USMLE : ENT-GIT 265 GD
A 28-year-old Caucasian male presents to the emergency department complaining of neck pain for the past two days. He states that a chicken bone scratched the back of his throat a week ago. Two weeks ago, he was in Arizona visiting his friends. He is otherwise healthy and has never been hospitalized. His temperature is 39°C (102.2F), blood pressure is 125/85 mmHg, and heart rate is 120/min. On examination, he refuses to fully open his mouth. Neck movements, especially neck extension, are restricted secondary to pain. Which of the following is the most likely diagnosis?
Meningitis
Herpangina
Epiglottitis
Diphtheria
Retropharyngeal abscess
A 55-year-old female presents to the office with a one-week history of left-sided ear pain and itchiness. The pain is especially bothersome at night, and is exacerbated by chewing. She denies any hearing loss. Her past medical history is significant for hypertension, type 2 diabetes mellitus, hyperlipidemia, and gout. Current medications include lisinopril, allopurinol, and metformin. She has missed her last two appointments with her primary care physician. Her temperature is 38.3°C (101.0F), blood pressure is 140/90 mmHg, and pulse is 98/min. On examination, there is granulation tissue in the left ear canal with a scant amount of discharge. Which of the following is the best initial treatment for this patient?
Topical neomycin
Topical low-strength corticosteroids
Ciprofloxacin
Ampicillin/sulbactam
Surgical debridement
A 7-year-old boy with a 6-day history of nasal discharge presents with a swollen and painful left eye. His blood pressure is 100/70 mm Hg, pulse is 92/min, respirations are 18/min, and temperature is 39.4°C (103F). Examination of the left eye reveals swollen and erythematous eyelids, mild protrusion of the eyeball, and pain with eye movements. The affected eye is tender and his visual acuity is decreased. Funduscopic examination is normal. Which of the following is the most likely diagnosis?
Anterior uveitis
Cavernous sinus thrombosis
Conjunctivitis
Optic neuritis
Orbital cellulitis
A 45-year-old Asian male complains of a progressively worsening sore throat and difficulty swallowing for the past 24 hours. You notice that his voice is muffled and he is drooling. He also has a harsh shrill associated with respiration. His temperature is 39.3°C (103F), blood pressure is 120/80 mmHg, pulse is 106/min, and respiratory rate is 22/min. On examination, a few cervical lymph nodes are palpable and there is tenderness to palpation over his larynx. Which of the following are the two most common organisms that cause this condition?
Haemophilus influenzae and Streptococcus pyogenes
Mycobacterium tuberculosis and herpes simplex virus
Haemophilus influenzae and Candida species
Streptococcus pyogenes and Klebsiella pneumoniae
Staphylococcus aureus and Pseudomonas aeruginosa
A 60-year-old man comes to your office complaining of difficulty hearing for the past few weeks. He has type 2 diabetes mellitus, which is well-controlled by diet alone. His past medical history is also significant for essential hypertension, congestive heart failure secondary to diastolic dysfunction, and chronic renal failure. Medications include aspirin, diuretics, an ACE inhibitor, and a beta-blocker. His pulse is 82/min, blood pressure is 140/90 mmHg, and respirations are 14/min. Examination reveals hearing loss in both ears Which of the following medication is a potential cause of this patient's hearing problems?
Lisinopril
Aspirin
Metoprolol
Furosemide
Hydrochlorothiazide
A 32-year-old male complains of difficulty hearing in his left ear for the past month. He denies any headaches, fever, chills, weight loss, or ear discharge. He is HIV positive, and is currently being treated with highly active antiretroviral therapy (HAART). He also takes trimethoprim/sulfamethoxazole daily. His most recent CD4 count was 425/ mm3. Examination of the affected ear shows a dull, hypomobile tympanic membrane. What is the most likely cause of hearing loss in this patient?
Neoplasia
Non-infectious effusion
Otosclerosis
Opportunistic infection
Demyelinization
A 65-year-old female complains of difficulty eating over the last two days. She states that food drops out of her mouth. She has also been having some discharge in her left ear recently. She denies any sore throat, nasal discharge, chest pain, cough, or difficulty breathing. Her past medical history is significant for type 2 diabetes mellitus, hypertension, and hyperlipidemia. She has been poorly complaint with follow-up appointments. Her temperature is 38.8°C (101.7 F), pulse is 96/min, blood pressure is 140/90 mmHg, and respirations are 18/min. Examination of the left ear canal shows granulations. There is facial asymmetry, and the angle of the mouth on the left is deviated downward. Which of the following is the most likely causative organism for this patient's condition?
Rhizopus species
Pseudomonas aeruginosa
Staphylococcus aureus
Aspergillus niger
Herpes zoster
A 7 -year-old boy is brought to your office with a sore throat, decreased appetite, and nausea. His past medical history is insignificant. All of his vaccinations are up-to-date. He has no known allergies. His temperature is 39.0°C (102.5F), blood pressure is 110/70 mmHg, pulse is 104/min, and respirations are 16/min. On examination, the pharynx and tonsils are red, swollen, and have white exudates on their surface. There is also bilateral tender cervical lymphadenopathy. The rapid diagnostic test for streptococcal antigen is positive. What is the most appropriate next step in management?
Throat culture
Monospot test
Antistreptolysin 0 antibodies
Oral penicillin V
Oral azithromycin
A 37-year-old woman presents to your office with severe vertigo, postural instability, and vomiting. She also complains of "a buzzing sound" in her right ear. She has had two similar episodes over the previous year that lasted several hours and resolved spontaneously. She has no other medical problems. Her mother died of breast cancer at 55 years of age and her father is currently suffering from colon cancer. Her heart rate is 90/min and blood pressure is 130/80 mmHg. Her BMI is 25.3 kg/m2. Examination reveals horizontal nystagmus. Which of the following could have prevented this patient's symptoms?
Caloric restriction
Low salt diet
Gluten-free diet
High complex carbohydrate diet
Calcium supplementation
A 36-year-old woman presents to your office with complaints of worsening throat pain for the past six days. She also has pain in her ears and neck as well as difficulty swallowing. On examination, she has excessive salivation and difficulty opening her mouth. Her temperature is 39°C (102.2F), blood pressure is 130/80 mmHg, pulse is 100/min, and respiratory rate is 18/min. Which of the following neck space infections carries the highest risk of mediastinal involvement?
Submandibular space
Sublingual space
Parapharyngeal space
Retropharyngeal space
Retro-obital
A 23-year-old male comes to your office with a 10-day history of severe headaches. He states that they are sharp in character and are mostly right-sided involving the frontal area. The headaches interfere with his sleep, and he also complains of double vision, nausea, and malaise. His blood pressure is 120/80 mm Hg, pulse is 103/min, respirations are 14/min, and temperature is 38.0°C (100.5F). Examination reveals bilateral periorbital edema. There is subtle right-sided lateral gaze palsy. Which of the following is the most likely diagnosis?
Orbital cellulitis
Acute angle-closure glaucoma
Common migraine
Cavernous sinus thrombosis
Cluster headaches
A 24-year-old Caucasian female complains of recurrent painful ulcers in her mouth and occasional abdominal pain. She has also unintentionally lost 5 pounds over the last six months. She is not sexually active, and denies use of tobacco, alcohol, or drugs. Past medical history is noncontributory and she takes no regular medications. Her mother suffers from asthma and her father has prostate cancer. She is afebrile with a blood pressure of 118/69 mmHg and pulse of 71/min. Physical examination reveals mild abdominal tenderness primarily in the lower abdomen without guarding or rebound. Several shallow ulcers are seen on the buccal mucosa. A biopsy of one of the ulcers demonstrates granulomatous inflammation. Her hematocrit is 42%. Which of the following is the most likely cause of this patient's complaints?
Celiac disease
Folic acid deficiency
Crohn's disease
Oral candidiasis
Squamous cell carcinoma
A 70-year-old man comes to your office with complaints of difficulty hearing. His wife says that he has been raising the television volume much louder recently. The patient claims that he can hear well when he talks to his family members at home, but he has significant difficulty hearing in restaurants or during other family gatherings, which is why he prefers to stay at home most of the time. He worked in a shipbuilding yard for 30 years, and retired five years ago. He has no history of significant noise exposure. What is the most likely diagnosis?
Otosclerosis
Presbycusis
Middle ear effusion
Meniere's disease
Acoustic neuroma
A 12-year-old girl comes to the office complaining of a small amount of left-sided ear discharge that has persisted for the last three weeks. She has completed two courses of antibiotics that were prescribed during her previous visits. She also complains of hearing loss on the left side. On examination, she is afebrile. Otoscopy reveals an intact left tympanic membrane with peripheral granulation and some skin debris. The patient should be evaluated for which of the following?
Meniere's disease
Craniopharyngioma
Otosclerosis
Cholesteatoma
Middle ear osteoma
A 33-year-old Caucasian female has suffered from recurrent episodes of dizziness over the last six months. She describes the episodes as a sensation of severe spinning that last one to two hours and are accompanied by intense nausea. She also feels unsteady during the episode, and has to lie down with her eyes closed for relief. There is no particular factor that precipitates the episodes. She denies any headaches, but complains of fullness in her right ear. She has no ear pain or ear discharge. She has used some over-the-counter ear drops with minimal relief of the fullness sensation. She prefers holding her cell phone on the left side. Which of the following is the most likely cause of this patient's condition?
Middle ear disease
Inner ear disease
Cranial nerve VIII lesion
Cerebellar disease
Lesion in the medulla
A 62-year-old male comes to your office for a routine follow-up appointment. He has smoked one pack of cigarettes per day for the past 30 years and adamantly refuses to quit. He also drinks six to ten beers each weekend. His past medical history is significant for type 2 diabetes mellitus and hypertension. His last hemoglobinA1c was 8.3%. He is overweight with a current BMI of 27.5 kg/m2. While examining him, you notice a whitish patch over the anterior floor of his mouth. The lesion appears to have a granular texture and is not removed by scraping with a tongue depressor. Which of the following is most likely cause of his oral lesion?
Candidiasis
Leukoplakia
Herpes simplex virus infection
Melanoma
Squamous cell carcinoma
6-year-old boy is brought to the office by his mother due to a decreased appetite and irritability for the past three days. He also had an episode of diarrhea yesterday. Lately, he has been sitting close to the television with the volume turned up very loudly. His temperature is 38.1°C (100.5.F), blood pressure is 110/60 mmHg, and heart rate is 110/min. On examination, there is left-sided yellowish ear discharge. His nasal mucosa appears boggy and postnasal drip is present. What is the most likely diagnosis?
Bullous myringitis
Acute otitis media
Otitis extern a
Cholesteatoma
Sinusitis
A 28-year-old African American female complains of recurrent nasal discharge and increasing nasal congestion. She has a constant sensation of dripping in the back of her throat, and states that food has tasted bland to her recently. She is known to have sickle cell trait. She came to the emergency department for severe wheezing after taking naproxen for menstrual cramping one year ago. She has no history of head trauma. She does not smoke cigarettes, but she admits to smoking marijuana occasionally. Which of the following is the most likely diagnosis?
Angiofibroma
Inverted papilloma
Nasal polyp
Perforated nasal septum
Pyogenic granuloma
A 26-year-old man comes to your office with a one-week history of right-sided ear pain. The pain often wakes him up at night, and increases in severity when he chews food. He cannot recall any recent episodes of pharyngitis. He denies having any ear discharge, sinus tenderness, or skin rash. He exercises by swimming frequently at a local club. He is sexually active and uses condoms "quite regularly." He lives with his brother, who often comments on his habit of grinding his teeth at night. On examination, his ears are normal with a mild amount of wax. Pain is not elicited by pulling on the pinna. There are no hearing deficits appreciated. Mobility of the tympanic membrane is normal, and the Weber and Rinne test results are within normal limits. What is the most likely diagnosis?
Ramsay Hunt syndrome
Glossopharyngeal neuralgia
Otitis media
Temporomandibular joint dysfunction
Otitis externa
A 30-year-old school teacher presents with a three-day history of fever, chills, and sore throat. He also complains of difficulty swallowing that started yesterday. He denies any cough, chest pain, or difficulty breathing. He is married and denies any new sexual encounters. His temperature is 39°C (102.2F), blood pressure is 118/76 mmHg, pulse is 102/min, and respirations are 19/min. On examination, his voice is muffled. Enlarged, tender cervical lymph nodes are palpated on the left, and his uvula is deviated to the right. What is the most appropriate treatment for this patient?
Throat swabs and oral antibiotics
Monospot test and oral antibiotics
Emergency laryngoscopy
Cricothyroidotomy
Needle peritonsillar aspiration
An 82-year-old woman presents 1-hour after the sudden onset of moderate-to-severe epigastric pain. The pain radiates to her back, both scapulae, and both arms. She has been nauseated and vomited three times in the past hour. Her past medical history is remarkable for peptic ulcer disease 10-years ago, cholelithiasis for the past 6years, and stable angina pectoris for the past 3-years. She has had occasional episodes of biliary colic and two bouts of acute cholecystitis which were treated conservatively. Her temperature is 36.8C (98.2F), blood pressure is 120/70 mm Hg, pulse is 90/min, and respirations are 14/min. The lungs are clear to auscultation. Abdominal examination shows a soft abdomen with mild tenderness to palpation in the epigastrium. Murphy's sign is negative. Which of the following studies should be done first?
Abdominal ultrasound
Upper Gl endoscopy
Electrocardiogram
Upright abdominal x-ray
Serum amylase and lipase
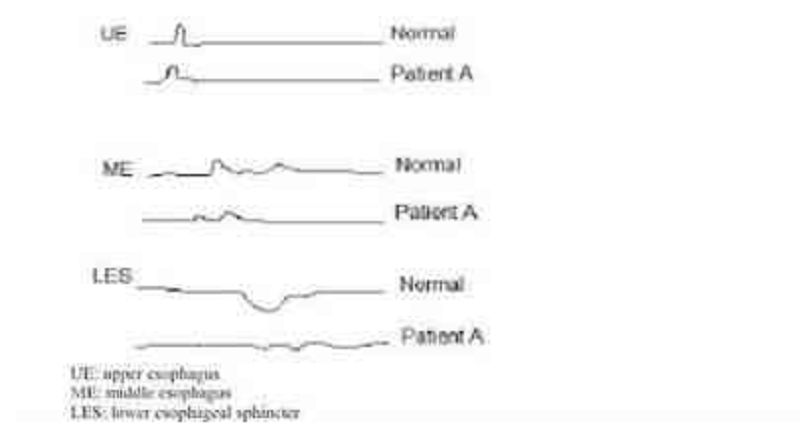
A 43-year-old male (Patient A) is being evaluated for an esophageal disorder. Esophageal manometry tracings after a single swallow of 5 ml of water are shown on the slide below. Which of the following is the most likely diagnosis in this patient?
Cricopharyngeal dysfunction
Diffuse esophageal spasm
Achalasia
Gastroesophageal reflux
Mallory-Weiss syndrome
A 45-year-old nurse practitioner presents to the emergency department due to painful abdominal cramps and watery diarrhea. She has about 10 to 20 bowel movements a day. She also has nocturnal bowel movements. She has had multiple hospitalizations in the past for similar problems without a definite diagnosis. A lower GI endoscopy during a previous hospitalization showed dark brown discoloration of the colon with lymph follicles shining through as pale patches. Which of the following is the most likely diagnosis?
Factitious diarrhea
Irritable bowel syndrome
Celiac disease
Infectious diarrhea
Non-Hodgkin's lymphoma
A 65-year-old woman presents with a 2-month history of fatigue and dyspnea on exertion. She takes no medication. Her temperature is 36.7C (98F), blood pressure is 162/83 mm Hg, pulse is 100/min, and respirations are 21/min. Auscultation shows a 2/6 systolic murmur in the 2nd right intercostal space. No peripheral edema is noted. Rectal examination shows no abnormalities. Test of the stool for occult blood is negative. EKG shows sinus tachycardia and non-specific ST-T changes. Laboratory studies show: Hemoglobin 8.1 g/L MCV 73 fl Platelets 360,000/mm3 Leukocyte count 4,500/mm3 Neutrophils 56% Eosinophils 1% Lymphocytes 33% Monocytes 10% Which of the following is the most appropriate next step in management?
Echocardiography
Bone marrow biopsy
Gastro-duodenoscopy
Colonoscopy
Isotope-labeled erythrocytes scintigraphy

A 44-year-old white female presents with a 2-month history of low-grade fever, abdominal pain and bloody diarrhea. Over the past two days, her symptoms have increased. She does not use medications and she has no allergies. She has had a 10 lb (4.5 kg) weight loss over the past four weeks. Her temperature is 38.9C (102F), blood pressure is 102/70 mm Hg, pulse is 118/min, and respirations are 22/min. Examination shows pale and dry mucus membranes. Abdominal examination shows diffuse tenderness and distention. Laboratory studies show: Hb 9.5 g/dl WBC 16,000/cmm Serum Na 145 mEq/L Serum K 3.0 mEq/L An x-ray film of the abdomen is shown below: Which of the following is the most likely diagnosis?
Crohn's disease
Pseudomembranous colitis
Toxic megacolon from ulcerative colitis
S. Aureus gastroenteritis
Obstructed colon cancer
A 45-year-old Mexican male presents with a 2-day history of traces of blood on the tissue paper after he wipes. He does not have gross blood mixed with stool, but on one occasion there were drops of blood in the toilet after defecation. He has no past medical history or family history of cancer or other significant disease. Which of the following is the most appropriate next step in management?
Colonoscopy
Fecal occult blood test
Anoscopy
Sigmoidoscopy
Barium enema
A 65-year-old man comes to the physician's office with a 2-month history of dysphagia. He initially had difficulty swallowing solids, but now this includes liquids. He has occasional heartburn, which usually responds well to antacids. He has lost 20 lbs of weight in the past 2 months. He has a 40 pack-year history of smoking. He has been a chronic alcoholic for 20 years. His temperature is 36.7C(98F), blood pressure is 110/80 mm Hg, pulse is 66/min, and respirations are 14/min. Physical examination shows no abnormalities. Barium studies show a minimally dilated esophagus with beak-shaped narrowing. Manometry shows increased lower esophageal sphincter tone. Which of the following is the most likely diagnosis?
Achalasia
Sophageal cancer
Scleroderma
Peptic stricture
Diffuse esophageal spasm
A 73-year-old woman is transferred to the hospital from the nursing home because of diverticulitis. A prior CT scan showed inflamed sigmoid colon. Transferred records indicate a 2-day history of fever and abdominal pain. On admission, her white count is 22,000/cmm, and she is started on IV antibiotics and IV fluids. Over the ensuing few days, her white count starts to come down and she has no nausea, vomiting or fever; however, she suddenly develops a cough and increasing abdominal pain. Abdominal examination shows guarding and tenderness in the left lower quadrant. An upright x-ray film of the chest shows free air under the left diaphragm. Which of the following is the most appropriate next step in management?
CT scan of the abdomen
Colonoscopy
Barium enema
Continue antibiotics and observe
Laparotomy
A 51-year-old obese male presents to your office complaining of difficulty swallowing solids but not liquids. His medical history is significant for GERD. Six months ago he was diagnosed with Barrett's esophagus. He reports that three months after the diagnosis of Barrett's esophagus, his heartburn resolved. Barium swallow now reveals an area of symmetric, circumferential narrowing affecting the distal esophagus. Which of the following best explains this finding
Esophageal adenocarcinoma
Hiatal hernia
Achalasia
Peptic stricture
Vascular ring
Ms. Lee, a 62-year-old Chinese woman, comes with yellowness in her eyes for the past 6 weeks. She is generally feeling tired, has lost some weight, and occasionally had some nausea. She denies any altered bowel habits. She is a non-smoker but drinks 2-3 beers each night. Her dad is suffering from high cholesterol and also has had stroke. She had a dilatation and curettage for an abnormal pap smear 15 years ago. Her vitals are stable and she is afebrile. She has marked scleral icterus. An abdominal examination reveals normal bowel sounds and no organomegaly. Her stools were occult blood negative. Her liver function tests and enzymes were ordered and the results are Total protein 6.1 g/dl Albumin 39 g/dl AST 67U/L ALT 52U/L Alkaline phosphatase 290 U/L Total bilirubin 96 mg/dl Direct bilirubin 89 mg/dl Serum lipase is 46 U/L Anti-mitochondrial antibodies negative. Which of the following is the most likely cause of these findings?
Primary biliary cirrhosis
Chronic pancreatitis
Viral hepatitis
Pancreatic carcinoma
Hepatocellular carcinoma
A 23-year-old man comes to the physician because of a two-month history of loose stools, decreased appetite, and weight loss. He has no history of medical problems. He takes no medications. His temperature is 36.7C (98F), blood pressure is 120/76 mmHg, pulse is 90/min, and respirations are 16/min. Laboratory studies show: Hemoglobin 11.2 g/dL MCV 80 fl Leukocyte count 9,500/cmm Segmented Neutrophils 65% Bands 3% Eosinophils 1% Basophils 0% Lymphocytes 25% Monocytes 6% Platelets 550,000/cmm ESR 50 mm/hr Serum sodium 145 mEq/L Serum potassium 4.0 mEq/L Test of the stool for occult blood is positive. Which of the following is the most likely type of diarrhea in this patient?
Inflammatory
Secretory
Osmotic
Motor
Factitial
A 35-year-old Hispanic male comes to the office because of excruciating pain during defecation for the past week. The pain is so severe that he avoids using the toilet. He also adds that he has noticed bright red blood in his stool. The caliber of his stool has not changed. His past medical history is significant for chronic constipation. Rectal examination shows a posterior mucosal tear of the anus. Which of the following is the most appropriate next step in management?
Colonoscopy
Local anesthetic and stool softeners
Lateral sphincterotomy
Antibiotics
Gradual dilatation of the sphincter
A 27 -year-old man complains of episodic abdominal pain. The pain is concentrated in the epigastrium and is gnawing in quality. It wakes him up during the night and is promptly relieved by a glass of water and a piece of bread. He denies vomiting or diarrhea, but has experienced an occasional "dark stool." He has no significant past medical history and does not take any medications. His family history is significant for biliary disease in his mother and stomach cancer in his father. He smokes one pack of cigarettes a day and consumes a can of beer almost every day. His vital signs are with in normal limits. Physical examination shows mild epigastric discomfort on deep palpation. Which of the following is most likely to provide long-term symptom relief in this patient?
Four weeks of omepra zole
Antibiotics and pantoprazole
NSAIDs as needed
Smoking cessation
No alcohol consumption
A 66-year-old man presents with a four-week history of increasing back pain and severe constipation. He has no weakness or sensory symptoms in his legs. He takes acetaminophen for back pain, metoprolol for high blood pressure, and an over-the-counter fiber supplement for constipation. A screening colonoscopy 5-year ago was unremarkable. Rectal examination shows no abnormalities. Examination of the stool for occult blood is negative. His blood pressure is 135/80 mmHg and heart rate is 80/min. Abdominal examination shows no abnormalities. Laboratory studies show: Hb 9.5 g/dl WBC 7,000/cmm Platelets 300,000/cmm BUN 28 mg/dl Serum Creatinine 1.9 mg/dl ESR 80/hr Which of the following is the best explanation for this patient's constipation?
Mechanical obstruction
Medication effect
Electrolyte disturbances
Hormonal disturbances
Neurologic dysfunction
A 26-year-old man presents with a 1-week history of intermittent, crampy, lower abdominal pain accompanied by rectal urgency, bloody diarrhea, nausea and vomiting. His symptoms have become more severe over the past 24 hours. His past medical history is unremarkable. He denies any recent travel or antibiotic use. His temperature is 38.5C (102.0F), blood pressure is 120/80 mm Hg, pulse is 95/min, and respirations are 15/min. Abdominal examination reveals distension and tenderness to palpation without rebound or guarding. The bowel sounds are decreased. Rectal examination shows marked rectal tenderness and mucus mixed with blood in the vault. An x-ray film of the abdomen shows distended colon filled with gas. Laboratory studies show: Hb 10.8 g/dl WBC 19,600/cmm Platelet count 459,000/cmm ESR 54/hr Which of the following is the most appropriate next step in management?
Stool for ova, parasites and culture
Barium enema
Proctosigmoidoscopy and biopsy
Serology for Entamoeba histolytica
T scan of the abdomen
A 64-year-old white male with a history of severe stable angina and peripheral vascular disease undergoes coronary artery bypass surgery. His post-operative course is complicated by hypotension, which is treated successfully; however, a few hours later, he experiences abdominal pain followed by bloody diarrhea. His temperature is 37.8C (100 F), blood pressure is 110/60 mmHg, pulse is 110/min, and respirations are 20/min. Abdominal examination is benign. Laboratory studies show a WBC count of 15,000/cmm with 7% bands. The lactic acid level is elevated. A CT scan is ordered. Which of the following areas of the colon will most likely show abnormal findings?
Sigmoid colon
Splenic flexure
Ascending colon
Mid transverse colon
Hepatic flexure
A 49-year-old woman presents to the emergency department (ED) with profuse, foul-smelling, watery diarrhea and abdominal pain. Five days ago, she was hospitalized for urosepsis and treated with amoxicillin and sulbactam. She recovered well, and was discharged three days ago with a prescription for oral amoxicillin plus clavulanic acid. Her current temperature is 38.8C (101.9F), blood pressure is 110/70 mm Hg, pulse is 102/min, and respirations are 15/min. Abdominal examination shows tenderness in the left lower quadrant. CBC shows a WBC count of 25,000/microl. She is started on intravenous normal saline in the ED. Which of the following is the most appropriate next step in management?
