Surgery kb,part 1

Surgery Knowledge Quiz: Part 1
Challenge your knowledge of surgical procedures and their associated conditions with our comprehensive Surgery Knowledge Quiz. Designed for medical professionals and students alike, this quiz covers a wide range of topics, ensuring you test your understanding of key concepts and clinical situations.
Get ready to delve into:
- Gastrointestinal surgery
- Complications of surgical procedures
- Management of surgical cases
- Preoperative and postoperative care
1. 74-year-old woman is admitted with upper gastrointestinal (GI) bleeding. She is started on H 2 blockers, but experiences another bleeding episode. Endoscopy documents diffuse gastric ulcerations. Omeprazole is added to the H2 antagonists as a therapeutic approach to the management of acute gastric and duodenal ulcers. Which of the following is the mechanism of action of omeprazole?
Blockage of the breakdown of mucosa-damaging metabolites of nonsteroidal anti-inflammatory drugs (NSAIDs)
Provision of a direct cytoprotective effect
Buffering of gastric acids
Inhibition of parietal cell hydrogen potassium ATPase (adenosine triphosphatase)
Inhibition of gastrin release and parietal cell acid production
2. A 35-year-old woman presents with frequent and multiple areas of cutaneous ecchymosis. Workup demonstrates a platelet count of 15,000/μL, evaluation of the bone marrow reveals a normal number of megakaryocytes, and ultrasound examination demonstrates a normal-sized spleen. Based on the exclusion of other causes of thrombocytopenia, she is given a diagnosis of immune (idiopathic) thrombocytopenic purpura (ITP). Which of the following is the most appropriate treatment upon diagnosis?
Expectant management with close follow-up of platelet counts
Immediate platelet transfusion to increase platelet counts to greater than 50,000/μL
Glucocorticoid therapy
Intravenous immunoglobulin (IVIG) therapy
Referral to surgery for laparoscopic splenectomy
3. A 59-year-old woman presents with right lower quadrant pain, nausea, and vomiting. She undergoes an uncomplicated laparoscopic appendectomy. Postoperatively, the pathology reveals a 2.5 cm mucinous adenocarcinoma with lymphatic invasion. Staging workup, including colonoscopy, chest x-ray, and computed tomography (CT) scan of the abdomen and pelvis, is negative. Which of the following is the most appropriate next step in her management?
A. No further intervention at this time; follow-up every 6 months for 2 years
B. Chemotherapy alone
C. Neoadjuvant chemotherapy followed by right hemicolectomy
D. Ileocecectomy
D. Right hemicolectomy
4. A 41-year-old man complains of regurgitation of saliva and of undigested food. An esophagram reveals a dilated oesophagus and a bird’s-beak deformity. Manometry shows a hypertensive lower esophageal sphincter with failure to relax with deglutition. Which of the following is the safest and most effective treatment of this condition?
A. Medical treatment with sublingual nitroglycerin, nitrates, or calcium-channel blockers
B. Repeated bougie dilations
C. Injections of botulinum toxin directly into the lower esophageal sphincter
D. Dilation with a Gruntzig-type (volume-limited, pressure-control) balloon E. Surgical
E. Surgical esophagomyotomy
5. A 32-year-old man with a 3-year history of ulcerative colitis (UC) presents for discussion for surgical intervention. The patient is otherwise healthy and does not have evidence of rectal dysplasia. Which of the following is the most appropriate elective operation for this patient?
A. Total proctocolectomy with end ileostomy
B. Total proctocolectomy with ileal pouch-anal anastomosis and diverting ileostomy
C. Total proctocolectomy with ileal pouch-anal anastomosis, anal mucosectomy, and diverting ileostomy
D. Total abdominal colectomy with ileal-rectal anastomosis
E. Total abdominal colectomy with end ileostomy and very low Hartmann
6. A 39-year-old previously healthy male is hospitalized for 2 weeks with epigastric pain radiating to his back, nausea, and vomiting. Initial laboratory values revealed an elevated amylase level consistent with acute pancreatitis. Five weeks following discharge, he complains of early satiety, epigastric pain, and fevers. On presentation, his temperature is 38.9°C (102°F) and his heart rate is 120 beats per minute; his white blood cell (WBC) count is 24,000/mm3 and his amylase level is normal. He undergoes a CT scan demonstrating a 6 cm by 6 cm rim-enhancing fluid collection in the body of the pancreas. Which of the following would be the most definitive management of the fluid collection?
A. Antibiotic therapy alone
B. CT-guided aspiration with repeat imaging in 2 to 3 days
C. Antibiotics and CT-guided aspiration with repeat imaging in 2 to 3 days D. Antibiotics and percutaneous catheter drainage
D. Antibiotics and percutaneous catheter drainage
E. Surgical internal drainage of the fluid collection with a cyst-gastrostomy or Roux-en-Y cyst-jejunostomy

7. A previously healthy 79-year-old woman presents with early satiety and abdominal fullness. CT scan of the abdomen, pictured here, reveals a cystic lesion in the body and tail of the pancreas. CT-guided aspiration demonstrates an elevated carcinoembryonic antigen (CEA) level. Which of the following is the most appropriate treatment option for this patient?
A. Distal pancreatectomy
B. Serial CT scans with resection if the lesion increases significantly in size
C. Internal drainage with Roux-en-Y cyst-jejunostomy
D. Percutaneous drainage of the fluid-filled lesion
E. Endoscopic retrograde cholangiopancreatography (ERCP) with pancreatic stent placement
8. A 56-year-old woman is referred to you about 3 months after a colostomy subsequent to a sigmoid resection for cancer. She complains that her stoma is not functioning properly. Which of the following is the most common serious complication of an end colostomy?
A. Bleeding
B. Skin breakdown
C. Parastomalhernia
D. Colonic perforation during irrigation
E. Stomal prolapse
9. A 56-year-old previously healthy physician notices that his eyes are yellow and he has been losing weight. On physical examination the patient has jaundice and scleral icterus with a benign abdomen. Transcutaneous ultrasound of the abdomen demonstrates biliary ductal dilation without gallstones. Which of the following is the most appropriate next step in the workup of this patient?
A. Esophagogastroduodenoscopy (EGD)
B. Endoscopic retrograde cholangiopancreatography (ERCP)
C. Acute abdominal series
D. Computed tomography (CT) scan
E. Positron emission tomography (PET) scan
10. A 45-year-old woman with history of heavy nonsteroidal anti-inflammatory drug ingestion presents with acute abdominal pain. She undergoes exploratory laparotomy 30 hours after onset of symptoms and is found to have a perforated duodenal ulcer. Which of the following is the procedure of choice to treat her perforation?
A. Simple closure with omental patch
B. Truncal vagotomy and pyloroplasty
C. Truncal vagotomy and antrectomy
D. Highly selective vagotomy with omental patch
E. Hemigastrectomy
11. A 45-year-old man with a history of chronic peptic ulcer disease undergoes a truncal vagotomy and antrectomy with a Billroth II reconstruction for gastric outlet obstruction. Six weeks after surgery, he returns, complaining of postprandial weakness, sweating, light-headedness, crampy abdominal pain, and diarrhea. Which of the following would be the best initial management strategy?
A. Treatment with a long-acting somatostatin analog
B. Dietary advice and counseling that symptoms will probably abate within 3 months of surgery
C. Dietary advice and counseling that symptoms will probably not abate but are not dangerous
D. Workup for neuroendocrine tumor (eg, carcinoid)
E. Preparation for revision to Roux-en-Y gastrojejunostomy
12. A 60-year-old male patient with hepatitis C with a previous history of variceal bleeding is admitted to the hospital with hematemesis. His blood pressure is 80/60 mmHg, physical examination reveals splenomegaly and ascites, and initial hematocrit is 25%. Prior to endoscopy, which of the following is the best initial management of the patient?
A. Administration of intravenous octreotide
B. Administration of a β-blocker (eg, propranolol)
C. Measurement of prothrombin time and transfusion with cryoglobulin if elevated
D. Empiric transfusion of platelets given splenomegaly
E. Gastric and esophageal balloon tamponade (Sengstaken-Blakemore tube)
13. A 32-year-old alcoholic with end-stage liver disease has been admitted to the hospital 3 times for bleeding esophageal varices. He has undergone banding and sclerotherapy previously. He admits to currently drinking a 6 packs of beer per day. On his abdominal examination, he has a fluid wave. Which of the following is the best option for long-term management of this patient’s esophageal varices?
A. Orthotopic liver transplantation
B. Transection and reanastomosis of the distal esophagus
C. Distal splenorenal shunt
D. End-to-side portocaval shunt
E. Transjugular intrahepatic portosystemic shunt (TIPS)
14. A 55-year-old man complains of chronic intermittent epigastric pain. A gastroscopy demonstrates a 2-cm prepyloric ulcer. Biopsy of the ulcer yields no malignant tissue. After a 6 week trial of medical therapy, the ulcer is unchanged. Which of the following is the best next step in his management?
A. Repeat trial of medical therapy
B. Local excision of the ulcer
C. Highly selective vagotomy
D. Partial gastrectomy with vagotomy and Billroth I reconstruction
E. Vagotomy and pyloroplasty
15. A 45-year-old man was discovered to have a hepatic flexure colon cancer during a colonoscopy for anemia requiring transfusions. Upon exploration of his abdomen in the operating room, an unexpected discontinuous 3-cm metastasis is discovered in the edge of the right lobe of the liver. Preoperatively, the patient was counseled of this possibility and the surgical options. Which of the following is the most appropriate management of this patient?
A. A diverting ileostomy should be performed and further imaging obtained
B. Right hemicolectomy
C. Right hemicolectomy with local resection of the liver metastasis
D. Closure of the abdomen followed by chemotherapy
E. Right hemicolectomy with postoperative radiation therapy to the liver
16. A 42-year-old man with no history of use of NSAIDs presents with recurrent gastritis. The patient was diagnosed and treated for Helicobacter pylori 6 months ago. Which of the following tests provides the least invasive method to document eradication of the infection?
A. Serology testing for H pylori
B. Carbon-labeled urea breath test
C. Rapid urease assay
D. Histologic evaluation of gastric mucosa
E. Culturing of gastric mucosa
17. A 22-year-old college student notices a bulge in his right groin. It is accentuated with coughing, but is easily reducible. Which of the following hernias follows the path of the spermatic cord within the cremaster muscle?
A. Femoral
B. Direct inguinal
C. Indirect inguinal
D. Spigelian
E. Interparietal
18. An 80-year-old man with history of symptomatic cholelithiasis presents with signs and symptoms of a small- bowel obstruction. Which of the following findings would provide the most help in ascertaining the diagnosis?
A. Coffee-grounds aspirate from the stomach
B. Pneumobilia
C. A leukocyte count of 40,000/mL
D. A pH of 7.5, PCO2 of 50 kPa, and paradoxically acid urine
E. A palpable mass in the pelvis
19. A 42-year-old man has bouts of intermittent crampy abdominal pain and rectalbleeding. Colonoscopy is performed and demonstrates multiple hamartomatous polyps. The patient is successfully treated by removing as many polyps as possible with the aid of intraoperative endoscopy and polypectomy. Which of the following is the most likely diagnosis?
A. Ulcerative colitis
B. Villous adenomas
C. Familial polyposis
D. Peutz-Jeghers syndrome
E. Crohn colitis
20. A 70-year-old woman has nausea, vomiting, abdominal distention, and episodic crampy midabdominal pain. She has no history of previous surgery but has a long history of cholelithiasis for which she has refused surgery. Her abdominal radiograph reveals a spherical density in the right lower quadrant. Which of the following is the definitive treatment for this patient’s bowel obstruction?
A. Ileocolectomy
B. Cholecystectomy
C. Ileotomy and extraction
D. Nasogastric (NG) tube decompression
E. Intravenous antibiotics
21. A 53-year-old man presents to the emergency room with left lower quadrant pain, fever, and vomiting. CT scan of the abdomen and pelvis reveals a thickened sigmoid colon with inflamed diverticula and a 7-cm by 8- cm rim-enhancing fluid collection in the pelvis. After percutaneous drainage and treatment with antibiotics, the pain and fluid collection resolve. He returns as an outpatient to clinic 1 month later. He undergoes a colonoscopy, which demonstrates only diverticula in the sigmoid colon. Which of the following is the most appropriate next step in this patient’s management?
A. Expectant management with sigmoid resection if symptoms recur
B. Cystoscopy to evaluate for a fistula
C. Sigmoid resection with end colostomy and rectal pouch (Hartmann procedure)
D. Sigmoid resection with primary anastomosis
E. Long-term suppressive antibiotic therapy
22. A 29-year-old woman complains of postprandial right upper quadrant pain and fatty food intolerance. Ultrasound examination reveals no evidence of gallstones or sludge. Upper endoscopy is normal, and all of her liver function tests are within normal limits. Which of the following represents the best management option?
A. Avoidance of fatty foods and reexamination in 6 months.
B. Ultrasound examination should be repeated immediately, since the falsenegative rate for ultrasound in detecting gallstones is 10% to 15%.
C. Treatment with ursodeoxycholic acid.
D. CCK-HIDA scan should be performed to evaluate for biliary dyskinesia.
E. Laparoscopic cholecystectomy for acalculous cholecystitis.
23. A 47-year-old asymptomatic woman is incidentally found to have a 5-mm polyp and no stones in her gallbladder on ultrasound examination. Which of the following is the best management option?
A. Aspiration of the gallbladder with cytologic examination of the bile
B. Observation with repeat ultrasound examinations to evaluate for increase in polyp size
C. Laparoscopic cholecystectomy
D. Open cholecystectomy with frozen section
E. En bloc resection of the gallbladder, wedge resection of the liver, and portal lymphadenectomy
24. A 48-year-old woman develops pain in the right lower quadrant while playing tennis. The pain progresses and the patient presents to the emergency room later that day with a low-grade fever, a WBC count of 13,000/mm3 and complaints of anorexia and nausea as well as persistent, sharp pain of the right lower quadrant. On examination, she is tender in the right lower quadrant with muscular spasm, and there is a suggestion of a mass effect. An ultrasound is ordered and shows an apparent mass in the abdominal wall. Which of the following is the most likely diagnosis?
A. Acute appendicitis
B. Cecalcarcinoma
C. Hematoma of the rectus sheath
D. Torsion of an ovarian cyst
E. Cholecystitis
25. A 32-year-old alcoholic man, recently emigrated from Mexico, presents with right upper quadrant pain and fevers for 2 weeks. CT scan of the abdomen demonstrates a non–rim-enhancing fluid collection in the periphery of the right lobe of the liver. The patient’s serology is positive for antibodies to Entamoeba histolytica. Which of the following is the best initial management option for this patient?
