Surgery USMLE (827-926)
A 30-year-old man comes to the physician because of a 2-week history of swelling and pain in the right knee. He first experienced pain when he twisted his leg while playing football 15 days ago. He felt something 'popping' in the knee at that time but ignored it. The pain and swelling has been increasing since, and he feels sudden pain with extension of his leg. Examination shov1s the right knee is swollen and tender along the medial side. Full extension of the right knee is not possible due to sudden pain during terminal extension. Snapping can be felt in the right knee on tibial torsion with the knee flexed at 90 degrees. An x-ray film of the knee joint shows no abnormalities. Which of the following is the most likely diagnosis?
Anterior cruciate ligament injury
Posterior cruciate ligament injury
Medial meniscus tear
Medial collateral ligament tear
Lateral collateral ligament tear
A 25-year-old male is brought to the emergency department following a motor vehicle accident in which he was the unrestrained driver. The emergency response team's reports indicate that his breath smelled of alcohol at the scene. En route to the hospital, the patient receives 2 liters of intravenous normal saline, and in the ED his blood pressure is 100/60 mmHg, heart rate is 120/min, and respiratory rate is 34/min. His neck veins are flat. You note multiple bruises overlying his anterior chest wall and upper abdomen. On inspiration, there is inward motion of the right side of his chest wall. His abdomen is soft and non-distended. He is put on positive pressure mechanical ventilation and his chest movements become symmetric. Which of the following is the most likely diagnosis?
Tracheobronchial disruption
Esophageal rupture
Flail chest
Pneumothorax
Air embolism
A 55-year-old man comes to the emergency department because of severe right-sided chest pain. His temperature is 37.8° C (1000 F), blood pressure is 138/88 mm Hg, pulse is 88/min and respirations are 19/min and shallow. Examination shows decreased respiratory movements on the right side of the chest and tenderness on palpation over the right mid-chest. An x-ray film of the chest shows a fracture of the right 6th rib. Which of the following is the most important goal in management of the rib fracture in this patient?
To achieve a tidal volume of 500 ml with intubation
To use only intravenous colloids
To ensure appropriate analgesia
To provide mechanical stabilization to the chest wall
To give prophylactic antibiotics
A 5-year-old child presents with a small mass near the anterior border of the sternocleidomastoid muscle. The mass is associated with localized erythema and induration, and the child is febrile. Which of the following is the definitive treatment of this problem?
Antibiotic therapy
Incision and drainage
Incision and drainage followed by complete excision after resolution of the inflammation and infection
Partial excision followed by clinical observation
Immediate excision followed by postoperative antibiotic therapy for 1 week
A 21-year-old woman asks you to evaluate a small painless lump in the midline of her neck that moves with swallowing. You make the clinical diagnosis of thyroglossal duct cyst. Which of the following is the most appropriate management of this patient?
Excision of the cyst
Excision of the cyst and the central portion of the hyoid bone
Excision of the cyst, the central portion of the hyoid bone, and the tract to the base of the tongue
Excision of the cyst, the central portion of the hyoid bone, and the tract to the base of the tongue, with sampling of central cervical lymph nodes
Excision of the cyst, the central portion of the hyoid bone, and the tract to the base of the tongue, with biopsy of the thyroid gland
A 60-year-old smoker is seen because of a 3-cm midline ulcerating mass that is visualized when he sticks out his tongue. Biopsy establishes that this is squamous cell carcinoma. Which of the following is the most appropriate treatment of his cancer?
Radiation therapy alone
Partial glossectomy
Partial glossectomy and cervical lymph node sampling
Partial glossectomy and bilateral neck dissections
Partial glossectomy followed by chemoradiation
A 56-year-old woman is referred to you about 3 months after a colostomy subsequent to a sigmoid resection for cancer. She complains that her stoma is not functioning properly. Which of the following is the most common serious complication of an end colostomy?
Bleeding
Skin breakdown
Parastomal hernia
Colonic perforation during irrigation
Stomal prolapse
A 56-year-old previously healthy physician notices that his eyes are yellow and he has been losing weight. On physical examination the patient has jaundice and scleral icterus with a benign abdomen. Transcutaneous ultrasound of the abdomen demonstrates biliary ductal dilation without gallstones. Which of the following is the most appropriate next step in the workup of this patient?
Esophagogastroduodenoscopy (EGD)
Endoscopic retrograde cholangiopancreatography (ERCP)
Acute abdominal series
Computed tomography (CT) scan
Positron emission tomography (PET) scan
A 45-year-old woman with history of heavy nonsteroidal anti-inflammatory drug ingestion presents with acute abdominal pain. She undergoes exploratory laparotomy 30 hours after onset of symptoms and is found to have a perforated duodenal ulcer. Which of the following is the procedure of choice to treat her perforation?
Simple closure with omental patch
Truncal vagotomy and pyloroplasty
Truncal vagotomy and antrectomy
Highly selective vagotomy with omental patch
Hemigastrectomy
A 45-year-old man with a history of chronic peptic ulcer disease undergoes a truncal vagotomy and antrectomy with a Billroth II reconstruction for gastric outlet obstruction. Six weeks after surgery, he returns, complaining of postprandial weakness, sweating, light- headedness, crampy abdominal pain, and diarrhea. Which of the following would be the best initial management strategy?
Treatment with a long-acting somatostatin analog
Dietary advice and counseling that symptoms will probably abate within 3 months of surgery
Dietary advice and counseling that symptoms will probably not abate but are not dangerous
Workup for neuroendocrine tumor (eg, carcinoid)
Preparation for revision to Roux-en-Y gastrojejunostomy
A 60-year-old male patient with hepatitis C with a previous history of variceal bleeding is admitted to the hospital with hematemesis. His blood pressure is 80/60 mmHg, physical examination reveals splenomegaly and ascites, and initial hematocrit is 25%. Prior to endoscopy, which of the following is the best initial management of the patient?
Administration of intravenous octreotide
Administration of a β-blocker (eg, propranolol)
Measurement of prothrombin time and transfusion with cryoglobulin if elevated
Empiric transfusion of platelets given splenomegaly
Gastric and esophageal balloon tamponade (Sengstaken-Blakemore tube)
A 32-year-old alcoholic with end-stage liver disease has been admitted to the hospital 3 times for bleeding esophageal varices. He has undergone banding and sclerotherapy previously. He admits to currently drinking a 6 packs of beer per day. On his abdominal examination, he has a fluid wave. Which of the following is the best option for long-term management of this patient’s esophageal varices?
Orthotopic liver transplantation
Transection and reanastomosis of the distal esophagus
Distal splenorenal shunt
End-to-side portocaval shunt
Transjugular intrahepatic portosystemic shunt (TIPS)
A 55-year-old man complains of chronic intermittent epigastric pain. A gastroscopy demonstrates a 2-cm prepyloric ulcer. Biopsy of the ulcer yields no malignant tissue. After a 6weeks trial of medical therapy, the ulcer is unchanged. Which of the following is the best next step in his management?
Repeat trial of medical therapy
Local excision of the ulcer
Highly selective vagotomy
Partial gastrectomy with vagotomy and Billroth I reconstruction
Vagotomy and pyloroplasty
A 45-year-old man was discovered to have a hepatic flexure colon cancer during a colonoscopy for anemia requiring transfusions. Upon exploration of his abdomen in the operating room, an unexpected discontinuous 3-cm metastasis is discovered in the edge of the right lobe of the liver. Preoperatively, the patient was counseled of this possibility and the surgical options. Which of the following is the most appropriate management of this patient?
A diverting ileostomy should be performed and further imaging obtained
Right hemicolectomy
Right hemicolectomy with local resection of the liver metastasis
Closure of the abdomen followed by chemotherapy
Right hemicolectomy with postoperative radiation therapy to the liver
A 42-year-old man with no history of use of NSAIDs presents with recurrent gastritis. The patient was diagnosed and treated for Helicobacter pylori 6 months ago. Which of the following tests provides the least invasive method to document eradication of the infection?
