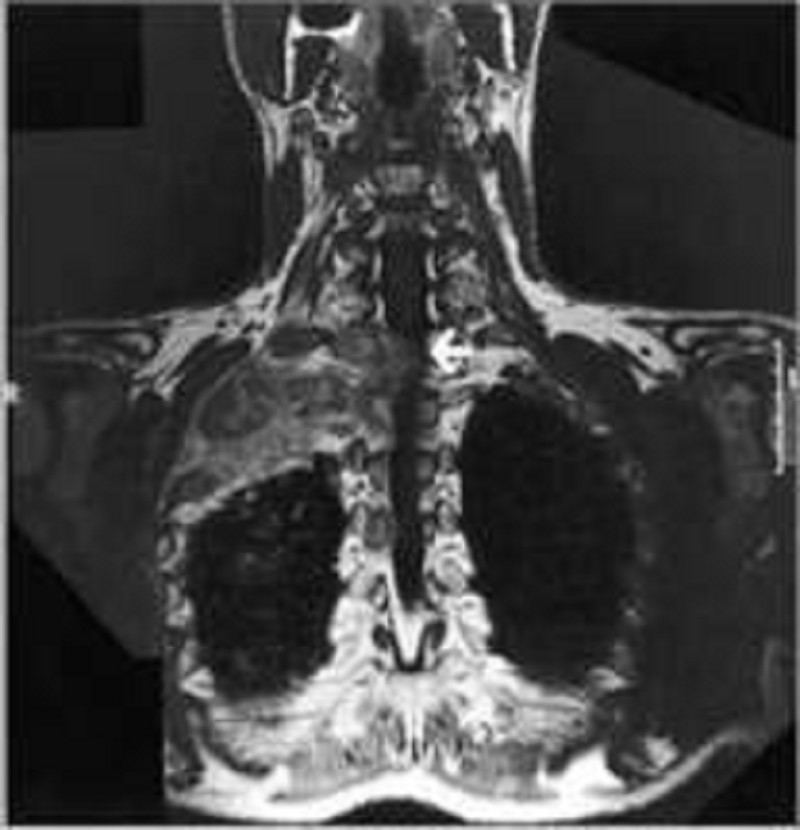
A 64-year -old African American male presents to you with complaints of a dry cough, weight loss and pain in his right arm. The symptoms started approximately 2 months ago. His past medical history is significant for type 2 diabetes mellitus and hypertension. He smokes 1 pack per day and drinks alcohol occasionally. He denies any drug allergies. Physical examination is unremarkable. ECG reveals normal sinus rhythm. An MRI of his chest is shown below. Which of the following is most likely responsible for this patient's symptoms?
Aspergilloma
Superior sulcus tumor
Cryptogenic organizing pneumonia
Lung abscess
Bronchial carcinoid
A 64-year-old diabetic with a long history of uncontrolled hypertension is admitted for chest pain. ECG reveals elevated ST segments in the anterior wall leads. Cardiac enzymes are elevated and the patient is admitted to the ICU for supportive care. He receives low molecular weight heparin and is placed on a nitroglycerin drip. He continues to have chest pain and requires intravenous morphine. Three days later, the patient is transferred to the floor and he remains on bed rest. During the night the nurse on call informs you that the patient has a cold leg. On examination, the left leg is cold and there are no distal pulses. There is minimal swelling and the leg appears mottled. Emergency vascular surgery consult was placed and the appropriate treatment was given. Which of the following should also be considered in this patient?
Venous duplex study
Chest x-ray
Echocardiogram
V/Q scan
D-dimer level
A 64-year-old man presents to the emergency department after a motor vehicle crash and receives a CT of the abdomen that shows a finding of a unilateral mass in the left adrenal gland. He is unharmed from the accident, feels well, and has never smoked. His blood pressure is 155/90 mmHg, deep tendon reflexes are 3/4, and muscle strength is 4/5. Laboratory studies show: Na+: 150 mEq/L, K+: 3.0 mEq/L, Cl−: 105 mEq/L, HCO −: 36 mEq/L. Plasma renin activity is also decreased. Which of the following is most likely to be increased?
Aldosterone
Anion gap
Carcinoembryonic antigen
Prostate-specific antigen
Troponin
A 64-year-old man presents with symptoms of malaise, shortness of breath, edema, and no urine output for 24 hours. His past medical history is not significant, and his only medication is daily aspirin. On examination his JVP is 4 cm, heart sounds are normal, lungs are clear, and the abdomen is soft. A Foley catheter is inserted into his bladder for 200 cc of urine, which is sent for urinalysis. His urine output still remains low. Which of the following is the most appropriate initial diagnostic test?
Renal ultrasound
Renal venogram blood urea nitrogen (BUN)/creatinine ratio
Blood cultures
Urine cultures
Inferior vena cavagram with selective
A 64-year-old white man with type 2 diabetes mellitus presents to the emergency department after “passing out.” While climbing the stairs, he felt dyspneic and lost consciousness as he reached the top. Before the event he experienced no palpitations or change in vision. When he awoke he felt alert and called for help immediately. He reports dyspnea on exertion for the past year. He has no history of chest pain, seizures, or recent illnesses. Medications include calcium and vitamin D supplements, glyburide, and synthroid. He is allergic to penicillin. Family history is noncontributory. He drinks wine socially and does not smoke or use illicit substances. His blood pressure is 136/92 mmHg, heart rate is 88/min, respiratory rate is 14/min, and temperature is 36.5°C (97.7°F). Physical examination reveals a systolic crescendodecrescendo murmur best heard in the second right intercostal space with a soft S2. ECG shows nonspecific ST-segment changes and left ventricular hypertrophy with a normal heart rate and rhythm. Which of the following interventions will most likely reveal the cause of this syncopal event?
ECG
Sublingual nitroglycerin and serial cardiac enzymes
Echocardiography
Electroencephalography
Exercise stress test with echocardiogram
A 64-year-old woman comes to the hospital due to an "irritating sore throat for 3 months." She admits to smoking 1 pack of cigarettes daily for the past 29 years, and continues to smoke. She was jailed twice for driving under the influence of alcohol, and went to Alcohol Rehabilitation last year. She currently denies any alcohol intake. She has no fever or any other complaints. She had a complete hysterectomy several years ago for symptomatic fibroids. Her vital signs are stable. Physical examination reveals a 1.5-cm right cervical lymph node. The rest of the examination is normal. Biopsy of the lymph node reveals metastatic squamous cell carcinoma. The CT scan of the chest is negative. What is the best next step in the management of this patient?
Empirical chemotherapy
Repeat CT in 3 months
Pan-endoscopy
Screening mammogram
Radical neck dissection
A 65-year-old Asian male presents to the physician with a four-week history of weakness and vague postprandial epigastric pain. His past medical history is insignificant. He does not take any medications. He smokes 1½packs of cigarettes daily and drinks alcohol occasionally. The fecal occult blood test is positive. Gastroduodenoscopy shows an antral ulcer. Four of seven biopsies taken from the margins of the ulcer are consistent with adenocarcinoma. Which of the following is the most appropriate next step in management?
