Med management 2 Q1 to 50
1) A 10-year-old girl with blue eyes and blonde hair is brought to the office by her mother for a routine check-up. All her immunizations are up to date. Her family history is significant for myocardial infarction in her father and schizophrenia in a maternal uncle. There is no family history of any skin malignancies. Her height is at the 60th percentile, and weight is at the 56th percentile. While you are examining her, the mother says with much concern that she saw a television program that claimed that the incidence of skin cancer is increasing dramatically. She wants to know the best way to prevent skin cancer in her daughter, especially since they live in California. What is the best advice to help prevent malignant melanoma in this child?
. Sun screen lotion with SPF (sun protection factor) 15
. Sun screen lotion with SPF 30
. Protective clothing
. Avoid going outdoors
. No action needs to be taken, since there is no family history of melanoma
2) A 50-year-old man comes to the emergency department due to acute onset respiratory difficulty. He also has periorbital, circumoral and facial edema. Two weeks ago, he experienced chest pain, profuse sweating and anxiety, and was subsequently admitted to the cardiac intensive care unit. At that time, his ECG showed ST segment elevation and Q waves in the inferior leads. He was taken to the catheterization lab and had an angioplasty with stent done for 100% occlusion of the right coronary artery. He was discharged with the following medications: aspirin, clopidogrel, metoprolol, enalapril, simvastatin and isosorbide mononitrate. In the ED, his pulse is 102/min, blood pressure is 110/70 mmHg, respirations are 24/min and temperature is 36.8°C (98.4°F). Which of the following is most likely responsible for his present symptoms?
. Metoprolol
. lsosorbide
. Clopidogrel
. Aspirin
. Enalapril
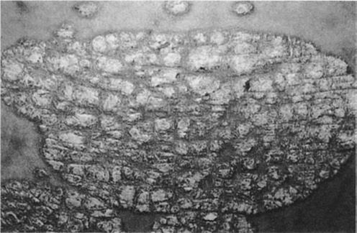
3) A 25-year-old male presents with skin lesions over his elbows, knees and neck. He complains of intense itching and burning sensation over these lesions for the past 10 days. He was advised to follow a gluten-free diet on his previous visit, but was not compliant. His vital signs are stable. On examination, there are flesh-colored to erythematous vesicles distributed over the extensor aspects of elbows, knees, posterior neck and shoulders. Some of these lesions are shown in the picture below. Which of the following is the drug of choice for his skin condition?

Image

. High potency steroids
. Low dose acyclovir
. 1% lindane solution
. Azathioprine
. Dapsone
4) A 20-year-old woman complains of skin problems and is noted to have erythematous papules on her face with blackheads (open comedones) and whiteheads (closed comedones). She has also had cystic lesions. She is prescribed topical tretinoin, but without a totally acceptable result. You are considering oral antibiotics, but the patient requests oral isotretinoin, which several of her college classmates have used with benefit. Which of the following statements is correct?
. The teratogenic effects of isotretinoin are its only clinically important side effects
. The patient will not benefit from topical antibiotics since she did not respond to topical retinoids
. Intralesional triamcinolone should be avoided due to its systemic effects
. Systemically administered isotretinoin therapy cannot be considered unless concomitant contraceptive therapy is provided
. Antimicrobial therapy is of no value since bacteria are not part of the pathogenesis of the process
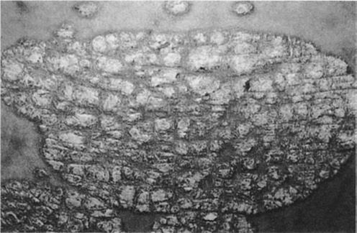
5) A 22-year-old male presents with a 6-month history of a red, nonpruritic rash over the trunk, scalp, elbows, and knees. These eruptions are more likely to occur during stressful periods and have occurred at sites of skin injury. The patient has tried topical hydrocortisone without benefit. On examination, sharply demarcated plaques are seen with a thick scale. Pitting of the fingernails is present. There is no evidence of synovitis. What is the best first step in the therapy of this patient’s skin disease?
Image
. Photochemotherapy (PUVA)
. Oral methotrexate
. Topical calcipotriene
. Oral cyclosporine
. Topical fluticasone
6) A 35-year-old woman develops an itchy rash over her back, legs, and trunk several hours after swimming in a lake. Erythematous, edematous papules and plaques are noted. The wheals vary in size. There are no mucosal lesions and no swelling of the lips. What is the best first step in management of her symptomatic rash?
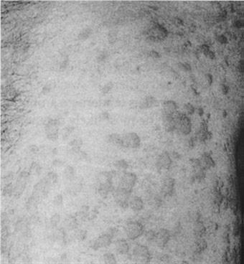
Image
. Subcutaneous epinephrine
. Intravenous glucocorticoids
. Oral antihistamines (H1 blockers)
. Aspirin
. Oral doxycycline
7) A 64-year-old woman presents with diffuse hair loss. She says that her hair is “coming out by the handfuls” after shampooing. She was treated for severe community-acquired pneumonia 2 months ago but has regained her strength and is exercising regularly. She is taking no medications. Examination reveals diffuse hair loss. Several hairs can be removed by gentle tugging. The scalp is normal without scale or erythema. Her general examination is unremarkable; in particular, her vital signs are normal, she has no pallor or inflammatory synovitis, and her reflexes are normal with a normal relaxation phase. What is the best next step in her management?
