Emergency Housemanship Assessment

Emergency Housemanship Assessment Quiz
Test your knowledge and skills with our comprehensive Emergency Housemanship Assessment Quiz tailored for healthcare professionals. This quiz covers critical topics in emergency medicine, ensuring you are well-prepared for real-life scenarios.
Key Features:
- 30 questions covering a wide range of emergency topics
- Multiple-choice format with immediate feedback
- Designed for aspiring doctors and healthcare workers
MCQ: Regarding STEMI according to Ministry of Health Clinical Practice Guideline 2019
A. Diagnosis must be made within 30 minutes of arrival to A&E Department
B. Oral aspirin 300mg must be given to patient with suspected acute coronary syndrome (ACS) in an ambulance, even before reaching a hospital.
C. Door to needle time for reperfusion therapy is 15 minutes
D. Previous IV administration of streptokinase is an absolute contraindication for thrombolytic therapy.
E. Early PCI should be considered in failed reperfusion or re-occlusion after fibrinolytic therapy.
MCQ: Regarding status epilepticus:
A. Define as seizures last for 5 or more minutes of either continuous seizures activity or repetitive seizures with no intervening recovery of consciousness.
B. Patient with seizures that last more than 5 minutes are likely to recover spontaneously
C. First line treatment is iv Diazepam 5mg up to 10mg/dose
D. 2nd line treatment is IV infusion Phenytoin 20mg/kg
E. Seizure control must take precedence over airway control
MCQ: In management of supraventricular tachycardia (SVT):
A. IV Adenosine is given as a rapid bolus due to its short half-life.
B. Vagal maneuver I.e. Carotid sinus massage can be done prior to pharmacological intervention if not contraindication.
C. IV verapamil is contraindicated
D. Synchronized DC Cardioversion is indicated in unstable SVT
E. Sign of unstable SVT include systolic blood pressure (SBP) <100 mmHg.
MCQ: Regarding drug overdose and its respective antidote, which pair(s) is/ are CORRECT?
A. Tricyclic antidepressant overdose – IV sodium bicarbonate
B. Atenolol overdose – IV glucagon
C. Midazolam overdose – IV Flumazenil
D. Paracetamol overdose – N-acetylcystine (NAC)
E. Diltiazem overdose – IV sodium bicarbonate
MCQ: You are attending to a trauma patient with multiple fractures at the Emergency Department. When treating a trauma patient, the following statement(s) is/are TRUE:
A. Femoral midshaft fracture is managed by using a non traction splint
B. Both closed and open femoral midshaft fracture may cause hypovoleamic shock.
C. A fracture dislocation of the knee may cause vascular injury to the popliteal artery
D. Heamodynamically unstable ‘open book’ pelvic fractures have a mortality rate as high as 70%.
E. Blood loss is more in a close fracture compared to the open fracture from any fracture site
MCQ: A 30-year-old male presented with history of fever for 4 days with chills and rigor. Upon further questioning, he was complaining having a diarrhea and vomiting of 5-6 times per day, retro-orbital pain and headache. He lives in dengue prone area whereby recent fogging was done. Among of the above information, which are considered as warning sign for dengue fever?
A. Chills and rigor.
B. Persistent vomiting.
C. Retro-orbital pain.
D. Persistent diarrhea.
E. Lives in dengue prone area.
MCQ: The following are clinical criteria for diagnosing Thyroid Storm
A. High grade body temperature
B. Present of 3rd degree Heart Block
C. Gastrointestinal-hepatic dysfunction
D. Heart rate <60 beat/ min.
E. Confusion
MCQ: Which statement is/ are CORRECT regarding base of skull fracture?
A. ‘Halo Sign’ is a bruising of overlying skin of the mastoid process
B. Associated with “Raccoon eye sign”.
C. Meningoencephalitis is its known complication
D. Can precipitate uncontrolled bleeding causing Disseminated Intravascular Coagulopathy (DIVC).
E. Can cause cerebrospinal fluid (CSF) rhinorrhea or otorrhea
MCQ: During the primary survey in Trauma management, the following are the life threatening conditions that must be managed immediately:
A. Airway obstruction
B. Cardiac contusion
C. Simple pneumothorax
D. Massive heamothorax
E. Flail chest
MCQ: Which of the following statement/s regarding shock is/are correct?
A. There is a relative intravascular volume depletion in hypovolemic shock.
B. Cardiogenic shock is caused by a cardiac pump failure
C. Shock index >0.5 is associated with poor prognosis
D. Urine output <1ml/kg/hr is an indicator of shock
E. In haemorrhagic shock, initial changes in haemodynamic status is reflected by a pulse pressure
OBA: To minimize transfer times and maximize neurological outcomes, the American Stroke Association has described the stroke “Chain of Survival”. Which of the following is NOT in this “Chain of Survival”?