Helicobacter pylori testing
Serologic markers
A CT scan
Laparoscopy
Exploratory laparotomy
A 65-year-old black female presents for an annual examination. Physical examination is unremarkable for her age. In completing the appropriate screening tests, you order a dual x-ray absorptiometry (DXA) to evaluate whether the patient has osteoporosis. DXA results reveal a T-score of -3.0 at the total hip and −2.7 at the spine, consistent with a diagnosis of osteoporosis. Since her Z-score is -2.0, you proceed with an initial evaluation of secondary osteoporosis. Laboratory evaluation reveals: Calcium: 9.7 mg/dL, Cr: 1.0 mg/dL, Bun: 19 mg/d, Glucose: 98 mg/dL, 25, OH vitamin D: 12 ng/mL (optimal > 25), WBC: 7700/μL, Hg: 12 g/dL, HCT: 38 g/dL, PLT: 255,000/μL. Based on the above information, additional laboratory would most likely reveal which of the following?
Elevated iPTH (intact parathormone), low ionized calcium, normal alkaline phosphatase
Normal iPTH, normal ionized calcium, elevated alkaline phosphatase
Elevated iPTH, low ionized calcium, normal alkaline phosphatase
Normal iPTH, low ionized calcium, elevated alkaline phosphatase
Elevated iPTH, normal ionized calcium, elevated alkaline phosphatase
A 65-year-old Caucasian male comes to the physician because of shortness of breath, fever, and a productive cough for the last four days. He is a chronic smoker and alcoholic. He quit smoking two years ago. His medical problems include hypertension, chronic obstructive pulmonary disease, paroxysmal atrial fibrillation, and coronary artery disease. He is taking daily-inhaled ipratropium bromide, albuterol, metformin, metoprolol, warfarin, and diltiazem. His temperature is 38.9°C (102°F), blood pressure is 140/88 mmHg, pulse is 110/min, and respirations are 28/min. Pulse oximetry showed 88% on room air. Examination shows decreased breath sounds and crackles over the right lower lobe of the lung. Which of the following is the most appropriate next step in his management?
Bronchoscopy
Sputum gram stain
Chest x-ray
Mycoplasma serology
Sputum culture
A 65-year-old female undergoes total right hip replacement after fracturing the neck of her femur. There are no surgical complications, and afterwards she is started on enoxaparin (low molecular weight heparin) for deep venous thrombosis prophylaxis. On the third postoperative day, she suddenly becomes anxious and complains of right sided chest pain and shortness of breath. She has a history of hypertension, diabetes and hyperlipidemia. She has a 20 pack-year smoking history, but quit 10 years ago. On exam, her temperature is 37.2°C (98.9°F), blood pressure is 126/76 mm Hg, pulse is 110/min and respirations are 30/min. Her oxygen saturation is 88% on room air. She is diaphoretic but her chest is clear to auscultation. A portable chest x-ray shows no abnormalities. EKG reveals sinus tachycardia and non-specific ST/T-wave changes. Which of the following studies would most likely reveal the diagnosis?
Serial cardiac enzymes
Echocardiogram
Helical CT pulmonary angiography
Arterial blood gas analysis
B-type natriuretic peptide levels
A 65-year-old G3P3 presents to your office for annual checkup. She had her last well-woman examination 20 years before when she had a hysterectomy for fibroids. She denies any medical problems, except some occasional stiffness in her joints early in the morning. She takes a multivitamin daily. Her family history is significant for cardiac disease in both her parents and breast cancer in a maternal aunt at the age of 42 years. Her physical examination is normal. Which of the following is the most appropriate set of laboratory tests to order for this patient?
Lipid profile, fasting blood sugar, TSH, and urinalysis
Lipid profile, fasting blood sugar, TSH, urinalysis, and CA-125
Lipid profile, fasting blood sugar, TSH, and CA-125
Lipid profile and fasting blood sugar
Lipid profile, fasting blood sugar, and TSH

A 65-year-old male comes to the office on a hot summer afternoon. He complains of blisters and intense itching all over his body for the past 2 days. He has been having "itchy red swelling all over" for the past 2 months, which he thinks is due to the summer heat. His pulse is 82/min, blood pressure is 140/80 mmHg, respirations are 14/min, and temperature is 36.8°C (98.4°F). On examination, lesions are seen on both normal and erythematous skin over flexural areas of the groin, axilla and legs. An image of one of these lesions is shown below. Which of the following is most likely seen with this patient's condition?
IgG and C3 deposits at the dermal-epidermal junction
Intradermal edema with leukocyte infiltration
C3 at the basement membrane zone
IgG deposits in a linear band at the dermal-epidermal junction
IgG deposits intercellularly in the epidermis
A 65-year-old male is brought by his wife to the emergency department because of a very high fever. He has also had a cough productive of greenish, nonbloody sputum for the past two days. He is diabetic, and had pneumonia 3 months ago. He has been smoking one pack of cigarettes daily for 27 years. His temperature is 38.4° C (101.2°F), blood pressure is 118/74 mm Hg, pulse is 98/min, and respirations are 24/min. Physical examination reveals cervical lymphadenopathy, and some scattered rales are heard on the right lung base. Chest-x ray shows a right lower lobe infiltrate. Laboratory studies reveal: Hb 12.6 gm/dL, WBC 40,000/cmm, Platelets 190,000/cmm. Peripheral smear: Segmented neutrophils 10%, Bands 4%, Lymphocytes 85%, Monocytes 1%. Some variant lymphocytes, and smudge cells are seen on the peripheral smear. What is the most appropriate way to confirm the diagnosis of this patient?
Epstein Barr virus serology
Bone marrow biopsy
Lymph node biopsy
Cytogenetic analysis
Lung biopsy
A 65-year-old man comes to the physician because of increased urinary frequency and urgency, as well as suprapubic discomfort His temperature is 37C(98.6F), blood pressure is 130/75 mm Hg, pulse is 76/min, and respirations are 14/min. Rectal examination shows prostatic induration; physical examination otherwise shows no abnormalities. Urinalysis shows no abnormalities. Expressed prostatic secretions show a leukocyte count of 20 WBCs/HPF (normal is less than 10 WBCs/HPF). They are sent for culture and sensitivity, and fail to grow any bacteria. Serum prostatic specific antigen is 2 ng/ml (normal value is less than 4ng/ml). A diagnosis of nonbacterial prostatitis is suggested. Which of the following is the most appropriate next step in management?
Repeat urinalysis
Treatment with oral erythromycin
Perform urinary cytology and cystoscopy
Treatment with oral trimethoprim-sulphamethoxazole
Repeat culture of prostatic secretions
A 65-year-old man comes to the physician for a health maintenance examination. Which of the following screening methods would allow the highest detection rate of prostatic carcinoma in early stages?
Digital rectal examination alone
Serum PSA and digital rectal examination
Cytologic examination of prostatic secretion
Transrectal ultrasonography
Serum PSA determination alone
A 65-year-old man comes to the physician four years after suffering a burn injury to his entire right leg. One area of the leg never healed and has now started increasing in size. He has constant pain and drainage from the site of the lesion. Several topical creams and antibiotics have not helped. Biopsy of the lesion is attempted. Which of the following is most likely be identified on biopsy?
Malignant melanoma
Squamous cell carcinoma
Basal cell carcinoma
Dysplastic nevus
Actinic keratosis
A 65-year-old man develops the onset of severe knee pain over 24 hours. The knee is red, swollen, and tender. He has a history of diabetes mellitus and cardiomyopathy. An x-ray of the knee shows linear calcification. Definitive diagnosis is best made by which of the following?
