DES C_Management (7) Prepared : CHILLY
A 38-year-old woman, gravida 4, para 4, comes to the physician 8 days after a cesarean delivery complaining of redness and pain at the leftmost aspect of her incision. Her cesarean delivery was performed secondary to a non reassuring fetal heart rate tracing. She was feeling well after the operation until 4 days ago, when she developed pain and redness around her incision. Her temperature is 37 C (98.6 F), blood pressure is 118/78 mm Hg, pulse is 88/min, and respirations are 12/min. There is marked erythema and induration around the incision. At the left margin of the incision there is a fluctuant mass. Which of the following is most appropriate next step in management?
Oral antibiotics only
Incision and drainage
Laparotomy
IV antibiotics only
Expectant management
A 39-year-old G3P3 comes to see you on day 5 after a second repeat cesarean delivery. She is concerned because her incision has become very red and tender and pus started draining from a small opening in the incision this morning. She has been experiencing general malaise and reports a fever of 38.8C (102F). Physical examination indicates that the Pfannenstiel incision is indeed erythematous and is open about 1 cm at the left corner, and is draining a small amount of purulent liquid. There is tenderness along the wound edges. Which of the following is the best next step in the management of this patient?
Reapproximate the wound edge under local analgesia
Take the patient to the OR for debridement and closure of the skin
Apply Steri-Strips to close the wound
Probe the fascia
Administer antifungal medication
A 39-year-old Japanese-American woman with insulin-dependent diabetes and asthma presents to her primary care physician complaining of trouble swallowing for the past few months. She explains that it started with solids, and then progressed to liquids. She states it now is hard even to swallow water and that she is often very thirsty. She says she has lost about 3.2 kg (7 lb), but says she is working out frequently. Her blood pressure is 118/76 mm Hg, pulse is 86/min, respiratory rate is 16/min, and temperature is 37.2°C (98.9°F). Laboratory tests show: Na+: 144 mEq/L, K+: 4.0 mEq/L, Cl−: 100 mEq/L, Carbon dioxide: 22 mmol/L Blood urea nitrogen: 18 mg/dL Creatinine: 1.0 mg/dL, Glucose: 88 mg/dL. Her hemoglobin A1c level, measured 3 months earlier, was 6.1%. A barium swallow is performed, which reveals a dilated esophagus, especially distally, that flares out near the lower esophageal junction. Still not completely sure of the diagnosis, esophageal manometry is performed, which reveals abnormal peristalsis and increased lower sphincter pressure. Which of the following is the most appropriate management?
Pneumatic dilation
Surgery to remove diverticula
Instructions to elevate the bed, avoid fatty foods, and consider a histamine blocker
Cholinergic agents
Glucose pharmacotherapy
A 39-year-old man is undergoing resuscitation with blood products for an upper GI bleed. He is suspected of having a hemolytic transfusion reaction. Which of the following is appropriate in the management of this patient?
Fluid restriction
Steroids
Fluids and mannitol
0.1 M HCl infusion
Removal of nonessential foreign body irritants, for example, Foley catheter
A 39-year-old man presents with an isolated fracture of the tibia after being hit on the leg with a car. The patient is stable and a radiograph of the leg shows a tibial shaft fracture with severe dislocation. Which of the following is the most appropriate management of the fracture?
Surgical fixation with unreamed nailing
Closed reduction and application of a long leg cast
Intramedullary nailing
External fixation
Plate fixation
A 39-year-old nulligravid woman comes to the physician because of a persistent vaginal itch, vaginal discharge, and dysuria. She has had these same symptoms several times over the past 2 years and each time has been diagnosed with Candida vulvovaginitis. On physical examination, she has a thick, white vaginal discharge and significant vulvar and vaginal erythema. A potassium hydroxide (KOH) smear shows pseudohyphae; the normal saline smear is negative. Which of the following is the most appropriate next step in management?
Refer to psychiatry Screen for cocaine abuse Screen for diabetes Screen for thalassemia Treat with metronidazole
Screen for cocaine abuse
Treat with metronidazole
Screen for thalassemia
Screen for diabetes
Refer to psychiatry
A 39-year-old previously healthy male is hospitalized for 2 weeks with epigastric pain radiating to his back, nausea, and vomiting. Initial laboratory values revealed an elevated amylase level consistent with acute pancreatitis. Five weeks following discharge, he complains of early satiety, epigastric pain, and fevers. On presentation, his temperature is 38.9°C (102°F) and his heart rate is 120 beats per minute; his white blood cell (WBC) count is 24,000/mm3 and his amylase level is normal. He undergoes a CT scan demonstrating a 6 cm by 6 cm rim-enhancing fluid collection in the body of the pancreas. Which of the following would be the most definitive management of the fluid collection?
Surgical internal drainage of the fluid collection with a cyst-gastrostomy or Roux-en-Y cyst-jejunostomy
Antibiotics and percutaneous catheter drainage
Antibiotics and CT-guided aspiration with repeat imaging in 2 to 3 days
CT-guided aspiration with repeat imaging in 2 to 3 days
Antibiotic therapy alone
A 39-year-old woman completed her last course of postoperative adjuvant chemotherapy for breast cancer 6 months ago. She now comes to the clinic complaining of constant back pain for about 3 weeks. She is tender to palpation over two well-circumscribed areas in the thoracic and lumbar spine. Which of the following is the most appropriate next step in management?
X-ray films of the affected areas
Needle biopsy of the tender spots
Sonogram of the affected areas
CT scan of the trunk
Radionuclide bone scan
A 39-year-old woman is admitted to the gynecology service for hysterectomy for symptomatic uterine fibroids. Postoperatively the patient develops an ileus accompanied by severe nausea and vomiting; ondansetron is piggybacked into an IV of D5 ½ normal saline running at 125 cc/h. On the second postoperative day the patient becomes drowsy and displays a few myoclonic jerks. Stat labs reveal Na 118, K 3.2, Cl 88, HCO3 22, BUN 3, and creatinine 0.9. Urine studies for Na and osmolality are sent to the lab. What is the most appropriate next step?
Change the ondansetron to promethazine, change the IV fluid to lactated Ringer solution, and recheck the Na in 4 hours
Make the patient NPO and send for stat CT scan of the head to look for cerebral edema
Change the IV fluid to normal saline and give furosemide 40 mg IV stat
Start 3% (hypertonic) saline, make the patient NPO, and transfer to the ICU
Change the IV fluid to 0.9% (normal) saline and restrict free-water intake to 600 cc/d
A 39-year-old woman is involved in a head-on, highspeed automobile collision. She arrives at the emergency department in a deep coma, with bilaterally fixed dilated pupils. She has normal blood pressure and pulse rate. CT scan of the head shows diffuse blurring of the gray-white interface and multiple small punctate hemorrhages. There is no single large hematoma or displacement of the midline structures. Extension of the CT to include the neck shows no cervical spine fractures. Which of the following is the most appropriate initial step in management?
Surgical evacuation of the multiple punctate hemorrhages
Prevention of further damage due to development of increased intracranial pressure
Preservation of neurologic function by the use of hyperbaric oxygen
Improvement of cerebral perfusion by the use of systemic vasodilators
Improvement of cerebral perfusion by infusion of large amounts of TV fluids
A 39-year-old woman known to have fibrocystic disease of the breast complains of persistent fullness and pain in both breasts. Which of the following drugs will be most effective in relieving her symptoms?
Tamoxifen
Danazol
Hydrochlorothiazide
Medroxyprogesterone acetate
Bromocriptine
A 39-year-old woman presents to the physician’s office for evaluation of a palpable nodule in the neck of 2 years’ duration. Her past history is pertinent for Hashimoto’s disease diagnosed 5 years ago, for which she takes thyroid hormone. She has a history of low-dose chest irradiation for an enlarged thymus gland during infancy. On examination, a 2.5-cm nodule is palpable in the left lobe of the thyroid and is firm and non-tender. Which of the following is the most appropriate next step in her management?
Thyroid scinti-scan
FNA of the nodule
CT scan of the neck and chest
MRI of the neck
Ultrasound of the neck
A 39-year-old woman with a known history of von Willebrand disease has a ventral hernia after a previous cesarean section and desires to undergo elective repair. Which of the following should be administered preoperatively?
Low-molecular-weight dextran
Cryoprecipitate
Whole blood
Fresh-frozen plasma (FFP)
High-purity factor VIII: C concentrates
A 39-year-old woman with no significant past medical history and whose only medication is oral contraceptive pills (OCP) presents to the emergency room with right upper quadrant pain. CT scan demonstrates a 6-cm hepatic adenoma in the right lobe of the liver. Which of the following describes the definitive treatment of this lesion?
Embolization of the right portal vein
Intra-arterial embolization of the hepatic adenoma
Systemic chemotherapy
Resection of the hepatic adenoma
Cessation of oral contraceptives and serial CT scans
A 39-year-old woman, gravida 3, para 2 at 34 weeks' gestation, with a known history of chronic hypertension, is found to have a blood pressure of 180/115 mm Hg at a routine prenatal visit. Her prenatal course had been otherwise unremarkable. She is transferred to the labor and delivery ward for further management. IV antihypertensive medications should be given to this patient with a goal of which of the following blood pressures?
