999 Questions Pediatrie-MCQ-(301-600) Part 2 NR
A 4-week-old boy is brought to clinic by his mother because of a 1day history of labored breathing. His birth was uneventful and immunizations have been up to date. His mother reports that the patient developed conjunctivitis on the fourth day of life. On physical examination, he is breathing rapidly at 40 breaths per minute and is afebrile. His chest reveals bilateral inspiratory crackles and a slight wheeze. On chest x-ray, bilateral pneumonia is evident. The leukocyte count is elevated at 15,000 with 40% eosinophils. Which of the following is the most likely pathogen causing the patient's symptoms?
Chlamydia trachomatis
Ascaris lumbricoides
Mycoplasma pneumoniae
Pneumocystis carinii
Varicella zoster virus
A 15-year-old girl with type 1 diabetes mellitus presents to her primary care doctor for a routine check up. Perusal of her blood sugar chart indicates that her recorded blood glucose levels are routinely between 120 and 150 mg/dL before breakfast, dinner and bedtime, with the normal being 116 mg/dL. She is on NPH and regular insulin. Which of the following is the next appropriate step?
Make no changes and obtain a glycosylated Hb test
Decrease the dosage of NPH
Decrease the dosage of Regular insulin
Increase the dosage of NPH
Decrease the dosage of Regular insulin

A previously healthy 4-year-old boy is brought to the physician for evaluation of fever and respiratory distress. The patient developed fever three days ago. Since then, he has had increasing fatigue, irritability, and respiratory distress. His temperature is 100 0F (38.2 0C), pulse is 144/min, respiratory rate is 45/min, and blood pressure is 95/60 mm Hg. On examination, the child appears to be in moderate respiratory distress with tachypnea and subcostal retractions. He is tachycardic with an III/IV holosystolic murmur best heard at the cardiac apex. Peripheral pulses are present and capillary refill is three seconds. His liver is palpated three centimeters below the costal margin. A chest radiograph is shown below. Which of the following is the most likely cause of this patient's symptoms?
Myocarditis
Community-acquired pneumonia
Viral hepatitis
Rheumatic fever
Kawasaki disease
A previously healthy 5-year-old girl is brought to the emergency room from a camping trip because her parents are concerned about rabies. This morning, they found a bat in the child's tent. There were no obvious bite marks on the child. Afterwards, the girl helped her father clean animals he had brought back from a hunt, including squirrels, rabbits, and chipmunks. Later, while packing up the campsite, the child was bitten on the arm by a rat. Her encounter with which of the following animals most warrants post-exposure rabies prophylaxis?
Bat
Squirrel
Rabbit
Rat
Chipmunk
A 1-year-old child is brought in for a regular "well baby" check-up. The child appears to have strabismus. The reflection of a bright light from the ceiling of the examination room comes from a different place in each eye. The family explains that the child has always looked that way, and there has been no recent change in the appearance of his eyes. Which of the following is the most effective management?
Surgical correction as soon as it is practical to do it
No treatment unless the condition has not resolved spontaneously by age 7
Corrective lenses
Each eye patched for a month at a time, alternating sides
Surgical correction whenever he is old enough to decide whether he wants it for cosmetic reasons
A 6-year-old boy presents in clinic for a routine visit. Examination reveals coarse, dark pubic hair, an enlarged penis and testes, and acne of the face and upper back. His mother notes that he has a body odor similar to that of her teenage son after playing sports. The child is in file 99th percentile of height for his age group. Which of the following is the most likely diagnosis?
Hypothalamic tumor
Congenital adrenal hyperplasia
Klinefelter syndrome
Male pseudohermaphroditism
XYY syndrome
A 10-year-old girl is brought to a pediatrician because her mother notices that she stumbles frequendy at night, even with adequate lighting. Visual field testing demonstrates a relatively narrow mid-peripheral ring scotoma. Ophthalmoscopy demonstrates dark pigmentation in a bone spicule configuration involving the equatorial retina. Additional findings include a waxy yellow appearance to the disk and narrowed retinal arteries. Which of the following is the most likely diagnosis?
Retinitis pigmentosa
Cataract
Central retinal artery occlusion
Retinal detachment
Uveitis
A 6-week-old boy is brought to the physician because of a rash involving the diaper area. On examination, there are erythematous, slightly scaly patches covering the buttocks and the lower abdomen. Skin creases appear spared. The baby is otherwise healthy. Physical examination reveals no lymphadenopathy, fever, or other signs of organic illness. Which of the following is the most common cause of this condition?
Irritant contact dermatitis
Candidiasis
Langerhans cell histiocytosis
Psoriasis
Seborrheic dermatitis
A 1-day-old infant appears dusky in the newborn nursery during feeding. Oxygen is immediately administered by nasal cannula. Shortly afterward, she develops tachypnea. On physical examination, her blood pressure from the right upper arm is 50/30 mm Hg, her pulse is 180/min, and her respirations are 60/min. An echocardiogram is consistent with hypoplastic left heart syndrome. Which of the following would likely be found on auscultation?
No murmur, precordial hyperactivity, loud second heart sound
Continuous ductal murmur, bounding pulses
Continuous ductal murmur, poor peripheral pulses
Holosystolic murmur, poor peripheral pulses, quiet second heart sound
No murmur, precordial hyperactivity, quiet second heart sound
A 3-year-old boy was bitten while teasing a neighborhood cat. On examination, there are two puncture wounds on the right hand and some superficial scratch marks. There is erythema, warmth, and induration around the puncture sites. Which of the following organisms most likely caused the infection?
Pasturella multicoda
Bartonella henselae
Eikenella corrodens
Peptostreptococcus species
Alpha Streptococci
A 5-week-old bottle-fed boy presents with persistent and worsening projectile vomiting, poor weight gain, and hypochloremic metabolic alkalosis. Of the following diagnostic modalities, which would most likely reveal the diagnosis?
A 5-week-old bottle-fed boy presents with persistent and worsening projectile vomiting, poor weight gain, and hypochloremic metabolic alkalosis. Of the following diagnostic modalities, which would most likely reveal the diagnosis?
Barium enema
Evaluation of stool for ova and parasites
Testing well water for presence of nitrites
Serum thyroxine
A 16-year-old male is brought to the emergency department with a crush injury due to a farm accident. His immunization status is unknown. The wound is heavily contaminated with soil, and you are concerned about tetanus. Which of the following is the most appropriate management step?
Administer Tdap and tetanus immune globulin (TIG)
Administer a Tdap vaccination
Administer a Td vaccine only
Administer TIG only
Await immunization records
Children with sickle cell anemia are at increased risk of developing overwhelming infection with certain microorganisms. Which of the following is the most reasonable step to prevent such infection?
Prophylactic administration of oral penicillin daily
Periodic injections of gamma globulin
Injection of VZIG after exposure to varicella
Withholding live virus vaccines
Early use of amoxicillin at home for episodes of fever
A 14-year-old boy is brought to your office by his mother because of a two-week history of generalized edema, fatigue, and abdominal pain. His past medical history is insignificant, and the boy is not taking any medications. His BP is 110/70 mmHg and heart rate is 80/min. Urinalysis reveals proteinuria 4+, but urine sediment findings are within normal limits. Which of the following light microscopy finding would you expect in this patient's kidney biopsy?
Normal findings
Diffuse thickening of glomerular basement membrane
Subepithelial spikes
Mesangial hypercellularity
Crescent formation
While making rounds in the newborn nursery, the nurses ask you to examine a 2-day-old infant who is not feeding well. The nurse reports that the infant is irritable, is not sleeping well, and has had several episodes of vomiting and loose stools today. A review of the maternal history reveals that she had poor prenatal care and the pregnancy was complicated by intrauterine growth restriction. On examination, the infant is diaphoretic and has a high-pitched cry. The infant is also noted to have occasional sneezing and is mildly tachypneic. No dysmorphic features are noted and the remainder of the examination is unremarkable. This infant's symptoms are most likely caused by prenatal exposure to which of the following?
Heroin
Valproic acid
Phenytoin
Alcohol
Cocaine
A 5-year-old child was hit in the right eye by a toy. He is rubbing at his eye, which is watering profusely. There is a small abrasion at the corner of the eye. He is mildly photophobic, but his pupils are equal, symmetric, and reactive to light and accommodation. His vision is normal. Which of the following is the most appropriate next step in the management of this patient?
Perform a fluorescein dye stain of the cornea to determine if there is a corneal abrasion
Refer him immediately to an ophthalmologist
Irrigate the eye with sterile normal saline
Discharge him to home with antibiotic eye ointment
Apply a patch to the eye and follow-up in a week
A 9-month-old male is in for a well-child checkup. He is greater than 90th percentile for height, and he weighs 25 lbs. He no longer fits in his infant car seat, which is only recommended for use by children under 20 lbs. Which of the following is the safest car seat option for him?
A rear-facing car seat suitable for a larger child (20–40 lbs), in the rear seat of the car
To remain in the rear-facing infant seat until he is 1 year old, in the rear seat of the car
Turn the infant seat to face forward, in the rear seat of the car
A forward-facing car seat suitable for a larger child (20–40 lbs), in the rear seat of the car
A forward-facing car seat suitable for a larger child (20–40 lbs), in the front seat of the car
A 2-year-old boy has had a purulent drainage from the right nostril for a week. He is afebrile and has had no associated symptoms, such as cough. Which of the following is the most likely diagnosis?
A foreign body in the right nostril
Sinusitis
Nasal polyps
An upper respiratory infection
Allergic rhinitis
A 7 -year-old boy is brought to the office by his mother due to nocturnal enuresis. He has been wetting his bed at night for the past two years. He is otherwise healthy and has no psychological or behavioral problems. His mother is desperately asking for your help because she has tried alarms and bladder training, all to no success. What is the most appropriate next step in the management of this patient?
Desmopressin
Insulin
Prazosin
Haloperidol
Clonidine
You are called to examine a male newborn because his first feeding caused him to choke, cough and regurgitate. He was born at term via normal vaginal delivery. On examination, he has excessive salivation, fine, frothy bubbles in the mouth, abdominal distention and rattling breath sounds. Radiographs of the chest and abdomen reveal bilateral atelectasis and gastric distension. Which of the following can best explain the above findings?
Esophageal atresia
Diaphragmatic hernia
Unilateral choanal atresia
Vascular ring
Duodenal atresia
A 2-week-old neonate is brought to the office due to poor feeding and persistent vomiting. He had an episode of jerky movements of his limbs this morning. He was delivered at term with no complications and weighed 2.7kg (6 Ib) at birth. He appears lethargic, irritable and jaundiced. On examination, he weighs 2.2kg (5 Ib). His liver and spleen are enlarged. Bilateral cataracts are evident. Which of the following is most consistent with these findings?