Arthrocentesis and identification of positively birefringent rhomboid crystals
Rheumatoid factor
Serum uric acid
Serum calcium
ANA
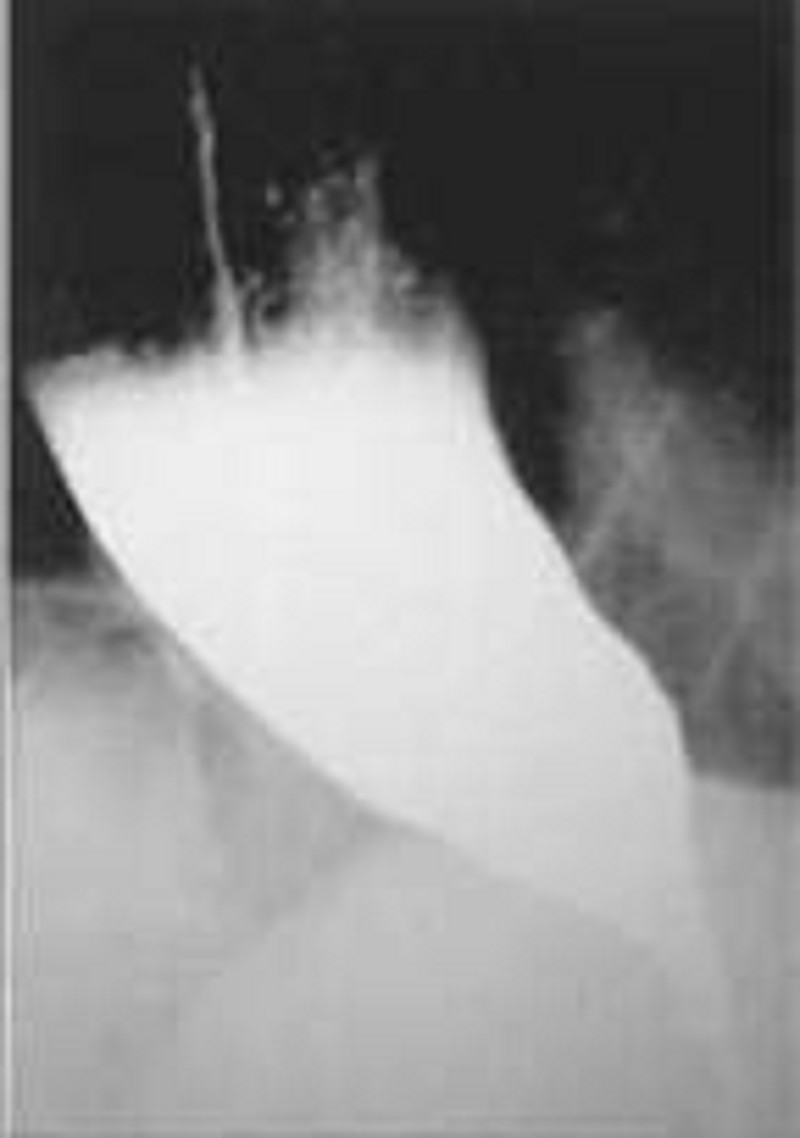
A 65-year-old man presents to his physician complaining of difficulty swallowing, occasional chest pain, and regurgitation of food. Over the past 2 months he has lost about 7 kg (15 lb). Results of a barium swallow study are shown in the image. What test should be performed to look for possible causes of his condition?
24-hour pH monitoring
Serum gastrin level measurement
Upper endoscopy
Urease breath test
Esophageal manometry
A 65-year-old man presents to the physician’s office for his yearly examination. His past history is pertinent for a 40 pack-year smoking history and colon cancer 3 years ago for which he underwent a sigmoid colectomy. The most recent colonoscopic follow-up 3 months ago was negative. His physical examination is normal. Laboratory results show a normal CBC and electrolytes, markedly elevated cholesterol, and a CEA of 12 compared to values of less than 5 obtained every 6 months since colectomy. A repeat CEA 4 week later was 15, and liver fun
Positron emission tomography (PET) scan
Radionuclide liver scan
Ultrasound
CT scan
MRI scan
A 65-year-old man presents to your office complaining of progressive breathing difficulty. His past medical history is significant for hypertension, diabetes mellitus, type 2, and myocardial infarction experienced two years ago. His current medications are hydrochlorothiazide, atenolol, glipizide, and aspirin. He does not smoke or consume alcohol. His vital signs are BP 156/96 mmHg, PR 65/min, RR 18/min, T 36.7°C (98°F). Physical examination shows mild symmetric edema of the lower extremities. Hepatojugular reflex is positive. Point of maximal impulse is displaced downward and to the left. Soft blowing systolic murmur is heard on the apex. Breath sounds are diminished on the right side. Serum protein level is 6.5 g/dl and serum LDH is 200 mg/ml. After taking a chest radiograph, you suspect pleural effusion on the right and decide to perform diagnostic thoracocentesis. Which of the following findings, on pleural fluid analysis, is most consistent with this patient's condition?
LDH level of 180 mg/ml
Protein level of 5.0 g/dl
Glucose 60 mg/dl
PH of 7.35
High amylase level
A 65-year-old man presents with acute onset of pain, swelling, and erythema of the left knee. He denies previous episodes or trauma to the knee. The differential diagnosis includes septic arthritis and gout. Which of the following is the best study to differentiate between gout and septic arthritis?
X-ray of the knee
Bone scan
White blood cell count
Evaluation of synovial fluid aspirate
Magnetic resonance imaging (MRI) of the knee
A 65-year-old man presents with right shoulder pain and weakness after falling on his outstretched hand. The pain is worse when he tries to position his arm above the shoulder level or when he pulls or pushes. He also complains of pain when he lies on the affected shoulder. He has a 40-pack-year history of cigarette smoking. His father died of multiple myeloma. His vital signs are within normal limits. Examination shows limitation of mid arc abduction and external rotation that does not improve after lidocaine injection. There is no swelling, redness or warmth of the joint. Radial pulse is normal. Muscle tone and bulk is within normal limits. Which of the following would be most helpful in confirming the patient's diagnosis?
X-ray shoulder
Chest-X ray
Bone marrow biopsy
MRI of the shoulder
MRI of the cervical spine
A 65-year-old man who had a 25-lb weight loss over the previous 6 months is diagnosed with adenocarcinoma of the distal esophagus. He undergoes a transhiatal esophagectomy complicated by a cervical leak. He is receiving enteral feeds through a jejunostomy tube. After a week, his physicians wish to assess his nutritional resuscitation. Which of the following is the most accurate measure of adequacy of his nutritional support?
Urinary nitrogen excretion level
Serum albumin level
Total serum protein level
Serum transferrin level
Respiratory quotient
A 65-year-old woman comes to the physician because of a two-month history of fatigue and weight gain. She has rheumatoid arthritis and hypertension. She takes hydrochlorothiazide and naproxen. She does not use tobacco, alcohol, or drugs. Her blood pressure is 120/70 mm Hg, pulse is 80/min, and respirations are 14/min. Physical examination shows generalized edema; liver is palpated 2 cm below the costal margin. Urinalysis shows 4+ proteinuria. Ultrasound of the kidneys shows slight enlargement. Renal biopsy was performed. Which of the following is the most likely finding on renal specimen analysis?