Serology testing for H pylori
Carbon-labeled urea breath test
Rapid urease assay
Histologic evaluation of gastric mucosa
Culturing of gastric mucosa
A 22-year-old college student notices a bulge in his right groin. It is accentuated with coughing, but is easily reducible. Which of the following hernias follows the path of the spermatic cord within the cremaster muscle?
Femoral
Direct inguinal
Indirect inguinal
Spigelian
Interparietal
An 80-year-old man with history of symptomatic cholelithiasis presents with signs and symptoms of a small-bowel obstruction. Which of the following findings would provide the most help in ascertaining the diagnosis?
Coffee-grounds aspirate from the stomach
Pneumobilia
A leukocyte count of 40,000/mL
A pH of 7.5, PCO2 of 50 kPa, and paradoxically acid urine
A palpable mass in the pelvis
A 42-year-old man has bouts of intermittent crampy abdominal pain and rectal bleeding. Colonoscopy is performed and demonstrates multiple hamartomatous polyps. The patient is successfully treated by removing as many polyps as possible with the aid of intraoperative endoscopy and polypectomy. Which of the following is the most likely diagnosis?
Ulcerative colitis
Villous adenomas
Familial polyposis
Peutz-Jeghers syndrome
Crohn colitis
A 70-year-old woman has nausea, vomiting, abdominal distention, and episodic crampy midabdominal pain. She has no history of previous surgery but has a long history of cholelithiasis for which she has refused surgery. Her abdominal radiograph reveals a spherical density in the right lower quadrant. Which of the following is the definitive treatment for this patient’s bowel obstruction?
Ileocolectomy
Cholecystectomy
Ileotomy and extraction
Nasogastric (NG) tube decompression
Intravenous antibiotics

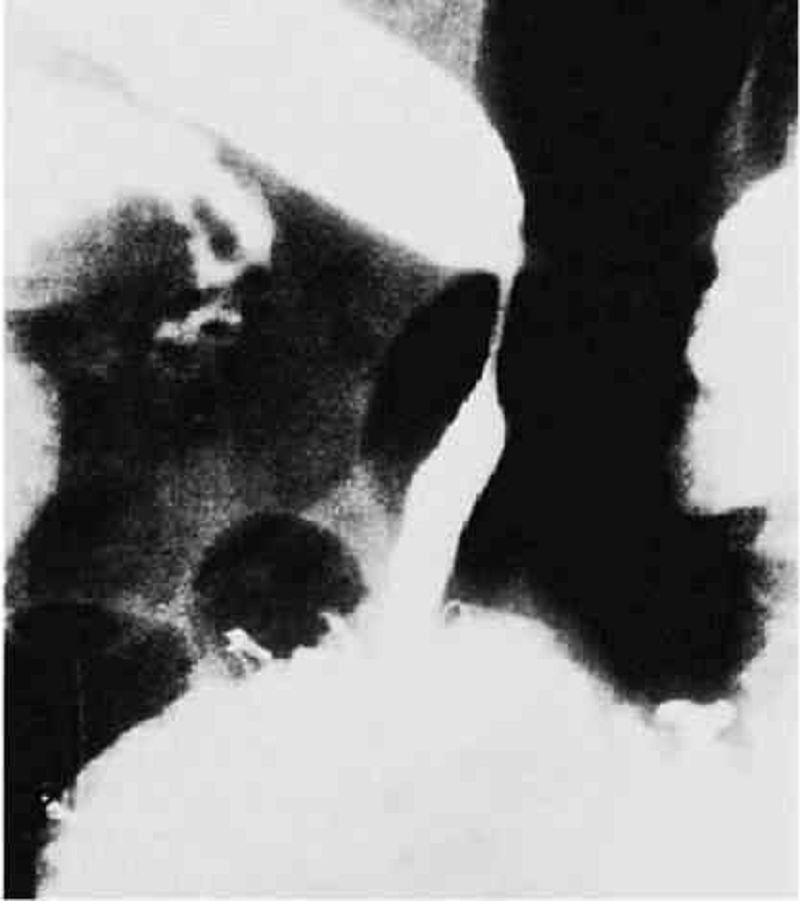
A 35-year-old man is brought to the emergency department after a motorcycle accident. He is unconscious when the emergency medical team arrived. He regains consciousness on the way to the emergency department. Upon arrival, he is mildly confused and complains of headache and nausea. His temperature is 36.9° C (98.5° F), blood pressure is 102/60 mm Hg, pulse is 116/min, and respirations are 22/min. Pupils are equal and reactive to light. He moves all extremities on command, and deep tendon reflexes are symmetric. Head CT scan shows: Which of the following is the most likely diagnosis?
Acute epidural hematoma
Acute subdural hematoma
Concussion
Diffuse axonal injury
Lntracerebral bleeding
A 65-year-old male presented to the ER with increasing shortness of breath, fever and productive cough of 2 days duration. He has smoked for several years and has been on home oxygen. Chest x-ray showed right lower lobe consolidation. His vital signs on admission were temperature 38.7°C (101.7°F), blood pressure 120/76 mm Hg, and pulse 110/min and respirations 26/min. His condition worsened over the next several hours and required orotracheal intubation and mechanical ventilation. He was transferred to the intensive care unit. Placement of a central venous catheter in the right subclavian vein for IV access was attempted. After the line is successfully placed, the patient begins to deteriorate. Repeat vital signs are blood pressure 80/50 mm Hg and pulse 130/min. Examination shows absent breath sounds on the right side and distended neck veins. Which of the following is the most appropriate next step in management?
Stat chest x-ray
Arterial blood gas analysis
Pericardiocentesis
Needle thoracostomy
Intravenous fluids and dopamine
A 54-year-old woman comes to the clinic because of a forceful hyperextension injury to her hand after falling down. She complains of pain and swelling of the right wrist and pain associated with movement. She has no other complaints. She has no other medical conditions and takes no medication. Her blood pressure is 110/60 mm Hg, pulse is 84/min, and respirations are 12/min. Examination shows maximal tenderness in the anatomic snuffbox and pain with radial deviation of the wrist. The rest of the examination shows no other injuries. X-ray imaging of the wrist in multiple views does not reveal a fracture. Which of the following is the most appropriate next step in management?
Administer analgesics and recommend rest
Obtain an ultrasonogram of the wrist
Place a thumb spica cast and repeat the radiography in 7- 10 days
Obtain a DEXA scan to screen for osteoporosis
Administer a steroid injection
An 18-year-old woman at 9 weeks' gestation is brought to the emergency department because of an open fracture of the tibia and fibula. She is hemodynamically stabilized and referred to the orthopedic department. She is scheduled for internal fixation of the tibia for the following day. However, before the surgery she develops severe dyspnea and confusion. Her temperature is 37.7° C (99.9° F), blood pressure is 110/70 mmHg, pulse is 110/min, and respirations are 22/min. Examination shows numerous non-palpable petechiae in the upper part of the body. Which of the following is the most likely diagnosis?