Rapid recognition and reaction to stroke warning signs.
Rapid emergency medical service ambulance dispatch.
Pre-arrival notification to the receiving facility.
Rapid diagnosis and treatment in hospital
Aspirin is given before arrival at the hospital.
OBA: The mother of a 5-year-old boy complains that since this morning her son is noted to be drooling, preferring to sit up, and also has noisy breathing. Which of the following is the MOST likely diagnosis?
Bronchial asthma
Acute bronchiolitis
Acute epiglottitis
Interstitial lung disease
Diabetic ketoacidosis
OBA: With regards to cardiac arrest, which of the following is the most common rhythm at the onset of arrest?
Ventricular tachycardia
Rapid atrial fibrillation
Ventricular asystole
Complete heart block
Ventricular fibrillation
OBA: A thoracostomy tube was inserted into a 30-year-old male with a large pneumothorax. There was a gush of air noted with the insertion. Choose the correct acute complication following the procedure in this patient.
Hemothorax from injury to intercostal vessels
Infection of thoracostomy site
C. Mucus plugging of thoracostomy tube
D. Re-expansion pulmonary oedema
E. Tension pneumothorax
OBA: A 36-year-old woman complains of headache lasting for 3 hours. Which of the following statements is INCORRECT?
A. Meningitis can be presented even if the classical triad of fever, neck stiffness and altered mental state is not complete.
B. A change in headache pattern can be a clue to a life threatening cause.
C. Pre-eclampsia can present as acute headache.
D. Acute angle closure glaucoma can present as acute headache.
E. There is a correlation between high blood pressure and headache.
OBA: A 75-year-old man presents with acute abdominal pain lasting for 4 hours. He has a history of atrial fibrillation for 10 years. Which of the following statements is INCORRECT?
Normal abdominal examination findings rules out mesenteric ischaemia as a cause of pain.
B. The possibility of acute coronary syndrome needs to be considered.
C. A leaking abdominal aortic aneurysm can be a cause for the pain.
D. Acute appendicitis needs to be considered.
E. A perforated gastric ulcer can present this way.
OBA: A 45-year-old man construction worker sustained a blunt injury to the chest when he slipped on a slippery floor and fell onto a concrete slab. He is suspected to have a tension pneumothorax. Which of the following clinical features is NOT consistent with such a diagnosis?
A. Distended neck veins
B. Unilateral decrease chest movement
C. Shifting of tracheal contralateral to the side with decreased chest movement
D. Hypotension
E. Paradoxical chest movement.
OBA: A 35-year-old male was involves in a chain saw accident and cut his foot off. He had massive blood loss at the scene. He presents with a blood pressure of 84/60 mmHg and a heart rate of 150 beats / min. He appeared drowsy and weak. The patient is in which class of heamorrhagic shock?
Class 1 shock
Class 2 shock
Class 3 shock
Class 4 shock
Not in Shock
OBA: An 88-year-old male falls and hits his head, chest and hip. The most UNLIKELY injury for the patient to suffer is?
A. Epidural heamatoma
B. Hip fracture
C. Odontoid fracture
D. Rib fracture
E. Subdural heamatoma
OBA: A 44-year-old female involved in a downhill skiing crash with an obvious head injury is brought to ED. Her vital signs are heart rate 125 beats/ min, blood pressure 100/60 mmHg and respiratory rate 14 breath/ min. She opens her eyes to voice, is moaning and appears to withdraw from painful stimuli. What is this patient’s Glasgow Coma Scale score?
3
4
7
9
12
OBA: Which of the following may prevent secondary brain injury?
A. Hyperventilation to a PaCO2 of less than 20 mmHg
B. Maintaining PaO2 of greater than 60 mmHg
C. Permissive hyperglyceamia
D. Permissive hypotension
E. Keep patient to lie supine in bed
OBA: A construction worker is struck on the top of the head with a manhole cover that was dislodged during an explosion. The manhole cover landed directly on the top of his head. What type of cervical spine injury is this patient most likely going to have?
A. Chance fracture
B. Clay shoveler fracture
C. Dens fracture
D. Hangman fracture
E. Jefferson fracture
OBA: Which of the following side effects is more common when an opioid analgesic is administrated intravenously rather than orally?
A. Constipation
B. Gastrointestinal bleeding
C. Nausea
D. Respiratory depression
E. Vomiting
OBA: Which of the following is NOT a complication of high-voltage electric injury?
