DES C_Management (5) Prepared : CHILLY
A 30-year-old man presents to the ED complaining of sudden onset of abdominal bloating and back pain lasting for 2 days. The pain woke him up from sleep 2 nights ago. It radiates from his back to his abdomen and down toward his scrotum. He is in severe pain and is vomiting. His temperature is 101.2°F and HR is 107 beats per minute. A CT scan reveals a 9-mm obstructing stone of the left ureter with hydronephrosis. Urinalysis is positive for 2+ blood, 2+ leukocytes, 2+ nitrites, 40 to 50 WBCs, and many bacteria. You administer pain medicine, antiemetics, and antibiotics. Which of the following is the most appropriate next step in management?
Discharge patient with antibiotics, pain medicine, and instructions to drink large amounts of water and cranberry juice
Discharge patient with instructions to consume large amounts of water
Discharge with antibiotics and pain medicine
Observe in ED for another 6 hours to see if stone passes
Admit for IV antibiotics and possible surgical removal of stone
A 30-year-old man presents to the emergency department with sudden onset of severe epigastric pain and vomiting 3 hours ago. He reports a 6-month history of chronic epigastric pain occurring nearly every day and relieved by antacids. On examination, he appears sweaty and avoids movement. Vital signs reveal a temperature of 100°F, BP of 100/60 mmHg, pulse rate of 110/min, and respiratory rate of 12/min. The remainder of his examination reveals diminished bowel sounds and a markedly tender and rigid abdomen. A chest x-ray and abdominal films reveal pneumoperitoneum. Which of the following is the most appropriate next step in management?
Fluid resuscitation
Placement of a central venous line
Administration of H2 blockers
Nonoperative management with NG decompression and antibiotics
Immediate laparotomy
A 30-year-old man presents to the resuscitation bay with gunshot wounds in the anterior and posterior left chest. Although in distress and dyspneic, the patient is cooperative. He has a patent airway and is moving all extremities. His pulse is 120/min, blood pressure is 120/90 mm Hg, and respiratory rate is 30/min. He has bounding distal pulses, and no other injuries are identified on secondary examination. X-ray of the chest reveals fluid in the pleural space, and a left chest tube thoracostomy yields 600 mL of bright red fluid. Over the next hour 750 mL of blood is collected. What is the most appropriate next step in management?
Remove the chest tube and suture the incision closed
Thoracentesis
Insert another chest tube
Left thoracotomy
Autotransfuse with the collected blood and continue to observe closely
A 30-year-old obese G3P2 woman is in active labor at 41 weeks’ gestation. She has no significant past medical history, and had an uncomplicated pregnancy with appropriate prenatal evaluation. The patient ruptured membranes spontaneously 30 minutes ago. Contractions occur regularly every 2–3 minutes. Early decelerations are noted on the fetal heart rate monitor with each of the past five contractions. Which is the most appropriate next step in management?
Prepare for emergent cesarean delivery
Start an amnioinfusion of saline
No further management is required
Place a fetal scalp probe
Change the maternal position
A 30-year-old obese white female comes to the physician with a six months history of oligomenorrhea. She never had this problem before. She has no galactorrhea. She has gained significant weight over the past two years despite a regular exercise program. She has also experienced hair loss during this time. She has had regular Pap smears since the age of 20; pap smears have shown no abnormalities. She takes no medications. She does not use tobacco, alcohol, or drugs. Her mother has a history of endometrial carcinoma and her grandmother had a history of ovarian carcinoma. Physical examination shows male pattern baldness. Abdominal and pelvic examination shows no abnormalities. A urine pregnancy test is negative. Serum prolactin level and thyroid fun
Screening mammogram
CA-125 levels, annually
Diagnostic laparoscopy
Oral glucose tolerance test
Iron studies
A 30-year-old school teacher presents with a three-day history of fever, chills, and sore throat. He also complains of difficulty swallowing that started yesterday. He denies any cough, chest pain, or difficulty breathing. He is married and denies any new sexual encounters. His temperature is 39°C (102.2°F), blood pressure is 118/76 mmHg, pulse is 102/min, and respirations are 19/min. On examination, his voice is muffled. Enlarged, tender cervical lymph nodes are palpated on the left, and his uvula is deviated to the right. What is the most appropriate treatment for this patient?
Emergency laryngoscopy
Needle peritonsillar aspiration
Cricothyroidotomy
Monospot test and oral antibiotics
Throat swabs and oral antibiotics
A 30-year-old white, HIV-infected male from Ohio presents with low-grade fever, anorexia and weight loss of 3.6kg (Bib) for the past 3 weeks. His baseline PPD test was negative. His pulse is 87/min, blood pressure is 126/76 mm Hg, temperature is 38.3°C (101°F), and respirations are 18/min. Examination shows oropharyngeal ulcers and hepatosplenomegaly. Lab testing shows: Hematocrit 36%, Platelet count 50,000/microL, WBC count 3,100/microL. Blood culture establishes the diagnosis of histoplasmosis. What is the most appropriate next step in the management of this patient?
Lifelong treatment with itraconazole
IV amphotericin B plus itraconazole till the cultures become negative
Itraconazole till the cultures become negative
IV amphotericin B till the cultures become negative
IV amphotericin B followed by lifelong treatment with itraconazole
A 30-year-old woman comes to the physician 6 hours after falling on her outstretched right hand. She has pain and limitation of movement in her wrist, but denies sensations of tingling or numbness. The right wrist is mildly swollen, and its range of passive motion is limited compared with the left side. Palpation elicits maximal tenderness in the area of the anatomic snuffbox, between the tendons of the extensor pollicis longus and abductor pollicis muscles. Ulnar and radial pulses are normal, and Tinel's and Phalen's tests are negative. Further examination rules out signs of nerve or vascular damage. Plain x-ray films performed in the anteriorposterior, lateral, and oblique views fail to show any evidence of fractures. At this time, which of die following is the most appropriate next step in management?
Treatment for wrist sprain
Angiography Pulmonaire
Treatment for scaphoid fracture
Bone scanning
MRI examination of the wrist
A 30-year-old woman comes to the physician due to the recent onset of occipital headaches. She has taken acetaminophen several times, but the pain returns. She has no fever or visual problems. She has not had similar episodes in the past. She has no history of serious illness. Her temperature is 36.1°C (98°F), blood pressure is 160/90 mm Hg, pulse is 88/min, and respirations are 16/min. Physical examination shows a rightsided renal bruit Which of the following is the most appropriate treatment for this patient's condition?
ACE inhibitors
Surgery
Oral prednisone
Angioplasty with stent placement
Furosemide
A 30-year-old woman in her last trimester of pregnancy suddenly develops massive swelling of the left lower extremity. Which of the following would be the most appropriate workup and treatment at this time?
Duplex ultrasonography, heparin, warfarin (Coumadin)
Duplex ultrasonography and heparin
Duplex ultrasonography, heparin, and vena caval filter
Impedance plethysmography, warfarin
Venography and heparin
A 30-year-old woman with a genetic disorder characterized by a deficiency of phenylalanine hydroxylase is planning a first pregnancy. Her physician explains the increased risk of mental retardation, as well congenital heart disease, in the infant. Which of the following should also be recommended?
Vitamin B6 should be administered to the neonate on delivery
There is no need for diet control if phenylalanine levels are mildly elevated
Dietary supplementation with L-carnitine is recommended
Dietary supplementation with glycine is recommended
Low phenylalanine diet should be initiated before conception
A 30-year-old woman, gravida 2, para 1, at 37 weeks gestation is brought to the emergency department because of acute onset intense uterine contractions and vaginal bleeding. She has been followed closely for pre-eclampsia since her 32nd week of gestation. Her temperature is 37.0°C (98.7°F), blood pressure is 140/86mmHg, pulse is 92/min and respirations are 18/min. Physical examination shows uterine tenderness and hyperactivity and moderate vaginal bleeding. Pelvic examination shows an effaced and 3cm dilated cervix. Ultrasonography shows a fundic placenta and a fetus in the cephalic position. Fetal heart tracing shows 140/min with good long-term and beat-to beat variability. After initial resuscitation the bleeding is stopped. Which of the following is the most appropriate next step in management?
Forceps delivery
Conservative management at home
Perform tocolysis and schedule cesarean section within 48 hours
Vaginal delivery with augmentation of labor, if necessary
Emergency cesarean section
A 30-year-old woman, gravida 2, para 1, at 37 weeks gestation is brought to the emergency department because of acute onset intense uterine contractions and vaginal bleeding. She has been followed closely for pre-eclampsia since her 32nd week of gestation. Her temperature is 37.0 C (98.7F), blood pressure is 140/86mmHg, pulse is 92/min and respirations are 18/min. Physical examination shows uterine tenderness and hyperactivity and moderate vaginal bleeding. Pelvic examination shows an effaced and 3cm dilated cervix. Ultrasonography shows a fundic placenta and a fetus in the cephalic position. Fetal heart tracing shows 140/min with good long-term and beat-to-beat variability. After initial resuscitation the bleeding is stopped Which of the following is the most appropriate next step in management?
Forceps delivery
Conservative management at home
Perform tocolysis and schedule cesarean section within 48 hours
Vaginal delivery with augmentation of labor, if necessary
Emergency cesarean section
A 30-year-old woman, gravida 3, para 2, at 32 weeks gestation comes to the physician because of a decrease in fetal movements. She has felt few fetal kicks the past 20 hours. Her prenatal course, prenatal tests and fetal growth have been normal. She has chronic hypertension and is now taking methyldopa and labetalol. Her previous pregnancies were uncomplicated and both delivered vaginally. She does not use tobacco, alcohol or drugs. Fetal heart tones are heard by Doppler. Non-stress test is reactive. Which of the following is the most appropriate next step in management?
Deliver the baby immediately
Perform contraction stress test
Give vibroacoustic stimulation
Biophysical profile
Repeat non-stress test weekly
A 31 -year-old man is brought to the emergency department after a motor vehicle accident. He sustained a severe head injury and, on arrival to the emergency department, has a Glasgow coma score of 8. His blood pressure is stable, and an urgent CT scan of the head reveals a large subdural bleed with evidence of a midline shift and cerebellar tonsillar compression. The patient is breathing spontaneously without any respiratory assistance and is not intubated. Which of the following is the most appropriate next step in management?
Initiate immediate surgical decompression
Perform endotracheal intubation and hyperventilation
Induce a barbiturate coma
Obtain an urgent head MRI to evaluate for herniation
Administer IV mannitol
A 31-year-old African American man presents with dyspnea on exertion. He also has fever and red tender rash on his shins. Physical examination reveals fine inspiratory crackles in both lower lung lobes and tender erythematous nodules on his legs. CXR shows bilateral hilar adenopathy and reticulonodular changes in both lungs. Transbronchial biopsy reveals noncaseating granulomas. Which of the following is the most appropriate next step in management?