90/60 mm Hg
150/95 mm Hg
180/110 mm Hg
100/75 mm Hg
120/80 mm Hg
A 39-year-old woman, gravida 3, para 2, at 39 weeks’ gestation comes to the labor and delivery ward with regular contractions and gush of fluid 1 hour ago. On examination she is found to have rupture of membranes and is 4 cm dilated. She is admitted to labor and delivery. Her prenatal course was significant for a 36-week vaginal culture that was positive for Group B Streptococcus (GBS) that is sensitive to clindamycin. She also has gestational diabetes that is treated with diet. She has no other medical problems and has never had surgery. She takes no medications and is allergic to penicillin. After she is admitted to the labor and delivery ward, a penicillin infusion is erroneously started. Soon thereafter, the patient develops generalized pruritus and urticaria with angioedema and difficulty breathing. Which of the following is the most appropriate next step in the management of this patient?
Administer epinephrine
Stop the penicillin infusion
Intubate the patient
Administer magnesium sulfate
Administer diphenhydramine
A 39-year-old woman, gravida 3, para 2, at 40 weeks' gestation comes to the labor and delivery ward after a gush of fluid with regular, painful contractions every two minutes. She is found to have rupture of the membranes and to have a cervix that is 5 centimeters dilated, a fetus in vertex presentation, and a reassuring fetal heart rate tracing. She is admitted to the labor and delivery ward. Two hours later she states that she feels hot and sweaty. Temperature is 38.3 C (101 F). She has mild uterine tenderness. Her cervix is now 8 centimeters dilated and the fetal heart tracing is reassuring. Which of the following is the most appropriate management of this patient?
Perform intra-amniotic injection of antibiotics
Perform cesarean delivery and then administer antibiotics to the mother
Administer antibiotics to the mother now and allow vaginal delivery
Perform cesarean delivery
Administer antibiotics to the mother after vaginal delivery
A 39-year-old woman, gravida 3, para 2, at term comes to the labor and delivery ward complaining of a gush of fluid. Examination shows her to be grossly ruptured, and ultrasound reveals that the fetus is in vertex presentation. The fetal heart rate is in the 120s and reactive. After a few hours, with no contractions present, oxytocin is started. Three hours later, the tocodynamometer shows the patient to be having contractions every minute and lasting for approximately 1 minute with almost no rest in between contractions. The fetal heart rate changes from 120s and reactive to a bradycardia to the 80s. Sterile vaginal examination shows that the cervix is 6 cm dilated. Which of the following is the most appropriate next step in management?
Perform vacuum assisted vaginal delivery
Perform cesarean delivery
Perform forceps assisted vaginal delivery
Discontinue oxytocin
Start magnesium sulfate
A 39-year-old woman, gravida 4, para 3, comes to the physician for a prenatal visit. Her last menstrual period was 8 weeks ago. She has had no abdominal pain or vaginal bleeding. She has no medical problems. Examination is unremarkable except for an 8-week sized, nontender uterus. Prenatal labs are sent. The rapid plasma reagin (RPR) test comes back as positive and a confirmatory microhemagglutination assay for antibodies to Treponema pallidum (MHA-TP) test also comes back as positive. Which of the following is the most appropriate pharmacotherapy?
Erythromycin
Metronidazole
Penicillin
Tetracycline
Levofloxacin
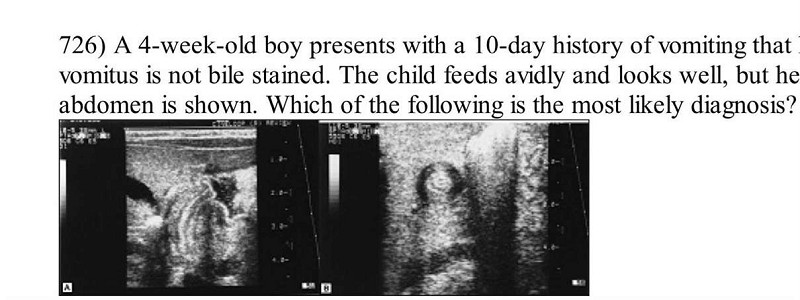
A 4-week-old boy presents with a 10-day history of vomiting that has increased in frequency and forcefulness. The vomitus is not bile stained. The child feeds avidly and looks well, but he has been losing weight. An ultrasound of the abdomen is shown. Which of the following is the most likely diagnosis?
Computed tomography (CT) of the brain
Intravenous (IV) fluids alone to maintain hydration
Air contrast enema
Upper GI with small-bowel follow through
Surgical consultation for pyloromyotomy
A 4-week-old infant presents with tachycardia, tachypnea, and poor weight gain. His arterial blood gas shows a pH of 7.34, a PaCO2 of 41 mm Hg, and a PaO2 of 74 mm Hg. A chest radiograph shows cardiomegaly. Echocardiography reveals a structurally normal heart, left ventricular dilatation, a left ventricular ejection fraction of 20%, and mild mitral and tricuspid regurgitation. IV administration of which of the following medications is the best initial step in management of this patient?
Digoxin
Angiotensin-converting enzyme inhibitor
Corticosteroid
Epinephrine
Furosemide
A 4-week-old male infant has been spitting up his formula feedings for the past few days. He does not vomit bilious material or blood. The spitting up is gradually becoming more frequent, and forceful vomiting ensues. The vomitus seems to shoot straight out and nearly hit the wall. On examination, the baby seems hungry and is chewing his fist. His mucous membranes appear dry. A small, round mass, about the size of an adult thumbnail, is palpated in the upper abdomen. Laboratory data reveal Na+ of 133 mEq/L, K+ of 3.5 mEq/L, CI of 93 mEq/L, and HC0 3 - of 29 mEq/L. Which of the following is the most appropriate next step in management?
Insert a nasogastric tube
Begin parenteral antibiotics
Obtain flat plate and upright x-ray films of the abdomen
Obtain a surgical consult immediately
Change the feedings to clear liquids or Pedialyte
A 4-year-old boy is brought to the emergency department for a painful and swollen right forearm. He was bitten and scratched by a family cat 2 days ago in the affected area. His temperature is 39.6 C (103.2 F). The right forearm is erythematous, edematous, and tender to touch. Which of the following is the most appropriate antibiotic treatment for this patient?
Ampicillin
Trimethoprim-sulfamethoxazole
Clindamycin
Tetracycline
Amoxicillin-clavulanate
A 4-year-old boy presents with 5-day history of fever and increased irritability. His temperature is 40.2 C (104.3 F), blood pressure is 98/68 mm Hg, pulse is 112/min, and respirations are 24/min. On physical examination, he is noted to have bilateral cervical lymphadenopathy, cracked lips, strawberry tongue, and bilateral conjunctival injection. His palms and soles are erythematous. There is a polymorphous macular rash generalized on his body. Which of the following is the most appropriate pharmacotherapy?
Aspirin and corticosteroid
IV immune globulin
Corticosteroid
Aspirin and IV immune globulin
Amoxicillin

A 4-year-old boy presents with a history of constipation since the age of 6 months. His stools, produced every 3 to 4 days, are described as large and hard. Physical examination is normal; rectal examination reveals a large ampulla, poor sphincter tone but present anal wink, and stool in the rectal vault. The plain film of his abdomen is shown. Which of the following is the most appropriate next step in the management of this child?
Upper GI barium study
Parental reassurance and dietary counselling
Serum electrolyte measurement
Initiation of thyroid-replacement hormone
Lower gastrointestinal (GI) barium study
A 4-year-old child with grade III vesicoureteral reflux has recurrent UTIs despite adequate antibiotic prophylaxis. Which of the following is the most appropriate next step in the treatment of this patient?
Antireflux surgery
IV antibiotic treatment for 2 weeks
Addition of vitamin C (ascorbic acid) to the treatment regimen
Repeat renal scan
Renal arteriogram
A 4-year-old female is brought to the emergency department for evaluation of vaginal discharge. She has had foul-smelling vaginal discharge for 1 week. Her mother has also noted a small amount of vaginal bleeding. The mother called her primary physician and was told to use an over-the-counter cream and to stop letting the child take bubble baths. However, the symptoms have not improved. The child complains of pruritus in her vaginal area. She was potty trained at age 2. While mother is at work, the baby is with her stepfather. On examination, the perineal area is erythematous with a purulent, foul-smelling vaginal discharge. Visual inspection of the vagina reveals a greenish foreign body inside the vagina. Which of the following is the next best step?
Notify Child Protective Services immediately
CT scan of the pelvis
Bimanual examination under general anesthesia
Cultures for gonorrhea and chlamydia
Irrigation with warmed fluid
A 4-year-old female is brought to the emergency department for evaluation of vaginal discharge. She has had foul-smelling vaginal discharge for 1 week. Her mother has also noted a small amount of vaginal bleeding. The mother called her primary physician and was told to use an over-the-counter cream and to stop letting the child take bubble baths. However, the symptoms have not improved. The child complains of pruritis in her vaginal area. She was potty trained at age 2. While mother is at work, the baby is with her stepfather. On examination, the perineal area is erythematous with a purulent, foul-smelling vaginal discharge. Visual inspection of the vagina reveals a greenish foreign body inside the vagina. Which of the following is the next best step?
Notify Child Protective Services immediately
CT scan of the pelvis
Cultures for gonorrhea and chlamydia
Bimanual examination under general anesthesia
Irrigation with warmed fluid
A 4-year-old girl is brought to the physician by her mother because of a bloody, greenish, malodorous vaginal discharge. The discharge was first noted 3 days ago and has worsened since then. The girl has no other symptoms. The mother reports no concerns regarding abuse of the child. Examination is attempted but impossible because of the child's absolute refusal to be examined. Several efforts at persuasion are made but are unsuccessful. Which of the following is the most appropriate next step in management?
Pelvic examination with physical restraint
Antibiotic administration
Examination under anesthesia
Police notification
Reassurance and expectant management
A 4-year-old girl presents to the emergency department with fever and a petechial rash. A sepsis workup is performed, and IV antibiotics are administered. Gram-negative diplococci are identified in the CSF. Which of the following is true of this condition?