Crescent formation on light microscopy
Linear immunoglobulin deposits revealed on immunofluorescence microscopy
Deposits revealed under polarized light
Granular immunoglobulin deposits revealed on immunofluorescence microscopy
Normal light microscopy findings
A 65-year-old woman presents to the physician’s office for a second opinion on the management options for recently diagnosed breast cancer. She presents with a 2.5-cm mass in the upper outer quadrant of the left breast associated with a palpable axillary node suspicious for metastatic disease. The remainder of her examination is normal. Mammography demonstrates the cancer and shows no other suspicious lesions in either breast. Chest x-ray, bone scan, and blood test panel, including liver fun
Yes, and if the SLN is negative, then an axillary dissection can be avoided
No, because the success of SLN biopsy in patients over age 60 is decreased
Yes, and if the SLN if positive, then a complete axillary dissection should be performed
No, because SLN biopsy is contraindicated when a palpable axillary node is suspicious for metastatic disease
No, because SLN biopsy is contraindicated for tumors greater than 2 cm

A 65-year-old woman presents to the physician’s office for her yearly physical examination. She has no complaints except for a recent 10-lb weight loss. Past history is pertinent for a 40 pack-year smoking history, hypertension, asthma, and hypothyroidism. Examination reveals a thin woman with normal vital signs and unremarkable heart and abdominal examinations. Lung examination reveals mild wheezing and a few bibasilar rales. A chest x-ray is obtained and is shown in Figure 6-13. A chest x-ray obtained 3 years ago was normal. Yearly laboratory tests including a CBC, electrolytes, and lipid panels are normal. Which of the following is the most appropriate next diagnostic test?
Percutaneous needle biopsy
CT scan
Pulmonary function tests
Mediastinoscopy
Bronchoscopy

A 65-year-old woman presents to the physician’s office with a 6-month history of epigastric discomfort, poor appetite, and 10-lb weight loss. Past history is pertinent for hypertension, diabetes, a 30 pack-year smoking history, and occasional alcohol intake. Examination is unremarkable except for mild epigastric tenderness to deep palpation. An abdominal ultrasound reveals cholelithiasis, and one view of a UGI x-ray series is shown in Figure 6-8. Which of the following is the most appropriate next step in management?
H2 blockers with re-evaluation by UGI in 6 month
Vagotomy and pyloroplasty
Total gastrectomy
Endoscopy
CT scan
A 65-year-old woman presents with a 2-month history of fatigue and dyspnea on exertion. She takes no medication. Her temperature is 36.7°C (98°F), blood pressure is 162/83 mmHg, pulse is 100/min, and respirations are 21/min. Auscultation shows a 2/6 systolic murmur in the 2nd right intercostal space. No peripheral edema is noted. Rectal examination shows no abnormalities. Test of the stool for occult blood is negative. EKG shows sinus tachycardia and non-specific ST-T changes. Laboratory studies show: Hemoglobin 8.1 g/L, MCV 73 fl, Platelets 360,000/mm3, Leukocyte count 4,500/mm3, Neutrophils 56%, Eosinophils 1%, Lymphocytes 33%, Monocytes 10%. Which of the following is the most appropriate next step in management?
Echocardiography
Gastro-duodenoscopy
Bone marrow biopsy
Colonoscopy
Isotope-labeled erythrocytes scintigraphy
A 66-year-old man presents to the office for a well visit. He has no complaints and feels well. His wife has been complaining that his belly has been increasing in girth over the past year. His vital sign is stable. What is the best next step in the management of this patient?
Abdominal radiography
Magnetic resonance imaging (MRI) of the abdomen
Angiography
Ultrasonography
Computed tomography (CT) scan of the abdomen
A 66-year-old man presents with progressive jaundice, which he first noticed 6 weeks ago. He has a total bilirubin of 22 mg/dL, with a direct (conjugated) bilirubin of 16 mg/dL. His transaminases are minimally elevated, whereas his alkaline phosphatase is about six times the upper limit of normal. A sonogram shows dilated intrahepatic ducts, dilated extrahepatic ducts, and a much distended, thin-walled gallbladder without stones. Which of the following is the most appropriate next step in diagnosis?
Endoscopic retrograde cholangiopancreatography (ERCP)
Percutaneous transhepatic cholangiogram (PTC)
CT scan of the upper abdomen
Serologies to define the type of hepatitis
Exploratory laparotomy
A 66-year-old man returns to the emergency department (ED) for a second time because of persistent left lower quadrant pain and developing fever, despite 48 hours of oral antibiotics. He had presented to the ED 2 days ago because of left lower quadrant pain. He was able to tolerate a diet and had no fever; he was then sent home on antibiotics, and instructed to return if there was no improvement. He has a 2-week history of constipation without regular bowel movements. Laxatives have not relieved his symptoms. His diet consists of meat with very few vegetables. His vital signs are within normal limits, except for a low-grade fever. Abdominal examination shows left lower quadrant tenderness and guarding. Rectal examination shows no abnormalities. Laboratory studies show a WBC of 16,400/cmm. He is admitted and started on IV antibiotics. Forty-eight hours later, his symptoms persist without any improvement. Which of the following is the most appropriate next step in management?
Abdominal x-rays
Flexible sigmoidoscopy
Colonoscopy
CT scan
Barium enema
A 66-year-old woman presents with severe right lower extremity claudication. Surgery is considered, but her hypertension, smoking, and diabetes puts her at risk for associated coronary heart disease. What test is most predictive of postoperative ischemic cardiac events following surgery?
Exercise stress testing
Dipyridamole-thallium imaging
Electrocardiography (ECG)
Coronary angiography
Transesophageal echocardiography
A 67-year-old male presents to your clinic to establish primary care; he is asymptomatic. He has a history of hypertension for which he takes hydrochlorothiazide. His father had a myocardial infarction at age 62. The patient smoked until 5 years ago, but has been abstinent from tobacco since then. His blood pressure in the office today is 132/78 mmHg. Aside from being overweight, the remainder of the physical examination is unremarkable. Which of the following preventive health interventions would be most appropriately offered to him today?
Abdominal ultrasound to evaluate for aortic aneurysm
Lipoprotein assay to evaluate coronary heart disease risk
Carotid ultrasound to evaluate for carotid artery stenosis
Exercise (treadmill) stress testing to evaluate for coronary artery disease
Homocysteine level to evaluate coronary heart disease risk
A 67-year-old male presents to your office after community ultrasound screening revealed an aortic aneurysm measuring 3.0 x 3.5 cm. Physical examination confirms a palpable, pulsatile, nontender abdominal mass just above the umbilicus. The patient’s medical conditions include hypertension, hyperlipidemia, and tobacco use. What is the best recommendation for the patient to consider?
