QCU/DES/USMLE/PEDIATRIC 1-250 part1

Pediatric Medical Knowledge Quiz
Test your knowledge of pediatric medicine with our extensive 250-question quiz. Covering a wide range of topics from common conditions to emergency scenarios, this quiz is ideal for anyone looking to enhance their understanding in the field of pediatrics.
Whether you are a medical student, a healthcare professional, or just someone with an interest in pediatric health, this quiz will provide an engaging and educational experience. Key features include:
- 250 carefully curated questions
- Multiple choice format
- Immediate feedback on your answers
201. A 4-year-old girl is brought to the physician because of a crusted honey-colored erythema resulting from rupture of tiny vesicles and pustules. Her temperature is 37.7 C (102 F). Skin lesions are distributed over the face and extremities. Physical examination reveals enlargement of lymph nodes in the cervical and axillary regions. Which of the following is the most frequent pathogen of this skin infection?
A. Human herpesvirus 7
B. Staphylococcus aureus
C. Streptococcus pyogenes
E. Trychophyton fung
D. Propionibacterium acnes
202. A 4-year-old boy presents to the emergency department with generalized tonic-clonic seizures. On physical examination, the child is noted to be lethargic. His temperature is 37.4 C (99.3 F), blood pressure is 100/60 mm Hg, pulse is 72/min, and respirations are 16/min. His oral mucosa is moist, and there is no peripheral edema. Laboratory tests show: Blood: Sodium 120 mEq/L Potassium 4.2 mEq/L Chloride 96 mEq/L Bicarbonate 20 mEq/L Blood urea nitrogen 9.6 mg/dL Creatinine 0.4 mg/dL Glucose 88 mg/dL Urine: Sodium 55 mEq/L Potassium 16 mEq/L Osmolality 530 mOsmol/kg Which of the following is the most likely diagnosis?
(A) Acute renal failure
(B) Addison disease
(C) Congestive heart failure
(D) Hyponatreraic dehydration
(E) Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
203. A 1-month-old, previously healthy infant develops forceful projectile vomiting. No bile is seen in the vomitus. After the infant feeds, gastric peristaltic waves are visible crossing the epigastrium from left to right. Several minutes later, the projectile vomiting occurs. Which of the following is the most likely diagnosis?
(A) Diaphragmatic hernia
(B) Duodenal atresia
(C) Esophageal atresia
(D) Hypertrophic pyloric stenosis
(E) Meconium plug syndrome
204. A 23-year-old man comes to the emergency department (ED) at 2:00 am due to severe pain all over his body for the past few hours. He was diagnosed with sickle cell anemia at 6 months of age, and has had previous episodes of unbearable pain in his chest, abdomen, thighs and lower back. He was hospitalized six times in the past twelve months. He does not have regular follow-up visits up with his physician, and comes to see him "only if required." His blood pressure is 110/80 mmHg, pulse is 80/min, respirations are 16/min and temperature is 37 C (98F). Adequate hydration and analgesics are administered in the ED. What is the best intervention to prevent his painful episodes?
A. Folic acid supplements
B. Prophylactic antibiotics
C. Periodic blood transfusions
D. Hydroxyurea
E. Erythropoietin
205. A 5-year-old boy is brought to an emergency room because of a painful, swollen knee joint. The boy had fallen while playing, and the joint had subsequently begun to swell. The mother reports that the boy was known to have hemophilia B. Replacement of which of the following is indicated?
A. Factor C
B. Factor S
C. Factor VII
D. Factor VIII
E. Factor IX
206. A 5-month-old male infant has a urine output of less than 0.1 mL/kg/hr shortly after undergoing major surgery. On examination, he has generalized edema. His blood pressure is 94/48 mm Hg, pulse is 140/min, and respirations are 20/min. His blood urea nitrogen is 38 mg/dL, and serum creatinine is 1.4 mg/dL. Initial urinalysis shows a specific gravity of 1.018 and 2+ protein. Microscopic examination of the urine sample reveals 1 WBC per high-power field (HPF), 18 RBCs per HPF, and 5 granular casts per HPF. His fractional excretion of sodium is 3.2 %. Which of the following is the most appropriate next step in diagnosis?
A. CT of the abdomen and pelvis
B. Cystourethrography
C. Intravenous pyelography
D. Renal biopsy
E. Renal ultrasonography
207. An 8-year-old boy is brought to your office with the complaint of abdominal pain. The pain is worse during the week and seems to be less prominent during the weekends and during the summer. The patient’s growth and development are normal. The physical examination is unremarkable. Laboratory screening, including stool for occult blood, CBC, urinalysis, and chemistry panel, yields normal results. Which of the following is the best next step in the care of this patient?
A. Perform an upper GI series
B. Perform CT of the abdomen
C. Administer a trial of H2 blockers
D. Observe the patient and reassure the patient and family
E. Recommend a lactose-free diet
208. A 5-month-old girl is brought to the office by her mother, who states that the girl had an episode following feeding during which she began to breathe deeply, became blue, and then lost consciousness. The mother states that she picked her up and held her, and the infant regained her usual color and became alert. Physical examination reveals a harsh systolic murmur. Which of the following is the most likely diagnosis?
A. Aortic stenosis
B. Coarctation of the aorta
C. Patent ductus arteriosus
D. Tetralogy of Fallot
E. Ventricular septal defect
209. Physical examination of an infant delivered to a 42-year-old, gravida 3, para 2, woman, is remarkable for slight hypotonia and a poor Moro reflex. Further examination reveals upslanting palpebral fissures, epicanthal folds, excess nuchal skin, an enlarged tongue, clinodactyly of the fifth fingers, and a single transverse palmar crease. Which of the following is the most likely diagnosis?
A. Down syndrome
B. Edwards syndrome
C. Fetal alcohol syndrome
D. Marfan syndrome
E. Turner syndrome
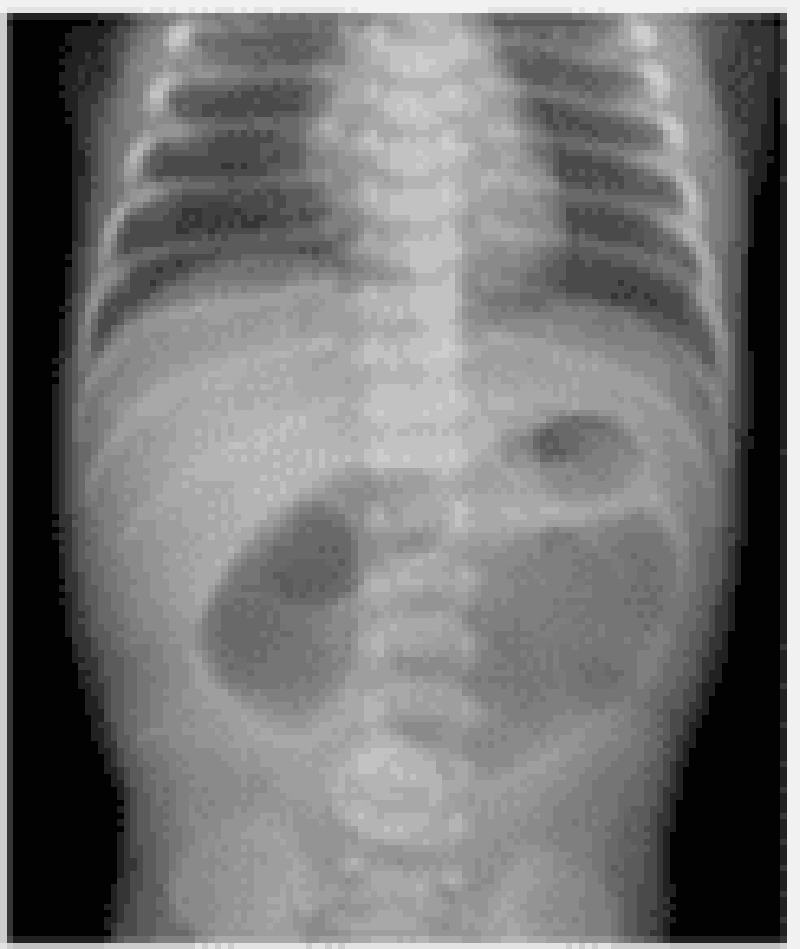
210. You are called to the newborn nursery to evaluate a term infant with bilious emesis. Although the mother had poor prenatal care, she had a normal vaginal delivery with no complications. The infant began having bilious vomiting several hours after birth. The infant has urinated, but has not had a bowel movement. Vital signs are temperature 36.9 0C (98.4 0F), pulse 150/min, and respiratory rate 40/min. On examination, the abdomen is distended and there are decreased bowel sounds. The remainder of the physical examination is unremarkable. An abdominal radiograph is shown below. Which of the following is the most likely diagnosis?
A. Pyloric stenosis
B. Intestinal atresia
C. Hirschsprung disease
D. Necrotizing enterocolitis
E. Gastroesophageal reflux
211. A 2-month-old child of an HIV-positive mother is followed in your pediatric practice. Which of the following therapies should be considered for this child?
B. Prophylaxis against Pneumocystis jiroveci pneumonia (Pneumocystis carinii)
A. Monthly evaluation for Kaposi sarcoma
C. Vitamin C supplementation
D. Oral polio virus vaccine
E. Bone marrow transplantation
212. A 10-month-old infant on long-term aspirin therapy for Kawasaki disease develops sudden onset of high fever, chills, diarrhea, and irritability. A rapid swab in your office identifies influenza A, adding her to the long list of influenza patients you have seen this December. Over the next few days, she slowly improves and becomes afebrile. However, 5 days after your last encounter you hear from the hospital that she has presented to the emergency center obtunded and posturing with evidence of liver dysfunction. Which of the following statements about her current condition is correct?
A. With proper supportive care, the overall mortality rate is low.
B. With her progressiveliver dysfunction, increased total serum bilirubin is anticipated.
C. Administration of N-acetylcysteine is first-line therapy.
D. Seizures are uncommon with this condition.
E. Death is usually associated with increased intracranial pressures and herniation.
213. The parents of a 7-month-old boy arrive in your office with the child and a stack of medical records for a second opinion. The boy first started having problems after his circumcision in the nursery when he had prolonged bleeding. Studies were sent at the time for hemophilia, but factor VIII and IX activity were normal. At 2 months he developed bloody diarrhea, which his doctor assumed was a milk protein allergy and changed him to soy; his parents note he still has occasional bloody diarrhea. He has seen a dermatologist several times for eczema, and he has been admitted to the hospital twice for pneumococcal bacteremia. During both admissions, the parents were told that the infant’s platelet count was low, but they have yet to attend the hematology appointment arranged for them. The child’s WBC count and differential were normal. Which of the following is the most likely diagnosis in this child?
A. Idiopathic thrombocytopenic purpura
B. Wiskott-Aldrich syndrome
C. Acute lymphocytic leukemia
D. Adenosine deaminase deficiency
E. Partial thymic hypoplasia
214. A one-day-old infant with Down syndrome has developed persistent vomiting. He was delivered vaginally at 34 weeks without any complications. On examination, he appears dehydrated and slightly tachypneic. His abdomen is soft and not distended. Abdominal x-ray reveals two large distinct air bubbles, but there are no dilated bowel loops or air fluid levels. What is the most likely diagnosis of this patient?
B. Reflux disorder
A. Pyloric stenosis
C. Tracheoesophageal fistula
D. Bowel obstruction
E. Duodenal atresia
215. A 10-year-old boy from the Connecticut coast is seen because of discomfort in his right knee. He had a large, annular, erythematous lesion on his back that disappeared 4 weeks prior to the present visit. His mother recalls pulling a small tick off his back. Which of the following is a correct statement about this child’s likely illness?
A. Thetickwasprobablya Dermacentor andersoni.
B. The disease is caused by a rickettsial agent that is transmitted by the bite of a tick.
C. In addition to skin and joint involvement, CNS and cardiac abnormalities may be present.
D. Therapy with antibiotics has little effect on the resolution of symptoms.
E. The pathognomonic skin lesion is required for diagnosis.
216. Two weeks ago, a 5-year-old boy developed diarrhea, which has persisted to the present time despite dietary management. His stools have been watery, pale, and frothy. He has been afebrile. Microscopic examination of his stools is likely to show which of the following?
a. Salmonella sonnei
B. Enterobius vermicularis
C. Sporothrix schenckii
D. Toxoplasmagondii
E. Cryptosporidium
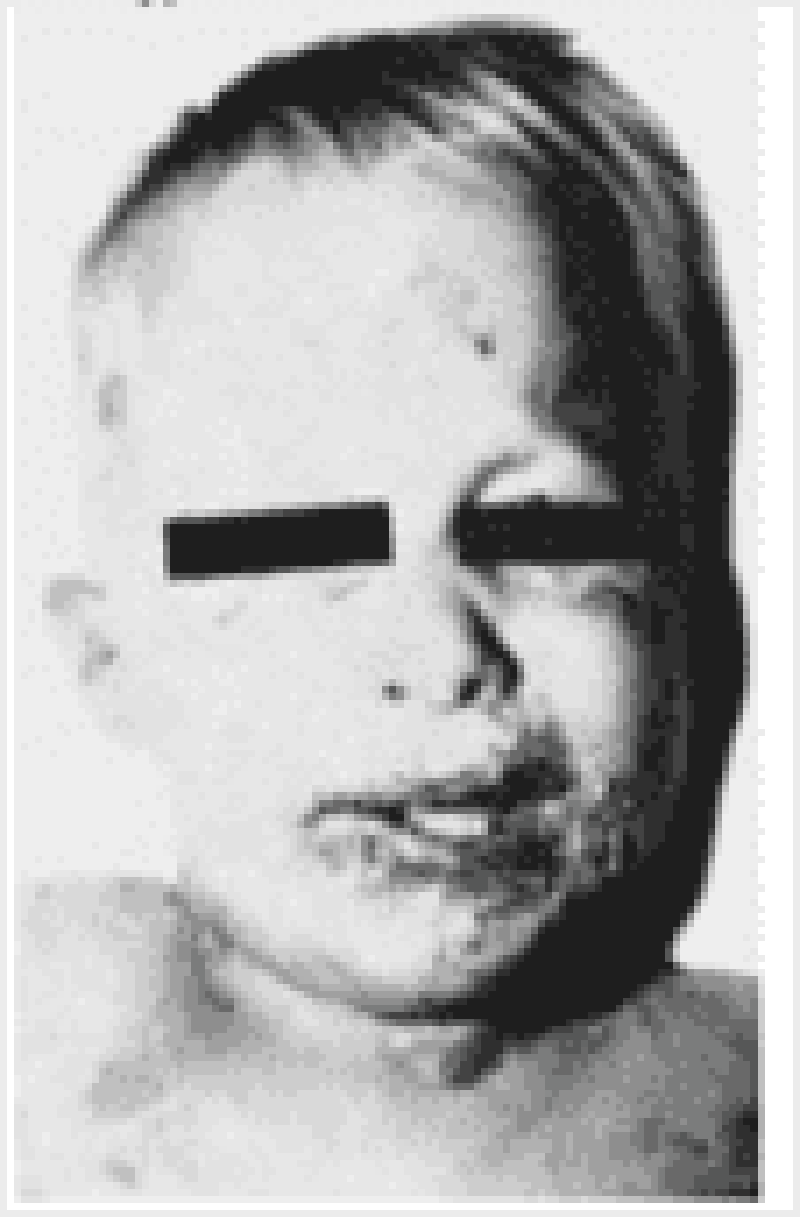
217. The rash and mucous membrane lesions shown in the photograph below develop in an infant 5 days into the course of an upper respiratory infection with otitis media; the child is being treated with amoxicillin. The child’s condition is likely which of the following?
A. Urticaria
B. Rubeola
C. Stevens-Johnson syndrome
D. Kawasaki disease
E. Scarlet fever
218. A 6-year-old boy is brought to the physician for evaluation of behavior problems. His parents report he is "hyperactive all the time." They cannot get him to sit still. When he does sit, he fidgets and tries to get out of his seat. He is easily distracted and frequently changes from one activity to another. He does not seem to listen when his parents talk to him, and often forgets to do his chores. He talks excessively and often interrupts other people. His parents state that he has been like this for a few years, but they had originally assumed his behavior was normal for his age. His physical examination is unremarkable. Which of the following will be of most help in establishing the diagnosis?
A Family history of similar behavior
B. Educational testing
C. Teacher evaluations
D. Sleep history
E. Symptoms of an anxiety disorder
219. An 18-month-old girl is brought to the hospital with a history of 6 days of bloody diarrhea. She has been drinking well but has not been wetting her diaper. She has been irritable. On physical examination, she has periorbital edema. She appears pale and is tachycardic. Her CBC shows a hemoglobin of 6 g/dL and a platelet count of 100,000/mm3. Her blood urea nitrogen (BUN) is 50 mg/dL and creatinine is 5.5 mg/dL. Her urinalysis shows gross hematuria. Which of the following is the most likely causative organism for her clinical problem?
(A) E. coli 0157:H7
(B) group A Streptococci
(C) group B Streptococci (GBS)
(D) S. aureus
(E) the cause of this illness is not known
220. A 1-year-old child with ALL in remission for 3 months is in the office for a health maintenance visit. He is due for multiple vaccinations including hepatitis B vaccine, inactivated polio vaccine (IPV), varicella vaccine H. influenzae B vaccine (Hib), and pneumococcal vaccine (PCV). You remember that some of these vaccines are live attenuated viruses and are contraindicated in immunocompromised patients. Which vaccine will you not give to this patient?
(A) PCV
(B) varicella vaccine
(C) hepatitis B vaccine
(D) Hib
(E) IPV
221. A 3-month-old Jewish infant is brought to the emergency department because of a generalized seizure 1 hour ago. He is lethargic, weighs 2.7kg (61b), and has a doll-like face with fat cheeks, relatively thin extremities, and a protuberant abdomen. His liver is felt 5cm (2in) below the right costal margin. His kidneys are enlarged. His blood sugar level is 40mg/dl. His serum uric acid, total cholesterol, triglycerides and lactic acid levels are elevated. The levels of his liver transaminases are normal. What is the most likely cause of this infant's symptoms?
A. Glucose-6-phosphatase deficiency
B. Acid maltase deficiency
C. Deficiency of glycogen debranching enzyme activity
D. Deficiency of branching enzyme activity
E. Liver phosphorylase deficiency
222. An 8-year-old boy is brought to the office due to headaches and impaired walking. These symptoms started seven days ago, and progressed gradually. He just recently recovered from otitis media that was superimposed on an acute respiratory infection. His past medical history is significant for three episodes of otitis media and one episode of pneumonia. His temperature is 36.7C(98F), blood pressure is 100/60 mm Hg, pulse is 11 0/min, and respirations are 20/min. Physical examination reveals mild right-sided hemiparesis and a slightly dilated left pupil. The funduscopic examination is normal. Which of the following is the most likely diagnosis?
A. Brain abscess
B. Bacterial meningitis
C. Toxoplasmosis
D. Venous thrombosis
E. Arterial thrombosis
223. A 1-day-old male infant has bilious vomiting after every feeding. He hasn't passed any stools yet. He had no prenatal care, and was delivered vaginally at term. He weighs 3kg (6.61b), and his APGAR scores were 6 and 7 at 1 min and 5 min, respectively. On examination, the neonate is hypotonic, he has a flat facial profile, short ears with downfolding ear lobes, a single palmar crease, and a depressed fontanel. There is abdominal distention which is most prominent in the upper abdomen. His abdominal x-rays show gastric and duodenal gas distension with no air distally. What other anomaly can also be expected in this infant?
A. Sigmoid volvulus
B. Meconium plug syndrome
C. Hirschsprung's disease
D. Intussusception
E. Meckel's diverticulum
224. A 14-year-old boy is brought to the emergency room because of persistent midepigastric pain for two days. The pain is getting no better, yet it is no worse, and radiates to his back. The boy also has had fever, as well as nausea and vomiting that is worse when his temperature rises in the afternoon. On examination, his temperature is 39.2 C (102.5 F) and there is marked upper abdominal tenderness with guarding. Mild abdominal distention is present with no audible bowel sounds. A complete blood count reveals an elevated leukocyte count and a normal serum amylase. Which of the following is the most likely diagnosis?
A. Fitz-Hugh-Curtis syndrome
B. Intussusception
C. Wilms tumor
D. Pancreatitis
E. Pyelonephritis
225. A baby is born at 34 weeks gestation. The amniotic fluid is brown and murky. The baby has low APGAR scores and appears to be septic, with lethargy, apnea, bradycardia, and temperature instability. The mother lives on a farm and gives a history of a flu-like illness one month before delivery. Gram's stain of a smear from the mother's cervix demonstrates abundant, pleomorphic, gram-variable coccobacillary forms. Which of the following is the most likely diagnosis?
B. Congenital rubella
A. Congenital cytomegalovirus infection
C. Congenital syphilis
D. Neonatal herpes simplex infection
E. Neonatal listeriosis
226. A 14-year-old black male comes to the office for the evaluation of pain in his right hip that started several weeks ago. The pain has gradually progressed, and now it limits his daily activities. He has sickle cell disease and was hospitalized three months ago due to a painful crisis that was successfully treated with hydration, oxygen, and analgesics. His temperature is 37.2C (99F), blood pressure is 100/70 mmHg, pulse is 80/min, and respirations are 16/min. Physical examination reveals no local tenderness, but there is restriction of abduction and internal rotation of the hip What is the most likely diagnosis?
A. Osteomyelitis caused by Salmonella
B. Osteomyelitis caused by Staphylococcus
C. Joint effusion from septic arthritis
D. Avascular necrosis
E. Femoral fracture
227. A 9-year-old boy is brought to the emergency department by his father due to a sudden onset of difficulty with writing and jerky movements. He recently had a mild sore throat which quickly resolved, but now seems to have recurred and have worsened. He also had a low-grade fever last week, but no chills. Physical examination reveals a pericardial friction rub and subcutaneous nodules over the hands. Laboratory studies show an elevated ESR. What is the most likely cause of this child's symptoms?