Continue rehydration
Start oral metronidazole
Discontinue antibiotics
Discontinue antibiotics and start oral metronidazole
Discontinue antibiotics and start oral vancomycin
A 52-year-old man presents to your office after passing a black stool. He also describes occasional abdominal discomfort and nausea but denies hematemesis. He says that food seems to help his abdominal pain, so he eats frequently during the day and keeps some snacks on his night stand. As a consequence, he has gained 5 pounds over the last year. He admits that his diet is lacking in vegetables and fruit. He drinks one to two cans of beer nightly, but does not smoke or use illicit drugs. He says that his father died of colon cancer and his mother died from a stroke. Physical examination reveals a right-sided carotid bruit. The fecal occult blood test is positive. Which of the following is the most likely cause of his condition?
Mesenteric ischemia
Mallory-Weiss tear
Lnflammatory bowel disease
Erosive gastritis
Peptic ulcer disease
A 35-year-old Caucasian female presents to your office with several months history of heartburn. She also describes a periodic 'sticking sensation' in her throat during the meal. Her past medical history is significant for asthma that is controlled with inhaled steroids, and acoustic neuroma that was removed 2 years ago. She does not smoke or consume alcohol. She denies any recreational drug use. She is not allergic to any medications. She works as a secretary at a private firm, and considers her work moderately stressful. Her family history is significant for breast cancer in her mother and prostate cancer in her father. Endoscopic evaluation shows mild hyperemia in the distal esophagus. Esophageal manometry reveals absent peristaltic waves in the lower two-thirds of the esophagus and a significant decrease in lower esophageal sphincter tone. Which of the following is the most likely cause of this patient's complaints?
Achalasia
GERD with or without hiatal hernia
Scleroderma
Non-ulcer dyspepsia
Diffuse esophageal spasm
A 34-year-old woman complains of occasional diarrhea and crampy lower abdominal pain. She says that at times her symptoms hamper her performance in important business meetings. The pain sometimes occurs after meals but is not always preceded by eating. The pain is often accompanied by diarrhea with small amounts of stool and mucus. Her past medical history is significant for bleeding hemorrhoids. Her mother died of colon cancer. Which of the following findings is most likely in this patient?
Normal colonic mucosa
Crypt abscesses
Folic acid deficiency
Duodenal ulcer
Intestinal villous atrophy
A 55-year-old obese male presents to his physician for a routine annual physical examination. A review of systems is insignificant, except for constipation which has been present for several years. He does not have major medical problems and is not on any prescription or over-the-counter medications. He has smoked one and- a-half packs of cigarettes daily for 30 years. He drinks 4 oz of alcohol daily. Physical examination is unremarkable. As part of the routine screening, a colonoscopy is performed, which shows multiple diverticuli at the sigmoid colon. He is concerned about the diverticulosis. Which of the following is the most appropriate next step in the management of this patient's diverticulosis?
Advise him to stop smoking
Advise him to stop drinking alcohol
Increase dietary fiber intake
Explain his surgical options
Educate about prophylactic antibiotics
A 40-year-old female presents with abdominal discomfort. The discomfort is localized to the center of the upper abdomen and is not related to meals or fatty food. She has a history of similar symptoms. She has not had gastrointestinal bleeding, fatigue, dysphagia, or weight loss. Her mother has a history of gastric ulcer. Her vital signs are within normal limits. Complete physical examination is unremarkable. Stool for heme occult is negative. Complete blood count and serum chemistries are within normal limits. Which of the following is the most appropriate next step in management?
Barium swallow
Endoscopy
Empiric trial of H2 blockers
H. Pylori breathe test
Empirical antibiotic trial
A 64-year-old man is brought to the ER after an episode of coffee ground emesis followed by lightheadedness. He has been having black, tarry stools for the past few days. He has a history of coronary artery disease and he underwent coronary artery bypass surgery three years ago. He is currently taking aspirin, metoprolol, lisinopril, and pravastatin. He drinks 2-3 beers over the weekend but he quit smoking after the bypass surgery. His temperature is 36.7C (98F), pulse is 110/min, respirations are 16/min, and blood pressure is 90/60 mmHg. Examination shows coffee ground-like material in the oropharynx. His lungs are clear. Abdomen is slightly tender in the epigastrium. Laboratory studies show Complete blood count: Leukocyte count 9,500/mm3 Hemoglobin 8.1 g/L Platelets 130,000/mm3 Chemistry panel: Serum sodium 140 mEq/L Serum potassium 3.5 mEq/L Bicarbonate 27 mEq/L Blood urea nitrogen (BUN) 54 mg/dL Serum creatinine 1.2 mg/dL Which of the following is the most appropriate next step in management of this patient?
Whole blood transfusion
Acked red blood cell transfusion
Fresh frozen plasma infusion
Emodialysis
Platelet transfusion
A 12-year-old girl comes to the physician for chronic weight loss and fatigue. She has a history of bulky, floating, foul-smelling stools, flatulence and meteorism. She also has bone pain and easy bruising. Laboratory studies show anemia with serum iron: 25 mg/dl, ferritin: 25 mg/dl and serum total iron binding capacity 600 mg/dl (normal 300-360 mg/dL); PT is 16 sec. Physical examination shows loss of subcutaneous fat, pallor, hyperkeratosis and abdominal distention; bowel sounds are increased. Which of the following is most likely associated with this patient's condition?
Anti-endomysial antibodies
Anti-Scl-70 antibodies
Antinuclear antibodies
Anticentromere antibodies
Anti-mitochondrial antibodies
A 30-year-old woman presents with a 5-month history of episodic retrosternal pain that radiates to the interscapular region. The pain episodes typically last 15 minutes, and are precipitated by emotional stress and hot or cold food. Her relative gave her sublingual nitroglycerine tablets, which alleviated the pain. Her past medical history is unremarkable, and she does not take any other medications. There is no family history of coronary artery disease. Her vital signs are within normal limits. Physical examination shows no abnormalities. A lipid profile is within normal limits. An EKG shows a normal sinus rhythm. A stress test fails to reproduce the symptoms or to induce ST/T wave changes. Chest x-ray, upper GI endoscopy, and echocardiography show no abnormalities. Which of the following is the most appropriate next step in diagnosis?
CT scan of the chest with contrast
Sophageal motility studies (manometric recordings)
Coronary angiogram
Acid perfusion (Bernstein) test
Pulmonary perfusion/ventilation scintigraphy
A 45-year-old male comes to the physician for epigastric pain and diarrhea. His past medical history is significant for chronic duodenal ulcers. He has been smoking 2 packs of cigarettes daily for the past 10 years. He occasionally drinks alcohol. He denies illegal drug use or multiple sexual partners. Physical examination shows abdominal tenderness without rebound or rigidity. Endoscopy shows prominent gastric folds, chronic duodenal ulcer, and upper jejunal ulceration. Which of the following is the most appropriate next step in the diagnosis of this patient?
Secretin stimulation test
Gastric acid secretion study
Erum chromogranin A
Calcium infusion study
Serum gastrin concentration
A 42-year-old male comes to the physician's office for evaluation of skin rash and hair loss. He has a long history of Crohn's disease and has had extensive small bowel resection resulting in short bowel syndrome. He is currently receiving total parenteral nutrition. When he does try to eat, he complains that the food does not taste good. His vital signs are stable. Examination shows alopecia and bullous, pustular lesions around the perioral and periorbital areas. Which of the following is the most likely cause of his current symptoms?
Celiac disease
Zinc deficiency
Vitamin A deficiency
Vitamin B 12 deficiency
Systemic lupus erythematosus
A 32-year-old female from South America presents with a 3-month history of progressive difficulty with swallowing for both liquids and solids. At night she has a bitter taste in her mouth. Over the past two months, she has had a 10 lb (4.54 kg) weight loss. She has not had any previous illnesses, and does not take any medication. Physical examination is unremarkable. A lateral x-ray film of the chest shows extreme dilatation of the esophagus with an air fluid level. Which of the following is the diagnostic test for this patient's condition?
Barium swallow
Endoscopy
PH monitoring
Manometry
Tscan
A 45-year-old Hispanic male comes to the emergency department because of a two-day history of intermittent abdominal pain and bloody diarrhea. He has had four similar episodes in the past year. He is subsequently admitted to the floor. Radiographic and endoscopic evaluations show extensive disease from the terminal ileum to the rectum with multiple ulcerations and pseudopolyps. Biopsy of the lesion shows noncaseating granulomas and crypt abscess. Which of the following is the most characteristic feature which favors the diagnosis of Crohn's disease against that of ulcerative colitis?
Crypt abscess
Abdominal pain and bloody diarrhea
Non-caseating granulomas
Disease from terminal ileum to rectum
Pseudopolyps
A 50-year-old female presents with heartburn and gnawing abdominal pain. She was diagnosed with peptic ulcer disease 3 years ago, but she has been non-adherent to her medications. She asks you if her nonadherence puts her at increased risk of any complications. Which of the following is the most common complication of peptic ulcer disease?
Perforation
Penetration
Gastric outlet obstruction
Hemorrhage
Atrophic gastritis
A 56-year-old woman with cirrhosis presents with a 2-week history of increasing abdominal distension. She has mild encephalopathy and esophageal varices without bleeding. Her cirrhosis is due to chronic hepatitis type B. She has a past history of ascites treated successfully with conservative management. She is currently on sodium, water and protein restriction, maximal doses of spironolactone and furosemide, and lactulose. Her temperature is 36.6C (97.9F), blood pressure is 120/70 mm Hg, pulse is 80/min, and respirations are 30/min. She has a flapping tremor and labored breathing. Abdominal examination shows marked abdominal distension. An x-ray film of the chest is unremarkable. Abdominal ultrasound shows peritoneal fluid and splenomegaly, liver hyperechogenicity and nodularity, and portal vein width of 16 mm; no masses are evident. Which of the following is the most appropriate next step in the management of this patient's ascites?
Intravenous furosemide therapy
Tapping of some amount of ascitic fluid
Peritonea-jugular shunt
Distal spleno-renal shunt (selective shunt)
Side-to-side porto-caval shunt (non-selective shunt)
A 44-year-old male who has had an extensive small bowel resection for Crohn's disease has been on total parenteral nutrition for two years. He presented to the hospital with epigastric and right upper quadrant pain. He has been taking azathioprine. His vital signs are within normal limits. Physical examination shows mild right upper quadrant tenderness. An ultrasonogram shows several gallstones; an ultrasonogram performed two years ago did not demonstrate gall stones. Which of the following is the most likely cause of his gallstones?
Increased cholesterol secretion
Increased red blood cell destruction
Mpaired gallbladder contraction
Increased enterohepatic recycling of bile acids
Increased calcium absorption

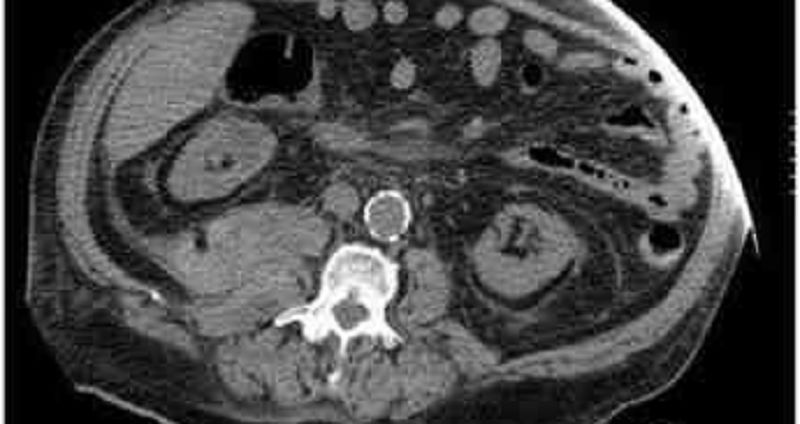
A 54-year-old male presents to the emergency department with a 1-week history of abdominal pain. His other symptoms are nausea, vomiting, low-grade fever, and loss of appetite. He does not use alcohol. He has a seizure disorder, for which he takes a "prescription drug." X-ray films of his chest and abdomen show no abnormalities. His abdominal CT scan is shown below.Which of the following is the most likely explanation for this patient's abdominal symptoms?
Gall bladder pathology
Kidney pathology
Pancreas pathology
Air in the stomach
Liver pathology
A 50-year-old man presents with a 3-hour history of right arm pain. Two weeks ago, he was treated for superficial thrombophlebitis of the right cephalic and right saphenous veins. For the past two months, he has had significant back pain, which is being treated with NSAIDs. His temperature is 37.0C (98.6F), blood pressure is 140/80 mm Hg, pulse is 70/min, and respirations are 10/min. Physical examination shows a swollen, ruddy and warm right arm, but is otherwise unremarkable. Cervical and chest x-ray films show no abnormalities. Laboratory studies show: Hct 50% Platelets 120,000/cmm WBC 9,600/cmm Neutrophils 60% Eosinophils 2% Basophils 0% Lymphocytes 31% Monocytes 7% PT 25 sec PTT 39 sec Fibrinogen 300 mg/dL Fibrin split products positive Which of the following is the most appropriate next step in management?
Protein C, S and antithrombin III levels
Perfusion scintigraphy of the lungs
Venography of right brachial, axillary and subclavian veins
CT of the chest abdomen and pelvis
CT of the thoracic outlet
A 70-year-old male presents to the emergency room complaining of weakness, dizziness and back pain. He denies nausea, vomiting, diarrhea, chest pain, palpitations, shortness of breath, urinary symptoms, or black stools. His past medical history is significant for diabetes mellitus, diabetic nephropathy and retinopathy, hypertension, atrial fibrillation and chronic leg cellulitis. He takes warfarin for chronic anticoagulation. On physical examination, his blood pressure is 139/75 mmHg and his heart rate is 110 and irregular. His WBC count is 10,500/mm3, hemoglobin level is 7.0 mg/dl and platelet count is 170,000/mm3. An abdominal CT image is shown on the slide below.Which of the following is the most likely diagnosis?
Renal cell carcinoma
Vertebral fracture
Retroperitoneal hematoma
Hydronephrosis
Mesenteric ischemia
A 43-year-old man is evaluated for a one-year history of chronic abdominal pain. He describes episodes of epigastric and left upper quadrant pain that last for hours and are not relieved by antacids. Certain foods can precipitate the pain. He also complains of occasional diarrhea. The patient has lost 10 pounds over the last 6 months. Four years ago he was hospitalized for three days with acute abdominal pain. He smokes one pack of cigarettes a day and consumes alcohol regularly. His family history is significant for diabetes mellitus in his mother and prostate cancer in his father. Which of the following is most likely to diagnose this patient's condition?
D -xylose absorption test
Serum amylase and lipase
Adioisotope (HIDA) scans
CA 19-9 and CEA levels
Stool elastase
A 50-year-old woman comes to clinic due to several episodes of severe watery diarrhea for the past 15 days. There is 4/10 pain all over her abdomen but she has not noticed any blood in her stools. She has normal diet and has not travelled anywhere recently. She denies any one around her having similar complaints. She also had occasional cramps in her leg muscles and feels dehydrated. She smokes one to two cigarettes a day and drinks socially. Her temperature is 36.8C (98.1F), blood pressure is 108/64 mm Hg, pulse is 118/min, and respirations are 18/min. On examination her abdomen is slightly tender. Laboratory results are as follows. WBC 5600mm3 Hemoglobin 13.6 Hematocrit: 41%, Platelets 209,000mm3 Sodium 138mEq/L Potassium: 2.1mEq/L Bicarbonate: 35mEq/L Blood urea nitrogen: 16 mg/dl Creatinine: 0.8 mg/dl Glucose 106 mg/dl A CT abdomen is ordered which shows a mass in the head of pancreas. What is the most probable diagnosis?
Pancreatic adenocarcinoma
Glucagonoma
Lnsulinoma
VIPoma
Gastrinoma
A 37 -year-old male is brought to the emergency department due to an episode of hematemesis. He has a history of peptic ulcer disease. A nasogastric tube lavage yields coffee-ground-like material. Physical examination reveals pallor and delayed capillary refill, without cyanosis. His temperature is 36.7C (98F), blood pressure is 85/40 mm Hg, pulse is 125/min, and respirations are 18/min. Which of the following is the most appropriate first step in management?
Intravenous octreotide
Upper GI endoscopy
Surgical intervention
Intravenous pantoprazole
Fluid resuscitation
A 35-year-old Caucasian male presents to the emergency department with two episodes of bloody vomiting which occurred one-half hour ago. He has a history of migraines. For the past two days, he has been having severe headaches and has taken 20 tablets of aspirin without relief. He then resorted to heavy drinking and forgot about the pain. He drinks alcohol "occasionally" and has been smoking 1 pack of cigarettes daily for the past 18 years. Which of the following is the most likely explanation for this patient's hematemesis?
Esophageal variceal bleeding
Acute erosive gastritis
Mallory Weiss syndrome
Ulminant hepatic failure
Acute platelet dysfunction
A 52-year-old woman with cirrhosis presents with increasing abdominal distension. Her treatment regimen was amended three days ago, when furosemide was added to spironolactone and sodium/water restriction. However, her distension persists, and today she is very somnolent and has passed very little urine. Her past medical history is remarkable for chronic hepatitis type B, cirrhosis, encephalopathy, and 2 bleeding episodes from esophageal varices; the bleeding was controlled with sclerotherapy. Her temperature is 36.5C (97.6F), blood pressure is 90/60 mm Hg, pulse is 80/min, and respirations are 18/min. Abdominal examination shows distension, shifting dullness, and no tenderness; bowel sounds are present. Laboratory studies show: Hemoglobin 11.0 g/L Leukocyte count 3,500/mm3 Serum sodium 125 mEq/L Serum potassium 5.5 mEq/L Chloride 103 mEq/L Blood urea nitrogen 60 mg/dL Serum creatinine 1.8 mg/dL Prothrombin time 18 sec Partial thromboplastin time 35 sec Urinalysis shows no abnormalities. Ultrasound of the kidney is unremarkable. Which of the following is the most appropriate next step in management?
Increase the dose of furosemide to its maximum
Careful volume loading and discontinuation of furosemide and spironolactone
Tapping of ascites
Renal biopsy
Intravenous pyelography
An 83-year-old woman presents with a 1-year history of progressively severe crampy abdominal pain after eating. She has started avoiding food because of the pain. The pain is often associated with bloating, nausea, and occasional diarrhea. She has had a 15 kg (331b) weight loss over the past year. Her other medical problems include hypertension, diabetes mellitus-type 2, hypercholesterolemia, peripheral vascular disease, coronary artery disease and myocardial infarction. Social history is not significant. Abdomen is soft, nontender and nondistended. Abdominal x-ray and CT scan are unremarkable. Which of the following is the most likely diagnosis?
Chronic pancreatitis
Atherosclerosis of the mesenteric arteries
Crohn' s disease
Irritable bowel syndrome
Celiac disease
A 45-year-old Asian-American female comes to the physician due to bloating, flatulence, abdominal cramps and explosive watery diarrhea. These symptoms occur after ingesting dairy products. She has not had any weight loss. She has not had bone pain or easy bruising. Physical examination shows abdominal distention and borborygmi. You decide to investigate the patient further. Which of the following test results is most likely to be observed?
Positive urine test for reducing substances
Decreased stool osmotic gap
Positive hydrogen breath test
Alkaline stool pH
Positive acid steatocrit test
A 50-year-old male undergoes vagotomy and pyloroplasty for a peptic ulcer perforation. His early postoperative course is complicated by fever and hypotension, which are treated with broad-spectrum antibiotics and IV fluid support. He then recovers well; however, on post-operative day 6 he develops nausea, vomiting, abdominal pain, and profuse, watery diarrhea. His temperature is 38.9 C (102 F), blood pressure is 110/70 mmHg, pulse is 120/min, and respirations are 18/min. Abdominal examination shows tenderness in the sigmoidal area. Test of the stool for occult blood is negative. Laboratory studies show: Hb 11.5g/dL Platelet count 180, 000/cmm Leukocyte count 17, 500/cmm Segmented neutrophils 75% Bands 10% Eosinophils 1% Lymphocytes 14% Which of the following is the most appropriate next step in management?
Blood cultures
Colonoscopy
Stool cultures
Cytotoxin assay in the stool
Observation
A 65-year-old woman presents with painless intermittent rectal bleeding. The bleeding is bright red in color. She does not have abdominal pain, nausea, or vomiting. She has a history of hypertension, diabetes mellitus, and hypercholesterolemia. Her temperature is 36.7C (98 F), blood pressure is 140/80 mmHg, pulse is 80/min, and respirations are 16/min. Physical examination shows a systolic ejection murmur in the right second intercostal space; examination is otherwise unremarkable. Sigmoidoscopy shows no abnormalities. Which of the following is the most likely diagnosis?
Vascular ectasia
Diverticulosis
Ischemic colitis
Arcinoma colon
Hemorrhoids
A 45-year-old white male comes to your office for evaluation of diarrhea of 8-months duration. He says that he has lost almost 15 lbs during the past 8 months. He denies any blood in the stools. 24-hour stool collection reveals fecal fat of 10 gm/day. Stool microscopy reveals no pathogens and no leucocytes. D-xylose test was performed which shows that less than 2 grams of D-xylose is excreted in urine in 5 hours. D-xylose test was re-performed after 4-week treatment with antibiotics but excretion is still less than 2 grams in 5 hours. Based on these findings, what is the most likely diagnosis in this patient?
Lactose intolerance
Bacterial overgrowth
Pancreatic insufficiency
Celiac disease
Terminal ileal disease
A 27 -year-old male presents with a history of intermittent abdominal distention, flatulence and greasy stools. He also complains of fatigue. He has no other medical problems. His family history is unremarkable. He does not use tobacco, alcohol or smoking. His vital signs are within normal limits. Physical examination shows a pruritic, papulovesicular rash over the extensor surfaces of the extremities and over the trunk, scalp and neck. His abdomen is soft, nontender and non-distended. Stool for occult blood testing is negative. Lab studies show: Hemoglobin 10.0 g/L MCV 75 fl Platelets 340,000/mm3 Leukocyte count 4,500/mm3 Neutrophils 56% Eosinophils 1% Lymphocytes 33% Monocytes 10% Which of the following is the most likely diagnosis of his skin condition?
Guttate psoriasis
Dermatitis herpetiformis
Pityriasis rosea
Seborrheic dermatitis
Bullous pemphigoid
A 68-year-old woman with a history of heavy alcohol use and chronic pancreatitis presents with a several month history of recurrent epigastric pain. The pain is occasionally associated with nausea and vomiting. She has lost 15 lbs (6.8 kg) over the past 3 months. She is afebrile. Physical examination shows scleral icterus. Laboratory studies show: Albumin 3.0 mgldl Total bilirubin 3.5 mgldl Direct bilirubin 24 mgldl Alkaline phosphatase 220 U/L Aspartate aminotransferase (SGOT) 28 U/L Alanine aminotransferase (SGPT) 25 U/L Amylase 145 U/L Lipase 100 U/L Which of the following is the most appropriate next step in management?
ERCP
CT scan of the abdomen
MRI of the abdomen
Plain abdominal radiography
Upper GI endoscopy
A 29-year-old male with a 6-year history of HIV infection presents with chronic, severe diarrhea associated with malaise, nausea, anorexia and abdominal cramps. His last CD4 count was 80cells/mm3. A modified acid-fast stain of a stool specimen shows 4-6 mm oocysts. Which of the following is the most likely microorganism responsible for this condition?
Mycobacterium avium complex
Cryptosporidium parvum
Isospora belli
Pneumocystis jiroveci
Microsporidia
A 56-year-old man comes to the emergency department due to a one-day history of abdominal pain and increasing distension. He has not passed flatus during this time. He has had nausea without vomiting. He has a history of cirrhosis secondary to chronic alcoholism. He is taking spironolactone and furosemide. His temperature is 38.0C (101.3F), blood pressure is 120/70 mm Hg, pulse is 100/min, and respirations are 24/min. Physical examination shows a slightly confused man with a flapping tremor. Breathing is labored and lungs are clear to auscultation. Abdominal examination shows distension, tenderness to palpation with rebound, and no guarding; a fluctuating wave and shifting dullness are present. Abdominal auscultation shows splashing and markedly decreased bowel sounds. An x-ray film of the chest shows no abnormalities. An x-ray film of the abdomen shows gas in the small and large bowels without air-fluid levels. Which of the following is the most appropriate next step in management?
Barium enema
Sigmoidoscopy
Ultrasound of abdomen
Diagnostic peritoneal lavage
Diagnostic paracentesis
A 49-year-old woman presents with a two-week history of lower abdominal pain and severe diarrhea. The stools are watery without blood or mucus. The abdominal pain is mild and unrelated to her stools. She has had recent episodes of flushing. She has not had fever. There is no history of travel. She does not smoke or drink alcohol. Her past surgical history includes a fracture repair of her right leg 3 years ago. Her temperature is 36.6C (97.8F), blood pressure is 106/68 mm Hg, pulse is 103/min, and respirations are 20/min. Oxygen saturation is 99% on room air. Physical examination shows facial flushing, a prominent jugular venous pulse and expiratory wheezes. Which of the following is the most likely diagnosis?
Diverticulitis
Infectious gastroenteritis
Lnflammatory bowel disease
Carcinoid syndrome
Irritable bowel syndrome
A 42-year-old male presents with a 2-year history of heartburn. The heartburn occurs after heavy meals and while supine. Over time, his symptoms have been increasing in severity and frequency. His symptoms used to be alleviated with the use of over-the-counter antacids, but these have become ineffective in the past two months. He also complains of epigastric pain and occasional vomiting, both of recent onset, especially in the morning. He denies dysphagia or odynophagia. He eats junk food and drinks two cups of coffee daily. He regularly drinks grape brandy and smokes 1 pack of cigarettes/day. Abdominal examination shows epigastric tenderness. Abdominal ultrasound is unremarkable. Test of the stool for occult blood is negative. Which of the following is the most appropriate next step in management?
Treatment with ranitidine
Upper Gl endoscopy
Barium swallow
Manometric studies
Reassurance
A 45-year-old Caucasian male presents with a 2-year history of progressive heartburn which is most severe while supine. Over-the-counter antacids have not relieved his symptoms. Endoscopy shows a hiatal hernia. The patient is reluctant to accept any treatment. Which of the following is he at risk for if his condition is left untreated?