Aspirin
Nitrogen mustard
No therapy
Steroids
Isoniazid (INH) and streptomycin
A 31-year-old African-American woman is diagnosed with uterine fibroids. Which of the following types of fibroids is most likely to interfere with conception and pregnancy?
Intracavitary
Pedunculated
Submucosal
Subserosal
Intramural
A 31-year-old Caucasian male complains of joint pains. He describes right knee pain, right heel pain and lowback pain. He was recently treated for urethral discharge at an outside clinic. He has no history of trauma or illicit drug use. He is afebrile, and his vital signs are stable. His right knee is swollen, tender and warm to touch; tenderness is also present over the Achilles tendon. Oral examination shows mouth ulcers. Synovial fluid analysis from the right knee shows a white blood cell count of 10,000/mm3 with many polymorphonuclear leukocytes but a negative Gram stain. Which of the following is the most appropriate initial pharmacotherapy for this patient?
Colchicine
Antihistamines
NSAIDs
Antibiotics
Allopurinol
A 31-year-old G3P2 woman at 37 weeks’ gestation presents to the labor and delivery floor after 2 hours of contractions of increasing frequency and intensity. An epidural anesthetic is requested on admission and placed. The patient continues to have contractions for the next 15 hours, during which time her membranes rupture spontaneously. Vaginal examination at that time reveals a cervix that is soft, 3 cm dilated, in an anterior position, and 80% effaced. The fetal head is at the -1 station. Fetal heart tracings reveal a baseline heart rate of 156/min, with variable accelerations and no significant decelerations. Which of the following is the best next step in management?
Proceed to cesarean section
Begin an infusion of oxytocin
Attempt forceps-facilitated delivery
Apply intravaginal prostaglandin E2
Increase the rate of intravenous fluids to hydrate the patient
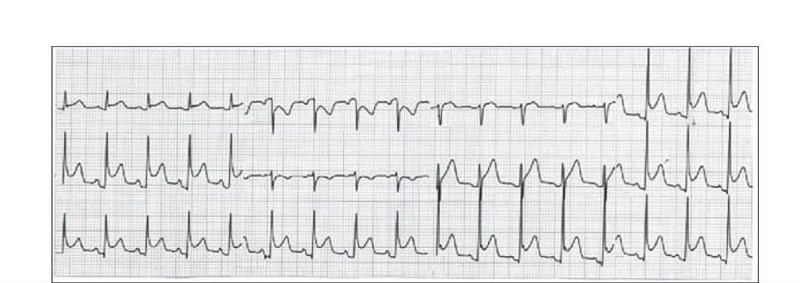
A 31-year-old kindergarten teacher presents to the ED complaining of acute-onset substernal chest pain that is sharp in nature and radiates to her back. The pain is worse when she is lying down on the stretcher and improves when she sits up. She smokes cigarettes occasionally and was told she has borderline diabetes. She denies any recent surgeries or long travel. Her BP is 145/85 mmHg, HR is 99 beats per minute, RR is 18 breaths per minute, and temperature is 100.6°F. Examination of her chest reveals clear lungs and a friction rub. Her abdomen is soft and nontender to palpation. Her legs are not swollen. Chest radiography and echocardiography are unremarkable. Her ECG is shown below. Which of the following is the most appropriate next step in management?
Anticoagulate and CT scan to evaluate for a PE
Prescribe antibiotics and discharge the patient
Administer thrombolytics if the pain persists
Aspirin, heparin, clopidogrel, and admit for ACS
Prescribe a NSAID and discharge the patient
A 31-year-old male immigrant from India is found on a routine physical examination to have a single, 2-cm nodule in the right lobe of his thyroid gland. The mass is firm, moves up and down with swallowing, and is not tender. The skin of his face and neck is pitted with multiple scars, which suggest smallpox; however, he explains that the scars are due to very severe acne that he had as a youngster, for which he eventually received external beam radiation therapy at the age of 14. His thyroid fun
No further care is needed
Thyroid lobectomy
FNA should be repeated until it can be read as benign or malignant
Thyroid scan and sonogram are needed
Thyroid function tests should be repeated yearly
A 31-year-old man from Florida presents to the ED complaining of severe pain that starts in his left flank and radiates to his testicle. The pain lasts for about 1 hour and then improves. He had similar pain last week that resolved spontaneously. He noted some blood in his urine this morning. His BP is 145/75 mm Hg, HR is 90 beats per minute, temperature is 98.9°F, and his RR is 24 breaths per minute. His abdomen is soft and nontender. As you examine the patient, he vomits and has trouble lying still in his stretcher. Which of the following is the most appropriate next step in management?
Start intravenous (IV) fluids and administer an IV nonsteroidal anti-inflammatory drug (NSAID) and antiemetic
Call surgery consult to evaluate the patient for appendicitis
Perform an ultrasound to evaluate for testicular torsion
Perform an ultrasound to evaluate for an abdominal aortic aneurysm (AAA)
Order an abdominal CT
A 31-year-old man is brought to the ER following an automobile accident in which his chest struck the steering wheel. Examination reveals stable vital signs and no evidence of respiratory distress, but the patient exhibits multiple palpable rib fractures and paradoxical movement of the right side of the chest. Chest x-ray shows no evidence of pneumothorax or hemothorax. Which of the following is the most appropriate initial management of this patient?
Pain control, chest physiotherapy, and close observation
Stabilization with towel clips
Immediate operative stabilization
Stabilization of the chest wall with sandbags
Intubation, mechanical ventilation, and positive end-expiratory pressure
A 31-year-old man who works for a moving company presents to the ED because he thinks he was having a heart attack. He does not smoke, and jogs 3 days a week. His father died of a heart attack in his sixties. He describes a gradual onset of chest pain that is worse with activity and resolves when he is at rest. His HR is 68 beats per minute, BP is 120/70 mmHg, and RR is 14 breaths per minute. On examination, his lungs are clear and there is no cardiac murmur. You palpate tenderness over the left sternal border at the third and fourth ribs. An ECG reveals sinus rhythm at a rate of 65. A chest radiograph shows no infiltrates or pneumothorax. Which of the following is the most appropriate next step in management?
Administer ibuprofen and reassure the patient that he is not having a heart attack
Administer aspirin, clopidogrel, and heparin, and admit for acute coronary syndrome (ACS)
Observe the patient for 6 hours
Inject corticosteroid into the costochondral joint to reduce inflammation
Administer aspirin and send for a troponin
A 31-year-old woman comes to the physician for follow-up after an abnormal Pap test and cervical biopsy. The patient's Pap test showed a high-grade squamous intraepithelial lesion (HGSIL). This was followed by colposcopy and biopsy of the cervix. The biopsy specimen also demonstrated HGSIL. The patient was counseled to undergo a loop electrosurgical excision procedure (LEEP). Which of the following represents the potential long-term complications from this procedure?
Urinary incontinence and urinary retention
Hernia and intraperitoneal adhesions
Cervical incompetence and cervical stenosis
Constipation and fecal incontinence
Abscess and chronic pelvic inflammatory disease
A 31-year-old woman comes to your office seeking advice about birth control. She had her third child 3 months ago and does not wish to get pregnant in the near future. Her medical history is significant for HIV infection with a CD4 count of 500 cells/mm3 and a viral load of 2000 copies/mL. She also has migraine headaches with an aura that she has had since the age of 14 years. She has never had surgery. She takes no medications and has no known drug allergies. She has a family history significant for breast, endometrial, and ovarian cancers. Her physical examination, including breast and pelvic examination, is normal. Which of the following conditions represents a contraindication to the combined oral contraceptive pill for this patient?
Human immunodeficiency virus infection
Family history of endometrial cancer
Family history of ovarian cancer
Migraine with aura
Family history of breast cancer
A 31-year-old woman smashes her car against a bridge abutment. She sustains multiple injuries, including upper and lower extremity fractures. She is fully awake and alert, and she reports that she was not wearing a seat belt and distinctly remembers hitting her abdomen against the steering wheel. Her blood pressure is 135/75 mm Hg, and her pulse is 88/min. Physical examination shows that she has a rigid, tender abdomen, with guarding and rebound in all four quadrants. She has no bowel sounds. Which of the following would be the most appropriate step in evaluating potential intra-abdominal injuries?
Sonogram of the abdomen
Exploratory laparotomy
Diagnostic peritoneal lavage
Continued clinical observation
CT scan of the abdomen
A 31-year-old woman, gravida 1, para 0, at 36-weeks' gestation with twins comes to the physician for a prenatal visit. The patient has had no contractions, bleeding from the vagina, or loss of fluid, and the babies are moving well. An ultrasound that was performed today shows that the presenting fetus is vertex and the non-presenting fetus is breech. Both fetuses are appropriately grown and greater than 2000 g. The patient wants to know if she should have a vaginal or cesarean delivery. Which of the following is the proper counseling for this patient?
Vaginal delivery is mandated because the first twin is vertex
Vaginal delivery is mandated because the fetuses are > 2000g
Cesarean delivery is mandated because the second twin is breech
Cesarean delivery is mandated because the fetuses are > 2000g
Both vaginal delivery and cesarean delivery are acceptable
A 31-year-old, HIV-positive woman, gravida 3, para 2, at 32-weeks' gestation comes to the physician for a prenatal visit. Her prenatal course is significant for the fact that she has taken zidovudine throughout the pregnancy. Otherwise, her prenatal course has been unremarkable. She has no history of mental illness. She states that she has been weighing the benefits and risks of cesarean delivery in preventing transmission of the virus to her baby. After much deliberation, she has decided that she does not want a cesarean delivery and would like to attempt a vaginal delivery. Which of the following is the most appropriate next step in management?
Contact the hospital lawyers to get a court order for cesarean delivery
Contact psychiatry to evaluate the patient
Respect the patient's decision and perform the vaginal delivery
Perform cesarean delivery once the patient is in labor
Perform cesarean delivery at 38 weeks
A 32-year-old alcoholic man, recently emigrated from Mexico, presents with right upper quadrant pain and fevers for 2 weeks. CT scan of the abdomen demonstrates a non–rim-enhancing fluid collection in the periphery of the right lobe of the liver. The patient’s serology is positive for antibodies to Entamoeba histolytica. Which of the following is the best initial management option for this patient?