A. Group A streptococcus
B. Mycoplasma pneumoniae
C. Respiratory syncytial virus
D. Paramyxovirus
E. Epstein-Barr virus
228. A 6-year-old Caucasian male is brought to your office with a two-week history of right shoulder pain. Physical examination reveals localized swelling below the shoulder joint, and x-ray shows a single lytic lesion in the right humeral head. Laboratory analyses show mild hypercalcemia but are otherwise within normal limits. Which of the following is the most likely diagnosis?
A. Osteoporosis
B. Sarcoidosis
C. Langerhans histiocytosis
D. Primary hyperparathyroidism
E. Osteogenesis imperfect
229. An infant is born prematurely and is small for gestational age. At birth, the infant is obviously ill with jaundice, fever, hepatosplenomegaly, myocarditis, and rashes. Neurologic involvement is prominent, with hydrocephalus, intracranial calcifications, and seizures. The mother has a cat and continued to clean the cat's litter box during the pregnancy. Which of the following is the most likely causative agent?
A. Cytomegalovirus
B. Herpes simplex
C. Rubella virus
D. Toxoplasma
E. Treponema pallidum
230. A 17-year-old adolescent female is 6 weeks postpartum. She presents to the emergency room with the complaints of increased jaundice, abdominal pain, nausea, vomiting, and fever. Her examination is remarkable for jaundice, pain of the right upper quadrant with guarding, and a clear chest. Chest radiographs appear normal. Which of the following tests is most likely to reveal the cause of this pain?
B. Complete blood count (CBC) with platelets and differential
A. Serum chemistries
C. Ultrasound of the right upper quadrant
D. Upper GI series
E. Hepatitis panel
231. An 8-year-old is accidentally hit in the abdomen by a baseball bat. After several minutes of discomfort, he seems to be fine. Over the ensuing 24 hours, however, he develops a fever, abdominal pain radiating to the back, and persistent vomiting. On examination, the child appears quite uncomfortable. The abdomen is tender, with decreased bowel sounds throughout, but especially painful in the midepigastric region with guarding. Which of the following tests is most likely to confirm the diagnosis?
A. Serum amylase levels
B. CBC with differential and platelets
C. Serum total and direct bilirubin levels
D. Abdominal radiograph
E. Electrolyte panel
232. A 10-month-old baby boy, recently adopted from Guyana, has a 5-hour history of crying, with intermittent drawing up of his knees to his chest. On the way to the emergency room he passes a loose, bloody stool. He has had no vomiting and has refused his bottle since the crying began. Physical examination is noteworthy for an irritable infant whose abdomen is very difficult to examine because of constant crying. His temperature is 38.8C (101.8F). The rectal ampulla is empty, but there is some gross blood on the examining finger. Which of the following studies would be most helpful in the immediate management of this patient?
A. Stool culture
B. Examination of the stool for ova and parasites
C. Air contrast enema
D. Examination of the blood smear
E. Coagulation studies
233. A beekeeper’s previously healthy 6-month-old son develops gradual onset of lethargy, poor feeding, constipation, and generalized weakness. On taking a history, you determine that the child has recently been placed on a homemade formula consisting of evaporated milk, water, and honey. Which of the following is the most likely explanation for this symptom complex?
(A) sodium intoxication
(B) Hirschsprung disease
(C) hypothyroidism
(D) spinal cord tumor
(E) botulism
234. A 12-month-old patient has allergies to multiple foods. The child’s mother has eliminated the foods from the diet and wants to know if these allergies will be lifelong. You tell her that some allergies do get better if the food is eliminated for 1–2 years. In which of the following is the allergy most likely to resolve, with elimination of the food from the diet?
(B) milk
(A) peanuts
(C) nuts
(E) shellfish
(D) fish
235. A 4-year-old child manifests symptoms of fever, sore throat, and swollen lymph nodes. The spleen tip is palpable. Throat culture and rapid slide (Monospot) test results are negative. The next logical diagnostic procedure would involve which of the following?
(C) Epstein-Barr virus (EBV) titer
(A) rapid streptococcal antigen test
(B) heterophil titer
(D) chest x-ray
(E) bone marrow examination
236. The mother of a 2-year-old boy comes to the physician because her child awakens at night, with a blank gaze, screaming in bed without recognizing his parents. These episodes have occurred three times in the past 2 weeks, always in the first few hours of the night. The child goes back to sleep and seems to retain no memory of the episode the next morning. Which of the following is the most appropriate next step in management?
(B) Avoidance of TV before going to bed
(A) Reassurance of parents about the nature of these manifestations
(C) Behavioral therapy
(D) Therapy with chloral hydrate
(E) Therapy with a tricyclic antidepressant
237. A 12-year-old girl is taken to a pediatrician complaining of a sore mouth. On questioning, the child states that she has been feeling poorly, with fatigue and weakness. She began menstruating briefly and then stopped. Physical examination is notable for focal white crusting of the oral cavity; biopsy of one of these areas later shows candidiasis, Laboratory studies show the following: Sodium 127 mEq/L Potassium 5.3 mEq/L Bicarbonate 24 mEq/L Calcium 7.5 mEq/dL Phosphorus 5.5 mg/dL Glucose 87 mg/dL Which of the following is the most likely diagnosis?
A. Multiple endocrine neoplasia, type I
B. Multiple endocrine neoplasia, type IIA
C. Polyglandular deficiency syndrome, type I
D.Polyglandular deficiency syndrome, type II
E. Polyglandular deficiency syndrome, type III
238. A 6-year-old boy is brought to the clinic for the evaluation of a large, red, circular rash on his left thigh which has been present since two weeks and has been enlarging. He has a mild headache and myalgia, but is afebrile. Three weeks ago, he and his family visited relatives at a rural farm in Connecticut and went hiking in the woods. His temperature is 37.2 C (99 F) and pulse is 90/min. He is alert, active, appears non-toxic, and not in distress. On the anterior surface of his left thigh, there is a red ring that is 7 cm in diameter with central clearing, and a central brownish-red macule that is 3 mm in diameter. Which of the following measures would have prevented this condition?
A. Childhood vaccinations as recommended by American Association of Pediatrics
B. Careful sanitary measures in food preparation
C. Avoiding water intake from streams
D. Wearing light-colored clothing. Long-sleeved shirts and tucking pants into socks or boot tops
E. No wearing light-colored clothing. Short-sleeved shirts and tucking pants into socks or boot tops
239. A 1-week-old female infant is brought to the office by her 30-year-old AfricanAmerican mother because she has been "crying a lot." She was born at term. Her mother was diagnosed with gestational diabetes mellitus (GDM) at 24 weeks gestation and had been on insulin injections since. During labor, there was a prolonged second stage due to difficulty in delivering the shoulders. Her Apgar scores were 8 and 10 at 1 and 5 minutes, respectively. Her birth weight is 3.8 kg (8.5 Ib). On examination, the infant is active. On sudden extension of the head, there is extension of all the extremities, except for the left upper extremity. There is crepitus over the left clavicular bone. Which of the following statements is true for this baby?
A. This infant has clavicular fracture and should be treated with a figure of eight bandage.
B. This is a clavicular fracture and the infant should be evaluated for child abuse.
C. This is Erb Duchenne palsy due to difficult shoulder delivery.
D. This is a common outcome with large babies and related to gestational diabetes.
E. This infant has clavicular fracture and should be treated with a surgery.
240. A 15-year-old girl presents with a 2-day history of pain and swelling in her left knee. She plays soccer regularly on her school team. There is no history of trauma. On physical examination, there is marked swelling and tenderness over her anterior tibial tuberosity. A radiograph of her left knee reveals irregularities of the tubercle contour and haziness of the adjacent metaphyseal border. Which of the following is the most likely explanation for her symptoms?
A. Avascular necrosis of the hip
B. Legg-Calve-Perthes disease
C. Osgood-Schlatter disease
D. Septic arthritis
E. Slipped capital femoral epiphysis
241. A 12-year-old girl with a history of asthma has been admitted to intensive care units two times in the past and has had three emergency department visits during the past 12 months. Her only medication is inhaled albuterol as needed, and she uses it two to three times a day. She has nocturnal symptoms about two times a week. She is free of symptoms now but reports that she gets short of breath easily. Which of the following pharmacologic interventions is most appropriate?
A. Anticholinergic agent
B. Cromolyn sodium
C. Inhaled corticosteroid
D. Long-term bronchodilator
E. Nedocromil sodium
242. A 15-year-old girl presents with a 2-day history of pain and swelling in her left knee. She plays soccer regularly on her school team. There is no history of trauma. On physical examination, there is marked swelling and tenderness over her anterior tibial tuberosity. A radiograph of her left knee reveals irregularities of the tubercle contour and haziness of the adjacent metaphyseal border. Which of the following is the most likely explanation for her symptoms?
A. Avascular necrosis of the hip
B. Legg-Calve-Perthes disease
C. Osgood-Schlatter disease
D. Septic arthritis
E. Slipped capital femoral epiphysis
243. A 12-year-old girl with a history of asthma has been admitted to intensive care units two times in the past and has had three emergency department visits during the past 12 months. Her only medication is inhaled albuterol as needed, and she uses it two to three times a day. She has nocturnal symptoms about two times a week. She is free of symptoms now but reports that she gets short of breath easily. Which of the following pharmacologic interventions is most appropriate?
B. Cromolyn sodium
A. Anticholinergic agent
C. Inhaled corticosteroid
D. Long-term bronchodilator
E. Nedocromil sodium
244. A one-month-old child is brought to the office due to persistent vomiting for the last six days. His mothercomplains of increasing episodes of projectile vomiting. These episodes occur every time she attempts tofeed him, and have persisted despite changing formulas. On physical examination, peristaltic waves are seenover the upper abdomen, and an olive-sized mass is palpated. Laboratory studies reveal a potassium level of 3.0mEq/mL. Which of the following is the most appropriate next step in management?
A. Immediate surgery
B. Medical treatment with metoclopramide
C. Surgery before school age
D. Intravenous hydration and potassium replacement
E. Avoid milk products
245. A 4-year-old female is brought to the emergency department for evaluation of vaginal discharge. She has had foul-smelling vaginal discharge for 1 week. Her mother has also noted a small amount of vaginal bleeding. The mother called her primary physician and was told to use an over-the-counter cream and to stop letting the child take bubble baths. However, the symptoms have not improved. The child complains of pruritus in her vaginal area. She was potty trained at age 2. While mother is at work, the baby is with her stepfather. On examination, the perineal area is erythematous with a purulent, foul-smelling vaginal discharge. Visual inspection of the vagina reveals a greenish foreign body inside the vagina. Which of the following is the next best step?
A. Irrigation with warmed fluid
B. Bimanual examination under general anesthesia
C. Cultures for gonorrhea and chlamydia
D. Notify Child Protective Services immediately
E. CT scan of the pelvis
246. A 1-year-old child is brought to the physician for a routine visit. He was born full term with a birth weight of 71b 8oz (34 kg) and a birth length of 20 in (50.8cm). He has had no major illnesses or hospitalizations His parents report that he was breastfed exclusively for 6 months. He now eats a variety of baby foods and is being transitioned to whole milk. He can pull up to stand and cruise around holding onto objects, but cannot walk independently yet. He can feed himself small pieces of table food with his thumb and first finger. The only words he knows are mama, dada, and ball. His parents are concerned about his growth because some of the other children in his daycare class are bigger than him. On physical examination, he weighs 221bs (10 kg) and is 30 in (76.2cm) long. A complete examination is unremarkable. Which of the following should you tell his parents?
A. His weight is normal, but his height is less than expected.
B. His weight is less than expected, but his height is normal.
C. His growth is normal, but he has delayed motor development.
D. His growth is normal, but he has delayed speech development.
E. The child's growth and development are normal
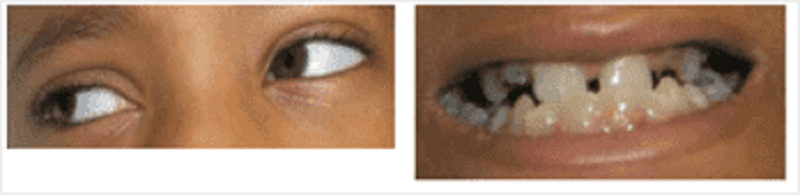
247. A 7-year-old male is brought to the emergency department for a suspected femur fracture. He has had multiple fractures in the past after minor trauma. Today, his mother states that he was running and fell. He complained of pain in his thigh after he fell. His examination is remarkable for tenderness to palpation and slight deformity of his right proximal thigh. He has decreased muscle tone throughout. His eye examination is shown below. Which of the following is the most likely associated finding?
A. Aortic root dilatation
B. Horseshoe kidney
C. Opalescent teeth
D. Mental retardation
E. Ash leaf macules
248. A 2-day-old male infant presents with multiple episodes of bilious vomiting over the past 24 hours. He has a prominent tongue, flat occiput and slanting eyes. His hands are short, and there are wide gaps between his first and second digits. His abdomen is soft and without any distention, guarding or rigidity. On auscultation of the chest, there is a systolic ejection murmur along the left sternal border, with a wide and fixed splitting of S2. Abdominal x- rays show air trapped in the first portion of the duodenum and stomach. What is the most likely cause of the child's symptoms?
A. Pyloric stenosis
B. Gastroesophageal reflux
C. Duodenal atresia
D. Mesenteric adenitis
E. Acute appendicitis
249. A 2-year-old girl presents to the office with a dry cough and a low-grade fever. Over the last two days, she has become very irritable and difficult to feed. She has also had a runny nose. On examination, there is significant wheezing and tachycardia. Evaluation of the nasal discharge confirms the diagnosis of respiratory syncytial virus infection. In the future, which of the following does this child have a slight risk of developing?
A. Pneumonia
B. Lung abscess
C. Cystic fibrosis
D. Asthma
E. Aspergillosis
250. An infant has had repeated pneumonias and middle ear infections that began at about 5 months of age. At 1 year of age, serum electrophoresis demonstrated hypogammaglobulinemia. T cell function was normal. By 2 years of age, the child's infection rate has decreased, and repeat serum electrophoresis is normal. Which of the following immunoglobulins was likely decreased in this child during the period of increased susceptibility to infection?
(B) IgD
(A) IgA
(C) IgE
(D) IgG
(E) IgM
1. A 16-year-old female presents to the emergency room with severe right- sided abdominal pain. Her last menstrual period was 2 weeks ago and felt to be normal. She displays painful difficulty in positioning herself on the examination table. Her temperature is 38.5 C (101.3 F), blood pressure is 128/75 mm Hg, pulse is 80/min, and respirations are 22/min. Examination of the throat reveals mild pharyngitis. Her abdomen is diffusely tender, especially the lower abdomen. Rectal examination reveals tenderness anteriorly on the right side. Stool guaiac is negative. A pelvic examination is performed, and there is evidence of cervical tenderness and questionable fullness in the right adnexal area. Which of the following is the most likely diagnosis?
B. Pyelonephritis
A. Ovarian cyst
C. Pelvic inflammatory disease
D. Constipation
E. Endometriosis
2. Your sister who lives in another state sends via e-mail photographs of her 6-month-old infant. You note the child has a white reflection from one of his eyes. You hastily assist in arranging an urgent pediatric ophthalmologic evaluation. Your sister immediately accesses the Internet and begins to ask questions of you. Which of the following statements found by your sister is correct?
B. Cure rates for retinoblastoma treated in the United States exceed 90%.
A. Most cases of retinoblastoma are unilateral and hereditary.
C. Biopsy is usually performed to confirm the diagnosis.
D. Intraocular calcifications are an unusual finding and suggest worse prognosis
E. Patients with the hereditary form of retinoblastoma are at significantly increased risk of leukemia in later years.
3. A 2950-g (6.5-lb) black baby boy is born at home at term. On arrival at the hospital, he appears pale, but the physical examination is otherwise normal. Laboratory studies reveal the following: mother’s blood type A, Rh-positive; baby’s blood type O, Rh-positive; hematocrit 38%; and reticulocyte count 5%. Which of the following is the most likely cause of the anemia?
B. ABO incompatibility
A. Fetomaternal transfusion
C. Physiologic anemia of the newborn
D. Sickle-cell anemia
E. Iron-deficiency anemia
4. A 5-year-old boy is brought to the physician's office because of a cough. He has episodes of successive and rapid coughs, which seems like he is choking, followed by a deep and loud inspiratory sound. He has vomited a few times after these bursts of cough. His symptoms have been progressively worsening for the past week, and were preceded by congestion, serous rhinorrhea and sneezing. His past medical history is insignificant. His vital signs are stable. Lung auscultation is unremarkable. Which of the following is the most appropriate pharmacotherapy for this patient?
B. Ampicillin
A. Erythromycin
C. Rifampin
D. Treatment is ineffective at this stage
E. Cephalexin
5. A 1-week-old male newborn is seen in the office for "noisy breathing." The mother says that the "noisy breathing" is more prominent when the infant is lying on his back, and improves when he is in a prone position with his chin up. The newborn is afebrile and has no cough, vomiting, or cyanosis. There are no inspiratory retractions or wheezes. On direct laryngoscopy, the epiglottis is rolled in from side to side. Which of the following statements is true about the child's condition?
B. The child requires immediate tracheostomy
A. The child should be held in an upright position for 30 minutes after feeding and never fed while lying down
C. The child should be treated with intravenous ceftriaxone
D. The child's condition is likely to deteriorate as the age advances
E. In this condition the stridor improves when the child cries
6. A 2-month-old infant comes to the emergency center with fever for 2 days, emesis, a petechial rash, and increasing lethargy. In the ambulance he had a 3-minute generalized tonic/clonic seizure that was aborted with lorazepam. He does not respond when blood is drawn or when an IV is placed, but he continues to ooze blood from the skin puncture sites. On examination, his anterior fontanelle is open and bulging. His CBC shows a WBC of 30,000 cells/L with 20% band forms. Which of the infant’s problems listed below is a contraindication to lumbar puncture?
A. Uncorrected bleeding diathesis
B. Bulging fontanelle
C. Dehydration
D. History of recent seizure
E. Significantly elevated WBC count consistent with bacteremia
7. The mother of one of your regular patients calls your office. She reports that her daughter has a 3-day history of subjective fever, hoarseness, and a bad barking cough. You arrange for her to be seen in your office that morning. Upon seeing this child, you would expect to find which of the following?
A. A temperature greater than 38.9C (102F)
B. Expiratorystridor
C. Infection with parainfluenza virus
D. Hyperinflation on chest x-ray
E. A child between 6 and 8 years of age
8. A 2-week-old baby girl is brought to the clinic for the evaluation of vaginal discharge. Her mother has noticed a cloudy white vaginal discharge mixed with blood since yesterday. She was born by normal vaginal delivery at term, and no congenital anomalies were noted at birth. Physical examination reveals a blood-stained, odorless vaginal discharge. Her vital signs are stable. What is the most appropriate next step in the management of this patient?
A. Treatment for Chlamydia
B. Treatment for HSV-2
C. Rule out vaginal cancer
D. Reassurance
E. Treatment for Trichomonas vaginalis
9. A 6-month-old male infant is brought to the physician's office by his mother due to failure to thrive. According to the mother, the child always regurgitates shortly after feedings, and has even had a few episodes of blood-stained projectile vomiting. During the vomiting episodes, the child tilts his head to the left and arches his back. On examination, the child is afebrile. His abdomen is soft and non-tender to palpation. Laboratory evaluation shows hypochromic microcytic anemia. What is the most appropriate test to confirm the most likely diagnosis of this child?
B. 24-hour esophageal pH monitoring
A. Chest x-ray
C. Esophageal manometry
D. Barium swallow
E. Technetium (Tc) sulfur colloid gastroesophageal scan

10. An infant weighing 1400 g (3 lb) is born at 32 weeks’ gestation. Initial evaluation was benign, and the infant was transferred to the level 2 nursery for prematurity. The nurse there calls at 1 hour of life and reports the infant is tachypneic. Vital signs include a heart rate of 140 beats per minute, a respiratory rate of 80 breaths per minute, a temperature of 35°C (95°F), and a peripheral oxygen saturation of 98%. The lungs are clear with bilateral breath sounds and there is no murmur; the infant is in no dis- tress. The child’s chest radiograph is shown. Which of the following is the most appropriate next step in evaluating the infant?
A. Obtain a complete blood count and differential.
B. Perform a lumbar puncture.
C. Administer intravenously 5cc of D50W.
D. Place the infant under a warmer.
E. Administer supplemental oxygen.
11. A 14-year-old boy is evaluated for short stature. He has no significant past medical history and is considered otherwise healthy by his parents. He eats a normal diet and has regular meals. His height and weight have been consistently at the 5th percentile since early childhood. His physical examination is normal, with genitalia at Tanner stage 3. Which of the following is the most likely laboratory finding for this boy?
A. Bone age that is equivalent to chronologic age
B. Decreased complement C3 level
C. Decreased serum albumin concentration
D. Decreased thyroid stimulating hormone
E. Increased serum creatinine concentration
12. A 2-month-old infant is brought to the emergency department with irritability and lethargy. The parents state that he was well until he rolled off the couch on to the floor yesterday. On examination, he is inconsolable and afebrile. The fontanels are full and tense. He has a generalized tonic-clonic seizure. Which of the following is the most important initial diagnostic study to order?
(A) serum calcium, phosphorus, and magnesium levels
(B) analysis of cerebrospinal fluid (CSF)
(C) cranial computed tomography (CT) scan
(D) serum ammonia level
(E) serum acetaminophen level
13. Two weeks after a viral syndrome, a 2-year-old child develops bruising and generalized petechiae, more prominent over the legs. No hepatosplenomegaly or lymph node enlargement is noted. The examination is otherwise unremarkable. Laboratory testing shows the patient to have a normal hemoglobin, hematocrit, and white blood cell (WBC) count and differential. The plateletcount is 15,000/L. Which of the followingis the most likely diagnosis?