Air embolism
Amniotic fluid embolism
Thromboembolism
Fat embolism
Acute respiratory distress syndrome

A 46-year-old man is brought to the emergency department after a fall during a downhill bike race. He lost consciousness for approximately 1 minute after the fall. He complains of severe back and abdominal pain. He has no other medical problems. Head computed tomography (CT) scan shows no intracranial bleeding. Lumbar films suggest a compression wedge fracture of the body of L2 vertebra, and a brace is placed. Abdominal CT scan shows a small retroperitoneal bleed and splenic laceration. He is conservatively treated with analgesics and supportive measures. On hospital day three, he complains of abdominal pain and nausea. His abdomen is distended, tympanic, and mildly tender, without rebound or guarding. Bowel sounds are absent. X-ray of the abdomen reveals:
Erosive gastritis
Expanding retroperitoneal hematoma
Colonic pseudoobstruction
Mesenteric ischemia
Paralytic ileus

A 22-year-old man who was involved in a motor vehicle accident undergoes intravenous fluid resuscitation with 2 L normal saline over 20 minutes. He is in respiratory distress, with a respiratory rate of 40/min. He receives bilateral chest tubes. Endotracheal intubation is performed and mechanical ventilation is initiated due to progressive respiratory failure. His blood pressure is 92/50 mm Hg and pulse is 121/min. The patient is responsive to painful stimuli only. Pulmonary examination shows coarse breath sounds bilaterally. The chest x-ray is shown below. Which of the following most likely contributed to this patient's progressive respiratory failure?
Diaphragmatic tear
Esophageal rupture
Flail chest
Pulmonary edema
Tension pneumothorax
A 38-year-old woman who underwent total thyroidectomy for multinodular goiter 6 months ago presents with persistent hoarseness. Which of the following nerves was most likely injured during her operation?
Superior laryngeal nerve
Bilateral recurrent laryngeal nerves
Unilateral recurrent laryngeal nerve
Hypoglossal nerve
Marginal mandibular branch of the facial nerve

A 4-year-old boy is brought into the emergency room by his parents for difficulty in breathing and swallowing. On physical examination the child is febrile, tachycardic, and tachypneic. He is anxious, drooling, and becomes increasingly exhausted while struggling to breathe. A lateral cervical spine radiograph is shown here. Which of the following is the most appropriate management of this patient?
Examine the larynx at bedside
IV antibiotics and admission to the floor
Immediate endotracheal intubation in the emergency room
Immediate endotracheal intubation in the operating room
Immediate tracheostomy in the operating room
A 58-year-old man is found to have a small mass in the right neck on a yearly physical examination. The patient reports that the mass has been slowly growing for the last few months and is not associated with pain or drainage. He has an otherwise negative review of systems. On examination there is a hard, mobile 2 cm mass along the mid-portion of the right sternocleidomastoid muscle. Which of the following is the most appropriate initial step in the workup of the neck mass?
No further workup is needed. Reevaluate the mass after a course of antibiotics for 2 weeks.
Fine-needle aspiration (FNA)
Core needle biopsy
Incisional biopsy
Excisional biopsy
A 53-year-old man presents to the emergency room with left lower quadrant pain, fever, and vomiting. CT scan of the abdomen and pelvis reveals a thickened sigmoid colon with inflamed diverticula and a 7-cm by 8-cm rim-enhancing fluid collection in the pelvis. After percutaneous drainage and treatment with antibiotics, the pain and fluid collection resolve. He returns as an outpatient to clinic 1 month later. He undergoes a colonoscopy, which demonstrates only diverticula in the sigmoid colon. Which of the following is the most appropriate next step in this patient’s management?
Expectant management with sigmoid resection if symptoms recur
Cystoscopy to evaluate for a fistula
Sigmoid resection with end colostomy and rectal pouch (Hartmann procedure)
Sigmoid resection with primary anastomosis
Long-term suppressive antibiotic therapy
A 29-year-old woman complains of postprandial right upper quadrant pain and fatty food intolerance. Ultrasound examination reveals no evidence of gallstones or sludge. Upper endoscopy is normal, and all of her liver function tests are within normal limits. Which of the following represents the best management option?
Avoidance of fatty foods and reexamination in 6 months
Ultrasound examination should be repeated immediately, since the falsenegative rate for ultrasound in detecting gallstones is 10% to 15%
Treatment with ursodeoxycholic acid
CCK-HIDA scan should be performed to evaluate for biliary dyskinesia
Laparoscopic cholecystectomy for acalculous cholecystitis
A 47-year-old asymptomatic woman is incidentally found to have a 5-mm polyp and no stones in her gallbladder on ultrasound examination. Which of the following is the best management option?
Aspiration of the gallbladder with cytologic examination of the bile
Observation with repeat ultrasound examinations to evaluate for increase in polyp size
Laparoscopic cholecystectomy
Open cholecystectomy with frozen section
In bloc resection of the gallbladder, wedge resection of the liver, and portal lymphadenectomy
A 48-year-old woman develops pain in the right lower quadrant while playing tennis. The pain progresses and the patient presents to the emergency room later that day with a low-grade fever, a WBC count of 13,000/mm3 and complaints of anorexia and nausea as well as persistent, sharp pain of the right lower quadrant. On examination, she is tender in the right lower quadrant with muscular spasm, and there is a suggestion of a mass effect. An ultrasound is ordered and shows an apparent mass in the abdominal wall. Which of the following is the most likely diagnosis?
Acute appendicitis
Cecal carcinoma
Hematoma of the rectus sheath
Torsion of an ovarian cyst
Cholecystitis
A 32-year-old alcoholic man, recently emigrated from Mexico, presents with right upper quadrant pain and fevers for 2 weeks. CT scan of the abdomen demonstrates a non–rim- enhancing fluid collection in the periphery of the right lobe of the liver. The patient’s serology is positive for antibodies to Entamoeba histolytica. Which of the following is the best initial management option for this patient?
Treatment with antiamebic drugs
Percutaneous drainage of the fluid collection
Marsupialization of the fluid collection
Surgical drainage of the fluid collection
Liver resection
A 45-year-old executive experiences increasingly painful retrosternal heartburn, especially at night. He has been chewing antacid tablets. An esophagogram shows a hiatal hernia. In determining the proper treatment for a sliding hiatal hernia, which of the following is the most useful modality?
Barium swallow with cinefluoroscopy during Valsalva maneuver
Flexible endoscopy
Twenty-four-hour monitoring of esophageal pH
Measurement of the size of the hernia on upper GI
Assessment of the patient’s smoking and drinking history
A 22-year-old woman is seen in a surgery clinic for a bulge in the right groin. She denies pain and is able to make the bulge disappear by lying down and putting steady pressure on the bulge. She has never experienced nausea or vomiting. On examination she has a reducible hernia below the inguinal ligament. Which of the following is the most appropriate management of this patient?
Observation for now and follow-up in surgery clinic in 6 months
Observation for now and follow-up in surgery clinic if she develops further symptoms
Elective surgical repair of hernia
Emergent surgical repair of hernia
Emergent surgical repair of hernia with exploratory laparotomy to evaluate the small bowel
A 22-year-old woman presents with a painful fluctuant mass in the midline between the gluteal folds. She denies pain on rectal examination. Which of the following is the most likely diagnosis?
Pilonidal abscess
Perianal abscess
Perirectal abscess
Fistula-in-ano
Anal fissure
A 72-year-old man status post–coronary artery bypass graft (CABG) 5 years ago presents with hematochezia, abdominal pain, and fevers. Colonoscopy reveals patches of dusky-appearing mucosa at the splenic flexure without active bleeding. Which of the following is the most appropriate management of this patient?
Angiography with administration of intra-arterial papaverine
Emergent laparotomy with left hemicolectomy and transverse colostomy
Aortomesenteric by pass
Exploratory laparotomy with thrombectomy of the inferior mesenteric artery
Expectant management
A 62-year-old man has been diagnosed by endoscopic biopsy as having a sigmoid colon cancer. He is otherwise healthy and presents to your office for preoperative consultation. He asks a number of questions regarding removal of a portion of his colon. Which of the following is most likely to occur after a colon resection?
The majority (> 50%) of normally formed feces will comprise solid material
Patients who undergo major colon resections suffer little long-term change in their bowel habits following operation
Sodium, potassium, chloride, and bicarbonate will be absorbed by the colonic epithelium by an active transport process.
