Pediatrics A Mock exam
A 4 y/o male with nephrotic syndrome had proteinuria of +3 one day PTA. He now complains of dizziness and decreased urine output. BP was 60 palpatory. What is the best thing to do immediately?
Give epinephrine 0.3 cc IV
Start IV fluid at maintenance rate
Start oral prednisone and observe
Give albumin transfusion at 1-2 gm/kg
NEPHROTIC SYNDROME MANAGEMENT
Triad of clinical findings associated with nephrotic syndrome:
1. Hypoalbuminemia (≤2.5 g/dL)
2. Edema
3. Hyperlipidemia (cholesterol >200 mg/dL)
Nephrotic Management
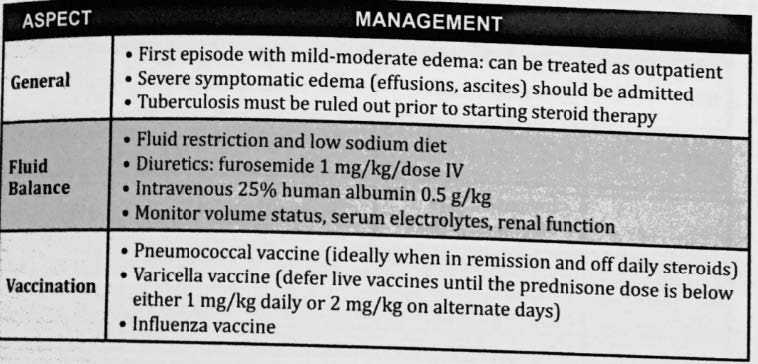
Based sa platinum the first line of treatment for proteinuria is corticosteroids which is letter C. however, this is not for the acute management as you are required to correct the fluid imbalance first by giving IV albumin which is letter D. YOU
DON’T GIVE IV FLUIDS because bale wala lang yun if there is persistent protein loss as there will be a continuous shift in the starling forces. Which rules out Letter B. Letter A. Is for mema lang go ka na for letter D
DON’T GIVE IV FLUIDS because bale wala lang yun if there is persistent protein loss as there will be a continuous shift in the starling forces. Which rules out Letter B. Letter A. Is for mema lang go ka na for letter D
NEPHROTIC SYNDROME MANAGEMENT
Triad of clinical findings associated with nephrotic syndrome:
1. Hypoalbuminemia (≤2.5 g/dL)
2. Edema
3. Hyperlipidemia (cholesterol >200 mg/dL)
Nephrotic Management
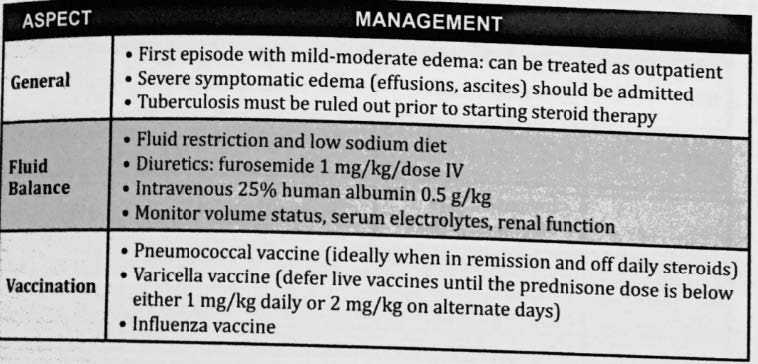
Based sa platinum the first line of treatment for proteinuria is corticosteroids which is letter C. however, this is not for the acute management as you are required to correct the fluid imbalance first by giving IV albumin which is letter D. YOU
DON’T GIVE IV FLUIDS because bale wala lang yun if there is persistent protein loss as there will be a continuous shift in the starling forces. Which rules out Letter B. Letter A. Is for mema lang go ka na for letter D
DON’T GIVE IV FLUIDS because bale wala lang yun if there is persistent protein loss as there will be a continuous shift in the starling forces. Which rules out Letter B. Letter A. Is for mema lang go ka na for letter D
Massive protein losses in nephrotic syndrome is due to injury of the:
Endothelial cells
Epithelial cells
Juxtaglomerular cells
Podocytes
Nephrotic syndrome- increased permeability of glomerular
capillary wall leading to massive proteinuria and hypoalbuminemia
Podocyte injury- underlying mechanism of proteinuria
Function:
- Structural support of capillary loop
- Major component of glomerular filtration barrier to proteins
- Synthesis and repair of glomerular basement membrane
Nephrotic syndrome- increased permeability of glomerular
capillary wall leading to massive proteinuria and hypoalbuminemia
Podocyte injury- underlying mechanism of proteinuria
Function:
- Structural support of capillary loop
- Major component of glomerular filtration barrier to proteins
- Synthesis and repair of glomerular basement membrane
. The drug of choice for newly diagnosed idiopathic nephrotic syndrome is:
Prednisone
High protein diet
Diuretics
Penicillin
For children with idiopathic nephrotic syndrome, corticosteroids are the mainstay of treatment
NS= Nephrotic Syndrome
In prelims ratio recording: Idiopathic nephrotic Syndrome encompasses the different types of histologic types of NS= Nephrotic Syndrome
In prelims ratio recording: Idiopathic nephrotic Syndrome encompasses the different types of histologic types of Nephrotic Syndrome. However,initial management would
usually involve the use of your steroid so Prednisone is the correct answer.
usually involve the use of your steroid so Prednisone is the correct answer.
For children with idiopathic nephrotic syndrome, corticosteroids are the mainstay of treatment
NS= Nephrotic Syndrome
In prelims ratio recording: Idiopathic nephrotic Syndrome encompasses the different types of histologic types of NS= Nephrotic Syndrome
In prelims ratio recording: Idiopathic nephrotic Syndrome encompasses the different types of histologic types of Nephrotic Syndrome. However,initial management would
usually involve the use of your steroid so Prednisone is the correct answer.
usually involve the use of your steroid so Prednisone is the correct answer.
A 9-month-old baby was brought due to red colored urine with some red particles on the diaper. He also had URTI for 4 days ago. What is the probable diagnosis?
Acute kidney injury
Hemorrhagic cystitis
Glomerulonephritis
Pyelonephritis
100. A 5-year-old female presented with fever of 40C, vomiting and poor intake with no other symptoms. Urinalysis showed hematuria, pyuria, leucocyte esterase +, nitrite +. Urine culture showed E. Coli at 100,000 cfu/mL. What is the diagnosis?
Acute pyelonephritis
Acute kidney parenchymal injury
Acute cystitis
Covert bacteriuria
This statement is TRUE of chronic kidney disease:
Proteinuria of 30 mg/m2/ hr of 12 weeks duration.
Anemia is usually secondary to a dilutional type
GFR of less than 60ml/1.73m2/ hr of 3 months duration.
Growth is normal.
Criteria for Definition of Chronic Kidney Disease (NKF KDOQI Guidelines)
Patient has chronic kidney disease (CKD) if either of the
following criteria are present:
1. Kidney damage for ≥ 3 mo, as defined by structural or functional abnormalities of the kidney, with or without decreased GFR, manifested by one or more of the following features:
• Abnormalities in the composition of the blood or urine
• Abnormalities in imaging tests
• Abnormalities on kidney biopsy
2. GFR < 60 mL/min/1.73 m2 for ≥ 3 mo, with or without the other signs of kidney damage described above
Criteria for Definition of Chronic Kidney Disease (NKF KDOQI Guidelines)
Patient has chronic kidney disease (CKD) if either of the
following criteria are present:
1. Kidney damage for ≥ 3 mo, as defined by structural or functional abnormalities of the kidney, with or without decreased GFR, manifested by one or more of the following features:
• Abnormalities in the composition of the blood or urine
• Abnormalities in imaging tests
• Abnormalities on kidney biopsy
2. GFR < 60 mL/min/1.73 m2 for ≥ 3 mo, with or without the other signs of kidney damage described above
. An 8-year-old was brought to the ER for oliguria and hypertension. Patient had tea-colored urine, edema for 3 days. Mother reported that 4 weeks prior, he also had multiple crusting lesions over his nose and legs that spontaneously resolved. What antihypertensive is ideal for this patient?
Loop diuretic
Alpha-1 blocker
Beta 2 antagonist
Calcium channel blocker
● Thiazide (hydrochlorothiazide, chlorothiazide) or loop diuretics (furosemide) can be helpful in controlling hypertension related to salt and fluid retention.
Source: page 10899, Chapter 550.2 Chronic Kidney Disease,Nelson Textbook
of Pediatrics,21st edition
● Since oliguric si px,Diuresis may be augmented by the administration of loop diuretics (furosemide), orally or intravenously
Source: page 10822,Nelson Textbook of Pediatrics,21st edition
● Thiazide (hydrochlorothiazide, chlorothiazide) or loop diuretics (furosemide) can be helpful in controlling hypertension related to salt and fluid retention.
