Part 20 (164)
Infectious Diseases Quiz
Test your knowledge of infectious diseases with this comprehensive quiz designed for healthcare professionals and students alike. With 164 carefully curated questions covering a range of topics, you'll be challenged to identify pathogens, understand mechanisms of disease, and apply clinical reasoning.
- Covers a variety of infectious diseases
- Great for exam preparation
- Ideal for medical students and healthcare professionals
A 31-year-old, HIV-infected man from New York presents to the ER with anorexia, malaise, night sweats, fever, and weight loss of 6.8kg (15 lb) over the past one month. He also has a cough productive of yellow sputum. He was diagnosed with HIV two years ago. When last checked two months ago, his CD4 count was 220/microL. He is not taking any medications. His temperature is 39.2°C (102.2°F), pulse is 96/min, and blood pressure is 120/80 mm Hg. Physical examination reveals rales in his right upper chest. Laboratory studies show: Hematocrit 30%, WBC count 3,400/microL, Neutrophils 86%, Bands 2%, Lymphocytes 4%, Monocytes 8%. PPD test shows 3 mm induration. Chest x-ray reveals a right upper lobe cavitation. Sputum examination shows partially acid-fast, filamentous, branching rods. Based on these findings, which of the following organism is the most likely cause of this patient's pulmonary disease?
Pneumocystis jiroveci
Mycobacterium tuberculosis
Coccidioides species
Nocardia species
Streptococcus pneumonia
A 45-year-old man comes to the office and complains of intermittent, bloody diarrhea and abdominal pain for the past month. During this time period, he has lost six pounds. He was diagnosed with HIV infection in the past, but has refused antiretroviral therapy. Laboratory results show a CD4 count of 50cells/µL. The stool examination is negative. Colonoscopy with biopsy shows multiple colonic ulcerations and mucosal erosions. The biopsy shows large cells containing eosinophilic intranuclear and basophilic intracytoplasmic inclusions. What is the most likely cause of this patient's diarrhea?
Cryptosporidium
Cytomegalovirus
Entamoeba
Kaposi sarcoma
Mycobacterium avium complex
A 73-year-old diabetic man presents with low-grade fever, facial pain over his right maxilla, and bloody nasal discharge for the last three days. For the last day, he has had diplopia. He was diagnosed with diabetes mellitus 10 years ago. For the last year, he has been on insulin. His most recent hemoglobinA1C was 12.0. His temperature is 39.0°C (102.2°F), pulse is 88/min, and blood pressure is 130/76mm Hg. Examination shows right-sided nasal congestion and necrosis of the right nasal turbinate with tenderness over the right maxillary sinus. There is chemosis and proptosis of his right eye. CT scan shows opacification of the right maxillary sinus. Which of the following is the most likely causative organism?
Rhizopus species
Staphylococcus aureus
Pseudomonas aeruginosa
Haemophilus influenzae
Moraxella catarrhalis
A 43-year-old HIV-positive male presents to your office with several exophytic purple skin masses on his lower abdomen. Physical examination reveals tender hepatomegaly and an abdominal CT scan shows nodular, contrast-enhanced intrahepatic lesions of variable size. Liver biopsy is attempted but severe hemorrhage results. Which of the following is the most likely cause of this patient's condition?
Mycobacteria
Spirochetes
Bartonella
Clostridia
Brucella
A 23-year-old, HIV-infected female presents with a five-day history of fever and productive cough. She is on antiretroviral therapy, and her CD4 count is 300/mm3. Her temperature is 39.0°C (102.5°F), pulse is 95/min, respirations are 22/min, and blood pressure is 115/76 mm Hg. Physical exam reveals dullness to percussion and bronchial breath sounds in the right lung base. Chest x-ray is shown below. What is the most likely cause of this patient's symptoms?
Streptococcus pneumonia
Mycobacterium tuberculosis
Disseminated coccidioidomycosis
Pneumocystis jiroveci (P. jiroveclj)
Pseudomonas aeruginosa
A 75-year-old female nursing home resident complains of cough and fever. Her past medical history is significant for hypertension, myocardial infarction (experienced two years ago), and a traumatic right foot amputation. Her current medications are atenolol, hydrochlorothiazide, and aspirin. Her temperature is 39.4°C (103°F), pulse is 110/min, respirations are 22/min, and blood pressure is 110/76 mmHg. Crackles are present at right lung base. Chest x-ray reveals a right lower lobe infiltrate. Which of the following pathogens is the most likely cause of this patient's condition?
Staphylococcus aureus
Streptococcus pneumoniae
Haemophilus influenzae
Anaerobic bacteria
Gram-negative rods
A 45-year-old man presents to the emergency room with a two-day history of fever, dyspnea, abdominal pain, and diarrhea. He has no chest pain, but complains of dry cough. His past medical history is significant for bone marrow transplantation for acute myeloid leukemia (AML) three months ago. His temperature is 39°C (102.2°F), blood pressure is 122/80 mm Hg, pulse is 98/min, and respirations are 22/min. Exam of the oropharynx reveals thrush. Lungs exam demonstrates bilateral diffuse rales. Heart sounds are regular. Nonspecific abdominal tenderness is present. The chest radiograph shows multifocal, diffuse patchy infiltrates. Which of the following is the most likely cause of this patient's current condition?
Mycoplasma pneumoniae
Pneumocysfis jiroveci
Graft-versus-host disease
Cytomegalovirus
Aspergillus fumigatus
A 55-year-old woman presents with a three-week history of low-grade fever, weight loss of 4.5kg (10 lb), and malaise. She is known to have mitral valve prolapse, but is otherwise healthy. She underwent a tooth extraction one month ago. She denies alcohol, tobacco, and illicit drug use. Her temperature is 38.5°C (101.3°F), pulse is 90/min, respirations are 18/min, and blood pressure is 145/76 mm Hg. Her chest is clear to auscultation and percussion. Cardiac examination reveals a III/IV holosystolic murmur at the apex that radiates to the axilla. Chest x-ray is normal. Urinalysis is unremarkable. Blood cultures are drawn and empiric antibiotics are started. Echocardiogram shows mitral regurgitation with vegetation on the mitral valve. Which of the following organisms is the most likely cause of this patient's condition?
Staphylococcus aureus
Staphylococcus epidermidis
Staphylococcus saprophyticus
Viridans group streptococci
Enterococcus species
A 50-year-old man presents to the office with fatigue, malaise, and disabling joint pain in his fingers, wrists, shoulder, hips, knees, and ankles. His pain is severe and associated with a mild degree of morning stiffness for 10-15 minutes. He occasionally takes acetaminophen and ibuprofen for this pain. He has a 10-pack-year smoking history. He does not drink alcohol. Family history includes an uncle who died of liver cancer. On examination, there is grayish skin pigmentation, most prominent on the exposed parts. Abdominal examination is significant for liver enlargement 2 cm below the costal margin. Laboratory studies reveal the following: Hemoglobin 13.0 g/L, Leukocyte count 5,500/mm3, Serum creatinine 0.8 mg/dl, Blood glucose 218mg/dl, Aspartate aminotransferase (SGOT) 128 U/L, Alanine aminotransferase (SGPT) 155 U/L, Alkaline phosphatase 120 U/L , Serum iron 450 mol/L (50-170g/dL), Transferrin saturation of iron 62% (22-47%), Serum Ferritin 3000ng/L (15-200 ng/ml, males). X-ray of the joints shows narrowing of joint spaces and diffuses demineralization. This patient's condition makes him more vulnerable to which of the following infections?
Listeria monocytogenes
Streptococcus pneumoniae
Escherichia coli
Chlamydia psittaci
Epstein Barr virus
A 19-year-old white male presents with nausea, vomiting, and abdominal cramps. He has had four episodes of vomiting over the last two hours. He has not had diarrhea or fever. Four hours ago, he ate a salad from a local restaurant. His pulse is 82/min, blood pressure is 120/80 mm Hg, and temperature is 37.2°C (99°F). Abdominal and rectal examinations are unremarkable. Which of the following is the most likely cause of this patient's symptoms?
Staphylococcus aureus
Bacillus cereus
Clostridium perfringens
Clostridium difficile
Enterotoxigenic E coli
A 72-year-old male presents with a two-day history of intense pain in his right ear, along with ear discharge. The pain is so severe that he is unable to sleep. It radiates to his temporomandibular joint and is aggravated by chewing. His disease has worsened despite the use of topical antibiotics. He takes metformin and enalapril. On physical examination, granulation tissue is noted in the lower part of his external auditory canal. Cranial nerves are intact. Oropharynx is clear without exudate. Which of the following is the most likely causative organism of this patient's ear condition?
Pseudomonas aeruginosa
Staphylococcus aureus
Bacteroides species
Peptostreptococcus species
Aspergillus fumigatus
A 26-year-old male presents to your office with periodic flank pain. He also noticed that his urine was red during the last several days. He is known to be HIV-positive. One month ago, he presented with thrush. At that time, he was found to have a CD4 count of 100, and was started on anti-retroviral therapy. His current CD4 count is 250. Physical examination reveals no oral cavity lesions. The lungs are clear on auscultation. The serum creatinine level is 2.2 mg/dl. Urinalysis shows hematuria and needle-shaped crystals in the sediment. Which of the following is the most likely cause of this patient's current condition?
Nucleoside reverse transcriptase inhibitor (NRTI)
Non-nucleoside reverse transcriptase inhibitor (NNRTI)
Protease inhibitor
Viral infection
Neoplastic process
A 12-year-old boy is brought to the emergency department because of severe pain near his left knee. He has sickle cell disease, and has been hospitalized previously for sickle cell crisis. Vital signs are notable for mild fever. Examination of the left lower extremity reveals a normal knee joint with marked tenderness and swelling over the proximal tibia. Labs show leukocytosis and elevated ESR. He is subsequently diagnosed with osteomyelitis. Which of the following organisms is the most likely cause of his condition?
Escherichia coli
Pseudomonas species
Salmonella species
Staphylococcus aureus
Group B streptococcus
A 67-year-old man presents to his primary care provider in January with fever and a productive cough. The patient had been seen ten days earlier with complaints of fever to 102°F (39.0°C), myalgias, rhinorrhea, and dry cough. At that time, his lung exam revealed occasional crackles. He was given a medication and told to follow up if his symptoms worsened. The symptoms did remit over the first five days, but he began to feel worse again two days ago. He smokes a half-pack of cigarettes per day and drinks alcohol several times a week. On exam today, his temperature is 102.3°F (39.3°C), and lung exam reveals increased tactile fremitus in the left lower lobe. What is the most likely pathogen responsible for his current condition?
Pneumocystis jiroveci
Klebsiella pneumoniae
Pseudomonas aeruginosa
Mycoplasma pneumoniae
Staphylococcus aureus
A 33-year-old man presents with low-grade fever, abdominal cramps, and diarrhea for the past six hours. He has had eight episodes of loose, watery stool containing blood and mucus over this time period. Last night, he ate shrimp and crab meat at a local restaurant. His current pulse is 85/min, blood pressure is 110/80 mm Hg, and temperature is 37.7°C (99.9°F). There are no significant findings on abdominal or rectal examinations. Stool examination shows numerous red blood cells and leukocytes. Which of the following is the most likely causative organism of this patient's condition?
Shigella species
Enterohemorrhagic E coli
Vibrio parahaemolytious
Yersinia enterocolitica
Campylobacter jejuni
A 46-year-old farmer comes to the physician because of pain and swelling of his right heel. He accidentally stepped on a rusty nail while working 2 weeks ago. Although he applied over the-counter antibiotic cream locally and took acetaminophen orally, he continued to have pain at the site of the injury. He has no other medical problems and takes no medication. He has no known drug allergies. He smokes 2-3 cigarettes a day and drinks alcohol occasionally. His temperature is 38.3°C (101°F), blood pressure is 140/90 mm Hg, pulse is 84/min and respirations are 14/min. On examination, the right heel is swollen, red, and warm and tender to touch. A small puncture wound is visible. Laboratory reports show mild leukocytosis. X-ray of the right foot shows features suggestive of osteomyelitis. The most likely cause of the patient's symptoms is infection with which of the following?
Beta-hemolytic streptococci
Staphylococcus epidermidis
Clostridium tetani
Pseudomonas aeruginosa
Escherichia coli
A 31-year-old, HIV-infected man from New York presents to the ER with anorexia, malaise, night sweats, fever, and weight loss of 6.8kg (151b) over the past one month. He also has a cough productive of yellow sputum. He was diagnosed with HIV two years ago. When last checked two months ago, his CD4 count was 220/microL. He is not taking any medications. His temperature is 39.2°C (102.2°F), pulse is 96/min, and blood pressure is 120/80mm Hg. Physical examination reveals rales in his right upper chest. Laboratory studies show: Hematocrit 30%, WBC count 3,400/microL, Neutrophils 86%, Bands 2%, Lymphocytes 4%, Monocytes 8%. PPD test shows 3 mm induration. Chest x-ray reveals a right upper lobe cavitation. Sputum examination shows partially acid-fast, filamentous, branching rods. Based on these findings, which of the following organism is the most likely cause of this patient's pulmonary disease?
Pneumocystis jiroveci
Mycobacterium tuberculosis
Coccidioides species
Nocardia species
Streptococcus pneumonia
A 26-year-old man comes to his physician with a two-week history of fatigue, fever, muscle aches, and arthralgias. He denies any weight loss. His temperature is 37.7°C (99.9°F), blood pressure is 115/75 mm Hg, respirations are 14/min, and pulse is 75/min. Physical examination is unremarkable, except for splenomegaly. Laboratory studies show: Hemoglobin 13 gm/dL, WBC count 12,000/microL, Neutrophils 22%, Lymphocytes 70%, Monocytes 5%, Basophils 1%, Eosinophils 2%, Platelet count 220,000/microL. Peripheral blood smear shows large basophilic lymphocytes with a vacuolated appearance. Heterophile antibody test is negative. What is the most likely cause of this patient's symptoms?
Chronic fatigue syndrome
Cytomegalovirus infection
Acute toxoplasmosis
Mycobacterial infection
Chronic lymphocytic leukemia
A 27-year-old man presents with symptoms of fever, chills, malaise, and joint discomfort in his hands and knees. He looks unwell, his temperature is 39.4°C, blood pressure 115/70 mm Hg, pulse 110/min, head and neck is normal, and his jugular venous pressure (JVP) has a prominent c-v wave. There is also a 3/6 pan-systolic murmur heard at the right sternal border that increases with respiration. His lungs are clear, abdomen is soft, and hand joints are normal. He has multiple puncture sites on his forearms from injection drug use. Which of the following is the most likely causative organism?
Staphylococcus aureus
Staphylococcus epidermidis
Streptococcus viridans
Enterococci
Candida
A 73-year-old man from a nursing home develops headache, fever, cough, sore throat, malaise, and severe myalgia during a community outbreak affecting numerous other residents at the home. The symptoms gradually resolve after 3 days, and he starts feeling better but then there is a reappearance of his fever, with cough and yellow sputum production. On examination, his temperature is 38.5°C, pulse 100/min, respiration 24/min, oxygen saturation 88% and crackles in the right lower lung base, bronchial breath sounds and dullness on percussion. CXR reveals a new infiltrate in the right lower lobe. Which of the following is the most likely causative organism?