The remaining colon will absorb less water
The remaining colon will absorb long-chain fatty acids that result from bacterial breakdown of lipids.
A 39-year-old woman with no significant past medical history and whose only medication is oral contraceptive pills (OCP) presents to the emergency room with right upper quadrant pain. CT scan demonstrates a 6-cm hepatic adenoma in the right lobe of the liver. Which of the following describes the definitive treatment of this lesion?
Cessation of oral contraceptives and serial CT scans
Intra-arterial embolization of the hepatic adenoma
Embolization of the right portal vein
Resection of the hepatic adenoma
Systemic chemotherapy
A 43-year-old man without symptoms is incidentally noted on CT scan to have a 4 cm lesion in the periphery of the left lobe of the liver. The lesion enhances on the arterial phase of the CT scan and has a central scar suggestive of focal nodular hyperplasia (FNH). Which of the following is the recommended treatment of this lesion?
No further treatment is necessary
Wedge resection of the lesion
Formal left hepatectomy
Intra-arterial embolization of the lesion
Radiofrequency ablation of the liver lesi
A 57-year-old previously alcoholic man with a history of chronic pancreatitis presents with hematemesis. Endoscopy reveals isolated gastric varices in the absence of esophageal varices. His liver function tests are normal and he has no stigmata of end-stage liver disease. Ultrasound examination demonstrates normal portal flow but a thrombosed splenic vein. He undergoes banding, which is initially successful, but he subsequently rebleeds during the same hospitalization. Attempts tocontrol the bleeding endoscopically are unsuccessful. Which of the following is the most appropriate next step in management?
Transjugular intrahepatic portosystemic shunt
Surgical portocaval shunt
Surgical mesocaval shunt
Splenectomy
Placement of a Sengstaken-Blakemore tube
A previously healthy 15-year-old boy is brought to the emergency room with complaints of about 12 hours of progressive anorexia, nausea, and pain of the right lower quadrant. On physical examination, he is found to have a rectal temperature of 38.18°C (100.72°F) and direct and rebound abdominal tenderness localizing to McBurney point as well as involuntary guarding in the right lower quadrant. At operation through a McBurney-type incision, the appendix and cecum are found to be normal, but the surgeon is impressed by the marked edema of the terminal ileum, which also has an overlying fibrinopurulent exudate. Which of the following is the most appropriate next step?
Transjugular intrahepatic portosystemic shunt
Surgical portocaval shunt
Surgical mesocaval shunt
Splenectomy
Placement of a Sengstaken-Blakemore tube
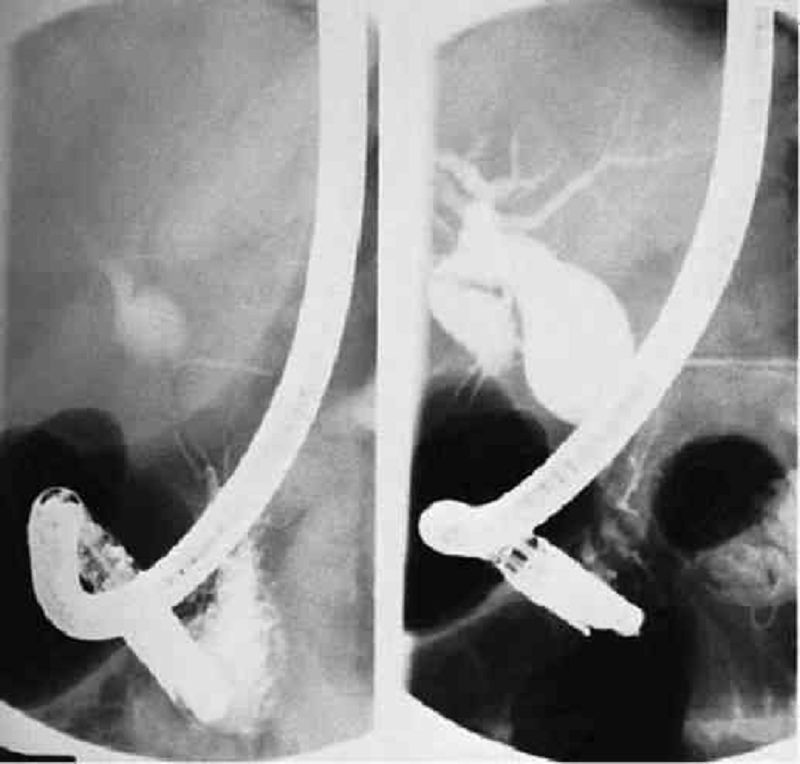
A 32-year-old woman undergoes a cholecystectomy for acute cholecystitis and is discharged home on the sixth postoperative day. She returns to the clinic 8 months after the operation for a routine visit and is noted by the surgeon to be jaundiced. Laboratory values on readmission show total bilirubin 5.6 mg/dL, direct bilirubin 4.8 mg/dL, alkaline phosphatase 250 IU (normal 21-91 IU), serum glutamic oxaloacetic transaminase (SGOT) 52 kU (normal 10-40 kU), and serum glutamic pyruvic transaminase (SGPT) 51 kU (normal 10-40 kU). An ultrasonogram shows dilated intrahepatic ducts. The patient undergoes the transhepatic cholangiogram seen here. Which of the following is the most appropriate next management step?
Choledochoplasty with insertion of a T tube
End-to-end choledochocholedochal anastomosis
Roux-en-Y hepaticojejunostomy
Percutaneous transhepatic dilatation
Choledochoduodenostomy
After complete removal of a sessile polyp of 2.0 cm by 1.5 cm found 1 finger length above the anal mucocutaneous margin, the pathologist reports it to have been a villous adenoma that contained carcinoma in situ. Which of the following is the most appropriate next step in management?
Reexcision of the biopsy site with wider margins
Abdominoperineal rectosigmoid resection
Anterior resection of the rectum
External radiation therapy to the rectum
No further therapy
A 62-year-old man has been noticing progressive difficulty swallowing, first solid food and now liquids as well. A barium study shows a ragged narrowing just below the carinal level. Endoscopic biopsy confirms squamous cell carcinoma. Which of the following provides the most accurate information regarding the T stage of an esophageal carcinoma?
Computed tomography
Positron emission tomography
Magnetic resonance imaging
Endoscopic ultrasound
Bronchoscopy
A 53-year-old woman with a history of a vagotomy and antrectomy with Billroth II reconstruction for peptic ulcer disease presents with recurrent abdominal pain. An esophagogastroduodenoscopy (EGD) demonstrates that ulcer and serum gastrin levels are greater than 1000 pg/mL on three separate determinations (normal is 40-150). Which of the following is the best test for confirming a diagnosis of gastrinoma?
A 24-hour urine gastrin level
A secretin stimulation test
A serum glucagon level
A 24-hour urine secretin level
A serum glucose to insulin ratio
A 52-year-old man with a family history of multiple endocrine neoplasia type 1 (MEN1) has an elevated gastrin level and is suspected to have a gastrinoma. Which of the following is the most likely location for his tumor?
Fundus of the stomach
Antrum of the stomach
Within the triangle formed by the junction of the second and third portions of the duodenum, the junction of the neck and body of the pancreas, and the junction of the cystic and common bile duct
Tail of the pancreas
Within the triangle formed by the inferior edge of the liver, the cystic duct, and the common hepatic duct
A 73-year-old woman presents to the emergency room complaining of severe epigastric pain radiating to her back, nausea, and vomiting. CT scan of the abdomen demonstrates inflammation and edema of the pancreas. A right upper quadrant ultrasound demonstrates the presence of gallstones in the gallbladder. Which of the following is an important prognostic sign in acute pancreatitis according to Ranson’s criteria?