Source: page 10899, Chapter 550.2 Chronic Kidney Disease,Nelson Textbook
of Pediatrics,21st edition
● Since oliguric si px,Diuresis may be augmented by the administration of loop diuretics (furosemide), orally or intravenously
Source: page 10822,Nelson Textbook of Pediatrics,21st edition
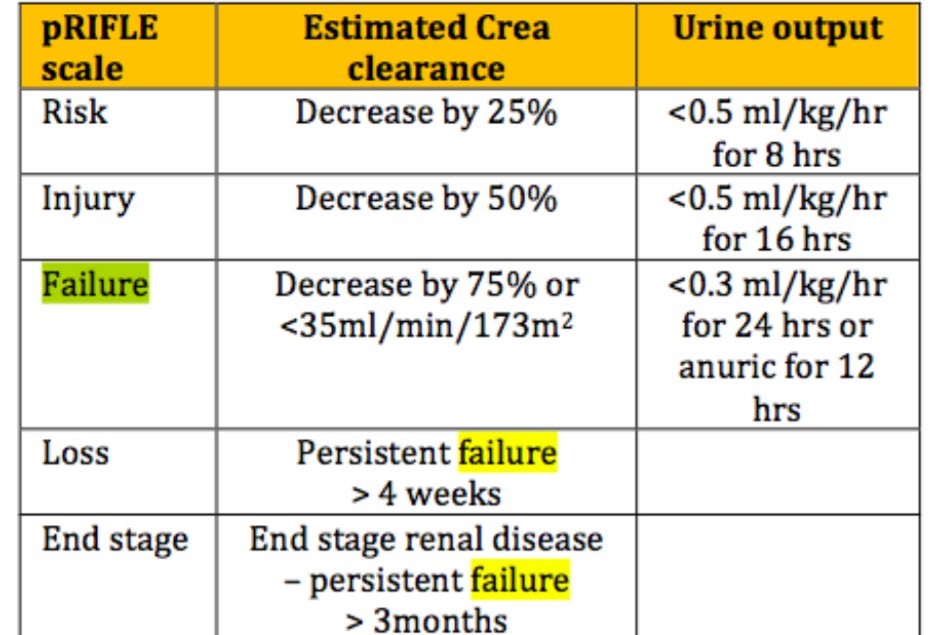
A 5 y/o male, 18 kg was seen because of vomiting and diarrhea of 2 days. At the ER he was hypotensive with severe signs of dehydration, urine output of 125 cc in the past 16 hours. He was hooked to IVF at 20 cc/kg x 2 doses; after 1 hour, VS improved with appearance of urine output. He is classified as PRIFLE category:
Failure
Injury
Risk
Loss
SD is a 5-year-old girl who complained of tea colored urine a day prior to consult. She has a history of sore throat 3 weeks pta. Which of the following laboratory result would support your diagnosis?
Low serum C3
Enlarged kidneys on ultrasound
Elevated BUN and Creatinine
Hyponatremia
A patient with acute Post Strep glomerulonephritis is recovering from the acute phase of the disease. After 3 months, repeat the serum C3 was still low. What would be the proper advice for this patient?
Observe the patient further as the C3 remains at low levels up to 6 months
Start another course of antibiotics
Advise the patient to undergo a renal biopsy
Start steroids
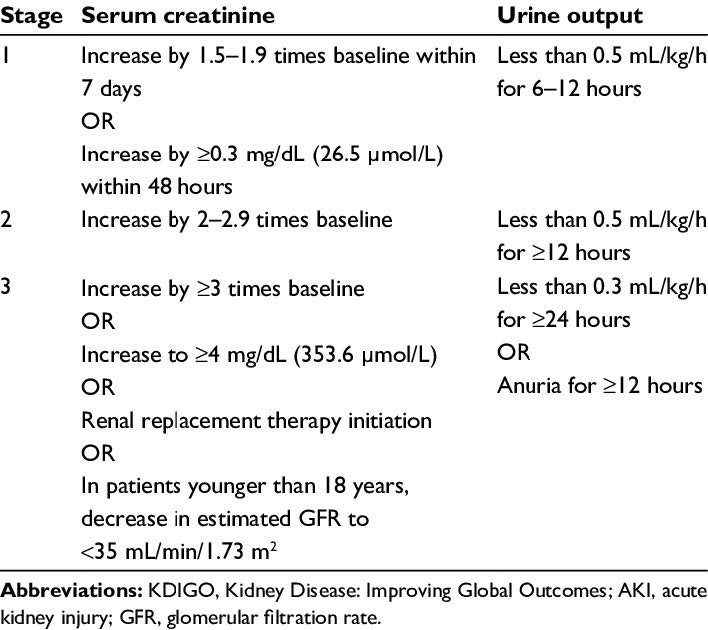
A 5y/o child, 18 kg was seen at the ER due to| vomiting and diarrhea of 1 day. He was hypotensive with severe signs of dehydration UO was 100 cc for the past 16 hours. He was given IF at 20 cc/kg × 2 doses as fast drip. After 1 hour, VS improved and with urine output. Creatinine level was increased at 9 mg/dL Under KDIGO staging of AKI, the staging of our patient is:
Stage I
Stage III
Stage II
Stage IV
A 3 year ols was seen at the ER due to weakness of 3 days. BP 90/60, CR=89/min, RR=23/min. Urinalysis: alkaline urine, hematuria. Serum Na= 143, K= 2, Cl= 126, ABG: pH 7.25, HCO3 11, CO2 30, O2 99. What is the blood anion gap?
10
5
14
6
A 3-year-old had weakness of 5 days. Weight: 10 kgs, Length: 75 cms, BP: 90/60, CR: 89/min, RR: 23/min. UA pH: 8, RBC and WBC: 0-1/hpf. CBG: 100 mg/dl, Serum Na: 140 mmol/l, K: 2 mmol/l, Cl: 120 mmol/l, ABG showed pH: 7.25, HCO3: 10, CO2: 30, O2: 99. KUB UTZ: nephrocalcinosis. Interpret the blood anion gap:
Decreased
Normal
Not significant
Increased
Computation:
[140] - [120 + 10] = 10
Interpretation:
NORMAL
Computation:
[140] - [120 + 10] = 10
Interpretation:
NORMAL
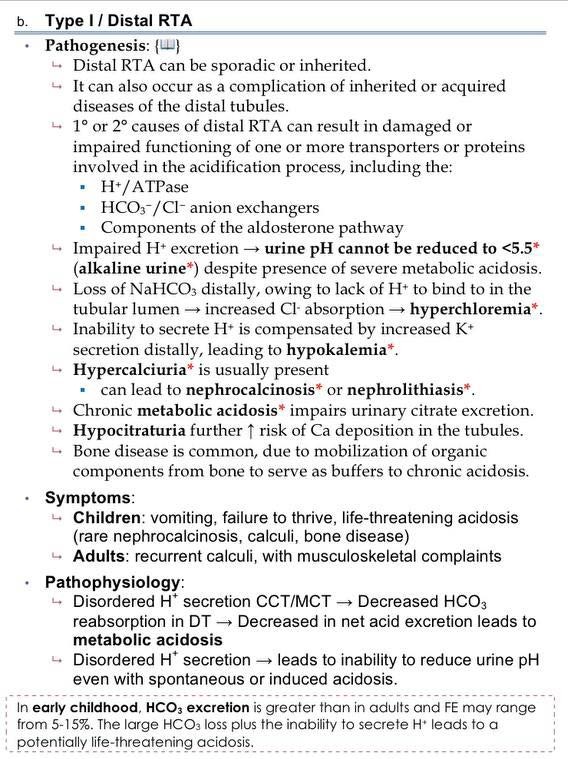
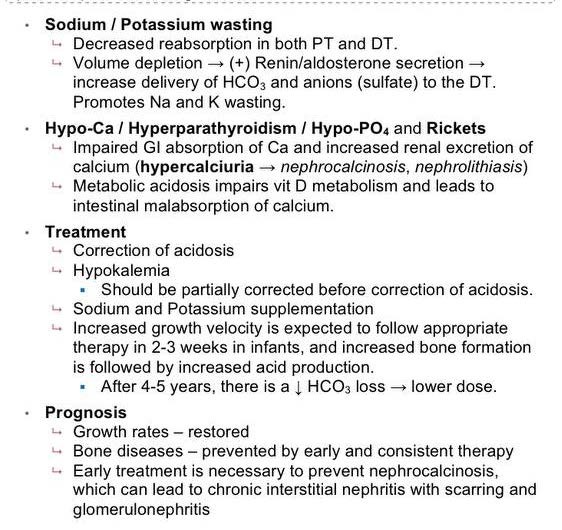
A 5 y/o male was seen due to weakness and diarrhea. PE: severely stunted, moderately wasted, with moderate dehydration. Labs: alkaline urine, hypokalemia and metabolic acidosis which persisted despite adequate hydration and potassium correction for 3 days. Urine anion gap is + 3. The type of RTA is most likely:
RTA type IV
RTA type I
RTA type III
RTA type II
RATIO
a. RTA type IV hyperkalemic RTA due to a defect in aldosterone-sensitive acid secretion
c. RTA type III combined proximal and distal RTA as a result of inherited carbonic anhydrase II
deficiency
d. RTA type II proximal RTA: negative urine anion gap, urinary pH <5.5 acidic urine pH (under mildmoderate metabolic acidosis urinary pH may be >5.5)
RATIO
a. RTA type IV hyperkalemic RTA due to a defect in aldosterone-sensitive acid secretion
c. RTA type III combined proximal and distal RTA as a result of inherited carbonic anhydrase II
deficiency
d. RTA type II proximal RTA: negative urine anion gap, urinary pH <5.5 acidic urine pH (under mildmoderate metabolic acidosis urinary pH may be >5.5)
The following are crieria for the diagnosis of recurrent UTI, EXCEPT
2 or more episodes of acute cystitis
2 or more episodes of acute pyelonephritis
3 episodes of acute cystitis
1 episodes of acute pyelonephritis and 2 episode of cystitis
A 5 y/o male was seen due to weakness and diarrhea. PE: severely stunted, moderately wasted child with moderate dehydration. There was persistent of hypokalemia, alkaline urine, and presence of metabolic acidosis despite adequate hydration and potassium correction. The anion gap is 10. What work up would differentiate RTA type I to RTA type II?