. Reassurance
. Measurement of serum testosterone and DHEA-S levels
. Topical minoxidil
. Topical corticosteroids
. CBC and antinuclear antibodies
8) A 63-year-old retired farmer presents to the clinic complaining of red scaly spots on his head for the past 9 months. Physical examination is remarkable for numerous erythematous hyperkeratotic papules and plaques. The lesions are confined to the head and forehead and have poorly defined borders. Which of the following is the most appropriate next step in management of this patient?
. Punch biopsy of one of the lesions
. Application of hydrocortisone cream to affected areas and follow-up in 4 weeks
. Reassurance that this is a benign finding and follow-up in 6 months
. Application of fluocinide cream to affected areas and follow-up in 4 weeks
. Application of 5-fluorouracil cream to affected areas and follow-up in 4 weeks
9) A 21-year-old female presents with an annular pruritic rash on her neck. She explains that the rash has been present for the past 3 weeks and that her roommate had a similar rash not long ago. Physical examination is remarkable for a 20-mm scaling, erythematous plaque with a serpiginous border. Which of the following is the most appropriate initial treatment for this condition?
. Griseofulvin
. Oral cephalexin
. Topical mupirocin ointment
. Topical ketoconazole
. Hydrocortisone cream
10) A 50-year-old male comes to the office due to an ulcer in his right foot. He has type 2 diabetes, for which he takes glyburide. Laboratory investigations reveal an HbA1c of 9%, and random blood sugar of 180 mg/dL. X-ray of the leg/foot is normal. A picture of the foot ulcer is shown below. Which of the following is the most appropriate management of this patient's foot ulcer?

Image

. Start aspirin and atorvastatin
. Perform thorough debridement of the wound
. Prescribe tight-fitting shoes
. Prescribe oral antibiotics and follow-up as an outpatient
. Amputation
11) A 65-year-old Caucasian male comes to the office because of bilateral foot pain, which is present at rest and worsens at night. He has been having this symptom for the past few months. Other accompanying symptoms are hyperesthesia and paresthesia in both lower limbs. His medical problems include diabetes for the past twenty years. His daily medication is insulin. Physical examination reveals bilateral loss of ankle reflexes, loss of vibratory sensation and altered proprioception below the knees. His HbA1c level is 9%. Urine is positive for microalbuminuria. Which of the following is the most appropriate treatment for his leg pain?
. Amitriptyline
. Corticosteroids
. Oxycodone
. Acetaminophen
. Ketorolac
12) A 55-year-old African-American male comes to the office for a routine follow-up visit. His past medical history is significant for type 2 diabetes mellitus (OM), hypertension for the last 5 years, and an acute myocardial infarction 2 years ago. His mother died of a heart attack at the age of 72 years, and his father died in a motor vehicle accident at the age of 42 years. He has no siblings. He is currently on glyburide, captopril and baby aspirin. He is very compliant with his diet and medication. His glycemic control was very good until a few months ago, when he noticed that his blood sugar levels were running high. This morning, his finger stick reading was 200 mg/dL. He weighs 188 lbs and is 5'8" tall. His physical examination is otherwise unremarkable. His blood work done three days ago showed blood urea nitrogen of 14 mg/dL and a creatinine level of 1.0 mg/dL. His HBA1c one month ago was 8.0%. Which of the following is the most appropriate next step in management?
. Discontinue captopril because it is known to produce diabeticogenic state
. Discontinue captopril since glyburide efficacy is reduced with simultaneous usage of captopril
. Start the patient on human insulin 70/30
. Add metformin to achieve better glycemic control
. Add pioglitazone to achieve better glycemic control
13) A 60-year-old male comes to the office due to edema of his face and ankles of two weeks duration. He denies any chest pain or breathlessness. He is a known diabetic for the past 15 years. His diabetes is being managed with exercise, dietary modification and glyburide. His glycosylated hemoglobin (HbA1C) level one month ago was 7.5%. His temperature is 37.0°C (98.6°F), pulse is 75/min, blood pressure is 146/87 mmHg, and respirations are 15/min. Examination is unremarkable, except for bilateral pitting edema around the ankles and periorbital edema. Lab results show: Serum sodium 140 mEq/L, Potassium 4.3 mEq/L, Bicarbonate 20 mEq/L, Blood glucose120 mg/dL, Blood urea nitrogen 37 mg/dL, Serum creatinine 24 mg/dL, Total cholesterol 300 mg/dl. EKG is normal. 24 hour urine collection shows 3.7 g protein/day. To alter the course of this patient's diabeticnephropathy, what is the most appropriate next step in management?