A. Treatment with antiamebic drugs
B. Percutaneous drainage of the fluid collection
C. Marsupialization of the fluid collection
D. Surgical drainage of the fluid collection
E. Liver resection
26. A 45-year-old executive experiences increasingly painful retrosternalheartburn, especially at night. He has been chewing antacid tablets. An esophagogram shows a hiatal hernia. In determining the proper treatment for a sliding hiatal hernia, which of the following is the most useful modality?
A. Barium swallow with cinefluoroscopy during Valsalva maneuver
B. Flexible endoscopy
C. Twenty-four-hour monitoring of esophageal pH
D. Measurement of the size of the hernia on upper GI
E. Assessment of the patient’s smoking and drinking history
27. A 22-year-old woman is seen in a surgery clinic for a bulge in the right groin. She denies pain and is able to make the bulge disappear by lying down and putting steady pressure on the bulge. She has never experienced nausea or vomiting. On examination she has a reducible hernia below the inguinal ligament. Which of the following is the most appropriate management of this patient?
A. Observation for now and follow-up in surgery clinic in 6 months
B. Observation for now and follow-up in surgery clinic if she develops further symptoms
C. Elective surgical repair of hernia
D. Emergent surgical repair of hernia
E. Emergent surgical repair of hernia with exploratory laparotomy to evaluate the small bowel
28. A 22-year-old woman presents with a painful fluctuant mass in the midline between the gluteal folds. She denies pain on rectal examination. Which of the following is the most likely diagnosis?
A. Pilonidal abscess
B. Perianalabscess
C. Perirectalabscess
D. Fistula-in-ano
E. Anal fissure
29. A 72-year-old man status post–coronary artery bypass graft (CABG) 5 years ago presents with hematochezia, abdominal pain, and fevers. Colonoscopy reveals patches of dusky-appearing mucosa at the splenic flexure without active bleeding. Which of the following is the most appropriate management of this patient?
A. Angiography with administration of intra-arterial papaverine
B. Emergent laparotomy with left hemicolectomy and transverse colostomy
C. Aortomesenteric by pass
D. Exploratory laparotomy with thrombectomy of the inferior mesenteric artery
E. Expectant management
30. A 62-year-old man has been diagnosed by endoscopic biopsy as having a sigmoid colon cancer. He is otherwise healthy and presents to your office for preoperative consultation. He asks a number of questions regarding removal of a portion of his colon. Which of the following is most likely to occur after a colon resection?
A. The majority (> 50%) of normally formed feces will comprise solid material.
B. Patients who undergo major colon resections suffer little long-term change in their bowel habits following operation.
C. Sodium, potassium, chloride, and bicarbonate will be absorbed by the colonic epithelium by an active transport process.
D. The remaining colon will absorb less water.
E. The remaining colon will absorb long-chain fatty acids that result from bacterial breakdown of lipids.
31. A 39-year-old woman with no significant past medical history and whose only medication is oral contraceptive pills (OCP) presents to the emergency room with right upper quadrant pain. CT scan demonstrates a 6-cm hepatic adenoma in the right lobe of the liver. Which of the following describes the definitive treatment of this lesion?
A. Cessation of oral contraceptives and serial CT scans
B. Intra-arterial embolization of the hepatic adenoma
C. Embolization of the right portal vein
D. Resection of the hepatic adenoma
E. Systemic chemotherapy
32. A 43-year-old man without symptoms is incidentally noted on CT scan to have a 4 cm lesion in the periphery of the left lobe of the liver. The lesion enhances on the arterial phase of the CT scan and has a central scar suggestive of focal nodular hyperplasia (FNH). Which of the following is the recommended treatment of this lesion?
A. No further treatment is necessary
B. Wedge resection of the lesion
C. Formal left hepatectomy
D. Intra-arterial embolization of the lesion
E. Radiofrequency ablation of the liver lesion
33. A 57-year-old previously alcoholic man with a history of chronic pancreatitis presents with hematemesis. Endoscopy reveals isolated gastric varices in the absence of esophageal varices. His liver function tests are normal and he has no stigmata of end-stage liver disease. Ultrasound examination demonstrates normal portal flow but a thrombosed splenic vein. He undergoes banding, which is initially successful, but he subsequently rebleeds during the same hospitalization. Attempts tocontrol the bleeding endoscopically are unsuccessful. Which of the following is the most appropriate next step in management?
A. Transjugular intrahepatic portosystemic shunt
B. Surgical portocaval shunt
C. Surgical mesocavalshunt
D. Splenectomy
E. Placement of a Sengstaken-Blakemore tube
34. A previously healthy 15-year-old boy is brought to the emergency room with complaints of about 12 hours of progressive anorexia, nausea, and pain of the right lower quadrant. On physical examination, he is found to have a rectal temperature of 38.18°C (100.72°F) and direct and rebound abdominal tenderness localizing to McBurney point as well as involuntary guarding in the right lower quadrant. At operation through a McBurney-type incision, the appendix and cecum are found to be normal, but the surgeon is impressed by the marked edema of the terminal ileum, which also has an overlying fibrinopurulent exudate. Which of the following is the most appropriate next step?
A. Close the abdomen after culturing the exudate.
B. Perform a standard appendectomy.
C. Resect the involved terminal ileum.
D. Perform an ileocolic resection.
E. Perform an ileocolostomy to bypass the involved terminal ileum

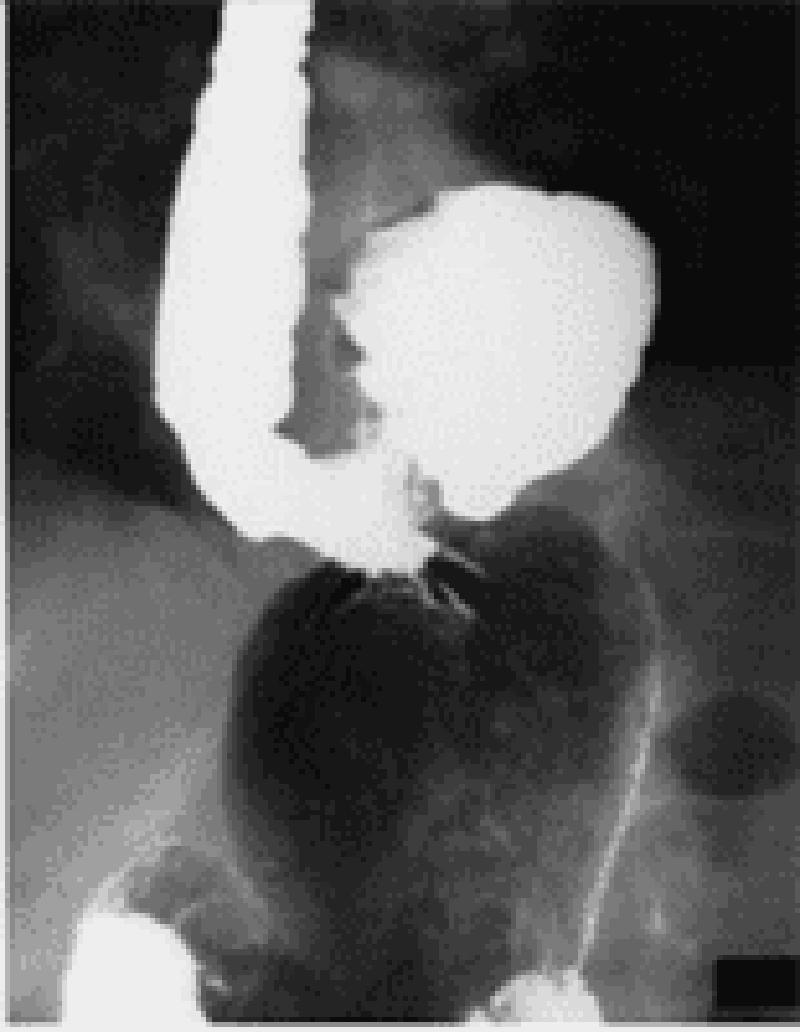
35. A 32-year-old woman undergoes a cholecystectomy for acute cholecystitis and is discharged home on the sixth postoperative day. She returns to the clinic 8 months after the operation for a routine visit and is noted by the surgeon to be jaundiced. Laboratory values on readmission show total bilirubin 5.6 mg/dL, direct bilirubin 4.8 mg/dL, alkaline phosphatase 250 IU (normal 21-91 IU), serum glutamic oxaloacetic transaminase (SGOT) 52 kU (normal 10-40 kU), and serum glutamic pyruvic transaminase (SGPT) 51 kU (normal 10-40 kU). An ultrasonogram shows dilated intrahepatic ducts. The patient undergoes the transhepatic cholangiogram seen here. Which of the following is the most appropriate next management step?
A. Choledochoplasty with insertion of a T tube
B. End-to-end choledochocholedochal anastomosis
C. Roux-en-Y hepaticojejunostomy
D. Percutaneous transhepatic dilatation
E. Choledochoduodenostomy
36. After complete removal of a sessile polyp of 2.0 cm by 1.5 cm found 1 finger length above the anal mucocutaneous margin, the pathologist reports it to have been a villous adenoma that contained carcinoma in situ. Which of the following is the most appropriate next step in management?
A. Reexcision of the biopsy site with wider margins
B. Abdominoperineal rectosigmoid resection
C. Anterior resection of the rectum
D. External radiation therapy to the rectum
E. No further therapy
37. A 62-year-old man has been noticing progressive difficulty swallowing, first solid food and now liquids as well. A barium study shows a ragged narrowing just below the carinal level. Endoscopic biopsy confirms squamous cell carcinoma. Which of the following provides the most accurate information regarding the T stage of an esophageal carcinoma?
A. Computed tomography
B. Positron emission tomography
C. Magnetic resonance imaging
D. Endoscopic ultrasound
E. Bronchoscopy
38. A 53-year-old woman with a history of a vagotomy and antrectomy with Billroth II reconstruction for peptic ulcer disease presents with recurrent abdominal pain. An esophagogastroduodenoscopy (EGD) demonstrates that ulcer and serum gastrin levels are greater than 1000 pg/mL on three separate determinations (normal is 40-150). Which of the following is the best test for confirming a diagnosis of gastrinoma?
A. A 24-hour urine gastrin level
B. A secretin stimulation test
C. A serum glucagon level
D. A 24-hour urine secretin level
E. A serum glucose to insulin ratio
39. A 52-year-old man with a family history of multiple endocrine neoplasia type 1 (MEN1) has an elevated gastrin level and is suspected to have a gastrinoma. Which of the following is the most likely location for his tumor?
A. Fundus of the stomach
B. Antrum of the stomach
C. Within the triangle formed by the junction of the second and third portions of the duodenum, the junction of the neck and body of the pancreas, and the junction of the cystic and common bile duct Q
D. Tail of the pancreas
E. Within the triangle formed by the inferior edge of the liver, the cystic duct, and the common hepatic duct
40. A 73-year-old woman presents to the emergency room complaining of severe epigastric pain radiating to her back, nausea, and vomiting. CT scan of the abdomen demonstrates inflammation and edema of the pancreas. A right upper quadrant ultrasound demonstrates the presence of gallstones in the gallbladder. Which of the following is an important prognostic sign in acute pancreatitis according to Ranson’s criteria?
A. Amylase level
B. Age
C. Total bilirubin level
D. Albumin level
E. Lipase level
41. A 55-year-old man who is extremely obese reports weakness, sweating, tachycardia, confusion, and headache whenever he fasts for more than a few hours. He has prompt relief of symptoms when he eats. Labarotory examination reveals an inappropriately high level of serum insulin during the episodes of fasting. Which of the following is the most appropriate treatment for this condition?
A. Diet modification to include frequent meals
B. Long-acting somatostatin analogue octreotide
C. Simple excision of the tumor
D. Total pancreatectomy
E. Chemotherapy and radiation
42. A 57-year-old woman sees blood on the toilet paper. Her doctor notes the presence of an excoriated bleeding 2.8-cm mass at the anus. Biopsy confirms the clinical suspicion of anal cancer. In planning the management of a 2.8-cm epidermoid carcinoma of the anus, which of the following is the best initial management strategy?
A. Abdominoperineal resection
B. Wide local resection with bilateral inguinal node dissection
C. Local radiation therapy
D. Systemic chemotherapy
E. Combined radiation therapy and chemotherapy
43. An 80-year-old man is admitted to the hospital complaining of nausea, abdominal pain, distention, and diarrhea. A cautiously performed transanal contrast study reveals an apple-core configuration in the rectosigmoid area. Which of the following is the most appropriate next step in his management
A. Colonoscopic decompression and rectal tube placement
B. Saline enemas and digital disimpaction of fecal matter from the rectum
C. Colon resection and proximal colostomy
D. Oral administration of metronidazole and checking a Clostridium difficile titer
E. Evaluation of an electrocardiogram and obtaining an angiogram to evaluate for colonic mesenteric ischemia
44. A 46-year-old woman who was recently diagnosed with Crohn disease asks about the need for surgery. Which of the following findings would be an indication for an immediate exploratory laparotomy?
A. Intestinal obstruction
B. Enterovesical fistula
C. Ileum-ascending colon fistula
D. Enterovaginal fistula
E. Free perforation

45. A 50-year-old man presents to the emergency room with a 6-hour history of excruciating abdominal pain and distention. The abdominal film shown here is obtained. Which of the following is the most appropriate next diagnostic maneuver?
A. Emergency celiotomy
B. Upper GI series with small-bowel follow-through
C. CT scan of the abdomen
D. Barium enema
E. Sigmoidoscopy
46. A septuagenarian woman undergoes an uncomplicated resection of an abdominal aneurysm. Four days after surgery the patient presents with sudden onset of abdominal pain and distention. An abdominal radiograph demonstrates an air-filled, kidney-bean–shaped structure in the left upper quadrant. Which of the following is the most appropriate management at this time?
A. Decompression of the large bowel via colonoscopy
B. Placement of the NG tube and administration of low-dose cholinergic drugs
C. Administration of a gentle saline enema and encouragement of ambulation
D. Operative decompression with transverse colostomy
E. Right hemicolectomy
47. A 45-year-old man presents with right upper quadrant abdominal pain and fever. CT scan shows a large, calcified cystic mass in the right lobe of the liver. Echinococcus is suggested by the CT findings. Which of the following is the most appropriate management of echinococcal liver cysts?
