Ichigo USLME Med Management P2
1) A 10-year-old girl with blue eyes and blonde hair is brought to the office by her mother for a routine check-up. All her immunizations are up to date. Her family history is significant for myocardial infarction in her father and schizophrenia in a maternal uncle. There is no family history of any skin malignancies. Her height is at the 60th percentile, and weight is at the 56th percentile. While you are examining her, the mother says with much concern that she saw a television program that claimed that the incidence of skin cancer is increasing dramatically. She wants to know the best way to prevent skin cancer in her daughter, especially since they live in California. What is the best advice to help prevent malignant melanoma in this child?
. Sun screen lotion with SPF (sun protection factor) 15
. Sun screen lotion with SPF 30
. Protective clothing
. Avoid going outdoors
. No action needs to be taken, since there is no family history of melanoma
2) A 50-year-old man comes to the emergency department due to acute onset respiratory difficulty. He also has periorbital, circumoral and facial edema. Two weeks ago, he experienced chest pain, profuse sweating and anxiety, and was subsequently admitted to the cardiac intensive care unit. At that time, his ECG showed ST segment elevation and Q waves in the inferior leads. He was taken to the catheterization lab and had an angioplasty with stent done for 100% occlusion of the right coronary artery. He was discharged with the following medications: aspirin, clopidogrel, metoprolol, enalapril, simvastatin and isosorbide mononitrate. In the ED, his pulse is 102/min, blood pressure is 110/70 mmHg, respirations are 24/min and temperature is 36.8°C (98.4°F). Which of the following is most likely responsible for his present symptoms?
. Metoprolol
. lsosorbide
. Clopidogrel
. Aspirin
. Enalapril
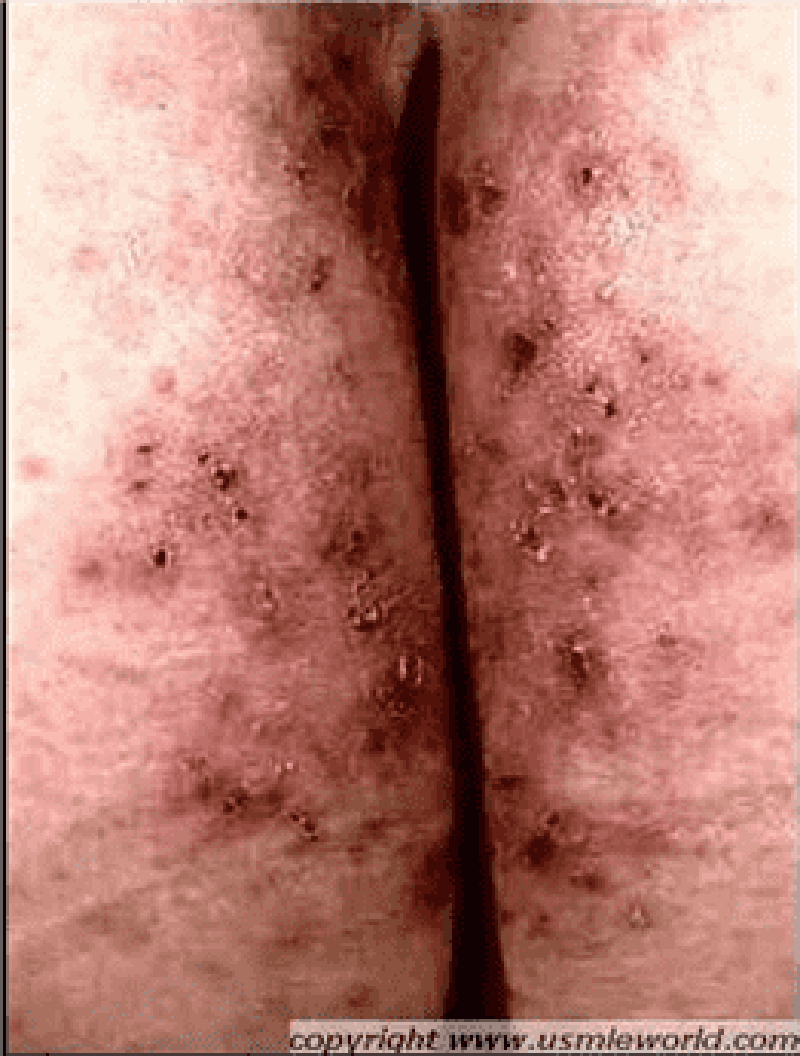
3) A 25-year-old male presents with skin lesions over his elbows, knees and neck. He complains of intense itching and burning sensation over these lesions for the past 10 days. He was advised to follow a gluten-free diet on his previous visit, but was not compliant. His vital signs are stable. On examination, there are flesh-colored to erythematous vesicles distributed over the extensor aspects of elbows, knees, posterior neck and shoulders. Some of these lesions are shown in the picture below. Which of the following is the drug of choice for his skin condition?
. High potency steroids
. Low dose acyclovir
. 1% lindane solution
. Azathioprine
. Dapsone
4) A 20-year-old woman complains of skin problems and is noted to have erythematous papules on her face with blackheads (open comedones) and whiteheads (closed comedones). She has also had cystic lesions. She is prescribed topical tretinoin, but without a totally acceptable result. You are considering oral antibiotics, but the patient requests oral isotretinoin, which several of her college classmates have used with benefit. Which of the following statements is correct?
. Intralesional triamcinolone should be avoided due to its systemic effects
. Systemically administered isotretinoin therapy cannot be considered unless concomitant contraceptive therapy is provided
. Antimicrobial therapy is of no value since bacteria are not part of the pathogenesis of the process
. The teratogenic effects of isotretinoin are its only clinically important side effects
. The patient will not benefit from topical antibiotics since she did not respond to topical retinoids
5) A 22-year-old male presents with a 6-month history of a red, nonpruritic rash over the trunk, scalp, elbows, and knees. These eruptions are more likely to occur during stressful periods and have occurred at sites of skin injury. The patient has tried topical hydrocortisone without benefit. On examination, sharply demarcated plaques are seen with a thick scale. Pitting of the fingernails is present. There is no evidence of synovitis. What is the best first step in the therapy of this patient’s skin disease?
. Photochemotherapy (PUVA)
. Oral methotrexate
. Topical calcipotriene
. Oral cyclosporine
. Topical fluticasone
6) A 35-year-old woman develops an itchy rash over her back, legs, and trunk several hours after swimming in a lake. Erythematous, edematous papules and plaques are noted. The wheals vary in size. There are no mucosal lesions and no swelling of the lips. What is the best first step in management of her symptomatic rash?
. Subcutaneous epinephrine
. Intravenous glucocorticoids
. Oral antihistamines (H1 blockers)
. Aspirin
. Oral doxycycline
7) A 64-year-old woman presents with diffuse hair loss. She says that her hair is “coming out by the handfuls” after shampooing. She was treated for severe community-acquired pneumonia 2 months ago but has regained her strength and is exercising regularly. She is taking no medications. Examination reveals diffuse hair loss. Several hairs can be removed by gentle tugging. The scalp is normal without scale or erythema. Her general examination is unremarkable; in particular, her vital signs are normal, she has no pallor or inflammatory synovitis, and her reflexes are normal with a normal relaxation phase. What is the best next step in her management?
. Reassurance
. Measurement of serum testosterone and DHEA-S levels
. Topical minoxidil
. Topical corticosteroids
. CBC and antinuclear antibodies
8) A 63-year-old retired farmer presents to the clinic complaining of red scaly spots on his head for the past 9 months. Physical examination is remarkable for numerous erythematous hyperkeratotic papules and plaques. The lesions are confined to the head and forehead and have poorly defined borders. Which of the following is the most appropriate next step in management of this patient?
. Punch biopsy of one of the lesions
. Application of hydrocortisone cream to affected areas and follow-up in 4 weeks
. Reassurance that this is a benign finding and follow-up in 6 months
. Application of fluocinide cream to affected areas and follow-up in 4 weeks
. Application of 5-fluorouracil cream to affected areas and follow-up in 4 weeks
9) A 21-year-old female presents with an annular pruritic rash on her neck. She explains that the rash has been present for the past 3 weeks and that her roommate had a similar rash not long ago. Physical examination is remarkable for a 20-mm scaling, erythematous plaque with a serpiginous border. Which of the following is the most appropriate initial treatment for this condition?
. Griseofulvin
. Oral cephalexin
. Topical mupirocin ointment
. Topical ketoconazole
. Hydrocortisone cream

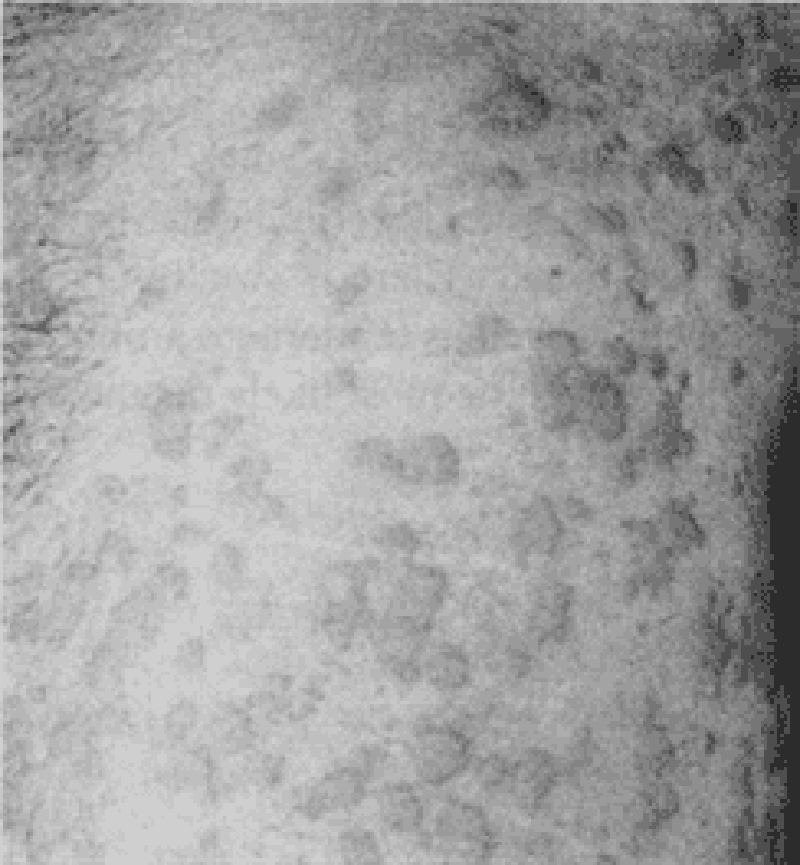
10) A 50-year-old male comes to the office due to an ulcer in his right foot. He has type 2 diabetes, for which he takes glyburide. Laboratory investigations reveal an HbA1c of 9%, and random blood sugar of 180 mg/dL. X-ray of the leg/foot is normal. A picture of the foot ulcer is shown below. Which of the following is the most appropriate management of this patient's foot ulcer?
. Start aspirin and atorvastatin
. Perform thorough debridement of the wound
. Prescribe tight-fitting shoes
. Prescribe oral antibiotics and follow-up as an outpatient
. Amputation
11) A 65-year-old Caucasian male comes to the office because of bilateral foot pain, which is present at rest and worsens at night. He has been having this symptom for the past few months. Other accompanying symptoms are hyperesthesia and paresthesia in both lower limbs. His medical problems include diabetes for the past twenty years. His daily medication is insulin. Physical examination reveals bilateral loss of ankle reflexes, loss of vibratory sensation and altered proprioception below the knees. His HbA1c level is 9%. Urine is positive for microalbuminuria. Which of the following is the most appropriate treatment for his leg pain?