Primary viral pneumonia
An autoimmune reaction
Mycoplasma pneumoniae
Streptococcus pneumoniae
Neisseria catarrhalis
A 56-year-old man is having intermittent fevers and malaise for the past 2 weeks. He has no other localizing symptoms. Two months ago, he had valve replacement surgery for a bicuspid aortic valve. A mechanical valve was inserted and his postoperative course was uncomplicated. On examination, his temperature is 38°C, blood pressure 124/80 mm Hg, pulse 72/min, and head and neck are normal. There is a 3/6 systolic ejection murmur, the second heart sound is mechanical, and a 2/6 early diastolic murmur is heard. The lungs are clear and the skin examination is normal. Three sets of blood cultures are drawn and an urgent echocardiogram is ordered. Which of the following is the most likely causative organism?
Staphylococcus aureus
S. epidermidis
S. viridans
Enterococci
Candida
A 25-year-old woman is admitted with fever and hypotension. She has a 3-day history of feeling feverish. She has no history of chronic disease, but she uses tampons for heavy menses. She is acutely ill and, on physical examination, found to have a diffuse erythematous rash extending to palms and soles. She is confused. Initial blood tests are as follows: White blood cell count: 22,000/μL, Na+: 125 mEq/L, K+: 3.0 mEq/L, Ca++: 8.0 mEq/mL, Activated partial thromboplastin time (PTT): 65 (normal 21 to 36), Prothrombin time (PT): 12s (normal < 15s), Aspartate aminotransferase: 240 U/L (normal < 40), Creatinine: 3.0 mg/dL, Antinuclear antibodies: negative, Anti-DNA antibodies: negative, Serologic tests for RMSF, leptospirosis, measles: negative. Which of the following best describes the pathophysiology of the disease process?
Acute bacteremia
Toxin-mediated inflammatory response syndrome
Exacerbation of connective tissue disease
Tick-borne rickettsial disease
Allergic reaction
A 21-year-old woman visits her physician because of 3 weeks of a flu-like‖ illness. She reports symptoms of malaise, fever, fatigue, and a sore throat. There is no weight loss or night sweats, and she has not traveled out of country. Her past medical history is not significant and she is not taking any medications. Physical examination is normal except for enlarged cervical lymph nodes. Laboratory data show hemoglobin 13.2 g/dL; hematocrit 42%; platelets 380,000/mL; WBC 8500/mL, with 35% segmented neutrophils, 1% eosinophils, and 64% lymphocytes, of which 36% were atypical. A heterophil antibody (sheep cell agglutination) test is negative. Which of the following is the most likely causative organism?
Herpes simplex
Echovirus
CMV
Coxsackievirus
Reovirus
A 4-year-old boy is sent to the emergency room because of clinical suspicion of meningitis. He has been ill for 2 days with fever and lethargy. On examination, he is febrile, the neck is stiff, and papilledema is present. There is no rash, the lungs are clear, and heart sounds normal. Which of the following is the most likely causative organism?
Neisseria meningitidis
Streptococcus pneumoniae
Haemophilus influenzae
Staphylococcus
Listeria species
A 24-year-old woman presents with chills and rigors. She looks unwell, and her temperature is 39.4°C, blood pressure 100/60 mm Hg, pulse 110/min, and oxygen saturation 95%. There is a 3/6 pansystolic murmur at the right sternal border, which increases with inspiration. Her arms have multiple tattoos and needle marks from injection drug use. Blood cultures (2/2 sets) are positive for S. aureus, and she is started on appropriate antibiotics. Her renal function is mildly impaired and her urinalysis is positive for protein, and microscopy reveals red cell casts. Which of the following mechanisms is the most likely explanation for her renal abnormalities?
Septic emboli
Cardiac failure with prerenal azotemia
A high level of circulating immune complexes
Fungal disease
Inevitable progression to renal failure
A recent outbreak of severe diarrhea is currently being investigated. Several adolescents developed bloody diarrhea, and one remains hospitalized with acute renal failure. A preliminary investigation has determined that all the affected ate at the same restaurant. The food they consumed was most likely to be which of the following?
Pork chops
Hamburger
Gefilte fish
Sushi
Soft-boiled eggs
A 23-year-old woman presents with a painless chronic vulvar ulcer. She recently arrived to study in the United States from Southern India. The lesion began as a papule and then ulcerated. It has persisted for several months. Currently, physical examination reveals a painless elevated area of beefy red, friable granulation tissue. She has been sexually active for several years. Which of the following is the most likely causative organism?
Spirochete
Gram-positive coccus
Intracellular Gram-negative bacteria
Chronic viral infection
Fungus
An 18-year-old man develops fever, neck stiffness, and headache. On examination, his blood pressure is 105/80 mm Hg, pulse 100/min, temperature 38.7°C, and neck flexion is very painful. The ears, throat, and sinuses are normal; there are no focal neurologic signs, and the remaining examination is normal. His is the second case of meningitis in his university dormitory building. Which of the following is the most likely causative organism?
Neisseria meningitidis
Streptococcus pneumoniae
Haemophilus influenzae
Staphylococcus
Listeria species
A 19-year-old woman was traveling in a rural area of South America. She returned 3 weeks ago and, over the past few days, has gradually developed lower abdominal pain and diarrhea. Now the symptoms are much worse with 10 stools a day consisting mostly of mucus and blood. She is afebrile, the abdomen is tender in left lower quadrant, and the remaining examination is normal. Her stool is mostly comprised of blood and mucus. Which of the following is the most likely causative organism?
Escherichia coli infection
Salmonella infection
Shigella infection
Vibrio parahaemolyticus infection
E. Histolytica infection
An 18-year-old man develops fever, neck stiff- ness, and headache. On examination, his blood pressure is 110/80 mm Hg, pulse 100/min, temperature 38.7°C, and neck flexion is very painful. The ears, throat, and sinuses are normal; there are no focal neurologic signs; and the remaining examination is normal. There are no reported similar cases in the community. Which of the following is the most likely causative organism?
Neisseria meningitides
Streptococcus pneumoniae
Haemophilus influenzae
Staphylococcus
Listeria species
A previously well 28-year-old female has developed gradual onset of fever and malaise over 2–3 weeks. She also complains of arthralgias and myalgias. Repeated measurement of her temperature reveals a low grade fever between 38°C and 39°C. Physical examination reveals an oval retinal hemorrhage with a clear, pale center; a pansystolic cardiac murmur heard best at the apex; and small, tender nodules on her fingertips. Which of the following is the most likely causative organism?
Staphylococcus aureus
S. epidermidis
Viridans streptococci
Enterococcus
Candida
A 70-year-old patient with long-standing type 2 diabetes mellitus presents with complaints of pain in the left ear with purulent drainage. On physical examination, the patient is afebrile. The pinna of the left ear is tender, and the external auditory canal is swollen and edematous. The white blood cell count is normal. Which of the following organisms is most likely to grow from the purulent drainage?
Pseudomonas aeruginosa
Streptococcus pneumoniae
Candida albicans
Haemophilus influenzae
Moraxella catarrhalis
Three hours after a church social, eight people develop severe diarrhea. Other symptoms included nausea, vomiting, and abdominal cramps. Food served included chicken salad and cream-filled pastries. All affected individuals had the chicken salad. Which of the fol- lowing is the most likely causative organism?
Staphylococcal enterotoxin
C. botulinum
Clostridium perfringens
Salmonella species
Ptomaine poisoning
A 9-year-old boy has a severe sore throat with fever and dysphagia. On examination, there are grayish-white papulovesicular lesions on an erythematous base that ulcerate. They are located on the soft palate, anterior pillars of the tonsils and uvula. There are no lesions on the gingiva, tongue, or lips. A clinical diagnosis of herpangina is made. Which of the following is the most likely causative organism?
Measles (Morbillivirus)
Rubella (rubivirus)
Coxsackievirus A
HSV-1
HSV-2
A 10-year-old boy presents with fever, headache, photophobia, and neck discomfort in the middle of summer. He is alert and oriented, but has neck pain with flexion and extension of the head. His fundi are normal, and there are no focal neurologic findings or skin changes. A lumbar puncture reveals normal protein and glucose with a cell count of 240/mL (90% lymphocytes). Which of the following is the most likely causative organism?
Enterovirus (coxsackievirus or echovirus)
Streptococcus pneumoniae
Neisseria meningitides
Listeria monocytogenes
HSV-1
A 60-year-old man presents with fever and malaise 6 weeks after mitral valve replacement. On examination, his temperature is 38°C, blood pressure 130/80 mm Hg, pulse 80/min, and a loud pansystolic murmur at the apex, which radiates to the axilla. He has no skin or neurologic findings. Which of the following is the most likely causative organism?
Staphylococcus aureus
A fungus
Staphylococcus saprophyticus
Pneumococcus
Staphylococcus epidermidis
A previously healthy 25-year-old music teacher develops fever and a rash over her face and chest. The rash is itchy and, on examination, involves multiple papules and vesicles in varying stages of development. One week later, she complains of cough and is found to have an infiltrate on x-ray. Which of the following is the most likely etiology of the infection?
Streptococcus pneumoniae
Mycoplasma pneumoniae
Histoplasma capsulatum
Varicella-zoster virus
Gonococcus pneumoniae
A 19-year-old male has a history of athlete’s foot but is otherwise healthy when he develops sudden onset of fever and pain in the right foot and leg. On physical examination, the foot and leg are fiery red with a welldefined indurated margin that appears to be rapidly advancing. There is tender inguinal lymphadenopathy. The most likely organism to cause this infection is which of the following?
Staphylococcus epidermidis
Tinea pedis
Streptococcus pyogenes
Mixed anaerobic infection
Alpha-hemolytic streptococci
A 60-year-old woman comes to the physician because of a 3-month history of worsening fatigue and back pain. She has had diabetes mellitus for the past three years, and hypertension for the past ten years. Laboratory studies show: Hb 9.0 mg/dL, Serum calcium 11.2 mg/dL, Serum phosphorus 3.5 mg/dL, BUN 38 mg/dL, Serum creatinine 2.0 mg/dL. Which of the following is the most likely cause of this patient's renal failure?
Hypertension
Diabetes mellitus
Para protein
Primary hyperparathyroidism
Renal artery stenosis
A 70-year-old man comes to the physician due to a 4-6 month history of "almost continuous urinary dribbling." This symptom is present both day and night, and is progressively getting worse. He denies dysuria and hematuria. He has a 20-year history of diabetes mellitus-type 2, hypertension, alcoholic hepatitis and coronary artery disease. He had a gastric emptying study done a few weeks ago because of continuous nausea and early satiety. He had laser photocoagulation of both eyes for diabetic retinopathy. He has smoked one pack of cigarettes daily for 50 years, and drinks 4 to 6 beers daily. He takes NPH insulin, regular insulin, metformin, aspirin, metoprolol, lisinopril and metoclopramide. His vital signs are stable. Physical examination shows a well-appearing man. Pertinent physical findings are a normal sized prostate, decreased sensation in both legs below the knees, and absent Achilles tendon and knee reflexes bilaterally. Fecal occult blood test is negative. Postvoid residual volume is 550 ml. Urinalysis shows: Specific gravity 1.020, Blood trace, Glucose positive, Ketones negative, Protein moderate, Leukocyte esterase negative, Nitrites negative, WBC 1-2/hpf, RBC 3-4/hpf. Which of the following is the most likely cause of this patient's incontinence?
Multiinfarct dementia
Overflow incontinence due to detrusor weakness
Overflow incontinence from bladder outlet obstruction
Urinary tract infection
Overflow incontinence due to medication
A 46-year-old man complains of right flank discomfort. He describes decreased urination over the last week with occasional episodes of high urine output and weakness. He is otherwise healthy. There is no family history of renal disease. On physical examination, his blood pressure is 140/90 mmHg and his heart rate is 80/min. The serum creatinine level is 2.1 mg/dl. Urinalysis shows few red blood cells, white blood cells, trace protein, and no casts. Which of the following is the most likely cause of his complaints?
Hematologic malignancy
Renal artery stenosis
Inherited renal disease
Interstitial nephritis
Urinary outflow obstruction
A 17-year-old man comes to the emergency department and complains of intensive left flank pain that radiates to the groin. He refers to his symptom as "stone passage," which he has experienced "for so many times since childhood." His uncle has the same problem. Urinalysis shows hexagonal crystals. The urinary cyanide nitroprusside test is positive. Which of the following is the most likely cause of this patient's condition?
Amino acid transport abnormality
Parathyroid adenoma
Abnormality of uric acid metabolism
Excessive intestinal reabsorption of oxalate
Infection
) A 12-year-old girl comes to the physician because of a 2-day history of periorbital edema and abdominal distention. She has no other complaints. She has never been diagnosed with hypertension. Her father died at the age of 40, with renal failure. Her temperature is 37.1°C (98.9°F), blood pressure is 125/75 mm Hg, pulse is 80/min, and respirations are 14/min. Examination shows facial puffiness, shifting dullness, and 1+ bilateral pitting pedal edema. Urinalysis shows 3+ proteinuria and lipid laden casts. 24-hour urinary protein excretion is 5 g/day, total serum protein is 4.5 g/dl and serum albumin is 2.3 g/dl. Which of the following is this patient at increased risk of developing?
Macrocytic normochromic anemia
Accelerated atherogenesis
Hypergammaglobulinemia
Hypercalcemia
Hypoparathyroidism
A 20-year-old man is brought to the emergency department by his mother because of a one-day history of fever, headache, and altered mental status. He has no history of medical illness. Herpes simplex encephalitis is suspected after cerebral spinal fluid analysis shows lymphocytic pleocytosis, elevated protein level, and normal glucose level; in addition, CT scan shows contrast enhancement in the temporoparietal area. High-dose intravenous acyclovir therapy is started. Two days after the beginning of the therapy, the neurologic status improves, but the patient develops oliguria. Laboratory studies show: Serum sodium 140 mEq/L, Serum potassium 4.5 mEq/L, Serum creatinine 2.8 mg/dl, BUN 25 mg/dl. Which of the following is the most likely cause of renal damage in this patient?
Prerenal azotemia
Renal tubular obstruction
Glomerular injury
Interstitial nephritis
Bladder neck obstruction
A 65-year-old male has been having a non-productive, hacking cough for over a week. He takes an over-the-counter medication containing guaifenesin and diphenhydramine in an effort to improve his symptoms. The next day, he complains of lower abdominal discomfort and difficulty voiding. Which of the following most likely accounts for this patient's new complaint?
Detrusor inactivity
Urethral obstruction
Detrusor-sphincter dyssynergia
Overactive bladder
Abdominal muscle weakness
A 12-year-old girl is brought to the clinic due to a 2-month history of headaches. Her headaches last 1-2 hours and have no fixed time of occurrence. She denies nausea, vomiting, chills or fevers. She has no other medical problems and takes no medication. Her family history is significant for hypertension and diabetes. Her blood pressure is 156/90 mm Hg, pulse is 80/min, and respirations are 14/min. Examination shows an alert child in no distress. There is a soft to-and-fro bruit heard at the right costovertebral angle. Which of the following is the most likely cause of her hypertension?
Coarctation of aorta
Renal artery atherosclerosis
Pheochromocytoma
Fibromuscular dysplasia
Conn's syndrome
A 59-year-old man comes to the physician because of dysuria, urinary urgency, and frequency. He also complains of hematuria, nocturia, decreased force of stream, and a feeling of incomplete voiding. These symptoms have been present for more than a month. For the past few days he has been experiencing dull, non-radiating suprapubic pain. He has also been having low-grade fever and malaise for the past couple of days. He has been taking analgesics for osteoarthritis of his right knee for more than 10 years. He has a 40-pack-years history of cigarette smoking and does not use alcohol or drugs. Rectal examination shows a smooth, firm enlargement of the prostate without induration or asymmetry. Neurological examination shows no abnormalities. Urinalysis shows hematuria with isomorphic red blood cells. Laboratory studies show a serum creatinine of 1.5 mg/dl, and a PSA of 2 ng/ml. Which of the following is the most likely explanation for this patient's symptoms?