Blood anion gap
Fractional excretion of sodium
TTKG
Urine anion gap
Urine anion gap- calculated to confirm diagnosis of distal RTA
Fractional Excretion of Sodium (FENa)
Most discriminating test to differentiate prerenal from intrinsic
Urine pH- distinguish distal from proximal RTA
Urine pH <5.5 in the presence of acidosis suggests pRTA dRTA typically have a urine pH >6.0
Urine anion gap- calculated to confirm diagnosis of distal RTA
Fractional Excretion of Sodium (FENa)
Most discriminating test to differentiate prerenal from intrinsic
Urine pH- distinguish distal from proximal RTA
Urine pH <5.5 in the presence of acidosis suggests pRTA dRTA typically have a urine pH >6.0
The following test/tests for specific IgE:
Patch test
Skin prick test
Test dosing
A & B
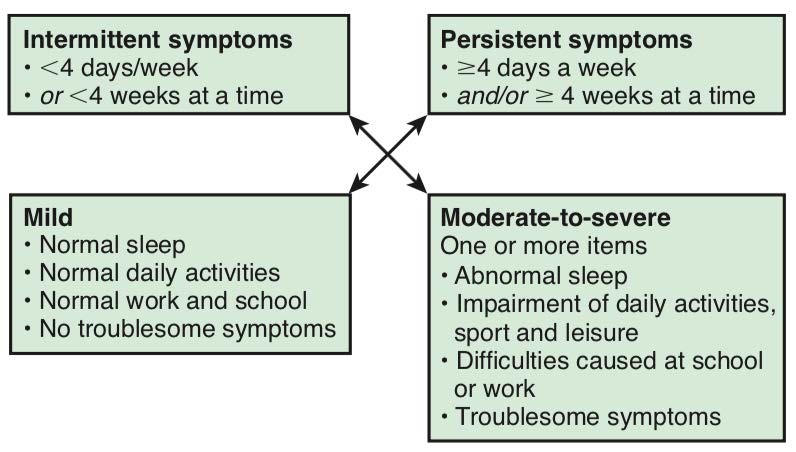
The classification of allergic rhinitis of 4 days duration with no troublesome symptoms is?
Intermittent mild
Intermittent severe
Persistent mild
Persistent severe
The drug of choice for anaphylaxis is:
Epinephrine 1:1,000 at 0.1 ml/kg IM
Epinephrine 1:10,000 at 0.1 ml/kg IM
Epinephrine 1:10,000 at 0.01 ml/kg IM
Epinephrine 1:1,000 at 0.01 ml/kg IM
● Anaphylaxis is a medical emergency requiring aggressive management with
intramuscular (first line) or intravenous epinephrine, intramus- cular or
intravenous H1 and H2 antihistamine antagonists, oxygen, intravenous
fluids, inhaled β-agonists, and corticosteroids
● Epinephrine should be given by the intramuscular route to the lateral thigh
(1:1,000 dilution, 0.01 mg/kg; max 0.5 mg).
● Anaphylaxis is a medical emergency requiring aggressive management with
intramuscular (first line) or intravenous epinephrine, intramus- cular or
intravenous H1 and H2 antihistamine antagonists, oxygen, intravenous
fluids, inhaled β-agonists, and corticosteroids
● Epinephrine should be given by the intramuscular route to the lateral thigh
(1:1,000 dilution, 0.01 mg/kg; max 0.5 mg).
The following statement characterizes atopic dermatitis:
Majority appears after 5 years of age
Majority appears after 5 years of age
Commonly involves the diaper area
Chronic relapsing course
ATOPIC DERMATITIS (ATOPIC ECZEMA)
● Most common chronic relapsing skin disease seen in infancy and childhood
● Affects 10-30% of children worldwide and frequently occurs in families with other atopic diseases, such as asthma, allergic rhinitis, and food allergy
● Typically begins in infancy. Approximately 50% of patients experience symptoms in the 1st year of life, and an additional 30% are diagnosed between 1 and 5 yr of age.
● Generally more acute in infancy and involves the face, scalp, and extensor surfaces of the extremities. The diaper area is usually spared.
ATOPIC DERMATITIS (ATOPIC ECZEMA)
● Most common chronic relapsing skin disease seen in infancy and childhood
● Affects 10-30% of children worldwide and frequently occurs in families with other atopic diseases, such as asthma, allergic rhinitis, and food allergy
● Typically begins in infancy. Approximately 50% of patients experience symptoms in the 1st year of life, and an additional 30% are diagnosed between 1 and 5 yr of age.
● Generally more acute in infancy and involves the face, scalp, and extensor surfaces of the extremities. The diaper area is usually spared.
A 16-year-old was brought in due to colds of 4 weeks. This is not associated with fever nor difficulty in breathing. However, mother would note that patient would frequently rub his nose and eyes until they are swollen. What is your complete diagnosis?
Allergic rhinitis, mild intermittent
Allergic rhinitis, moderate-severe intermittent
Allergic rhinitis, mild persistent
Allergic rhinitis, moderate-severe persistent
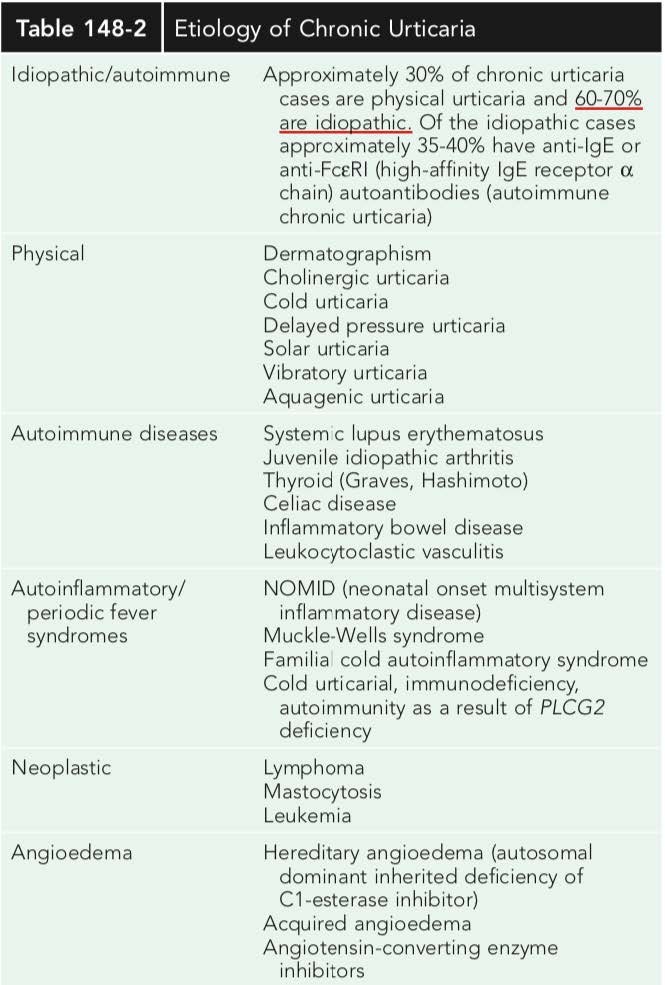
The most common cause of chronic urticarial rash is:
Food preservative
Autoimmune disorder
Idiopathic
Inhalants
A 13-year-old was brought to your clinic due to pruritic erythematous excoriated plaques on flexural areas, wrists and ankles.
Dennie-Morgan folds
Ichthyosis
Xerosis
Pruritus
The following are used in the pharmacotherapy of this condition EXCEPT:
Topical calcineurin inhibitors
Systemic corticosteroids
Dupilumab
Allergen immunotherapy
A 3 yo child has sudden onset of fever, cough and rhinorrhea. On PE you noted watery nasal discharge and with expiratory wheeze. No family history of asthma or allergy. Your plan of management:
Diphenhydramine, salbutamol nebulization, prednisone
Saline nasal spray, Anti-leukotriene
Diphenhydramine, Ipratropium nebulization, paracetamol
Saline spray, Salbutamol, Amoxicillin
A child with rhinorrhea and congestion and facial pain of 3 weeks duration. After a thorough PE and sinus plain films your diagnosis is acute Pansinusitis. What is the possible age of this child?
6 years old
4 years old
2 years old
8 years old
A 7 yo child has a symptoms most days or waking with asthma once a week with low lung function from the last 4 weeks:
Med dose ICS-LABA and Reliever needed for symptoms
Medium dose ICS and reliever needed for symptoms
Low dose ICS and Reliever needed for symptoms
Low dose ICS-LABA, and Reliever needed for symptoms
7 yo Josh had 2 episode of wheeze and needs to be worked up to diagnose asthma. But clinically he still experiences interval exacerbations. Your approach for Josh:
Do allergy test and desensitization
Do Diagnostic spirometry testing within 6 months
Check for Peak flow average daily diurnal PEF variability more than 20%
Give empiric treatment with ICS and prn SABA. Review response
A 6 yo child brought to ER Talks in words, sits hunched forwards, agitated RR 55 breaths/min Accessory muscles in use, Pulse rate125 bpm and known asthmatic. Your initial management:
SABA 4 puffs by pMDI and Prednisolone 1 mg/kg
SABA and ipratropium bromide, 6lpm oxygen via face mask
SABA and ipratropium bromide, O2, IV corticosteroid
SABA 4 puffs by pMDI, repeat every 20 min. for 1 hour and O2
In common colds, rhinorrhea is treated with one of the listed drugs to counter act the stimulation of the cholinergic receptor in the airway by the virus:
Chlorpheniramine
Cetirizine
Loratadine
Phenylephrine
A 7yo child with scratchy throat and fever followed by runny nose. On the 4th day of illness the nonproductive cough occurs mostly during daytime and more prominent when the child reclines to bed. The rest of the chest PE is unremarkable. What are the medications needed to prescribe for this child:
Paracetamol, loratadine, and salbutamol
Paracetamol,oxymetazoline, and saline nasal spray
Paracetamol, chlorpheniramine and saline nasal spray
Paracetamol, diphenhramine and oseltamivir
A 13 year old was seen in the emergency room because of difficulty in ambulation. He had diarrhea 2 weeks prior to consult. On examination motor strength 3/5 on both lower extremeties sensory is intact with areflexia. What is your diagnosis?
Myasthenia Gravis
Transverse myelitis
Botulinism
Guillan Barre
Which of the following is the sign of Chiari crisis?
Increasing head size
Stridor
Seizures
Increase urine output
A 7-year-old fell from a 5 feet high tree about 5 hours prior to consult. He then compiled of headache and had a vomiting episode. In time for mealtime the mother noted he was difficult to arouse. On PE he did not have spontaneous eye opening in deep sternal pain, no verbal and motor response. What is the GCS of the patient?
