Orthopedic Disorders Quiz

Orthopedic Disorders Quiz
Test your knowledge on orthopedic disorders with our comprehensive quiz designed for medical students, professionals, and enthusiasts alike!
Challenging questions cover a wide array of topics:
- Osteoarthritis and its features
- Bone disorders and syndromes
- Neoplasms of the musculoskeletal system
Which of the following features is characteristic of osteoarthritis?
A. Pannus formation
B. Heberdon nodes
C. Baker cyst
D. Sacroiliitis
Failure of osteoclasts to resorb bone thereby resulting in thickened sclerotic bones with reduced mechanical strength is a characteristic feature of
A. Osteogenesis imperfecta
B. Osteopetrosis
C. Paget’s disease
D. Fibrous dysplasia
A couple brings their 2-year-old daughter to the clinic for the first time for a well-child check-up . Physical examination reveals short stature, a flat midface with a prominent forehead, and shortening of the limbs. The child's father exhibits similar physical features
A. Autosomal dominant cell -signaling defect of fibroblast growth factor receptor 3
B. Autosomal dominant defect in fibrillin 1
C. Autosomal recessive defect in fibrillin 1
D. X-linked recessive defect
This seronegative spondyloarthropathy is a chronic inflammatory joint disease that typically affects the axial joints (especially the sacroiliac joints) of persons 20- 30 years of age, who also test positive for HLA-B27.
A. Rheumatoid arthritis
B. Ankylosing spondylitis
C. Reiter syndrome
D. Osteomyelitis

A 54-year-old male complains of right knee swelling and pain. Microscopic findings of synovial fluid aspiration are shown on the image below. Which of the following is the most likely cause of this patient's symptoms?
A. Cartilage wear-and-tear injury
B. Immune complex deposition
C. Crystal arthropathy
D. Joint infection Traumatic joint injury
A 15-year-old boy notices a swelling around his left knee, which has been progressive over the past few months. The swelling is associated with pain, which becomes unbearable. He is brought by his parents to the emergency department. Radiographic analysis of his left knee reveals an elevation of the periosteum and an infiltrative mass in the distal femur.What is the most likely diagnosis?
A. Osteosarcoma
B. Ewing sarcoma
C. Chondrosarcoma
D. Metastatic colonic adenocarcinoma
A 16-year-old boy has noted pain in his left knee after each hockey practice session for the past month. On examination there is tenderness to palpation of his left knee, with reduced range of motion. A plain film radiograph of the left leg reveals a mass of the proximal tibial metaphysis that erodes the bone cortex, lifting up the periosteum where reactive new bone is apparent. The mass does not extend into the epiphyseal region. A bone biopsy is performed and microscopic examination shows atypical, elongated cells with hyperchromatic nuclei in an osteoid stroma. Which of the following neoplasms is he most likely to have?
A. Ewing sarcoma
B. Osteosarcoma
C. Chondrosarcoma
D. Multiple myeloma
E. Metastatic seminoma
A 13-year-old boy complains of pain persisting in his left leg for 3 weeks. On physical examination his temperature is 37.9 C. A radiograph of the leg reveals a mass in the diaphyseal region of the left femur with overlying cortical erosion and soft tissue extension. A bone biopsy is performed and the lesion on microscopic examination shows numerous small round blue cells. Which of the following neoplasms is he most likely to have?
A. Ewing sarcoma
B. Medulloblastoma
C. Neuroblastoma
D. Chondroblastoma
E. Osteoblastoma
A 58-year-old man has the sudden onset of severe pain in his left great toe. There is no history of trauma. On examination there is edema with erythema and pain on movement of the left 1st metatarsophalangeal joint, but there is no overlying skin ulceration. A joint aspirate is performed and on microscopic examination reveals numerous neutrophils and needle-shaped crystals. Over the next 3 weeks, he has two more similar episodes. On physical examination between these attacks, there is minimal loss of joint mobility. Which of the following laboratory test findings is most characteristic for his underlying disease process?
A. Hyperglycemia
B. Positive antinuclear antibody
C. Hyperuricemia
D. Hypercalcemia
A 14-year-old West African man has a history of multiple episodes of sudden onset of severe abdominal pain and back pain lasting for hours. Each time this happens, his peripheral blood smear demonstrates numerous sickled erythrocytes. A hemoglobin electrophoresis shows 94% Hgb S, 5% Hgb F, and 1% Hgb A2. He now has a painful right hip that is tender to palpation. A radiograph reveals irregular bony destruction of the femoral head. Which of the following infectious agents is most likely responsible for his findings?
A. Yersinia pestis
B. Clostridium
C. Salmonella
D. Candida
An 80-year-old woman has had no major medical problems, but she has never been physically active for most of her life. One day she falls out of bed and immediately notes a sharp pain in her left hip. She is subsequently unable to ambulate without severe pain. Radiographs show not only a fracture of the left femoral head, but also a compressed fracture of T10. Which of the following conditions is she most likely to have?
A. Vitamin D deficiency
B. Osteomyelitis
C. Osteoporosis
D. Metastatic cancer
An 11-year-old boy has pain in his left leg that has persisted for 3 weeks. On physical examination his temperature is 37.9°C. A radiograph of the leg reveals a mass in the diaphyseal region of the left femur with overlying cortical erosion and soft tissue extension. A bone biopsy is performed and the lesion on microscopic examination shows numerous small round blue cells. Karyotypic analysis of these cells shows t(11;22). Which of the following neoplasms is he most likely to have? (
A. Ewing sarcoma
B. Medulloblastoma
C. Chondroblastoma
D. Osteoblastoma
. A 51-year-old man has noted constant, dull right hip pain for the past 3 months. On physical examination he has diminished range of motion of the right hip. A radiograph reveals a 10 x 13 cm mass involving the right ischium of the pelvis. The mass has irregular borders and there are extensive areas of bony destruction along with some scattered calcifications. The lesion is resected, and grossly the mass has a bluish-white cut surface. Which of the following is the most likely diagnosis?
A. Osteosarcoma
B. Osteoblastoma
C. Chondrosarcoma
D. Osteoid osteoma
An otherwise healthy 44-year-old man with no prior medical history has had increasing back pain and right hip pain for the past decade. The pain is worse at the end of the day. On physical examination he has bony enlargement of the distal interphalangeal joints (DIP). A radiograph of the spine reveals the presence of prominent osteophytes involving the vertebral bodies. There is sclerosis with narrowing of the joint space at the right acetabulum seen on a radiograph of the pelvis. Which of the following diseases is he most likely to have?
A. Gout
B. Rheumatoid arthritis
C. Osteoarthritis
D. Pseudogout
A 16-year-old boy has noted pain in his left knee after each hockey practice session for the past month. On examination there is tenderness to palpation of his left knee, with reduced range of motion. A plain film radiograph of the left leg reveals a mass of the proximal tibial metaphysis that erodes bone cortex, lifting up the periosteum where reactive new bone is apparent. The mass does not extend into the epiphyseal region. A bone biopsy is performed and microscopic examination shows atypical, elongated cells with hyperchromatic nuclei in an osteoid stroma. Which of the following neoplasms is he most likely to have?
A. Ewing sarcoma
B. Osteosarcoma
C. Multiple myeloma
D. Seminoma
A 55-year-old obese male with history of HTN, diabetes, and lumbago presents with bilateral knee pain that has worsened slowly over the last 2 years. The knee pain is worse in the morning, lasts less than 30 minutes, and improves with activity. What physical exam finding would be present in patients?
A. Heberdon nodes and Bouchard nodes
B. Boutonniere Deformity and swan-neck deformities
C. High risk of urate nephropathy
D. Heliotrope Rash and Gottron Papules
A 37-year-old previously healthy male presents with difficulty walking due to severe pain, swelling, redness, and warmth of his right great toe over the last 24 hours after partying all night at a friend’s bachelor party. His hangover has subsided, but his big toe pain continues despite taking Tylenol. What finding is diagnostic?
A. Whewellite crystals with the typical ovoid shape
B. Hexagonal yellowish crystals with a waxy appearance microscopically
Needle-shaped negatively birefringent crystals within PMNs under a polarized light microscope
Multiple enchondromas are a feature of:
A. Ollier disease
B. Maffucci syndrome
C. McCune-Albright syndrome
D. Osteogenesis imperfacta
A 42-year-old woman Paro presents with slowly progressive syndrome comprising of features like pain and tender ness in multiple joints, with joint stuffiness on rising in the morning. Joint involvement is symmetric, with the proximal interphalangeal and metacarpophalangeal joints especially involved. The physician finds presence of tenderness in all the inflamed joints. Which of the following laboratory abnormalities is most likely asso ciated in this patient?
A. Antibodies to double-stranded DNA
B. IgM anti-IgG antibodies
C. Urate crystals and neutrophils in synovial fluid
D. Anti-DNAase B
E. HLA-B27 antigen
A 37-year-old man presents with lower back pain. He complains of stiffness in his axial spine that usually improves over the course of the morning with activity. X-ray of the lumbar spine is normal, while x-ray of the sacroiliac joints shows bilateral abnormality including irregular joint space widening with bone erosions and subchondral sclerosis. HLA-B27 is positive. Which of the following is the most likely diagnosis?
A. Ankylosing spondylitis
B. Osteoarthritis
C. Gouty arthritis
D. Rheumatoid arthritis
A 47-year-old man presents to his primary doctor with 2 weeks of fever, headache, and muscle aches. He also has noted a nonpruritic erythematous rash in the right groin. The rash has been enlarging for the past week, with new areas of clearing resulting in concentric rings of erythema. The patient is a Boy Scout leader and recently returned from a camping trip in Connecticut. Which of the following is the most likely diagnosis?
A. Reiter's syndrome
B. Lyme disease
C. Rheumatoid arthritis
D. Gonococcal arthritis
In osteoarthritis:
A. There is a marked synovial reaction.
B. Chrondrocytes play a role in cartilage destruction.
C. Osteophytes develop on top of the articular surface.
D. Cbrondrocytes excrete digestive enzymes into the matrix in active forms.
A 5-year-old girl presents to the pediatrician for evaluation of short stature. On physical exam she has multiple lower extremity bruises and bluish scleral discoloration. Dental exam reveals multiple cavities. Audiological evaluation reveals a conductive hearing loss. Radiographic skeletal survey reveals healed right seventh rib and right humerus fractures and a healing left midshaft clavicle fracture. The physician does not suspect child abuse. Which of the following is the most likely diagnosis?
A. Paget disease
B. Osteopetrosis
C. Osteoporosis
D. Osteogenesis imperfecta
A 24-year-old male presents with history of diarrhea 3 weeks ago and returns to the clinic with redness in the eyes, tearing, painful urination, mouth sores, and right knee pain. What is the diagnosis?
A. Osteoarthritis
B. Psoriatic arthritis
C. Septic arthritis
D. Reiter syndrome
You encountered a 35-year old patient with necrotizing granulomas along the respiratory tract and the lungs. He eventually died of crescentic glomerulonephritis. Which of the following markers would turn out positive in this patient?
A. c-ANCA
B. p-ANCA
C. Anti-centromere
D. Anti-Smith
Which of the following is most likely associated with the Philadelphia chromosome?
A. Found in AML
B. t (9;23)
C. BCR-ABL gene
D. Good prognosis
A 40 year old male suddenly experienced severe headache. Upon consultation, his BP is noted to be at 200/120. Past history shows normal BP on regular checkups. Anti hypertensive are immediately given. However, BP remains in the range of 200/120-180/100. Nicardipine drip is instituted. Two days later, the patient died becasue of intracerebral hemorrhage. Biopsy of the kidney revealed onion skin, concentric, laminated thickening of the walls of arterioles with progressive narrowing of the lumina consistent with what kind of arteriolosclerosis?
A. Hyaline arteriolosclerosis
B. Hyperplastic arteriolosclerosis
C. Focal segmental nephrosclerosis
D. Benign nephrosclerosis
A 65 year old female presents with fever, headache and diplopia. On palpation, tenderness is noted along the course of the temporal artery. A biopsy would most likely confirm which of the following diagnosis?