Galactose- 1-phosphate uridyl transferase deficiency
Galactokinase deficiency
Uridyl diphosphate galactose-4-epimerase deficiency
This is a self-limiting condition and does not need any intervention
Early diagnosis and treatment does not have any effect on the patient's eyesight
A 9-year-old boy is brought to the office by his parents due to headaches, vomiting and visual disturbances. One week ago, he began to experience headaches that were most prominent in the morning. He also became lethargic, and had a decreased appetite and decline in school performance. The pertinent physical findings include an unbalanced gait, trunk dystaxia, horizontal nystagmus, and papilledema. If this child had a medulloblastoma, which structure would most likely be affected?
Cerebellar vermis
Cerebellar hemispheres
Spinocerebellar tracts
Cerebellar peduncles
Frontal lobe
A 7 -year-old girl is brought to the clinic by her mother due to a persistent postnasal drip and repeated episodes of a runny nose. In the winter, she experiences several episodes of upper respiratory tract infections, which last for two to three weeks at a time. She snores, and is unable to smell her favorite food. Her immunizations are up-to-date. On examination, she is mildly underweight for her age. She has a runny nose, and her nasal drainage is colorless and stringy. Nasal inspection reveals bilateral nasal polyps, and auscultation of the chest reveals coarse rales. What is the one condition that you would like to rule out in this child?
Cystic fibrosis
Leukemia
Foreign body aspiration
Nasal septal deviation
Allergic rhinitis
A previously heathy 3-year-old boy is brought to the emergency department (ED) due to stridor of sudden onset. Last night, he suddenly developed a high fever followed by breathing difficulty. His temperature is 40C (1 04F), pulse is 130/min, and respirations are 40/min. In the ED, the child is toxic-appearing, sitting up, leaning forward and drooling. His lungs are clear, and oxygen saturation is 85% in room air. What is the most appropriate next step in management?
Endotracheal intubation with a set-up for tracheostomy
Admit the patient and start him on broad spectrum antibiotics
Start the patient on intravenous methylprednisolone
Admit the patient and start him on nebulized racemic epinephrine
Start the patient on oral dexamethasone
A 2-week-old neonate is brought to the office due to poor feeding and persistent vomiting. He had an episode of jerky movements of his limbs this morning. He was delivered at term with no complications and weighed 2.7kg (6 Ib) at birth. He appears lethargic, irritable and jaundiced. On examination, he weighs 2.2kg (5 Ib). His liver and spleen are enlarged. Bilateral cataracts are evident. Which of the following is most consistent with these findings?
Galactose-1 -phosphate uridyl transferase deficiency
Galactokinase deficiency
Uridyl diphosphate galactose-4-epimerase deficiency
This is a self-limiting condition and does not need any intervention
Early diagnosis and treatment does not have any effect on the patient's eyesight
A 2-year-old boy is brought by his mother to the emergency department because of a high-grade fever which "does not go away" with acetaminophen. For the last four days, the child has been very irritable and is crying a lot. He is also pulling his ear and not eating well. He has been generally well, other than the occasional sore throat this season. His temperature is 38.8° C (102.2° F}, blood pressure is 90/60 mm Hg, pulse is 119/min, and respirations are 24/min. He appears well nourished, but is irritable. Physical examination reveals enlarged cervical lymph nodes and splenomegaly. The tympanic membranes are inflamed. CBC shows: WBC 81,100mm3 Hemoglobin 8.0 g/dL Hematocrit 25% Platelets 16,000 mm3 Blast forms 80% Prolymphocytes 10% Lymphocytes 10% The blast cells have condensed nuclear chromatin, small nucleoli and scant agranular cytoplasm. Subsequent histochemical staining reveals strongly positive periodic acid Schiff (PAS) reaction. No Auer rods were seen. Which of the following is the most likely diagnosis?
Acute lymphoblastic leukemia
Burkitt lymphoma
Acute myelocytic leukemia
Prolymphocytic leukemia
Myelodysplastic syndrome
An 8-month-old infant arrives to the emergency department (ED) with a 2-day history of diarrhea and poor fluid intake. Your quick examination reveals a lethargic child; his heart rate is 180 beats per minute, his respiratory rate is 30 breaths per minute, and his blood pressure is low for age. He has poor skin turgor, 5-second capillary refill, and cool extremities. Which of the following fluids is most appropriate management for his condition?
Normal saline
Dextrose 5% in 1/4 normal saline (D5 1/4 NS)
Dextrose 5% in 1/2 normal saline (D5 1/2 NS)
Whole blood
Dextrose 10% in water (D10W)
During the examination of a 2-month-old infant, you note that the infant’s umbilical cord is still firmly attached. This finding prompts you to suspect which of the following?
Leukocyte adhesion deficiency
Occult omphalocele
IgG subclass deficiency
Umbilical granuloma
Persistent urachus (urachal cyst)
You are seeing an established patient, a 4-year-old girl brought in by her mother for vaginal itching and irritation. She is toilet trained and has not complained of frequency or urgency, nor has she noted any blood in her urine. Her mother noted she has been afebrile and has not complained of abdominal pain. Mom denies the risk of inappropriate contact; the girl also denies anyone “touching her there.” Your physical examination of the perineum is significant for the lack of foul odor or discharge. You do note some erythema of the vulvar area but no evidence of trauma. Which of the following is the most appropriate course of action?
Counsel mother to stop giving the girl bubble baths, have the girl wear only cotton underwear, and improve hygiene
Refer to pediatric gynecology for removal under anesthesia of a suspected foreign body in the vagina
Refer to social services for suspected physical or sexual abuse
Swab for gonorrhea and plate on chocolate agar, and send urine for Chlamydia
Treat with an antifungal cream for suspected yeast infection
A 16-year-old girl presents with a history of primary amenorrhea. On examination, short stature and a short neck with a low posterior hairline are noted. Chromosomal analysis most likely would reveal which of the following?
45,XO
Fragile X
Trisomy 18
Trisomy 21
XXY
A 2-year-old child is brought to the emergency department with sudden onset of unresponsiveness, miosis, bradycardia, and muscle fasciculations. These findings are most suggestive of poisoning with which of the following?
Organophosphates
Acetaminophen
Salicylates
Tricyclic antidepressants
Vitamin A
A 2-year-old girl presents with fever of 39.3 C and irritability. She has had an upper respiratory tract infection for 4 days. On examination, the right ear is bulging and has poor movement on insufflation. Which of the following organisms is most likely responsible for these findings?
S. pneumoniae
S. aureus
M. pneumoniae
E. coli
Group A Streptococcus
An infant is delivered vaginally to a 30-year-old G1P1 woman whose pregnancy was uneventful. Examination of the newborn reveals mild atrophy of the left calf. His left calcaneum and talus are in equinus and varus positions, his midfoot is in varus position, and his forefoot is in adduction. Dorsiflexion and plantar flexion of the ankle are limited. The neurologic examination is normal. What is the next best step in the management of this patient?
Stretching, manipulation, followed by serial casting
Reassurance
Casting of the whole leg up to the hip
Surgical correction within the first month of life
Watchful waiting
A 14-year-old boy is brought to your office by his mother because of a two-week history of generalized edema, fatigue, and abdominal pain. His past medical history is insignificant, and the boy is not taking any medications. His BP is 110/70 mmHg and heart rate is 80/min. Urinalysis reveals proteinuria 4+, but urine sediment findings are within normal limits. Which of the following light microscopy finding would you expect in this patient's kidney biopsy?
Normal findings
Diffuse thickening of glomerular basement membrane
Subepithelial spikes
Mesangial hypercellularity
Crescent formation
A young infant is noted to have developed constipation over the past week, and then facial diplegia and difficulty sucking and swallowing. The child has been colicky, and the maternal grandmother has been treating the child with a mixture of weak tea, rice water, and honey. Which of the following disorders is the most likely culprit in this child?
Botulism
Infantile spinal muscular atrophy
Myastheniagravis
Congenital myotonic dystrophy
Duchenne muscular dystrophy
At birth, an infant is noted to have an abnormal neurologic examination. Over the next few weeks he develops severe progressive central nervous system (CNS) degeneration, an enlarged liver and spleen, macroglossia, coarse facial features, and a cherry-red spot in the eye. Which of the following laboratory findings most likely explains this child’s problem?
Deficient activity of acid -galactosidase
Reduced serum hexosaminidase A activity
Defective gene on the X chromosome
Complete lack of acid -galactosidase activity
Deficientactivityofgalactosyl-3-sulfate-ceramidesulfatase(cerebrosidesulfatase)
A 3-year-old boy from a refugee camp is brought to the clinic for examination. His medical history is unknown. On examination, there is marked photophobia. He appears malnourished, and his weight is <5th percentile for age after hydration. His bones and ribs are prominent, and little subcutaneous fat is identified. His abdomen is concave with decreased bowel sounds. There is marked scaling and fissuring at the corners of his mouth, as well as inflammation and cracking of his lips. His tongue is atrophic. The tongue and oropharyngeal mucous membranes are dark red. Conjunctival pallor is present. There are pinkish-red, erythematous, scaly patches on his eyebrows, cheeks, and nose. This dermatitis is also present on the scrotal skin and extends onto the medial aspect of both thighs. Otherwise, his skin is very pale, and his fingernails and toenails are brittle. What is the most appropriate intervention for this patient?
Riboflavin (vitamin B 2)
Dermatology referral
Ascorbic acid (vitamin C)
Niacin (vitamin B 3)
Thiamine (vitamin B 1)
14-year-old boy comes to the office because he has been feeling a mass under his right nipple for the last three weeks. The physical examination reveals clinical findings suggestive of right gynecomastia with very mild tenderness. The left breast and the rest of the physical exam is unremarkable. His testis is 2 cm in length and has 3 ml volume. What is the most appropriate next step in the management of this patient?
Reassurance
Biopsy of breast mass
Karyotyping
MRI brain
Serum prolactin levels
The parents of a 2-year-old bring her to the emergency center after she had a seizure. Although the parents report she was in a good state of health, the vital signs in the emergency center reveal a temperature of 39C (102.2F). She is now running around the room. Which part of the story would suggest the best outcome in this condition?
Otitis media on examination
A CSF white count of 100/L.
The seizure lasted 30 minutes
The child was born prematurely with an intraventricular hemorrhage
The family reports the child to have had right-sided tonic-clonic activity only
About 12 days after a mild upper respiratory infection, a 12-year-old boy complains of weakness in his lower extremities. Over several days, the weakness progresses to include his trunk. On physical examination, he has the weakness described and no lower extremity deep tendon reflexes, muscle atrophy, or pain. Spinal fluid studies are notable for elevated protein only. Which of the following is the most likely diagnosis in this patient?
Guillain-Barré syndrome
Bell palsy
Muscular dystrophy
Charcot-Marie-Tooth disease
Werdnig-Hoffmann disease
A premature neonate develops respiratory distress syndrome several hours after birth. The infant is placed on a respirator and given other appropriate care. However, when the infant reaches a corrected gestational age of 36 weeks, he does not tolerate weaning from the ventilator. A chest x-ray film demonstrates alternating areas of hyperaeration and pulmonary scarring, resulting in parenchymal streaks and hyperexpanded areas. Which of the following is the most likely diagnosis?