. Intensive glycemic control
. Intensive blood pressure control
. Very low protein diet
. Aggressive lipid management
. Aspirin therapy
14) A 40-year-old white female presents with complaints of heat intolerance, sweating and palpitations. She also reports menstrual irregularities, increased appetite and diarrhea. She has had these symptoms for the past 4 Months. Her pulse is 102/min and regular, blood pressure is 116/80 mmHg, temperature is 37.2°C (99°F), and respirations are 14/min. Physical examination reveals a non-tender, diffuse swelling in front of her neck; it moves upwards with deglutition. Her TSH level is 0.05 mU/L. Free T4 and T3 levels are increased. Radioactive iodine uptake at 24 hours is significantly increased. Pregnancy test is negative. Which of the following is the most appropriate long-term treatment modality for this patient?
. Surgery
. Propylthiouracil
. Iodinated contrast agents
. Radioactive iodine therapy
. Propranolol
15) A 50-year-old Caucasian male comes to the office for the evaluation of polyuria and polydypsia for the last two months. He also complains of weakness and fatigue. He had one episode of transient proximal muscle weakness which lasted 30 minutes. He has a 20-pack year history of smoking. He does not drink alcohol. His past medical and family histories are insignificant. His pulse is 78/min, blood pressure is 150/96 mmHg and temperature is 36.7°C (98°F). The rest of the examination, including the neurological examination, is normal. Labs show: Plasma sodium 150 mEq/L, Potassium 2.6 mEq/L, Serum creatinine 0.8 mg/dL. Which of the following is the most appropriate next step in the management of this patient?
. Measurement of plasma renin activity and aldosterone concentration
. Measurement of 24 hour urinary potassium excretion
. Aldosterone suppression testing
. Imaging of adrenals by CT scan
. Adrenal vein sampling
16) A 78-year-old female is being evaluated for recent weight loss and fatigue. Laboratory tests reveal abnormal thyroid function. She begins treatment with a single agent, but soon after is hospitalized with new onset atrial fibrillation and hand tremor. Which of the following treatments had she most likely received?
. Propylthiouracil
. Lopanoic acid
. Radioactive iodine
. Propranolol
. Prednisone
17) A 60-year-old female presents with transient loss of consciousness. She appears lethargic and confused. She also complains of hemoptysis and weight loss of 10 lbs (4.5kg) over a period of 2 months. She has smoked one pack of cigarettes daily for the last 40 years. Her temperature is 37.0°C (98.6°F), pulse is 75/min, blood pressure is 110/70 mmHg, and respirations are 16/min. Her mucus membranes are moist. There is no jugular venous distention. Her neurological examination is non-focal, and cardiovascular examination is unrevealing. There is no ankle edema or ascites. Serum studies show: Sodium 115 mEq/L, Potassium 3.7 mEq/L, Bicarbonate 22 mEq/L, Blood glucose 100 mg/dL, BUN 10.0 mg/dL. Serum osmolality is 250 mOsm/Kg, and urine osmolality is 500 mOsm/Kg. Urine sodium concentration is 40 mEq/L. Chest x-ray shows a mass in the right hilar region. What is the most appropriate next step in the management of this patient?
. Normal saline
. Loop diuretics
. Water restriction
. Hypertonic saline
. Demeclocycline
18) A 40-year-old African American female comes to the office for a routine medical check-up. She has no complaints. She has twenty pack-year smoking history but she stopped smoking one year ago. Her mother and one maternal uncle have diabetes. Her height is 5'7" inches, and weight is 150 lbs. Her blood pressure is 122/80 mmHg, pulse is 80/min, respirations are 14/min and temperature is 37°C (98°F). She agrees to have diabetes mellitus screening. Her plasma glucose level after an overnight fast is 130 mg/dL. What is the most appropriate next step in the management of this patient?
. Repeat fasting blood glucose measurement
. Perform 75 g oral glucose tolerance test
. Start therapy with oral hypoglycemic agents
. Start therapy with insulin
. Recommend lifestyle changes
19) A 22-year-old female presents with complaints of heat intolerance, sweating and palpitations. She also reports menstrual irregularities, increased appetite and diarrhea. Her pulse is 102/min and regular, blood pressure is 116/80 mmHg, temperature is 37.2°C (99°F), and respirations are 14/min. Physical examination reveals a diffusely enlarged, nontender thyroid gland. TSH level is 0.05 mU/L. Free T4 and T3 levels are elevated. Radioactive iodine uptake at 24 hours is 50 percent. Thyroid stimulating immunoglobulins are present. She is started on propylthiouracil 300 mg daily in three divided doses. After two weeks, she returns and complains of a sore throat. Her pulse is 98/min and regular, temperature is 38.6°C (101.5°F), blood pressure is 115/76 mmHg, and respirations are 15/min. The soft palate, pharynx, and tonsils are red and swollen. What is the most appropriate next step in the management of this patient?