Benign prostatic hyperplasia
Carcinoma of bladder
Carcinoma of prostate
Urethral stricture
Neurogenic bladder
An 80-year-old female is brought from a nursing home with a two day history of poor oral intake and lethargy. Her past medical history is significant for hypertension, diabetes mellitus, coronary artery disease with coronary stenting two years ago and Alzheimer's disease. She was hospitalized six months ago with pneumonia. Her current medications are aspirin, lisinopril, metoprolol, hydrochlorothia zide, metformin and memantine. Her blood pressure is 95/60 mmHg and heart rate is 90/min. Physical examination reveals fine crackles at the right lung base. Her mucous membranes are dry. Her laboratory findings are significant for WBC of 15,000/mm3, creatinine of 2.1 and BUN of 61 mg/dl. Her creatinine was 0.9 mg/dl during the last admission. Which of the following is the best explanation for the abnormal laboratory findings in this patient?
Age-related renal function decline
Renal inflammatory infiltration
Renal tubular dysfunction
Renal vasoconstriction
Obstructive uropathy
A 60-year-old man comes to the physician because of worsening fatigue and nausea. He had a carotid angiogram for the evaluation of symptomatic carotid artery stenosis 15 days ago, and was discharged home three days after the procedure. His medical problems are hypercholesterolemia, coronary artery disease, intermittent claudication, hypertension for 18 years, and diabetes mellitus for 15 years. Physical examination shows painless, reddish-blue mottling of the skin of the extremities. Laboratory studies show: Hb 10.5 g/dl, WBC 10,000/cmm with 12% eosinophils, BUN 46 mg/dl, Serum creatinine 3.0 mg/dl, Serum C3 level Decreased. Urinalysis:pH Normal,Esterase Negative, Nitrite Negative, Protein 1+, WBC Many eosinophils, RBC 1-2/HPF. Which of the following is the most likely cause of this patient's findings?
Contrast nephropathy
Cholesterol embolism
Diabetic nephropathy
Post streptococcal glomerulonephritis
Acute allergic interstitial nephropathy
A 40-year-old man comes to the physician because of a two-week history of fatigue, lower extremity edema and dark urine. He has no history of serious illnesses. He takes no medications. He does not use tobacco, alcohol, or drugs. His blood pressure is 130/80 mm Hg and pulse is 80/min. Physical examination shows symmetric pitting edema of lower extremities. Laboratory studies show a serum creatinine level of 1.1 mg/dl. Urinalysis shows 4+ proteinuria and microhematuria. Light microscopy of the specimen obtained from kidney biopsy shows dense deposits within glomerular basement membrane that stain for C3, not immunoglobulins. Which of the following is the most likely pathophysiologic mechanism that explains this patient's condition?
Anti-GBM antibodies
Circulating immune complexes
Persistent activation of the alternative complement pathway
Cell-mediated injury
Non-immunologic damage
A 65-year-old male comes to the physician's office after noticing blood in his urine. He denies any abdominal pain or dysuria. He denies any recent illness. The review of systems is otherwise unremarkable. His past medical history is significant for hypertension and a transient ischemic attack. He takes a baby aspirin and hydrochlorothiazide daily. His temperature is 36.7°C (98°F), blood pressure is 130/86 mm Hg, pulse is 80/min and respirations are 16/min. A complete physical examination is unremarkable. Which of the following is the most likely cause of his symptoms?
Polycystic kidney disease
Renal cell carcinoma
Bladder mass
Acute glomerulonephritis
Schistosoma infection
A 62-year-old woman presents to your office complaining of urinary frequency and burning during urination. She denies fever, chills, nausea, back pain or abdominal pain. Her past medical history is significant for a long history of diabetes mellitus and hypertension. She does not use tobacco or consume alcohol. Her blood pressure is 160/100 mmHg and her heart rate is 70/min. Her hematocrit is 43% and her WBC count is 8,500/mm3 Urinalysis reveals the following: Glucose negative, Ketones negative, Nitrates positive, Protein 2+, WBC 20-25/hpf, RBC 3-5/hpf. She is given a three-day course of levofloxacin. Urinalysis two weeks later reveals 2+ protein but no nitrates, WBCs, or RBCs. Which of the following is most likely responsible for her persistent urinalysis abnormality?
Atherosclerotic narrowing of the renal arteries
Glomerular basement membrane changes
Cystic transformation of the renal parenchyma
Parenchymal atrophy due to calyceal dilation
Insoluble crystal precipitation in the tubular lumen
A 60-year-old man comes to the physician because of a 2-day history of fever and left-sided scrotal pain. The pain has progressed in severity and it radiates to the flank. His has also had increased urinary frequency and urgency along with dysuria. His temperature is 38.1°C (100.8°F), blood pressure is 130/75mm Hg, pulse is 86/min, and respirations are 15/min. Physical examination shows left scrotal swelling and a tender scrotal mass; there is no urethral discharge. Rectal examination shows a tender prostate. Laboratory studies show a WBC count of 14,000/microl with a left shift. Urinalysis shows bacteriuria and pyuria. Which of the following is the most likely organism responsible for this patient's findings?
Escherichia coli
Pseudomonas
Chlamydia trachomatis
Gonococcus
Staphylococcus aureus
A 40-year-old man comes to the physician because of increasing urinary frequency and urgency. He has had these symptoms in the past, but they are more troublesome now. He has also had urinary hesitancy and interruption of flow. His temperature is 37°C (98.6°F), blood pressure is 130/75mm Hg, pulse is 76/min, and respirations are 15/min. Physical examination shows no abnormalities except increased tone of the anal sphincter and mild periprostatic tenderness. Urinalysis and urine culture shows no abnormalities and expressed prostatic secretions show a leukocyte count of four WBCs/HPF (normal is less than 10 WBCs/HPF). Serum prostate-specific antigen is 2 ng/ml (normal value is less than 4ng/ml). Which of the following is the most likely diagnosis?
Chronic bacterial prostatitis
Inflammatory chronic prostatitis
Non-inflammatory chronic prostatitis
Prostatic cancer
Acute bacterial prostatitis
A 16-year-old girl presents with a 2-day history of lower abdominal discomfort, burning micturition and increased frequency of urination. She had her first sexual intercourse last week. Her vital signs are stable. Examination shows suprapubic tenderness. Urinalysis shows positive nitrites, positive esterase, 50+ WBC, and many bacteria. Which of the following is the most likely mechanism responsible for her clinical condition?
Sexual transmission
Hematogenous spread of infection
Lymphatic spread of infection
Poor genital hygiene
Ascending infection
A 68-year-old Caucasian man is admitted with a diagnosis of left lower lobe pneumonia, and is started on gatifloxacin. He has a long history of diabetes, hypothyroidism, hypercholesterolemia, and hypertension. He also has diabetic retinopathy, peripheral neuropathy, and nephropathy. He has an arterio-venous fistula placed for a possible dialysis. His medications are insulin, furosemide, atorvastatin, metoprolol and levothyroxine. After having his blood drawn for some laboratory studies today, he bleeds persistently. Laboratory studies show: Hb 11.5 g/dl, Platelets 160,000/cmm, Blood glucose 178 mg/dl, BUN 56 mg/dl, Serum creatinine 3.5 mg/dl. His baseline creatinine level is between 3.2-3.5 mg/dl. Which of the following is the most likely cause of his bleeding?
Disseminated intravascular coagulation
Platelet dysfunction
Factor VIII deficiency
Consumptive coagulopathy
Thrombocytopenia
A 56-year-old male with a long history of diabetes mellitus complains of nocturnal urinary frequency, occasional dribbling and difficulty completing his stream. His past medical history is significant for a myocardial infarction two years ago and moderately decreased visual acuity. On physical examination, his blood pressure is 160/100 mmHg and his heart rate is 70/min. There is a carotid bruit auscultated on the left side as well as trace ankle edema. Post-void bladder catheterization yields 60 ml of urine. Dipstick urinalysis reveals 2+ protein and 3-4 WBC/hpf. The patient's serum creatinine level is 2.4 mg/dl. Which of the following is the most likely cause of his renal dysfunction?
Ascending infection
Obstructive uropathy
Microangiopathy
Renal hypoperfusion
Cystic kidney disease
A 62-year-old man presents to the emergency department with severe back pain that began suddenly after he attempted to lift a heavy box. He says the pain radiates down his right thigh and leg and that coughing and moving make the pain “unbearable” The patient also complains of an inability to urinate since the pain started. On physical examination, he has no focal lower extremity weakness or numbness, and pinprick testing in the perianal area elicits a quick spasm of the anal sphincter. Rectal exam reveals an enlarged, smooth, nontender prostate. Which of the following best explains this patient's urinary retention?
Severe pain
Nerve root injury
Detrusor instability
Hypertonic bladder
Urethral injury
A 25-year-old woman presents with nausea and vomiting of 2 days duration. She is not on any medications and was previously well until now. Her physical examination is normal except for a postural drop in her blood pressure from 110/80 mm Hg supine to 90/80 mm Hg standing. Her serum electrolytes are sodium 130 mEq/L, potassium 3 mEq/L, chloride 90 mEq/L, bicarbonate 30 mEq/L, urea 50 mg/dL, and creatinine 0.8 mg/dL. Which of the following electrolytes is most likely to be filtered through the glomerulus but unaffected by tubular secretion?
Potassium
Sodium
Bicarbonate
Urea
Creatinine
A 29-year-old man with HIV, on a highly active antiretroviral therapy (HAART) regimen including the protease inhibitor indinavir, presents with severe edema and a serum creatinine of 2.0 mg/dL. He has had bone pain for 5 years and takes large amounts of acetaminophen with codeine, aspirin, and ibuprofen. He is on prophylactic trimethoprim-sulfamethoxazole. Blood pressure is 170/110 mm Hg; urinalysis shows 4+ protein, 5 to 10 RBC, 0 WBC; 24-hour urine protein is 6.2 g. The serum albumin is 1.9 g/L (normal above 3.7). Which of the following is the most likely cause of his renal disease?
Indinavir toxicity
Analgesic nephropathy
Trimethoprim-sulfamethoxazole–induced interstitial nephritis
Focal glomerulosclerosis
Renal artery stenosis
) A 74-year-old man presents with fatigue, short- ness of breath on exertion, and back and rib pain, which is made worse with movement. Investigations reveal he is anemic, calcium, urea, and creatinine are elevated. X-rays reveal multiple lytic lesions in the long bones and ribs, and protein electrophoresis is positive for an immunoglobulin G (IgG) paraprotein. Which of the following is the most likely mechanism for the renal injury?
Plasma cell infiltrates
Tubular damage by light chains
Glomerular injury
Vascular injury by light chains
Uric acid crystals
A 23-year-old woman with no other past medical history was diagnosed with hypertension 6 months ago. She was initially treated with hydrochlorothiazide, followed by the addition of lisinopril, followed by high doses of a beta-blocker, but her blood pressure has not been well controlled. She assures the provider that she is taking all of her medicines. On examination her blood pressure is 165/105 mm Hg in each arm, and 168/105 mm Hg when checked by large cuff in the lower extremities. Her pulse is 60. Cardiac examination reveals an S4 gallop but no murmurs. She has a soft mid-abdominal bruit. Distal pulses are intact and equal. She does not have hyperpigmentation, hirsutism, genital abnormalities, or unusual distribution of fat. Her sodium is 140, potassium 4.0, HCO3 22, BUN 15, and creatinine 1.5. Which of the following is the most likely cause of her difficult-to-control hypertension?
Primary hyperaldosteronism (Conn syndrome)
Cushing syndrome
Congenital adrenal hyperplasia
Fibromuscular dysplasia
Coarctation of the aorta
A 60-year-old woman with heart failure and normal renal function is started on furosemide (Lasix) 80 mg/day. She notices a good diuretic response every time she takes the medication. A few weeks later, she is feeling unwell because of fatigue and muscle weakness, but her heart failure symptoms are better. Which of the following is the most likely explanation for her muscle weakness?
Hyponatremia
Hypernatremia
Hypokalemia
Hyperkalemia
Anemia
A 65-year-old diabetic man with a creatinine of 1.6 was started on an angiotensin-converting enzyme inhibitor for hypertension and presents to the emergency room with weakness. His other medications include atorvastatin for hypercholesterolemia, metoprolol and spironolactone for congestive heart failure, insulin for diabetes, and aspirin. Laboratory studies include: K: 7.2 mEq/L, Creatinine: 1.8 mg/dL, Glucose: 250 mg/dL, CK: 400 IU/L. Which of the following is the most likely cause of hyperkalemia in this patient?
Worsening renal function
Uncontrolled diabetes
Statin-induced rhabdomyolysis
Drug-induced effect on the renin-angiotensin-aldosterone system
High-potassium diet
A 27-year-old alcoholic man presents with decreased appetite, mild generalized weakness, intermittent mild abdominal pain, perioral numbness, and some cramping of his hands and feet. His physical examination is initially normal. His laboratory returns with a sodium level of 140 mEq/L, potassium 4.0 mEq/L, calcium 6.9 mg/dL, albumin 3.5 g/dL, magnesium 0.7 mg/dL, and phosphorus 2.0 mg/dL. You go back to the patient and find that he has both a positive Trousseau and a positive Chvostek sign. Which of the following is the most likely cause of the hypocalcemia?
Poor dietary intake
Hypoalbuminemia
Pancreatitis
Decreased end-organ response to parathyroid hormone because of hypomagnesemia
Osteoporosis caused by hypogonadism
A 27-year-old woman presents to the emergency room with a panic attack. She appears healthy except for tachycardia and a respiratory rate of 30. Electrolytes include calcium 10.0 mg/dL, albumin 4.0 g/dL, phosphorus 0.8 mg/dL, and magnesium 1.5 mEq/L. Arterial blood gases include pH of 7.56, PCO2 21 mm Hg, and PO2 99 mm Hg. Which of the following is the most likely cause of the hypophosphatemia?
Hypomagnesemia
Hyperparathyroidism
Respiratory alkalosis with intracellular shift
Poor dietary intake
Vitamin D deficiency
A 57-year-old male is hospitalized for hyponatremia. Physical examination reveals no signs of fluid overload. Serum analysis reveals a sodium concentration of 125mEq/1, glucose level of 12mg/dl, BUN of 8mg/dl, and creatinine of 0.7mg/dl. The urine osmolarity is 330mOsm/l and urine sodium concentration is 45mEq/1. After a 2L normal saline infusion, the serum sodium is 126mEq/1 and the urine sodium excretion is increased to 90 mEq/1. Which of the following is the most likely cause of this patient's hyponatremia?
Inappropriate ADH secretion
Psychogenic polydipsia
Surreptitious diuretic use
Advanced liver disease
Interstitial renal disease
A 27-year-old female is brought into the emergency room by the local paramedics. She was found unconscious at the scene of a house fire. On examination it does not appear that she has suffered any burns. Black soot is noted near her nares and mouth. Her respirations are slow but spontaneous. Her capillary refill time is 4 seconds. Supplemental oxygen by a non-rebreather mask is begun. Her arterial blood gas and preliminary laboratory values are shown below: Blood pH 7.22, PaO2 100 mmHg, PaCO2 39 mmHg, HC03- 11 mEq/L, WBC count 9,000/cmm, Hb 14 mg/dl, Na+ 138 mEq/L, K+ 4 mEq/l, CI- 98 mEq/L, Troponin 0.4ng/ml. Which of the following is the most likely primary cause of the patient's acid-base disturbance?