Bronchopulmonary dysplasia
Apnea of prematurity
Cystic fibrosis
Persistent pulmonary hypertension of the newborn
Transient tachypnea of the newborn
Approximately 19 days after having had a severe sore throat, a 10-year-old girl is taken to a pediatrician because she is complaining that her arms and legs hurt. The mother reports that before the extremity pain began, the child had a rash with irregular boundaries that lasted about a day. Physical examination demonstrates mild fever, as well as swelling and erythema around several large joints. Laboratory studies show an elevated erythrocyte sedimentation rate, and ECG demonstrates a prolonged PR interval. Which of the following is the most likely explanation for these findings?
Antigenic mimicry
Bacterial infection of valves
Parasitic infection of myocytes
Toxin production
Viral infection of myocytes
A neonate has Down syndrome. Maternal hydrammos had been noted prenatally. After the first feeding, the infant has projectile vomiting with bile-stained vomitus. An x-ray film demonstrates a "double-bubble sign" in the abdomen. Which of the following is the most likely diagnosis?
Duodenal atresia
Esophageal atresia
Hirschsprung disease
Hypertrophic pyloric stenosis
Meconium plug syndrome
A 1 0-year-old boy is brought to the office by his parents because he is developing dark facial hair, deepening of the voice and a rapid height increase. He also complains of persistent headaches which are resistant to over-the-counter analgesics for the past 2 weeks. He denies nausea, vomiting or visual disturbances. His medical history is unremarkable. Physical examination reveals coarse pubic and axillary hair. Other pertinent findings include lid retraction, paralysis of upward and downward gaze, and poor pupillary reaction to light. His deep tendon reflexes are normal, Babinski sign is negative, and there are no focal neurologic signs. What tumor is most likely responsible for this child's symptoms?
Pinealoma
Medulloblastoma
Neuroblastoma
Oligodendroglioma
Craniopharyngioma
A mother brings her daughter into the clinic for a routine health-care visit. On examination, you note that she walks alone, knows two words, throws objects, and comes when called. What is the most likely age of this infant?
12 months
6 months
9 months
15 months
18 months
A 16-year-old Caucasian male presents to the office with pain and limited motion of the right knee. His right knee, as well as his right ankle, has swelled several times before. He has a history of easy bruising since childhood, and an episode of excessive bleeding after a tooth extraction. His uncle had similar problems. Which of the following is the most likely cause of this patient's joint pain?
Hemosiderin deposition and fibrosis
Granulomatous inflammation
Immunologic tissue injury
Wear-and-tear phenomenon
Traumatic injury
A 17-year-old girl comes to the clinic with several weeks of joint pain and rash. The joint pain is most prominent in the hands. She states that the pain is most severe in the morning and tends to improve over the day. She has noted some swelling of her fingers. She has also had a rash on her face that becomes more prominent when she is outdoors. She states that sunlight tends to bother her eyes. On further questioning, she states that she has not felt well for several months. She has had intermittent fever, has been more tired than usual, and has lost weight although she has not been restricting her diet. On physical examination, she looks tired. She has lost 5 lbs since her last visit 1 year ago. She has an erythematous rash on her cheeks. She has several shallow ulcers in her mouth. She has fusiform swelling of her fingers and pain with movement of her fingers. Which of the following is the most likely diagnosis?
Systemic lupus erythematosus (SLE)
Dermatomyositis
Juvenile rheumatoid arthritis
Rheumatic fever
Lyme disease
A full-term newborn develops cyanosis a few hours after birth. Oxygen administration does not improve color or oxygen saturations. Which of the following is the most likely diagnosis?
Pulmonary stenosis
Aortic stenosis
Atrial septal defect
Ventricular septal defect
Patent ductus arteriosus
As part of your anticipatory guidance to new parents of a healthy new- born, you suggest putting the child in which of the following positions for sleep?
Supine position
Prone position
Seated position
Trendelenburg position
A hammock
A mentally retarded 14-year-old boy has a long face, large ears, micropenis, and large testes. Chromosome analysis is likely to demonstrate which of the following?
Fragile X syndrome
Trisomy 21
Trisomy 18
Trisomy 13
Williams syndrome
A 5-month-old child with poor growth presents to the ER with generalized tonic-clonic seizure activity of about 30-minute duration that stops upon the administration of lorazepam. Which of the following historical bits of information gathered from the mother is most likely to lead to the correct diagnosis in this patient?
The mother has been diluting the infant’s formula to make it last longer
The child has had congestion without fever for the past 3 days
The child is developmentally normal, as are his siblings
The mother reports there are two dogs and one cat at home
The mother previously worked as an attorney in an energy-trading firm
A 13-year-old girl presents with parental concerns of poor posture. She has not had any back pain. On examination, she has unequal shoulder height, asymmetric flank creases, and a forward-bending test that shows rib asymmetry. The physical examination is otherwise normal. Which of the following is the most likely cause of her condition?
Idiopathic scoliosis
Congenital scoliosis
Leg length inequality
Postural roundback
Scheuermann kyphosis
After 10 days of nasal congestion and rhinorrhea, a 3-month-old infant develops a severe hacking cough during which he repeatedly turns dusky and appears to choke on or to vomit profuse thick, clear nasopharyngeal mucus. For 7 days, the coughing continues unabated. On physical examination, he is afebrile and his lungs are clear. His chest x-ray is normal. His WBC count is 24,000/mm3, with 15% polymorphonuclear cells, 82% lymphocytes, and 3% monocytes. Which of the following antibiotics should be used to treat this patient?
Erythromycin
Amoxicillin
Amoxicillin-clavulanic acid
Tetracycline
No antibiotics are necessary
An 18-month-old boy presents with a history of fever to 39.0°C for 5 days. He has also been irritable and has not been drinking well. Associated symptoms include red eyes, a rash, and some trouble walking. On physical examination, he has a temperature of 39.5°C. He has bilateral bulbar conjunctivitis, a strawberry tongue, an inflamed oral pharynx, edema of the hands and feet, a morbilliform rash, and cervical lymphadenopathy. He is very irritable. His CBC shows a WBC of 15,000/mm3 with 60% neutrophils, 35% lymphocytes, and 5% monocytes. His hemoglobin is 12.0 g/dL and platelet count is 500,000/ mm3. Which of the following is the most likely diagnosis?
Kawasaki disease
Erythema infectiosum (fifth disease)
Rubella
Rubeola (measles)
Rheumatic fever
A 6 month old male is brought in to the Emergency Room by his mother who states that when she picked him up from the baby-sitter he was not acting right. The baby-sitter stated that he was sleeping more and was fussy. On examination the baby is stuporous. His temperature is 37.8 C (99.9 F), pulse is 140/min, and respirations are 36/min. A 4 cm ecchymosis is noted on his right cheek. The remainder of the physical examination is unremarkable. The physician suspects possible physical abuse. He orders a CT scan of the head, skeletal survey, chemistry panel and complete blood count. Which of the following diagnostic tests should also be ordered?
Coagulation studies
Ammonia level
Lipid panel
Thyroid studies
Urine electrolytes
An infant is delivered at full term by a spontaneous vaginal delivery to a 29-year-old primigravida. At delivery, the infant is noted to have subcostal retractions and cyanosis despite good respiratory effort. The abdomen is scaphoid. On bag and mask ventilation, auscultation of the lungs reveals decreased breath sounds on the left, with heart sounds louder on the right. Which of the following is the most likely diagnosis?
Diaphragmatic hernia
Dextrocardia with situs inversus
Pneumonia
Pulmonary hypoplasia
Spontaneous pneumothorax
A 12-year-old girl comes to the physician for an annual examination. She has been in good health for the past year and has no complaints. She began having menses this year and, after a few irregular cycles, is now having a monthly period. Past medical history is significant for multiple episodes of otitis media as a child. Past surgical history is unremarkable. She takes no medications and has no known drug allergies. Physical examination is unremarkable. If not currently immune, which of the following immunizations should this patient most likely receive?
Hepatitis B virus immunization
HIV immunization
Japanese encephalitis virus immunization
Rabies virus immunization
Salmonella typhi immunization

A 4-week-old boy presents with a 10-day history of vomiting that has increased in frequency and forcefulness. The vomitus is not bile stained. The child feeds avidly and looks well, but he has been losing weight. An ultrasound of the abdomen is shown. Which of the following is the most likely diagnosis?
Surgical consultation for pyloromyotomy
Upper GI with small-bowel follow through
Intravenous (IV) fluids alone to maintain hydration
Air contrast enema
Computed tomography (CT) of the brain
A 12-month-old girl has been spitting up her meals since 1 month of age. Her growth is at the 95th percentile, and she is otherwise asymptomatic and without findings on physical examination. Which of the following is the most likely diagnosis?
Gastroesophageal reflux
Pyloric stenosis
Partial duodenal atresia
Hypothyroidism
Tracheoesophageal fistula
A 14-year-old girl has a 9-month history of diarrhea, abdominal pain (usually periumbilical and postprandial), fever, and weight loss. She has had several episodes of blood in her stools. Which of the following is the most likely diagnosis?
Crohn disease
Chronic appendicitis
Chronic pancreatitis
Bulimia
Gallstones
A 12-year-old girl complains of intermittent palpitations. She had previously been in excellent health and has met all development milestones. There is no family history of heart disease. She is on no medications and takes no drugs. She states that the palpitations begin and end suddenly and usually last a couple of hours. She is otherwise asymptomatic between episodes. The physical examination is normal. An ECG reveals a shortened PR interval and a slow upstroke of the QRS wave in lead III. Which of the following is the most likely diagnosis?
Wolff-Parkinson-White syndrome
Anxiety attack
Lown-Ganong-Levine syndrome
Nodal reentrant tachycardia
Sinus tachycardia
An 11-year-old boy is brought to the office by his mother because "he is sick." He has had headaches for the past several weeks, and has vomited 4 times in the past 5 days. He drinks large amounts of water and goes to the bathroom all the time. He is no longer interested in playing football and going out with his friends. His temperature is 37.0C (98.6F), blood pressure is 11 8/78 mm Hg, pulse rate is 84/min, and respirations are 16/min. On examination, there is loss of peripheral visual fields. His laboratory findings are as follows: W BC 7,800/mm3 Hemoglobin 12.6 g/dl Hematocrit 35% Platelets 199,000/mm3 Sodium 145 mEq/L Potassium 3.6 mEq/L Bicarbonate 24 mEq/L Blood urea nitrogen 18 mg/dl Serum creatinine 1.0 mg/dl Blood glucose 88 mg/dl X-rays of the head reveal a calcified lesion above the sella. What is the most likely diagnosis?