A. Von Willebrand disease (vWD)
B. Acute leukemia
C. Idiopathic (immune) thrombocytopenic purpura (ITP)
D. Aplastic anemia
E. Thrombotic thrombocytopenicpurpura
14. An 11-month-old African American boy has a hematocrit of 24% on a screening laboratory done at his well-child checkup. Further testing demonstrates: hemoglobin 7.8 g/dL; hematocrit 22.9%; leukocyte count 12,200/L with 39% neutrophils, 6% bands, 55% lymphocytes; hypochromia on smear; free erythrocyte protoporphyrin (FEP) 114 g/dL; lead level 6 g/dL whole blood; platelet count 175,000/L; reticulocyte count 0.2%; sickle-cell preparation negative; stool guaiac-negative; and mean corpuscular volume (MCV) 64 fL. Which of the following is the most appropriate recommendation?
B. Oral ferrous sulfate
A. Blood transfusion
C. Intramuscular iron dextran
D. An iron-fortified cereal
E. CalciumEDTA
15. A 7-year-old girl presents with hives, which developed after a bee sting. She has no other symptoms. The hives resolve with diphenhydramine. Which of the following is the most appropriate management?
(B) Provide an Epi-pen Jr (epinephrine auto injector) to be carried at all times, as well as a prescription for diphenhydramine
(A) Write a prescription for diphenhydramine in case she is bitten again.
(C) Admit to the hospital for observation for delayed hypersensitivity symptoms.
(D) Refer her to an allergist for desensitization.
(E) Order a skin-prick test with hymenoptera venom.

16. A 15-year-old presents with the complaint of a rash, as pictured below. Which of the following statements is correct concerning the management of this common condition?
A. Fried foods must be avoided.
B. Frequent scrubbing of the affected areas is key.
C. Topical antibiotics are of no value.
D. Topical benzoyl peroxide is the mainstay of treatment.
E. This rash is solely a disease of the adolescent.
17. The recent suicide of a well-known high school cheerleader in your community has generated an enormous amount of community concern and media coverage. A girl who was close friends with the deceased makes an appointment and comes in to your office to discuss the event with you. You ask, and she denies suicidal ideation, but she has many questions about suicide. Correct statements about adolescent suicide include which of the following?
A. Girls tend to use more lethal means.
B. The number of attempted suicides is much higher among boys.
D. Inquiry by pediatricians, high school teachers, parents, or friends about suicidal thoughts typically precipitates the act.
E. The number of suicides in adolescents 10 to 19 years of age has decreased significantly since the 1950s.
C. Those who are successful have a history of a prior attempt or prior serious suicidal ideation.
18. A 2-month-old male is brought to the emergency department for evaluation of cyanosis, which occurred earlier in the day while the infant was taking his bottle. Initially, he became fussy and sweaty, then his mother noticed that his lips turned blue. He became intermittently tachypneic and continued to cry. As the crying continued, the cyanosis worsened. His temperature is 3 0C (98.6 0F), blood pressure is 80/50 mmHg, pulse is 150/min, and respiratory rate is 45/min. On examination, the child is alert, cyanotic, and tachypneic. Cardiac auscultation reveals a normal S 1 followed by a systolic ejection click. A grade 2/6 crescendo-decrescendo systolic ejection murmur is heard at the left upper sternal border. The patient is immediately placed in a knee-chest position. This maneuver will improve this patient's condition by which of the following mechanisms?
A. Increased systemic venous return
B. Decreased pulmonary blood flow
C. Increased systemic vascular resistance
D. Increased respiratory drive
E. Increased right to left shunting
19. A 2-year-old child is brought to the physician for a routine visit. He is growing and developing appropriately. He drinks 3-4 glasses of whole milk each day. He is starting to put words together into short sentences. His mother has no concerns. Physical examination shows mild pallor. Laboratory studies show the following: Hemoglobin 9.5 g/dL RDW 21% MCV 70 fl Platelet count 284,000/mm3 Leukocyte count 6,500/mm3 Which of the following additional findings is most likely in this patient?
A. Abnormal hemoglobin electrophoresis
B. Low reticulocyte count
C. Low serum total iron binding capacity
D. High indirect bilirubin
E. Positive fecal occult blood test
20. A 10-year-old child arrives with the complaint of new-onset bed-wetting. He has had no fever, his urine culture is negative, and he has had no new stresses in his life. He is well above the 95th percentile for weight as is much of his family. Which of the following is most helpful in making a diagnosis?
A. Fasting plasma glucose of 135 mg/dL
B. Random plasma glucose of 170 mg/dL
C. Two-hour glucose during glucose tolerance test of 165 mg/dL
D. Acanthosis nigricans on the neck
E. Symptoms alone are enough to make the diagnosis
21. You are called to the ER to see one of your patients. The father of this 14-year-old mildly retarded child says that he found the child about 20 minutes ago in the neighbor’s garden shed with an unknown substance in his mouth. The child first had a headache, but then became agitated and confused; while you are talking to the father in the ER the child begins to have a seizure and dysrhythmia on the cardiac monitor. The blood gas demonstrates a severe metabolic acidosis. Which of the following agents is most likely the culprit?
B. Chlorophenothane (DDT)
A. Organophosphate
C. Sodium cyanide
D. Warfarin
E. Paraquat
22. An 8-year-old boy is brought to his physician by his mother, who is worried by the child's frequent episodes of daydreaming, which have apparently resulted in a decline in school performance. The child's psychomotor development appears normal. EEG recording reveals bilateral and symmetric 3 Hz spike-and-wave discharges, which begin and end abruptly on a normal background. Which of the following is the most likely diagnosis?
(B) Complex partial seizures
(A) Absence seizures (petit mal)
(C) Pseudoseizures
(D) Simple partial seizures
(E) Tonic-clonk seizures (grand mal)
23. A pregnant woman has premature rupture of membranes. Her baby is born 3 days later, at 37 weeks' gestation. The 5-minute APGAR score is 4. Lung sounds are reduced, and the infant appears to be in respiratory distress. Peripheral blood smear with differential counts demonstrates a neutrophil count of 30,000/mL, with toxic granules evident in many neutrophils. Gram stain of buffy coat demonstrates small gram-positive cocci in chains. Which of the following is the most likely causative organism?
(B) Group B Streptococcus
(A) Group A Streptococcus
(C) Methicillin-resistant Staphylococcus aureus
(D) Methicillin-sensitive Staphylococcus aureus
(E) Neisseria meningitides
24. A 15-year-old girl is seen in your clinic with a sprained ankle, which occurred the previous day while she was exercising in her room. You realize that you have not seen her for quite some time, and begin to expand your examination beyond the ankle. You find relatively minimal swelling on her right ankle. She has dental decay, especially of anterior teeth and a swollen, reddened, irritated uvula. She seems to be somewhat hirsute on her arms and legs, but has thinning of her hair of the head. She has a resting heart rate of 60 beats per minute, and her oral temperature is 35.5°C (96F). Further questioning suggests that she has developed secondary amenorrhea. Which of the following is the most appropriate next step in the management of this girl?
B. Radiograph of ankle
A. Human immunodeficiency virus (HIV) testing
C. Thyroid function panel
D. Comparison of current and past weights
E. Pregnancy testing
25. A 17-year-old sexually active girl comes to your office complaining of acne that is unresponsive to the usual treatment regimen. Physical examination reveals severe nodulocystic acne of her face, upper chest, and back. You consider prescribing isotretinoin (Accutane), but you are concerned about side effects. Reviewing the literature, you find which of the following to be true about isotretinoin?
B. It is not known to be a teratogen.
A. Its efficacy can be profound and permanent.
C. Most patients experience excessive tearing and salivation.
D. Severe arthritis necessitating cessation of the drug occurs in about 15% of patients
E. Significant decrease in serum triglyceride levels are noted in 25% of patients.
26. A 6-year-old boy has multiple, honey-colored, crusted lesions on his face, periungual areas, and forearms. The first lesion appeared 2 weeks ago on his philtrum. Since then the lesions have spread to his hands and arms. Each began as a small pustule on an erythematous base and eventually ruptured to form the crusted lesions now present. His temperature is 100.6 F, pulse is 100/min, and respirations are 14/min. The remainder of the physical examination is unremarkable. Which of the following is the most appropriate treatment?
(B) Dicloxacillin
(A) Clarithromycin
(C) Penicillin G
(D) Penicillin V
(E) Vancomycin
27. A 30-minute-old male newborn is noted to have central cyanosis. He was born to a 16-yearold white female at 28 weeks gestation. His respirations are rapid and shallow at 70/min. His other vital signs are stable. On examination, there is audible grunting, intercostal and subcostal retractions, nasal flaring, and duskiness. On auscultation, fine rales are heard over the lung bases. Nasal oxygenation does not improve his cyanosis. A chest roentgenogram shows fine reticular granularity, predominantly in the lower lobes. Arterial blood gas analysis shows evidence of hypoxemia and metabolic acidosis. What is the most likely diagnosis of this patient?
A. Transient tachypnea of the newborn
B. Hyaline membrane disease (HMO)
C. Persistent pulmonary hypertension of the newborn (PPHN)
D. Meconium aspiration syndrome
E. Lntracranial hemorrhage
28. A 16-year-old Asian boy presents with a two-day history of fever, malaise, and painful enlargement of his parotid glands. He has no significant past medical history. He was born in India, and has not received any childhood vaccinations. He recently returned from a one-week vacation in India. His vital signs are stable, except for a mild fever. Examination shows bilateral parotid enlargement. The rest of the examination is unremarkable. Which of the following organs is most likely to be affected by this patient's illness?
B. Pancreas
A. Testes
C. Liver
D. Kidney
E. Spleen
29. The parents of a 14-year-old boy are concerned about his short stature and lack of sexual development. By history, you learn that his birth weight and length were 3 kg and 50 cm, respectively, and that he had a normal growth pattern, although he was always shorter than children his age. The physical examination is normal and his growth curve is shown on the next page. His upper-to-lower segment ratio is 0.98. A small amount of fine axillary and pubic hair is present. There is no scrotal pigmentation; his testes measure 4.0 cm3 and his penis is 6 cm in length. In this situation, which of the following is the most appropriate course of action?
B. Obtain a computed tomographic (CT) scan of the pituitary area
A. Measure pituitary gonadotropin
C. Biopsy his testes
D. Measure serum testosterone levels
E. Reassure the parents that the boy is normal
30. Friends are considering adopting a “special needs” child from another country. The family has few details, but the information they have received so far suggests the 4-year-old child has had surgery for an endocardial cushion defect, is short for his age, and had a history of what sounds like surgically repaired duodenal atresia at birth. You are suspicious this child may have which of the following syndromes?
B. Waardenberg
A. Kleinfelter
C. Marfan
D. Down
E. Turner
31. The parents of a 1-month-old infant bring him to the emergency center in your local hospital for emesis and listlessness. Both of his parents wanted a natural birth, so he was born at home and has not yet been to see a physician. On examination, you find a dehydrated, listless, and irritable infant. Although you don’t have a birth weight, the parents do not feel that he has gained much weight. He has significant jaundice. His abdominal examination is significant for both hepatomegaly and splenomegaly. Laboratory values include a total bilirubin of 15.8 mg/dL and a direct bilirubin of 5.5 mg/dL. His liver function tests are elevated and his serum glucose is 38 mg/dL. Serum ammonia is normal. A urinalysis is negative for glucose, but it has a “mouse-like” odor. These findings are consistent with which of the following conditions?
B. Maple syrup urine disease
A. Homocystinuria
C. Galactosemia
D. Ornithine transcarbamylase deficiency
E. Phenylketonuria
32. An 8-year-old African American boy is brought in for evaluation of a mass on the scalp. On examination, he is afebrile and nontoxic. There is a boggy mass on his scalp with alopecia. His posterior cervical lymph nodes are enlarged but nontender. Which of the following is the most appropriate treatment?
(B) oral amoxicillin
(A) incision and drainage
(C) IV naficillin
(D) selenium sulfide shampoo twice a week
(E) oral griseofulvin and selenium sulfide shampoo twice weekly
33. A 4-year-old child presents to your office in July with a history of a low-grade fever (38.1°C) and “sores” in his mouth for 2 days. He has been refusing to eat but has been drinking an adequate amount of liquids. On examination, he is afebrile and seems well hydrated. He has ulcers on his tongue and posterior pharynx, which are 4 mm in diameter. You also note a few vesicles on his hands and feet, which are 3–4 mm in size and mildly tender. Which of the following is the most likely diagnosis?
(B) coxsackie virus
(A) herpes simplex virus (HSV)
(C) aphthous ulcers
(D) Behçet syndrome
(E) traumatic ulcers
34. A 6-year-old obese girl is brought to the clinic by her mother, who is concerned that the child does not exercise and constantly eats. The mother has tried to enroll her in gym and fitness classes, but without success. The mother seems helpless and asks for your help. Which of the following is not a complication of obesity later in life?
A Slipped capital femoral epiphysis
B. Type I diabetes
D. Decreased self esteem
C. Hypertension
C. Hypertension
35. After an uneventful labor and delivery, an infant is born at 32 weeks’ gestation weighing 1500 g (3 lb, 5 oz). Respiratory difficulty develops immediately after birth and increases in intensity thereafter. At 6 hours of age, the child’s respiratory rate is 60 breaths per minute. Examination reveals grunting, intercostal retraction, nasal flaring, and marked cyanosis in room air. Auscultation reveals poor air movement. Physiologic abnormalities compatible with these data include which of the following?
B. Decreased lung compliance, increased lung volume, left-to-right shunt of blood
A. Decreased lung compliance, reduced lung volume, right-to-left shunt of blood
C. Normal lung compliance, reduced lung volume, left-to-right shunt of blood
D. Normal lung compliance, increased lung volume, right-to-left shunt of blood
E. Decreased lung compliance, reduced lung volume, left-to-right shunt of blood
36. You have been recently named as the medical director of the normal newborn nursery in your community hospital and have been asked to write standardized admission orders for all pediatricians to follow. Which of the following vaccines will you include on these orders?
B. Hepatitis B vaccine
A. Hepatitis A vaccine
C. Combination diphtheria, tetanus, and acellular pertussis vaccine
D. Inactivated polio virus
E. Haemophilus influenza B vaccine
37. A 30-minute-old male newborn is noted to have central cyanosis. He was born to a 16-yearold white female at 28 weeks gestation. His respirations are rapid and shallow at 70/min. His other vital signs are stable. On examination, there is audible grunting, intercostal and subcostal retractions, nasal flaring, and duskiness. On auscultation, fine rales are heard over the lung bases. Nasal oxygenation does not improve his cyanosis. A chest roentgenogram shows fine reticular granularity, predominantly in the lower lobes. Arterial blood gas analysis shows evidence of hypoxemia and metabolic acidosis. What is the most likely diagnosis of this patient?
B. Hyaline membrane disease (HMD)
A. Transient tachypnea of the newborn
C. Persistent pulmonary hypertension of the newborn (PPHN)
D. Meconium aspiration syndrome
E. Intracranial hemorrhage
38. A 9-year-old girl is seen in the office for unsteady gait and weakness in the lower limbs. On examination she is found to have a wide-based gait with constant shifting of position to maintain her balance. There is decreased vibratory and position sense in the lower extremities, and ankle jerks are absent bilaterally. Her feet are deformed with high plantar arches. MRI of the brain and spinal cord shows marked atrophy of the cervical spinal cord and minimal cerebellar atrophy. Nerve conduction velocity results are within normal limits. EKG shows Twave inversions in the inferior and lateral chest leads. The mother says that her other child, a 3-year-old boy, is completely normal. He shares toys with his sister and plays well with other children at playschool. He is able to copy squares and crosses but is unable to copy a triangle. Which of the following statements would you advance while discussing the girl's condition with her mother?
B. It is most likely a result of spontaneous mutation & the chances of your boy developing the same condition are minimal
A. There is nothing to worry about since it's a non-progressive condition
C. The EKG abnormalities are most likely due to myocardial ischaemia
D. The inability of your boy to copy a triangle worries me since it may be an early manifestation of the same condition your daughter is suffering from
E. I advise you to go for prenatal counseling if you desire any future pregnancies

39. A 10-year-old patient (pictured below) calls his parents from summer camp to state that he has had fever, muscular pain (especially in the neck), headache, and malaise. He describes the area from the back of his mandible toward the mastoid space as being full and tender and that his earlobe on the affected side appears to be sticking upward and outward. Drinking sour liquids causes much pain in the affected area. When his father calls your office, you remind him that he had refused immunizations for his child on religious grounds. Which of the following preventable diseases has this child acquired?
B. Varicella
A. Mumps
C. Rubella
D. Measles
E. Diphtheria
40. A healthy 1-year-old child comes to your office for a routine checkup and for immunizations. His parents have no complaints or concerns. The next day, the CBC you performed as customary screening for anemia returns with the percentage of eosinophils on the differential to be 30%. Which of the following is the most likely explanation?
B. Chronic allergic rhinitis
A. Bacterial infections
C. Fungal infections
D. Helminthinfestation
E. Tuberculosis
41. A 1400-g infant, born at 35 weeks' gestation, is 42 cm in length and a head circumference of 28 cm. One day after birth, she becomes very irritable, tremulous, and inconsolable. Her cry is high-pitched. Her pulse is 174/min. There are no dysmorphic facial features. To which of the following substances was this newborn most likely exposed in utero?
B. Barbiturates
A. Alcohol
C. Cocaine
D. Marijuana
E. Opiates
42. A 9-month-old infant is seen in the pediatrician's office because of failure to gain weight. Her length and weight are both below the 5th percentile at her age. The patient's chart indicates that at the age of age of 6 months, her length and weight were at the 50th percentile. A careful history reveals that the mother returned to work when the infant was 6 months old, and the grandmother assumed the care of the infant most of the time since then. She is receiving 6-8 oz of iron-fortified, cow protein-based formula every 4 hours. Which of the following is the best initial step in the management of this infant?
B. Obtain a detailed family history for lactose intolerance
A. Ask how the formula is mixed
C. Obtain a stool specimen
D. Obtain a sweat chloride test
E. Obtain a urinalysis

43. A very upset mother brings her 8-month-old child to the emergency room because he will not move his leg. She reports that when she was carrying him to the car about half an hour ago, she slipped on some ice and fell on top of him. The mother, an 18-year-old African American woman, has been exclusively breast-feeding her child. She has only recently started him on cereals, and has not supplemented his diet with vitamins. A radiograph of the child’s leg is shown below. Which of the following laboratory findings would be expected?
B. Hypophosphaturia
A. Hypocalcemia
C. Redueced serum alkaline phosphatas
D. Hypocalciuria
E. Hyperphosphatemia
44. A small-for-gestational-age infant is born at 30 weeks’ gestation. At 1 hour of age, his serum glucose is noted to be 20 mg/dL (normally greater than 40 mg/dL). Which of the following is the most likely explanation for hypoglycemia in this infant?
B. Adrenal immaturity
A. Inadequate stores of nutrients
C. Pituitary immaturity
D. Insulin excess
E. Glucagondeficiency
45. A 30-hour-old infant has not passed meconium since birth. He was full term with a birth weight of 3856 g (8 lb 8 oz). The pregnancy was uncomplicated. The baby appears well with no respiratory distress. Slight abdominal distention is noted. Rectal examination reveals a slightly tight rectum and results in a greenish gush of stool. Which of the following tests will probably confirm the likely diagnosis?
B. A rectal biopsy
A. A stool culture
C. A barium enema
D. An alpha1-antitrypsin level
E. A serum TSH level
46. A 2-month-old girl presents to her pediatrician's office for well-child care. Her mother complains of excessive tearing of the baby's left eye for the past 4 weeks. Each morning, a yellow crusty discharge is noted along the lashes of the left eye. The conjunctiva appears uninflamed. The right eye is not affected. On physical examination, the infant is otherwise well and achieving adequate weight gain on an exclusive breast milk diet. She is developmentally appropriate, including visually tracking 180 degrees. Which of the following is the most likely diagnosis?
(B) Gonococcal conjunctivitis
(A) Dacryostenosis
(C) Normal infant eye
(D) Viral conjunctivitis
(E) Vitamin A deficiency
47. A primiparous woman whose blood type is O positive gives birth at term to an infant who has A-positive blood and a hematocrit of 55%. A total serum bilirubin level obtained at 36 hours of age is 12 mg/dL. Which of the following additional laboratory findings would be characteristic of ABO hemolytic disease in this infant?
B. A positive direct Coombs test
A. A normal reticulocyte count
C. Crescent-shaped red blood cells in the blood smear
D. Elevated hemoglobin
E. Petechiae

48. The nurse from the level 2 neonatal intensive care nursery calls you to evaluate a baby. The infant, born at 32 weeks’ gestation, is now 1 week old and had been doing well on increasing nasogastric feedings. This afternoon, how- ever, the nurse noted that the infant has vomited the last two feedings and seems less active. Your examination reveals a tense and distended abdomen with decreased bowel sounds. As you are evaluating the child, he has a grossly bloody stool. The plain film of his abdomen is shown. The next step in your management of this infant should include which of the following?
A. Surgical consultation for an emergent exploratory laparotomy.
B. Continued feeding of the infant, as gastroenteritis is usually self-limited.
C. Stool culture to identify the etiology of the bloody diarrhea and an infectious diseases consultation.
D. Stopping feeds, beginning intravenous fluids, ordering serial abdominal films, and initiating systemic antibiotics.
E. Removal of nasogastric tube, placement of a transpyloric tube and, after confir- mation via radiograph of tube positioning, switching feeds from nasogastric to nasoduodenal.
49. A term neonate is small for date and has a small head. Further physical examination of the infant demonstrates small eyes with short palpebral fissures, a flattened nose, and abnormal palmar creases. With which of the following maternal conditions is this presentation most likely associated?