. Add propranolol
. Increase propylthiouracil dose
. Stop propylthiouracil
. Throat culture
. Oral penicillin
20) A 35-year-old female presents to the emergency department with a 30-minute history of severe headache, palpitations, abdominal pain, nausea, and vomiting. She had similar episodes twice during the last month, but those were not so severe and resolved spontaneously in 30-40 minutes. She visited a doctor recently, and hypertension with elevated urinary vanillylmandelic acid level was diagnosed. She is not taking any medications, and denies substance abuse. Her blood pressure is 200/130 mmHg and heart rate is 130/min. She appears frightened. Physical examination reveals hand tremors and excessive sweating. Slow intravenous infusion of propranolol is started while waiting for the routine labs. What is the most probable reaction to the treatment given to the patient?
. Blood pressure will slowly decrease
. Blood pressure will rapidly decrease
. Heart rate will increase
. Heart rate will not change
. Blood pressure will rapidly increase
21) A 65-year-old male comes to the office and complains of nausea and early satiety for the past several months. His other complaints are anorexia and abdominal bloating. He denies any heartburn or epigastric pain. He has diabetes, and has been taking insulin for the last fifteen 15 years. His blood glucose readings using the home blood glucose monitor range between 40 to 400 mg/dL. Most of the low blood glucose readings occur after meals. Which of the following is the most appropriate management of this patient's symptoms?
. Ondansetron
. Ibuprofen
. Metoclopramide
. Ranitidine
. Promethazine
22) Four of your patients who came to the office today all have signs and symptoms of hyperthyroidism. After the appropriate evaluation, you decided to treat them with radioactive iodine. Hyperthyroid patients with which of the following disorders are most likely to develop hypothyroidism following radioactive therapy?
. Graves' disease
. Toxic adenoma
. Multinodular goiter
. Ectopic production of thyroid hormones
. Thyroid Cancer
23) A 60-year-old Caucasian male presents to the office with erectile dysfunction that progressed slowly over the last several months. He finds it difficult to obtain an erection, and has noted a decrease in nocturnal erections. His past medical history is significant for diabetes mellitus, type 2 and benign prostatic hypertrophy (BPH). His current medications are glyburide and doxazosin. Physical examination is insignificant. HbA1c level measured two weeks ago was 7.5%. He is asking about a prescription for sildenafil. Which of the following is the best statement concerning the treatment of erectile dysfunction in this patient?
. Tightening of glycemic control improves erectile dysfunction
. Sildenafil is not a drug of choice for diabetics with erectile dysfunction
. Sildenafil and doxazosin should be given with at least a 4-hour interval
. Prostaglandins (alprostadil) are preferred in this patient
. Sildenafil should not be combined with glyburide
24) A 58-year-old asymptomatic male is found to have elevated levels of serum alkaline phosphate. His serum calcium and phosphate levels are normal. He denies any bone pain or deformity. His liver function tests are normal. The urinary hydroxyproline levels are increased. Nuclear bone scan reveals an increased uptake in the right scapula. Plain radiography confirms Paget's disease. Which of the following is the most appropriate next step in the management of this patient?
. No treatment is indicated at this stage
. Treatment with bisphosphonates
. Treatment with nasal calcitonin
. Treatment with calcium and vitamin D
. A CT scan of lung
25) A 25-year-old female comes to the office for a follow-up visit. She was just diagnosed with type 1 diabetes mellitus a few days ago, when she presented at the emergency department with ketoacidosis. After successful management of her diabetic ketoacidosis (DKA), she was sent home on an insulin regimen with the following dosage: Before breakfast 10 units of NPH and 10 units of regular insulin, Before supper 10 units of NPH and 4 units of regular insulin. During this office visit, she shows the record of her fingerstick readings at home. For the last 2 days, her blood glucose levels were (see in pic). What is the most likely explanation for her 7:00 am blood glucose level?
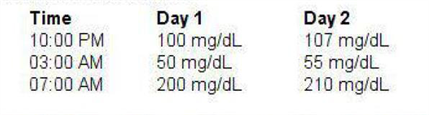
Image
. Spikes of growth hormone release
. Epinephrine, norepinephrine, & glucagon release
. Waning of insulin levels
. Destruction of glucagon-secreting cells
. Decrease Insulin-secretor
26) A 46-year-old male comes to your office for a routine health examination. He has no current physical complaints and says he is compliant with his medications. His past medical history is significant for type 2 diabetes diagnosed two years ago that he has been able to control with diet, exercise and metformin. The patient also takes a daily aspirin. On physical examination, he has a temperature of 36.7°C (98°F), a blood pressure of 140/86 mmHg, a pulse of 80/min, and respirations of 14/min. His laboratory studies show: Total cholesterol 170 mg/dl, High density lipoprotein (HDL) 50 mg/dl, Low density lipoprotein (LDL) 65 mg/dl, Triglycerides (TG) 150 mg/dl, HbA1C 7.0. Serum chemistries are with in normal limits. Which of the following is the most appropriate next step in the management of this patient?