Surgical drainage of the fluid collection
Liver resection
Marsupialization of the fluid collection
Treatment with antiamebic drugs
Percutaneous drainage of the fluid collection
A 32-year-old alcoholic with end-stage liver disease has been admitted to the hospital 3 times for bleeding esophageal varices. He has undergone banding and sclerotherapy previously. He admits to currently drinking 6 packs of beer per day. On his abdominal examination, he has a fluid wave. Which of the following is the best option for long-term management of this patient’s esophageal varices?
Transjugular intrahepatic portosystemic shunt (TIPS)
Distal splenorenal shunt
End-to-side portocaval shunt
Transection and reanastomosis of the distal esophagus
Orthotopic liver transplantation
A 32-year-old anxious-appearing male is wheeled into the emergency room with the sudden onset of excruciating left-sided chest pain. His temperature is 37.2°C (99°F), blood pressure is 160/88 mmHg, pulse is 125/min, regular and respirations are 20/min. Physical examination is normal, except for multiple venous track marks on his extremities and atrophic nasal mucosa. An EKG is done which shows ST depression and T wave inversion in leads V1-V6. Cardiac enzymes including CK-MB and Troponin Tare not elevated. Which of the following is the most appropriate next step in the management of this patient?
Administer metoprolol
Intravenous diazepam
Close observation
Administer thrombolytics
Cardiac catheterization
A 32-year-old Caucasian female presents to your office for a routine check-up. Her past medical history is significant for generalized seizures controlled with chronic phenytoin therapy. The last seizure was six months ago. She does not smoke or consume alcohol. Physical examination is insignificant, except mild pallor. Laboratory values are: Hb 10.8 g/dL, MCV 105 fl, Platelet count 180,000/cmm, Leukocyte count 7,500/cmm, Segmented neutrophils 68%, Bands 1%, Eosinophils 1%, Lymphocytes 24%, Monocytes 6%. Which of the following supplementations could have prevented this patient's anemia?
Folic acid
Iron
Vitamin B6
Vitamin B1
Vitamin B12
A 32-year-old Caucasian male comes to the emergency department due to progressive ascending paralysis, which began 18 hours ago. He initially noticed paresthesias in his lower limbs, followed by a sense of fatigue and weakness. He denies any history of headache, fever, and recent infection or illness. His blood pressure is 120/80 mm Hg, pulse is 80/min, respirations are 16/min, and temperature is 37.3°C (99.2°F). The physical examination reveals intact cranial nerves, absent deep tendon reflexes, and a normal sensory exam. Laboratory studies reveal a normal WBC count. No abnormalities are noted on CSF examination. While evaluating the patient in the hospital, he quickly deteriorates. What is the most appropriate next step in the management of this patient?
IV methylprednisolone
IV immunoglobulin and plasmapheresis
Administer botulinum antitoxin
Meticulous search for a tick
MRI of the spine
A 32-year-old Caucasian male is admitted to the hospital due to a 1-week history of progressive paralysis of his upper and lower extremities. He had a flu-like illness 3 weeks ago, followed by paresthesias in his fingertips and toes. The weakness initially started in his lower extremities. He denies any changes in bowel and bladder fun
Intravenous methyl prednisolone
Intravenous ceftriaxone and ampicillin
Botulinum antitoxin
Intravenous acyclovir therapy
Intravenous immunoglobulin therapy
A 32-year-old female is crying as she approaches the office. She has had severe, unbearable pain in her face for the past five days. She describes the pain as knife-like, comes in paroxysms, occurs 10-20 times a day, and lasts a few seconds. She does not know what precipitates the attacks, but she has been unable to sleep, eat or go to work because of her symptoms. She has tried numerous pain medications, but nothing seems to relieve the pain. She denies any history of trauma, medication use or recent surgery. Vital signs are within normal limits. Physical examination is within normal limits. Which of the following agents will best benefit this patient?
Levodopa
Carbamazepine
Lithium
Morphine
Methotrexate
A 32-year-old female presents for her yearly examination. She has been smoking one pack of cigarettes a day for the past 12 years. She wants to stop, and you make some recommendations to her. Which of the following is true regarding smoking cessation in women?
Nicotine replacement in the form of chewing gum or transdermal patches has not been shown to be effective in smoking cessation programs
No matter how long has been smoking, smoking cessation appears to improve the health of the lungs
Stopping cold turkey is the only way to successfully achieve smoking cessation
Smokers do not benefit from repeated warnings from their doctor to stop smoking
Ninety percent of those who stop smoking relapse within 3 months
A 32-year-old G2P0101 presents to labor and delivery at 34 weeks of gestation, complaining of regular uterine contractions about every 5 minutes for the past several hours. She has also noticed the passage of a clear fluid per vagina. A nurse places the patient on an external fetal monitor and calls you to evaluate her status. The external fetal monitor demonstrates a reactive fetal heart rate tracing, with regular uterine contractions occurring about every 3 to 4 minutes. On sterile speculum examination, the cervix is visually closed. A sample of pooled amniotic fluid seen in the vaginal vault is fern and nitrazine-positive. The patient has a temperature of 38.8C, pulse 102 beats per minute, blood pressure 100/60 mm Hg, and her fundus is tender to deep palpation. Her admission blood work comes back indicating a WBC of 19,000. The patient is very concerned because she had previously delivered a baby at 35 weeks who suffered from respiratory distress syndrome (RDS). You perform a bedside sonogram, which indicates oligohydramnios and a fetus whose size is appropriate for gestational age and with a cephalic presentation. Which of the following is the most appropriate next step in the management of this patient?
Perform emergent cesarean section
Administer betamethasone
Administer antibiotics
Place a cervical cerclage
Administer tocolytics
A 32-year-old G2P1 woman at 16 weeks gestation presents to her obstetrician complaining of fatigue, anxiety, and palpitations. She says she has been feeling warm, even in her air-conditioned home, and has been having three or four loose stools per day, as compared to one or two prior to her pregnancy. She has a temperature of 37.1°C (98.9°F), heart rate of 105/min, and blood pressure of 128/76 mmHg. Neck examination reveals mild diffuse enlargement of the thyroid gland with no lymphadenopathy. Relevant laboratory findings include a total triiodothyronine level of 400 ng/dL, free thyroxine of 6.8 ng/dL, and thyroid-stimulating hormone of 0.01 μU/mL (normal: 0.4–4 μU/L). Results of a thyroid- stimulating hormone-receptor antibody test are positive. Which of the following is the most appropriate therapy for this patient?
Methimazole
High-dose iodine therapy
Surgical resection
Propylthiouracil
Radioiodine ablation
A 32-year-old G2P1 woman at 35 weeks’ gestation presents to her obstetrician for a routine prenatal check-up. The mother has been previously diagnosed with mild preeclampsia, which the obstetrician has chosen to manage expectantly. During the visit, a biophysical profile is performed and the amniotic fluid index is found to be < 5 cm, indicating the development of oligohydramnios. The biophysical profile is otherwise normal, with a total score of 8/10 and reassuring fetal heart tracings. How should oligohydramnios be managed in this patient?
Emergent cesarean section
No change in management is necessary
Biweekly fetal biophysical profiles
Amnioinfusion with normal saline solution
Administration of betamethasone, then cesarean section in 24 hours
A 32-year-old G2P1001 at 20 weeks gestational age presents to the emergency room complaining of constipation and abdominal pain for the past 24 hours. The patient also admits to bouts of nausea and emesis since eating a very spicy meal at a new Thai restaurant the evening before. She denies a history of any medical problems. During her last pregnancy, the patient underwent an elective cesarean section at term to deliver a fetus in the breech presentation. The emergency room doctor who examines her pages you and reports that the patient has a low-grade fever of 37.7C (100F), with a normal pulse and blood pressure. She is minimally tender to deep palpation with hypoactive bowel sounds. She has no rebound tenderness. The patient has a WBC of 13,000, and electrolytes are normal. Which of the following is the most appropriate next step in the management of this patient?
The history and physical examination are consistent with constipation, which is commonly associated with pregnancy; the patient should be discharged with reassurance and instructions to give herself a soapsuds enema and follow a high-fiber diet with laxative use as needed
The patient should be prepped for the operating room immediately to have an emergent appendectomy
The patient should be reassured that her symptoms are a result of the spicy meal consumed the evening before and should be given Pepto-Bismol to alleviate the symptoms
Intravenous antiemetics should be ordered to treat the patient’s hyperemesis gravidarum
The patient should be sent to radiology for an upright abdominal x-ray
A 32-year-old G3P2 at 39 weeks gestation with an epidural has been pushing for 30 minutes with good descent. The presenting fetal head is left occiput anterior with less than 45 degree of rotation with a station of +3 of 5. The fetal heart rate has been in the 90s for the past 5 minutes and the delivery is expedited with forceps. Which of the following best describes the type of forceps delivery performed?
Outlet forceps
High forceps
Rotational forceps
Low forceps
Midforceps
A 32-year-old G3P2 woman at 35 weeks’ gestation has a past medical history significant for hypertension. She was well-controlled on hydrochlorothiazide and lisinopril as an outpatient, but these drugs were discontinued when she found out that she was pregnant. Her blood pressure has been relatively well controlled in the 120–130 mm Hg systolic range without medication, and urinalysis has consistently been negative for proteinuria at each of her prenatal visits. She presents now to the obstetric clinic with a blood pressure of 142/84 mmHg. A 24hour urine specimen yields 0.35 g of proteinuria. Which of the following is the most appropriate next step?
Restricted activity and close monitoring as an outpatient following initial inpatient evaluation
Start hydralazine
Prepare for emergent delivery
Restart the patient’s prepregnancy antihypertensive regimen
Administer oral furosemide
A 32-year-old G3P3 woman is postoperative day 5 after an emergent cesarean section due to fetal distress. The patient progressed rapidly through passive labor without incident, but after her membranes were ruptured manually, a fetal scalp probe was placed in the active phase secondary to several runs of mid-late decelerations. Cesarean section was ultimately performed after 2 hours of active labor secondary to fetal distress. The patient presents now with a fever to 38.7C (101.7F) and uterine tenderness. Laboratory tests reveal a WBC count of 14,000/mm3, with 70% neutrophils and 4% bands. Which of the following is the most appropriate treatment?
Cefotaxime and levofloxacin
Metronidazole and doxycycline
Clindamycin and gentamicin
Imipenem
Ampicillin and gentamicin
A 32-year-old G3P3 woman presents to her obstetrician for help conceiving. She states her menstrual cycles have not been regular since the birth of her third child 3 years ago. Furthermore, although she readily became pregnant with her other three children, she has failed to become pregnant despite trying over the past 2 years. She has no significant past medical history and takes only prenatal vitamins. Although she says she has not been ill lately, she reports feeling “tired and cold all the time.” She also reports she has had trouble sleeping over the past several months. Her physical examination is normal. Laboratory tests show: WBC count: 9000/mm3; Hemoglobin: 8.0 g/dL; Platelet count: 300,000/mm3; Hematocrit: 40%; Thyroid-stimulating hormone level: 0.5 μU/mL; Free thyroxine: 2.0 ng/dL; Luteinizing hormone: 0.5 mU/mL; Follicle-stimulating hormone: 0.5 mU/mL. Which of the following will this woman likely need to take to conceive?