Amylase level
Age
Total bilirubin level
Albumin level
Lipase level
A 55-year-old man who is extremely obese reports weakness, sweating, tachycardia, confusion, and headache whenever he fasts for more than a few hours. He has prompt relief of symptoms when he eats. Labarotory examination reveals an inappropriately high level of serum insulin during the episodes of fasting. Which of the following is the most appropriate treatment for this condition?
Diet modification to include frequent meals
Long-acting somatostatin analogue octreotide
Simple excision of the tumor
Total pancreatectomy
Chemotherapy and radiation
A 57-year-old woman sees blood on the toilet paper. Her doctor notes the presence of an excoriated bleeding 2.8-cm mass at the anus. Biopsy confirms the clinical suspicion of anal cancer. In planning the management of a 2.8-cm epidermoid carcinoma of the anus, which of the following is the best initial management strategy?
Abdominoperineal resection
Wide local resection with bilateral inguinal node dissection
Local radiation therapy
Systemic chemotherapy
Combined radiation therapy and chemotherapy
An 80-year-old man is admitted to the hospital complaining of nausea, abdominal pain, distention, and diarrhea. A cautiously performed transanal contrast study reveals an apple-core configuration in the rectosigmoid area. Which of the following is the most appropriate next step in his management?
Colonoscopic decompression and rectal tube placement
Saline enemas and digital disimpaction of fecal matter from the rectum
Colon resection and proximal colostomy
Oral administration of metronidazole and checking a Clostridium difficile titer
Evaluation of an electrocardiogram and obtaining an angiogram to evaluate for colonic mesenteric ischemia
A 40-year-old female is brought to the emergency department following a motor vehicle accident in which she was the front seat passenger. She reports hitting her head against the windshield and hurting her right leg. She appears completely alert and oriented. Glasgow Coma Scale =15/15. Her pupils are equal and reactive to light. There is a bruise over the right forehead, but no tenderness is present on palpation of the cranial bones. Examination of the right leg reveals a hematoma over the thigh. Knee extension on the right is markedly reduced when compared to the left. Sensory examination reveals decreased sensory perception to both sharp and dull stimuli over the medial side of the right lower thigh and leg. All other dermatomes are intact. What nerve injury is most likely present in this patient?
Femoral nerve
Tibial nerve
Obturator nerve
Common peroneal nerve
Fibular nerve
A 28-year-old man is brought to the emergency department after being an unrestrained passenger in a motor vehicle collision. In the ambulance on the way to the hospital, he receives 2 L normal saline intravenously and 5 Umin of oxygen by nasal cannula. His blood pressure is 80/42 mm Hg, pulse is 135/min, and respirations are 40/min. He is agitated and moves all 4 extremities spontaneously. His pupils are symmetric and reactive to light. Neck veins are distended, and his trachea is deviated to the right. Which of the following is the best initial management for this patient?
Chest tube placement in the fifth intercostal space in the left midaxillary line
Chest x-ray to confirm pneumothorax
Endotracheal intubation to establish an adequate airway
Imaging to exclude cervical spine injury
Needle insertion into the second intercostal space in the left midclavicular line
A 46-year-old woman who was recently diagnosed with Crohn disease asks about the need for surgery. Which of the following findings would be an indication for an immediate exploratory laparotomy?
Intestinal obstruction
Enterovesical fistula
Ileum-ascending colon fistula
Enterovaginal fistula
Free perforation

A 50-year-old man presents to the emergency room with a 6-hour history of excruciating abdominal pain and distention. The abdominal film shown here is obtained. Which of the following is the most appropriate next diagnostic maneuver?
Emergency celiotomy
Upper GI series with small-bowel follow-through
CT scan of the abdomen
Barium enema
Sigmoidoscopy
A septuagenarian woman undergoes an uncomplicated resection of an abdominal aneurysm. Four days after surgery the patient presents with sudden onset of abdominal pain and distention. An abdominal radiograph demonstrates an air-filled, kidney-bean–shaped structure in the left upper quadrant. Which of the following is the most appropriate management at this time?
Decompression of the large bowel via colonoscopy
Placement of the NG tube and administration of low-dose cholinergic drugs
Administration of a gentle saline enema and encouragement of ambulation
Operative decompression with transverse colostomy
Right hemicolectomy
A 45-year-old man presents with right upper quadrant abdominal pain and fever. CT scan shows a large, calcified cystic mass in the right lobe of the liver. Echinococcus is suggested by the CT findings. Which of the following is the most appropriate management of echinococcal liver cysts?
Percutaneous catheter drainage.
Medical treatment with albendazole.
Medical treatment with steroids.
Medical treatment with metronidazole.
Total pericystectomy.
A 28-year-old woman who is 15 weeks pregnant has new onset of nausea, vomiting, and right sided abdominal pain. She has been free of nausea since early in her first trimester. The pain has become worse over the past 6 hours. Which of the following is the most common non- obstetric surgical disease of the abdomen during pregnancy?
Appendicitis
Cholecystitis
Pancreatitis
Intestinal obstruction
Acute fatty liver of pregnancy
A 56-year-old woman has nonspecific complaints that include an abnormal sensation when swallowing. An esophagram is obtained. Which of the following is most likely to require surgical correction?
Large sliding esophageal hiatal hernia
Paraesophageal hiatal hernia
Traction diverticulum of esophagus
Schatzki ring of distal esophagus
Esophageal web

A 65-year-old man who is hospitalized with pancreatic carcinoma develops abdominal distention and obstipation. The following abdominal radiograph is obtained. Which of the following is the most appropriate initial management of this patient?
Urgent colostomy or cecostomy
Discontinuation of anticholinergic medications and narcotics and correction of metabolic disorder
Digital disimpaction of fecal mass in the rectum
Diagnostic and therapeutic colonoscopy
Detorsion of volvulus and colopexy or resection
A 48-year-old man presents with jaundice, melena, and right upper quadrant abdominal pain after undergoing a percutaneous liver biopsy. Endoscopy shows blood coming from the ampulla of Vater. Which of the following is the most appropriate first line of therapy for major hemobilia?
Correction of coagulopathy, adequate biliary drainage, and close monitoring
Transarterial embolization (TAE)
Percutaneous transhepatic biliary drainage (PTBD)
Ligation of bleeding vessels
Hepatic resection
A 30-year-old female patient who presents with diarrhea and abdominal discomfort is found at colonoscopy to have colitis confined to the transverse and descending colon. A biopsy is performed. Which of the following is a finding consistent with this patient’s diagnosis?
The inflammatory process is confined to the mucosa and submucosa.
The inflammatory reaction is likely to be continuous.
Superficial as opposed to linear ulcerations can be expected.
Noncaseating granulomas can be expected in up to 50% of patients.
Microabscesses within crypts are common.
A 24-year-old man presents to the emergency room with abdominal pain and fever. CT scan of the abdomen reveals inflammation of the colon. He is referred to a gastroenterologist to be evaluated for inflammatory bowel disease (Crohn disease versus ulcerative colitis). Which of the following indications for surgery is more prevalent in patients with Crohn disease?
Toxic megacolon
Massive bleeding
Fistulas between the colon and segments of intestine, bladder, vagina, urethra, and skin
Intractable disease
Dysplasia or carcinoma
A 62-year-old man presents with a 3-month history of an enlarged lymph node in the left neck. He is a long-time smoker of cigarettes and denies fevers, night sweats, fatigue, or cough. On physical examination there is a 1.5 cm hard, fixed mass below the angle of the mandible in the left neck. Which of the following is the most likely cause of an enlarged lymph node in the neck?