A. Percutaneous catheter drainage.
B. Medical treatment with albendazole.
C. Medical treatment with steroids.
D. Medical treatment with metronidazole.
E. Total pericystectomy.
48. A 28-year-old woman who is 15 weeks pregnant has new onset of nausea, vomiting, and right sided abdominal pain. She has been free of nausea since early in her first trimester. The pain has become worse over the past 6 hours. Which of the following is the most common non-obstetric surgical disease of the abdomen during pregnancy?
A. Appendicitis
B. Cholecystitis
C. Pancreatitis
D. Intestinal obstruction
E. Acute fatty liver of pregnancy
49. A 56-year-old woman has nonspecific complaints that include an abnormal sensation when swallowing. An esophagram is obtained. Which of the following is most likely to require surgical correction?
A. Large sliding esophagealhiatal hernia
B. Paraesophagealhiatal hernia
C. Traction diverticulum of esophagus
D. Schatzki ring of distal esophagus
E. Esophageal web

50. A 65-year-old man who is hospitalized with pancreatic carcinoma develops abdominal distention and obstipation. The following abdominal radiograph is obtained. Which of the following is the most appropriate initial management of this patient?
A. Urgent colostomy or cecostomy
B. Discontinuation of anticholinergic medications and narcotics and correction of metabolic disorders
C. Digital disimpaction of fecalmass in the rectum
D. Diagnostic and therapeutic colonoscopy
E. Detorsion of volvulus and colopexy or resection
51. A 48-year-old man presents with jaundice, melena, and right upper quadrant abdominal pain after undergoing a percutaneous liver biopsy. Endoscopy shows blood coming from the ampulla of Vater. Which of the following is the most appropriate first line of therapy for major hemobilia?
A. Correction of coagulopathy, adequate biliary drainage, and close monitoring
B. Transarterial embolization (TAE)
C. Percutaneous transhepatic biliary drainage (PTBD)
D. Ligation of bleeding vessels
E. Hepatic resection
52. A 30-year-old female patient who presents with diarrhea and abdominal discomfort is found at colonoscopy to have colitis confined to the transverse and descending colon. A biopsy is performed. Which of the following is a finding consistent with this patient’s diagnosis?
A. The inflammatory process is confined to the mucosa and submucosa.
B. The inflammatory reaction is likely to be continuous.
C. Superficial as opposed to linear ulcerations can be expected.
D. Noncaseating granulomas can be expected in up to 50% of patients.
E. Microabscesses within crypts are common.
53. A 24-year-old man presents to the emergency room with abdominal pain and fever. CT scan of the abdomen reveals inflammation of the colon. He is referred to a gastroenterologist to be evaluated for inflammatory bowel disease (Crohn disease versus ulcerative colitis). Which of the following indications for surgery is more prevalent in patients with Crohn disease?
A. Toxic megacolon
B. Massive bleeding
C. Fistulas between the colon and segments of intestine, bladder, vagina, urethra, and skin
D. Intractable disease
E. Dysplasia or carcinoma
54. An upper GI series is performed on a 71-year-old woman who presented with severalmonths of chest pain that occurs when she is eating. The film shown here is obtained. Investigation reveals a microcytic anemia and erosive gastritis on upper endoscopy. Which of the following is the most appropriate initial management of this patient?
A. Cessation of smoking, decreased caffeine intake, and avoidance of large meals before lying down
B. Antacids
C. Histamine-2 blocker
D. Proton-pump inhibitor
E. Surgical treatment
55. A 54-year-old man complains that his eyes are yellow. His bilirubin is elevated. His physical examination is unremarkable. A CT of the abdomen shows a small mass in the head of the pancreas encasing the superior mesenteric artery. Cytology from the ERCP is positive for cancer. Which of the following is the most appropriate treatment for this patient?
A. Pancreaticoduodenectomy
B. Pancreaticoduodenectomy with reconstruction of the superior mesenteric artery
C. Total pancreatectomy
D. Total pancreatectomy with reconstruction of the superior mesenteric artery
E. Chemoradiation therapy
56. A 28-year-old woman presents with hematochezia. She is admitted to the hospital and undergoes upper endoscopy that is negative for any lesions. Colonoscopy is performed and no bleeding sources are identified, although the gastroenterologist notes blood in the right colon and old blood coming from above the ileocecal valve. Which of the following is the test of choice in this patient?
A. Angiography
B. Small-bowel enteroclysis
C. CT scan of the abdomen
D. Technetium 99m (99mTc) pertechnetate scan
E. Small-bowel endoscopy
57. A 32-year-old woman undergoes an uncomplicated appendectomy for acute appendicitis. The pathology report notes the presence of a 1-cm carcinoid tumor in the tip of the appendix. Which of the following is the most appropriate management of this patient?
A. Right hemicolectomy
B. Right hemicolectomy and chemotherapy
C. Chemotherapy only
D. Radiation only
E. No further treatment
58. A 58-year-old man presents with a bulge in his right groin associated with mild discomfort. On examination the bulge is easily reducible and does not descend into the scrotum. Which of the following changes is most concerning for possible strangulation requiring emergent repair of the hernia?
A. Increase in size of the hernia
B. Descent of hernia into the scrotum
C. Development of a second hernia in the left groin
D. Inability to reduce hernia
E. Worsening pain over the hernia with walking

59. A 35-year-old woman presents with abdominal pain and jaundice. Subsequent ERCP reveals the congenital cystic anomaly of her biliary system illustrated in the film shown here. Which of the following is the most appropriate treatment?
A. Cholecystectomy with resection of the extrahepatic biliary tract and Roux-en-Y hepaticojejunostomy
B. Internal drainage via choledochoduodenostomy
C. Internal drainage via choledochocystojejunostomy
D. Percutaneous transhepatic biliary drainage
E. Liver transplantation
60. A 36-year-old man is in your intensive care unit on mechanical ventilation following thoracotomy for a 24- hour-old esophageal perforation. His WBC is markedly elevated, and he is febrile, hypotensive, and coagulopathic. His NG tube fills with blood and continues to bleed. Which of the following findings on upper endoscopy would be most suspicious for stress gastritis?
A. Multiple, shallow lesions with discrete areas of erythema along with focal hemorrhage in the antrum
B. Multiple, shallow lesions with discrete areas of erythema along with focal hemorrhage in the fundus
C. Multiple deep ulcerations extending into and through the muscularis mucosa in the antrum
D. Multiple deep ulcerations extending into and through the muscularis mucosa in the fundus
E. Single deep ulceration extending into and through the muscularis mucosa in the fundus
61. A 35-year-old man presents with right upper quadrant pain, fever, jaundice, and shaking chills. Ultrasound of the abdomen demonstrates gallstones, normal gallbladder wall thickness, and common bile duct of 1.0 cm. The patient is admitted to the hospital and given IV fluids and antibiotics. He continues to be febrile with increasing WBCs. Which of the following is the most appropriate next step in this patient’s management?
A. Endoscopic retrograde cholangiopancreatography (ERCP)
B. Placement of a cholecystostomy tube
C. Laparoscopic cholecystectomy
D. Open cholecystectomy
E. Emergent operation and decompression of the common bile duct with a T tube
62. An 88-year-old man with a history of end-stage renal failure, severe coronary artery disease, and brain metastases from lung cancer presents with acute cholecystitis. His family wants “everything done.” Which of the following is the best management option in this patient?
A. Tube cholecystostomy
B. Open cholecystectomy
C. Laparoscopic cholecystectomy
D. Intravenous antibiotics followed by elective cholecystectomy
E. Lithotripsy followed by long-term bile acid therapy

63. After a weekend drinking binge, a 45-year-old man presents to the hospital with abdominal pain, nausea, and vomiting. On physical examination, the patient is noted to have tenderness to palpation in the epigastrium. Laboratory tests revealan amylase of 25,000 U/dL (normal < 180U/dL). The patient is medically managed and sent home after 1 week. A CT scan done 4 weeks later is pictured here. Currently the patient is asymptomatic. Which of the following is the most appropriate initial management of this patient?
A. Distal pancreatectomy
B. Percutaneous catheter drainage
C. Endoscopic drainage
D. Surgical drainage
E. No intervention is warranted at this time
64. A 54-year-old man presents with sudden onset of massive, painless, recurrent hematemesis. Upper endoscopy is performed and reveals bleeding from a lesion in the proximal stomach that is characterized as an abnormally large artery surrounded by normal-appearing gastric mucosa. Endoscopic modalities fail to stop the bleeding. Which of the following is the most appropriate surgical management of this patient?
A. Wedge resection of the lesion
B. Wedge resection of the lesion with truncal vagotomy
C. Wedge resection of the lesion with highly selective vagotomy
D. Wedge resection of the lesion with truncal vagotomy and antrectomy
E. Subtotal gastrectomy
65. During an appendectomy for acute appendicitis, a 4-cm mass is found in the midportion of the appendix. Frozen section reveals this lesion to be a carcinoid tumor. Which of the following is the most appropriate management of this patient?
A. Appendectomy
B. Appendectomy followed by a colonoscopy
C. Appendectomy followed by a PET scan
D. Right hemicolectomy
E. Total proctocolectomy
66. A 45-year-old man is examined for a yearly executive physical. A mass is palpated in the rectum, and a biopsy suggests carcinoid. Which of the following findings is most likely to be associated with the carcinoid syndrome?
A. Tumor < 2 cm
B. Tumor < 2 cm with ulceration
C. Tumor > 2 cm
D. Involvement of regional lymph nodes
E. Hepatic metastases
67. An ultrasound is performed on a patient with right upper quadrant pain. It demonstrates a large gallstone in the cystic duct but also a polypoid mass in the fundus. Which of the following is an indication for cholecystectomy for a polypoid gallbladder lesion?
A. Size greater than 0.5 cm
B. Presence of clinical symptoms
C. Patient age of older than 25 years
D. Presence of multiple small lesions
E. Absence of shadowing on ultrasound
68. An alcoholic man has been suffering excruciating pain from chronic pancreatitis recalcitrant to analgesics and splanchnic block. A surgeon recommends total pancreatectomy. A patient who has a total pancreatectomy might be expected to develop which of the following complications?
A. Diabetes mellitus and steatorrhea
B. Diabetes mellitus and constipation
C. Hypoglycemia
D. Hypoglycemia and steatorrhea
E. Hypoglycemia and constipation
69. A 45-year-old woman has an incidental finding of a liver mass on a CT scan. Magnetic resonance imaging (MRI) is suggestive of a hemangioma. Which of the following is the most appropriate management strategy for this patient?
A. Observation
B. Discontinuation of oral contraceptive pills
C. Percutaneous biopsy of the lesion to confirm the diagnosis
D. Resection of the hemangioma
E. Liver transplantation
70. A 57-year-old woman presents with adenocarcinoma of the right colon. Laboratory evaluation demonstrates an elevation of carcinoembryonic antigen (CEA) to 123 ng/mL. Which of the following is the most appropriate use of CEA testing in patients with colorectal cancer?
A. As a screening test for colorectal cancer
B. To determine which patients should receive adjuvant therapy
C. To determine which patients should receive neoadjuvant therapy
D. To monitor for postoperative recurrence
E. To monitor for preoperative metastatic disease
71. A 61-year-old woman with a history of unstable angina complains of hematemesis after retching and vomiting following a night of binge drinking. Endoscopy reveals a longitudinal mucosal tear at the gastroesophageal junction, which is not actively bleeding. Which of the following is the next recommended step in the management of this patient?
A. Angiography with embolization
B. Balloon tamponade
C. Exploratory laparotomy, gastrotomy, and oversewing of the tear
D. Systemic vasopressin infusion
E. Expectant management
72. A teenage boy falls from his bicycle and is run over by a truck. On arrival in the emergency room (ER), he is awake and alert and appears frightened but in no distress. The chest radiograph suggests an air-fluid level in the left lower lung field and the nasogastric tube seems to coil upward into the left chest. Which of the following is the next best step in his management?
A. Placement of a left chest tube
B. Thoracotomy
C. Laparotomy
D. Esophagogastroscopy
E. Diagnostic peritoneal lavage
73. A 10-year-old boy was the backseat belted passenger in a high-speed motor vehicle collision. On presentation to the ER, he is awake, alert, and hemodynamically stable. He is complaining of abdominal pain and has an ecchymosis on his anterior abdominal wall where the seatbelt was located. Which of the following is the best next step in his management?
A. Discharge him home without any other workup.
B. Discharge him home if his amylase level is normal.
C. Discharge him home if his abdominal plain films are negative for the presence of free air.
D. Discharge him home if an abdominal computed tomography (CT) scan is negative.
E. Observe him regardless of negative test results.
74. A 65-year-old man who smokes cigarettes and has chronic obstructive pulmonary disease falls and fractures the third, fourth, and fifth ribs in the left anterolateral chest. Chest x-ray is otherwise normal. Which of the following would be the most appropriate next step in his management?
A. Strapping the chest with adhesive tape
B. Admission to the hospital and treatment with oral analgesia
C. Tube thoracostomy
D. Placement of an epidural for pain management
E. Surgical fixation of the fractured ribs
75. A 36-year-old man who was hit by a car presents to the ER with hypotension. On examination, he has tenderness and bruising over his left lateral chest below the nipple. An ultrasound examination is performed and reveals free fluid in the abdomen. What is the most likely organ to have been injured in this patient?
A. Liver
B. Kidney
C. Spleen
D. Intestine
E. Pancreas
76. A 52-year-old man is pinned against a loading dock. The patient has a fractured femur, a pelvic fracture, a tender abdomen, and no pulses in the right foot with minimal tissue damage to the right leg. Angiography discloses a popliteal artery injury with obstruction. At surgery, the popliteal vein is also transected. His blood pressure is 85/60 mm Hg. Which of the following is the best management strategy for his vascular injuries?
A. Repair of the popliteal vein with simple closure
B. Repair of the popliteal vein with saphenous vein patch
C. Repair of the popliteal vein with a synthetic interposition graft
D. Ligation of the popliteal vein
E. Amputation of the right lower extremity above the knee
77. A 27-year-old man sustains a single gunshot wound to the left thigh. In the ER, he is noted to have a large hematoma of his medial thigh. He complains of paresthesias in his left foot. On examination, there are weak pulses palpable distal to the injury and the patient is unable to move his foot. Which of the following is the most appropriate initial management of this patient?
A. Angiography
B. Immediate exploration and repair in the operating room
C. Fasciotomy of the anterior compartment of the calf
D. Observation for resolution of spasm
E. Local wound exploration at the bedside
78. A 25-year-old woman arrives in the ER following an automobile accident. She is acutely dyspneic with a respiratory rate of 60 breaths per minute. Breath sounds are markedly diminished on the right side. Which of the following is the best first step in the management of this patient?