A. Blunt trauma from being hurled from the source
B. Cardiac and respiratory arrest
C. Compartment syndrome
D. Fern pattern burn
E. Tetanic contractions
OBA: A 12-year-old boy arrives by EMS due to lethargy and dehydration. Parents report that he has been tired the past few days with increase thirst and going to the bathroom a lot. You appreciate a fruity odor to his breath along with tachypnea and dehydration. Bedside glucose reads as high. Venous blood gas has pH 7.12 and HCO3 of 8. You instruct the nurse that the priority is:
A. Administer insulin subcutaneously
B. Administer sodium bicarbonate
C. Intravenous fluid therapy
D. Obtain serum ketone level
E. Portable chest x-ray
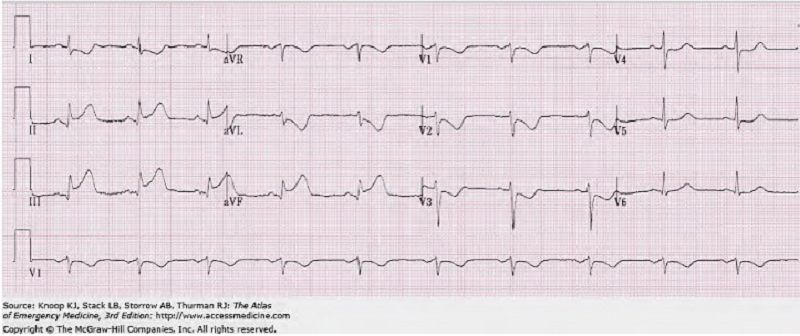
OBA: A 64-year-old woman arrives by ambulance with crushing substernal chest pain for the past 40 minutes. She received aspirin and a large bore IV en route. Several tubes of blood are available. Her past medical history includes diabetes mellitus and hypertension, controlled by metformin and lisinopril, respectively. Vital signs are BP 86/64 mmHg, heart rate 115 bpm, respiratory rate 28, temperature 37°C, SpO2 96% under room air. The patient appears ashen and diaphoretic, with cool, mottled extremities. She is awake but answer questions slowly. Heart sounds are regular with an S4 gallop but without murmurs or rubs. Lungs sound are equal bilaterally and clear to auscultation. Her abdomen is soft, non tender, without palpable masses. Femoral pulses are equal. Extremities are cool, but without oedema. Peripheral pulses are faint but equal. The ECG is shown here in Figure 2. While arranging for early revascularization is made with the cardiologist, which of the following is the next MOST appropriate action.
A. Administered propranolol
B. Infuse 250-500 mL of 0.9% NaCl
C. Initiate thrombolytic therapy
D. Start dobutamine drip
E. Start a phenylephrine drip
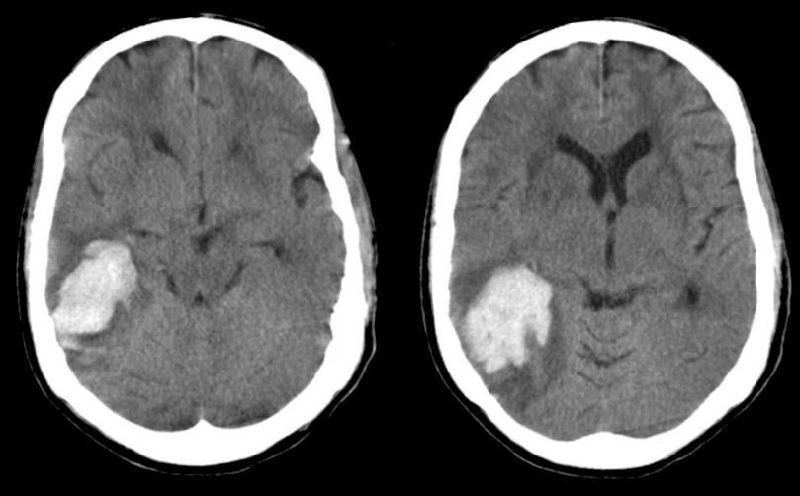
OBA: An 80-year-old lady with a history of atrial fibrillation presents with sudden-onset headache, vomiting and somnolence. She takes warfarin. Her blood pressure is 140/90 mmHg. She is sleepy but easily arousable and answers questions appropriately. She has moderate left sided weakness and numbness and ignores the nurse standing to her left. Head CT is as shown in Figure 3. The INR is 3.9. Which of the following actions is most likely to reduce this patient’s mortality?