9
7
5
3
A 14 year old male was brought to the OPD due to overweight. On examination you noted he was obese with bitemporal hemianopsia. Where is the most likely location of the pathology?
Brainstem
Sella-supra sellar
Cerebrum
Cerebellum
What is the percentage of patients with port wine stain are truly Sturge Weber cases?
50-70%
5-20%
8-33%
80-100%
Survival rate is poorest for patients with
Astrocytoma
Atypical rhabdoid
Ependymoma
Medulloblastoma
A 17-year old was brought to the emergency room due to a vehicular accident, on examination the left pupils measure 7 mm non-reactive to light with apnea and absence of the corneal reflex. What is the kind of herniation did the patient have?
Transcalvarial herniation
Tonsillar herniation
Subfalcine herniation
Uncal herniation
Which of the following is a characteristic of a neuromuscular junction weakness?
Muscle biopsy is important for confirmatory diagnosis
Creatinine kinase is elevated
Proximal and distal muscles are equally affected
Deep tendon reflex is decreased
This type of drug hypersensitivity involves IgM or IgG antibodies that recognize drug antigen on cell surface:
Type I
Type IV
Type III
Type II
The following is an associated feature of atopic dermatitis?
Facial erythema or pallor
Chronic or relapsing dermatitis
Facial and extensor edema in infant
Pruritus
In Wiskott-Aldrich Syndrome, there is presence of atopic dermatitis, thrombocytopenic purpura with small defective platelets and:
Decreased IgE
Increased IgG
Decreased IgA
Decreased IgM
A 32 kg 10 year old developed pruritic maculopapular lesions, difficulty in breathing and abdominal pain 5 minutes after the 2nd dose of Covid 19 vaccination. What should you do?
Give epi at 0.1ml/kg
Give diphenhydramine at 1mg/kg
Give diphenhydramine at 0.3ml/kg
Give epi at 0.3ml/kg
The following is a risk factor for hypersensitivity reaction except:
Genetic predisposition
Route of administration
Prior exposure
Atopy
What is the responsible to the clinical manifestation of Erysipelas?
Exfoliative toxin
Erythrogenic toxin
Exotoxin A
M protein
Rifampicin is given as prophylaxis in which of the following bacterial infections?
Pneumococcal penumonia
Meningococcemia
Pneumococcal meningitis
Pertussis
Treatment options of Streptococcal pharyngitis include the following EXCEPT?
Benzathin Penicillin IM single dose
Penicillin x 10 days
Azithromycin x 10 days
Amoxicillin x 10 days
The drug of choice for treatment of pneumococcal meningitis is?
Clindamycin
Ceftriaxone
Cefuroxime
Ampicillin
The most common cause of pyogenic infections is children is:
S. pyogenes
S. aureus
H. influenza
Strep.pneumonia
A 3 year old child was brought in because of high grade fever of 2 days and difficulty of breathing. The patient did not receive any vaccination. PPE: in respiratory distress, leaning forward and very ill looking. The ER resident warned you not to examine the throat. Your impression is:
Croup
Epiglottitis
Exudative Tonsillopharyngitis
Diptheria
The following are suggestive of streptococcal pharyngitis EXCEPT?
Tender cervical lymph adenopathy
Petechiae at the soft palate
Conjunctivitis
Diffuse beefy red tonsillar pillars
Most common cause o osteomyelitis in children
Streptococcus pyogenes
Strep. pneumoniae
Staphylococcus aureus
H. influenzae
An 11-year-old child was brought in due to easy fatigability and knee pain with swelling relieved by aspirin. He had recurrent pharyngitis few years ago. Your impression is:
Post streptococcal reactive arthritis
Septic arthritis
Gouty arthritis
Rheumatic fever
The following statements are TRUE about typhoid fever EXCEPT:
Intestinat hemorrhage and/ or perforation commonly occur within the first week of fever
Hepatomegaly, splenomegaly and/or distended abdomen with sustained fever are common on the 2nd week of illness
Diarrhea may occur several days after the onset of fever in younger children while constipation occurs more often in older children.
The symptoms and PE findings may gradually resolve within 2-4 weeks if uncomplicated
Which organism is associated with a diarrheal disease where some patients go on to develop acute kidney failure, thrombocytopenia and microangiopathic hemolytic anemia?
Enteroinvasive E.coli
Shiga toxin-producing E.coli
Enterotoxigenic E.coli
Enteroaggregative E. coli
A 15y/o had fever and cough, headache, sore throat for 12 days. His mother self-medicated with amoxicillin 500mg 3x/day starting on day 7 of illness but without relief. He was not in distress, but with occasional crackles and wheezes. CBC was normal. Tuberculin test: non-reactive. CXR showed interstitial pneumonia. What is an appropriate antibiotic to give?
Cephalexin
Cefuroxime
Amoxicillin with clavulanate
Azithromycin
Which of these statements about Chlamydophila pneumonia infections is NOT TRUE?
Mild illness can be pertussis like
CXR findings are more significant than the clinical status
Pneumonia is more commonly associated with severe constitutional symptoms like fever, headache, cough and pharyngitis
Can trigger hyperactivity among asthmatics
Children infected with this organism can present as watery or bloody diarrhea with crampy periumbilical pain that may persist even after the diarrhea resolves. The abdominal pain cann mimic appendicitis, colitis or intussusception
Enterogenic E. coli
Enteropathogenic E.coli
Salmonella
Campylobacter
The nontreponemal tests like VDL or RPR are not used for?
Detecting re-infection
Establishing the diagnosis of syphilis
Monitoring response of treatment
Rapid and easy screening
A 7y/o girl had cough and colds for 7 days. Past medical history was unremarkable. Mother denied any exposure to TB but they live in a crowded neighborhood. PE was normal. CXR showed interstitial pneumonitis with prominent hilar nodes. WHat is your assessment?
Clinically diagnosed Pullmonary TB
Bacteriologically confirmed PTB
Presumptive TB
Latent TB
Most cases of congenital syphilis are asymptomatic and identified only by prenatal screening. But, this can be an early clinical sign:
Saber shin
Olympian brow
Osteochodritis
Rhagades
A 5-year-old girl was seen because of vaginal discharge. She is allegedly being sexually molested by her stepfather. Urinalysis was normal. Gram stain of the vaginal discharge showed gram negative intracellular diploccoci. What empirical treatment will you consider?
Single dose of ceftriaxone
7 days of ceftriaxone + 7 days of azithromycin
Single dose of ceftriaxone + 7 days of oral erythromycin
Single dose of ceftriaxone + 7 days of oral doxycycline
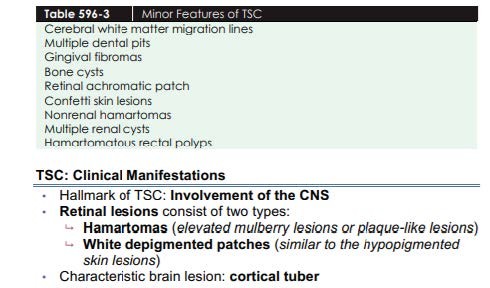
Which of the following provides an accepted and convenient method for reporting the status pf the newborn infant immediately after birth and the response to resuscitation if it is needed?
Dubowitz scoring
Apgar scoring
Crib scoring
Ballard's scoring
A 40 week AOG neonate would need the following in order to have a normal transition from intrauterine life to birth, EXCEPT which of the ff:
Surfactant secretion
Increase in pulmonary vascular resistance
Clearance of fetal lung fluid
Thermogenesis
In fetal circulation, which of the following blood vessel acts as a shunt to bypass the pulmonary circulation.
Ductus arteriosus
Umbilical vein
Umbilical artery
Ductus venosus
Which of the ff. Antimicrobial agents maybe used for eye prophylaxis in the immediate care of the newborn?
ALL OF THE CHOICES ARE CORRECT
1% silver nitrate drops
2.5% povidine iodine eye drops
Erythromycin ophthalmic ointment
What are the primary mediators that prepare the fetus for birth and support the multi-organ transition?
Cortisol and cathecolamine
Cathecolamine and thyroid hormone
Prostaglandins and cortisol
Catecholamine and prostaglandin
What is responsible for the decrease in the resistance to blood flow in the arterial bed of lung of a fetus after birth so that all blood coming from the right side of the heart would go to the lungs for oxygenation?
Decreasing both O2 and CO2 in pulmonary bed
Increasing both O2 and CO2 in pulmonary bed
Increasing O2 and Decreasing CO2 in pulmonary blood
Increasing CO2 and decreasing O2 in pulmonary blood
Infants of diabetic mothers are at increased risk for becoming hypoglycemic because they have
Glucagon insufficiency
Increased utilization of glucose
Increased levels of insulin
Decrease glycogen stores
Which of the following is the treatment of choice for symptomatic polycythemia with a central hematocrit of 70..
Phlebotomy
Prbc transfusion
Double volume exchange transfusion with saline
Partial exchange with saline solution
Which of the following is a risk factor for late onset neonatal sepsis? a.
Indwelling venous or arterial catheters
Chorioamnionitis
Premature rupture of membranes of more than 18 hours
Maternal UTI
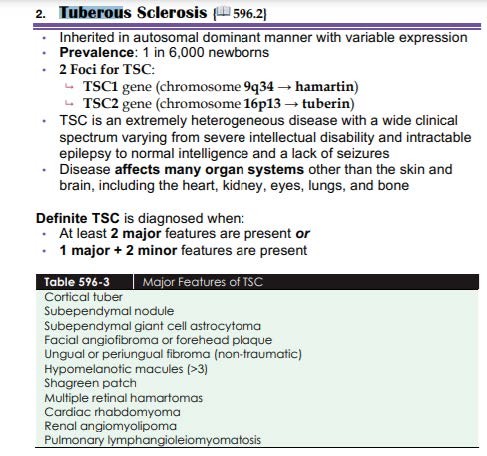
A 2-month-old female was brought to the emergency room due to exaggerated startle reflex. On examination you noted whitish macules seen in the trunk and extremities. The birth, maternal, family history are unremarkable. What is the most likely diagnosis of your patient?