Increased metabolic rate
Decreased oxygen delivery to tissue
Reduced oxygen utilization by tissues
Impaired excretion of lactic acid
Increased gut absorption
A 32-year-old female is brought to the emergency department with complaints of weakness, tingling and numbness of her extremities. She is not on any medication. Her pulse is 90/min, respirations are 14 /min and blood pressure is 110/70 mm Hg. The physical examination is unremarkable. Her laboratory profile is shown below: Blood pH 7.56, HCO3- 37 mEq/L, Urine Na+ 16 mEq/L, Urine K+ 20 mEq/L, Urine Cl- 7 mEq/L, Serum sodium 135 mEq/L, Serum potassium 2.9 mEq/L, Serum chloride 92 mEq/L, Blood urea nitrogen 22 mg/dl, Serum creatinine 0.9 mg/dl. Which of the following is the most likely cause of this patient's condition?
Surreptitious vomiting
Persistent diarrhea
Bartter's syndrome
Type I renal tubular acidosis
Hyperventilation syndrome
A 55-year-old homeless man presents to the emergency room complaining of muscle cramps and perioral numbing. The patient looks malnourished. He says that he consumed a lot of alcohol recently. His past medical history is significant for chronic and recurrent abdominal pain for which he was advised to quit drinking alcohol. His temperature is 36.7°C (98°F), blood pressure is 110/65 mmHg, pulse is 80/min, and respirations are 18/min. The laboratory values are: Hemoglobin 7.2 g/dl, MCV 105 fl, Leukocyte count 9,000/cmm, Platelets 200,000/cmm, ESR 20 mm/hr, Serum sodium 145 mEq/L, Serum potassium 4.0 mEq/L, Serum calcium 6.8 mg/dl, Serum phosphorus 2.5 mg/dl. What is the most probable cause of hypocalcemia observed in this patient?
Renal failure
Primary hypoparathyroidism
Pseudohypoparathyroidism
Hypoalbuminemia
Malabsorption
A 24-year-old female is brought to the emergency room because of dizziness and near syncope. She says that every time she stands up, she feels lightheaded. She has no significant past medical problems. She does note having broken up with her boyfriend three months ago, which has caused her to have decreased appetite and an associated ten-pound weight loss. She has also missed her last two menstrual periods. She denies using tobacco, alcohol or drugs. On physical examination, her temperature is 36.7°C (98°F). When lying supine, her blood pressure is 100/70 mm Hg and her pulse is 88/min. When she stands up, her blood pressure is 80/50 mm Hg and her pulse is 120/min. Other than dry skin and mucous membranes, her physical examination is unremarkable. Initial laboratory studies reveal: Serum sodium low, Serum potassium low, Urine sodium increased, Urine potassium increased. This patient's dizziness is most likely due to which of the following?
Low caloric intake
Self-induced vomiting
Laxative abuse
Diuretic abuse
Mineralocorticoid deficiency
A 52-year-old alcoholic man presents to the emergency department because of anxiety and tremors. His last drink of alcohol was 2 days ago. His initial electrolyte panel is: Sodium 132 mEq/L, Potassium 2.9 mEq/L, Chloride 100 mEq/L, Bicarbonate 25 mEq/L. He is treated for alcohol withdrawal, and given aggressive intravenous and oral potassium supplementation. Three days later, his electrolyte panel is: Sodium 135 mEq/L, Potassium 3.1 mEq/L, Chloride 102 mEq/L, Bicarbonate 28 mEq/L. Which of the following explains why this patient's potassium level is so difficult to correct?
Poor oral absorption
Hypophosphatemia
Alcohol withdrawal
Hypomagnesemia
Thiamine deficiency
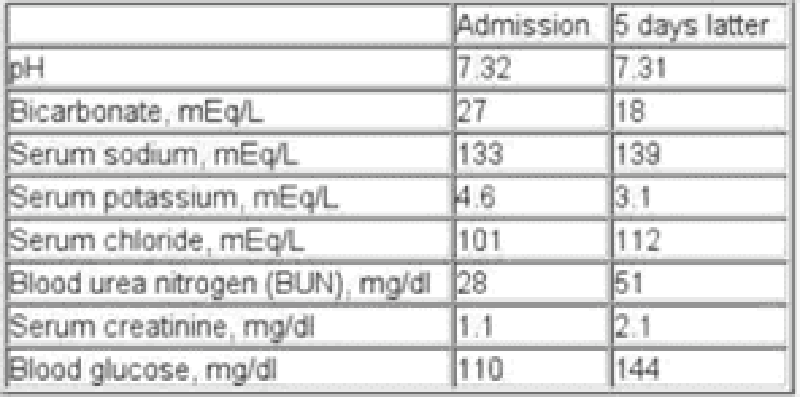
A 65-year-old chronic smoker presents to the hospital with increasing shortness of breath for the past few hours. He has been using albuterol occasionally, but it has not been helping him. He has been non-adherent to doctor's appointments and continues to smoke. He is afebrile. His oxygen saturation on room air is 86%. Examination shows elevated jugular venous pressure and lung auscultation reveals diffuse wheezing with no crackles. His heart sounds are muffled. Mild hepatomegaly and bilateral pitting pedal edema is present. Chest x-ray reveals hyperinflated lungs and a flattened diaphragm with no infiltrates. He is started on systemic steroids, bronchodilator nebulization and furosemide. His laboratory studies are shown below at the time of admission and five days later. Which of the following best explains the acid-base status change in this patient?
Acute renal failure
Development of ketoacidosis
Glucocorticoid treatment
Obstructive sleep apnea
Worsening respiratory failure
A 32-year-old pregnant female is being evaluated at her 32nd week of gestation. Her lab profile shows the following: Blood pH 7.44, PaO2 100 mmHg, PaCO2 30 mmHg, HCO3- 20 mEq/L, WBC count 9,000/cmm, Hb 11 mg/dl, Na+ 134 mEq/L, K+ 3.6 mEq/1, Cl- 98 mEq/L, BUN 5 mg/dlCreatinine 0.6 mg/dl. Which of the following can best explain her acid-base status?
Anemia
Pulmonary embolism
Obesity
Normal phenomenon of pregnancy
Hyperemesis gravidarum
A 59-year-old female is hospitalized due to lower gastrointestinal bleeding. Her past medical history includes diabetes mellitus, hypertension, chronic obstructive pulmonary disease, cor pulmonale and recurrent urinary tract infections. Her condition initially stabilized with fluid resuscitation and blood transfusions, but she subsequently developed an acute renal failure. Her urine output has been between 300 and 400 ml per day for the last couple of days. On the 10th day of her hospitalization she is lethargic. Serum analysis reveals: Hemoglobin 10.2 g/dl, Hematocrit 30%, WBC 14,300/mm3, Blood glucose 93 mg/dl, BUN 141 mg/dl, Creatinine 4.1 mg/dl, Sodium 133 mEq/L, Potassium 5.0 mEq/L, pH 7.15, pO2 90 mmHg, pCO2 60 mmHg, HCO3 18 mEq/L. Which of the following is the most likely cause of her lethargy?
Poor tubular bicarbonate reabsorption
Low tubular ammonium production
Renal tubular chloride loss
Decreased anion gap
Hypoventilation
A 32-year-old Caucasian male presents to the ER with a 12-hour history of anorexia and vomiting. He says that he feels “a little dizzy”. He denies abdominal pain or diarrhea. His past medical history is insignificant His blood pressure is 110/70 mmHg while supine and 100/60 mmHg while sitting. His heart rate is 90/min. His laboratory values are: Serum sodium 139 mEq/L, Serum potassium 3.1 mEq/L, Serum calcium 8.9 mEq/L, Serum chloride 88 mEq/L, Serum bicarbonate 33 mEq/L, Blood glucose 95 mg/dl, BUN 20 mg/dl, Serum creatinine 1.1 mg/dl. Which of the following is the most likely cause of the decreased chloride level in this patient?
Gastrointestinal loss
Bicarbonate reabsorption in the kidney
Metabolic alkalosis
Intracellular shift
Volume depletion
A 22-year-old female is hospitalized after a car accident. She sustained a hip fracture, fractures of several ribs and a blunt abdominal injury that required a laparotomy. The laparotomy revealed a liver laceration and extensive hemoperitoneum. In the early postoperative period, the patient is noted to have hyperactive deep tendon reflexes. Which of the following electrolyte abnormalities may be responsible for this condition?
Hypokalemia
Hyperkalemia
Hyponatremia
Hypocalcemia
Hypermagnesemia
A 44-year-old obese female undergoes an open cholecystectomy for a complicated acute cholecystitis. On her third post-operative day, her temperature is 36.7°C (98.2°F), blood pressure is 110/80 mm Hg and pulse is 92/min. Her arterial blood gas shows the following: Blood pH 7.28, PaO2 62 mmHg, PaCO2 54 mmHg, HCO3- 30 mEq/L. What is the most likely cause of acidosis in this patient?
Alveolar hypoventilation
Acute pulmonary embolism
Atelectasis
Pulmonary edema
Pleural effusion
A 32-year-old male with type 1 diabetes and severe depression is brought to the emergency department because of a 2-day history of nausea and abdominal pain. His temperature is 37.6°C (99.7°F), blood pressure is 122/86 mmHg, respirations are 25/min and pulse is 88/min. His lab values are as follows: Blood pH 7.31, PaO2 90mm Hg, PaCO2 29 mmHg, HCO3- 14 mEq/L, Blood glucose 450 mg/dl, Serum sodium 132 mEq/L, Serum potassium 5.0 mEq/L, Serum chloride 85mEq/L, Blood urea nitrogen 19 mg/dl, Serum creatinine 1.1 mg/dl. Which of the following best describes this patient's acid-base status?
Primary metabolic acidosis with respiratory compensation
Primary metabolic acidosis without compensation
Respiratory acidosis with compensation
Primary metabolic alkalosis with renal compensation
Normal acid base status
A 28-year-old primigravida is admitted to the hospital at 10weeks gestation. Her right leg is swollen. Her BMI is 30 Kg/m2. Her temperature is 36.7°C (98.2°F), respirations are 12/min and pulse is 96/min. Her ABG shows the following: pH 7.49, PaCO2 50 mm Hg, HCO3- 44 mEq/L. Which of the following is the most likely cause of her abnormal arterial blood gas?
Normal phenomenon of pregnancy
Pulmonary embolism
Obesity
Aspiration pneumonitis
Hyperemesis gravidarum
A 54-year-old woman presents to your office complaining of difficulty walking. She describes severe weakness and occasional pain in her thigh muscles. She has stumbled and fallen several times over the last week. Her past medical history is significant for hypertension treated with hydrochlorothiazide and metoprolol. She consumes two to three cans of beer on weekends. Her younger brother died of a neurological disease when he was 20 years old. Her mother suffers from hypertension and diabetes mellitus. Her heart rate is 90/min and blood pressure is 170/100 mmHg. Chest examination is within normal limits. A bruit is heard over the left carotid artery. Neurologic examination reveals hyporeflexia and decreased strength in all muscle groups. Her ESR is 12 mm/hr. ECG shows flat and broad T waves with occasional premature ventricular contractions. Which of the following is the most likely cause of this patient's current complaints?
Ischemic stroke
Epidural hematoma
Subdural hematoma
Lumbar spinal stenosis
Electrolyte disturbance
A 73-year-old Caucasian man is brought to the office by his daughter, who is concerned that he might be depressed. He is a retired surgeon, and has lived alone ever since his wife died a year ago. His daughter visits him every 6 months; she feels bad about not being able to visit him more frequently because her job and family keep her very busy. He denies having any feelings of sadness, guilt, weight loss, loss of appetite, suicidal ideation, deafness, vertigo, and decreased or blurred vision. His medical problems include hypertension, diabetes mellitus-type 2 and a myocardial infarction 10 years ago. His current medications are glyburide, aspirin and enalapril. He denies the use of tobacco, alcohol, or drugs. His vital signs are within normal limits. He appears withdrawn, less energetic than usual, and walks stiffly. He sits with a stooped posture. He has a fixed facial expression, and his voice sounds monotonous. His deep tendon reflexes are 2+. Sensations and motor strength are normal. There is increased resistance to passive flexion. Which of the following types of gait is most likely to be present in this patient?
Cerebellar ataxia
Hypokinetic gait
Waddling gait
Spastic gait
Gait disequilibrium
A 65-year-old woman complains of periodic headaches in the temporal region, visual disturbances, and neck stiffness. Treatment is initiated early and biopsy of a scalp artery is consistent with arteritis. Two months later, the patient presents to your office with weakness. She says that her headaches are gone but she has difficulty climbing stairs and getting up from a chair. Her serum CK level and ESR are normal. Which of the following is the most likely cause of this patient's current complaints?
Polymyalgia rheumatica
Mononeuritis multiplex
Symmetric polyneuropathy
Inflammatory myositis
Drug-induced myopathy
A 54-year-old female complains of muscle weakness. She describes difficulty getting up from a chair and combing her hair. She does not use tobacco, alcohol or drugs. She takes no medication. Her vital signs are within normal limits. Physical examination reveals bilateral ptosis. Which of the following is the most likely cause of this patient's complaints?
Ischemic stroke
Epidural hematoma
Subdural hematoma
Thyroid myopathy
Neuromuscular junction disease
A 56-year-old male complains of occasional dizziness. He gets a brief spinning sensation while getting out of bed. He sometimes feels dizzy while turning in bed or looking up. He denies any nausea, diaphoresis, chest pain or tinnitus. His past medical history is significant for long-standing hypertension, which is being treated with hydrochlorothiazide, and hyperlipidemia, which is being treated with simvastatin. His father died of a stroke at the age of 62 years. His blood pressure is 130/80 mmHg while supine, and 135/85 mmHg while standing. His heart rate is 77/min. A grade II/VI ejection murmur is heard over the aortic area. ECG reveals left ventricular hypertrophy and premature ventricular contractions. Which of the following is the most likely cause of this patient's complaints?
Transient ischemic attacks
Labyrinthine dysfunction
Aortic stenosis
Extracellular sodium loss
Cardiac arrhythmia
A 43-year-old man is being evaluated for one month of blurred vision, frontal headaches and occasional falls. He reports that the blurry vision is worse when he leans forward. He relates his symptoms to a recent break-up with his girlfriend. On physical examination, his blood pressure is 160/100 mmHg and his heart rate is 60/min. Which of the following is most likely responsible?
Bitemporal muscle contraction
High intraocular pressure
Vascular dilatation
Intracranial hypertension
Meningeal irritation
A 19-year-old man is brought in to the emergency department after being stabbed in the back. He has no past medical history and takes no medications. Muscle strength is absent and tone is decreased in the right leg. The right patellar and Achilles reflexes are absent. Babinski sign is present on the right. There is a loss of vibratory sense and toe joint position on the right. There is a loss of pain and temperature sensation below T12 on the left. Which of the following will cause a loss of pain and temperature sensation on the left side, beginning at T12?
Damage to left-sided lateral spinothalamic tracts at T10
Damage to left-sided lateral spinothalamic tracts at T12
Damage to left-sided lateral spinothalamic tracts at L1
Damage to right-sided lateral spinothalamic tracts at T10
Damage to right-sided lateral spinothalamic tracts at T12
A 64-year-old woman presents to your office after falling in the grocery store earlier today. She says she was doing her usual shopping when she felt weak in her legs and fell down. She denies hitting her head, headache, or loss of consciousness, but does complain of low back pain. Her past medical history is significant for diabetes mellitus, hypertension, severe osteoporosis, chronic neck pain and congestive heart failure. She has had three transient ischemic attacks, each lasting 15-20 minutes and characterized by slurred speech, in the past. Her medications include insulin, lisinopril, carvedilol, alendronate, aspirin, and acetaminophen. Her blood pressure is 160/90 mmHg and her heart rate is 73/min. Physical exam reveals muscular weakness, increased deep tendon reflexes, and mildly decreased pinprick sensation in both lower extremities. Which of the following is most likely responsible?