Thyroglossal duct cyst
Dermoid tumor
Carotid body tumor
Branchial cleft cyst
Metastatic squamous cell carcinoma
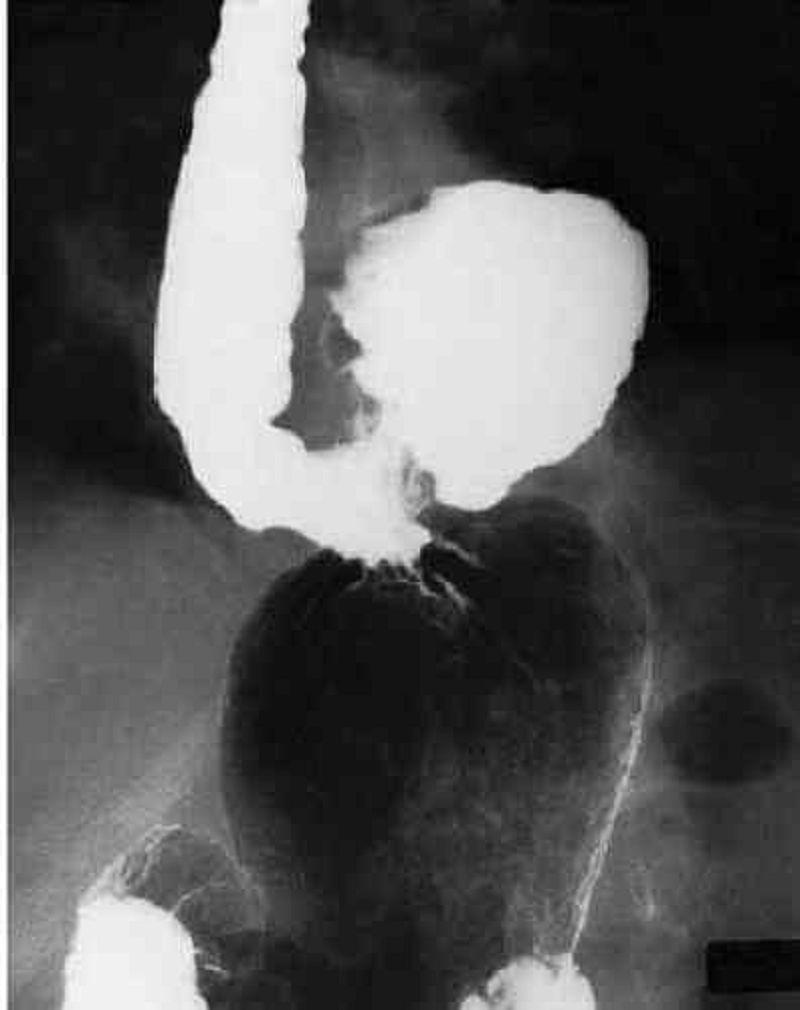
An upper GI series is performed on a 71-year-old woman who presented with several months of chest pain that occurs when she is eating. The film shown here is obtained. Investigation reveals a microcytic anemia and erosive gastritis on upper endoscopy. Which of the following is the most appropriate initial management of this patient?
Cessation of smoking, decreased caffeine intake, and avoidance of large meals before lying down
Antacids
Histamine-2 blocker
Proton-pump inhibitor
Surgical treatment
A 54-year-old man complains that his eyes are yellow. His bilirubin is elevated. His physical examination is unremarkable. A CT of the abdomen shows a small mass in the head of the pancreas encasing the superior mesenteric artery. Cytology from the ERCP is positive for cancer. Which of the following is the most appropriate treatment for this patient?
Pancreaticoduodenectomy
Pancreaticoduodenectomy with reconstruction of the superior mesenteric artery
Total pancreatectomy
Total pancreatectomy with reconstruction of the superior mesenteric artery
Chemoradiation therapy
A 28-year-old woman presents with hematochezia. She is admitted to the hospital and undergoes upper endoscopy that is negative for any lesions. Colonoscopy is performed and no bleeding sources are identified, although the gastroenterologist notes blood in the right colon and old blood coming from above the ileocecal valve. Which of the following is the test of choice in this patient?
Angiography
Small-bowel enteroclysis
CT scan of the abdomen
Technetium 99m (99mTc) pertechnetate scan
Small-bowel endoscopy
A 32-year-old woman undergoes an uncomplicated appendectomy for acute appendicitis. The pathology report notes the presence of a 1-cm carcinoid tumor in the tip of the appendix. Which of the following is the most appropriate management of this patient?
Right hemicolectomy
Right hemicolectomy and chemotherapy
Chemotherapy only
Radiation only
No further treatment
A 44-year-old man is brought to the emergency department after a motor vehicle accident. His cervical spine is immobilized and 2 large-bore intravenous lines are placed. His breath smells of alcohol. The patient is lethargic but responds to commands appropriately. A 3- cm laceration is present on his forehead. Ecchymoses are seen on his back and over the abdominal wall in the distribution of the seat belt. The lungs are clear to auscultation. The trachea is midline and the neck veins are collapsed. Passive movement of the right hip is limited due to pain. At the scene of the accident, blood pressure was 90/60 mm Hg and pulse was 130/min. After receiving a 1 L bolus of intravenous fluids, the patient's blood pressure remains 90/60 mm Hg and his pulse is now 122/min. Portable chest x-ray shows no pneumothorax or pleural effusions. A bedside abdominal ultrasound is inconclusive for hemoperitoneum or intra- abdominal injury due to poor image quality. What is the most appropriate next step in management of this patient?
Computed tomography scan of the abdomen
Computed tomography scan of the head
Diagnostic peritoneal lavage
Immediate laparotomy
Plain x-ray films of the abdomen
A 43-year-old mildly overweight female complains of periodic right knee swelling and pain with physical activity for the past three months. She says that this problem started while on a hiking trip three months ago, at which point she experienced a 'popping' sensation in her right knee. She recalls that her knee was swollen the next day, and responded to over-the-counter pain killers. Recently, she has been having to limit her physical activities due to knee pain. On physical examination, there is tenderness of the anterior and medial right knee joint. Which of the following is the most likely diagnosis?
Anterior cruciate ligament tear
Meniscal tear
Osteoarthritis
Patellar tendonitis
Anserine bursitis
A 53-year-old male is brought to the emergency room after a high-speed motor vehicle accident. He was an unrestrained driver and admits to consuming a moderate amount of alcohol before driving. In the ER, he complains of bilateral chest pain and left leg pain. His past medical history is significant for emphysema, diabetes mellitus and remote drug abuse. A traumatic fracture of the left femur is evident on physical examination. His initial arterial blood gas analysis shows a pH of 7.45, p02 of 81 mmHg and pC02 of 32 mmHg. His pulmonary capillary wedge pressure is 1OmmHg. After a 2000 ml IV fluid challenge, his p02 is 76 mmHg and his pulmonary capillary wedge pressure is 12 mmHg. Chest x-ray shows alveolar opacities over the right and left lower lobes. Hours after the accident, he complains of continued chest pain and shortness of breath. Which of the following diagnoses is most likely responsible for his shortness of breath?
Aspiration pneumonia
Hemothorax
Pulmonary contusion
Myocardial contusion
Aortic rupture
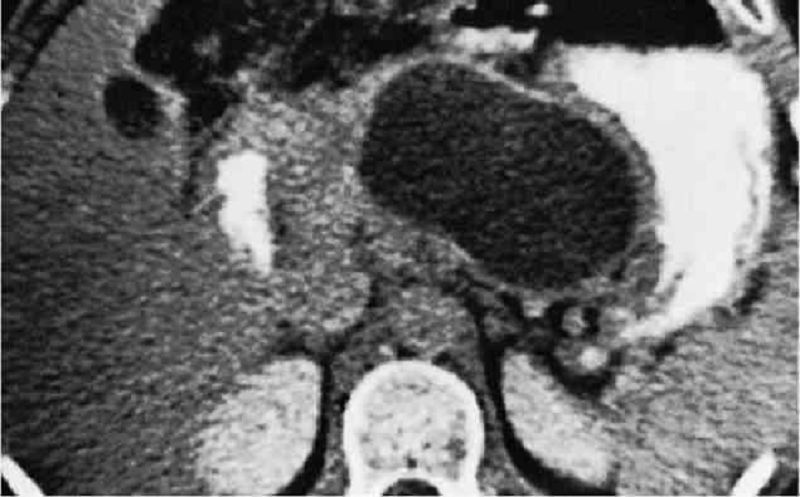
A 35-year-old woman presents with abdominal pain and jaundice. Subsequent ERCP reveals the congenital cystic anomaly of her biliary system illustrated in the film shown here. Which of the following is the most appropriate treatment?