. Add niacin
. Add gemfibrozil
. Add lisinopril
. Add ezetimibe
. Add insulin
27) A 60-year-old asymptomatic man presents to your office for a routine check-up. He has a 10-year history of type 2 DM, and a 12-year history of hypertension. His current medications include low-dose glyburide and a low-dose thiazide diuretic. His blood pressure is 140/90 mmHg and heart rate is 65/min. Physical examination shows a soft ejection systolic murmur at the base of the heart. Ophthalmoscopic evaluation reveals no abnormalities. ECG recorded 6 months ago showed left ventricular hypertrophy and non-specific ST segment and T-wave abnormalities. His recent fasting glucose level was in the range of 120 to 150 mg/dl, and HbA1c was 7.1 % (normal< 6%). 24-hour urine collection reveals microalbuminuria. Which of the following is the best measure to slow end-organ damage in this patient?
. Increase the dose of glyburide
. Increase the dose of thiazide diuretic
. Switch to insulin
. Add ACE inhibitor
. Add beta-blocker
28) A 21-year-old man with type 1 diabetes mellitus presents to the emergency department with complaints of abdominal pain, nausea and vomiting. His temperature is 36.0°C (97.0°F), pulse is 110/min, blood pressure is 102/60 mmHg, and respirations are 26/min. Lungs are clear to auscultation. Abdomen is soft, non-tender and non-distended. Chemistry panel shows: Sodium 130 mEq/L, Potassium 5.2 mEq/L, Chloride 90 mEq/L, Bicarbonate 10 mEq/L, Blood glucose 450 mg/dl. Which of the following is the most appropriate next step in management?
. Normal saline and regular insulin
. 0.45% saline and regular insulin
. Normal saline and NPH insulin
. 5% dextrose and NPH insulin
. Sodium bicarbonate
29) A 40-year-old female patient is brought to the office by her husband due to altered mental status and confusion of recent onset. According to her husband, she has been complaining of intense thirst, craving for ice water, and experiencing increased urination for the past few days. Her only medication is lithium for bipolar depression. Her temperature is 39.0°C (102.5°F), pulse is 102/min, blood pressure is 90/60 mmHg, and respirations are 15/min. Physical examination reveals a disoriented patient with dry skin and mucous membranes. Blood chemistry panel reveals: Sodium 156 mEq/L, Potassium 4.1 mEq/L, Bicarbonate 26 mEq/L, Blood glucose 102 mg/dl, BUN 27 mg/dl. Serum osmolality is 328 mOsm/kg, and urine osmolality is 180mOsm/Kg. What is the most appropriate next step in the management of this patient?
. Water deprivation test
. Plain water drinking
. IV infusion of normal saline
.IV infusion of 045% saline
. IV infusion of 5% dextrose
30) A 40-year-old asymptomatic male comes to the office for a routine physical examination. His serum chemistry panel shows: Sodium 140 mEq/L, Potassium 4.0 mEq/L, Bicarbonate 25 mEq/L, Chloride 101 mEq/L, Calcium 11.8 mg/dL, Albumin 4.0 g/dL, Phosphorus 2.2 mg/dL. 24-hour urine collection reveals a calcium level of 200 mg, and creatinine level of 1.7 g. Serum PTH level is increased. Bone mineral density by dual energy X-ray absorptiometry (DEXA) shows normal bone mineral density. Neck examination reveals no masses. What is the most appropriate next step in the management of this patient?
. Bisphosphonate therapy
. Surgical exploration of the neck
. Medical surveillance
. Loop diuretics
. Thiazide diuretics
31) A 38-year-old woman presents with several months of decreased libido and a 4.5-kg (10-lb) weight gain. She has not had her menstrual period for the past 3 months. Physical examination is unremarkable except that a small amount of white discharge is manually expressed from the nipples bilaterally. The serum prolactin level is 300 ng/mL. Which of the following is the most appropriate first-line treatment?
Bromocriptine
Cortisol
Methyldopa
Metoclopramide
Octreotide
32) A 72-year-old woman presents to her physician complaining of fatigue, malaise, weight loss, and salt cravings. The patient has chronic obstructive pulmonary disease and is intermittently treated with corticosteroids but is not using home oxygen. Her oxygen saturation is 97% on room air with a blood pressure of 115/65 mmHg, which is significantly lower than her baseline of 125/78 mmHg. On auscultation she has good breath sounds bilaterally without wheeze, although the expiratory phase is slightly prolonged. Five weeks ago she received a corticosteroid treatment for an acute chronic obstructive pulmonary disease exacerbation, for which she was hospitalized and given 3 L of oxygen via nasal cannula. However, she admits that after discharge she was having continued difficulty breathing and did not follow the taper of the corticosteroids. The patient has smoked one pack of cigarettes per day for the past 51 years. Which of the following is the appropriate first step in the management of this patient?
3 L of oxygen via nasal cannula
CT scan of the chest
Intravenous fluids
Restart corticosteroids and follow a strict taper
X-ray of the chest
33) An obese patient with a long-standing history of type 2 DM presents to his primary care physician. On examination he has decreased sensation in both lower extremities. Upon questioning of his compliance with his prescribed medications, he reports that he has stopped taking one medication because it gave him flatulence and abdominal pain. Which of the following did this man most likely stop taking?