A. Takayasu arteritis
B. Retinoblastoma
C. Giant cell arteritis
D. Kaposi sarcoma
A 27-year-old man who is an IV drug user presents to the emergency department because of abdominal pain. He reports red discoloration of his urine. On examination, he is hypertensive and has no dyspnea, chest pain, or hemoptysis. After initial evaluation in the clinic, the patient is admitted to the hospital. A chest radiograph and radiographic imaging of the kidneys, bladder, and pelvis reveal no abnormalities. Laboratory studies reveal elevated levels of amylase and lipase and an elevated level of creatinine. The patient is positive for hepatitis B surface antigen. Which of the following is the most likely diagnosis?
A. Polyarteritis nodosa
B. Kawasaki disease
C. Goodpasture syndrome
D. Acute pancreatitis
A 70-year-old woman complains of a throbbing unilateral headache and vision problems. She reports weight loss and mandibular pain while eating. The patient also has a history of recurrent bouts of fever accompanied by malaise and muscle aches. Physical examination reveals nodular enlargement of the temporal artery with pain on palpation. A biopsy is obtained (shown in the image). What is the appropriate diagnosis?
A. Giant cell arteritis
B. Hypersensitivity angiitis
C. Kawasaki disease
D. Polyarteritis nodosa
E. Wegener granulomatosis
A 19-year-old young woman who emigrated from Taiwan 8 years ago presents with fever, malaise, myalgias, and arthritis and “coldness” in her upper extremities. She has a weak radial pulse bilaterally, and a magnetic resonance angiogram demonstrates nearly 75% stenosis of the main arteries originating from the aorta. She likely has which of the following rheumatologic conditions?
A. Buerger disease
B. Kawasaki disease
C. Raynaud disease
D. Takayasu arteritis
E. Temporal arteritis
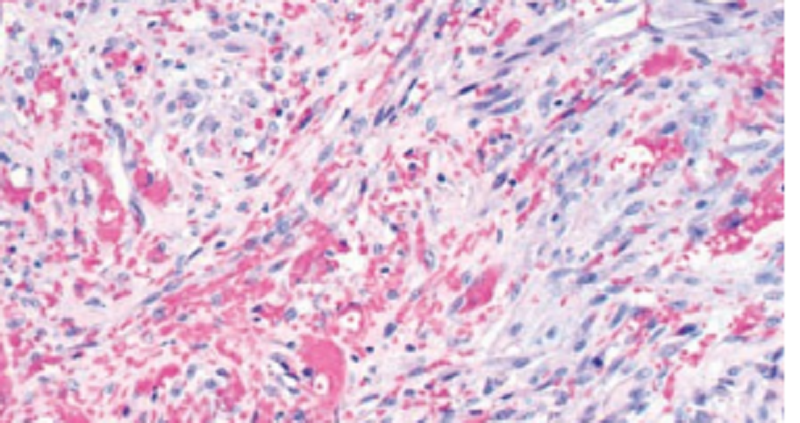
A 33-year-old man with AIDS presents with multiple, purplecolored skin nodules on his hands and feet. The lesions vary in size from 1 mm to 1 cm in diameter. Biopsy of lesional skin is shown in the image. Which of the following viruses is implicated in the pathogenesis of this patient’s skin neoplasm?
A. Cytomegalovirus
B. Human herpesvirus-6
C. Human herpesvirus-8
D. Human immunodefi ciency virus
E. Human papillomavirus
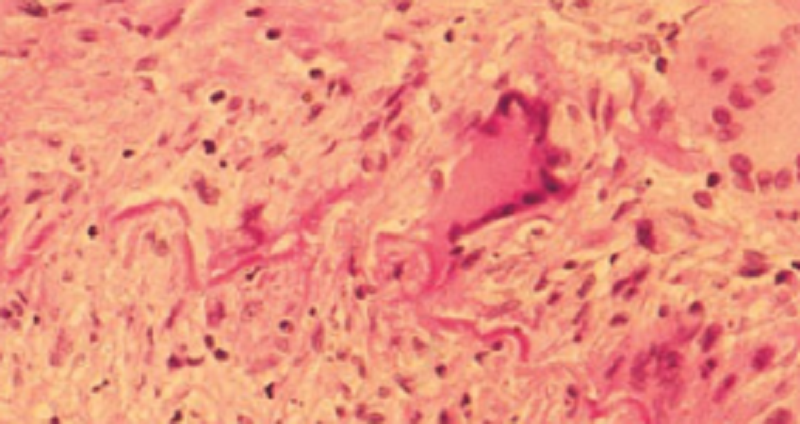
A 70-year-old woman complains of a throbbing unilateral headache and vision problems. She reports weight loss and mandibular pain while eating. The patient also has a history of recurrent bouts of fever accompanied by malaise and muscle aches. Physical examination reveals nodular enlargement of the temporal artery with pain on palpation. A biopsy is obtained (shown in the image). What is the appropriate diagnosis?
A. Giant cell arteritis
B. Hypersensitivity angiitis
C. Kawasaki disease
D. Polyarteritis nodosa
E. Wegener granulomatosis

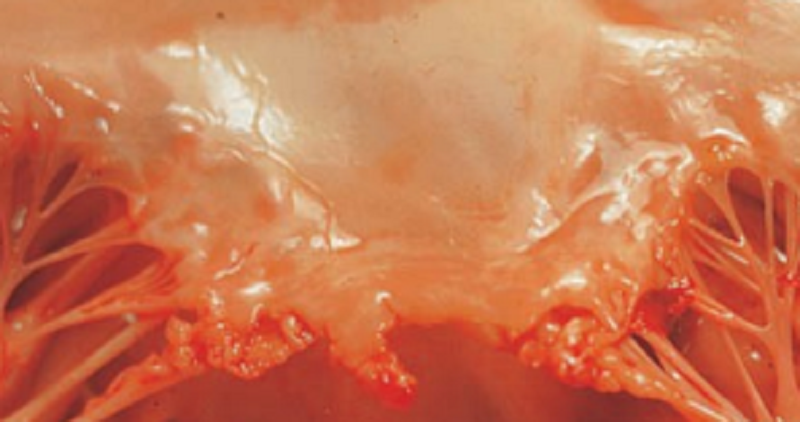
A 45-year-old man is brought to the emergency room with rapid pulse and cold and clammy skin. Blood pressure is 90/50 mm Hg. An X-ray film of the chest demonstrates dilation of the ascending aorta. Cardiac auscultation reveals a diastolic murmur in the aortic region. Laboratory studies show that serum cholesterol is 160 mg/dL, hematocrit is 35%, and hemoglobin is 13.6 g/dL. The fluorescent Treponema antibody test is positive. The patient suddenly becomes hypotensive and dies. The luminal surface of the ascending aorta at autopsy is shown in the image. Which of the following was most likely involved in the pathogenesis of this aortic lesion?
A. Arterial wall defect due to diabetes
B. Atherosclerosis
C. Congenital defect of the arterial wall
D. Cystic medial necrosis
E. Endarteritis of the vasa vasorum
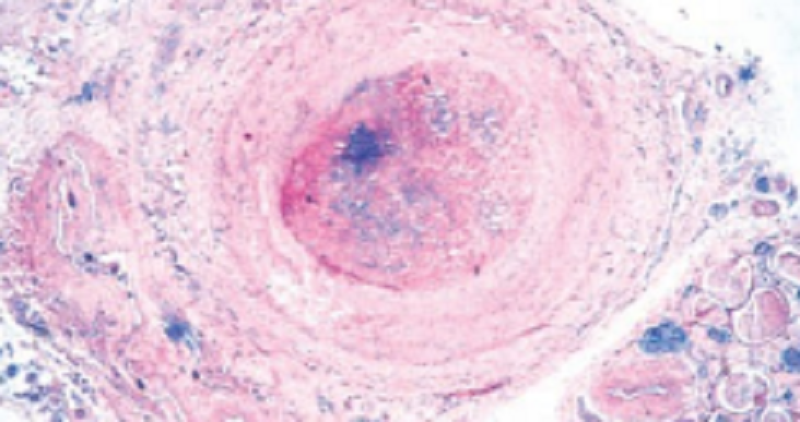
. A 45-year-old man presents with pain in the legs upon exercise and destruction of the tips of his fingers. He has an 80-packyear history of smoking. Laboratory values include hemoglobin of 16 g/dL, WBC of 8,500/μL, serum cholesterol of 220 mg/dL, fasting blood sugar of 90 mg/dL, and negative tests for antinuclear antibodies. Biopsy of the affected area (shown in the image) reveals intraluminal thrombi in medium-sized arteries and inflammation extending from arteries to neighboring veins and nerves. What is the appropriate diagnosis? (Vascula
A. Buerger disease
B. Churg-Strauss disease
C. Kawasaki disease
D. Polyarteritis nodosa
E. Takayasu arteritis

An 80-year-old man with long-standing diabetes and systemic hypertension dies of congestive heart failure. The luminal surface of the abdominal aorta is shown in the image. Which of the following pathologic changes would you expect to see on microscopic examination?
A. Acute infl ammation of the vessel wall
B. Bacterial colonies in the vessel wall
C. Cystic medial necrosis
D. Lipid deposition and smooth muscle cell hyperplasia
E. Obliterative endarteritis of the vasa vasorum
A 20-year-old woman complains of double vision, fainting spells, tingling of the fingers of her left hand, and numbness of the fingers of her right hand. Physical examination reveals absence of pulse in her right arm. Laboratory tests show elevated erythrocyte sedimentation rate and thrombocytosis. An aortogram demonstrates narrowing and occlusion of branching arteries, including the right subclavian artery. The patient subsequently develops heart failure and dies of massive pulmonary edema. At autopsy, the aorta has a thickened wall and shows vasculitis and fragmentation of elastic fibers. Which of the following is the most likely diagnosis?
A. Buerger disease
B. Churg-Strauss disease
C. Kawasaki disease
D. Polyarteritis nodosa
E. Takayasu arteritis
A 20-year-old woman presents with increasing fatigue, muscle pain, and visual disturbances. Physical examination finds weak pulses in her upper extremities, and further evaluation finds thickening of the aortic arch and narrowing of the blood vessels that originate from the aortic arch. Which of the following is the most likely diagnosis?
A. Goodpasture disease
B. Kawasaki disease
C. Polyarteritis nodosa
D. Takayasu disease
During a routine checkup in the GP, a 34-year-old man had consistently high blood pressure of 149 mmHg systolic. Benign hypertension is characterized by: C
A. Fibroelastic thinning of the intima
B. Hyaline deposition in arteriole walls
C. Sudden and severe increase in blood pressure
A 70-year-old woman presents with recurrent headaches, blurred vision, and a 1- week history of joint pain and flu-like symptoms. Physical examination finds focal tenderness in her right temporal area, and laboratory examination reveals a markedly elevated erythrocyte sedimentation rate. A biopsy from her right temporal artery reveals granulomatous inflammation with giant cells in the inner tunica media of the vessel wall. Without treatment, what is the worst complication associated with this individual's disease?
A. Aspiration pneumonia
B. Embolic stroke
C. Hearing loss
D. Irreversible blindness
Upon autoposy an incidental finding of atherosclerosis was made. Which of the following is true of atherosclerosis?
A. It is common in the pulmonary arteries
B. It is associated with hypocholesterolaemia
C. It may be seen as a pathological response to endothelial injury
D. It is characterized by neutrophil lipid uptake to form foam cells
A 3-year-old boy comes to the pediatrician with fever, conjunctivitis, erythema in the oral mucosa, and cervical lymphadenopathy. The boy suddenly becomes hypotensive and goes into cardiac arrest and dies shortly thereafter. Autopsy shows aneurysmal dilations of the left circumflex and right coronary arteries. The boy’s disease is characterized as a self-limiting disease that most commonly affects the coronary arteries. Which of the following diseases is the correct diagnosis?