Craniopharyngioma
Pituitary adenoma
Meningioma
Empty sella syndrome
Ependymoma
A 4-week-old male infant is brought to the office due to several episodes of projectile vomiting for the last few days. The vomitus contains milk and doesn't contain bile or blood. The child's appetite has increased for the last few days. He has been fed with goat's milk since birth, but doesn't seem to tolerate it anymore for the last few days. He vomits a few minutes after feedings. He appears dehydrated, and abdominal examination reveals no mass. Blood tests reveal macrocytosis. What is the most appropriate next step in the management of this patient?
Ultrasound of the abdomen
Barium swallowing
Substitute goat's milk with another form of milk
Divide his feedings
Add folic acid to relieve his vomiting
A 6-year-old Hispanic boy is brought to your office by his mother because of severe pain in his right hip and refusal to walk for the last 2 days. His blood pressure is 100/70 mm Hg, pulse is 90/min, respirations are 18/min, and temperature is 38.7C (102.7F). His WBC count is 19,000/mm3 and ESR is 55 mm at one hour. On examination, he keeps his right hip externally rotated, and cries out in pain on any movement involving the right hip. Joint aspiration reveals a turbid fluid with total WBC: 90,000/mm3 and numerous bacteria. What is the most appropriate management in this patient?
Emergency surgical drainage
Salicylates, rest and physical therapy
Intravenous antibiotics
Oral antibiotics
Splint the hip joint and administer intravenous antibiotics
A 6-week-old child arrives with a complaint of “breathing fast” and a cough. On examination you note the child to have no temperature elevation, a respiratory rate of 65 breaths per minute, and her oxygen saturation to be 94%. Physical examination also is significant for rales and rhonchi. The past medical history for the child is positive for an eye discharge at 3 weeks of age, which was treated with a topical antibiotic drug. Which of the following organisms is the most likely cause of this child’s condition?
Chlamydia trachomatis
Neisseria gonorrhoeae
Staphylococcus aureus
Group B streptococcus
Herpesvirus
A full-term neonate presents with hypotonia, lethargy and poor feeding over the past three hours. The pregnancy was uneventful, but during delivery, the neonate presented with shoulder dystocia and subsequently obtained a fracture of the clavicle. His Apgar scores are 7 and 8 at one and five minutes, respectively. His birth weight is 4000g. His vital signs are normal. Physical examination reveals an enlarged tongue, mild microcephaly, prominent occiput, prominent eyes and omphalocele. Abdominal palpation reveals an enlarged liver and kidneys. The initial work-up reveals hypoglycemia and hyperinsulinemia. What is the most likely diagnosis?
Beckwith-Wiedemann syndrome
Congenital hypothyroidism
Maternal diabetes
WAGR syndrome
Denys-Drash syndrome
A 4-year-old child is brought to the emergency department after he ingested liquid oven cleaner. His vital signs are stable. He is crying and drooling with blood-tinged secretions. His lips and chin are swollen and erythematous. His clothes are contaminated with the material. His breathing appears normal. His lungs are clear. Based on these findings, what is the best next step in the management of this patient?
Upper gastrointestinal endoscopy
Barium swallow
High dose corticosteroids
Antibiotics
Nasogastric lavage
A male infant is born to a primigravid woman whose pregnancy was uneventful. The delivery was uncomplicated. Physical examination of the newborn reveals deformity of the feet, specifically adduction of the anterior aspect of the foot with a convex lateral border and concave medial border. The ankle movements are normal, and passive and active movement of the foot overcorrects the deformity into abduction. AP radiographs reveal mild adduction of the metatarsals at the tarsometatarsal articulation, and an increased angle between the 1st and 2nd metatarsals. What is the best next step in the management of this patient?
Reassurance
Immediate casting
Surgical correction at age two
Surgical correction within the first month of life
Orthosis
You are called to a delivery of a term infant, about to be born via cesarean section to a mother with multiple medical problems, including a 1-month history of a seizure disorder, for which she takes phenytoin; rheumatic heart disease, for which she must take penicillin daily for life; hypertension, for which she takes propranolol; acid reflux, for which she takes aluminum hydroxide; and a deep venous thrombosis in her left calf diagnosed 2 days ago, for which she was started on a heparin infusion. The obstetrician is concerned about the possible effects of the mother’s multiple medications on the newborn infant. Which of the following medications is most likely to cause harm in this newborn infant at delivery?
Propranolol
Penicillin
Aluminum hydroxide
Phenytoin
Heparin
Your older sister, her husband, their 2-day-old infant, and their pet Chihuahua arrive at your door. The parents of the child are concerned because the pediatrician noted the child was “yellow” and ordered some studies. They produce a wad of papers for you to review. Both the mother and baby have O-positive blood. The baby’s direct serum bilirubin is 0.2 mg/dL, with a total serum bilirubin of 11.8 mg/dL. Urine bilirubin is positive. The infant’s white blood cell count is 13,000/μL with a differential of 50% polymorphonuclear cells, 45% lymphocytes, and 5% monocytes. The hemoglobin is 17 g/dL, and the platelet count is 278,000/μL. Reticulocyte count is 1.5%. The peripheral smear does not show fragments or abnormal cell shapes. Which of the following is the most likely explanation for this infant’s skin color?
Physiologic jaundice
Rh or ABO hemolytic disease
Sepsis
Congenital spherocytic anemia
Biliary atresia
A 14-day-old male infant is brought to the emergency department due to spasms involving the whole body. He has been having very poor suckling over the last couple of days. He was delivered vaginally by an untrained birth attendant, and his mother never sought any pre- or antenatal care. The pertinent physical finding is a swollen and erythematous umbilical cord. What is the most likely diagnosis of this patient?
Tetanus
Congenital syphilis
Group B streptococcal infection
Congenital rubella
Toxoplasmosis
A 4-year-old boy falls from the jungle gym at preschool. He sustains minor abrasions and contusions, and is taken care of by the school nurse. His parents take him that same afternoon to his regular pediatrician and demand "a thorough check-up" for possible internal injuries. The pediatrician complies, and a complete physical examination is normal. His hemoglobin is 14 g/dL, and a urinalysis shows the presence of microhematuria. Which of the following is the most appropriate next step in management?
Urologic workup, starting with a sonogram
CT scan of the abdomen and pelvis
Reassure the parents that microhematuria from minor trauma will resolve spontaneously
Serial hemoglobin and hematocrit determinations
Retrograde ureterogram and cystogram
A 9-year-old boy is brought to the pediatric clinic by his mother, who noticed that the left side of his mouth has started to droop over the past several days. In addition, he is unable to close his left eye completely and complains of it burning. Review of systems reveals a cold approximately two weeks ago and recent decreased taste sensation. Physical examination reveals a well nourished male with normal vital signs. There is left eye ptosis and mild erythema of the left conjunctiva. His smile is asymmetrical on the left. Laboratory evaluation, including a complete blood count and chemistry profile, are normal. Which of the following infections is most closely associated with this patient's condition?
Epstein-Barr Virus
Group A Streptococcus
Human Immunodeficiency Virus
Influenza
Measles

A 5-year-old girl is brought to the physician with low grade fever and rhinorrhea. Her symptoms began ten days ago. She has also had persistent purulent rhinorrhea, nasal congestion, and a dry cough during the day that worsens at night. Her symptoms do not seem to be improving. On examination, the child has erythema and swelling of the nasal turbinates with purulent nasal drainage. She has evidence of drainage in the posterior pharynx as well. The remainder of her examination is unremarkable. Computed topography of her face is shown below. Which of the following is the most common predisposing factor for her condition?
Viral upper respiratory infection
Allergic rhinitis
Septal deformities
Adenoidal hypertrophy
Environmental mucosal irritants

A 1-week-old previously healthy infant presents to the emergency room with the acute onset of bilious vomiting. The abdominal plain film in the emergency department (A) and the barium enema done after admission (B) are shown. Which of the following is the most likely diagnosis for this patient?
Malrotation with volvulus
Jejunal atresia
Hypertrophic pyloric stenosis
Acute appendicitis
Intussusception
A 3-year-old child presents to your office for an evaluation of constipation. The mother notes that since birth, and despite frequent use of stool softeners, the child has only about one stool per week. He does not have fecal soiling or diarrhea. He was born at term and without pregnancy complications. The child stayed an extra day in the hospital at birth because he did not pass stool for 48 hours, but has not been in the hospital since. Initial evaluation of this child should include which of the following?
A barium enema and rectal manometry
A child psychiatry evaluation for stool retention and parenting assistance
Plain films of the abdomen
Dietary log and observation
Beginning oral antispasmodic medication
A 3-month-old boy is brought to the pediatrician because of a red growth on his arm. The pregnancy had been uncomplicated, and the infant has been meeting all development milestones. He has been healthy so far and has received all scheduled immunizations. He is currently being breast-fed. His skin was clear at birth, but when he was 2 months old, his mother noted a light red growth on his arm. Within the past month, it has increased in size and has turned bright red. Which of the following is the most appropriate treatment for this disorder?
Observation
Topical corticosteroids
Argon laser therapy
Radiation therapy
Surgery
A 2-year-old boy is hospitalized for severe pneumonia requiring endotracheal intubation and mechanical ventilation. His hemoglobin level is 13.2 mg/dl and his WBC count is 3,200/mm3. The absolute level of CD3- positive lymphocytes is normal but the level of CD 19-positive lymphocytes is very low. This patient would benefit most from which of the following as a maintenance therapy?
Intravenous infusion of immune globulin
Antiretroviral therapy
Administration of live attenuated vaccines
White blood cell transfusion
Enzyme replacement therapy
A 14-year-old African-American boy presents to your office with difficulty walking for the past several weeks. He complains of pain in the right hip. He describes two episodes of severe hip pain and one previous episode of abdominal pain requiring hospitalization. Physical examination reveals motion restriction in the right hip joint. His joint is not erythematous or tender to palpation. His hematocrit is 22%. This patient's difficulty walking is most likely secondary to which of the following:
Osteonecrosis
Osteoarthritis
Septic arthritis
Gouty arthritis
Osteoporosis
A 2-week-old boy in the neonatal intensive care unit had a birth weight of 1200 g. Ultrasound of the head reveals grade II intraventricular hemorrhage and periventricular leukomalacia. An ophthalmologic examination reveals retinopathy of prematurity of both eyes. In addition, a hearing screen demonstrates bilateral hearing deficits. Which of the following is the most important determinant of this child's neurodevelopmental outcome?
Length of gestation
Maternal education
Outcome of the mother's previous pregnancies
Quality of prenatal care
Socioeconomic status of the family
A 2-year-old girl is brought to her pediatrician by her parents because of increasing lethargy and irritability. She has just started walking, and is teething and likes to chew on the woodwork around the windows. Physicalexamination reveals a tender abdomen. Laboratory studies indicate high iron and ferritin levels. The peripheral blood smear shows basophilic stippling. Which of the following is the most likely diagnosis?