. Amitriptyline
. Corticosteroids
. Oxycodone
. Acetaminophen
. Ketorolac
12) A 55-year-old African-American male comes to the office for a routine follow-up visit. His past medical history is significant for type 2 diabetes mellitus (OM), hypertension for the last 5 years, and an acute myocardial infarction 2 years ago. His mother died of a heart attack at the age of 72 years, and his father died in a motor vehicle accident at the age of 42 years. He has no siblings. He is currently on glyburide, captopril and baby aspirin. He is very compliant with his diet and medication. His glycemic control was very good until a few months ago, when he noticed that his blood sugar levels were running high. This morning, his finger stick reading was 200 mg/dL. He weighs 188 lbs and is 5'8" tall. His physical examination is otherwise unremarkable. His blood work done three days ago showed blood urea nitrogen of 14 mg/dL and a creatinine level of 1.0 mg/dL. His HBA1c one month ago was 8.0%. Which of the following is the most appropriate next step in management?
. Discontinue captopril because it is known to produce diabeticogenic state
. Discontinue captopril since glyburide efficacy is reduced with simultaneous usage of captopril
. Start the patient on human insulin 70/30
. Add metformin to achieve better glycemic control
. Add pioglitazone to achieve better glycemic control
13) A 60-year-old male comes to the office due to edema of his face and ankles of two weeks duration. He denies any chest pain or breathlessness. He is a known diabetic for the past 15 years. His diabetes is being managed with exercise, dietary modification and glyburide. His glycosylated hemoglobin (HbA1C) level one month ago was 7.5%. His temperature is 37.0°C (98.6°F), pulse is 75/min, blood pressure is 146/87 mmHg, and respirations are 15/min. Examination is unremarkable, except for bilateral pitting edema around the ankles and periorbital edema. Lab results show: Serum sodium 140 mEq/L, Potassium 4.3 mEq/L, Bicarbonate 20 mEq/L, Blood glucose120 mg/dL, Blood urea nitrogen 37 mg/dL, Serum creatinine 24 mg/dL, Total cholesterol 300 mg/dl. EKG is normal. 24 hour urine collection shows 3.7 g protein/day. To alter the course of this patient's diabeticnephropathy, what is the most appropriate next step in management?
. Intensive glycemic control
. Intensive blood pressure control
. Very low protein diet
. Aggressive lipid management
. Aspirin therapy
14) A 40-year-old white female presents with complaints of heat intolerance, sweating and palpitations. She also reports menstrual irregularities, increased appetite and diarrhea. She has had these symptoms for the past 4 Months. Her pulse is 102/min and regular, blood pressure is 116/80 mmHg, temperature is 37.2°C (99°F), and respirations are 14/min. Physical examination reveals a non-tender, diffuse swelling in front of her neck; it moves upwards with deglutition. Her TSH level is 0.05 mU/L. Free T4 and T3 levels are increased. Radioactive iodine uptake at 24 hours is significantly increased. Pregnancy test is negative. Which of the following is the most appropriate long-term treatment modality for this patient?
. Surgery
. Propylthiouracil
. Iodinated contrast agents
. Radioactive iodine therapy
. Propranolol
15) A 50-year-old Caucasian male comes to the office for the evaluation of polyuria and polydypsia for the last two months. He also complains of weakness and fatigue. He had one episode of transient proximal muscle weakness which lasted 30 minutes. He has a 20-pack year history of smoking. He does not drink alcohol. His past medical and family histories are insignificant. His pulse is 78/min, blood pressure is 150/96 mmHg and temperature is 36.7°C (98°F). The rest of the examination, including the neurological examination, is normal. Labs show: Plasma sodium 150 mEq/L, Potassium 2.6 mEq/L, Serum creatinine 0.8 mg/dL. Which of the following is the most appropriate next step in the management of this patient?
. Measurement of plasma renin activity and aldosterone concentration
. Measurement of 24 hour urinary potassium excretion
. Aldosterone suppression testing
. Imaging of adrenals by CT scan
. Adrenal vein sampling
16) A 78-year-old female is being evaluated for recent weight loss and fatigue. Laboratory tests reveal abnormal thyroid function. She begins treatment with a single agent, but soon after is hospitalized with new onset atrial fibrillation and hand tremor. Which of the following treatments had she most likely received?
. Propylthiouracil
. Lopanoic acid
. Radioactive iodine
. Propranolol
. Prednisone
17) A 60-year-old female presents with transient loss of consciousness. She appears lethargic and confused. She also complains of hemoptysis and weight loss of 10 lbs (4.5kg) over a period of 2 months. She has smoked one pack of cigarettes daily for the last 40 years. Her temperature is 37.0°C (98.6°F), pulse is 75/min, blood pressure is 110/70 mmHg, and respirations are 16/min. Her mucus membranes are moist. There is no jugular venous distention. Her neurological examination is non-focal, and cardiovascular examination is unrevealing. There is no ankle edema or ascites. Serum studies show: Sodium 115 mEq/L, Potassium 3.7 mEq/L, Bicarbonate 22 mEq/L, Blood glucose 100 mg/dL, BUN 10.0 mg/dL. Serum osmolality is 250 mOsm/Kg, and urine osmolality is 500 mOsm/Kg. Urine sodium concentration is 40 mEq/L. Chest x-ray shows a mass in the right hilar region. What is the most appropriate next step in the management of this patient?
. Normal saline
. Loop diuretics
. Water restriction
. Hypertonic saline
. Demeclocycline
18) A 40-year-old African American female comes to the office for a routine medical check-up. She has no complaints. She has twenty pack-year smoking history but she stopped smoking one year ago. Her mother and one maternal uncle have diabetes. Her height is 5'7" inches, and weight is 150 lbs. Her blood pressure is 122/80 mmHg, pulse is 80/min, respirations are 14/min and temperature is 37°C (98°F). She agrees to have diabetes mellitus screening. Her plasma glucose level after an overnight fast is 130 mg/dL. What is the most appropriate next step in the management of this patient?
. Repeat fasting blood glucose measurement
. Perform 75 g oral glucose tolerance test
. Start therapy with oral hypoglycemic agents
. Start therapy with insulin
. Recommend lifestyle changes
19) A 22-year-old female presents with complaints of heat intolerance, sweating and palpitations. She also reports menstrual irregularities, increased appetite and diarrhea. Her pulse is 102/min and regular, blood pressure is 116/80 mmHg, temperature is 37.2°C (99°F), and respirations are 14/min. Physical examination reveals a diffusely enlarged, nontender thyroid gland. TSH level is 0.05 mU/L. Free T4 and T3 levels are elevated. Radioactive iodine uptake at 24 hours is 50 percent. Thyroid stimulating immunoglobulins are present. She is started on propylthiouracil 300 mg daily in three divided doses. After two weeks, she returns and complains of a sore throat. Her pulse is 98/min and regular, temperature is 38.6°C (101.5°F), blood pressure is 115/76 mmHg, and respirations are 15/min. The soft palate, pharynx, and tonsils are red and swollen. What is the most appropriate next step in the management of this patient?
. Add propranolol
. Increase propylthiouracil dose
. Stop propylthiouracil
. Throat culture
. Oral penicillin
20) A 35-year-old female presents to the emergency department with a 30-minute history of severe headache, palpitations, abdominal pain, nausea, and vomiting. She had similar episodes twice during the last month, but those were not so severe and resolved spontaneously in 30-40 minutes. She visited a doctor recently, and hypertension with elevated urinary vanillylmandelic acid level was diagnosed. She is not taking any medications, and denies substance abuse. Her blood pressure is 200/130 mmHg and heart rate is 130/min. She appears frightened. Physical examination reveals hand tremors and excessive sweating. Slow intravenous infusion of propranolol is started while waiting for the routine labs. What is the most probable reaction to the treatment given to the patient?
. Blood pressure will slowly decrease
. Blood pressure will rapidly decrease
. Heart rate will increase
. Heart rate will not change
. Blood pressure will rapidly increase
21) A 65-year-old male comes to the office and complains of nausea and early satiety for the past several months. His other complaints are anorexia and abdominal bloating. He denies any heartburn or epigastric pain. He has diabetes, and has been taking insulin for the last fifteen 15 years. His blood glucose readings using the home blood glucose monitor range between 40 to 400 mg/dL. Most of the low blood glucose readings occur after meals. Which of the following is the most appropriate management of this patient's symptoms?
. Promethazine
. Ondansetron
. Ibuprofen
. Metoclopramide
. Ranitidine
22) Four of your patients who came to the office today all have signs and symptoms of hyperthyroidism. After the appropriate evaluation, you decided to treat them with radioactive iodine. Hyperthyroid patients with which of the following disorders are most likely to develop hypothyroidism following radioactive therapy?
. Graves' disease
. Toxic adenoma
. Multinodular goiter
. Ectopic production of thyroid hormones
. Thyroid Cancer
23) A 60-year-old Caucasian male presents to the office with erectile dysfunction that progressed slowly over the last several months. He finds it difficult to obtain an erection, and has noted a decrease in nocturnal erections. His past medical history is significant for diabetes mellitus, type 2 and benign prostatic hypertrophy (BPH). His current medications are glyburide and doxazosin. Physical examination is insignificant. HbA1c level measured two weeks ago was 7.5%. He is asking about a prescription for sildenafil. Which of the following is the best statement concerning the treatment of erectile dysfunction in this patient?
. Tightening of glycemic control improves erectile dysfunction
. Sildenafil is not a drug of choice for diabetics with erectile dysfunction
. Sildenafil and doxazosin should be given with at least a 4-hour interval
. Prostaglandins (alprostadil) are preferred in this patient
. Sildenafil should not be combined with glyburide
24) A 58-year-old asymptomatic male is found to have elevated levels of serum alkaline phosphate. His serum calcium and phosphate levels are normal. He denies any bone pain or deformity. His liver function tests are normal. The urinary hydroxyproline levels are increased. Nuclear bone scan reveals an increased uptake in the right scapula. Plain radiography confirms Paget's disease. Which of the following is the most appropriate next step in the management of this patient?
. No treatment is indicated at this stage
. Treatment with bisphosphonates
. Treatment with nasal calcitonin
. Treatment with calcium and vitamin D
. A CT scan of lung
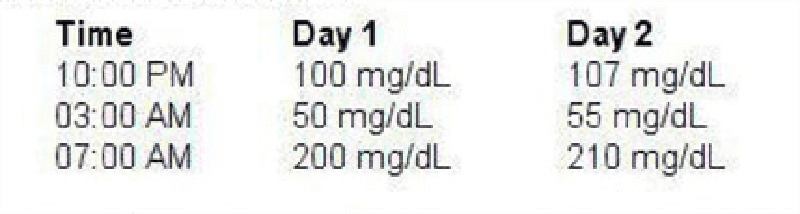
25) A 25-year-old female comes to the office for a follow-up visit. She was just diagnosed with type 1 diabetes mellitus a few days ago, when she presented at the emergency department with ketoacidosis. After successful management of her diabetic ketoacidosis (DKA), she was sent home on an insulin regimen with the following dosage: Before breakfast 10 units of NPH and 10 units of regular insulin, Before supper 10 units of NPH and 4 units of regular insulin. During this office visit, she shows the record of her fingerstick readings at home. For the last 2 days, her blood glucose levels were (see in pic). What is the most likely explanation for her 7:00 am blood glucose level?