(B) Cirrhosis
(A) Alcohol abuse
(C) Cocaine abuse
(D) Diabetes mellitus
(E) Hypothyroidism
50. The parents of a 3-year-old patient followed in your clinic recently took their child on quickly planned 5-day trip to Africa to visit an ill grandparent. Everyone did well on the trip, but since their return about 10 days ago the boy has been having intermittent, spiking fevers associated with headache, sweating, and nausea. The parents had not been too concerned since he was relatively well, except for being tired, between the fevers. Today, however, they feel that he looks a bit pale and his eyes appear “yellow.” Which of the following is likely to reveal the source of his problem?
B. Complete blood count (CBC) with smear
A. Hepatitis A IgG and IgM titers
C. Hemoglobin electrophoresis
D. Tuberculosis skin test
E. Hepatitis B IgG and IgM titers
51. A 15-year old girl presents with a 5-day history of sore throat, low-grade fever, and easy fatigability. Physical examination shows bilateral tonsillar enlargement with exudate. Her spleen is palpable 3 cm below the left costal margin. Her throat culture is negative for group A Streptococcus. Monospot test is positive. Which of the following is the most appropriate management for this patient?
A) Abdominal ultrasound
(B) Avoidance of all contact sports
(C) Complete blood count
(D) Oral penicillin
(E) Splenectomy
52. A 4-year-old girl is brought to the office due to seizures that occurred 2 hours ago. This is her first episode. Her parents are also concerned because she is not able to carry on activities that children of her age are expected to do. On examination, there is a red flat lesion covering the left eye area and adjacent facial skin, which does not blanch on pressure, and which the parents say has been present since birth. Other pertinent findings are hemianopia, hemiparesis, and hemisensory disturbances. An x-ray of the skull shows tramline intra-cranial calcifications. What is the most likely diagnosis?
A. Sturge-Weber syndrome
B. Tuberous sclerosis
C. Capillary hemangioma
D. Epilepsy
E. Neurofibromatosis
53. An infant is born to a woman who has received very little prenatal care. The mother is anxious, complains of heat intolerance and fatigue, and reports that she has not gained much weight despite having an increased appetite. On examination the mother is tachycardic, has a tremor, and has fullness in her neck and in her eyes. The infant is most likely at risk for development of which of the following?
A. Constipation
B. Heart failure
B. Heart failure@ c. Macrocephaly
D. Third-degree heart block
E. Thrombocytosis
54. An otherwise healthy 7-year-old girl is brought to your office by her father because she has some acne, breast development, and fine pubic hair. Which of the following is the most likely etiology for her condition?
B. A gonadotropin-producing tumor
A. A feminizing ovarian tumor
C. A lesion of the central nervous system (CNS)
D. Exogenous estrogens
E. Early onset of “normal” puberty (constitutional)
55. A 10-day-old infant is brought to the office by her mother for the evaluation of purulent discharge from both eyes. The discharge appeared three days ago, after which the child developed a cough. On examination, the infant's eyes appear normal, except for the presence of purulent discharge. Auscultation reveals diffuse rales without wheezing. Chest radiograph shows a hyperinflated thorax. What is the most likely diagnosis?
A. Gonococcal conjunctivitis
B. Chemical conjunctivitis
C. Congenital chlamydial infection
D. Congenital rubella infection
E. Adenovirus infection
56. A 14-year-old girl presents to clinic for an annual check up. Her parents are concerned that the child is not meeting normal milestones of adolescent growth. The patient reports no recent illnesses. She is up-to-date on her vaccines, and is not having any trouble in school. She denies drug use and is active in sports. On examination, her vital signs are stable. Her lungs are clear and heart is regular in rate and rhythm. Breast and areolar enlargement is noted with no contour separation of the areola. Pubic hair is noted to be dark. The patient also reports that she started menstruating 8 months ago. Which of the following is the most likely Tanner stage of development in this patient?
A. Stage I
B. Stage II
C. Stage III
D. Stage IV
E. Stage V
57. A 3-day-old infant, born at 32 weeks’ gestation and weighing 1700 g (3 lb, 12 oz), has three episodes of apnea, each lasting 20 to 25 seconds and occurring after a feeding. During these episodes, the heart rate drops from 140 to 100 beats per minute, and the child remains motionless; between episodes, however, the child displays normal activity. Blood sugar is 50 mg/dL and serum calcium is normal. Which of the following is most likely true regarding the child’s apneic periods?
B. They are a part of periodic breathing.
A. They are due to an immature respiratory center.
C. They are secondary to hypoglycemia.
D. They are manifestations of seizures.
E. They are evidence of underlying pulmonary disease.
58. You have an 11-day-old term infant in your office for a well-child visit. The mother notes that she received a letter that day from the state’s Department of Health reporting that her child’s newborn screen had come back abnormal, indicating possible galactosemia. Which of the following is the most appropriate management at this point?
A. Discontinue oral feeds and begin total parenteral nutrition.
B. Supplement her breast-feeding with a multivitamin.
C. Refer to endocrinology for evaluation.
D. Discontinue breast-feeding and initiate soy formula feedings
E. Ultrasound of pancreas.
59. A 3-week-old female infant born at 38 weeks' gestation through an uncomplicated vaginal delivery, presents to the emergency department with 2-day history of fever. The infant had been healthy since birth. Her temperature in the emergency department is 40.0 C (104.0 F). She appears to be quite lethargic. A culture taken from the infant grows group B Streptococcus (GBS) in 24 hours. Which of the following infections is most consistent with this presentation?
B. Gastroenteritis C
A. Endocarditis
C. Meningitis
D. Pneumonia
E. Pyelonephritis
60. A 9-year-old boy is being evaluated for a syncopal episode. He was playing basketball when the syncope occurred. The episode lasted about 1-2 minutes, and then the patient woke up on his own. His mother also noticed that he has been having hearing problems. His physical examination is unremarkable. An ECG shows a prolonged Q-T interval, with a QTc of 0.49 sec. Which of the following is the most appropriate management if he has long Q-T syndrome?
B. Angiotensin converting enzyme inhibitor
A. Alpha-adrenergic blocker
C. Beta-adrenergic blocker
D. Calcium channel blocker
E. Diuretic
61. A 4-year-old child has mental retardation, shortness of stature, brachydactyly (especially of the fourth and fifth digits), and obesity with round facies and short neck. The child is followed by an ophthalmologist for subcapsular cataracts, and has previously been noted to have cutaneous an subcutaneous calcifications, as well as perivascular calcifications of the basal ganglia. This patient is most likely to have which of the following features?
A. Hypercalcemia
B. Hypophosphatemia
C. Elevated concentrations of parathyroid hormone
D. Advanced height age
E. Decreased bone density, particularly in the skull
62. A 1-day-old normal-appearing infant develops tetany and convulsions. He was born at 34 weeks’ gestation with Apgar scores of 2 and 4 (at 1 and 5 minutes, respectively) to a woman whose pregnancy was complicated by diabetes mellitus and pregnancy-induced hypertension. Which of the following serum chemistry values is likely to be the explanation for his condition?
A. Serum bicarbonate level of 22 mEq/dL
B. Serum calcium of 6.2 mg/dL
C. Serum glucose of 45 mg/dL
D. Serum magnesium level of 5.0 mg/dL
E. Intracranial hemorrhage
63. An 11-month-old girl is brought by her mother to the office due to fever, fussiness, and irritability. The girl has a tendency to hold and pull on her left ear. For the past few days, she has had rhinorrhea and nasal congestion. Her medical history reveals nothing particular. Her temperature is 38.9C (102F). Otoscopic examination reveals a bulging, erythematous tympanic membrane with decreased mobility on air compression. What is the most likely organism responsible for the patient's condition?
A. Haemophilus influenzae
B. Streptococcus pneumoniae
C. Moraxella catarrhalis
D. Pseudomonas aeruginosa
E. Group A Streptococcus
64. A 2 and a half-year-old child is brought to the office for the evaluation of easy bruising, nosebleeds, and decreased activity over the past week. He had an upper respiratory infection that was treated with an antibiotic 2 weeks ago. On examination, he is well-developed, seems well-nourished, anicteric, and pale. Pertinent findings include some small palpable posterior cervical lymph nodes, sinus tachycardia, a grade I/VI systolic ejection murmur, ecchymoses on his left shoulder and both lower extremities, and petechiae over his extremities and groin. There is no hepatosplenomegaly. The laboratory findings are as follows: Hemoglobin 7.9 g/dl Hematocrit 24% Platelet count 12, 000/mm3 WBC 3,000/mm3 Reticulocyte count 0.5% A bone marrow biopsy reveal a markedly hypocellular marrow with decreased megakaryocytes and precursors of the erythroid and myeloid cell lines. What is the most likely diagnosis?
A. Acquired aplastic anemia
B. Fanconi's anemia
C. Diamond-Biackfan anemia
D. Transient erythroblastopenia
E. Acute myeloid leukemia
65. A 10-year-old boy is brought to clinic because of increasing weakness and dyspnea over the past 6 months. He has been previously healthy and is on no medications. There is no significant family history of illness. On examination, he appears pale. His hematocrit is 20%, mean corpuscular volume (MCV) is 60/um3, and iron level is normal. Smear reveals basophilic stippling. Hemoglobin electrophoresis is consistent with the absence of one betaglobin gene. Which of the following is the most likely diagnosis?
(A) EUiptocytosis
(B) Hemoglobin S-C disease
(C) Porphyria
(D) Sickle cell disease
(E) Thalassemia
66. The child shown below presents with a 3-day history of malaise, fever to 41.1C (106F), cough, coryza, and conjunctivitis. He then develops the erythematous, maculopapular rash pictured. He is noted to have white pinpoint lesions on a bright red buccal mucosa in the area opposite his lower molars. Which of the following is the most likely diagnosis?
B. Rubella
A. Parvovirus
C. Herpes
D. Rubeola
E. Varicella
67. A 3-month-old girl is brought to the pediatrician for a scheduled visit. She has been meeting all development milestones but has been vomiting after each feeding. The infant weighed 3 kg (6 lb 10 oz) at birth and now weighs 6 kg (13 lb 3 oz). She does not have diarrhea and is afebrile. The remainder of the physical examination is unremarkable. Which of the following is the most likely cause of this patient's vomiting?
(A) Adrenogenital syndrome
(B) Child abuse
(C) Inborn error of metabolism
(D) Overfeeding
(E) Pyloric stenosis
68. A neonate is noted to have aniridia of the right eye on physical examination. He was born by spontaneous vaginal delivery after an uncomplicated full-term pregnancy. The remainder of the physical examination is normal. Which of the following is the most appropriate next step before the infant is released from the hospital?
(A) An abdominal ultrasound
(B) An echocardiogram
(C) A neurology consult
(D) A rapid plasmin reagin (RPR) test
(E) TV antibiotics
69. A 7-year-old boy presents to the physician's office with a 3-week history of left-sided anterior cervical lymph node enlargement. The enlarged nodes are not tender to palpation. A few papules developed on the left forearm at the onset of lymphadenopathy. The boy has a kitten at home. Which of the following is the most likely organism causing lymphadenopathy in this child?
A. Actinomyces israelii
B. Bartonella henselae
C. Francisella tularensis
D. Mycobacterium tuberculosis
E. Staphylococcus aureus
70. A 28-year-old Caucasian female comes to the office due to fever for the past 3 days. She also complains of pain and swelling in her right breast for the past 4 days. She exclusively breastfeeds her 3-month-old baby. On examination, she is febrile. Her right breast is engorged, red and tender, without any area of fluctuation. She wants to know if she can continue to breastfeed. Which of the following is a contraindication to breastfeeding?
A Mastitis
B. Acquired immune deficiency syndrome
C. Maternal rubella infection
D. Breast milk jaundice
E. Hemolytic disease of the newborn
71. A female infant develops cyanosis. She was delivery vaginally at 43 weeks' gestation, and the amniotic fluid had a greenish color. She has dry, peeling skin, emaciated extremities and long fingernails. Tachypnea, nasal flaring, and sub- and intercostal retractions are observed. Auscultation reveals rales and rhonchi. The chest radiograph reveals flattening of the diaphragm, hyperinflation of the lungs, and patchy opacities diffusely distributed over both lung fields. Arterial blood gases reveal hypoxia and hypercarbia. What is most likely impairing the normal respiratory function of this newborn?
A. Fetal lung fluid
B. Poor alveolar compliance
C. Meconium
D. Paralysis of the diaphragm
E. Fibrosis of the lungs
72. A 10-year-old boy comes to the office with fever and chills for 5 days and myalgia. He has recently returned from a 2-week vacation to New England with his family. On physical examination he has mild splenomegaly. Which of the following is the most likely cause of his symptoms?
(B) pneumococcus
(A) Kawasaki disease
(C) babesiosis
(D) leptospirosis
(E) psittacosis
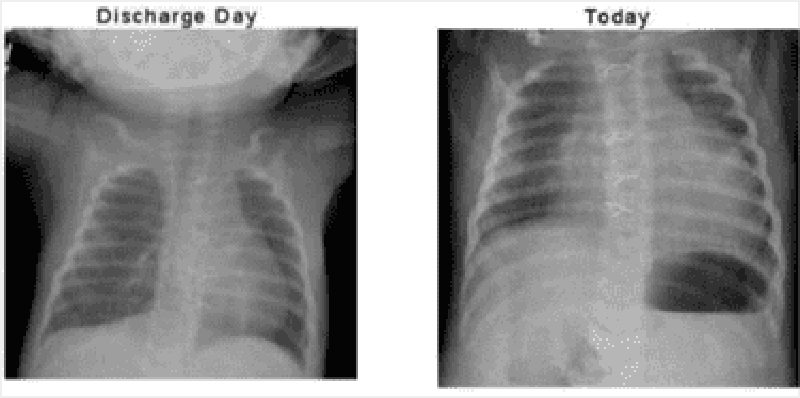
73. A 3-week-old infant with hypoplastic left heart syndrome comes to the physician for a followup visit. The infant was born at term via normal spontaneous vaginal delivery. The patient had the first of 3 palliative heart surgeries shortly after birth. He did well after surgery and was discharged home one week ago. Over the last 24 hours, the infant has difficulty feeding and one episodes of vomiting. On examination, the infant is afebrile, pulse is 160/min, respiratory rate is 55/min, blood pressure is 90/50mmHg, and pulse oximetry is 80% on room air. He is mildly cyanotic, small, but well developed. His cardiovascular exam reveals tachycardia and distant heart sounds with a systolic ejection murmur heard throughout the precordium. His chest radiographs from discharge and today are shown below. What is the most likely diagnosis?
B. Endocarditis
A. Congestive heart failure
C. Pleural effusion
D. Pericardial effusion
E. Myocarditis
74. A 4-year-old female is brought to the emergency department for evaluation of vaginal discharge. She has had foul-smelling vaginal discharge for 1 week. Her mother has also noted a small amount of vaginal bleeding. The mother called her primary physician and was told to use an over-the-counter cream and to stop letting the child take bubble baths. However, the symptoms have not improved. The child complains of pruritis in her vaginal area. She was potty trained at age 2. While mother is at work, the baby is with her stepfather. On examination, the perineal area is erythematous with a purulent, foul-smelling vaginal discharge. Visual inspection of the vagina reveals a greenish foreign body inside the vagina. Which of the following is the next best step?
B. Bimanual examination under general anesthesia
A. Irrigation with warmed fluid
C. Cultures for gonorrhea and chlamydia
D. Notify Child Protective Services immediately
E. CT scan of the pelvis
75. A 5-month-old boy is brought in for a routine check-up. He was born at 37 weeks' gestation and has had persistent wheezing since shortly after birth despite inhaled bronchodilator and oral corticosteroid therapy. His diet consists of 32 ounces of iron-fortified cow's milk-based formula daily. On physical examination, the child appears well-nourished and happy. You note moderate relief of his wheezing with neck extension. Which of the following is the most likely mechanism of this infant's wheezing?
B. Aspiration of a foreign body
A. Allergic reaction to cow's milk
C. Compression of the airway by a vascular ring
D. Chronic upper respiratory tract infection
E. Asthma
76. A mother calls you frantic because she has just been diagnosed with chicken pox. She delivered 7 days ago a term infant that appears to be eating, stooling, and urinating well. The child has been afebrile and seems to be doing well. Which of the following is the most appropriate step in management?
B. Hospitalize the infant in the isolation ward.
A. Isolate the infant from the mother.
C. Administer acyclovir to the infant.
D. Administer varicella-zoster immunoglobulin to the infant.
E. Advise the mother to continue regular well-baby care for the infant.
77. A mother wishes to breast-feed her newborn infant, but is worried about medical conditions that would prohibit her from doing so. You counsel her that of her listed conditions, which of the following is a contraindication to breast-feeding?
B. Cracked and bleeding nipples
A. Upper respiratory tract infection
C. Mastitis
D. Inverted nipples
E. HIV infection
78. A mother delivers a neonate with meconium staining and Apgar scores of 3 at 1 and 5 minutes of life. She had no prenatal care and the delivery was by emergency cesarean section for what the obstetricians report as “severe fetal bradycardia.”Which of the following sequelae could be expected to develop in this intubated neonate with respiratory distress?
B. Hyperactive bowel sounds
A. Sustained rise in pulmonary arterial pressure
C. Microcephaly with micrognathia
D. Cataracts
E. Thrombocytosis
79. A mother brings her 6-year-old daughter for evaluation because she has never been able to toilet train her. The child states that she perceives the sensation of having to void, and empties her bladder normally at normal intervals, but is nonetheless wet with urine all the time. Which of the following is the most likely diagnosis?
(B) Meatal stenosis
(A) Low implantation of one ureter
(C) Ureteropelvic junction obstruction
(D) Ureterovesical reflux
(E) Urethral valves
80. A neonate is noted to have an abnormally shaped face with a very small jaw. Several hours after birth, the baby develops convulsions and tetany. Serum chemistries show the following: Sodium 1 40 mEq/L Potassium 4 mEq/L Chloride 100 mEq/L Bicarbonate 24 mEq/L Magnesium 2 mEq/L Calcium 5 mg/dL Glucose 100 mg/dL This child's disorder is associated with aplasia or hypoplasia of which of the following organs?
(A) Ovaries
(B) Pancreas
(C) Pituitary
(D) Thymus
(E) Thyroid
81. A 10-year-old girl is brought to the physician because of throat pain, anorexia, and fever for 2 days. Her temperature is 38.9 C (102 F). The patient's history is negative for allergic diseases. She has had two episodes of pharyngotonsillitis over the past several years. Examination reveals a purulent exudate in the posterior oropharynx and enlarged tonsils. There is bilateral tender enlargement of anterior cervical lymph nodes. Cardiac and chest auscultation is normal. A rapid strep test is positive. Which of the following is the most appropriate next step in management?
(B) Symptomatic treatment with nonsteroidal antiinflammatory drugs
(A) Confirmatory throat cultures before treatment
(C) Symptomatic treatment and oral penicillin V
(D) Symptomatic treatment and a broad-spectrum cephalosporin
(E) Surgical referral for tonsillectomy
82. A 12-year-old girl is seen by a pediatrician for a mild case of pneumonia. She is treated with an intramuscular injection of penicillin. About 15 minutes later, she develops extreme itchiness, accompanied by the development of wheals scattered over her chest and extremities. She also begins to wheeze and complain of difficulty breathing. The color of her lips and face remains rosy. Which of the following is the most appropriate first step in management?
(A) Epinephrine injection
(A) Epinephrine injection
(C) Intubation
(D) Oral corticosteroids
(E) No specific therapy is needed
83. An 11-month-old boy is brought to the emergency department by his parents. The child has a fracture of the right femur. The father reports this was sustained as a result of falling out of the crib. The child is also noted to have bruises on his shoulders and back. The rest of his examination is unremarkable. Which of the following is the most appropriate next step in diagnosis?
(A) Social services consult
(B) Chest x-ray
(C) CT of the head
(D) Funduscopic exam
(E) Lumbar puncture
84. A 5-year-old boy is brought to the physician for evaluation of left hip pain after his parents saw him limping this morning. He spent time on the playground yesterday but his parents do not think he was injured then. The boy complains that the pain in his hip worsens when he moves or walks. For the past 3 days, he has had a runny nose and congestion. Review of systems is otherwise negative. His grandmother has rheumatoid arthritis treated with methotrexate. His temperature is 37.2° C (99° F), blood pressure is 100/65 mm Hg, pulse is 92/min, and respirations are 18/min. Physical examination shows a well-appearing child with clear rhinorrhea and intermittent dry cough. Lungs are clear to auscultation bilaterally. His left hip is slightly abducted and externally rotated with mildly decreased range of motion. He is able to stand and bear weight. The remainder of his examination is normal. X-rays of both hips are normal. His laboratory results are as follows: Complete blood count Hemoglobin 12.5 g/dL Platelets 287,000/mm3 Leukocyte count 8,500/mm3 Neutrophils 30% Eosinophils 1% Lymphocytes 64% Monocytes 5% Erythrocyte sedimentation rate 30 mm/h C-reactive protein 9 mg/L (N: ≤ 8 mg/L) Which of the following is the best next step in management of this patient?
A. Ibuprofen, rest, and follow-up in 1 week
B. Intravenous antibiotics
C. Magnetic resonance imaging of the left hip
D. Serum antinuclear antibodies
E. Synovial fluid aspiration of the left hip

85. A 2-day-old boy in the newborn nursery was born at 39 weeks gestation to a 38-year-old woman by vaginal delivery. The mother received epidural fentanyl for severe painful contractions during labor, but the delivery was uncomplicated. Since birth, the boy has shown little interest in breast or bottle feeding. He spit up the last feed but has not vomited. He has not yet passed meconium. Physical examination shows a newborn with generalized hypotonia, a flat facial profile, low-set folded earlobes, and a single transverse crease on each palm. His abdomen is firm and distended. Digital rectal examination is notable for a tight anal canal and relieves an expulsion of gas and stool. Abdominal x-ray shows markedly distended loops of bowel with no gas in the rectum. What is the mostly likely mechanism for his findings?