Ischemic stroke
Intracranial bleeding
Spinal cord compression
Polyneuropathy
Neuromuscular junction disease
A 76-year-old man presents with several months of urinary incontinence. He denies associated dysuria, nocturia, or penile discharge, and has otherwise been feeling well aside from moderate left arm pain following a fall three days ago. He denies headache or head trauma. His medical history is significant for osteoarthritis and glaucoma, which are controlled with medications. On exam, his vital signs are within normal limits. His heart, lungs, and prostate are unremarkable. The cranial nerves are all intact, fundoscopic exam is normal, and there is no tremor. His gait is wide-based and shuffling, and he scores 24/30 on the Folstein mini-mental status exam. His muscle power is 5/5 in all four extremities and the deep tendon reflexes are normal. What is the most likely cause of his current condition?
Increased CSF production
Small vessel cerebral ischemia
Decreased CSF absorption
Amyloid protein deposits in the brain
Spinal cord compression
A 33-year-old white female comes to the office for the evaluation of weakness in her upper extremities. She thinks she is unable to feel pain or heat, because she recently noted some burn wounds on her fingertips, and does not know how she got them. She denies weakness in her lower limbs, as well as any history of trauma, headache, bowel or bladder problems, neck pain or facial pain. Examination reveals absent reflexes in her upper limbs. There is absent pain and temperature sensation on the nape of neck, shoulders and upper arms in a 'cape' distribution. Vibration and position sensations are preserved. Which of the following is the most likely pathology of the patient's condition?
Caudal displacement of the cerebellar tonsils and vermis
Caudal displacement of the fourth ventricle
Cord cavitation
Focal cord enlargement
Disc herniation and cord compression
A 67-year-old woman is being evaluated for periodic confusion, insomnia, and frequent falls as well as episodes of decreased alertness and visual hallucinations. On physical examination, she has increased lower extremity muscle tone but downgoing Babinski reflexes bilaterally. Which of the following pathologic findings most likely underlies her condition?
Neurofibrillary tangle
Lewy bodies
Impaired CSF absorption
Multiple lacunar strokes
Corticospinal tract demyelinization
A 65-year-old man was brought to the emergency department after his wife and son were unable to wake him up this morning. His past medical history is significant for hypertension for the past 7 years. For the past year, he has had several episodes of chest pain, which was triggered by physical activity and relieved by rest. His current medications are nitrates and "baby aspirin." His blood pressure is 140/80 mm Hg, heart rate is 85/min, and respirations are 15/min. The physical examination reveals an obese man with impaired consciousness. He has a Glasgow score of 6, asymmetric pupils, and brisk deep tendon reflexes in the left extremities. Plantar stimulation provokes extension of the left great toe. The EKG shows no abnormalities. His CK-MB serum levels are within the normal range, and his LDL cholesterol level is 150 mg/dl. What is the most likely etiopathology of this patient's symptoms?
Atherosclerotic emboli obstructing a major cerebral artery
Acute left ventricular failure with decreased cerebral perfusion
Thrombus migration from the left side of the heart
Hemorrhagic stroke resulting from hypertensive crisis
Chronic subdural hematoma
An 84-year-old female is hospitalized with right-sided hemiplegia secondary to an ischemic stroke. She has a complex past medical history including hypertension, diabetes mellitus, hypercholesterolemia and mild Alzheimer disease. Her current medications include lisinopril, metoprolol, insulin glargine, simvastatin and aspirin. On physical examination, her blood pressure is 140/60 mm Hg and her heart rate is 62/min. Her neck is supple and without jugular venous distension. Her lungs are clear to auscultation and her abdomen is soft and non-distended. She cannot move her right arm or right leg. There is a partial thickness ulcer on her right heel. Her wound is most likely the result of which of the following?
Poor glucose control
Ischemia
Venous thrombosis
Bacterial infection
. Denervation
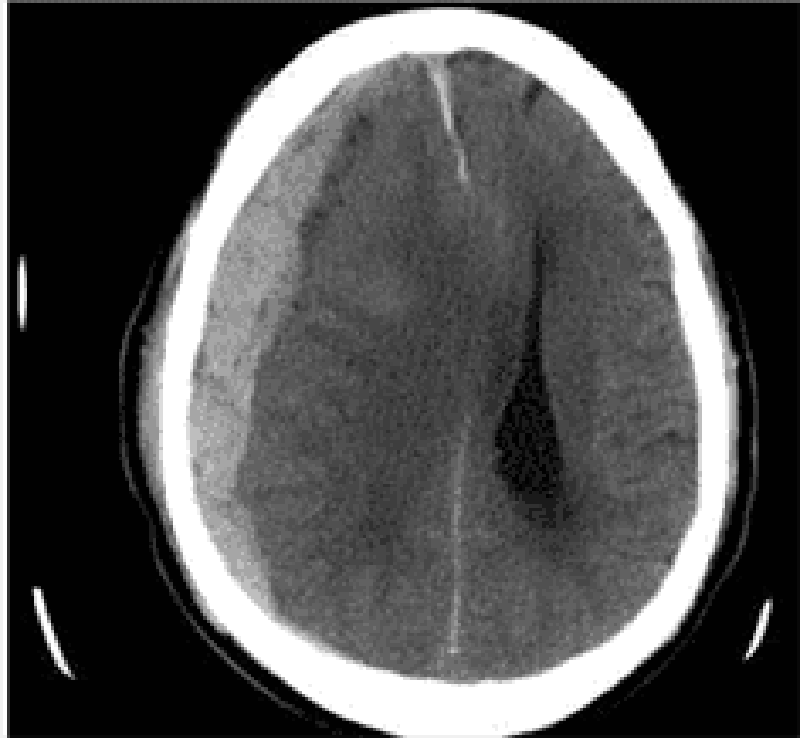
) A 76-year-old man is brought to the emergency department by his son who found him confused in his apartment. The son also reports that his father has been limping for the past two days. The patient's past medical history is significant for hypertension, diabetes mellitus, and cataract surgery six months ago. His medications are metoprolol, enalapril, and glyburide. He has also been taking ibuprofen for recent headaches. A head CT scan is obtained and is shown below. Which of the following is the most likely cause of this patient's condition?
Carotid artery atherosclerosis
Small vessel hyalinosis
Blunt head trauma
Ruptured aneurysm
Recent eye surgery
A 59-year-old male presents to the ER with diplopia that started several hours ago. He has no other complaints. His past medical history is significant for long-standing diabetes with poor glycemic control, right knee osteoarthritis, and peptic ulcer disease. Physical examination reveals right-sided ptosis with the right eye looking down and out. Pupils are equal and reactive to light. This patient's condition is most likely due to which of the following?
Nerve compression
Nerve ischemia
Nerve inflammation
Lacunar stroke
Muscle infiltration
A 52-year-old male is referred to the neurology clinic for the evaluation of EEG abnormalities. He presented with rapidly increasing memory impairment, and denied any history of seizures or head trauma. The physical examination revealed no abnormalities, except a myoclonus. An extensive work-up ruled out the presence of any medical illness; however, the EEG report revealed sharp, triphasic and synchronous discharges. Which of the following abnormalities is most likely in this patient?
Defect in an autosomal dominant gene on chromosome 4
Spongiform encephalopathy caused by a prion
Loss of nigrostriatal dopaminergic neurons
Histopathological findings of neurofibrillary tangles and amyloid plaques
Neurodegeneration of frontal and temporal lobes
A 67 -year-old male presents to the emergency department with severe dizziness and the inability to walk. He complains of repetitive vomiting and occipital headache. The symptoms started two hours ago when he was playing golf in sunny weather with his friends. His past medical history is significant for hypertension and diabetes. He underwent coronary stenting two years ago for recurrent chest pain. His current medications are aspirin, glipizide, enalapril and metoprolol. His blood pressure is 210/110 mmHg, heart rate is 78/min, temperature is 37.8°C (100°F), and respirations are 18/min. Muscle strength is preserved in all four extremities, and there are no sensory abnormalities. Which of the following is the most likely cause of this patient's symptoms?
Heat stroke
Posterior cerebral artery occlusion
Cerebellar haemorrhage
Vestibular neuronitis
Meniere disease
A 24-year-old athlete was running a marathon on a bright sunny and humid day, when he suddenly collapsed. He was disoriented at the scene. He has no medical history and takes no medication. He does not use tobacco, alcohol or drugs. Family history is insignificant. On arrival to the emergency room, his temperature is 41°C (105.8°F), blood pressure is 90/60mm Hg, pulse is 140/min, and respirations are 22/min. Mucous membranes and skin are dry. Neck is supple. Auscultation of the chest is unremarkable. Abdomen is soft and non-tender. Muscle tone and reflexes are within normal limits. Labs show a hematocrit of 52%. Chest x-ray is within normal limits. Urinalysis shows large blood but no red blood cells. Which of the following is the most likely underlying pathophysiology of his current condition?
Systemic cytokine activation
Failure of thermoregulatory center
Uncontrolled efflux of calcium from sarcoplasmic reticulum
Inadequate fluid and salt replacement
Cardiac outlet obstruction
A 21 -year-old male has been experiencing severe headaches for the past week. He also describes difficulty grasping objects in his right hand and difficulty getting dressed, which both started today. CT scan of the head shows a ring-enhancing lesion in the left frontal lobe and a fluid collection in the left maxillary sinus. Tissue biopsy of the brain lesion is most likely to demonstrate which of the following?
Neoplastic cells
Anaerobic bacteria
Toxoplasma trophozoites
Staphylococcus aureus
Acid-fast bacilli
A 30-year-old Caucasian male comes to the office due to symmetric weakness of his lower extremities. He also has paresthesias in his toes and fingers, and lower back pain. The neurological examination shows symmetric weakness, diminished reflexes, and intact sensation in his lower extremities. Orthostatic hypotension is also noted. Electrophysiological studies show slowed nerve conduction velocities. Lumbar puncture reveals normal opening pressure. CSF examination shows few cells, and a protein concentration of 90 mg/dL. Which of the following organisms is involved in the pathogenesis of this disorder?
Campylobacter jejuni
Chlamydia
Shigella
Salmonella
E coli (O157: H7)
A 65-year-old Caucasian male presents to your office complaining of an episode of slurred speech and clumsiness of his right hand. The episode lasted 15 minutes and resolved spontaneously. He had a similar episode one week ago. His past medical history is significant for moderate hypertension, diabetes mellitus (OM) type 2 and osteoarthritis of the right knee. He has smoked one pack of cigarettes daily for 35 years, and drinks 1-2 glasses of wine daily. His current medications include metoprolol, glyburide and naproxen. His blood pressure is 160/95 mmHg, pulse is 65/min, respirations are 16/min, and temperature is 36.7°C (98°F). The physical findings are within normal limits. The lab studies show: Fasting blood glucose 200 mg/dl, Total cholesterol 240 mg/dl, LDL cholesterol 140 mg/dl, HDL cholesterol 76 mg/dl. What is the most important risk factor for a stroke in this patient?
Hypertension
Smoking
Elevated cholesterol level
Alcohol consumption
Diabetes mellitus
) A 65-year-old bedridden woman is brought in with complaints of weight loss, weakness and malaise. Her past medical history includes chronic obstructive pulmonary disease (diagnosed fifteen years ago) and hypertension of ten years' duration. She quit smoking two years ago, but previously smoked three packs of cigarettes daily since she was 20 years of age. Her vital signs are stable. Her physical examination reveals severe weakness in her proximal muscles, and loss of deep tendon reflexes. Chest x-ray shows a right upper lung mass with mediastinal lymphadenopathy. Which of the following is the most likely cause of her weakness?
Autoantibodies against post synaptic receptors
Immune mediated muscle inflammation
Upper and lower motor neuron degeneration
Multicentric CNS inflammation and demyelination
Antibodies to voltage gated calcium channels
A 16-year-old female complains of headaches and visual impairment for the past month. She says that the headaches are worst in the morning and are associated with nausea. Her medical history is also significant for severe acne for which she takes oral isotretinoin. On physical examination, her temperature is 36.7°C (98°F), blood pressure is 130/80 mm Hg, pulse is 70/min, and respirations are 15/min. She has papilledema and decreased visual acuity. There is no neck stiffness. Motor examination shows 5/5 power, 2+ deep tendon reflexes, and a normal plantar response. Sensory examination is unremarkable. CT scan of the head is within normal limits. Lumbar puncture reveals the following: Opening pressure 250 cm H20, CSF glucose 40 mg/dL, CSF protein 40 mg/dL, WBC 3/mm3. Which of the following is the most likely cause of her symptoms?
Normal pressure hydrocephalus
Classic migraine
Cluster headaches
Multiple sclerosis
Medication side effect
A 26-year-old man comes to the emergency department because he is "suffering from the worst headache of his life." He feels nauseated and is photosensitive. His blood pressure is 160/90 mm Hg, heart rate is 88/min, and temperature is 36.5°C (97.7°F). The physical examination reveals no focal neurological symptoms, except for some meningismus and vertigo, which is not localized to either side. CSF examination reveals the presence of xanthochromia. What is the major cause of morbidity and mortality in a patient with the above condition?
Post-angiographic complications
Vasospasm with symptomatic ischemia and infarction
Secondary infection
Post-surgical complications
Nimodipine use
A 53-year-old man comes to the office because of difficulty reading fine print over the last year. He now has to hold books, menus, and magazines at an arm’s length in order to read them. He has never had visual problems before. Which of the following is most likely abnormal in this patient?
Corneal shape
Lens elasticity
Lens opacity
Macula
Peripheral retina
A 35-year-old HIV-positive male is complaining of deterioration of his vision over the past week. He initially experienced eye pain and mild conjunctivitis, followed by rapid progressive visual loss. Examination of his eyes reveals marked keratitis. Funduscopy shows widespread, pale, peripheral retinal lesions and central necrosis of the retina. Which of the following is the most likely causative organism of this patient's condition?
Pseudomonas
Cytomegalovirus
Herpes simplex
Candida albicans
Epstein Barr virus
) A 57-year-old female with a history of type 2 diabetes mellitus complains of fatigue, urinary frequency, increasingly blurred vision and worsening leg cramps over the past week. She reports that the symptoms all began following an upper respiratory infection 7 or 8 days ago. She does not take any medications, but adheres to a diet low in saturated fat and simple carbohydrates to manage her diabetes. On physical examination, her blood pressure is 160/90 mmHg and her heart rate is 90/min. Her mucous membranes are dry. Her urine is positive for glucose but negative for ketones. Which of the following is the most likely cause of this patient's vision impairment?
Cataracts
Diabetic retinopathy
Arterial hypertension
Hyperosmolarity
Eye infection
) A 34-year-old obese Caucasian female complains of periodic visual obscurations. She has episodes during which she "goes blind" for several seconds when standing up or stooping forward abruptly. She also describes frequent morning headaches over the last two months for which she has had to take ibuprofen or aspirin almost every morning. She takes no other medications. Past medical history is insignificant aside from one uncomplicated vaginal delivery. She denies use of alcohol, tobacco, or illicit drugs. She is afebrile with a blood pressure of 138/88 mmHg and pulse of 93/min. Visual field testing shows enlarged blind spots. There are no other significant findings on neurologic examination. Which of the following is the most likely cause of this patient's symptoms?