Sturge Weber
Incontinentia pigmenti
Tuberous sclerosis
Hypomelanosis of Ito
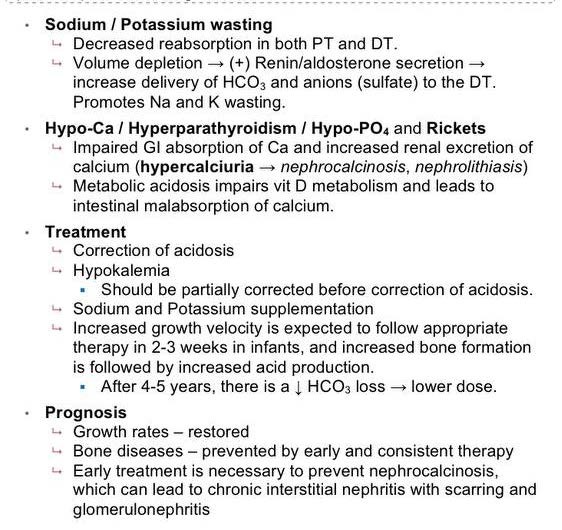
A 15-year-old boy was seen in the OPD due to cyanosis and clubbing of the lower extremities. What is the most possible diagnosis if this is due to a congenital heart disease?
PDA with pulmonary hypertension
AVSD
ASD with pulmonary hypertension
VSD with pulmonary hypertension
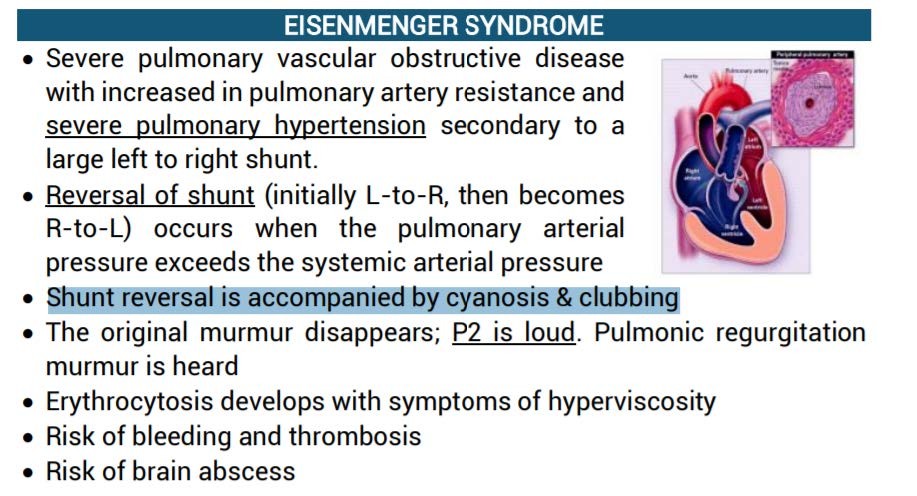
RATIO: NATURAL HISORY OF PDA - EISENMENGER SYNDROME
Small PDA usually remains asymptomatic HOWEVER persistence of LV volume overload and LV failure may Pulmonary Hypertension (Eisenmenger Syndrome)
RATIO: NATURAL HISORY OF PDA - EISENMENGER SYNDROME
Small PDA usually remains asymptomatic HOWEVER persistence of LV volume overload and LV failure may Pulmonary Hypertension (Eisenmenger Syndrome)
At birth, a 39 weeks AOG neonate was acrocyanotic with slight grimace on suctioning, some flexion, heart rate 80/min and crying. The following resuscitative measures are needed in the above situation EXCEPT:
Tactile stimulation
Keep baby warm
Delivery of oxygen thru intubation
Clear oropharyngeal area with secretions
A 5-year-old boy had large stools with occasional blood streaks and noted to be withholding his stools when he feels the urge to defecate. His history would reveal intoxication of which of the following vitamins?
Vitamin D
Vitamin C
Vitamin B
Vitamin A
A 24-month-old baby was brought due decreased intake for more than 2 weeks. He was also noted to be less playful. His mother is on 2nd month of HRZE. Tuberculin test of the baby showed 5 mm induration. CXR result is pending. What is your impression?
Clinically diagnosed PTB
Latent TB
Presumptive TB
Bacteriologically diagnosed PTB
3 y/o boy in severe respiratory distress was referred to you. PPE: awake, highly febrile, with drooling of saliva, mouth open, head slightly tilted up, both hands on thighs with arms extended supporting the body. Which is the best treatment option?
Start IV dexamethasone
Nebulize with epinephrine
Do tracheotomy
Start high dose antibiotics
A 3 y/o girl has poor appetite, fever, and sore throat. PE: small vesicles and multiple punched out ulcers in the posterior pharynx. The etiology of this infection is most likely
Grp A -hemolytic Streptococcus
Epstein-Barr virus
Coxsackie virus
Adenovirus
Which of the following best describes GI duplication?
Lining of the duplication is extraintestinal with tendency to malignancy
Most common location is in the duodenum
Located on the mesenteric border of the duplicated portion
Blood supply of the duplication comes from a separate vascular system A
A 3 y/o boy was seen with fever of 38.5C, colds and ear pain. He has good suck, tolerates milk feeding and sits on his mother’s lap. The following will be your initial management on the child:
Start Amoxicillin at 80mg/kg /day
Paracetamol + observe + follow up at 72 hours
Start Amoxicillin Clavulanate 90mg/kg/day
Paracetamol + Chlorpheniramine + phenylephrine
A 12-year-old boy with history of recurrent tonsillitis presents with fever, migrating polyarthritis and a new murmur. The most common cardiac valve pathology in this case is:
Mitral valve regurgitation
Tricuspid valve regurgitation
Aortic valve regurgitation
Mitral valve stenosis
This is true about Non-typhoidal salmonella gastroenteritis:
It presents solely as watery, non-bloody diarrhea
Symptoms usually subside within 2-7 days in healthy children
There is no risk for bacteremia
It is usually afebrile
Unconjugated hyperbilirubinemia which is noted on the tenth day of life in a well, purely breastfeeding infant is probably due to:
Biliary atresia
Breastfeeding jaundice
Neonatal hepatitis
Breastmilk jaundice
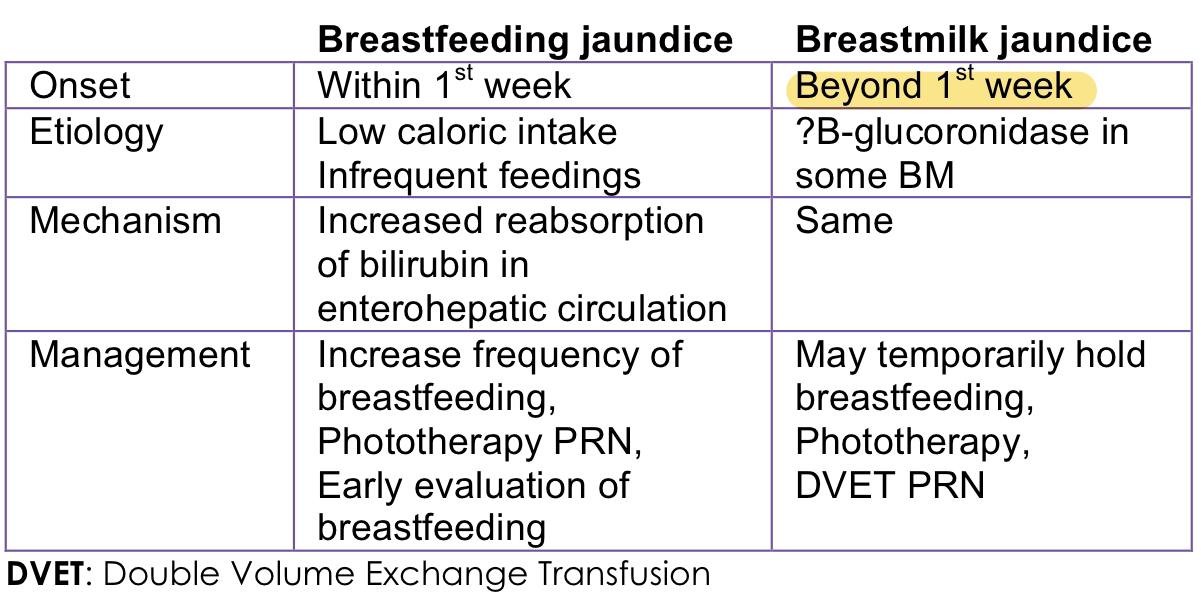
A biliary atresia causes direct hyperbilirubinemia
C the first biochemical evidence of HBV infection is elevation of serum ALT levels. The illness ispreceded by a serum sickness-like prodrome marked by arthralgia or skin lesions, including urticarial,purpuric, macular, or maculopapular rashes. Jaundice is present in approximately 25% of acutely infected patients and usually begins approximately 8 weeks after exposure and lasts for 4 weeks.