B. Failure of neural crest cell migration during fetal intestinal development
A. Constipation from decreased levels of thyroxine
C. Intestinal ileus from exposure to maternal epidural analgesia
D. Intestinal obstruction from inspissated meconium
E. Lnvagination of a part of the intestine into itself
86. A 6-day-old girl who was born at home is being evaluated for bruising and gastrointestinal bleeding. Laboratory findings include partial thromboplastin time and prothrombin time, greater than 2 minutes; serum bilirubin, 4.7 mg/dL; alanine aminotransferase, 18 mg/dL; platelet count, 330,000/mm3; and hemoglobin, 16.3 g/dL. Which of the following is the most likely cause of her bleeding?
A. Factor VIII deficiency
B. Factor IX deficiency
C. Idiopathic thrombocytopenic purpura
D. Liver disease
E. Vitamin K deficiency
87. A 7-year-old boy is brought to the clinic for a lifetime history of bedwetting. He has otherwise been completely healthy and has met all development milestones. His parents deny a history of trauma, and the history is not consistent with abuse. The patient has been wetting every night but not during the daytime. He has no incontinence. Which of the following is the most appropriate next step in his evaluation?
A. Intravenous pyelogram
B. Renal ultrasound
C. 24-hour urine collection
D. Urinalysis
E. CT of pelvis
88. A 1-year-old African American infant is in for well-child care. He is primarily breast-fed. His parents do not give him much solid food because he has no teeth. He receives no medications or supplements. His parents are concerned about his bowed legs. On examination, you note some other bony abnormalities including frontal bossing, enlargement of the costochondral junctions, a protuberant sternum (pigeon chest), and severe bowing of the legs. You obtain xrays to confirm your clinical diagnosis and also note a healing fracture of the left femur. Which of the following is the most likely diagnosis?
(A) osteogenesis imperfecta
(B) scurvy
(C) congenital syphilis
(D) rickets
(E) chondrodystrophy
89. A 6-month-old infant is brought to the clinic for the evaluation of sudden episodes of jerky movements of the neck, arms, and legs onto the trunk for past month. These episodes occur in clusters, last for a few minutes, and are often preceded by a cry. Her development has been normal. Her vital signs are normal. She is at 50th percentile for height, weight and head circumference. She has multiple small 1-2 cm oval irregular hypopigmented macules on her trunk and extremities. A head CT scan reveals cortical tubers in the cerebral cortex and multiple subependymal nodules in the lateral ventricles. Her EEG shows "hypsarrhythmia." What is the best medication for this patient's seizure?
B. ACTH
A. Vigabatrin
C. Ethosuximide
D. Carbamazepine
E. Phenobarbital
90. A 3-week-old male infant is brought to the office for the evaluation of red eyes. His temperature is 37.2 C (99F), pulse is 100/min, and respirations are 34/min. On examination, the infant has conjunctival congestion and scant mucoid discharge. The rest of the physical examination is normal. What is the most appropriate next step in the management of this patient?
B. Topical silver nitrate
A Topical erythromycin
C. Topical steroids
D. Oral erythromycin
E. Oral tetracycline
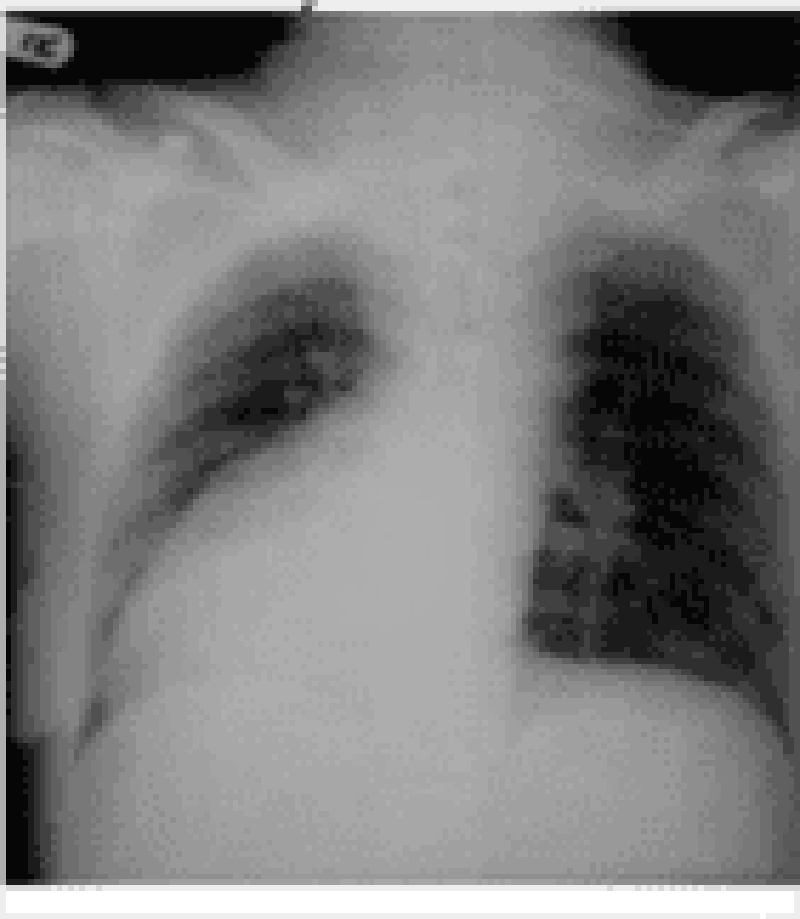
91. A 2-year-old boy is brought to the emergency department by his mother for the evaluation of a productive cough and low-grade fever. He has had ten such infections over the past year, all of which required antibiotics. He was delivered vaginally without any complications. He is an only child. His mother's siblings have a history of similar infections. He is alert and has normal vital signs, except for a mild fever. Auscultation reveals rales and rhonchi in both lungs. The chest x-ray is shown below.What is the most likely diagnosis?
A Cystic fibrosis
B. Foreign body
C. Kartagener's syndrome
D. Immunoglobulin deficiency
E. Congenital bronchiectasis
92. A 14-year-old boy presents with sudden onset of pain and swelling of his right testicle. There was no history of trauma, he is not sexually active, and denies any history of penile discharge. On examination, the scrotum is swollen and tender. The cremasteric reflex is absent. A testicular flow scan shows a “cold spot” or absent flow to the affected side. Which of the following is the most likely cause?
(A) inguinal hernia
(B) hydrocele
(C) epididymitis
(D) testicular torsion
(E) torsion of the appendix testis
93. Otitis media occurring during the first 8 weeks of life deserves special consideration, because the bacteria responsible for infections during this time may be different from those that affect older infants and children. Which of the following organisms is the most likely to cause otitis media in these infants?
(A) Chlamydia trachomatis
(B) E. coli
(C) Neisseria gonorrhoeae
(D) Treponema pallidum
(E) Toxoplasma gondii
94. Among the conditions that cause edema of the eyelids is orbital cellulitis. This is a serious infection that must be recognized early and treated aggressively if complications are to be avoided. Which of the following features is useful in differentiating orbital cellulitis from periorbital (preseptal) cellulitis?
(A) proptosis
(B) elevated WBC count
(C) fever
(D) lid swelling
(E) conjunctival inflammation

95. A 7-year-old boy was brought to the emergency department after falling onto his outstretched arm. He complains of pain in his left arm and refuses to move his arm at the elbow. On examination, the left arm is swollen, slightly pale, and edematous. His radial pulse is intact. The patient's radiograph is shown below.While the patient is waiting for the orthopedic resident on call to examine him, he continues to complain of increasing pain despite multiple doses of pain medication. Which of the following should you be most concerned about in this patient?
B. Transient neuropraxia
A. Displacement of the fracture
C. Brachial artery injury
D. Compartment syndrome
E. Narcotic abuse
96. A 9-year-old male is brought to the emergency department with respiratory disease after being stung by a bee. He requires resuscitation with epinephrine injection. On discharge, which of the following recommendations to the boy's mother is most appropriate?
A. Do not allow him to play outside
B. Wear colorful clothes while outside
C. Give prophylactic antihistamine agents daily
D. Provide epinephrine to carry with him
E. Use insect repellants
97. A 1-year-old boy is brought to the physician by his parents for evaluation of bruising and blood in his stool. The child has had multiple episodes of otitis media and has been hospitalized twice with pneumonia, but has never had bleeding or easy bruising in the past. He has been eating and drinking well with no vomiting or diarrhea. He is afebrile with a heart rate of 150/min and a blood pressure of 80/40 mmHg. On examination, he is well-developed, well-nourished, and has a fair complexion. There are dry, scaly patches on his cheeks and lower extremities. He also has bruising and purpura on his lower extremities. His diaper contains a small amount of occult blood positive stool, but no fissures are seen on rectal examination. The remainder of the physical examination is unremarkable. Laboratory studies show: Complete blood count Hemoglobin 11 .5 g/dL Platelet count 20,000/mm3 Leukocyte count 6,500/mm3 Neutrophils 76% Eosinophils 1% Lymphocytes 13% Monocytes 10% A peripheral smear reveals a low number of platelets, and the platelets that are seen are small. Which of the following is the most likely cause of his bleeding?
A. Bone marrow infiltration
B. Platelet antibodies
C. Nutritional deficiency
D. Platelet activation and consumption
E. Impaired platelet production
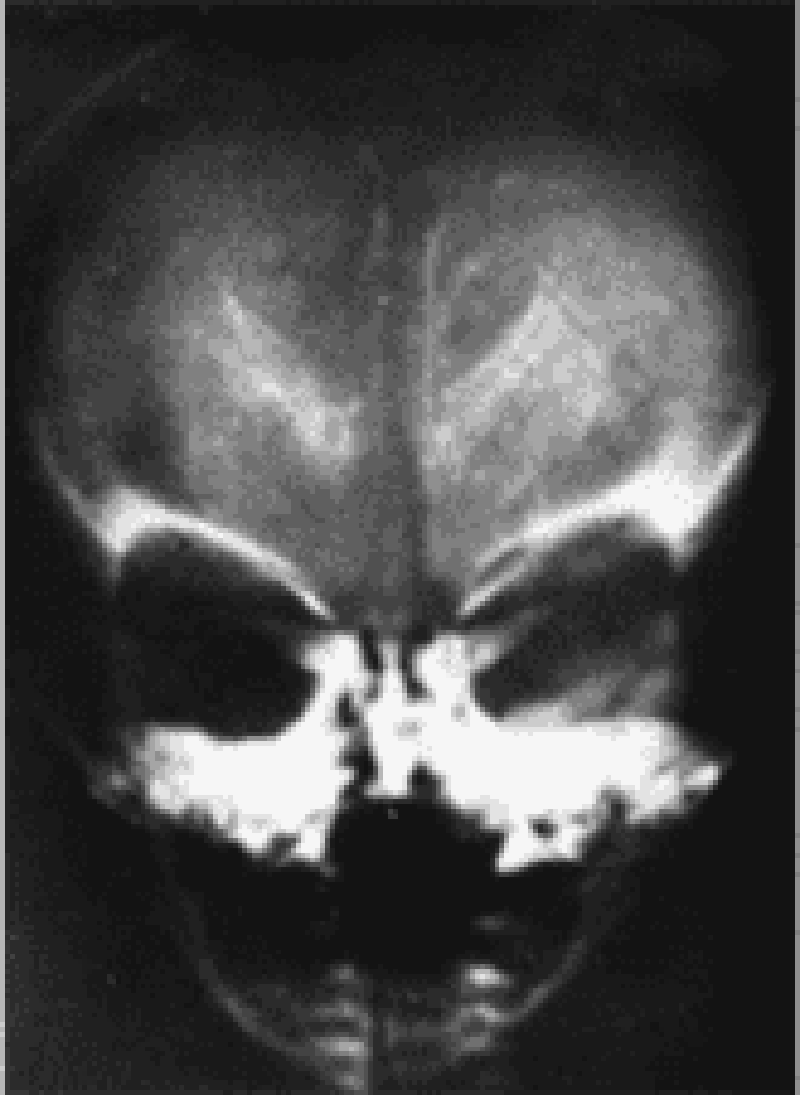
98. The developmentally delayed 6-month-old child in the picture below had intrauterine growth retardation (including microcephaly), hepatosplenomegaly, prolonged neonatal jaundice, and purpura at birth. The calcific densities in the skull x-ray shown are likely the result of which of the following?
B. Congenital toxoplasmosis infection
A. Congenital cytomegalovirus (CMV) infection
C. Congenital syphilis infection
D. Tuberculous meningitis
E. Craniopharyngioma
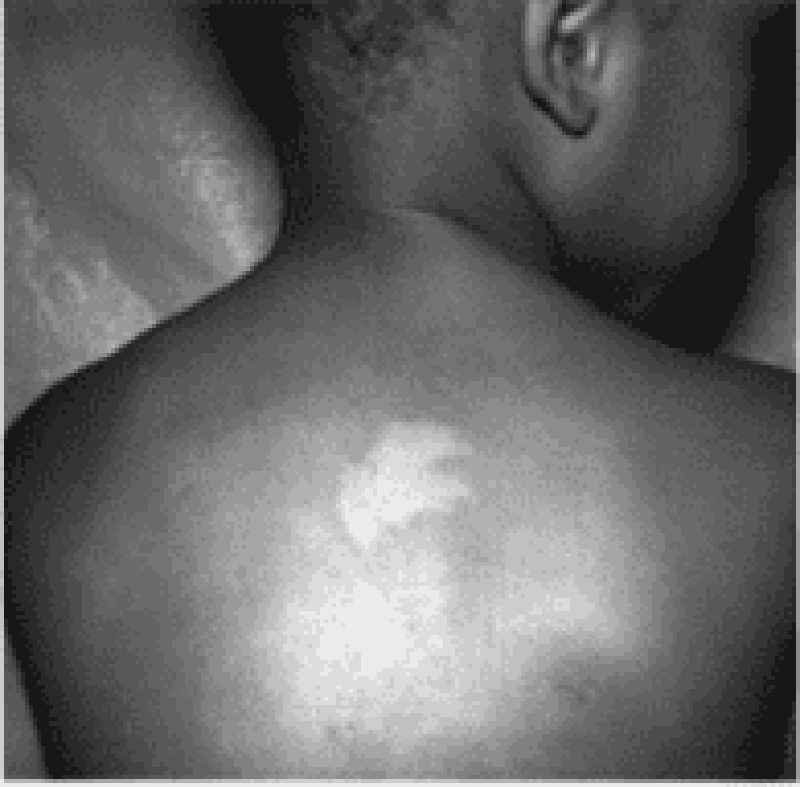
99. The infant pictured below develops infantile spasms. Which of the following disorders is most likely to be affecting this infant?
A.Neurofibromatosis
B. Tuberous sclerosis
C. Incontinentiapigmenti
D. Pityriasis rosea
E. Psoriasis
100. A 7 -year-old Caucasian boy is brought to the clinic due to malaise and headache for the past 2 weeks. He was apparently normal until 3 weeks ago, when he went on a hiking trip with his family to Connecticut. His father found a tick attached to his thigh; however, a red macule remains at the site where the tick was attached. One week after the tick was removed, a red ring developed around the macule, and then the ring appeared to grow larger by expanding outward, leaving an area of central clearing. What is the most appropriate next step in the management of this patient?
B. Amoxicillin
A Doxycycline
C. Ceftriaxone
D. Penicillin G
E. Erythromycin
101. A child is brought to the physician for a routine visit. On examination, the child can name multiple items in the examination room, and can also combine 2 words into a short sentence. His mother estimates that he knows about 200 words. When his mother tries to help him onto the examination table, he says "me do it." Although his mother seems to understand most of what he says, you can only understand about half of his speech. Which of the following is the most likely age of this child?
B. 15 months
A 12 months
C. 18 months
D. 24 months
E. 36 months
102. A one-month-old child is brought to the office due to persistent vomiting for the last six days. His mother complains of increasing episodes of projectile vomiting. These episodes occur every time she attempts to feed him, and have persisted despite changing formulas. On physical examination, peristaltic waves are seen over the upper abdomen, and an olive-sized mass is palpated. Laboratory studies reveal a potassium level of 3 mEq/mL. What is the most appropriate management for this patient?
B. Medical treatment with metoclopramide
A. Immediate surgery
C. Surgery before school age
D. Intravenous hydration and potassium replacement
E. Avoid milk products
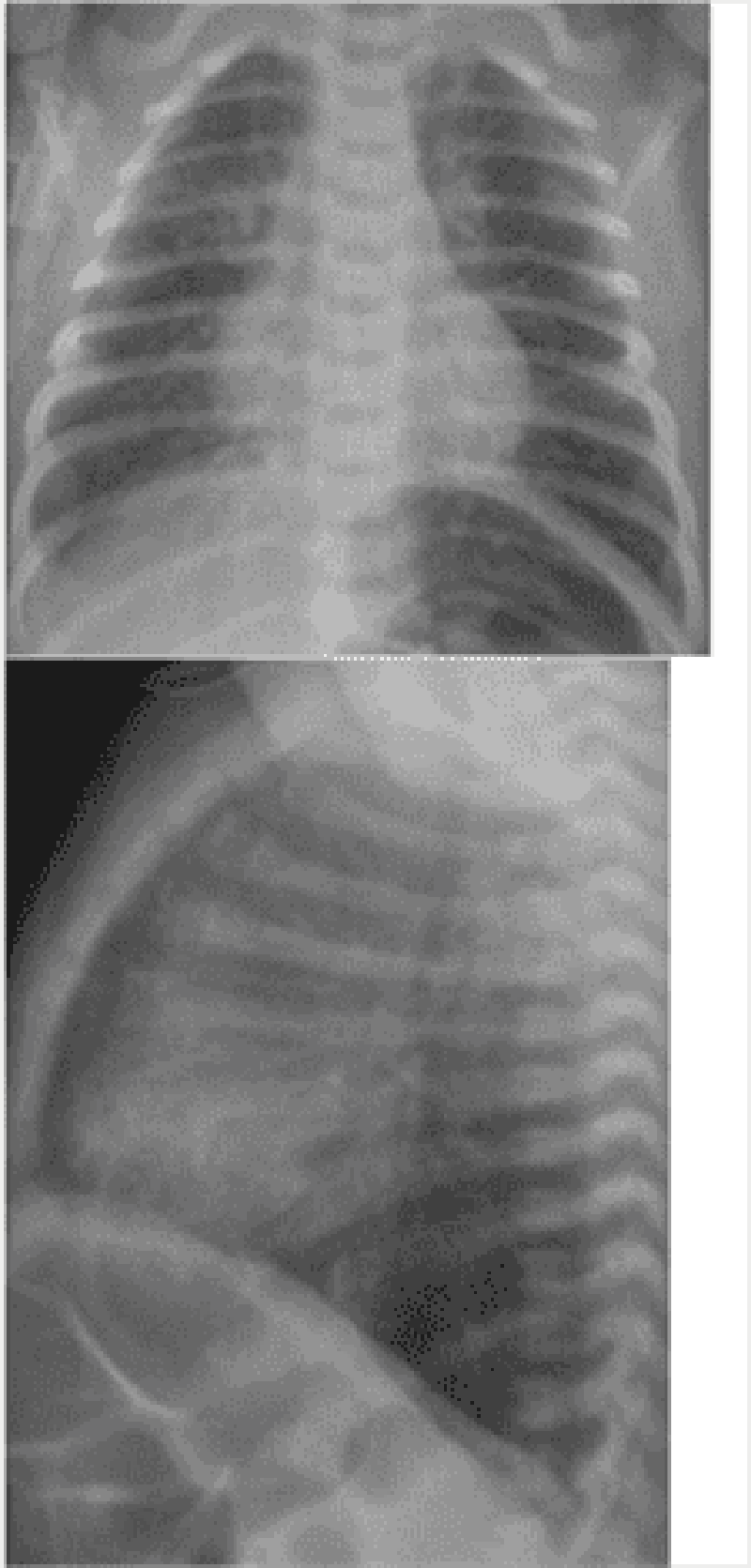
103. A previously well 1-year-old infant has had a runny nose and has been sneezing and coughing for 2 days. Two other members of the family had similar symptoms. Four hours ago, his cough became much worse. On physical examination, he is in moderate respiratory distress with nasal flaring, hyper- expansion of the chest, and easily audible wheezing without rales. His chest radiographs are shown. Which of the following is the appropriate next course of action?
A. Monitoring oxygenation and fluid status alone
B. Inhaled epinephrine and a single dose of steroids
C. Acute-acting bronchodilators and a short course of oral steroids
D. Emergent intubation and antibiotics
E. Chest tube placement

104. A 6-year-old girl presents with a 2-day history of cough and fever. At your office she has a temperature of 39.4°C (103°F), a respiratory rate of 45 breaths per minute, and decreased breath sounds on the left side. Her chest x-ray is shown below. Which of the following is the most appropriate initial treatment?
A. N-acetylcysteine chest physiotherapy
B. Vancomycin
C. Partial lobectomy
D. Postural drainage
E. Placement of tuberculosis skin test
105. A 2-year-old girl is playing in the garage with her Chihuahua, only par- tially supervised by her father, who is weed-whacking around the garden gnomes in the front yard. He finds her in the garage, gagging and vomiting. She smells of gasoline. In a few minutes she stops vomiting, but later that day she develops cough, tachypnea, and subcostal retractions. She is brought to your emergency center. Which of the following is the most appropriate first step in management?
A. Administer charcoal
B. Begin nasogastric lavage
C. Administer ipecac
D. Perform pulse oximetry and arterial blood gas
E. Administer gasoline-binding agent intravenously
106. A 3-day-old girl has trouble feeding and pulmonary congestion. The mother says that the infant is so busy breathing, that she literally has no time to suckle. The girl was bom at home, with the delivery attended by a midwife. Physical examination confirms that she is in respiratory distress and shows bounding peripheral pulses with a loud continuous precordial machinerylike murmur. X-ray films show increased pulmonary vascular markings. Shortly thereafter, the infant goes into overt heart failure. Which of the following would most likely be required to correct this problem?