Vancomycin administered intravenously is the treatment of choice
The presence of meningitis decreases the survival rate
Shock is the usual cause of death
The most common neurologic residual is seizures
Antibiotic prophylaxis of fellow daycare attendees is not necessary
A 4-year-old girl with sickle cell disease presents to the emergency department with a temperature of 39.6 C (103.2F). Other than irritability, the physical examination is unremarkable. Laboratory evaluations reveal a white blood cell count of 18,200/mm3, with 88% polymorphonuclear neutrophils, 10% lymphocytes, and 2% monocytes, and a hemoglobin of 7.6 g/dL. Which of the following is the most appropriate next step in management?
Administer vancomycin and gentamicin intravenously
Administer ceftazidime and gentamicin intravenously
Administer ceftriaxone intravenously
Observe the child pending blood culture results
Administer amoxicillin orally
A 4-year-old previously healthy girl presents to the emergency department with a 24-hour history of rectal bleeding and dizziness. She has no other gastrointestinal symptoms. On examination, she appears pale. Her heart rate is 140 beats/min, and she has a 20 mmHg postural drop in systolic blood pressure. The child’s abdomen is nondistended and nontender, and fresh blood and clots are in the rectal vault on rectal examination. Definitive management of this child should include which of the following?
IV fluid resuscitation, transfusion with blood products as indicated, followed by a laparotomy with Meckel’s diverticulectomy and ileal resection
Immediate exploratory laparotomy
Stool softeners and topical steroids
IV fluid resuscitation, followed by a colonoscopic polypectomy
Hemorrhoidectomy
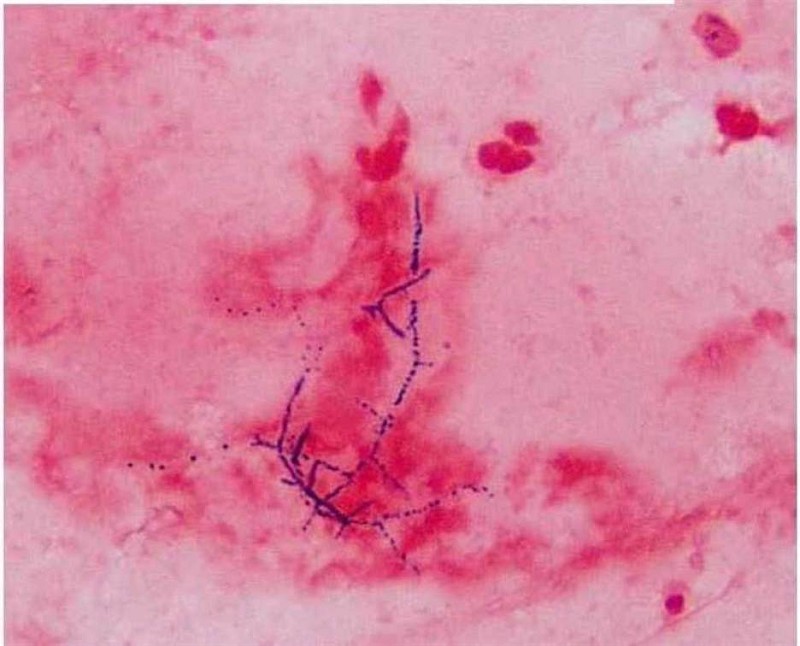
A 40-year -old man who underwent a renal transplant six months ago comes to the clinic with fever, chills, and a productive cough. His temperature is 39.4°C (103°F), pulse is 110/min, respirations are 22/min, and blood pressure is 110/65 mmHg. Chest x-ray shows a right lower lobe nodule with a cavity. Sputum gram stain is shown below. What is the most appropriate treatment of this patient's condition?
Penicillin
Metronidazole
Vancomycin
Gentamycin
Trimethoprim-sulfamethoxazole
A 40-year-old African American female comes to the office for a routine medical check-up. She has no complaints. She has twenty pack-year smoking history but she stopped smoking one year ago. Her mother and one maternal uncle have diabetes. Her height is 5'7" inches, and weight is 150 lbs. Her blood pressure is 122/80 mmHg, pulse is 80/min, respirations are 14/min and temperature is 37°C (98°F). She agrees to have diabetes mellitus screening. Her plasma glucose level after an overnight fast is 130 mg/dL. What is the most appropriate next step in the management of this patient?
Start therapy with insulin
Recommend lifestyle changes
Start therapy with oral hypoglycemic agents
Perform 75 g oral glucose tolerance test
Repeat fasting blood glucose measurement
A 40-year-old alcoholic is brought to the emergency department with frostbite to both lower extremities. His core body temperature is 36°C. Which of the following is the most appropriate initial treatment for the patient’s thermal injury?
Slow rewarming at room temperature
Rapid rewarming in warm water
Slow rewarming with dry heat
Sympathectomy without any delay
Debridement of devitalized tissues
A 40-year-old asymptomatic male comes to the office for a routine physical examination. His serum chemistry panel shows: Sodium 140 mEq/L, Potassium 4.0 mEq/L, Bicarbonate 25 mEq/L, Chloride 101 mEq/L, Calcium 11.8 mg/dL, Albumin 4.0 g/dL, Phosphorus 2.2 mg/dL. 24-hour urine collection reveals a calcium level of 200 mg, and creatinine level of 1.7 g. Serum PTH level is increased. Bone mineral density by dual energy X-ray absorptiometry (DEXA) shows normal bone mineral density. Neck examination reveals no masses. What is the most appropriate next step in the management of this patient?
Surgical exploration of the neck
Loop diuretics
Thiazide diuretics
Medical surveillance
Bisphosphonate therapy
A 40-year-old female patient is brought to the office by her husband due to altered mental status and confusion of recent onset. According to her husband, she has been complaining of intense thirst, craving for ice water, and experiencing increased urination for the past few days. Her only medication is lithium for bipolar depression. Her temperature is 39.0°C (102.5°F), pulse is 102/min, blood pressure is 90/60 mmHg, and respirations are 15/min. Physical examination reveals a disoriented patient with dry skin and mucous membranes. Blood chemistry panel reveals: Sodium 156 mEq/L, Potassium 4.1 mEq/L, Bicarbonate 26 mEq/L, Blood glucose 102 mg/dl, BUN 27 mg/dl. Serum osmolality is 328 mOsm/kg, and urine osmolality is 180mOsm/Kg. What is the most appropriate next step in the management of this patient?
IV infusion of normal saline
IV infusion of 5% dextrose
IV infusion of 045% saline
Water deprivation test
Plain water drinking
A 40-year-old female presents to the emergency room with palpitations and lightheadedness of acute onset. Also, she has experienced insomnia, fatigability, and weight loss lately. She does not smoke or consume alcohol. She is not taking any medication. Her blood pressure is 110/80 mmHg and heat rate is 120/min, irregular. Physical examination reveals lid lag and fine tremor of the outstretched hands. ECG shows atrial fibrillation with rapid ventricular response. What is the next best step in the management of this patient?
Digoxin
Immediate cardioversion
Propranolol
Lidocaine
Quinidine
A 40-year-old male developed shortness of breath during the postoperative recovery period. He had a large ventral hernia repair a few hours ago. He has no significant past medical history. He has never smoked. His temperature is 37.6C (99.8F), blood pressure is 100/60 mm Hg, pulse is 100/min and respirations are 30/min. Lungs are clear to auscultation except for a few rales at the bases. An x-ray film of the chest shows bibasilar atelectasis. Arterial blood analysis shows: pH 7.35, P02 70 mm Hg, PC02 45 mm Hg, HC03 28 mEq/L. Which of the following is the most appropriate next step in management?
Physiotherapy and respiratory exercises
Check serial cardiac enzymes
Administer bronchodilators and steroids
Perfusion/ventilation scintigraphy
Begin broad-spectrum antibiotics
A 40-year-old male presents with six months of worsening dyspnea. His symptoms have progressed to the point that walking even one block causes him to become shot of breath. He has a history of cigarette smoking, but quit 10 years ago. He drinks approximately one alcoholic drink daily. His medical history is significant for peptic ulcer disease for which he takes antacids. On physical examination, he is afebrile. His pulse is 86/min, blood pressure is 140/56 mmHg, and respiratory rate is 14/min. While examining his heat you note a high-pitched blowing, early diastolic, decrescendo murmur, which is heard best in the left third intercostal space and is intensified by handgrip. There is prominent cardiomegaly on chest x-ray. Which of the following medications would improve both this patient’s symptoms and cardiomegaly?
Quinidine
Nifedipine
Ephedrine
Amiodarone
Metoprolol
A 40-year-old man complains of exquisite pain and tenderness in the left ankle. There is no history of trauma. The patient is taking hydrochlorothiazide for hypertension. On examination, the ankle is very swollen and tender. There are no other physical examination abnormalities. Which of the following is the best next step in management?
Obtain ankle x-ray to rule out fracture
Apply a splint or removable cast
Begin allopurinol if uric acid level is elevated
Begin colchicine and broad-spectrum antibiotics
Perform arthrocentesis
A 40-year-old man with a recent history of exploratory laparotomy for a stabbing injury presents to the emergency department with diffuse cramping abdominal pain for 1 day, accompanied by nausea, multiple episodes of brown colored vomitus, and lack of stool, but he reports some flatulence. He denies any fever. On physical examination, the patient has stable vital signs, and there is diffuse distention in the abdomen with guarding and tenderness but no rebound, as well as high-pitched bowel sounds. Rectal examination reveals no fecal impaction in the rectal vault, and the stool was guaiac-negative. Complete blood cell count reveals no significant abnormalities and serum chemistry shows a mild metabolic alkalosis. CT demonstrates a noticeable difference in the diameter of proximal and distal small bowel. Which of the following is the most appropriate management?