Clomiphene
Progesterone
Propylthiouracil
Levothyroxine
Prednisone
A 32-year-old generally healthy woman presents to the office for a routine preemployment physical. She uses a vaginal ring for birth control. Her LMP was 2 weeks ago. She has been pregnant three times and has had two full-term births via normal spontaneous vaginal delivery. She had one spontaneous miscarriage at 10 weeks' gestation. She is only sexually active with her husband. She has a family history of breast cancer in her mother. Her mother had breast cancer at age 40 years and again at age 56 years. Her aunt also had breast cancer at an early age. Her last Pap smear, including human papillomavirus (HPV) was negative last year. BP, 120/80 mm Hg; P, 75 beats/min; R, 14 breaths/min; T, 98.4°F. Physical examination: Gen: Awake, alert, oriented x3, CVS: S1S2+ RRR no m/r/g, Lungs: Clear to auscultation bilaterally, Breast: No breast mass felt. What should be done as a part of the evaluation?
Gonorrhea screening
Mammography
Pap-smear
BRCA gene testing
Chlamydia screening
A 32-year-old Hispanic woman presents to the emergency department complaining of heavy vaginal bleeding. Her temperature is 37 C (98.6 F), blood pressure is 80/50 mm Hg, pulse is 110/min, and respirations are 18/min. Her abdomen is soft, non-tender and non-distended. Her pelvic examination reveals approximately 200 mL of clotted blood in the vagina, an open cervical os with tissue protruding from it, and a 10-week-sized, non-tender uterus. Leukocyte count is 9000/mm3, hematocrit is 22%, and platelet count is 275,000/mm3. Quantitative hCG is 100,000mIU/L (normal: 5-200,000mIU/L). Pelvic ultrasound shows echogenic material within the uterine cavity consistent with blood or tissue, no adnexal masses, and no free fluid. No viable pregnancy is seen. Which of the following is the most appropriate next step in management?
Culdocentesis
Discharge to home
Dilation and evacuation
Laparoscopy
Laparotomy
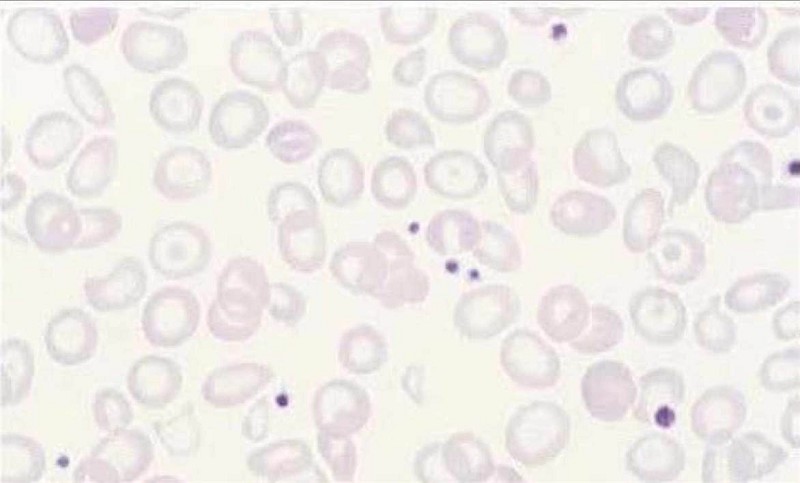
A 32-year-old Italian-American man presents to your office for a routine check-up. He works as a business executive and admits to being under a lot of stress recently. He drinks alcohol occasionally and smokes one pack of cigarettes per day. Laboratory analyses reveal: Hemoglobin 10.1 mg/dl, RBC count 4.0 x 10^12/L, MCV 70fl, WBC count 5,500/mm3, Platelets 170,000/mm3, Serum calcium 10.1 mg/dl, Serum potassium 4.5 meq/L, Serum sodium 135 meq/L. Serial fecal occult blood tests are negative. A peripheral blood smear reveals the following: Which of the following is the best treatment for this patient?
Iron
Reassurance
Erythropoietin
Folic acid
Cobalamin
A 32-year-old man from Arkansas presents to physician with a two-day history of fever, headache, malaise, and myalgias. His family says that he seems slightly confused. He recalls having a tick bite two weeks ago after walking through the woods. His temperature is 39°C (102°F), pulse is 90/min, and blood pressure is 125/80 mm Hg. Neck is supple and there is no lymphadenopathy noted. Oropharynx is clear. Chest auscultation is unremarkable. Abdomen is soft and non-tender. There is no rash evident. Neurologic examination is nonfocal. Laboratory testing shows: Complete blood count:Hemoglobin 14.0 g/L, MCV 88 fL, Platelets 78,000/mm3, Leukocyte count 2,500/mm3, Neutrophils 56%, Eosinophils 1%, Lymphocytes 33%, Monocytes 10%. Liver studies:Total protein, serum 6.5 g/dL, Total bilirubin 1.0 mg/dL, Direct bilirubin 0.8 mg/dL, Alkaline phosphatase 110 U/L, Aspartate aminotransferase (SGOT) 98 U/L, Alanine aminotransferase (SGPT) 105 U/L. What is the most appropriate next step in the management of this patient?
Doxycycline
Ceftriaxone
Hepatitis serology
Chloramphenicol
Erythromycin
A 32-year-old man presents to his primary care physician complaining of diffuse muscle weakness, dry and puffy skin, and patchy areas of hair loss on his scalp. He also notes numbness around his mouth and a tingling sensation in his hands and feet. He has a history of seizure disorder, and has been taking carbamazepine for the past 5 years. On physical examination he has dry skin and coarse, brittle hair with patchy alopecia. Tapping his right cheek causes contraction of the muscles at the corner of his mouth, nose, and eye on the right side. Which of the following could best have prevented the development of the patient’s current problem?
Parathyroidectomy
Vitamin D supplementation
Vitamin C supplementation
Thyroid hormone
Magnesium supplementation
A 32-year-old man presents to the emergency department with pain and swelling in the right leg. He was recently hospitalized for a right lower extremity deep venous thrombosis and discharged on warfarin. Today his INR is 1.12. Ultrasound reveals a right popliteal vein thrombosis extending into the deep femoral vein. What is the best initial management step for this patient?
Discontinue warfarin and reassure
Place inferior vena cava filter
Start intravenous unfractionated heparin
Initiate thrombolytic therapy
Increase warfarin dose for goal INR > 2.0
A 32-year-old man presents with an asymptomatic mass in his right testicle. On examination, the mass cannot be transilluminated. Ultrasound shows a solid mass in the right testicle. Which of the following is the most accurate method in obtaining a diagnosis of testicular cancer?
Excisional biopsy of the testicular mass through a scrotal incision
Radical inguinal orchiectomy
Incisional biopsy of the testicular mass through a scrotal incision
Percutaneous biopsy of the testicular mass
Serum levels of alpha-fetoprotein and beta human chorionic gonadotrophin
A 32-year-old man with a 3-year history of ulcerative colitis (UC) presents for discussion for surgical intervention. The patient is otherwise healthy and does not have evidence of rectal dysplasia. Which of the following is the most appropriate elective operation for this patient?
Total abdominal colectomy with end ileostomy and very low Hartmann
Total abdominal colectomy with ileal-rectal anastomosis
Total proctocolectomy with ileal pouch-anal anastomosis, anal mucosectomy, and diverting ileostomy
Total proctocolectomy with ileal pouch-anal anastomosis and diverting ileostomy
Total proctocolectomy with end ileostomy
A 32-year-old multiparous African-American woman comes for her initial prenatal visit at 14 weeks' gestation. She complains of the recent appearance of facial hair and acne. The beta-HCG level is consistent with gestational age. Examination shows hirsutism. Ultrasonogram shows an intrauterine gestation consistent with dates and bilateral solid nodular masses in both ovaries. Which of the following is the most appropriate next step in management?
Reassurance and follow-up with ultrasonogram
Ultrasound guided aspiration of the mass
Diagnostic laparoscopy
Suction evacuation of uterus
Exploratory laparotomy
A 32-year-old nulliparous woman at 38 weeks' gestation comes to the labor and delivery ward with regular painful contractions after a gush of fluid two hours ago. Her temperature is 98.6 F (37 C). She is found to have gross rupture of membranes and to have a cervix that is 6 centimeters dilated. The fetus is in breech position. The patient is then brought to the operating room for cesarean delivery. Which of the following represents the correct procedure for antibiotic administration?
Administer oral antibiotics for 1 week following the procedure
Administer intravenous antibiotics for 24 hours after the procedure
Administer intravenous antibiotics immediately after the procedure
Administer intravenous antibiotics after the cord is clamped
Administer intravenous antibiotics 30 minutes prior to the procedure
A 32-year-old white woman complains of abdominal pain off and on since the age of 17. She notices abdominal bloating relieved by defecation as well as alternating diarrhea and constipation. She has no weight loss, GI bleeding, or nocturnal diarrhea. On examination, she has slight LLQ tenderness and gaseous abdominal distension. Laboratory studies, including CBC, are normal. Which of the following is the most appropriate initial approach?
Order small bowel biopsy
Order UGI series with small bowel follow-through
Obtain antiendomysial antibodies
Refer to gastroenterologist for colonoscopy
Recommend increased dietary fiber, antispasmodics as needed, and follow-up examination in 2 months
A 32-year-old woman comes to the hospital for an elective repeat cesarean delivery. Four years ago she had a primary cesarean delivery for a nonreassuring fetal heart rate tracing. Two years ago she chose to have an elective repeat cesarean delivery rather than attempt a vaginal birth after cesarean (VBAC). Her prenatal course was uncomplicated except that she has mitral valve prolapse. An echocardiograph demonstrated the mitral valve prolapse, but no other structural cardiac disease. Which of the following is the correct management of this patient?