Watchful waiting is the best course until the first onset of abdominal pain
Surgery is indicated except for the excess operative risk represented by the patient’s risk factors
Serial follow-up with ultrasound, CT, or MRI is indicated, with the major determinant for surgery being aneurysmal size greater than 5 to 6 cm
Serial follow-up with ultrasound, CT, or MRI is indicated, with the major determinant for surgery being involvement of a renal artery
Unlike stents in coronary artery disease, endovascular stent grafts have proven unsuccessful in the management of AAAs
A 68-year-old Caucasian male complains of right-sided leg pain over the last year. The pain is poorly controlled with over-the-counter pain medications. He also complains of frequent headaches. His past medical history is significant for hypertension and recent hearing loss. An X-ray of the skull shows areas of bone resorption and sclerosis. Which of the following are the most likely findings on laboratory work-up? (Serum calcium, serum phosphate, alkaline phosphatase, Urinary hydroxyproline)
Normal Normal Normal High
High Low High Normal
Normal Normal High High
High Normal Normal Normal
Low High Normal Normal
A 68-year-old Caucasian male presents to the emergency room with a three-week history of progressive dyspnea, orthopnea, and lower extremity edema. His past medical history is significant for hypertension, type 2 diabetes mellitus, myocardial infarction experienced eight years ago, and congestive heart failure. His current medications include metoprolol, digoxin, enalapril, furosemide, spironolactone, and aspirin. His blood pressure is 145/90 mmHg, and heart rate is 75/min. Symmetric 2+ pitting edema of the lower extremities is present. Point of maximal impulse is displaced to the left and soft holosystolic murmur is heard on the apex. Bilateral crackles are present over the lower lobes. His laboratory values are: Hemoglobin 11.0 g/dl, Leukocyte count 7 ,500/cmm, Platelets 300,000/cmm, Serum sodium 128 mEq/L, Serum potassium 5.3 mEq/L, Serum calcium 9.0 mg/dl, Serum phosphorus 4.0 mg/dl, Serum creatinine 1.9 mg/dl. ECG does not reveal acute ischemic changes. Which of the following is most likely correct concerning this patient's condition?
Serum norepinephrine level is low
The combination of furosemide and enalapril is the cause of hyperkalemia
Increasing sodium intake will help to control the electrolyte abnormalities
Increasing the dose of digitalis may be indicated
Hyponatremia indicates severe heart failure
A 68-year-old female is admitted with a broken hip after a fall. She undergoes a left hip replacement, which was uneventful. After spending two days in bed, she undergoes partial non-weight bearing physiotherapy. Five days later, she has developed shortness of breath and a swollen leg. A deep vein thrombosis is discovered. An arterial blood gas evaluation is done for suspected pulmonary embolism. What is the most consistent finding of pulmonary embolism?
Elevated PaCO2
Right axis deviation on ECG
Decreased A-a gradient
Decreased PO2
Pulmonary infarction
A 68-year-old man complains of several blisters arising over the back and trunk for the preceding 2 weeks. He takes no medications and has not noted systemic symptoms such as fever, sore throat, weight loss, or fatigue. The general physical examination is normal. The oral mucosa and the lips are normal. Several 2 to 3 cm bullae are present over the trunk and back. A few excoriations where the blisters have ruptured are present. The remainder of the skin is normal, without erythema or scale. What is the best diagnostic approach at this time?
CT scan of the chest and abdomen looking for occult malignancy
Combination of oral H1 and H2 antihistamines
Biopsy of the edge of a bulla with some surrounding intact skin
Culture of vesicular fluid for herpes viruses
Trial of corticosteroids
A 68-year-old man is admitted to the coronary care unit with an acute myocardial infarction. His postinfarction course is marked by congestive heart failure and intermittent hypotension. On the fourth day in hospital, he develops severe midabdominal pain. On physical examination, blood pressure is 90/60 mm Hg and pulse is 110 beats per minute and regular; the abdomen is soft with mild generalized tenderness and distention. Bowel sounds are hypoactive; stool Hematest is positive. Which of the following is the most appropriate next step in this patient’s management?
Barium enema
Upper gastrointestinal series
Angiography
Ultrasonography
Celiotomy
A 68-year-old man is brought to the emergency room after he passed out for one minute during an early morning jog. He was not confused after the episode and did not have bowel or bladder incontinence. He has been having exertional chest pain and shortness of breath for the past few months. He has never had any resting chest pain. He has been healthy except for hypertension, for which he takes hydrochlorothiazide. He has a 20 pack year smoking history and occasionally drinks a glass of wine. His blood pressure is 142/90 mm Hg, pulse is 80/min, and respirations are 16/min. Carotid pulse is delayed S2 is weak and an S4 is present. A grade 3/6 systolic ejection murmur is in the right 2nd intercostal space, radiating to the carotids. Neurological examination reveals no focal findings, and there are no signs of head trauma. An EKG shows left ventricular hypertrophy. The first set of cardiac enzymes is negative. Which of the following is the most appropriate next step in management?
CT scan of the head
Electroencephalogram (EEG)
Exercise stress test
Echocardiogram
CT angiogram of the chest
A 68-year-old man is diagnosed with lung cancer. In preparation for pulmonary resection he undergoes pulmonary fun
Carbon monoxide diffusing capacity (DLCO) less than 40%
Low FEV1/FVC (forced vital capacity)
Forced expiratory volume in 1 second (FEV1) more than 60% of predicted
Normal FEV1/FVC
Elevated PCO2
A 68-year-old man presents to the ED 4 hours after an upper endoscopy was performed for 5 months of progressive dysphagia. During the procedure, a 1-cm ulcerated lesion was found and biopsied. Now, the patient complains of severe neck and chest pain. His vitals are as follows: BP 135/80 mm Hg, HR 123 beats per minute, RR 26 breaths per minute, and temperature 101°F. On physical examination, he appears diaphoretic and in moderate distress with crepitus in the neck and a crunching sound over the heart. You obtain an electrocardiogram (ECG), which is notable for sinus tachycardia. After obtaining a surgical consult, which of the following is the next best step in management?
Perform an immediate bronchoscopy
Give aspirin 325 mg and obtain a cardiology consult for possible cardiac catheterization
Order an immediate esophagram with water-soluble agent
Perform an immediate thoracotomy
Repeat the endoscopy to evaluate the biopsy site
A 68-year-old man presents to the physician’s office complaining of progressive dysphagia over the last 3 months associated with mild chest discomfort. He reports a 15-lb weight loss, a 30 pack-year smoking history, and occasional alcohol intake. The physical examination, including vital signs, is unremarkable. A chest x-ray was normal, and a barium esophagogram shows an irregular filling defect in the distal third of the esophagus with distortion and narrowing of the lumen. Which of the following is the most appropriate next step in management?
CT scan
Esophagoscopy
MRI scan
Surgical resection
Bronchoscopy
A 68-year-old white male comes to the emergency department due to a sudden onset of right-sided hemiplegia, headache and impaired consciousness. There is no prior history of transient ischemic attacks. His medical problems include hypertension, obesity, hypercholesterolemia, tobacco abuse, benign essential tremor, gout, and benign prostatic hyperplasia. His medications include amlodipine, simvastatin, colchicine, propranolol, and doxazosin. The neurological exam shows right-sided weakness and hemi-sensory loss. There is a carotid bruit on his left side. Which of the following is the most appropriate next step in management?
Anticoagulate with heparin
CT scan of head with contrast
Give aspirin
CT scan of head without contrast
Perform MRI scan of head
A 68-year-old woman comes to the physician because of a painful lump in her vagina. She states that the lump has been there for a few months, but has recently begun to cause her pain. She has hypertension, for which she takes a diuretic, but no other medical problems. Examination shows a 4 cm cystic mass near the patient's introitus by the right labia. The mass is mildly tender. The remainder of the pelvic examination is normal. Which of the following is the most appropriate next step in management?