A. Take a chest x-ray.
B. Draw arterial blood for blood-gas determination.
C. Decompress the right pleural space.
D. Perform pericardiocentesis.
E. Administer intravenous fluids.
79. A 17-year-old adolescent boy is stabbed in the left seventh intercostal space, midaxillary line. He presents to the ER with a heart rate of 86 beats per minute, blood pressure of 125/74 mm Hg, and oxygen saturation of 98%. Breath sounds are equal bilaterally. Which of the following is the most appropriate next step in his workup?
A. Local exploration of the wound
B. Left tube thoracostomy
C. Diagnostic laparoscopy
D. CT scan of the abdomen
E. Echocardiography
80. Your hospital is conducting an ongoing research study involving the hormonal response to trauma. Blood is drawn regularly (with Institutional Review Board [IRB] approval) for various studies. Which of the following values are likely to be seen after a healthy 36-year-old man is hit by a bus and sustains a ruptured spleen and a lacerated small bowel?
A. Increased secretion of insulin
B. Increased secretion of thyroxine
C. Decreased secretion of vasopressin (antidiuretic hormone [ADH])
D. Decreased secretion of glucagon
E. Decreased secretion of aldosterone
81. A 29-year-old man sustained a gunshot wound to the right upper quadrant. He is taken to the operating room and, after management of a liver injury, is found to have a complete transection of the common bile duct with significant tissue loss. Which of the following is the optimal surgical management of this patient’s injury?
A. Choledochoduodenostomy
B. Loop choledochojejunostomy
C. Primary end-to-end anastomosis of the transected bile duct
D. Roux-en-Y choledochojejunostomy
Bridging of the injury with a T tube
82. You evaluate an 18-year-old man who sustained a right-sided cervical laceration during a gang fight. Your intern suggests nonoperative management and observation. Which of the following is a relative, rather than an absolute, indication for neck exploration?
A. Expanding hematoma
B. Dysphagia
C. Dysphonia
D. Pneumothorax
E. Hemoptysis
83. Following blunt abdominal trauma, a 12-year-old girl develops upper abdominal pain, nausea, and vomiting. An upper gastrointestinal series reveals a total obstruction of the duodenum with a coiled spring appearance in the second and third portions. In the absence of other suspected injuries, which of the following is the most appropriate management of this patient?
A. Gastrojejunostomy
B. Nasogastric suction and observation
C. Duodenal resection
D. TPN (total parental nutrition) to increase the size of the retroperitoneal fat pad
E. Duodenojejunostomy
84. A 45-year-old man presents after a high-speed motor vehicle collision. He has a seatbelt sign across his neck and chest with an ecchymosis over his left neck. He is hemodynamically stable and neurologically intact. A CT angiogram shows a left carotid dissection. In the absence of other significant injuries, what is the next step in his management?
A. Antiplatelet therapy
B. Systemic anticoagulation with heparin
C. Neck exploration and left carotid artery repair
D. Neck exploration and left intra-extracranial bypass
E. Angiography and left carotid artery stenting
85. An 18-year-old man was assaulted and sustained significant head and facial trauma. Which of the following is the most common initial manifestation of increased intracranial pressure?
A. Change in level of consciousness
B. Ipsilateral (side of hemorrhage) pupillary dilation
C. Contralateral pupillary dilation
D. Hemiparesis
E. Hypertension
86. A 28-year-old man is brought to the ER for a severe head injury after a fall. He was intubated in the field for his decreased levelof consciousness. He is tachycardic and hypotensive. On examination, he is noted to have an obvious skull fracture and his right pupil is dilated. Which of the following is the most appropriate method for initially reducing his intracranial pressure?
A. Elevation of the head of the bed
B. Saline-furosemide (Lasix) infusion
C. Mannitol infusion
D. Intravenous dexamethasone (Decadron)
E. Hyperventilation
87. A 45-year-old man was an unhelmeted motorcyclist involved in a high-speed collision. He was ejected from the motorcycle and was noted to be apneic at the scene. After being intubated, he was brought to the ER, where he is noted to have a left dilated pupil that responds only sluggishly. What is the pathophysiology of his dilated pupil?
A. Infection within the cavernous sinus
B. Herniation of the uncal process of the temporal lobe
C. Laceration of the corpus callosum by the falx cerebri
D. Occult damage to the superior cervical ganglion
E. Cerebellar hypoxia
88. A 31-year-old man is brought to the ER following an automobile accident in which his chest struck the steering wheel. Examination reveals stable vital signs and no evidence of respiratory distress, but the patient exhibits multiple palpable rib fractures and paradoxical movement of the right side of the chest. Chest x-ray shows no evidence of pneumothorax or hemothorax. Which of the following is the most appropriate initial management of this patient?
A. Intubation, mechanical ventilation, and positive end-expiratory pressure
B. Stabilization of the chest wall with sandbags
C. Stabilization with towel clips
D. Immediate operative stabilization
E. Pain control, chest physiotherapy, and close observation
89. A 30-year-old man is stabbed in the arm. There is no evidence of vascular injury, but he cannot flex his three radial digits. Which of the following structures has he most likely injured?
A. Flexor pollicis longus and flexor digitus medius tendons
B. Radial nerve
C. Median nerve
D. Thenar and digital nerves at the wrist
E. Ulnar nerve
90. Following a 2-hour firefighting episode, a 36-year-old fireman begins complaining of a throbbing headache, nausea, dizziness, and visual disturbances. He is taken to the ER, where his carboxyhemoglobin (COHb) level is found to be 31%. Which of the following is the most appropriate next step in his treatment?
A. Begin an immediate exchange transfusion.
B. Transfer the patient to a hyperbaric oxygen chamber.
C. Begin bicarbonate infusion and give 250 mg acetazolamide (Diamox) intravenously
D. Administer 100% oxygen by mask.
E. Perform flexible bronchoscopy with further therapy determined by findings.
91. A 75-year-old man with a history of coronary artery disease, hypertension, and diabetes mellitus undergoes a right hemicolectomy for colon cancer. On the second postoperative day, he complains of shortness of breath and chest pain. He becomes hypotensive with depressed mental status and is immediately transferred to the intensive care unit. After intubation and placement on mechanical ventilation, an echocardiogram confirms cardiogenic shock. A central venous catheter is placed that demonstrates a central venous pressure of 18 mm Hg. Which of the following is the most appropriate initial management strategy?
A. Additional liter fluid bolus
B. Inotropic support
C. Mechanical circulatory support with intra-aortic balloon pump (IABP)
D. Cardiac catheterization
E. Heart transplant
92. An 18-year-old man climbs up a utility pole to retrieve his younger brother’s kite. An electrical spark jumps from the wire to his metal belt buckle and burns hisabdominal wall, knocking him to the ground. Which of the following should guide your treatment of this patient?
A. Injuries are generally more superficial than those from thermal burns.
B. Intravenous fluid replacement is based on the percentage of body surface area burned.
C. Electric burns often result in a transient traumatic optic neuropathy.
D. Evaluation for fracture of the other extremities and visceral injury is indicated.
E. Cardiac conduction abnormalities are unlikely.
93. A 22-year-old man is examined following a motor vehicle accident. He has a right knee dislocation which is reduced in the emergency room. He has palpable pedal pulses and is neurologically intact. Which of the following is an appropriate next step in his workup and management?
A. Measurement of ankle-brachial indices
B. Angiography of the right lower extremity
C. Prophylactic below-knee 4 compartments fasciotomies
D. Surgical exploration of the right popliteal artery
E. Observation with serial pulse checks
94. A 23-year-old, previously healthy man presents to the ER after sustaining a single gunshot wound to the left chest. The entrance wound is 3 cm inferior to the nipple and the exit wound is just below the scapula. A chest tube is placed that drains 400 mL of blood and continues to drain 50 to 75 mL/h during the initial resuscitation. Initial blood pressure of 70/0 mm Hg has responded to 2L crystalloid and is now 100/70 mm Hg. Abdominal examination is unremarkable. Chest x-ray reveals a re-expanded lung and no free air under the diaphragm. Which of the following is the best next step in his management?
A. Admission and observation
B. Peritoneal lavage
C. Exploratory thoracotomy
D. Exploratory celiotomy
E. Local wound exploration
95. A patient is brought to the ER after a motor vehicle accident. He is unconscious and has a deep scalp laceration and one dilated pupil. His heart rate is 120 beats per minute, blood pressure is 80/40 mm Hg, and respiratory rate is 35 breaths per minute. Despite rapid administration of 2 L normal saline, the patient’s vital signs do not change significantly. Which of the following is the most appropriate next step in the workup of his hypotension?
A. Neurosurgical consultation for emergent ventriculostomy to manage his intracranial pressure
B. Neurosurgical consultation for emergent craniotomy for suspected subdural hematoma
C. Emergent burr hole drainage at the bedside for suspected epidural hematoma
D. Administration of mannitol and hyperventilation to treat his elevated intracranial pressure
E. Abdominal ultrasound (focused assessment with sonography in trauma [FAST])
96. A 25-year-old man is involved in a gang shoot-out and sustains an abdominal gunshot wound from a .22 pistol. At laparotomy, it is discovered that the left transverse colon has incurred a through-and-through injury with minimal fecal soilage of the peritoneum. Which of the following is the most appropriate management of this patient?
A. A colostomy should be performed regardless of the patient’s hemodynamic status to decrease the risk of an intraabdominal infection.
B. Primary repair should be performed, but only in the absence of hemodynamic instability.
C. Primary repair should be performed with placement of an intra-abdominal drain next to the repair.
D. Primary repair should be performed and intravenous antibiotics administered for 14 days.
E. The patient should undergo a 2-stage procedure with resection of the injured portion and reanastomosis 48 hours later when clinically stabilized.

97. A 34-year-old prostitute with a history of long-term intravenous drug use is admitted with a 48-hour history of pain in her left arm. She is tachycardic to 130 and her systolic blood pressure is 80 mm Hg. Physical examination is remarkable for crepitus surrounding needle track marks in the antecubital space with a serous exudate. The plain x-ray of the arm is shown here. Which of the following is the most appropriate next step in her management?
A. Treatment with penicillin G and close observation
B. MRI of the arm
C. CT scan of the arm
D. Surgical exploration and debridement
E. Hyperbaric oxygen therapy
98. A 47-year-old man is extricated from an automobile after a motor vehicle accident. He is hypotensive with a systolic blood pressure of 80. The patient has a steering wheelbruise on the anterior chest. His electrocardiogram (ECG) shows some premature ventricular complexes, and his cardiac isoenzymes are elevated. Which of the following is the best next test for evaluation for a blunt cardiac injury?
A. Measurement of serial creatinine phosphokinase and creatinine kinase (including the myocardial band) levels
B. Thallium stress test
C. Echocardiography
D. Single photon emission computed tomography (SPECT)
E. Multiple acquisition scans (MUGA)
99. A 70-year-old man presents to the ER with severalfractures and a ruptured spleen after falling 20 ft. Which of the following will occur in response to the injury?
A. Decreased liver gluconeogenesis
B. Inhibition of skeletal muscle breakdown by interleukin 1 and tumor necrosis factor (TNF, cachectin)
C. Decreased urinary nitrogen loss
D. Hepatic synthesis of acute-phase reactants
E. Decreased glutamine consumption by fibroblasts, lymphocytes, and intestinal epithelial cells
100. A 36-year-old man sustains a gunshot wound to the left buttock. He is hemodynamically stable. There is no exit wound, and an x-ray of the abdomen shows the bullet to be located in the right lower quadrant. Which of the following is most appropriate in the management of his suspected rectal injury?
A. Bariumstudiesofthecolonandrectum
B. Barium studies of the bullet track
C. CT scan of the abdomen and pelvis
D. Angiography
E. Sigmoidoscopy in the ER
101. A 27-year-old man presents to the ER after a high-speed motor vehicle collision with chest pain and marked respiratory distress. On physical examination, he is hypotensive with distended neck veins and absence of breath sounds in the left chest. Which of the following is the proper initial treatment?
A. Intubation
B. Chest x-ray
C. Pericardiocentesis
D. Chest decompression with a needle
E. Emergent thoracotomy
102. A 48-year-old man sustains a gunshot wound to the right upper thigh just distal to the inguinal crease. He is immediately brought to the ER. Peripheral pulses are palpable in the foot, but the foot is pale, cool, and hypesthetic. The motor examination is normal. Which of the following statements is the most appropriate next step in the patient’s management?
A. The patient should be taken to the operating room immediately to evaluate for a significant arterial injury.
B. A neurosurgical consult should be obtained and somatosensory evoked potential monitoring performed.
C. A fasciotomy should be performed prophylactically in the emergency room.
D. A duplex examination should be obtained to rule out a venous injury.
E. The patient should be observed for at least 6 hours and then reexamined for changes in the physical examination.
103. A 62-year-old woman is seen after a 3-day history of fever, abdominal pain, nausea, and anorexia. She has not urinated for 24 hours. She has a history of previous abdominal surgery for inflammatory bowel disease. Her blood pressure is 85/64 mm Hg, and her pulse is 136. Her response to this physiologic state includes which of the following?
A. Increase in sodium and water excretion
B. Increase in renal perfusion
C. Decrease in cortisol levels
D. Hyperkalemia
Hypoglycemia
104. A 20-year-old man presents after being punched in the right eye and assaulted to the head. On a facial CT scan, he is noted to have a blowout fracture of the right orbital floor. Which of the following findings mandates immediate surgical intervention?
A. A fracture 25% of the orbital floor
B. 1 mm of enophthalmos
C. Periorbital ecchymosis
D. Inability to move the right eye upward
E. Traumatic optic neuropathy
105. A 33-year-old woman is seen in the ER with severe rectalbleeding. She has a history of ulcerative colitis. Her blood pressure is 78/56 mm Hg, her pulse is 144, and she is pale and clammy. Which of the following responses is likely to occur after administration of Ringer lactate solution?
A. Increase in serum lactate concentration
B. Impairment of liver function
C. Improvement in hemodynamics by alleviating the deficit in the interstitial fluid compartment
D. Increase in metabolic acidosis
E. Increase in the need for blood transfusion
106. An 18-year-old high school football player is kicked in the left flank. Three hours later he develops hematuria. His vital signs are stable. A CT scan demonstrates a grade II renal injury based on the Urologic Injury Scale of the American Association for the Surgery of Trauma. Which of the following is the most appropriate treatment for this patient?