(B) Digitalis and diuretics
(A) Indomethacin
(C) Emergency surgical closure of atrial septal defect
(D) Emergency surgical closure of ventricular septal defect
(E) Emergency surgical division of patent ductus arteriosus
107. A 12-year-old girl presents with a 2-month history of vaginal discharge. She describes it as clear and states that it stains her underwear. She says that she hates boys, and that "no way" has she ever had sex or even kissed a boy. She reports having had developing breasts for 2 years and thinks that her growth spurt was about a year ago. Genital findings include a pubic hair stage of Tanner III with no evidence of redness or irritation of the vulvovaginal area. A slight amount of odorless, clear mucus is seen. Microscopic examination of the mucus reveals epithelial cells and a few bacteria, but no white cells. The pH is between 3.5 and 4. Which of the following is the most appropriate next step in management?
(B) Advise the girl to discontinue all bubble baths and wipe herself front to back after voiding
(A) No treatment, but the girl should he reassessed in a few months
(C) Pelvic examination to obtain cultures for gonorrhea and Chlamydia
(D) Clotrimazole cream to be applied once a day for 10 days
(E) Sitz baths one or two times a day and 1% hydrocortisone cream applications once a day for a week
108. A 10-year-old girl is involved in a motor vehicle accident, sustaining multiple injuries to her head, arms, and abdomen. Her blood pressure is 90/60 mm Hg, and her pulse is 120/min. Her forearm is disfigured, and bone can be seen through the wound. She is breathing periodically and has cyanotic lips. Her abdomen is rigid, and there is flank discoloration. Which of the following is the most appropriate next step in management?
(A) Splint the arm and cover wound with sterile gauze
(B) Administer crystalloid solution
(C) Administer vasopressors immediately
(D) Administer packed red blood cells
(E) Perform exploratory laparotomy
109. An 18-year-old male undergoes elective hernia repair. During the operation, he suffers considerable blood loss, and receives a blood transfusion. He then experiences an anaphylactic transfusion reaction. He is resuscitated and further hospital course is uncomplicated. His past medical history is significant for recurrent sinopulmonary infections and intermittent episodes of diarrhea since childhood. Which of the following is the most likely cause of his symptoms?
B. DiGeorge Syndrome
A. lgA deficiency
C. X linked agammaglobulinemia
D. Wiskott-Aldrich syndrome
E. Cystic fibrosis
110. A 12-year-old boy is brought to the emergency department because of severe pain near his left knee. He has sickle cell disease and has been hospitalized previously for sickle cell crisis. Vital signs are notable for persistent fever. Examination of the left lower extremity reveals a normal knee joint with marked tenderness and swelling over the proximal tibia. Laboratory studies show leukocytosis and elevated ESR. Imaging studies confirm the diagnosis of osteomyelitis. Which of the following organisms is the most likely cause of his condition?
B. Pseudomonasspecies
A. Escherichia coli
C. Salmonella species
D. Streptococcus pneumoniae
E. Group B streptococcus
111. A 2-hour-old male neonate has developed worsening cyanosis over the past few minutes. The infant was vaginally delivered (assisted with forceps) at full term and weighed 4.1 kg (9 lb). The Apgar scores were 7 and 8 at 1 and 5 minutes, respectively. Oxygen is administered by mask but does not relieve the cyanosis. Further examination reveals tachypnea, subcostal retractions, a normal first heart sound, a single and loud second heart sound (S2), and no murmur. Which of the following is the most likely cause of the infant's cyanosis?
A. Transposition of the great vessels
B. Atrial septaI defect
C. Coarctation of the aorta
D. Ventricular septal defect
E. Patent ductus arteriosus
112. A 4-week-old infant is brought to the office due to several episodes of vomiting over the past week. The episodes have progressively become more frequent and forceful, but the vomitus never contains any blood or bile. The infant has been breastfed since birth. His vital signs are stable, and he is afebrile. An olive-shaped mass is palpated just to the right of the umbilicus, and peristaltic waves are seen in the upper abdomen. Lab studies reveal a sodium level of 135 mEq/L, potassium level of 3.3 mEq/L, chloride level of 92 mEq/L and bicarbonate level of 30 mEq/L. Which of the following is the most appropriate diagnostic test for this patient?
A. Abdominal ultrasound
B. Plain abdominal x-rays
C. Contrast radiography
D. Gastroduodenoscopy
E. CT scan of the abdomen
113. A one-year-old girl is brought to the office for the evaluation of sickle cell anemia. Both her parents have sickle cell trait, and her elder sister has sickle cell anemia. Her vital signs are stable. Her height and weight are appropriate for age. On examination, she appears healthy and normal. Her birth and past medical histories are insignificant. Hemoglobin electrophoresis reveals 40% hemoglobin S. What is the most common presentation of this condition?
A. Acute painful episodes
B. Painless hematuria
C. Splenic infarction
D. Dactylitis
E. Frequent UTI
114. A boy is brought to the office by his parents for a routine visit. During the physical examination, he can obey two-step commands, use two- to three-word phrases, and can build a tower of six blocks. According to his mother, he can walk up and down the stairs without help. What is the most likely age of this child?
B. 18 months
A. 15 months
C. 2 years
D. 3 years
E. 4 years
115. A 5-year-old girl presents to the emergency department with acute onset of muscle weakness. The mother carried the girl to the examination room and states that the muscle weakness started in her daughter's legs yesterday. The weakness became worse today and progressed to the trunk and both arms. She was also complaining difficulty of breathing earlier today. She has been otherwise healthy but had a common cold about 10 days ago. On examination, her respirations are 26/min and shallow. She has profound muscle weakness in her lower extremities, and moderate weakness in her upper extremities. Her deep tendon reflexes are absent. A lumbar puncture is performed, which shows increased protein concentration but no pleocytosis. Which of the following is the most likely diagnosis?
B. Dermatomyositis
A. Botulism
C. Guillain-Barré syndrome
D. Myasthenia gravis
E. Toxic neuropathy
116. A full-term infant is brought to the office on her 6th day of life because her mother noted that she looked "yellow". The mother states that the infant is strictly breast-fed and has been eating every 2-3 hours. On examination, she is noted to be jaundiced over her trunk and face. There is no scleral icterus. She is otherwise healthy. Both the mother and baby are Rh positive. Which of the following is the most likely cause of this infant's jaundice?
B. Glucose-6-phosphate dehydrogenase (G6PD) deficiency
A. Breast-feeding jaundice
C. Hypothyroidism
D. Physiologic jaundice
E. Rh incompatibility
117. A 4-year-old girl was diagnosed of left-side otitis media about 10 days ago and was prescribed oral amoxicillin, 40 mg/kg/day for 7 days. She has since developed bloody diarrhea with mucus, crampy abdominal pain, and fever. On physical examination, her temperature is 39.4 C (102.9 F), pulse is 88/min, and respirations are 16/min. She has normal bowel sounds and is diffusely tender to palpation. Which of the following is the most appropriate initial step in diagnosis?
A. Barium enema
B. Evaluation of stool for Clostridium difficile toxins
C. Evaluation of stool for rotavirus
D. Stool examination for ova and parasites
E. Stool Hemoccult test
118. A 5-year-old pedestrian is hit by a car in a mall parking lot and he is brought to the emergency department. There was loss of consciousness for less than 1 minute. On evaluation, the child has no neurologic deficits and a CT scan of the head reveals no intracranial abnormalities and no obvious skull fractures. The parents want to know what possible long-term problems there might be. You remember that problems after head trauma may include the development of seizures and that the risk of developing posttraumatic epilepsy is increased by which of the following?
(B) an acute intracranial hemorrhage
(A) a brief loss of consciousness
(C) retrograde amnesia
(D) posttraumatic vomiting
(E) a small linear skull fracture
119. A 4-year-old previously healthy but unimmunized boy presents with sudden onset of high fever, inspiratory stridor, and refusal to drink. Of the following causes of inspiratory stridor, which best fits this clinical scenario?
(B) vascular ring
(A) epiglottitis
(C) croup
(D) foreign body aspiration
(E) laryngeal tumor
120. A week-old infant presents blood in his stools. He was born at home, with the father assisting in the delivery; no physician or midwife was present. He has been breast-fed and has been nursing well. On examination, you also note some blood in his nose. He is not jaundiced; a rectal examination and guaic test of the stool confirms that blood is present. His examination is otherwise normal. He is on no medications. Which of the following is the most likely diagnosis?
(B) vitamin K deficiency
(A) child abuse
(C) breast milk allergy
(D) sepsis
(E) liver disease
121. A 16-year-old boy with a history of ulcerative colitis presents to the physician complaining of diarrhea and a rash. He states that his appetite has been decreased recently, and also complains of nausea and abdominal pain in addition to watery diarrhea. He has an erythematous rash on his distal arms and legs that "burns". His mother reports that he has had poor concentration and has been irritable lately. Vital signs are stable. Examination reveals a beefy red tongue that appears swollen. Abdominal examination is normal. The rash resembles a sunburn and is located on his distal arms and legs. It is symmetrical and tender to palpation. Neurological examination is normal. This patient's symptoms are most likely due to a deficiency of which of the following vitamins?
A. Thiamine
B. Riboflavin
C. Niacin
D. Pyridoxine
E. Cyanocobalamin
122. A 9-month-old child comes in for a routine visit. She has had several episodes of otitis media in the past, but no major illnesses or hospitalizations. Her mother is concerned because the child was previously happy and social around other people, but now cries if her mother is not in the room. The child constantly wants to be held by her mother and becomes upset if her mother walks into the next room. Her grandmother keeps her during the day, and she now cries when her mother leaves her in the morning. Developmentally, she is crawling and waves bye-bye. She does not yet respond to her name or say words. She previously babbled but stopped several months ago. When you hide a toy with your hand, she lifts your hand to look for the toy. Which of the following is the best next step in the management of this child?
B. Audiology evaluation
A. Psychological evaluation
C. Physical therapy evaluation
D. Social services referral
E. Reassure the mother that the child's development is normal.
123. A 12-year-old American boy comes to you with the complaints of abdominal pain and dark urine. On examination he has normal vitals, icteric sclerae, and abdominal tenderness with a mass palpable in right upper quadrant. His laboratory report shows bilirubin: 6.5 mg/di, negative viral serologies and mild elevations of amylase and lipase. Ultrasonography shows a cystic extra hepatic mass and a gall bladder separated from the mass. What is the most likely diagnosis in this patient?
A. Caroli's syndrome
B. Choledochal cyst
C. Biliary abscess.
D. Biliary atresia.
E. Pseudo pancreatic cyst
124. A 10-year-old boy has been having “bellyaches” for about 2 years. They occur at night as well as during the day. Occasionally, he vomits after the onset of pain. Occult blood has been found in his stool. His father also gets frequent, nonspecific stomachaches. Which of the following is the most likely diagnosis?
B. Appendicitis
A. Peptic ulcer
C. Meckel diverticulum
D. Functional abdominal pain
E. Pinworm infestation
125. An 8-year-old boy presents to your office for a second opinion. He has a 2-year history of intermittent vomiting, dysphagia, and epigastric pain. His father reports he occasionally gets food “stuck” in his throat. He has been on a proton pump inhibitor for 18 months without symptom relief. His past history is significant only for eczema and a peanut allergy. Endoscopy was performed 6 months ago; no erosive lesions were noted and a biopsy was not performed. You arrange for a repeat endoscopy with biopsy. Microscopy on the biopsy sample reveals many eosinophils. Treatment of this condition should include which of the following?
B. Prolonged acid blockade
A. Corticosteroids
C. Treatment for Candida sp
D. Treatmentfor Aspergillus sp
E. Observation
126. A 4-year-old girl presents to the emergency department with fever and a petechial rash. A sepsis workup is performed, and IV antibiotics are administered. Gram-negative diplococci are identified in the CSF. Which of the following is true of this condition?
(A) Antibiotic prophylaxis of fellow daycare attendees is not necessary.
(B) The most common neurologic residual is seizures.
(C) The presence of meningitis decreases the survival rate.
(D) Shock is the usual cause of death.
(E) Vancomycin administered intravenously is the treatment of choice.
127. A 3-year-old boy suddenly begins choking and coughing while eating peanuts. On physical examination he is coughing frequently. He has inspiratory stridor and mild intercostal and suprasternal retractions. Initial management should include which of the following?
(B) abdominal thrusts
(A) back blows
(C) blind finger-sweeps of the hypopharynx
(D) permitting him to clear the foreign body by coughing
(E) emergency tracheostomy
128. During a well-child visit, the grandmother of an 18-month-old patient is concerned because the child’s feet turn inward. She first noticed this when her grandson began to walk. It does not seem to bother the child. On examining his gait, his knees point forward and his feet turn inward. Which of the following is the most likely cause of this condition?
(B) femoral anteversion
(A) adducted great toe
(C) Legg-Calvé-Perthes disease
(D) medial tibial torsion
(E) metatarsus adductus
129. Two weeks after a viral syndrome, a 9-year-old boy presents to your clinic with a complaint of several days of weakness of his mouth. In addition to the drooping of the left side of his mouth, you note that he is unable to completely shut his left eye. His smile is asymmetric, but his examination is otherwise normal. Which of the following is the most likely diagnosis?
B. Botulism
A. Guillain-Barré syndrome
C. Cerebral vascular accident
D. Brainstem tumor
E. Bell palsy
130. An infant can regard his parent’s face, follow to the midline, lift his head from the examining table, smile spontaneously, and respond to a bell. He does not yet regard his own hand, follow past the midline, nor lift his head to a 45° angle off the examining table. Which of the following is the most likely age of the infant?
B. 3 months
A. 1 month
C. 6 months
D. 9 months
E. 12 months
131. A child is brought to your clinic for a routine examination. She can put on a T-shirt but requires a bit of help dressing otherwise. She can copy a circle well but has difficulty in copying a square. Her speech is understandable and she knows four colors. She balances proudly on each foot for 2 seconds but is unable to hold the stance for 5 seconds. Which of the following is the most likely age of this child?
B. 2 years
A. 1 year
C. 3 years
D. 4 years
E. 5 years

132. A 4-year-old girl is noticed by her grandmother to have a limp and a some-what swollen left knee. The parents report that the patient occasionally com- plains of pain in that knee. An ophthalmologic examination reveals findings as depicted in the photograph. Which of the following conditions is most likely to be associated with these findings?
B. Slipped capital femoral epiphysis
A. Juvenile rheumatoid arthritis
C. Henoch-Schönlein purpura
D. Legg-Calvé-Perthes disease
E. Osgood-Schlatter disease
133. A 1-month old boy is brought to the emergency department by his mother, who states that he has been having what she describes as "projectile vomiting" for the past several days. She states that he vomits every time she feeds him, and the situation seems to be getting worse, although he does not seem to be in pain. She describes the vomitus as non-bilious, and he has had normal stools with no blood in them. On examination, the infant appears to be mildly dehydrated, his abdomen is soft, and there is a palpable, olive-sized, firm moveable mass in the right upper quadrant. Which of the following is the most likely diagnosis?
B. Intussusception
A. Duodenal atresia
C. Hirschsprung disease
D. Midgut volvulus
E. Pyloric stenosis
134. A 3-month old infant is brought to a pediatrician's office because of increased lethargy and irritability. The parents state that the child rolled off the couch and fell on the floor one day prior to presentation. His parents report that the child has been previously healthy and is up to date on his vaccinations. He has been meeting his development milestones. His fontanelles are full. While in office the patient develops a tonic-clonic seizure. Which of the following is the next appropriate step?
B. Perform a retinoscopic examination
A. Obtain a head computerized tomography scan
C. Check serum levels of ammonia
D. Administer intravenous benzodiazepines
E. Perform a lumbar puncture
135. A toddler is brought to the emergency department with burns on both of his buttocks. The areas are moist, have blisters, and are exquisitely painful to touch. The parents explain that the child accidentally pulled a pot of boiling water over himself. Which of the following is the most important step in management?
B. Early excision and grafting of the burned areas
A. Application of mafenide acetate to the burned areas
C. Education of the parents on accident prevention
D. Prompt administration of fluid resuscitation
E. Referral to the proper authorities for suspected child abuse
136. A pediatrician examines a 2-month-old infant who had been born at term. The pediatrician hears a continuous murmur at the upper left sternal border. The peripheral pulses in all extremities are full and show widened pulse pressure. Which of the following is the most likely diagnosis?
A. Coarctation of the aorta
B. Patent ductus arteriosus
C. Peripheral pulmonic stenosis
D. Persistent truncus arteriosus
E. Ventricular septal defect
137. A 3-week-old infant is being evaluated for hema- : tochezia. His mother states that the infant passed stools j that contain both blood and mucus. There were no complications during her pregnancy, and the infant has been otherwise healthy. On physical examination, his temperature is 37.1 C (98.9 F), pulse is 110/min, and respirations are 18/min. He appears well, and his fontanelle is flat and level. Abdominal examination reveals normal active bowel sounds; his abdomen is nontender to palpation and there is no mass. His diaper contains stool that has bright red blood on it with mucus. Which of the following is the most likely explanation of his hematochezia?
(A) Food allergy-induced colitis
(B) Meckel diverticulum
(C) Necrotizing enterocolitis
(D) Rectal fissure
(E) Ulcerative colitis j
138. A 7-year-old boy is brought to the physician because of a persistent mucopurulent nasal discharge for 2 weeks following a common cold. The mother also reports that the child has had frequent cough during the day and occasional temperatures up to 38.0 C (100.5 F). The child does not appear critically ill, but he complains of mild pain in the maxillary region and nasal obstruction. Rhinoscopic examination reveals a rivulet of purulent fluid coming from the inferior meatus. The rest of the physical examination is normal. Which of the following is the most likely diagnosis?
(A) Acute bacterial sinusitis
(B) Acute otitis media
(C) Acute viral rhinitis
(D) Allergic rhinosinusitis
(E) Asthma
139. A9-year-old boy presents with a several-day history of progressive arm and leg weakness. He has been well except for an upper respiratory infection 2 weeks ago. The patient is alert and oriented. On repeated examination, the heart rate varies between 60 and 140 beats/min, and the blood pressure (BP) varies between 90/60 and 140/90 mmHg. Respirations are shallow, with a rate of 50/min. There is symmetric weakness of the face and all four extremities. Deep tendon reflexes are absent. Sensation is intact. Which of the following is the most likely diagnosis?
(B) myasthenia gravis
(A) polymyositis
(C) transverse myelitis
(D) Guillain-Barré syndrome
(E) viral encephalitis
140. An 18-month-old boy is brought to the clinic for a checkup. As part of his routine care, a serum lead level is obtained. It is 25 g/mL. Which of the following is the most appropriate next step in his management?
(A) chelation with CaEDTA
(B) chelation with succimer
(C) investigation of his home for lead hazards
(D) reassurance that this level is not a problem
(E) repeating the level in 6 months
141. An infant is due for her first dose of polio vaccine. Her parents have heard that there are two different types of vaccine for polio. They want to know why their daughter needs to get another shot rather than just taking the oral form of the vaccine. You tell the parents the major advantage of the injectable vaccine is which of the following?
(B) increased mucosal immunity
(A) lower cost
(C) better efficacy
(D) avoidance of vaccine-associated paralytic poliomyelitis
(E) boosting her immunity through secondary transmission
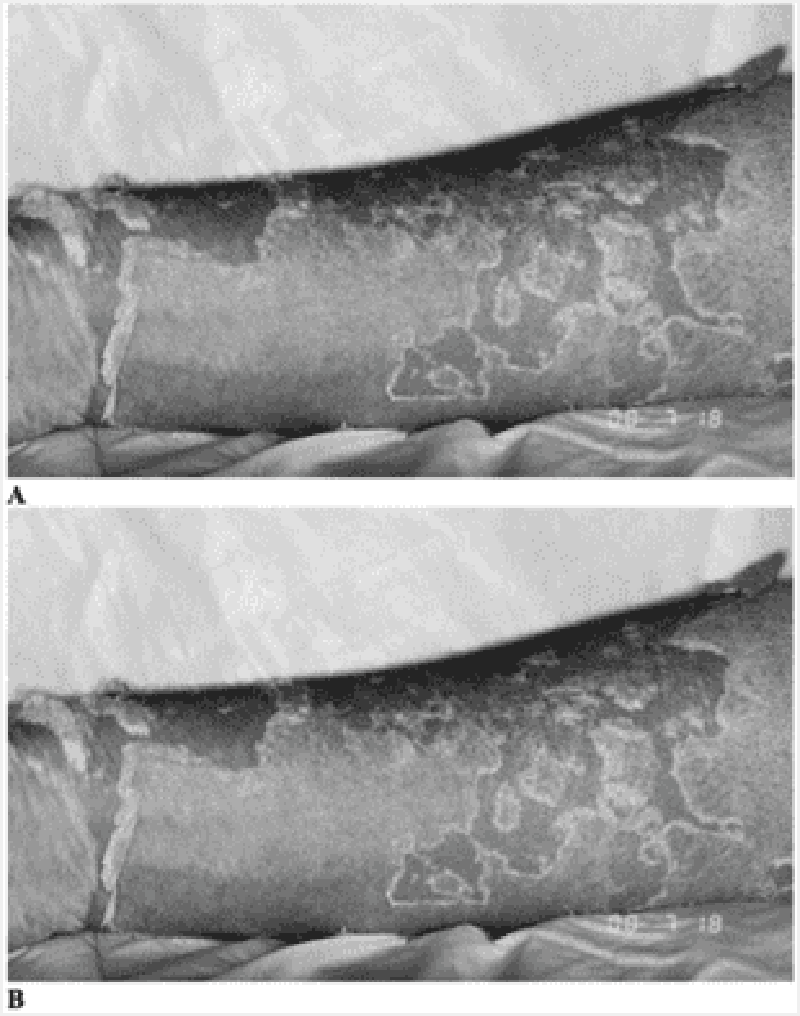
142. A previously healthy 4-year-old child pictured below presents to the emergency room (ER) with a 2-day history of a brightly erythematous rash and temperature of 40°C (104°F). The exquisitely tender, generalized rash is worse in the flexural and perioral areas. The child is admitted and over the next day develops crusting and fissuring around the eyes, mouth, and nose. The desquamation of skin shown in the photograph occurs with gentle traction. Which of the following is the most likely diagnosis?