Expectant management
Sitz baths
Oral antibiotics
Biopsy of the mass
Word catheter placement
A 68-year-old woman presents with an obviously incarcerated umbilical hernia. She has gross abdominal distention, is clinically dehydrated, and reports persistent fecaloid vomiting for the past 3 days. Although tired, weak, and thirsty, she is awake and alert and her sensorium is not particularly affected. Laboratory analysis reveals a serum sodium concentration of 118mEq/L. Which of the following is the most likely physiologic explanation for the serum sodium?
She has acute water intoxication
She has been vomiting and trapping hypertonic fluids in the bowel lumen
She has vomited and sequestered sodium-containing fluids, and has retained endogenous and ingested water
There must be a laboratory error, because such a serum sodium level would have produced coma
Volume deprivation leads to renal wasting of sodium
A 68-year-old woman with a history of heavy alcohol use and chronic pancreatitis presents with a several month history of recurrent epigastric pain. The pain is occasionally associated with nausea and vomiting. She has lost 15 lbs (6.8 kg) over the past 3 months. She is afebrile. Physical examination shows scleral icterus. Laboratory studies show: Albumin 3.0 mg/dl, Total bilirubin 3.5 mg/dl, Direct bilirubin 24 mg/dl, Alkaline phosphatase 220 U/L, Aspartate aminotransferase (SGOT) 28 U/L, Alanine aminotransferase (SGPT) 25 U/L, Amylase 145 U/L, Lipase 100 U/L. Which of the following is the most appropriate next step in management?
ERCP
MRI of the abdomen
CT scan of the abdomen
Plain abdominal radiography
Upper GI endoscopy
A 69-year-old comatose man is brought to the emergency department by an ambulance. His wife says that he has been hypertensive for the past twenty years, and he is not compliant with his medication. His pulse is 80/min and blood pressure is 240/140 mm Hg. The physical examination reveals reactive pupils, no oculocephalic reflexes, no nystagmus, positive conjugate gaze deviation to the left, and reflexes of 3/4 on the right and 2/4 on the left side. Which of the following is most likely to be seen on computed tomography?
Bleeding into brain tumor
Normal brain
Ruptured aneurysm
Basal ganglia haemorrhage
Brain abscess
A 69-year-old man has had pain in left lower quadrant (LLQ) for 3 days. The pain was intermittent, but since yesterday it has been constant. He also had sweating and chills for the last 2 days. He hasn't had a bowel movement for 4 days, but has passed flatus. He vomited once and still has nausea. His past medical history is remarkable for constipation and nephrolithiasis. His vital signs are: PR: 110/min; BP: 122/80mm Hg; RR: 24/min; Temperature: 38.6°C (101.3°F). His abdomen is soft and tender to palpation in the left lower quadrant. Deep palpation is difficult but reveals no masses or organomegaly. Bowel sounds are decreased. Rectal exam is positive for enlarged prostate. Costovertebral angle tenderness is absent. Ultrasound shows bilateral hydronephrosis and stones in the kidneys. His laboratory test results are: WBC 14,500/cmm, Hb 11.7gm/dl, Hct 34%, ESR 40/hour, BUN43 mg/dl, Creatinine 2.0 mg/dl. Urinalysis RBC 4-10/hpf; WBC 3/hpf; few hyaline casts; many oxalate crystals. The next step should be?
Intravenous pyelography
Sigmoidoscopy
Contrast enema
CT of abdomen
Upright abdominal film
A 69-year-old man who smokes and drinks and has rotten teeth, has a hard, fixed, 4-cm mass in his left neck. The mass is just medial to and in front of the sternomastoid muscle, at the level of the upper notch of the thyroid cartilage. It has been there for at least 6 months, and it is growing. Which of the following is the most appropriate next step in diagnosis?
Panendoscopy (triple endoscopy) and mucosal biopsies
Open incisional biopsy of the mass
Radionuclide scan of the thyroid gland
Sputum cytology and CT scan of the lungs
Open excisional biopsy of the mass
A 69-year-old man, who smokes and drinks heavily, complains of an earache on his left side. The earache has been present for 6 weeks and is not getting any better despite systemic antibiotics and ear drops. On physical examination, he is found to have very poor oral hygiene, only a few remaining stumps of rotten teeth, and big tonsils that are hard to see because he gags easily. Otoscopic examination shows a perfectly normal right tympanic membrane, although the left is distorted by what appears to be a serous otitis media. Tuning fork testing shows conductive hearing loss on the left but equal bone conduction on both sides. He is afebrile. Which of the following will most likely confirm the diagnosis?
Audiometry
Biopsies of the tympanic membrane and ear canal
MRI studies of the eighth nerve
Culture of fluid aspirated from the left ear
Panendoscopy and biopsies
A 69-year-old patient is brought to the office by his daughter because his behavior changed progressively for the past several months. He roams in the apartment at night, and forgets his grandchildren's names. Three days ago, he was found by the doorman urinating by the building's gates. His wife died three years ago. He insists that there is nothing wrong with him, and tries to give excuses for what his daughter is reporting. He does not feel particularly fatigued and has a good appetite. He does not smoke, has no history of alcohol abuse, and no history of diabetes. His blood pressure is 155/85 mm Hg, pulse is 90 /min, and respirations are 15/min. Although the neurologic exam was difficult to assess, there were no abnormalities found. The Babinski sign is negative bilaterally. There is no evidence of rectal or bladder incontinence. The mini-mental state examination (MMSE) score is 15/30 (normal > 24). The laboratory studies show: Hb 13.5 g/dl, RBC 4.5 million/mm3, Hct 45%, Leukocyte count 4,500/mm3, Platelet count 230,000/mm3, MCV 83 um3, MCHC 32% Hb/cell, S. calcium 9.0 mg/dl, S. sodium 137 mEq/dL, S. potassium 4.0 mEq/dL, S. creatinine 1.1 mg/dl, S. glucose 100 mg/dl, TSH 3 uU/mL, Total cholesterol 180 mg/dl. CT scan is done. Which of the following abnormalities would you expect to see on the CT scan?
Enlargement of the ventricle without cortical atrophy
Marked atrophy of the frontal and temporal cortices
Diffuse cortical and subcortical atrophy
Normal appearance
Hypodense images involving different brain regions
A 69-year-old woman has recently returned on an overnight flight from Europe. She now complains of vague chest discomfort and shortness of breath. On examination, she is comfortable, blood pressure 130/80 mm Hg, pulse 90/min, respirations 18/min, and oxygen saturation 97%. Her heart and lungs are normal on auscultation, and there is no edema or leg tenderness on palpation. A quantitative (ELISA) D-dimer assay is positive. Which of the following statements regarding the D-dimer assay is correct?