A. Resumption of normal daily activity excluding sports
B. Exploration and suture of the laceration
C. Exploration and wedge resection of the left kidney
D. Nephrostomy
E. Strict bed rest with serial hemoglobin levels
107. A 32-year-old man is in a high-speed motorcycle collision and presents with an obvious pelvic fracture. On examination, he has a scrotal hematoma and blood at his urethral meatus. Which of the following is the most appropriate next step in his management?
A. Placement of a Foley catheter
B. Cystoscopy
C. CT of the pelvis
D. Retrograde urethrogram
E. Nephrostomy tube placement
108. A 17-year-old adolescent boy sustains a small-caliber gunshot wound to the mid-epigastrium with no obvious exit wound. His abdomen is very tender; he is taken to the operating room and the bullet appears to have tracked through the stomach, distal pancreas, and spleen. The duct appears to have been injured. Which of the following is the best strategy for the management of this patient’s pancreatic injury?
A. Drainage alone
B. Roux-en-Y pancreaticojejunostomy
C. Pancreaticoduodenectomy
D. Frey procedure
E. Distal pancreatectomy
109. A 22-year-old woman who is 4 months pregnant presents after a motor vehicle collision complaining of abdominal pain and right leg pain. She has an obvious deformity of her right femur. She is hemodynamically stable. Which of the following is the best next step in her management?
A. Observation with serial abdominal exams
B. Diagnostic peritoneal lavage
C. Plain film of the abdomen with a lead apron as a shield
D. Focused assessment with sonography for trauma (FAST) examination of the abdomen
E. MRI of the abdomen
110. The victim of a motor vehicle accident who was in shock is delivered to your trauma center by a rural ambulance service. On examination, his blood pressure is 80/60 mm Hg and he has an unstable pelvis. X-rays reveal a pelvic fracture. Chest x-ray is normal. FAST examination shows free fluid near the spleen. There are no major extremity deformities noted. A pelvic binder is placed. Which of the following statements is the best next step in the management of this patient?
A. Computed tomography of the chest
B. Computed tomography of the abdomen and pelvis
C. Angiography
D. Diagnostic peritoneal lavage
E. Exploratory laparotomy with pelvic packing
111. A radio transmission is received in your trauma unit stating that a victim of a motor vehicle collision is en route to your ER with no vital signs. The ambulance is 3 minutes away. As you formulate your plan, which of the following situations would constitute an indication for ER thoracotomy?
A. Massive hemothorax following blunt trauma to the chest
B. Blunt trauma to multiple organ systems with obtainable vital signs in the field, but none on arrival in the ER
C. Rapidly deteriorating patient with cardiac tamponade from penetrating thoracic trauma
D. Penetrating thoracic trauma and no signs of life in the field
E. Penetrating abdominal trauma and no signs of life in the field
112. A 22-year-old man sustains a gunshot wound to the abdomen. At exploration, an apparently solitary distal small-bowel injury is treated with resection and primary anastomosis. On postoperative day 7, small-bowel fluid drains through the operative incision. The fascia remains intact. The fistula output is 300 mL/day and there is no evidence of intra-abdominal sepsis. Which of the following is the most appropriate treatment strategy?
A. Early reoperation to close the fistula tract
B. Broad-spectrum antibiotics
C. Total parenteralnutrition
D. Somatostatin to lower fistula output
E. Loperamide to inhibit gut motility
113. A 26-year-old man complains of pelvic pain after a motorcycle collision. Physical and radiologic examinations confirm a pelvic fracture. Urologic workup reveals a normal urethrogram and an extraperitoneal bladder injury. Which of the following is the most appropriate treatment for his bladder injury?
A. Immediate surgical exploration and repair
B. Placement of a permanent suprapubic tube
C. Catheter drainage followed by definitive repair after 2 weeks
D. Catheter drainage for 2 weeks followed by repeat imaging
E. Bilateral nephrostomy tubes
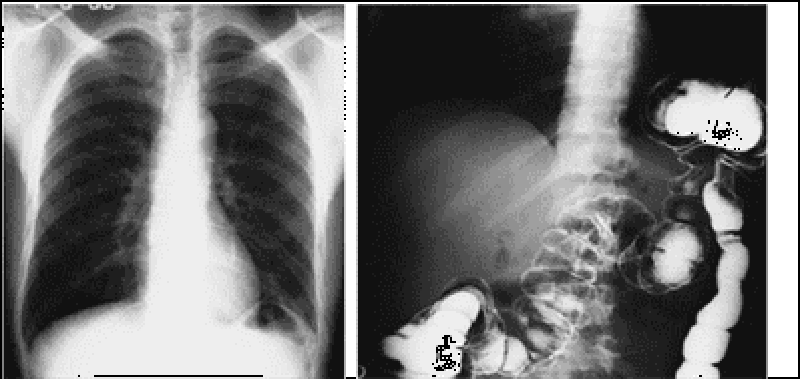
114. The patient shown in this chest x-ray film and contrast study was hospitalized after a car collision 2 days ago in which he suffered blunt trauma to the abdomen. He sustained severalleft rib fractures, but was hemodynamically stable. Which of the following is the appropriate next step in the patient’s management?
A. Observation and serial abdominal exams
B. Immediate left posterolateral thoracotomy and repair of the injury
C. Immediate exploratory laparotomy and repair of the injury
D. Delayed left posterolateral thoracotomy and repair of the injury
E. Delayed exploratory laparotomy and repair of the injury
115. A 56-year-old woman sustains blunt abdominal trauma from an assault. Her blood pressure is 107/56 mm Hg and her pulse is 92. She complains of abdominal pain. She undergoes CT scanning of the abdomen and pelvis, which demonstrates a splenic injury. Which of the following would preclude an attempt at nonoperative management of the patient?
A. Presence of a subcapsular hematoma involving more than 25% of the surface area of the spleen
B. Presence of a subcapsular hematoma involving more than 50% of the surface area of the spleen
C. Evidence of a blush on CT scan
D. A red blood cell (RBC) count of 120,000/μL on diagnostic peritoneal lavage
E. Peritoneal signs on abdominal examination
116. A 49-year-old man was the restrained driver in a motor vehicle collision. He decelerated rapidly in order to avoid hitting another car and swerved into a ditch. He complains of chest pain. Which of the following findings on chest x-ray would be most suspicious for an aortic injury?
A. Multiple right-sided rib fractures
B. A left pulmonary contusion
C. A left pneumothorax
D. Widening of the mediastinum greater than 8 cm
E. Pneumomediastinum
117. A 29-year-old woman was hit by a car while crossing the street. She is hemodynamically unstable with a heart rate of 124 beats per minute and a systolic blood pressure of 82/45 mmHg. The ultrasound machine is broken, and therefore a diagnostic peritoneal lavage (DPL) is performed. Which of the following findings on DPL is an indication for exploratory laparotomy in this patient?
A. Aspiration of 5 cc of gross blood initially
B. Greater than 50,000/μL red blood cells (RBCs)
C. Greater than 100,000/μL RBCs
D. Greater than 100/μL white blood cells (WBCs)
E. Greater than 250/μL WBCs
118. A 27-year-old construction worker falls about 30 ft from a scaffold. At the scene, he complains of inability to move his lower extremities. On arrival in the ER, he has a heart rate of 45 beats per minute and a blood pressure of 78/39 mm Hg. His extremities are warm and pink. His blood pressure improves with 1 L of crystalloid. A central venous catheter is placed for further resuscitation and his central venous pressure is 2 mm Hg. Which of the following is the best initial treatment strategy for improving his blood pressure?
A. Immediate celiotomy
B. Fluid resuscitation with crystalloids
C. Administration of O-negative blood
D. Administration of a peripheral vasoconstrictor
E. Administration of intravenous corticosteroids
119. A 22-year-old man undergoes an exploratory laparotomy after a gunshot wound to the abdomen. The patient has multiple injuries, including a significant liver laceration, multiple small-bowel and colon injuries, and an injury to the infrahepatic vena cava. The patient receives 35 units of packed RBCs, 15 L of crystalloid, 12 units of fresh-frozen plasma (FFP), and a 12 packs of platelets. The patient’s abdomen is packed closed and he is taken to the intensive care unit for further resuscitation. Which of the following warrants a decompressive laparotomy?
A. Increased peak airway pressure
B. Increased cardiac output
C. Decreased systemic vascular resistance
D. Decreased plasma renin and aldosterone
E. Increased cerebralperfusion pressure
120. A 10-year-old girl is the unrestrained backseat passenger in a high-speed motor vehicle collision. She is intubated in the field for unresponsiveness and on presentation to the ER, her heart rate is 160 beats per minute, and her blood pressure is 60/35 mm Hg. She weighs 30 kg. Which of the following is the most appropriate recommendation for her fluid resuscitation?
A. Bolus 1 L of normal saline initially.
B. Bolus 1 L of 5% albumin initially
C. Transfuse 300 cc of packed RBCs initially
D. Bolus 600 cc of normal saline initially. Transfuse if no response
E. Bolus 600 cc of normal saline initially followed by a repeat bolus. Transfuse if no response
121. A 21-year-old woman sustains a stab wound to the middle of the chest. Upon arrival to the ER she has equal breath sounds, blood pressure of 85/46 mm Hg, distended neck veins, and pulsus paradoxus. Which of the following is the most appropriate management of this patient?
A. Emergent intubation and mechanical ventilation in the ER
B. Emergent pericardiocentesis in the ER
C. Emergent thoracotomy in the ER
D. Emergent pericardiocentesis or subxiphoid pericardial drainage after anesthetic induction in the operating room
E. Emergent pericardiocentesis or subxiphoid pericardial drainage under local anesthesia in the operating room.
122. A 58-year-old man presents to the ER after falling 10 ft from a ladder. Examination reveals stable vital signs, no evidence of respiratory distress, and multiple right-sided rib fractures. Chest x-ray shows a hemothorax on the right side and a right tube thoracostomy is performed in the ER. Approximately 700 mL of blood is immediately drained with placement of the thoracostomy tube. Over the next 4 hours he continues to drain 300 mL/h after the original evacuation. Which of the following is the definitive treatment for this patient?
A. Platelets
B. Fresh-frozen plasma
C. Second tube thoracostomy
D. Thoracotomy in the operating room
E. Thoracotomy in the ER
123. A 65-year-old woman is involved in a motor vehicle collision and sustains multiple left-sided rib fractures. Upon presentation to the ER her vital signs are stable and she is in no respiratory distress. Chest x-ray reveals fractures of ribs 4 to 7 on the left side without evidence of hemothorax or pneumothorax. She is admitted for observation and a few hours later she develops shortness of breath. A repeat chest x-ray demonstrates a well- defined infiltrate in her left lung. What is the most likely diagnosis?
A. Pulmonary contusion
B. Pulmonary embolus
C. Pneumonia
D. Myocardial infarction
E. Cardiac tamponade
124. Following a head-on motor vehicle collision, a 21-year-old unrestrained passenger presents to the ER with dyspnea and respiratory distress. She is intubated and physical examination reveals subcutaneous emphysema and decreased breath sounds. Chest x-ray reveals cervical emphysema, pneumomediastinum, and a right-sided pneumothorax. What is the most likely diagnosis?
A. Tension pneumothorax
B. Open pneumothorax
C. Tracheobronchial injury
D. Esophageal injury
E. Pulmonary contusion
125. An intoxicated 22-year-old man is a restrained driver in a high-speed motor vehicle collision. Examination reveals normal vital signs, but the rest of the examination is unreliable secondary to the patient’s intoxicated state from alcohol. Which of the following sole findings on a CT scan of the abdomen and pelvis mandates an exploratory laparotomy?
A. Free fluid in the pelvis
B. Pelvic fracture
C. Liver hematoma
D. Splenic hematoma
E. Renal hematoma
126. A 23-year-old man arrives in the ER after a motor vehicle collision. Examination reveals an unstable pelvis and blood at the urethral meatus. Which of the following studies would most accurately identify a urethral injury?
A. CT scan of the pelvis
B. Intravenous pyelogram
C. Stress cystogram
D. Antegrade urethrogram
E. Retrograde urethrogram
127. A 48-year-old woman develops constipation postoperatively and self-medicates with milk of magnesia. She presents to clinic, at which time her serum electrolytes are checked, and she is noted to have an elevated serum magnesium level. Which of the following represents the earliest clinical indication of hypermagnesemia?
A. Loss of deep tendon reflexes
B. Flaccid paralysis
C. Respiratory arrest
D. Hypotension
E. Stupor
128. Five days after an uneventful cholecystectomy, an asymptomatic middle-aged woman is found to have a serum sodium level of 125 mEq/L. Which of the following is the most appropriate management strategy for this patient?
A. Administration of hypertonic saline solution
B. Restriction of free water
C. Plasma ultrafiltration
D. Hemodialysis
E. Aggressive diuresis with furosemide
129. A 50-year-old patient presents with symptomatic nephrolithiasis. He reports that he underwent a jejunoileal bypass for morbid obesity when he was 39. Which of the following is a complication of jejunoileal bypass?
A. Pseudohyperparathyroidism
B. Hyperuric aciduria
C. Hungry bone syndrome
D. Hyperoxaluria
E. Sporadic unicameral bone cysts
130. Following surgery a patient develops oliguria. You believe the oliguria is due to hypovolemia, but you seek corroborative data before increasing intravenous fluids. Which of the following values supports the diagnosis of hypovolemia?
A. Urine sodium of 28 mEq/L
B. Urine chloride of 15 mEq/L
C. Fractional excretion of sodium less than 1
D. Urine/serum creatinine ratio of 20
E. Urine osmolality of 350 mOsm/kg
131. A 45-year-old woman with Crohn disease and a small intestinal fistula develops tetany during the second week of parenteralnutrition. The laboratory findings include: Na: 135 mEq/L K: 3.2 mEq/L Cl: 103 mEq/L HCO3: 25 mEq/L Ca: 8.2 mEq/L Mg: 1.2 mEq/L PO4: 2.4 mEq/L Albumin: 2.4 An arterial blood gas sample reveals a pH of 7.42, PCO2 of 38 mm Hg, and PO2 of 84 mm Hg. Which of the following is the most likely cause of the patient’s tetany?
A. Hyperventilation
B. Hypocalcemia
C. Hypomagnesemia
D. Essential fatty acid deficiency
E. Focal seizure
132. A patient with a nonobstructing carcinoma of the sigmoid colon is being prepared for elective resection. Which of the following reduces the risk of postoperative infectious complications?