A. Epidermolysis bullosa
B. Staphylococcal scalded skin syndrome
C. Erythema multiforme
D. Drug eruption
E. Scarlet fever
143. A patient comes to your office for a hospital follow-up. You had sent him to the hospital 3 weeks earlier for persistent fevers but no other symptoms; he was diagnosed with endocarditis and is currently being treated appropriately. Advice to this family should now include which of the following?
A. Restrict the child from all strenuous activities.
B. Give the child a no-salt-added diet.
C. Provide the child with antibiotic prophylaxis for dental procedures
D. Test all family members in the home with repeated blood cultures.
E. Avoid allowing the child to get upset or agitated.
144. A mother calls you on the telephone and says that your 4-year-old son bit the hand of her 2-year-old son 48 hours previously. The area around the injury has become red, indurated, and swollen, and he has a temperature of 39.4°C (103°F). Which of the following is the most appropriate response?
B. Admit the child to the hospital immediately for surgical debridement and antibiotic treatment
A. Arrange for a plastic surgery consultation at the next available appointment.
C. Prescribe penicillin over the telephone and have the mother apply warm soaks for 15 minutes four times a day.
D. Suggest purchase of bacitracin ointment to apply to the lesion three times a day.
E. See the patient in the ER to suture the laceration.
145. A 6-year-old boy is brought to the emergency department (ED) by the paramedics due to nausea, vomiting, diarrhea and abdominal pain over the past hour. His mother found an open multivitamin supplement bottle and some pills scattered on the kitchen floor. After his admission to the ED, he starts hyperventilating and experiences hematemesis. His blood pressure is 90/60 mmHg, pulse is 130/min, respirations are 50/min and temperature is 37.2 C (99F). Abdominal plain x-ray reveals several small opacities in the stomach and duodenum. Lab results are: Hb 13.5 g/dL Ht 42% WBC 10,000/cmm Platelets 300,000/cmm Blood Glucose 118 mg/dL Serum Na 135 mEq/L Serum K 34 mEq/L Chloride 102 mEq/L Bicarbonate 16 mEq/L BUN 16 mg/dL Serum Creatinine 1.0 mg/dL pH 7.30 P02 90 mm Hg PC02 29 mm Hg What is the most likely diagnosis?
B. Vitamin A poisoning
A Riboflavin poisoning
C. Vitamin D poisoning
D. Vitamin K poisoning
E. Iron poisoning
146. A 3-year-old boy is brought to the office by his mother because he has been having painless passage of black stools for the past few days. Otherwise, his bowel habits are normal. He has no other medical problems. He takes no medication. His vital signs are within normal limits. The physical examination is unremarkable. What is the most likely diagnosis of this patient?
B. Anal fissure
A. Peptic ulcer disease
C. Intussusception
D. Inflammatory bowel disease
E. Meckel's diverticulum
147. A 3-year-old boy is brought to the office by his parents for the evaluation of dry eyes and photophobia. He has some difficulty in adapting to darkness. He is a very poor eater, and his diet consists mainly of canned foods, and very rarely, fresh vegetables or milk. Examination reveals dry, scaly skin, follicular hyperkeratosis in the extensor surfaces of the extremities, and dry, silver-gray plaques on the bulbar conjunctiva. What is the most likely diagnosis of this patient?
B. Thiamine deficiency
A Vitamin A deficiency
C. Ariboflavinosis
D. Scurvy
E. Hypervitaminosis A
148. A 2-week-old Caucasian male presents with constipation since birth. He was born full term via a normal vaginal delivery. He did not pass meconium till his 3rd day of life, after he was given a glycerin suppository. He has since stooled every 3–4 days, only with the help of a suppository. The stools are pellet like. He has had increasing abdominal distention. On rectal examination, tone appears normal and the ampulla contains no stool. Which of the following is the most likely cause?
(B) Hirschprung disease
(A) cystic fibrosis
(C) anal stenosis
(D) functional constipation
(E) hypothyroidism
149. Which of the following is the most appropriate evaluative procedure for an otherwise normal 7-day-old boy with perineal hypospadias?
(A) renal ultrasonography
(B) serum creatinine determination
(C) cystography
(D) circumcision
(E) intravenous pyelography (IVP)
150. A 44 year old woman delivers a 3120 g (6 lb 14 oz) newborn male. Her pregnancy was normal except that she noted decreased fetal movement compared to her previous pregnancies. She declined an amniocentesis offered by her obstetrician. Physical examination of the newborn reveals an infant with facial features suggestive of Down Syndrome. The infant then has bilious vomiting. An x-ray film showing the kidneys, ureters, and bladder (KUB) is performed, which shows a "double bubble" sign. Which of the following is the most likely cause of the abdominal signs and symptoms?
A. Duodenal atresia
B. Hirschsprung Disease
C. Malrotation
D. Meconium ileus
E. Pyloric stenosis
151. The parents of a 10-year-old girl with newly diagnosed, generalized tonic-clonic epilepsy come to the physician seeking advice regarding what they should do when the child has a seizure. Which of the following suggestions is appropriate?
B. Put something in the child's mouth at the onset of seizure
A. Call an ambulance immediately as soon as seizure begins
C. Try to place the child on her side during the seizure
D. Try to restrain the child during the seizure
E. Do not allow the child to return to her activities after recovery
152. A 10-year-old boy has a long history of recurrent infections. These have included pneumonia, suppurative lymphadenitis, persistent rhinitis, dermatitis, diarrhea, and perianal abscesses. Involved organisms have included Staphylococcus aureus, Serratia, Escherichia coli, and Pseudomonas. Biopsy of skin and lymph nodes have demonstrated granulomatous lesions, even though the only species isolated were those noted above. Immunoglobulin levels are higher than normal. Which of the following findings would be most helpful in establishing the diagnosis?
A. Absent B cells and normal numbers of T cells
B. Deficient nitroblue tetrazolium dye reduction in neutrophils
C. High serum IgM and very low serum IgG
D. Very low CD11 on the surface of white blood cells
E. Very low serum calcium levels
153. A 9-year-old Caucasian male complains of fever, sore throat and difficulty swallowing. Small tender lymph nodes are palpated in the cervical region. The symptoms subside quickly on penicillin therapy. Ten days later, the patient presents again with fever, skin rash and fleeting joint pain in the lower extremities. Physical examination reveals scattered urticaria and palpable lymph nodes in the cervical, axillary and inguinal regions. Which of the following is the most likely cause of this patient's current complaints?
B. Drug-induced reaction
A. Rheumatic fever
C. Lymphoproliferative disorder
D. Henoch-Schonlein purpura
E. Infective endocarditis
154. A 4-week-old male infant is brought to the office due to several episodes of projectile vomiting for the last few days. The vomitus contains milk and doesn't contain bile or blood. The child's appetite has increased for the last few days. He has been fed with goat's milk since birth, but doesn't seem to tolerate it anymore for the last few days. He vomits a few minutes after feedings. He appears dehydrated, and abdominal examination reveals no mass. Blood tests reveal macrocytosis. What is the most appropriate next step in the management of this patient?
B. Ultrasound of the abdomen
A. Barium swallowing
C. Substitute goat's milk with another form of milk
D. Divide his feedings
E. Add folic acid to relieve his vomiting
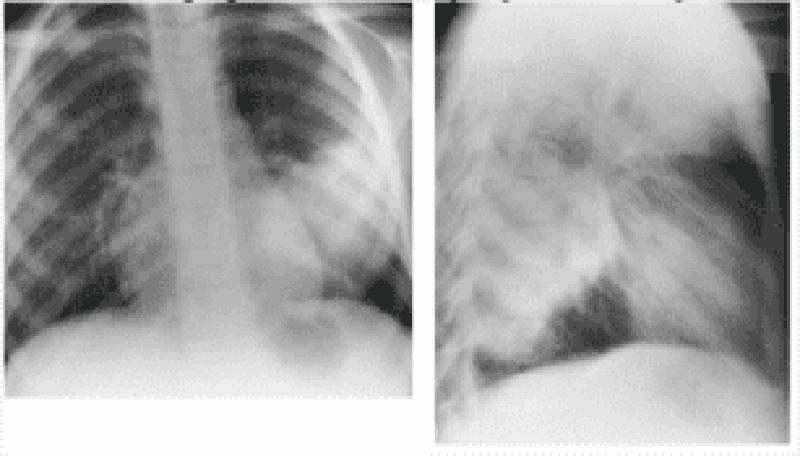
155. A 10-year-old boy presents with a 1-day history of fever, cough, and chest pain. He has not been eating and has been listless. He does not have any previous history of health problems. On physical examination, his temperature is 40°C, and he is tachypneic. He looks ill. He has rales on his left posterior lower lung fields. You order a chest x-ray. Which of the following organisms is most likely responsible for his pneumonia?
(A) Haemophilus influenzae
(B) Mycoplasma pneumoniae
(C) Pneumocystis carinii
(D) Staphylococcus aureus
(E) Streptococcus pneumoniae
156. A 10-year-old patient with sickle cell disease comes to the physician for a routine visit. The patient has a history of multiple pain crises and pneumonias. He was started on hydroxyurea one year ago and has not had any further pain crises since then. He has had no recent illnesses or hospitalizations. His physical examination is unremarkable. The patient's laboratory results are shown below. Complete blood count Hemoglobin 9.0 g/L Erythrocyte count 2.2 mln/mm3 MCHC 32% MCV 105 fl Reticulocytes 2.0% Platelets 212,000/mm3 Leukocyte count 9500/mm3 Neutrophils 56% Eosinophils 3% Lymphocytes 36% Monocytes 5% Which of the following best describes the role of hydroxyurea in the treatment of patients with sickle cell disease?
B. Lyses microthrombi in the circulation
A. Removes sickled red blood cells from the circulation
C. Protects against encapsulated bacterial infections
D. Increases fetal hemoglobin
E. Chelates iron to prevent iron toxicity
157. A 2-year-old child is brought to the physician for a routine visit. He is growing and developing appropriately. He eats a variety of foods including meat, vegetables, and fruits, and drinks 3-4 glasses of whole milk each day. He is starting to put words together into short sentences. His mother has no concerns. Physical examination is unremarkable. Routine laboratory studies show the following: Hemoglobin 9.5 g/dl RDW 14% MCV 65 fl Reticulocyte count 3.0% Platelet count 212,000/mm3 Leukocyte count 6,500/mm3 TIBC 300 mcg/dl (240-450 mcg/dl) Ferritin 1 00 ng/ml (7 -140 ng/ml) What is the most likely cause for this child's anemia?
B. Anemia of chronic disease
A. Iron deficiency
C. Thalassemia trait
D. Cyanocobalamin deficiency
E. Spherocytosis
158. A previously healthy 5-year-old girl is brought to the physician for evaluation of night awakenings. She has woken up screaming in each of the past three nights about one hour after going to sleep. When her parents go to her room, she is crying, sweating, and looks frightened. She does not respond to her parents and does not seem fully awake. When her parents hold her, she calms down and goes back to sleep. The next morning, she does not recall the incident. She started kindergarten this week and has just begun going all day without taking a nap. On examination, she is afebrile and her vital signs are within normal limits. A complete physical examination is unremarkable. What is the most likely diagnosis?
B. Somnambulism
A Nightmare
C. Epilepsy
D. Night terrors
E. Benign paroxysmal vertigo
159. A 3-year-old boy is brought to the ER with a two-day history of decreased appetite, neck swelling, and irritability. He keeps his head rotated slightly to the right side. He resists passive flexion of the neck and rotation to the left side. Which of the following is the best next step in managing this patient?
B. Soft neck collar
A Direct laryngoscopy
C. X-ray of the neck
D. Lumbar puncture
E. Botulinum toxin injection
160. A previously healthy 15-month-old girl is brought to the emergency department after she had several episodes in which she lost consciousness after crying. Her parents state that the episodes always occur when the child gets frustrated or upset. She has no cyanosis or incontinence. The episodes last about 45 seconds each. After the episode, she is alert and appropriate. Physical examination is unremarkable. What is the next best step in the management of this patient?
B. Obtain an electroencephalogram
A. Reassure the parents
C. Obtain an electrocardiogram
D. Computed tomography of the head
E. Magnetic resonance imaging of the brain
161. A patient has the sudden onset of fretfulness and pain. He curls up with his legs drawn in to his abdomen. Over the next few hours he continued to have episodes of pain and cries with tears, but between these times he acts normally. The patient's mother fears something is terribly wrong and brings him to the hospital. His past medical history was unremarkable. The previous week he had had a cold with a runny nose. His stools had been normal that day. On examination he is quiet and his abdomen is surprisingly soft and normal. In the emergency room there is a semi-soft stool with some blood mixed with mucus. This classic presentation of intussusception is most likely to occur in which of the following age groups?
B. 6 to 12 months of age
A. Birth to 4 weeks of age
C. 3 to 5 years of age
D. Early adolescence
E. Late adolescence
162. A 12-year-old boy is brought to the clinic because of a several-month history of strange behavior. According to his parents, the boy occasionally will start staring and not respond. He will also have tears in his eyes. These episodes last several seconds and he then returns to his baseline. He has not sustained any head trauma and is on no medications. Which of the following drugs is the most appropriate treatment?
B. Diphenhydramine
A. Diazepam
C. Ethosuximide
D. Phenobarbital
E. Phenytoin
163. A 9-month-old is brought to the emergency center by ambulance. The child had been having emesis and diarrhea with decreased urine output for several days, and the parents noted that she was hard to wake up this morning. Her weight is 9 kg, down from 11 kg the week prior at her 9-month checkup. You note her heart rate and blood pressure to be normal. She is lethargic, and her skin is noted to be “doughy.” After confirming that her respiratory status is stable, you send electrolytes, which you expect to be abnormal. You start an IV. Which of the following is the best solution for an initial IV bolus?
B. D10 water (100 g glucose/L)
A. One-fourth normal saline (38.5 mEq sodium/L)
C. Normal saline (154 mEq sodium/L)
D. 3% saline (513 mEq sodium/L)
E. Fresh-frozen plasma
164. You are admitting to the hospital a 3-month-old infant who has been having poor feeding, emesis, and diarrhea for 3 days. In the emergency center, her electrolytes were found to be: sodium 157 mEq/L, potassium 2.6 mEq/L, chloride120 mEq/L, bicarbonate 14 mEq/L,creatinine1.8 mEq/L, blood urea nitrogen(BUN) 68 mEq/L, and glucose195 mEq/L. She was given a fluid bolus in the emergency center and has subsequently produced urine. Which of the following is the most appropriate next step in her management?
B. Continued rapid volume expansion with 1/4 normal saline
A. Slow rehydration over 48 hours
C. Packed red blood cells (RBCs)
D. Rehydration with free water
E. Urinary electrolytes
165. At exploratory laparotomy for blunt abdominal trauma, a 14-year-old boy is found to have a ruptured spleen. The spleen is shattered into multiple fragments, and there are other serious intraabdominal injuries that will require significant operative time. For the above reasons, it is decided that a quick splenectomy is indicated, and it is done. In the postoperative period, this young man should receive which of the following treatments?
(B) Long-term prophylactic antibiotics
(A) Anticoagulation
(C) Platelet transfusions
(D) Prolonged parenteral nutrition
(E) Vaccinations for encapsulated organisms
166. A 10-year-old girl has bullous target lesions and mucosal erythema, which developed after her third dose of trimethoprim-sulfamethoxazole for a urinary tract infection. Which of the following is a likely associated clinical finding?
(B) Fever
(A) Diarrhea
(C) Lymphadenopathy
(D) Vomiting
(E) Nausea
167. A 16-year-old boy is brought into the emergency department by his friends. He is semicomatose, with a pulse of 60/min and respirations of 6-8/min. His pupils are constricted. Which of the following will most likely be revealed on a urine toxicology screen?
B. Cocaine intoxication
A. Amphetamine intoxication
C. Ethanol intoxication
D. Opiate intoxication
E. Tricyclic antidepressant intoxication
168. A 6-month-old previously health child is brought to the doctor's office because of sudden onset of lethargy, constipation, generalized weakness and poor feeding. He has been meeting all development milestones and his immunization schedule is up to date. On further questioning, his parents mention that his diet was recently advanced to a homemade formula of evaporated milk and honey. On physical examination, he has stable vital signs, clear lungs, normal skin turgor and full fontanelles. Which of the following is the most likely explanation for the patient's presentation?
B. Hirschsprung disease
A. Botulism
C. Hypernatremia
D. Hyponatremia
E. Hypothyroidism
169. A 12-year-old girl was hit in the face by a baseball 15 minutes earlier and has had her mandibular incisors knocked out. Which of the following represents the best plan of action?
B. Foreign matter adhering to the teeth should be immediately scrubbed off.
A. The teeth should be rinsed in hot water then carefully dried.
C. The teeth may be transported in tea, juice, or cola.
D. Avulsed teeth can be transported in the mouth of the parent or a cooperative patient.
E. A dental appointment should be made within 48 to 72 hours.

170. A 55-day-old infant born prematurely at 27 weeks of gestation is shown below. The swelling is not tender, firm, hot, or red, and it does not transil luminate. It seems to resolve with pressure, but returns when the infant cries or strains. Which of the following is the most appropriate course of action at this point?
B. Perform a needle aspiration
A. Obtain a surgical consultation
C. Order a barium enema
D. Order a KUB (plain radiographs of kidney, ureter, and bladder)
E. Observe the patient and reassure the patient and family
171. A 17-year-old boy comes to medical attention because of recurrent sinusitis and pneumonia, and persistent watery diarrhea due to Giardia lamblia. His parents and a sister are in excellent health. Physical examination reveals enlarged lymph nodes in cervical, axillary and inguinal regions. A lymph node biopsy shows hyperplastic follicles with an absence of plasma cells. Laboratory investigations show: Hematocrit.......................44% Leukocyte count...............9,800/mm3 Neutrophils.....................55% Lymphocytes..................30% Monocytes.....................5% CD4 T-cell count............1000 cells/mm3 Proteins, serum...............6.2 g/dL Albumin........................5.0 g/dL Globulin........................1.2 g/dL Additional studies demonstrate severely depressed levels of serum IgG, with slightly belownormal levels of IgM and IgA. Which of the following is the most likely diagnosis?
B. Common variable immunodeficiency
A. Acquired immunodeficiency syndrome (AIDS)
C. Hodgkin disease
D. Isolated IgA deficiency
E. X-linked agammaglobulinemia of Bruton
172. An 8-year-old boy presents with a 2-day history of rash. The rash started on the head and spread downward to his trunk and extremities. He also complains of a fever, cough, and a runny nose for the past 5 days. On physical examination, his temperature is 38.2 C (100.7 F), blood pressure is 88/56 mm Hg, pulse is 76/min, and respirations are 16/min. There is a small, irregular red spot with a central gray color on his buccal mucosa. The rash on his body is erythematous and maculopapular in quality. Which of the following is the most likely diagnosis?
B. Hand-foot-mouth disease
A. Erythema infectiosum
C. Measles
D. Roseola infantum
E. Rubella
173. A 4-week-old male infant has been spitting up his formula feedings for the past few days. He does not vomit bilious material or blood. The spitting up is gradually becoming more frequent, and forceful vomiting ensues. The vomitus seems to shoot straight out and nearly hit the wall. On examination, the baby seems hungry and is chewing his fist. His mucous membranes appear dry. A small, round mass, about the size of an adult thumbnail, is palpated in the upper abdomen. Laboratory data reveal Na+ of 133 mEq/L, K+ of 3.5 mEq/L, CI of 93 mEq/L, and HC0 3 - of 29 mEq/L. Which of the following is the most appropriate next step in management?
(A) Change the feedings to clear liquids or Pedialyte
(B) Obtain a surgical consult immediately
(C) Obtain flat plate and upright x-ray films of the abdomen
(D) Insert a nasogastric tube
(E) Begin parenteral antibiotics
174. A 3-year-old child presents in clinic with marked erythema of the cheeks, with no prior symptoms. The rash soon involves the arms and has a reticular erythematous maculopapular appearance. The patient has been previously healthy and is not on any medications. He has not been exposed to any other ill individual. Which of the following is the most likely diagnosis?
(B) Measles
(A) Fifth disease (erythema infectiosum)
(C) Roseola
(D) Rubella
(E) Varicella
175. The mother of a 6-month-old infant is concerned that her baby may be teething. You explain to her that the first teeth to erupt in most children are which of the following?
B. Maxillary lateral incisors
A. Mandibular central incisors
C. Maxillary first molars
D. Mandibular cuspids (canines)
E. First premolars (bicuspids)
176. A male infant born at term is found to have bilateral colobomas, choanal atresia, ear anomalies, and cryptorchidism. There is no history maternal drug or alcohol abuse during pregnancy. There is no family history of similar congenital defects. Which of the following is the most appropriate initial test to exclude any associated abnormalities?
B. Echocardiography
A. Barium swallow
C. Fiberoptic bronchoscopy
D. Renal ultrasonography
E. Skeletal survey
177. A 15-year-old girl presents to the emergency department with the sudden onset of watery diarrhea tinged with blood. The girl was previously healthy. Her only medications are topical benzoyl peroxide and oral clindamycin for acne vulgaris. Physical examination reveals a slightly distended abdomen that is diffusely tender. Her temperature is 38.1 C (100.5 F). She has not been exposed to any uncooked meat and has not eaten any unusual foods. Which of the following is the most likely diagnosis?