A. Polyarteritis nodosa
B. Kawasaki’s disease
C. Wegener’s granulomatosis
D. Takayasu’s arteritis
A 69-year-old woman has been bedridden while recuperating from a bout of viral pneumonia complicated by bacterial pneumonia for the past 2 weeks. Physical examination now shows some swelling and tenderness of the right leg, which worsens when she raises or moves the leg. Which of the following terms best describes the condition involving her right leg? (
A. Disseminated intravascular coagulation
B. Lymphedema
C. Thromboangiitis obliterans
D. Thrombosis of deep veins
E. Varicose veins
A Young scientist studies chronic vasculitis, involving small and medium-sized arteries. The etiology of this vasculitis is unknown, but in 30 % of cases, it is associated with Hepatitis B infection. This adult type vasculitis does not involve pulmonary arteries and does not cause glomerulonephritis. There is perivascular inflammation resulting in nodularity, mIcroaneurysms are seen in 50% of cases. Which of the following most likely represents this vasculitis?
A. Churg strauss
B. Takayasu arteritis
C. Polyarteritis nodosa
D. Kawasaki disease
E. Wegener granulomatosis
A previously healthy 67-year-old man presents to the emergency room with numbness of his left leg. Temperature and blood pressure are normal. Physical examination shows pallor and a cool left leg with absence of distal pulse An ECG reveals no abnormalities. An arteriogram demonstrates a markedly dilated abdominal aorta and occlusion of the left popliteal artery. The blockage is removed surgically, and the patient recovers. Which of the following is the most likely source of the arterial thromboembolus in this patient?
A. Deep venous thrombosis
B. Left ventricular mural thrombus
C. Nonbacterial endocarditis
D. Septic pylephlebitis
E. Thrombosis in an aneurysm
A 60-year-old man presents with dizziness, nausea, and severe shortness of breath of several months’ duration. Physical examination shows hepatomegaly, ascites, and anasarca. His blood pressure is 200/115 mm Hg. An X-ray fi lm of the chest demonstrates cardiomegaly and mild pulmonary edema. Although different mechanisms may have contributed to the pathogenesis of hypertension in this patient, the common end result for all of them is which of the following?
A. Arterial cystic medial necrosis
B. Decreased plasma oncotic pressure
C. Generalized vasodilation
D. Increased peripheral vascular resistance
E. Increased vascular permeability
A 32-year-old female was brought to the cardiologist with fever, night sweats, myalgias. Physical examination shows diminished carotid and absent brachial pulsations. ESR was markedly elevated. Treatment with prednisolone was started. Which of the following vasculitis does she have?
A. Obliteration of small vessels
B. Granulomatous thickening and narrowing of the aortic arch
C. Narrowing of small veins
D. Leukocytoclastic vasculitis
E. Infiltration of the small vessels by macrophages
A 6-year-old girl presents with a 2-week history of a skin rash over her buttocks and legs and joint pain. The parents report seeing blood in the urine. Physical examination reveals palpable purpuric skin lesions and markedly swollen knees. The results of laboratory studies reveal abnormally high erythrocyte sedimentation rate (30 mm/h), BUN of 25 mg/dL, and serum creatinine of 3 mg/dL. Urinalysis demonstrates RBCs and RBC casts. The stool guaiac test is positive. Biopsy of lesional skin reveals deposits of IgA in the walls of small blood vessels. Which of the following is the most likely diagnosis?
A. Henoch-Schönlein purpura
B. Hypersensitivity vasculitis
C. Kawasaki disease
D. Polyarteritis nodosa
E. Poststreptococcal glomerulonephritis
A 45-year-old black man undergoes renal biopsy for evaluation of chronic renal failure. The patient has a 60-pack-year history of smoking. Physical examination reveals a blood pressure of 190/120 mm Hg. A renal biopsy shows thickening of small arteries and arterioles, as well as edematous intimal expansion and fi brinoid necrosis. The Congo red stain is negative. Laboratory studies show hemoglobin is 10.2 g/dL and serum cholesterol is 250 mg/dL. BUN and serum creatinine are 42 and 5.5 mg/dL, respectively. Which of the following is the most likely cause of renal failure in this patient? (
A. Amyloid nephropathy
B. Chronic pyelonephritis
C. Malignant hypertension
D. Polyarteritis nodosa
E. Proliferative glomerulonephritis
.A 52-year-old woman comes to the emergency department due to increasing dyspnea and chest tightness over the past 2 weeks. She has a history of stage 4 chronic kidney disease due to chronic glomerulonephritis. Temperature is 36.6 C (97.8 F), blood pressure is 106/82 mm Hg, and pulse is 98/min. Systolic blood pressure decreases by 12 mm Hg during inspiration. Physical examination shows distant heart sounds and clear lungs. Echocardiography in this patient is the most likely to reveal which the following findings?
A. Severe tricuspid regurgitation
B. Engorged inferior vena cava
C. Dilation of all cardiac chambers
D. Apical wall motion abnormality
E. Systolic anterior motion of the mitral valve
An young athlete dies suddenly and unexpectedly. Autopsy reveals massive myocardial hypertrophy with disproportionate thickening of the ventricular septum. What is the most likely pathologic etiology of this condition?
A. Previous viral myocardial infection
B. Atherosclerotic blockage of coronary arteries
C. Radiation-induced myocardial fibrosis
D. Mutation of gene encoding beta-myosin heavy chain
E. None of the above
A 44-year-old woman dies as a consequence of a "stroke". At autopsy, she is found to have a large right basal ganglia hemorrhage. She has an enlarged 550 gm heart with predominantly left ventricular hypertrophy. Her kidneys are small, about 80 gm each, with cortical scarring, and microscopically they demonstrate small renal arterioles that have luminal narrowing from concentric intimal thickening. Which of the following is the most likely condition associated with her findings?
A. Autosomal dominant polycystic kidney disease
B. Diabetes mellitus, type II
C. Hypercholesterolemia
D. Malignant hypertension
E. Monckeberg's sclerosis
A 17-year-old high school student dies suddenly while playing basketball. At autopsy, asymmetric hypertrophy of the interventricular septum is discovered. Histologic sections from this area reveal disorganization of the myofibers, which are thicker than normal and have hyperchromatic nuclei. What is the most likely diagnosis?
A. Hypertrophic cardiomyopathy
B. Dilated cardiomyopathy
C. Constrictive cardiomyopathy
D. Secondary cardiomyopathy
E. Endomyocardial fibrosis
A 4-year-old child from China was brought to the pediatrician due to fevers lasting 5 days. Fever is unresponsive to acetaminophen. Physical examination shows the desquamation of the skin on fingers, as well as edema of the hands and feet. The patient has bilateral conjunctival injection, cervical lymphadenopathy, erythema of the tongue. Immediate treatment with Aspirin and intravenous immunoglobulin was started to avoid which of the following complications?
A. Buerger disease
B. Takayasu arteritis
C. Kawasaki disease
D. Polyarteritis nodosa
E. Behcet disease
A 17-year-old girl is short in stature for her age. She has not yet shown any changes of puberty. On physical examination her vital signs include T 37°C, RR 18/minute, P 75/minute, and BP 165/85 mm Hg. She has a continuous murmur heard over both the front of the chest as well as her back. Her lower extremities are cool with diminished pulses and poor capillary filling. She has a webbed neck. A chest radiograph reveals a prominent left heart border, no edema or effusions, and rib notching. Which of the following cardiovascular abnormalities is she most likely to have? (
A. Shortening and thickening of chordae tendineae of the mitral valve
B. Narrowing of the aorta past the ductus arteriosus
C. Supravalvular narrowing in the aortic root
D. Lack of development of the spiral septum and partial absence of conus musculature
A 45-year-old man was rushed to the hospital following the sudden onset of an episode of crushing substernal chest pain. He receives advanced life support measures. An EKG shows changes consistent with a large transmural anterolateral area of infarction involving wall of the left ventricle. He develops cardiogenic shock. Which of the following microscopic findings is most likely to be present in this area 4 days following the onset of his chest pain?
A. Fibroblasts and collagen deposition
B. Myofiber necrosis with neutrophils
C. Granulomatous inflammation
D. Perivascular lymphocytic infiltrates
A 69-year-old woman with a 7 kg weight loss over the past 6 months now has developed painless jaundice over the past 2 weeks. On physical examination she is afebrile. An abdominal CT scan shows a large mass involving the head of the pancreas, along with widespread nodules in the liver. Nodules are seen in both lungs by chest radiograph. Which of the following cardiac lesions is she most likely to develop?
A. Dilated cardiomyopathy
B. Non-bacterial thrombotic endocarditis
C. Endocardial fibrosis
D. Acute myocardial infarction
A 66-year-old man has had congestive heart failure with increasing pulmonary congestion and edema for the past year. He had been previously healthy all his life with no major illnesses. On physical examination his blood pressure is 125/85 mm Hg and he is afebrile. A systolic ejection click is auscultated. A chest x-ray shows cardiomegaly with a prominent left heart border and pulmonary edema. Laboratory studies show a serum glucose of 95 mg/dL and total serum cholesterol of 175 mg/dL. His serum creatine kinase is not elevated. Which of the following underlying diseases is he most likely to have?
A. Alcoholic cardiomyopathy
B. Calcified bicuspid aortic valve
C. Tricuspid valve endocarditis
D. Aortic dissection
A 44-year-old woman dies as a consequence of a "stroke". At autopsy, she is found to have a large right basal ganglia hemorrhage. She has an enlarged 550 gm heart with predominantly left ventricular hypertrophy. Her kidneys are small, about 80 gm each, with cortical scarring, and microscopically they demonstrate small renal arterioles that have luminal narrowing from concentric intimal thickening. Which of the following is the most likely condition associated with her findings?
A. Autosomal dominant polycystic kidney disease
B. Diabetes mellitus, type II
C. Hypercholesterolemia
D. Hypertensive emergency
A 40-year-old woman presents with dyspnea, heart palpitations, and pitting edema. She was seen for fl u-like symptoms and prominent muscle pain 3 weeks ago. Physical examination shows tachycardia and irregular heart beats. A chest X-ray reveals cardiomegaly and pulmonary edema. The patient subsequently dies of cardiorespiratory failure. Histopathology of the heart muscle at autopsy is shown in the image. What is the appropriate diagnosis?
A. Acute bacterial endocarditis
B. Acute myocardial infarction
C. Endocardial fibroelastosis
D. Rheumatic heart disease
E. Viral myocarditis
A 25-year-old man dies suddenly and unexpectedly while at a nightclub late one evening. The medical examiner performs an autopsy. There is no evidence for trauma on external examination of the body. There are no gross pathologic findings of internal organs. Postmortem toxicologic findings are significant for high blood levels of cocaine and its metabolite benzoylecgonine. Which of the following is the most likely histopathologic finding involving his heart?
A. Contraction band necrosis
B. Lymphocytic myocarditis
C. Myofiber disarray
D. Coronary thrombosis
A 49-year-old woman had atrial fibrillation that was poorly controlled, even with amiodarone therapy. She suffered a 'stroke' and died. At autopsy, her 600 gm heart is noted to have a mitral valve with partial fusion of the leaflets along with thickening and shortening of the chordae tendineae. There is an enlarged left atrium filled with mural thrombus. Which of the following underlying causes of death is she most likely to have?
A. Systemic lupus erythematosus
B. Marantic endocarditis
C. Rheumatic heart disease
D. Cardiac amyloidosis
A 72-year-old woman has had no major illness throughout her life. She has had three syncope episodes during the past 2 weeks. Over the past two days she has developed shortness of breath and coupled with production of frothy white sputum. On physical examination she is afebrile. Her blood pressure is 135/90 mm Hg. She has no peripheral edema. A chest radiograph reveals a prominent left heart border in the region of the left ventricle, but the other chambers do not appear to be prominent. Which of the following is the most likely diagnosis?