A. Administering aspirin
B. Administering fresh frozen plasma and vitamin K
C. Intubation for airway protection
D. Lowering the blood pressure
E. Therapeutic hypothermia
OBA: A 77-year-old man is brought in by his family for unusual behavior. He has been confused and paranoid for he past 4 days, repeatedly claiming that the neighbours are poisoning him. He is worse at night and is sleeping irregularly. He has a history of schizophrenia, diabetes and benign prostatic hyperplasia. At triage, the patient was disorientated to time and place and answered questions nonsensically. Vital sign are as follows: temperature 38.4°C, blood pressure 110/85 mmHg, heart rate 105, respiratory rate 18, spO2 98% on room air. On exam, he is orientated to self, place and year and answers some questions appropriately but has difficulty paying attention and occasionally nods off to sleep. He complains, “my penis is on fire.” What is the most likely explanation for the change in his mental status?
A. Delirium
B. Dementia
C. Mania
D. Paranoid personality disorder
E. Psychosis
OBA: A 24-year-old pregnant female with a 24-week gestation presents in acute respiratory distress. Past medical history is significant for asthma normally controlled with a metered dose inhaler on as needed basis. She states that she used her inhaler at least eight times before arrival and feels no better. On arrival to the ED, she was in acute distress, bilateral wheeze on physical examination. SpO2 92% on room air. An arterial blood gas (ABG) has the following values: pH 7.34 paCO2 40 paO2 59 SaO2 90% What is your assessment and plan?
A. The patient has a moderate asthma exacerbation and should receive supplemental oxygen, salbutamol by metered dose inhaler.
B. The patient has a moderate asthma exacerbation and should receive supplemental oxygen, salbutamol by metered dose inhaler and oral steroids.
C. The patient has a moderate exacerbation of asthma and should receive supplemental oxygen, nebulized salbutamol and ipratropium, as well as begin steroids.
D. The patient has severe exacerbation of asthma with evidence of respiratory failure. Administer supplemental oxygen, initiate nebulized salbutamol and begin steroid as soon as possible.
E. The patient has severe exacerbation of asthma with evidence of respiratory failure. Administer supplemental oxygen, initiate nebulized salbutamol and ipratropium, begin steroids and initiate fetal monitoring.
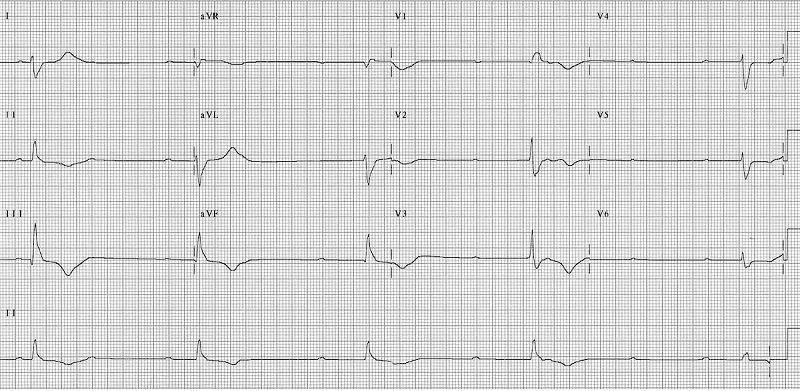
OBA: A 72-year-old woman presents to Ed with a painful infected ingrown toenail. On physical examination, her heart rate is 42 bpm and ECG as shown in Figure 5. Her blood pressure is 165/85 mmHg, her mental status is normal and she has no other complaints. Of the following, which is the best course of action in ED before refer to cardiologist?
A. Atropine 1mg IV
B. Adrenaline 1:1000, 0.3 mg IV
C. Glucagon 0.1 mg test dose, followed by 1 mg IV
D. Isoproterenol drip
E. Close observation with continuous cardiac monitoring
{"name":"Emergency Housemanship Assessment", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge and skills with our comprehensive Emergency Housemanship Assessment Quiz tailored for healthcare professionals. This quiz covers critical topics in emergency medicine, ensuring you are well-prepared for real-life scenarios.Key Features:30 questions covering a wide range of emergency topicsMultiple-choice format with immediate feedbackDesigned for aspiring doctors and healthcare workers","img":"https:/images/course1.png"}
More Quizzes
new Part 4 (765-865) (765-1019) NR 3
100500
Part 4O
65320
What Disney Princess Are You?
10513
Are you radical
740
Is My Mom Jealous of Me? Free to Spot the Signs
201017555
Ryan Gosling Character - Which One Are You?
201016624
After Applying the Primer - Sculptured Nail Service
201016858
90s Trivia Time Capsule: 201+ Free Questions
201015344
Pyromaniac Test - Am I a Pyromaniac? Free Online
201018648
Polyatomic Ions - Free Chemistry Practice
201016289
Identify Claims in Arguments - Practice with Answers
201016454
Yugioh - Which Monster Are You?
201017041