An α-glucosidase inhibitor
Meglitinide
Metformin
Sulfonylurea
Thiazolidinedione
34) A 19-year-old G1P0 woman at 32 weeks gestation presents for scheduled prenatal appointment. The pregnancy has been uncomplicated to date. However, she mentions that she recently noticed a hard lump on her neck. She denies pain or difficulty swallowing, speaking, or breathing. Physical examination reveals a firm, nontender, immobile, solitary nodule on the left hemithyroid. Ultrasound reveals a solid 2-cm mass. There is no cervical lymphadenopathy. Thyroid function tests reveal a thyroid-stimulating hormone level of 1.2 μU/mL and free thyroxine level of 0.9 ng/dL. Results of fine-needle aspiration biopsy are shown in the image. Which of the following is the best next step in management?
Image
Left hemithyroidectomy
Monitor until after delivery
Radioablation therapy
Start methimazole
Start propylthiouracil
35) A 49-year-old man presents to the clinic for a health maintenance visit. He has a family history of type 2 DM. His medical history is significant for gastroesophageal reflux disease, for which he takes omeprazole and over-the-counter antacids. He smokes one pack of cigarettes per day and drinks an average of two beers per night. The patient’s body mass index is 32 kg/m². Which of the following most greatly reduce(s) the patient’s risk of future coronary artery disease, renal failure, and retinopathy?
Alcohol avoidance
Daily multivitamin
Diet rich in fruit and vegetables
Smoking cessation
Weight loss and exercise
36) A 37-year-old white female presents with galactorrhea and amenorrhea for the past 7 months. She denies any headaches, visual problems, vaginal dryness or dyspareunia. She is married, has two children, and remarks that her family is "complete." She does not use tobacco, alcohol or drugs. Her blood pressure is 120/80 mmHg, pulse is 72/min, temperature is 36.7°C (98.6°F) and respirations are 14/min. Visual field testing is within normal limits. Pregnancy test is negative. Her serum prolactin level is 150ng/ml. Pituitary MRI shows a 6mm pituitary adenoma. Which of the following is the most appropriate next step in the management of this patient?
. Surgery
. Treatment with cabergoline
. Treatment with estrogens
. Radiotherapy
. Monitoring by serum prolactin and MRI
37) A 32-year-old man presents to his primary care physician complaining of diffuse muscle weakness, dry and puffy skin, and patchy areas of hair loss on his scalp. He also notes numbness around his mouth and a tingling sensation in his hands and feet. He has a history of seizure disorder, and has been taking carbamazepine for the past 5 years. On physical examination he has dry skin and coarse, brittle hair with patchy alopecia. Tapping his right cheek causes contraction of the muscles at the corner of his mouth, nose, and eye on the right side. Which of the following could best have prevented the development of the patient’s current problem?
Magnesium supplementation
Parathyroidectomy
Thyroid hormone
Vitamin C supplementation
Vitamin D supplementation
38) A 30-year-old Caucasian female comes to the physician's office because of polyuria and polydipsia of recent onset. She has no other medical problems. She does not use tobacco, alcohol or drugs. She has no known drug allergies. Her mother has diabetes. Her temperature is 36.7°C (98°F), pulse is 75/min, blood pressure is 110/70 mmHg, and respirations are 15/min. The initial lab results are: Hb 12.7 g/dl, WBC 5,000 /cmm, Platelets 380,000/cmm, Blood glucose 90 mg/dl, Serum sodium 142 mEq/L, Serum potassium 4.0 mEq/L, Bicarbonate 26 mEq/L, BUN 15 mg/dl, Serum creatinine 0.9 mg/dl, Serum uric acid 9 mg/dl, Serum osmolality 295 mOsm/kg, Urine osmolality 160 mOsm/kg. After 12 hours of water deprivation, lab testing reveals:Serum sodium 151 mEq/L, Serum potassium 4.2 mEq/L, Bicarbonate 26 mEq/L, Serum osmolality 300 mOsm/kg, Urine osmolality 186 mOsm/kg. One hour after the subcutaneous administration of arginine vasopressin, the urine osmolality is 400mosm/kg. Which of the following is the most appropriate treatment for this patient?
. Psychotherapy
. Intranasal desmopressin acetate
. Indomethacin
. Hydrochlorothiazide
. Demeclocycline
39) A 42-year-old woman with no significant past medical history presents for a routine health maintenance visit. On physical examination a solitary nodule is palpated in the thyroid. She denies pain, dysphagia, or hoarseness. She also denies fatigue, weight change, heat or cold intolerance, diarrhea, or constipation. There is no family history of thyroid cancer. Her serum thyroid-stimulating hormone level is normal. Which of the following is the most appropriate next step in evaluation?
Fine-needle aspiration
MRI
Radionuclide scan
Thyroid lobectomy
Ultrasonography
40) A patient comes to your office for a new-patient visit. He has moved recently to your city due to a job promotion. His last annual examination was 1 month prior to his move. He received a letter from his primary physician stating that laboratory workup had revealed an elevated alkaline phosphatase and that he needed to have this evaluated by a physician in his new location. On questioning, his only complaint is pain below the knee that has not improved with over-the-counter medications. The pain increases with standing. He denies trauma to the area. On examination you note slight warmth just below the knee, no deformity or effusion of the knee joint, and full ROM of the knee without pain. You order an x-ray, which shows cortical thickening of the superior fibula and sclerotic changes. Laboratory evaluation shows an elevated alkaline phosphatase of 297 mg/dL with an otherwise normal metabolic panel. Which of the following is the treatment of choice for this patient?