Peptic ulceration
Squamous cell carcinoma of esophagus
Aspiration pneumonia
Mallory Weiss syndrome
Adenocarcinoma of esophagus
A 34-year-old Caucasian male presents to the office with a 4-week history of diarrhea. He just returned from a trip to South America, where he developed foul-smelling stools, abdominal cramps and bloating. A three-day course of ciprofloxacin did not relieve his symptoms. His vital signs are within normal limits. Physical examination shows no abnormalities. Which of the following is the most appropriate next step in management?
Schedule colonoscopy
Obtain CT scan of the abdomen
Prescribe oral metronidazole
Prescribe another course of ciprofloxacin
Prescribe oral ampicillin
A 55-year-old male comes to the physician with a history of diarrhea, weight loss, bloating, and excessive flatulence. His symptoms began soon after having "stomach surgery" two years ago. He has a history of gastric ulcers. Physical examination shows scarring associated with past surgery, and abdominal distention with identifiable succussion splash. Laboratory studies show anemia with MCV of 100fl. Which of the following is the most likely diagnosis?
Short bowel syndrome
Bacterial overgrowth
Peptic ulcer disease
Crohn's disease
Ulcerative colitis
A 45-year-old male comes to the physician with a 6-month history of periodic abdominal pain. He tried several over-the-counter medications including H2 blockers and proton pump inhibitors with moderate success. Workup, including an upper GI series and endoscopy, showed multiple duodenal ulcers and a single jejunal ulcer. Test of the stool for occult blood is positive. Test of the stool for fat is positive. Which of the following is the best explanation for this patient's impaired fat absorption?
Pancreatic enzyme deficiency
Pancreatic enzyme inactivation
Reduced bile salt absorption
Defective intestinal absorption
Bacterial proliferation
A 66-year-old man returns to the emergency department (ED) for a second time because of persistent left lower quadrant pain and developing fever, despite 48 hours of oral antibiotics. He had presented to the ED 2 days ago because of left lower quadrant pain. He was able to tolerate a diet and had no fever; he was then sent home on antibiotics, and instructed to return if there was no improvement. He has a 2-week history of constipation without regular bowel movements. Laxatives have not relieved his symptoms. His diet consists of meat with very few vegetables. His vital signs are within normal limits, except for a low-grade fever. Abdominal examination shows left lower quadrant tenderness and guarding. Rectal examination shows no abnormalities. Laboratory studies show a WBC of 16,400/cmm. He is admitted and started on IV antibiotics. Forty-eight hours later, his symptoms persist without any improvement. Which of the following is the most appropriate next step in management?
Abdominal x-rays
Lexible sigmoidoscopy
Colonoscopy
CTscan
Barium enema
A 58-year-old man presents with a one-year history of diarrhea. The stools are watery and accompanied by abdominal cramps. He denies any fever, blood per rectum, or foul-smelling stools. He has also experienced frequent episodes of dizziness, flushing, wheezing, and a feeling of warmth. He has taken herbal medicines, which failed to relieve his symptoms. He is depressed about his illness, and feels hopeless about diagnosis and treatment. He appears ill. Auscultation of the chest shows a 2/6 systolic murmur over the left lower sternal border. Abdominal examination shows hepatomegaly 3cm below the right costal margin, mild shifting dullness, and no abdominal tenderness. Laboratory studies show: Hb 13.0gm/dl MCV 90fl WBC 6,100/cmm Platelets 210,000/cmm AST101 U/L ALT 99 U/L Alkaline phosphatase 400 mg/dl This patient is at risk of developing a deficiency of which vitamin or mineral?
Vitamin A
Lron
Niacin
Calcium
Vitamin C
A 50-year-old female presents with a 3-year history of abdominal pain and diarrhea. She has not been evaluated by a physician. Recently, her symptoms have been progressively worsening. Endoscopy shows multiple ulcerations of the duodenum and prominent gastric folds. Secretin stimulation test shows increased gastrin secretion. Which of the following is most likely associated with this patient's condition?
Medullary thyroid cancer
Pheochromocytoma
Primary hyperparathyroidism
Neuromas
Marfanoid habitus
A 58-year-old woman presents to the emergency department with right subcostal heaviness, intermittent pain, food intolerance, and 13.2 lbs-weight loss (6kg) over the past 2 months. Her pain has been worsening for the past 2 days; it was initially localized to the right upper quadrant, but has now shifted to her back. Her past medical history is remarkable for appendicitis, which was complicated by perforation and peritonitis 20 years ago. Abdominal examination shows epigastric tenderness. There is a palpable mass below the right costal margin. Murphy's sign is negative. Abdominal ultrasound shows an enlarged gallbladder and dilation of the hepatic ducts. Laboratory studies show: WBC 11,000/cmm Total bilirubin 24 mg/dl Direct bilirubin 1.6 mg/dl Alkaline phosphatase 310 U/L Aspartate aminotransferase (SGOT) 87 U/L Alanine aminotransferase (SGPT) 56 U/L Amylase 140 U/L Which of the following is the most appropriate next step in management?
Plain abdominal film
Endoscopic retrograde cholangiopancreatography
Percutaneous transhepatic cholangiography
CT scan of the abdomen
HIDA scan for cystic duct obstruction
A 50-year-old white male presents with complaints of bitter taste and central chest pain. He further describes he pain as moderate-to-severe, occurring during or after meals, non-radiating, and burning. The pain is relieved with antacids, and worsened by lying supine. He has lost 10 lbs (4.5kg) over the past 5-months (unintentional). He has smoked 2 packs of cigarettes daily for 20 years. His vital signs are stable, and he is afebrile. The physical examination is unremarkable. Chest x-ray and EKG show no abnormalities. Which of the following is the most appropriate next step in management?
Treatment with antacids
Treatment with famotidine
Treatment with omeprazole
Esophagoscopy
Esophageal pH monitoring
A 63-year-old man presents with a 2-month history of dysphagia for both solids and liquids. He has had a 6.6 lb (3kg) weight loss over this time. His past medical history is remarkable for a transient ischemic attack 6 months ago, two bouts of pneumonia in the past 3 months, and chronic heartburn treated with over-the-counter antacids. Physical examination shows a supple neck without masses. Abdominal examination shows mild epigastric tenderness to deep palpation. Chest x-ray is normal for his age. Which of the following is the most appropriate next step in diagnosis?
Endoscopy
Barium swallow
Otility studies
Video fluoroscopy
24-hour pH monitoring
A 27-year-old Caucasian woman presents with abdominal pain, diarrhea and a 4.5 (2kg) weight loss for the past two months. She describes the abdominal pain as intermittent, moderate-to-severe, and located in the right lower quadrant. Over the past 48 hours, the pain has intensified. Her temperature is 37.6C (99.6F), blood pressure is 120/70 mm Hg, pulse is 100/min, and respirations are 14/min. Several shallow ulcers are present in her mouth. Abdominal examination shows tenderness in the right lower quadrant without rebound. Rectal examination shows mucus. Rectosigmoidoscopy is unremarkable. An x-ray film of the abdomen shows gas in the small and large bowels. Laboratory studies show: Hb 10.2 g/dL WBC 16,500/cmm Platelet count 530,000/cmm ESR 48/hr Which of the following is the most likely diagnosis?
Diverticulitis
Celiac disease
Irritable bowel syndrome
Crohn's disease
Ulcerative colitis
A 65-year-old man treated for heart failure with enalapril and digoxin presents to the emergency department (ED) with palpitations. His blood pressure is 160/ 100 mmHg, and heart rate is 110/min. His rhythm is irregular. His lungs are clear on auscultation. His abdomen is soft and non-distended. Mild epigastric tenderness is elicited on deep palpation. ECG shows atrial fibrillation without acute ischemic changes. Cardiac enzyme levels are normal. Treatment with warfarin and verapamil is initiated, and the patient is eventually discharged home. After two weeks, he returns to the ED to complain of profound anorexia. Which of the following is the most likely cause of his current complaint?
Gastric irritation
Pancreatitis
Drug interaction
Occult carcinoma
Gastrointestinal bleeding
A 65-year-old Caucasian male presents to your office with a several month history of difficulty swallowing. He has noticed a right-sided neck mass which increases in size while drinking fluids. His past medical history is significant for hypertension, gastroesophageal reflux disease, and osteoarthritis of his right knee. His current medications include hydrochlorothiazide, ranitidine, and occasional naproxene. You order a barium examination of the esophagus to visualize the abnormality. Which of the following is the most important pathogenetic factor in the development of this patient's problem?
Motor dysfunction
Metabolic abnormalities
Acid reflux
Lnflammation
Abnormal proliferation
A 52-year-old Caucasian male comes to you for a routine health check-up. You decide to do age-appropriate screening in this patient and order a colonoscopy. The colonoscopy is normal, except for a 1.5cm polyp in the left descending colon. A colonoscopic polypectomy is done and the biopsy results are pending. The patient is anxious to know the expected biopsy results and the risk of cancer. Which of the following types of polyps is considered to be most premalignant?
Hamartomatous polyp
Hyperplastic polyp
Villous adenoma
Tubulovillous adenoma
Tubular adenoma
A 47 -year-old male comes to the emergency department complaining of an intense burning pain in his abdomen. The pain started a couple of hours ago and is getting worse. He also has nausea and vomited twice. The vomitus is described as dark red-brown in color. He drank "quite a bit of alcohol' last night. He has had several episodes of this type of pain before, and was diagnosed with peptic ulcer disease five years ago. Several courses of H. Pylori eradication therapy have been prescribed in the past, but the patient admits to being non-compliant. He admits to smoking and drinking heavily. His temperature is 36.8 C (98.2 F), blood pressure is 126/88 mm Hg, pulse is 98/min, and oxygen saturation is 96% on room air. The physical examination is remarkable for marked epigastric tenderness. No masses or rebound tenderness are appreciated. IV fluids are administered, blood tests are taken, and upper GI endoscopy is being arranged. Which of the following serum markers is most likely to be elevated in this patient?
Platelet count
Blood urea nitrogen
Prothrombin time
Potassium
Creatinine
A 65-year-old male complains of fatigue for the past one month. He has been living alone since the death of his wife one year ago. He does not like to cook, and his diet consists mostly of canned food, hot tea, and toast. He drinks one glass of white wine nightly with dinner. Examination shows pallor of the skin, nail beds and conjunctiva. Rectal exam is heme-negative. His physical examination is otherwise unremarkable. Administration of which of the following would be most helpful in treating his condition?
Vitamin 8 12
Folic acid
Vitamin C
Vitamin D
Vitamin E
A 50-year-old white male comes to the physician's office because of diarrhea, abdominal pain and weight loss. He has bulky, foul-smelling stools, abdominal distension and flatulence. He also has arthralgias and a chronic cough. His temperature is 37.8C (100F), blood pressure is 120/80 mm Hg, pulse is 80/min, and respirations are 18/min. Physical examination shows generalized lymphadenopathy, skin hyperpigmentation and a diastolic murmur in the aortic area. Small bowel biopsy shows villous atrophy with numerous PAS-positive materials in the lamina propria. Which of the following is the most likely diagnosis?
Celiac disease
Tropical sprue
Crohn's disease
Whipple's disease
Cystic fibrosis
A 65-year-old Asian male presents to the physician with a four-week history of weakness and vague postprandial epigastric pain. His past medical history is insignificant. He does not take any medications. He smokes 1½packs of cigarettes daily and drinks alcohol occasionally. The fecal occult blood test is positive. Gastroduodenoscopy shows an antral ulcer. Four of seven biopsies taken from the margins of the ulcer are consistent with adenocarcinoma. Which of the following is the most appropriate next step in management?
Helicobacter pylori testing
Serologic markers
A CTscan
Laparoscopy
Exploratory laparotomy
A 20-year-old male university student presents with a one-month history of 4 to 6 loose watery bowel movements per day with occasional tenesmus, urgency, and abdominal cramps. He also describes a two-week history of intermittent bright red blood per rectum. His appetite and energy levels are excellent and his weight is stable. He is otherwise healthy and takes no medications. His family history is unremarkable. He has not recently used antibiotics nor has he traveled outside the country. He does not use tobacco, alcohol or drugs. Sigmoidoscopy demonstrates mild erythema and rectal biopsy confirms acute mucosal inflammation. Which of the following is a potential complication of this condition requiring regular surveillance?
Toxic megacolon
Perianal fistula
Sclerosing cholangitis
Uveitis
Colorectal carcinoma
A 27 -year-old male returning home after a three-month visit to Puerto Rico presents with diarrhea for the past 6 weeks. Other accompanying symptoms include cramps, gas, fatigue and progressive weight loss. Abdominal auscultation shows hyperactive bowel sounds, and borborygmi. The family history is unremarkable for intestinal disease. Laboratory studies show anemia with a hematocrit of 25% and MCV of 105fl; stool examination for ova and parasites is negative. Small intestinal mucosal biopsy shows blunting of villi with infiltration of chronic inflammatory cells, including lymphocytes, plasma cells, and eosinophils. Which of the following is the most likely diagnosis?
Celiac disease
Amoebiasis
Tropical sprue
Bacterial overgrowth
Giardiasis
A 46-year -old alcoholic man comes to the emergency department because of several episodes of vomiting. The last episode of emesis contained blood. Five hours ago, he had a fatty meal and several alcoholic drinks. Two days ago, he had an upper GI tract endoscopy and abdominal ultrasound for the evaluation of dyspepsia. The endoscopy was unremarkable, and the ultrasound showed a hyperechogenic enlarged liver and stones in the gallbladder. His temperature is 36.6C (97.9F), blood pressure is 120/70 mm Hg, pulse is 95/min, and respirations are 15/min. Laboratory studies show: Hb 12.8 g/dl WBC 5,400/cmm BUN 26 mg/dl Creatinine 1.1 mg/dl AST 100 U/L ALT 45 U/L Bilirubin 0.7 mg/dl Nasogastric suction shows normal stomach contents mixed with bright red blood. The rectal examination shows no melena. Which of the following is the most likely explanation for this patient's bloody vomiting?
Ruptured submucosal esophageal veins
Endoscopy-related esophageal perforation
Stress gastritis
Hemobilia
Tears in the mucosa of the cardia
A 45-year-old male presents to the office with complaints of progressive difficulty in swallowing both solids and liquids. His other complaints include occasional regurgitation of undigested food, and a nighttime cough which disturbs his sleep. The physical examination is unremarkable. Barium studies show a dilated esophagus, loss of esophageal peristalsis, and smooth tapering of the distal esophagus. Which of the following is the most appropriate next step in management?
Esophagoscopy
Esophageal manometry
Esophageal pH monitoring
Botulinum toxin injection
Pneumatic dilation
A 53-year-old woman presents to your office with right-sided abdominal pain that started two days ago. She describes the pain as constant and burning in nature. There is no associated nausea, vomiting or diarrhea. The patient reports taking over-the-counter antacids and ibuprofen, which brought no relief. Her medical history is significant for breast cancer diagnosed one year ago, for which she underwent a modified radical mastectomy and is receiving chemotherapy, the last course of which was completed two months ago. On physical examination, her temperature is 36.7C (98.F), blood pressure is 120/70 mm Hg, pulse is 80/min, and respirations are 16/min. Her lung fields are clear to auscultation and her abdomen is soft and non-distended. The liver span is 10 cm and the spleen is not palpable. Lightly touching the skin to the right of the umbilicus elicits intense pain. In one week the patient is most likely to develop:
Intestinal obstruction
Skin lesions
Fever and jaundice
Ascites
Black stool
A 76-year-old man with multi-infarct dementia is brought to the emergency department because of lethargy. For the past 6 months, he has had difficulties with feeding and occasionally regurgitates undigested food. In recent days, his condition has deteriorated, and he has become lethargic. He has a history of hypertension for 15 years, chronic atrial fibrillation for 7 years, dementia for 5 years, and frequent respiratory tract infections for the past year. His temperature is 37.8C (101.5F), blood pressure is 150/95 mm Hg, pulse is 120/min, and respirations are 26/min. Physical examination shows foul-smelling breath; there is a fluctuating mass in the left side of his neck. Auscultation shows crackles in the right lung base. An x-ray film of the chest shows multiple infiltrates without cavitation in the right lower lung field. The patient is admitted, sputum and blood cultures are sent, and antibiotics are started. Which of the following is the most appropriate next step in management?
Puncture of the neck mass
Esophagoscopy
Esophagography
Bronchoscopy
T of the neck
A 69-year-old man has had pain in left lower quadrant (LLQ) for 3 days. The pain was intermittent, but since yesterday it has been constant. He also had sweating and chills for the last 2 days. He hasn't had a bowel movement for 4 days, but has passed flatus. He vomited once and still has nausea. His past medical history is remarkable for constipation and nephrolithiasis. His vital signs are: PR: 110/min; BP: 122/80mm Hg; RR: 24/min; Temperature: 38.6C (101.3F). His abdomen is soft and tender to palpation in the left lower quadrant. Deep palpation is difficult but reveals no masses or organomegaly. Bowel sounds are decreased. Rectal exam is positive for enlarged prostate. Costovertebral angle tenderness is absent. Ultrasound shows bilateral hydronephrosis and stones in the kidneys. His laboratory test results are: WBC 14,500/cmm Hb 11.7gm/dl Hct 34% ESR 40/hour BUN43 mg/dl Creatinine 2.0 mg/dl Urinalysis RBC 4-10/hpf; WBC 3/hpf; few hyaline casts; many oxalate crystals. The next step should be:
Intravenous pyelography
Sigmoidoscopy
Contrast enema
CT of abdomen
Upright abdominal film
A 33-year-old male is admitted to the hospital after an episode of tonic-clonic seizures. He is a known IV drug abuser. He admits 'shooting' cocaine and heroin prior to the seizure. He has never had seizures before. Fallowing the seizure, he complains of muscle pain but otherwise feels normal. His temperature is 37.2°C (98.9°F) and his blood pressure is 156/90 mm Hg. Laboratory analyses reveal the following: CPK 11,200 U/ml AST 545 U/L ALT 560U/L Troponin T normal Anti-HAV antibodies negative HBsAg negative Anti-HBsAg negative Anti-HCV antibodies positive He reports that a recent HIV test was negative. Which of the following is the best management for this patient?
Fluid restriction
Metoprolol
Hepatitis B vaccination
Life-long phenytoin therapy
No intervention
A 46-year-old white male presents with chronic diarrhea, abdominal distention, flatulence, and weight loss. He also has arthralgias and bulky, frothy stools. He has never had blood transfusions, tattooing or highrisk sexual behaviors. His temperature is 38.3C (101F), blood pressure is 130/90 mm Hg, pulse is 84/min, and respirations are 16/min. Physical examination shows generalized lymphadenopathy and skin hyperpigmentation Which of the following is the most appropriate diagnostic test?
SerumTSH
Antinuclear antibody (ANA) titer
Gamma-glutamyl transpeptidase levels
ELISA for anti-HIV antibodies
Endoscopy with small bowel biopsy
A 40-year-old male comes to the physician complaining of diarrhea with pale, voluminous, foul-smelling stools that are difficult to flush. He has had this problem sporadically for years, but has neglected medical care. He also has severe, intermittent, epigastric pain lasting 15 to 30 minutes after eating. He admits to chronic alcohol consumption. Physical examination shows no abnormalities. Which of the following is the best test to confirm fat malabsorption in this patient?
Sudan Ill stain
72-hour fecal fat collection
Acid steatocrit
D-xylose test
Lactose tolerance test
A 37-year-old male prisoner has been complaining of fever, chills and abdominal pain over the last week. He vomited once before reaching the emergency room. On physical examination, his blood pressure is 112/63 mmHg and his heart rate is 115/min. Breath sounds are diminished at the left lung base and there is marked left upper quadrant tenderness. Laboratory values are given below: WBC count 23,500/mm3 Neutrophils 65% Bands 11% Hemoglobin 12.5 mg/dL Platelets 250,000/mm3 Total bilirubin 3.1 mg/dL AST 46 units/L AL T 70 units/L Alkaline phosphatase 120 units/L CT scan of the abdomen reveals a fluid collection within the spleen. Which of the following is the most likely diagnosis?
Functional asplenia
Infectious endocarditis
Lnflammatory bowel disease
Portal hypertension
Infectious mononucleosis
A 20-year-old Caucasian male presents with lower abdominal pain for the past few hours. The pain first started around the umbilicus, but then shifted to the right lower abdominal area. He has had one episode of vomiting. Physical examination shows tenderness at McBurney's point. CT scan of the abdomen confirms the diagnosis of acute appendicitis. Which of the following explains the pathophysiology of the shifting of pain from the periumbilical area to the right lower quadrant in acute appendicitis?
Movement of inflammed appendix with bowel movements
Visceral followed by somatic pain
Somatic followed by visceral pain
Referred pain
Rupture of appendix with pus draining into right lower quadrant
A 40-year-old female presents with a 12-month history of episodes of chest pain and dysphagia. The episodes last from a few seconds to a few minutes. She has not had weight loss, fevers or chills. Chest-x ray, ECG and barium swallow show no abnormalities. Manometric studies show simultaneous high amplitude contractions with normal relaxation of the lower esophageal sphincter. Which of the following is the most likely diagnosis?
Zenker's diverticulum
Diffuse esophageal spasm
Achalasia
Scleroderma
Infectious esophagitis
A 29-year-old man presents to the ED complaining of RLQ pain for 24 hours. He states that the pain first began as a dull feeling around his umbilicus and slowly migrated to his right side. He has no appetite, is nauseated, and vomited twice. His BP is 130/75 mm Hg, HR is 95 beats per minute, temperature is 100.9°F, and his RR is 16 breaths per minute. His WBC is 14,000/μL. As you palpate the LLQ of the patient’s abdomen, he states that his RLQ is painful. What is the name of this sign?
Blumberg sign
Psoas sign
Obturator sign
Raynaud sign
Rovsing sign
A 40-year-old man with long-standing alcohol abuse complains of abdominal swelling, which has been progressive over several months. He has a history of gastrointestinal bleeding. On physical examination, there are spider angiomas and palmar erythema. Abdominal collateral vessels are seen around the umbilicus. There is shifting dullness, and bulging flanks are noted. Which of the following is the most important first step in the patient’s evaluation?
Diagnostic paracentesis
Upper GI series
Ethanol level
CT scan of the abdomen
Examination of peripheral blood smear
A 70-year-old man presents with a complaint of fatigue. There is no history of alcohol abuse or liver disease; the patient is taking no medications. Scleral icterus is noted on physical examination; the liver and spleen are nonpalpable. The patient has a normocytic, normochromic anemia. Urinalysis shows bilirubinuria with absent urine urobilinogen. Serum bilirubin is 12 mg/dL, AST and ALT are normal, and alkaline phosphatase is 300 U/L (three times normal). Which of the following is the best next step in evaluation?
Ultrasound or CT scan of the abdomen
Viral hepatitis profile
Reticulocyte count
Serum ferritin
Antimitochondrial antibodies
A 54-year-old man is brought to the ER because of an episode of coffee ground emesis and lightheadedness. He has a history of intravenous drug use, hepatitis C infection, and alcohol use. He says he has not had an alcoholic drink for about three days. He has been noncompliant with medications and follow-ups. He takes no medications. His temperature is 36.7C (98F), pulse is 110/min, respirations are 16/min, and blood pressure is 90/60 mmHg. Scleral icterus is present. Examination shows coffee ground material in the oropharynx. His lungs are clear. His abdomen is distended and a fluid wave is present. He is slightly tender to palpation in the epigastrium. Laboratory studies show: Complete blood count: Leukocyte count 9,500/mm3 Hemoglobin 10.0 g/L Platelets 120,000/mm3 Chemistry panel: Serum sodium 140 mEq/L Serum potassium 3.5 mEq/L Bicarbonate 27 mEq/L Blood urea nitrogen (BUN) 34 mg/dL Serum creatinine 0.8 mg/dL Coagulation studies : Prothrombin time 27 sec Partial thromboplastin time 42 sec Which of the following is the most appropriate next step in the management of this patient?
Whole blood transfusion
Fresh frozen plasma infusion
Hemodialysis
Pooled platelet transfusion
Plasmapheresis
A 55-year-old man with hypertension and end-stage renal disease requiring hemodialysis presents with 2 days of painless hematochezia. He reports similar episodes of bleeding in the past, which were attributed to angiodysplasia. He denies abdominal pain, nausea, vomiting, diarrhea, and fever. His vitals include HR of 90 beats per minute, BP of 145/95 mm Hg, RR of 18 breaths per minute, and temperature of 98°F. His abdomen is soft and nontender and his stool is grossly positive for blood. Which of the following statements are true regarding angiodysplasia?
They are responsible for over 50% of acute lower GI bleeding
They are more common in younger patients.
Angiography is the most sensitive method for identifying angiodysplasias.
They are less common in patients with end-stage renal disease.
The majority of angiodysplasias are located on the right side of the colon
A 70-year-old woman presents to the ED with dark stool for 3 weeks. She occasionally notes bright red blood mixed with the stool. Review of systems is positive for decreased appetite, constipation, and a 10-lb weight loss over 2 months. She denies abdominal pain, nausea, vomiting, and fever, but feels increased weakness and fatigue. She also describes a raspy cough with white sputum production over the previous 2 weeks. Examination reveals she is pale, with a supine BP of 115/60 mm Hg and HR of 90 beats per minute. Standing BP is 100/50 mm Hg, with a pulse of 105 beats per minute. Which of the following is the most likely diagnosis?
Hemorrhoids
Diverticulitis
Mallory-Weiss tear
Diverticulosis
Adenocarcinoma
A 52-year-old man has episodes of severe chest pain associated with dysphagia. He has been seen twice in the emergency room, and both times the symptoms responded to sub-lingual nitroglycerin. He then had a full cardiac evaluation including electrocardiogram (ECG), cardiac biomarkers, and an exercise stress test, which were all normal. Which of the following is the most likely diagnosis?