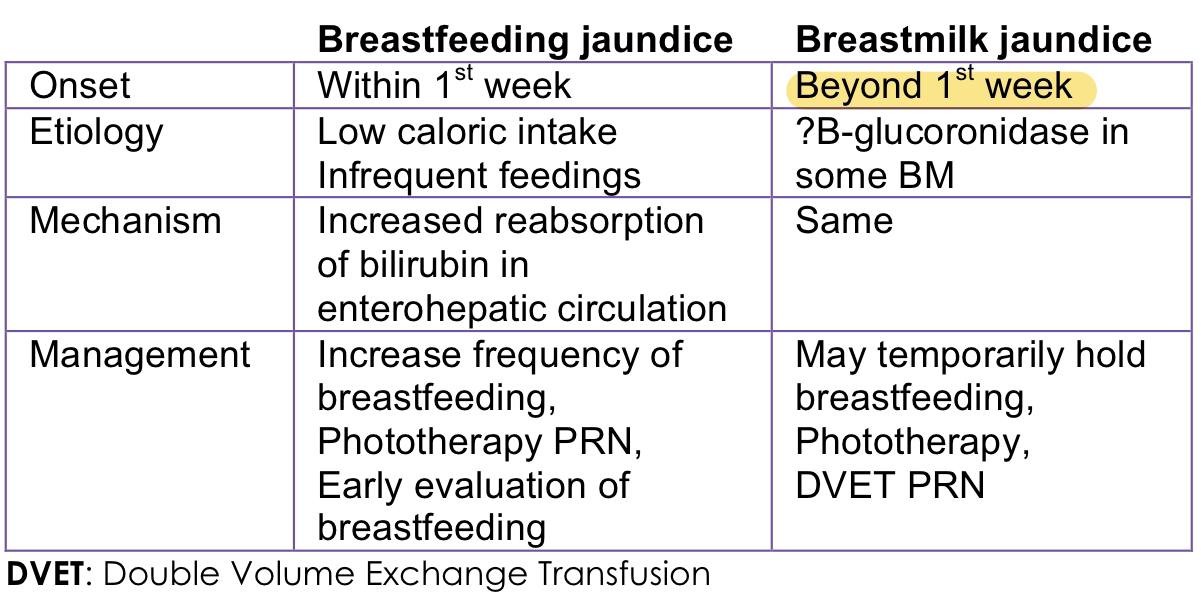
A biliary atresia causes direct hyperbilirubinemia
C the first biochemical evidence of HBV infection is elevation of serum ALT levels. The illness ispreceded by a serum sickness-like prodrome marked by arthralgia or skin lesions, including urticarial,purpuric, macular, or maculopapular rashes. Jaundice is present in approximately 25% of acutely infected patients and usually begins approximately 8 weeks after exposure and lasts for 4 weeks.
Balloon atrial septostomy is indicated in this congenital heart disease.
Tricuspid atresia
TGA with large VSD
Truncus arteriosus
TOF
Atrial septostomy is indicated for TGA with intact septum, TVA, and TAPVR
B PGE1 infusion, balloon atrial septostomy, aortopulmonary shunt, Rastelli, Mustard operation. These are the treatment options for TGA with VSD and pulmonary stenosis according to Nelson. I’m not sure which ones are indicated for large VSD and I’m not sure if atrial septostomy is only indicated for TGA with intact septum or even small VSD. Read chapter 457.6 page 2405 Nelson 21st edition.
C treatment is Rastelli procedure
D treatment is aortopulmonary (MBTS, Central) shunt
Atrial septostomy is indicated for TGA with intact septum, TVA, and TAPVR
B PGE1 infusion, balloon atrial septostomy, aortopulmonary shunt, Rastelli, Mustard operation. These are the treatment options for TGA with VSD and pulmonary stenosis according to Nelson. I’m not sure which ones are indicated for large VSD and I’m not sure if atrial septostomy is only indicated for TGA with intact septum or even small VSD. Read chapter 457.6 page 2405 Nelson 21st edition.
C treatment is Rastelli procedure
D treatment is aortopulmonary (MBTS, Central) shunt
Early laboratory findings in Salicylate poisoning include
Respiratory acidosis
Hypoglycemia
Abnormal coagulation studies
Hyperglycemia
Following a planned home birth, a term female infant is brought to the ER at two hours of life due to respiratory distress. The right hand O2 saturation reading is 70%. Her saturation quickly increases to 96% during crying and drops again to 70% when she stops crying. This pattern of saturation change is typical of which condition?
Choanal atresia
Cyanotic congenital heart disease d.
Pneumonia
Persistent pulmonary hypertension b.
A 4-year old female was admitted because of urticaria after eating lobsters. The rash subsided after 48 hours but her mother was hesitant to go home. On the 4TH hospital day, she became febrile & had productive cough. On examination, her RR was 46 CPM. She had crackles on both lung fields. Which of the following pathogens should be suspected?
Staphylococcus aureus
Hemophilus influenzae
Mycobacterium tuberculosis
Streptococcus pneumoniae
Which of the following structures in the fetus has the highest oxygen saturation?
Descending aortic arch
Ductus venosus
Right ventricle
Superior vena cava
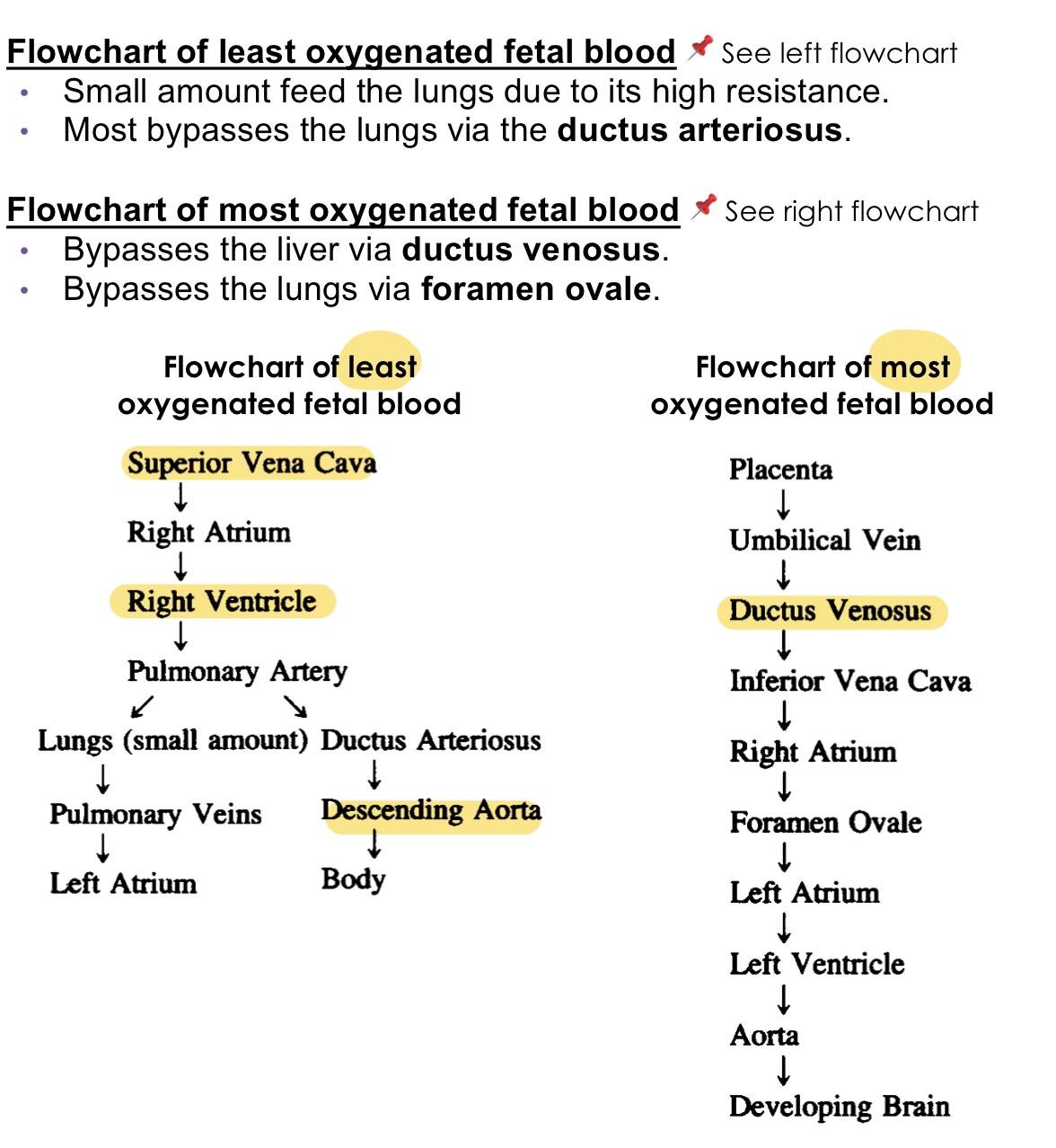
The placenta is not as efficient an oxygen-exchange organ as the lungs, so that umbilical venous partial pressure of oxygen (PO2), the highest O2 level provided to the fetus, is only 30-35 mmHg. Approximately 50% of the umbilical venous blood enters the hepatic circulation, whereas the rest bypasses the liver and joins the
inferior vena cava via the ductus venosus, where it partially mixes with poorly oxygenated IVC blood derived from the lower part of the body.
inferior vena cava via the ductus venosus, where it partially mixes with poorly oxygenated IVC blood derived from the lower part of the body.