Lead poisoning
Cobalamin deficiency
Diphyllobothriasis
Iron deficiency
Porphyria
A 15-month-old boy is brought to the ER because of fever and a rash. Six hours earlier he was fine, except for tugging on his ears; another physician diagnosed otitis media and prescribed amoxicillin. During the interim period, the child has developed an erythematous rash on his face, trunk, and extremities. Some of the lesions, which are of variable size, do not blanch on pressure. The child is now very irritable, and he does not interact well with the examiner. Temperature is 39.5C (103.1F). He continues to have injected, immobile tympanic membranes, but you are concerned about his change in mental status. Which of the following is the most appropriate next step in the management of this infant?
Perform a lumbar puncture
Begin administration of IV ampicillin
Begin diphenhydramine
Discontinue administration of ampicillin and begin trimethoprim with sulfamethoxazole
Perform bilateral myringotomies
The 3-year-old sister of a newborn baby develops a cough diagnosed as pertussis by nasopharyngeal culture. The mother gives a history of having been immunized as a child. Which of the following is a correct statement regarding this clinical situation?
Erythromycin should be administered to the infant
The mother has no risk of acquiring the disease because she was immunized
Hyperimmune globulin is effective in protecting the infant
The risk to the infant depends on the immune status of the mother
The 3-year-old sister should be immediately immunized with an additional dose of pertussis vaccine
A 10-hour-old newborn is noted to have a swelling in the scalp which was not present at birth. The swelling is limited to the surface of one cranial bone. There are no visible pulsations, indentations of the skull, or discoloration of the overlying scalp. What is the most likely diagnosis?
Cephalohematoma
Caput succedaneum
Cranial meningocele
Intracranial hemorrhage
Depressed skull fracture
A 3-year-old boy is brought by his father to the Emergency Department with fever, headache and neck pain that developed over the past several hours. The father states he is not the birth father, and that he and his wife adopted the boy at 18 months of age after his birth mother abandoned him. Physical examination reveals a lethargic male with a temperature of 39.7 C (103.5 F). There is photophobia, and mildly injected conjunctiva are appreciated. Pupils are equal and reactive and funduscopic examination is unremarkable. The patient has neck stiffness with a positive Kernig's sign. A complete blood count reveals a leukocyte count of 24,000/mm3 with 64 segmented neutrophils and 25 bands. A lumbar puncture is performed that reveals elevated CSF pressure, decreased glucose, and elevated protein. A Gram's stain shows gram-negative pleomorphic rods. There is no growth on blood agar. Growth on chocolate agar reveals white colonies. Which of the following is the most likely pathogen?
Haemophilus influenzae type b
Haemophilus ducreyi
Neisseria meningitidis
Listeria monocytogenes
Streptococcus pneumoniae
A 16-month-old girl is brought to medical attention because of irritability, poor feeding, and temperatures up to 39.4 C (103 F). Careful history and physical examination fail to disclose any identifiable cause of her fever. There is some degree of abdominal tenderness on palpation. Which of the following is the most appropriate next step in diagnosis?
Culture of urine obtained by transurethral catheterization
Microscopic examination and culture of stool
Renal ultrasound
Chest x-ray films
Voiding cystourethrogram
A premature neonate with respiratory distress syndrome is maintained on mechanical ventilation in a neonatal intensive care unit. Two weeks after delivery, the nurses in the intensive care unit notice that higher ventilation settings are needed and that more secretions are being suctioned from the endotracheal tube. A chest x-ray film shows questionable new infiltrates. Which of the following is the most likely pathogen?
Coagulase-negative oxacillin-resistant Staphylococcus
Coagulase-negative oxacjllin-sensitive Staphylococcus
Group B Streptococcus
Methkillin-resistant Staphylococcus aureus
Methicillin-sensitive Staphylococcus aureus
A 2-year-old boy is brought to the emergency department (ED) in acute respiratory distress. He is afebrile, and has a heart rate of 100/min, respiratory rate of 80/min, and Sa02 of 84% on room air. He is sitting upright, and has significant nasal flaring and intercostal retractions. He is given supplemental oxygen in the ED. Chest x-ray reveal hyperinflation of the right lung, mediastinal shift to the left, and a severely hypoinflated left lung Which of the following is the most appropriate next step in management?
Direct laryngoscopy and rigid bronchoscopy
Bronchodilator therapy
Direct laryngoscopy and flexible bronchoscopy
Segmental lung resection
CT scan of the chest
A 2-year-old presents to the emergency center with several days of rectal bleeding. The mother first noticed reddish-colored stools 2 days prior to arrival and has since changed several diapers with just blood. The child is afebrile, alert, and playful, and is eating well without emesis. He is slightly tachycardic, and his abdominal examination is normal. Which of the following is the best diagnostic study to order to confirm the diagnosis?
Radionucleotide scan
Exploratory laparotomy
Barium enema
Ultrasound of the abdomen
Stool culture
A 4-year-old boy is brought to the office because his school teacher thinks that his dusky blue appearance may have something to do with his inability to participate in regular school activities. His mother says that he has always appeared slightly out of breath. He has no history of any trauma, past surgery or medical conditions. His birth history is unremarkable. Physical examination reveals perioral cyanosis and a systolic murmur along the left sternal border. When the child squats, the murmur disappears and the cyanosis slightly improves. What is the most likely diagnosis of this patient?
Tetralogy of Fallot
Ventricular septal defect
Atrial septal defect
Coarctation of aorta
Eisenmenger syndrome
25. The 1-year-old brother of a child with known abetalipoproteinemia is evaluated by a pediatrician for the disease. The 1 -year-old has been exhibiting steatorrhea and ataxia. Which of the following would most strongly support the suspected diagnosis?
Acanthocytes on peripheral smear
"Crumpled silk" histiocytes on bone marrow biopsy
Globoid cells on brain biopsy
Metachromatic deposits on sural nerve biopsy
"Sea-blue" histiocytes on bone marrow biopsy
A 2-month-old infant is evaluated by a pediatric cardiologist. The infant was noted at birth to have an upper left sternal border ejection murmur. The infant at that time was not cyanotic, but slowly developed cyanosis over the next two months. At the time of the pediatric cardiologist's examination, an ECG showed right axis deviation and right ventricular hypertrophy. A chest x-ray film showed a small heart with a concave main pulmonary artery segment and diminished pulmonary blood flow. Which of the following is the most likely diagnosis?
Tetralogy of Fallot
Complete atrioventricular canal defect
Hypoplastic left ventricle
Isolated atrial septal defect
Transposition of the great arteries
A 6-year-old boy is brought to the emergency department because of the acute onset of headache, nausea, and vomiting. On arrival, physical examination reveals marked nuchal rigidity and funduscopic evidence of papilledema. A head CT scan reveals a solid tumor in the posterior fossa, centered in the cerebellar vermis and extending to the fourth ventricle. An emergency craniotomy is performed, during which a small sample of the tumor is sent to the pathologist for a frozen section consultation. Which of the following is the most likely diagnosis?
Medulloblastoma
Ependymoma
Glioblastoma multiforme (GBM)
Hemangioblastoma
Oligodendroglioma
A 15-month-old girl is brought to the office by her mother due to failure to thrive. For the past three months, the child has had foul-smelling, non-bloody, loose stools 7 to 8 times daily. On examination, she is irritable and has a protruding belly and trace pre-tibial edema. There are erythematous vesicles symmetrically distributed over the extensor surfaces of her elbows and knees. Preliminary laboratory investigations are significant for hypochromic microcytic anemia, and stool examination is negative for ova or parasites. What is the most likely cause of failure to thrive in this child?
Celiac disease
Lactose intolerance
Laxative abuse
Giardiasis
Shigella gastroenteritis

The 4-year-old child pictured below is noted to have the tooth decay as shown. This characteristic pattern of tooth decay is caused by which of the following?
Prolonged use of a baby bottle
Excessive use of fluoride
Tetracycline
Use of bottled water that lacks fluoride
Consumption of too much candy
A 5-month-old infant is brought to the office for the evaluation of persistent vomiting, failure to thrive, and developmental delay. His antenatal and postnatal histories are not known to his Caucasian foster parents, who adopted him when he was 4 months old. The physical examination reveals an infant with blonde hair, fair skin and blue eyes. His urine has a peculiar musty odor. His plasma phenylalanine level is 40 mg/dl and tyrosine level is normal. His urinary phenylpyruvic and a-hydroxy phenylacetic acid levels are both increased. What is the most likely etiology of this child's symptoms?
Classic phenylketonuria
Benign hyperphenylalaninemia
Transient hyperphenylalaninemia
Tyrosinemia
Alcaptonuria
A 2 1/2-year-old child is evaluated by a neurologist because of difficulty walking. Neurological examination documents ataxia and mental retardation. The neurologist notes the presence of multiple telangiectasias involving the conjunctiva, ears, and antecubital fossae. The child also has a history of multiple respiratory tract infections. Immunoglobulin studies on the child would most likely demonstrate an absence of which of the following?
IgA and IgE
IgA and IgG
IgE and IgG
IgE and IgM
IgM and IgG
A 15-year-old boy with Duchenne muscular dystrophy is brought to the emergency department with increasing respiratory distress and cyanosis. On examination, he is diaphoretic, with gasping respirations, poor air entry, and diminished responsiveness. He is tachycardic at 160 beats/min. His chest x-ray film shows a lingular pneumonia, and he is intubated. He improves over the next 10 days with antibiotics but is not extubated secondary to hypoventilation on weaning because of muscle weakness. Which of the following modalities will most likely help wean him off the ventilator?