. Spikes of growth hormone release
. Epinephrine, norepinephrine, & glucagon release
. Waning of insulin levels
. Destruction of glucagon-secreting cells
. Decrease Insulin-secretor
26) A 46-year-old male comes to your office for a routine health examination. He has no current physical complaints and says he is compliant with his medications. His past medical history is significant for type 2 diabetes diagnosed two years ago that he has been able to control with diet, exercise and metformin. The patient also takes a daily aspirin. On physical examination, he has a temperature of 36.7°C (98°F), a blood pressure of 140/86 mmHg, a pulse of 80/min, and respirations of 14/min. His laboratory studies show: Total cholesterol 170 mg/dl, High density lipoprotein (HDL) 50 mg/dl, Low density lipoprotein (LDL) 65 mg/dl, Triglycerides (TG) 150 mg/dl, HbA1C 7.0. Serum chemistries are with in normal limits. Which of the following is the most appropriate next step in the management of this patient?
. Add niacin
. Add gemfibrozil
. Add lisinopril
. Add ezetimibe
. Add insulin
27) A 60-year-old asymptomatic man presents to your office for a routine check-up. He has a 10-year history of type 2 DM, and a 12-year history of hypertension. His current medications include low-dose glyburide and a low-dose thiazide diuretic. His blood pressure is 140/90 mmHg and heart rate is 65/min. Physical examination shows a soft ejection systolic murmur at the base of the heart. Ophthalmoscopic evaluation reveals no abnormalities. ECG recorded 6 months ago showed left ventricular hypertrophy and non-specific ST segment and T-wave abnormalities. His recent fasting glucose level was in the range of 120 to 150 mg/dl, and HbA1c was 7.1 % (normal< 6%). 24-hour urine collection reveals microalbuminuria. Which of the following is the best measure to slow end-organ damage in this patient?
. Increase the dose of glyburide
. Increase the dose of thiazide diuretic
. Switch to insulin
. Add ACE inhibitor
. Add beta-blocker
28) A 21-year-old man with type 1 diabetes mellitus presents to the emergency department with complaints of abdominal pain, nausea and vomiting. His temperature is 36.0°C (97.0°F), pulse is 110/min, blood pressure is 102/60 mmHg, and respirations are 26/min. Lungs are clear to auscultation. Abdomen is soft, non-tender and non-distended. Chemistry panel shows: Sodium 130 mEq/L, Potassium 5.2 mEq/L, Chloride 90 mEq/L, Bicarbonate 10 mEq/L, Blood glucose 450 mg/dl. Which of the following is the most appropriate next step in management?
. Normal saline and regular insulin
. 0.45% saline and regular insulin
. Normal saline and NPH insulin
. 5% dextrose and NPH insulin
. Sodium bicarbonate
29) A 40-year-old female patient is brought to the office by her husband due to altered mental status and confusion of recent onset. According to her husband, she has been complaining of intense thirst, craving for ice water, and experiencing increased urination for the past few days. Her only medication is lithium for bipolar depression. Her temperature is 39.0°C (102.5°F), pulse is 102/min, blood pressure is 90/60 mmHg, and respirations are 15/min. Physical examination reveals a disoriented patient with dry skin and mucous membranes. Blood chemistry panel reveals: Sodium 156 mEq/L, Potassium 4.1 mEq/L, Bicarbonate 26 mEq/L, Blood glucose 102 mg/dl, BUN 27 mg/dl. Serum osmolality is 328 mOsm/kg, and urine osmolality is 180mOsm/Kg. What is the most appropriate next step in the management of this patient?
. Water deprivation test
. Plain water drinking
. IV infusion of normal saline
.IV infusion of 045% saline
. IV infusion of 5% dextrose
30) A 40-year-old asymptomatic male comes to the office for a routine physical examination. His serum chemistry panel shows: Sodium 140 mEq/L, Potassium 4.0 mEq/L, Bicarbonate 25 mEq/L, Chloride 101 mEq/L, Calcium 11.8 mg/dL, Albumin 4.0 g/dL, Phosphorus 2.2 mg/dL. 24-hour urine collection reveals a calcium level of 200 mg, and creatinine level of 1.7 g. Serum PTH level is increased. Bone mineral density by dual energy X-ray absorptiometry (DEXA) shows normal bone mineral density. Neck examination reveals no masses. What is the most appropriate next step in the management of this patient?
. Bisphosphonate therapy
. Surgical exploration of the neck
. Medical surveillance
. Loop diuretics
. Thiazide diuretics
31) A 38-year-old woman presents with several months of decreased libido and a 4.5-kg (10-lb) weight gain. She has not had her menstrual period for the past 3 months. Physical examination is unremarkable except that a small amount of white discharge is manually expressed from the nipples bilaterally. The serum prolactin level is 300 ng/mL. Which of the following is the most appropriate first-line treatment?
Bromocriptine
Cortisol
Methyldopa
Metoclopramide
Octreotide
32) A 72-year-old woman presents to her physician complaining of fatigue, malaise, weight loss, and salt cravings. The patient has chronic obstructive pulmonary disease and is intermittently treated with corticosteroids but is not using home oxygen. Her oxygen saturation is 97% on room air with a blood pressure of 115/65 mmHg, which is significantly lower than her baseline of 125/78 mmHg. On auscultation she has good breath sounds bilaterally without wheeze, although the expiratory phase is slightly prolonged. Five weeks ago she received a corticosteroid treatment for an acute chronic obstructive pulmonary disease exacerbation, for which she was hospitalized and given 3 L of oxygen via nasal cannula. However, she admits that after discharge she was having continued difficulty breathing and did not follow the taper of the corticosteroids. The patient has smoked one pack of cigarettes per day for the past 51 years. Which of the following is the appropriate first step in the management of this patient?
3 L of oxygen via nasal cannula
CT scan of the chest
Intravenous fluids
Restart corticosteroids and follow a strict taper
X-ray of the chest
33) An obese patient with a long-standing history of type 2 DM presents to his primary care physician. On examination he has decreased sensation in both lower extremities. Upon questioning of his compliance with his prescribed medications, he reports that he has stopped taking one medication because it gave him flatulence and abdominal pain. Which of the following did this man most likely stop taking?
An α-glucosidase inhibitor
Meglitinide
Metformin
Sulfonylurea
Thiazolidinedione
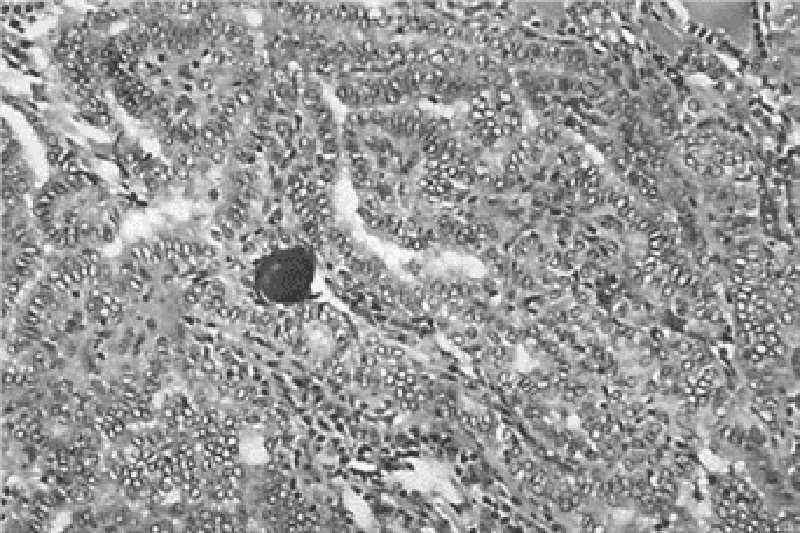
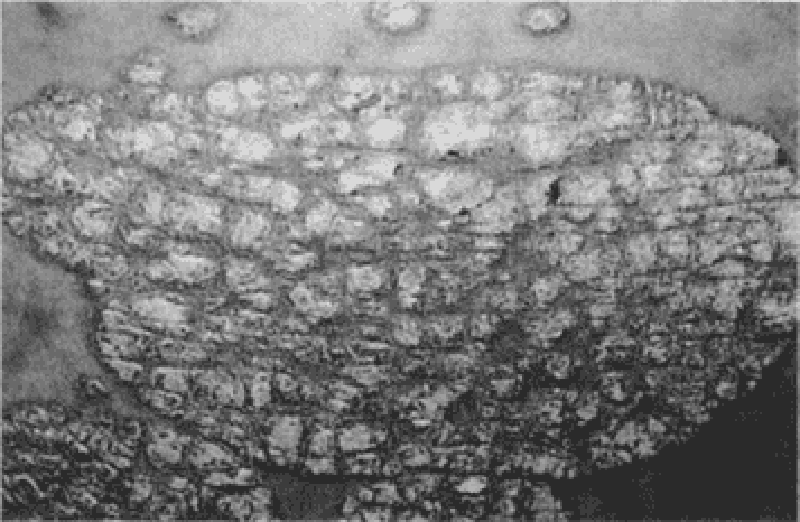
34) A 19-year-old G1P0 woman at 32 weeks gestation presents for scheduled prenatal appointment. The pregnancy has been uncomplicated to date. However, she mentions that she recently noticed a hard lump on her neck. She denies pain or difficulty swallowing, speaking, or breathing. Physical examination reveals a firm, nontender, immobile, solitary nodule on the left hemithyroid. Ultrasound reveals a solid 2-cm mass. There is no cervical lymphadenopathy. Thyroid function tests reveal a thyroid-stimulating hormone level of 1.2 μU/mL and free thyroxine level of 0.9 ng/dL. Results of fine-needle aspiration biopsy are shown in the image. Which of the following is the best next step in management?
Left hemithyroidectomy
Monitor until after delivery
Radioablation therapy
Start methimazole
Start propylthiouracil
35) A 49-year-old man presents to the clinic for a health maintenance visit. He has a family history of type 2 DM. His medical history is significant for gastroesophageal reflux disease, for which he takes omeprazole and over-the-counter antacids. He smokes one pack of cigarettes per day and drinks an average of two beers per night. The patient’s body mass index is 32 kg/m². Which of the following most greatly reduce(s) the patient’s risk of future coronary artery disease, renal failure, and retinopathy?
Alcohol avoidance
Daily multivitamin
Diet rich in fruit and vegetables
Smoking cessation
Weight loss and exercise
36) A 37-year-old white female presents with galactorrhea and amenorrhea for the past 7 months. She denies any headaches, visual problems, vaginal dryness or dyspareunia. She is married, has two children, and remarks that her family is "complete." She does not use tobacco, alcohol or drugs. Her blood pressure is 120/80 mmHg, pulse is 72/min, temperature is 36.7°C (98.6°F) and respirations are 14/min. Visual field testing is within normal limits. Pregnancy test is negative. Her serum prolactin level is 150ng/ml. Pituitary MRI shows a 6mm pituitary adenoma. Which of the following is the most appropriate next step in the management of this patient?