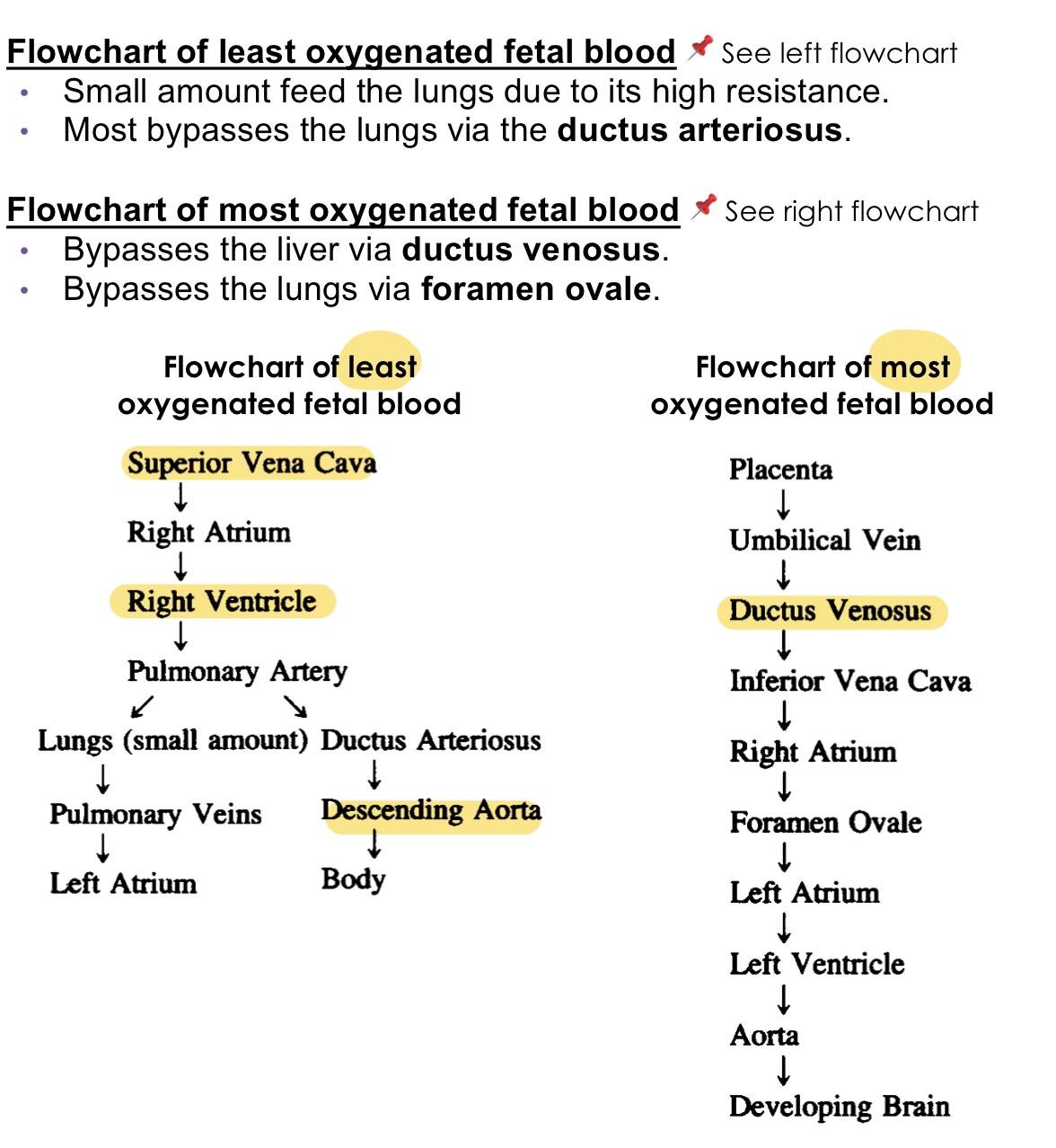
The placenta is not as efficient an oxygen-exchange organ as the lungs, so that umbilical venous partial pressure of oxygen (PO2), the highest O2 level provided to the fetus, is only 30-35 mmHg. Approximately 50% of the umbilical venous blood enters the hepatic circulation, whereas the rest bypasses the liver and joins the
inferior vena cava via the ductus venosus, where it partially mixes with poorly oxygenated IVC blood derived from the lower part of the body.
inferior vena cava via the ductus venosus, where it partially mixes with poorly oxygenated IVC blood derived from the lower part of the body.
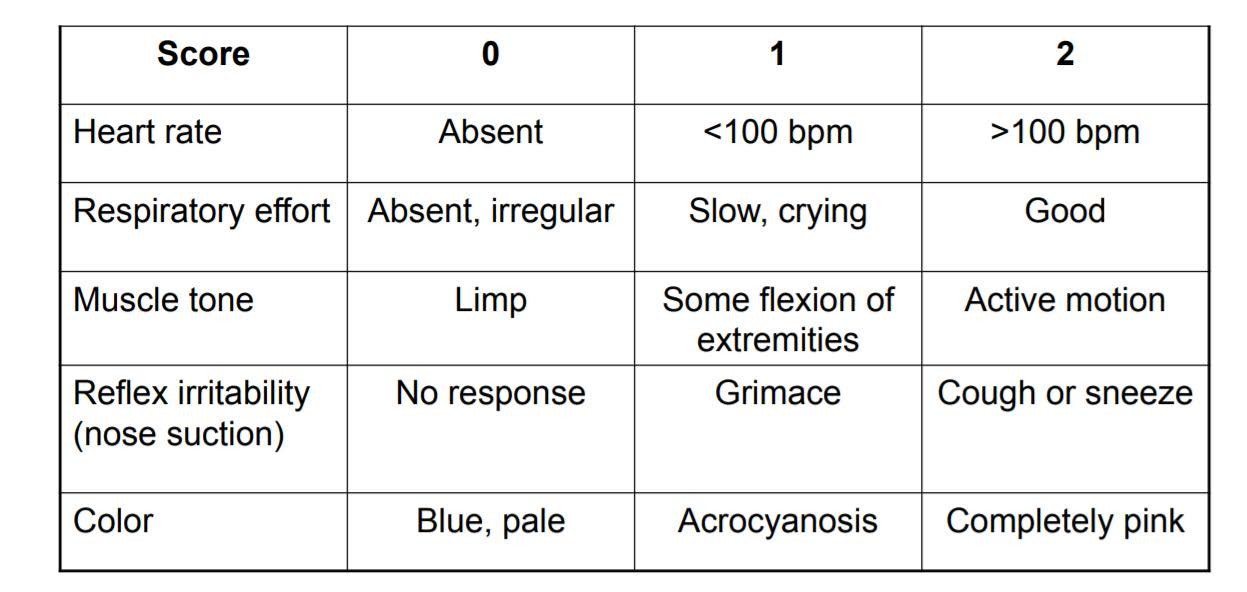
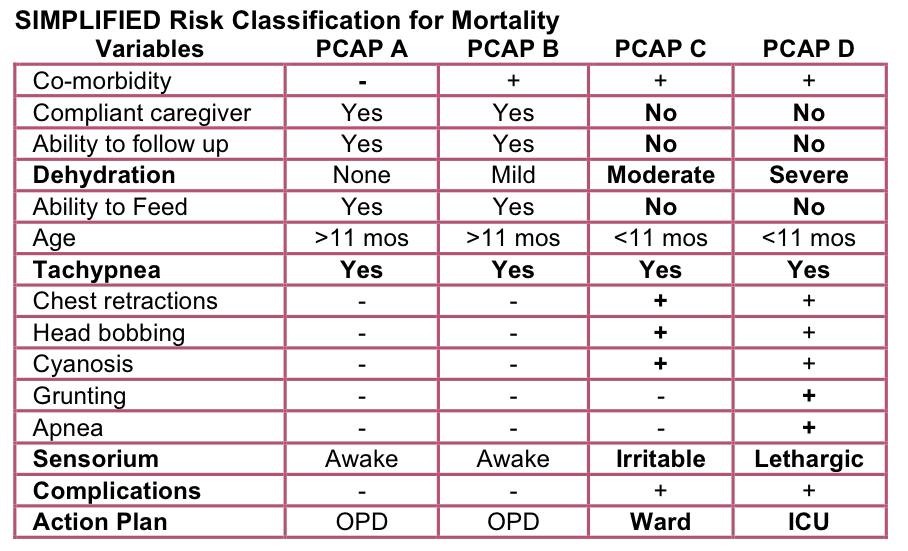
A 1-year-old child has cough, fever and mild dehydration. PPE: RR: 65 cpm, symmetrical chest expansion, no retractions, equal breath sounds with crackles on both lung fields. Your most likely impression is
PCAP C
PCAP D
PCAP A
PCAP B
Ingestion of this foreign body needs to be removed within 2 hours because it can induce mucosal injury in as little as 1 hour:
Button batteries
Coin
Sharp objects
Magnets
A 16-year-old was noted to have generalized seizure. History revealed that he was noted to have jerky movements in the morning and disappears about mid-morning. The drug of choice for this patient is:
Vigabatrin
Valproic Acid
Topiramate
Carbamazepine
You saw a patient at the ER with muffled heart sounds, hypotension and distended neck veins. What are the expected ECG findings in this patient?
Tall QRS complexes on left chest leads
QRS complexes within normal limits but with isolated ventricular arrhythmias
Normal ECG for age
Low voltage QRS complexes
This may be a case of acute pericarditis with pericardial effusion and signs of cardiac tamponade. The findings make up the Beck’s triad which is characteristic of cardiac tamponade.
This may be a case of acute pericarditis with pericardial effusion and signs of cardiac tamponade. The findings make up the Beck’s triad which is characteristic of cardiac tamponade.
The damaging pneumonitis caused by proximal blind esophageal atresia and distal TEF is best prevented by:
Surgical ligation
Aspiration of gastric content via distal fistula
Antibiotic therapy
Endotracheal intubation
The cornerstone in the management of purulent skin and soft tissue infections is
Culture of abscess
Drainage of Abscess
Topical Mupirocin
Antibiotics
The best management in a patient who has deepening jaundice and progressively elevated bilirubin levels despite phototherapy is:
Exchange transfusion
Continue phototherapy
Blood transfusion
Antibiotic treatment
RATIO:
Jaundice / Hyperbilirubinemia: Treatment
Phototherapy
o Works by structural and configurational photo-isomerization; photo-oxidation
o Maximum intensive phototherapy – uses blue lamps (420-470 nm), distance of 15-20 cm from infant, phototherapy blanket;
o Complications: Loose stools, rash, overheating, dehydration, Bronze Baby Syndrome (BBS)
Exchange transfusion (ET)
o Done if phototherapy fails; critical level for a particular infant may be an indication for ET during the 1st 2 days of life when further rise is expected, but not typically on D4 in term or D7 in the PT as hepatic conjugation matures
RATIO:
Jaundice / Hyperbilirubinemia: Treatment
Phototherapy
o Works by structural and configurational photo-isomerization; photo-oxidation
o Maximum intensive phototherapy – uses blue lamps (420-470 nm), distance of 15-20 cm from infant, phototherapy blanket;
o Complications: Loose stools, rash, overheating, dehydration, Bronze Baby Syndrome (BBS)
Exchange transfusion (ET)
o Done if phototherapy fails; critical level for a particular infant may be an indication for ET during the 1st 2 days of life when further rise is expected, but not typically on D4 in term or D7 in the PT as hepatic conjugation matures
This medication will promote closure of PDA in a preterm infant
Prostaglandin
Dopamine
Adenosine
Paracetamol
Ratio
Indomethacin, Ibuprofen and Paracetamol - These 3 drugs are used for medical closure of the PDA.