Herpetic infection
A motor disorder
Midesophageal cancer
Peptic stricture
External esophageal compression
A 16-year old girl has recently been referred to your family practice. She is a recent immigrant from Southeast Asia, and has been taking isoniazid (INH) and rifampin for uncomplicated tuberculosis. Routine blood tests are unremarkable, except for an elevated direct bilirubin. Other liver enzymes and function tests are completely normal. Which of the following is the most likely diagnosis?
Hemolytic anemia
INH toxicity
Crigler-Najjar syndrome type I
Rifampin toxicity
Rotor’s syndrome
A 45-year-old woman presents with a 1-week history of jaundice, anorexia, and right upper quadrant discomfort. On examination she is icteric, with a tender right upper quadrant and liver span of 14 cm. There is no shifting dullness or pedal edema and the heart and lungs are normal. On further inquiry, she reports consuming one bottle of wine a day for the past 6 months. Which of the following lab- oratory tests are most likely to be characteristic of a patient with jaundice secondary to alcoholic hepatitis? 64
Ratio of AST: ALT is 3:1 and the AST is 500 U/L
Ratio of AST: ALT is 2:1 and the AST is 250 U/L
Ratio of AST: ALT is 1:1 and the AST is 500 U/L
Ratio of AST: ALT is 1:1 and the AST is 250 U/L
Ratio of AST: ALT is 1:3 and the AST is 750
A husband and wife present to the ED with 1 day of subjective fever, vomiting, watery diarrhea, and abdominal cramps. They were at a restaurant a day before for dinner and both ate the seafood special, which consisted of raw shellfish. In the ED, they are both tachycardia with temperatures of 99.8°F and 99.6°F for him and her, respectively. Which of the following is responsible for the majority of acute episodes of diarrhea?
Parasites
Viruses
Enterotoxin-producing bacteria
Anaerobic bacteria
Invasive bacteria
A 78-year-old woman is brought to the ED by EMS complaining of vomiting and abdominal pain that began during the night. EMS reports that her BP is 90/50 mm Hg, HR is 110 beats per minute, temperature is 101.2°F, and RR is 18 breaths per minute. After giving her a 500 mL bolus of NS, her BP is 115/70 mm Hg. During the examination, you notice that her face and chest appear jaundiced. Her lungs are clear to auscultation and you do not appreciate a murmur on cardiac examination. She winces when you palpate her RUQ. An ultrasound reveals dilation of the common bile duct and stones in the gallbladder. What is the most likely diagnosis?
Cholecystitis
Acute hepatitis
Cholangitis
Pancreatic cancer
Bowel obstruction
A 62-year-old man with a history of hypertension presents to the ED with severe constant mid-epigastric pain for the past hour. Over the last several months, he has had intermittent pain shortly after eating, but never this severe. He states he now has generalized abdominal pain that began suddenly about 15 minutes ago. He has no history of trauma, has never had surgery, and takes no medications. His vitals include HR of 115 beats per minute lying supine, increasing to 135 when sitting up, BP of 170/105 mm Hg supine, falling to 145/85 mm Hg when sitting up. He appears pale. His abdomen is rigid and diffusely tender with guarding and rebound. Bowel sounds are absent and stool hemoccult is positive. The white blood cell (WBC) count is 8500/μL, hemoglobin 8.5 mg/dL, hematocrit 27%, and platelets 255/μL. Which of the following is the most likely diagnosis?
Boerhaave syndrome
Perforated gastric ulcer
Abdominal aortic aneurysm (AAA)
Inflammatory bowel disease (IBD)
Diverticulosis
A 60-year-old man with a history of alcohol abuse presents to the ED with hematemesis for 1 day. He denies abdominal or chest pain. On physical examination, his eyes appear reddened which he attributes to having drunken heavily the night before (he also reveals vomiting several times after this recent binge). Vital signs are HR 115 beats per minute, BP 130/85 mm Hg, RR 18 breaths per minute, and temperature 99.5°F. Chest radiograph is unremarkable. Laboratory results reveal a WBC 10,000/μL, haemoglobin 14 mg/dL, hematocrit 40%, and platelets 210/μL. Which diagnosis is endoscopic evaluation most likely to confirm?
Esophageal varices
Boerhaave syndrome
Curling ulcer
Perforated gastric ulcer
Mallory-Weiss tear
A 40-year-old man with a recent history of exploratory laparotomy for a stabbing injury presents to the emergency department with diffuse cramping abdominal pain for 1 day, accompanied by nausea, multiple episodes of brown colored vomitus, and lack of stool, but he reports some flatulence. He denies any fever. On physical examination, the patient has stable vital signs, and there is diffuse distention in the abdomen with guarding and tenderness but no rebound, as well as high-pitched bowel sounds. Rectal examination reveals no fecal impaction in the rectal vault, and the stool was guaiac-negative. Complete blood cell count reveals no significant abnormalities and serum chemistry shows a mild metabolic alkalosis. CT demonstrates a noticeable difference in the diameter of proximal and distal small bowel. Which of the following is the most appropriate management?
Broad-spectrum antibiotics
Colonoscopy
Exploratory laparotomy with lysis of adhesions
Give the patient nothing by mouth, insert a nasogastric tube, and perform intravenous correction of electrolyte abnormalities
Serial abdominal examinations
The physician on call is called to the well-baby nursery because a full-term, African-American boy who is 49 hours old has not passed meconium. The pregnancy was uncomplicated. The neonate’s blood pressure is 70/50 mm Hg, heart rate is 140/min, and respiratory rate is 36/ min. The neonate is crying but is easily consolable. His abdomen is markedly distended. A barium enema is ordered, which shows dilated proximal bowel and a narrowed distal segment. Which of the following would provide a definitive diagnosis in this child?
Absent ganglion cells on rectal biopsy
Absent ligament of Treitz on upper gastro- intestinal series
Air bubbles in the stomach and duodenum on x-ray film of the abdomen
Positive sweat test
Telescoping of bowel on air contrast barium enema
A 73-year-old man comes to his primary care physician for his yearly check-up. His medical history is significant for obesity, new onset diabetes mellitus, and a remote history of tobacco use. The patient has noticed that his stool has been darker for the past 3 months, although he has only seen gross blood in his stool once, a week ago. He also complains of recent fatigue and occasional light-headedness when standing up from sitting. On examination the patient has fecal occult blood and a hematocrit of 32%. Colonoscopy and upper gastrointestinal endoscopy reveal no obvious pathology. Which of the following is the best diagnostic test to locate this patient’s hemorrhage?
Angiography
Barium enema
Colonoscopy
CT scan with contrast
Tagged RBC scan
A pregnant 16-year-old girl with no prior pre- natal care presents to the emergency department in labor. A male infant is delivered precipitously. Prenatal laboratory test results are unknown. There is no meconium. He has a birth weight of 3 kg (6 lb 10 oz). He is pink and is crying, heart rate is 130/min, and respiratory rate is 36/min, with good respiratory effort. The emergency medicine resident notices the infant has ascites and a membranecovered anterior abdominal mass at the base of his umbilical cord. Which of the following is the most likely diagnosis?
Duodenal atresia
Gastroschisis
Hirschsprung’s disease
Meckel’s diverticulum
Omphalocele
A 50-year-old man is brought to the ED by ambulance with significant hematemesis. In the ambulance, paramedics placed two large-bore IVs and began infusing normal saline. In the ED, his HR is 127 beats per minute, BP is 79/45 mm Hg, temperature is 97.9°F, RR is 24 breaths per minute, and oxygen saturation is 96%. On physical examination, his abdomen is nontender, but you note spider angiomata, palmar erythema, and gynecomastia. Laboratory results reveal WBC 9000/μL, hematocrit 28%, platelets 40/μL, aspartate transaminase (AST) 675 U/L, alanine transaminase (ALT) 325 U/L, alkaline phosphatase 95 U/L, total bilirubin 14.4 mg/dL, conjugated bilirubin 12.9 mg/dL, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 110 mEq/L, bicarbonate 26 mEq/L, blood urea nitrogen (BUN) 20 mg/dL, creatinine 1.1 mg/dL, and glucose 150 mg/dL. Which of the following is the most likely diagnosis?
Perforated gastric ulcer
Diverticulosis
Splenic laceration
Esophageal varices
Ruptured AAA
A 70-year-old woman with a history of hypertension, congestive heart failure, and atrial fibrillation presents to the ED with several hours of acute onset diffuse abdominal pain. She denies any nausea or vomiting. The pain is constant, but she is unable to localize it. She was diagnosed with a renal artery thrombosis several years ago. Vital signs include HR of 95 beats per minute, BP of 110/70 mm Hg, and temperature of 98°F. Her abdomen is soft and mildly tender, despite her reported severe abdominal pain. Her WBC count is 12,000/μL, hematocrit 38%, platelets 250/μL, and lactate 8 mg/dL. The stool is traced heme-positive. You are concerned for acute mesenteric ischemia. What is the best way to diagnose this condition?
Serum lactate levels
Abdominal radiograph (supine and upright)
CT scan
Angiography
Barium contrast study
An 81-year-old diabetic woman with a history of atrial fibrillation is transferred to your emergency department (ED) from the local nursing home. The note from the facility states that the patient is complaining of abdominal pain, having already vomited once. Her vital signs in the ED are temperature 100.1°F, blood pressure (BP) 105/75 mm Hg, heart rate (HR) 95 beats per minute, and respiratory rate (RR) 18 breaths per minute. You examine the patient and focus on her abdomen. Considering that the patient has not stopped moaning in pain since arriving to the ED, you are surprised to find that her abdomen is soft on palpation. You decide to order an abdominal radiographic series. Which of the findings on plain abdominal film is strongly suggestive of mesenteric infarction?
Sentinel loop of bowel
No gas in the rectum
Presence of an ileus
Pneumatosis intestinalis
Air fluid levels
As you palpate the right upper quadrant (RUQ) of a 38-year-old woman’s abdomen, you notice that she stops her inspiration for a brief moment. During the history, the patient states that over the last 2 days she gets pain in her RUQ that radiates to her back shortly after eating. Her vitals include a temperature of 100.4°F, HR of 95 beats per minute, BP of 130/75 mm Hg, and RR of 16 breaths per minute. What is the initial diagnostic modality of choice for this disorder?
Plain film radiograph
Computed tomography (CT) scan
Magnetic resonance imaging (MRI)
Radioisotope cholescintigraphy (HIDA scan)
Ultrasonography
An undomiciled 41-year-old man walks into the ED complaining of abdominal pain, nausea, and vomiting. He tells you that he has been drinking beer continuously over the previous 18 hours. On examination, his vitals are BP 150/75 mm Hg, HR 104 beats per minute, RR 16 breaths per minute, oxygen saturation 97% on room air, temperature of 99.1°F rectally, and finger stick glucose 81 mg/dL. The patient is alert and oriented, his pupils anicteric. You notice gynecomastia and spider angiomata. His abdomen is soft but tender in the RUQ. Laboratory tests reveal an AST of 212 U/L, ALT 170 U/L, alkaline phosphatase of 98 U/L, total bilirubin of 1.9 mg/dL, international normalized ratio (INR) of 1.3, WBC 12,000/μL. Urinalysis shows 1+ protein. Chest x-ray is unremarkable. Which of the following is the most appropriate next step in management?
Place a nasogastric tube in the patient’s stomach to remove any remaining ethanol.
Order a HIDA scan to evaluate for acute cholecystitis.
Administer hepatitis B immune globulin.
Send viral hepatitis titers.
Provide supportive care by correcting any fluid and electrolyte imbalances.
A 23-year-old woman presents to the ED complaining of lower abdominal pain and vaginal spotting for 2 days. Her menstrual cycle is irregular. She has a history of ovarian cysts and is sexually active but always uses condoms. Her BP is 115/75 mm Hg, HR is 75 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. Which of the following tests should be obtained next?
Chlamydia antigen test.
β-Human chorionic gonadotropin (β-hCG)
Transvaginal ultrasound.
Abdominal radiograph.
Observe her abdominal pain, if it resolves discharge her with a diagnosis of menstruation.
A 71-year-old obese man is brought to the ED complaining of constant left mid quadrant (LMQ) abdominal pain with radiation into his back. His past medical history is significant for hypertension, peripheral vascular disease, peptic ulcer disease, kidney stones, and gallstones. He smokes a pack of cigarettes and consumes a pint of vodka daily. His BP is 145/80 mm Hg, HR is 90 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. Abdominal examination is unremarkable. An ECG is read as sinus rhythm with an HR of 88 beats per minute. An abdominal radiograph reveals normal loops of bowel and curvilinear calcification of the aortic wall. Which of the following is the most likely diagnosis?
Biliary colic
Nephrolithiasis
Pancreatitis
Small bowel obstruction (SBO)
Abdominal aortic aneurysm
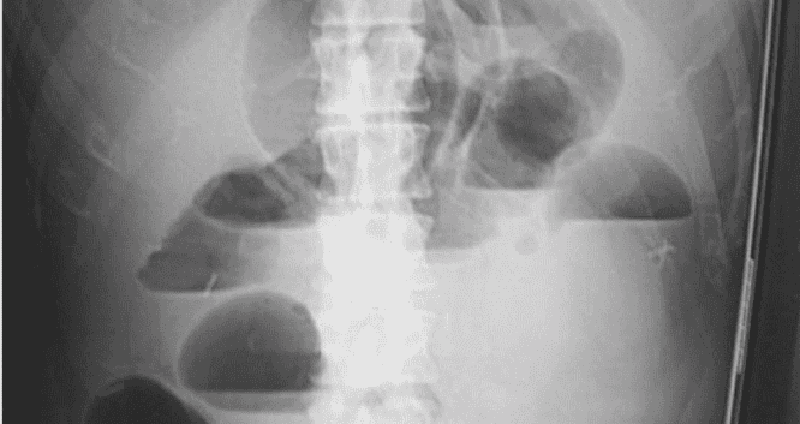
A 73-year-old man is seen in the ED for abdominal pain, nausea, and vomiting. His symptoms have progressively worsened over the past 2 to 3 days. The pain is diffuse and comes in waves. He denies fever or chills, but has a history of constipation. He reports no flatus for 24 hours. Physical examination is notable for diffuse tenderness and voluntary guarding. There is no rebound tenderness. An abdominal radiograph is seen below. Which of the following is the most likely diagnosis?
Constipation
SBO
Cholelithiasis
Large bowel obstruction
Inflammatory bowel disease
For which of the following patients is an abdominal CT scan contraindicated?
A 52-year-old man with abdominal pain after blunt trauma, negative focused assessment with sonography for trauma (FAST) examination, BP 125/78 mm Hg, and HR 109 beats per minute
A 22-year-old woman with RLQ pain, negative β-hCG, temperature 100.6°F
A 45-year-old man with abdominal pain, temperature 100.5°F, WBC 11,200/μL, BP 110/70 mm Hg, HR 110 beats per minute, and lipase 250 IU
A 70-year-old man with abdominal pain, an 11-cm pulsatile mass in the epigastrium, BP of 70/50 mm Hg, and HR of 110 beats per minute
A 65-year-old woman with right flank pain that radiates to her groin, microhematuria, BP 165/85 mm Hg, and HR 105 beats per minute
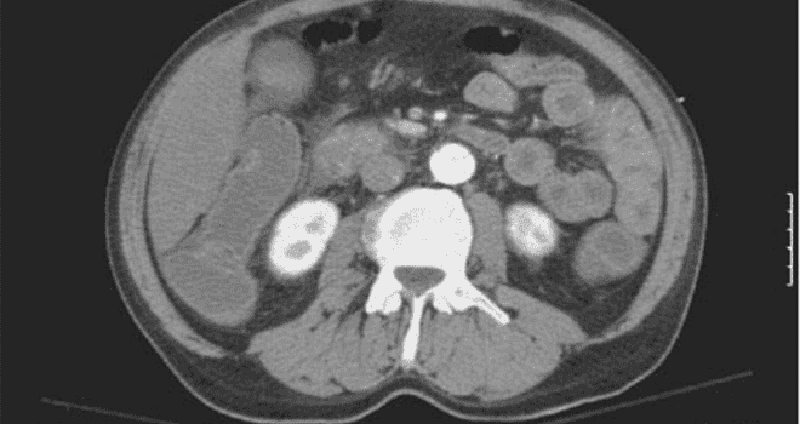
A 63-year-old man is brought to the ED by EMS complaining of severe abdominal pain that began suddenly 6 hours ago. His BP is 145/75 mm Hg and HR is 105 beats per minute and irregular. On examination, you note mild abdominal distention and diffuse abdominal tenderness without guarding. Stool is heme positive. Laboratory results reveal WBC 12,500/μL, haematocrit 48%, and lactate 4.2 U/L. ECG shows atrial fibrillation at a rate of 110.A CT scan is shown below. Which of the following is the most likely diagnosis?
Abdominal aortic aneurysm
Mesenteric ischemia
Diverticulitis
SBO
Crohn disease
A 21-year-old woman presents to the ED complaining of diarrhea, abdominal cramps, fever, anorexia, and weight loss for 3 days. Her BP is 127/75 mm Hg, HR is 91 beats per minute, and temperature is 100.8°F. Her abdomen is soft and nontender without rebound or guarding. WBC is 9200/μL, β-hCG is negative, urinalysis is unremarkable, and stool is guaiac positive. She tells you that she has had this similar presentation four times over the past 2 months. Which of the following extraintestinal manifestations is associated with Crohn disease but not ulcerative colitis?
Ankylosing spondylitis
Erythema nodosum
Nephrolithiasis
Thromboembolic disease
Uveitis
An 84-year-old woman with coronary artery disease, congestive heart failure, peripheral vascular disease, and atrial fibrillation presents to the emergency department with dizziness, weakness, and sudden-onset crampy periumbilical pain. The pain is associated with one episode of diarrhea and one episode of emesis. The patient notes she has been having similar pain after meals for “several months” but never this severe. Her temperature is 37.2°C (98.9°F), heart rate is 135/min, blood pressure is 96/60 mm Hg, and respiratory rate is 16/min. Physical examination is notable for a slightly distended abdomen that is extremely tender to palpation with diminished bowel sounds. There is no rigidity or rebound tenderness noted on the abdominal examination. In addition, the patient has heme positive stool. Her WBC count is 19,500/mm³, hemoglobin is 10.9 g/dL, and platelet count is 159,000/mm³. Liver function testing results are normal. After stabilizing the patient, what is the best next step in management?
Barium enema
Colonoscopy
Laparotomy
Obstruction series
Warfarin therapy
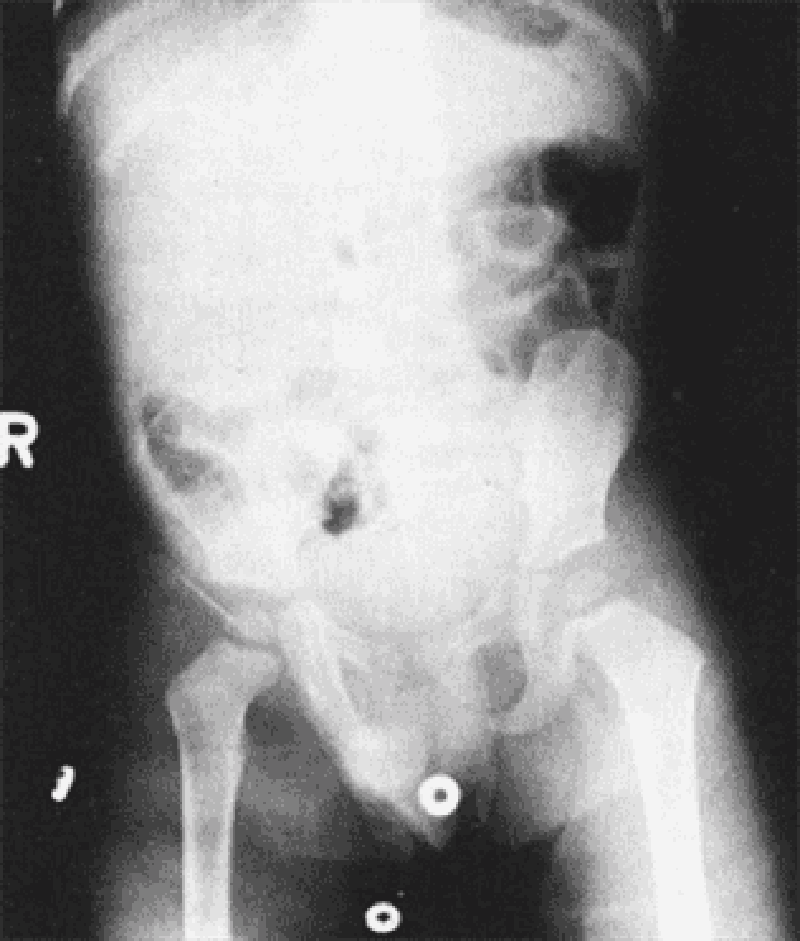
A 2-year-old boy is brought to the emergency department. His mother reports that the patient had been well until 3 days ago, when he developed a fever and nasal congestion. He was diagnosed with otitis media in his right ear, and was started on amoxicillin with clavulanic acid by his pediatrician. He appeared to be improving until this morning, when he began to complain of abdominal pain. The pain has been intermittent, with episodes occurring every 20 minutes for several minutes each time. However, the episodes appear to be worsening and lasting longer with increasing pain. Thirty minutes ago he had an episode of nonbloody, nonbilious emesis that was followed by passage of blood- and mucus-stained stools. He is currently in no acute distress, and his vital signs are normal. A firm sausage-shaped mass is palpable in the RUQ of his abdomen. A rectal examination yields bloody mucus. He does not have any skin lesions or rashes. X-ray of the abdomen is shown in the image. Which of the following is the most likely diagnosis?
Cystic fibrosis
Enterocolitis
Henoch-Schönlein purpura
Idiopathic intussusception
Meckel’s diverticulum
A 59-year-old man presents for his routine colonoscopy and during his visit he has numerous large adenomas removed from his colon. Which of the following is the most effective strategy for follow-up of this patient?
Elective colectomy
Repeat colonoscopy in 10 years
Repeat colonoscopy in 3 years
Sigmoidoscopy in 10 years
Urgent colectomy
A 67-year-old woman is currently postoperative day 8 after an emergent laparoscopic cholecystectomy for acute cholecystitis. On postoperative day 2 she spiked a temperature of 40°C (101.4°F) and began to complain of some shortness of breath. X-ray of the chest revealed right lower lobe pneumonia, and the patient was started on clindamycin. Today she is experiencing multiple episodes of foul-smelling, watery diarrhea that is green tinged but non-bloody. She also complains of lower abdominal cramping. Her temperature is 37.8°C (100°F), pulse is 90/min, respiratory rate is 15/min, and blood pressure is 110/70 mm Hg. Which of the following is the most likely explanation for these findings?
Ingestion of preformed enterotoxins, cytotoxins, and/or neurotoxins
Production of cytotoxins within the gastro- intestinal tract
Production of enterotoxins and cytotoxins within the gastrointestinal tract
Production of enterotoxins within the gastrointestinal tract
Viral invasion and damage of villous epithelial cells within the gastrointestinal tract

A male infant is delivered at 37 weeks’ gestation via cesarean section for breech presentation. The pregnancy was complicated by polyhydramnios. The 34-year-old mother is rubella immune and has blood type B. She is negative for Rh antibody, Group B streptococci, rapid plasma reagin, hepatitis B surface antigen, gonorrhea, and Chlamydia. At delivery there is no meconium. He has a birth weight of 2.7 kg (6 lb). The baby has a weak cry and is pale and frothing at the nose and mouth. He has nasal flaring and retractions, with a respiratory rate of 56/min. Heart rate is 140/min and he has a regular rhythm and a harsh 2/6 holosystolic murmur that is best heard at the left sternal border. On auscultation he has fine diffuse crackles in his lungs bilaterally. The infant is missing both thumbs and has fusion of the remaining digits of his upper extremities bilaterally. The pediatric resident is able to suction secretions from the patient’s nasopharynx and oropharynx; however, she is unable to pass a nasogastric or orogastric tube more than 10 cm down. X-ray of the chest is shown in the image. Which of the following is the most likely diagnosis?
Congenital diaphragmatic hernia
Pyloric stenosis
Respiratory distress syndrome
Tracheoesophageal fistula
Transient tachypnea of the new-born
A 51-year-old man is brought to the emergency department (ED) by emergency medical services (EMS) with a blood pressure (BP) of 90/60 mm Hg, heart rate (HR) of 110 beats per minute, respiratory rate (RR) of 18 breaths per minute, and oxygen saturation of 97% on room air. The patient tells you that he has a history of bleeding ulcers. On examination, his abdomen is tender in the epigastric area. He is guaiac positive, with black stool. He has a bout of hematemesis and you notice that his BP is now 80/50 mm Hg, HR is 114 beats per minute, as he is slowly starting to drift off. Which of the following is the most appropriate next step in therapy?
Assess airway, establish two large-bore intravenous (IV) lines, cross-match for two units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy.
Assess airway, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor.
Place two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy.
Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, administer 1 to 2 L of normal saline, and schedule an emergent endoscopy.
Intubate the patient, establish two large-bore IVs, cross-match for 2 units of blood, and administer a proton pump inhibitor.
A 19-year-old woman presents to the ED with 1 hour of acute-onset progressively worsening pain in her RLQ. She developed nausea shortly after the pain and vomited twice over the last hour. She had similar but less severe pain 2 weeks ago that resolved spontaneously. Her BP is 123/78 mm Hg, HR is 99 beats per minute, temperature is 99.1°F, and her RR is 16 breaths per minute. On physical examination, the patient appears uncomfortable, not moving on the gurney. Her abdomen is nondistended, diffusely tender, worst in the RLQ. Pelvic examination reveals a normal-sized uterus and moderate right-sided adnexal tenderness. Laboratory results reveal WBC 10,000/μL, hematocrit 38%, and a negative urinalysis and β-hCG. Pelvic ultrasound reveals an enlarged right ovary with decreased flow. Which of the following is the most appropriate management for this patient?