A. Acute rheumatic fever
B. Mitral valve insufficiency
C. Calcific aortic stenosis
D. Infective endocarditis
A 58-year-old man develops deep venous thrombosis during a hospitalization for prostatectomy. He exhibits decreased mental status 10 days postoperatively, with right hemiplegia. A CT scan of the head shows an acute cerebral infarction in the distribution of the left middle cerebral artery. A chest radiograph reveals cardiac enlargement and prominence of the main pulmonary arteries consistent with pulmonary hypertension. Laboratory studies show a serum troponin I of <0.4 ng/mL. Which of the following lesions is most likely to be present on echocardiography?
A. Coarctation of the aorta
B. Tetralogy of Fallot
C. Atrial septal defect
D. Dextrocardia
A 27-year-old G2 P1 woman has a screening ultrasound performed at 18 weeks gestation. The fetus is appropriate in size for 18 weeks. The fetal kidneys, liver, head, and extremities appear normal. However, the fetus has a heart with a membranous ventricular septal defect, overriding aorta, and marked pulmonic atresia. If the baby were to be liveborn, which of the following characteristics on physical examination would most likely result from these cardiac defects?
A. Systemic hypertension
B. Weak lower extremity pulses
C. Telangiectasias
D. Cyanosis
A 51-year-old woman has had several syncopal episodes over the past year. Each episode is characterized by sudden but brief loss of consciousness. She reports no chest pain. On physical examination her vital signs show T 36.9°C, P 80/minute, RR 16/minute, and BP 110/75 mm Hg. She has no pedal edema. On brain MR imaging there is a 1.5 cm cystic area in the left parietal cortex. A chest radiograph shows no cardiac enlargement, and her lung fields are normal. Her serum total cholesterol is 165 mg/dL. Which of the following cardiac lesions is she most likely to have?
A. Cardiac amyloidosis
B. Left atrial myxoma
C. Tuberculous pericarditis
D. Mitral valve prolapse
A 53-year-old woman presents with a 6-week history of fever, fatigue, and weight loss. Her temperature is 38.7°C (103°F), pulse rate 110 per minute, and blood pressure 140/80 mm Hg. Physical examination reveals petechiae and clubbing of the fingers. The patient develops mental status changes, suffers a massive stroke, and expires. The mitral valve is examined at autopsy (shown in the image). Which of the following is the appropriate pathologic diagnosis?
A. Bacterial endocarditis
B. Carcinoid heart disease
C. Libman-Sacks endocarditis
D. Marantic endocarditis
E. Mitral valve prolapse
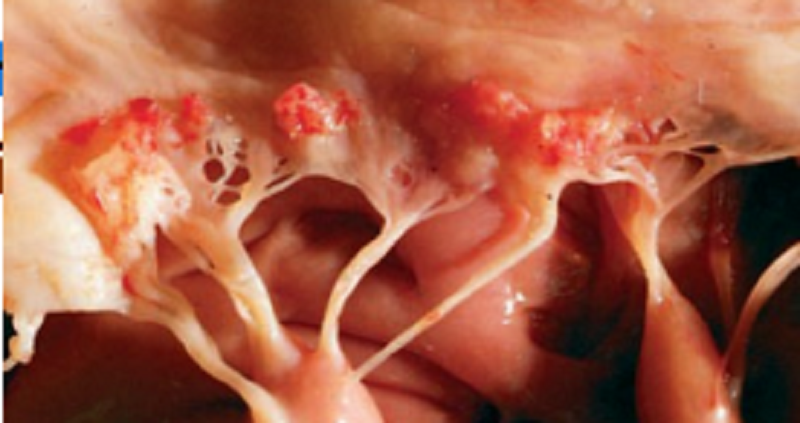
A 50-year-old man with adenocarcinoma of the pancreas is brought to the emergency room in a comatose state. A CT scan of the brain is consistent with a recent infarct in the left temporal lobe. Blood cultures are negative. The patient never regains consciousness and expires 2 days later. The heart at autopsy is shown in the image. Which of the following is the most likely underlying cause of stroke in this patient? (Cardio)
A. Calcifi c aortic stenosis
B. Carcinoid heart disease
C. Cardiac metastases
D. Nonbacterial thrombotic endocarditis
E. Subacute bacterial endocarditis
A 63-year-old woman has the sudden onset of 'knife-like' pain in the chest radiating to the back. She has been previously healthy except for a history of poorly controlled hypertension. She is transported to the hospital and on arrival she has a heart rate of 90/minute, respirations 20/minute, temperature 36.8°C, and blood pressure 150/100 mm Hg. No murmurs, rubs, or gallops are audible. A chest radiograph reveals a widened mediastinum. Laboratory findings include a total serum creatine kinase of 55 U/L, creatinine 0.9 mg/dL, and glucose 123 mg/dL. Which of the following is the most likely diagnosis?
A. Aortic dissection
B. Myocardial infarction
C. Pericarditis
D. Gastric ulcer rupture
A 19-year-old woman has had increasing malaise for the past 5 months. On physical examination she has a cardiac murmur characterized by a mid systolic click. An echocardiogram demonstrates mitral insufficiency with upward displacement of one leaflet. There is aortic root dilation to 4 cm. She has a dislocated right ocular crystalline lens. A year later she dies suddenly and unexpectedly. The medical examiner finds a prolapsed mitral valve with elongation, thinning, and rupture of chordae tendineae. A mutation involving which of the following genes is most likely to be present in this patient? (
A. Beta-myosin
B. CFTR
C. Fibrillin
D. Spectrin
A 65-year-old man has sudden onset of severe abdominal pain that has persisted for 3 hours. Physical examination reveals his temperature is 37°C, heart rate 110/minute, respirations 25/minute, and blood pressure 145/100 mmHg. He has diminished pulses in the lower extremities. There is a pulsatile abdominal mass. His serum creatine kinase is not elevated. He has had fasting blood glucose measurements in the range of 140 to 180 mg/dL for over 20 years. Which of the following conditions is he most likely to have?
A. Superior mesenteric artery thrombosis
B. Atherosclerotic aortic aneurysm
C. Polyarteritis nodosa
D. Monckeberg's medial calcific sclerosis
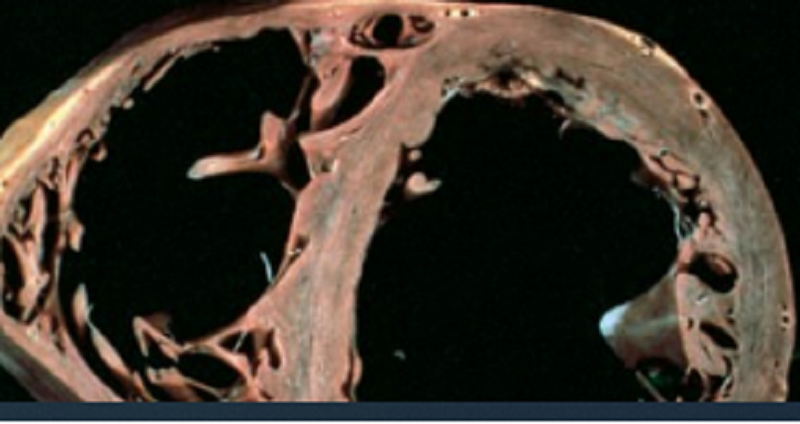
A 50-year-old man underwent heart transplantation for lowoutput heart failure that was unresponsive to medical treatment. The affected heart at autopsy is shown in the image. It weighs 950 g (normal up to 350 g) and shows no evidence of coronary artery atherosclerosis. Histologically, the myocardium demonstrates hypertrophic myocytes and foci of myocardial fibrosis but no evidence of inflammation or myofiber disarray. Which of the following is the most likely diagnosis?
A. Cardiac amyloidosis
B. Dilated cardiomyopathy
C. Hypertrophic cardiomyopathy
D. Restrictive cardiomyopathy
E. Ventricular aneurysm
Endocarditis in IV drug users typically (
A. Involves the mitral valve
B. Is caused by candida albicans
C. Does not cause fever
D. Has a better prognosis than other causes of endocarditis
E. Is caused by staph aureus

A 50-year-old woman presents with fatigue and shortness of breath. Physical examination shows clinical evidence of pulmonary edema, enlargement of the left atrium, and calcification of the mitral valve. A CT scan demonstrates a large mass in the left atrium. Before open heart surgery can be performed, the patient expires of an ischemic stroke. The heart at autopsy is shown in the image. Which of the following is the most likely diagnosis?
A. Calcific aortic stenosis
B. Cardiac myxoma
C. Fibroelastoma
D. Mural thrombus
Which of the following is characteristic of stable angina pectoris?
A. It is relieved by rest or medication.
B. It usually occurs at rest or at night.
C. Patients are at very high risk for immediate myocardial infarction.
D. It is usually caused by coronary vasospasm.
A 56-year-old-man with a 25 pack-year smoking history sees his physician with complaints of dyspnea and weight gain. Chest x-ray shows pulmonary artery enlargement and echo shows right ventricular hypertrophy. Which of the following is the most likely diagnosis?
A. Hypertrophic cardiomyopathy
B. Cor pulmonale
C. Dilated Cardiomyopathy
D. Isolated Left-sided heart failure
. An 8-month-old girl with Turner syndrome is brought to the emergency room by her parents, who complain that their daughter is breathing rapidly and not eating. Physical examination reveals tachypnea, pallor, absent femoral pulses, and a murmur heard at the left axilla. There is hypertension in the upper extremities and low blood pressure in both legs. A chest x-ray shows notching or scalloping of the ribs. What is the appropriate diagnosis?
A. Patent ductus arteriosus
B. Aortic valve stenosis
C. Coarctation of aorta
D. Atrial septal defect

A 5-year-old boy comes to the ED with spots on the abdomen. His mother reports he has had a fever for a week. Physical exam reveals conjunctivitis, mucositis, and edema of the hands and feet (PIC 4). Which of the following is the most likely diagnosis?
A. Polyarteritis nodosa
B. Granulomatosis with polyangiitis
C. Kawasaki disease
D. Churg-Strauss syndrome
A 55-year-old male with history of HTN, diabetes, hyperlipidemia, smoking, peripheral vascular disease s/p vascular bypass presents to your clinic complaining of fatigue and substernal chest discomfort for the last few weeks. He describes the chest pain as a band-like squeezing sensation that gradually comes on with exertion and is relieved with rest. On occasions the discomfort radiates down his left arm with crushing chest discomfort. The chest pain does not change with position or respiration. He came in today because the pain has not gone away for hours. What do you suspect?
A. Typical angina
B. Prinzmetal's angina
C. Atypical angina
D. A myocardial infarction
A 2-week-old girl is found to have a harsh murmur along the left sternal border. The parents report that the baby gets “bluish” when she cries or drinks from her bottle. Echocardiogram reveals a congenital heart defect associated with pulmonary stenosis, ventricular septal defect, dextroposition of the aorta, and right ventricular hypertrophy. What is the appropriate diagnosis?
A. Atrial septal defect
B. Coarctation of aorta, postductal
C. Coarctation of aorta, preductal
D. Tetralogy of Fallot
E. Truncus arteriosus
The following are features of right sided heart failure EXCEPT
A. Ascites
B. Cardiac cirrhosis
C. Peripheral oedema
D. Pulmonary Edema
E. Jugular vein distension
A 24-year-old man was found to have a ventricular septal defect upon echocardiogram. Which of the following is true of ventricular septal defect:
A. Usually produces a right-to-left shunt of blood
B. Produces respiratory depression
C. May be of a membranous or muscular location
D. Is the least common congenital cardiac abnormality
A 67-year-old man presents to the GP with breathlessness upon exertion, orthopnea and oedema of legs, feet and ankles. Which of the following of heart failure is true?
A. Is when the heart is unable to maintain cardiac output or can do so only by increasing filling pressure
B. Right-sided heart failure is more common than leftsided failure
C. Left-sided heart failure may commonly develop as a result of right-sided failure
D. Is not a complication of myocardial infarction
Pulmonary hypertension that results from the reversal of the direction of blood flow through a congenital heart defect that initially had produced a left-to-right shunt is a characteristic feature of which of the following disorders?