. Surgery
. Treatment with cabergoline
. Treatment with estrogens
. Radiotherapy
. Monitoring by serum prolactin and MRI
37) A 32-year-old man presents to his primary care physician complaining of diffuse muscle weakness, dry and puffy skin, and patchy areas of hair loss on his scalp. He also notes numbness around his mouth and a tingling sensation in his hands and feet. He has a history of seizure disorder, and has been taking carbamazepine for the past 5 years. On physical examination he has dry skin and coarse, brittle hair with patchy alopecia. Tapping his right cheek causes contraction of the muscles at the corner of his mouth, nose, and eye on the right side. Which of the following could best have prevented the development of the patient’s current problem?
Magnesium supplementation
Parathyroidectomy
Thyroid hormone
Vitamin C supplementation
Vitamin D supplementation
38) A 30-year-old Caucasian female comes to the physician's office because of polyuria and polydipsia of recent onset. She has no other medical problems. She does not use tobacco, alcohol or drugs. She has no known drug allergies. Her mother has diabetes. Her temperature is 36.7°C (98°F), pulse is 75/min, blood pressure is 110/70 mmHg, and respirations are 15/min. The initial lab results are: Hb 12.7 g/dl, WBC 5,000 /cmm, Platelets 380,000/cmm, Blood glucose 90 mg/dl, Serum sodium 142 mEq/L, Serum potassium 4.0 mEq/L, Bicarbonate 26 mEq/L, BUN 15 mg/dl, Serum creatinine 0.9 mg/dl, Serum uric acid 9 mg/dl, Serum osmolality 295 mOsm/kg, Urine osmolality 160 mOsm/kg. After 12 hours of water deprivation, lab testing reveals:Serum sodium 151 mEq/L, Serum potassium 4.2 mEq/L, Bicarbonate 26 mEq/L, Serum osmolality 300 mOsm/kg, Urine osmolality 186 mOsm/kg. One hour after the subcutaneous administration of arginine vasopressin, the urine osmolality is 400mosm/kg. Which of the following is the most appropriate treatment for this patient?
. Psychotherapy
. Intranasal desmopressin acetate
. Indomethacin
. Hydrochlorothiazide
. Demeclocycline
39) A 42-year-old woman with no significant past medical history presents for a routine health maintenance visit. On physical examination a solitary nodule is palpated in the thyroid. She denies pain, dysphagia, or hoarseness. She also denies fatigue, weight change, heat or cold intolerance, diarrhea, or constipation. There is no family history of thyroid cancer. Her serum thyroid-stimulating hormone level is normal. Which of the following is the most appropriate next step in evaluation?
Fine-needle aspiration
MRI
Radionuclide scan
Thyroid lobectomy
Ultrasonography
40) A patient comes to your office for a new-patient visit. He has moved recently to your city due to a job promotion. His last annual examination was 1 month prior to his move. He received a letter from his primary physician stating that laboratory workup had revealed an elevated alkaline phosphatase and that he needed to have this evaluated by a physician in his new location. On questioning, his only complaint is pain below the knee that has not improved with over-the-counter medications. The pain increases with standing. He denies trauma to the area. On examination you note slight warmth just below the knee, no deformity or effusion of the knee joint, and full ROM of the knee without pain. You order an x-ray, which shows cortical thickening of the superior fibula and sclerotic changes. Laboratory evaluation shows an elevated alkaline phosphatase of 297 mg/dL with an otherwise normal metabolic panel. Which of the following is the treatment of choice for this patient?
. Observation
. Nonsteroidal anti-inflammatory
. A bisphosphonate
. Melphalan and prednisone
. Ursodeoxycholic acid (UDCA)
41) Your patient is a 48-year-old Hispanic male with a 4-year history of diabetes mellitus type 2. He is currently utilizing NPH insulin/Regular insulin 40/20 units prior to breakfast and 20/10 units prior to supper. His supper time has become variable due to a new job and ranges from 5 to 8 PM. In reviewing his glucose diary, you note some very low readings (40-60 mg/dL) during the past few weeks at 3 AM. When he awakens to urinate, he feels sweaty or jittery so has been checking a fingerstick blood glucose. Morning glucose levels following these episodes are always higher (200-250) than his average fasting glucose level (120-150). Which change in his insulin regimen is most likely to resolve this patient’s early AM hypoglycemic episodes?
. Increase morning NPH and decrease evening NPH
. Decrease morning NPH and decrease evening regular insulin
. Change regimen to glargine at bedtime and continue morning and evening regular insulin
. Discontinue both NPH and regular insulin; implement sliding scale regular insulin with meals
. Change regimen to glargine at bedtime with lispro prior to each meal
42) A 32-year-old G2P1 woman at 16 weeks gestation presents to her obstetrician complaining of fatigue, anxiety, and palpitations. She says she has been feeling warm, even in her air-conditioned home, and has been having three or four loose stools per day, as compared to one or two prior to her pregnancy. She has a temperature of 37.1°C (98.9°F), heart rate of 105/min, and blood pressure of 128/76 mmHg. Neck examination reveals mild diffuse enlargement of the thyroid gland with no lymphadenopathy. Relevant laboratory findings include a total triiodothyronine level of 400 ng/dL, free thyroxine of 6.8 ng/dL, and thyroid-stimulating hormone of 0.01 μU/mL (normal: 0.4–4 μU/L). Results of a thyroid- stimulating hormone-receptor antibody test are positive. Which of the following is the most appropriate therapy for this patient?
High-dose iodine therapy
Methimazole
Propylthiouracil
Radioiodine ablation
Surgical resection
43) A 50-year-old female is 5 ft 7 in tall and weighs 185 lb. There is a family history of diabetes mellitus. Fasting blood glucose (FBG) is 160 mg/dL and 155 mg/dL on two occasions. HgA1c is 7.8%. You educate the patient on medical nutrition therapy. She returns for reevaluation in 8 weeks. She states she has followed diet and exercise recommendations but her FBG remains between 130 and 140 and HgA1C is 7.3%. She is asymptomatic, and physical examination shows no abnormalities. Which of the following is the treatment of choice?
. Thiazolidinediones
. Encourage compliance with medical nutrition therapy
. Insulin
. Metformin
. Observation with repeat HgA1C in 6 weeks
44) A 49-year-old woman presents to her physician’s office with a long-standing history of polydipsia, polyuria, central obesity, and hyperlipidemia. She is currently taking metformin, a sulfonylurea, and an angiotensin-converting enzyme (ACE) inhibitor. ACE inhibitors are most beneficial in preventing or slowing the progression of which of the following diabetic complications?
Diabetic ketoacidosis
Diabetic nephropathy
Diabetic neuropathy
Diabetic retinopathy
Peripheral vascular disease
45) A 42-year-old woman presents to her physician with complaints of fever (38.2°C [100.8°F]) and mild-to-moderate anterior neck pain. On examination the physician finds her to be tachycardic and sweating, and to have an exquisitely tender thyroid gland. Her blood work shows a depressed thyroid-stimulating hormone level and increased free thyroxine. Which of the following is the most appropriate treatment at this time?
Acetaminophen
Ibuprofen
Levothyroxine
Prednisone
Radioactive iodine
46) A 53-year-old woman suffers from long-standing obesity complicated by DJD of the knees, making it difficult for her to exercise. Recently her fasting blood glucose values have been 148 mg/dL and 155 mg/dL; you tell her that she has developed type 2 diabetes. She wonders if diet will allow her to avoid medications. In addition, her daughter also suffers from obesity and has impaired fasting glucose, and the patient wonders about the management of her prediabetes. Which of the following is a correct statement based on the American Diabetes Association 2008 guidelines regarding nutrition recommendations and interventions for diabetes?
. Low-carbohydrate diets such as “South Beach” and “Atkins” should be avoided
. Outcomes studies show that medical nutrition therapy (MNT) can produce a 1 to 2-point decrease in hemoglobin A1c in type 2 diabetics
. Prediabetic patients should be instructed to lose weight and exercise but a referral to a medical nutritionist is not necessary until full-blown diabetes is diagnosed
. Very low-calorie diets (< 800 cal/day) produce weight loss that is usually maintained after the diabetic patient returns to a self-selected diet
. Bariatric surgery may be considered for patients with type 2 diabetes and a BMI of > 30 kg/m2
47) A 45-year-old G2P2 female presents for annual examination. She reports regular menstrual cycles lasting 3 to 5 days. She exercises 5 times per week and reports no difficulty sleeping. Her weight is stable 140 lbs and she is 5 ft 8 in tall. Physical examination is unremarkable. Laboratory studies are normal with the exception of a TSH value of 6.6 mU/L (normal 0.4-4.0 mU/L). Which of the following represents the best option for management of this patient’s elevated TSH?
. Repeat TSH in 3 months and reassess for signs of hypothyroidism
. Begin low dose levothyroxine (25-50 μg/d)
. Recommend dietary iodide supplementation
. Order thyroid uptake scan
. Measure thyroid peroxidase antibodies (TPOAb)
48) A 28-year-old patient with known Addison’s disease presents with abdominal pain and is hypotensive to a systolic pressure of 88 mmHg. He has a 2-week history of progressively worse nonproductive dry cough, sore throat, malaise, and headache. He has not checked his temperature at home but complains of constant chills. Which of the following is the best initial management?
Azithromycin
Check serum glucose
Hydrocortisone
Intravenous fluids
X-ray of the chest
49) A generally healthy 74-year-old woman who recently moved into the area visits the physician’s office for her first well-visit. She states that her previous doctor had been treating her with propylthiouracil (PTU) for subclinical hyperthyroidism, but that her prescription ran out several months ago. Laboratory studies reveal that her free thyroxine and triiodothyronine levels are normal, but her thyroid-stimulating hormone is depressed. PTU therapy is most important in this patient to prevent the development of which disorder?
Cardiac dysrhythmias
Hypothyroidism
Pretibial myxedema
Thyroid cancer
Thyroid storm
50) You recently evaluated a 28-year-old woman who presented with complaints of shakiness and heat intolerance. The patient plans to have children and is currently using no contraception. On examination you noted tachycardia with an HR of 102, a fine tremor, a diffuse goiter, and proptosis. You now have the laboratory results and note a TSH < 0.001, elevated total T4 of 17.8, and increased T3 uptake. Radionuclide uptake by the thyroid gland is elevated. You tell her that she has Graves’ disease. What is the best treatment plan for this patient?
. Propylthiouracil
. Radioactive iodine
. Propranolol
. Thyroid surgery
. Oral corticosteroids
51) A 61-year-old obese man with a history of chronic alcohol abuse is diagnosed with type 2 DM. In addition to diet modification and exercise, his physician recommends he begin therapy with a hyperglycemic agent. Several days after starting therapy, his wife comes home from work and finds him sitting on the couch staring into space and breathing rapidly. When she speaks to him, she finds he is quite confused, and immediately takes him to the emergency department. Arterial blood gas analysis shows: pH: 7.2, HCO −: 19 mEq/L. Partial carbon dioxide pressure: 32 mmHg Partial oxygen pressure: 80 mmHg Lactate: 6 mmol/L. Which of the following drugs is most likely responsible for this patient’s symptoms?
Acarbose
Glipizide
Insulin
Metformin
Rosiglitazone
52) A 56-year-old woman presents to the outpatient clinic for a routine visit. On physical examination a 1-cm nodule is palpated in her thyroid. Her physical examination is otherwise unremarkable. Her heart rate is 70/min and regular, blood pressure is 126/82 mmHg, and temperature is 36.7°C (98.0°F). Which of the following is a poor prognostic indicator for the thyroid nodule?