Administer oral antibiotics 6 hours after the procedure
No antibiotics are needed
Administer intravenous antibiotics for 24 hours after the procedure
Administer intravenous antibiotics immediately after the procedure
Administer intravenous antibiotics 30 minutes prior to the procedure
A 32-year-old woman comes to the physician because of amenorrhea. She had menarche at age 13 and has had normal periods since then. However, her last menstrual period was 8 months ago. She also complains of an occasional milky nipple discharge. She has no medical problems and takes no medications. She is particularly concerned because she would like to become pregnant as soon as possible. Examination shows a whitish nipple discharge bilaterally, but the rest of the examination is unremarkable. Urine human chorionic gonadotropin (hCG) is negative. Thyroid stimulating hormone (TSH) is normal. Prolactin is elevated. Head MRI scan is unremarkable. Which of the following is the most appropriate pharmacotherapy?
Bromocriptine
Oral contraceptive pill (OCP)
Thyroxine
Dicloxacillin
Magnesium sulfate
A 32-year-old woman comes to the physician because of recurrent painful outbreaks on her labia and vagina. Her first outbreak was six years ago. At that time she developed what she thought was a bad "flu" with malaise and a fever, along with a painful rash on her labia. This initial outbreak resolved, but since then she has had approximately 8 -10 outbreaks each year. Each outbreak is preceded by burning in her perineal area. A few days later she develops vesicles, then shallow, painful ulcers that resolve in about 10 days. Which of the following is the most appropriate pharmacotherapy?
Daily oral estrogen
Daily oral penicillin
Daily oral ferrous sulfate
Daily topical estrogen
Daily oral acyclovir
A 32-year-old woman comes to your office for re-evaluation of her birth control method. She wants her intrauterine device (IUD) removed because it is causing her pelvic pain. She wants to be placed on oral contraceptive pills (OCPs). She has had hypertension for the past five years controlled with hydrochlorothiazide and atenolol. She has a family history of diabetes mellitus and ovarian carcinoma. Her body mass index (BMI) is 34 kg/m2. Physical examination is unremarkable. If she starts taking oral contraceptive pills, which of the following statement is most correct?
She will develop benign breast disease
She is at risk of endometrial cancer
Her hypertension may worsen
She will become diabetic
She is at risk of ovarian cancer
A 32-year-old woman has a CXR screening, and a 1.5-cm mass is noted in the right lower lobe. She is a nonsmoker. Bronchoscopy shows a mass in the right lower lobe orifice, covered with mucosa. Biopsy indicates this is compatible with a carcinoid tumor. Imaging suggests ipsilateral mediastinal lymph node involvement but no extrathoracic disease. Which of the following is the most appropriate treatment plan?
Chemoradiation
Neoadjuvant chemoradiation followed by right lower lobectomy and mediastinal lymph node dissection
Neoadjuvant chemotherapy followed by right lower lobectomy and mediastinal lymph node dissection
Right lower lobectomy and mediastinal lymph node dissection followed by adjuvant chemotherapy
Right lower lobectomy and mediastinal lymph node dissection
A 32-year-old woman in the 2nd month of pregnancy is found to have a 5-cm mass in the upper outer quadrant of her left breast. Mammogram shows no other lesions, and core biopsy reveals infiltrating ductal carcinoma. Which of the following would be the best course of action at this time?
Immediate therapeutic abortion and palliative breast surgery
Modified radical mastectomy now, deferring systemic therapy until later
Lumpectomy and axillary sampling, followed in 6 weeks by radiotherapy
Radiation therapy now, deferring surgery until after delivery
Chemotherapy now, deferring surgery until after delivery
A 32-year-old woman presents to the emergency department for left lower quadrant abdominal pain for thepast2 days. The patient states the pain is 8 of10 on the pain scale, non-radiating, and started off intermittent. The pain is now constant. She denies vomiting, diarrhea, and constipation but has nausea intermittently. Her last menstrual period was around 3 or 4 weeks ago. She has one sexual partner, and they have been trying to get pregnant. BP, 140/90 mm Hg; P, 90 beats/min; R, 15 breaths/min; T, 98.4°F. Review of system: Negative except for above. PE: Abd: Soft, tender in the left lower quadrant on palpation, + bowel sounds. Which of the following is the next step in the management of this patient?
Complete blood count (CBC)
Transvaginal ultrasonography (US)
MRI
Computed tomography (CT) scan of the abdomen and pelvis
Beta-human chorionic gonadotropin (BHCG)
A 32-year-old woman presents to your office for her well-woman examination. She is also worried because she has not been able to achieve orgasm with her new partner, with whom she has had a relationship for the past 3 months. She had three prior sexual partners and achieved orgasm with them. She is taking a combined oral contraceptive pill for birth control and an antihypertensive medication for chronic hypertension. She has also been on fluoxetine for depression for the past 2 years. She smokes one pack per day and drinks one drink per week. She had a cervical cone biopsy for severe cervical dysplasia 6 months ago. Which of the following is the most likely cause of her sexual dysfun
Clonidine
Fluoxetine
Nicotine
Disruption of cervical nerve pathways
Contraceptive pill
A 32-year-old woman presents to your office with dysuria, urinary frequency, and urinary urgency for 24 hours. She is healthy but is allergic to sulfa drugs. Urinalysis shows large blood, leukocytes, and nitrites in her urine. Which of the following medications is the best to treat this patient’s condition?
Dicloxacillin
Nitrofurantoin
Azithromycin
Flagyl
Bactrim
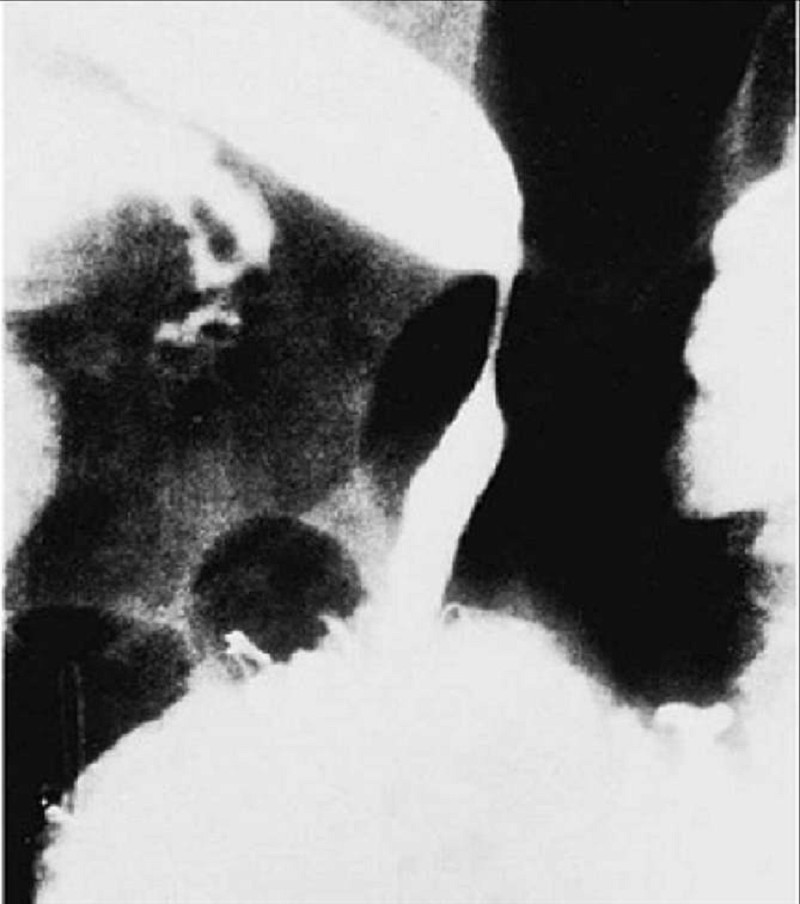
A 32-year-old woman undergoes a cholecystectomy for acute cholecystitis and is discharged home on the sixth postoperative day. She returns to the clinic 8 months after the operation for a routine visit and is noted by the surgeon to be jaundiced. Laboratory values on readmission show total bilirubin 5.6 mg/dL, direct bilirubin 4.8 mg/dL, alkaline phosphatase 250 IU (normal 21-91 IU), serum glutamic oxaloacetic transaminase (SGOT) 52 kU (normal 10-40 kU), and serum glutamic pyruvic transaminase (SGPT) 51 kU (normal 10-40 kU). An ultrasonogram shows dilated intrahepatic ducts. The patient undergoes the transhepatic cholangiogram seen here. Which of the following is the most appropriate next management step?
Roux-en-Y hepatico-jejunostomy
Choledochoduodenostomy
Percutaneous transhepatic dilatation
End-to-end choledochocholedochal anastomosis
Choledochoplasty with insertion of a T tube
A 32-year-old woman undergoes an uncomplicated appendectomy for acute appendicitis. The pathology report notes the presence of a 1-cm carcinoid tumor in the tip of the appendix. Which of the following is the most appropriate management of this patient?
Right hemicolectomy and chemotherapy
No further treatment
Radiation only
Chemotherapy only
Right hemicolectomy
A 32-year-old woman who is 40 weeks pregnant comes to the maternity unit in active labor. She states that she has painful genital blisters and ulcers, which she has experienced intermittently in the past. Pelvic examination reveals exquisitely tender vesicles and ulcers on her labia and vagina consistent with an active genital herpes infection. She is advised by the obstetrician that she should undergo a primary cesarean section delivery because of the increased risk of fetal infection via passage through an infected birth canal. She is mentally competent and tells the obstetrician that she refuses to have a cesarean section because her mother died during a surgical procedure. Although the doctor explains the risks of a vaginal delivery, she still refuses. The obstetrician should do which of the following?
Refer her to another physician
Obtain the consent of the husband to perform the cesarean delivery
Perform the cesarean section without her consent
Obtain a court order to perform the cesarean delivery
Allow a vaginal delivery
A 32-year-old woman who is one week postpartum presents with dull pain in her left leg for the past three days. She denies any history of trauma, fever or chills. Her pregnancy and delivery were uncomplicated, and her past medical history is unremarkable. She does not use tobacco, alcohol or illicit drugs. Her temperature is 37.2C (98.9 F) and blood pressure is 120/76 mm Hg. Physical examination reveals a swollen, tender, and mildly erythematous left leg. Doppler ultrasonogram reveals a thrombus in the superficial part of the femoral vein of the left leg. Which of the following is the most appropriate next step in management?
Inferior vena cava filter
Antistaphylococcal antibiotics
Thrombolytic therapy
Reassurance and ibuprofen
Anticoagulation with heparin
A 32-year-old woman with a history of diabetes presents with an IUP at 5 weeks. She has been taking metformin, glyburide, and lisinopril. Her glucose has been well controlled on these medications. Vital sign: BP, 120/80 mm Hg; P, 75 beats/min; R, 12 breaths/min; T, 98°F (37 C). She denies leakage of fluid, denies contractions, denies fetal movement, denies vaginal bleeding, and denies abdominal pain. What is the next best step in the management?