. Observation
. Nonsteroidal anti-inflammatory
. A bisphosphonate
. Melphalan and prednisone
. Ursodeoxycholic acid (UDCA)
41) Your patient is a 48-year-old Hispanic male with a 4-year history of diabetes mellitus type 2. He is currently utilizing NPH insulin/Regular insulin 40/20 units prior to breakfast and 20/10 units prior to supper. His supper time has become variable due to a new job and ranges from 5 to 8 PM. In reviewing his glucose diary, you note some very low readings (40-60 mg/dL) during the past few weeks at 3 AM. When he awakens to urinate, he feels sweaty or jittery so has been checking a fingerstick blood glucose. Morning glucose levels following these episodes are always higher (200-250) than his average fasting glucose level (120-150). Which change in his insulin regimen is most likely to resolve this patient’s early AM hypoglycemic episodes?
. Increase morning NPH and decrease evening NPH
. Decrease morning NPH and decrease evening regular insulin
. Change regimen to glargine at bedtime and continue morning and evening regular insulin
. Discontinue both NPH and regular insulin; implement sliding scale regular insulin with meals
. Change regimen to glargine at bedtime with lispro prior to each meal
42) A 32-year-old G2P1 woman at 16 weeks gestation presents to her obstetrician complaining of fatigue, anxiety, and palpitations. She says she has been feeling warm, even in her air-conditioned home, and has been having three or four loose stools per day, as compared to one or two prior to her pregnancy. She has a temperature of 37.1°C (98.9°F), heart rate of 105/min, and blood pressure of 128/76 mmHg. Neck examination reveals mild diffuse enlargement of the thyroid gland with no lymphadenopathy. Relevant laboratory findings include a total triiodothyronine level of 400 ng/dL, free thyroxine of 6.8 ng/dL, and thyroid-stimulating hormone of 0.01 μU/mL (normal: 0.4–4 μU/L). Results of a thyroid- stimulating hormone-receptor antibody test are positive. Which of the following is the most appropriate therapy for this patient?
High-dose iodine therapy
Methimazole
Propylthiouracil
Radioiodine ablation
Surgical resection
43) A 50-year-old female is 5 ft 7 in tall and weighs 185 lb. There is a family history of diabetes mellitus. Fasting blood glucose (FBG) is 160 mg/dL and 155 mg/dL on two occasions. HgA1c is 7.8%. You educate the patient on medical nutrition therapy. She returns for reevaluation in 8 weeks. She states she has followed diet and exercise recommendations but her FBG remains between 130 and 140 and HgA1C is 7.3%. She is asymptomatic, and physical examination shows no abnormalities. Which of the following is the treatment of choice?
. Thiazolidinediones
. Encourage compliance with medical nutrition therapy
. Insulin
. Metformin
. Observation with repeat HgA1C in 6 weeks.
44) A 49-year-old woman presents to her physician’s office with a long-standing history of polydipsia, polyuria, central obesity, and hyperlipidemia. She is currently taking metformin, a sulfonylurea, and an angiotensin-converting enzyme (ACE) inhibitor. ACE inhibitors are most beneficial in preventing or slowing the progression of which of the following diabetic complications?
Diabetic ketoacidosis
Diabetic nephropathy
Diabetic neuropathy
Diabetic retinopathy
Peripheral vascular disease
45) A 42-year-old woman presents to her physician with complaints of fever (38.2°C [100.8°F]) and mild-to-moderate anterior neck pain. On examination the physician finds her to be tachycardic and sweating, and to have an exquisitely tender thyroid gland. Her blood work shows a depressed thyroid-stimulating hormone level and increased free thyroxine. Which of the following is the most appropriate treatment at this time?
Acetaminophen
Ibuprofen
Levothyroxine
Prednisone
Radioactive iodine
46) A 53-year-old woman suffers from long-standing obesity complicated by DJD of the knees, making it difficult for her to exercise. Recently her fasting blood glucose values have been 148 mg/dL and 155 mg/dL; you tell her that she has developed type 2 diabetes. She wonders if diet will allow her to avoid medications. In addition, her daughter also suffers from obesity and has impaired fasting glucose, and the patient wonders about the management of her prediabetes. Which of the following is a correct statement based on the American Diabetes Association 2008 guidelines regarding nutrition recommendations and interventions for diabetes?