Give the patient nothing by mouth, insert a nasogastric tube, and perform intravenous correction of electrolyte abnormalities
Exploratory laparotomy with lysis of adhesions
Broad-spectrum antibiotics
Serial abdominal examinations
Colonoscopy
A 40-year-old previously healthy man presents with sudden onset of severe abdominal pain that radiates from the right loin (flank) to groin. This pain is associated with nausea, sweating, and urinary urgency. He is distressed and restless, but an abdominal examination is normal. Which of the following is the most appropriate next step in management?
Urine culture, followed by initiation of antibiotic therapy
Cystoscopy and retrograde pyelogram
IV fluid hydration, IV analgesics, and arrangements for lithotripsy
IV fluid hydration, IV analgesics, and nonenhanced computed tomography (CT) scan
Insertion of a urethral catheter
A 40-year-old white female presents with complaints of heat intolerance, sweating and palpitations. She also reports menstrual irregularities, increased appetite and diarrhea. She has had these symptoms for the past 4 Months. Her pulse is 102/min and regular, blood pressure is 116/80 mmHg, temperature is 37.2°C (99°F), and respirations are 14/min. Physical examination reveals a non-tender, diffuse swelling in front of her neck; it moves upwards with deglutition. Her TSH level is 0.05 mU/L. Free T4 and T3 levels are increased. Radioactive iodine uptake at 24 hours is significantly increased. Pregnancy test is negative. Which of the following is the most appropriate long-term treatment modality for this patient?
Surgery
Radioactive iodine therapy
Propranolol
Propylthiouracil
Iodinated contrast agents
A 40-year-old white male develops a proximal deep vein thrombosis in the left lower extremity. Detailed history, examination and lab testing fail to reveal any obvious cause or risk factor for his deep venous thrombosis. Idiopathic deep vein thrombosis is diagnosed and the patient starts a 6-month course of warfarin anticoagulation. What is the goal INR therapeutic range in this patient?
1.0 to 1.5
2.5 to 3.5
Greater than 4
1.5 to 2.0
2.0 to 3.0
A 40-year-old woman cut her finger while cooking in her kitchen. Two days later she became rapidly ill with fever and shaking chills. Her hand became painful and mildly erythematous. Later that evening her condition deteriorated as the erythema progressed and the hand became a dusky red. Bullae and decreased sensation to touch developed over the involved hand. What is the most important next step in the management of this patient?
Evaluation for acute osteomyelitis
Vancomycin to cover community-acquired methicillin-resistant Staphylococcus
Treatment with penicillin for clostridia infection
Treatment with clindamycin for mixed aerobic-anaerobic infection
Surgical consultation and exploration of the wound
A 40-year-old woman presents with a rash involving the nipple-areola complex for the last month with associated itching. On physical examination there is crusting and ulceration of the nipple with surrounding erythema involving the areola and surrounding skin, no palpable breast masses, and no cervical or axillary lymphadenopathy. Which of the following is the most appropriate next step in the management of this patient?
Mammogram and biopsy of the affected area
Corticosteroid cream to the affected area
Administration of oral antibiotics
Modified radical mastectomy
Reexamine the patient in 1 month
A 40-year-old woman undergoes an incisional biopsy of a pigmented lesion on her right thigh. Pathologic examination reveals malignant melanoma with a thickness of 3 mm. Findings on examination of the groin is normal. Which of the following is the most appropriate next step in her management?
Wide local excision of the melanoma with a 2-cm margin from the tumor and groin lymph node dissection
Wide local excision of the melanoma with a 2-cm margin from the tumor and sentinel lymph node biopsy
Wide local excision of the melanoma with a 1-cm margin from the tumor and groin lymph node dissection
Wide local excision of the melanoma with a 1-cm margin from the tumor and sentinel lymph node biopsy
Wide local excision of the melanoma with a 1-cm margin from the tumor, followed by radiation to the groin
A 40-year-old, obese, white woman, mother of five children, gives a history of repeated episodes of right upper quadrant abdominal pain. The pain is brought about by the ingestion of fatty foods and is relieved by the administration of anticholinergic medications. The pain is colicky, radiates to the right shoulder and around to the back, and is accompanied by nausea and occasional vomiting. The patient has no pain at this time, but is anxious to avoid further episodes. She is afebrile, and physical examination is unremarkable. Which of the following is the most appropriate next step in management?
Endoscopic retrograde cholangiopancreatogram (ERCP)
Exploratory surgery
Antibiotics, IV fluids, and nothing by mouth
Upper gastrointestinal series with barium
Sonogram of the biliary tract and gallbladder
A 41-year-old G1P0 at 39 weeks, who has been completely dilated and pushing for 3 hours, has an epidural in place and remains undelivered. She is exhausted and crying and tells you that she can no longer push. Her temperature is 38.3C (101F). The fetal heart rate is in the 190s with decreased variability. The patient’s membranes have been ruptured for over 24 hours, and she has been receiving intravenous penicillin for a history of colonization with group B streptococcus bacteria. The patient’s cervix is completely dilated and effaced and the fetal head is in the direct OA position and is visible at the introitus between pushes. Extensive caput is noted, but the fetal bones are at the +3 station. Which of the following is the most appropriate next step in the management of this patient?
Rebolus the patient’s epidural
Cut a fourth-degree episiotomy
Attempt operative delivery with forceps
Encourage the patient to continue to push after a short rest
Deliver the patient by cesarean section
A 41-year-old man complains of regurgitation of saliva and of undigested food. An esophagram reveals a dilated oesophagus and a bird’s-beak deformity. Manometry shows a hypertensive lower esophageal sphincter with failure to relax with deglutition. Which of the following is the safest and most effective treatment of this condition?
Dilation with a Gruntzig-type (volume-limited, pressure-control) balloon
Surgical esophagomyotomy
Injections of botulinum toxin directly into the lower esophageal sphincter
Repeated bougie dilations
Medical treatment with sublingual nitroglycerin, nitrates, or calcium-channel blockers
A 41-year-old man underwent successful living-related kidney transplantation 1 year ago with good results. Preoperatively, he was noted to have an elevated calcium level; post-transplantation, he continues to have elevated calcium levels and associated symptoms. Which of the following is the most appropriate next step in management?
Measurement of urinary calcium levels
Total parathyroidectomy with autotransplantation of a portion of a gland into the forearm
99mTc sestamibi scanning
Ultrasound of the neck
CT scan of the neck and mediastinum
A 41-year-old woman comes to the office for the evaluation of a lump on her left breast. She feels, "generally well," and denies having any medical problems. She takes a multivitamin and Tums daily. She stopped smoking after getting married 21 years ago. She drinks wine only on weekends. Her only surgery was a bilateral tubal ligation last year, after giving birth to her fourth child. Physical examination of the left breast reveals a 4 cm lump at the 11 O'clock position and two axillary nodes on the left side. Mammography shows irregular micro-calcifications. The result of the FNA is suggestive for infiltrating ductal carcinoma. Which of the following is the single most important prognostic factor in this patient?
Irregular micro calcifications in mammogram
Her-2/neu oncogene expression
Histological grade of the tumor
Estrogen and progesterone receptor status
TNM staging
A 41-year-old woman has noted bilateral thin serous discharge from her breasts. There seems to be no mass associated with it. Which of the following statements would be appropriate to tell the patient?
Pathologic discharge is usually bilateral
Galactorrhea is indicative of an underlying malignancy
Absence of a mass on mammogram rules out malignancy
Expressible nipple discharge is an indication for open biopsy
Intermittent thin or milky discharge can be physiologic
A 41-year-old woman, gravida 4, para 3, at term is admitted to the labor and delivery ward with regular contractions every 2 minutes. Examination shows that her membranes are grossly ruptured and that her cervix is 5cm dilated. Over the following 3 hours, she progresses to full dilation and +2 station. A fetal bradycardia develops, and the decision is made to proceed with vacuum-assisted vaginal delivery. A 7 pound, 8ounce boy is delivered. APGAR scores are 8 at 1 minute and 9 at 5 minutes. Which of the following best represents an advantage of vacuum extraction over the forceps for expediting delivery?
The vacuum can be used in face presentations
The vacuum can be used for fetuses in breech presentation
The vacuum can be used at higher stations
The vacuum does not occupy space next to the fetal head
The vacuum can be used with intact membranes
A 42-year-old African-American woman presents to your office with bilateral knee pain that severely limits her mobility. She also complains of joint stiffness in the morning that takes several hours to improve. Her hand joints are symmetrically swollen. She has been taking over-the-counter ibuprofen and aspirin with little relief of symptoms. She has no other medical problems and does not use tobacco, alcohol, or illicit drugs. Her vital signs are within normal limits. Physical examination shows pain and swelling of both wrists and knees. Laboratory studies reveal: Hemoglobin 8.4 mg/dl, Serum iron 30 µg/dL (normal 50-150 µg/dL), Total iron binding capacity 230 µg/dL (normal 300-360 µg/dL), Ferritin 300 ng/dl. Which of the following is most likely to improve this patient's anemia?
Folic acid supplementation
Infliximab
Splenectomy
Iron supplementation
Cyanocobalamin supplementation
A 42-year-old Caucasian man presents to the emergency department complaining of a two-day history of fever to 40°C (104°F), headache, and vomiting. Physical examination reveals petechiae and purpura on his trunk and lower extremities. Examination of his cerebrospinal fluid is consistent with bacterial meningitis. The patient is told of his diagnosis and the need for antibiotics and hospitalization is discussed. The patient refuses to be admitted to the hospital, however, and insists upon being treated at home. What is the most appropriate next step?