Admit to the gynecology service for observation.
Administer IV antibiotics and operate once inflammation resolves.
Attempt manual detorsion.
Order an abdominal CT.
Go for immediate laparoscopic surgery.
A 23-year-old woman presents to the ED with RLQ pain for the last 1 to 2 days. The pain is associated with nausea, vomiting, diarrhea, anorexia, and a fever of 100.9°F. She also reports dysuria. The patient returned 1 month ago from a trip to Mexico. She is sexually active with one partner but does not use contraception. She denies vaginal bleeding or discharge. Her last menstrual period was approximately 1 month ago. She has a history of pyelonephritis. Based on the principles of emergency medicine, what are the three priority considerations in the diagnosis of this patient?
Perihepatitis, gastroenteritis, cystitis
Ectopic pregnancy, appendicitis, pyelonephritis
Pelvic inflammatory disease (PID), gastroenteritis, cystitis
Ectopic pregnancy, PID, menstrual cramps
Gastroenteritis, amebic dysentery, menstrual cramps
A 73-year-old woman presents to the emergency room with black tarry stools and symptoms of presyncope when standing up. Digital rectal examination confirms the presence of melena. She recently started using ibuprofen for hip discomfort. Upper endoscopy confirms the diagnosis of a gastric ulcer. Which of the following is the most likely explanation for the gastric ulcer?
Increasing acid production
Causing direct epithelial cell death
Promoting replication of Helicobacter pylori
an antiplatelet effect
Inhibiting mucosal repair
A 73-year-old woman presents to the emergency room with black tarry stools and symptoms of presyncope when standing up. Digital rectal examination confirms the presence of melena. She recently started using ibuprofen for hip discomfort. Upper endoscopy confirms the diagnosis of a gastric ulcer. Which of the following is the most likely explanation for the gastric ulcer?
Increasing acid production
Causing direct epithelial cell death
Promoting replication of Helicobacter pylori
an antiplatelet effect
Inhibiting mucosal repair
A 52-year-old woman is experiencing abdominal discomfort after meals as well as early in the morning. There is no weight loss or constitutional symptoms, and she has tried antacids but experienced minimal relief. Upper endoscopy reveals a duodenal ulcer and the biopsy is negative for malignancy. Which of the following is the most appropriate next step in management?
6–8 weeks of omeprazole or ranitidine
Long-term acid suppression with omeprazole
Antibiotic therapy
Antibiotic therapy with omeprazole
Bismuth citrate therapy
A 52-year-old woman is experiencing abdominal discomfort after meals as well as early in the morning. There is no weight loss or constitutional symptoms, and she has tried antacids but experienced minimal relief. Upper endoscopy reveals a duodenal ulcer and the biopsy is negative for malignancy. Which of the following is the most appropriate next step in management?
6–8 weeks of omeprazole or ranitidine
Long-term acid suppression with omeprazole
Antibiotic therapy
Antibiotic therapy with omeprazole
Bismuth citrate therapy
A 28-year-old man presents with symptoms of frequent bowel movements, crampy abdominal pain, and the passage of mucus. There is no history of any bloody diarrhea, but recently, he developed joint discomfort in his hands, knees, and back. On examination he is thin, and his abdomen is soft with voluntary guarding in the left lower quadrant. His joints are not actively inflamed and there is an asymmetric distribution. Which of the following is the most likely diagnosis?
Lymphoma of the bowel
Amyloid infiltration
Chronic pancreatitis
Ulcerative colitis
Tropical sprue
A 28-year-old man presents with symptoms of frequent bowel movements, crampy abdominal pain, and the passage of mucus. There is no history of any bloody diarrhea, but recently, he developed joint discomfort in his hands, knees, and back. On examination he is thin, and his abdomen is soft with voluntary guarding in the left lower quadrant. His joints are not actively inflamed and there is an asymmetric distribution. Which of the following is the most likely diagnosis?
Lymphoma of the bowel
Amyloid infiltration
Chronic pancreatitis
Ulcerative colitis
Tropical sprue
A 64-year-old white woman presents to her primary care physician complaining of difficulty and pain with swallowing, as well as occasional chest pain. She has a history of breast cancer treated with lumpectomy and radiation, hyper- tension, high cholesterol, and ovarian polyps. She indicates that her current problem started with liquids, but has progressed to solids, and that the food “just gets stuck in my throat.” The chest pain was once so bad that she took one of her husband’s nitroglycerin pills and the pain subsided, but it has since occurred many times. The physician orders an x-ray of the chest, but it is not diagnostic. Manometry is conducted, and it shows uncoordinated contractions. Which of the following is the most likely diagnosis?
Breast cancer relapse
Diffuse esophageal spasm
Esophageal cancer
Myocardial infarction
Nutcracker esophagus
A 64-year-old white woman presents to her primary care physician complaining of difficulty and pain with swallowing, as well as occasional chest pain. She has a history of breast cancer treated with lumpectomy and radiation, hyper- tension, high cholesterol, and ovarian polyps. She indicates that her current problem started with liquids, but has progressed to solids, and that the food “just gets stuck in my throat.” The chest pain was once so bad that she took one of her husband’s nitroglycerin pills and the pain subsided, but it has since occurred many times. The physician orders an x-ray of the chest, but it is not diagnostic. Manometry is conducted, and it shows uncoordinated contractions. Which of the following is the most likely diagnosis?
Breast cancer relapse
Diffuse esophageal spasm
Esophageal cancer
Myocardial infarction
Nutcracker esophagus
A 22-year-old woman is brought to the ED by ambulance complaining of sudden onset of severe abdominal pain for 1 hour. The pain is in the RLQ and is not associated with nausea, vomiting, fever, or diarrhea. On the pelvic examination you palpate a tender right adnexal mass. The patient’s last menstrual period was 6 weeks ago. Her BP is 95/65 mm Hg, HR is 124 beats per minute, temperature is 99.8°F, and RR is 20 breaths per minute. Which of the following are the most appropriate next steps in management?
Provide her oxygen via face mask and administer morphine sulfate.
Administer morphine sulfate, order an abdominal CT with contrast, and call an emergent surgery consult.
Send the patient’s urine for analysis and order an abdominal CT.
Bolus 2 L NS, order a type and crossmatch and β-hCG, and call gynecology for possible surgery
Provide oxygen via face mask, give morphine sulfate, and order a transvaginal ultrasound.
A 22-year-old woman is brought to the ED by ambulance complaining of sudden onset of severe abdominal pain for 1 hour. The pain is in the RLQ and is not associated with nausea, vomiting, fever, or diarrhea. On the pelvic examination you palpate a tender right adnexal mass. The patient’s last menstrual period was 6 weeks ago. Her BP is 95/65 mm Hg, HR is 124 beats per minute, temperature is 99.8°F, and RR is 20 breaths per minute. Which of the following are the most appropriate next steps in management?
Provide her oxygen via face mask and administer morphine sulfate.
Administer morphine sulfate, order an abdominal CT with contrast, and call an emergent surgery consult.
Send the patient’s urine for analysis and order an abdominal CT.
Bolus 2 L NS, order a type and crossmatch and β-hCG, and call gynecology for possible surgery
Provide oxygen via face mask, give morphine sulfate, and order a transvaginal ultrasound.
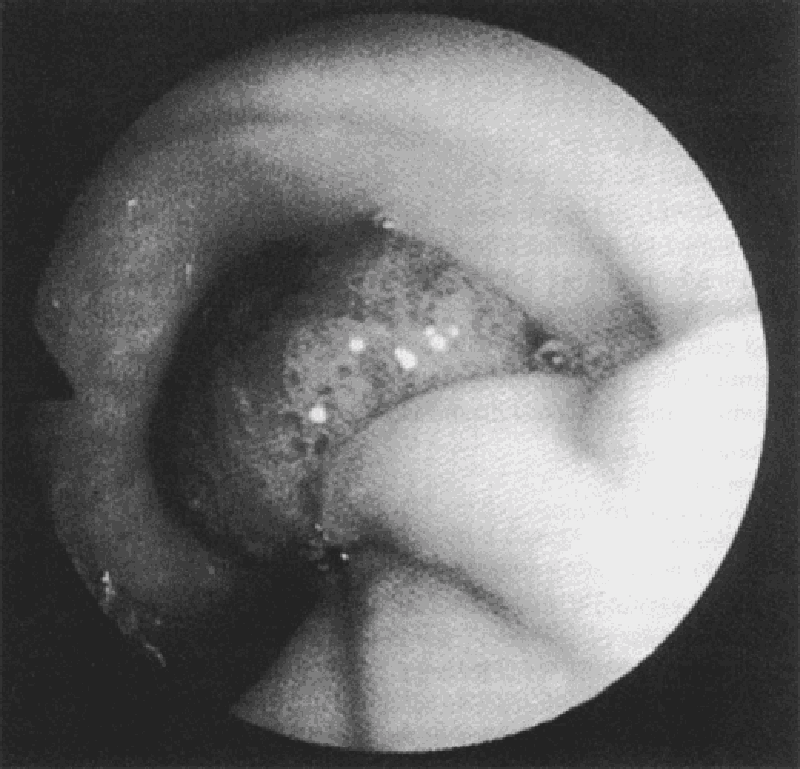
A 58-year-old white man complains of intermittent rectal bleeding and, at the time of colonoscopy, is found to have internal hemorrhoids and the lesion shown at the splenic flexure. Pathology shows tubulovillous changes. Repeat colonoscopy should be recommended at what interval?
In 1 to 2 months
In 1 year
In 3 years
In 10 years
Repeat colonoscopy is not necessary
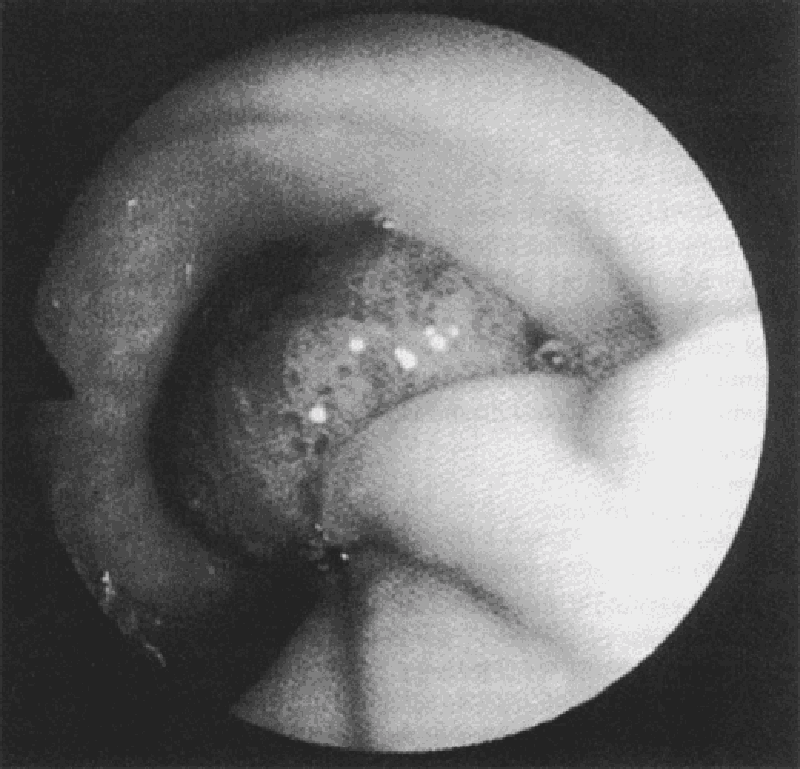
A 58-year-old white man complains of intermittent rectal bleeding and, at the time of colonoscopy, is found to have internal hemorrhoids and the lesion shown at the splenic flexure. Pathology shows tubulovillous changes. Repeat colonoscopy should be recommended at what interval?
In 1 to 2 months
In 1 year
In 3 years
In 10 years
Repeat colonoscopy is not necessary
A 36-year-old man presents for a well-patient examination. He gives a history that, over the past 20 years, he has had three episodes of abdominal pain and hematemesis, the most recent of which occurred several years ago. He was told that an ulcer was seen on a barium upper GI radiograph. You obtain a serum assay for H Pylori IgG, which is positive. What is the most effective regimen to eradicate this organism?
Omeprazole 20 mg orally once daily for 6 weeks
Ranitidine 300 mg orally once daily at bedtime for 6 weeks
Omeprazole 20 mg twice daily, amoxicillin 1000 mg twice daily, and clarithromycin 500 mg twice daily for 14 days
Pepto-Bismol and metronidazole twice daily for 7 days
Benzathine penicillin, 1.2 million units intramuscularly weekly for three doses
A 36-year-old man presents for a well-patient examination. He gives a history that, over the past 20 years, he has had three episodes of abdominal pain and hematemesis, the most recent of which occurred several years ago. He was told that an ulcer was seen on a barium upper GI radiograph. You obtain a serum assay for H Pylori IgG, which is positive. What is the most effective regimen to eradicate this organism?
Omeprazole 20 mg orally once daily for 6 weeks
Ranitidine 300 mg orally once daily at bedtime for 6 weeks
Omeprazole 20 mg twice daily, amoxicillin 1000 mg twice daily, and clarithromycin 500 mg twice daily for 14 days
Pepto-Bismol and metronidazole twice daily for 7 days
Benzathine penicillin, 1.2 million units intramuscularly weekly for three doses
An otherwise healthy 40-year-old woman sees you because of recurrent abdominal pain. In the past month she has had four episodes of colicky epigastric pain. Each of these episodes has lasted about 30 minutes and has occurred within an hour of eating. Two of the episodes have been associated with sweating and vomiting. None of the episodes have been associated with fever or shortness of breath. She has not lost weight. She does not drink alcohol or take any prescription or over-the-counter medications. Other than three previous uneventful vaginal deliveries, she has never been hospitalized. Her examination is negative except for mild obesity (BMI = 32). A complete blood count and multichannel chemistry profile that includes liver function test is normal. A gallbladder sonogram reveals multiple gallstones. What is the next best step in the treatment of this patient?
Omeprazole, 20 mg daily for eight weeks.
Ursodeoxycholic acid
Observation without specific therapy
Laparoscopic cholecystectomy
Weight reduction
An otherwise healthy 40-year-old woman sees you because of recurrent abdominal pain. In the past month she has had four episodes of colicky epigastric pain. Each of these episodes has lasted about 30 minutes and has occurred within an hour of eating. Two of the episodes have been associated with sweating and vomiting. None of the episodes have been associated with fever or shortness of breath. She has not lost weight. She does not drink alcohol or take any prescription or over-the-counter medications. Other than three previous uneventful vaginal deliveries, she has never been hospitalized. Her examination is negative except for mild obesity (BMI = 32). A complete blood count and multichannel chemistry profile that includes liver function test is normal. A gallbladder sonogram reveals multiple gallstones. What is the next best step in the treatment of this patient?
Omeprazole, 20 mg daily for eight weeks.
Ursodeoxycholic acid
Observation without specific therapy
Laparoscopic cholecystectomy
Weight reduction
A 56-year-old chronic alcoholic has a 1-year history of ascites. He is admitted with a 2-day history of diffuse abdominal pain and fever. Examination reveals scleral icterus, spider angiomas, a distended abdomen with shifting dullness, and diffuse abdominal tenderness. Paracentesis reveals slightly cloudy ascitic fluid with an ascitic fluid PMN cell count of 1000/μL. Which of the following statements about treatment is true?
Antibiotic therapy is unnecessary if the ascitic fluid culture is negative for bacteria.
The addition of albumin to antibiotic therapy improves survival
Repeated paracenteses are required to assess the response to antibiotic treatment.
After treatment of this acute episode, a recurrent episode of spontaneous bacterial peritonitis would be unlikely.
Treatment with multiple antibiotics is required because polymicrobial infection is common.
A 60-year-old man with known hepatitis C and a previous liver biopsy showing cirrhosis requests evaluation for possible liver transplantation. He has never received treatment for hepatitis C. Though previously a heavy user of alcohol, he has been abstinent for over 2 years. He has had 2 episodes of bleeding esophageal varices. He was hospitalized 6 months ago with acute hepatic encephalopathy. He has a 1-year history of ascites that has required repeated paracentesis despite treatment with diuretics. Medications are aldactone 100 mg daily and lactulose 30 cc 3 times daily. On examination he appears thin, with obvious scleral icterus, spider angiomas, palmar erythema, gynecomastia, a large amount ascites, and small testicles. There is no asterixis. Recent laboratory testing revealed the following: hemoglobin = 12.0 mg/dL (normal 13.5-15.0), MCV = 103 fL (normal 80-100), creatinine = 2.0 mg/dL (normal 0.7-1.2), bilirubin = 6.5 mg/dL (normal 0.1-1.2), AST = 25 U/L (normal < 40), ALT= 45 U/L (normal < 40), INR = 3.0 (normal 0.8-1.2). What is the next best step?
Repeat liver biopsy.
Start treatment with interferon and ribavirin.
Refer the patient for hospice care.
Continue to optimize medical treatment for his ascites and hepatic encephalopathy and tell the patient he is not eligible for liver transplantation because of his previous history of alcohol abuse.
Refer the patient to a liver transplantation center
A 32-year-old white woman complains of abdominal pain off and on since the age of 17. She notices abdominal bloating relieved by defecation as well as alternating diarrhea and constipation. She has no weight loss, GI bleeding, or nocturnal diarrhea. On examination, she has slight LLQ tenderness and gaseous abdominal distension. Laboratory studies, including CBC, are normal. Which of the following is the most appropriate initial approach?
Recommend increased dietary fiber, antispasmodics as needed, and follow-up examination in 2 months.
Refer to gastroenterologist for colonoscopy
Obtain antiendomysial antibodies.
Order UGI series with small bowel follow-through.
Order small bowel biopsy
A 27-year-old female is found to have a positive hepatitis C antibody at the time of plasma donation. Physical examination is normal. Liver enzymes reveal ALT of 62 U/L (normal < 40), AST 65 U/L (normal < 40), bilirubin 1.2 mg/dL (normal), and alkaline phosphatase normal. Hepatitis C viral RNA is 100,000 copies/mL. Hepatitis B surface antigen and HIV antibody are negative. Which of the following statements is true?
Liver biopsy is necessary to confirm the diagnosis of hepatitis C.
Most patients with hepatitis C eventually resolve their infection without permanent sequelae.
This patient should not receive vaccinations against other viral forms of hepatitis.
Serum ALT levels are a good predictor of prognosis.
Patients with hepatitis C genotype 2 or 3 are more likely to have a favourable response to treatment with interferon and ribavirin.
A 45-year-old woman presents to the ED with 1 day of painful rectal bleeding. Review of systems is negative for weight loss, abdominal pain, nausea, and vomiting. On physical examination, you note an exquisitely tender swelling with engorgement and a bluish discoloration distal to the anal verge. Her vital signs are HR 105 beats per minute, BP 140/70 mm Hg, RR 18 breaths per minute, and temperature 99°F. Which of the following is the next best step in management?
Recommend warm sitz baths, topical analgesics, stool softeners, a high-fiber diet, and arrange for surgical followup.
Incision and drainage under local anesthesia or procedural sedation followed by packing and surgical follow-up
Obtain a complete blood cell (CBC) count, clotting studies, type and cross, and arrange for emergent colonoscopy.
Excision under local anesthesia followed by sitz baths and analgesics
Surgical consult for immediate operative management.
A 68-year-old man presents to the ED 4 hours after an upper endoscopy was performed for 5 months of progressive dysphagia. During the procedure, a 1-cm ulcerated lesion was found and biopsied. Now, the patient complains of severe neck and chest pain. His vitals are as follows: BP 135/80 mm Hg, HR 123 beats per minute, RR 26 breaths per minute, and temperature 101°F. On physical examination, he appears diaphoretic and in moderate distress with crepitus in the neck and a crunching sound over the heart. You obtain an electrocardiogram (ECG), which is notable for sinus tachycardia. After obtaining a surgical consult, which of the following is the next best step in management?
Perform an immediate bronchoscopy.
Give aspirin 325 mg and obtain a cardiology consult for possible cardiac catheterization.
Repeat the endoscopy to evaluate the biopsy site
Perform an immediate thoracotomy.
Order an immediate esophagram with water-soluble agent.
A 65-year-old man with a history of occasional painless rectal bleeding presents with 2 to 3 days of constant, dull RLQ pain. He also complains of fever, nausea, and decreased appetite. He had a colonoscopy 2 years ago that was significant for sigmoid and cecal diverticula but was otherwise normal. On physical examination he has RLQ tenderness with rebound and guarding. His vitals include HR of 95 beats per minute, BP of 130/85 mm Hg, and temperature of 101.3°F. The abdominal CT demonstrates the presence of sigmoid and cecal diverticula, inflammation of pericolic fat, thickening of the bowel wall, and a fluid-filled appendix. Which of the following is the most appropriate next step in management?
Discharge the patient with broad-spectrum oral antibiotics and surgical follow-up.
Begin IV hydration and broad-spectrum antibiotics, keep the patient npo (nothing by mouth), and admit the patient to the hospital
Begin IV antibiotics and call a surgical consult for an emergent operative procedure.
Arrange for an emergent barium enema to confirm the diagnosis.
Begin sulfasalazine 3 to 4 g/d along with IV steroid therapy
A 49-year-old man presents to the ED with nausea, vomiting, and abdominal pain that began approximately 2 days ago. The patient states that he usually drinks a six pack of beer daily, but increased his drinking to 2 six packs daily over the last week because of pressures at work. He notes decreased appetite over the last 3 days and states he has not had anything to eat in 2 days. His BP is 125/75 mm Hg, HR is 105 beats per minute, and RR is 20 breaths per minute. You note generalized abdominal tenderness on examination. Laboratory results reveal the following: White blood cells (WBC) 9000/μL Sodium 131 mEq/L Hematocrit 48% Potassium 3.5 mEq/L Platelets 210/μL Chloride 101 mEq/L Aspartate transaminase (AST) 85 U/L Bicarbonate 10 mEq/L Alanine transaminase (ALT) 60 U/L Blood urea nitrogen (BUN) 9 mg/dL Alkaline phosphatase 75 U/L Creatinine 0.5 mg/dL Total bilirubin 0.5 mg/dL Glucose 190 mg/dL Lipase 40 IU Nitroprusside test weakly positive for ketones Which of the following is the mainstay of therapy for patients with thiscondition?
Normal saline (NS) solution
Half normal saline (. NS)
Glucose solution (D5W)
Solution containing both saline and glucose (D 5/NS or D 5. NS)
The type of solution is irrelevant
A 31-year-old man from Florida presents to the ED complaining of severe pain that starts in his left flank and radiates to his testicle. The pain lasts for about 1 hour and then improves. He had similar pain last week that resolved spontaneously. He noted some blood in his urine this morning. His BP is 145/75 mm Hg, HR is 90 beats per minute, temperature is 98.9°F, and his RR is 24 breaths per minute. His abdomen is soft and nontender. As you examine the patient, he vomits and has trouble lying still in his stretcher. Which of the following is the most appropriate next step in management?
Call surgery consult to evaluate the patient for appendicitis.
Order an abdominal CT.
Start intravenous (IV) fluids and administer an IV nonsteroidal anti-inflammatory drug (NSAID) and antiemetic
Perform an ultrasound to evaluate for an abdominal aortic aneurysm (AAA)
Perform an ultrasound to evaluate for testicular torsion.
A 24-year-old man woke up from sleep 1 hour ago with severe pain in his right testicle. He states that he is sexually active with multiple partners. On examination, the right scrotum is swollen, tender, and firm. You cannot elicit a cremasteric reflex. His BP is 145/75 mm Hg, HR is 103 beats per minute, RR is 14 breaths per minute, temperature is 98.9°F, and oxygen saturation is 99% on room air. Which of the following is the most appropriate next step in management?
Administer one dose of ceftriaxone and doxycycline for 10 days and have him follow-up with a urologist.
Swab his urethra, send a culture for gonorrhea and Chlamydia, and treat if positive.
Send a urinalysis and treat for a urinary tract infection (UTI) if positive.
Treat the patient for epididymitis and have him return if symptoms persist.
Order a statim (STAT) color Doppler ultrasound and urologic consultation.
A 22-year-old man presents to the ED complaining of dysuria for 3 days. He states that he has never had this feeling before. He is currently sexually active and uses a condom most of the time. He denies hematuria but notes a yellowish discharge from his urethra. His BP is 120/75 mm Hg, HR is 60 beats per minute, and temperature is 98.9°F. You send a clean catch urinalysis to the laboratory that returns positive for leukocyte esterase and 15 white blood cells per high power field (WBCs/hpf). Which of the following is the most appropriate next step in management?
Send a urethral swab for culture and administer 125 mg ceftriaxone intramuscularly and 1 g azithromycin orally.
Send urine for culture and administer SMX/TMP orally.
Discharge the patient with strict instructions to return if his symptoms worsen.
Order a CT scan to evaluate for a kidney stone.
Have him follow-up immediately with a urologist to evaluate for testicular cancer.
A 59-year-old man presents to the ED complaining of vomiting and sharp abdominal pain in the epigastric area that began abruptly this afternoon. He describes feeling nauseated and has no appetite. Laboratory results reveal WBC 18,000/μL, hematocrit 48%, platelets 110/μL, AST 275 U/L, ALT 125 U/L, alkaline phosphatase 75 U/L, amylase 1150 U/L, lipase 1450 IU, LDH 400 U/L, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 110 mEq/L, bicarbonate 20 mEq/L, BUN 20 mg/dL, creatinine 1.5 mg/dL, and glucose 250 mg/dL. Which of the following laboratory results correlate with the poorest prognosis?