Optic neuritis
Glaucoma
Cataract
Papilledema
Amaurosis fugax
A 30-year-old man is concerned about "floating spots" and blurred vision in his right eye. He had a serious injury of his left eye several weeks ago, which eventually led to vision loss in that eye. Inspection reveals a moderate perilimbal flush. What is the most probable cause of this patient's condition?
Reagin-mediated disease
Circulating immune complexes
Non-caseating granulomas
Uncovering of 'hidden' antigens
Non-immune injury
A 67-year-old Caucasian male complains of progressive visual loss in his right eye over the past several months. He has a history of hypertension and type 2 diabetes mellitus. Current medications include a daily baby aspirin, hydrochlorothiazide, lisinopril, and metformin. There is no family history of visual problems. He has a 35 pack year smoking history and admits to occasional alcohol use. He is afebrile with a blood pressure of 137/82 mmHg and pulse of 73/min. Cardiac and pulmonary examinations are unremarkable. A neurologic examination demonstrates no focal motor or sensory abnormalities. The patient is asked to cover his left eye and to look at a small spot on a grid made of parallel vertical and horizontal lines. He describes the vertical lines as being bent and wavy. Which of the following is the most likely cause of this patient's complaints?
Lens opacity
Enlarged blind spot
Increased intraocular pressure
Macular degeneration
Peripheral retinal degeneration
A 35-year-old white female is complaining of blurry vision and pain with eye movements. She is on no medications and denies any trauma. Last year, she developed bladder incontinence and an episode of leg weakness, which both improved without therapy. Physical examination reveals reduced vision and swollen optic discs. The one diagnosis that may explain her symptoms is:
Parkinson disease
Myasthenia gravis
Multiple sclerosis
Subdural hematoma
Transient ischemic attacks
A 67-year-old male presents with a one-month history of dyspnea on exertion and chest pain. He denies hemoptysis, cough, fever, night sweats or weight loss. His past medical history is significant for hypertension and chronic obstructive pulmonary disease. He has a 48 pack-year smoking history but quit six years ago. He works as a salesman. On physical examination, the patient has a temperature of 38.2°C (100.8°F), blood pressure of 128/72 mm Hg, pulse of 92/minute, and respirations of 20 breaths/minute. His complete blood count, chemistry panel, and hepatic function tests are all within normal limits. A chest x-ray and computed tomography scan of the chest reveal a right-sided pleural effusion and calcified nodules in both upper lobes. The patient undergoes thoracentesis. Characteristics of the pleural fluid are given below: Total protein 5.2 g/dl, Glucose 83 mg/dl, Adenosine deaminase 98.5 U/L. Cytologic examination reveals 600 white blood cells/mm3, 1% macrophages and 99% leukocytes. Of the leukocytes, 45% are neutrophils, 50% are lymphocytes, and 5% are monocytes, with no basophils or eosinophils. No neoplastic cells are found. Which of the following is the most likely mechanism underlying development of this pleural effusion?
Elevation of hydrostatic pressure
Decreased plasma osmotic pressure
Increased capillary permeability
Passage of fluid through openings in the diaphragm
Reduction of pleural space pressures
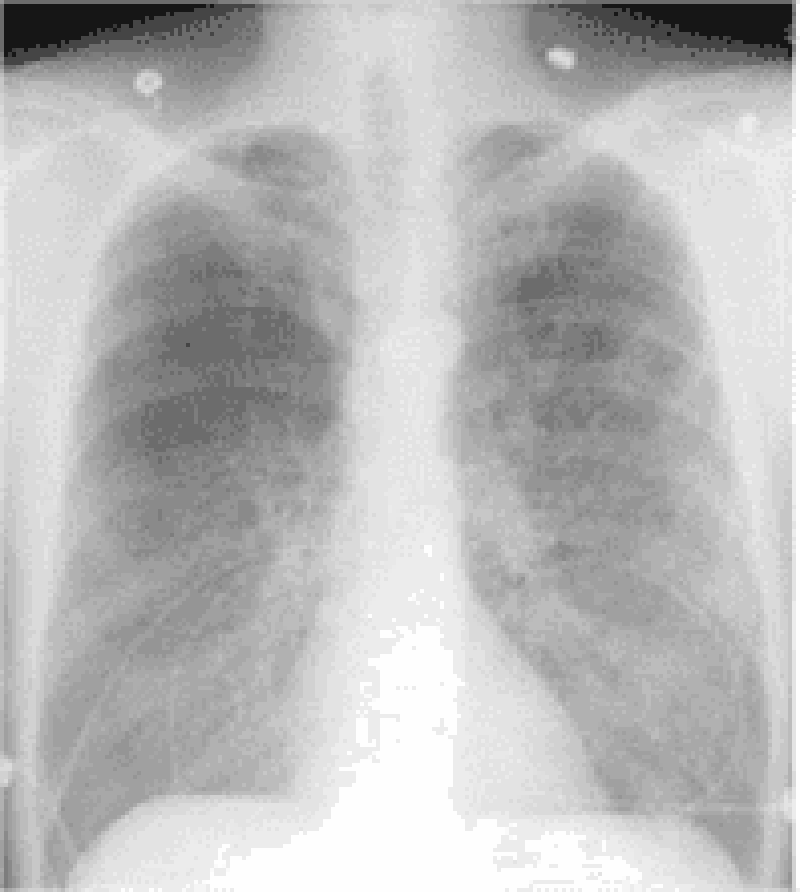
A 61-year-old man is being evaluated for progressive exertional dyspnea and decreased exercise tolerance. He has also noticed some ankle swelling. The patient has a 40 pack-year smoking history but denies illicit drug use or occupational exposures. His chest x-ray is shown below. The abnormal diaphragmatic contour seen here most likely results in which of the following?
Higher inspiratory flow
Reduced expiratory effort
Increased work of breathing
Increased thoracic wall recoil
Decreased lung compliance
A 65-year-old man complains of two years of persistent cough. He says that he coughs up whitish sputum almost every morning on waking, and then continues coughing throughout the day. He also complains of exertional shortness of breath that becomes disabling if he gets an upper respiratory infection. He has smoked one pack of cigarettes daily for the past 40 years. Pulmonary function testing reveals a vital capacity that is 65% of his predicted. Which of the following best explains this finding?
Alveolar-capillary membrane thickening
Decreased functional residual capacity
Air trapping during expiration
Decreased lung distensibility
Respiratory muscle fatigue
A 71-year-old man is brought to the ER after a witnessed tonic-clonic seizure. He is somnolent and intermittently combative on exam. No past medical history is available. His arterial blood gas (ABG) at room air is given below: pH 7.23, pCO2 69 mmHg, pO2 57 mmHg, HCO3 28 mmHg. Which of the following best explains the acid-base disturbances in this patient?
Lactic acid accumulation
Hypoventilation
Pulmonary embolism
Renal failure
Protracted vomiting
A 60-year-old white male presents to the Emergency Room with sudden onset of dyspnea. He is a truck driver and just returned from a long trip. His past medical history is insignificant. He is not taking any medications. His blood pressure is 110/70 mmHg and heart rate is 110/min. Physical examination reveals a moderately overweight man with tachypnea. Lungs are clear on auscultation. ECG shows right axis deviation. You order ventilation/perfusion scanning. Which of the following findings will help you the most to confirm the diagnosis?
An area of ventilation defect without perfusion defect
An area of perfusion defect without ventilation defect
An area of ventilation and perfusion defect
Several small perfusion and ventilation defects
Absence of ventilation and perfusion abnormalities
A 74-year-old nursing home resident is brought to the ER with a low-grade fever, cough and shortness of breath for the last two days. The cough is productive of small amounts of greenish sputum. His past medical history is significant for hypertension, diabetes mellitus type 2, COPD, hypercholesterolemia and mild dementia. His blood pressure is 152/78 mmHg and his heart rate is 89/min, regular. Physical examination reveals decreased breath sounds, coarse rhonchi, and increased fremitus over the lower left lung field. His oxygen saturation is 92% on room air when lying on his right side but drops to 84% when he lies on his left. Which of the following best explains this finding?
Increased dead space ventilation
Decreased cardiac output
Decreased oxygen diffusion capacity
Increased arterio-venous shunting
Effort-dependent hypoventilation
A 60-year-old man comes to the office with worsening shortness of breath over the last 5 months. He has had two episodes of bronchitis over the last 12 months. He now has a mild nonproductive cough. He denies any fever, chills, hemoptysis, chest pain, or difficulty breathing while lying on his back. His medications include an ipratropium inhaler, aspirin, and amlodipine. He was hospitalized twice in the last 3 years due to an exacerbation of his chronic obstructive pulmonary disease. He has been smoking 1 pack of cigarettes per day for the last 40 years. His temperature is 99°F (37.2°C), blood pressure is 130/86 mm Hg, pulse is 98/min, and respirations are 18/min. Examination shows a thin man in mild respiratory distress with increased anteroposterior chest diameter, diffuse expiratory wheeze and loud S2. Chest X-ray shows hyperinflation of bilateral lung fields with diaphragm flattening and small heart size. Which of the following is the most effective measure to decrease mortality in this patient?
Adding a short acting beta-agonist inhaler
Adding an inhaled corticosteroid
Adding a long-acting beta agonist
Adding systemic corticosteroids
Smoking cessation
A 64-year-old man presents to the emergency department with progressive exertional dyspnea that worsened after he contracted an upper respiratory infection. He also complains of bilateral ankle swelling. He has a 40 pack-year history of smoking. Physical examination reveals a mildly overweight patient in mild respiratory distress. Lung auscultation reveals bilateral wheezes and a prolonged expiratory phase. His white blood cell count is 14,500/mm3 and his hemoglobin level is 16 mg/dl. Arterial blood gas analysis reveals the following: pH 7.37, pO2 65mmHg, pCO2 60mmHg. Absence of marked acidosis in this patient is best explained by which of the following?
Increased minute ventilation
Increased dead space ventilation
Pulmonary vasoconstriction
Renal tubular compensation
Erythrocyte chloride shift
) A 43-year-old woman with congestive heart failure, rheumatoid arthritis and chronic hepatitis C complains of abdominal discomfort and difficulty breathing. Physical examination shows dullness to percussion at the right lung base. Chest x-ray reveals a large right-sided pleural effusion. Thoracentesis yields pleural fluid with a glucose content of 30 mg/dl and an LDH of 192units/L. Which of the following explains the pleural fluid glucose concentration?
Increased pleural membrane permeability
Increased capillary hydrostatic pressure
Increased permeability of the right hemidiaphragm
High white blood cell content of the pleural fluid
High amylase content of the pleural fluid
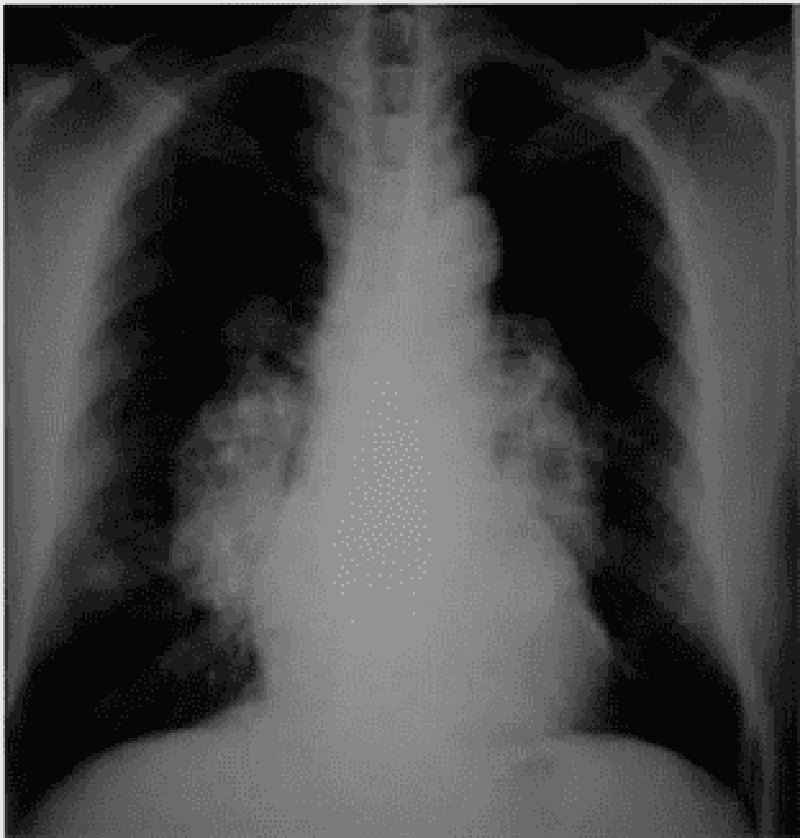
A 45-year-old black female presents to you because of a dry cough and has not been feeling well for the past month. She did have some pain in her shins a few weeks ago. She denies any allergies, smoking, or other medical problems. Her ECG shows normal sinus rhythm. The chest x-ray is shown below. What is the most likely pathophysiology in this patient?
Pulmonary venous congestion
Lupus pneumonitis
Inflammatory granulomas
Malignancy of the lung
Interstitial lung disease
A 42-year-old morbidly obese man is being evaluated for poor sleep. He complains of frequent awakenings due to a choking sensation and says that the resulting tiredness severely limits his physical activity. He also complains of chronic leg swelling. He denies cigarette, alcohol, or drug use. On physical examination, his blood pressure is 160/100 mmHg and his heart rate is 110/min. Which of the following additional findings is most likely to be present in this patient
Anemia due to low erythropoietin
Decreased chloride due to bicarbonate retention
Decreased sodium due to increased ADH secretion
Decreased C02 due to persistent hypoxia
Increased BUN due to volume constriction
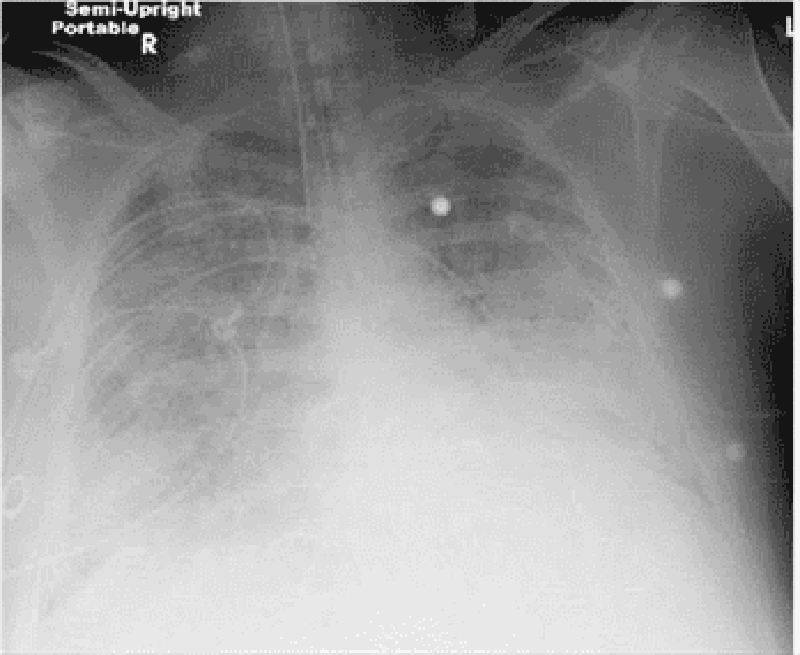
A 38-year -old male is brought to the emergency room with high-grade fever, shaking chills, productive cough and shortness of breath that started two days ago. His medical history is significant for two hospital admissions for alcohol withdrawal seizures. He continues to drink alcohol every day. He has no other medical problems and does not take any medications. On admission, his temperature is 39.7°C (103.5°F), pulse is 110/min, blood pressure is 100/70 mmHg, and respirations are 20/min. His skin and mucous membranes are dry. Physical examination reveals crackles and bronchial breath sounds in the right lower lobe. Chest x-ray demonstrates right lower lobe consolidation. He is started on ceftriaxone, azithromycin and intravenous normal saline at 200 ml/hr. Six hours later the nurse calls you because he is breathing at 38/min and requiring 100% oxygen. Emergent intubation is performed. A repeat chest x-ray is shown below. Which of the following is now most likely to be present in this patient?