Obtain a court order to proceed with treatment
Respect the patient's decision and arrange for home antibiotic therapy
Consult with the hospital ethics committee
Discuss the situation with the patient's wife and ask that she convince him to accept hospitalization
Treat the patient against his wishes
A 42-year-old G4P3104 presents for her well-woman examination. She has had three vaginal deliveries and one cesarean delivery for breech. She states her cycles are regular and denies any sexually transmitted diseases. Currently she and her husband use condoms, but they hate the hassle of a coital-dependent method. She is interested in a more effective contraception because they do not want any more children. She reports occasional migraine headaches and had a serious allergic reaction to anesthesia as a child when she underwent a tonsillectomy. She drinks and smokes socially. She weighs 78 kg, and her blood pressure is 142/89 mm Hg. During her office visit, you counsel the patient at length regarding birth control methods. Which of the following is the most appropriate contraceptive method for this patient?
Bilateral tubal ligation
Diaphragm
Transdermal patch
Combination oral contraceptives
Intrauterine device
A 42-year-old homeless man presents with a 3-week history of shortness of breath, fevers, and pleuritic chest pain. Chest x-ray (CXR) reveals a large left pleural effusion. Thoracentesis reveals thick, purulent-appearing fluid, which is found to have glucose less than 40 mg/dL and a pH of 6.5. A chest tube is placed, but the pleural effusion persists. Which of the following is the most appropriate management of this patient?
Thoracotomy with decortication and antibiotic therapy
Thoracotomy with instillation of antibiotics into the pleural space
Infusion of antibiotics via the chest tube
Intravenous antibiotics for 6 weeks
Placement of a second chest tube at the bedside and antibiotic therapy
A 42-year-old male is brought to the emergency department immediately after having a prolonged seizure episode. His family describes a past medical history of grand mal seizures. He has been on phenytoin for the past 10 years, but stopped taking the drug six months ago because he had not had any seizures in the last nine years. He is otherwise healthy and had been doing well until this seizure episode. He does not use tobacco, alcohol or drugs. He is afebrile. His blood pressure is 136/88 mm Hg, respirations are 18/min and pulse is 96/min. He appears confused and lethargic. Chest auscultation is unremarkable, and his abdomen is soft and nontender. A limited neurologic examination is non-focal. His laboratory report shows: Serum sodium 140 mEq/L, Serum potassium 4.0 mEq/L, Chloride 103 mEq/L, Bicarbonate 17 mEq/L, Blood urea nitrogen (BUN) 20 mg/dl, Serum creatinine 0.8 mg/dl, Blood glucose 98 mg/dl. Chest x-ray and urinalysis are within normal limits, and a CT scan of the head is unremarkable. Which of the following is the most appropriate next step in the management of this patient's metabolic acidosis?
Observe and repeat the labs after 2 hours
Start dopamine
Give intravenous bicarbonate
Check serum lipase
Check serum ketones
A 42-year-old man comes to the physician because of a 3-month history of burning substernal chest pain after every meal. His other medical problems include chronic alcoholism. Upper endoscopy shows mucosal irregularity and ulceration of the squamocolumnar junction above the lower esophageal sphincter. Multiple biopsies are taken. He complains of worsening substernal pain radiating to the back, left chest pain, and mild shortness of breath 4 hours later. His temperature is 37.1°C (98.9°F), blood pressure is 110/70 mm Hg, pulse is 120/min, and respirations are 34/min. A chest x-ray shows a small left pleural effusion that was not present on a chest radiograph taken 2 weeks ago. Which of the following is the most appropriate next step in management?
Wait until the pathologic diagnosis is ready
Perform thoracocentesis
Check serum amylase and lipase levels
Order water-soluble contrast esophagram
Repeat the endoscopy
A 42-year-old man develops right calf pain one week after having a left hemi-colectomy. On physical examination, there is moderate right ankle edema and right calf pain with dorsiflexion of the right foot. Duplex ultrasonography shows a clot in the right superficial femoral vein. Which of the following is the most appropriate initial treatment?
Aspirin
Tissue plasminogen activator
Heparin
Streptokinase
Warfarin
A 42-year-old man is found unconscious at the scene of a motor vehicle collision. He is rushed to the emergency department, where his blood pressure is found to be 70/40 mm Hg and his respirations are 28/min. On physical examination, his trachea is deviated to the left and his breath sounds are decreased on the right side. His neck veins are distended bilaterally. You also note significant swelling over the right femur. Which of the following is the most appropriate next step in the management of this patient?
Immediate thoracotomy
Intravenous fluid resuscitation
Chest tube placement
Intubation and mechanical ventilation
100% oxygen via face mask
A 42-year-old man presents to the clinic for routine evaluation. His medical history is signified cant for gallstones. The patient denies smoking and drinks alcohol occasionally. His mother had a heart attack at the age of 63 years. His blood pressure is 134/77 mmHg. The patient is overweight with well-healed laparoscopic cholecystectomy scars. Fasting laboratory tests show: Aspartate aminotransferase: 37 U/L, Alanine aminotransferase: 28 U/L, Alkaline phosphatase: 88 U/L, Total cholesterol: 268 mg/dL, LDL cholesterol: 183 mg/dL, HDL cholesterol: 46 mg/dL, Triglycerides: 166 mg/dL. What is the most appropriate next step in management?
A trial of lifestyle modification combined with statin therapy
Niacin therapy
Statin therapy
A trial of lifestyle modification combined with statin and niacin therapy
A trial of lifestyle modification alone (diet, exercise, and weight loss)
A 42-year-old man sustains a gunshot wound to the abdomen and is in shock. Multiple units of packed red blood cells are transfused in an effort to resuscitate him. He complains of numbness around his mouth and displays carpopedal spasm. An electrocardiogram demonstrates a prolonged QT interval. Which of the following is the most appropriate treatment?
Intravenous potassium
Intravenous bicarbonate
Intravenous parathyroid hormone
Intravenous digoxin
Intravenous calcium
A 42-year-old man with advanced HIV infection has a two-week history of pain and difficulty with swallowing. He was given fluconazole for these symptoms one week ago, but his pain has worsened. His current medications include tenofovir, emtricitabine, efavirenz, and trimethoprim-sulfamethoxazole. His CD4 count is 90/microl and viral load is 300,000copies/ml. Endoscopy reveals large, irregular, linear ulcers in the esophagus. A biopsy of the abnormal mucosa reveals tissue destruction and the presence of intranuclear and intracytoplasmic inclusions. Which of the following is the most appropriate pharmacotherapy for this patient?
Prednisone
Pentamidine
Ganciclovir
Itraconazole
Acyclovir
A 42-year-old mildly overweight Caucasian male is being worked-up for his second episode of deep venous thrombosis in two years. Both episodes seem to have been unprovoked. He denies any recent prolonged immobility, long-distance travel or lower extremity trauma. He has no past medical history of diabetes, cancer or liver disease. A thrombophilia work-up is ordered for this patient. Use of which of the following drugs is most likely to give a false-positive result for protein S deficiency?
Heparin
Aspirin
Clopidogrel
Simvastatin
Warfarin
A 42-year-old moderately obese female complains of abdominal discomfort two days after undergoing an elective cholecystectomy. Her past medical history is significant for hypertension, diabetes mellitus and hyperlipidemia. Her blood pressure is 132/90 mmHg and her heart rate is 76/min. Physical examination reveals a distended abdomen with decreased bowel sounds. Which of the following is most likely contributing to her current condition?
Perioperative antibiotics
Absence of bile storage reservoir
Metoclopramide for nausea
Insulin for glucose control
Morphine for pain relief
A 42-year-old postmenopausal woman presents to the clinic complaining of vague abdominal pain, early satiety, and a 9-kg (20-lb) unintended weight loss. She has a history of normal Pap smears. On physical examination her abdomen is firm, with evidence of ascites and a firm, irregular, and fixed left adnexal mass palpated on vaginal examination. CT scan of the abdomen and pelvis confirms the presence of an ovarian mass that has features that are highly suspicious for cancer. What is the best means to correctly diagnose and stage this mass?
Surgical exploration with tumor debulking and nodal sampling
Percutaneous needle biopsy of the tumor for histopathologic staining
Measurement of cancer antigen 125 level
Measurement of α-fetoprotein, β-human chorionic gonadotropin, and lactate dehydrogenase levels
MRI of the abdomen and pelvis
A 42-year-old woman comes to your office for an annual examination. She states that she has been feeling good over the past year. She exercises three times a week and watches her diet. She has no medical problems. She had an appendectomy at the age of 25, and no other surgeries. She uses a 35μg combined oral contraceptive pill (OCP) daily, and takes no other medications. She has been on “the pill” for birth control for the past 10 years and is happy with it. She has no known drug allergies. Physical examination, including breast and pelvic exams, is normal. She wants to know if she can continue to take the oral contraceptive pill. Which of the following is the most appropriate advice to give her?
Stop the OCP immediately
Change to HRT plus aspirin now
Continue on the OCP
Stop the OCP gradually over the next 3 years
Change from the combined OCP to hormone replacement therapy (HRT) now
A 42-year-old woman drops a hot iron on her lap while doing the laundry. She comes in with the shape of the iron clearly delineated on her upper thigh. The area is white, dry, leathery, and anesthetic. Which of the following is the most appropriate next step in management?