Amylase 950, lipase 1250, LDH 400
Lipase 1250, LDH 400, bicarbonate 20
Lipase 1250, creatinine 1.5, potassium 3.5
WBC 18,000, LDH 400, glucose 250
WBC 18,000, amylase 950, lipase 1250
An 18-year-old woman presents to the ED complaining of acute onset of RLQ abdominal pain. She also describes the loss of appetite over the last 12 hours, but denies nausea and vomiting. Her BP is 124/77 mm Hg, HR is 110 beats per minute, temperature is 102.1°F, RR is 16 breaths per minute, and oxygen saturation is 100% on room air. Abdominal examination reveals lower abdominal tenderness bilaterally. On pelvic examination you elicit cervical motion tenderness and note cervical exudates. Her WBC is 20,500/μL and β-hCG is negative. Which of the following is the most appropriate next step in management?
Bring her to the OR for an appendectomy.
Begin antibiotic therapy
Perform a culdocentesis
Bring her to the OR for immediate laparoscopy.
Order an abdominal plain film.
A 27-year-old man is seen in the ED for a leak around a surgical G-tube that was placed 2 weeks ago and has been used for enteral feeding for 1 week. Inspection reveals the tube is pulled out from the stoma, but is still in the cutaneous tissue. The abdomen is soft and nondistended and there are no signs of skin infection. Which of the following is the most appropriate next step in management?
Insert a Foley catheter into the tract and aspirate. If gastric contents are aspirated the tube can be used for feeding.
Insert a Foley catheter into the tract, instill water-soluble contrast, and obtain an abdominal radiograph prior to using for feeding
Remove the tube and admit the patient for observation.
Remove the tube and immediately obtain a CT scan of the abdomen.
Return to the OR for closure of gastrotomy and placement of a new tube.
A 30-year-old man presents to the ED complaining of sudden onset of abdominal bloating and back pain lasting for 2 days. The pain woke him up from sleep 2 nights ago. It radiates from his back to his abdomen and down toward his scrotum. He is in severe pain and is vomiting. His temperature is 101.2°F and HR is 107 beats per minute. A CT scan reveals a 9-mm obstructing stone of the left ureter with hydronephrosis. Urinalysis is positive for 2+ blood, 2+ leukocytes, 2+ nitrites, 40 to 50 WBCs, and many bacteria. You administer pain medicine, antiemetics, and antibiotics. Which of the following is the most appropriate next step in management?
Admit for IV antibiotics and possible surgical removal of stone
Observe in ED for another 6 hours to see if stone passes.
Discharge with antibiotics and pain medicine.
Discharge patient with instructions to consume large amounts of water.
Discharge patient with antibiotics, pain medicine, and instructions to drink large amounts of water and cranberry juice.
A 24-year-old woman presents to the ED after being sexually assaulted. She is a college student with no past medical history. Her BP is 130/75 mm Hg, HR is 91 beats per minute, temperature is 98.6°F, and RR is 16 breaths per minute. On physical examination you observe vaginal trauma and scattered bruising and abrasions. Which of the following medications should be offered to the patient in this scenario?
Ceftriaxone, azithromycin, metronidazole, antiretrovirals, emergency contraception
Ceftriaxone, tetanus, metronidazole, antiretrovirals, emergency contraception
Ceftriaxone, azithromycin, tetanus, metronidazole, emergency contraception
Ceftriaxone, azithromycin, tetanus, antiretrovirals, emergency contraception
Ceftriaxone, azithromycin, tetanus, metronidazole, antiretrovirals, emergency contraception
A 43-year-old man presents to the ED complaining of progressively worsening abdominal pain over the past 2 days. The pain is constant and radiates to his back. He also describes nausea and vomiting and states he usually drinks six pack of beer daily, but has not had a drink for 2 days. His BP is 144/75 mm Hg, HR is 101 beats per minute, temperature is 99.8°F, and RR is 14 breaths per minute. He is lying on his side with his knees flexed. Examination shows voluntary guarding and tenderness to palpation of his epigastrium. Laboratory results reveal WBC 10,500/μL, hematocrit 51%, platelets 225/μL, and lipase 620 IU. An abdominal radiograph reveals a nonspecific bowel gas pattern. There is no free air under the diaphragm. Which of the following is the most appropriate next step in management?
Observe in the ED.
Send home with antibiotic therapy.
Admit to the hospital for endoscopy.
Admit to the hospital for exploratory laparotomy.
Admit to the hospital for medical management and supportive care.
A 43-year-old man presents to the ED complaining of progressively worsening abdominal pain over the past 2 days. The pain is constant and radiates to his back. He also describes nausea and vomiting and states he usually drinks six pack of beer daily, but has not had a drink for 2 days. His BP is 144/75 mm Hg, HR is 101 beats per minute, temperature is 99.8°F, and RR is 14 breaths per minute. He is lying on his side with his knees flexed. Examination shows voluntary guarding and tenderness to palpation of his epigastrium. Laboratory results reveal WBC 10,500/μL, hematocrit 51%, platelets 225/μL, and lipase 620 IU. An abdominal radiograph reveals a nonspecific bowel gas pattern. There is no free air under the diaphragm. Which of the following is the most appropriate next step in management?
Observe in the ED.
Send home with antibiotic therapy.
Admit to the hospital for endoscopy.
Admit to the hospital for exploratory laparotomy.
Admit to the hospital for medical management and supportive care.
A 77-year-old woman is brought to the emergency room because of nonspecific abdominal discomfort. She has no anorexia, fever, chills, or weight loss. Her abdomen is soft and non-tender on physical examination. Abdominal x-rays show lots of stool in the colon, but no free air or air-fluid levels. The amylase is 150 U/L (25– 125U/L), and the rest of her biochemistry and complete blood count are normal. Which of the following conditions can cause a false positive elevation in the serum amylase?
Aturity-onset diabetes mellitus (DM)
Gastric ulcer
Renal failure
Sulfonamide therapy
Gastric carcinoma
A 76-year-old woman with a history of congestive heart failure, coronary artery disease, and an “irregular heart beat” is brought to the ED by her family. She has been complaining of increasing abdominal pain over the past several days. She denies nausea or vomiting and bowel movements remain unchanged. Vitals are HR of 114 beats per minute, BP 110/75 mm Hg, and temperature 98°F. On cardiac examination, her HR is irregularly irregular with no murmur detected. The abdomen is soft, nontender, and nondistended. The stool is heme-positive. This patient is at high risk for which of the following conditions?
Perforated gastric ulcer
Diverticulitis
Acute cholecystitis
Mesenteric ischemia
Sigmoid volvulus
A 78-year-old man with a history of atherosclerotic heart disease and congestive heart failure presents with increasing abdominal pain. The pain began suddenly a day ago and has progressively worsened since then. He denies nausea, vomiting, and diarrhea, but states that he had black tarry stool this morning. He denies any history of prior episodes of similar pain. Vitals are BP 120/65 mm Hg, HR 105 beats per minute, and temperature 99°F. The patient is at high risk for which of the following conditions?
Cholecystitis
Cecal volvulus
Mesenteric ischemia
Perforated peptic ulcer
Small bowel obstruction
A 22-year-old woman presents with chronic diarrhea. She has no abdominal discomfort, feels well, and reports no weight loss or systemic symptoms. Physical examination reveals a healthy young woman who is 5’7” tall and weighs 150 lb. The complete physical examination is normal. Which of the following is the most likely cause of a secretory diarrhea in this young woman?
Surreptitious use of stimulant laxatives
Carcinoid tumor
Ulcerative colitis
Lactose deficiency
Celiac disease
A 23-year-old woman presents with weight loss and chronic diarrhea. She appears unwell and cachectic. Routine laboratory tests reveal a low hemoglobin level and an increased international normalized ratio (INR) even though she is not taking any anticoagulants. The liver enzymes are normal, but the albumin and calcium levels are low, suggesting generalized malnutrition. Which of the following is the most appropriate initial diagnostic test for malabsorption?
Xylose absorption
Chilling test
X-ray studies
Stool fat quantitation
Small intestinal biopsy
A 29-year-old man with acquired immune deficiency syndrome (AIDS) comes to the emergency department because of progressively increasing abdominal discomfort. Examination shows voluntary guarding in the upper abdomen. His biochemistry is normal except for an elevated amylase at 370 U/L (25–125 U/L). Which of the following infections can trigger this disorder in AIDS patients?
Toxoplasmosis
Mycobacterium avium complex
Mycobacterium tuberculosis
Pneumocystis carinii
Herpes virus
A full-term 5-day-old African-American girl is taken to the pediatrician because her “eyes look yellow.” She is being exclusively formula- fed with an iron-rich formula. She has six wet diapers a day and stools twice a day. The pregnancy was uncomplicated and she was delivered by spontaneous vaginal delivery. Her Apgar scores were 9 and 10 at 1 and 5 minutes, respectively. Her temperature is 37°C (98.6°F), her head circumference is in the 50th percentile, and her weight is 3420 g (3 g below her birth weight). Her sclerae are icteric. There is no hepatomegaly or splenomegaly. Her total bilirubin is 9 mg/dL and her conjugated bilirubin is 0.2 mg/dL. Hemoglobin is 15 g/dL. Which of the following is the most likely diagnosis?
α1-Antitrypsin deficiency
Biliary atresia
Dubin-Johnson syndrome
Physiologic jaundice
Rotor syndrome
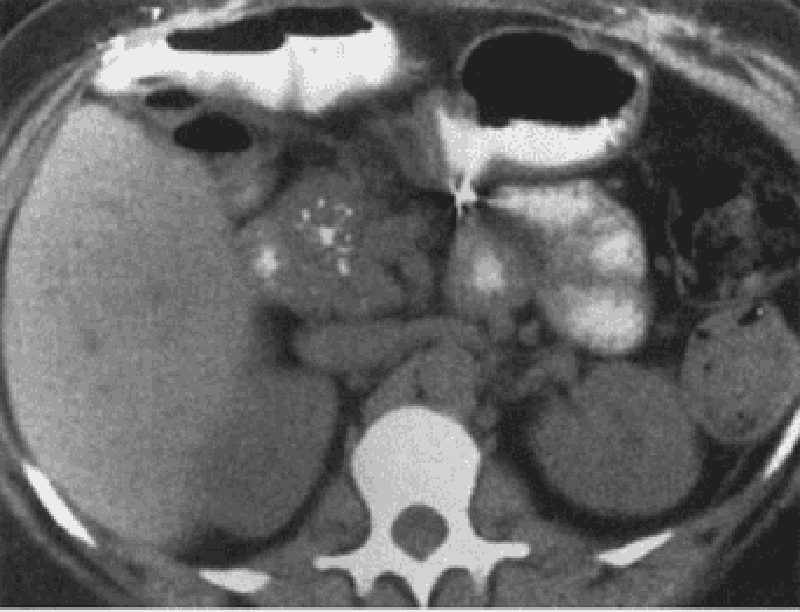
A 76-year-old man who has had multiple episodes of pancreatitis presents to his physician’s office with mild epigastric pain and 9.1-kg (20.0-lb) weight loss over the past 6 months. The patient also describes daily foulsmelling stools that “float” in the toilet bowl. The physician pulls up his electronic medical record and finds that the patient presented to the emergency department last week for the same symptoms. During that visit he had a CT of the abdomen (see image). Which of the following is the most appropriate treatment?
Endoscopic retrograde cholangiopancreatography
Pancreatic enzyme replacement
Pancreaticogastrostomy
Surgical resection of pancreas
Whipple procedure
A 50-year-old man with a history of alcohol and tobacco abuse has complained of difficulty swallowing solid food for the past 2 months. More recently, swallowing fluids has also become a problem. He has noted black, tarry stools on occasion. The patient has lost 10 lb. Which of the following statements is correct?
A CT scan of the abdomen and pelvis is the best next test
Barium contrast esophagram will likely establish a diagnosis.
The most likely diagnosis is peptic ulcer disease.
The patient has achalasia.
Herpes simplex virus infection of the esophagus is likely.
A 34-year-old man presents with substernal discomfort. The symptoms are worse after meals, particularly a heavy evening meal, and are sometimes associated with hot/sour fluid in the back of the throat and nocturnal awakening. The patient denies difficulty swallowing, pain on swallowing, or weight loss. The symptoms have been present for 6 weeks; the patient has gained 20 lb in the past 2 years. Which of the following is the most appropriate initial approach?
Therapeutic trial of ranitidine
Exercise test with thallium imaging
Esophagogastroduodenoscopy
CT scan of the chest
Coronary angiography
A 48-year-old woman presents with a change in bowel habit and 10-lb weight loss over the past 2 months despite preservation of appetite. She notices increased abdominal gas, particularly after fatty meals. The stools are malodorous and occur 2 to 3 times per day; no rectal bleeding is noticed. The symptoms are less prominent when she follows a clear liquid diet. Which of the following is the most likely histological abnormality associated with this patient’s symptoms?
Signet ring cells on gastric biopsy
Mucosal inflammation and crypt abscesses on sigmoidoscopy
Villous atrophy and increased lymphocytes in the lamina propria on small bowel biopsy
Small, curved gram-negative bacteria in areas of intestinal metaplasia on gastric biopsy
Periportal inflammation on liver biopsy
A 62-year-old woman is transferred to the medical service with an appendiceal mass serendipitously picked up at the edge of an x-ray taken of a broken femur in the emergency department. Otherwise, the patient has no significant past medical history and no current symptoms. Which of the following studies is most likely to be useful?
Arterial blood gas
CT of the chest and abdomen
Immediate ECG
MRI of the chest and abdomen
Room air oxygen saturation
A 60-year-old woman complains of fever and constant left lower quadrant pain of 2 days duration. She has not had vomiting or rectal bleeding. She has a history of hypertension but is otherwise healthy. She has never had similar abdominal pain, and has had no previous surgeries. Her only regular medication is lisinopril. On examination blood pressure is 150/80, pulse 110, and temperature 38.9°C (102°F). She has normal bowel sounds and left lower quadrant abdominal tenderness with rebound. A complete blood count reveals WBC = 28,000. Serum electrolytes, BUN, creatinine and liver function tests are normal. What is the next best step in evaluating this patient’s problem?
Colonoscopy
Barium enema
Exploratory laparotomy
Ultrasound of the abdomen
CT scan of the abdomen and pelvis
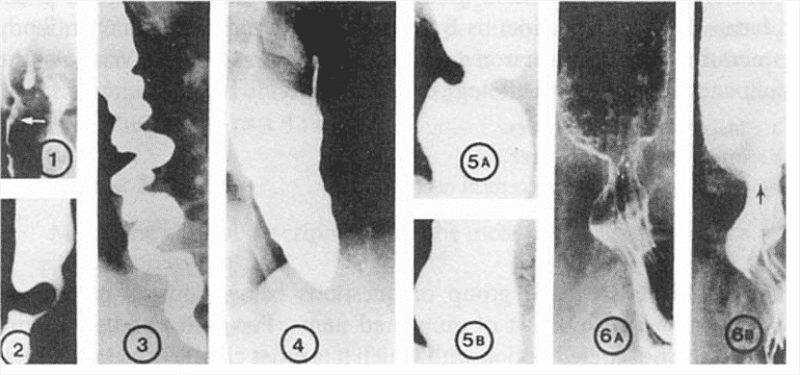
A 72-year-old woman notices progressive dysphagia to solids and liquids. There is no history of alcohol or tobacco use, and the patient takes no medications. She denies heartburn, but occasionally notices the regurgitation of undigested food from meals eaten several hours before. Her barium swallow is shown. Which of the following is the cause of this condition?
Growth of malignant squamous cells into the muscularis mucosa
Scarring caused by silent gastroesophageal reflux
Spasm of the lower esophageal sphincter
Loss of intramural neurons in the esophagus
Psychiatric disease
A 37-year-old woman presents for evaluation of abnormal liver chemistries. She has long-standing obesity (current BMI 38) and has previously taken anorectic medications but not for the past several years. She takes no other medications and has not used parenteral drugs or had high risk sexual exposure. On examination, her liver span is 13 cm; she has no spider angiomas or splenomegaly. Several sets of liver enzymes have shown transaminases two to three times normal. Bilirubin and alkaline phosphatase are normal. Hepatitis B surface antigen and hepatitis C antibody are normal, as are serum iron and total iron-binding capacity. Which of the following is the likely pathology on liver biopsy?
Macrovesicular fatty liver
Microvesicular fatty liver
Portal triaditis with piecemeal necrosis
Cirrhosis
Copper deposition
A 20-year-old man presents to the ED with fever and severe right lower quadrant (RLQ) pain for 1 day. Prior to this episode, he reports 2 months of crampy abdominal pain, generalized malaise, a 10-lb weight loss, and occasional bloody diarrhea. On examination, his HR is 115 beats per minute, BP is 125/70 mm Hg, RR is 18 breaths per minute, and temperature is 100.8°F. His only significant past medical history is recurrent perirectal abscesses. On physical examination, the patient appears uncomfortable and has a tender mass in the RLQ, without guarding or rebound. Rectal examination is positive for trace heme-positive stool. An abdominal computed tomographic (CT) scan reveals no periappendiceal fat stranding. There is inflammation of the distal ileum and several areas of the colon. There are no rectal inflammatory changes. Which of the following is the most likely diagnosis?
Crohn disease (CD)
Ulcerative colitis (UC)
Appendicitis
Pseudomembranous enterocolitis
Diverticulitis
A 55-year-old white woman with a history of iron deficiency anemia has had intermittent trouble swallowing solids for the past few years. She denies alcohol or tobacco use. Her vital signs are stable. Her iron level is 40μg/dL and total iron binding capacity is 500 μg/dL. Other laboratory tests are within normal limits. Which of the following is the most likely diagnosis?
Achalasia
Barrett’s esophagus
Esophageal carcinoma
Mallory-Weiss syndrome
Plummer-Vinson syndrome
A 55-year-old man from China is known to have chronic liver disease, secondary to hepatitis B infection. He has recently felt unwell, and his hemoglobin level has increased from 130 g/L, 1 year ago, to 195 g/L. Which of the following is the most appropriate initial diagnostic test?
Alkaline phosphatase
Alpha-fetoprotein (AFP)
Aspartate transaminase (AST)
Alanine transaminase (ALT)
Unconjugated bilirubin
A 67-year-old man is brought to the ED by emergency medical service (EMS). His wife states that the patient was doing his usual chores around the house when all of a sudden he started complaining of severe abdominal pain. He has a past medical history of coronary artery disease and hypertension. His BP is 85/70 mm Hg, HR is 105 beats per minute, temperature is 98.9°F, and his RR is 18 breaths per minute. On physical examination, he is diaphoretic and in obvious pain. Upon palpating his abdomen, you feel a large pulsatile mass. An electrocardiogram (ECG) reveals sinus tachycardia. You place the patient on a monitor, administer oxygen, insert two largebore IVs, and send his blood to the laboratory. His BP does not improve after a 1-L fluid bolus. Which of the following is the most appropriate next step in management?
Order a CT scan to evaluate his aorta.
Call the angiography suite and have them prepare the room for the patient.
Order a portable abdominal radiograph.
Call surgery and have them prepare the operating room (OR) for an exploratory laparotomy.
Call the cardiac catheterization laboratory to prepare for stent insertion.
A 48-year-old man with a past medical history of hepatitis C and cirrhosis presents to the ED complaining of acute-onset abdominal pain and chills. His BP is 118/75 mm Hg, HR is 105 beats per minute, RR is 16 breaths per minute, temperature is 101.2°F rectally, and oxygen saturation is 97% on room air. His abdomen is distended, and diffusely tender. You decide to perform a paracentesis and retrieve 1 L of cloudy fluid. Laboratory analysis of the fluid shows a neutrophil count of 550 cells/mm 3. Which of the following is the most appropriate choice of treatment?
Metronidazole
Vancomycin
Sulfamethoxazole/trimethoprim (SMX/TMP)
Neomycin and lactulose
Cefotaxime
A 64-year-old woman develops sudden-onset abdominal discomfort after eating a large meal. The pain is constant, localizes to the epigastric area with radiation to her right scapula. She also has nausea and vomiting. It eventual subsides 1 hour later. An ultrasound of the abdomen reveals a dilated common bile duct secondary to stones. Which of the following statements regarding common bile duct stones is most likely true?
All originate in the gallbladder
Always produce jaundice
Produce constant level of jaundice
Can be painless
Indicate anomalies of the bile duct
A 29-year-old woman complains of dysphagia with both solids and liquids, worse when she is eating quickly or is anxious. Manometry reveals normal basal esophageal sphincter pressure, with no relaxation of the sphincter on swallowing. Which of the following is the most appropriate next step in management?
Beta-blocker therapy
Partial esophagectomy
Anticholinergic drugs
Calcium channel blockers
Dietary modification
A 33-year-old woman develops mild epigastric abdominal pain with nausea and vomiting of 2 days duration. Her abdomen is tender on palpation in the epigastric region, and the remaining examination is normal. Her white count is 13,000/mL, and amylase is 300 U/L (25–125 U/L). Which of the following is the most common predisposing factor for this disorder?
Drugs
Gallstones
Malignancy
alcohol
Hypertriglyceridemia
A 54-year-old man complains of burning epigastric pain that usually improves after a meal, and is occasionally relieved with antacids. On examination, he appears well and besides some epigastric tenderness on palpation, the rest of the examination is normal. Upper endoscopy confirms a duodenal ulcer. Which of the following statements concerning PUD is most likely correct?
Duodenal ulcer is seen more often in older people than is gastric ulcer
Clinically, gastric ulcers are more common than duodenal ulcers
Duodenal ulcers can frequently be malignant
Infection can cause both types of peptic ulcer
Peptic gastric ulcers are usually quite proximal in the stomach
A 30-year-old man complains of chronic diarrhea for the past 6 months. There is no weight loss, fever, or abdominal pain. He takes no medications and feels fine. His physical examination is completely normal. Further history reveals that this man does not take laxatives; however, in an effort to stay slim he eats a lot of sugar-free gum and sugarless candy. Which of the following explanations is the most likely cause of his diarrhea?
Direct stimulant effect of chemicals in the candies
Lack of fiber in his diet
Pancreatic insufficiency secondary to chronic protein-calorie malnutrition
Secondary intestinal mucosal atrophy
Nonabsorbed carbohydrates
A 32-year-old man with Crohn’s disease presents to the emergency department with acute-onset diffuse abdominal pain and emesis. The patient states these symptoms are different than his usual Crohn’s disease flareups. The pain is severe (10/10) and is cramping in nature. He says his abdomen feels larger than usual. His Crohn’s disease has been well managed on 6-mercaptopurine for the past 6 months. The patient denies any recent sick contacts or eating underprepared foods. He states he had a bowel movement and flatus since the abdominal pain began. In addition to Crohn’s disease, the patient had appendicitis for which he underwent an appendectomy 12 years ago. His temperature is 37.1°C (98.7°F), blood pressure is 135/86 mm Hg, pulse is 84/min, and respiratory rate is 14/ min. On physical examination the abdomen is distended and diffusely tender with highpitched bowel sounds. There is rebound tenderness throughout the abdomen along with guarding. The remainder of the physical examination is noncontributory. An x-ray of the abdomen shows dilated small loops of bowel along with absence of gas in the colon. What is the best next step in management?
Bowel rest only
Intravenous fluids and antibiotics only
Laparotomy
MRI of the abdomen
Ultrasound
A 39-year-old Japanese-American woman with insulin-dependent diabetes and asthma presents to her primary care physician complaining of trouble swallowing for the past few months. She explains that it started with solids, and then progressed to liquids. She states it now is hard even to swallow water and that she is often very thirsty. She says she has lost about 3.2 kg (7 lb), but says she is working out frequently. Her blood pressure is 118/76 mm Hg, pulse is 86/min, respiratory rate is 16/min, and temperature is 37.2°C (98.9°F). Laboratory tests show Na+: 144 mEq/L K+: 4.0 mEq/L Cl−: 100 mEq/L Carbon dioxide: 22 mmol/L Blood urea nitrogen: 18 mg/dL Creatinine: 1.0 mg/dL Glucose: 88 mg/dL Her hemoglobin A1c level, measured 3 months earlier, was 6.1%. A barium swallow is per- formed, which reveals a dilated esophagus, especially distally, that flares out near the lower esophageal junction. Still not completely sure of the diagnosis, esophageal manometry is performed, which reveals abnormal peristalsis and increased lower sphincter pressure. Which of the following is the most appropriate management?
Cholinergic agents
Glucose pharmacotherapy
Instructions to elevate the bed, avoid fatty foods, and consider a histamine blocker
Pneumatic dilation
Surgery to remove diverticula
A 42-year-old previously well woman presents with pruritus. She is not taking any medications, and only drinks alcohol on a social basis. Her physical examination is entirely normal with no signs of chronic liver disease or jaundice. Laboratory evaluation reveals an alkaline phosphatase level of three times normal, and an ultrasound of the liver and gallbladder is normal. Which of the following is the most appropriate next step in diagnosis?
INR or prothrombin time
Antinuclear antibodies
Protein immunoelectrophoresis
Abdominal ultrasound
Antimitochondrial antibodies

A 22-year-old man with inflammatory bowel disease is noted to have a “string sign” in the ileal area on barium enema. In which of the following conditions is this sign most often seen?
In the stenotic or nonstenotic phase of the disease
In the stenotic phase only
As a rigid, nondistensible phenomenon
With gastric involvement
With rectal involvement
A 24-year-old man with a history of depression is brought to the emergency room because of a drug overdose. He is experiencing some nausea and vomiting, but no other symptoms. Physical examination and vital signs are normal. Six hours prior to presentation, he intentionally took 40 tablets of acetaminophen (500mg/tablet). Which of the following is the most appropriate next step in management?
Give ethanol to compete with the parent drug for metabolism, therefore preventing formation of toxic metabolites
Give Narcan to block its actions directly
Give intravenous prostacyclins to maintain cellular integrity
Give N-acetylcysteine to allow binding of the toxic metabolite
Give glucocorticoids to block the immune cascade
A 16-year-old girl is referred to the office because of chronic diarrhea and weight loss. She is experiencing large-volume watery diarrhea that is painless. The symptoms persist even when she is fasting, and there is no relationship to foods or liquids. She is not on any medications, and there is no travel history or other constitutional symptoms. Her physical examination is normal. Which of the following is the most likely diagnosis?