Stop both metformin and glyburide and start rosiglitazone
Stop both metformin and glyburide and change to acarbose
Continue both metformin and glyburide
Continue metformin but discontinue glyburide
Switch the patient to insulin
A 32-year-old woman, gravida 1, para 0, with a history of infertility, underwent ovulation induction resulting in a twin pregnancy, now at 31 weeks’ gestation. An early obstetric sonogram at 7 weeks’ gestation showed dichorionic placentation. She has a positive group B –hemolytic streptococcus vaginal culture. Because of epigastric pain, vaginal bleeding, and uterine contractions, she is evaluated at the maternity unit. An obstetric sonogram shows twin A to be a female fetus in breech presentation and twin B to be a male fetus in transverse lie with the back down. The sonogram also shows a marginal anterior placenta previa. Her initial vital signs are as follows: temperature, 37.2C (99.0F); pulse, 95/min; respiration, 18/min; blood pressure, 165/115 mm Hg. Her urine dipstick test shows 2 glucose and 3 albumin. Which of the following is a contraindication to tocolysis in this case?
Positive group B -hemolytic streptococcus vaginal culture
Multiple gestation
Early gestational age
Severe preeclampsia
Marginal placenta previa
A 32-year-old woman, gravida 2, para 2, comes to the physician for follow-up of an abnormal Pap test. One month ago, her Pap test showed a high-grade squamous intraepithelial lesion (HGSIL). Colposcopy demonstrated acetowhite epithelium at 2 o'clock. A biopsy taken of this area demonstrated HGSIL. Endocervical curettage (ECC) was negative. The patient has no other medical problems, has never had cervical dysplasia, and takes no medications. Which of the following is the most appropriate next step in management?
Loop electrode excision procedure (LEEP)
Hysterectomy
Repeat colposcopy in 6 months
Repeat Pap test in 6 months
Repeat Pap test in 1 year
A 32-year-old woman, gravida 3, para 0, at 29 weeks' gestation comes to the physician for a prenatal visit. She has no complaints. She had a prophylactic cerclage placed at 12 weeks' gestation because of her history of two consecutive 20-week losses. These spontaneous abortions were both characterized by painless cervical dilation, with the membranes found bulging into the vagina on examination. Ultrasound now demonstrates her cervix to be long and closed with no evidence of funneling. Which of the following is the most appropriate time to remove the cerclage from this patient?
30-32 weeks
36-38 weeks
38-40 weeks
32-34 weeks
34-36 weeks
A 32-year-old woman, gravida 3, para 2, at 14 weeks' gestation comes to the physician for a prenatal visit. She has some mild nausea, but otherwise no complaints. She has no significant medical problems and has never had surgery. She takes no medications and has no known drug allergies. She is concerned for two reasons. First, the "flu season" is coming, and she seems to get sick every year. Second, a child at her son's daycare center recently broke out with welts and was sent home. Which of the following vaccinations should this patient most likely be given?
Varicella
Influenza
Measles
Mumps
Rubella
A 32-year-old woman, gravida 3, para 2, at 30 weeks gestation comes to the hospital because of new onset painful, regular uterine contractions that began 5 hours ago. Her pregnancy has been uncomplicated. Her second pregnancy was complicated by preterm labor at 28 weeks gestation. She has no discharge, leakage of fluid or bleeding from the vagina; she has no dysuria or urgency. Her temperature is 37.0C (98.7F), blood pressure is 125/70 mmHg, pulse is 80/min and respirations are 18/min. Pelvic examination shows a soft, partially effaced and posterior cervix dilated to 2cm. A Nitrazine test is negative. Nonstress test shows a reassuring fetal heart pattern and uterine contractions occurring every 7 minutes. Which of the following is the most appropriate next step in management?
Tocolysis
Cervical cerclage
Augment delivery
Reassure and discharge home
Amnioinfusion
A 32-year-old woman, gravida 4, para 3, at 39 weeks' gestation comes the labor and delivery ward with painful contractions. Her prenatal course was unremarkable. Examination shows that her cervix is 5 cm dilated, 100% effaced and the fetal heart rate is in the 130s and reactive. She is given meperidine for pain control. She progresses rapidly and less than 2 hours later she delivers a 7-pound, 6-ounce (3,345g) male fetus. The one-minute APGAR score is 1 and the infant is making little respiratory effort. Which of the following is the most appropriate next step in management?
Blood transfusion
Penicillin
Sodium bicarbonate
Glucose
Naloxone
A 32-year-old women presents to the emergency room complaining of severe lower abdominal pain. She says she was diagnosed with pelvic inflammatory disease by her gynecologist last month, but did not take the medicine that she was prescribed because it made her throw up. She has had fevers on and off for the past 2 weeks. In the emergency room, the patient has a temperature of 38.3C (101F). Her abdomen is diffusely tender, but more so in the lower quadrants. She has diminished bowel sounds. On bimanual pelvic examination, bilateral adnexal masses are palpated. The patient is sent to the ultrasound department, and a transvaginal pelvic ultrasound demonstrates bilateral tubo-ovarian abscesses. Which of the following is the most appropriate next step in the management of this patient?
Admit the patient for exploratory laparotomy, TAH/BSO
Admit the patient for intravenous antibiotic therapy
Send the patient home and arrange for intravenous antibiotics to be administered by a home health agency
Call interventional radiology to perform CT-guided percutaneous drainage of the abscesses
Admit the patient for emergent laparoscopic drainage of the abscesses
A 32-year-old, gravida 3, para 2 woman at 35 weeks gestation comes to the hospital because of regular and painful uterine contractions occurring every 5 - 6 minutes. She also has continuous leakage of clear fluid from her vagina that started 10 hours earlier. She has chronic hypertension and was prescribed methyldopa throughout pregnancy but has been noncompliant. She also has a history of drug abuse and has missed two previous antenatal appointments. Her temperature is 37.0C (98.7F), blood pressure is 160/100 mmHg, pulse is 80/min and respirations are 16/min. Sterile speculum examination shows pooling of amniotic fluid in the vagina; the cervix is 80% effaced and 3cm dilated. Ultrasound shows a small for gestational age fetus in the vertex presentation with a decreased amniotic fluid index. Fetal heart monitoring shows repetitive late decelerations. Uterine contractions are now occurring every 4 minutes. Which of the following is the most appropriate next step in management?
Cesarean section
Expectant management
Betamethasone IM
Augmentation of labor
Tocolysis
A 32-year-old, HIV-positive, primigravid woman comes to the physician for a prenatal visit at 30 weeks. Her prenatal course has been notable for her use of zidovudine (ZDV) during the pregnancy. Her viral load has remained greater than 1000 copies per milliliter of plasma throughout the pregnancy. She has no other medical problems and has never had surgery. Examination is appropriate for a 30-week gestation. She wishes to do everything possible to prevent the transmission of HIV to her baby. Which of the following is the most appropriate next step in management?
Recommend forceps-assisted vaginal delivery
Recommend vaginal delivery
Offer elective cesarean section at 34 weeks
Offer elective cesarean section at 38 weeks
Offer elective cesarean section after amniocentesis to determine lung maturity
A 32-year-old, previously healthy man is a victim of a drive-by shooting, sustaining a gunshot wound to the left lower extremity. The entrance wound is located over the medial aspect of the calf, with an exit wound over the anterior pretibial region. Neurovascular examination of the extremity is normal. There is associated soft-tissue injury from the blast effect and a severely comminuted tibial fracture demonstrated on radiographs. Appropriate management of this injury includes which of the following?
Local wound irrigation, closure of the soft-tissue defect, closed reduction, and immobilization in a long-leg cast
Local wound irrigation with antibiotic solution, closed reduction, and immobilization in a long-leg cast, with continued local wound care through an anterior cast window
Tetanus prophylaxis, intravenous (IV) antibiotics, and operative wound irrigation and debridement, with application of an external fixation device
Tetanus prophylaxis, IV antibiotics, operative wound irrigation with closure of the soft-tissue defect, closed reduction, and immobilization in a long-leg cast
Tetanus prophylaxis, IV antibiotics, long leg splint for immobilization, and operative intervention during elective surgical schedule
A 33-year-old businessman with an unremarkable past medical history presents to you complaining of fatigue and some weight loss over the past three months. He awakens at 4:00 am each morning and is unable to fall back asleep. He also mentions that he used to enjoy playing golf twice per week, but now has little interest. Although he used to excel at work, he now finds himself losing interest and "spacing out" at times. He denies considering suicide. His TSH is normal. He is diagnosed with major depression and prescribed fluoxetine, and is asked to return for a follow-up appointment in two weeks. At the return visit, he states that his symptoms have not worsened, but have not improved either. He says, "I don't feel like the medication is doing anything." What is the most appropriate next step in the management of this patient's condition?
Continue fluoxetine and add amitriptyline
Discontinue fluoxetine and begin amitriptyline
Discontinue fluoxetine and begin sertraline
Increase the dose of fluoxetine
Continue with fluoxetine at the same dose
A 33-year-old computer programmer was diagnosed with ulcerative colitis last year. He had a colonoscopy and biopsy that showed pancolitis, after which no further work-up was done. This is his first visit to a physician in 6 months. He takes aminosalicylates and is in remission, without any symptoms. He is a member of the Ulcerative Colitis Support Group, which recently sent him a letter that said he should be screened for colon cancer. His vital signs are stable. Physical examination reveals mild tenderness on deep palpation of the lower abdomen. What is the best advice for him regarding his concerns?
He has an increased risk of colon cancer and he should have periodic colonoscopy eight years later
He has an increased risk of colon cancer and he should have colonoscopy every year
He has an increased risk of colon cancer and he should have prophylactic colectomy
Since he does not have any signs and symptoms, he has no increased risk and doesn't need any surveillance
He has an increased risk of colon cancer, and he should have a biopsy
A 33-year-old G1P1 woman presents to her gynecologist for a Pap smear. It has been several years since she last saw a physician. She is not currently sexually active, but takes oral contraceptives. Her vaginal examination is normal, but her Pap smear shows moderate-grade cervical intraepithelial neoplasia. The patient undergoes colposcopy and biopsies, which confirm the diagnosis. What is the most appropriate management of this patient?
Serial colposcopies every 3–4 months
Radiation therapy
Total abdominal hysterectomy
Loop electrosurgical excision procedure
Continued annual Pap smears
A 33-year-old male is admitted to the hospital after an episode of tonic-clonic seizures. He is a known IV drug abuser. He admits 'shooting' cocaine and heroin prior to the seizure. He has never had seizures before. Fallowing the seizure, he complains of muscle pain but otherwise feels normal. His temperature is 37.2°C (98.9°F) and his blood pressure is 156/90 mm Hg. Laboratory analyses reveal the following: CPK 11,200 U/ml, AST 545 U/L, ALT 560U/L, Troponin T normal, Anti-HAV antibodies negative, HBsAg negative, Anti-HBsAg negative, Anti-HCV antibodies positive. He reports that a recent HIV test was negative. Which of the following is the best management for this patient?
