Function of Ceruminous Glands: Earwax Secretions Quiz
Quick integumentary practice test on earwax gland secretions. Instant results.

This quiz helps you check your understanding of the function of ceruminous glands and their earwax secretions. You will answer quick questions that reinforce what cerumen does, how it protects the canal, and where these glands sit in the skin. For a wider review, explore the anatomy of the ear quiz, layers of the skin quiz, and ear labeling quiz.
Study Outcomes
- Identify Skin Layers -
Readers will be able to recognize the epidermis, dermis, and hypodermis and describe their major functions.
- Differentiate Skin Glands -
Readers will distinguish eccrine, apocrine, and sebaceous glands, understanding their secretions and physiological roles.
- Explain Protective Mechanisms -
Readers will clarify how the integumentary system safeguards against pathogens, UV damage, and dehydration.
- Apply Knowledge in Quizzes -
Readers will leverage questions about the integumentary system in our integumentary quiz and integumentary practice test to reinforce concepts and prepare for an integumentary system exam.
- Analyze Thermoregulatory Processes -
Readers will assess how sweat glands, blood flow, and hair follicles collaborate to maintain body temperature.
- Recall Key Facts for Mastery -
Readers will retrieve essential terminology and facts to enhance retention and confidence in integumentary system quizzes.
Cheat Sheet
- Master the Epidermal Strata -
Understand the five layers of the epidermis - stratum corneum, lucidum, granulosum, spinosum, and basale - using the mnemonic "Come, Let's Get Sun Burned." According to Gray's Anatomy, memorizing this hierarchy is a staple for any integumentary quiz or integumentary system exam question. Regularly test yourself with sample integumentary practice test items to reinforce these layers in a questions about the integumentary system format.
- Differentiating Sweat Gland Types -
Eccrine glands regulate body temperature through watery secretion while apocrine glands, found in axillae and groin, release lipid-rich sweat tied to emotional stimuli. The American Academy of Dermatology notes that eccrine activity peaks in palms and soles, a fact often quizzed on integumentary system quizzes. Try drawing a simple diagram labeling each gland's location to cement this concept for your next integumentary quiz.
- Melanin Synthesis Pathway -
Melanocytes in the stratum basale convert tyrosine to DOPA via tyrosinase, ultimately producing melanin that shields DNA from UV damage. This enzyme-driven reaction, detailed in peer-reviewed dermatology journals, is central for understanding skin pigmentation questions about the integumentary system. A quick tip: remember "Tyrosinase Tackles Tyrosine" to recall the enzyme's role on your integumentary practice test.
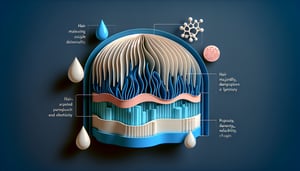
- Barrier Function of the Stratum Corneum -
The "brick-and-mortar" model describes corneocytes as bricks and intercellular lipids as mortar, forming a waterproof barrier that prevents transepidermal water loss. Studies from the National Institute of Arthritis and Musculoskeletal and Skin Diseases emphasize ceramides' role in maintaining this barrier, a high-yield topic on any integumentary system exam. Sketching this model helps you visualize and ace those integumentary system quizzes.
- Phases of Wound Healing -
Wound repair occurs in four phases - Hemostasis, Inflammation, Proliferation, and Remodeling - often recalled by the acronym "H I P R." The Journal of Dermatological Science highlights growth factors like PDGF in the proliferation phase, a concept that frequently appears in integumentary quiz questions. Create flashcards for each phase to boost confidence and accuracy on your next practice test.