Female gender
Hoarseness
Palpitations
Patient age of 56 years
Slow growth of nodule
53) A 55-year-old female presents to the office with a one-week history of left-sided ear pain and itchiness. The pain is especially bothersome at night, and is exacerbated by chewing. She denies any hearing loss. Her past medical history is significant for hypertension, type 2 diabetes mellitus, hyperlipidemia, and gout. Current medications include lisinopril, allopurinol, and metformin. She has missed her last two appointments with her primary care physician. Her temperature is 38.3°C (101°F), blood pressure is 140/90 mmHg, and pulse is 98/min. On examination, there is granulation tissue in the left ear canal with a scant amount of discharge. Which of the following is the best initial treatment for this patient?
. Topical neomycin
. Topical low-strength corticosteroids
. Ciprofloxacin
. Ampicillin/sulbactam
. Surgical debridement
54) A 60-year-old man comes to your office complaining of difficulty hearing for the past few weeks. He has type 2 diabetes mellitus, which is well-controlled by diet alone. His past medical history is also significant for essential hypertension, congestive heart failure secondary to diastolic dysfunction, and chronic renal failure. Medications include aspirin, diuretics, an ACE inhibitor, and a beta-blocker. His pulse is 82/min, blood pressure is 140/90 mmHg, and respirations are 14/min. Examination reveals hearing loss in both ears. Which of the following medication is a potential cause of this patient's hearing problems?
. Lisinopril
. Aspirin
. Metoprolol
. Furosemide
. Hydrochlorothiazide
55) A 7-year-old boy is brought to your office with a sore throat, decreased appetite, and nausea. His past medical history is insignificant. All of his vaccinations are up-to-date. He has no known allergies. His temperature is 39.0°C (102.5°F), blood pressure is 110/70 mmHg, pulse is 104/min, and respirations are 16/min. On examination, the pharynx and tonsils are red, swollen, and have white exudates on their surface. There is also bilateral tender cervical lymphadenopathy. The rapid diagnostic test for streptococcal antigen is positive. What is the most appropriate next step in management?
. Throat culture
. Monospot test
. Antistreptolysin O antibodies
. Oral penicillin V
. Oral azithromycin
56) A 37-year-old woman presents to your office with severe vertigo, postural instability, and vomiting. She also complains of "a buzzing sound" in her right ear. She has had two similar episodes over the previous year that lasted several hours and resolved spontaneously. She has no other medical problems. Her mother died of breast cancer at 55 years of age and her father is currently suffering from colon cancer. Her heart rate is 90/min and blood pressure is 130/80 mmHg. Her BMI is 25.3 kg/m2. Examination reveals horizontal nystagmus. Which of the following could have prevented this patient's symptoms?
. Caloric restriction
. Low salt diet
. Gluten-free diet
. High complex carbohydrate diet
. Calcium supplementation
57) A 30-year-old school teacher presents with a three-day history of fever, chills, and sore throat. He also complains of difficulty swallowing that started yesterday. He denies any cough, chest pain, or difficulty breathing. He is married and denies any new sexual encounters. His temperature is 39°C (102.2°F), blood pressure is 118/76 mmHg, pulse is 102/min, and respirations are 19/min. On examination, his voice is muffled. Enlarged, tender cervical lymph nodes are palpated on the left, and his uvula is deviated to the right. What is the most appropriate treatment for this patient?
. Throat swabs and oral antibiotics
. Monospot test and oral antibiotics
. Emergency laryngoscopy
. Cricothyroidotomy
. Needle peritonsillar aspiration
58) A 73-year-old woman is transferred to the hospital from the nursing home because of diverticulitis. A prior CT scan showed inflamed sigmoid colon. Transferred records indicate a 2 day history of fever and abdominal pain. On admission, her white count is 22,000/cmm, and she is started on IV antibiotics and IV fluids. Over the ensuing few days, her white count starts to come down and she has no nausea, vomiting or fever; however, she suddenly develops a cough and increasing abdominal pain. Abdominal examination shows guarding and tenderness in the left lower quadrant. An upright x-ray film of the chest shows free air under the left diaphragm. Which of the following is the most appropriate next step in management?
. CT scan of the abdomen
. Colonoscopy
. Barium enema
. Continue antibiotics and observe
. Laparotomy
59) A 35-year-old Hispanic male comes to the office because of excruciating pain during defecation for the past week. The pain is so severe that he avoids using the toilet. He also adds that he has noticed bright red blood in his stool. The caliber of his stool has not changed. His past medical history is significant for chronic constipation. Rectal examination shows a posterior mucosal tear of the anus. Which of the following is the most appropriate next step in management?
. Colonoscopy
. Local anesthetic and stool softeners
. Lateral sphincterotomy
. Antibiotics
. Gradual dilatation of the sphincter
60) A 27-year-old man complains of episodic abdominal pain. The pain is concentrated in the epigastrium and is gnawing in quality. It wakes him up during the night and is promptly relieved by a glass of water and a piece of bread. He denies vomiting or diarrhea, but has experienced an occasional "dark stool." He has no significant past medical history and does not take any medications. His family history is significant for biliary disease in his mother and stomach cancer in his father. He smokes one pack of cigarettes a day and consumes a can of beer almost every day. His vital signs are with in normal limits. Physical examination shows mild epigastric discomfort on deep palpation. Which of the following is most likely to provide long-term symptom relief in this patient?
. Four weeks of omepra zole
. Antibiotics and pantoprazole
. NSAIDs as needed
. Smoking cessation
. No alcohol consumption
61) A 55-year-old obese male presents to his physician for a routine annual physical examination. A review of systems is insignificant, except for constipation which has been present for several years. He does not have major medical problems and is not on any prescription or over-the-counter medications. He has smoked one and- a-half packs of cigarettes daily for 30 years. He drinks 4 oz of alcohol daily. Physical examination is unremarkable. As part of the routine screening, a colonoscopy is performed, which shows multiple diverticuli at the sigmoid colon. He is concerned about the diverticulosis. Which of the following is the most appropriate next step in the management of this patient's diverticulosis?
. Advise him to stop smoking
. Advise him to stop drinking alcohol
. Increase dietary fiber intake
. Explain his surgical options
. Educate about prophylactic antibiotics
62) A 56-year-old woman with cirrhosis presents with a 2-week history of increasing abdominal distension. She has mild encephalopathy and esophageal varices without bleeding. Her cirrhosis is due to chronic hepatitis type B. She has a past history of ascites treated successfully with conservative management. She is currently on sodium, water and protein restriction, maximal doses of spironolactone and furosemide, and lactulose. Her temperature is 36.6°C (97.9°F), blood pressure is 120/70 mmHg, pulse is 80/min, and respirations are 30/min. She has a flapping tremor and labored breathing. Abdominal examination shows marked abdominal distension. An x-ray film of the chest is unremarkable. Abdominal ultrasound shows peritoneal fluid and splenomegaly, liver hyperechogenicity and nodularity, and portal vein width of 16 mm; no masses are evident. Which of the following is the most appropriate next step in the management of this patient's ascites?
. Intravenous furosemide therapy
. Tapping of some amount of ascitic fluid
. Peritonea-jugular shunt
. Distal spleno-renal shunt (selective shunt)
. Side-to-side porto-caval shunt (non-selective shunt)
63) A 52-year-old woman with cirrhosis presents with increasing abdominal distension. Her treatment regimen was amended three days ago, when furosemide was added to spironolactone and sodium/water restriction. However, her distension persists, and today she is very somnolent and has passed very little urine. Her past medical history is remarkable for chronic hepatitis type B, cirrhosis, encephalopathy, and 2 bleeding episodes from esophageal varices; the bleeding was controlled with sclerotherapy. Her temperature is 36.5°C (97.6°F), blood pressure is 90/60 mm Hg, pulse is 80/min, and respirations are 18/min. Abdominal examination shows distension, shifting dullness, and no tenderness; bowel sounds are present. Laboratory studies show: Hemoglobin 11.0 g/L, Leukocyte count 3,500/mm3, Serum sodium 125 mEq/L, Serum potassium 5.5 mEq/L, Chloride 103 mEq/L, Blood urea nitrogen 60 mg/dL, Serum creatinine 1.8 mg/dL, Prothrombin time 18 sec, Partial thromboplastin time 35 sec. Urinalysis shows no abnormalities. Ultrasound of the kidney is unremarkable. Which of the following is the most appropriate next step in management?
. Increase the dose of furosemide to its maximum
. Careful volume loading and discontinuation of furosemide and spironolactone
. Tapping of ascites
. Renal biopsy
. Intravenous pyelography
64) A 34-year-old Caucasian male presents to the office with a 4-week history of diarrhea. He just returned from a trip to South America, where he developed foul-smelling stools, abdominal cramps and bloating. A three-day course of ciprofloxacin did not relieve his symptoms. His vital signs are within normal limits. Physical examination shows no abnormalities. Which of the following is the most appropriate next step in management?
. Schedule colonoscopy
. Obtain CT scan of the abdomen
. Prescribe oral metronidazole
. Prescribe another course of ciprofloxacin
. Prescribe oral ampicillin
65) A 65-year-old male complains of fatigue for the past one month. He has been living alone since the death of his wife one year ago. He does not like to cook, and his diet consists mostly of canned food, hot tea, and toast. He drinks one glass of white wine nightly with dinner. Examination shows pallor of the skin, nail beds and conjunctiva. Rectal exam is heme-negative. His physical examination is otherwise unremarkable. Administration of which of the following would be most helpful in treating his condition?
. Vitamin B12
. Folic acid
. Vitamin C
. Vitamin D
. Vitamin E
66) A 33-year-old male is admitted to the hospital after an episode of tonic-clonic seizures. He is a known IV drug abuser. He admits 'shooting' cocaine and heroin prior to the seizure. He has never had seizures before. Fallowing the seizure, he complains of muscle pain but otherwise feels normal. His temperature is 37.2°C (98.9°F) and his blood pressure is 156/90 mm Hg. Laboratory analyses reveal the following: CPK 11,200 U/ml, AST 545 U/L, ALT 560U/L, Troponin T normal, Anti-HAV antibodies negative, HBsAg negative, Anti-HBsAg negative, Anti-HCV antibodies positive. He reports that a recent HIV test was negative. Which of the following is the best management for this patient?
. Fluid restriction
. Metoprolol
. Hepatitis B vaccination
. Life-long phenytoin therapy
. No intervention
67) A 40-year-old man with a recent history of exploratory laparotomy for a stabbing injury presents to the emergency department with diffuse cramping abdominal pain for 1 day, accompanied by nausea, multiple episodes of brown colored vomitus, and lack of stool, but he reports some flatulence. He denies any fever. On physical examination, the patient has stable vital signs, and there is diffuse distention in the abdomen with guarding and tenderness but no rebound, as well as high-pitched bowel sounds. Rectal examination reveals no fecal impaction in the rectal vault, and the stool was guaiac- negative. Complete blood cell count reveals no significant abnormalities and serum chemistry shows a mild metabolic alkalosis. CT demonstrates a noticeable difference in the diameter of proximal and distal small bowel. Which of the following is the most appropriate management?