Tracheostomy
Nasopharyngeal tube
Pressure controlled ventilation
Pressure supported ventilation
Supplemental oxygen
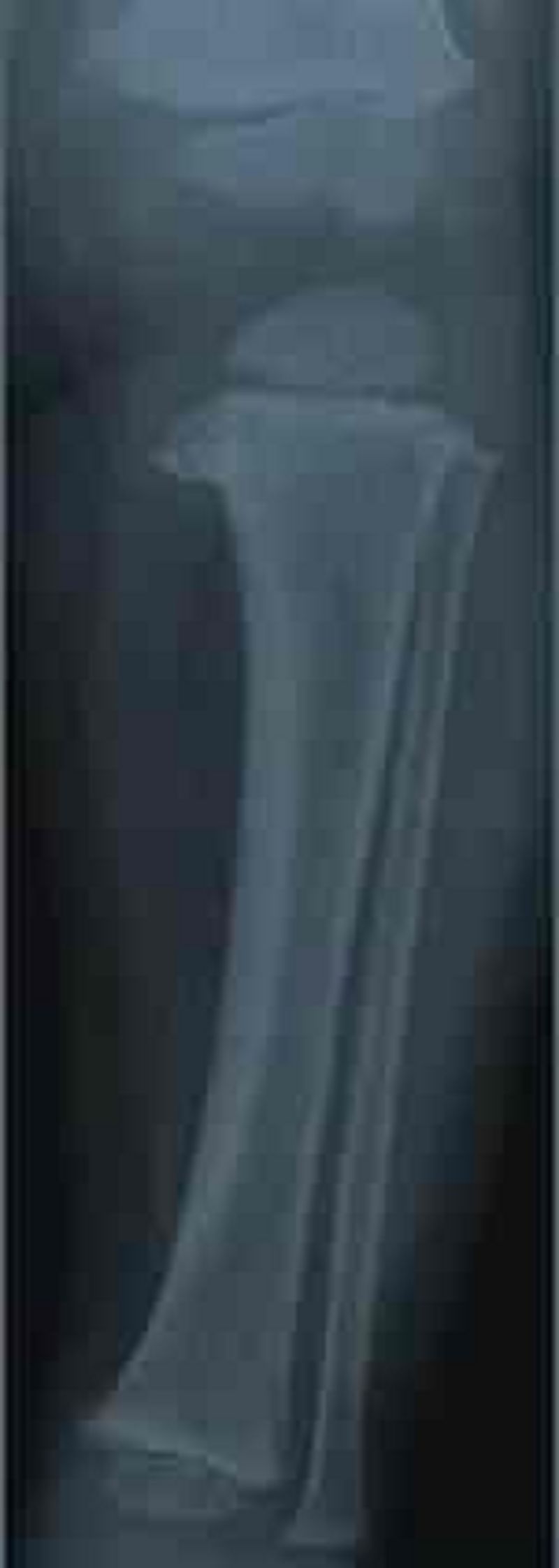
A 2-year-old child presents to the office with a paternal complaint of “bowlegs.” The girl has always had bowlegs; her previous pediatrician told the family she would grow out of it. Now, however, it seems to be worsening. Her weight is greater than 95% for age, and she has significant bowing out of her legs and internal tibial torsion; otherwise, her examination is normal. A radiograph of her lower leg is shown. Which of the following is the most likely diagnosis?
Blount disease
Osgood-Schlatter disease
Physiologic genu varum
Slipped capital femoral epiphysis
Legg-Calvé-Perthes disease
A 14-year-old high school student arrives to your clinic for well-child care. In reviewing his records you determine that his most recent immunization for tetanus was at 4 years of age. Which of the following should you recommend?
Tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine adsorbed (Tdap)
Tetanus toxoid
Adult tetanus and diphtheria toxoid (Td)
Diphtheria toxoid, whole cell pertussis, and tetanus toxoid (DPT) booster
Tetanus toxoid and tetanus immune globulin
A 20-month-old male is brought to ER with high fever, confusion and a skin rash suggestive of measles. He has a history of recurrent respiratory infections over the last 6 months. The patient's family has recently emigrated from a rural Russian province. Which of the following forms of vitamin supplementation should be considered in this patient?
Vitamin A
Vitamin K
Vitamin D
Vitamin E
Vitamin B 12
A 3-year-old male is brought to the emergency department for evaluation of right neck swelling. His parents noticed a lump on his right neck yesterday, which has since increased in size and is now erythematous and tender. He has been previously healthy except for mild upper respiratory tract symptoms last week. His temperature is 38.0 0C (100.4 0F), pulse is 90/min, and respiratory rate is 25/min. On examination, he is nontoxic appearing. A 5-cm anterior cervical lymph node is palpated on the right side. It is poorly mobile, warm, erythematous, and tender to palpation. There is no fluctuance or induration. What is the most likely organism causing these symptoms?
Staphylococcus aureus
Francisella tularensis
Peptostreptococcus
Nontuberculous mycobacteria
Epstein-Barr virus
A 5-year-old boy is brought into the ER immediately after an unfortunate altercation with a neighbor’s immunized Chihuahua that occurred while the child was attempting to dress the dog as a superhero. The fully immunized child has a small, irregular, superficial laceration on his right forearm that has stopped bleeding. His neuromuscular examination is completely normal, and his perfusion is intact. Management should include which of the following?
Copious irrigation
Irrigation and antimicrobial prophylaxis
Tetanus booster immunization and tetanus toxoid in the wound
Primary rabies vaccination for the child
Destruction of the dog and examination of brain tissue for rabies
Aunt Mary is helping her family move to a new apartment. During the confusion, 3-year-old Jimmy is noted to become lethargic. The contents of Aunt Mary’s purse are strewn about on the floor. In the ER, the lethargic Jimmy is found to have miosis, bradycardia, and hypotension. He develops apnea, respiratory depression, and has to be intubated. His condition would most likely benefit from which of the following therapies?
Pediatric intensive care unit (PICU) support and trial of naloxone
Deferoxamine
N-acetylcysteine (Mucomyst)
Atropine
Dimercaptosuccinic acid (DMSA, succimer)
As a city public health officer, you have been charged with the task of screening high-risk children for lead poisoning. Which of the following is the best screen for this purpose?
Blood lead level
Careful physical examination of each infant and child
Erythrocyte protoporphyrin levels (EP, FEP, or ZPP)
CBC and blood smear
Environmental history
An infant is born at terrn to a 27-year-old Caucasian female. The prenatal course was uncomplicated. The amniotic fluid is clear. Immediately after the delivery, the infant starts crying and is moving all four extremities actively. Heart rate is 140/rnin. He is making a grimace on the attempt to put the suction catheter into his nostrils. His body is pink, but extremities are cyanotic. Which of the following is the next best step in the management of the infant?
Dry the infant and keep warm
Intubate the child
Apply silver nitrate solution to the eyes
Administer vitamin K (IM)
Place umbilical catheter
A 25-year-old woman brings her 5-day-old infant to the emergency room after noticing that he bruises very easily. Her pregnancy was normal, and the baby was born at term via vaginal delivery at home. This is the child's first visit to the doctor. He is exclusively breast-fed, and there is no family history of bleeding disorders. On physical examination, his vital signs are within normal limits. You note several ecchymotic skin lesions, but his exam is otherwise normal. Laboratory studies show the following: Prothrombin time 20 sec Partial thromboplastin time 37 sec Platelets 200,000/mm3 Which of the following is the most likely cause of his current condition?
Vitamin K deficiency
Factor VIII deficiency
Impaired synthesis of von Willebrand factor
Excessive destruction of platelets
Consumption of coagulation factors
A 7-year-old girl is brought to the physician because of an exanthematous rash associated with malaise and headache for 2 days. On examination, the child shows a fiery red facial rash with a characteristic "slapped cheek" pattern and pallor around the mouth. There is no fever. In immunocompromised patients, the pathogen that causes this condition may result in which of the following manifestations?
Aplastic anemia
Encephalitis
Non-Hodgkin lymphoma
Progressive multifocal leukoencephalopath (PML)
Symmetric polyarthritis
In the 2nd week of life, a previously healthy newborn develops diarrhea. The stools are watery and voluminous and continue even when the infant is fasting. Which of the following is the most likely pathogen?
Rotavirus
Campylobacter jejuni
Enteroinvasive Escherichia coli
Salmonella species
Shigella species
A 17-year-old girl presents to the office with a 5-day history of a malodorous vaginal discharge. She is sexually active and uses condoms for sexual intercourse. On examination, a thin, white discharge is seen. A "fishy" odor is produced when KOH is added to the discharge. The vaginal fluid has a pH of 5. Which of the following is the most likely finding on a microscopic examination of the vaginal fluid?
Clue cells
Gram-negative diplococci
Lactobacilli
Pseudohyphae
Trichomonads
A 9-month-old child comes in for a routine visit. She has had several episodes of otitis media in the past, but no major illnesses or hospitalizations. Her mother is concerned because the child was previously happy and social around other people, but now cries if her mother is not in the room. The child constantly wants to be held by her mother and becomes upset if her mother walks into the next room. Her grandmother keeps her during the day, and she now cries when her mother leaves her in the morning. Developmentally, she is crawling and waves bye-bye. She does not yet respond to her name or say words. She previously babbled but stopped several months ago. When you hide a toy with your hand, she lifts your hand to look for the toy. Which of the following is the best next step in the management of this child?
Audiology evaluation
Psychological evaluation
Physical therapy evaluation
Social services referral
Reassure the mother that the child's development is normal
A 14-year-old boy is seen in the ER because of a 3-week history of fever between 38.3C and 38.9C (101F and 102F), lethargy, and a 2.7-kg (6-lb) weight loss. Physical examination reveals marked cervical and inguinal adenopathy, enlarged tonsils with exudate, small hemorrhages on the soft palate, a WBC differential that has 50% lymphocytes (10% atypical), and a palpable spleen 2 cm below the left costal margin. Which of the following therapies should be initiated?
Avoidance of contact sports
Initiation of zidovudine
IV acyclovir
IV infusion of immunoglobulins and high-dose aspirin
Intramuscular penicillin
A 2-year-old child is seen in the emergency center with a 10-day complaint of fever and a limp. The child has an elevated erythrocyte sedimentation rate (ESR) and the radiograph shown below. Which of the following statements about this child’s condition is correct?
It can arise following development of deep cellulitis
Itismostcommonlycausedby Streptococcus pyogenes
It usuallyresultsin tendernessin the region of infection that is diffuse, notlocalized
It causes diagnostic radiographic changes on plain films within 48 hours of the beginning of symptoms
It requires antibiotic therapy usually for 10 to 14 days
A 12-year-old boy with cystic fibrosis presents to the emergency department with a 3-day history of severe coughing, which is productive of a yellow-greenish purulent sputum. He had fever and chills at home. He also complains of chest congestion and chest pain that is worse with coughing. On physical examination, his temperature is 39.6 C (103.2 F), blood pressure is 98/68 mm Hg, pulse is 102/min, and respirations are 24/min. He is noted to be lethargic. He has rales on the left lower lung field on auscultation, and chest radiography shows an infiltrate in the left lower lobe. Which of the following is the most appropriate initial antimicrobial therapy for this patient?
Ceftazidime and tobramycin
Amoxicillin-clavulanate and gentamicin
Azithromycin and ceftriaxone
Levofloxacin and metronidazole
Trimethoprim-sulfamethoxazole and vancomycin
A 12-year-old boy is brought to the physician because of pain in his right leg for the past 3 weeks. The pain frequently occurs at night and is localized to the tibia, a few centimeters below the knee. The mother reports that the pain is promptly relieved by aspirin and that the child has had no fever. Examination reveals no tissue swelling or redness about the site of pain. X-ray films show a 1-cm radiolucent focus in the tibial cortex surrounded by marked bone sclerosis. Which of the following is the most likely diagnosis?
Osteoid osteoma
Aneurysmal bone cyst
Enchondroma
Ewing sarcoma
Osteosarcoma
A 16-year-old African American male with sickle cell anemia presents complaining of a 1-week history of exertional dyspnea, fatigue, and generalized weakness. He denies fevers, chills, night sweats, or cough. His only medication is oxycodone for chronic pain. On physical examination, he weighs 68 kg (150 lbs) and is 168cm (66 in) tall His temperature is 36.7 0C (98 0F), blood pressure is 120/70 mm Hg, pulse is 76/min, and respirations are 18/min. All organ systems appear normal Laboratory studies show: Hematocrit 20% Mean corpuscular volume 110 fl Reticulocyte count 1.0% Which of the following is the most likely mechanism underlying these findings?