A. Chagas disease
B. Eisenmenger syndrome
C. Libman-Sach disease
D. Lutembacher syndrome
. A 53-year-old man presents with recurrent chest pain that has gotten progressively worse over the last several weeks. He says that approximately a year ago the pain would occasionally occur when he was mowing his yard but now the pain sometimes occurs while he is sitting in a chair at night reading a book. The pain, which is localized over the sternum, lasts much longer now than it did a few months ago. What type of angina does this individual have at present?
A. Prinzmetal angina
B. Stable angina
C. Unstable angina
A medical student working in the emergency department sees a female baby, born 2 weeks ago, who is brought in by her anxious mother. The mother tells the student that her baby seems “purple,” especially her fingers and toes, and looks extremely blue when crying. On physical examination the sleeping baby has mild cyanosis of the face and trunk, but moderate cyanosis of the extremities. What is the most common cause of cyanosis within the first few weeks of life?
A. Atrial septal defect
B. Patent ductus arteriosus
C. Tetralogy of Fallot
D. Ventricular septal defect
An 11-month-old girl is noted to have blue lips and some fatigue after running around the room for 4 minutes. She was the product of a normal delivery. The family recently immigrated from Mexico, and she has not been evaluated by a doctor. Which of the following is the most likely diagnosis?
A. Tetralogy of Fallot
B. Atrial septal defect
C. Ventricular septal defect
Which of the following type of infection, precedes by several weeks, the development of acute rheumatic fever?
A. Streptococcus pyogenes infection of the skin
B. Treponema pallidum infection of the abdominal aorta
C. Staphylococcus aureus infection of the lungs
D. Group A β-hemolytic Streptococcal infection of the pharynx
A 72-year-old man complains of the sudden onset of headache, blurred vision, and tenderness and severe throbbing pain over his left temple region. He also has experienced flu-like symptoms and joint stiffness over the last week. He previously had been in good health. The physical examination reveals tenderness and induration of the left temporal region
A. Temporal arteritis
B. Polyarteritis Nodosa
C. Kawasaki Disease
D. Takayasu Arteritis
A 56-year-old man experiences episodes of severe substernal chest pain every time he performs a task that requires moderate exercise. The episodes have become more frequent and severe over the past year, but they can be relieved by sublingual nitroglycerin. On physical examination, he is afebrile, his pulse is 78/min and regular, and there are no murmurs or gallops. Laboratory studies show creatinine, 1.1 mg/dL; glucose, 130 mg/dL; and total serum cholesterol, 223 mg/ dL. Which of the following cardiac lesions is most likely to be present in this man?
A. Coronary atherosclerosis
B. Restrictive cardiomyopathy
C. Rheumatic mitral stenosis
D. Serous pericarditis
A 19-year-old man has had a low-grade fever for 3 weeks. On physical examination, his temperature is 38.3° C, pulse is 104/min, respirations are 28/min, and blood pressure is 95/60 mm Hg. A tender spleen tip is palpable. There are splinter hemorrhages under the fingernails and tender hemorrhagic nodules on the palms and soles. A heart murmur is heard on auscultation. Which of the following infectious agents is most likely to be cultured from this patient's blood?
A. Mycobacterium tuberculosis
B. Viridans streptococci
C. Trypanosoma cruzi
D. Candida albicans
A 50-year-old man has sudden onset of severe substernal chest pain that radiates to the neck. On physical examination, he is afebrile, but has tachycardia, hyperventilation, and hypotension. No cardiac murmurs are heard on auscultation. Emergent coronary angiography shows a thrombotic occlusion of the left circumflex artery and areas of 50% to 70% narrowing in the proximal circumflex and anterior descending arteries. Which of the following complications of this disease is most likely to occur within 1 hour of these events?
A. Myocardial rupture
B. Pericarditis
C. Ventricular fibrillation
D. Thromboembolism
A 68-year-old man has had progressive dyspnea for the past year. On physical examination, extensive rales are heard in all lung fields. An echocardiogram shows that the left ventricular wall is markedly hypertrophied. A chest radiograph shows pulmonary edema and a prominent left-sided heart shadow. Which of the following conditions has most likely produced these findings? (
A. Centrilobular emphysema
B. Systemic hypertension
C. Tricuspid valve regurgitation
D. Chronic alcoholism
A 9-year-old girl is diagnosed with acute rheumatic fever. Instead of recovering as expected, her condition worsens, and she dies. Which of the following is the most likely cause of death?
A. Central nervous system involvement
B. Endocarditis
C. Myocarditis
D. Streptococcal sepsis
Glanzmann thrombasthenia is a deficiency of?
A. vWF
B. Factor IX
C. GpIIb
D. GpIIb-IIIa complex
Hemolysis and Vaso-occlusive crisis are common in this form of anemia caused by mutation of glutamic acid to valine at amino acid 6 of beta chain.
A. Thalassemia
B. Hemoglobin C
C. Sickle cell anemia
D. Hereditary spherocytosis
E. G6PD Deficiency
Which of the following laboratory findings will you expect in patients with hemophilia A?
A. Prolonged prothrombin time
B. Prolonhged partial thromboplastin time
C. Decreased platelet count
D. Prolonged bleeding time
E. Both A and D
The presence of Heinz bodies and bite cells in a patient having hemolytic anemia strongly suggests:
A. Sickle cell anemia
B. G6PD deficiency
C. Alpha thalassemia
D. Multiple myeloma
E. Hereditary spherocytosis
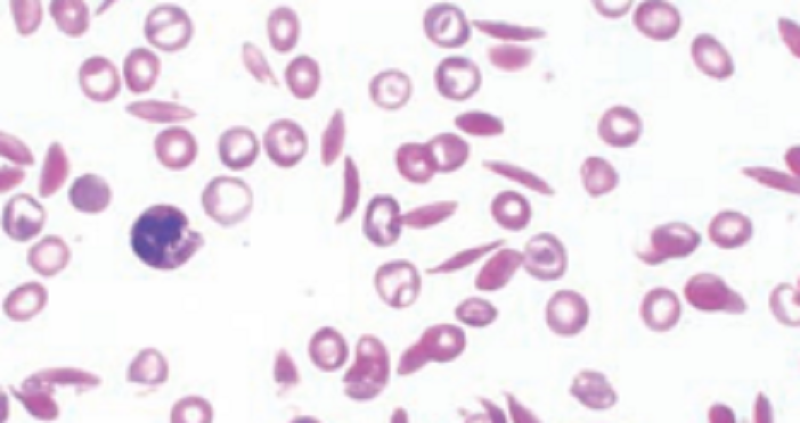
A 10-year-old black girl is brought to the emergency room. She complains of severe pain in her chest, abdomen, and bones. Physical examination reveals jaundice and anemia. Her parents state that she has been anemic since birth. A CBC shows normocytic anemia with marked poikilocytosis. A peripheral blood smear is shown in the image. Hemoglobin electrophoresis demonstrates hemoglobin S. This child’s chest and bone pain is most likely caused by which of the following mechanisms?
A. Amyloidosis
B. Coagulopathy
C. Infection
D. Ischemia
E. Vasculitis
You suspect Glucose 6-phosphate Dehydrogenase Deficiency, and microscopic analysis of the child's blood showing
A. Target Cells
B. Tear drop erthyrocytes
C. Heinz bodies in red blood cells
D. Howell-Jolly bodies

A 40-year-old woman complains of fatigue and nausea of 3 months in duration. Physical examination reveals numerous pustules on the face, as well as splenomegaly and hepatomegaly. Laboratory studies show hemoglobin of 6.3 g/dL and platelets of 50,000/mL. A peripheral smear shows malignant cells with Auer rods (arrow). The patient develops diffuse purpura, bleeding from the gums, and laboratory features of disseminated intravascular coagulation (DIC). Which of the following is the appropriate diagnosis?
A. Acute lymphoblastic leukemia
B. Acute megakaryocytic leukemia
C. Acute promyelocytic leukemia
D. Chronic myelogenous leukemia
E. Monocytic leukemia
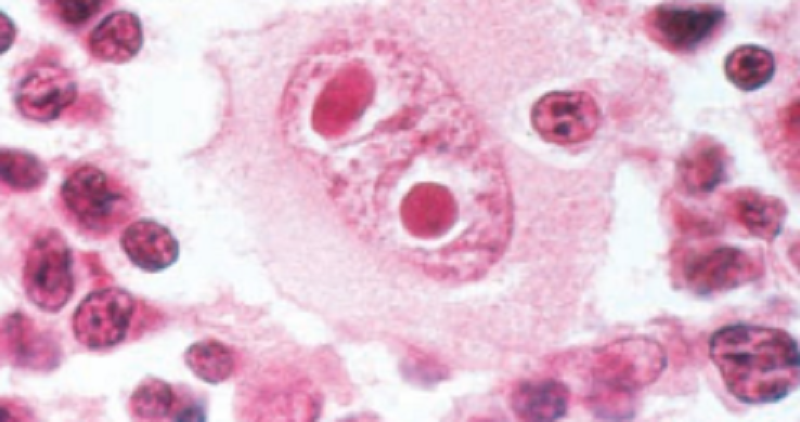
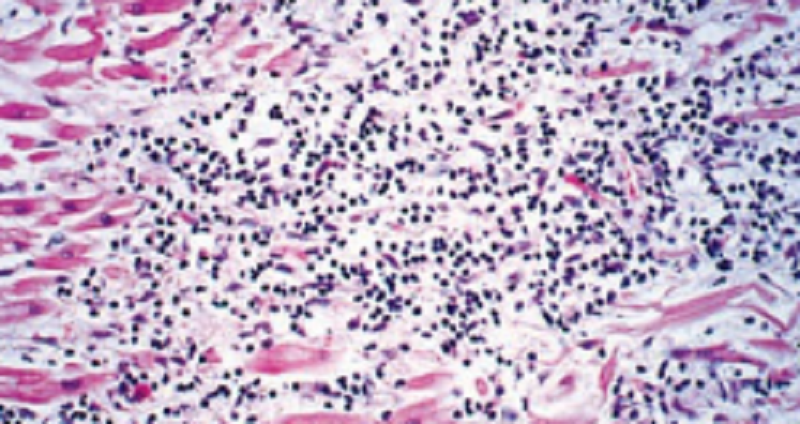
A 27-year-old man presents with an 8-week history of fevers, chills, pruritis, and night sweats. Two months ago, he experienced a flu-like illness. A nagging cough with occasional hemoptysis persisted for several weeks following resolution of his other symptoms. Physical examination reveals moderately enlarged, firm, nontender lymph nodes located in the right supraclavicular region. A lymph node biopsy is shown in the image. What is the appropriate diagnosis?
A. Acute myelogenous leukemia
B. Burkitt lymphoma
C. Hodgkin lymphoma
D. Infectious mononucleosis
E. Lymphoblastic lymphoma

A 40-year-old woman complains of fatigue and nausea of 3 months in duration. Physical examination reveals numerous pustules on the face, as well as splenomegaly and hepatomegaly. Laboratory studies show hemoglobin of 6.3 g/dL and platelets of 50,000/mL. A peripheral smear shows malignant cells with Auer rods (arrow). The patient develops diffuse purpura, bleeding from the gums, and laboratory features of disseminated intravascular coagulation (DIC). Cytogenetic studies in malignant cells from the patient described in Question 30 demonstrate a chromosomal translocation. Which of the following genes is most likely found at the translocation site?