Broad-spectrum antibiotics
Colonoscopy
Exploratory laparotomy with lysis of adhesions
Give the patient nothing by mouth, insert a nasogastric tube, and perform intravenous correction of electrolyte abnormalities
Serial abdominal examinations
68) A 52-year-old woman is experiencing abdominal discomfort after meals as well as early in the morning. There is no weight loss or constitutional symptoms, and she has tried antacids but experienced minimal relief. Upper endoscopy reveals a duodenal ulcer and the biopsy is negative for malignancy. Which of the following is the most appropriate next step in management?
. 6–8 weeks of omeprazole or ranitidine
. long-term acid suppression with omeprazole
. Antibiotic therapy
. Antibiotic therapy with omeprazole
. Bismuth citrate therapy
69) A 36-year-old man presents for a well-patient examination. He gives a history that, over the past 20 years, he has had three episodes of abdominal pain and hematemesis, the most recent of which occurred several years ago. He was told that an ulcer was seen on a barium upper GI radiograph. You obtain a serum assay for H pylori IgG, which is positive. What is the most effective regimen to eradicate this organism?
. Omeprazole 20 mg orally once daily for 6 weeks
. Ranitidine 300 mg orally once daily at bedtime for 6 weeks
. Omeprazole 20 mg twice daily, amoxicillin 1000 mg twice daily, and clarithromycin 500 mg twice daily for 14 days
. Pepto-Bismol and metronidazole twice daily for 7 days
. Benzathine penicillin, 1.2 million units intramuscularly weekly for three doses
70) An otherwise healthy 40-year-old woman sees you because of recurrent abdominal pain. In the past month she has had four episodes of colicky epigastric pain. Each of these episodes has lasted about 30 minutes and has occurred within an hour of eating. Two of the episodes have been associated with sweating and vomiting. None of the episodes have been associated with fever or shortness of breath. She has not lost weight. She does not drink alcohol or take any prescription or over-the-counter medications. Other than three previous uneventful vaginal deliveries, she has never been hospitalized. Her examination is negative except for mild obesity (BMI = 32). A complete blood count and multichannel chemistry profile that includes liver function test is normal. A gallbladder sonogram reveals multiple gallstones. What is the next best step in the treatment of this patient?
. Omeprazole, 20 mg daily for eight weeks
. Ursodeoxycholic acid
. Observation without specific therapy
. Laparoscopic cholecystectomy
. Weight reduction
71) A 56-year-old chronic alcoholic has a 1-year history of ascites. He is admitted with a 2-day history of diffuse abdominal pain and fever. Examination reveals scleral icterus, spider angiomas, a distended abdomen with shifting dullness, and diffuse abdominal tenderness. Paracentesis reveals slightly cloudy ascitic fluid with an ascitic fluid PMN cell count of 1000/μL. Which of the following statements about treatment is true?
. Antibiotic therapy is unnecessary if the ascitic fluid culture is negative for bacteria
. The addition of albumin to antibiotic therapy improves survival
. Repeated paracenteses are required to assess the response to antibiotic treatment
. After treatment of this acute episode, a recurrent episode of spontaneous bacterial peritonitis would be unlikely
. Treatment with multiple antibiotics is required because polymicrobial infection is common
72) A 60-year-old man with known hepatitis C and a previous liver biopsy showing cirrhosis requests evaluation for possible liver transplantation. He has never received treatment for hepatitis C. Though previously a heavy user of alcohol, he has been abstinent for over 2 years. He has had 2 episodes of bleeding esophageal varices. He was hospitalized 6 months ago with acute hepatic encephalopathy. He has a 1 year history of ascites that has required repeated paracentesis despite treatment with diuretics. Medications are aldactone 100 mg daily and lactulose 30 cc 3 times daily. On examination he appears thin, with obvious scleral icterus, spider angiomas, palmar erythema, gynecomastia, a large amount ascites, and small testicles. There is no asterixis. Recent laboratory testing revealed the following: hemoglobin = 12.0 mg/dL (normal 13.5-15.0), MCV = 103 fL (normal 80-100), creatinine = 2.0 mg/dL (normal 0.7-1.2), bilirubin = 6.5 mg/dL (normal 0.1-1.2), AST = 25 U/L (normal < 40), ALT= 45 U/L (normal < 40), INR = 3.0 (normal 0.8-1.2). What is the next best step?
. Repeat liver biopsy
. Start treatment with interferon and ribavirin
. Refer the patient for hospice care
. Continue to optimize medical treatment for his ascites and hepatic encephalopathy and tell the patient he is not eligible for liver transplantation because of his previous history of alcohol abuse
. Refer the patient to a liver transplantation center
73) A 32-year-old white woman complains of abdominal pain off and on since the age of 17. She notices abdominal bloating relieved by defecation as well as alternating diarrhea and constipation. She has no weight loss, GI bleeding, or nocturnal diarrhea. On examination, she has slight LLQ tenderness and gaseous abdominal distension. Laboratory studies, including CBC, are normal. Which of the following is the most appropriate initial approach?
. Recommend increased dietary fiber, antispasmodics as needed, and follow-up examination in 2 months
. Refer to gastroenterologist for colonoscopy
. Obtain antiendomysial antibodies
. Order UGI series with small bowel follow-through
. Order small bowel biopsy
74) A 27-year-old female is found to have a positive hepatitis C antibody at the time of plasma donation. Physical examination is normal. Liver enzymes reveal ALT of 62 U/L (normal < 40), AST 65 U/L (normal < 40), bilirubin 1.2 mg/dL (normal), and alkaline phosphatase normal. Hepatitis C viral RNA is 100,000copies/mL. Hepatitis B surface antigen and HIV antibody are negative. Which of the following statements is true?
. Liver biopsy is necessary to confirm the diagnosis of hepatitis C
. Most patients with hepatitis C eventually resolve their infection without permanent sequelae
. This patient should not receive vaccinations against other viral forms of hepatitis
. Serum ALT levels are a good predictor of prognosis
. Patients with hepatitis C genotype 2 or 3 are more likely to have a favourable response to treatment with interferon and ribavirin
75) A 45-year-old woman presents to the ED with 1 day of painful rectal bleeding. Review of systems is negative for weight loss, abdominal pain, nausea, and vomiting. On physical examination, you note an exquisitely tender swelling with engorgement and a bluish discoloration distal to the anal verge. Her vital signs are HR 105 beats per minute, BP 140/70 mm Hg, RR 18 breaths per minute, and temperature 99°F. Which of the following is the next best step in management?
. Recommend warm sitz baths, topical analgesics, stool softeners, a high-fiber diet, and arrange for surgical follow-up
Surgical follow-up . Incision and drainage under local anesthesia or procedural sedation followed by packing and surgical follow-up
. Obtain a complete blood cell (CBC) count, clotting studies, type and cross, and arrange for emergent colonoscopy
. Excision under local anesthesia followed by sitz baths and analgesics
. Surgical consult for immediate operative management
76) A 65-year-old man with a history of occasional painless rectal bleeding presents with 2 to 3 days of constant, dull RLQ pain. He also complains of fever, nausea, and decreased appetite. He had a colonoscopy 2 years ago that was significant for sigmoid and cecal diverticula but was otherwise normal. On physical examination he has RLQ tenderness with rebound and guarding. His vitals include HR of 95 beats per minute, BP of 130/85 mm Hg, and temperature of 101.3°F. The abdominal CT demonstrates the presence of sigmoid and cecal diverticula, inflammation of pericolic fat, thickening of the bowel wall, and a fluid-filled appendix. Which of the following is the most appropriate next step in management?
. Discharge the patient with broad-spectrum oral antibiotics and surgical follow-up
. Begin IV hydration and broad-spectrum antibiotics, keep the patient npo (nothing by mouth), and admit the patient to the hospital
. Begin IV antibiotics and call a surgical consult for an emergent operative procedure
. Arrange for an emergent barium enema to confirm the diagnosis
. Begin sulfasalazine 3 to 4 g/d along with IV steroid therapy
77) A 49-year-old man presents to the ED with nausea, vomiting, and abdominal pain that began approximately 2 days ago. The patient states that he usually drinks a six pack of beer daily, but increased his drinking to 2 six packs daily over the last week because of pressures at work. He notes decreased appetite over the last 3 days and states he has not had anything to eat in 2 days. His BP is 125/75 mm Hg, HR is 105 beats per minute, and RR is 20 breaths per minute. You note generalized abdominal tenderness on examination. Laboratory results reveal the following: White blood cells (WBC) 9000/μL Sodium 131 mEq/L Hematocrit 48% Potassium 3.5 mEq/L Platelets 210/μL Chloride 101 mEq/L Aspartate transaminase (AST) 85 U/L Bicarbonate 10 mEq/L Alanine transaminase (ALT) 60 U/L Blood urea nitrogen (BUN) 9 mg/dL Alkaline phosphatase 75 U/L Creatinine 0.5 mg/dL Total bilirubin 0.5 mg/dL Glucose 190 mg/dL Lipase 40 IU Nitroprusside test weakly positive for ketones Which of the following is the mainstay of therapy for patients with thiscondition?
. Normal saline (NS) solution
. Half normal saline (NS)
. Glucose solution (D5W)
. Solution containing both saline and glucose (D 5/NS or D 5 NS)
. The type of solution is irrelevant
78) A 31-year-old man from Florida presents to the ED complaining of severe pain that starts in his left flank and radiates to his testicle. The pain lasts for about 1 hour and then improves. He had similar pain last week that resolved spontaneously. He noted some blood in his urine this morning. His BP is 145/75 mm Hg, HR is 90 beats per minute, temperature is 98.9°F, and his RR is 24 breaths per minute. His abdomen is soft and nontender. As you examine the patient, he vomits and has trouble lying still in his stretcher. Which of the following is the most appropriate next step in management?
. Call surgery consult to evaluate the patient for appendicitis
. Order an abdominal CT
. Start intravenous (IV) fluids and administer an IV nonsteroidal anti-inflammatory drug (NSAID) and antiemetic
. Perform an ultrasound to evaluate for an abdominal aortic aneurysm (AAA)
. Perform an ultrasound to evaluate for testicular torsion
79) A 22-year-old man presents to the ED complaining of dysuria for 3 days. He states that he has never had this feeling before. He is currently sexually active and uses a condom most of the time. He denies hematuria but notes a yellowish discharge from his urethra. His BP is 120/75 mm Hg, HR is 60 beats per minute, and temperature is 98.9°F. You send a clean catch urinalysis to the laboratory that returns positive for leukocyte esterase and 15 white blood cells per high power field (WBCs/hpf). Which of the following is the most appropriate next step in management?
. Send a urethral swab for culture and administer 125 mg ceftriaxone intramuscularly and 1 g azithromycin orally
. Send urine for culture and administer SMX/TMP orally
. Discharge the patient with strict instructions to return if his symptoms worsen
. Order a CT scan to evaluate for a kidney stone
. Have him follow-up immediately with a urologist to evaluate for testicular cancer
80) An 18-year-old woman presents to the ED complaining of acute onset of RLQ abdominal pain. She also describes the loss of appetite over the last 12 hours, but denies nausea and vomiting. Her BP is 124/77 mm Hg, HR is 110 beats per minute, temperature is 102.1°F, RR is 16 breaths per minute, and oxygen saturation is 100% on room air. Abdominal examination reveals lower abdominal tenderness bilaterally. On pelvic examination you elicit cervical motion tenderness and note cervical exudates. Her WBC is 20,500/μL and β-hCG is negative. Which of the following is the most appropriate next step in management?