Partial small bowel obstruction
Partial large bowel obstruction
Osmotic diarrhea
Secretory diarrhea
Inflammatory bowel disease
A 55-year-old man is brought to the ED by his family. They state that he has been vomiting large amounts of bright red blood. The patient is an alcoholic with cirrhotic liver disease and a history of portal hypertension and esophageal varices. His vitals on arrival are HR 110 beats per minute, BP 80/55 mm Hg, RR 22 breaths per minute, and temperature 99°F. The patient appears pale and is in moderate distress. Which of the following is an inappropriate option in the initial management of a hypotensive patient with a history of known esophageal varices presenting with hematemesis?
Sengstaken-Blakemore tube placement
Two large-bore IV lines and volume repletion with crystalloid solutions
Nasogastric (NG) lavage
IV octreotide
Gastrointestinal (GI) consult
A 59-year-old woman presents to the ED complaining of worsening lower abdominal pain over the previous 3 days. She describes feeling constipated recently and some burning when she urinates. Her BP is 135/75 mm Hg, HR is 89 beats per minute, temperature is 101.2°F, and her RR is 18 breaths per minute. Her abdomen is mildly distended, tender in the LLQ, and positive for rebound tenderness. CT scan is consistent with diverticulitis with a 7-cm abscess. Which of the following is the most appropriate management for this condition?
Reserve the OR for emergent laparotomy
Start treatment with ciprofloxacin and metronidazole and plan for CT-guided draining of the abscess.
Give an IV dose of ciprofloxacin and have the patient follow up with her primary physician.
Start treatment with ciprofloxacin and metronidazole and plan for an emergent barium enema.
Start treatment with ciprofloxacin and metronidazole and prepare for an emergent colonoscopy.
A 60-year-old man is brought to the ED complaining of generalized crampy abdominal pain that occurs in waves. He has been vomiting intermittently over the last 6 hours. His BP is 150/75 mm Hg, HR is 90 beats per minute, temperature is 99.8°F, and his RR is 16 breaths per minute. On abdominal examination you notice an old midline scar across the length of his abdomen that he states was from surgery after a gunshot wound as a teenager. The abdomen is distended with hyperactive bowel sounds and mild tenderness without rebound. An abdominal plain film confirms your diagnosis. Which of the following is the most appropriate next step in management?
Begin fluid resuscitation, bowel decompression with a nasogastric tube, and request a surgical consult
Begin fluid resuscitation, administer broad-spectrum antibiotics, and admit the patient to the medical service.
Begin fluid resuscitation, give the patient stool softener, and administer a rectal enema.
Begin fluid resuscitation, administer broad-spectrum antibiotics, and observe the patient for 24 hours.
Order an abdominal ultrasound, administer antiemetics, and provide pain relief.
A 52-year-old man has suffered with chronic diarrhea for several years, but has refused to see a doctor. He finally comes because he is having trouble driving at night, because of difficulty seeing. Physical examination reveals a slender, pale, unwell-looking man. He has a microcytic anemia, low calcium, and albumin levels. Which of the following is the most likely cause for his diarrhea?
Malabsorption
Osmotic diarrhea
Secretory diarrhea
Inflammatory bowel disease
Colonic tumor
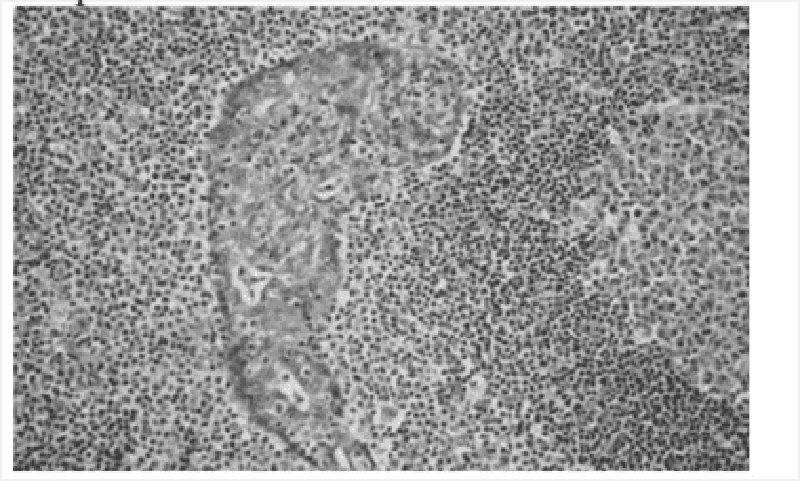
A 54-year-old man presents to his primary care provider with the complaint of upper abdominal fullness and pain. He states that he has lost 2.3-4.6 kg (5-10 lb), but denies other symptoms. Physical examination reveals a firm mass in the epigastric area. Ultrasonography reveals a mass in the gastric antrum. A salivary gland biopsy reveals the pathology shown in the image. Which of the following therapies is expected to be part of his treatment plan?
Antibiotic therapy
Bone marrow transplantation
Gene therapy
Liver transplantation
Multiagent chemotherapy
A 55-year-old white man with a 20-year history of gastroesophageal reflux visits the clinic for worsening reflux symptoms over the past 18 months. His last visit was 7 years ago and he claims to be otherwise in good health. He has been compliant with his antireflux medications, including an H2-blocker and a proton pump inhibitor. Which of the following is the best next step in management?
Double the dose of his H2-blocker and schedule him for follow-up in 4 weeks
Double the dose of his proton pumps inhibitor and schedule him for follow-up in 4 weeks
Perform an esophagoscopy
Schedule him for elective esophagectomy
Schedule him for emergent Nissen fundoplication
The physician on call is paged to the well-baby nursery because a full-term, 3-hour-old boy has had green emesis twice, once after each of his feedings. He is being breast-fed. He was born by spontaneous vaginal delivery following a pregnancy complicated by polyhydramnios. His Apgar scores were 8 and 9 at 1 and 5 minutes, respectively. His temperature is 37°C (98.6°F), blood pressure is 70/50 mm Hg, pulse is 150/min, and respiratory rate is 24/ min. His upper abdomen is distended, soft, and without palpable masses. Air is visualized in the duodenum and the stomach on x-ray. Which of the following is the most likely diagnosis?
Duodenal atresia
Hirschsprung’s disease
Intussusception
Malrotation with volvulus
Pyloric stenosis
A 68-year-old African-American man presents to his primary care physician for a check-up. He has not been to the physician’s office in over 15 years. He reports that he is fine but that his wife keeps telling him that he has to “go see the doctor.” He says he has never been sick, despite smoking three packs of cigarettes per day for over 40 years. He also says that he drinks 2–3 beers a night but never had a problem with that either. He’s as healthy “as a bull,” he says. His wife is in the room and says that he recently has had some problems swallowing food and that he is losing weight. He laughs and says, “I just need to chew more and eat more.” His vital signs are normal, as are his laboratory values. The physician is concerned and orders an endoscopy, which reveals a biopsy positive for squamous cell carcinoma of the esophagus. Which of the following most likely could have prevented this condition?
Avoiding fruits and vegetables
Eating more meats, especially smoked meats
Eliminating smoking and alcohol consumption
Getting a colonoscopy every 5 years
Taking proton pump inhibitors regularly
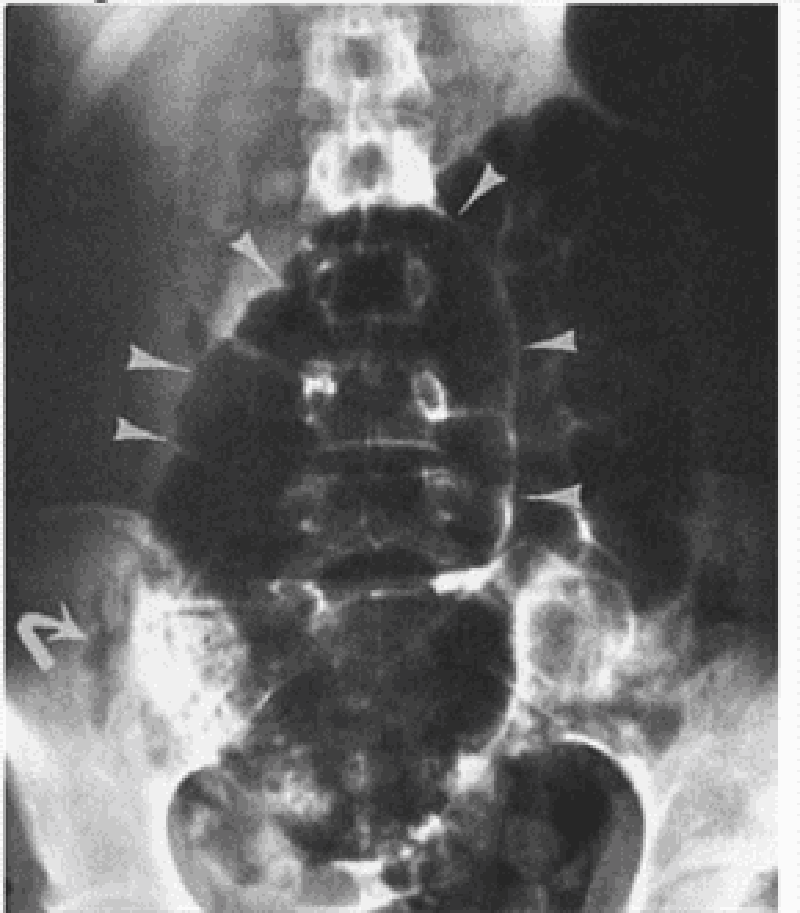
A 58-year-old man comes to the emergency department complaining of colicky abdominal pain over the past 3 days that suddenly became more severe and constant over the past 6 hours. A contrast study is performed and results are shown in the image. What is the first-line treatment after fluid resuscitation and nasogastric tube placement?
Colonoscopy
Hemicolectomy
Proximal colostomy with delayed resection
Sigmoid colectomy
Sigmoidoscopy
A full-term 6-day-old boy presents to a physician’s office for routine care. He is tolerating breast milk well. He is urinating, defecating, and sleeping normally. Physical examination reveals an alert newborn with mild eczema, good skin turgor, normal reflexes, and a musty odor. His newborn laboratory screen is notable for phenylketones in the urine. What is the best advice to give his parents regarding the boy’s diet?
Increase iron
Increase niacin
Increase phenylalanine
Increase tyrosine
Increase vitamin D
A 59-year-old woman with renal cell carcinoma presents to the emergency department with severe right upper quadrant (RUQ) pain. She is afebrile, acutely tender in the RUQ, and has shifting dullness and a palpable liver edge. Murphy’s sign is negative. Laboratory studies show: Na+: 138 mEq/L K+: 3.6 mEq/L Glucose: 80 mg/dL Aspartate aminotransferase: 50 U/L Alanine aminotransferase: 43 U/L Alkaline phosphatase: 138 U/L Total protein: 6.4 g/dL Albumin: 3.8 g/dL Total bilirubin: 1.1 mg/dL Imaging demonstrates a spider web of collateral veins in the liver. Although extensive measures are taken, the patient dies 6 hours after arriving. Which of the following was the most likely initial treatment?
β-Blocker followed by lactulose
Cholecystectomy
Endoscopic retrograde cholangiopancreatography with dilation of the common bile duct
Exploratory laparotomy
Tissue plasminogen activator followed by anticoagulation

A 65-year-old man presents to his physician complaining of difficulty swallowing, occasional chest pain, and regurgitation of food. Over the past 2 months he has lost about 7 kg (15 lb). Results of a barium swallow study are shown in the image. What test should be performed to look for possible causes of his condition?
24-hour pH monitoring
Esophageal manometry
Serum gastrin level measurement
Upper endoscopy
Urease breath test
A 63-year-old man with a long history of alcohol abuse presents with ascites. He is experiencing mild abdominal discomfort and nausea. Examination reveals tense ascites and generalized tenderness but no rigidity. A diagnostic paracentesis of the fluid is performed. Which of the following ascitic fluid results is most likely to suggest an uncomplicated ascites due to portal hypertension from cirrhosis?
Hemorrhage
Protein >25 g/L
Bilirubin level twice that of serum
Serum to ascites albumin gradient >1.1 g/dL
Ore than 1000 white cells/mm 3
A 67-year-old woman with a history of hypertension and congestive heart failure presents with “burning” epigastric pain that began 2 hours after eating a meal. She states that she has had similar pain over the past several weeks, and has been taking antacids and a medication that her primary care physician had prescribed with moderate relief. The pain has occurred with increasing frequency and now awakens her from sleep. She states she came to the ED today because the pain was not relieved with her usual medications. She denies nausea, vomiting, diarrhea, or fever. She also denies hematemesis, black stool, or bright red blood per rectum. On physical examination, she is tender at the epigastrium, with an otherwise normal abdominal, pulmonary, and heart examination. Stool guaiac tests positive for occult blood. Which of the following is the most common serious complication of peptic ulcer disease?
GI haemorrhage
GI perforation
GI penetration
Gastric outlet obstruction
Pernicious anemia
A 60-year-old man with no past medical history undergoes upper endoscopy and biopsy for an upset stomach that is worsened by eating. He is found to have inflammation predominantly in the antrum of the stomach. Which of the following is the most likely etiology of this condition?
Alcohol abuse
Cigarette smoking
Iatrogenic
Infection
Spicy foods
A 21-year-old man presents to the clinic feeling tired and generally unwell. He has fallen several times over the past month and has developed a slight tremor in both hands. Physical examination is significant for scleral icterus, ankle edema, and a distended and tense abdomen. Laboratory studies show: Hemoglobin: 7 g/dL Reticulocyte count: 7% Total bilirubin: 3.1 mg/dL Aspartate aminotransferase: 84 U/L Alanine aminotransferase: 92 U/L Ceruloplasmin: 5 mg/dL (normal: 20–45 mg/dL) Results of a Coombs’ test are negative. Which of the following is an appropriate preventive management step after chelation therapy?
Blood protein electrophoresis
Colonoscopy
ECG
Schilling test
Upper endoscopy
A 70-year-old man with a history of constipation has been experiencing intermittent left- sided abdominal pain and fevers for 2 days. He came to the emergency department immediately after he noticed blood in his toilet this morning. His heart rate is 110/min, blood pressure is 90/50 mm Hg, respiratory rate is 18/ min, and oxygen saturation is 95% on room air. On physical examination the physician notes copious amounts of bright red blood per rectum. The physician immediately places two large bore intravenous lines, administers fluid, and sends blood for type and screen. Which of the following is the best next step in management?
Arteriography
Colonoscopy
Endoscopy
Nasogastric tube aspiration
Surgical consultation
A 23-year-old woman presents to the ED complaining of pain with urination. She has no other complaints. Her symptoms started 3 week ago. During this time, she has been to the clinic twice, with negative urine cultures each time. Her condition has not improved with antibiotic therapy with sulfonamides or quinolones. Physical examination is normal. Wet mount showed epithelial cells. Which of the following organisms is most likely responsible for the patient’s symptoms?
Staphylococcus aureus
Herpes simplex virus
Trichomonas vaginalis
Escherichia coli
Chlamydia trachomatis
A 35-year-old alcoholic man is admitted with nausea, vomiting, and abdominal pain that radiates to the back. He has had several previous episodes of pancreatitis presenting with the same symptoms. Which of the following laboratory values suggests a poor prognosis in this patient?
Elevated serum lipase
Elevated serum amylase
Leukocytosis of 20,000/μm
Diastolic blood pressure greater than 90 mm Hg
Heart rate of 100 beats/minute
A 60-year-old woman with depression and poorly controlled type 2 diabetes mellitus complains of episodic vomiting over the last three months. She has constant nausea and early satiety. She vomits once or twice almost every day. In addition, she reports several months of mild abdominal discomfort that is localized to the upper abdomen and that sometimes awakens her at night. She has lost 5 lb of weight. Her diabetes has been poorly controlled (glycosylated hemoglobin recently was 9.5). Current medications are glyburide, metformin, and amitriptyline. Her physical examination is normal except for mild abdominal distention and evidence of a peripheral sensory neuropathy. Complete blood count, serum electrolytes, BUN, creatinine, and liver function tests are all normal. Gallbladder sonogram is negative for gallstones. Upper GI series and CT scan of the abdomen are normal. What is the best next step in the evaluation of this patient’s symptoms?
Barium esophagram
Scintigraphic gastric emptying study
Colonoscopy
Liver biopsy
Small bowel biopsy
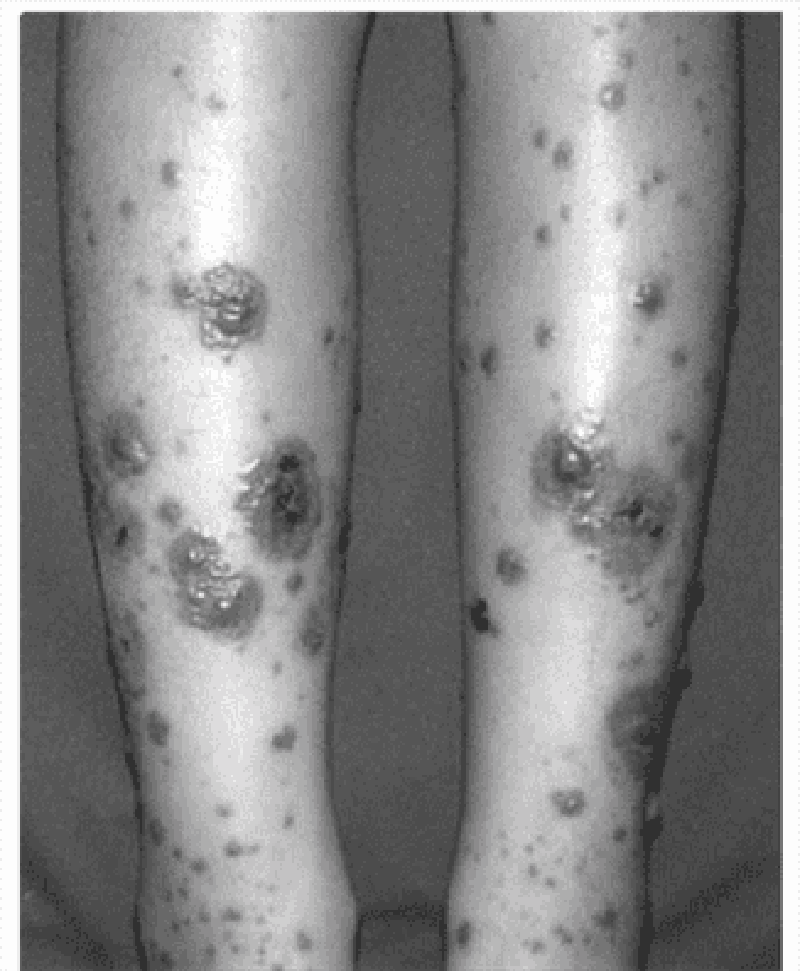
A 3-year-old boy is brought to the pediatrician because his mother noticed a reddish-purple rash on his buttocks and thighs (see image). She notes that he has not seemed well since he had a mild cold 2 weeks earlier; he has been complaining of aches and pains in his legs and a stomach ache. Urinalysis shows 10–20 RBCs/ mm³ and 2+proteinuria. Which of the following is associated with this patient’s disease process?
Hemoptysis
High antistreptolysin O titer
Impaired glucose tolerance
Intussusception
Malar rash
A 63-year-old man with diabetes is called by his primary care physician because of abnormal liver function test results, as follows: Aspartate aminotransferase: 85 U/L Alanine aminotransferase: 102 U/L Alkaline phosphatases: 180 U/L Total bilirubin: 1.9 mg/dL. On physical examination his liver is enlarged. His skin has a slightly yellow hue, especially on his face. The review of symptoms is significant for some weight loss, weakness, arthritis in his hands, and inability to achieve an erection. What test would generate the most likely diagnosis and should be done first?
Blood smear
CT scan of the abdomen
Endoscopic retrograde cholangiopancreatography
Fasting transferrin saturation levels
Liver biopsy
A 28-year-old man presents to the ED complaining of constant vague, diffuse epigastric pain. He describes having a poor appetite and feeling nauseated ever since eating sushi last night. His BP is 125/75 mm Hg, HR is 96 beats per minute, temperature is 100.5°F, and his RR is 16 breaths per minute. On examination, his abdomen is soft and moderately tender in the right lower quadrant (RLQ). Laboratory results reveal a WBC of 12,000/ μL. Urinalysis shows 1+ leukocyte esterase. The patient is convinced that this is food poisoning from the sushi and asks for some antacid. Which of the following is the most appropriate next step in management?
Order a plain radiograph to look for dilated bowel loops.
Administer 40 cc of Maalox and observe for 1 hour.
Send the patient for an abdominal ultrasound.
Order an abdominal CT scan.
Discharge the patient home with ciprofloxacin.
A 23-year-old woman presents to the ED in moderate pain in her left lower quadrant (LLQ). She states that the pain began suddenly and is associated with nausea and vomiting. She had a bout of diarrhea yesterday. This is the second time this month that she experienced pain in this location, however, never with this severity. Her BP is 120/75 mm Hg, HR is 101 beats per minute, temperature is 99.5°F, and RR is 18 breaths per minute. She has a tender LLQ on abdominal examination and a tender adnexa on pelvic examination. Which of the following is the most appropriate diagnostic test for the patient?
CT scan
MRI
X-ray
Doppler ultrasound
Laparoscopy
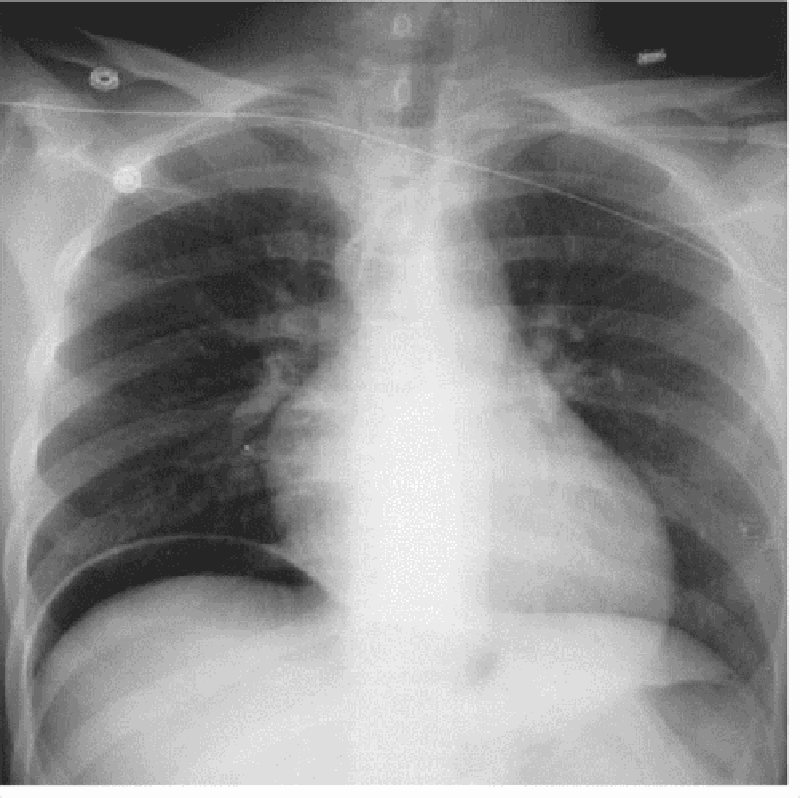
A 55-year-old man presents to the ED complaining of mild diffuse abdominal pain. He states that he underwent a routine colonoscopy yesterday and was told “everything is fine.” The pain began upon waking up and is associated with some nausea. He denies fever, vomiting, diarrhea, and rectal bleeding. His BP is 143/71 mm Hg, HR is 87 beats per minute, temperature is 98.9°F, and RR is 16 breaths per minute. His abdomen is tense but only mildly tender. You order baseline laboratory tests. His chest radiograph is seen below. Which of the following is the most likely diagnosis?
Ascending cholangitis
Acute pulmonary edema
Acute liver failure
Pancreatitis
Pneumoperitoneum
A 34-year-old woman complains bitterly of heartburn. Physical examination reveals healing lesions of the fingertips that she says were small ulcers, and there are small areas of telangiectasias on her face. Esophageal manometry reveals a decrease in the expected amplitude of smooth muscle contraction. Lower esophageal sphincter tone is subnormal, but relaxes normally with swallowing. Which of the following statements regarding this condition is most likely correct?
Characterized by systemic signs of inflammation
Predominantly treated symptomatically
Characterized by a poor prognosis
Usually more frequent in men
Characterized by death secondary to a renal crisis

A 35-year-old White man has a long past his- tory of diarrhea, rectal bleeding, crampy abdominal pain, and the passage of mucus. He now presents with a worsening of his symptoms despite taking his medications. A barium enema is performed and is shown in Fig. Which of the following is the most likely diagnosis of this new complication?
Toxic megacolon
amoebic colitis
Appendicitis
Ischemic colitis
Annular carcinoma

A 45-year-old man with a long history of alcohol intake comes into the emergency room with upper gastrointestinal (UGI) bleeding. Urgent endoscopy reveals the following findings. Which of the following is the most likely diagnosis?
Esophageal varices
Esophageal carcinoma
Foreign body
tertiary waves
Barrett’s esophagus
A 50-year-old woman undergoes screening colonoscopy at her primary care physician’s recommendation. She has no family history of colorectal cancer. A single lesion is removed during the procedure and sent for pathologic examination. Which of the following findings carries the greatest risk of malignancy?
Lymphoid polyp
Peutz-Jeghers polyp
Tubular adenoma
Tubulovillous adenoma
Villous adenoma
A 61-year-old man in previously excellent health presents to his physician with complaints of hematochezia tenesmus, and rectal pain. On work-up the physician discovers that he has a rectal tumor that is 5 cm (2.0 in) from the anal verge. Which of the following is the most appropriate treatment?