Normal pulmonary capillary wedge pressure
Increased lung compliance
Increased left ventricular end diastolic pressure
Normal pulmonary arterial pressure
Normal alveolar-arterial oxygen gradient
A 53-year-old homosexual man comes to the ER with shortness of breath and dry cough over the past week. You note that he was hospitalized for Candida esophagitis one month ago, but left against medical advice. On physical examination, his blood pressure is 120/70 mmHg, heart rate is 120/min and regular, oxygen saturation is 89% on 2Umin of oxygen by nasal cannula, and temperature is 38.3°C (101°F). There are extensive white plaques over the oral mucosa and there is a soft 2/6 systolic murmur over the cardiac apex. Lung auscultation is remarkable for faint bilateral crackles. Which of the following is most likely responsible?
Increased pulmonary capillary wedge pressure
Alveolar hypoventilation
Increased alveolar-arterial oxygen gradient
Increased lung compliance
Pulmonary hypertension
A 56-year-old male presents with progressively worsening dyspnea over a 4 month period. He denies fever, chest pain, cough or ankle swelling and does not use tobacco, alcohol or drugs. He works for a home insulation and plumbing company. He has never been abroad and does not own any pets. His only medications are hydrochlorothiazide and metoprolol for blood pressure control. On physical examination, his temperature is 36.8°C (98.2°F), pulse is 76/min, blood pressure is 130/78 mmHg, and respirations are 15/min. Examination shows digital clubbing and fine bibasilar end-inspiratory crackles. Jugular venous pressure is 7 cm and there is no peripheral edema. Which of the following additional findings is most likely in this patient?
Increased pulmonary capillary wedge pressure
Decreased diffusion lung capacity (DLCO)
Decreased pulmonary arterial pressure
Increased residual lung volume
Reduced FEV1/FVC ratio
An 80-year-old Caucasian female is brought to the emergency room by her son with a three-day history of fever and a foul-smelling, productive cough. Her past medical history is significant for advanced dementia, diabetes, and hypertension. She takes aspirin, metformin, insulin, and atenolol. She was admitted two times with pneumonia during the past two months. Her temperature is 38.3°C (101°F), blood pressure is 100/70mmHg, pulse is 105/min, and respirations are 20/min. The patient is not oriented in time and place. Physical examination reveals dry mucus membranes and decreased skin turgor. Breath sounds are decreased to the right. A chest x-ray revealed right, lower lobe infiltrate. Which of the following is the most important predisposing factor for this condition in this patient?
Decreased lung elasticity
Gastro-esophageal reflux
Impaired epiglottic reflex
Decreased thyroid function
Depressed cell-mediated immunity
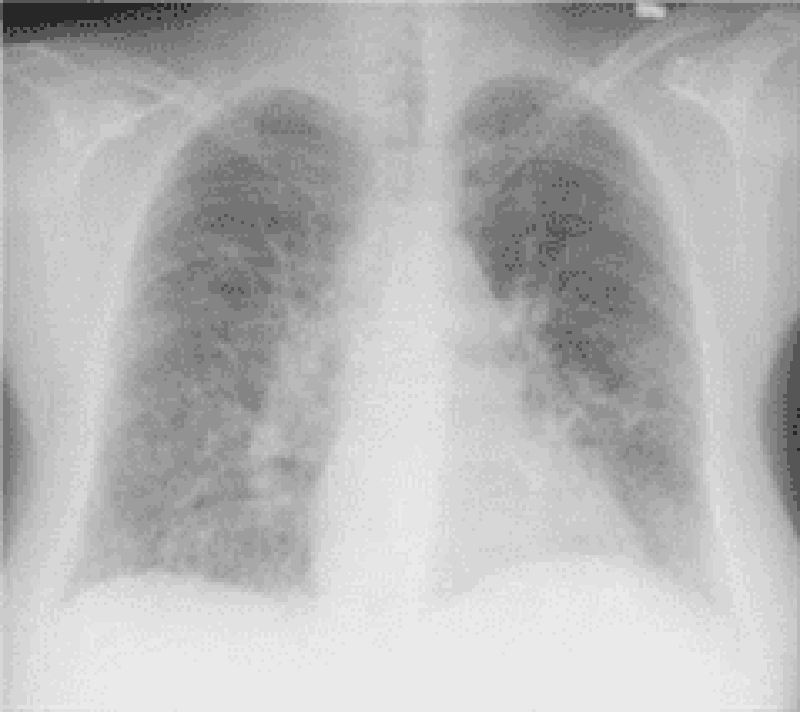
A 65-year-old female presents with 6 months of worsening dyspnea and dry cough. Whereas she had previously enjoyed an active lifestyle, she now becomes breathless after walking just a few steps. The patient denies fever or chest pain and does not use tobacco, alcohol or illicit drugs. Her only medicine is hydrochlorothiazide for hypertension. She is retired and lives with her husband. She has never travelled abroad and denies any history of exposure to pets. On physical examination, her temperature is 37.2°C (98.9°F), blood pressure is 140/86 mm Hg, pulse is 84/min and respirations are 18/min. Examination shows dry, late inspiratory crackles and finger clubbing. Her chest x-ray is shown below. Which of the following abnormalities is most likely to be present in this patient?
Increased diffusing capacity of carbon monoxide
Decreased FEV1/FVC ratio
Increased residual volume
Increased PaCO2
Increased A-a gradient
) A 44-year-old woman presents with increased shortness of breath, cough, and sputum production. She has had asthma since childhood and uses her medications as directed. Recently, she noticed that her peak flow readings were decreasing after the symptoms started. On examination, she is in moderate respiratory distress, respirations 25/min, there are bilateral wheezes and oxygen saturation is 90% on room air. On her blood gas, the PCO2 is 50 mm Hg. Which of the following is the most likely mechanism for her carbon dioxide retention?
Impaired diffusion syndromes
Right-to-left shunt
Hyperventilation
Ventilation-perfusion ratio inequality
Mechanical ventilation at fixed volume
A 57-year-old man with a 40-pack-per-year history of smoking experiences symptoms of shortness of breath on exertion. He has bilateral wheezes on expiration and increased resonance to percussion of the chest. Pulmonary function tests confirm the diagnosis of chronic obstructive lung disease (COPD). Which of the following is the best definition of this condition
It is caused by bronchial asthma
It is preceded by chronic bronchitis
It is airflow limitation that is not fully reversible
It is due to destruction and dilatation of lung alveoli
Is due to small airways disease only
A 38-year-old man is being seen in his physician’s office after being involved in a car accident. He has a vague pain along his right sternal border, where he crashed into the steering wheel. His temperature is 36.6°C (97.8°F), pulse is 80/min, blood pressure is 123/75 mm Hg, respiratory rate is 14/min, and oxygen saturation is 99% on room air. Physical examination is significant for point tenderness over the right sternal border. X-ray of the chest shows no broken ribs but a single, well-circumscribed pulmonary nodule, 1.5 cm in diameter, located in the left lower lung field. A search through the patient’s electronic medical file reveals that he had an x-ray of the chest taken 2 years ago. The radiology report from that time reveals that the nodule was only 0.75 cm in diameter. To characterize the lesion, CT of the chest is performed and shows dense, flocculated calcification within the lesion. Which of the following risk factors most increases the chances of malignancy in this patient?
Increased doubling time of tumor
Increased patient age
Nodule diameter of 1.5 cm or higher
Presence of discrete border
Presence of flocculated calcification
A 32-year-old man develops symptoms of wheezing, cough, and shortness of breath. He has bilateral expiratory wheezes, and the rest of the examination is normal. Further evaluation with pulmonary function tests reveals a reduced FEV1/FVC ratio that corrects with bronchodilators. Which of the following statements about a diagnosis of idiosyncratic asthma (also called nonatopic) is correct?
Known antigenic stimulus
Adult onset
History of atopy
Positive skin tests
High immunoglobulin E (IgE) levels

A 25-year-old man is recovering in the hospital from an open repair of his broken femur, which he suffered during an automobile accident. On postoperative day 3 he develops sudden onset shortness of breath and vague chest discomfort. His temperature is 37.6°C (99.6°F), heart rate is 108/min, blood pressure is 95/62 mm Hg, respiratory rate is 42/min, and oxygen saturation is 89% on room air. Physical examination is significant for jugular venous distention to 9 cm and an accentuated pulmonic component of S2. A pulmonary angiogram is shown in the image. Which of the following is most likely to be decreased?
Airway resistance
Alveolar dead space
Alveolar ventilation
Pulmonary compliance
Pulmonary vascular resistance
Syndrome. She becomes progressively more short of breath and hypoxemic requiring intubation and mechanical ventilation. Her repeat CXR in the intensive care unit now shows diffuse pulmonary infiltrates and a diagnosis of acute respiratory distress syndrome (ARDS) is made. Which of the following mechanisms is the most likely cause for the early exudative‖ phase of ARDS?
Increased lung compliance
Increased interstitial fibrosis
Increased vascular permeability to fluid and proteins
Decreased pulmonary perfusion
Decreased ventilatory dead space
A 55-year-old woman is in the intensive care unit on a ventilator for hypoxemia following “flash” pulmonary edema. Her PO2 on the blood gas prior to intubation was 44 mm Hg, and now while breathing 100% oxygen on the ventilator her repeat blood gas reveals a PO2 of 80 mm Hg. Hypoxemia while receiving 100% oxygen indicates which of the following problems?
Ventilation-perfusion ratio inequality
Right-to-left shunt
Hypoventilation
Impaired diffusion
Interstitial lung disease
You are the internist caring for a 26-year-old male who is stricken with alcoholic gastritis. The man has remained absent from his work as a waiter for several days due to his illness. His employer calls you for more information about the illness and the prognosis. He says that he just spoke with his employee on the phone and was granted permission to talk with you. What is the most appropriate response to this request?
"I'm sorry, but I cannot share such information with you at this point."
"The diagnosis is alcoholic gastritis, and I expect it will clear up spontaneously at some point in the near future."
"I can assure you that the illness does not pose a health risk to any of your employees or customers."
"I will need to have a release of information document signed by my patient before we can discuss this matter."
"I will need to have a verbal waiver of confidentiality granted to me by telephone before we can discuss this matter. Let me call you back."
A 34-year-old obese female is brought to the emergency department complaining of severe right upper quadrant abdominal pain that began suddenly earlier this morning. She is accompanied by her husband. An ultrasound evaluation is performed and the woman is diagnosed with acute cholecystitis. Because her symptoms worsen with conservative treatment, the decision is made to operate. The patient is discharged home five days after her successful cholecystectomy. Upon discharge, the patient and her husband request all medical records associated with her stay. What is the most appropriate response on the behalf of the physician?
Provide a copy of the original records
Refuse to provide the records
Politely inform the couple that it is unlawful to provide patients with their medical records
Give them the medical chart in its entirety
Inquire as to why the records are needed
A long-time patient calls your office to speak with you directly. She voices frustration with your receptionist, who has repeatedly refused to allow her to schedule an appointment to see you. The patient says that at her last visit, she had a heated argument with the receptionist about a minor detail regarding her insurance coverage. When she has called since then, the receptionist always responds by saying, "I'm sorry, but there are too many patients waiting ahead of you." Which of the following defense mechanisms is the receptionist demonstrating?
Distortion
Displacement
Acting out
Introjection
Introjection
A 34-year-old woman who describes herself as a "holistic healer" brings her two children aged four years and three years to the pediatrician for routine physical examinations. This is a first visit as they have recently moved from another state. The medical records for the children indicate that no immunizations have been given. When the mother is questioned about this, she proudly replies, "My children are wonderfully healthy on their own and have no need for these artificial vaccines." The principles and benefits of immunization are discussed at length, as well as the risks inherent in not being immunized. The physician recommends that the children be given all age-appropriate vaccinations today. The mother remains convinced that immunizations cause more harm than good, and she steadfastly refuses to allow her children to be vaccinated. What is the most appropriate next step?
Obtain a court order for immunization of children
Proceed with immunizations today
Inform mother that she will be reported to the local health department
Document in the medical chart that the risks and benefits of vaccination have been explained
Request to speak with her husband
A 48-year-old woman notices a firm, fixed mass in her right breast but chooses to ignore it. The mass is then detected on her annual physical examination eight months later. By that point, the mass has increased greatly in size. When questioned as to why she did not report the mass when she first noticed it, the woman states that she was not concerned about the mass because she does not have a family history of breast cancer This response is an example of which of the following defense mechanisms?
Repression
Dissociation
Denial
Rationalization
Intellectualization
A 60-year-old physician is admitted to the hospital for jaundice and weight loss. He denies other symptoms, including abdominal pain and alterations in bowel movements. His past medical history is noncontributory. He denies any history of significant alcohol intake but admits to a 30-pack-year smoking history. A detailed work-up eventually reveals the diagnosis of pancreatic carcinoma. Shortly after his discharge, he spends several hours per day on his laptop computer so that he can obtain the latest information on his illness. Which of the following psychological defense mechanisms is this physician most likely employing?
Intellectualization
Rationalization
Denial
Isolation
Resistance
A 54-year-old male with a history of chronic alcoholism is admitted to the hospital with hematemesis and abdominal distension. Upper gastrointestinal endoscopy reveals the presence of esophageal varices. Continued workup of his condition results in a diagnosis of cirrhosis of the liver. He is treated appropriately and strongly counseled about the need to abstain from alcohol. He is then discharged home. After discharge, he begins to work as a full-time volunteer for a non-profit organization that assists patients with alcoholic cirrhosis. Which of the following defense mechanisms is this man using?
. Reaction formation
Denial
Sublimation
Altruism
Suppression
) A 21-year-old college junior requests an urgent appointment with her family physician to discuss a "personal concern." During her conversation with the doctor, the woman appears tense, speaks very little, and makes minimal eye contact. After gentle questioning, she breaks down and says that her father is taking lithium for a manic episode experienced two years ago. She had not realized this could have any bearing on her own situation until she encountered an article on the Internet that mentioned genetics appears to play a role in the pathogenesis of bipolar disorder. Since then, she has had disturbed sleep and has been very worried that she too will one day develop bipolar disorder. Based on clinical data, what is the likelihood that she will have a manic episode during her lifetime?
1%
10%
40%
60%
75%
A 25-year-old married female is brought to the emergency department by her mother for excruciating right-sided abdominal pain. A urine pregnancy test is positive and a pelvic ultrasound reveals an empty uterus. Ruptured ectopic pregnancy is suspected, and an operating room is reserved for an emergent laparotomy. The patient's medical history is unremarkable except for a psychiatric diagnosis of paranoid schizophrenia. Who should sign the informed consent paperwork for the procedure?
The patient's husband
The patient's mother
The court
The patient
No consent is necessary as the patient is incompetent
A 31-year-old woman voices her anger at the increasing number of immigrants who compete for job opportunities in her chosen field of computer science. She observes that many of her friends in the local community are also experiencing difficulty in securing appealing employment because of the influx of immigrants. This woman volunteers in her spare time to provide vocational guidance to new immigrant families in the community. Which of the following psychological defense mechanisms is she demonstrating?