A. bcl-1
B. bcl-2
C. myc
D. Retinoic acid receptor
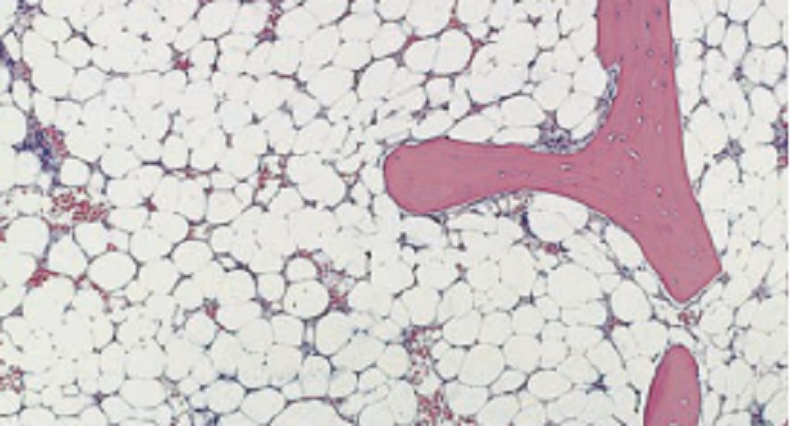
A 32-year-old man presents with mild fever and increasing fatigue. He is an immigrant from Russia and worked in a benzene factory. Physical examination does not reveal lymphadenopathy or splenomegaly, but petechial skin lesions are noted. A CBC demonstrates severe pancytopenia, with normocytic red cell indices. A bone marrow biopsy is shown in the image. Which of the following is the most likely underlying mechanism in the development of this patient’s anemia?
A. Damage to stem cells
B. Decreased erythropoietin production by the kidneys
C. Folate defi ciency
D. Impaired globin chain synthesis
The following statements are appropriate in relation to platelet disorders
C. Patients with von Willebrand disease will have prolonged bleeding time
D. Patients with Glanzmann’s thrombasthenia will have a normal platelet count
A. Patients with von Willebrand disease characteristically have a prolonged bleeding time and a prolonged activated partial thromboplastin time
B. Bernard–Soulier syndrome is caused by impaired platelet aggregation from genetic deficiency of GpIIIB/IIIa
13-Thalassemia
A. May involve an asymptomatic carrier state, with no demonstrable red cell abnormalities.
B. Results in marked peripheral haemolysis requiring transfusion in the most severe cases.
C. Is a major cause of hydrops foetalis and foetal death.
D. May result in iron overload and haemochromatosis.
The laboratory findings observed in hereditary spherocytosis is
A. Increased MCV
B. Decreased MCHC
C. Decreased erythropoiesis
D. Increased osmotic fragility
The feature indicative of extravascular red cell destruction is
A. Hemoglobinemia
B. Decreased haptoglobin
C. Splenomegaly
D. Hemoglobinuria
A 21-year-old college student presents with complaints of heavy menstrual bleeding throughout her life, frequent epistaxis, and an odd rash on her lower extremities after taking aspirin. Upon chart review, you note in the family history that the patient’s mother required blood transfusions with her pregnancy. CBC shows prolonged bleeding time and prolonged PPT, Which do you suspect?
A. Hemophillia
B. von Willebrand disease (vWD)
C. Glanzmann thrombasthenia (GT)
D. Bernard-Soulier syndrome (BSS)
The hematological disorder benefited by splenectomy is
A. Thalassemia
B. Hereditary spherocytosis
C. Sickle cell anemia
D. Pernicious anemia
The most common cause of secondary hypertension is:
A. Pregnancy
B. Renal disease
C. Stress
D. Coarctation of the aorta
E. Pheochromocytoma
A 26-year-old woman presents to her primary care physician complaining of 1 year of heavy menses. On physical examination there are several red pinpoint macules on the buccal mucosa and there are ecchymoses on the extremities. Platelet count is 18,000/μL. CBC shows isolated thrombocytopenia, increased number of egakaryocytes, PT/INR, PTT, fibrinogen are all normal. Bleeding time is prolonged. Which of the following is the most likely diagnosis? (
A. Heparin-induced thrombocytopenia (HIT)
B. Immune thrombocytopenic purpura (ITP)
C. Hemophillia
D. von Willebrand disease (vWD)
A 4-year-old male is evaluated for frequent epistaxis and mucous membrane bleeding. Physical examination shows diffuse petechiae on the patient’s distal extremities. Peripheral blood smear shows an absence of platelet clumping. An ELISA binding assay reveals that platelet surfaces are deficient in GIIb/IIIa receptors. Serum platelet count is normal. Which of the following is the most likely diagnosis?
A. Hemophilia A
B. Thrombotic thrombocytopenic purpura
C. Bernard-Soulier disease
D. Glanzmann’s thrombasthenia
Which of the following appear in the red cells of syndrome/asplenic individuals?
A. Macroovalocytes
B. Basophilic stippling
C. Howell-Jolly bodies
D. Target cells
An 8-year-old boy presents to the pediatrician with yellow eyes, pale skin, and dark urine. His mother states that he began having upper respiratory symptoms 2 days ago. She also states that her brother has similar episodes when he gets a cold. CBC is notable for normocytic anemia, elevated bilirubin, and negative fluorescent spot test. Peripheral blood smear reveals Heinz bodies and bite cells. Which of the following is the most likely diagnosis?
A. Glucose-6 phosphate dehydrogenase deficiency
B. Myelopathic anemia
C. Megaloblastic anemia
D. Iron deficiency anemia
What does it mean if you have schistocytes in the peripheral blood?
A. Hemolytic anemia due to hypersplenism
B. Hemolysis is due to immune complex mediated red blood cell injury
C. Hemolysis is due to mechanical trauma
D. Most common cause of hemolysis is due to extravascular erythrocyte degradation
A 40-year-old female is referred to medical assessment unit by her physician for querying thrombotic thrombocytopenic purpura (TTP) after she presented with a temperature of 38.9ºC. Her subsequent urea and electrolytes showed deteriorating renal function with a creatinine 3 times greater than her baseline. What is the underlying pathophysiology of TTP?
A. Autoimmune destruction of red blood cells
B. Failure to cleave von Willebrand factor normally
C. Anti-bodies against von Willebrand factor
D. Autoimmune destruction of platelets
A patient with severe anemia has a peripheral blood smear with oval macrocytes, hypersegmented neutrophils, and decreased platelets. The most likely cause of the anemia is
A. A red cell membrane protein defect.
B. An amino acid substitution in the β-globin chain.
C. Iron deficiency.
D. vitamin B12 or folate deficiency.
Is the likely diagnosis in a 50-year-old male who presents with worsening back pain and persistent tiredness. Bone imaging show lytic bone lesions and serum electrophoresis reveals an intense gammaglobulin band
A. Multiple Myeloma
B. Hodgkin’s disease
C. Chronic myeloid leukaemia
D. Thalassaemia
A 39-year-old woman who presented with increasing fatigue and muscle weakness is found have a microcytic and hypochromic anemia. Which of the following is the most likely cause of her anemia?
A. Folate deficiency
B. Iron deficiency
C. Vitamin B12 deficiency
D. Vitamin C deficiency
A 36-year-old woman presents with muscle pain, fever, and chronic sinusitis. Physical examination finds mucosal ulcerations of the nasopharynx and signs of renal disease. A biopsy from her nasopharynx reveals a necrotizing vasculitis with chronic inflammatory cells and giant cells surrounding localized necrotic areas. The presence of which of the types of autoantibodies listed below would be most consistent with a diagnosis of Wegener granulomatosis?
A. Antigliadin antibodies
B. Antimitochondrial antibodies
C. Antineutrophil cytoplasmic antibodies
D. Antismooth muscle antibodies
Which is not true regarding Bernard Soulier syndrome
A. Deficiency of GPIb receptor for vWF causes impaired platelet adhesion
B. Affects males and females equally
C. Inherited deficiency of GpIIb-IIIa results in a bleeding disorder called Bernard Soulier syndrome
D. Bernard soulier syndrome is Autosomal recessive platelet disorder
Which of the following autoantibodies is most likely to be present in a patient with pernicious anemia?
A. Anticentromere antibodies
B. Anti-intrinsic factor antibodies
C. Antimitochondrial antibodies
D. Anti-smooth muscle antibodies
A 7-year-old African-American boy is brought to see his pediatrician. His father says he has noticed that the boy has been complaining of right knee pain for the past week. On physical exam, multiple ecchymoses are noted on both upper and lower extremities. His father claims that the boy has always bruised easily, and he has recently learned how to ride a bicycle. Which of the following elements of the coagulation cascade is most likely to be missing in this child?
A. Antithrombin III
B. Factor VII
C. Factor VIII
D. Protein C
A 72-year-old man who has recently had an aortic valve replacement now presents with pallor and fatigue. The red blood cell count is decreased, and schistocytes are reported on examination of a peripheral blood smear. In addition, his indirect (unconjugated) bilirubin is significantly elevated. The cause of the anemia is likely
A. Cold agglutinin disease.
B. Hereditary spherocytosis.
C. Mechanical disruption of red cells.
D. Paroxysmal nocturnal hemoglobinuria
A 12-year-old girl has the sudden onset of severe abdominal pain and back pain. On physical examination her abdomen is diffusely tender, but there are no masses. She is afebrile. A CBC shows Hgb 6.5 g/dL, Hct 19.0%, MCV 99 fL, platelet count 149,000/microliter, and WBC count 11,200/microliter. Examination of her peripheral blood smear shows nucleated RBCs and sickled RBCs. Which of the following types of gene mutation is she most likely to have?
A. Deletion
B. Duplication
C. Insertion
D. Missense
E. Nonsense
A 65-year-old female was brought to the physician due to jaw claudication and headaches lasting approximately a month. Laboratory shows markedly elevated ESR. Which of the following is the most likely diagnosis?
A. Blindness
B. Intermittent claudication
C. Necrosis of the index finger
D. Coronary artery aneurysm
A 76-year-old woman notices that small, pinpoint-to-blotchy areas of superficial hemorrhage have appeared on her gums and on the skin of her arms and legs over the past 3 weeks. On physical examination, she is afebrile and has no organomegaly. Laboratory studies show a normal prothrombin time and partial thromboplastin time. CBC shows hemoglobin of 12.7 g/dL, hematocrit of 37.2%, MCV of 80 μm3, platelet count of 276,000/mm3, and WBC count of 5600/mm3. Platelet function studies and fibrinogen level are normal, and no fibrin split products are detectable. Which of the following conditions best explains these findings?
A. Macronodular cirrhosis
B. Meningococcemia
C. Vitamin C deficiency
D. Metastatic carcinoma
A 23-year-old African-American man with a history since early childhood of severe anemia requiring many transfusions has nonhealing leg ulcers and recurrent periods of abdominal and chest pain. These signs and symptoms are most likely to be associated with which of the following laboratory abnormalities?
A. Decreased erythropoietin
B. Increased erythrocyte osmotic fragility
C. Sickle cells on peripheral blood smear
D. Teardrop-shaped cells
A 31-year-old male complains of such difficulty in chewing that he no longer buys gum. He also describes diplopia when reading or watching television for long periods. He has no extremity weakness. He has no other medical problems and takes no medication. He does not use tobacco, alcohol or illicit drugs. This patient's condition is most likely associated with which of the following neoplastic processes?
A. Lung cancer
B. Hodgkin lymphoma
C. Adrenal tumor
D. Thymoma
An 18-year-old man complains of shortness of breath. Radiograph demonstrates a large mediastinal mass. Biopsy of the mass shows a mixed inflammatory infiltrate with occasional larger cells having two nuclear lobes and prominent eosinophilic nucleoli. What is the diagnosis?
A. Precursor T-cell acute lymphoblastic leukemia/lymphoma (pre-T ALL)
B. Nodular lymphocyte predominant Hodgkin lymphoma
C. Classic Hodgkin lymphoma
D. Thymoma
E. Diffuse large B-cell lymphoma
A 45 year old woman presents with recurrent infections and on PE was found to have marked splenomegaly. Her leukocyte count is increased to 300,000. The differential count reveals the presence of myeloblasts and promyelocytes, with predominance of myelocytes, metamyelocytes, bands and segmented neutrophils. Basophils are also increased in number. The patient is not anemic. Leukocyte alkaline phosphatase is decreased. Which of the following describes a major characteristic of this disorder?