Fluid restrictio
No intervention
Life-long phenytoin therapy
Metoprolol
Hepatitis B vaccination
A 33-year-old man presents with a 1-day history of localized, small swelling along the margin of the upper eyelid. He feels pain, which does not seem to come from the conjunctival surface. He has a 10-pack year smoking history. He occasionally drinks alcohol. He is sexually active, and does not use condoms regularly. He is worried about the swelling. What is the best next step in the management of this patient?
Incision and drainage
Oral Penicillin
Take biopsy of the lesion
Incision and curettage
Use warm compresses
A 33-year-old pregnant woman notices a persistent, painless lump in the left breast. On examination the left breast has a single mobile mass without evidence of skin changes or lymphadenopathy in the neck or axilla. An ultrasound demonstrates a solid, 1-cm mass in the upper outer quadrant of the breast. A core-needle biopsy shows invasive ductal carcinoma. The patient is in her first trimester of pregnancy. Which of the following is the most appropriate management of this patient?
Termination of the pregnancy followed by modified radical mastectomy
Immediate administration of chemotherapy followed by modified radical mastectomy after delivery of the baby
Administration of radiation in the third trimester followed by modified radical mastectomy after delivery of the baby
Modified radical mastectomy
Total mastectomy with sentinel lymph node biopsy
A 33-year-old primigravid woman at 18 weeks' gestation comes to the physician for a prenatal visit. Her prenatal course has been uncomplicated thus far. She has no complaints. She has had no loss of fluid, bleeding, or contractions. She has hypothyroidism, for which she takes thyroid hormone replacement. The patient states that a friend of hers recently had a preterm delivery. The patient is quite concerned about preterm delivery and wants to know whether home uterine activity monitoring (HUAM) is recommended. Which of the following is the most appropriate response?
HUAM should be started at 35 weeks
HUAM should be started immediately
HUAM has not been proven to prevent preterm birth
HUAM has been proven to prevent preterm birth
HUAM has been proven to cause preterm birth
A 33-year-old white female complains of repeated episodes of fever, malaise, chills, breathlessness and dry cough over the past 6 months. She says that each episode starts suddenly and lasts for several days. She otherwise has no significant past medical history and does not take any medications. There is no family history of lung disorders. She does not smoke cigarettes or drink alcohol. She has never been abroad, and has had no sick contacts. She breeds budgerigars (a small Australian parrot) as a hobby. Chest x-ray shows diffuse generalized haziness in both lower lung fields. Pulmonary fun
Inhaled beclomethasone
Reassurance
Avoid exposure to birds
Inhaled cromolyn
Oral prednisolone
A 33-year-old woman at 10 weeks presents for her first prenatal examination. Routine labs are drawn and her hepatitis B surface antigen is positive. Liver fun
Provide immune globulin to the mother
Provide immune globulin and the hepatitis B vaccine to the neonate
Provide hepatitis B vaccine to the neonate
Provide hepatitis B vaccine to the mother
Perform a cesarean delivery at term
A 33-year-old woman comes to the clinic at 16 weeks’ gestation with no complaints. This is her second pregnancy. During the first pregnancy she delivered an 8.5 lb. infant. The patient reports hydramnios during that pregnancy. She has no prior medical history and is on no medications. On physical examination, she has a firm uterus. Which of the following is the appropriate management of this patient?
Maternal serum alpha-fetoprotein
Triple screen test
Pelvic Ultrasound
Genetic amniocentesis
Glucose testing
A 33-year-old woman comes to the physician because she has not had a menstrual period for 6 months. Prior to this she had a normal period every 29 days that lasted for 4 days. She has noted some weight gain in the past few months. She has a history of hepatitis A infection 6 years ago and had an appendectomy at age 12. She takes no medications and has no allergies to medications. Her father died of acute pancreatitis 3 years ago. Her mother is alive and well with no medical problems. Which of the following is the most appropriate next step in diagnosis?
Amylase
P-hCG
Liver function tests
TSH
FSH
A 33-year-old woman is 12 weeks pregnant with her third pregnancy. Her prior two pregnancies were uncomplicated and resulted in two normal spontaneous vaginal deliveries. It has been 7 years since her last delivery, and 4 years ago she was diagnosed with chronic hypertension. She was managed on an ACE-inhibitor but discontinued all medication when she started trying to conceive 6 months ago. She is doing well during the pregnancy except for some mild nausea and rare vomiting. Her physical examination is within normal limits for a woman at 12 weeks’ gestation. Her current blood pressure is 100/60 mmHg. At which of the following blood pressures should antihypertensive therapy be initiated in this patient?
120/80 mm Hg
100/60 mm Hg
110/70 mm Hg
140/90 mm Hg
150/111 mm Hg
A 33-year-old woman is found to have a palpable thyroid nodule during a routine medical checkup. A sonogram confirms the presence of a solid, 1.5-cm nodule in the right lobe of the thyroid gland. Fine needle aspirate cytology (FNA) is reported as "follicular tumor, otherwise unspecified." At surgery, a frozen section is read as follicular carcinoma. With the neck open, the surgeon can feel for enlarged jugular and peritracheal lymph nodes, and finds none. Which of the following is the most appropriate treatment?
Total thyroidectomy, radical neck dissection, and postoperative radioactive iodine
Total thyroidectomy plus postoperative radioactive iodine
Enucleation of the tumor
Total thyroidectomy
Right thyroid lobectomy
A 33-year-old woman is undergoing a diagnostic work-up because she appears to have Cushing syndrome. She has elevated levels of cortisol, which are not suppressed when she is given high-dose dexamethasone. ACTH levels are greater than 200 pg/ mL. A chest x-ray film shows a central, 3-cm round mass on the hilum of the right lung. Bronchoscopy and biopsies confirm a diagnosis of small cell carcinoma of the lung. Which of the following is the preferred treatment for this woman?
Trans-sphenoidal hypophysectomy and pulmonary lobectomy
Radiation and chemotherapy directed at the lung cancer
Bilateral adrenalectomy
Pneumonectomy
General support only
A 33-year-old woman is very depressed about her recurrent pregnancy loss. She has had four pregnancies that all have ended in spontaneous abortion before 8 weeks. Her past medical history is otherwise unremarkable. She has never had surgery. She takes acetaminophen occasionally for headaches, but otherwise uses no medications and has no known drug allergies. Physical examination is normal. Laboratory evaluation demonstrates that she is positive for lupus anticoagulant and that she is positive for anticardiolipin IgG. These results are again positive 8 weeks later. Which of the following is the most appropriate management of this patient during her next pregnancy?
Paternal leukocyte immunization and intravenous immune globulin
Paternal leukocyte immunization
Daily heparin and low dose aspirin
Daily low dose aspirin
Daily heparin
A 33-year-old woman, gravida 1, para 0, comes for a routine prenatal visit. According to her history, she is at 18-weeks gestation. Her family history is significant for Down syndrome on her maternal side. She does not use tobacco, alcohol or drugs. Vital signs are normal, and physical examination is unremarkable. Initial laboratory studies show a decreased maternal serum alpha-fetoprotein (MSAFP). Which of the following is the most appropriate next step in management?
Amniocentesis
Urinary estradiol levels
Ultrasonogram
Cordocentesis
Chorionic villus sampling
A 34-year-old Caucasian female presents to the ER with a rash and pruritis. She says that she has had a sore throat for several days, and her friend gave her amoxicillin that turned out to be out dated. The rash developed about 30 minutes after she took the drug. Her blood pressure is 110/70 mmHg and heart rate is 80/min. Physical examination reveals wide spread urticaria and excoriations. Pharyngeal mucosa and tonsils are hyperemic, and tender lymph nodes are palpated in the submandibular area. Lungs are clear on auscultation. Which of the following is the best next step in the management of this patient?
Prescribe antihistamines
Administer adrenalin immediately
Prescribe steroids
Schedule for dialysis
Continue amoxicillin therapy with non-outdated drug
A 34-year-old Caucasian male presents to the office with a 4-week history of diarrhea. He just returned from a trip to South America, where he developed foul-smelling stools, abdominal cramps and bloating. A three-day course of ciprofloxacin did not relieve his symptoms. His vital signs are within normal limits. Physical examination shows no abnormalities. Which of the following is the most appropriate next step in management?
Prescribe another course of ciprofloxacin
Prescribe oral ampicillin
Obtain CT scan of the abdomen
Prescribe oral metronidazole
Schedule colonoscopy
A 34-year-old G1P0 woman at 29 weeks’ gestation presents to the emergency department complaining of 2 hours of vaginal bleeding. The bleeding recently stopped, but she was diagnosed earlier with placenta previa by ultrasound. She denies any abdominal pain, cramping, or contractions associated with the bleeding. Her temperature is 36.8C (98.2F), blood pressure is 118/72 mm Hg, pulse is 75/min, and respiratory rate is 13/min. She reports she is Rh positive, her hemoglobin is 11.1 g/dL, and coagulation tests, fibrinogen, and D-dimer levels are all normal. On examination her gravid abdomen is non-tender. Fetal heart monitoring is reassuring, with a heart rate of 155/min, variable accelerations, and no decelerations. Two large-bore peripheral intravenous lines are inserted and two units of blood are typed and crossed. What is the most appropriate next step in management?
Emergent cesarean section
Admit to the antenatal unit for bed rest and treatment with RhO(D) immune globulin
Admit to the antenatal unit for bed rest and blood transfusion
Admit to the antenatal unit for bed rest and betamethasone
Outpatient expectant management
A 34-year-old G1P1 with a history of pulmonary embolism presents to your office to discuss contraception. Her cycles are regular. She has a history of pelvic inflammatory disease last year, for which she was hospitalized. She has currently been sexually active with the same partner for the past year. She wants to use condoms and a spermicide. You counsel her on the risks and benefits. Which of the following statements is true regarding spermicides found in vaginal foams, creams, and suppositories?
These agents are associated with an increased incidence of congenital malformations
Effectiveness is higher in younger users
The active agent in these spermicides is levonorgestrel
Effectiveness is higher than that of the diaphragm
The active agent in these spermicides is nonoxynol-9
A 34-year-old G2P1 at 31 weeks gestation with a known placenta previa is admitted to the hospital for vaginal bleeding. The patient continues to bleed heavily and you observe persistent late decelerations on the fetal heart monitor with loss of variability in the baseline. Her blood pressure and pulse are normal. You explain to the patient that she needs to be delivered. The patient is delivered by cesarean section under general anesthesia. The baby and placenta are easily delivered, but the uterus is noted to be boggy and atonic despite intravenous infusion of Pitocin. Which of the following is contraindicated in this patient for the treatment of uterine atony?