Repeated debridement and wet to dry dressings
Immediate excision and grafting
Application of mafenide acetate
Use of triple antibiotic ointment
Application of silver sulfadiazine
A 42-year-old woman is brought to the emergency department after being involved in a motor vehicle collision. On arrival she is unconscious with bilaterally round and reactive pupils. Her temperature is 37C (98.6F), blood pressure is 70/20 mm Hg, pulse is 11 0/min and respirations are 22/min. There is a low jugular venous pulse. She does not respond to vocal commands but responds to pain with all 4 limbs. She is not vocalizing. Lung auscultation is unremarkable. Abdominal examination shows a distended abdomen with absent bowel sounds and some bruising. She is intubated and is rapidly infused with 2L of lactated Ringer's solution. Her blood pressure is now 80/30 mm Hg and her pulse is 118/min. Which of the following is the most appropriate next step in management?
X-ray of abdomen
Chest x-ray
Lateral x-ray of spine
Exploratory laparotomy
CT scan of head
A 42-year-old woman presents to her physician with complaints of fever (38.2°C [100.8°F]) and mild-to-moderate anterior neck pain. On examination the physician finds her to be tachycardic and sweating, and to have an exquisitely tender thyroid gland. Her blood work shows a depressed thyroid-stimulating hormone level and increased free thyroxine. Which of the following is the most appropriate treatment at this time?
Acetaminophen
Prednisone
Radioactive iodine
Levothyroxine
Ibuprofen
A 42-year-old woman presents to the ER with the worst headache of her life. A noncontrast CT scan of the head is negative for lesions or hemorrhage. She then undergoes a lumbar puncture, which appears bloody. All 4 tubes collected have red blood cell counts greater than 100,000/mL. Which of the following steps is the most appropriate management of this patient?
Consult neurosurgery for immediate ventriculostomy
Perform a 4-vessel cerebral angiogram
Administer a dose of mannitol
Perform an angiogram of the aorta and lumbar branches for immediate embolization of the injured vessel
Repeat the head CT scan with intravenous contrast
A 42-year-old woman returns to the clinic following an uneventful biopsy for a well-defined, mobile mass. The pathology report describes the mass as a fibro adenoma, but LCIS is identified in the breast parenchyma adjacent to the fibro adenoma and extending to the margin of resection. She has no current illnesses, is on no medications, and her family history is negative for breast cancer. Breast imaging studies show fatty breasts with no abnormal findings except for the fibro adenoma. Which of the following is the most appropriate management option?
Observation including examinations and mammography
Bilateral total mastectomies
Ipsilateral mastectomy
Contralateral breast biopsy
Re-excision of the biopsy cavity to gain negative margins of resection
A 42-year-old woman sees her physician because she has been depressed for the past 4 months. She also notes that she has gained 20 lb without trying to. She notes that she does not take pleasure in the activities that she once enjoyed and seems fatigued most of the time. These symptoms have caused the patient to withdraw from many of the social fun
Recommend that the patient begin psychotherapy
Take a substance abuse history from the patient
Tell the patient that she should wait another 6 weeks, during which time her mood will improve
Increase the patient’s thyroid supplementation
Start the patient on an antidepressant medication
A 42-year-old woman with hypertension and a past history of an ectopic pregnancy 18 years earlier comes to your office and reports one episode of unprotected sexual intercourse 6 days ago. Her last menstrual period was normal and occurred 2 weeks earlier. She is concerned about unintended pregnancy and asks you about the “Morning After” pill. She reports no other complaints, has been healthy recently, and her hypertension has been well controlled. She has smoked one pack of cigarettes per day for the past 20 years. Which of the following factors in this patient would be a relative contraindication to prescribing hormonal emergency contraception?
History of ectopic pregnancy
Smoking status
History of hypertension
Greater than 5 days since unprotected intercourse
Age
A 42-year-old woman with no significant past medical history presents for a routine health maintenance visit. On physical examination a solitary nodule is palpated in the thyroid. She denies pain, dysphagia, or hoarseness. She also denies fatigue, weight change, heat or cold intolerance, diarrhea, or constipation. There is no family history of thyroid cancer. Her serum thyroid-stimulating hormone level is normal. Which of the following is the most appropriate next step in evaluation?
Fine-needle aspiration
Ultrasonography
Radionuclide scan
Thyroid lobectomy
MRI
A 42-year-old woman, gravida 2, para 1, at 10 weeks' gestation comes to the physician for her first prenatal visit. She has no complaints. She has a history of Trichomonas infection, but no other medical problems. Examination is significant for a 10-week sized, nontender uterus. During the speculum examination, a Pap smear is performed and gonorrhea and Chlamydia screening tests are taken. The next day, the gonorrhea test returns as positive. Which of the following is the most appropriate pharmacotherapy?
Ceftriaxone
Levofloxacin
Metronidazole
Clindamycin
Doxycycline
A 42-year-old woman, gravida 4, para 3, at 38 weeks' gestation, comes to the labor and delivery ward complaining of contractions. She has had type 1 diabetes since the age of 20. She has a history of syphilis that was adequately treated 4 years ago. She took insulin and prenatal vitamins throughout the pregnancy. Otherwise, her prenatal course was unremarkable, including normal screening. Her blood pressure is 140/90 mm Hg. Her cervix is 4 cm dilated and 100% effaced. She is admitted. Which of the following IV medications will this patient likely require during labor and delivery to prevent neonatal complications?
Hydralazine
Labetalol
Meperidine
Penicillin
Insulin
A 43-year-old Caucasian man with a two-year history of diabetes mellitus presents to your office for a routine. He has no complaint His medications are metformin and aspirin. He works as a computer programmer and has a sedentary lifestyle. He drinks one to two cans of beer on weekends and smokes one pack of cigarettes per day. On physical examination, his blood pressure is 153/94 mmHg and his heat rate is 82/min. His BMI is 32.5 kg/m2. The remainder of the physical examination is unremarkable. Laboratory studies reveal an HbA1c of 7.6%. At his check-up one month ago, his blood pressure was 149/92 mmHg. Which of the following interventions would be most effective for controlling his blood pressure?
Aerobic exercise
Quitting alcohol
Better diabetes control
Weight loss
Smoking cessation
A 43-year-old construction worker presents to your office 2 weeks after an episode of acute back pain. The pain started after lifting a heavy box, was localized to the lower back with little radiation to the buttocks, and quickly responded to conservative treatment. His past medical history is insignificant. He smokes 2 packs a day and consumes alcohol occasionally. He is concerned about the possibility of recurrence of the pain. Which of the following would be most helpful in preventing another episode of back pain in this patient?
Keep the back straight while lifting an object
Regular exercise with repetitive twisting and bending
Limiting the physical activity as much as possible
Bend at the waist, not at the knees
Sleep on the stomach
A 43-year-old female with history of hepatitis C, alcohol use and cirrhosis is admitted to the hospital for severe vomiting for the last 2 days. Her temperature is 36.7°C (98.2°F), pulse is 90/min, respirations are 14/min and blood pressure is 100/70 mmHg supine. Her lungs are clear to auscultation. She has mild epigastric tenderness, but there is no abdominal distention. Extremities have no edema. Her laboratory profile shows: Blood PH 7.49, PaO2 100 mmHg, PaCO2 41 mm Hg, HCO3- 30 mEq/L, Sodium 138 mEq/L, Potassium 3.0 mEq/L, Chloride 95 mEq/L. Which of the following is the most appropriate treatment for the patient's alkalosis?
Intravenous normal saline and potassium
Dialysis
Intravenous hydrochloric acid and potassium
Intravenous mannitol
Intravenous ammonium chloride and potassium
A 43-year-old G1P0 who conceived via in vitro fertilization comes into the office for her routine OB visit at 38 weeks. She denies any problems since she was seen the week before. She reports good fetal movement and denies any leakage of fluid per vagina, vaginal bleeding, or regular uterine contractions. She reports that sometimes she feels crampy at the end of the day when she gets home from work, but this discomfort is alleviated with getting off her feet. The fundal height measurement is 36 cm; it measured 37 cm the week before. Her cervical examination is 2 cm dilated. Which of the following is the most appropriate next step in the management of this patient?
Order the patient to undergo a nonstress test
Do a fern test in the office
Send the patient for a sonogram to determine the amniotic fluid index
Admit the patient for induction caused by a diagnosis of fetal growth lag
Instruct the patient to return to the office in 1 week for her next routine visit
A 43-year-old man presents to the ED complaining of progressively worsening abdominal pain over the past 2 days. The pain is constant and radiates to his back. He also describes nausea and vomiting and states he usually drinks six pack of beer daily, but has not had a drink for 2 days. His BP is 144/75 mm Hg, HR is 101 beats per minute, temperature is 99.8°F, and RR is 14 breaths per minute. He is lying on his side with his knees flexed. Examination shows voluntary guarding and tenderness to palpation of his epigastrium. Laboratory results reveal WBC 10,500/μL, hematocrit 51%, platelets 225/μL, and lipase 620 IU. An abdominal radiograph reveals a nonspecific bowel gas pattern. There is no free air under the diaphragm. Which of the following is the most appropriate next step in management?
Admit to the hospital for medical management and supportive care
Admit to the hospital for endoscopy
Observe in the ED
Admit to the hospital for exploratory laparotomy
Send home with antibiotic therapy
A 43-year-old man without symptoms is incidentally noted on CT scan to have a 4 cm lesion in the periphery of the left lobe of the liver. The lesion enhances on the arterial phase of the CT scan and has a central scar suggestive of focal nodular hyperplasia (FNH). Which of the following is the recommended treatment of this lesion?