A. A single preoperative parenteraldose of antibiotic effective against aerobes and anaerobes
B. Avoidance of oral antibiotics to prevent emergence of Clostridium difficile
C. Postoperative administration for 48 hours of parenteralantibiotics effective against aerobes and anaerobes
D. Postoperative administration of parenteralantibiotics effective against aerobes and anaerobes until the patient’s intravenous lines and all other drains are removed
E. Redosing of antibiotics in the operating room if the case lasts for more than 2 hours
133. A 75-year-old man with a history of myocardial infarction 2 years ago, peripheral vascular disease with symptoms of claudication after walking half a block, hypertension, and diabetes presents with a large ventral hernia. He wishes to have the hernia repaired. Which of the following is the most appropriate next step in his preoperative workup?
A. He should undergo an electrocardiogram (ECG).
B. He should undergo an exercise stress test.
C. He should undergo coronary artery bypass prior to operative repair of his ventral hernia
D. He should undergo a persantine thallium stress test and echocardiography.
E. His history of a myocardial infarction within 3 years is prohibitive for elective surgery. No further testing is necessary.
134. A previously healthy 55-year-old man undergoes elective right hemicolectomy for a stage I (T2N0M0) cancer of the cecum. His postoperative ileus is somewhat prolonged, and on the fifth postoperative day his nasogastric tube is still in place. Physical examination reveals diminished skin turgor, dry mucous membranes, and orthostatic hypotension. Pertinent laboratory values are as follows: Arterial blood gases: pH 7.56, PCO2 50 mm Hg, PO2 85 mm Hg. Serum electrolytes (mEq/L): Na+ 132, K+ 3.1, Cl- 80; HCO-3 42. Urine electrolytes (mEq/L): Na+ 2, K+ 5, Cl- 6. What is the patient’s acid–base abnormality?
A. Uncompensated metabolic alkalosis
B. Respiratory acidosis with metabolic compensation
C. Combined metabolic and respiratory alkalosis
D. Metabolic alkalosis with respiratory compensation
E. Mixed respiratory acidosis and respiratory alkalosis
135. A 52-year-old man with gastric outlet obstruction secondary to a duodenal ulcer presents with hypochloremic, hypokalemic metabolic alkalosis. Which of the following is the most appropriate therapy for this patient?
A. Infusion of 0.9% NaClwith supplemental KCl until clinical signs of volume depletion are eliminated
B. Infusion of isotonic (0.15 N) HCl via a centralvenous catheter
C. Clamping the nasogastric tube to prevent further acid losses
D. Administration of acetazolamide to promote renal excretion of bicarbonate
E. Intubation and controlled hypoventilation on a volume-cycled ventilator to further increase PCO2
136. A 23-year-old woman is brought to the emergency room from a halfway house, where she apparently swallowed a handful of pills. The patient complains of shortness of breath and tinnitus, but refuses to identify the pills she ingested. Pertinent laboratory values are as follows: Arterial blood gases: pH 7.45, PCO2 12 mm Hg, PO2 126 mm Hg. Serum electrolytes (mEq/L): Na+ 138, K+ 4.8, Cl− 102, HCO3− 8. An overdose of which of the following drugs would be most likely to cause the acid–base disturbance in this patient?
A. Phenformin
B. Aspirin
C. Barbiturates
D. Methanol
E. Diazepam (Valium)
137. An 18-year-old previously healthy man is placed on intravenous heparin after having a pulmonary embolism (PE) after exploratory laparotomy for a small-bowel injury following a motor vehicle collision. Five days later, his platelet count is 90,000/μL and continues to fall over the next severaldays. The patient’s serum is positive for antibodies to the heparin-platelet factor complexes. Which of the following is the most appropriate next management step?
A. Cessation of all anticoagulation therapy
B. Cessation of heparin and immediate institution of high-dose warfarin therapy
C. Cessation of heparin and institution of low-molecular-weight heparin
D. Cessation of heparin and institution of lepirudin
E. Cessation of heparin and transfusion with platelets
138. A 65-year-old man undergoes a technically difficult abdominal–perineal resection for a rectalcancer during which he receives 3 units of packed red blood cells. Four hours later, in the intensive care unit (ICU), he is bleeding heavily from his perineal wound. Emergency coagulation studies reveal normal prothrombin, partial thromboplastin, and bleeding times. The fibrin degradation products are not elevated, but the serum fibrinogen content is depressed and the platelet count is 70,000/μL. Which of the following is the most likely cause of his bleeding?
A. Delayed blood transfusion reaction
B. Auto-immune fibrinolysis
C. A bleeding blood vessel in the surgical field
D. Factor VIII deficiency
E. Hypothermic coagulopathy
139. A 78-year-old man with a history of coronary artery disease and an asymptomatic reducible inguinal hernia requests an elective hernia repair. Which of the following would be a valid reason for delaying the proposed surgery?
A. Coronary artery bypass surgery 3 months earlier
B. A history of cigarette smoking
C. Jugular venous distension
D. Hypertension
E. Hyperlipidemia
140. A 68-year-old man is admitted to the coronary care unit with an acute myocardial infarction. His postinfarction course is marked by congestive heart failure and intermittent hypotension. On the fourth day in hospital, he develops severe midabdominal pain. On physical examination, blood pressure is 90/60 mm Hg and pulse is 110 beats per minute and regular; the abdomen is soft with mild generalized tenderness and distention. Bowel sounds are hypoactive; stool Hematest is positive. Which of the following is the most appropriate next step in this patient’s management?
A. Barium enema
B. Upper gastrointestinal series
C. Angiography
D. Ultrasonography
E. Celiotomy
141. A 30-year-old woman in her last trimester of pregnancy suddenly develops massive swelling of the left lower extremity. Which of the following would be the most appropriate workup and treatment at this time?
A. Venography and heparin
B. Duplex ultrasonography and heparin
C. Duplex ultrasonography, heparin, and vena caval filter
D. Duplex ultrasonography, heparin, warfarin (Coumadin)
E. Impedance plethysmography, warfarin
142. A 20-year-old woman with a family history of von Willebrand disease is found to have an activated partial thromboplastin time (aPTT) of 78 (normal = 32) on routine testing prior to cholecystectomy. Further investigation reveals a prothrombin time (PT) of 13 (normal = 12), a platelet count of 350,000/mm3, and an abnormal bleeding time. Which of the following should be administered in the perioperative period?
A. Factor VIII
B. Platelets
C. Vitamin K
D. Aminocaproic acid
Desmopressin (DDAVP)
143. A 65-year-old man undergoes a low anterior resection for rectalcancer. On the fifth day in hospital, his physical examination shows a temperature of 39°C (102°F), blood pressure of 150/90 mm Hg, pulse of 110 beats per minute and regular, and respiratory rate of 28 breaths per minute. A computed tomography (CT) scan of the abdomen reveals an abscess in the pelvis. Which of the following most accurately describes his present condition?
Systemic inflammatory response syndrome (SIRS)
B. Sepsis
C. Severe sepsis
D. Septic shock
E. Severe septic shock
144. A victim of blunt abdominal trauma has splenic and liver lacerations as well as an unstable pelvic fracture. He is hypotensive and tachycardic with a heart rate of 150 despite receiving 2 L of crystalloid en route to the hospital. He was intubated prior to arrival due to declining mental status. He is taken emergently to the operating room for exploratory laparotomy and external fixation of his pelvic fracture. Which of the following is the best resuscitative strategy?
A. Infusion of another liter of crystalloid
B. Infusion of 500 mL of 5% albumin
C. Infusion of packed red blood cells followed by fresh-frozen plasma and platelets as indicated by the PT and platelet counts on laboratory values
D. Infusion of packed red blood cells and early administration of fresh-frozen plasma and platelets prior to return of laboratory values
E. Infusion of packed red blood cells and vitamin K
145. A 62-year-old woman undergoes a pancreaticoduodenectomy for a pancreatic head cancer. A jejunostomy is placed to facilitate nutritional repletion as she is expected to have a prolonged recovery. What is the best method for delivering postoperative nutrition?
A. Institution of enteralfeeding via the jejunostomy tube after return of bowel function as evidenced by passage of flatus or a bowel movement
B. Institution of enteralfeeding via the jejunostomy tube within 24 hours postoperatively
C. Institution of supplemental enteralfeeding via the jejunostomy tube only if oral intake is inadequate after return of bowel function
D. Institution of a combination of immediate trophic (15 mL/h) enteral feeds via the jejunostomy tube and parenteralnutrition to provide total nutritional support
A. Complete nutritional support with total parenteralnutrition
146. A 65-year-old woman has a life-threatening pulmonary embolus 5 days following removal of a uterine malignancy. She is immediately heparinized and maintained in good therapeutic range for the next 3 days, then passes gross blood from her vagina and develops tachycardia, hypotension, and oliguria. Following resuscitation, an abdominal CT scan reveals a major retroperitoneal hematoma. Which of the following is the best next step in management?
A. Immediately reverse heparin by a calculated dose of protamine and place a vena caval filter (eg, a Greenfield filter).
B. Reverse heparin with protamine, explore and evacuate the hematoma, and ligate the vena cava below the renal veins.
C. Switch to low-dose heparin
D. Stop heparin and observe closely
E. Stop heparin, give fresh-frozen plasma (FFP), and begin warfarin therapy.
147. A 71-year-old man develops dysphagia for both solids and liquids and weight loss of 60 lb over the past 6 months. He undergoes endoscopy, demonstrating a distal esophageal lesion, and biopsies are consistent with squamous cell carcinoma. He is scheduled for neoadjuvant chemoradiation followed by an esophagectomy. Preoperatively he is started on total parenteralnutrition, given his severe malnutrition reflected by an albumin of less than 1. Which of the following is most likely to be a concern initially in starting total parenteral nutrition in this patient?
A. Hyperkalemia
B. Hypermagnesemia
C. Hypoglycemia
D. Hypophosphatemia
E. Hypochloremia
148. An elderly diabetic woman with chronic steroid-dependent bronchospasm has an ileocolectomy for a perforated cecum. She is taken to the ICU intubated and is maintained on broad-spectrum antibiotics, renal dose dopamine, and a rapid steroid taper. On postoperative day 2, she develops a fever of 39.2°C (102.5°F), hypotension, lethargy, and laboratory values remarkable for hypoglycemia and hyperkalemia. Which of the following is the most likely explanation for her deterioration?
A. Sepsis
B. Hypovolemia
C. Adrenal insufficiency
D. Acute tubular necrosis
E. Diabetic ketoacidosis
149. A cirrhotic patient with abnormal coagulation studies due to hepatic synthetic dysfun
A. The day before surgery
B. The night before surgery
C. On call to surgery
D. Intraoperatively
E. In the recovery room
150. On postoperative day 5, an otherwise healthy 55-year-old man recovering from a partial hepatectomy is noted to have a fever of 38.6°C (101.5°F). Which of the following is the most common nosocomial infection postoperatively?
A. Wound infection
B. Pneumonia
C. Urinary tract infection
D. Intra-abdominal abscess
E. Intravenous catheter-related infection
151. Ten days after an exploratory laparotomy and lysis of adhesions, a patient, who previously underwent a low anterior resection for rectalcancer followed by postoperative chemoradiation, is noted to have succus draining from the wound. She appears to have adequate source control—she is afebrile with a normal white blood count. The output from the fistula is approximately 150 cc per day. Which of the following factors is most likely to prevent closure of the enterocutaneous fistula?
A. Previous radiation
B. Previous chemotherapy
C. Recent surgery
D. History of malignancy
E. More than 100-cc output per day
152. A 26-year-old man is resuscitated with packed red blood cells following a motor vehicle collision complicated by a fractured pelvis and resultant hemorrhage. A few hours later the patient becomes hypotensive with a normal centralvenous pressure (CVP), oliguric, and febrile. Upon examination, the patient is noted to have profuse oozing of blood from his intravenous (IV) sites. Which of the following is the most likely diagnosis?
A. Hypovolemic shock
B. Acute adrenalinsufficiency
C. Gram-negative bacteremia
D. Transfusion
E. Ureteralobstruction
153. A 16-year-old adolescent boy with a history of severe hemophilia A is undergoing an elective inguinal hernia repair. Which of the following is the best option for preventing or treating a bleeding complication in the setting of this disease?
A. Fresh-frozen plasma
B. Combination of desmopressin and fresh-frozen plasma
C. DDAVP
D. Combination of ε-aminocaproic acid and desmopressin
E. Factor IX concentrate
154. A 59-year-old man is planning to undergo a coronary artery bypass. He has osteoarthritis and consumes nonsteroidal anti-inflammatory drugs (NSAIDs) for the pain. Which of the following is the most appropriate treatment prior to surgery to minimize his risk of bleeding from his NSAID use?
A. Begin vitamin K 1 week prior to surgery.
B. Give FFP few hours before surgery.
C. Stop the NSAIDs 1 week prior to surgery
D. Stop the NSAIDs 3 to 4 days prior to surgery.
E. Stop the NSAIDs the day before surgery
155. A 63-year-old man undergoes a partial gastrectomy with Billroth II reconstruction for intractable peptic ulcer disease. He presents severalmonths postoperatively with a megaloblastic anemia. Which of the following is the best treatment for this surgical complication?
A. Transfusion with 1 unit of packed red blood cells
B. Oraliron supplementation
C. Oral vitamin B 12 supplementation
D. Intravenous vitamin B12 (cyanocobalamin) supplementation
E. Oral folate supplementation
156. A 52-year-old woman undergoes a sigmoid resection with primary anastomosis for recurrent diverticulitis. She returns to the emergency room 10 days later with left flank pain and decreased urine output; laboratory examination is significant for a white blood cell (WBC) count of 20,000/mm3. She undergoes a CT scan that demonstrates new left hydronephrosis, but no evidence of an intra-abdominal abscess. Which of the following is the most appropriate next step in management?
A. Intravenous pyelogram
B. Intravenous antibiotics and repeat CT in 1 week
C. Administration of intravenous methylene blue
D. No further management if urinalysis is negative for hematuria
E. Immediate reexploration
157. A 23-year-old woman undergoes total thyroidectomy for carcinoma of the thyroid gland. On the second postoperative day, she begins to complain of a tingling sensation in her hands. She appears quite anxious and later complains of muscle cramps. Which of the following is the most appropriate initial management strategy?
A. 10 mL of 10% magnesium sulfate intravenously
B. Oralvitamin D
C. 100 μg oral Synthroid
D. Continuous infusion of calcium gluconate
E. Oral calcium gluconate
158. A 65-year-old man has an enterocutaneous fistula originating in the jejunum secondary to inflammatory bowel disease. Which of the following would be the most appropriate fluid for replacement of his enteric losses?