. Low-carbohydrate diets such as “South Beach” and “Atkins” should be avoided
. Outcomes studies show that medical nutrition therapy (MNT) can produce a 1 to 2-point decrease in hemoglobin A1c in type 2 diabetics
. Prediabetic patients should be instructed to lose weight and exercise but a referral to a medical nutritionist is not necessary until full-blown diabetes is diagnosed
. Very low-calorie diets (< 800 cal/day) produce weight loss that is usually maintained after the diabetic patient returns to a self-selected diet
. Bariatric surgery may be considered for patients with type 2 diabetes and a BMI of > 30 kg/m2
47) A 45-year-old G2P2 female presents for annual examination. She reports regular menstrual cycles lasting 3 to 5 days. She exercises 5 times per week and reports no difficulty sleeping. Her weight is stable 140 lbs and she is 5 ft 8 in tall. Physical examination is unremarkable. Laboratory studies are normal with the exception of a TSH value of 6.6 mU/L (normal 0.4-4.0 mU/L). Which of the following represents the best option for management of this patient’s elevated TSH?
. Repeat TSH in 3 months and reassess for signs of hypothyroidism
. Begin low dose levothyroxine (25-50 μg/d)
. Recommend dietary iodide supplementation
. Order thyroid uptake scan
. Measure thyroid peroxidase antibodies (TPOAb)
48) A 28-year-old patient with known Addison’s disease presents with abdominal pain and is hypotensive to a systolic pressure of 88 mmHg. He has a 2-week history of progressively worse nonproductive dry cough, sore throat, malaise, and headache. He has not checked his temperature at home but complains of constant chills. Which of the following is the best initial management?
Azithromycin
Check serum glucose
Hydrocortisone
Intravenous fluids
X-ray of the chest
49) A generally healthy 74-year-old woman who recently moved into the area visits the physician’s office for her first well-visit. She states that her previous doctor had been treating her with propylthiouracil (PTU) for subclinical hyperthyroidism, but that her prescription ran out several months ago. Laboratory studies reveal that her free thyroxine and triiodothyronine levels are normal, but her thyroid-stimulating hormone is depressed. PTU therapy is most important in this patient to prevent the development of which disorder?
Cardiac dysrhythmias
Hypothyroidism
Pretibial myxedema
Thyroid cancer
Thyroid storm
50) You recently evaluated a 28-year-old woman who presented with complaints of shakiness and heat intolerance. The patient plans to have children and is currently using no contraception. On examination you noted tachycardia with an HR of 102, a fine tremor, a diffuse goiter, and proptosis. You now have the laboratory results and note a TSH < 0.001, elevated total T4 of 17.8, and increased T3 uptake. Radionuclide uptake by the thyroid gland is elevated. You tell her that she has Graves’ disease. What is the best treatment plan for this patient?
. Propylthiouracil
. Radioactive iodine
. Propranolol
. Thyroid surgery
. Oral corticosteroids
{"name":"Med management 2 Q1 to 50", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"1) A 10-year-old girl with blue eyes and blonde hair is brought to the office by her mother for a routine check-up. All her immunizations are up to date. Her family history is significant for myocardial infarction in her father and schizophrenia in a maternal uncle. There is no family history of any skin malignancies. Her height is at the 60th percentile, and weight is at the 56th percentile. While you are examining her, the mother says with much concern that she saw a television program that claimed that the incidence of skin cancer is increasing dramatically. She wants to know the best way to prevent skin cancer in her daughter, especially since they live in California. What is the best advice to help prevent malignant melanoma in this child?, 2) A 50-year-old man comes to the emergency department due to acute onset respiratory difficulty. He also has periorbital, circumoral and facial edema. Two weeks ago, he experienced chest pain, profuse sweating and anxiety, and was subsequently admitted to the cardiac intensive care unit. At that time, his ECG showed ST segment elevation and Q waves in the inferior leads. He was taken to the catheterization lab and had an angioplasty with stent done for 100% occlusion of the right coronary artery. He was discharged with the following medications: aspirin, clopidogrel, metoprolol, enalapril, simvastatin and isosorbide mononitrate. In the ED, his pulse is 102\/min, blood pressure is 110\/70 mmHg, respirations are 24\/min and temperature is 36.8°C (98.4°F). Which of the following is most likely responsible for his present symptoms?, 3) A 25-year-old male presents with skin lesions over his elbows, knees and neck. He complains of intense itching and burning sensation over these lesions for the past 10 days. He was advised to follow a gluten-free diet on his previous visit, but was not compliant. His vital signs are stable. On examination, there are flesh-colored to erythematous vesicles distributed over the extensor aspects of elbows, knees, posterior neck and shoulders. Some of these lesions are shown in the picture below. Which of the following is the drug of choice for his skin condition? Image","img":"https://www.quiz-maker.com/3012/images/ogquiz.png"}
More Quizzes
Study
210
Test
100
Questionnaire sur les notions du cours #1
7416
Past Tense
8450
Free Classifying Quadrilaterals
201022317
Which Wednesday Character Are You? Free Personality
201029232
Free Consumer Behavior Knowledge
201021683
Free Loyalty Program Dining Knowledge
201022154
Health Behaviors and Cognition
15823182
Ecosystem Biogeochemistry
15824138
Got Every Tech Question Right? Take Our Free IT!
201055383
Eukaryotic Cell Biology Laboratory
15824138