It is specific but not sensitive
A negative result suggests myocardial ischemia
It is sensitive but not specific
It is neither specific nor sensitive
It is both sensitive and specific
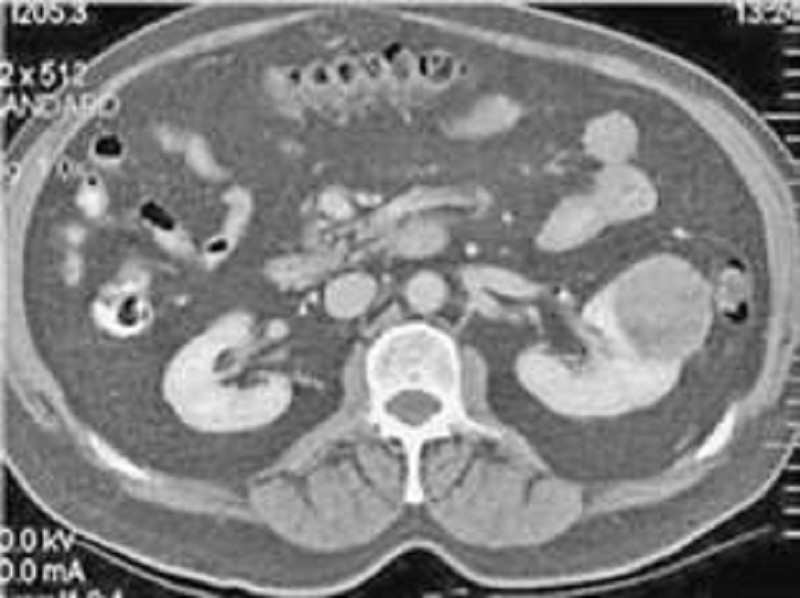
A 69-year-old woman presents with left flank pain and hematuria. Physical examination suggests a left-sided abdominal mass. Computerized tomography (CT) scan of the abdomen reveals a 5-cm mass in the left kidney. Which of the following laboratory abnormalities might also be present (See Fig.)?
Polycythemia
Thrombocytopenia
Hypocalcemia
Leukocytosis
High renin hypertension
A 7 -year-old African American boy is brought to your clinic with complaints of bedwetting. He was toilet trained at the age of 4. He has been able to pass urine normally in daytime, but has never been dry at night. There is no history of urgency or frequency during daytime. There is no history suggestive of child abuse. He had two episodes of urinary tract infections (UTI) from birth until he was 2-years-old, but he has not had any episodes ever since. What is the next best step in the management of this patient?
Urinalysis
Ultrasound of the kidneys
Intravenous pyelogram
Prescription of Imipramine
Behavioral modification
A 7 -year-old male child is brought to the office due to decreased urine output and lethargy for the past week. His birth and past medical histories are insignificant. His immunizations are up-to-date. Examination reveals no abnormalities. His BUN and creatinine levels are elevated. What is the most appropriate next step in the management of this patient?
Abdominal USG
Intravenous pyelogram
Urinalysis
CT scan of abdomen
Urine culture
A 7-day-old boy who is the product of an uncomplicated gestation is brought to the physician because of hypospadias. The baby is otherwise healthy, and is urinating without any difficulty. On physical examination, vital signs are stable, lungs are clear and the heart is beating at a regular rate. The only abnormal physical finding is the hypospadias. Urinalysis is negative for infection. Which of the following is the most appropriate next step?
Measuring serum creatinine level
Obtain an intravenous pyelogram
Schedule a renal ultrasound
Cystography
Performing a circumcision

A 7-week-old, breast-fed, term infant presents with increasing jaundice, abdominal distention, and abnormal stools (Figure 6-20). Liver fun
Radioisotope scanning
Abdominal ultrasound
CT scan of the abdomen
MRI scan of the abdomen
Radioisotope scanning with pre-imaging phenobarbital administration
A 7-year-old boy is brought to the clinic for a lifetime history of bedwetting. He has otherwise been completely healthy and has met all development milestones. His parents deny a history of trauma, and the history is not consistent with abuse. The patient has been wetting every night but not during the daytime. He has no incontinence. Which of the following is the most appropriate next step in his evaluation?
Intravenous pyelogram
Renal ultrasound
24-hour urine collection
Urinalysis
CT of pelvis
A 7-year-old boy is brought to the physician because of persistent nasal obstruction for 6 months. There is no: personal or family history of allergic disorders. Examination of the nasal fossae reveals bilateral ethmoidal polyps that protrude into the middle meatus and nasal cavity. Which of the following is the most appropriate next step in diagnosis?
Cutaneous allergen testing
Pilocarpine iontophoresis sweat test
Nasal provocation testing
Excisional biopsy
Radioallergosorbent test (RAST)
A 7-year-old boy passes a large, bloody bowel movement. He is hemodynamically stable, and he has hemoglobin of 14 g/dL. Nasogastric aspiration yields clear, greenish fluid. Physical examination, including anoscopy, is unremarkable. Which of the following is the most appropriate next diagnostic test?
Celiac arteriogram
Radioactively tagged red cell study
Colonoscopy
Radioactively labeled technetium scan
Upper gastrointestinal endoscopy
A 7-year-old girl was found in a routine health supervision visit to have bilateral breast tissue development. She also had long, pigmented hair over the labia majora. Her height and weight are both at the 80th percentile for her age. Which of the following is the most appropriate management?
CT of the head and abdomen
Thyroid stimulating hormone (TSH) level
Radiography of the head and wrist
Reassurance to the parents that it is normal
Pelvic ultrasonography
A 7-year-old is brought to the office with sore throat, poor appetite, and malaise over the last 2 days. He has no cough, rhinorrhea, or nasal congestion. The boy takes no medications, has no known allergies, and his immunization are up to date. Temperature is 38.9 C, BP is 110/70 mmHg, pulse is 130/min, and respitations are 16/min. On examination, his tonsils are swollen and covered with thin, with exudates. Small, tender anterior cervical lymph nodes are palpated. What is the most appropriate next step in management of this patient?
Amoxicillin
Azithromycin
Antistreptolysin O antibody testing
Rapid streptococcal antigen testing
Symptomatic treatement only
A 70-year-old male is brought to the ER, by his wife, because he lost consciousness while getting up in the morning. The syncopal episode lasted for several minutes, and the patient rapidly recovered consciousness. He had diarrhea and a decreased appetite one day earlier, which resolved spontaneously. His past medical history is significant for hypertension that is effectively controlled with the combination of hydrochlorothiazide/amiloride. His blood pressure is 120/70 mmHg, while supine, and 98/50 mmHg, while standing. The physical examination revealed a mucosal dryness. The EKG is normal. Which of the following laboratory values is the most sensitive indicator of the patient's underlying condition?
Decreased sodium concentration in the urine
Increased BUN/creatinine ratio
Hypokalemia
Metabolic acidosis
Decreased haematocrit
A 70-year-old man comes to his primary care physician for his annual check-up. He has a history of hypertension, hyperlipidemia, and coronary artery disease, and had coronary artery bypass grafting 6 years ago. On examination the physician notes a right carotid bruit. Which of the following is the most appropriate next step?
Carotid duplex ultrasound
Carotid endarterectomy
ECG
Referral to a neurologist
Transthoracic echocardiography
A 70-year-old man comes to the physician because of nocturia. He states that over the past two years his urinary frequency has increased and he has to strain while passing urine. He also notes dribbling of a few drops of urine at the end of voiding. Sometimes he has to void again within two hours. He has no other symptoms. He has no history of diabetes mellitus, stroke or trauma. He does not take any medication. His father had surgery of the prostate for benign prostatic hyperplasia. He has a 15-pack-years history of cigarette smoking. Rectal examination shows smooth, firm enlargement of the prostate with no induration. Neurological examination shows no abnormalities. Laboratory study shows a serum creatinine of 0.7 mg/dl. Which of the following studies is indicated at this time?