Increased demand for folic acid
Adverse drug reaction
Gastric mucosal atrophy
Bacterial overgrowth in the small intestine
Increased demand for vitamin B 12
A 15-year-old female with a history of bipolar disorder and psychosis presents to her physician's office requesting a pregnancy test. Her last menstrual period was 2 months ago. She states that her menses usually occur every 30 days. She is sexually active with one partner and occasionally uses condoms. She is concerned because she has gained 10 pounds in the last two months, and also complains of breast tenderness and milky white discharge from both nipples. She denies headaches, nausea, vomiting, diarrhea, or fever. Her vital signs are normal. Physical examination is unremarkable. A urine pregnancy test is negative. Which of the following is most likely responsible for this patient's symptoms?
Risperidone
Valproic acid
Aripiprazole
Lithium
Lamotrigine
A 7-year-old boy is brought to the physician because of recurrent headaches. The child feels nauseated before and during each attack, and derives some relief from lying down in a dark room. Noises, bright light, and fatigue seem to trigger the episodes. The child frequently complains of headaches at school, and his mother has been occasionally compelled to take him home. The mother is worried about the possibility of a serious illness. She reports that the child's father has similar headaches. The child's growth is normal, and a neurologic examination fails to reveal any abnormality. Which of the following is the most likely diagnosis?
Migraine
Brain tumor
Cluster headache
Conduct disorder
Tension headache
A 17 -year-old boy is brought to the emergency department by his father after the boy began threatening him at home. Over the last several months, the father reports, the boy has been increasingly abusive. He was recently involved in a fist fight at school. The boy states that there is nothing wrong. He is otherwise healthy. He denies alcohol use, but does admit to occasional marijuana use. On examination he has acne on his forehead and back and his hairline is receding. There is palpable tissue underneath his nipples bilaterally Heart and lung exams are normal. What substance is this boy most likely abusing?
Anabolic steroids
Cocaine
Heroin
Methamphetamine
Phencyclidine
A 9-month-old infant is brought to the emergency department with lethargy and tachypnea. He was healthy before developing fever and diarrhea four days ago. He has been taking some formula, but has had two to three episodes of diarrhea with each bottle. He has lost three pounds (1 .4 kg) since his routine check-up two weeks ago. He has had one wet diaper in the past twenty four hours. On examination, his temperature is 102.5F (39.1c), pulse is 200/min, respiratory rate is 42/min, and blood pressure is 70/45 mm Hg. He is lethargic with decreased tone and decreased deep tendon reflexes. His mucous membranes are dry. Cardiopulmonary exam reveals tachycardia and tachypnea. His abdominal exam is unremarkable. Capillary refill is four seconds. Laboratory results are shown below. Chemistry panel Serum sodium 165 mEq/L Serum potassium 4.5 mEq/L Chloride 108 mEq/L Bicarbonate 14 mEq/L Blood urea nitrogen (BUN) 20 mg/dl Serum creatinine 0.8 mg/dl Calcium 10.0 mg/dl Blood glucose 98 mg/dl Which of the following fluids should be used as a bolus in the resuscitation of this infant?
0.9% saline
0.45% saline
5% dextrose
5% albumin
Packed red blood cells
A 15-year-old otherwise healthy boy presents with a complaint of intermittent abdominal distention, crampy abdominal pain, and excessive flatulence. He first started noticing these symptoms when he moved into his father’s house, and his stepmother insisted on milk at dinner every night. He has normal growth, has not lost weight, and has no travel history. Which of the following is the most appropriate study to diagnose his condition?
Hydrogen excretion in breath after oral administration of lactose
Barium swallow and upper GI
Esophageal manometry
Stool pH after one to 2 weeks of a lactose-free diet
Fasting serum lactose levels
A 6-week-old infant is admitted to the hospital with jaundice. Her outpatient blood work demonstrated a total bilirubin of 12 mg/dL with a direct portion of 3.5 mg/dL. Which of the following disorders is most likely to be responsible?
Choledochal cyst
ABO incompatibility
Rh incompatibility
Gilbert disease
Crigler-Najjar syndrome
A 12-year boy is brought to the emergency room by his parents after a several day history of progressive weakness. He has been a healthy child who has met all development milestones and all his immunizations are up to date. He reports that he had an upper respiratory infection 2 weeks ago. On physical examination, his vital signs are labile with a pulse range of 60-100/ min and systolic blood pressure ranging from 80-120 mm Hg. He is alert and oriented. Neurologic examination is impressive for bilateral weakness in the upper and lower extremities. Deep tendon reflexes are absent and sensation is intact. Which of the following is the most likely diagnosis?
Guillain-Barré syndrome
Myasthenia gravis
Polymyositis
Transverse myelitis
Viral encephalitis
A 15-year-old boy with tall stature presents with decreased exercise tolerance over the past 2 months. He states that he used to play two games of basketball with no problem, but he now can play only one game. On physical examination, his weight is at the 25th percentile, and his height higher than the 95th percentile. He is thin and has a gangly body habitus. His fingers are long and thin. There is pectus deformity in his chest. His joints are hyperextensible. An ophthalmologic examination reveals mild subluxation of the lens. Which of the following is the most likely finding on an echocardiogram?
Aortic root dilatation
Aortic stenosis
Bicuspid aortic valve
Dextrocardia
Pulmonary stenosis
A 2-year-old arrives in the emergency center after having swallowed a button battery from one of her toys. She is breathing comfortably, without stridor. Radiographs show the battery to be lodged in the esophagus. Which of the following is the correct next step?
Immediate removal of the battery via endoscopy
Induce emesis with syrup of ipecac
Admit for observation, and obtain serial radiographs to document movement of the battery
Discharge home with instructions to monitor the stool for the battery
Encourage oral intake to assist in passage of the battery
A 2-year-old boy is brought to the office due to recurrent skin and soft tissue infections. When he was 2- months-old, he had a perianal furuncle that was incised and drained because it was unresponsive to oral antibiotics. At 7 months of age, he had a left inguinal Klebsiella pneumoniae lymphadenitis. His other past infections include a left calf cellulitis that grew Serratia marcescens and a left inguinal abscess that grew Staphylococcus epidermidis. On examination, he has hepatosplenomegaly, and enlarged axillary and inguinal lymph nodes. The screening tests for humoral, cell-mediated, and complement-mediated immunity are normal. The nitroblue tetra zolium (NBT) slide test is abnormal. What is the most likely diagnosis?
Chronic granulomatous disease (CGD)
Wiskott-Aidrich syndrome (WAS)
Chediak-Higashi syndrome
Leukocyte adhesion defect I
Hyper-lgE (Job's) syndrome
A previously healthy 2-year-old male is brought to the emergency department after experiencing a seizure-like episode. His parents report that he has been healthy with the exception of mild upper respiratory symptoms for the past 24 hours. During the episode, his parents state that he fell down and had rhythmic, jerking movements of his arms and legs. The episode lasted about three minutes. The patient was sleepy when the emergency personnel arrived. Vital signs are temperature 39 .2 c (102 .5 F), pulse 120/min, and respiratory rate 25/min. The patient is alert and oriented in the emergency department. On examination, there is mild rhinorrhea and the left tympanic membrane is erythematous, bulging, and poorly mobile. The neck is supple. A complete neurological exam is unremarkable. After treating this patient's fever, which of the following is the next best step in the management of this patient?
Discharge home with education
Electroencephalogram
Magnetic resonance imaging of the brain
Lumbar puncture
Admit for further observation
An awake, alert infant with a 2-day history of diarrhea presents with a depressed fontanelle, tachycardia, sunken eyes, and the loss of skin elasticity. Which of the following is the correct percentage of dehydration?
5% to 9%
Less than 1%
1% to 5%
10% to 15%
More than 20%
A newborn infant is brought to the nursery for evaluation after delivery. The mother reports that the pregnancy was uncomplicated, but she had only two prenatal visits. The infant was born via normal spontaneous vaginal delivery and required no resuscitation. The infant has hepatosplenomegaly on examination. While in the hospital, the infant requires treatment for anemia and hyperbilirubinemia. On subsequent examinations, the infant has clear rhinorrhea and ulcerative lesions on his feet. Which of the following congenital infections is most likely in this patient?
Syphilis
Toxoplasmosis
Rubella
Human immunodeficiency virus infection
Cytomegalovirus infection
A 2 week post mature baby is born and immediately exhibits severe respiratory distress. Previously, green-tinged meconium was noted in the amniotic fluid. Which of the following is the most appropriate next step?
Suction the mouth and nasopharynx
Chest x-ray film
Intubation with mechanical ventilation
Oxygen supplementation by face mask
Emergency tracheostomy
A fetus is delivered at 40 weeks' gestation. During labor, the fetal heart monitor shows late decelerations and loss of short- and long-term variability. The membranes are ruptured to expedite the delivery. The fluid is noted to contain meconium. The infant is delivered 45 minutes later. At delivery, the infant appears to be cyanotic and limp. He has poor tone and deep reflexes. Moro's reflex is absent. Ten hours later, he experiences a seizure. Which of the following best explains this infant's perinatal course?
Encephalopathy from asphyxia
Inborn error of metabolism
Respiratory distress
Subarachnoid hemorrhage
Werdnig-Hoffman disease
An 18-month-old infant is found with the contents of a bottle of drain cleaner in his mouth. Which of the following treatment options is most appropriate?
Endoscopic examination within the first 12 to 24 hours
Immediate emesis
Decontamination by activated charcoal
Neutralization by drinking a solution of the opposite pH
Have the patient drink copious amounts of milk or water
A 16-year-old male, despondent over a recent breakup, tries to commit suicide by taking an unknown quantity of an unknown material he found at home. He is brought to the emergency center by his parents within 30 minutes of the ingestion. For which of the following household materials and medications should he be given activated charcoal as part of his emergency center treatment?
Phenobarbital
Drain cleaner
Ethylene glycol
Bleach
Lithium
A 3-year-old African American boy is brought to the emergency department with sudden onset of difficulty walking. His mother reports that his right hand also seems "clumsy." The boy's past medical history is significant for a hospitalization one year ago for severe upper extremity pain and hand swelling. On physical examination, he has a blood pressure of 90/60 mmHg, heart rate of 120/min, temperature of 36.7°C (98°F), and respiratory rate of 22/min. Which of the following would be most helpful in diagnosing his condition?
CBC and reticulocyte count
Carotid ultrasonography
Antineutrophil cytoplasmic antibodies
Temporal artery biopsy
Lumbar puncture
A 25-year-old woman comes to your office for counseling. She says that her husband has cystic fibrosis, and that she has no family history of this disease. They are planning to have a child. She wonders what the probability is for their baby to have cystic fibrosis. Which of the following is your best response in this situation?