Suppression
Splitting
Reaction formation
Altruism
Sublimation
A 57-year-old Caucasian woman presents for a follow-up visit regarding her lower back pain. She originally presented with this complaint last month and was advised to limit activity and use ibuprofen as needed. When her pain persisted, she was scheduled for an MRI of her back. The MRI report returned today and describes the presence of metastatic deposits in her spine. The source of the primary neoplasm remains undetermined. The patient has not yet been told about the findings and will need to be informed today. Which of the following is the best means of initiating a conversation about her condition?
You have cancer, and it has metastasized to your back."
"You should have come earlier for a medical checkup. It is now too late."
"We will try our best. However, once a tumor metastasizes, the prognosis is poor."
"How are you feeling today?"
"You do not have a simple back strain."
A 23-year-old man comes to the psychiatrist with a chief complaint of a depressed mood. He is very anxious and obviously uncomfortable in the physician’s office. Which of the following actions should be used to help develop rapport with this patient?
Inform the patient that his problem is simple and easily fixed
Express compassion with the difficult position the patient is in
Tell the patient that you too are nervous when you see new patients
Ask the patient why he is so unusually anxious about seeing a psychiatrist
Get right to the patient’s complaint so that the patient can leave as soon as possible
A 37 year-old man with chronic schizophrenia is brought to see a new psychiatrist for treatment. While taking the history, the psychiatrist finds that the patient functions with a flat affect and circumstantial speech all the time. He has few friends. He is able to hold a menial job at the halfway house where he lives, and his behavior is not influenced by delusions or hallucinations currently. What should the psychiatrist rate the patient on Axis V (global assessment of functioning)?
. >95
. 70
55
30
15
An 18-year-old man is brought to the emergency room by police after he is found wandering in the street, screaming loudly at passersby. In the emergency room he is placed in an examination room, and paces the floor and pounds his fist against the door repeatedly. Which of the following actions should be taken by the psychiatrist first?
Rule out an organic mental disorder
Rule out psychosis
Give the patient 5 mg of haloperidol IM
Make sure the physical environment is safe for the interviewer
Put the patient into soft restraints
) A 24-year-old man returns from Iraq after a 13-month tour of duty. During that tour he was involved in battle situations and saw one of his friends injured by a car bomb. What percentage of American soldiers returning home from Iraq have posttraumatic stress disorder (PTSD)?
<1%
1% to 5%
15% to 20%
50% to 55%
85% to 90%
A 28-year-old woman is brought to see a psychiatrist by her mother. The patient insists that nothing is wrong with her, but the mother notes that the patient has been slowly but progressively isolating herself from everyone. She now rarely leaves the house. The mother says she can hear the patient talking to “people who aren’t there” while she’s in her room. On examination, the patient is noted to have auditory hallucinations and the delusional belief that her mother is going to kick her out of the house so that it can be turned into a theme park. Which of the following is the lifetime prevalence for this disorder?
1%
. 3%
5%
10%
15%
A 32-year-old man is admitted to the psychiatric unit after his wife brought him to the emergency room in a severe major depression. The patient signs himself in voluntarily because he “didn’t think he is safe” at home. Which of the following factors most increases a patient’s risk of suicide while on the inpatient unit?
The patient is in his first week of hospitalization
Staff morale is high on the unit
The patient is admitted in early July (new residents are on the unit
The patient is started on an SSRI the first day on the unit
The patient is told he will be evaluated for ECT
A 52-year-old female presents with a rash over her face for the past few weeks. She also complains of recent-onset difficulty with rising from a seated position and climbing stairs. On examination, you notice a dusky malar rash and a violaceous periorbital edema. Her vital signs are within normal limits. Examination shows symmetric proximal muscle weakness in legs. This patient's condition is most often associated with which of the following?
Aortic aneurysms
Renal failure
Alveolar hemorrhage
Malignancy
Carpal tunnel syndrome
A 50-year-old man presents to your office complaining of pain and swelling of the right knee. He bumped his right knee into a pole 2 days ago while working. He had one episode of similar pain two years ago that resolved with over-the-counter analgesics. He denies any illicit drug use. He has no other medical problems and does not take any medications. His temperature is 37.2°C (98.9°F), and blood pressure is 126/76 mmHg. Examination reveals swelling, warmth and decreased range of motion of the right knee. All other joints are within normal limits. Synovial fluid analysis shows positive birefringent crystals and negative Gram stain. These crystals are most likely composed of?
Hydroxyapatite
Monosodium urate
Calcium pyrophosphate
Calcium oxalate
Ammonium phosphate
A 53-year-old Caucasian man comes to the emergency department at 2 am because of severe pain in his right great toe for the past 2 hours. He complains that the pain began suddenly as a dull, aching pain, and has worsened over time to a severe throbbing pain, not relieved by acetaminophen. His other medical problems include hypertension, diabetes mellitus-type 2, hypercholesterolemia, and peptic ulcer disease. He has smoked 2 packs of cigarettes daily for 30 years. He drinks 5-6 ounces of alcohol daily. He eats a lot of junk food and exercises infrequently. Both his father and mother have diabetes and hypertension. His older brother died of a myocardial infarction 2 years ago. His medications include glyburide, lisinopril, atenolol, simvastatin and famotidine. His temperature is 37.8°C (100°F), blood pressure is 160/90 mm Hg, pulse is 88/min and respirations are 16/min. On examination, the right great toe appears markedly swollen, red, and is warm to touch. Aspiration of the joint fluid reveals negatively birefringent needle shaped crystals. Apart from prescribing oral indomethacin, what other intervention would be most important to prevent the development of further attacks?
Smoking cessation
Alcohol cessation
Stopping lisinopril
Stopping simvastatin
Stopping glyburide
A 32-year old woman comes to the physician because of pain and paresthesias in her thumb, first two fingers and the radial-half of the ring finger. Her pain is worse at night and interferes with sleep. She feels tired and unable to work effectively in her office lately. She takes an over-the-counter stool softener for constipation but otherwise has no known medical problems. Her vital signs are within normal limits. When you ask the patient to maintain acute wrist flexion for 30seconds she experiences severe pain and paresthesias. Her skin is dry. Which of the following is the most likely cause of her hand symptoms?
Amyloid fibril deposition
Tenosynovial inflammation
Accumulation of matrix substances
Synovial tendon hyperplasia
Accumulation of fluid in carpal tunnel
A 51 -year-old man complains of difficulty walking and mild right-sided foot pain for the past several weeks. His medical history is significant for type 1 diabetes mellitus, hypertension and hypercholesterolemia. Physical examination reveals a significantly deformed right foot and a mildly deformed left foot. X-rays suggest effusions in several of the tarsometatarsal joints, large osteophytes, and several extra articular bone fragments. Which of the following is the most likely cause of this patient's complaints?
Hyperuricemia
Poor vascular supply
Nerve damage
Rheumatoid arthritis
Bone demineralization
A 24-year-old Caucasian female complains of weakness, skin rash, low-grade fever and joint pain. She describes pain and swelling of the hand joints and pain in her knees. Her mother suffers from rheumatoid arthritis. Her blood pressure is 145/90 mmHg, and her heart rate is 90/min. Her hematocrit is 40% and ESR is 43 mm/hr. Urinalysis is 2+ for protein. Which of the following is the best statement about this patient's joint symptoms?
Excessive bony growth is characteristic
Permanent deformity is uncommon
Subluxation and tendon damage cause permanent deformity
Cartilage degradation and muscle atrophy cause deformity
Bone resorption of the distal phalanges may result
A 67-year-old man presents to your office with two days of back pain. He was moving boxes in the garage when the pain started. The pain is not relieved by lying down and increases in intensity upon straining and coughing. He could not sleep during the night due to pain and took several tablets of acetaminophen without relief. He has never had such pain before. Physical examination reveals symmetric knee reflexes. Plantar reflexes are flexor bilaterally. Straight leg raise is negative. Local tenderness is evident upon percussion of the fourth lumbar vertebra. Which of the following is the most likely cause of this patient's condition?
Ligamentous sprain
Intervertebral disk degeneration
Apophyseal joint arthritis
Nerve root demyelinization
Vertebral body demineralization
A 38-year-old male with steroid-dependent sarcoidosis presents to the physician's office because of progressive right hip pain. He localizes the pain to right groin and states that the pain is present on weight bearing and at rest. His temperature is 37.2°C (98.9°F) and blood pressure is 156/86 mm Hg. Examination shows decreased range of motion due to pain. He also has a round face and fullness in supraclavicular area. Purple striae are present on skin. Muscle power is slightly decreased in the proximal thigh muscles in both legs. Reflexes are 2+, and there are no sensory deficits. Plain films of the right hip show no significant abnormalities ESR is 10 mm/hr. Which of the following is the most likely cause of his hip pain?
Inflammatory arthritis
Cartilage degeneration
Disruption of bone vasculature
Inflammation of the trochanteric bursa
Aortoiliac occlusion
) A 65-year-old man comes to the emergency room complaining of 2 days of severe pain and swelling of his right knee. He denies any recent respiratory illness, diarrhea or urinary symptoms. He has a history of severe degenerative joint disease and underwent total knee replacement four years ago. He drinks one can of beer every night and does not use tobacco or illicit drugs. His temperature is 40°C (104°F), blood pressure is 120/60 mmHg, and pulse is 110/min. Examination shows warmth, swelling, and tenderness over the knee. His range of motion is restricted. Synovial fluid white blood cell count is 98,000/microl. Which of the following is the most likely cause of his current condition?
Streptococcus species
Staphylococcus aureus
Chlamydia trachomatis
Neisseria gonorrhoea
Borrelia burgdorferi

A 24-year-old woman comes to the physician complaining of a skin rash and pain in her wrists, ankles and elbows over the past 4 days. She has also had a fever and sweats, but denies headache, nausea or vomiting. She has no significant past medical history and does not take any medications. She recently took a vacation with her new boyfriend. She denies any previous sexually transmitted diseases but acknowledges having unprotected sex with her new boyfriend. She does not use tobacco, alcohol or illicit drugs. Her temperature is 38.5°C (101.3°F) and her pulse is 98/min. Her oropharynx is clear and there is no thrush or lymphadenopathy. Her abdomen is benign and the pelvic examination is within normal limits. She has pain along the tendon sheaths with active and passive hand movement. A photo of her skin rash is shown below. Which of the following is the most likely cause of her symptoms?
Lyme disease
Syphilis
Gonococcemia
Meningococcemia
Acute HIV infection
A 43-year-old Caucasian female has a long history of polyarthritis. She also complains of fatigue, low-grade fever, weakness and recent weight loss. Her current medications are methotrexate, naproxen and ranitidine. Physical examination reveals deformed hand joints and a soft, tender mass palpated in the right popliteal fossa. The latter finding is best explained by:
Subcutaneous abscess
Inflamed synovium
Lymphedema
Venous thrombosis
Bony growth
A 45-year-old woman with long-standing, well-controlled rheumatoid arthritis develops severe pain and swelling in the left elbow over 2 days. She is not sexually active. Arthrocentesis reveals cloudy fluid. Synovial fluid analysis reveals >100,000 cells/mL; 98% of these are PMNs. What is the most likely organism to cause this scenario?
Streptococcus pneumoniae
Neisseria gonorrhoeae
Staphylococcus aureus
Escherichia coli
Pseudomnonas aeruginosa
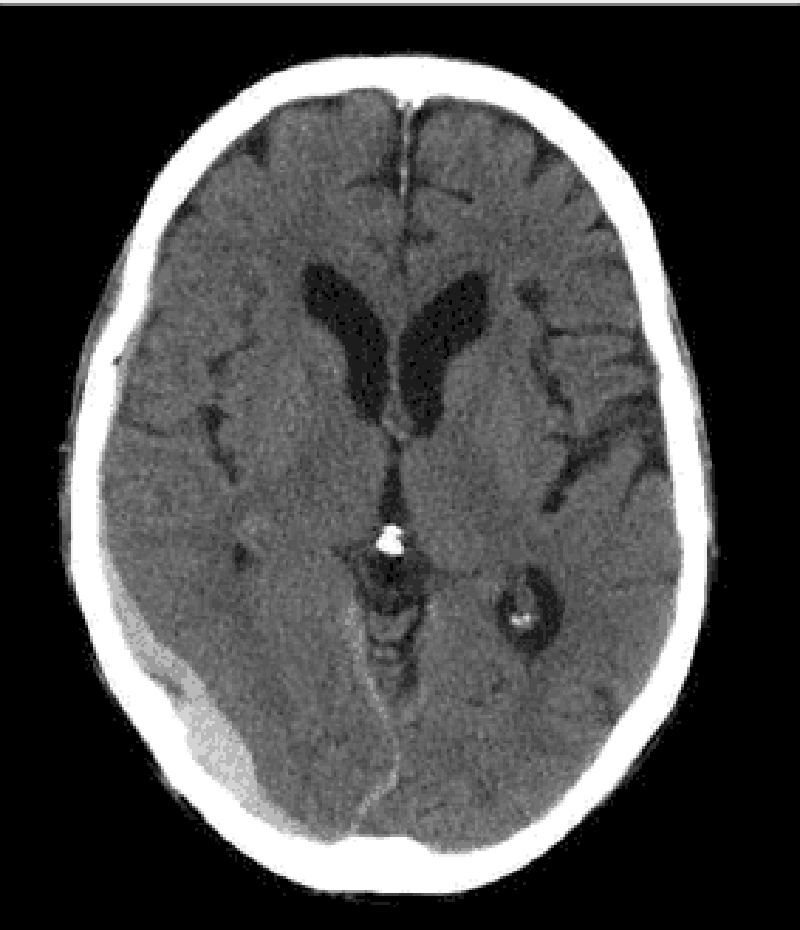
A 74-year-old Caucasian woman is brought to the emergency department after a fall. Her husband is concerned since she is on "blood thinners." Her other medical problems include hypertension, hearing loss, congestive heart failure, coronary artery bypass graft, transient ischemic attack, and atrial fibrillation. She does not use tobacco, alcohol, or drugs. Her medications include aspirin, metoprolol, digoxin, furosemide, and warfarin. Her temperature is 37.2°C (99°F), blood pressure is 140/90 mmHg, pulse is 72/min, and respirations are 14/min. CT scan of the head without contrast is shown below. Which of the following is the most likely cause of her condition?
Tearing of middle meningeal artery
Tearing of bridging veins
Hypertensive hemorrhage
Rupture of an aneurysm
Tumor of the arachnoid granulation
{"name":"Part 20 (164)", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge of infectious diseases with this comprehensive quiz designed for healthcare professionals and students alike. With 164 carefully curated questions covering a range of topics, you'll be challenged to identify pathogens, understand mechanisms of disease, and apply clinical reasoning.Covers a variety of infectious diseasesGreat for exam preparationIdeal for medical students and healthcare professionals","img":"https:/images/course6.png"}
More Quizzes
Micro GIT
221135
Infectiology
1005083
Are You A Bee, Larvae Or A Wasp?
10526
Fire Emblem Affinity Quiz
105972
Pharmacology - Test Your Drug Knowledge for Free
201018873
Which Statement Describes the Geologic Features? Free
201016226
Where the Red Fern Grows Dog Names - Can You Name Them?
201019123
5th Grade History Questions - Free Practice
201017610
LeBron James - How Well Do You Know the King?
201016614
Astraphobia Test: Can You Identify Common Phobias?
201018028
Fun Test to Take When Bored - Free Activity Finder
201018101
What Bending Element Am I? Avatar: The Last Airbender
201018248