A. D5W
B. 3% normal saline
C. Ringer lactate solution
D. 0.9% sodium chloride
E. 6% sodium bicarbonate solution
159. A 62-year-old man is suffering from arrhythmias on the night of his triple coronary bypass. Potassium has been administered. His urine output is 20 to 30 mL/h. Serum potassium level is 6.2. Which of the following medications counteracts the effects of potassium without reducing the serum potassium level?
A. Sodium polystyrene sulfonate (Kayexalate)
B. Sodium bicarbonate
C. 50% dextrose
D. Calcium gluconate
E. Insulin
160. An in-hospital workup of a 78-year-old hypertensive, mildly asthmatic man who is receiving chemotherapy for colon cancer reveals symptomatic gallstones. Preoperative laboratory results are notable for a hematocrit of 24% and urinalysis with 18 to 25 WBCs and gram-negative bacteria. On call to the operating room, the patient receives intravenous penicillin. His abdomen is shaved in the operating room. An open cholecystectomy is performed and, despite a lack of indications, the common bile duct is explored. The wound is closed primarily with a Penrose drain exiting a separate stab wound. On postoperative day 3, the patient develops a wound infection. Which of the following changes in the care of this patient could have decreased the chance of a postoperative wound infection?
A. Increasing the length of the preoperative hospital stay to prophylactically treat the asthma with steroids
B. Treating the urinary infection prior to surgery
C. Shaving the abdomen the night prior to surgery
D. Continuing the prophylactic antibiotics for 3 postoperative days
E. Using a closed drainage system brought out through the operative incision
161. A 72-year-old man undergoes a subtotal colectomy for a cecalperforation due to a sigmoid colon obstruction. He has had a prolonged recovery and has been on total parenteralnutrition (TPN) for 2 weeks postoperatively. After regaining bowel fun
A. Zinc
B. selenium
C. Molybdenum
D. Chromium
E. Thiamine
162. A 12-year-old boy with a femur fracture after a motor vehicle collision undergoes operative repair. After induction of anesthesia, he develops a fever of 40°C (104°F), shaking rigors, and blood-tinged urine. Which of the following is the best treatment option?
A. Alkalinization of the urine, administration of mannitol, and continuation with the procedure
B. Administration of dantrolene sodium and continuation with the procedure
C. Administration of dantrolene sodium and termination of the procedure
D. Administration of intravenous steroids and an antihistamine agent with continuation of the procedure
E. Administration of intravenous steroids and an antihistamine agent with termination of the procedure
163. A 24-year-old Jehovah’s Witness who was in a high-speed motorcycle collision undergoes emergent splenectomy. His estimated blood loss was 1500 mL. Which of the following strategy should be employed for his resuscitation?
A. Vasopressors should be primarily utilized for maintenance of his blood pressure.
B. Synthetic colloids should be administered as the primary resuscitation fluid in a 3:1 ratio to replace the volume of blood lost.
C. 0.9% normal saline should be administered in a 1:1 ratio to replace the volume of blood lost.
D. 0.45% normal saline should be administered in a 3:1 ratio to replace the volume of blood lost
E. Lactated Ringer solution should be administered in a ratio of 3:1 to replace the blood lost.
164. A 60-kg, 53-year-old man with no significant medical problems undergoes lysis of adhesions for a small-bowel obstruction. Postoperatively, he has high nasogastric output and low urine output. What is the most appropriate management of his fluids?
A. Infusion of D5 0.45% normal saline at 100 mL/h
B. Infusion of D5 0.9% normal saline at 100 mL/h
C. Infusion of D5 lactated Ringer at 100 mL/h
D. Replacement of nasogastric tube losses with lactated Ringer in addition to maintenance fluids
E. Replacement of nasogastric tube losses with 0.45% normal saline with 20 mEq/L of potassium chloride in addition to maintenance fluids
165. Four days after surgical evacuation of an acute subdural hematoma, a 44-year-old man becomes mildly lethargic and develops asterixis. He has received 2400 mL of 5% dextrose in water intravenously each day since surgery, and he appears well hydrated. Pertinent laboratory values are as follows: Serum electrolytes (mEq/L): Na+ 118, K+ 3.4, Cl− 82, HCO3− 24 Serum osmolality: 242 mOsm/L Urine sodium: 47 mEq/L Urine osmolality: 486 mOsm/L Which of the following is the best treatment of his hyponatremia?
A. Insulin infusion to keep his glucose level less than 110 mg/dL
B. Slow infusion of 3% normal saline until neurologic symptoms are improved
C. Rapid infusion of 3% normal saline to correct the sodium to norma
D. Desmopressin (DDAVP) administration
E. Administration of a loop diuretic
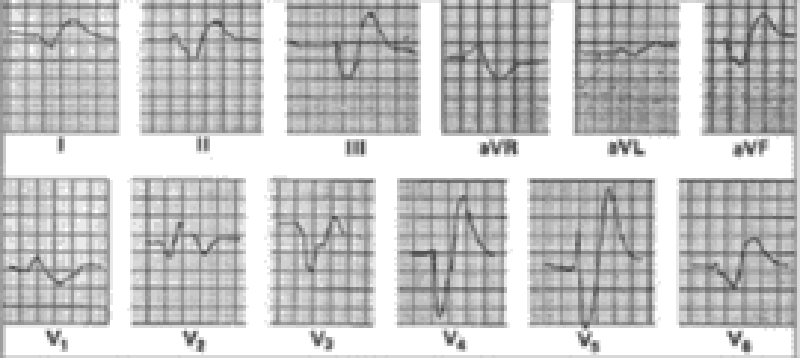
166. A 43-year-old woman develops acute renal failure following an emergency resection of a leaking abdominal aortic aneurysm. One week after surgery, the following laboratory values are obtained: Serum electrolytes (mEq/L): Na+ 127, K+ 5.9, Cl− 92, HCO3− 15 Blood urea nitrogen: 82 mg/dL Serum creatinine: 6.7 mg/dL The patient has gained 4 kg since surgery and is mildly dyspneic at rest. Eight hours after these values are reported, the following electrocardiogram is obtained. Which of the following is the most appropriate initial treatment in the management of this patient?
A. 10 mL of 10% calcium gluconate
B. 0.25 mg digoxin every 3 hours for 3 doses
C. Oral Kayexalate
D. 100 mg lidocaine
E. Emergent hemodialysis
167. A 63-year-old man with a 40-pack per year smoking history undergoes a low anterior resection for rectalcancer and on postoperative day 5 develops a fever, new infiltrate on chest x-ray, and leukocytosis. He is transferred to the ICU for treatment of his pneumonia because of clinical deterioration. Which of the following is a sign of early sepsis?
A. Respiratory acidosis
B. Decreased cardiac output
C. Hypoglycemia
D. Increased arteriovenous oxygen difference
E. Peripheral vasodilation
168. A 60-year-old woman with no previous medical problems undergoes a total colectomy with diverting ileostomy for a cecalperforation secondary to a sigmoid stricture. Postoperatively, she has 2 L of ileostomy output per day. Her heart rate is 110 beats per minute, her respiratory rate is 24 breaths per minute, and her oxygen saturation is 98% on 2-L nasalcannula (NC). Her hemoglobin levels have been stable postoperatively at 9.0 mg/dL. Her other laboratory values on postoperative day 6 are as follows: Na+: 128 K+: 3.0 Cl−: 102 HCO3-: 20 Which of the following statements is the best strategy for correcting her acid–base disorder?
A. Her maintenance fluids should be changed to 0.9% normal saline with 20 mEq/L of potassium chloride.
B. She should be intubated to correct her tachypnea and prevent respiratory alkalosis
C. She should be transfused 2 units of packed red blood cells
D. She should be treated with fluid replacement and stool-bulking agents.
E. She should undergo immediate dialysis.
169. A 39-year-old man is undergoing resuscitation with blood products for an upper GI bleed. He is suspected of having a hemolytic transfusion reaction. Which of the following is appropriate in the management of this patient?
A. Removal of nonessential foreign body irritants, for example, Foley catheter
B. Fluid restriction
C. 0.1 M HCl infusion
D. Steroids
E. Fluids and mannitol
170. A 45-year-old woman undergoes an uneventful laparoscopic cholecystectomy for which she receives 1 dose of cephalosporin. One week later, she returns to the emergency room with fever, nausea, and copious diarrhea and is suspected of having pseudomembranous colitis. She is afebrile and has no peritoneal signs on abdominal examination. She has a mild leukocytosis with a left shift. Which of the following is the appropriate initial management strategy?
A. Administration of an antidiarrheal agent
B. Exploratory laparotomy with left hemi-colectomy and colostomy
C. Exploratory laparotomy with subtotal abdominal colectomy and ileostomy
D. Administration of intravenous vancomycin
E. Administration of oral metronidazole
171. A 42-year-old man sustains a gunshot wound to the abdomen and is in shock. Multiple units of packed red blood cells are transfused in an effort to resuscitate him. He complains of numbness around his mouth and displays carpopedal spasm. An electrocardiogram demonstrates a prolonged QT interval. Which of the following is the most appropriate treatment?
A. Intravenous bicarbonate
B. Intravenous potassium
C. Intravenous calcium
D. Intravenous digoxin
E. Intravenous parathyroid hormone
172. A 75-year-old thin cachectic woman undergoes a tracheostomy for failure to wean from the ventilator. One week later, she develops significant bleeding from the tracheostomy. Which of the following would be an appropriate initial step in the management of this problem?
A. Remove the tracheostomy and place pressure over the wound
B. Deflate the balloon cuff on the tracheostomy
C. Attempt to reintubate the patient with an endotracheal tube
D. Upsize the tracheostomy
E. Perform fiberoptic evaluation immediately
173. A 53-year-old woman has been intubated for severaldays after sustaining a right pulmonary contusion after a motor vehicle collision as well as multiple rib fractures. Which of the following is a reasonable indication to attempt extubation?
A. Negative inspiratory force (NIF) of –15 cm H2O
B. PO2 of 60 mm Hg while breathing 30% inspired FiO2 with a positive end-expiratory pressure (PEEP) of 10 cm H2O
C. Spontaneous respiratory rate of 35 breaths per minute
D. A rapid shallow breathing index of 80
E. Minute ventilation of 18 L/min
174. A 19-year-old man receives un-cross-matched blood during resuscitation after a gunshot wound to the abdomen. He develops fever, tachycardia, and oliguria during the transfusion and is diagnosed as having a hemolytic reaction. Which of the following is the most appropriate next step in the management of this patient?
A. Administration of a loop diuretic such as furosemide
B. Treating anuria with fluid and potassium replacement
C. Acidifying the urine to prevent hemoglobin precipitation in the renal tubules
D. Removing foreign bodies, such as Foley catheters, which may cause hemorrhagic complications
E. Stopping the transfusion immediately
175. A 74-year-old woman with a history of a previous total abdominal hysterectomy presents with abdominal pain and distention for 3 days. She is noted on plain films to have dilated small-bowel and air-fluid levels. She is taken to the operating room for a small-bowel obstruction. Which of the following inhalational anesthetics should be avoided because of accumulation in air-filled cavities during general anesthesia?
A. Diethyl ether
B. Nitrous oxide
C. Halothane
D. Methoxyflurane
E. Trichloroethylene
176. A 61-year-old alcoholic man presents with severe epigastric pain radiating to his back. His amylase and lipase are elevated, and he is diagnosed with acute pancreatitis. Over the first 48 hours, he is determined to have 6 Ranson’s criteria, including a PaO2 less than 60 mm Hg. His chest x-ray reveals bilateral pulmonary infiltrates, and his wedge pressure is low. Which of the following criteria must be met to make a diagnosis of adult respiratory distress syndrome (ARDS)?
A. Hypoxemia defined as a PaO2 /FiO2 ratio of less than 200
B. Hypoxemia defined as a PaO2 of less than 60 mm Hg
C. A pulmonary capillary wedge pressure greater than 18 mm Hg
D. Lack of improvement in oxygenation with administration of a test dose of furosemide
E. Resence of a focal infiltrate on chest x-ray
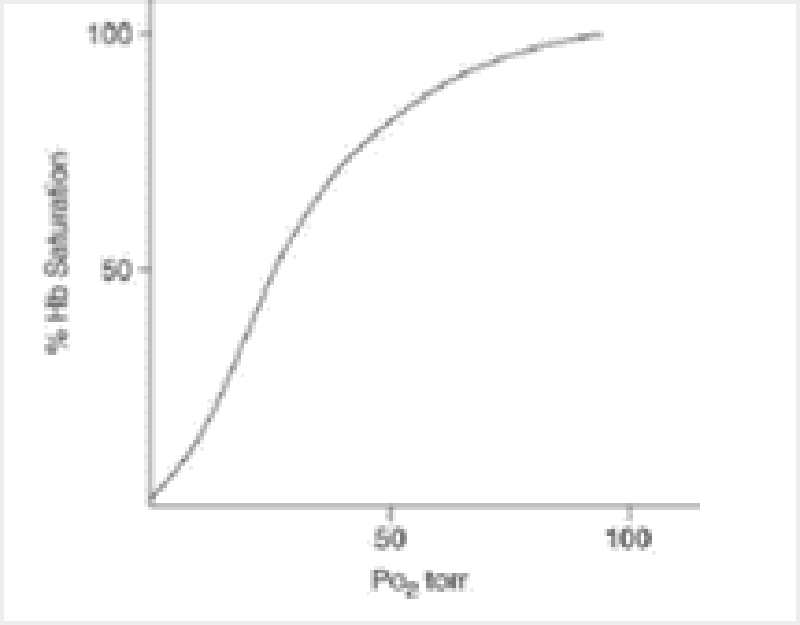
177. A 50-year-old man has respiratory failure due to pneumonia and sepsis after undergoing splenectomy for a traumatic injury. Which of the following management strategies will improve tissue oxygen uptake (ie, shifting the oxygen dissociation curve, depicted here, to the right)?
A. Transfusion of banked blood to correct acute anemia
B. Correction of acute anemia with erythropoietic stimulating agent
C. Administration of bicarbonate to promote metabolic alkalosis
D. Hypoventilation to increase the PaCO2
E. Administration of an antipyretic to lower the patient’s temperature
178. A 64-year-old man with history of severe emphysema is admitted for hematemesis. The bleeding ceases soon after admission, but the patient becomes confused and agitated. Arterial blood gases are as follows: pH 7.23; PO2 42 mm Hg; PCO2 75 mm Hg. Which of the following is the best initial therapy for this patient?