Intra-arterial embolization of the lesion
Radiofrequency ablation of the liver lesion
No further treatment is necessary
Formal left hepatectomy
Wedge resection of the lesion
A 43-year-old previously healthy male is hospitalized for acute pancreatitis. On day 3 of his admission, he develops respiratory distress. He is transferred to the intensive care unit and intubated. His initial ventilator settings are: FiO2 0.8 (80%), Respiratory rate 10/min, Tidal volume 500 ml, PEEP 5 mm H20. Ten minutes after being intubated, the man's blood pressure is 110/70 mmHg and his heart rate is 90/min. His arterial blood gases are: pH 7.42, pO2 105 mmHg, pCO2 37 mmHg. Which of the following is the best next step in the management of this patient?
Decrease the FiO2
Increase the respiratory rate
Decrease the respiratory rate
Decrease the positive end expiratory pressure (PEEP)
Decrease the tidal volume
A 43-year-old primigravid woman at 10 weeks' gestation comes to the physician for a prenatal visit. She is feeling well except for some occasional nausea. She has had no bleeding from the vagina, abdominal pain, dysuria, frequency, or urgency. She has asthma for which she occasionally uses an inhaler. Examination is normal for a woman at 10 weeks gestation. Urine dipstick is positive for nitrites and leukocyte esterase and a urine culture shows 50,000 colony forming units per milliliter of Escherichia coli. Which of the following is the most appropriate next step in management?
Obtain a renal ultrasound
Admit for intravenous antibiotics
Treat with oral antibiotics
Wait to see if symptoms develop
Resend another urine culture
A 43-year-old white male is found to have premature atrial complexes (PACs) on routine EKG. He denies chest pain, shortness of breath or lightheadedness. He has smoked 1-2 packs of cigarettes daily for the past 20 years. He also has a 20-year history of alcoholism, though recently he has limited his use to 1-2 beers/day. The patient's family history is significant for a myocardial infarction in his mother at age 65 and a stroke in his father at age 72. He has no personal history of hypertension or diabetes. Physical examination including vital signs, is entirely within normal limits. What is the best next step in the management of this patient?
Advise him to stop alcohol and tobacco
Reassurance
Start beta-blocker therapy
Echocardiogram
24-hour Halter monitoring
A 43-year-old woman comes in because of a breast mass. Two days ago, she noticed a lump on self-examination. She has a 2-cm, firm, nontender mass in the left breast, which is movable from the chest wall, but not movable within the breast. She has no prior history of breast disease, but she is well read and well informed, and she specifically requests that a biopsy be done with a mammotome. Before proceeding, which of the following is the most appropriate initial step?
Obtain a fine-needle aspirate and go no further if no malignant cells are found
First wait for two menstrual cycles to see whether there is spontaneous resolution
Do a mammogram to find any other lesions that might also need to be addressed
Do a mammogram to ascertain whether biopsy is needed
Discuss the surgical options in case cancer is found
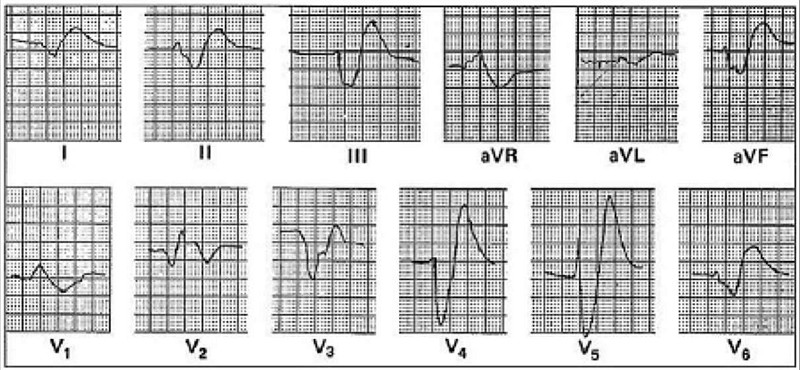
A 43-year-old woman develops acute renal failure following an emergency resection of a leaking abdominal aortic aneurysm. One week after surgery, the following laboratory values are obtained:Serum electrolytes (mEq/L): Na+ 127, K+ 5.9, Cl− 92, HCO3− 15Blood urea nitrogen: 82 mg/dLSerum creatinine: 6.7 mg/dLThe patient has gained 4 kg since surgery and is mildly dyspneic at rest. Eight hours after these values are reported, the following electrocardiogram is obtained. Which of the following is the most appropriate initial treatment in the management of this patient?
10 mL of 10% calcium gluconate
Emergent hemodialysis
100 mg lidocaine
Oral Kayexalate
0.25 mg digoxin every 3 hours for 3 doses
A 44-year-old homeless woman presents to the emergency department because she is "bleeding from the breast." Physical examination shows a huge, fungating, ulcerated mass that occupies the entire right breast and is firmly attached to the chest wall. The right axilla is full of hard masses that are not movable either. Core biopsies of the breast are read as highly undifferentiated infiltrating ductal carcinoma, and assay for estrogen and progesterone receptors are negative. Which of the following is the most appropriate next step in management?
Radical mastectomy with extended lymph node dissection
Tamoxifen therapy
Local wound care, but no specific antineoplastic therapy
Radiation and chemotherapy
Palliative mastectomy
A 44-year-old male has been abusing drugs for many years. Recently he started using the agent MPTP and he now presents to you in the ER. He says that he is not feeling well and wonders what is going on. He says he has a persistent tremor in his fingers and his body has become rigid. At times has had difficulty in walking. The CT scan of his brain is normal and all the blood work is within normal limits. You decide to treat him. Two years later you see him and he tells you that his symptoms have improved. He also noticed that he had a significant relief from the recurrent and persistent upper respiratory tract viral infections that he was so prone to. The agent you gave him was?
Bromocriptine
Amantadine
Benztropine
Acyclovir
Levodopa-Carbidopa
A 44-year-old male is involved in a serious motor vehicle accident. He is admitted to the intensive care unit with multiple fractures and internal bleeding, and is placed on mechanical ventilation. Over the next two days, his oxygen saturation repeatedly drops below 90%, requiring gradual increases in the FiO2. On day three of his admission, the patient's chest x-ray, which was initially clear, shows bilateral fluffy infiltrates. He has no prior medical problems and does not take any medications. Skin examination reveals no rashes. Lab studies show: Hemoglobin 10.1 g/L, Platelets 160,000/mm3, Leukocyte count 13,500/mm3. Sputum cultures are negative. The ventilator settings are: FiO2 90%, Tidal volume 400 ml (body weight 60 kg), Respiratory rate 12/min, PEEP 5cmH2O. The patient's oxygenation continues to drop below 90%. Which of the following interventions would be best for improving the patient's oxygenation?
Increase the PEEP
Administer packed red blood cells
Increase the intravenous fluids
Increase the respiratory rate
Increase the tidal volume
A 44-year-old man is brought to the emergency department after a motor vehicle accident. His cervical spine is immobilized and 2 large-bore intravenous lines are placed. His breath smells of alcohol. The patient is lethargic but responds to commands appropriately. A 3-cm laceration is present on his forehead. Ecchymoses are seen on his back and over the abdominal wall in the distribution of the seat belt. The lungs are clear to auscultation. The trachea is midline and the neck veins are collapsed. Passive movement of the right hip is limited due to pain. At the scene of the accident, blood pressure was 90/60 mm Hg and pulse was 130/min. After receiving a 1 L bolus of intravenous fluids, the patient's blood pressure remains 90/60 mm Hg and his pulse is now 122/min. Portable chest x-ray shows no pneumothorax or pleural effusions. A bedside abdominal ultrasound is inconclusive for hemoperitoneum or intra-abdominal injury due to poor image quality. What is the most appropriate next step in management of this patient?
Diagnostic peritoneal lavage
Plain x-ray films of the abdomen
Immediate laparotomy
Computed tomography scan of the abdomen
Computed tomography scan of the head
A 44-year-old obese male is brought to the ER after a motor vehicle accident. His cervical spine is immobilized. He is alert and able to speak in complete sentences. He complains of abdominal pain. At the scene of the accident, his blood pressure is 90/60 mm Hg and pulse is 120/min. Lungs are clearto auscultation. Ecchymosis is present over the abdominal wall in distribution of the seat belt. Bowel sounds are decreased. Neck veins are collapsed. After receiving one liter of intravenous fluids, his blood pressure remains at 90/60 mmHg. A focused assessment with sonography for trauma is inconclusive due to the poor image quality. Which of the following is the most appropriate next step in management of this patient?
Diagnostic peritoneal lavage
X-ray of the chest
Immediate laparotomy
CT scan of the abdomen
Plain X-ray films of the abdomen
A 44-year-old renal transplant patient develops severe cough and shortness of breath on exertion. On examination, he appears dyspneic, respirations 24/min, pulse 110/min, and oxygen saturation 88%. His lungs are clear on auscultation and heart sounds are normal. CXR shows bilateral diffuse perihilar infiltrates. Bronchoscopy and bronchial brushings show clusters of cysts that stain with methenamine silver. Which of the following is the most appropriate next step in management?
Amphotericin B
Aminoglycosides
Penicillins
Trimethoprim-sulfamethoxazole
Cephalosporins
A 44-year-old white male comes to the office and says, "I have had this persistent, upper abdominal pain for the past 2 months. My wife has peptic ulcer, and I think I also have an ulcer down there, so I take some of her medicines. At first, the medicines made the pain go away, but soon after the pain proved to be too tough for the medicines. I hardly want to eat anything now. Do you think all this is due to some reaction to those medicines?" Physical examination reveals mild tenderness in the epigastric region. Esophagogastroduodenoscopy reveals a mass in the pylorus, which the biopsy identifies as an infiltrating, low-grade, gastric mucosa-associated lymphoid tissue (MALT) lymphoma. Further work-up concludes that there are no regional lymph nodes involved. What is the best next step in the management of this patient?