Blood urea nitrogen
Urinalysis
Ultrasound of kidney, bladder and ureter
Serum prostate specific antigen
Cystoscopy
A 70-year-old man complains of fever and pain in his left knee. Several days previously, he suffered an abrasion of his knee while working in his garage. The knee is red, warm, and swollen. An arthocentesis is performed, which shows 200,000 leukocytes/μL and a glucose of 20 mg/dL. No crystals are noted. Which of the following is the most important next step?
Gram stain and culture of joint fluid
Uric acid level
Urethral culture
Antinuclear antibody
Antineutrophil cytoplasmic antibody
A 70-year-old man presents with a complaint of fatigue. There is no history of alcohol abuse or liver disease; the patient is taking no medications. Scleral icterus is noted on physical examination; the liver and spleen are nonpalpable. The patient has a normocytic, normochromic anemia. Urinalysis shows bilirubinuria with absent urine urobilinogen. Serum bilirubin is 12 mg/dL, AST and ALT are normal, and alkaline phosphatase is 300 U/L (three times normal). Which of the following is the best next step in evaluation?
Ultrasound or CT scan of the abdomen
Reticulocyte count
Viral hepatitis profile
Serum ferritin
Antimitochondrial antibodies
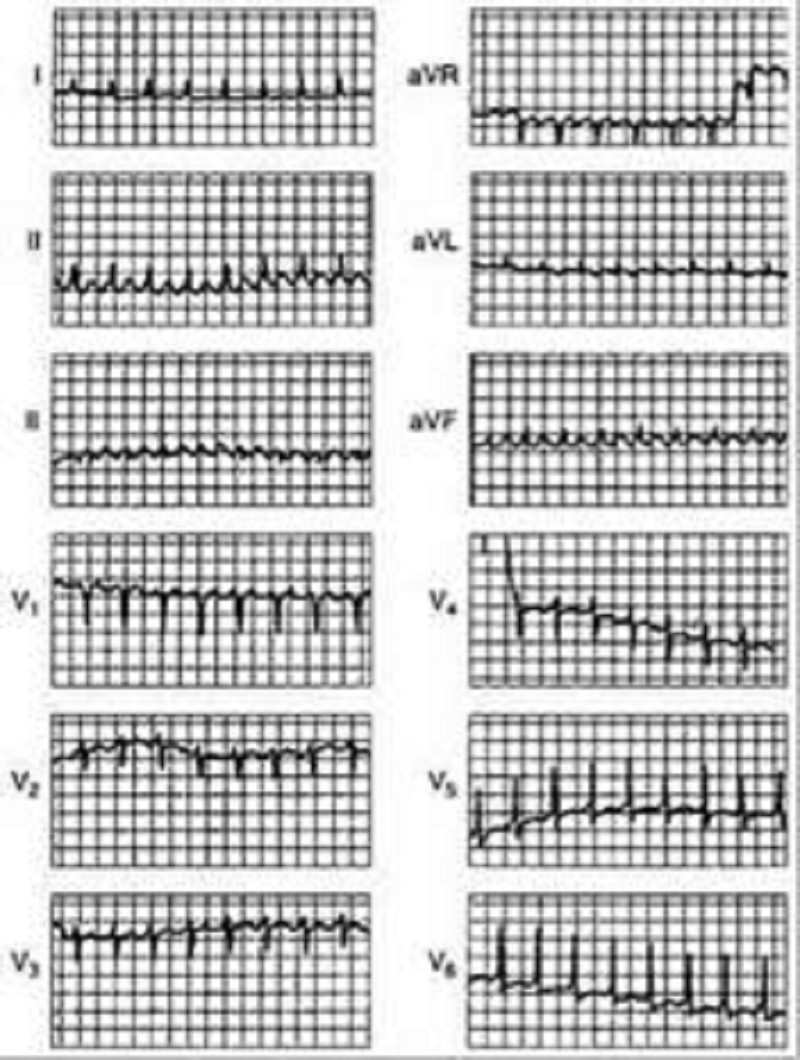
A 70-year-old man has dyspnea, orthopnea, and paroxysmal nocturnal dyspnea. He has generalized cardiomegaly and pulmonary and systemic venous hypertension. The ECG is shown in Fig.What is the cardiac rhythm?
Ectopic atrial tachycardia
Supraventricular tachycardia
Atrial fibrillation with rapid ventricular response
Atrial flutter with 2:1 AV conduction
Sinus tachycardia
A 70-year-old man presents with a complaint of fatigue. There is no history of alcohol abuse or liver disease; the patient is taking no medications. Scleral icterus is noted on physical examination; the liver and spleen are nonpalpable. The patient has a normocytic, normochromic anemia. Urinalysis shows bilirubinuria with absent urine urobilinogen. Serum bilirubin is 12 mg/dL, AST and ALT are normal, and alkaline phosphatase is 300 U/L (three times normal). Which of the following is the best next step in evaluation?
Viral hepatitis profile
Antimitochondrial antibodies
Reticulocyte count
Serum ferritin
Ultrasound or CT scan of the abdomen
{"name":"DES C_ParaClinic (5) Prepared : CHILLY", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 58-year-old postmenopausal female presents to your office on suggestion from a urologist. She has passed 3 kidney stones within the past 3 years. She is taking no medications. Her basic laboratory work shows the following: Na: 139 mEq\/L, K: 4.2 mEq\/L, HCO3: 25 mEq\/L, Cl: 101 mEq\/L, BUN: 19 mg\/dL, Creatinine: 1.1 mg\/dL, Ca: 11.2 mg\/dL. A repeat calcium level is 11.4 mg\/dL; PO4 is 2.3 mmol\/L (normal above 2.5). Which of the following tests will confirm the most likely diagnosis?, A 58-year-old white man complains of intermittent rectal bleeding and, at the time of colonoscopy, is found to have internal hemorrhoids and the lesion shown at the splenic flexure. Pathology shows tubulovillous changes. Repeat colonoscopy should be recommended at what interval?, A 58-year-old woman has had bilateral hip and knee pain for the past several months. The pain is worse with activity and better with rest. Recently she has noticed swelling of the right knee. She reports morning stiffness of about 10-15minutes duration. She denies fever or weight loss. Her past medical history is significant for hypertension, type 2 diabetes, gastroesophageal reflux disease, and obstructive sleep apnea. She takes hydrochlorothiazide, lisinopril, omeprazole, insulin and aspirin. She does not use tobacco, alcohol or drugs. Her temperature is 37.2°C (98.9°F), and blood pressure is 146\/86 mmHg. Examination shows a mild effusion, tenderness, and decreased range of motion of the right knee. Synovial fluid analysis reveals the following: Cell count 1100\/ml, Gram stain negative, Crystals absent. Plain films of her knee joint would most likely reveal?","img":"https://cdn.poll-maker.com/18-731849/image.jpeg?sz=1200"}
More Quizzes
What's your finance mindset
5222
Desert Quiz
210
Alex rider Quiz
630
Identify Types Of Inventory (A&B)
8431
Will He Be My Boyfriend - Find Out His Intentions
201019032
Dangling Modifier - Free Practice with Answers
201018940
Which FNAF 2 Character Are You? - Free
201020572
Alabama Football Trivia - Test Your Crimson Tide Knowledge
201020237
Latitude and Longitude - Test Your Map Skills
201024950
Carp Fishing - How Well Do You Know Carp?
201023888
What Lipstick Suits Me? Free to Find Your Shade
201018940
Ikigai Test - Find Your Purpose in Life (Free)
201020686