Terbutaline administered intravenously
Prostaglandin E2 suppositories
Misoprostol (Cytotec) suppositories
Prostaglandin F2α (Hemabate) suppositories
Methylergonovine (Methergine) administered intramuscularly
A 34-year-old G2P1 at 31 weeks gestation with a known placenta previa presents to the hospital with vaginal bleeding. On assessment, she has normal vital signs and the fetal heart rate tracing is 140 beats per minute with accelerations and no decelerations. No uterine contractions are demonstrated on external tocometer. Heavy vaginal bleeding is noted. Which of the following is the best next step in the management of this patient?
Induce labor
Administer methylergonovine
Perform cesarean delivery
Admit and stabilize the patient
Administer intramuscular terbutaline
A 34-year-old G2P1001 with an IUP at 38 weeks' gestation presents to labor and delivery for contractions. The patient states that she has had gestational diabetes that was diet controlled throughout her pregnancy. She states that she has had routine prenatal care. Vital sign: BP, 125/88 mm Hg; P, 95 beats/min; R, 12 breaths/min; T, 98.6°F. Contractions: Present, Fetal movement: Present. Physical examination: Gen: Awake, alert, oriented x3, mild pain distress, CVS: S1S2+ RRR no m/r/g, Vaginal bleeding: Absent, Leakage offluid: Present, Lungs: CTA bilaterally, Abd: Gravid, contractions present, Ext: 1+ edema bilaterally. Cervical Examination: 7 cm, 100% effaced, -1 station. Fetal Heart Monitoring: Reassuring, good variability, accelerations are present, no decelerations. What is the next step in the management of this patient?
Complete blood count (CBC)
Finger stick
HgbAlC
Administer insulin drip
Administer Ampicillin
A 34-year-old male calls his primary care physician's office, requesting an urgent appointment to discuss a personal problem. The receptionist informs him that the physician is preparing to leave as it is near closing time, but that an appointment is available for early the next morning. The patient declines the offer of an appointment and hangs up. Fifteen minutes later, as the physician is locking the office up, the patient arrives and insists on being seen immediately. He breathlessly says that he has "some kind of red rash" on his penis, which has him very worried. He asks again to be examined now. What is the most appropriate response?
"Although I understand your concern, we should address the issue tomorrow since it is not an emergency."
"Didn't I already inform you that it is closing time?''
"Your rash can most certainly wait until tomorrow."
"All right, we should look at your rash now. Come inside."
"It is extremely inappropriate on your part to come here despite my request that you make an appointment."
A 34-year-old male is brought to the emergency department by the paramedics after a gun-shot injury. His temperature is 37C (98.8F), blood pressure is 110/60 mm Hg, pulse is 96/min and respirations are 18/min. Examination shows a gunshot entry wound in the left 6th intercostal space anteriorly just lateral to the mid-clavicular line, and an exit wound in left 7th intercostal space posteriorly. After completing the primary survey by attending to airway, breathing and circulation, which of the following is the most appropriate next step in management?
Pericardiocentesis
Do a thoracotomy
Do an exploratory laparotomy
Do a diagnostic peritoneal lavage
Place a chest tube
A 34-year-old male presents to his physician's office for a routine health maintenance examination. He has a five-year history of bronchial asthma for which he uses an albuterol inhaler. He says that he uses the inhaler an average of two times per week during the day. In addition, he states that his asthma symptoms wake him from sleep approximately 3-4 times per month. He does not use tobacco, alcohol or illicit drugs. His family history is significant for asthma in his grandfather. Physical examination is unremarkable. Which of the following is the most appropriate next step in his management?
Continue current medical regimen
Add inhaled corticosteroids
Add oral prednisone
Add oral theophylline
Add long-acting beta-2 agonist inhaler
A 34-year-old male presents with palpitations for the past 4 hours without associated chest pain, shortness of breath, fevers, or chills. His medical history is significant for Wolff-Parkinson-White syndrome for the past ten years and three prior episodes of supraventricular tachycardia. He does not smoke cigarettes, and drinks alcohol on social occasions. He does report having had five cans of beer while at a party last night. On examination, his blood pressure is 120/80 mmHg and his pulse is irregularly irregular. EKG shows atrial fibrillation with a rate of 160/min. What is the best next step in the management of this patient?
Procainamide
Adenosine
Digoxin
Verapamil
Lidocaine
A 34-year-old male with a history of mitral valve prolapse and mitral regurgitation presents with one week of intermittent fevers and increasing fatigue. He was punched in the face during a street fight two weeks ago. On admission he receives empiric intravenous vancomycin and gentamicin. Three days later, three out of four blood cultures grow Streptococcus viridans highly sensitive to penicillin. Which of the following is the best next step in managing this patient?
Switch antibiotics to oral amoxicillin/clavulanate
Switch antibiotics to oral penicillin V
Switch antibiotics to IV aminoglycosides
Switch antibiotics to IV ceftriaxone
Continue current regimen
A 34-year-old man comes to the emergency department because of severe pain in his penis. He was having sex with his wife on top when he had sudden onset severe pain in the penis at the height of orgasm. Swelling of the penis and deviation of the penile shaft to the right followed the pain. Examination shows a man in severe distress. The penis is uncircumcised, grossly swollen and deviated to the right. There is no blood at the urethral meatus. Which of the following is the most appropriate next step in management?
Antibiotics, analgesics and anti-inflammatory and follow up in 24 hours
Do a circumcision
Retrograde urethrogram followed by surgical exploration of penis
Foley's catheterization
Surgical exploration of penis
A 34-year-old man is being evaluated for possible end-stage renal disease. He has a long history of diabetes, type 1. He previously developed chronic renal insufficiency despite being on enalapril and insulin. His renal fun
Hemodialysis
Renal transplantation from a living unrelated donor
Renal transplantation from a living related donor
Peritoneal dialysis
Renal transplantation from a cadaver
A 34-year-old man is brought to the emergency department after being involved in a motor vehicle collision. He has severe abdominal and left shoulder pain. His temperature is 36C (96.8F), blood pressure is 100/60 mm Hg, pulse is 110/min and respirations are 23/min. Examination shows tenderness in the left upper quadrant of the abdomen. An x-ray film of the chest shows fractures of the left 7th, 8th and 9th ribs. A CT scan of the abdomen is suggestive of splenic injury with some free fluid in the abdomen. He has not been vaccinated for H. Influenza or S. pneumoniae. Which of the following is the most important determinant for surgical versus non-surgical management in this patient?
Hemodynamic stability and hematocrit values
Presence of a rib fracture on chest x-ray
Unvaccinated status of the patient
Presence of free fluid in the abdomen
Presence of left shoulder pain
A 34-year-old man is extricated from an automobile after a motor vehicle collision. The patient has an obvious deformity of his right thigh consistent with a femur fracture. Upon closer examination of the right thigh, there is bone visible through an open wound. Which of the following is the most appropriate management of his open femur fracture?
Early irrigation and debridement, IV antibiotics, compartment decompression, and internal or external fixation
Early irrigation and debridement, IV antibiotics, and internal or external fixation
Early irrigation and debridement, IV antibiotics, and cast or splint placement
IV antibiotics and internal or external fixation
Intravenous (IV) antibiotics and cast or splint placement
{"name":"DES C_Management (5) Prepared : CHILLY", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 30-year-old man presents to the ED complaining of sudden onset of abdominal bloating and back pain lasting for 2 days. The pain woke him up from sleep 2 nights ago. It radiates from his back to his abdomen and down toward his scrotum. He is in severe pain and is vomiting. His temperature is 101.2°F and HR is 107 beats per minute. A CT scan reveals a 9-mm obstructing stone of the left ureter with hydronephrosis. Urinalysis is positive for 2+ blood, 2+ leukocytes, 2+ nitrites, 40 to 50 WBCs, and many bacteria. You administer pain medicine, antiemetics, and antibiotics. Which of the following is the most appropriate next step in management? . Admit for IV antibiotics and possible surgical removal of stone . Observe in ED for another 6 hours to see if stone passes . Discharge with antibiotics and pain medicine . Discharge patient with instructions to consume large amounts of water, A 30-year-old man presents to the emergency department with sudden onset of severe epigastric pain and vomiting 3 hours ago. He reports a 6-month history of chronic epigastric pain occurring nearly every day and relieved by antacids. On examination, he appears sweaty and avoids movement. Vital signs reveal a temperature of 100°F, BP of 100\/60 mmHg, pulse rate of 110\/min, and respiratory rate of 12\/min. The remainder of his examination reveals diminished bowel sounds and a markedly tender and rigid abdomen. A chest x-ray and abdominal films reveal pneumoperitoneum. Which of the following is the most appropriate next step in management? . immediate laparotomy . nonoperative management with NG decompression and antibiotics . fluid resuscitation . administration of H2 blockers . placement of a central venous line, A 30-year-old man presents to the resuscitation bay with gunshot wounds in the anterior and posterior left chest. Although in distress and dyspneic, the patient is cooperative. He has a patent airway and is moving all extremities. His pulse is 120\/min, blood pressure is 120\/90 mm Hg, and respiratory rate is 30\/min. He has bounding distal pulses, and no other injuries are identified on secondary examination. X-ray of the chest reveals fluid in the pleural space, and a left chest tube thoracostomy yields 600 mL of bright red fluid. Over the next hour 750 mL of blood is collected. What is the most appropriate next step in management? Autotransfuse with the collected blood and continue to observe closely Insert another chest tube Left thoracotomy Remove the chest tube and suture the incision closed Thoracentesis","img":"https://cdn.poll-maker.com/20-801188/image.jpeg?sz=1200"}
More Quizzes
Angular JS Quiz
1050
ARE YOU AN ACIDIC BONDING CONCENTRATE EXPERT?
4229
210
Are you 4chan or are you Reddit?
3273
Would You Survive a Horror Movie? Take the Free
201021001
Name the Superhero - Can You Name Them All?
201018822
What Truck Should I Buy - Find Your Ideal Pickup
201019096
Integer - Free Practice with Answers
201019884
Fighting - Are You a Strong Fighter? Free Online
201018472
Hannah Montana: Who Are You, Miley or Lilly?
201020422
Revelation Chapters 1 - 3 - Free Bible Trivia
201020535
Which Hogwarts Legacy Character Are You? Free
201018912