Abdominoperineal resection
Imatinib
Low anterior resection
Radiation alone
Radiation plus chemotherapy
A 45-year-old HIV-positive woman comes to her primary care physician complaining of a 2-day history of bloody diarrhea. She states that she has been feeling well until 2 days ago, when she developed abdominal pain. She denies fevers, chills, night sweats, nausea, or vomiting. She admits to feeling tired over the last couple of weeks and has had a 2.3-kg (5-lb) weight loss over the past 2 weeks. Her stool sample shows WBCs and RBCs. Her Gram stain is shown in the image. Her CD4+ cell count is 201/mm³. Which of the following is the most likely cause of this woman’s symptoms?
Escherichia coli
Kaposi’s sarcoma
Legionella
Mycobacterium avium complex
Mycobacterium tuberculosis
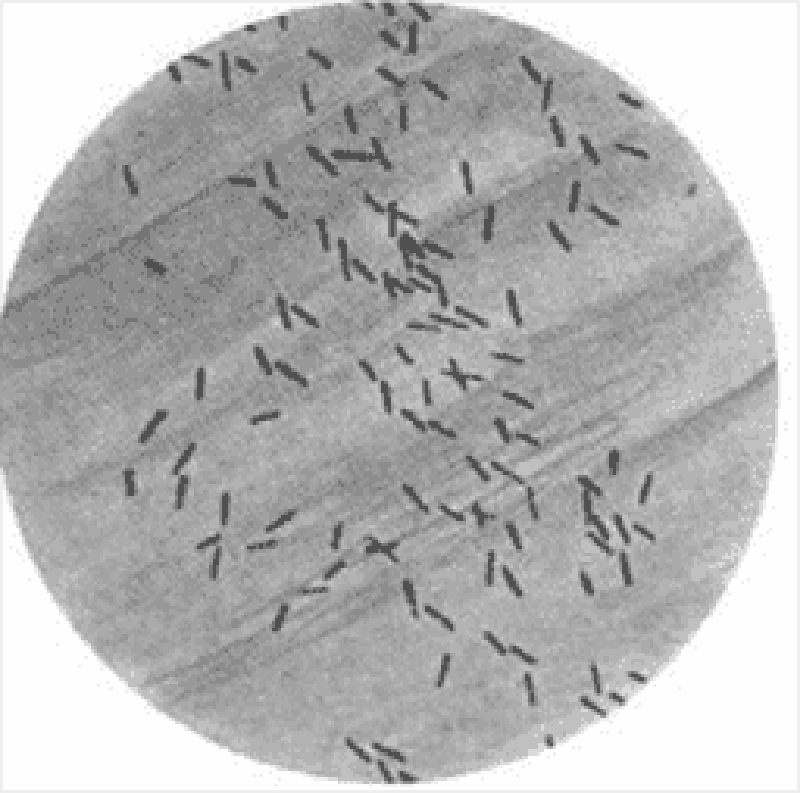
A 75-year-old woman with a history of diabetes and coronary heart failure presents to the emergency department because of increasing abdominal girth. In recent months she has been feeling increasingly fatigued, and although she has had decreased appetite, she has gained weight. Her heart rate is 100/min and blood pressure is 112/70 mm Hg. She has scleral icterus; the skin over her face, neck, and lower legs is slightly bronze in color; she has palmar erythema; and she has numerous ecchymoses over her body. Her abdominal examination is significant for ascites. Laboratory tests show: Aspartate transaminase: 102 U/L Alanine transaminase: 97 U/L Alkaline phosphatase: 300 U/L Total bilirubin: 1.9 mg/dL Albumin: 2.9 g/dL Prothrombin time: 22 sec Partial thromboplastin time: 42 sec An ultrasound of her abdomen shows a shrunken and nodular liver. A liver biopsy using Perls Prussian blue stain is shown in the image. Which of the following is the most likely complication of her disease?
Acute pancreatitis
Amyloidosis
Bone marrow failure
Hepatocellular carcinoma
Splenomegaly
A term boy with Apgar scores of 9 and 9 at 1 and 5 minutes has failed to pass meconium at 72 hours. He has had no episodes of emesis, and his abdomen is only mildly distended to palpation. The patient’s mother reports that her older son had the same problem at birth. A plain radiograph of the abdomen shows a small bowel obstruction with numerous air-filled loops of bowel. The patient is treated with a diatrizoate meglumine (Gastrografin) enema, with good results. Which of the following is the most likely mechanism for this infant’s acute intestinal problem?
Congenital aganglionosis of the colon
Deficiency of pancreatic enzymes
Intussusception of the large bowel
Total absence of the small bowel
Volvulus of the transverse colon
A 75-year-old woman comes to the emergency department with complaints of nausea and nonbilious, nonbloody vomiting over the past 4 days. The patient reports that both the nausea and vomiting come in “waves”; that is, several hours will pass during which she feels well before the vomiting suddenly recurs. A detailed history reveals that the woman was told several months ago that she “has stones in her gall-bladder,” but she has been too frightened to undergo surgery. She has not had a bowel movement for 7 days. Her temperature is 38.4°C (101.1°F) and the abdomen is distended with high-pitched bowel sounds. Which of the following is the most appropriate initial test for a patient with suspected gallstone ileus?
Abdominal ultrasound
Diagnostic laparoscopy
Endoscopic retrograde cholangiopancreatography
Hepatic iminodiacetic acid scan
Plain X-ray of the abdomen
A 62-year-old woman with a history of diabetes mellitus presents to the emergency department complaining of severe abdominal pain for the past 12 hours, first beginning as dull pain near the umbilicus but now localized to the right lower quadrant. She initially thought she was suffering from heartburn, but decided to come to the hospital because of the unrelenting pain. The patient reports that just prior to examination by the physician, she experienced a sudden decrease in intensity of pain, but she remains feeling very uncomfortable and must remain on the stretcher. On examination the patient appears in distress secondary to pain, tachycardic, slightly hypotensive, and febrile at 39°C (102°F). She has a diffusely tender abdomen with point tenderness over her right lower quadrant, accompanied by guarding and rebound. Laboratory values showed a leukocytosis of 20,000/mm³ with 95% polymorphonuclear lymphocytes. After confirming the diagnosis with imaging, which of the following is the most appropriate management?
Emergent appendectomy and postoperative antibiotics
Give nothing by mouth with intravenous hydration
Percutaneous drainage and interval appendectomy
Serial abdominal examinations
Urgent ECG and cardiac enzymes
A 24-year-old woman presents to her primary care provider because of bloody diarrhea for several months and uveitis. Complete blood cell count shows mild anemia but a normal WBC count. The erythrocyte sedimentation rate and the C-reactive protein level are not elevated. Which of the following is the most likely diagnosis?
Bacterial enterocolitis
Bowel ischemia
Colon carcinoma
Mallory-Weiss tear
Ulcerative colitis

A 47-year-old woman presents to the emergency department with an 8-day history of left lower quadrant pain and semi-formed stools. Starting this afternoon, she has noticed blood in her stool as well as dizziness when she gets up from sitting. She denies fever, nausea, vomiting, weight loss, and night sweats. Her temperature is 37°C (98.6°F), heart rate is 104/ min, blood pressure is 120/82 mm Hg supine and 103/63 mm Hg when she sits up, and respiratory rate is 18/min. Physical examination reveals no peritoneal signs and is remarkable only for fecal occult blood on rectal examination. Laboratory results reveal a WBC count of 13,000/mm³ and hematocrit of 29%. Results of an x-ray of the abdomen are shown in the image. What is the best next step in management?
Angiography with embolization
Immediate surgery for partial colectomy
Intravenous hydration and blood transfusion
Nothing by mouth, nasogastric tube, and broad-spectrum antibiotics
Place the patient on a high-fiber diet
A 66-year-old woman presents to her physician because of recurrent painless bleeding on defecation over the past month. She has regular, soft bowel movements and no history of constipation or diarrhea. A recent diagnosis of aortic stenosis was an incidental finding on echocardiogram. She takes calcium and vitamin D supplements daily. Her last colonoscopy (at age 60) was normal. Heart rate is 82/min, blood pressure is 133/72 mm Hg, respiratory rate is 12/min, and temperature is 36.6°C (97.8°F). Physical examination reveals her conjunctivae are pink and mucosa is moist. She has no abdominal tenderness or palpable masses and no hemorrhoids or fissures. Stool is hemoccult positive. Colonoscopy shows a spider-like lesion in the ascending colon. Which of the following is the most likely diagnosis?
Angiodysplasia
Crohn’s disease
Diverticulosis
Ischemic colitis
Peptic ulcer disease
A 61-year-old woman is brought to the emergency department drowsy and disoriented, able only to follow simple commands. On examination her abdomen is distended and nontender, her skin has a yellow hue, and there are multiple spider nevi on her chest. In her purse, the physician finds prescriptions for peginterferon and ribavirin. When asked to raise her hands, the physician notices a coarse tremor. Laboratory tests show: Blood urea nitrogen: 17 mg/dL Creatinine kinase: 1.1 mg/dL Aspartate aminotransferase: 89 U/L Alanine aminotransferase: 93 U/L Total bilirubin: 3.1 mg/dL Ammonia: 124 μg/dL Which of the following is the most likely diagnosis?
Bleeding esophageal varices
Hepatic encephalopathy
Hepatocellular carcinoma
Hepatorenal syndrome
Spontaneous bacterial peritonitis

A 74-year-old man presents to the emergency department with abdominal pain. The pain is deep and aching and is localized to the left lower quadrant. The man reports multiple episodes of diarrhea over the preceding week. He also reports having multiple similar episodes of abdominal pain in the past. On physical examination he is febrile and has tenderness to palpation of the left lower quadrant. His WBC count is 23,000/mm³. Results of CT are shown in the image. Which of the following is the most likely diagnosis?
Angiodysplasia
Carcinoid syndrome
Carcinoma of the colon
Diverticulitis
Infectious colitis
A 62-year-old woman presents to her physician with complaints of heartburn, fatigue, and intermittent upper abdominal pain. The pain is often worse after meals and especially with spicy foods. She reports no recent nausea, vomiting, weight loss, dysphagia, or bright-red blood per rectum. However, her stools are darker than normal. Her last colonoscopy 2 years ago was unremarkable. Stool guaiac test result is positive. An initial complete blood cell count reveals: Hemoglobin: 10.1 g/dL Hematocrit: 33.2% Mean corpuscular volume: 74.6/mm³ Mean corpuscular hemoglobin concentration: 25.8% WBC count: 9200/mm³ Platelet count: 176,000/mm³ Ferritin: 11 ng/mL The patient undergoes upper endoscopy, which reveals erosive gastritis. She is started on omeprazole, 40 mg twice a day and oral iron sulfate supplementation, 325 mg three times a day with meals. Six months into treatment, abdominal pain and heartburn are resolved, but the patient still has fatigue and is pale. Repeat laboratory tests show: Hemoglobin: 9.9 g/dL Hematocrit: 30.2% Mean corpuscular volume: 74.2/mm³ Mean corpuscular hemoglobin concentration: 25.1% WBC count: 9800/mm³ Platelet count: 198,000/mm³ Ferritin: 10 ng/mL Repeat upper endoscopy is negative for bleeding and erosive gastritis. Stool guaiac test result is negative. Which of the following is the next best step in management?
Bone marrow biopsy
Determine blood type and screen for trans- fusion
Discontinue omeprazole therapy
Initiate darbepoetin therapy
Initiate parenteral iron therapy
An 82-year-old woman is in the surgical intensive care unit after a carotid endarterectomy. She has been taking clindamycin and ciprofloxacin for the past 13 days. On postoperative day 2 the patient is febrile and tachycardic with a high WBC count and a low RBC count. She is also noted to be dehydrated and hypotensive. On physical examination she is distended and has abdominal tenderness with rebound and guarding. Barium enema reveals colonic dilatation of 8 cm. Stool is sent for Gram stain and analysis for fecal leukocytes, fecal occult blood, and Clostridium difficile toxin. Which of the following is most likely present in the stool sample?
Clostridium difficile toxin
Gram-negative rods
Gram-positive cocci
No fecal occult blood
Spores and hyphae
A 51-year-old man presents to the ED complaining of epigastric pain that radiates to his back. He states that he drinks six packs of beer daily. You suspect he has pancreatitis. His BP is 135/75 mm Hg, HR is 90 beats per minute, temperature is 100.1°F, and his RR is 17 breaths per minute. Laboratory results reveal WBC 13,000/μL, hematocrit 48%, platelets 110/μL, amylase 1150 U/L, lipase 1450 IU, lactate dehydrogenase (LDH) 150 U/L, sodium 135 mEq/L, potassium 3.5 mEq/L, chloride 105 mEq/L, bicarbonate 23 mEq/L, BUN 15 mg/dL, creatinine 1.1 mg/dL, and glucose 125 mg/dL. Which of the following laboratory values are most specific for pancreatitis?
Elevated amylase
Hyperglycemia
Elevated lipase
Elevated LDH
Leukocytosis
A 51-year-old man describes 1 week of gradually worsening scrotal pain and dysuria. He is sexually active with his wife. His temperature is 100.1°F, HR 81 beats per minute, BP 140/75 mm Hg, and oxygen saturation is 99% on room air. On physical examination, his scrotal skin is warm and erythematous. A cremasteric reflex is present. The posterior left testicle is swollen and tender to touch. Color Doppler ultrasonography demonstrates increased testicular blood flow. Urinalysis is positive for leukocyte esterase. What is the most likely diagnosis?
Epididymitis
Testicular torsion
UTI
Testicular tumor
Varicocele
A 40-year-old woman presents to the ED complaining of fever and 1 day of increasingly severe pain in her RUQ. She denies nausea or vomiting and has no history of fatty food intolerance. The patient returned from a trip to Mexico 6 months ago. About 2 weeks ago she experienced intermittent diarrhea with blood-streaked mucus. Her BP is 130/80 mm Hg, HR is 107 beats per minute, temperature is 102°F, and RR is 17 breaths per minute. Physical examination reveals decreased breath sounds over the right lung base. Abdominal examination shows tenderness to percussion over the RUQ and normal active bowel sounds. There is no Murphy sign. Her WBC is 20,500/μL. Chest radiograph reveals a small right-pleural effusion. Which of the following is the most likely diagnosis?
Amebic abscess
Cholecystitis
Cryptosporidium
Enterobiasis
Pyogenic abscess
A 25-year-old G3P1011 presents to the ED with a 6-hour history of worsening lower abdominal pain, mostly in the RLQ. She also noticed some vaginal spotting this morning. She is nauseated, but did not vomit. Her last menstrual period was 2 months ago, but her cycles are irregular. She is sexually active and has a history of pelvic inflammatory disease. Her BP is 120/75 mm Hg, HR is 95 beats per minute, temperature is 99.2°F, and RR is 16 breaths per minute. Her abdomen is tender in the RLQ. Pelvic examination reveals right adnexal tenderness. Her WBC count is slightly elevated and her β-hCG is positive. After establishing IV access, which of the following is the most appropriate next step in management?
Call the OR to prepare for laparoscopy.
Order an emergent CT scan of the abdomen
Perform a transvaginal ultrasound.
Order a urinalysis.
Swab her cervix and treat for gonorrhea and Chlamydia.
A 40-year-old Asian woman presents to the emergency department complaining of intermittent epigastric pain. The pain is severe, lasts for a few hours, and is sometimes accompanied by nausea and vomiting. Her bowel movements have been normal. Her temperature is 38.3°C (100.9°F), pulse is 100/min, blood pressure is 150/80 mm Hg, and respiratory rate is 22/min. Physical examination reveals moderate obesity and mildly icteric sclerae. Bowel sounds are normal, with an abrupt halt of inspiration upon palpation of the RUQ, and guarding is noted. Laboratory values reveal a WBC count of 13,000/mm³, total bilirubin of 3.3 mg/dL, and normal liver enzymes and alkaline phosphatase levels. Which of the following is the first diagnostic imaging study that should be performed?
CT
Flat and upright plain x-rays of the abdomen
Hepatobiliary iminodiacetic acid scan
MRI
Ultrasound of the RUQ
A 20-year-old man presents with several weeks of painful rectal bleeding. He denies fever, nausea, or vomiting. He is sexually active with women only and usually uses condoms. He denies any history of CD, UC, or malignancy. He states that the pain is most severe during and immediately after defecating. Bleeding is bright red and only enough to stain the toilet paper. Which of the following is the most common etiology of painful rectal bleeding?
External hemorrhoid
Anal fissure
Anorectal tumor
Internal hemorrhoid
Venereal proctitis
A 57-year-old woman presents to the ED with a basin in her hand and actively vomiting. You insert an IV catheter, start IV fluids, and administer an antiemetic agent. The patient feels much better but also complains of severe crampy abdominal pain that comes in waves. You examine her abdomen and note that it is distended and that there is a small midline scar in the lower abdomen. Upon auscultation, you hear high-pitched noises that sound like “tinkles.” Palpation elicits pain in all four quadrants but no rebound tenderness. She is guaiac negative. Which of the following is the most common cause of this patient’s presentation?
Travel to Mexico
Ethanol abuse
Hysterectomy
Hernia
Constipation
You are working in the ED on a Sunday afternoon when four people present with acute-onset vomiting and crampy abdominal pain. They were all at the same picnic and ate most of the same foods. The vomiting began approximately 4 hours into the picnic. They deny having any diarrhea. You believe they may have “food poisoning” so you place IV lines, administer IV fluids, and observe. Over the next few hours, the patients begin to improve, the vomiting stops, and their abdominal pain resolves. Which of the following is the most likely cause of their presentation?
Scombroid fish poisoning
Staphylococcal food poisoning
Clostridium perfringens food poisoning
Campylobacter
Salmonellosis
A premature newborn is being treated in the neonatal intensive care unit. On the sixth day of life he is noted to be lethargic and in mild respiratory distress. His heart rate is 162/min, blood pressure is 55/38 mm Hg, and respiratory rate is 56/min. In addition to a distended abdomen, he has guaiacpositive stools. X-ray of the abdomen shows gas bubbles within the bowel wall. From what potentially life-threatening condition is this patient most likely suffering?
Bowel obstruction
Intussusception
Meconium ileus
Meningitis
Necrotizing enterocolitis
A 45-year-old white man is brought to the emergency department by ambulance. He is waving wildly, trying to hit the “flying bats” that are all around him. He is very agitated and smells strongly of alcohol. The ambulance crew said they found the patient bleeding from the mouth outside a bar. They could not find any laceration on his mouth or lips and believe that the bleeding is internal. The patient screams that he will not stand for this maltreatment any longer and tries to stand up, at which point he begins to vomit. Blood pours out of his mouth, and the patient says, “Here we go again.” The ambulance crew tells the physician that there was also a lot of vomit at the bar where he was found. The physician is able to subdue the patient to obtain his vital signs. His blood pressure is 118/78 mm Hg, pulse is 98/ min, respiratory rate is 22/min, and temperature is 37.2°C (98.9°F). The physician is unable to obtain a history on the patient or con- tact any relatives or friends. No signs of obvious trauma are observed. Which of the following is the best next step in diagnosis?
Barium swallow
Electrocardiogram
Endoscopy
Esophageal manometry
X-ray of the chest
A 65-year-old man comes to the emergency department complaining of left lower abdominal pain that began the prior morning. He became concerned when he developed bloody diarrhea overnight. He has experienced similar pain, although to a lesser degree, over the past 2 months, especially after eating. The pain usually resolved within 1–2 hours, and he never had bloody diarrhea. His past medical history is significant for coronary artery disease and hypertension. He has smoked one pack of cigarettes per day for the past 30 years. On physical examination he is afebrile, heart rate is 90/min, and blood pressure is 135/85 mm Hg. He is visibly uncomfortable but in no apparent distress. His abdominal examination is significant for left lower quadrant tenderness but no guarding or rebound. Which of the following is the most likely diagnosis?
Acute mesenteric ischemia
Colon cancer
Diverticulitis
Infectious colitis
Inflammatory bowel disease
A 53-year-old man presents to the emergency department with severe epigastric abdominal pain. His temperature is 37.2C, blood pressure 110/70 mm Hg, pulse 110/min, and respirations 20/min. Examination of the heart and lungs is normal, and his abdomen is tender in the epigastric region. His white count is 15,000/mL and amylase is 450 U/L (25–125 U/L). Which of the following laboratory abnormalities is also most likely to be present?
Hypoglycemia
Hypercholesterolemia
Hyperglycemia
Hypercalcemia
Hypercarbia
A 43-year-old man feels vaguely unwell. Physical examination is unremarkable except for evidence of scleral icterus. The skin appears normal. Which of the following is the most likely explanation for why early jaundice is visible in the eyes but not the skin?
The high type II collagen content of scleral tissue
The high elastin content of scleral tissue
The high blood flow to the head with consequent increased bilirubin delivery
Secretion via the lacrimal glands
The lighter color of the sclera
A 25-year-old previously healthy man experiences fatigue and malaise. One week ago he had a “viral” type illness consisting of a sore throat, fever, and myalgias. He now appears jaundiced, but the rest of the physical examination is normal. His investigations reveal a total bilirubin of 4 mg/dL (0.1– 1.0 mg/dL) and a direct bilirubin of 0.3 mg/dL (0.0–0.3 mg/dL). Which of the following is the most likely diagnosis?
Hemolysis
Gallstones
Alcoholic liver disease
Pancreatic carcinoma
Dubin-Johnson syndrome
A 49-year-old man is brought to the ED by EMS stating that he vomited approximately three cups of blood over the last 2 hours. He also complains of epigastric pain. While examining the patient, he has another episode of hematemesis. You decide to place an NG tube. You insert the tube, confirm its placement, and attach it to suction. You retrieve 200 mL of coffee-ground blood. What is the most common etiology of an upper GI bleed?
Varices
Peptic ulcer
Gastric erosions
Mallory-Weiss tear
Esophagitis
A 56-year-old woman becomes the chief financial officer of a large company and, several months thereafter, develops upper abdominal pain that she ascribes to stress. She takes an over-the-counter antacid with temporary benefit. She uses no other medications. One night she awakens with nausea and vomits a large volume of coffee grounds-like material; she becomes weak and diaphoretic. Upon hospitalization, she is found to have an actively bleeding duodenal ulcer. Which of the following statements is true?
The most likely etiology is adenocarcinoma of the duodenum.
The etiology of duodenal ulcer is different in women than in men.
The likelihood that she harbors Helicobacter pylori is greater than 50%
Lifetime residence in the United States makes H pylori unlikely as an etiologic agent.
Organisms consistent with H pylori are rarely seen on biopsy in patients with duodenal ulcer.
A 63-year-old woman with cirrhosis caused by chronic hepatitis C is hospitalized because of confusion. She has guaiac-positive stools and a low-grade fever. She has received lorazepam for sleep disturbance. On physical examination, the patient is confused. She has no meningeal signs and no focal neurologic findings. There is hyperreflexia and a nonrhythmic flapping tremor of the wrists. Which of the following is the most likely explanation for this patient’s mental status change?
Tuberculous meningitis
Subdural hematoma
Alcohol withdrawal seizure
Hepatic encephalopathy
Central nervous system vasculitis from cryoglobulinemia
A 40-year-old white male complains of weakness, weight loss, and abdominal pain. On examination, the patient has diffuse hyperpigmentation and a palpable liver edge. Polyarthritis of the wrists and hips is also noted. Fasting blood sugar is 185 mg/dL. Which of the following is the most likely diagnosis?
Insulin-dependent diabetes mellitus
Pancreatic carcinoma
Addison disease
Hemochromatosis
Metabolic syndrome
A 55-year-old white woman has had recurrent episodes of alcoholinduced pancreatitis. Despite abstinence, the patient develops postprandial abdominal pain, bloating, weight loss despite good appetite, and bulky, foul-smelling stools. KUB shows pancreatic calcifications. In this patient, you should expect to find which of the following?
Diabetes mellitus
Malabsorption of fat-soluble vitamins D and K
Guaiac-positive stool
Courvoisier sign
Markedly elevated amylase
A 34-year-old white woman is treated for a UTI with amoxicillin. Initially she improves, but 5 days after beginning treatment, she develops recurrent fever, abdominal bloating, and diarrhea with six to eight loose stools per day. What is the best diagnostic test to confirm your diagnosis?
Identification of Clostridium difficile toxin in the stool
Isolation of C difficile in stool culture
Stool positive for white blood cells (fecal leukocytes)
Detection of IgG antibodies against C difficile in the serum
Visualization of clue cells on microscopic examination of stool
{"name":"USMLE : ENT-GIT 265 GD", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 28-year-old Caucasian male presents to the emergency department complaining of neck pain for the past two days. He states that a chicken bone scratched the back of his throat a week ago. Two weeks ago, he was in Arizona visiting his friends. He is otherwise healthy and has never been hospitalized. His temperature is 39°C (102.2F), blood pressure is 125\/85 mmHg, and heart rate is 120\/min. On examination, he refuses to fully open his mouth. Neck movements, especially neck extension, are restricted secondary to pain. Which of the following is the most likely diagnosis?","img":"https://cdn.poll-maker.com/10-457820/14699807-1138289712927932-1332690696-n.jpg?sz=1200-000000088053"}
More Quizzes
Fun Submarine quiz
10515
Safety Bubble
520
Week 4
940
What do you know about Copaiba?
520
Can You Master the Language Experience Approach?
201023842
International Collaborations for Global Impact
15822403
Take the Ultimate Free Should I Get a Dog Now!
201027572
Can You Ace the Leviticus 19-21? Test Your Bible IQ!
201035497
Dolly the Sheep Crossword: Challenge Your Brain Now
201040899
Geotechnical Engineering
15819853
Free Neuro-Linguistic Programming Knowledge Test
201022742
Think You Know American Culture? Take This Trivia Challenge!
201031129