Cholecystectomy with resection of the extrahepatic biliary tract and Roux-en-Y hepaticojejunostomy
Internal drainage via choledochoduodenostomy
Internal drainage via choledochocystojejunostomy
Percutaneous transhepatic biliary drainage
Liver transplantation
A 36-year-old man is in your intensive care unit on mechanical ventilation following thoracotomy for a 24-hour-old esophageal perforation. His WBC is markedly elevated, and he is febrile, hypotensive, and coagulopathic. His NG tube fills with blood and continues to bleed. Which of the following findings on upper endoscopy would be most suspicious for stress gastritis?
Multiple, shallow lesions with discrete areas of erythema along with focal hemorrhage in the antrum
Multiple, shallow lesions with discrete areas of erythema along with focal hemorrhage in the fundus
Multiple deep ulcerations extending into and through the muscularis mucosa in the antrum
Multiple deep ulcerations extending into and through the muscularis mucosa in the fundus
Single deep ulceration extending into and through the muscularis mucosa in the fundus
A 35-year-old man presents with right upper quadrant pain, fever, jaundice, and shaking chills. Ultrasound of the abdomen demonstrates gallstones, normal gallbladder wall thickness, and common bile duct of 1.0 cm. The patient is admitted to the hospital and given IV fluids and antibiotics. He continues to be febrile with increasing WBCs. Which of the following is the most appropriate next step in this patient’s management?
Endoscopic retrograde cholangiopancreatography (ERCP)
Placement of a cholecystostomy tube
Laparoscopic cholecystectomy
Open cholecystectomy
Emergent operation and decompression of the common bile duct with a T tube
An 88-year-old man with a history of end-stage renal failure, severe coronary artery disease, and brain metastases from lung cancer presents with acute cholecystitis. His family wants “everything done.” Which of the following is the best management option in this patient?
Tube cholecystostomy
Open cholecystectomy
Laparoscopic cholecystectomy
Intravenous antibiotics followed by elective cholecystectomy
Lithotripsy followed by long-term bile acid therapy
After a weekend drinking binge, a 45-year-old man presents to the hospital with abdominal pain, nausea, and vomiting. On physical examination, the patient is noted to have tenderness to palpation in the epigastrium. Laboratory tests reveal an amylase of 25,000 U/dL (normal < 180U/dL). The patient is medically managed and sent home after 1 week. A CT scan done 4 weeks later is pictured here. Currently the patient is asymptomatic. Which of the following is the most appropriate initial management of this patient?
Distal pancreatectomy
Percutaneous catheter drainage
Endoscopic drainage
Surgical drainage
No intervention is warranted at this time
A 54-year-old man presents with sudden onset of massive, painless, recurrent hematemesis. Upper endoscopy is performed and reveals bleeding from a lesion in the proximal stomach that is characterized as an abnormally large artery surrounded by normal-appearing gastric mucosa. Endoscopic modalities fail to stop the bleeding. Which of the following is the most appropriate surgical management of this patient?
Wedge resection of the lesion
Wedge resection of the lesion with truncal vagotomy
Wedge resection of the lesion with highly selective vagotomy
Wedge resection of the lesion with truncal vagotomy and antrectomy
Subtotal gastrectomy
A 31-year-old male is brought to the emergency department after being involved in a motor vehicle collision as an unrestrained passenger. He was given 3L of normal saline in the ambulance on his way to the hospital and has been receiving 5L/min of oxygen by nasal cannula. He is agitated and moves all four extremities spontaneously. His blood pressure is 85/55 mmHg and his heart rate is 120/min. His respiratory rate is 30/min. His pupils are symmetric and reactive to light. His neck veins are flat and his trachea is shifted slightly to the right. Over the left hemithorax, breath sounds are absent and there is dullness to percussion. Which of the following diagnoses is most likely?
Tension pneumothorax
Lung contusion
Lung atelectasis
Hemothorax
Diaphragmatic rupture
A 23-year-old woman comes to the physician because of right-sided foot pain. The pain started 5 weeks ago and is sharp and localized to the forefoot. She recalls no trauma or other inciting event but is an avid runner training for a long-distance race. The pain has been worsening over the past 1 week and prevents her from doing her daily running activities. She takes no medications. She is a vegetarian and does not drink soda. She does not use tobacco, alcohol, or illicit drugs. She is not sexually active, and her last menstrual period was 8 weeks ago. Her temperature is 37° C (98.6° F), blood pressure is 100/60 mm Hg, pulse is 68/min, and respirations are 12/min. Her body mass index is 15 kg/m2• Examination reveals tenderness to palpation along the first four metatarsal bones on the dorsal surface of the right foot, normal range of motion, and no erythema or bruising. Which of the following is the most likely diagnosis?
Morton neuroma
Plantar fasciitis
Stress fracture
Tarsal tunnel syndrome
Tenosynovitis
A neonate is examined in the nursery and found to have no anal orifice; only a small perineal fistulous opening is visualized. A complete workup is negative for any cardiac, esophageal, genitourinary, or musculoskeletal anomalies. Which of the following is the best next step in the management of this patient?
Diverting colostomy only
Posterior sagittal anorectoplasty only
Posterior sagittal anorectoplasty with diverting colostomy
Perineal operation only
Perineal operation with diverting colosto
A 2-month-old boy is examined because he has been straining while passing stool and has a distended abdomen. He is very low on the growth chart for age. The primary care physician suspects that the boy has Hirschsprung disease. Which of the following findings on workup is diagnostic?
Absence of ganglion cells on full-thickness rectal biopsy 2 cm above the dentate line
Absence of ganglion cells on full-thickness rectal biopsy 1 cm above the dentate line
Absence of ganglion cells on suction rectal biopsy 1 cm above the dentate line
Identification of a transition zone between the sigmoid colon and the distal rectum on barium enema
Inhibition of the resting anal inhibitory reflex on anorectal manometry
A newborn has a midline defect in the anterior abdominal wall. The parents ask what, if anything, should be done. Spontaneous closure of which of the following congenital abnormalities of the abdominal wall generally occurs by the age of 4?
Umbilical hernia
Patent urachus
Patent omphalomesenteric duct
Omphalocele
Gastroschisis
A neonate is found to have an imperforate anus. As the pediatric surgeon you recommend studies to search for other anomalies. Which of the following is an associated abnormality?
Congenital pulmonary airway malformation
Hydrocephalus
Duodenal atresia
Congenital heart disease
Corneal opacities

A 36-hour-old infant presents with bilious vomiting and an increasingly distended abdomen. At exploration, the segment pictured here is found as the point of obstruction. What is the best next step in management?
Gentle, persistent traction on the specimen
Enteroenterostomy
Small bowel resection with exteriorization of the ends
Small bowel resection with anastomosis
Lysis of Ladd band
During an appendectomy for acute appendicitis, a 4-cm mass is found in the midportion of the appendix. Frozen section reveals this lesion to be a carcinoid tumor. Which of the following is the most appropriate management of this patient?