A. 9:22 translocation
B. Expansion of mature B lymphocytes within multiple lymph nodes
C. Hypogammaglobulinemia
D. Neoplastic cells exhibiting hair-like filamentous projections
E. Peak incidence occurs at 65 years
A bone marrow aspirate was obtained from a 70-year-old man whose symptoms included weakness, weight loss, and recurrent infection. Laboratory finding included proteinuria, anemia, and an abnormal component in serum proteins. A photomicrograph of the bone marrow aspirate is shown below. The most probable diagnosis is
A. Monocytic leukemia
B. Non-Hodgkin lymphoma
C. Multiple myeloma
D. Myelomonocytic leukemia
Cold agglutinin disease is a form of autoimmune hemolytic anemia caused by cold-reacting autoantibodies. Autoantibodies bind to the erythrocyte membrane leading to premature erythrocyte destruction. Which antibody is commonly involved?
A. IgM
B. IgG
C. IgA
D. IgD
E. IgE
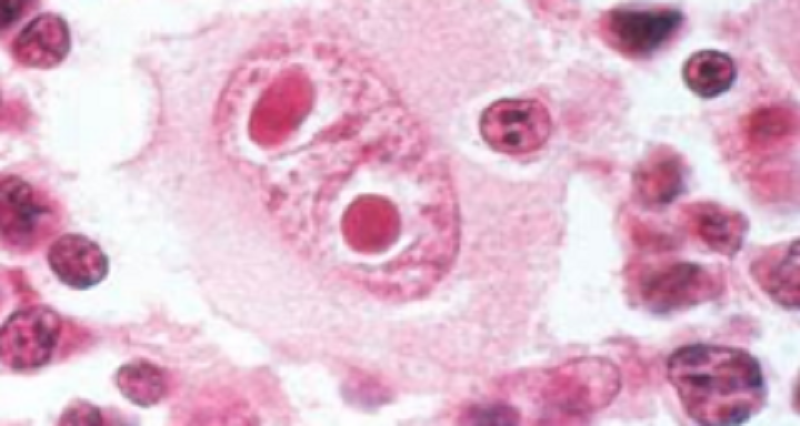
A 27-year-old man presents with an 8-week history of fevers, chills, pruritis, and night sweats. Two months ago, he experienced a flu-like illness. A nagging cough with occasional hemoptysis persisted for several weeks following resolution of his other symptoms. Physical examination reveals moderately enlarged, firm, nontender lymph nodes located in the right supraclavicular region. A lymph node biopsy is shown in the image. What is the appropriate diagnosis?
A. Acute myelogenous leukemia
B. Burkitt lymphoma
C. Hodgkin lymphoma
D. Infectious mononucleosis
E. Lymphoblastic lymphoma
Chromosome translocations are important in diagnosing and prognosticating certain types of cancers. Which of the following may be seen in Burkitt's lymphoma?
A. t9:22
B. T8:14
C. T14:18
D. T11:14
E. T15:17
A 70-year-old man presents with severe bone pain and frequent respiratory infections. Serum protein electrophoresis demonstrates an M protein spike in the gamma region. Radiographs of the skull, long bones, and spine demonstrate multiple “punchedout” lesions, and bone marrow aspiration demonstrates large numbers of neoplastic plasma cells. Which of the following statements is true of this disorder?
B. Renal insufficiency is a common cause of death.
C. The M spike is most often an IgM.
D. The M spike is most often polyclonal in nature.
E. This disorder is the most common T-cell neoplasm
A. Although this patient presents at 70 years of age, the average age of presentation is 50 years of age.
Hyperviscosity syndrome often is seen in
A. Waldenstrom's macroglobulinemia
B. Multiple myeloma
C. Hodgkin's lymphoma
D. Acute promyelocytic leukemia
Hyperviscosity syndrome often is seen in
E. Waldenstrom's macroglobulinemia
F. Multiple myeloma
G. Hodgkin's lymphoma
H. Acute promyelocytic leukemia
Over-expression of BCL-2 proteins occurs in
A. Burkitt’s lymphoma
B. Follicular lymphoma
C. Diffuse large B-cell lymphoma
D. Small lymphocytic lymphoma
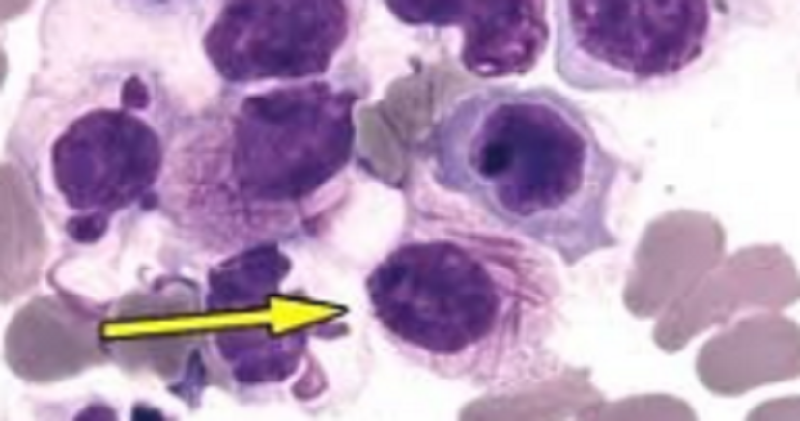
A patient with the condition shown in the image (PIC 5) would most likely have which of the following?
A. Chronic myeloid leukemia
B. Acute myeloid leukemia
C. Chronic promyelocytic leukemia
D. Acute promyelocytic leukemia

A child presented with a maxillary mass (PIC 8) which on further investigation showed the presence of “starry sky appearance” in the biopsy. The likely diagnosis of this condition is:
A. Marginal zone lymphoma
B. Mantle cell lymphoma
C. Burkitt lymphoma
D. Hodgkin lymphoma

Smudge cells" (PIC 7) in the peripheral smear are characteristics of:
A. Chronic lymphocytic leukemia
B. Chronic myelogenous leukemia
C. Acute lymphocytic leukemia
D. Acute myelogenous leukemia
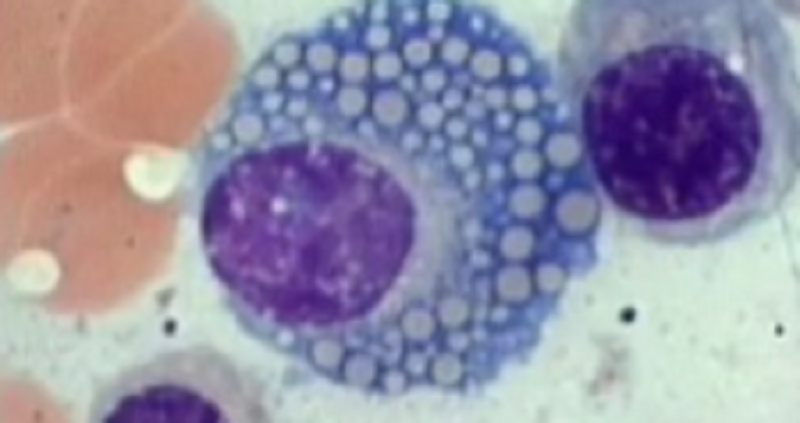
Identify the cell with arrow head (PIC 1)
A. Fungal bodies
B. Histoplasma inclusion
C. Gaucher Cell
D. Mott cell
The morphological type of leukemia which may show Auer rods is
A. Chronic lymphoid leukemia
B. Acute Myeloid Leukemia
C. Chronic myeloid leukemia
D. Acute lymphoblastic leukemia
A 12-year-old boy is taken to the physician because he has had increasing abdominal distention and pain for the past 3 days. Physical examination shows lower abdominal tenderness, and the abdomen is tympanitic with reduced bowel sounds. An abdominal CT scan shows a 7-cm mass involving the region of the ileocecal valve. Surgery is performed to remove the mass. Histologic examination of the mass shows sheets of intermediate-sized lymphoid cells, with nuclei having coarse chromatin, several nucleoli, and many mitoses. A bone marrow biopsy sample is negative for this cell population. Cytogenetic analysis of the cells from the mass shows a t(8;14) karyotype. Flow cytometric analysis reveals 40% of the cells are in S phase. The tumor shrinks dramatically in size after a course of chemotherapy. Which of the following is the most likely diagnosis?
A. Diffuse large B-cell lymphoma
B. Follicular lymphoma
C. Acute lymphoblastic leukemia
D. Burkitt lymphoma
A 9-year-old boy living in Uganda has had increasing pain and swelling on the right side of his face over the past 8 months. On physical examination, there is a large, nontender mass involving the mandible, which deforms the right side of his face. There is no lymphadenopathy and no splenomegaly, and he is afebrile. A biopsy of the mass is performed. Microscopically, the specimen is composed of intermediate-sized lymphocytes with a high mitotic rate. A chromosome analysis shows a 46,XY,t(8;14) karyotype in these cells. The hemoglobin concentration is 13.2 g/dL, platelet count is 272,000/mm3, and WBC count is 5820/mm3. Infection with which of the following is most likely to be causally related to the development of these findings?
A. Cytomegalovirus
B. Epstein-Barr virus
C. Human papillomavirus
D. Respiratory syncytial virus
A 58-year-old man from Nagasaki, Japan, has noted an increasing number of skin lesions for the past 8 months. On examination, there are scaling red-brown patches on all skin surfaces. He also has generalized lymphadenopathy and hepatosplenomegaly. Laboratory studies show hemoglobin, 9.7 g/dL; hematocrit, 31%; MCV, 89 μm3; platelet count, 177,000/mm3; and WBC count, 18,940/mm3 with differential count of 35 segmented neutrophils, 2 band neutrophils, 58 lymphocytes, and 5 monocytes. His serum calcium is 11.5 mg/dL. Examination of his peripheral blood smear shows multilobated “cloverleaf” cells. Despite aggressive chemotherapy, his condition worsens with development of paresthesias along with erythematous plaques and red-brown nodules on his skin. Which of the following infectious agents most likely caused his illness? (
A. Cytomegalovirus
B. Epstein-Barr virus (EBV)
C. HTLV-1
D. Rochalimaea henselae
Is a disorder in which the Philadelphia chromosome abnormality is defected within affected cells
A. Chronic lymphocytic leukaemia
B. Hodgkin’s disease
C. Chronic myeloid leukaemia
D. Acute myeloid leukaemia
E. Megaloblastic anaemia
A 43-year-old with a history of Hodgkin lymphoma presents with increasing shortness of breath. A chest x-ray reveals a right-sided pleural effusion. The pleural fluid is tapped, and laboratory examination reveals a milky white pleural fluid that is composed of finely emulsified fats. Which one of the listed terms BEST describes this pleural fluid?
A. Pnemothorax
B. Empyema
C. Chylothorax
D. Hydrothorax
E. Pneumothorax
This refers to the ratio of thickness of the mucous gland layer in the airways to that of the wall between the epithelial lining and the cartilage. It is utilized to assess chronic bronchitis:
A. Reid index
B. De Ritis ratio
C. Gleason score
D. Air passage
Pneumoconiosis refers to nonneoplastic lung reaction to inhalation of mineral dusts encountered in the work place. Which pneumoconiosis is characterized by discrete pale to blackened nodules in the upper zones of the lungs. Radiographically it presents as eggshell calcifications. This disease may be progressive even if patient is no longer exposed and it has also been associated with increased susceptibility to PTB.
A. Coal workers' pneumoconiosis
B. Silicosis
C. Asbestosis
D. Byssinosis
E. Sarcoidosis
A 65-year-old man comes to the office due to worsening exertional dyspnea over the past 3 months. Temperature is 36.7 C (98.1 F), pulse is 76/min, and respirations are 18/min. On physical examination, breath sounds are diffusely decreased. Chest radiography reveals flattened hemidiaphragms, increased radiolucency of the lungs, and a long, narrow heart shadow. This patient's pulmonary function testing will most likely show which of the following patterns of findings?