Give combination chemotherapy
Observation and strict surveillance
Radiotherapy
Give a combination of omeprazole, clarithromycin, and amoxicillin
Radical gastrectomy with en bloc resection of spleen and regional nodes
A 44-year-old woman has a 2-cm firm palpable mass in the upper outer quadrant of her right breast. The mass is freely movable, and her breast is of normal, rather generous size. There are no palpable axillary nodes. Mammogram shows no other lesions. A core biopsy establishes a diagnosis of infiltrating ductal carcinoma. She has no neurologic or skeletal symptoms, and a chest x-ray film and liver enzymes are normal. She understands that systemic therapy may eventually be needed once the full extent of her disease is known. Although she wants the best chance for cure, she is very concerned about cosmetic deformity and wants to know what can be done about the breast itself. Which of the following is the most appropriate management?
Modified radical mastectomy with immediate rectus abdominis flap reconstruction
Simple total subcutaneous mastectomy with implants
Lumpectomy, axillary sampling, and postoperative radiation
Radiation and chemotherapy without breast surgery
Radical mastectomy and postoperative radiation, with delayed reconstruction
A 44-year-old woman is recovering from a mild episode of acute ascending cholangitis secondary to choledocholithiasis. When seen initially, she had a spiking fever, leukocytosis, and a very high alkaline phosphatase; however, all these findings subsided rapidly after she was placed on IV antibiotics. A sonogram of the right upper quadrant on the day of admission showed the presence of gallstones in the gallbladder, but the diameter of the biliary ducts was normal. It was assumed that she had passed a common duct stone, and plans to do an endoscopic retrograde cholangiopancreatogram (ERCP) were canceled. While awaiting elective cholecystectomy, she again developed a fever and leukocytosis, and her liver fun
Metronidazole
Open surgical resection of the right lobe of the liver
Percutaneous drainage of the liver abscess
Long-term IV antibiotics
ERCP and biliary drainage
A 44-year-old woman presents for a follow-up visit regarding her severe depression. She has taken numerous antidepressants over the years with little symptomatic relief, and continues to spend the majority of her time in seclusion, experiencing intense feelings of worthlessness and despair. Her husband is deeply concerned about the impact her depression has had on their marriage and their two teenage children. He requests information about "all available options" to improve his wife's symptoms. The prospect of electroconvulsive therapy (ECT) is discussed, and the husband inquires about potential drawbacks to the procedure. Which of the following is a common side effect of electroconvulsive therapy?
Amnesia
Neuroleptic malignant syndrome
Epilepsy
Muscle paralysis
Elevated liver enzymes
A 45-year-old African-American woman who was diagnosed with PCOS in her early twenties presents to her gynecologist for her annual visit. One of her close friends has recently been diagnosed with ovarian cancer, so she is concerned about her own cancer risk. Menarche was at age 14 years, and she has yet to go through menopause. She has a healthy 19-year-old daughter. She has no family history of cancer. She does not smoke or drink and exercises regularly. Aside from a diagnosis of PCOS, she is otherwise in good health. Given her health history, which of the following statements is true?
She should have annual mammograms, although her risk of breast cancer is not changed relative to women without PCOS
She should have annual mammograms because she has an increased risk of developing breast cancer relative to women without PCOS
She should have annual Pap smears, although she has a decreased risk of developing cervical cancer relative to women without PCOS
She should have annual Pap smears because she has an increased risk of developing cervical cancer relative to women without PCOS
She should have annual Pap smears because she has an increased risk of developing ovarian cancer relative to women without PCOS
A 45-year-old G2P2 female presents for annual examination. She reports regular menstrual cycles lasting 3 to 5 days. She exercises 5 times per week and reports no difficulty sleeping. Her weight is stable 140 lbs and she is 5 ft 8 in tall. Physical examination is unremarkable. Laboratory studies are normal with the exception of a TSH value of 6.6 mU/L (normal 0.4-4.0 mU/L). Which of the following represents the best option for management of this patient’s elevated TSH?
Measure thyroid peroxidase antibodies (TPOAb)
Recommend dietary iodide supplementation
Order thyroid uptake scan
Begin low dose levothyroxine (25-50 μg/d)
Repeat TSH in 3 months and reassess for signs of hypothyroidism
A 45-year-old male comes to the emergency room complaining of shortness of breath that began 3 hours ago. He also has a nonproductive cough, a low-grade fever and right-sided chest pain that worsen with inspiration. He denies coughing up blood, wheezing, palpitations, leg pain or swelling of his lower extremities. He recently returned home from a trip to Singapore. He has a history of hypertension and diabetes mellitus. His takes fosinopril, metformin and glyburide. He doesn't use tobacco, alcohol or illicit drugs. His temperature is 98.0°F (36.6°C), blood pressure is 115/70 mmHg, pulse is 128/min, respirations are 32/min, and O2 saturation is 84% on room air. Physical examination shows a slightly obese man in acute respiratory distress. He is alert and cooperative without any cyanosis or jaundice. He has a slightly displaced apical impulse with a S4. Chest-x ray shows mild cardiomegaly with no infiltrates. EKG shows sinus tachycardia and left ventricular hypertrophy without ST-T wave changes. His arterial blood gas analysis shows pH 7.52, pCO2 30, pO2 55, HC03 22. What is the next best step in the management of this patient?
Spiral CT scans of the chest
Broad spectrum antibiotics
Initiate heparin weight-based protocol
Pulmonary angiogram
Lower extremity venous ultrasound
A 45-year-old male patient comes to the physician's office for a routine check-up. He denies any symptoms and says he feels "perfectly healthy." He was diagnosed with hypertension and mixed hypercholesterolemia a year ago. He is currently taking hydrochlorothiazide, amiloride and simvastatin daily. He does not use tobacco, alcohol or drugs. His blood pressure today is 135/85 mm Hg. Physical examination shows no abnormalities. Routine blood results reveal the following: CBC: Hb 14.2g/dL, Ht 42%, MCV 86 fl, Platelet count 260,000/cmm, Leukocyte count 8,500/cmm, Neutrophils 70%, Eosinophils 1%, Lymphocytes 24%, Monocytes 5%. Serum: Serum Na 140 mEq/L, Serum K 5.7 mEq/L, Chloride 100 mEq/L, Bicarbonate 24 mEq/L, BUN 10 mg/dL, Serum Creatinine 1.1 mg/dL, Calcium 9.0 mg/dL, Blood Glucose 118 mg/dL, Total cholesterol 220 mg/dL, LDL cholesterol 130 mg/dL. The blood sample is checked and is not hemolysed. The EKG shows normal sinus rhythm. What is the most appropriate next step in the management of this patient?
Stop HCTZ and recheck lab results in 1 week
Start patient on a low potassium diet
Stop amiloride and recheck lab results in 1 week
Intravenous calcium gluconate
Intravenous dextrose + insulin
A 45-year-old male presents to your clinic with complaints of pleuritic chest pain. He says he is a heavy smoker and has been having intermittent cough for the past 2 weeks. His blood work is normal and his chest x ray is clear. EKG reveals a normal sinus rhythm with a heart rate of 68. He does have a PR interval > 0.2 seconds. The next step in the management of his arrhythmia is:
Observation
Cardiac catheterization
Electrophysiology study
Atenolol
Pacemaker
A 45-year-old male with mild persistent asthma comes to you for a routine checkup. He is taking a low-dose beclomethasone inhaler daily and inhaled albuterol, as needed, for the last year. His past medical history is otherwise not significant. His family history is significant for diabetes mellitus type 2, hypertension and obesity. His blood pressure is 136/90 mmHg and his heart rate is 80/min. His BMI is 26 kg/m2. Which of the following is the most likely complication of chronic beclomethasone use in this patient?
Cushing's syndrome
Adrenal suppression
Purpura
Thrush
Osteoporosis
A 45-year-old man complains of sudden pain and swelling in his left first metatarsophalangeal joint. He is undergoing high dose induction chemotherapy for acute leukemia. Joint fluid aspiration reveals negative birefringent crystals and elevated white cell count. Which of the following prophylactic measures would most likely have prevented this condition?
Adequate hydration
Urine acidification
N-acetylcysteine
Mesna
Allopurinol
{"name":"DES C_Management (7) Prepared : CHILLY", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 38-year-old woman, gravida 4, para 4, comes to the physician 8 days after a cesarean delivery complaining of redness and pain at the leftmost aspect of her incision. Her cesarean delivery was performed secondary to a non reassuring fetal heart rate tracing. She was feeling well after the operation until 4 days ago, when she developed pain and redness around her incision. Her temperature is 37 C (98.6 F), blood pressure is 118\/78 mm Hg, pulse is 88\/min, and respirations are 12\/min. There is marked erythema and induration around the incision. At the left margin of the incision there is a fluctuant mass. Which of the following is most appropriate next step in management?","img":"https://cdn.poll-maker.com/20-805835/image.jpeg?sz=1200"}
More Quizzes
Discover Your Persona: A Fun Quiz!
10512
Which Doctor-Who character are you? (11th Doctor Characters)
320
Friends
12612
Satéprikker
320
Quiz
210
SFAR
70350
Elite 8: Best Character of the 80/90s
420
How well do you know this dum Trash cunt?
1269
Which Member of the Loric Garde are you?
21100
210
Navigational Skills Assessment Quiz
231257
How well do you know ramez
14713