B. Irritable bowel syndrome
A. Gastroenteritis
C. Pseudomembranous enterocolitis
D. Salmonella infection
E. Ulcerative colitis
178. A 22-year-old woman has just delivered a male infant at 41 weeks of gestation. Her medical history is normal and her pregnancy was uncomplicated. She is an assistant in a veterinary clinic. Examination of the infant reveals jaundice, hepatosplenomegaly, and generalized lymphadenopathy. During the examination, he suddenly begins to have tonicclonic seizures. The CT scan reveals active inflammatory lesions, hydrocephalus and intracranial calcifications. What is the most likely diagnosis of this patient?
B. Congenital rubella
A. Congenital syphilis
C. Congenital toxoplasmosis
D. Congenital herpes simplex
E. Congenital hepatitis B
179. A 5-year-old girl is brought to the physician's office for a follow-up visit after recovering from an episode of acute bacterial meningitis. Five weeks ago, she developed pneumococcal meningitis, and was admitted to the hospital, where she underwent lumbar puncture, CT scan of the head, and ceftriaxone therapy. She was discharged in a stable condition. According to the mother, the child has not been performing well in school since her illness. She also noticed that the child has forgotten how to copy figures such as triangles and squares, and is unable to identify colors accurately. What is the most likely cause for the regression of milestones in this patient?
B. Lumbar puncture
A. Drug reaction
C. Meningitis
D. Alexia
E. Amnesia
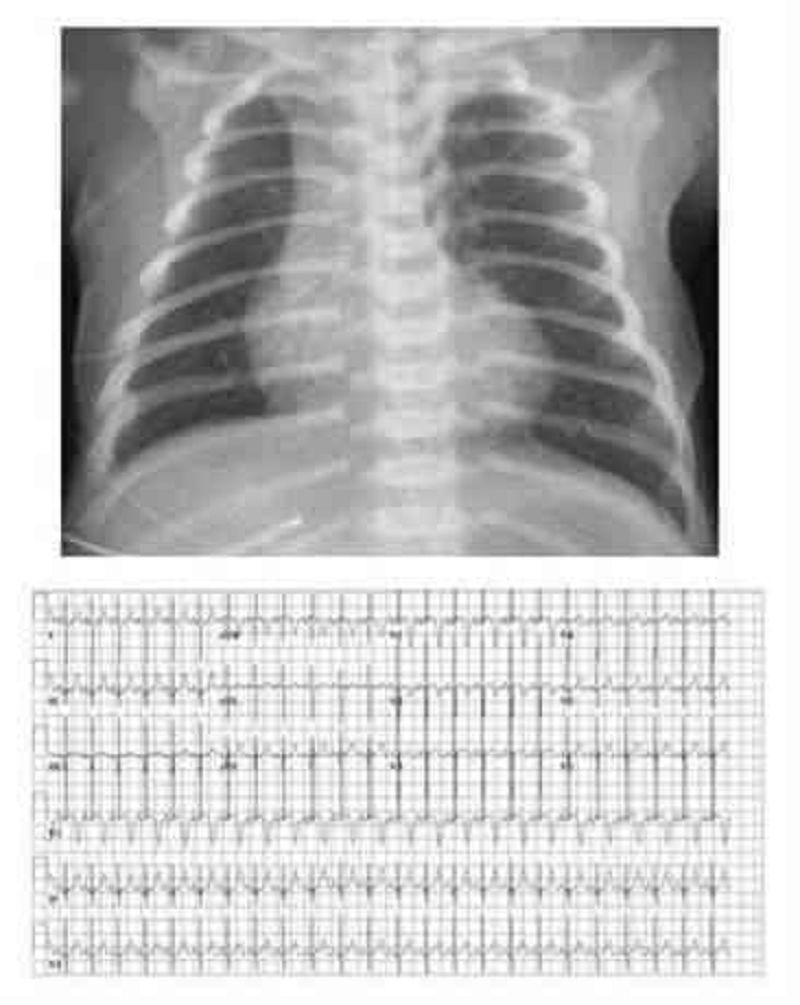
180. You are seeing a 2-year-old boy for the first time. His father denies any past medical or surgical history, but does note that the child’s day care recently sent a note home asking about several episodes, usually after the child does not get what he wants, when he “breathes funny” and sits in a corner with his knees under his chin for a few minutes. The day-care staffers think this “self-imposed time-out” is a good thing, but they worry about the breathing. One teacher even though he once looked blue, but decided that it was probably because of the finger paints he had been using. On examination, you identify a right ventricular impulse, a systolic thrill along the left sternal border, and a harsh systolic murmur (loudest at the left sternal border but radiating through the lung fields). His chest radio- graph and ECG are shown. Which of the following congenital cardiac lesions would you expect to find in this child?
B. Right ventricular outflow obstruction
A. Patent ductus arteriosus
C. Atrial septal defect (ASD)
D. Transposition of the great vessels with a patent foramen ovale
E. Hypoplastic left heart
181. The parents of a 2-month-old baby boy are concerned about his risk of coronary artery disease because of the recent death of his 40-year-old maternal uncle from a myocardial infarction. Which of the following is the most appropriate management in this situation?
B. Counsel the parents regarding appropriate dietary practices for a 2-monthold infant and test him for total cholesterol at 6 months of age.
A. Screen the parents for total cholesterol
C. Reduce the infant’s dietary fat to less than 30% of his calories by giving him skim milk.
D. Initiate lipid-lowering agents.
E. Recommend yearly ECGs for the patient.
182. An 8-month-old female infant is brought to the clinic for a well-baby examination. She was born prematurely at 35 weeks gestation. She weighs 2.3kg (5 Ib). She cannot sit unsupported. Physical examination reveals mild facial hypoplasia, epicanthal folds, micrognathia, long nasal philtrum, thin upper lip and short palpebral fissures. Auscultation of the heart reveals an III/ IV harsh holosystolic murmur over the precordium. Her karyotype is normal. What is the most likely cause of these findings?
B. Moderate or excessive intake of alcohol during pregnancy
A. Maternal age
C. Treatment with lithium for manic disorder
D. Maternal hyperglycemia
E. Infection with rubella during pregnancy
183. A 12-year-old boy is brought to the clinic by his parents because "he cannot walk anymore." Yesterday, he became irritable, uneasy, and complained of tingling and weakness in both his legs. This morning, he couldn't stand up or move his legs, and complained of pain in his leg and thigh muscles. He denies any headaches, nausea or vomiting. He had an episode of febrile diarrhea 10 days ago. His family history is unremarkable. Physical examination reveals symmetric flaccid paralysis of both legs, absent deep tendon reflexes, and decreased superficial touch and vibratory sense. There is no nuchal rigidity. What structure is most likely affected in this patient's condition?
B. Medial lemniscus
A. Cerebral cortex
C. Corticospinal tract
D. Gracile fasciculus
E. Peripheral nerves
184. A 5-month-old infant is brought to the physician for a routine visit. The child was born full term without complications. The infant has been seen several times for poor weight gain. The infant takes 5 ounces of formula every 4 hours, and has been tried on increased calorie formula without success. Family history is significant only for nephrolithiasis. On examination, the infant's weight is <5%, height is at the 20% and head circumference is at the 20%. The infant appears thin, but the remainder of the physical examination is unremarkable. Screening labs are shown below. Chemistry panel Serum sodium 140 mEq/L Serum potassium 3.0 mEq/L Chloride 113 mEq/L Bicarbonate 15 mEq/L Blood urea nitrogen (BUN) 10 mg/dl Serum creatinine 0.5 mg/dl Calcium 9.0 mg/dl Blood glucose 98 mg/dl The urine pH is 7.9 and urinary sodium and potassium are within normal limits. What is the most likely cause for this patient's failure to thrive?
B. Lactic acidosis
A. Insufficient calories
C. Cystic fibrosis
D. Renal tubular acidosis
E. Gastroesophageal reflux
185. A 6-year-old boy has had a fever for 8 days. He just finished a 5-day course of amoxicillin for otitis media. On examination, his temperature is 38.6 C (101.4 F). He has meningismus and palsy of the left sixth cranial nerve. Cerebrospinal fluid (CSF) analysis reveals 200 white cells per mL with 80% lymphocytes and 20% polymorphonuclear leukocytes, glucose of 18 mg/dL, protein of 260 mg/dL, and a negative Gram stain. There is basilar enhancement without focal lesions on CT. Which of the following CSF tests will most likely identify the cause of meningitis?
(B) Bacterial culture
(A) Antigen test for Cryptococcus
(C) Culture for mycobacteria
(D) Latex agglutination test for pneumococcus
(E) Test for Treponema pallidum
186. A previously healthy 5-month-old boy has been irritable and has had a decreased oral intake for 2 days. His rectal temperature is 37.4 C (99.3 F), pulse is 220/min, and respirations are 50/min. The radial and posterior tibial pulses are diminished with good brachial and femoral pulses. ECG shows tachycardia; QRS complexes are narrow without preceding P waves. Which of the following is the most appropriate initial step in management?
(B) Administer verapamil intravenously
(A) Administer adenosine intravenously
(C) Apply an ice-filled plastic bag to the entire face for 5-10 seconds
(D) Cardiac pacing
(E) Perform synchronized direct current cardioversion
187. A 5-year-old boy suffers from a condition characterized by recurrent fungal and viral infections, thymic hypoplasia, tetany, and abnormal facies. Serum levels of immunoglobulins are mildly depressed, and lymph node biopsy shows lymphocyte depletion of T-dependent areas. Which of the following is the underlying pathogenetic mechanism?
B. In utero infection by human immunodeficiency virus (HIV)
A. Developmental defect of the third/fourth pharyngeal pouches
C. Mutations of an autosomal gene encoding adenosine deaminase
D. Mutations of an X-linked gene coding for a cytokine receptor subunit
E. Mutations of an X-linked gene coding for a tyrosine kinase
188. A 5-year-old boy is brought to the physician because of a malodorous discharge coming from his right nostril. His parents report that the child developed frequent sneezing and mucus discharge for one week. They thought it was a common cold. The child is afebrile and in apparent good health. There is no history of allergic diseases or recurrent infections. Examination reveals obstruction of the right nasal fossa with associated purulent discharge from the right nostril. Which of the following is the most likely diagnosis?
B. Juvenile angiofibroma
A. Allergic rhinitis
C. Nasal foreign body
D. Nasal polyp
E. Rhinitis medicamentosa
189. A 4-year-old girl is brought to your office by her mother for recent onset of fever and rash. For the past 4 days, she has had headaches, fever, and sore throat. She was apparently normal4 days ago, and upon presentation of the symptoms, her mother thought that she was having a simple viral fever which would go away with time; however, she then developed a pale pink maculo-papular rash, first on the face and neck, and then it rapidly spread onto the trunk and limbs. On examination, the child is afebrile and doesn't appear ill, but there are few palpable suboccipital and posterior auricular lymph nodes. What is the most likely cause of this patient's condition?
B. Measles virus
A. Group A beta- hemolytic streptococci
C. Rubella virus
D. Varicella virus
E. Human parvovirus
190. While working in the newborn nursery, you have the chance to counsel a first time mother. She had a healthy pregnancy and good prenatal care. The infant was delivered via normal spontaneous vaginal delivery and is doing well. You are counseling the mother on the benefits of breastfeeding, and she asks you what the differences are between human milk and formula. Which of the following is a true statement?
B. Human milk provides adequate amounts of vitamin D
A. Human milk has more calcium and phosphorus than formula
C. Human milk contains only trace amounts of immunoglobulin A
D. Human milk protein absorbs better and improves gastric emptying
E. The main advantage of formula is it decreases colic
191. An 18-month-old male infant is brought to the office by his parents for a follow-up visit. He has a congenital condition that started at the age of 6 months with repeated vomiting and hypotonia, and progressively evolved into choreoathetosis, spasticity and dystonia. Over the past month, he has started biting his hands and arms, pinching himself and banging his limbs against the wall. His family history is unremarkable. On examination, he has several scars, cuts and bruises over his arms and hands. His uric acid levels are elevated. What is the most likely deficient enzyme in this patient?
B. Xanthine oxidase
A. Glutamine-phosphorylase pyrophosphate aminotransferase
C. Hypoxanthine-guanine phosphoribosyl transferase
D. Adenyl succinate synthase
E. Purine nucleoside phosphorylase
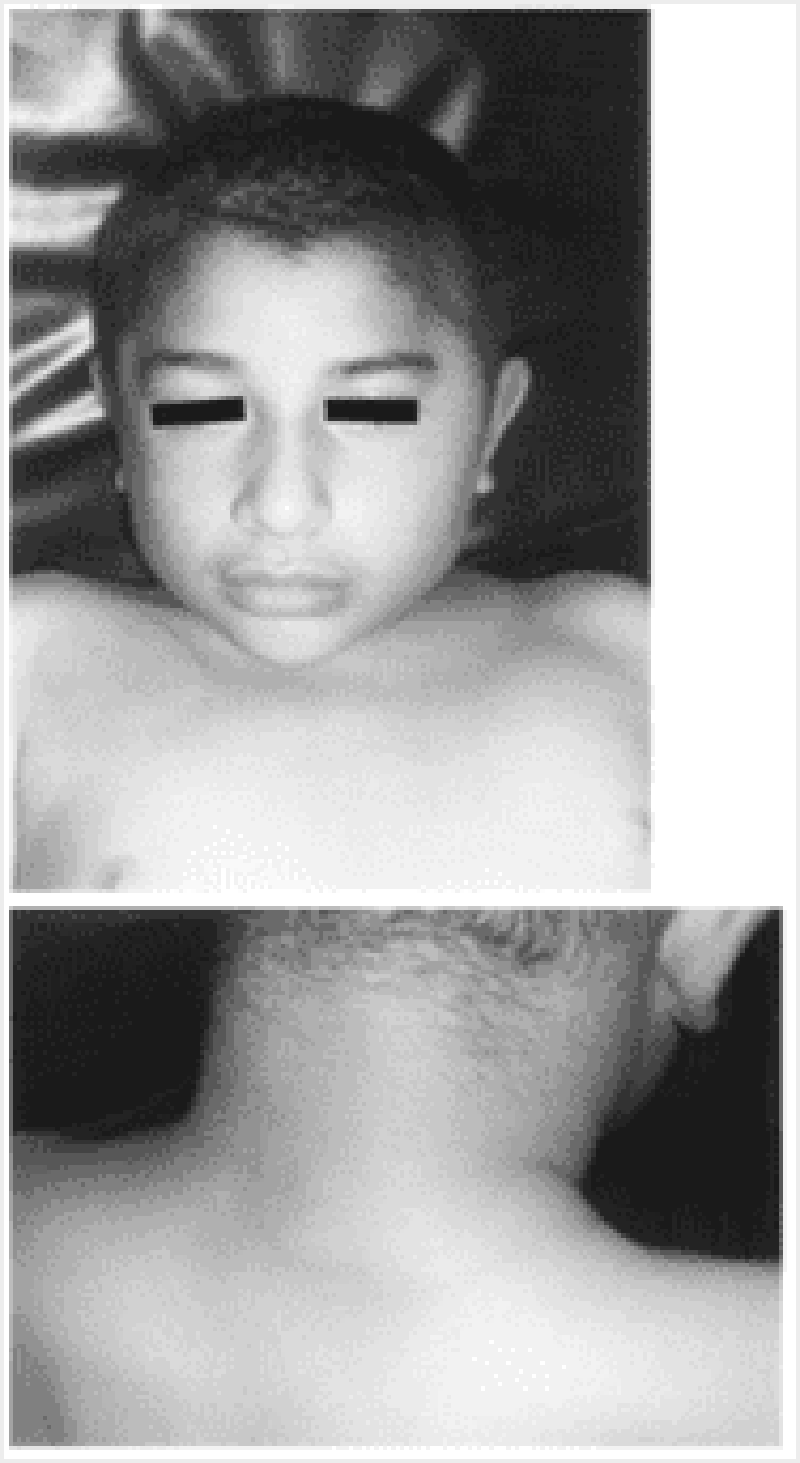
192. For the past year, a 12-year-old boy has had recurrent episodes of swelling of his hands and feet, which has been getting worse recently. These episodes occur following exercise and emotional stress, last for 2 to 3 days, and resolve spontaneously. The last episode was accompanied by abdominal pain, vomiting, and diarrhea. The results of routine laboratory workup are normal. An older sister and a maternal uncle have had similar episodes, but they were not given a diagnosis. He presents today with another episode as shown in the photographs on the next page. Which of the following is the most likely diagnosis?
B. Focal glomerulosclerosis
A. Systemic lupus erythematosus
C. Congenital nephrotic syndrome
D. Hereditary angioedema
E. Henoch-Schönlein purpura
193. A newborn is diagnosed with congenital heart disease. You counsel the family that the incidence of heart disease in future children is which of the following?
B. 2% to 6%
A. 1%
C. 8% to 10%
D. 15% to 20%
E. 25% to 30%
194. A 5-year-old girl is brought to medical attention by her parents 12 hours after the onset of generalized tonicoclonic seizures. She never had similar episodes in the past. The girl is otherwise healthy. Her temperature is 37 C (98.6 F). Physical examination is unremarkable. There is no evidence that the girl had a fever at the onset of the convulsive episode. The parents fear that seizures may damage the child's brain and may eventually recur. Which of the following is the most appropriate next step in management?
(B) Admit patient to the hospital for further evaluation
(A) Provide reassurance to child and family
(C) Perform electroencephalographic studies
(D) Perform CT/MW studies of the brain
(E) Start antiepileptic medication
195. An otherwise healthy 13-year-old boy has seasonal allergic rhinitis. He complains of excessive rhinorrhea, frequent sneezing, and nasal congestion. He has a nasal voice and breathes with his mouth. He derives some relief from keeping windows closed at home and spending as litde time as possible outdoors in periods of high pollen concentration. However, he is excessively bothered by nasal congestion. Which of the following drugs would be most effective in relieving nasal congestion?
(B) Antihistamines such as chlorpheniramine
(A) Alpha-adrenergic agents such as phenylephrine
(C) Antihistamines such as loratadine
(D) Cromoglycate or similar mast cell stabilizers
(E) Ipratropium bromide
196. During a regular checkup of an 8-year-old child, you note a loud first heart sound with a fixed and widely split second heart sound at the upper left sternal border that does not change with respirations. The patient is otherwise active and healthy. Which of the following heart lesions most likely explains these findings?
B. Ventricular septal defect (VSD)
A. Atrial septal defect (ASD)
C. Isolated tricuspid regurgitation
D. Tetralogy of Fallot
E. Mitral valve prolapse
197. A 2-year-old child with minimal cyanosis has an S3 and S4 (a quadruple rhythm), a systolic murmur in the pulmonic area, and a middiastolic murmur along the lower left sternal border. An ECG shows right atrial hypertrophy and a ventricular block pattern in the right chest leads. Which of the following is the most likely diagnosis?
B. Pulmonic stenosis and a VSD (tetralogy of Fallot)
A. Tricuspid regurgitation and pulmonic stenosis
C. Atrioventricular canal
D. Ebstein anomaly
E. Wolff-Parkinson-White syndrome
198. A woman brings her 3-year-old son to the emergency room after witnessing him swallow a disk-shaped battery. She adds that he vomited once on the way to the hospital. The vomitus was non-bloody and did not contain the battery. Physical examination of the child's chest is unremarkable. Plain radiographs reveal that the battery is located in the esophagus. What is the most appropriate next step in the management of this patient?
B. Observation for next 24-48 hours for spontaneous expulsion
A. Induce emesis to expel the battery
C. Immediate endoscopic removal
D. Advance the battery into the stomach with a nasogastric tube
E. Increase gastrointestinal motility with metoclopramide
199. A 7 -year-old Caucasian boy is brought to the emergency room with a severe headache, vomiting, and altered mental status of acute onset. His temperature is 36.7 C (98 F), blood pressure is 130/70 mm Hg, pulse is 60/min, and respirations are 18/min. Neurologic examination reveals nuchal rigidity, but no focal neurologic signs. A CT scan shows blood in the subarachnoid space. Which of the following is the most probable additional finding in this patient?
B. Mental retardation
A. History of seizures
C. Congenital heart disease
D. Coagulation abnormalities
E. Trauma
200. A 28-month-old female has been living with her mother in a shelter for homeless women and children. She is brought to the Emergency Department in status epilepticus, which is stopped with intravenous lorazepam. She is placed on a cardiac monitor and a wide complex tachycardia is noted. The ventricular tachycardia reverts to sinus tachycardia after defibrillation is performed. Her temperature is 38.5 C (101.3 F), blood pressure is 120/80 mm Hg, pulse is 195, and respirations are 26. Physical examination reveals a lethargic, pale toddler with dilated and reactive pupils, dry mucous membranes, shallow respirations, diaphoresis and brisk deep tendon reflexes. A urine toxicology screen is most likely to detect which of the following substances?
B. Cocaine
A. Barbiturates
C. Heroin
D. Marijuana
E. PCP
{"name":"QCU\/DES\/USMLE\/PEDIATRIC 1-250 part1", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Test your knowledge of pediatric medicine with our extensive 250-question quiz. Covering a wide range of topics from common conditions to emergency scenarios, this quiz is ideal for anyone looking to enhance their understanding in the field of pediatrics.Whether you are a medical student, a healthcare professional, or just someone with an interest in pediatric health, this quiz will provide an engaging and educational experience. Key features include:250 carefully curated questionsMultiple choice formatImmediate feedback on your answers","img":"https:/images/course8.png"}
More Quizzes
Pediatric(201-227)
27140
TCP Quiz 2
4522164
Soso
1368
Guinea Pig Or Hamster
630
The Exorcist - How Well Do You Know the Movie?
201017918
Spring Season Trivia - Free with Answers
201020269
Which Singer Are You? - Free Music Match
201017181
Disney Stockholm Syndrome - Which Character Are You?
201017056
Which Avatar Character Are You? The Last Airbender
201018513
Harry Potter Girlfriend - Who Would You Date?
201016638
Orthopedic Sports Medicine - Free Practice Questions
15818359
Kiss the Ground Documentary - Test Your Knowledge
201021218