A. Total lung capacity ↓ Forced expiratory volume in 1 second/forced vital capacity ↑ Forced vital capacity ↓ Residual volume ↓
B. Total lung capacity ↑ Forced expiratory volume in 1 second/forced vital capacity ↓ Forced vital capacity ↓ Residual volume ↑
C. Total lung capacity ↓ Forced expiratory volume in 1 second/forced vital capacity ↓ Forced vital capacity Normal Residual volume ↑
D. Total lung capacity ↑ Forced expiratory volume in 1 second/forced vital capacity ↓ Forced vital capacity ↓ Residual volume ↓
E. Total lung capacity ↑ Forced expiratory volume in 1 second/forced vital capacity Normal Forced vital capacity ↑ Residual volume Normal
A 42 yo woman comes to the office due to several months of episodic shortness of breath and cough. The patient has a history of migraines and occasionally takes acetaminophen. She is a school teacher and does not use tobacco, alcohol, or illicit drugs. Her temperature is 36.1 C( 97 F), blood pressure is 110/80 and pulse is 84/min. Pulse ox show 96 % on room air. Lung examination and chest x-ray are normal. Spirometry shows FEV1 is 71% of the predicted value. Sputum analysis shows predominant eosinophils. This patient's symptoms are most likely related to exposure to which of the following?
A. gliadin-containing grains
B. Acetaminophen
C. Thermophilic actinomycetes
D. Histoplasma microconidia
E. House dust mites
F. Shellfish and other seafood
50 year old male chronic smoker presents with chronic cough dyspnea and sputum production. He also has bouts of easy fatigability. Patient also presents with increased anteroposterior diameter of the chest wall. Patient most likely has this type of emphysema
A. Panacinar
B. Centrilobular
C. Paraseptal
D. Alveolar
A 72-year-old man who works for a mine in Libby,Montana, has a clinical history of pulmonary function tests that show a decreased FEV1 and FVC, with a normal FEV1/FVC ratio. He dies and an autopsy is performed. The autopsy reveals a tumor in the right pleural cavity, which completely encases the lung. He also has tan-white pleural plaques in the right pleural cavity. Upon histologic examination of the lung, prominent alveolar septal fibrosis with honeycomb change is identified. This patient was most likely exposed to which of the following agents? (M2)
A. Cigarette smoke
B. Beryllium
C. Coal
D. Asbestos
Which of the following types of vasculitis is highly associated with cANCA or the antibodies against proteinase-3?
A. PAN
B. Takayasu arteritis
C. Wegener Granulomatosis
D. Microscopic polyangiitis
E. Churg-Strauss syndrome
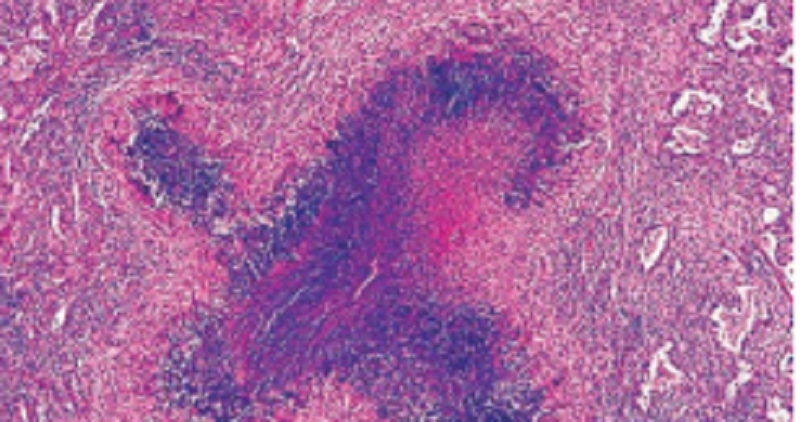
A 23-year-old man complains of nasal obstruction, serosanguinous discharge, cough, and bloody sputum. A chest X-ray shows cavitated lesions and multiple nodules over both lung fi elds. A CT scan discloses obliteration of several maxillary sinuses. Urinalysis reveals hematuria and RBC casts. Laboratory studies demonstrate anemia and elevated serum levels of C-ANCA. An open-lung biopsy is shown in the image. Which of the following is the most likely diagnosis?
A. Adenocarcinoma of lung
B. Churg-Strauss syndrome
C. Necrotizing sarcoid granulomatosis
D. Tuberculosis
E. Wegener granulomatosis
A 63-year-old man presents to your office complaining of worsening shortness of breath over the past year. You know that this patient has smoked two packs of cigarettes a day for the past 45 years. As you are talking to the patient, you notice that he is using his accessory muscles of respiration to breathe, that his chest is barrel shaped and that he is breathing carefully through pursed lips. Using a spirometer, you determine that he has a decreased FEV1/FVC ratio and an increased TLC. You tell the patient that it is imperative that he stop smoking and prescribe him a tiotropium inhaler.
Emphysema
Emphysema
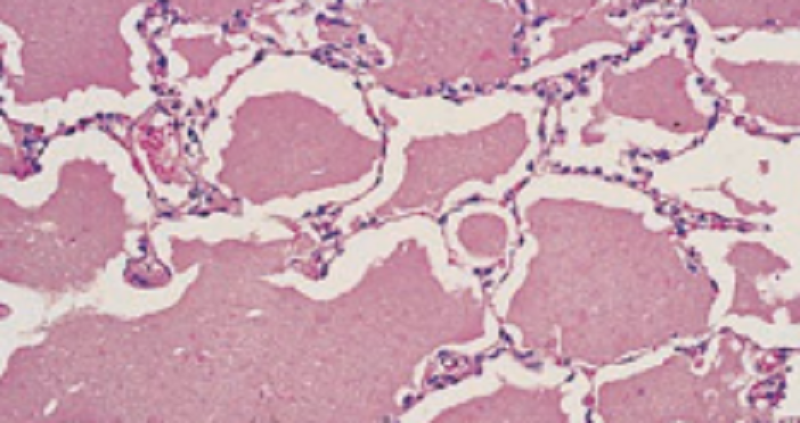
A 22-year-old man who is being treated for leukemia complains of shortness of breath on exertion, pleuritic chest pain, and a low-grade fever. Physical examination reveals crackles in both lung bases and clubbing of the fi ngers. Bronchoalveolar lavage demonstrates PASpositive material and elevated levels of surfactant proteins. An open-lung biopsy is shown in the image. Which of the following is the most likely diagnosis?
A. Alveolar proteinosis
B. Eosinophilic pneumonia
C. Goodpasture syndrome
D. Hyaline membrane disease
E. Radiation pneumonitis
A 10-year-old boy dies following a severe episode of status asthmaticus. Histologic examination of the lung at autopsy is shown in the image. Which of the following best describes the pathologic features evident in this autopsy specimen?
A. Destruction of the walls of airspaces without fibrosis
B. Hyaline membranes and interstitial edema
C. Interstitial fibrosis of the lung parenchyma
D. Intra-alveolar hemorrhage and exudates containing neutrophils
E. Smooth muscle hyperplasia and basement membrane thickening
A 34-year-old female was brought to the physician. The patient has sinusitis, cough, skin nodules, significant purpura also noted on the extremities as well as carpal tunnel syndrome. The patient's CBC shows eosinophilia. Pulmonary function tests show an obstructive pattern improved with beta-agonist and diagnosis of asthma was made. Which of the following is correct about her condition?
1- Patient is positive to anti ds DNA antibodies
2- Patient has inflammation of the aortic arch
3- Patient has elevated IgE levels
4- Her condition is inherited as autosomal dominant pattern
5- She has vasculitis associated with hepatitis C infection
Which of the following anemia profiles is typical of thalassemia?
1- ↓ MCV, ↓ plasma iron, ↓ ferritin, ↓ total iron binding capacity (TIBC)
2- ↓ MCV, ↓ ferritin, ↑ plasma iron, normal TIBC
3- ↑ MCV, normal ferritin, normal plasma iron, normal TIBC
4- ↓ MCV, normal ferritin, normal plasma iron, normal TIBC
Reed-Sternberg (RS )CD15 +and CD30+ seen in which of the following blood cell neoplasia?
1- Chronic myelogenous leukemia(CML )
2- Chronic lymphoblastic leukemia (CLL)
3- Hodgkin lymphoma (HL)
4- Non-Hodgkin lymphoma (NHL)
Which of the following is the BEST explanation of polycythemia?
1- An illegal way that professional athletes get a competitive edge
2- A blood disorder in which there are too many red blood cells
3- A blood disorder in which the red blood cells are lacking in enzymes
4- Ableeding disorder in which a person is missing important clotting factors.
A previously healthy 67-year-old man presents to the emergency room with numbness of his left leg. Temperature and blood pressure are normal. Physical examination shows pallor and a cool left leg with absence of distal pulse. An ECG reveals no abnormalities. An arteriogram demonstrates a markedly dilated abdominal aorta and occlusion of the left popliteal artery. The blockage is removed surgically, and the patient recovers. Which of the following is the most likely source of the arterial thromboembolus in this patient?
1- Deep venous thrombosis
2- Left ventricular mural thrombus
3- Nonbacterial endocarditis
4- Paradoxical emboli
5- Thrombus from an atheromatous aorta
80 year old patient, previously healthy woman feels a lump in her right breast. The physician palpates a 2.5-cm firm mass in the upper outer quadrant. Nontender right axillary lymphadenopathy is present. A lumpectomy with axillary lymph node dissection is performed. Microscopic examination shows that the mass is an infiltrating ductal carcinoma. Three of 10 axillary nodes contain metastases. Flow cytometry on the carcinoma cells shows a small aneuploid peak and high S-phase. Immunohistochemical tests show that the tumor cells are positive for estrogen and progesterone receptor (ER/PR), negative for HER2/neu expression, and positive for cathepsin D expression. What is the most important prognostic factor for this patient?"
1- Lack of HER2/neu expression in the carcinoma
2- Histologic subtype of carcinoma
3- Expression of stromal proteases in the carcinoma
4- Presence of lymph node metastases
5- Age at diagnosis
6- DNA content in the carcinoma
7- Estrogen receptor positivity
The osmotic fragility diagnostic test is used in which of the following anemias?
A. B12 deficiency anemia
B. Hereditary spherocytosis
C. Iron deficiency anemia
D. Aplastic anemia
E. Anemia chronic disease(ACD)
- A 45-year-old man has had a fever and a productive cough for the past 3 days. On physical examination there is dullness to percussion over the right upper lung. His temperature is 37.9°C. A chest radiograph reveals right upper lobe consolidation. Laboratory findings include serum total protein of 6.0 g/dL, albumin 2.7 g/dL, AST 185 U/L, ALT 98 U/L, total bilirubin 1.0 mg/dL, alkaline phosphatase 31 U/L, and prothrombin time 20 sec. An abdominal CT scan shows hepatomegaly with decreased hepatic attenuation. Which of the following conditions is the most likely underlying cause of death?
1- Alpha-1-antitrypsin deficiency
2- Wilson disease
3- Acute hepatitis C
4- Diabetes mellitus
{"name":"Orthopedic Disorders Quiz", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge on orthopedic disorders with our comprehensive quiz designed for medical students, professionals, and enthusiasts alike!Challenging questions cover a wide array of topics:Osteoarthritis and its featuresBone disorders and syndromesNeoplasms of the musculoskeletal system","img":"https:/images/course1.png"}
More Quizzes
Bones, Joints and soft tissue tumors, vascular , heart
582922
Ortho Exam 3 Practice Questions
321637
Healthy quiz
1050
EVALUACIÒN DIAGNÒSTICA
1050
Test Your Popoye Knowledge: Free & Trivia
201025223
What Conditions Cause the Contractile Vacuole to Fill with Water?
201087744
Pastor Lacey: Test Your Knowledge & Answers
201049395
Horse Breed: Discover What Horse Breed You Are!
201024159
Have I Met My Soulmate - Discover Your True Match
201025223
UNESCO Heritage: Discover World Wonders Today
201052900
Monster Hunter Stories Answers - Score Big Now
201028949
Email & Memo: Master Most Email Messages and Memos!
201031001