Appendectomy
Appendectomy followed by a colonoscopy
Appendectomy followed by a PET scan
Right hemicolectomy
Total proctocolectomy
A 45-year-old man is examined for a yearly executive physical. A mass is palpated in the rectum, and a biopsy suggests carcinoid. Which of the following findings is most likely to be associated with the carcinoid syndrome?
Tumor < 2 cm
Tumor < 2 cm with ulceration
Tumor > 2 cm
Involvement of regional lymph nodes
Hepatic metastases
An ultrasound is performed on a patient with right upper quadrant pain. It demonstrates a large gallstone in the cystic duct but also a polypoid mass in the fundus. Which of the following is an indication for cholecystectomy for a polypoid gallbladder lesion?
Size greater than 0.5 cm
Presence of clinical symptoms
Patient age of older than 25 years
Presence of multiple small lesions
Absence of shadowing on ultrasound
An alcoholic man has been suffering excruciating pain from chronic pancreatitis recalcitrant to analgesics and splanchnic block. A surgeon recommends total pancreatectomy. A patient who has a total pancreatectomy might be expected to develop which of the following complications?
Diabetes mellitus and steatorrhea
Diabetes mellitus and constipation
Hypoglycemia
Hypoglycemia and steatorrhea
Hypoglycemia and constipation
A 45-year-old woman has an incidental finding of a liver mass on a CT scan. Magnetic resonance imaging (MRI) is suggestive of a hemangioma. Which of the following is the most appropriate management strategy for this patient?
Observation
Discontinuation of oral contraceptive pills
Percutaneous biopsy of the lesion to confirm the diagnosis
Resection of the hemangioma
Liver transplantation
A 57-year-old woman presents with adenocarcinoma of the right colon. Laboratory evaluation demonstrates an elevation of carcinoembryonic antigen (CEA) to 123 ng/mL. Which of the following is the most appropriate use of CEA testing in patients with colorectal cancer?
As a screening test for colorectal cancer
To determine which patients should receive adjuvant therapy
To determine which patients should receive neoadjuvant therapy
To monitor for postoperative recurrence
To monitor for preoperative metastatic disease
A 61-year-old woman with a history of unstable angina complains of hematemesis after retching and vomiting following a night of binge drinking. Endoscopy reveals a longitudinal mucosal tear at the gastroesophageal junction, which is not actively bleeding. Which of the following is the next recommended step in the management of this patient?
Angiography with embolization
Balloon tamponade
Exploratory laparotomy, gastrotomy, and oversewing of the tear
Systemic vasopressin infusion
Expectant management
A teenage boy falls from his bicycle and is run over by a truck. On arrival in the emergency room (ER), he is awake and alert and appears frightened but in no distress. The chest radiograph suggests an air-fluid level in the left lower lung field and the nasogastric tube seems to coil upward into the left chest. Which of the following is the next best step in his management?
Placement of a left chest tube
Thoracotomy
Laparotomy
Esophagogastroscopy
Diagnostic peritoneal lavage
A 10-year-old boy was the backseat belted passenger in a high-speed motor vehicle collision. On presentation to the ER, he is awake, alert, and hemodynamically stable. He is complaining of abdominal pain and has an ecchymosis on his anterior abdominal wall where the seatbelt was located. Which of the following is the best next step in his management?
Discharge him home without any other workup.
Discharge him home if his amylase level is normal.
Discharge him home if his abdominal plain films are negative for the presence of free air.
Discharge him home if an abdominal computed tomography (CT) scan is negative. E. Observe him regardless of negative test results. @
Observe him regardless of negative test results.
A 65-year-old man who smokes cigarettes and has chronic obstructive pulmonary disease falls and fractures the third, fourth, and fifth ribs in the left anterolateral chest. Chest x-ray is otherwise normal. Which of the following would be the most appropriate next step in his management?
Strapping the chest with adhesive tape
Admission to the hospital and treatment with oral analgesia
Tube thoracostomy
Placement of an epidural for pain management
Surgical fixation of the fractured ribs
A 36-year-old man who was hit by a car presents to the ER with hypotension. On examination, he has tenderness and bruising over his left lateral chest below the nipple. An ultrasound examination is performed and reveals free fluid in the abdomen. What is the most likely organ to have been injured in this patient?
Liver
Kidney
Spleen
Intestine
Pancreas
A 52-year-old man is pinned against a loading dock. The patient has a fractured femur, a pelvic fracture, a tender abdomen, and no pulses in the right foot with minimal tissue damage to the right leg. Angiography discloses a popliteal artery injury with obstruction. At surgery, the popliteal vein is also transected. His blood pressure is 85/60 mm Hg. Which of the following is the best management strategy for his vascular injuries?
Repair of the popliteal vein with simple closure
Repair of the popliteal vein with saphenous vein patch
Repair of the popliteal vein with saphenous vein patch
Repair of the popliteal vein with a synthetic interposition graft
Ligation of the popliteal vein
Amputation of the right lower extremity above the knee
A 27-year-old man sustains a single gunshot wound to the left thigh. In the ER, he is noted to have a large hematoma of his medial thigh. He complains of paresthesias in his left foot. On examination, there are weak pulses palpable distal to the injury and the patient is unable to move his foot. Which of the following is the most appropriate initial management of this patient?
Angiography
Immediate exploration and repair in the operating room
Fasciotomy of the anterior compartment of the calf
Observation for resolution of spasm
Local wound exploration at the bedside
A 25-year-old woman arrives in the ER following an automobile accident. She is acutely dyspneic with a respiratory rate of 60 breaths per minute. Breath sounds are markedly diminished on the right side. Which of the following is the best first step in the management of this patient?
A 17-year-old adolescent boy is stabbed in the left seventh intercostal space, midaxillary line. He presents to the ER with a heart rate of 86 beats per minute, blood pressure of 125/74 mm Hg, and oxygen saturation of 98%. Breath sounds are equal bilaterally. Which of the following is the most appropriate next step in his workup?
Local exploration of the wound
Left tube thoracostomy
Diagnostic laparoscopy
CT scan of the abdomen
Echocardiography
A 31-year-old biker is involved in a motor vehicle accident after attending a party where he drank a lot of soda drinks. He describes a direct blow to his lower abdomen and pelvis during the accident. He complains of diffuse abdominal pain that refers to his left shoulder. Which of the following injuries most likely accounts for this patient's current symptoms?
Bladder neck
Bladder dome
Anterior bladder wall
Pseudomembranous urethra
Anterior urethra
{"name":"Surgery USMLE (827-926)", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"A 30-year-old man comes to the physician because of a 2-week history of swelling and pain in the right knee. He first experienced pain when he twisted his leg while playing football 15 days ago. He felt something 'popping' in the knee at that time but ignored it. The pain and swelling has been increasing since, and he feels sudden pain with extension of his leg. Examination shov1s the right knee is swollen and tender along the medial side. Full extension of the right knee is not possible due to sudden pain during terminal extension. Snapping can be felt in the right knee on tibial torsion with the knee flexed at 90 degrees. An x-ray film of the knee joint shows no abnormalities. Which of the following is the most likely diagnosis?","img":"https://cdn.poll-maker.com/18-742412/untitled-333psd.jpg?sz=1200"}
More Quizzes
Bullying
10517
Muscle AOI
4231
Baby Shower Trivia!
11611
Bill of Rights
10511
What Mobility Aid Is Right for Me? Free With Results
201021513
Recovery Trivia Questions with Answers - Free
201020532
The War Works Hard - Free Answer Key
201019661
How Many Calories Should I Eat a Day? Free
201017823
Find Your Ideal Pokémon with Our Favorite Pokémon Picker
201016619
Up - Test Your Disney Pixar Movie Knowledge
201018562
Central Nervous System Stimulant - Identify the Drug
201019940
Library Page Test - Free Practice Questions
201016619