The probability cannot be determined because her carrier status is unknown
Cystic fibrosis is an autosomal dominant disease, so the child will have the disease
Cystic fibrosis is an autosomal recessive disease, so the child has 25% probability of getting the disease
Cystic fibrosis is an autosomal recessive disease, so the child has 50% probability of getting the disease
The probability cannot be determined because cystic fibrosis does not follow Mendelian transmission
A 7-year-old boy is brought to the physician because of persistent nasal obstruction for 6 months. There is no: personal or family history of allergic disorders, Examination of the nasal fossae reveals bilateral ethmoidal polyps that protrude into the middle meatus and nasal cavity. Which of the following is the most appropriate next step in diagnosis?
Pilocarpine iontophoresis sweat test
Cutaneous allergen testing
Excisional biopsy
Nasal provocation testing
Radioallergosorbent test (RAST)
A neonate is very small for gestational age, shows hypotonia, marked skeletal muscle, and subcutaneous fat hypoplasia. During delivery, a large volume of amniotic fluid was released at rupture of membranes. The placenta was small, and only a single umbilical artery was noted. The face has a pinched appearance with hypoplastic orbital ridges, short palpebral fissures, and a small mouth and jaw. The head is small with prominence of the occiput. The ears are low set and malformed. The infant's fists are clenched, with overlapping of the third and fourth fingers. The feet are clubbed, and the great toe is shortened. Which of the following is most likely diagnosis?
Trisomy 18
47,XXY
TripleX
Trisomy 13
Trisomy 21

The delivery of a newborn boy is remarkable for oligohydramnios. The infant (pictured) is also noted to have undescended testes and clubfeet, and to be in respiratory distress. Which of the following is the most likely diagnosis to explain these findings?
Prune belly syndrome
Surfactant deficiency
Turner syndrome
Hermaphroditism
Congenital adrenal hyperplasia
A 17-year-old boy is brought to the emergency department by his parents with the complaint of coughing up blood. He is stabilized, and his hemoglobin and hematocrit levels are 11 mg/dL and 33%, respectively. During his hospitalization, he is noted to have systolic blood pressure persistently greater than 130 mm Hg and diastolic blood pressure greater than 90 mm Hg. His urinalysis is remarkable for hematuria and proteinuria. You are suspicious the patient has which of the following?
Goodpasture syndrome
Hemolytic-uremic syndrome
Nephrotic syndrome
Poststreptococcal glomerulonephritis
Renal vein thrombosis
A 10-year-old presents with 2months history of heavy menstrual-like bleeding. Menarche occurred 6 months ago and this first menses consisted of spotting for 3-4 days without cramps. Subsequent periods were light in flow but lasted 6 to 8 days. Which of the following is the most likely cause of her bleeding?
Dysfunctional uterine bleeding
Von Willebrand disease
Ovarian tumor
Thyroid disease
Pregnancy
A 4-year-old boy presents with 5-day history of fever and increased irritability. His temperature is 40. 2 C (104. 3 F), blood pressure is 98/68 mm Hg, pulse is 112/min, and respirations are 24/min. On physical examination, he is noted to have bilateral cervical lymphadenopathy, cracked lips, strawberry tongue, and bilateral conjunctival injection. His palms and soles are erythematous. There is a polymorphous macular rash generalized on his body. Which of the following is the most appropriate pharmacotherapy?
Aspirin and IV immune globulin
Amoxicillin
Aspirin and corticosteroid
Corticosteroid
IV immune globulin

A 13-year-old male is brought to the physician for evaluation of intermittent left knee pain that arose three months ago. He does not remember any trauma to his knee. The pain worsens after basketball games, but improves some with rest. He has been taking non-steroidal anti-inflammatory medications with some relief. On physical examination, he has edema and tenderness over the proximal tibia at the site of the patellar tendon insertion. Examination of the knee joint is normal and no effusion is present. His knee pain is reproducible by extending the knee against resistance. A lateral radiograph of his knee is shown below. Which of the following is the most likely cause of this patient's knee pain?
Traction apophysitis
Prepatellar bursitis
Patellar tendonitis
Tibial osteomyelitis
Patellofemoral stress syndrome
A 4-day-old infant is brought to the physician for an outpatient follow-up visit. The mother's pregnancy and delivery were uncomplicated. The infant weighed 3.4kg (7 .5 lb) and was 19 in (48.2 cm) long at birth. He did well in the newborn nursery and was discharged from the hospital on day 2 of life. Today his mother reports that he is exclusively breastfed, and nurses for 10 minutes every 3 hours. He has 3-4 wet diapers a day, and has not had a bowel movement for two days. On examination, he weighs 2.95 kg (6.5 lb) and is 19 in (48.2 cm) long. He appears jaundiced on the face and chest. The remainder of the physical examination is unremarkable. Laboratory values are shown below. Total bilirubin 15 mg/dl Direct bilirubin 1 mg/dl Infant's blood type O positive Mother's blood type A positive Which of the following is the most likely cause of this infant's hyperbilirubinemia?
Breastfeeding jaundice
Biliary atresia
Breast milk jaundice
Galactosemia
ABO incompatibility
A 16-year-old boy with a history of ulcerative colitis presents to the physician complaining of diarrhea and a rash. He states that his appetite has been decreased recently, and also complains of nausea and abdominal pain in addition to watery diarrhea. He has an erythematous rash on his distal arms and legs that "burns". His mother reports that he has had poor concentration and has been irritable lately. Vital signs are stable. Examination reveals a beefy red tongue that appears swollen. Abdominal examination is normal. The rash resembles a sunburn and is located on his distal arms and legs. It is symmetrical and tender to palpation. Neurological examination is normal. This patient's symptoms are most likely due to a deficiency of which of the following vitamins?
Niacin
Thiamine
Riboflavin
Pyridoxine
Cyanocobalamin
You are called by a general practitioner to consult on a patient admit- ted to the hospital 4 days ago. The patient is a 7-month-old white boy with poor weight gain for the past 3 months, who has not gained weight in the hospital despite seemingly adequate nutrition. You take a detailed diet his- tory from his foster mother, and the amounts of formula and baby food intake seem appropriate for age. Physical examination reveals an active, alert infant with a strong suck reflex who appears wasted. You note generalized lymphadenopathy with hepatomegaly. In addition, you find a severe case of oral candidiasis that apparently has been resistant to treatment. Which of the following is the most appropriate next step in the evaluation or treatment of this child?
Order human immunodeficiency virus (HIV) polymerase chain reaction (PCR). Testing because this is likely the presentation of congenitally acquired HIV
Increase caloric intake because this is probably a case of underfeeding
Draw blood cultures because this could be sepsis
Perform a sweat chloride test because this is probably cystic fibrosis
Send stool for fecal fat because this is probably a malabsorption syndrome

A 5-year-old boy presents with the severe rash shown in the photographs. The rash is pruritic, and it is especially intense in the flexural areas. The mother reports that the symptoms began in infancy (when it also involved the face) and that her 6-month-old child has similar symptoms. Which of the following is the most appropriate treatment of this condition?
Moisturizers and topical steroids
Coal-tar soaps and shampoo
Topical antifungal cream
Ultraviolet light therapy
Topical antibiotics
A 13-year-old girl returns to her physician for followup of a strep throat, for which she had been treated 3 weeks previously. After performing a throat culture, the physician asks how school is going. There is dead silence. Her mother says that her daughter has missed the last 4 weeks of school. Which of the following is the most appropriate initial step in management?
Contract with the girl to go back to school as you explore the problem
Write a medical excuse for her until the throat culture results come back
Tell them you must report her to the school authorities for truancy
Send the mother for supportive counseling
Send the girl for psychotherapy
A 1 -year old child is brought in for a well baby check-up. His parents report that he has been of good health and began walking a few weeks earlier. They are concerned that he tends to bump into things and falls more than his older sister did. Family history is significant for retinoblastoma. On examination, the pediatrician notes leukocoria of the left eye. No significant lymphadenopathy is present, and there is no enlargement of the liver or spleen. The child's height and weight are normal for age. Which of the following is the most appropriate next step in management?
Refer to ophthalmologist
Explain to parents what leukocoria is and reassure them that it is temporary
Return visit in 1 month
Refer to neurologist
Treat the eye with erythromycin ophthalmic ointment for 10 days
A 4-year-old boy is being evaluated for short stature. He has a history of multiple bone fractures in the past. He requires a wheelchair to ambulate and has hearing difficulty. On physical examination, his height is below the 5th percentile. His sclerae are blue in color. There is marked deformity of his lower extremities. Which of the following is the most likely diagnosis?
Osteogenesis imperfecta
Achondroplasia
Constitutional delay of growth
Developmental dysplasia of the hip
Familial short stature
{"name":"999 Questions Pediatrie-MCQ-(301-600) Part 2 NR", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 4-week-old boy is brought to clinic by his mother because of a 1day history of labored breathing. His birth was uneventful and immunizations have been up to date. His mother reports that the patient developed conjunctivitis on the fourth day of life. On physical examination, he is breathing rapidly at 40 breaths per minute and is afebrile. His chest reveals bilateral inspiratory crackles and a slight wheeze. On chest x-ray, bilateral pneumonia is evident. The leukocyte count is elevated at 15,000 with 40% eosinophils. Which of the following is the most likely pathogen causing the patient's symptoms?, A 15-year-old girl with type 1 diabetes mellitus presents to her primary care doctor for a routine check up. Perusal of her blood sugar chart indicates that her recorded blood glucose levels are routinely between 120 and 150 mg\/dL before breakfast, dinner and bedtime, with the normal being 116 mg\/dL. She is on NPH and regular insulin. Which of the following is the next appropriate step?, A previously healthy 4-year-old boy is brought to the physician for evaluation of fever and respiratory distress. The patient developed fever three days ago. Since then, he has had increasing fatigue, irritability, and respiratory distress. His temperature is 100 0F (38.2 0C), pulse is 144\/min, respiratory rate is 45\/min, and blood pressure is 95\/60 mm Hg. On examination, the child appears to be in moderate respiratory distress with tachypnea and subcostal retractions. He is tachycardic with an III\/IV holosystolic murmur best heard at the cardiac apex. Peripheral pulses are present and capillary refill is three seconds. His liver is palpated three centimeters below the costal margin. A chest radiograph is shown below. Which of the following is the most likely cause of this patient's symptoms?","img":"https://cdn.poll-maker.com/10-462909/1.jpg?sz=1200"}
More Quizzes
���ეოგრაფია-საქართველო-წიაღისეულები
1680
Reading
630
Garrotxa 2021
7419
Check that box
10525
Free Radio Listener Trivia
201023630
Topics in Anthropology
15827267
Free RNA: Practice Questions
201024846
Free Video Annotation Training
201025064
Which Super Smash Bros Character Are You? Take the
201031466
Free Medical Spanish Proficiency
201025515
Alberta Facts: Interesting & Cool Facts About Alberta
201024018
Free Basic Scored Knowledge
201021597