. Bring her to the OR for an appendectomy
. Begin antibiotic therapy
. Perform a culdocentesis
. Bring her to the OR for immediate laparoscopy
. Order an abdominal plain film
81) A 30-year-old man presents to the ED complaining of sudden onset of abdominal bloating and back pain lasting for 2 days. The pain woke him up from sleep 2 nights ago. It radiates from his back to his abdomen and down toward his scrotum. He is in severe pain and is vomiting. His temperature is 101.2°F and HR is 107 beats per minute. A CT scan reveals a 9-mm obstructing stone of the left ureter with hydronephrosis. Urinalysis is positive for 2+ blood, 2+ leukocytes, 2+ nitrites, 40 to 50 WBCs, and many bacteria. You administer pain medicine, antiemetics, and antibiotics. Which of the following is the most appropriate next step in management?
. Admit for IV antibiotics and possible surgical removal of stone
. Observe in ED for another 6 hours to see if stone passes
. Discharge with antibiotics and pain medicine
. Discharge patient with instructions to consume large amounts of water
. Discharge patient with antibiotics, pain medicine, and instructions to drink large amounts of water and cranberry juice
82) A 24-year-old woman presents to the ED after being sexually assaulted. She is a college student with no past medical history. Her BP is 130/75 mm Hg, HR is 91 beats per minute, temperature is 98.6°F, and RR is 16 breaths per minute. On physical examination you observe vaginal trauma and scattered bruising and abrasions. Which of the following medications should be offered to the patient in this scenario?
. Ceftriaxone, azithromycin, metronidazole, antiretrovirals, emergency contraception
. Ceftriaxone, tetanus, metronidazole, antiretrovirals, emergency contraception
. Ceftriaxone, azithromycin, tetanus, metronidazole, emergency contraception
. Ceftriaxone, azithromycin, tetanus, antiretrovirals, emergency contraception
. Ceftriaxone, azithromycin, tetanus, metronidazole, antiretrovirals, emergency contraception
83) A 43-year-old man presents to the ED complaining of progressively worsening abdominal pain over the past 2 days. The pain is constant and radiates to his back. He also describes nausea and vomiting and states he usually drinks six pack of beer daily, but has not had a drink for 2 days. His BP is 144/75 mm Hg, HR is 101 beats per minute, temperature is 99.8°F, and RR is 14 breaths per minute. He is lying on his side with his knees flexed. Examination shows voluntary guarding and tenderness to palpation of his epigastrium. Laboratory results reveal WBC 10,500/μL, hematocrit 51%, platelets 225/μL, and lipase 620 IU. An abdominal radiograph reveals a nonspecific bowel gas pattern. There is no free air under the diaphragm. Which of the following is the most appropriate next step in management?
. Observe in the ED
. Send home with antibiotic therapy
. Admit to the hospital for endoscopy
. Admit to the hospital for exploratory laparotomy
. Admit to the hospital for medical management and supportive care
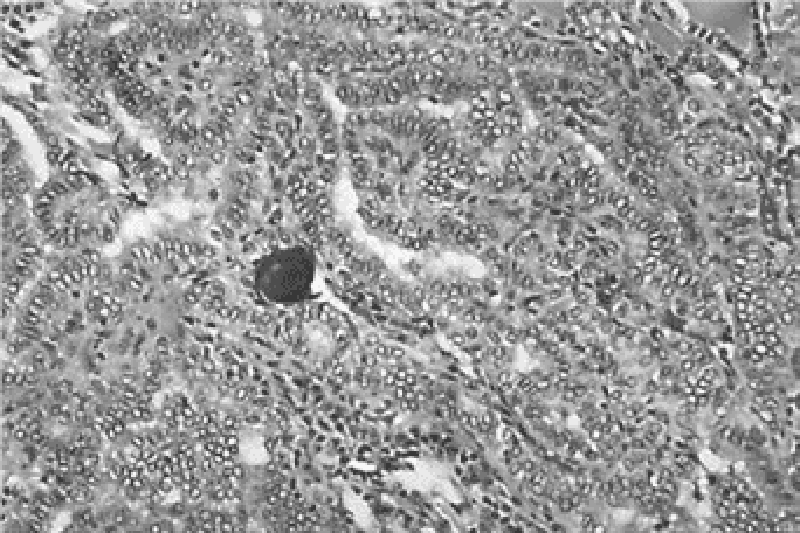
84) A 76-year-old man who has had multiple episodes of pancreatitis presents to his physician’s office with mild epigastric pain and 9.1-kg (20.0-lb) weight loss over the past 6 months. The patient also describes daily foul-smelling stools that “float” in the toilet bowl. The physician pulls up his electronic medical record and finds that the patient presented to the emergency department last week for the same symptoms. During that visit he had a CT of the abdomen (see image). Which of the following is the most appropriate treatment?
Endoscopic retrograde cholangiopancreatography
Pancreatic enzyme replacement
Pancreaticogastrostomy
Surgical resection of pancreas
Whipple procedure
85) A 34-year-old man presents with substernal discomfort. The symptoms are worse after meals, particularly a heavy evening meal, and are sometimes associated with hot/sour fluid in the back of the throat and nocturnal awakening. The patient denies difficulty swallowing, pain on swallowing, or weight loss. The symptoms have been present for 6 weeks; the patient has gained 20 lb in the past 2 years. Which of the following is the most appropriate initial approach?
. Therapeutic trial of ranitidine
. Exercise test with thallium imaging. Esophagogastroduodenoscopy
. Esophagogastroduodenoscopy
. CT scan of the chest
. Coronary angiography
86) A 48-year-old man with a past medical history of hepatitis C and cirrhosis presents to the ED complaining of acute-onset abdominal pain and chills. His BP is 118/75 mm Hg, HR is 105 beats per minute, RR is 16 breaths per minute, temperature is 101.2°F rectally, and oxygen saturation is 97% on room air. His abdomen is distended, and diffusely tender. You decide to perform a paracentesis and retrieve 1 L of cloudy fluid. Laboratory analysis of the fluid shows a neutrophil count of 550 cells/mm 3. Which of the following is the most appropriate choice of treatment?
. Metronidazole
. Vancomycin
. Sulfamethoxazole/trimethoprim (SMX/TMP)
. Neomycin and lactulose
. Cefotaxime
87) A 29-year-old woman complains of dysphagia with both solids and liquids, worse when she is eating quickly or is anxious. Manometry reveals normal basal esophageal sphincter pressure, with no relaxation of the sphincter on swallowing. Which of the following is the most appropriate next step in management?
. beta-blocker therapy
. Partial esophagectomy
. Anticholinergic drugs
. Calcium channel blockers
. Dietary modification
88) A 39-year-old Japanese-American woman with insulin-dependent diabetes and asthma presents to her primary care physician complaining of trouble swallowing for the past few months. She explains that it started with solids, and then progressed to liquids. She states it now is hard even to swallow water and that she is often very thirsty. She says she has lost about 3.2 kg (7 lb), but says she is working out frequently. Her blood pressure is 118/76 mm Hg, pulse is 86/min, respiratory rate is 16/min, and temperature is 37.2°C (98.9°F). Laboratory tests show: Na+: 144 mEq/L, K+: 4.0 mEq/L, Cl−: 100 mEq/L, Carbon dioxide: 22 mmol/L Blood urea nitrogen: 18 mg/dL Creatinine: 1.0 mg/dL, Glucose: 88 mg/dL. Her hemoglobin A1c level, measured 3 months earlier, was 6.1%. A barium swallow is performed, which reveals a dilated esophagus, especially distally, that flares out near the lower esophageal junction. Still not completely sure of the diagnosis, esophageal manometry is performed, which reveals abnormal peristalsis and increased lower sphincter pressure. Which of the following is the most appropriate management?
Cholinergic agents
Glucose pharmacotherapy
Instructions to elevate the bed, avoid fatty foods, and consider a histamine blocker
Pneumatic dilation
Surgery to remove diverticula
89) A 55-year-old man is brought to the ED by his family. They state that he has been vomiting large amounts of bright red blood. The patient is an alcoholic with cirrhotic liver disease and a history of portal hypertension and esophageal varices. His vitals on arrival are HR 110 beats per minute, BP 80/55 mm Hg, RR 22 breaths per minute, and temperature 99°F. The patient appears pale and is in moderate distress. Which of the following is an inappropriate option in the initial management of a hypotensive patient with a history of known esophageal varices presenting with hematemesis?
. Sengstaken-Blakemore tube placement
. Two large-bore IV lines and volume repletion with crystalloid solutions
. Nasogastric (NG) lavage
. IV octreotide
. Gastrointestinal (GI) consult
90) A 59-year-old woman presents to the ED complaining of worsening lower abdominal pain over the previous 3 days. She describes feeling constipated recently and some burning when she urinates. Her BP is 135/75 mm Hg, HR is 89 beats per minute, temperature is 101.2°F, and her RR is 18 breaths per minute. Her abdomen is mildly distended, tender in the LLQ, and positive for rebound tenderness. CT scan is consistent with diverticulitis with a 7-cm abscess. Which of the following is the most appropriate management for this condition?
. Reserve the OR for emergent laparotomy
. Start treatment with ciprofloxacin and metronidazole and plan for CT-guided draining of the abscess
. Give an IV dose of ciprofloxacin and have the patient follow up with her primary physician
. Start treatment with ciprofloxacin and metronidazole and plan for an emergent barium enema
. Start treatment with ciprofloxacin and metronidazole and prepare for an emergent colonoscop
91) A 60-year-old man is brought to the ED complaining of generalized crampy abdominal pain that occurs in waves. He has been vomiting intermittently over the last 6 hours. His BP is 150/75 mm Hg, HR is 90 beats per minute, temperature is 99.8°F, and his RR is 16 breaths per minute. On abdominal examination you notice an old midline scar across the length of his abdomen that he states was from surgery after a gunshot wound as a teenager. The abdomen is distended with hyperactive bowel sounds and mild tenderness without rebound. An abdominal plain film confirms your diagnosis. Which of the following is the most appropriate next step in management?
. Begin fluid resuscitation, bowel decompression with a nasogastric tube, and request a surgical consult
. Begin fluid resuscitation, administer broad-spectrum antibiotics, and admit the patient to the medical service
. Begin fluid resuscitation, give the patient stool softener, and administer a rectal enema
. Begin fluid resuscitation, administer broad-spectrum antibiotics, and observe the patient for 24 hours
. Order an abdominal ultrasound, administer antiemetics, and provide pain relief
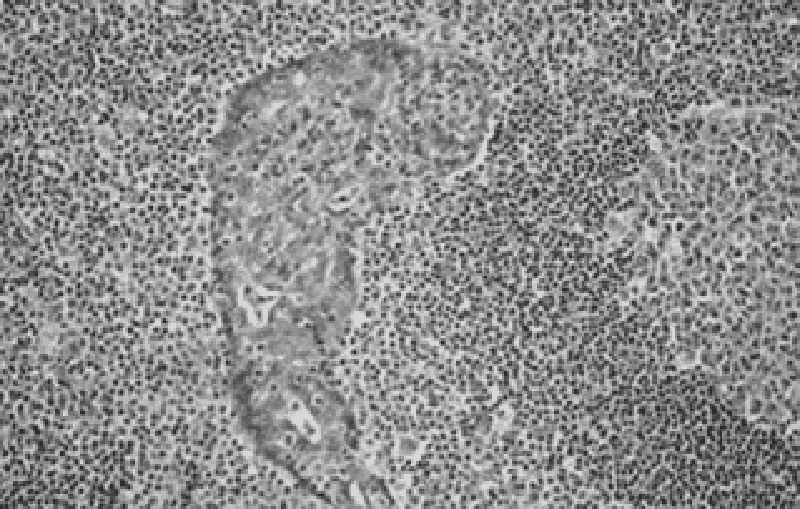
92) A 54-year-old man presents to his primary care provider with the complaint of upper abdominal fullness and pain. He states that he has lost 2.3-4.6 kg (5-10 lb), but denies other symptoms. Physical examination reveals a firm mass in the epigastric area. Ultrasonography reveals a mass in the gastric antrum. A salivary gland biopsy reveals the pathology shown in the image. Which of the following therapies is expected to be part of his treatment plan?