Indomethacin is less commonly used because of complications
Ratio
Indomethacin, Ibuprofen and Paracetamol - These 3 drugs are used for medical closure of the PDA.
Indomethacin is less commonly used because of complications
Which of the following describes the pathophysiology of Respiratory Distress Syndrome (RDS)?
Air leak
Granular membranes in bronchioles
Ball-valve effect
Microatelectasis
This condition should be highly suspected in patients with bronchopulmonary dysplasia not responding to therapy or with frequent exacerbation without clear triggers
Asthma
GERD
Cystic fibrosis
Chronic aspiration
Which is a consistent manifestation of intestinal obstruction in the newborn?
Abdominal distention
Constipation
Vomiting
Double bubble sign
Ratio:
Vomiting – Vomiting caused by obstruction of the GI tract is probably mediated by intestinal visceral afferent nerves stimulating the vomiting center. If obstruction occurs below the second part of the duodenum, vomitus is usually bile stained. Emesis can also become bile stained with repeated vomiting in the absence of obstruction when duodenal contents are refluxed into the stomach.
Nonobstructive lesions of the digestive tract can also cause vomiting; this includes diseases of the upper bowel, pancreas, liver, or biliary tree. CNS or metabolic derangements and cyclic vomiting syndrome can lead to severe, persistent emesis.
Double bubble sign- duodenal atresia
Constipation - Any definition of constipation is relative and depends on stool consistency,
stool frequency, and difficulty in passing the stool
Abdominal distention – enlargement of the abdomen which can result from diminished tone of the wall musculature or from increase content of fluid, gas, or solid
Ratio:
Vomiting – Vomiting caused by obstruction of the GI tract is probably mediated by intestinal visceral afferent nerves stimulating the vomiting center. If obstruction occurs below the second part of the duodenum, vomitus is usually bile stained. Emesis can also become bile stained with repeated vomiting in the absence of obstruction when duodenal contents are refluxed into the stomach.
Nonobstructive lesions of the digestive tract can also cause vomiting; this includes diseases of the upper bowel, pancreas, liver, or biliary tree. CNS or metabolic derangements and cyclic vomiting syndrome can lead to severe, persistent emesis.
Double bubble sign- duodenal atresia
Constipation - Any definition of constipation is relative and depends on stool consistency,
stool frequency, and difficulty in passing the stool
Abdominal distention – enlargement of the abdomen which can result from diminished tone of the wall musculature or from increase content of fluid, gas, or solid
What is the auscultatory finding of a patient with Rheumatic Heart Disease with Mitral Stenosis?
Systolic ejection murmur at the left upper sternal border
Diastolic rumbling murmur at the apex
Holosystolic murmur at the apex radiating to the back
Holosystolic murmur at the left lower sternal border accentuated by inspiration
Some babies are born small even if they are not premature due to complications of pregnancy such as hypertension or malnutrition. What will differentiate premature infants from those who are just small for gestational age?
Ballard’s scoring
Crib scoring
Apgar scoring
Last Menstrual Period (LMP)
RATIO:
Apgar score is useful for conveying information about the newborn’s overall status and response to resuscitation.
Crib scoring - predict initial risk of mortality amongst low birth weight babies
LMP – to determine AOG in pregnancy
RATIO:
Apgar score is useful for conveying information about the newborn’s overall status and response to resuscitation.
Crib scoring - predict initial risk of mortality amongst low birth weight babies
LMP – to determine AOG in pregnancy
The initial therapy of the toxic ingestion of this substance focuses on aggressive rehydration and correction of electrolyte abnormalities. Which substance is this?
Acetaminophen
Iron
Salicylate
Isoniazid
Which of the following correctly describes the principal characteristics of Kawasaki disease?
Polymorphic rash including maculopapular, erythema multiforme, bullous and vesicular
Bilateral conjunctival injection with limbal sparing and suppurative discharge
Nonsuppurative cervical lymphadenopathy, usually unilateral with node size more than 1.5 cm
Discrete lesions of the oral and buccal mucosa Ratio:
Ratio:
5 Principal Criteria of Kawasaki disease:
Fever for at least 5 days + at least 4 of the 5 principal features:
1. Conjunctival Injection - Bilateral, non-exudative, with limbal sparing
2. Erythema of the oral and pharyngeal mucosa - With strawberry tongue and red, cracked lips
3. Edema and erythema of the hands and feet - Acute – erythema and edema of hands and feet and
Subacute – periungual peeling of fingers, toes
4. Rash of various forms - Maculopapular, erythema multiforme, scarlatiniform, Polymorphic
except for the vesicular form
5. Cervical lymphadenopathy - Non-suppurative, usually unilateral, >1.5 cm in size
Ratio:
5 Principal Criteria of Kawasaki disease:
Fever for at least 5 days + at least 4 of the 5 principal features:
1. Conjunctival Injection - Bilateral, non-exudative, with limbal sparing
2. Erythema of the oral and pharyngeal mucosa - With strawberry tongue and red, cracked lips
3. Edema and erythema of the hands and feet - Acute – erythema and edema of hands and feet and
Subacute – periungual peeling of fingers, toes
4. Rash of various forms - Maculopapular, erythema multiforme, scarlatiniform, Polymorphic
except for the vesicular form
5. Cervical lymphadenopathy - Non-suppurative, usually unilateral, >1.5 cm in size
The following are characteristics of Streptococcal Pharyngitis EXCEPT:
Tender cervical lymphadenopathy
Beefy red throat
Hoarseness
Petechiae at the soft palate
Ratio:
Streptococcal Pharyngitis – Clinical manifestations
Rapid onset: prominent sore throat and fever
Headache and GIT symptoms are frequent
Pharynx is red (beefy red)
Enlarged Tonsils - Classically covered with a yellow, blood-tinged exudate
Petechiae or “doughnut” lesions on the soft palate and posterior pharynx
Uvula may be (beefy) red, stippled, and swollen
Anterior cervical lymph nodes are enlarged and tender
Ratio:
Streptococcal Pharyngitis – Clinical manifestations
Rapid onset: prominent sore throat and fever
Headache and GIT symptoms are frequent
Pharynx is red (beefy red)
Enlarged Tonsils - Classically covered with a yellow, blood-tinged exudate
Petechiae or “doughnut” lesions on the soft palate and posterior pharynx
Uvula may be (beefy) red, stippled, and swollen
Anterior cervical lymph nodes are enlarged and tender
Which of the following carbohydrates will not produce glucose during enzymatic hydrolysis at the brush borders of enterocytes?
Sucrose
Maltose
Lactose
Trehalose
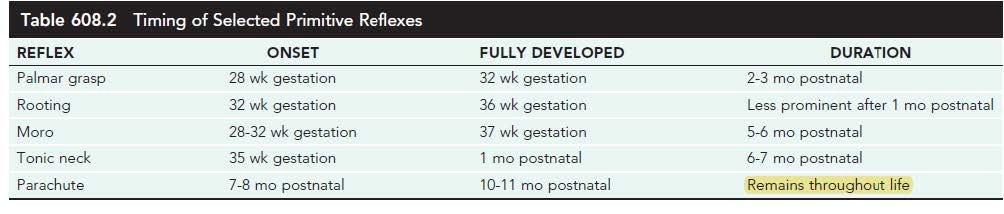
The only primitive reflex that gets modified in adulthood is
Parachute reflex
Asymmetric neck tonic reflex
Landau reflex
Hoffman’s reflex
Which of the following is the chest x-ray picture found in a patient with Transient Tachypnea of the Newborn?
Fine reticulogranularity, hyper aeration
Hyper aeration, flattened diaphragm
Low volume lungs, air bronchogram
Air bronchogram, pleural effusion
At birth, this term neonate should receive the following:
Hepatitis B vaccine 0.5 ml IM
Vit K 0.1 cc by IM
All choices are correct
Erythromycin ophthalmic ointment
The following are associated to both cleft lip and palate, EXCEPT:
Hearing loss
Misarticulation
Ethnicity
Genetics
{"name":"Pediatrics A Mock exam", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 4 y\/o male with nephrotic syndrome had proteinuria of +3 one day PTA. He now complains of dizziness and decreased urine output. BP was 60 palpatory. What is the best thing to do immediately?, NEPHROTIC SYNDROME MANAGEMENT Triad of clinical findings associated with nephrotic syndrome: 1. Hypoalbuminemia (≤2.5 g\/dL) 2. Edema 3. Hyperlipidemia (cholesterol >200 mg\/dL) Nephrotic Management Based sa platinum the first line of treatment for proteinuria is corticosteroids which is letter C. however, this is not for the acute management as you are required to correct the fluid imbalance first by giving IV albumin which is letter D. YOU DON’T GIVE IV FLUIDS because bale wala lang yun if there is persistent protein loss as there will be a continuous shift in the starling forces. Which rules out Letter B. Letter A. is for mema lang go ka na for letter D, Massive protein losses in nephrotic syndrome is due to injury of the:","img":"https://www.quiz-maker.com/3012/CDN/90-4386915/screenshot-690-.png?sz=1200-00328040000425005300"}
More Quizzes
Fair Use
6325
The Adrenaline Boredom Busting Quiz #1
20100
Do you have any recommendations in new papers today?
100
Which Apotelesma Realm Do You Belong In?
11613
Free Four Temperaments: Which Temperament Are You?
201027965
Which of the Following Is the Strongest Password? Free
201053617
Test Your Sales Logic: Free on Winning Sales Techniques
201082456
Free Text Structure
201023539
Think You Know Cameras? Take Our Camera & Prove It!
201045986
Which Starter Pokemon of Pokemon Black and White Are You?
201023729
Ace Your SPAB Certification: California Practice
201035165
Introduction to the Video Game Development Process
15823353