A. Correct hypoxemia with high-flow nasal O2
B. Correct acidosis with sodium bicarbonate
C. Administer 10 mg intravenous dexamethasone
D. Administer 2 mg intravenous Ativan
E. Intubate the patient
179. A 62-year-old woman with a history of coronary artery disease presents with a pancreatic head tumor and undergoes a pancreaticoduodenectomy. Postoperatively, she develops a leak from the pancreaticojejunostomy anastomosis and becomes septic. A Swan-Ganz catheter is placed, which demonstrates an increased cardiac output and decreased systemic vascular resistance. She also develops acute renal failure and oliguria. Which of the following is an indication to start dopamine?
A. To increase splanchnic flow
B. To increase coronary flow
C. To decrease heart rate
D. To lower peripheral vascular resistance
E. To inhibit catecholamine release
180. A 29-year-old woman on oral contraceptives presents with abdominal pain. A computed tomography (CT) scan of the abdomen demonstrates a large hematoma of the right liver with the suggestion of an underlying liver lesion. Her hemoglobin is 6, and she is transfused 2 units of packed red blood cells and 2 units of fresh frozen plasma. Two hours after starting the transfusion, she develops respiratory distress and requires intubation. She is not volume overloaded clinically, but her chest x-ray shows bilateral pulmonary infiltrates. Which of the following is the management strategy of choice?
A. Continue the transfusion and administer an antihistamine
B. Stop the transfusion and administer a diuretic
C. Stop the transfusion, perform bronchoscopy, and start broad-spectrum empiric antibiotics
D. Stop the transfusion and continue supportive respiratory care
E. Stop the transfusion and send a Coombs test
181. A 68-year-old hypertensive man undergoes successfulrepair of a ruptured abdominal aortic aneurysm. He receives 9 L Ringer lactate solution and 4 units of whole blood during the operation. Two hours after transfer to the surgical intensive care unit, the following hemodynamic parameters are obtained: systemic blood pressure (BP) 90/60 mm Hg, pulse 110 beats per minute, centralvenous pressure (CVP) 7 mm Hg, pulmonary artery pressure 28/10 mm Hg, pulmonary capillary wedge pressure (PCWP) 8 mm Hg, cardiac output 1.9 L/min, systemic vascular resistance 1400 (dyne.s)/cm5 (normal is 900-1300), PaO2 140 mm Hg (FiO2: 0.45), urine output 15 mL/h (specific gravity: 1.029), and hematocrit 35%. Given this data, which of the following is the most appropriate next step in management?
A. Administration of a diuretic to increase urine output
B. Administration of a vasopressor agent to increase systemic blood pressure
C. Administration of a fluid challenge to increase urine output
D. Administration of a vasodilating agent to decrease elevated systemic vascular resistance
E. A period of observation to obtain more data
182. A 59-year-old man with a history of myocardial infarction 2 years ago undergoes an uneventful aortobifemoral bypass graft for aortoiliac occlusive disease. Six hours later he develops ST segment depression, and a 12-lead electrocardiogram (ECG) shows anterolateral ischemia. His hemodynamic parameters are as follows: systemic BP 70/40 mm Hg, pulse 100 beats per minute, CVP 18 mm Hg, PCWP 25 mm Hg, cardiac output 1.5 L/min, and systemic vascular resistance 1000 (dyne · s)/cm5. Which of the following is the single best pharmacologic intervention for this patient?
A. Sublingual nitroglycerin
B. Intravenous nitroglycerin
C. A short-acting β-blocker
D. Sodium nitroprusside
E. Dobutamine
183. A 56-year-old man undergoes a left upper lobectomy. An epidural catheter is inserted for postoperative pain relief. Ninety minutes after the first dose of epidural morphine, the patient complains of itching and becomes increasingly somnolent. Blood-gas measurement reveals the following: pH 7.24, PaCO2 58, PaO2 100, and HCO3- 28. Which of the following is the most appropriate initial therapy for this patient?
A. Endotracheal intubation
B. Intramuscular diphenhydramine (Benadryl)
C. Epidural naloxone
D. Intravenous naloxone
E. Alternative analgesia
184. A 71-year-old man returns from the operating room (OR) after undergoing a triple coronary bypass. His initial cardiac index is 2.8 L/ (min·m2). Heart rate is then noted to be 55 beats per minute, BP is 110/80 mm Hg, wedge pressure is 15, and his cardiac index has dropped to 1.6 L/(min·m2 ). He has a normal left ventricle. Which of the following maneuvers will increase his cardiac output?
A. Increase his peripheral vascular resistance
B. Increase his CVP
C. Increase his heart rate to 90 by electrical pacing.
D. Increase his blood viscosity
E. Increase his inspired O2 concentration
185. A 73-year-old woman with a long history of heavy smoking undergoes femoral artery-popliteal artery bypass for rest pain in her left leg. Because of serious underlying respiratory insufficiency, she continues to require ventilatory support for 4 days after her operation. As soon as her endotrachealtube is removed, she begins complaining of vague upper abdominal pain. She has daily fever spikes of 39°C (102.2°F) and a leukocyte count of 18,000/mL. An upper abdominal ultrasonogram reveals a dilated gallbladder, but no stones are seen. A presumptive diagnosis of acalculous cholecystitis is made. Which of the following is the next best step in her treatment?
A. Nasogastric suction and broad-spectrum antibiotics
B. Immediate cholecystectomy with operative cholangiogram
C. Percutaneous drainage of the gallbladder
D. Endoscopic retrograde cholangiopancreatography (ERCP) to visualize and drain the common bile duct
E. Provocation of cholecystokinin release by cautious feeding of the patient
186. A 32-year-old man undergoes a distal pancreatectomy, splenectomy, and partial colectomy for a gunshot wound to the left upper quadrant of the abdomen. One week later he develops a shaking chill in conjunction with a temperature spike of 39.4°C (103°F). His blood pressure is 70/40 mm Hg, pulse is 140 beats per minute, and respiratory rate is 45 breaths per minute. He is transferred to the intensive care unit (ICU), where he is intubated and a Swan-Ganz catheter is placed. Which of the following is consistent with the expected initial Swan-Ganz catheter readings?
A. An increase in cardiac output
B. An increase in peripheral vascular resistance
C. An increase in pulmonary artery pressure
D. An increase in PCWP
E. An increase in central venous pressure
187. A 43-year-old trauma patient develops acute respiratory distress syndrome (ARDS) and has difficulty oxygenating despite increased concentrations of inspired O2. After the positive end-expiratory pressure (PEEP) is increased, the patient’s oxygenation improves. What is the mechanism by which this occurs?
A. Decreasing dead-space ventilation
B. Decreasing the minute ventilation requirement
C. Increasing tidal volume
D. Increasing functional residual capacity
E. Redistribution of lung water from the interstitial to the alveolar space
188. A 27-year-old man was assaulted and stabbed on the left side of the chest between the areola and the sternum. He is hemodynamically unstable with jugular venous distention, distant heart sounds, and hypotension. Which of the following findings would be consistent with a diagnosis of hemodynamically significant cardiac tamponade?
A. More than a 10 mm Hg decrease in systolic blood pressure at the end of the expiratory phase of respiration
B. Decreased right atrial pressures on Swan-Ganz monitoring
C. Equalization of pressures across the 4 chambers on Swan-Ganz monitoring
D. Compression of the left ventricle on echocardiography
E. Overfilling of the right atrium
189. A 55-year-old woman requires an abdominoperineal operation for rectalcancer. She has a history of stable angina. Which of the following clinical markers is most likely to predict a cardiac event during her noncardiac surgery and should prompt further cardiac workup prior to her operation?
A. Abnormal electrocardiogram
B. Prior stroke
C. Unstable angin
D. Uncontrolled hypertension
E. Her age
190. A 70-kg woman is to undergo nail removal from her right ring finger in the ambulatory surgery clinic. Which of the following is the most appropriate option for local anesthesia?
A. Digital block with 1% lidocaine without epinephrine up to 4.5 mg/kg
B. Digital block with 1% lidocaine with epinephrine up to 4.5 mg/kg
C. Digital block with 1% lidocaine with epinephrine up to 7 mg/kg
D. Local injection around the nail bed with 1% lidocaine with epinephrine up to 4.5 mg/kg
E. Local injection around the nail bed with 1% lidocaine with epinephrine up to 7 mg/kg/mL
191. A 22-year-old man sustains severe blunt trauma to the back. He notes that he cannot move his lower extremities. He is hypotensive and bradycardic. Which of the following is the best initial management of the patient?
A. Administration of phenylephrine
B. Administration of dopamine
C. Administration of epinephrine
D. Intravenous fluid bolus
E. Placement of a transcutaneous pacer
192. A 58-year-old woman with multiple comorbidities and previous cardiac surgery is in a high-speed motor vehicle collision. She is intubated for airway protection. Because of hemodynamic instability, a central venous catheter is placed in the right subclavian vein. While the surgeon is securing the catheter, the cap becomes displaced and air enters the catheter. Suddenly, the patient becomes tachycardic and hypotensive. What is the best next maneuver?
A. Decompression of the right chest with a needle in the second intercostal space
B. Placement of a right chest tube
C. Withdrawal of the central venous catheter severalcentimeters
D. Placement of the patient in a left lateral decubitus Trendelenburg position
E. Bilateral “clamshell” thoracotomy with aortic cross-clamping
193. A 30-year-old man is scheduled for a laparoscopic cholecystectomy for biliary colic. He reports a family history of prolonged paralysis during general anesthesia. Which of the following medications should be avoided during his procedure?
A. Succinylcholine
B. Vecuronium
C. Pancuronium
D. Halothane
E. Etomidate
194. An 18-year-old woman develops urticaria and wheezing after an injection of intravenous contrast for an abdominal CT scan. Her blood pressure is 120/60 mm Hg, heart rate is 155 beats per minute, and respiratory rate is 30 breaths per minute. Which of the following is the most appropriate immediate therapy?
A. Intubation
B. Epinephrine
C. β-Blockers
D. Iodine
E. Fluid challenge
195. A patient develops a fever and tachycardia during a blood transfusion after a redo coronary artery bypass procedure. The nurse subsequently discovers that there was a mix-up in the cross-match because of a labeling error. Which of the following is diagnostic in a patient with an immediate hemolytic reaction secondary to a blood transfusion?
A. Serum haptoglobin above 50 mg/dL
B. Indirect bilirubin greater than 5 mg/dL
C. Direct bilirubin greater than 5 mg/dL
D. Positive Coombs test
E. Myoglobinuria
196. A 72-year-old man with diabetes, renal insufficiency, and coronary artery disease presents in septic shock from emphysematous cholecystitis. His oxygen saturation is 100% on 6-L nasal cannula and his hemoglobin is 7.2 mg/dL. His mixed venous oxygen saturation is 58%. Which of the following treatment options will improve his oxygen delivery the most?
A. Increase his inspired oxygen concentration
B. Transfer him to a hyperbaric chamber
C. Administer ferrous sulfate
D. Administer an erythropoietic agent
E. Transfuse two units of packed red blood cells 7
197. An obese 50-year-old woman undergoes a laparoscopic cholecystectomy. In the recovery room, she is found to be hypotensive and tachycardic. Her arterial blood gases reveala pH of 7.29, PaO2 of 60 mm Hg, and PaCO2 of 54 mm Hg. Which of the following is the most likely cause of this patient’s problem?
A. Acute pulmonary embolism
B. Carbon dioxide (CO2) absorption from induced pneumoperitoneum
C. Alveolar hypoventilation
D. Pulmonary edema
E. Atelectasis from a high diaphragm
198. A 65-year-old man who had a 25-lb weight loss over the previous 6 months is diagnosed with adenocarcinoma of the distal esophagus. He undergoes a transhiatal esophagectomy complicated by a cervical leak. He is receiving enteral feeds through a jejunostomy tube. After a week, his physicians wish to assess his nutritional resuscitation. Which of the following is the most accurate measure of adequacy of his nutritional support?
A. Urinary nitrogen excretion level
B. Total serum protein level
C. Serum albumin level
D. Serum transferrin level
E. Respiratory quotient
199. A 63-year-old man with multiple rib fractures and a pulmonary contusion requires prolonged intubation. He is unable to be weaned from the ventilator and is on a volume control mode. He has a tracheostomy and a percutaneous gastrotomy in place through which he is being fed. The surgeon orders a respiratory quotient (RQ), which is the ratio of the rate of carbon dioxide production over the rate of oxygen uptake. The RQ is 1. Based on this information, which of the following is the next step in his management?
A. Decrease the inspired concentration of oxygen
B. Decrease the rate on the ventilator
C. Increase the rate on the ventilator
D. Decrease the carbohydrates in his enteralfeeds
E. Increase the total number of calories in his enteral feeds
200. A 22-year-old woman is involved in a major motor vehicle accident and receives a tracheostomy during her hospitalization. Five days after placement of the tracheostomy she has some minor bleeding around the tracheostomy site. Which of the following is the most appropriate immediate therapy?
A. Removal of tracheostomy at bedside.
B. Exchange the tracheostomy at bedside
C. Exchange the tracheostomy in the operating room
D. Bronchoscopic evaluation of the trachea at bedside
E. Bronchoscopic evaluation of the trachea in the operating room.
{"name":"Surgery kb,part 1", "url":"https://www.quiz-maker.com/QPREVIEW","txt":"Challenge your knowledge of surgical procedures and their associated conditions with our comprehensive Surgery Knowledge Quiz. Designed for medical professionals and students alike, this quiz covers a wide range of topics, ensuring you test your understanding of key concepts and clinical situations.Get ready to delve into:Gastrointestinal surgeryComplications of surgical proceduresManagement of surgical casesPreoperative and postoperative care","img":"https:/images/course8.png"}
More Quizzes
Surgery USMLE Part 4
2721360
Surgical Knowledge Challenge
53260
Are you ID, Ego, or Superego?
7435
Golf Blitz/SSG Course Quiz
11624
Am I a Lesbian - Free Orientation Self‑Check
201020251
General Insurance Knowledge - Free Online
201017766
5th Grade Spelling Test - Free Online Practice
201016687
Which Avatar Bender Are You? Take the Free
201019065
Movie Trivia for Teens - Free Online
201020657
Halogens & Noble Gases - Xenon Electron Configuration
201022525
Is My FWB Catching Feelings? Free with Instant Results
201017836
Codon Chart Practice - Translate mRNA to Protein
201015978