Antibiotic therapy
Bone marrow transplantation
Gene therapy
Liver transplantation
Multiagent chemotherapy
93) A 68-year-old African-American man presents to his primary care physician for a check-up. He has not been to the physician’s office in over 15 years. He reports that he is fine but that his wife keeps telling him that he has to “go see the doctor.” He says he has never been sick, despite smoking three packs of cigarettes per day for over 40 years. He also says that he drinks 2–3 beers a night but never had a problem with that either. He’s as healthy “as a bull,” he says. His wife is in the room and says that he recently has had some problems swallowing food and that he is losing weight. He laughs and says, “I just need to chew more and eat more.” His vital signs are normal, as are his laboratory values. The physician is concerned and orders an endoscopy, which reveals a biopsy positive for squamous cell carcinoma of the esophagus. Which of the following most likely could have prevented this condition?
Avoiding fruits and vegetables
Eating more meats, especially smoked meats
Eliminating smoking and alcohol consumption
Getting a colonoscopy every 5 years
Taking proton pump inhibitors regularly
94) A full-term 6-day-old boy presents to a physician’s office for routine care. He is tolerating breast milk well. He is urinating, defecating, and sleeping normally. Physical examination reveals an alert new-born with mild eczema, good skin turgor, normal reflexes, and a musty odor. His newborn laboratory screen is notable for phenylketones in the urine. What is the best advice to give his parents regarding the boy’s diet?
Increase iron
Increase niacin
Increase phenylalanine
Increase tyrosine
Increase vitamin D
95) A 34-year-old woman complains bitterly of heartburn. Physical examination reveals healing lesions of the fingertips that she says were small ulcers, and there are small areas of telangiectasias on her face. Esophageal manometry reveals a decrease in the expected amplitude of smooth muscle contraction. Lower esophageal sphincter tone is subnormal, but relaxes normally with swallowing. Which of the following statements regarding this condition is most likely correct?
. Characterized by systemic signs of inflammation
. Predominantly treated symptomatically
. Characterized by a poor prognosis
. Usually more frequent in men
. Characterized by death secondary to a renal crisis
96) A 61-year-old man in previously excellent health presents to his physician with com- plaints of hematochezia tenesmus, and rectal pain. On work-up the physician discovers that he has a rectal tumor that is 5 cm (2.0 in) from the anal verge. Which of the following is the most appropriate treatment?
Abdominoperineal resection
Imatinib
Low anterior resection
Radiation alone
Radiation plus chemotherapy
97) A 62-year-old woman presents to her physician with complaints of heartburn, fatigue, and intermittent upper abdominal pain. The pain is often worse after meals and especially with spicy foods. She reports no recent nausea, vomiting, weight loss, dysphagia, or bright-red blood per rectum. However, her stools are darker than normal. Her last colonoscopy 2 years ago was unremarkable. Stool guaiac test result is positive. An initial complete blood cell count reveals: Hemoglobin: 10.1 g/dL, Hematocrit: 33.2%, Mean corpuscular volume: 74.6/mm³, Mean corpuscular hemoglobin concentration: 25.8%, WBC count: 9200/mm³ Platelet count: 176,000/mm³ Ferritin: 11 ng/mL. The patient undergoes upper endoscopy, which reveals erosive gastritis. She is started on omeprazole, 40 mg twice a day and oral iron sulfate supplementation, 325 mg three times a day with meals. Six months into treatment, abdominal pain and heartburn are resolved, but the patient still has fatigue and is pale. Repeat laboratory tests show: Hemoglobin: 9.9 g/dL, Hematocrit: 30.2%, Mean corpuscular volume: 74.2/mm³, Mean corpuscular hemoglobin concentration: 25.1% , WBC count: 9800/mm³ Platelet count: 198,000/mm³ Ferritin: 10 ng/mL. Repeat upper endoscopy is negative for bleeding and erosive gastritis. Stool guaiac test result is negative. Which of the following is the next best step in management?
Bone marrow biopsy
Determine blood type and screen for transfusion
Discontinue omeprazole therapy
Initiate darbepoetin therapy
Initiate parenteral iron therapy
98) A 58-year-old nurse with node-positive metastatic breast cancer comes to the office for her monthly follow-up visit. The tumor is estrogen receptor (ER) and progesterone receptor (PR) positive, and her whole body bone scan is positive for metastatic disease. She is being treated with systemic chemotherapy and hormonal therapy (Tamoxifen). She feels weak with vague muscle, joint, and bone pains. Physical examination reveals a hard, well-defined dominant mass in the left breast. Mucus membranes are moist. Laboratory studies show the following results. Sodium 145 mEq/dL, Potassium 3.9 mEq/dL, Chloride 103 mEq/dL, Bicarbonate 24 mEq/dL, Calcium 11.3 mg/dl, BUN 18 mg/dl, Creatinine 0.8 mg/dl, Glucose 146 mg/dl. Which of the following is the best next step in the management of her hypercalcemia?
. Corticosteroid therapy
. Zoledronic acid therapy
. Intravenous normal saline
. Furosemide therapy
. Intravenous mithramycin
99) You are called to the oncology floor to examine a 57-year-old female who is complaining of severe nausea and vomiting. Her other symptoms include some general malaise and a sore throat. She is receiving combination ABVD chemotherapy (Doxorubicin, Bleomycin, Prednisone, and Procarbazine). She was diagnosed with stage II Hodgkin's lymphoma 4 weeks ago. She tells you that she does not want to continue her therapy anymore since it is "making life even more miserable." She has lost 30 lbs (12.6kg) in a month. Her temperature is 38.5°C (101.3°F), pulse is 88/min, respirations are 18/min, and blood pressure is 109/68mm Hg. Her pulse oximetry reading in room air is 92%. Physical examination reveals a significantly cachectic patient with a dry mouth, enlarged cervical lymph nodes and hepatomegaly. How can this patient's vomiting be best managed?
. Stop the chemotherapy drugs
. Ondansetron
. Metoclopramide
. Tell the patient that her nausea will get better with time
. Prochlorperazine
100) An 80-year-old man with advanced prostate cancer and bony metastasis is complaining of severe back pain that has been progressively worsening for the past two weeks. His pain is so severe that it restricts him from playing golf. Eight months ago, he underwent orchiectomy, after which he was free from bone pain until now. Physical examination reveals tenderness at two sites in the lumbar region. Radionuclide bone scan shows an increased uptake in these areas. Which of the following is the most appropriate next step in the management of this patient?
. Cervical cordotomy
. Etidronate disodium therapy
. Flutamide therapy
. Hypophysectomy
. Radiation therapy
101) A 65-year-old Hispanic male is brought to the emergency department after having one seizure episode. His past medical history is significant for non-small cell lung carcinoma, which was diagnosed two years ago and treated surgically. He had no residual disease at that time. CT scan of the brain with contrast now shows a solitary cortical mass in the right hemisphere of the brain at the grey-white matter junction. His chest x-ray is clear. He is admitted for further management and started on phenytoin. Which of the following is the most appropriate management for this patient?
. Focal radiation to brain mass
. Whole brain radiation
. Surgical resection of the mass
. Combination chemotherapy
. Palliative pain therapy and seizure prophyl
102) A 35-year-old Caucasian female is hospitalized with swelling and tenderness of her right calf. Deep venous thrombosis is diagnosed through imaging studies, and the appropriate therapy is initiated. Three days later, she complains of right arm pain. Physical examination reveals a cold right upper extremity with no palpable peripheral pulse. Her laboratory values are listed below: Hematocrit 42%, WBC count 8,500/mm3, Platelets 76,000/mm3, PT 13 sec, aPTT 63 sec. Which of the following drugs was most likely used to treat this patient's deep venous thrombosis?
. Aspirin
. Danaparoid
. Enoxaparin
. Unfractionated heparin
. Warfarin
103) A 21-year-old previously healthy man presents to your office for a routine check-up. He has no current complaints. He does not smoke or consume alcohol. His family history is significant for cystic fibrosis in his older brother. He is sexually active with one partner and uses condoms regularly. He visits a dentist twice per year. His temperature is 36.6°C (97.9°F), pulse is 78/min, respirations are 14/min, and blood pressure is 120/76 mmHg. Physical examination reveals several non-tender, rubbery cervical lymph nodes, each measuring approximately 1 cm in diameter. There is no hepatosplenomegaly. Which of the following is the best next step in management of this patient?
. Lymph node biopsy
. Dicloxacillin
. Prednisone
. Erythromycin
. Observation
104) A 32-year-old Caucasian female presents to your office for a routine check-up. Her past medical history is significant for generalized seizures controlled with chronic phenytoin therapy. The last seizure was six months ago. She does not smoke or consume alcohol. Physical examination is insignificant, except mild pallor. Laboratory values are: Hb 10.8 g/dL, MCV 105 fl, Platelet count 180,000/cmm, Leukocyte count 7,500/cmm, Segmented neutrophils 68%, Bands 1%, Eosinophils 1%, Lymphocytes 24%, Monocytes 6%. Which of the following supplementations could have prevented this patient's anemia?
. Folic acid
. Vitamin B12
. Iron
. Vitamin B6
. Vitamin B1
{"name":"Ichigo USLME Med Management P2", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"1) A 10-year-old girl with blue eyes and blonde hair is brought to the office by her mother for a routine check-up. All her immunizations are up to date. Her family history is significant for myocardial infarction in her father and schizophrenia in a maternal uncle. There is no family history of any skin malignancies. Her height is at the 60th percentile, and weight is at the 56th percentile. While you are examining her, the mother says with much concern that she saw a television program that claimed that the incidence of skin cancer is increasing dramatically. She wants to know the best way to prevent skin cancer in her daughter, especially since they live in California. What is the best advice to help prevent malignant melanoma in this child?","img":"https://cdn.poll-maker.com/20-806090/mp2-3.png?sz=1200"}
More Quizzes
Classical dances of India quiz
16833
Imm & Asylum
21100
Driver's License Test 3A
502536
Hinduismen och Buddhismen
924651
Classic Literature - Name the Novel
201017312
Alphabetical Order - Sort the Words Correctly
201019412
Strategic Management - Free Practice Questions
15815697
Kindness Questions: Test Your Compassion - Free
201017777
What Audiobook Should I Listen To? Free
201018663
What Do I Want to Eat? Free - Get Meal Ideas
201017312
Cynicism Test - See If You Match Diogenes' Outlook
201021411
Calculus 2 - Free Practice Problems & Answers
15816879